These participants were called over several days between October 24, 2011, and November 28, 2011. The limits of confidentiality were explained to each veteran before they were asked to participate in this initiative as an effort to improve the Atlanta VAMC’s tobacco cessation program.
Of the 229 possible participants, only 115 were accessible by phone over the survey period. One declined to participate, leaving 114 potential respondents. Of the 114, 13 reported that they either did not receive a referral for tobacco cessation over the past year or did not recall receiving such a referral. These 13 were removed from the respondent pool, leaving 101. Of these individuals, 5 reported that they did attend the tobacco cessation counseling sessions. These individuals were also removed from the respondent pool, leaving a total of 96 respondents to answer the remaining multipart question regarding barriers to attendance.
Measures and Analysis
Simple descriptive statistics were used to characterize the data from the survey portion of this study, determining frequencies of responses to different barriers. Since respondents were allowed to select as many barriers as applied to their situation, totals did not add to 100%. In addition, a separate variable, consisting of positive responses to barriers that represent accessibility (eg, distance, time, transportation, parking, gas), was used to develop a composite accessibility score to further analyze the comprehensive impact of access.
Results
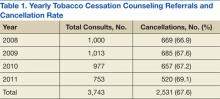
The rate of cancellations remained fairly stable between January 2008 and November 2011 (67%) (Table 1). The sample was representative of the male-dominated population at the VA with 84% of the respondents being male, aged 22 to 75 years. Of the 96 respondents who did not attend the cessation counseling, 85 reported they were still using tobacco products; 11 reported having quit. Of the 85 respondents who were still using tobacco products, the majority (97%) were smoking cigarettes, while 1% each reported using smokeless tobacco products such as chew, snuff, or a combination of these (Table 2).
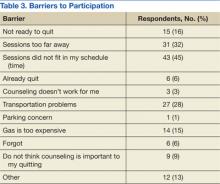
Of the 96 respondents who did not complete their tobacco cessation counseling referral, 45% reported that time or scheduling was a barrier to participation (Table 3). Thirty-two percent reported that distance to the counseling sessions was a barrier, and 28% reported transportation issues as a barrier. Also contributing to transportation issues, the cost of gasoline was given as a reason for not attending by 15% of the respondents. Sixteen percent reported that they were not yet ready to quit in spite of accepting a referral for cessation counseling. Smaller percentages reported that they had already quit (6%), believed that counseling did not work for them (3%), expressed that parking was a concern (1%), forgot (6%), or did not think that counseling was important to their quitting efforts (9%). Other reasons provided for nonattendance included concern that quitting is difficult, other medical and mental health priorities, discomfort in groups, and family illness.
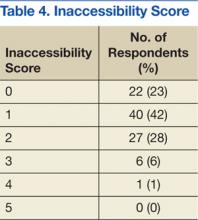
A final analysis was conducted, where an inaccessibility score was determined for each respondent based on barriers related to inaccessibility. A single point was given for each of the following answers reported as a barrier by the respondent: (1) too far away; (2) schedule/time; (3) transportation; (4) parking; or (5) gas. Twenty-three percent of the 96 respondents had no accessibility issues, reported as an inaccessibility score of 0. Most respondents had 1 inaccessibility issue (40%); while 28% reported 2, 6% reported 3, and only 1 individual reported having ≥ 4. Of note, a majority (77%) of the respondents reported 1 or more inaccessibility issues as a barrier to their attendance (Table 4).
Discussion
Studies abound regarding barriers to provider-offered smoking cessation counseling.9,10 Even oncologists report low levels of confidence in their ability to counsel patients to quit using tobacco.11 Physicians report lack of time, training, and patient willingness as barriers that prevent them from providing counseling on critical lifestyle issues. Few studies, however, have examined patient-reported barriers to tobacco counseling services. It bears examination, though, when 67% of the patients who accept a referral for tobacco cessation counseling, with no copay, fail to utilize the opportunity.
The results of this study suggest that accessibility issues played a major role in preventing participation, indicating that 77% of the respondents reported at least 1 accessibility issue (transportation, time, or cost) as a contributing factor that kept them from their appointment. The most common accessibility issues reported by this sample were timing and scheduling (45%), distance to the counseling sessions (32%), and transportation issues (28%). The VA is actively addressing these barriers through telehealth and computer-assisted options. In addition, a new telephone mobile application based on the integrated care model for smoking cessation is now available and provides tobacco quit tips for veterans with PTSD who smoke.12