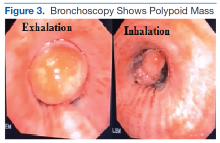
Salivary gland lung tumors are extremely rare intrathoracic malignancies, accounting for only 0.2% of all lung tumors.1 It has been postulated that these lung tumors arise from pluripotential cells in the epithelium of the submucosal bronchial glands and usually present as endoluminal lesions. The cause of salivary gland tumors is unclear. They seem to be unrelated to exposure to smoking, air pollutants, or other chemicals.2 Associated symptoms are generally related to endoluminal obstruction by the tumors, which are centrally located. Thus, presenting symptoms commonly include chronic cough, progressive dyspnea, hoarseness, wheezing, and occasional hemoptysis.3 Chest radiographs seem normal in most cases except those in which obstruction is present. Computed tomography usually shows well-defined endotracheal or endobronchial lesions that are lobulated, polypoid, or smooth, without infiltration into surrounding tissues.
Although basal cell adenocarcinoma (BCAC) was included in World Health Organization’s (WHO) Pathology and Genetics of Head and Neck Tumours in 1991, its definition—“an epithelial neoplasm that has cytological characteristics of basal cell adenoma (BCA), but a morphologic growth pattern indicative of malignancy”—did not appear until 2005.4 Basal cell adenocarcinoma generally is classified as a low-grade malignancy with a good long-term prognosis. It usually affects parotid and submandibular minor salivary glands.5
Histologic differentiation of BCAC and BCA is difficult and depends on whether local structures have been invaded or on which histologic features of perineural or vascular invasion are present.6 Basal cell adenocarcinoma also shows strong immunoreactivity to cytokeratin 7 (CK-7) and variable myoepithelial staining with S100.7 Because of the prognosis and potential treatment differences involved, BCAC must be differentiated from other basaloid cell tumors, such as BCA, adenoid cystic carcinoma, polymorphous low-grade adenocarcinoma, myoepithelial tumor, epithelial-myoepithelial carcinoma, and basaloid squamous cell carcinoma (SCC).8 Surgical excision is the primary treatment of choice.5 Rare in the salivary glands, BCA and BCAC are even rarer in salivary gland tissue outside the head and neck region. The authors report on a case of BCAC of the salivary gland tissue in the trachea.
Case Report
An 84-year-old man with diabetes mellitus and hypertension and a nonsmoker presented to the emergency department of the VA Caribbean Healthcare System in San Juan, Puerto Rico, with a dry cough and shortness of breath lasting 1 week, which worsened the day before
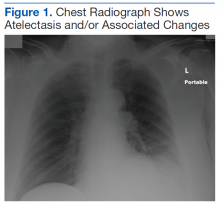
presentation. On physical examination, the patient was afebrile and in no respiratory distress, and his vital signs were within normal limits. There was no barrel chest, no prolonged expiratory phase, and occasional wheezing more prominent on the left side. A chest radiograph showed atelectasis and/or associated changes (Figure 1).
After the initial biopsy results led to a provisional diagnosis of basaloid neoplasm with squamous features, the patient underwent rigid bronchoscopic tracheal tumor debridement followed by cryotherapy at the base of the tumor.
Body imaging and physical examination revealed no masses in the head and neck region. The final diagnosis was then rendered: primary pulmonary, salivary gland, low-grade BCAC (Figure 5A & B) of the trachea. Immunohistochemical markers confirmed the basaloid and myoepithelial-like differentiation of the tumor (CK-7 positive, p63 positive, S100 positive, smooth muscle actin negative, CK-5/6 negative [Figure 6A-C]). Resection showed positive margins.Discussion
Primary tracheal tumors are rare, accounting for < 1% of all malignancies.9,10 According to the National Cancer Institute Surveillance, Epidemiology, and End Results database, the rate of new cases of primary carcinoma of the trachea was 2.6 per 1 million people per year.11 Of all primary tumors of the trachea, 80% are malignant9,10; the rest vary widely and include both malignant and benign histotypes.11