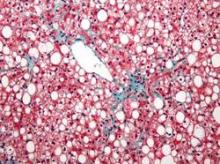
Administration of a novel fatty acid–bile acid conjugate safely and significantly reduced liver fat content in patients with nonalcoholic fatty liver disease in a phase II trial.
Administration of resveratrol for 8 weeks, however, failed to improve any features of the disease in a separate placebo-controlled study.
In 60 patients aged 18-75 years in a randomized, double-blind, placebo-controlled study of the fatty acid–bile acid conjugate aramchol (Trima Israel Pharmaceutical Products Ltd. Maabarot), 3 months of treatment was associated with a decrease in liver fat content by a mean of 12.57% as measured by magnetic resonance spectroscopy, compared with an increase in liver fat by a mean of 6.39% in patients who received placebo, Dr. Rifaat Safadi of Hadassah University Medical Center, Jerusalem and colleagues reported in the DEcember issue of Clinical Gastroenterology and Hepatology.
The difference between the treatment and placebo groups was significant, even after age, sex, and body mass index were adjusted for.
Liver fat content also decreased in patients who received treatment with a 100-mg dose of aramchol, but the difference compared with placebo was not statistically significant, indicating a dose-response relationship in treated patients, the investigators said (Clin Gastroenterol Hepatol 2014[doi:10.1016/j.cgh.2014.04.038]).
A trend was seen for improvements over time in endothelial function and levels of alanine aminotransferase and adiponectin.
Patients in the study were from 10 centers in Israel, and all had biopsy-confirmed NAFLD (54 patients) or nonalcoholic steatohepatitis (NASH, 6 patients). They were randomized to receive 100 or 300 mg of aramchol or placebo once daily for 3 months.
No serious or drug-related adverse events occurred in the treated patients, the investigators said.
The findings suggest that aramchol is a candidate for the treatment of fatty liver–related diseases, which are “an increasingly relevant public health issue because of their association with the worldwide epidemics of diabetes and obesity,” and for which treatments are lacking, they said, concluding that longer trials in patients with NASH and metabolic complications are warranted to evaluate metabolic and histologic benefits of treatment.
Findings from the resveratrol study were less encouraging.
Eight weeks of treatment at 3,000 mg daily in overweight or obese men with NAFLD who were recruited from clinics in Brisbane from 2011 through 2012 was no better than placebo for improving insulin resistance, hepatic steatosis, or abdominal fat distribution, Dr. Veronique S. Chachay of the University of Queensland, Brisbane, Australia and her colleagues also reported in the December issue of Clinical Gastroenterology and Hepatology.
No changes were observed in plasma lipids or antioxidant activity, and levels of alanine and aspartate aminotransferases increased significantly (from 45 to 63 U/L and from 35 to 45 U/L, respectively) until week 6 in the 10 treated patients, compared with the 10 who received placebo (40 to 48 U/L and 36 to 38 U/L, respectively). Resveratrol did not significantly alter transcription of NQ01, PTP1B, IL6, or H01, the investigators said (Clin Gastroenterol Hepatol 2014[doi:10.106/j.cgh.2014.02.024]).
NAFLD is associated with abdominal obesity, insulin resistance, and inflammation, and while weight loss via calorie restriction is known to reduce features of the disease, there is no pharmacologic therapy available to achieve this end.
The investigators sought to determine if resveratrol – a polyphenol that has been shown to prevent high-energy diet-induced steatosis and insulin resistance in animals – might be beneficial in patients with NAFLD.
“The present study demonstrates that the preventive role of resveratrol observed in diet-induced preclinical models of NAFLD does not translate into a therapeutic role in clinically established NAFLD,” they said, adding that clinical dose-finding studies are “paramount to elucidate the dose-response relationship” and that “the purported calorie-restriction mimicking of resveratrol may require investigation in combination with dietary prescription, standard care, and lifestyle modifications to target adequately the complexity of dysregulation in obesity-related chronic disease.”
The aramchol study was supported by Galmed Medical Research, Ltd. Dr. Safadi reported having no disclosures. The resveratrol study was supported by the Princess Alexandra Research Foundation, the Lions Medical Research Foundation, and the National Health and Medical Research Council of Australia. The authors reported having no disclosures.