User login
Sacral neuromodulation stimulation (SNS) offers a less invasive alternative treatment for a difficult challenge: how to improve quality of life for patients with refractory lower urinary/pelvic floor disorders. In the past, the options were limited to radical surgical procedures such as urinary diversion, augmentation cystoplasty, or cystectomy.
The neuromodulation technique has been used for treatment of other disorders such as deep brain stimulation for Parkinson’s disease and vagal nerve stimulation for epilepsy. SNS stimulates the sacral nerves to modulate the neural reflexes that influence the bladder sphincter and pelvic floor.
The implantable InterStim device is FDA approved for the treatment of both storage and release disorders:
This article discusses several clinical trials that investigated its effectiveness, indications, and adverse events.
InterStim: The backstory
What is InterStim?
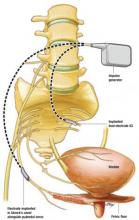
InterStim is an implantable system comprising a lead with 4 electrodes, an extension cable, and a programmable impulse generator. Usually, the lead is implanted into the S3 sacral nerve root, and the impulse generator is placed in the upper buttock region.
FDA approval
SNS for lower urinary tract disorders has been under investigation in clinical trials since 1981 and in multicenter trials conducted during the late 1980s. In 1997, the sacral neuromodulation system, InterStim (Medtronic Corp, Minneapolis, Minn), was FDA approved for treatment of urge incontinence, and, in 1999, for treatment of urinary frequency and urinary retention.
For tough cases
This method of therapy has proven to be an alternative treatment for a difficult patient group—those in whom pharmacological and behavioral management have failed. Therefore, considerable interest continues in the development of this method of therapy.
The delicate balance of stimulation and inhibition
A review of the neuroanatomy helps to explain the possible underlying mechanism of the workings of SNS. In the human, stimulation of the parasympathetic system through the pelvic nerves (S2–S4) leads to bladder emptying, and stimulation of the sympathetic system through the hypogastric nerves (T10–L2) leads to inhibition of bladder emptying.
The pudendal nerve receives information from Onuf’s nucleus in the S2–S4 level and innervates the skeletal muscle of the pelvic floor/external urethral sphincter.
The contraction and relaxation of these muscles are integral to micturition and bladder storage. A physiologic coordination exists between the somatic and the autonomic nervous system; it is when this delicate balance of stimulation and inhibition is changed by disease states that problems of urinary urgency, urge incontinence, and urinary retention result. Two guarding reflexes also work to prevent incontinence:
Bladder afferent pathways are mediated by unmyelinated C fibers (which detect noxious stimuli and trigger voiding) and small myelinated A fibers (which detect bladder muscle tension or fullness). Pudendal afferent input can turn on voiding reflexes by suppressing the guarding reflex pathways, and pudendal afferent input can also turn off overactive voiding by blocking ascending sensory pathways.
Thus, stimulation of the sacral nerves through pudendal afferent signaling influences bladder storage and emptying. Sacral neuromodulation affects these mechanisms by stimulating the somatic afferent inhibition of sensory processing in the spinal cord.
Does SNS successfully treat unrelenting urgency–frequency?
EFFICACY AND SAFETY
Hassouna M, Siegel S, Nyeholt A, et al. Sacral neuromodulation in the treatment of urgency–frequency symptoms: a multicenter study on efficacy and safety. J Urol. 2000;163:1849–1854.
All patients in this small, prospective, multicenter randomized trial had refractory urinary urgency–frequency. They completed extensive urologic evaluation consisting of voiding diaries, urodynamic testing, physical examination, and symptom questionnaires. Of the 51 patients, 90% were female and 10% were male. All patients underwent an office-based percutaneous stimulation trial of 3 to 7 days, to determine response to sacral nerve modulation. As practice guidelines dictate, a successful trial was determined if 50% or more of any urinary symptoms were relieved.
The patients were randomly assigned to 2 groups: the control group (n=26) that received no SNS and the study group (n=25), which underwent InterStim implantation. At 6 months, urinary symptoms in all patients were reassessed by urodynamic testing, SF-36 health survey, and voiding diaries.
In the control group, patients’ voiding diaries, symptoms, and urodynamic testing results remained unchanged. In the treatment group, 56% of patients had a greater than 50% reduction in the number of voids (<8) per day, compared with the control group. The treatment group had a significant increase in average voided volume from 118 to 226 cc, and a reduced degree of urgency. The treatment was associated with improved quality of life measured using the SF-36 health survey.
At 6 months, stimulation was turned off in 23 of the 26 patients in the treatment group. (One had the InterStim system explanted, and 2 refused to have the device turned off due to fear of return of symptoms.) When stimulation was turned off, symptoms did return to baseline. At 12 months, when the stimulation was turned back on, patients regained improvement in their urinary indices, which remained statistically significant. At 24 months, only 21 patients were evaluated on all analyses. The researchers reported that 43% of patients had maintained either fewer than 7 voids per day or at least a 50% reduction in the number of daily voids.
