User login
The authors report no financial relationships relevant to this article.
CASE Large baby, extensive tear
A 28-year-old primigravida undergoes a forceps delivery with a midline episiotomy for failure to progress in the second stage of labor. At birth, the infant weighs 4 kg (8.8 lb), and the episiotomy extends to the anal verge. The resident who delivered the child is uncertain whether the anal sphincter is involved in the injury and asks a consultant to examine the perineum.
What should this examination entail?
The obstetrician is rarely culpable when a third- or fourth-degree obstetric anal sphincter injury (OASIS) occurs—but there is little excuse for letting one go undetected.
To minimize the risk of undiagnosed OASIS, a digital anorectal examination is warranted—before any suturing—in every woman who delivers vaginally. This practice can help you avoid missing isolated tears, such as “buttonhole” of the rectal mucosa, which can occur even when the anal sphincter remains intact (FIGURE 1), or a third- or fourth-degree tear that can sometimes be present behind apparently intact perineal skin (FIGURE 2).1
Clinical training of physicians and midwives also needs to improve.
Every labor room should have a protocol for management of anal sphincter injury2; this article describes detection, diagnosis, and management, focusing on seven critical questions.
Only a physician formally trained in primary anal sphincter repair (or under supervision) should repair OASIS.
FIGURE 1 Buttonhole tear
A buttonhole tear of the rectal mucosa (arrow) with an intact external anal sphincter (EAS) demonstrated during a digital rectal examination. SOURCE: Sultan AH3 (used with permission).
FIGURE 2 Injury obscured by intact skin
(A) Intact perineum on visual examination. (B) Anal sphincter trauma detected after rectal examination. SOURCE: Sultan AH, Kettle C1 (used with permission).
1. When (and how) should the torn perineum be examined?
The first requisite is informed consent for vaginal and rectal examination immediately after delivery. Also vital are adequate exposure of the perineum, good lighting, and, if necessary, sufficient analgesia to prevent pain-related restriction of the evaluation. It may be advisable to place the patient in the lithotomy position to improve exposure.
After visual examination of the perineum, part the labia and examine the vagina to establish the full extent of the tear. Always identify the apex of the vaginal laceration.
Next, perform a rectal examination to exclude injury to the anorectal mucosa and anal sphincter.3
Palpation is necessary to confirm OASIS
Insert the index finger into the anal canal and the thumb into the vagina and perform a pill-rolling motion to palpate the anal sphincter. If this technique is inconclusive, ask the woman to contract her anal sphincter with your fingers still in place. When the sphincter is disrupted, you feel a distinct gap anteriorly. If the perineal skin is intact, there may be an absence of puckering on the perianal skin over any underlying defect that may not be evident under regional or general anesthesia.
Because the external anal sphincter (EAS) is in a state of tonic contraction, the sphincter ends will retract when it is disrupted. These ends need to be grasped and retrieved at the time of repair.
Also identify the internal anal sphincter (IAS). It is a circular smooth muscle (FIGURE 3) that is paler in appearance (similar to the flesh of raw fish) than the striated EAS (similar to raw red meat).4 Under normal circumstances, the distal end of the IAS lies a few millimeters proximal to the distal end of the EAS (FIGURE 4). However, if the EAS is relaxed due to regional or general anesthesia, the distal end of the IAS will appear to be at a lower level. If the IAS or anal epithelium is torn, the EAS is, invariably, torn, too.
General or regional (spinal, epidural, caudal) anesthesia provides analgesia and muscle relaxation and enables proper evaluation of the full extent of the injury.
FIGURE 3 Grade 3b tear
Grade 3b tear with an intact internal anal sphincter (IAS). The external sphincter (EAS) is being grasped with Allis forceps. Note the difference in appearance of the paler IAS and darker EAS. SOURCE: Sultan AH, Kettle C1 (used with permission).
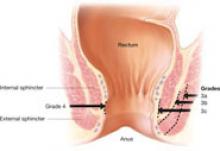
FIGURE 4 Classification of anal sphincter injury
First- and second-degree injuries are described below.
