Click to view more from Federal Health Care Data Trends 2024.
Data Trends 2024: Depression and PTSD
Reviewed by:
Jason C. DeViva, PhD
Associate Professor. Department of Psychiatry
Yale School of Medicine
New Haven, CT
Co-Director
PTSD Clinical Team
VA Connecticut Health Care System
West Haven, CT
Jason C. DeViva, PhD, has disclosed no relevant financial relationships.

1
-
-
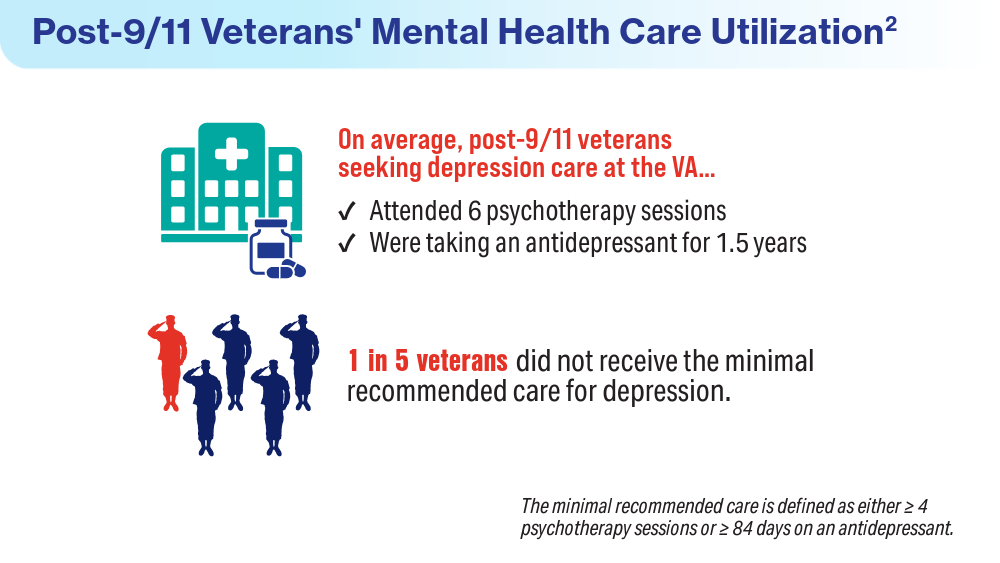
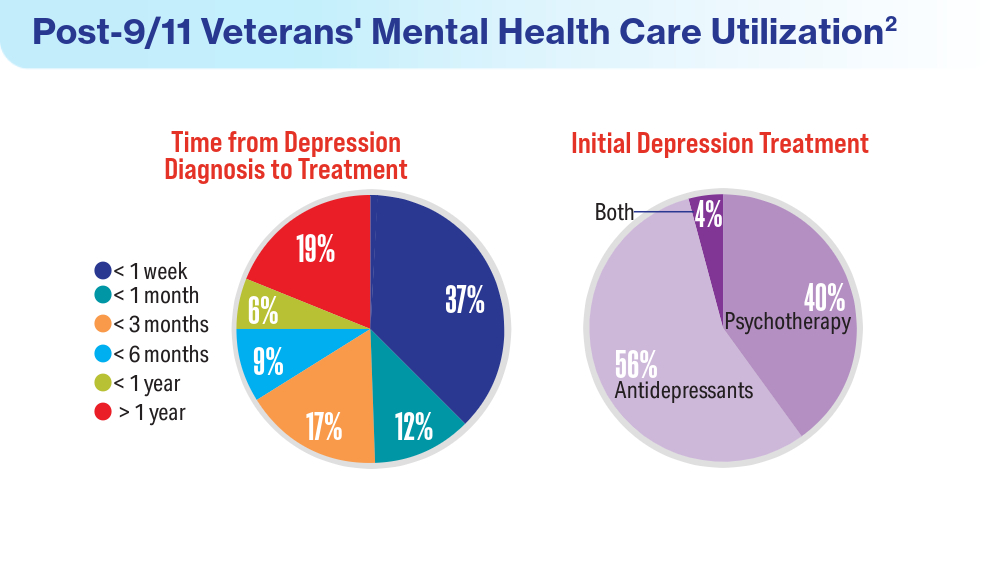
An analysis of 108,457 post-9/11 veterans with confirmed depression after deployment found that while most received the minimum recommended treatment, 21.6% did not. Underutilization was linked to male sex, minority status, and previous mental health care.
