Patients with stage IV lung or colorectal cancer who had end-of-life discussions with caregivers before the last 30 days of life were significantly less likely to receive aggressive care in their final days and more likely to get hospice care and to enter hospice earlier, a study of 1,231 patients found.
Nearly half received some kind of aggressive care in their last 30 days (47%), including chemotherapy in the last 14 days (16%), ICU care in the last 30 days (6%), and/or acute hospital-based care in the last 30 days of life (40%), Dr. Jennifer W. Mack and her associates reported.
Multiple current guidelines recommend starting end-of-life care planning for patients with incurable cancer early in the course of the disease while patients are relatively stable, not when they are acutely deteriorating.
Many physicians in the study postponed the discussion until the final month of life, and many patients didn’t remember or didn’t recognize the end-of-life discussions. Discussions that were documented in charts were not associated with less-aggressive care or greater hospice use, if patients or their surrogates said no end-of-life discussions took place.
Eighty-eight percent of patients in the current study had end-of-life discussions. Twenty-three percent of the discussion were reported by patients or their surrogates in interviews but not documented in records, 17% were documented in medical records but not reported by patients or surrogates, and 48% were both reported and documented.
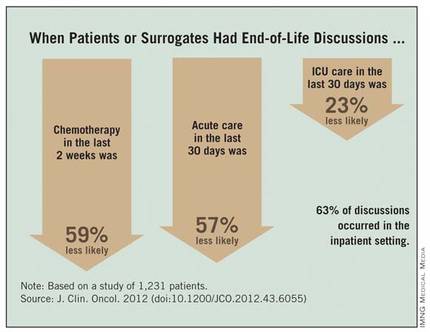
Among the 794 patients with end-of-life discussions documented in medical records, 39% took place in the last 30 days of life, 63% happened in the inpatient setting, and 40% included an oncologist. Fifty-eight percent of patients entered hospice care, which started in the last 7 days of life for 15% of them, reported Dr. Mack, a pediatric oncologist at the Dana-Farber Cancer Institute and Harvard Medical School, Boston.
The study was published online Nov. 13, 2012 by the Journal of Clinical Oncology (doi:10.1200/JCO.2012.43.6055).
Chemotherapy in the last 2 weeks of life was 59% less likely, acute care in the last 30 days was 57% less likely, and ICU care in the last 30 days was 23% less likely when patients or surrogates reported having end-of-life discussions.
Patients Followed 15 Months After Diagnosis
Patients whose first end-of-life discussion happened while they were hospitalized were more than twice as likely to get any kind of aggressive care at the end of life and three times more likely to get acute care or ICU care in the last 30 days and to have hospice care start within the last week before death.
Having a medical oncologist present at the first end-of-life discussion increased the odds of having chemotherapy in the last 2 weeks of life by 48%, decreased the odds of ICU care in the last 30 days by 56%, increased the likelihood of hospice care by 43%, and doubled the chance of hospice care starting in the last 7 days of life. All of these odds ratios were significant after controlling for other factors.
Data came from a larger cohort of 2,155 patients with stage IV lung or colorectal cancer receiving care in HMOs or Veterans Affairs medical centers in five states. All were followed for 15 months after diagnosis in the Cancer Care Outcomes Research and Surveillance Consortium.
An earlier analysis by the same investigators showed that 87% of the 1,470 patients who died and 41% of the 685 still alive by the end of follow-up had end-of-life care discussions, but oncologists documented end-of-life discussions with only 27% of their patients, suggesting that most discussions were with non-oncologists. Among those who died, documented discussions took place a median of 33 days before death (Ann. Intern. Med. 2012;156:204-10).
"Our previous study on this database found that most physicians do have end-of-life discussions before death, but most occur near the end of life," Dr. Mack said in an interview.
The current study analyzed data for 1,231 of the patients who died but who lived at least 1 month after diagnosis, in order to assess whether the timing of discussions influenced end-of-life care. "Besides the fact that that seems like logical practice, there really wasn’t a clear evidence base that that affects care," she said.
Patients were significantly less likely to say they’d had an end-of-life discussion if they were unmarried, black or non-white Hispanic, or not in an HMO.
Start Talks Closer to Diagnosis
When discussions don’t begin until the last 30 days of life, the end-of-life period usually is already underway, the investigators noted. Physicians should consider moving end-of-life care discussions closer to diagnosis, they suggested, while patients are relatively well and have time to plan for what’s ahead.