2. Is endoanal US helpful to detect OASIS?
Endoanal ultrasonography (US) to identify OASIS requires specific expertise, particularly in the immediate postpartum period, when the anal canal is lax (especially after an epidural). Ultimately, however, the diagnosis rests on clinical assessment and a rectal examination because, even if a defect is seen on US, it has to be clinically apparent to be repaired.
In a study by Faltin and colleagues, in which routine postpartum endoanal US was used as the gold standard for diagnosis of OASIS, five of 21 women had unnecessary intervention because the sonographic defect was not clinically visible despite exploration of the anal sphincter.5 As a result of this unnecessary exploration based on endoanal US, 20% of these women developed severe fecal incontinence. Therefore, we believe that OASIS is best detected clinically immediately after delivery, provided the physician performs a careful examination with palpation of the anal sphincter.6 In such a scenario, endoanal US is of limited value.
3. How is obstetric anal sphincter trauma classified?
To standardize the classification of perineal trauma, Sultan proposed the following system, which has been adopted by the Royal College of Obstetricians and Gynaecologists and internationally7-9:
First degree: Laceration of the vaginal epithelium or perineal skin only
Second degree: Involvement of the perineal muscles, but not the anal sphincter
Third degree: Disruption of the anal sphincter muscles (FIGURE 4):
- 3a: Less than 50% thickness of the external sphincter is torn
- 3b: More than 50% thickness of the external sphincter is torn
- 3c: Internal sphincter is also torn
Fourth degree: A third-degree anal tear with disruption of the anal epithelium (FIGURE 4).
If there is any ambiguity about grading of the injury, the higher grade should be selected. For example, if there is uncertainty between grades 3a and 3b, the injury should be classified as Grade 3b.
4. Is an operating room necessary?
OASIS should be repaired in the operating theater, where there is access to good lighting, appropriate equipment, and aseptic conditions. In our unit, we have a specially prepared instrument tray containing:
- a Weislander self-retaining retractor
- 4 Allis tissue forceps
- McIndoe scissors
- tooth forceps
- 4 artery forceps
- stitch scissors
- a needle holder.
In addition, deep retractors (e.g., Deavers) are useful when there are associated paravaginal tears.
5. What surgical technique is recommended?
Buttonhole injury
This type of injury can occur in the rectum without disrupting the anal sphincter or perineum. It is best repaired transvaginally using interrupted Vicryl (polyglactin) sutures.
To minimize the risk of persistent rectovaginal fistula, interpose a second layer of tissue between the rectum and vagina by approximating the rectovaginal fascia. A colostomy is rarely indicated unless a large tear extends above the pelvic floor or there is gross fecal contamination of the wound.
Fourth-degree tear
Repair torn anal epithelium with interrupted Vicryl 3-0 sutures, with the knots tied in the anal lumen. Proponents of this widely described technique argue that it reduces the quantity of foreign body (knots) within the tissue and lowers the risk of infection. Concern about a foreign body probably applies to the use of catgut, which dissolves by proteolysis, rather than to newer synthetic material such as Vicryl or Dexon (polyglycolic acid), which dissolves by hydrolysis.
Subcuticular repair of anal epithelium using a transvaginal approach has also been described and could be equally effective if the terminal knots are secure.10
Sphincter muscles
Repair these muscles using 3-0 polydioxanone (PDS) dyed sutures. Compared with braided sutures, monofilament sutures are believed to lessen the risk of infection, although a randomized controlled trial revealed no difference in suture-related morbidity between Vicryl and PDS at 6 weeks postpartum.11 Complete absorption of PDS takes longer than with Vicryl, with 50% tensile strength lasting more than 3 months, compared with 3 weeks for Vicryl.11 To minimize suture migration, cut suture ends short and ensure that they are covered by the overlying superficial perineal muscles.
Internal anal sphincter. Repair the IAS separately from the EAS. Grasp the ends of the torn muscle using Allis forceps and perform an end-to-end repair with interrupted or mattress 3-0 PDS sutures (FIGURE 5). Overlapping repair can be technically difficult.
There is some evidence that repair of an isolated IAS defect benefits patients with established anal incontinence.
