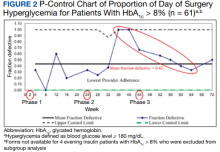
A subgroup analysis of DOS glucose levels in insulin-treated patients with preoperative HbA1c levels > 8% did not demonstrate a change in the rate of
DOS hyperglycemia with intensification of the dose of long-acting basal insulin on the evening before surgery (Figure 2). However, analysis of the statistical process p-control chart of this subgroup identified 2 outliers of DOS hyperglycemia in weeks 36 through 40 followed by a downward trend in the rate for weeks 40 through 64. A 12% decrease (89% vs 77%) in HCP adherence to the protocol after the phase 2 change (weeks 24-44) was observed immediately preceding the unusually high rate of DOS hyperglycemia in patients with HbA1c > 8%. With ongoing QI efforts and education, HCP adherence improved to 88% after the phase 3 change, correlating with the observed trend of improved DOS hyperglycemia rates.Only 7 of 424 (1.7%) patients with DM and 4 of 195 (2.1%) patients treated with evening, long-acting basal insulin had marked hyperglycemia (DOS glucose levels ≥ 300 mg/dL). Only 1 patient who was not on outpatient insulin treatment had surgery canceled for hyperglycemia.
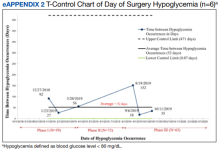
Clinically significant hypoglycemia (blood glucose level < 80 mg/dL) was rare (n = 6). The average time between hypoglycemic events was 52 days and was not affected by intensification of the evening, long-acting basal insulin dose (eAppendix 2, available at doi:10.2788/fp.0335). Variations in the measured time between rare events of hypoglycemia are explained by common cause or random variation, as the individual values did not approach or exceed the 3 SD limits set by the UCL and LCL.Overall, 89% of the HCPs followed the preoperative insulin protocol. HCP adherence to the protocol decreased to 77% after the phase 2 change, often related to deviations from the protocol or when a prior version was used. By the end of phase 3, HCP adherence returned to the baseline rate (88%). Patient adherence to medication instructions was not affected by protocol changes (86% throughout the study period). Prospective data collection was briefly interrupted between January 18, 2019, and March 5, 2019, while designing our phase 2 intervention. We were unable to track the total number of eligible patients during this time, but were able to identify 8 insulin-treated patients with DM who underwent elective noncardiac surgery and included their data in phase 1.
Discussion
The management and prevention of immediate perioperative hyperglycemia and glycemic variability have attracted attention as evidence has mounted for their association with postoperative morbidity and mortality.1,2,17 Available guidelines for preventing DOS hyperglycemia vary in their recommendations for preoperative insulin management.7-10 Notably, concerns about iatrogenic hypoglycemia often hinder efforts to lower rates of DOS hyperglycemia.4 We successfully implemented an iterative intensification protocol for preoperative long-acting basal insulin doses on the evening before surgery but did not observe a lower rate of hyperglycemia. Importantly, we also did not observe a higher rate of hypoglycemia on the DOS, as observed in a previous study.5
The observational study by Demma and colleagues found that patients receiving 75% of their evening, long-acting basal insulin dose were significantly more likely to achieve target blood glucose levels of 100 to 180 mg/dL than patients receiving no insulin at all (78% vs 0%; P = .001). However, no significant difference was noted when this group was compared with patients receiving 50% of their evening, long-acting basal insulin doses (78% vs 70%; P = .56). This is more clinically pertinent as it is generally accepted that the evening, long-acting insulin dose should not be entirely withheld on the evening before surgery.5