This is the second article in the series, "Heparin-Induced Thrombocytopenia." The remaining articles are Introduction; Diagnosis; Treatment/Management; and References.
Patient Presentation and History
The typical patient with HIT presents with a new or progressing thrombosis between days 5 and 14 of heparin therapy (with day 0 representing the day the first dose is administered); thrombosis can be venous or arterial, although venous thrombosis occurs much more frequently.1,5,9,15 As patients rarely remain hospitalized for such a long period, it is imperative that providers in clinic and emergency settings obtain detailed histories for patients who present with thrombocytopenia and/or thrombosis. HIT should be suspected in any such patient whose history shows heparin use within the previous two weeks (even if the drug has been discontinued).15
Two forms of atypical HIT are rapid-onset HIT and delayed-onset HIT. Rapid-onset HIT is defined by a platelet count that falls within 24 hours of exposure to heparin. This form is usually associated with previous heparin exposure (ie, within the previous 100 days, but most commonly within the previous 30 days). Affected patients have already developed circulating antiheparin PF4 antibodies, causing an immediate reaction when the patient is re-exposed to the drug.1,15
The less common delayed-onset HIT occurs in patients in whom heparin has been discontinued for as long as 40 days. Delayed-onset HIT carries the greatest risk for severe thrombosis.1,15
Physical Examination
Atypically, a patient may present with bleeding, skin necrosis, venous gangrene, or anaphylaxis,9 but skin necrosis at the site of heparin injection is strongly suggestive of HIT.12 However, neither physical signs nor symptoms, nor a thrombotic event is required to make a diagnosis of HIT. In fact, the preference is for a diagnosis to be made before thrombosis formation.5
The major manifestation of HIT is thrombocytopenia itself2,18 (see "Laboratory Findings"). Nevertheless, if physical signs and symptoms are evident, they will be related to the thrombosis, and the components of the physical exam will proceed accordingly.
Laboratory Findings
Platelet count monitoring and HIT antibody testing are the laboratory tests most commonly used when HIT is suspected. Although 25% of patients with HIT will experience a thrombotic event before the platelet count falls, monitoring the platelet count is considered the most effective means to identify patients with HIT.5 HIT antibody testing is not recommended unless the health care provider has a strong suspicion for HIT.19
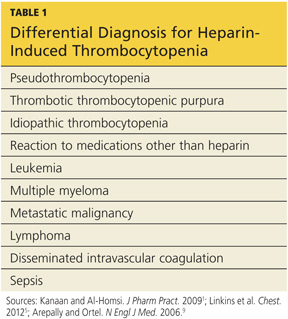
Thrombocytopenia is a common abnormality, especially in hospitalized patients, and its causes are numerous.11 Table 11,5,9 lists the differential diagnosis that the clinician who suspects HIT should consider.
Nevertheless, the ACCP guidelines5 recommend platelet count monitoring for all patients receiving heparin, beginning on day 4 of heparin therapy, then continuing every two to three days until treatment day 14 or heparin discontinuation, whichever occurs first.5,15 A platelet count decrease of 50% or more should raise a suspicion for HIT.15
The ACCP makes two principal exceptions to these recommendations.5 The first involves patients who have received UFH within the previous 100 days. These patients should undergo a baseline platelet count before heparin is administered, followed by a repeat platelet count within 24 hours. Any patient who experiences an anaphylactic reaction to UFH should undergo an immediate platelet count; a decrease in these patients is often transient.
The second exception pertains to medical and obstetric patients. Those receiving LMWH or UFH only to maintain line patency do not require platelet monitoring, as their risk for HIT is relatively low.1,5
Laboratory Interpretation
In HIT, thrombocytopenia is defined as a platelet count below 150,000/mm3 or a platelet count reduction of 50% or more from baseline, even if the platelet count remains above 150,000/mm3.9 (The patient's baseline platelet count is defined as the highest count recorded in the previous two weeks.1,5,15) The thrombocytopenia associated with HIT is rarely severe and can be easily overlooked.1
Once the platelet count suggests a diagnosis of HIT, heparin-dependent antibodies can be identified through immunologic or functional assays.1,9,15 Immunologic assays should be ordered immediately upon suspicion of HIT since they are simple tests with relatively rapid results. Immunologic assays detect immunoglobulin G (IgG), IgA, and IgM antibodies.9 Though lacking in specificity, the immunologic assay is highly sensitive.2,12,20 The most frequently used immunologic assay is the enzyme-linked immunosorbent assay (ELISA).1,2,9,20 The ELISA, which detects antiheparin PF4 antibodies, has a sensitivity greater than 97% but a specificity of only 74% to 86%.8,12
Functional assays,which are technically demanding, test the ability of PF4 antibodies to activate platelets in the presence of heparin. The functional assay is used to confirm the diagnosis of HIT when a positive ELISA result is obtained.1,9,15 Among the functional assays, the serotonin release assay (SRA) has been most completely studied. Though very expensive, the SRA is 89% to 100% specific in diagnosing HIT.2,12