-
-
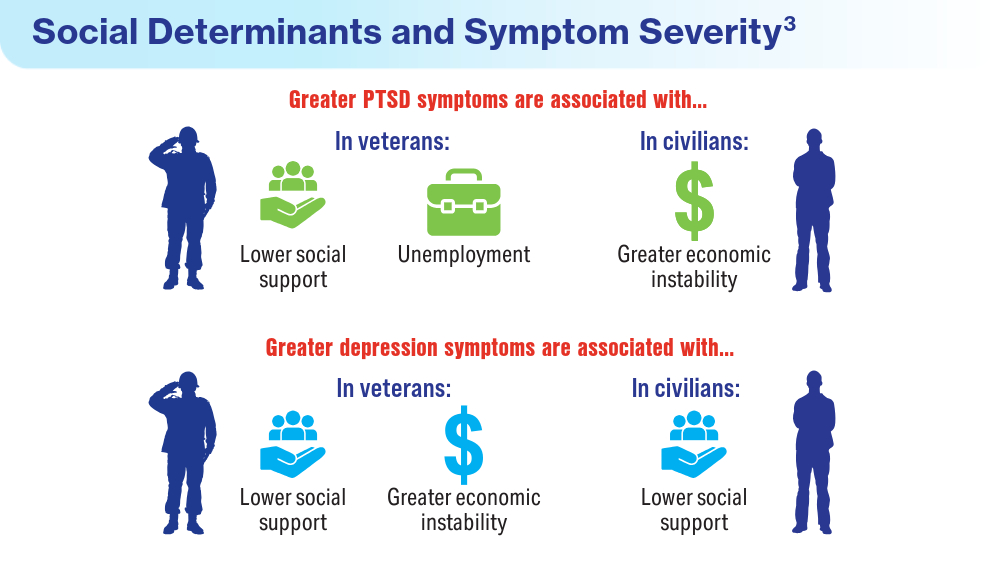
In addition to directly treating mental health symptoms, improving these social and economic factors should be a focus for future research and intervention.
-
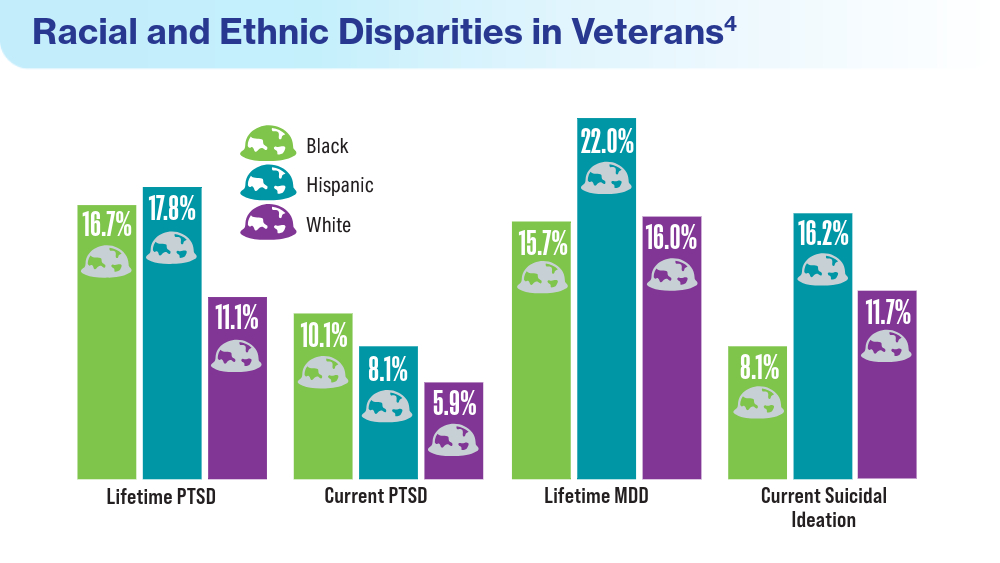
Black and Hispanic veterans have higher rates of PTSD and major depressive disorder (MDD), which may be attributed to characteristics such as younger age, lower household income, and female sex. Black veterans are also statistically more likely to have combat experience than White veterans.
