Evolving Therapeutic Goals in Crohn’s Disease Management
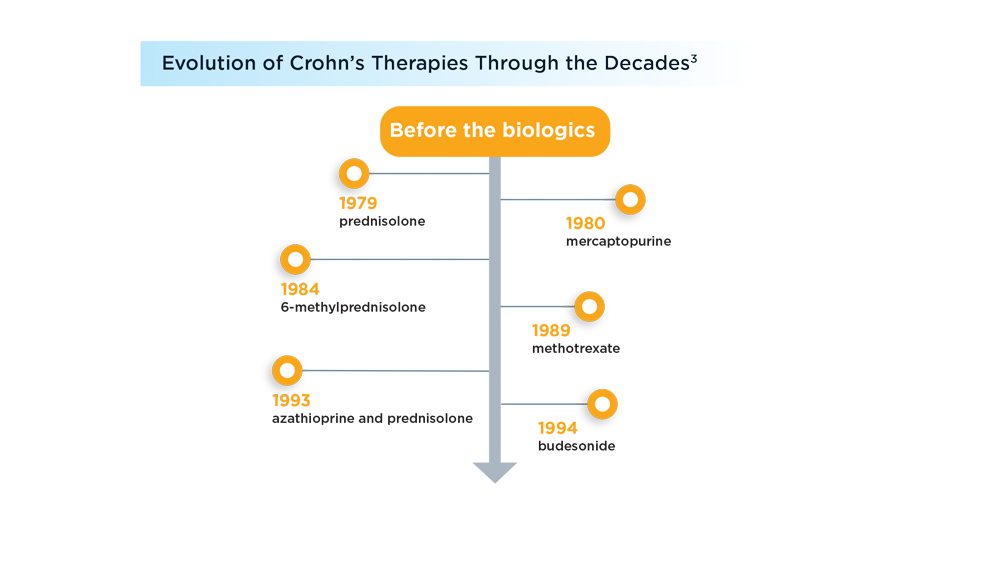
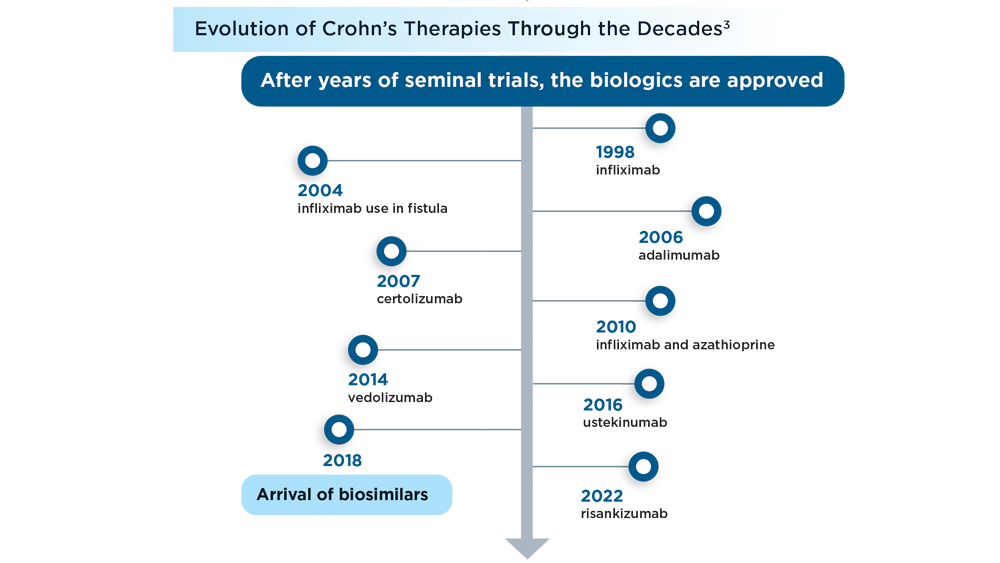
Over the last 2 decades, the armamentarium for Crohn’s disease has expanded with the introduction of targeted biologic therapies. Beginning with the approval of infliximab by the FDA in 1998, the treatment options for Crohn’s disease have greatly improved.1 Although steroids are still prescribed too frequently, novel therapies now can limit the use of steroids in these patients.2 In addition to anti-tumor necrosis factor alpha (anti-TNF-alpha) biologics, new therapies that target integrins, interleukin (IL)-12/23, and IL-23 have also demonstrated efficacy in inducing and maintaining clinical and endoscopic remission of Crohn’s disease.3
Other studies have shown what consistent therapeutic control can do for patients with Crohn’s disease. Effective therapies can maintain remission and even halt progression to complications if the disease is identified and treated in its early stages.4,5 Since the early 2000s, a significant drop in risk for surgery among patients with Crohn’s has also been observed because of improved management.6 Of course, patient acceptance and adherence to their regimens is critical. Patients who understand they need on-time treatment, have access to appropriate treatment, and get their questions answered in a timely fashion will be more adherent than those who do not.7 A key