Outcomes of Palliative Care Consults With Hospitalized Veterans
Families and patients receive emotional support and better care planning after palliative care consultations.
Dr. Manthri and Dr. Simmons are Fellows at St. Louis University in Missouri. Dr. Cepeda is a Palliative Care Physician at the John Cochran Division of the VA St. Louis Health Care System. Dr. Cepeda also is Director of the Hospice and Palliative Medicine Fellowship Program and Assistant Professor of Medicine at Saint Louis University School of Medicine.
Correspondence: Dr. Manthri (sukeshmanthri123@gmail.com)
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the US Government, or any of its agencies.
Inpatient palliative care (IPC) consultation services have been widely adopted in US hospitals. Outcomes research has demonstrated improved quality of life (QOL) for palliative inpatients for symptom control and satisfaction with care.1-5 Families benefit from emotional support, care planning, and transitions of care.4,6-8 Outcomes, including hospital length of stay, hospital costs, and discharge dispositionalso seem to improve.9-17 The Department of Veterans Affairs (VA) provides palliative care (PC) consultation teams at its hospitals nationwide; however, few studies exist to show how a PC service is used at a VA hospital. The following study of a PC consult team at an urban VA facility provides a unique picture of how a PC team is used.
Methods
The John Cochran Division of the VA St. Louis Health Care System (VASLHCS) in Missouri is a 509-bed adult acute care hospital with medical and surgical specialties and subspecialties available for veterans, including an intensive care unit (ICU). The PC team is one of the subspecialty teams following patients after consultation and consists of a PC physician, nurse practitioner, chaplain, social worker, and psychologist.
Data Collection
This study was exempt from internal review board approval. The attending physician kept track of each IPC encounter between September 2014 and April 2016. Data were retrieved from the Computerized Patient Record System by identifying charts that included family meeting notes during the specified time. All 130 patients included in this study were followed by the PC team. Patient charts were reviewed, and information was uploaded to spreadsheets, which became the database for this study. The data included age, patient location, diagnosis, number of days between admission and PC consultation, and number of days between admission and family meeting. Other data included code status changes and discharge dispositions. Only consultations that resulted in direct patient contact were included.
The VASLHCS requires therapeutic support level (TSL), or code status, documentation by the attending physician regarding the discussion with a competent patient or valid representative if the patient is incapacitated. Levels of support are TSL I ‘‘no limitation on care,’’ TSL II ‘‘partial code,’’ that is, usually no cardiopulmonary resuscitation or do not intubate with selected medical measures to continue, and TSL III ‘‘comfort measures only.’’ If a patient’s code level changed after IPC consultation, the change is recorded.
Data Analysis
The files were purged of all unique personal health history. Because there was no control group, multivariable analyses of association were not warranted. Analysis was confined to descriptive measures.
Results
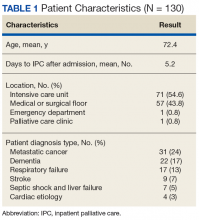
A total of 130 patients with IPC consultations were included in this retrospective study conducted from September 2014 to April 2016 (Table 1).
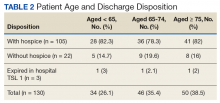
Most of the IPC consultations came from the ICU (54.6%), followed by medical and surgical care units Most common diagnoses were metastatic cancer (24%), dementia (17%), respiratory failure (13%), stroke (7%), and septic shock and liver failure (5%) for which IPC consultations were requested.The scope of IPC consultations usually include medical recommendations about symptom management, discharge planning, discussion about goals of care (GOC), code status and prognosis, managing expected in-hospital expirations (deaths), and determination of hospice eligibility. Of the IPC cohort, 74% were aged > 65 years; 26.1% were aged < 65 years (Table 2).
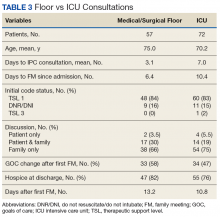
During the study, only 3 of 130 (2%) patients died who were TSL I in the hospital; the majority were discharged to hospice care (80%).The mean days for an initial IPC consultation following admission was 3 on the medical/surgical floors and 7 days for ICU (P = .003; 95% CI, -6.37 to 1.36).
The number of days from admission to family meeting was 6.4 days on the medical/surgical floors, 10.4 days in ICU (P = .01; 95% CI, -7.21 to 0.81) (Table 3). Overall, 80% of consultation patients were discharged with hospice services.Recommended Reading
Related Articles
-
Program Profile
Expanding the Scope of Telemedicine in Gastroenterology
- Author:
- Michelle Huntzinger, RN
- Klaus Bielefeldt, MD, PhD
A specialty outreach program relied on telemedicine to reach patients with gastrointestinal and liver diseases in a large service area.
-
Program Profile
Interprofessional Education in Patient Aligned Care Team Primary Care-Mental Health Integration
- Author:
- Rachel Molander, MD
- Kathleen Hodgkins, MSSW, LCSW
- Catherine Johnson, PharmD, MS, BCPP
- Anna White, BCPP
- Erica Frazier, BCPP
- Dean Krahn, MD
Interprofessional education is an effective approach for preparing health care providers
for team-based practice. -
Pilot Program
Addressing the Needs of Patients With Chronic Pain
- Author:
- Alisher R. Dadabayev, MD
- Brent Coy, PhD
- Todd Bailey
- Andrew J. Grzesiak
- Livia Franchina, RPh
- Mark S. Hausman, MD
- Sarah Krein, PhD, RN
A novel interdisciplinary team approach within a primary care setting may be a promising model for delivering effective treatment options for...