Although this report looked at effectiveness in only 51 patients, it did utilize a randomization method. A larger cohort, of 196 patients, was studied in a retrospective and prospective trial conducted by Spinelli and colleagues.
SHORT- AND LONG-TERM EFFICACY
Spinelli M, Bertapelle F, Cappellano F, et al, on behalf of the GINS Group. Chronic sacral neuromodulation in patients with lower urinary tract symptoms: results from a national register. J Urol. 2001;166:541–545.
A national register was created in Italy to collect results from all centers that were performing sacral neuromodulation. The investigators analyzed a total of 196 patients (46 males and 150 females).
Retrospective analysis
A total of 93 (18 male and 75 female) of the 196 were included, and 61 of the 93 patients were available for assessment. Mean follow-up was 41 months.
Prospective analysis
A total of 103 patients (28 males and 75 females) were followed, using voiding diaries, number of incontinence episodes, residual urine volume, number of catheterizations, pad use, and pain symptoms. Assessments were performed before percutaneous nerve evaluation and at 3-month intervals for 1 year, and at 6-month intervals for up to 2 years.
Detrusor instability. In the prospective register, 42 patients had detrusor instability. Compared with baseline, the mean number of incontinence episodes declined from 5.4 to1.1 at 12 months; 75% of patients had fewer than 8 micturitions per day at 3 months and 84% had fewer than 8 micturitions per day at 6 months, and this rate remained stable at 12 and 18 months. At 3 months, 57% of the study population was dry; at 6 months, 65% compared with baseline. At 18 months, 43% of the patients were completely dry. Improved quality of life was found in the patients with detrusor instability.
Voiding disorders. Of 103 patients, 35 had voiding disorders. At 3 and 6 months, 67% had stopped catheterization and 13% were catheterizing only once per day. At 9 and 12 months, 50% were not catheterizing and 33% to 13% were catheterizing once per day; 67% were not catheterizing at 18 months. However, the remaining 33% of patients had fluctuating results.
Complications and adverse events. In patients followed prospectively, 15.5% required surgical revision of the InterStim system due to pain at the implantation or to cable connection site or wound problems such as hematoma or lead fracture. Complete removal was performed in 3.9%.
ADDITIONAL REFERENCES
- Leng WW, Chancellor MB. How sacral nerve stimulation neuromodulation works. Urol Clin N Am. 2005;32:11–18.
- Weil EHJ, Ruiz-Cerda JL, Eerdsmans PHA, et al. Sacral root neuromodulation in the treatment of refractory urinary urge incontinence: a prospective randomized clinical trial. Eur Urol. 2000;37:161–171.
Sacral neuromodulation stimulation (SNS) is a minimally invasive treatment for refractory urinary urge incontinence, urinary urgency–frequency alone or in combination, and urinary retention
The InterStim implantable system comprises a lead with 4 electrodes and an extension cable. Its programmable impulse generator, usually placed in the upper buttock region, sends mild electrical pulses to the sacral nerve
Stimulation of the parasympathetic system through the pelvic nerves (S2–S4) leads to bladder emptying
Stimulation of the sympathetic system through the hypogastric nerves (T10–L2) leads to inhibition of bladder emptying
The pudendal nerve receives information from Onuf’s nucleus in the S2–S4 level and innervates the skeletal muscle of the pelvic floor/external urethral sphincter. Contraction and relaxation of these muscles are integral to micturition and bladder storage
2 guarding reflexes prevent incontinence: 1) between the bladder and the smooth muscles of the urethra, which is mediated by the efferent pathways of the sympathetic system, and2) between the afferent nerves in the bladder and the efferent pathways in the pudendal nerve, leading to contraction of the skeletal component of the urethra
Bladder afferent pathways are mediated by unmyelinated C fibers that detect noxious stimuli and trigger voiding, and by small myelinated A fibers that detect bladder muscle tension or fullness
Pudendal afferent input can turn on voiding reflexes by suppressing the guarding reflex pathways, and turn off overactive voiding by blocking ascending sensory pathways
Fecal incontinence improved, with and without treatment
Leroi AM, Parc Y, Lehur PA, et al. Efficacy of sacral nerve stimulation for fecal incontinence. Results of a multicenter double-blind crossover study. Ann Surg. 2005;242:662–669.
In this randomized crossover trial, 24 patients with fecal incontinence at least once a week for 3 months received InterStim. Patients were randomized to have the device ON or OFF for 1 month, and in the opposite mode (OFF or ON) for the 2nd month. At the end of the study, patients were given the option of keeping the SNS ON or OFF. Patients and outcome assessors were blinded to treatment assignment. All patients completed the study.
Primary outcomes were number of weekly incontinence and urgency episodes and mean delay for postponing defecation measured with patient diaries; quality of life as measured by the Cleveland Clinic score; and manometric data.