External anal sphincter. Because the EAS is normally under tonic contraction, it tends to retract when torn. Therefore, repair requires identification and grasping of the torn ends using Allis tissue forceps (FIGURE 6).
When the EAS is only partially torn (Grade 3a and some cases of Grade 3b), perform an end-to end repair using 2 or 3 mattress sutures, similar to repair of IAS injury, instead of hemostatic “figure of eight” sutures.
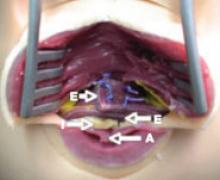
For a full-thickness tear (some cases of Grade 3b or 3c, or Grade 4), overlapping repair may be preferable in experienced hands. The EAS may need to be mobilized by dissecting it free of the ischioanal fat laterally using a pair of McIndoe scissors. The torn ends of the EAS can then be overlapped in “double-breasted” fashion (FIGURE 7) using PDS 3-0 sutures. Proper overlap is possible only when the full length of the torn ends is identified.
Overlapping the ends of the sphincter allows for greater surface area of contact between muscle. In contrast, end-to-end repair can be performed without identifying the full length of the EAS and may give rise to incomplete apposition. Fernando and colleagues demonstrated that, in experienced hands, early primary overlap repair carries a lower risk of fecal urgency and anal incontinence than does immediate primary end-to-end repair.12,13
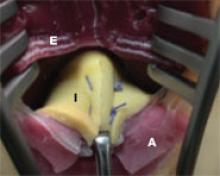
FIGURE 5 End-to-end repair
Internal anal sphincter (I) repair using mattress sutures, demonstrated on the latex Sultan model, used for training (www.perineum.net) (E, external sphincter; A, anal epithelium). SOURCE: Sultan AH, Thakar R2 (used with permission).
FIGURE 6 Locating the external anal sphincter
The external sphincter (E), grasped with Allis forceps, is surrounded by the capsule (C) and lies medial to the ischioanal fat. SOURCE: Sultan AH, Thakar R2 (used with permission).
FIGURE 7 Overlapping sphincter repair
Repair of a fourth degree tear (demonstrated on the Sultan model) using the overlap repair technique on the external sphincter (E). The anal epithelium (A) and the internal sphincter (I) have also been repaired. SOURCE: Sultan AH, Thakar R2 (used with permission).
Perineal muscles
After repair of the sphincter, suture the perineal muscles to reconstruct the perineal body and provide support to the repaired anal sphincter. A short, deficient perineum would leave the anal sphincter more vulnerable to trauma during a subsequent vaginal delivery.
Next, suture the vaginal skin and approximate the perineal skin using Vicryl Rapide 2-0 subcuticular suture.
Examine, and document, the repair
Perform a rectal and vaginal examination to confirm adequate repair and ensure that no other tears have been missed—and that all tampons or swabs have been removed.
Make detailed notes of the findings and repair. A pro forma pictorial representation of the tears proves very useful when notes are reviewed following complications or during audit or litigation.
6. What does postoperative care entail?
Prophylactic antibiotics are common
No randomized trials have substantiated the benefits of intraoperative and postoperative antibiotics after repair of OASIS. Nevertheless, these drugs are commonly prescribed, especially after fourth- degree tears, because infection and wound breakdown could jeopardize the repair and lead to incontinence or fistula.10,14
We prescribe intravenous broad-spectrum antibiotics such as cefuroxime and metronidazole intraoperatively and continue the drugs orally for 5 days.
Bladder catheterization is recommended
Severe perineal discomfort, especially after instrumental delivery, is a known cause of urinary retention. Moreover, after administration of regional anesthesia, it can take up to 12 hours before bladder sensation returns.
We recommend insertion of a Foley catheter for approximately 24 hours, unless medical staff can ensure that spontaneous voiding occurs at least every 3 to 4 hours without bladder overdistension.
