Statistical Analyses
Data on intervention type and encounter number were evaluated with descriptive statistics. The information was characterized and diagrammed with Excel (Microsoft, Redmond, WA) charts and graphs.
Cost-avoidance calculations were done using previously described methods and are included for exploratory analysis.11,12 Briefly, published estimates of cost avoidance associated with various interventions from the outpatient setting within a VAMC setting were applied as appropriate to the various interventions captured with the PhARMD tool.11,12 These estimates from Lee and colleagues were derived from detailed chart review of interventions made and the potential harm prevented.12 Costs or cost avoidances associated with interventions were calculated from pooled examination of 600 interventions in a VAMC with drug costs before and after the intervention, costs associated with harms prevented by the intervention, as well as the VAMC hourly pharmacist wages associated with making an intervention and processing and filling original vs recommended therapies.
The costs presented represent a “best-case” scenario in which all interventions made are expected to prevent patient harms. The costs related to avoided outcomes, facility overhead, and auxiliary staff cannot be included but highlight the many considerations that must be considered when examining potential cost-avoidance calculations. The estimates and methods at hand were chosen because, to our knowledge, no other consensus model exists that would be more appropriate for use in the situation and health care system at hand. Cost-avoidance estimates were calculated by extrapolating the 88-day study period values to a yearly estimate. All cost estimates were adjusted for inflation using the consumer price index calculator as per convention in previous analyses using the cost-avoidance estimates at hand.11-13
Results
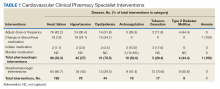
From July 6, 2015, through October 1, 2015, 301 patient encounters occurred, and 529 interventions were documented with the PhARMD tool. The mean number of interventions per encounter was 1.8. Interventions were 65.2% pharmacologic and 34.8% nonpharmacologic. Of pharmacologic interventions, 27.1% were for HF, 12.7% for hypertension, 8.8% for dyslipidemia, 2.8% for anticoagulation, 1.4% for tobacco cessation, 1.1% for T2DM, 0.3% for anemia, and 45.8% for other conditions (Table 1).
A total of 180 interventions were logged for “other” diseases or those not specifically identified above. These 180 interventions were divided among medication reconciliation (14.4%), medication monitoring (13.9%), adjusting dose or frequency of medication (11.7%), preventing or managing an ADE (11.7%), stopping a drug without indication (9.4%), change or discontinuation of medication (8.9%), adherence intervention (7.8%), management of drug-drug interaction (3.3%), medication initiation (2.2%), management of drug contraindication (1.7%), and other nonspecific nonpharmacologic intervention (15%).The main types of pharmacologic interventions across all diseases were related to adjustments in medication dose or frequency (42.3%) and change or discontinuation of medications (20.0%).
Pharmacologic interventions for other reasons were varied and included medication reconciliation (7.5%), medication monitoring (7.2%), preventing or managing ADEs (6.1%), drug not indicated (4.9%), medication initiation (1.2%), change or discontinuation of medication (4.6%), adjust dose or frequency of medication (6.1%), intensive adherence counseling (4.1%), drug interaction (1.7%), and contraindication (0.9%). Most nonpharmacologic interventions, 46.7%, were related to HF. The yearly estimated cost avoidance for all included interventions was calculated as $433,324.06 (Table 2).