The median frequency of fecal incontinence episodes was significantly decreased in the ON mode compared with the OFF mode. There was improvement in quality of life scores as well. There was no significant change in the frequency of urgency episodes, the delay in postponing defecation, or number of bowel movements per week. There was an increase in maximum anal resting pressure in the ON mode. There were no differences in any other manometric parameters between the 2 modes.
Although symptoms improved markedly during the ON crossover mode, there was also significant improvement in the OFF mode compared with baseline. The median frequency of fecal incontinence episodes decreased by 90% in the ON mode, but also decreased by 76% in the OFF mode. Also, 89% of patients reported improvement during the ON mode and 63% reported improvement during the OFF mode.
It is unclear if subjects were aware of which mode setting they were randomized to, or if there was significant placebo effect.
ADDITIONAL REFERENCES
- Rasmussen OO, Buntzen S, Sorensen M, Laurberg S, Christiansen J. Sacral nerve stimulation in fecal incontinence. Dis Colon Rectum. 2004;47:1158–1163.
Does the pudendal mini-stimulator improve detrusor overactivity?
Groen J, Amiel C, Rudd Bosch JLH. Chronic pudendal nerve neuromodulation in women with idiopathic refractory detrusor overactivity incontinence: results of a pilot study with a novel minimally invasive implantable mini-stimulator. Neurourol Urodynam. 2005;24:226–230.
The effectiveness of sacral neuromodulation has sparked innovations for other forms of neuromodulation besides the InterStim system. Utilizing the effects of stimulation on the pudendal afferents and in hopes of achieving similar results without central sacral stimulation, another type of neuromodulation has been developed: direct stimulation of the pudendal nerve by the Bion Device (Advanced Bionics Corp., Valencia, Calif). It is a self-contained, battery-powered mini-neurostimulator with integrated electrodes. It measures 28 x 3.3 mm and weighs 0.7 grams.
It is implanted in a minimally invasive fashion adjacent to the pudendal nerve at Alcock’s canal.
Other treatments had failed. This pilot study by Groen and colleagues evaluated short-term results of 6 women with refractory detrusor overactivity, in whom conservative and medical therapy and various forms of neuromodulation were unsuccessful, and who had positive percutaneous pudendal nerve screening tests.
Voiding–incontinence diaries, cystometrics, and the SF-36 quality-of-life health survey were measured. Women were followed for 6 months with the device ON, and for an additional 2 weeks with the device OFF.
Higher bladder volume remained better or returned to baseline
At the end of the 6-month ON period, the number of incontinence episodes per day, number of pads used per day, and leakage severity index decreased significantly compared with baseline (P<.05 for all). Cystometric comparisons revealed a higher bladder volume at the first involuntary detrusor contraction (P<.05). These values returned toward baseline when the device was turned OFF, although in most cases, still remained better than baseline.
There were no statistically significant changes in the 8 domains of the SF-36 survey, likely due to the small number of patients.
ADDITIONAL REFERENCES
- Bosch JLHR. The Bion Device: a minimally invasive implantable ministimulator for pudendal nerve neuromodulation in patients with detrusor overactivity incontinence. Urol Clin N Am. 2005;32:109–112.
- Daneshgari F. Applications of neuromodulation of the lower urinary tract in female urology. Int Braz J Urol. 2006;32:262–272.
- Spinelli M, Malaguti S, Giardiello G, et al. A new minimally invasive procedure for pudendal nerve stimulation to treat neurogenic bladder: description of the method and preliminary data. Neurourol Urodynam. 2005;24:305–309.
Sacral neuromodulation stimulation (SNS) offers a less invasive alternative treatment for a difficult challenge: how to improve quality of life for patients with refractory lower urinary/pelvic floor disorders. In the past, the options were limited to radical surgical procedures such as urinary diversion, augmentation cystoplasty, or cystectomy.
The neuromodulation technique has been used for treatment of other disorders such as deep brain stimulation for Parkinson’s disease and vagal nerve stimulation for epilepsy. SNS stimulates the sacral nerves to modulate the neural reflexes that influence the bladder sphincter and pelvic floor.
The implantable InterStim device is FDA approved for the treatment of both storage and release disorders:
This article discusses several clinical trials that investigated its effectiveness, indications, and adverse events.
InterStim: The backstory
What is InterStim?
InterStim is an implantable system comprising a lead with 4 electrodes, an extension cable, and a programmable impulse generator. Usually, the lead is implanted into the S3 sacral nerve root, and the impulse generator is placed in the upper buttock region.
FDA approval
SNS for lower urinary tract disorders has been under investigation in clinical trials since 1981 and in multicenter trials conducted during the late 1980s. In 1997, the sacral neuromodulation system, InterStim (Medtronic Corp, Minneapolis, Minn), was FDA approved for treatment of urge incontinence, and, in 1999, for treatment of urinary frequency and urinary retention.
For tough cases
This method of therapy has proven to be an alternative treatment for a difficult patient group—those in whom pharmacological and behavioral management have failed. Therefore, considerable interest continues in the development of this method of therapy.