-
-
-
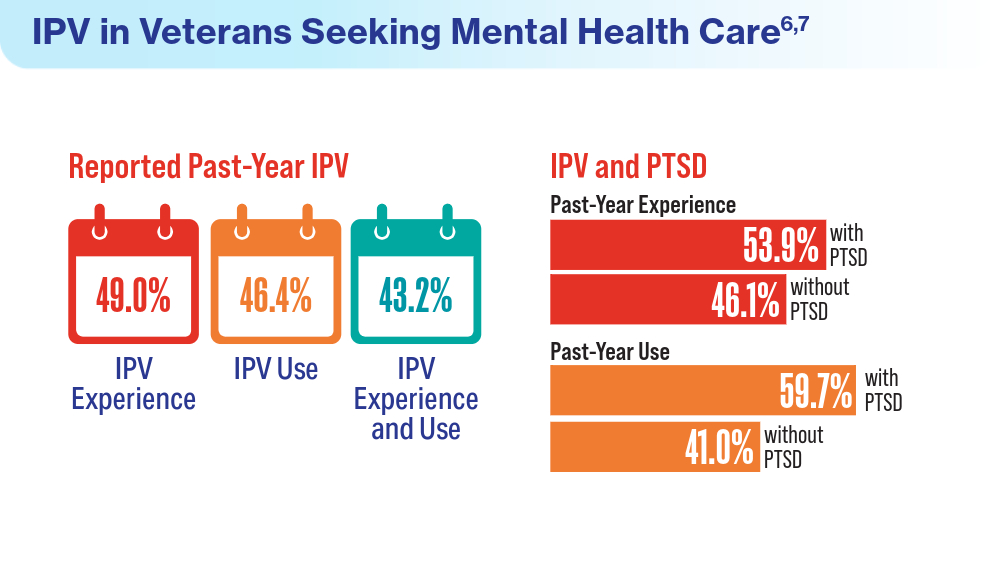
Intimate partner violence (IPV) includes screaming, insulting, threatening, sexual violence, and physical violence.
Patients seeking mental health care at the VHA represent a high-risk group for IPV, with higher rates observed in veterans and military personnel than among civilians. PTSD diagnosis was found to be the greatest predictor for engaging in these behaviors. No sex differences between IPV use and experience were identified, a shift from previous understanding of sex-based IPV behaviors.
