Our Diagnosis
Based on the clinical history of postprandial abdominal pain with prior cholecystectomy and leukocytosis, the initial differential diagnosis included peptic ulcer disease, gastroesophageal reflux, or delayed sequela of the cholecystectomy 6 months prior. Although suspicion remained for possible delayed postoperative complications from the cholecystectomy, ultrasound and hepatobiliary iminodiacetic acid (HIDA) scan were not pursued based on CT imaging findings. The needle-like hypodensity in the duodenum with surrounding inflammation visualized on CT was concerning for an unidentified penetrating foreign body with a possible retroperitoneal microperforation.
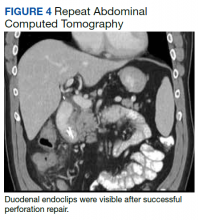
After these imaging findings were relayed from Radiology to the Gastroenterology Service, the patient underwent an upper gastrointestinal (GI) endoscopy to further evaluate the duodenum. Inspection revealed mild gastritis and a linear, clear piece of plastic with both ends firmly lodged within the mucosa from the distal duodenal bulb to the second portion of the duodenum; a significant mucosal defect of the bowel wall was visualized after careful extraction of the foreign body (Figure 2). The patient was diagnosed with a small duodenal perforation, which was sealed endoscopically with 2 endoclips. The extracted piece of plastic was examined and determined to be a broken cocktail pick (Figure 3). During discussion with the patient postprocedure, he stated that he ingested several olive martinis (which were served with cocktail picks) approximately 3 weeks prior to presentation and did not recall ingesting the cocktail pick. A repeat abdominal CT following the endoscopy demonstrated no leak or free air from the site of the repaired duodenal perforation (Figure 4). The patient avoided surgery and was permitted to resume a liquid diet prior to discharge.
Discussion
Foreign body ingestion in adults is most commonly unintentional with fish bones being the most common culprit.1 In unintentional instances of foreign body ingestion, many patients are not aware of the event, with dentures posing a significant well-known risk factor due to lack of palatal sensory feedback.2 Most ingested foreign bodies pass uninhibited through the GI tract without complications. However, less than 1% of ingested foreign bodies cause potentially life-threatening GI perforations.3
The risk of GI perforation due to foreign body ingestion is greatest with elongated, sharp objects, such as needles, bones, toothpicks, and cocktail picks. These objects tend to lodge at areas of narrowing or angulation, such as the appendix, ileocecal region, or as in this case, the duodenum.3 Passage of a foreign body through the duodenum is more likely to be inhibited if the object is longer than 6 cm and with a diameter > 2.5 cm.4 Signs of duodenal perforation are often subtle compared with jejunal or ileal perforations. Patients are commonly afebrile with normal white blood cell counts and are more likely to have chronic symptoms for > 3 days before the appropriate diagnosis of foreign body ingestion is made.1 Duodenal perforations may be more stable clinically compared with distal GI perforations in part due to the retroperitoneal location with relatively fewer bacteria present intraluminally. GI perforations may not occur acutely during passage of the foreign body but can present weeks, months, or even years later.5 Delayed onset of symptoms may happen when the foreign body becomes lodged and only partially perforates the bowel wall, resulting in a chronic inflammatory process. Other possible complications include fistulization and abscess formation from migrating linear sharp objects through the bowel wall, which is most observed with toothpicks and cocktail picks, specifically.5
Foreign bodies identified on plain radiographs commonly include radiopaque objects, such as glass, metallic objects, most animal bones and some fish bones, and some medications. However, radiolucent objects, such as toothpicks and cocktail picks, wood, plastic, most fish bones, and most medicines, often will not appear on radiographs. The diagnosis of ingested foreign body can therefore easily be delayed or overlooked on plain radiographs due to ingestion of radiolucent objects or lack of adequate patient history. A high index of suspicion is needed in such instances. The modality of choice for identifying GI perforation due to ingested foreign objects is CT.5 All of these commonly missed materials on radiographs will be visible on CT with variable densities. As an added benefit, CT also may reveal ingested objects not visualized on radiographs and show ancillary signs of perforation, such as extraluminal free air, localized inflammation, and fluid collections or abscess surrounding a segment of thickened bowel.5
Most ingested foreign bodies will pass through the GI system and can be managed with careful observation alone. However, upper endoscopy is emergently indicated in 3 scenarios of foreign body ingestion: (1) complete occlusion of the esophagus with salivary pooling due to risk of aspiration; (2) ingestion of batteries due to toxic substances; and (3) ingestion of sharp or pointed foreign bodies due to risk of perforation.4 Overall, endoscopic intervention is required in 20% of cases and surgical intervention remains rare at 1%.4 In the case of this patient, an emergent upper endoscopy was needed due to suspected duodenal perforation.
Treatment of duodenal perforations due to foreign bodies may involve conservative, surgical, or endoscopic management. Contained, small perforations in a stable patient may be treated conservatively with IV fluids, antibiotics, and proton pump inhibitors as they self-seal with omentum if the foreign body has passed.6 Retained duodenal foreign bodies pose a risk of persistent perforation or fistulization and must be removed. Anterior duodenal perforations pose a risk of peritonitis, whereas posterior duodenal perforations, although retroperitoneal and sparing the peritoneal cavity, may result in localized abscess formation necessitating foreign body removal. Endoscopic clipping is a modernized, less invasive way to close GI perforations. Through-the-scope clips (TTSCs) can close luminal defects < 2 cm in size.7 Defects > 1 cm may be repaired with combined TTSCs and endoloop or omental patching. Over-the-scope clips can close full thickness defects up to 2 to 3 cm with the advantage of being able to close leaks and fistulas involving inflamed or indurated tissue.7
Conclusions
Intestinal perforations related to foreign body ingestion are a rare complication occurring in < 1% of patients. Although most ingested foreign objects will pass through the GI tract, elongated or sharp objects pose a risk for perforation. In many cases, a history of foreign body ingestion is not obtained, and a high index of suspicion is required. Duodenal perforations due to foreign body ingestion should be included in the differential among the more common diagnoses of peptic ulcers, pancreatitis, and gallbladder disease in the setting of postprandial right upper quadrant abdominal pain. CT is the best modality for identifying foreign bodies, including objects that may be missed on plain radiographs.