The delicate balance of stimulation and inhibition
A review of the neuroanatomy helps to explain the possible underlying mechanism of the workings of SNS. In the human, stimulation of the parasympathetic system through the pelvic nerves (S2–S4) leads to bladder emptying, and stimulation of the sympathetic system through the hypogastric nerves (T10–L2) leads to inhibition of bladder emptying.
The pudendal nerve receives information from Onuf’s nucleus in the S2–S4 level and innervates the skeletal muscle of the pelvic floor/external urethral sphincter.
The contraction and relaxation of these muscles are integral to micturition and bladder storage. A physiologic coordination exists between the somatic and the autonomic nervous system; it is when this delicate balance of stimulation and inhibition is changed by disease states that problems of urinary urgency, urge incontinence, and urinary retention result. Two guarding reflexes also work to prevent incontinence:
Bladder afferent pathways are mediated by unmyelinated C fibers (which detect noxious stimuli and trigger voiding) and small myelinated A fibers (which detect bladder muscle tension or fullness). Pudendal afferent input can turn on voiding reflexes by suppressing the guarding reflex pathways, and pudendal afferent input can also turn off overactive voiding by blocking ascending sensory pathways.
Thus, stimulation of the sacral nerves through pudendal afferent signaling influences bladder storage and emptying. Sacral neuromodulation affects these mechanisms by stimulating the somatic afferent inhibition of sensory processing in the spinal cord.
Does SNS successfully treat unrelenting urgency–frequency?
EFFICACY AND SAFETY
Hassouna M, Siegel S, Nyeholt A, et al. Sacral neuromodulation in the treatment of urgency–frequency symptoms: a multicenter study on efficacy and safety. J Urol. 2000;163:1849–1854.
All patients in this small, prospective, multicenter randomized trial had refractory urinary urgency–frequency. They completed extensive urologic evaluation consisting of voiding diaries, urodynamic testing, physical examination, and symptom questionnaires. Of the 51 patients, 90% were female and 10% were male. All patients underwent an office-based percutaneous stimulation trial of 3 to 7 days, to determine response to sacral nerve modulation. As practice guidelines dictate, a successful trial was determined if 50% or more of any urinary symptoms were relieved.
The patients were randomly assigned to 2 groups: the control group (n=26) that received no SNS and the study group (n=25), which underwent InterStim implantation. At 6 months, urinary symptoms in all patients were reassessed by urodynamic testing, SF-36 health survey, and voiding diaries.
In the control group, patients’ voiding diaries, symptoms, and urodynamic testing results remained unchanged. In the treatment group, 56% of patients had a greater than 50% reduction in the number of voids (<8) per day, compared with the control group. The treatment group had a significant increase in average voided volume from 118 to 226 cc, and a reduced degree of urgency. The treatment was associated with improved quality of life measured using the SF-36 health survey.
At 6 months, stimulation was turned off in 23 of the 26 patients in the treatment group. (One had the InterStim system explanted, and 2 refused to have the device turned off due to fear of return of symptoms.) When stimulation was turned off, symptoms did return to baseline. At 12 months, when the stimulation was turned back on, patients regained improvement in their urinary indices, which remained statistically significant. At 24 months, only 21 patients were evaluated on all analyses. The researchers reported that 43% of patients had maintained either fewer than 7 voids per day or at least a 50% reduction in the number of daily voids.
Although this report looked at effectiveness in only 51 patients, it did utilize a randomization method. A larger cohort, of 196 patients, was studied in a retrospective and prospective trial conducted by Spinelli and colleagues.
SHORT- AND LONG-TERM EFFICACY
Spinelli M, Bertapelle F, Cappellano F, et al, on behalf of the GINS Group. Chronic sacral neuromodulation in patients with lower urinary tract symptoms: results from a national register. J Urol. 2001;166:541–545.
A national register was created in Italy to collect results from all centers that were performing sacral neuromodulation. The investigators analyzed a total of 196 patients (46 males and 150 females).
Retrospective analysis
A total of 93 (18 male and 75 female) of the 196 were included, and 61 of the 93 patients were available for assessment. Mean follow-up was 41 months.
Prospective analysis
A total of 103 patients (28 males and 75 females) were followed, using voiding diaries, number of incontinence episodes, residual urine volume, number of catheterizations, pad use, and pain symptoms. Assessments were performed before percutaneous nerve evaluation and at 3-month intervals for 1 year, and at 6-month intervals for up to 2 years.
Detrusor instability. In the prospective register, 42 patients had detrusor instability. Compared with baseline, the mean number of incontinence episodes declined from 5.4 to1.1 at 12 months; 75% of patients had fewer than 8 micturitions per day at 3 months and 84% had fewer than 8 micturitions per day at 6 months, and this rate remained stable at 12 and 18 months. At 3 months, 57% of the study population was dry; at 6 months, 65% compared with baseline. At 18 months, 43% of the patients were completely dry. Improved quality of life was found in the patients with detrusor instability.
