In the HAS-BLED bleeding risk score, patients receive 1 point for each component for a maximum score of 9 points. The score is stratified into low (0 points), intermediate (1 to 2 points), and high (≥ 3 points) bleeding risk.4
The HAS-BLED risk factors were obtained from patient chart review, including problem list, laboratory results, and PC CPS anticoagulation notes. Interventions included primary care provider (PCP) notification of elevated BP and offer of BP management by a PC CPS, patient education and/or PCP contact to discontinue concurrent NSAID or addition of a proton pump inhibitor (PPI) based on bleeding risk factor if the NSAID was deemed necessary, and discontinuation of concomitant antiplatelet drug(s) or reduction in aspirin dosage in consultation with patient’s PCP and cardiologist.9 In order to complete the initial HAS-BLED assessment and implement interventions, a note template was developed and entered into the electronic health record (EHR) that identified the patient’s modifiable risk factors.
Once the PCP and cardiologist (if applicable) responded to the note, by either accepting or declining the PC CPS recommendation(s), the HAS-BLED score was recalculated and recorded. If the provider did not respond to the initial note, an attempt was made to follow up at 3 months and at 6 months if necessary. If the provider did not respond at 6 months, the nonresponse was documented. For patients whose PCP requested PC CPS management of BP, the HAS-BLED score was recalculated 6 months after response from the PCP.
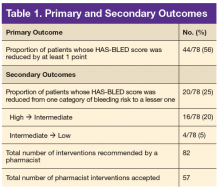
The primary outcome was the proportion of patients whose HAS-BLED score was reduced by at least 1 point. Secondary outcomes included the proportion of patients whose HAS-BLED score was reduced from one category of bleeding risk to a lesser one, total number of pharmacist interventions completed, number of pharmacist interventions made of each type (BP management, NSAID use, or antiplatelet drug use), and PCP acceptance rate.
Results
A total of 897 patients taking warfarin received anticoagulation management by a PC CPS at CJZVAMC in 2015. Of these, 819 patients were excluded based on the exclusion criteria (eFigure).
Reasons for exclusion included: indication other than nonvalvular AF (n = 474), nonvalvular AF and no modifiable risk factors (n = 277), and nonvalvular AF taking an antiplatelet therapy for unstable CAD, acute coronary syndrome within the past year, history of stent placement, carotid endarterectomy, carotid stenosis, or noncardioembolic stroke and no other modifiable risk factors (n = 68).Seventy-eight patients were included in the assessment. Baseline HAS-BLED scores were calculated, and recommendations were made via an EHR progress note to the PCP and cardiologist (if applicable). Recommended interventions in the 78 patients resulted in 44 patients (56%) who experienced reduction in their HAS-BLED score by at least 1 point (Table 1). Twenty patients (25%) saw their HAS-BLED category reduced from a higher level of bleeding risk to a lower risk. The average HAS-BLED score in the 44 patients was 2.38 before intervention and 1.55 after the intervention.
In 10 patients, the HAS-BLED score did not decrease despite accepted PC CPS intervention. Specifically, 7 patients were on both an antiplatelet agent and NSAID. As a result of the pharmacist intervention, the NSAID was discontinued, but the antiplatelet remained because of stent placement or carotid stenosis. In 1 patient, the aspirin dosage was decreased from 325 to 81 mg/d. In 2 patients where NSAID use was deemed necessary—meloxicam in both cases—a PPI was ordered based on bleeding risk.9
A total of 82 interventions were recommended; 57 interventions were accepted, resulting in a provider acceptance rate of 69.5% (Tables 2 and 3). Thirty-five of the accepted interventions (61%) involved discontinuing an antiplatelet (aspirin or clopidogrel) in consultation with the patient’s PCP and cardiologist. Twenty-seven of these patients had no documented CAD, and 8 of the patients had stable CAD. Seventeen (30%) of the accepted recommendations were for discontinuing NSAID therapy, 2 (4%) were for BP management by a PC CPS, 2 (4%) for addition of PPI with continued NSAID use (meloxicam), and 1 (1%) for decreasing aspirin dosage from 325 to 81 mg/d. The NSAIDs that were discontinued included ibuprofen, indomethacin, meloxicam, and naproxen.
Discussion
This project is the first, to the authors’ knowledge, to evaluate pharmacist interventions to reduce modifiable bleeding risk factors identified by the HAS-BLED bleeding risk score. Most of the patients with nonvalvular AF in the PC clinics did not have modifiable bleeding risk factors. However, of the patients who received a recommendation to reduce a specific modifiable risk factor, most of the interventions were accepted by PCPs and cardiologists, and the HAS-BLED score was reduced. Furthermore, many interventions also resulted in reduction of the bleeding risk level.