advance in management is the adoption of a treat-to-target strategy in which the therapeutic goal has evolved beyond symptom improvement to include the achievement of objective metrics of remission, in particular endoscopic healing.8
These successes are juxtaposed against Crohn’s disease incidence and prevalence figures, which are rising mostly everywhere.9 In 1999, 1.8 million adults in the United States had the disease; in 2015, that figure was 3.1 million.10 Crohn’s disease, usually considered a younger adult disease, is also growing in incidence in adults older than 60 years.9 While the underlying causes of this disease are not well understood, its development involves environmental factors, dysregulated innate and adaptive immune systems, and genetic predisposition.11 With increasing investigation focused on understanding the disease’s initial triggering events and how environmental factors, like diet, affect Crohn’s disease, there is hope these research findings will lead to better management and treatment options.12
1
-
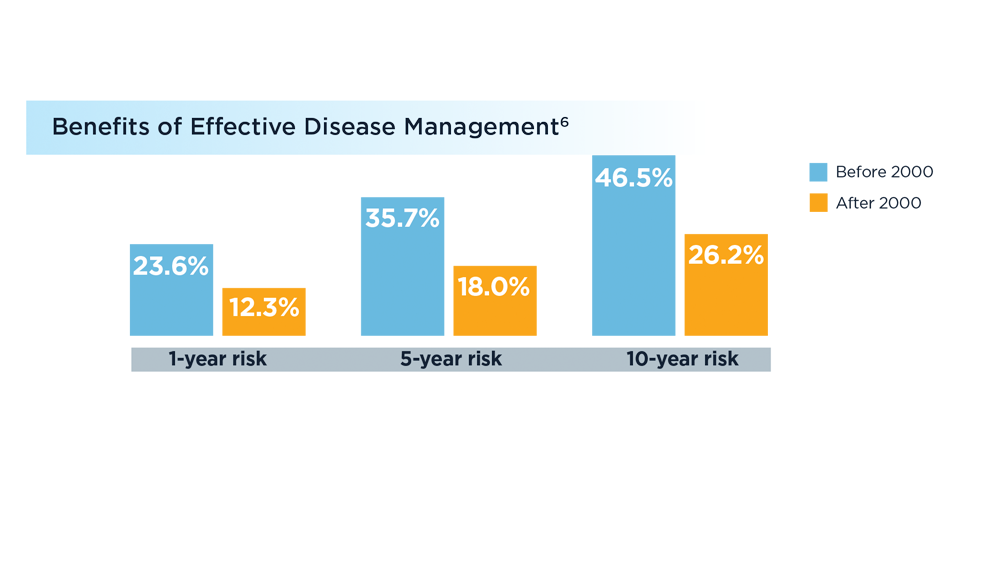
The risk of surgery for patients with Crohn's has been cut nearly in half (based on an analysis of 44 population-based cohort studies primarily in Europe and North America).
-
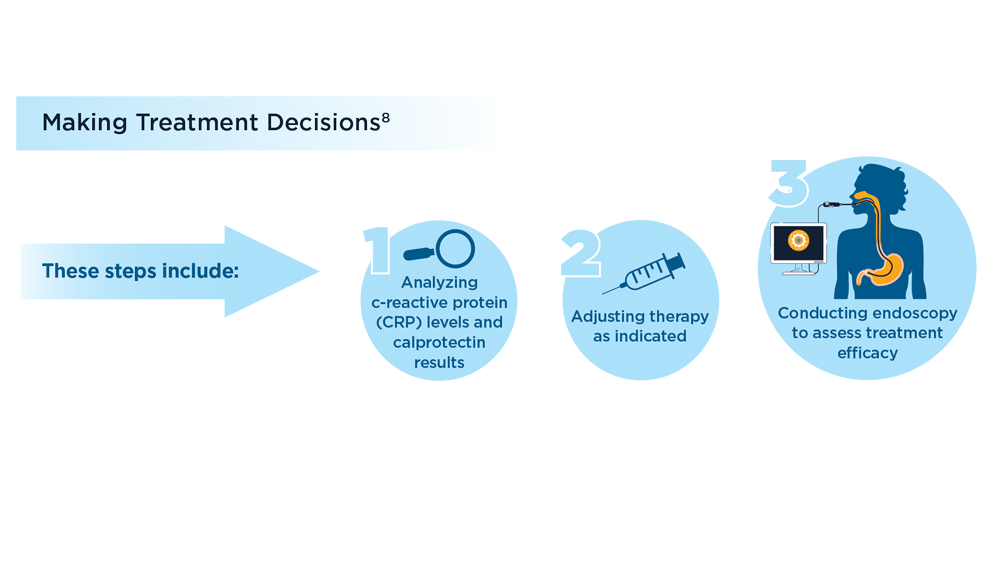
New treatment guidelines for IBD and related conditions like Crohn’s disease and ulcerative colitis now emphasize an iterative approach to management.