Voiding disorders. Of 103 patients, 35 had voiding disorders. At 3 and 6 months, 67% had stopped catheterization and 13% were catheterizing only once per day. At 9 and 12 months, 50% were not catheterizing and 33% to 13% were catheterizing once per day; 67% were not catheterizing at 18 months. However, the remaining 33% of patients had fluctuating results.
Complications and adverse events. In patients followed prospectively, 15.5% required surgical revision of the InterStim system due to pain at the implantation or to cable connection site or wound problems such as hematoma or lead fracture. Complete removal was performed in 3.9%.
ADDITIONAL REFERENCES
- Leng WW, Chancellor MB. How sacral nerve stimulation neuromodulation works. Urol Clin N Am. 2005;32:11–18.
- Weil EHJ, Ruiz-Cerda JL, Eerdsmans PHA, et al. Sacral root neuromodulation in the treatment of refractory urinary urge incontinence: a prospective randomized clinical trial. Eur Urol. 2000;37:161–171.
Sacral neuromodulation stimulation (SNS) is a minimally invasive treatment for refractory urinary urge incontinence, urinary urgency–frequency alone or in combination, and urinary retention
The InterStim implantable system comprises a lead with 4 electrodes and an extension cable. Its programmable impulse generator, usually placed in the upper buttock region, sends mild electrical pulses to the sacral nerve
Stimulation of the parasympathetic system through the pelvic nerves (S2–S4) leads to bladder emptying
Stimulation of the sympathetic system through the hypogastric nerves (T10–L2) leads to inhibition of bladder emptying
The pudendal nerve receives information from Onuf’s nucleus in the S2–S4 level and innervates the skeletal muscle of the pelvic floor/external urethral sphincter. Contraction and relaxation of these muscles are integral to micturition and bladder storage
2 guarding reflexes prevent incontinence: 1) between the bladder and the smooth muscles of the urethra, which is mediated by the efferent pathways of the sympathetic system, and2) between the afferent nerves in the bladder and the efferent pathways in the pudendal nerve, leading to contraction of the skeletal component of the urethra
Bladder afferent pathways are mediated by unmyelinated C fibers that detect noxious stimuli and trigger voiding, and by small myelinated A fibers that detect bladder muscle tension or fullness
Pudendal afferent input can turn on voiding reflexes by suppressing the guarding reflex pathways, and turn off overactive voiding by blocking ascending sensory pathways
Fecal incontinence improved, with and without treatment
Leroi AM, Parc Y, Lehur PA, et al. Efficacy of sacral nerve stimulation for fecal incontinence. Results of a multicenter double-blind crossover study. Ann Surg. 2005;242:662–669.
In this randomized crossover trial, 24 patients with fecal incontinence at least once a week for 3 months received InterStim. Patients were randomized to have the device ON or OFF for 1 month, and in the opposite mode (OFF or ON) for the 2nd month. At the end of the study, patients were given the option of keeping the SNS ON or OFF. Patients and outcome assessors were blinded to treatment assignment. All patients completed the study.
Primary outcomes were number of weekly incontinence and urgency episodes and mean delay for postponing defecation measured with patient diaries; quality of life as measured by the Cleveland Clinic score; and manometric data.
The median frequency of fecal incontinence episodes was significantly decreased in the ON mode compared with the OFF mode. There was improvement in quality of life scores as well. There was no significant change in the frequency of urgency episodes, the delay in postponing defecation, or number of bowel movements per week. There was an increase in maximum anal resting pressure in the ON mode. There were no differences in any other manometric parameters between the 2 modes.
Although symptoms improved markedly during the ON crossover mode, there was also significant improvement in the OFF mode compared with baseline. The median frequency of fecal incontinence episodes decreased by 90% in the ON mode, but also decreased by 76% in the OFF mode. Also, 89% of patients reported improvement during the ON mode and 63% reported improvement during the OFF mode.
It is unclear if subjects were aware of which mode setting they were randomized to, or if there was significant placebo effect.
ADDITIONAL REFERENCES
- Rasmussen OO, Buntzen S, Sorensen M, Laurberg S, Christiansen J. Sacral nerve stimulation in fecal incontinence. Dis Colon Rectum. 2004;47:1158–1163.
Does the pudendal mini-stimulator improve detrusor overactivity?
Groen J, Amiel C, Rudd Bosch JLH. Chronic pudendal nerve neuromodulation in women with idiopathic refractory detrusor overactivity incontinence: results of a pilot study with a novel minimally invasive implantable mini-stimulator. Neurourol Urodynam. 2005;24:226–230.
The effectiveness of sacral neuromodulation has sparked innovations for other forms of neuromodulation besides the InterStim system. Utilizing the effects of stimulation on the pudendal afferents and in hopes of achieving similar results without central sacral stimulation, another type of neuromodulation has been developed: direct stimulation of the pudendal nerve by the Bion Device (Advanced Bionics Corp., Valencia, Calif). It is a self-contained, battery-powered mini-neurostimulator with integrated electrodes. It measures 28 x 3.3 mm and weighs 0.7 grams.
