The negative impact of the unnecessary prescribing of antibiotic is well known. Consequences include exposing patients to antibiotic adverse effects, risk of overgrowth of pathogenetic organisms such as clostridial species, unnecessary cost of drugs, and development of selection of antibiotic-resistant organisms in the populace at large. Acute viral respiratory infections are among the leading causes of inappropriate antibiotic usage.1 In a study of 1000 adults with respiratory tract infections in an outpatient setting, 77% of patients were prescribed antibiotics, and the treatment was inappropriate in 64% of those who received prescriptions.2 Patient expectations and clinician perceptions of these expectations play a role. One study showed that 54% of clinicians felt their patients expected to receive antibiotics for a visit due to an acute respiratory infection (ARI), such as a cough or cold; 26% of patients did in fact have this expectation.3
The US Department of Veterans Affairs (VA) Central Ohio Health Care System is a large ambulatory care facility, with 4 associated community-based outpatient clinics, serving more than 43,000 central Ohio veterans and completing more than 500,000 medical appointments annually. An antimicrobial stewardship program has been in place since 2013. In May 2018, the clinical pharmacist assigned to the program alerted medical leadership that, of 67 patients seen in primary care for ARIs between April 16, 2018, and May 15, 2018, 42 (63%) had been prescribed an antibiotic. Based on this finding, clinical leadership designed a process improvement program aimed at reducing inappropriate antibiotic usage for the treatment of uncomplicated ARls likely due to viral pathogens. Key components were clinician and patient education and the substitution of a symptomatic treatment kit in place of an antibiotic prescription.
Methods
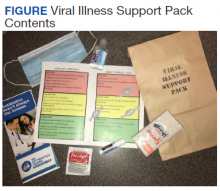
Facility clinical leadership, assisted by Volunteer Services, developed a Viral Illness Support Pack to be dispensed by primary care practitioners (PCPs) to patients presenting with symptoms of viral ARIs. The contents of this support pack are shown in the Figure. Patients were provided with tissues, throat lozenges, lip balm, acetaminophen, hand sanitizer, a surgical mask, patient instructions, and the Antibiotics Aren’t Always the Answer pamphlet.4 The contents of the viral support pack were purchased through Volunteer Services using donated funds. In total, 460 packs were distributed to the primary care patient aligned care teams (PACTs), including the community-based outpatient clinics.
Clinicians and care teams received academic detailing prior to distribution of the viral support packs, stressing the importance of avoiding antibiotics to treat viral illnesses. Viral illness support packs were available for distribution from December 1, 2018, through March 31, 2019. The frequency of antibiotic dispensing to patients coded for ARI during this period was compared with that of the same time period in the previous year. All charts were reviewed for coding accuracy. Patients with illnesses requiring antibiotic treatment, such as pneumonia, exacerbations of chronic obstructive pulmonary disease and chronic bronchitis, and streptococcal pharyngitis, were excluded from the study. Statistical significance was determined using the unpaired t test.
Results
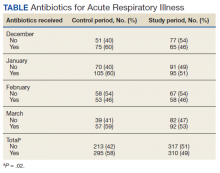
From December 1, 2018, to March 31, 2019, 357 viral support packs were distributed to patients (Table). For the historical control period from December 1, 2017, through March 31, 2018, 508 patients were treated for ARIs. Of these, 295 (58%) received clinically inappropriate antibiotics. In contrast, of the 627 patients treated for ARIs during the study period from December 1, 2018, through March 31, 2019, 310 (49%) received clinically inappropriate antibiotics. The 9% decrease during the period when viral support packs were distributed, compared with the prior year, was statistically significant (P = .02).
Discussion
The decrease in antibiotic prescriptions for ARIs was statistically significant. The success of this project can be attributed to 3 factors: clinician education, patient education, and the option for PCPs to provide symptomatic treatment for these patients rather than prescribe an antibiotic.
The importance of antibiotic stewardship has been emphasized to all PCPs at the VA Central Ohio Health Care System. Antibiotic stewardship has been the subject of grand rounds. Prior to distribution of the viral support pack, the chief of specialty medicine, the project’s champion, spoke to all PCPs. Adequate numbers of viral support packs were distributed to all primary care teams.
In addition to direct clinician-to-patient education at the time of the patients’ visits, educational materials were included in the viral support pack. The Antibiotics Aren’t Always the Answer pamphlet is available from the Centers for Disease Control and Prevention. It covers the importance of antibiotic awareness, discusses what antibiotics do and do not treat, how to stay healthy, and causes of antibiotic resistance. The pamphlet contains the clear message that antibiotics are not only ineffective against viral illness, but also can cause significant undesirable outcomes.