-
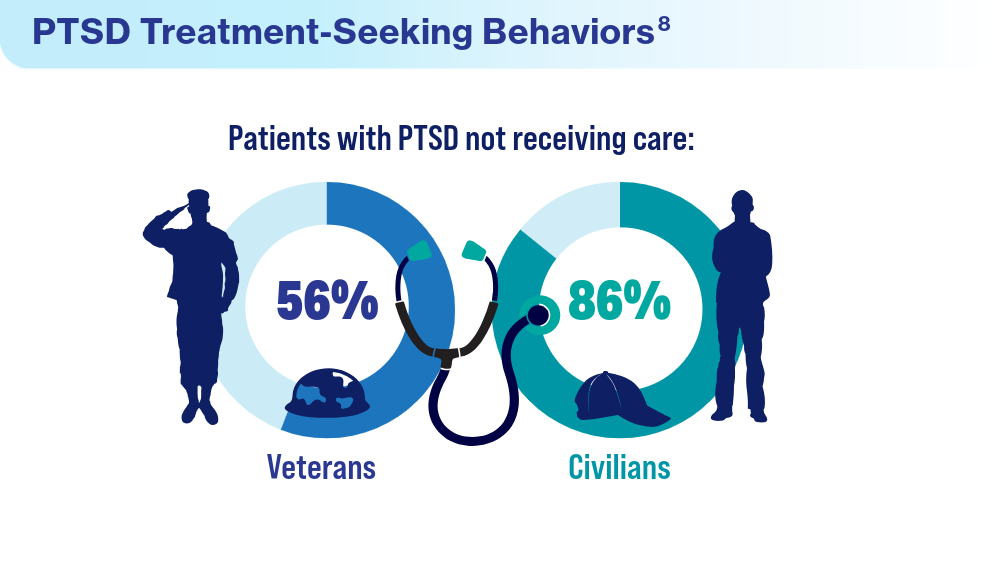
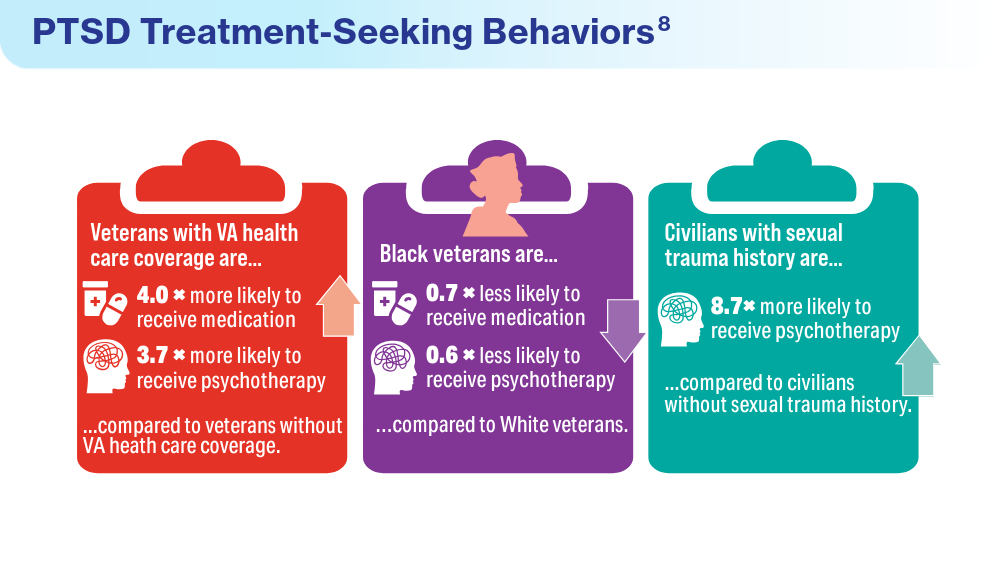
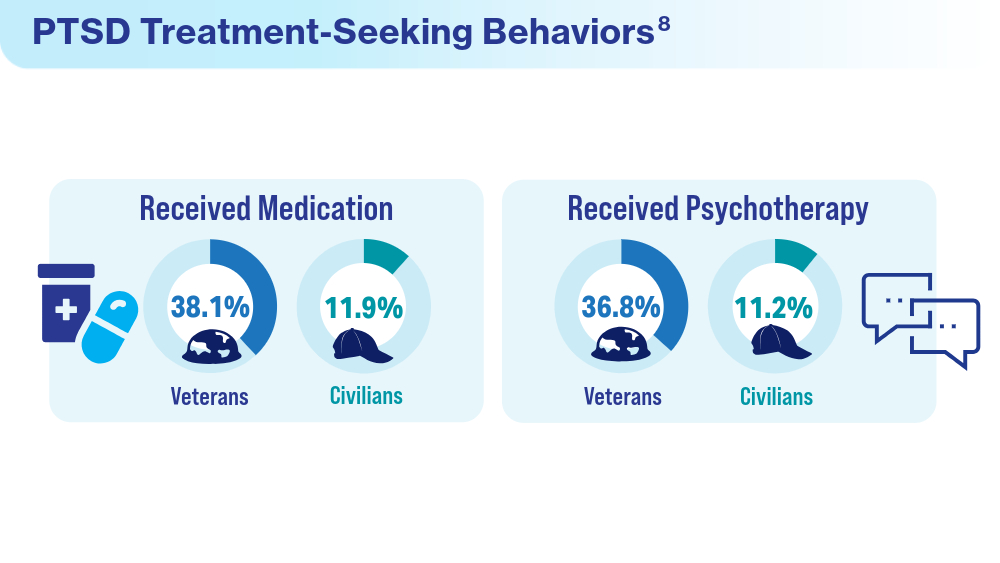
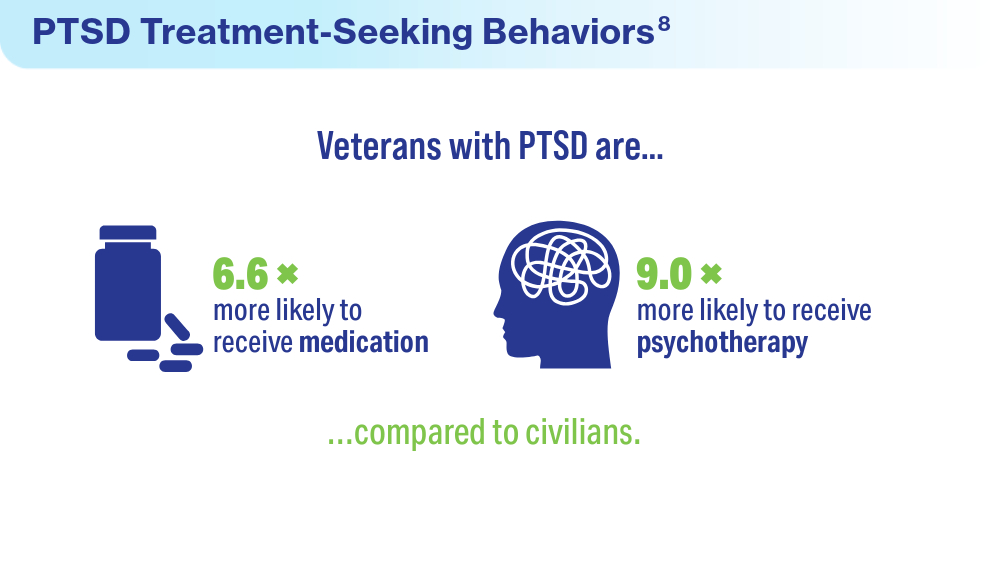
A recent national study found that although veterans are more likely to receive any PTSD care compared to civilians (especially if they have VA benefits), treatment utilization is low overall. A better understanding of PTSD treatment barriers is necessary so that interventions can be created to address this issue.
-
-
-