It is implanted in a minimally invasive fashion adjacent to the pudendal nerve at Alcock’s canal.
Other treatments had failed. This pilot study by Groen and colleagues evaluated short-term results of 6 women with refractory detrusor overactivity, in whom conservative and medical therapy and various forms of neuromodulation were unsuccessful, and who had positive percutaneous pudendal nerve screening tests.
Voiding–incontinence diaries, cystometrics, and the SF-36 quality-of-life health survey were measured. Women were followed for 6 months with the device ON, and for an additional 2 weeks with the device OFF.
Higher bladder volume remained better or returned to baseline
At the end of the 6-month ON period, the number of incontinence episodes per day, number of pads used per day, and leakage severity index decreased significantly compared with baseline (P<.05 for all). Cystometric comparisons revealed a higher bladder volume at the first involuntary detrusor contraction (P<.05). These values returned toward baseline when the device was turned OFF, although in most cases, still remained better than baseline.
There were no statistically significant changes in the 8 domains of the SF-36 survey, likely due to the small number of patients.
ADDITIONAL REFERENCES
- Bosch JLHR. The Bion Device: a minimally invasive implantable ministimulator for pudendal nerve neuromodulation in patients with detrusor overactivity incontinence. Urol Clin N Am. 2005;32:109–112.
- Daneshgari F. Applications of neuromodulation of the lower urinary tract in female urology. Int Braz J Urol. 2006;32:262–272.
- Spinelli M, Malaguti S, Giardiello G, et al. A new minimally invasive procedure for pudendal nerve stimulation to treat neurogenic bladder: description of the method and preliminary data. Neurourol Urodynam. 2005;24:305–309.
Sacral neuromodulation stimulation (SNS) offers a less invasive alternative treatment for a difficult challenge: how to improve quality of life for patients with refractory lower urinary/pelvic floor disorders. In the past, the options were limited to radical surgical procedures such as urinary diversion, augmentation cystoplasty, or cystectomy.
The neuromodulation technique has been used for treatment of other disorders such as deep brain stimulation for Parkinson’s disease and vagal nerve stimulation for epilepsy. SNS stimulates the sacral nerves to modulate the neural reflexes that influence the bladder sphincter and pelvic floor.
The implantable InterStim device is FDA approved for the treatment of both storage and release disorders:
This article discusses several clinical trials that investigated its effectiveness, indications, and adverse events.
InterStim: The backstory
What is InterStim?
InterStim is an implantable system comprising a lead with 4 electrodes, an extension cable, and a programmable impulse generator. Usually, the lead is implanted into the S3 sacral nerve root, and the impulse generator is placed in the upper buttock region.
FDA approval
SNS for lower urinary tract disorders has been under investigation in clinical trials since 1981 and in multicenter trials conducted during the late 1980s. In 1997, the sacral neuromodulation system, InterStim (Medtronic Corp, Minneapolis, Minn), was FDA approved for treatment of urge incontinence, and, in 1999, for treatment of urinary frequency and urinary retention.
For tough cases
This method of therapy has proven to be an alternative treatment for a difficult patient group—those in whom pharmacological and behavioral management have failed. Therefore, considerable interest continues in the development of this method of therapy.
The delicate balance of stimulation and inhibition
A review of the neuroanatomy helps to explain the possible underlying mechanism of the workings of SNS. In the human, stimulation of the parasympathetic system through the pelvic nerves (S2–S4) leads to bladder emptying, and stimulation of the sympathetic system through the hypogastric nerves (T10–L2) leads to inhibition of bladder emptying.
The pudendal nerve receives information from Onuf’s nucleus in the S2–S4 level and innervates the skeletal muscle of the pelvic floor/external urethral sphincter.
The contraction and relaxation of these muscles are integral to micturition and bladder storage. A physiologic coordination exists between the somatic and the autonomic nervous system; it is when this delicate balance of stimulation and inhibition is changed by disease states that problems of urinary urgency, urge incontinence, and urinary retention result. Two guarding reflexes also work to prevent incontinence:
Bladder afferent pathways are mediated by unmyelinated C fibers (which detect noxious stimuli and trigger voiding) and small myelinated A fibers (which detect bladder muscle tension or fullness). Pudendal afferent input can turn on voiding reflexes by suppressing the guarding reflex pathways, and pudendal afferent input can also turn off overactive voiding by blocking ascending sensory pathways.
Thus, stimulation of the sacral nerves through pudendal afferent signaling influences bladder storage and emptying. Sacral neuromodulation affects these mechanisms by stimulating the somatic afferent inhibition of sensory processing in the spinal cord.
Does SNS successfully treat unrelenting urgency–frequency?
EFFICACY AND SAFETY
Hassouna M, Siegel S, Nyeholt A, et al. Sacral neuromodulation in the treatment of urgency–frequency symptoms: a multicenter study on efficacy and safety. J Urol. 2000;163:1849–1854.
