Natural course of primary hepatic angiosarcoma with rupture
The pathology demonstrated slitlike vascular channels lined by spindle-shaped endothelial cells with large and hyperchromatic nuclei (Figure C). Primary hepatic angiosarcoma (PHA) was diagnosed. The patient declined operation because of poor prognosis and body performance. Ascites tapping was performed, and the fluid was bloody. The patient received a blood transfusion and died 2 days later.
PHA is an aggressive malignant tumor that originates from the endothelium of liver blood vessels. It is a rare condition and accounts for 0.6%-2.0% of all primary liver tumors and less than 5% of all angiosarcomas.1
Most PHAs exhibit no obvious symptoms and signs, particularly when they are small. As the disease progresses, symptoms and signs including abdominal pain, weakness, fatigue, weight loss, hepatomegaly, and ascites occur. The spontaneous rupture of PHA was reported in 15%-27% of patients in a previous study.2 As in our case, no obvious symptoms were noted in the early stage, and spontaneous rupture was observed in the later stage.
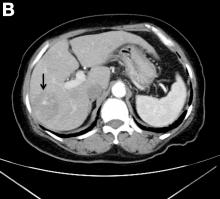
A CT scan of PHA reveals multiple nodules or a dominant mass and a diffusely infiltrating lesion. The tumor is composed of low-density lesions with small heterogeneous hypervascular foci.3 In our patient, a CT scan revealed a hepatic tumor that had a low density when it was small and multiple heterogeneous hypervascular foci when it grew large.
PHAs are very aggressive tumors, and most cases are diagnosed at an advanced stage. The median survival was reported to be 6 months without treatment. Complete resection with clear margins is the choice of treatment; however, the prognosis is poor even after complete resection.2 In our case, operation after diagnosis was declined because of the patient’s poor prognosis and body performance. She lived for 18 months after the diagnosis. The entire natural course of PHA from initial diagnosis to rupture was well presented in our case.
References
1. Zheng YW, Zhang XW, Zhang JL, et al. Primary hepatic angiosarcoma and potential treatment options. J Gastroenterol Hepatol. 2014;29:906–11.
2. Cawich SO, Ramjit C. Herald bleeding from a ruptured primary hepatic angiosarcoma: a case report. Mol Clin Oncol. 2015;3:1063–6.
3. Huang IH, Wu YY, Huang TC, et al. Statistics and outlook of primary hepatic angiosarcoma based on clinical stage. Oncol Lett. 2016;11:3218–22.
ginews@gastro.org