Pain may persist after severe injury
The degree of pain following perineal trauma is related to the extent of the injury. OASIS is frequently associated with other more extensive injuries such as paravaginal tears. In one study, 91% of women continued to complain of severe perineal pain 7 days after OASIS.15
In a systematic review, Hedayati and associates found rectal analgesia, such as diclofenac sodium, to be effective at reducing pain from perineal trauma within the first 24 hours after birth; they also found that women used less additional analgesia within the first 48 hours after birth.16 Diclofenac is almost completely bound to protein, so excretion in breast milk is negligible.17
In women who have undergone repair of a fourth-degree tear, administer oral diclofenac; suppositories may be uncomfortable, and there is a theoretical risk of poor healing associated with local anti-inflammatory agents.
Avoid codeine-based preparations because they may cause constipation and lead to excessive straining and disruption of the repair.
Recommend a stool softener
It is vital that constipation be avoided as the patient heals; passage of constipated stool or fecal impaction can disrupt the repair. We prescribe a stool softener (lactulose, 15 mL twice daily) for 10 to 14 days and have encountered no problem with bowel evacuation.18
We recommend that the patient telephone a healthcare provider 24 to 48 hours after hospital discharge to confirm that bowel evacuation has occurred. If it hasn’t, we add mineral oil, magnesium hydroxide, or another oral bowel stimulant to the stool softener and bulking agent.
Mahoney and colleagues conducted a randomized trial (n=105) of constipating versus laxative regimens and found the latter to be associated with earlier and less painful first bowel motion and earlier hospital discharge.19 Nineteen percent of women following the constipating regimen had troublesome constipation (two required hospitalization for fecal impaction), compared with 5% of women receiving a laxative. There were no significant differences in continence scores, anal manometry, and endoanal US findings.
Give the patient adequate information
Before the patient is discharged from the hospital, we give her a booklet that describes the implications of OASIS and explains when and where to seek help if symptoms of infection or incontinence develop. All women also complete a validated bowel-health and quality-of-life questionnaire regarding conditions prior to the delivery. We also recommend pelvic floor and anal sphincter exercises as soon as her discomfort resolves.
Perform a comprehensive follow-up exam
All women who sustain OASIS should be assessed by a senior obstetrician 6 to 8 weeks after delivery. In our practice, these women are seen in a dedicated perineal clinic.20 The clinic provides a supportive environment and increases the patient’s confidence in the team.21
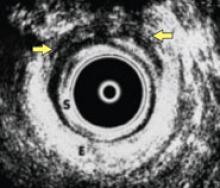
At the clinic, each woman completes the same symptom questionnaire that she was given before hospital discharge. She then undergoes a genital examination in which the physician checks the degree of scarring, residual granulation tissue, and tenderness; ensures that the patient understands the circumstances surrounding the delivery and injury; and addresses any concerns. All women then undergo anal manometry and endoanal US (FIGURE 8). Each patient is encouraged to continue pelvic floor exercises. If she has minimal sphincter contractility, she may need electrical stimulation.
If a dedicated perineal clinic is unavailable, the patient should be given clear instructions, preferably in writing, before leaving the hospital. During the 6 weeks immediately after delivery, she should be instructed to look for signs of infection or wound dehiscence and to telephone the physician to report any increase in pain or swelling, rectal bleeding, or purulent discharge. Any incontinence of stool or flatus also should be reported.
FIGURE 8 Defect visible on US
Endoanal sonogram showing a defect in the external anal sphincter between 11 o’clock and 1 o’clock (between the yellow arrows) (S, subepithelium; E, external anal sphincter). SOURCE: Sultan AH, Thakar R2 (used with permission).
7. Is vaginal delivery advisable after OASIS?
No randomized trials have determined the most appropriate mode of delivery after a third- or fourth-degree tear. We base our counseling of the patient on a completed symptom questionnaire and findings from manometry and endoanal US (FIGURE 8). If vaginal delivery is contemplated, these tests should be performed during the current pregnancy unless they were abnormal at an earlier date. FIGURE 9 is a simple flow diagram from our unit that illustrates management of subsequent delivery after OASIS.
When determining the mode of delivery, thorough counseling and clear documentation of that counseling are extremely important.
FIGURE 9 How do you determine the mode of delivery after OASIS?