-
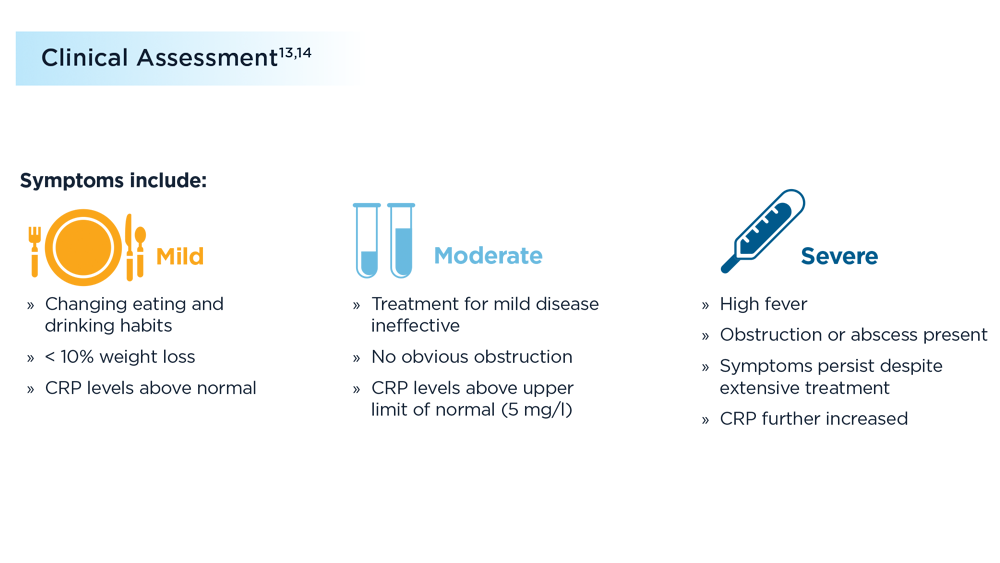
With Crohn’s disease, a decrease in symptoms is not necessarily indicative of a decrease in objective inflammation.
-
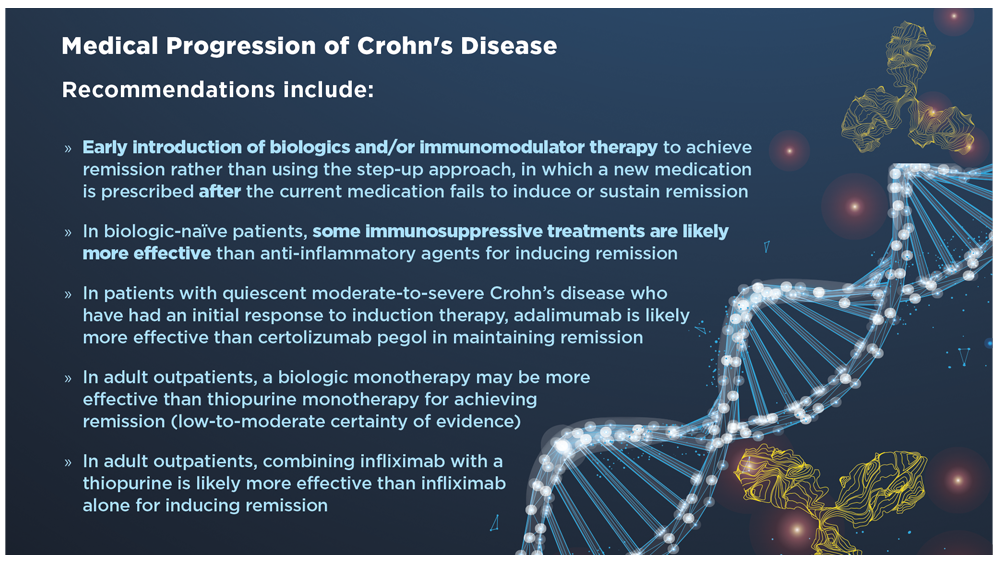
Patients with moderate-to-severe Crohn’s disease are at risk for disease complications including surgery, hospitalization, dependence on corticosteroids, infections, fistulae, and strictures (only moderate certainty of evidence included). The AGA released a technical review in 2021 aimed at answering key clinical questions in the management of moderate-to-severe Crohn’s disease.
-
-
More Crohn’s Disease News
Crohn's Disease Management



