What’s your diagnosis?
By Ravi B. Parikh, MD, George A. Alba, MD, and Lawrence R. Zukerberg, MD. Published previously in Gastroenterology (2013;144;272, 467).
A 36-year-old woman, originally from Haiti, presented to the emergency department with 2 weeks of abdominal distention, diarrhea, and blood-tinged emesis. She had given birth to her first child by uncomplicated cesarean section 9.5 weeks earlier. There was no history of recent travel, diet change, or sick contacts. She denied alcohol, tobacco, or illicit drug use and was not taking any medications or supplements. She was allergic to chloroquine (itchiness) and had no history of atopy. She was not aware of any family history of liver disease or allergy, although her paternal history was unknown.
Upon admittance to the general medicine service, the patient was afebrile and hemodynamically stable. She did not have any stigmata of chronic liver disease. Her abdomen was distended and diffusely tender with rebound tenderness and guarding (Figure A). Serum studies were notable for white blood cell count of 14.5 x 103/microL, with 46% eosinophils (absolute count 6660/mm3). Other values, including serum human chorionic gonadotropin, were normal.
Computed tomography of the abdomen and pelvis (Figure B) showed a large amount of abdominal and pelvic ascites (arrow) with mild small bowel wall thickening. There was no evidence of organomegaly or vessel thrombosis. Subsequent diagnostic paracentesis demonstrated an exudative effusion with total nucleated cells 4,545/mL, with 82% eosinophils. Large-volume paracentesis of 4,000 mL of straw-colored fluid relieved the patient’s abdominal pain. Fluid bacterial and tuberculosis cultures were negative, and cytology showed no evidence of malignancy. Peripheral blood smear was unremarkable. Stool culture, stool ova and parasites, urine culture, and blood culture were all negative.
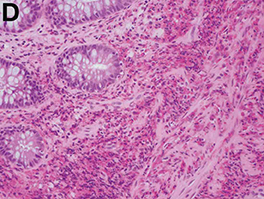
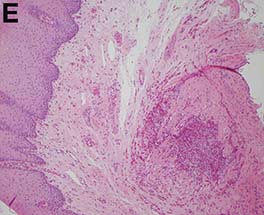
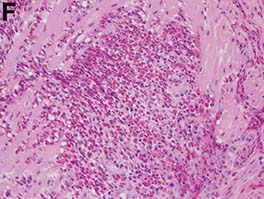
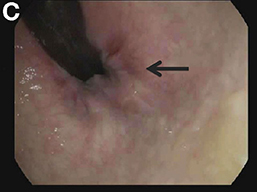
Because of these findings, the gastroenterology service was consulted. Esophagogastroduodenoscopy and colonoscopy showed mild rectal mucosal erythema (arrow) without masses, bleeding, ulcers, or polyps (Figure C).
What is the diagnosis? What is the appropriate management?