Vaginal delivery is possible unless anal sphincter function is impaired
One study found that when a large sonographic defect (more than one quadrant) is present, or the squeeze-pressure increment (above resting pressure) is less than 20 mm Hg, the risk of impaired continence after a subsequent delivery increases dramatically.22
Based on these findings, we conducted a prospective study that found no deterioration of sphincter function or increase in symptoms after vaginal delivery unless the patient had significant compromise of anal sphincter function before the pregnancy.23 Therefore, we encourage asymptomatic women who have minimal compromise of anal sphincter function to undergo vaginal delivery.
Routine episiotomy is not protective
There is no evidence that routine episiotomy prevents recurrent OASIS. If episiotomy is deemed to be necessary—e.g., for a thick inelastic or scarred perineum—mediolateral episiotomy is preferred.
High likelihood of success in some women
Women who have minimal compromise of anal sphincter function should be counseled that they have an 88% (in centers practicing midline episiotomy) to 95% (in centers practicing mediolateral episiotomy) chance of delivering without sustaining another OASIS.24,25 This should reassure them if they have misgivings about vaginal delivery.
Threshold for C-section is lower if additional risk factors are present
If traumatic delivery is anticipated, as in the presence of one or more additional risk factors (macrosomia, shoulder dystocia, prolonged labor, difficult instrumental delivery), cesarean section may be appropriate.
Consider emotional needs
Some women who have sustained OASIS may be scarred emotionally as well as physically and may find it difficult to cope with the thought of another vaginal delivery. These women deserve sympathy, psychological support, and consideration of their request for cesarean section.
When cesarean is a good idea
Women who have a minor degree of incontinence (e.g., fecal urgency or flatus incontinence) may be managed with dietary advice, constipating agents (loperamide or codeine phosphate), and physiotherapy or biofeedback. These women who have some degree of anal sphincter compromise but whose symptoms are controlled should be counseled that cesarean delivery is recommended (FIGURE 9).
Women who have sustained a previous third- or fourth-degree tear with subsequent severe incontinence should be offered secondary sphincter repair by a colorectal surgeon or urogynecologist with expertise in secondary sphincter repair. All subsequent deliveries by these women should be by cesarean section.
Some women with fecal incontinence may choose to complete their family before embarking on anal sphincter surgery. It remains unclear whether these women should be allowed a vaginal delivery, but it is likely that most damage has already occurred and that the risk of further injury is minimal and possibly insignificant. The benefit of cesarean delivery, if any, should be weighed against its risks for all subsequent pregnancies.
Women who have undergone a previous successful secondary sphincter repair for fecal incontinence should be delivered by cesarean delivery.9
Not all women fit neatly into one category
There are going to be women who do not entirely fit any of the categories described—such as those who have isolated internal sphincter defects or irritable bowel syndrome. Management of these women should be individualized, with the mode of delivery determined by mutual agreement after taking into account symptoms and clinical and other findings.
If there are no facilities for anal manometry and US, the physician should base management on symptoms and clinical evaluation. Asymptomatic women who do not have clinical evidence of sphincter compromise during anal tone assessment may be allowed to undergo vaginal delivery. All women who are symptomatic should be referred to a center with facilities for anorectal assessment to establish the ideal management and mode of delivery.
Pay attention to modifiable risk factors
In the case described at the beginning of this article, two risk factors could have been modified to minimize the patient’s risk of OASIS—namely, midline episiotomy and forceps delivery. In a quasirandomized study by Coats, involving 407 nulliparous women, which compared mediolateral and midline episiotomy (when episiotomy was necessary), tears into or through the anal sphincter occurred in 12% of women undergoing midline episiotomy and 2% of those undergoing mediolateral episiotomy.26
If operative vaginal delivery is required, vacuum extraction is preferred. In a meta-analysis of randomized studies, Thakar and Eason found that fewer women have anal sphincter trauma with vacuum delivery than with forceps.27 One anal sphincter tear is avoided for every 18 women delivered by vacuum extraction instead of forceps. A randomized trial conducted in the United Kingdom involving mediolateral episiotomy found severe vaginal laceration in 17% of forceps deliveries and 11% of vacuum deliveries.28 A randomized controlled trial in Canada involving midline episiotomy found third- or fourth-degree tears in 29% of forceps deliveries, versus 12% of vacuum deliveries.29
Q. What is the proper code for reporting an anal sphincter injury incurred in pregnancy?
A. That depends—on when the tear occurred, whether the patient is currently pregnant, and whether there were additional lacerations of the perineum.