All patients in this small, prospective, multicenter randomized trial had refractory urinary urgency–frequency. They completed extensive urologic evaluation consisting of voiding diaries, urodynamic testing, physical examination, and symptom questionnaires. Of the 51 patients, 90% were female and 10% were male. All patients underwent an office-based percutaneous stimulation trial of 3 to 7 days, to determine response to sacral nerve modulation. As practice guidelines dictate, a successful trial was determined if 50% or more of any urinary symptoms were relieved.
The patients were randomly assigned to 2 groups: the control group (n=26) that received no SNS and the study group (n=25), which underwent InterStim implantation. At 6 months, urinary symptoms in all patients were reassessed by urodynamic testing, SF-36 health survey, and voiding diaries.
In the control group, patients’ voiding diaries, symptoms, and urodynamic testing results remained unchanged. In the treatment group, 56% of patients had a greater than 50% reduction in the number of voids (<8) per day, compared with the control group. The treatment group had a significant increase in average voided volume from 118 to 226 cc, and a reduced degree of urgency. The treatment was associated with improved quality of life measured using the SF-36 health survey.
At 6 months, stimulation was turned off in 23 of the 26 patients in the treatment group. (One had the InterStim system explanted, and 2 refused to have the device turned off due to fear of return of symptoms.) When stimulation was turned off, symptoms did return to baseline. At 12 months, when the stimulation was turned back on, patients regained improvement in their urinary indices, which remained statistically significant. At 24 months, only 21 patients were evaluated on all analyses. The researchers reported that 43% of patients had maintained either fewer than 7 voids per day or at least a 50% reduction in the number of daily voids.
Although this report looked at effectiveness in only 51 patients, it did utilize a randomization method. A larger cohort, of 196 patients, was studied in a retrospective and prospective trial conducted by Spinelli and colleagues.
SHORT- AND LONG-TERM EFFICACY
Spinelli M, Bertapelle F, Cappellano F, et al, on behalf of the GINS Group. Chronic sacral neuromodulation in patients with lower urinary tract symptoms: results from a national register. J Urol. 2001;166:541–545.
A national register was created in Italy to collect results from all centers that were performing sacral neuromodulation. The investigators analyzed a total of 196 patients (46 males and 150 females).
Retrospective analysis
A total of 93 (18 male and 75 female) of the 196 were included, and 61 of the 93 patients were available for assessment. Mean follow-up was 41 months.
Prospective analysis
A total of 103 patients (28 males and 75 females) were followed, using voiding diaries, number of incontinence episodes, residual urine volume, number of catheterizations, pad use, and pain symptoms. Assessments were performed before percutaneous nerve evaluation and at 3-month intervals for 1 year, and at 6-month intervals for up to 2 years.
Detrusor instability. In the prospective register, 42 patients had detrusor instability. Compared with baseline, the mean number of incontinence episodes declined from 5.4 to1.1 at 12 months; 75% of patients had fewer than 8 micturitions per day at 3 months and 84% had fewer than 8 micturitions per day at 6 months, and this rate remained stable at 12 and 18 months. At 3 months, 57% of the study population was dry; at 6 months, 65% compared with baseline. At 18 months, 43% of the patients were completely dry. Improved quality of life was found in the patients with detrusor instability.
Voiding disorders. Of 103 patients, 35 had voiding disorders. At 3 and 6 months, 67% had stopped catheterization and 13% were catheterizing only once per day. At 9 and 12 months, 50% were not catheterizing and 33% to 13% were catheterizing once per day; 67% were not catheterizing at 18 months. However, the remaining 33% of patients had fluctuating results.
Complications and adverse events. In patients followed prospectively, 15.5% required surgical revision of the InterStim system due to pain at the implantation or to cable connection site or wound problems such as hematoma or lead fracture. Complete removal was performed in 3.9%.
ADDITIONAL REFERENCES
- Leng WW, Chancellor MB. How sacral nerve stimulation neuromodulation works. Urol Clin N Am. 2005;32:11–18.
- Weil EHJ, Ruiz-Cerda JL, Eerdsmans PHA, et al. Sacral root neuromodulation in the treatment of refractory urinary urge incontinence: a prospective randomized clinical trial. Eur Urol. 2000;37:161–171.
