In Australia, a study conducted among bereaved and current caregivers for patients with severe COPD showed that > 20% of patients who had died of COPD required hands-on care by their caregivers.11 The caregivers also reported similar concerns as those patients with COPD, which included uncertainty about the future, fear of exacerbations, social isolation, and deteriorating health.11 They also reported competing emotions of loyalty, resentment, guilt, and exhaustion.11 Caregivers identified areas they felt could have improved their ability to provide care, such as availability of adaptive equipment, contingency plans for emergency situations, education on the illness, its symptoms and prognosis, and advance care planning information.11 The caregivers believed that receiving this information might have lessened their stress and plan for the future.11 Although most of the aspects of care that they identified as important are components of palliative care, most of the caregivers were unfamiliar with the term palliative care.11
QI Initiative
To improve palliative care education and use in the ICUs of the VA hospitals, the VHA conducted training, which was made available to intensive care providers on improving EOL care and communication. An attending physician in the ICU who also is a pulmonologist took part in this training in July 2013. To evaluate the outcome of this educational effort, the authors’ reviewed the palliative care referrals from 2012 to 2014.
Results
There were a total of 29 patients with COPD who were referred for palliative care services. Sixteen (55%) were referred by pulmonology. Medical oncology and primary care each referred 4 patients (14%). Acute care referred 5 patients (17%). Emergency department (ED) visits were compared 1 year prior with postpalliative care involvement in the patients’ care (Figure 1). The average ED visit for these patients prepalliative care was 3.2 days, and this dropped to 1.7 days postpalliative care involvement. Of the 29 patients, there were 7 who were never seen in the ED for symptoms of COPD prior to palliative care involvement in their care, and 17 who did not have ED visits after palliative care’s involvement in their care. Of the 29 patients, 3 had frequent visits to the ED (more than 10 days total) prepalliative care, and only 1 had frequent visits to the ED following involvement in the palliative care clinic.
According to the JDDVAMC Managerial Cost Accounting Office (MCAO), the average cost to care for a patient who is presenting to the ED with symptoms related to COPD is $527. The cost of caring for the 22 patients who were seen at least once in the ED for symptoms related to their COPD would be $11,594. With palliative care involvement, only 12 of the 29 patients were seen in the ED for symptoms related to COPD for a total of $6,324, a savings of $5,270 for single ED visits for this set of patients.
Prior to palliative care involvement for the 29 patients, there were 27 admissions, which dropped to 15 admissions after palliative care involvement. According to the MCAO, the average cost to care for a patient who is admitted to the hospital due to an exacerbation of COPD is $20,944. With 27 admissions prior to palliative care involvement, the results total $565,488 compared with $314,160 for 15 admissions with palliative care involvement, showing a cost savings of $251,328.
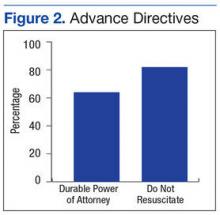
Fourteen of the 29 patients had advance directive discussions, 9 of which were completed by assigning a durable power of attorney and/or completing a living will. There were 22 (76%) of the 29 patients who had code status discussions, and 18 (62%) elected not to be resuscitated (Figure 2). According to MCAO, the average cost to care for a patient in the ICU who required ventilator support for at least 96 hours is $102,175. For the 18 patients who decided not to pursue cardiopulmonary resuscitation, this results in a potential cost savings of $1,839,150.
Conclusion
The outcome of this QI initiative is congruent with the findings published in the literature on the benefits of palliative care involvement in the care of patients with COPD. Palliative care involvement improved goals of care discussions and resulted in decreased ED visits. Palliative care educational outreach also seems to improve palliative care referrals.
[embed:render:related:node:108952]
In 2007, the American Thoracic Society issued a policy statement recommending that palliative care should be available at any stage during the course of a progressive or chronic respiratory disease or critical illness when the patient becomes symptomatic.12 Compared with patients with lung cancer, patients with COPD have to cope with symptom burden for a longer period. Breathlessness seems to be the most debilitating physical symptom for COPD and should trigger a palliative care referral.7 Comprehensive respiratory care similar to that for cancer care should be considered for severe COPD and should involve both the palliative care team and the pulmonary care teams for optimal results.
The results of this QI initiative also seem to support the potential benefits of palliative care involvement in the care of patients with other chronic illnesses that are expected to progress over time, leading to a shortened life expectancy.