ICD-9-CM offers four codes in this setting. Choose one, as follows:
- If you note an anal tear at the time of, or after, delivery but there is no perineal laceration, report 664.6×. This code takes a fifth digit: “1,” for the patient who has just delivered, or “4,” if you are treating the tear after she has been discharged.
- If the tear is noted in addition to a third-degree perineal tear, report 664.2× instead; fifth-digit choices for this code are also “1” and “4.”
- If the patient had an anal tear before delivery, from a prior pregnancy, code 654.8× [congenital or acquired abnormality of the vulva].
- Last, if you are treating the patient for an old anal tear and she is not pregnant at the moment, report 569.43 and add any additional codes that have resulted from the tear, such as fecal incontinence (787.6).
—Melanie Witt, RN, CPC-OGS, MA
1. Sultan AH, Kettle C. Diagnosis of perineal trauma. In: Sultan AH, Thakar R, Fenner DE, eds. Perineal and Anal Sphincter Trauma. London: Springer; 2007:13-19.
2. Sultan AH, Thakar R. Third and fourth degree tears. In: Sultan AH, Thakar R, Fenner DE, eds. Perineal and Anal Sphincter Trauma. London: Springer; 2007:33-51.
3. Sultan AH. Primary repair of obstetric anal sphincter injury. In: Staskin DR, Cardozo L, ed. Textbook of Female Urology and Urogynaecology. London: ISIS Medical Media; 2006.
4. Thakar R, Fenner DE. Anatomy of the perineum and the anal sphincter. In: Sultan AH, Thakar R, Fenner DE, eds. Perineal and Anal Sphincter Trauma. London: Springer; 2007:1-12.
5. Faltin DL, Boulvain M, Floris LA, Irion O. Diagnosis of anal sphincter tears to prevent fecal incontinence: a randomized controlled trial. Obstet Gynecol. 2005;106:6-13.
6. Andrews V, Thakar R, Sultan AH. Occult anal sphincter injuries—myth or reality. Br J Obstet Gynaecol. 2006;113:195-200.
7. Sultan AH. Obstetric perineal injury and anal incontinence. Clin Risk. 1999;5:193-196.
8. Royal College of Obstetricians and Gynaecologists. Management of third and fourth degree perineal tears following vaginal delivery. Guideline 29. London: RCOG Press; 2001.
9. Norton C, Christensen J, Butler U, et al. Anal Incontinence. 2nd ed. Plymouth: Health Publication Ltd; 2005:985-1044.
10. Sultan AH, Thakar R. Lower genital tract and anal sphincter trauma. Best Pract Res Clin Obstet Gynaecol. 2002;16:99-116.
11. Williams A, Adams EJ, Tincello DG, Alfirevic Z, Walkinshaw SA, Richmond DH. How to repair an anal sphincter injury after vaginal delivery: results of a randomised controlled trial. BJOG. 2006;113:201-207.
12. Fernando RJ, Sultan AH, Kettle C, Radley S, Jones P, O’Brien PMS. Repair techniques for obstetric anal sphincter injuries. A randomized controlled trial. Obstet Gynecol. 2006;107:1261-1268.
13. Fernando R, Sultan AH, Kettle C, Thakar R, Radley S. Methods of repair for obstetric anal sphincter injury. Cochrane Database Syst Rev. 2006;3:CD002866.-
14. Fernando RJ, Sultan AH, Radley S, Jones PW, Johanson RB. Management of obstetric anal sphincter injury: a systematic review and national practice survey. BMC Health Serv Res. 2002;2:9.-
15. MacArthur AJ, MacArthur C. Incidence, severity, and determinants of perineal pain after vaginal delivery: a prospective cohort study. Am J Obstet Gynecol. 2004;191:1199-1204.
