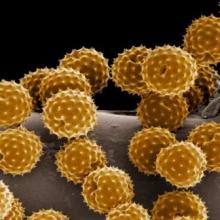
during ragweed pollen season, compared with placebo, according to recent research that was to be presented as an abstract for the American Academy of Allergy, Asthma & Immunology annual meeting. The AAAAI canceled its annual meeting and provided abstracts and access to presenters for press coverage.
David I. Bernstein, MD, professor emeritus in the division of immunology, allergy and rheumatology at the University of Cincinnati and principal investigator at the Bernstein Clinical Research Center, examined exploratory endpoints of an international, double-blind, placebo-controlled trial evaluating ragweed SLIT tablets (Ragwitek; Merck) in 1,022 children with AR/C. The children enrolled were aged 5-17 years with ragweed AR/C, with 42.7% of the group having a history of asthma and the rest without asthma. Participants were included if they had a predicted first expiratory volume in 1 second (FEV1) of ≥ 80% and if they required high-dose inhaled corticosteroids (ICS) to control their asthma or had severe, unstable, or uncontrolled asthma. The children were randomized to receive a 12 Amb a 1-unit dose of the ragweed SLIT tablet or placebo each day for 28 weeks.
The primary outcome was the total combined score (TCS), which was the sum of the daily symptom score and medication scores during ragweed season, but researchers also examined three exploratory endpoints. All patients were evaluated for their average asthma daily symptom score at the peak of ragweed pollen season and during the entire season, which was measured on a 0-3 scale based on symptoms of cough, wheeze, and chest tightness or shortness of breath. Within a subgroup of 406 participants with asthma, Dr. Bernstein and colleagues examined use of average daily short-acting beta agonists (SABA), and the number of times per week a participant would use a SABA at night at the peak of ragweed season as well as across the whole season.
Researchers found the TCS improved by 38% during ragweed pollen season in the group receiving ragweed SLIT tablets (least-square [LS] mean TCS, 7.12), compared with placebo (LS mean TCS, 4.39; P < .001). Among the asthma exploratory outcomes, asthma daily symptom scores improved by 30.7% during the peak of the season (–46.9% vs. –9.6%; LS mean difference, –0.13) and by 23.1% during the whole season (–38.7% vs. –2.3%; LS mean difference, –0.09), compared with the placebo group. The mean number of daily puffs of rescue medication also decreased by 68.1% in the peak of ragweed season (–87.6% vs. –39.0%; LS mean difference, −0.14) and by 61.4% during the whole season (–80.9% vs. −32.9%; LS mean difference, –0.12) among participants taking ragweed SLIT tablets, compared with placebo. Participants in the group receiving ragweed SLIT tablets also had fewer nights awake using rescue medication, with a relative improvement of 75.1% during peak season (−99.3% vs. −35.2%; LS mean difference, −0.08) and 52.2% during the whole season (−80.4% vs. −3.7%; LS mean difference, −0.03), compared with the placebo group.
This magnitude of difference in the number of nocturnal awakenings in the treated group, compared with the placebo group, is similar to what researchers have seen in trials evaluating ICS or mometasone/formoterol, Dr. Bernstein said in an interview.
“Even though the magnitude in terms of difference in asthma symptoms and requirements for short-acting beta agonists was less than that of other studies of other drugs, it may reflect the fact these participants have less severe asthma,” said Dr. Bernstein. “But, there was an effect, and we did see some interesting differences between the placebo group and the treated group. This, I think, does generate at least a hypothesis that this could be an effective treatment for seasonal asthma, which would require future studies to determine that.”
Dr. Bernstein said that there were no adverse events from ragweed SLIT tablets unique to children with or without asthma, and although the data from this study cannot be compared directly to an adult population, there appeared to be a greater effect size for children than in trials evaluating adults. Compared with treatment options like subcutaneous immunotherapy, ragweed SLIT tablets may offer a relatively safer and more effective option for children and their parents, he said.
“The problem with kids is that they don’t particularly like the idea of getting injections. There’s a lot of needle-type injection phobia,” Dr. Bernstein said. “For a child who has maybe one or two major problem pollen seasons like during the ragweed and grass, they could do this.”