Sacral neuromodulation stimulation (SNS) is a minimally invasive treatment for refractory urinary urge incontinence, urinary urgency–frequency alone or in combination, and urinary retention
The InterStim implantable system comprises a lead with 4 electrodes and an extension cable. Its programmable impulse generator, usually placed in the upper buttock region, sends mild electrical pulses to the sacral nerve
Stimulation of the parasympathetic system through the pelvic nerves (S2–S4) leads to bladder emptying
Stimulation of the sympathetic system through the hypogastric nerves (T10–L2) leads to inhibition of bladder emptying
The pudendal nerve receives information from Onuf’s nucleus in the S2–S4 level and innervates the skeletal muscle of the pelvic floor/external urethral sphincter. Contraction and relaxation of these muscles are integral to micturition and bladder storage
2 guarding reflexes prevent incontinence: 1) between the bladder and the smooth muscles of the urethra, which is mediated by the efferent pathways of the sympathetic system, and2) between the afferent nerves in the bladder and the efferent pathways in the pudendal nerve, leading to contraction of the skeletal component of the urethra
Bladder afferent pathways are mediated by unmyelinated C fibers that detect noxious stimuli and trigger voiding, and by small myelinated A fibers that detect bladder muscle tension or fullness
Pudendal afferent input can turn on voiding reflexes by suppressing the guarding reflex pathways, and turn off overactive voiding by blocking ascending sensory pathways
Fecal incontinence improved, with and without treatment
Leroi AM, Parc Y, Lehur PA, et al. Efficacy of sacral nerve stimulation for fecal incontinence. Results of a multicenter double-blind crossover study. Ann Surg. 2005;242:662–669.
In this randomized crossover trial, 24 patients with fecal incontinence at least once a week for 3 months received InterStim. Patients were randomized to have the device ON or OFF for 1 month, and in the opposite mode (OFF or ON) for the 2nd month. At the end of the study, patients were given the option of keeping the SNS ON or OFF. Patients and outcome assessors were blinded to treatment assignment. All patients completed the study.
Primary outcomes were number of weekly incontinence and urgency episodes and mean delay for postponing defecation measured with patient diaries; quality of life as measured by the Cleveland Clinic score; and manometric data.
The median frequency of fecal incontinence episodes was significantly decreased in the ON mode compared with the OFF mode. There was improvement in quality of life scores as well. There was no significant change in the frequency of urgency episodes, the delay in postponing defecation, or number of bowel movements per week. There was an increase in maximum anal resting pressure in the ON mode. There were no differences in any other manometric parameters between the 2 modes.
Although symptoms improved markedly during the ON crossover mode, there was also significant improvement in the OFF mode compared with baseline. The median frequency of fecal incontinence episodes decreased by 90% in the ON mode, but also decreased by 76% in the OFF mode. Also, 89% of patients reported improvement during the ON mode and 63% reported improvement during the OFF mode.
It is unclear if subjects were aware of which mode setting they were randomized to, or if there was significant placebo effect.
ADDITIONAL REFERENCES
- Rasmussen OO, Buntzen S, Sorensen M, Laurberg S, Christiansen J. Sacral nerve stimulation in fecal incontinence. Dis Colon Rectum. 2004;47:1158–1163.
Does the pudendal mini-stimulator improve detrusor overactivity?
Groen J, Amiel C, Rudd Bosch JLH. Chronic pudendal nerve neuromodulation in women with idiopathic refractory detrusor overactivity incontinence: results of a pilot study with a novel minimally invasive implantable mini-stimulator. Neurourol Urodynam. 2005;24:226–230.
The effectiveness of sacral neuromodulation has sparked innovations for other forms of neuromodulation besides the InterStim system. Utilizing the effects of stimulation on the pudendal afferents and in hopes of achieving similar results without central sacral stimulation, another type of neuromodulation has been developed: direct stimulation of the pudendal nerve by the Bion Device (Advanced Bionics Corp., Valencia, Calif). It is a self-contained, battery-powered mini-neurostimulator with integrated electrodes. It measures 28 x 3.3 mm and weighs 0.7 grams.
It is implanted in a minimally invasive fashion adjacent to the pudendal nerve at Alcock’s canal.
Other treatments had failed. This pilot study by Groen and colleagues evaluated short-term results of 6 women with refractory detrusor overactivity, in whom conservative and medical therapy and various forms of neuromodulation were unsuccessful, and who had positive percutaneous pudendal nerve screening tests.
Voiding–incontinence diaries, cystometrics, and the SF-36 quality-of-life health survey were measured. Women were followed for 6 months with the device ON, and for an additional 2 weeks with the device OFF.
Higher bladder volume remained better or returned to baseline
At the end of the 6-month ON period, the number of incontinence episodes per day, number of pads used per day, and leakage severity index decreased significantly compared with baseline (P<.05 for all). Cystometric comparisons revealed a higher bladder volume at the first involuntary detrusor contraction (P<.05). These values returned toward baseline when the device was turned OFF, although in most cases, still remained better than baseline.
There were no statistically significant changes in the 8 domains of the SF-36 survey, likely due to the small number of patients.
ADDITIONAL REFERENCES
- Bosch JLHR. The Bion Device: a minimally invasive implantable ministimulator for pudendal nerve neuromodulation in patients with detrusor overactivity incontinence. Urol Clin N Am. 2005;32:109–112.
- Daneshgari F. Applications of neuromodulation of the lower urinary tract in female urology. Int Braz J Urol. 2006;32:262–272.
- Spinelli M, Malaguti S, Giardiello G, et al. A new minimally invasive procedure for pudendal nerve stimulation to treat neurogenic bladder: description of the method and preliminary data. Neurourol Urodynam. 2005;24:305–309.