16. Hedayati H, Parsons J, Crowther CA. Rectal analgesia for pain from perineal trauma following childbirth. Cochrane Database Syst Rev. 2003;(3):CD003931.-
17. Kettle C, Hills RK, Jones P, Darby L, Gray R, Johanson R. Continuous versus interrupted perineal repair with standard or rapidly absorbed sutures after spontaneous vaginal birth: a randomised controlled trial. Lancet. 2002;359:2217-2223.
18. Sultan AH, Monga AK, Kumar D, Stanton SL. Primary repair of obstetric anal sphincter rupture using the overlap technique. Br J Obstet Gynaecol. 1999;106:318-323.
19. Mahony R, Behan M, O’Herlihy C, O’Connell PR. Randomized, clinical trial of bowel confinement vs. laxative use after primary repair of a third-degree obstetric anal sphincter tear. Dis Colon Rectum. 2004;47:12-17.
20. Thakar R, Sultan A. Postpartum problems and the role of a perineal clinic. In: Sultan AH, Thakar R, Fenner DE, eds. Perineal and Anal Sphincter Trauma. London: Springer; 2007:65-79.
21. Williams A, Lavender T, Richmond DH, Tincello DG. Women’s experiences after a third-degree obstetric anal sphincter tear: a qualitative study. Birth. 2005;32:129-136.
22. Fynes M, Donnelly V, Behan M, O’Connell PR, O’Herlihy C. Effect of second vaginal delivery on anorectal physiology and faecal continence: a prospective study. Lancet. 1999;354:983-986.
23. Scheer I, Thakar R, Sultan A. Should women who sustained obstetric anal sphincter injuries be allowed a vaginal delivery? Neurourol Urodynam. 2006;25:512-513.
24. Peleg D, Kennedy CM, Merrill D, Zlatnik FJ. Risk of repetition of a severe perineal laceration. Obstet Gynecol. 1999;93:1021-1024.
25. Harkin R, Fitzpatrick M, O’Connell PR, O’Herlihy C. Anal sphincter disruption at vaginal delivery: is recurrence predictable? Eur J Obstet Gynaecol Reprod Biol. 2003;109:149-152.
26. Coats PM, Chan KK, Wilkins M, Beard RJ. A comparison between midline and mediolateral episiotomies. Br J Obstet Gynaecol. 1980;87:408-412.
27. Thakar R, Eason E. Prevention of perineal trauma. In: Sultan AH, Thakar R, Fenner DE, eds. Perineal and Anal Sphincter Trauma. London: Springer; 2007:52-64.
28. Johanson RB, Rice C, Doyle M. A randomised prospective study comparing the new vacuum extractor policy with forceps delivery. Br J Obstet Gynaecol. 1993;100:524-530.
29. Bofill JA, Rust OA, Schorr SJ, et al. A randomized prospective trial of the obstetric forceps versus the M-cup vacuum extractor. Am J Obstet Gynecol. 1996;175:1325-1330.
The authors report no financial relationships relevant to this article.
CASE Large baby, extensive tear
A 28-year-old primigravida undergoes a forceps delivery with a midline episiotomy for failure to progress in the second stage of labor. At birth, the infant weighs 4 kg (8.8 lb), and the episiotomy extends to the anal verge. The resident who delivered the child is uncertain whether the anal sphincter is involved in the injury and asks a consultant to examine the perineum.
What should this examination entail?
The obstetrician is rarely culpable when a third- or fourth-degree obstetric anal sphincter injury (OASIS) occurs—but there is little excuse for letting one go undetected.
To minimize the risk of undiagnosed OASIS, a digital anorectal examination is warranted—before any suturing—in every woman who delivers vaginally. This practice can help you avoid missing isolated tears, such as “buttonhole” of the rectal mucosa, which can occur even when the anal sphincter remains intact (FIGURE 1), or a third- or fourth-degree tear that can sometimes be present behind apparently intact perineal skin (FIGURE 2).1
Clinical training of physicians and midwives also needs to improve.
Every labor room should have a protocol for management of anal sphincter injury2; this article describes detection, diagnosis, and management, focusing on seven critical questions.
Only a physician formally trained in primary anal sphincter repair (or under supervision) should repair OASIS.
FIGURE 1 Buttonhole tear
A buttonhole tear of the rectal mucosa (arrow) with an intact external anal sphincter (EAS) demonstrated during a digital rectal examination. SOURCE: Sultan AH3 (used with permission).
FIGURE 2 Injury obscured by intact skin
(A) Intact perineum on visual examination. (B) Anal sphincter trauma detected after rectal examination. SOURCE: Sultan AH, Kettle C1 (used with permission).
1. When (and how) should the torn perineum be examined?
The first requisite is informed consent for vaginal and rectal examination immediately after delivery. Also vital are adequate exposure of the perineum, good lighting, and, if necessary, sufficient analgesia to prevent pain-related restriction of the evaluation. It may be advisable to place the patient in the lithotomy position to improve exposure.
After visual examination of the perineum, part the labia and examine the vagina to establish the full extent of the tear. Always identify the apex of the vaginal laceration.
Next, perform a rectal examination to exclude injury to the anorectal mucosa and anal sphincter.3
Palpation is necessary to confirm OASIS
Insert the index finger into the anal canal and the thumb into the vagina and perform a pill-rolling motion to palpate the anal sphincter. If this technique is inconclusive, ask the woman to contract her anal sphincter with your fingers still in place. When the sphincter is disrupted, you feel a distinct gap anteriorly. If the perineal skin is intact, there may be an absence of puckering on the perianal skin over any underlying defect that may not be evident under regional or general anesthesia.
Because the external anal sphincter (EAS) is in a state of tonic contraction, the sphincter ends will retract when it is disrupted. These ends need to be grasped and retrieved at the time of repair.
Also identify the internal anal sphincter (IAS). It is a circular smooth muscle (FIGURE 3) that is paler in appearance (similar to the flesh of raw fish) than the striated EAS (similar to raw red meat).4 Under normal circumstances, the distal end of the IAS lies a few millimeters proximal to the distal end of the EAS (FIGURE 4). However, if the EAS is relaxed due to regional or general anesthesia, the distal end of the IAS will appear to be at a lower level. If the IAS or anal epithelium is torn, the EAS is, invariably, torn, too.
General or regional (spinal, epidural, caudal) anesthesia provides analgesia and muscle relaxation and enables proper evaluation of the full extent of the injury.
FIGURE 3 Grade 3b tear
Grade 3b tear with an intact internal anal sphincter (IAS). The external sphincter (EAS) is being grasped with Allis forceps. Note the difference in appearance of the paler IAS and darker EAS. SOURCE: Sultan AH, Kettle C1 (used with permission).
FIGURE 4 Classification of anal sphincter injury
First- and second-degree injuries are described below.
2. Is endoanal US helpful to detect OASIS?
Endoanal ultrasonography (US) to identify OASIS requires specific expertise, particularly in the immediate postpartum period, when the anal canal is lax (especially after an epidural). Ultimately, however, the diagnosis rests on clinical assessment and a rectal examination because, even if a defect is seen on US, it has to be clinically apparent to be repaired.
In a study by Faltin and colleagues, in which routine postpartum endoanal US was used as the gold standard for diagnosis of OASIS, five of 21 women had unnecessary intervention because the sonographic defect was not clinically visible despite exploration of the anal sphincter.5 As a result of this unnecessary exploration based on endoanal US, 20% of these women developed severe fecal incontinence. Therefore, we believe that OASIS is best detected clinically immediately after delivery, provided the physician performs a careful examination with palpation of the anal sphincter.6 In such a scenario, endoanal US is of limited value.
3. How is obstetric anal sphincter trauma classified?
To standardize the classification of perineal trauma, Sultan proposed the following system, which has been adopted by the Royal College of Obstetricians and Gynaecologists and internationally7-9:
First degree: Laceration of the vaginal epithelium or perineal skin only
Second degree: Involvement of the perineal muscles, but not the anal sphincter
Third degree: Disruption of the anal sphincter muscles (FIGURE 4):
- 3a: Less than 50% thickness of the external sphincter is torn
- 3b: More than 50% thickness of the external sphincter is torn
- 3c: Internal sphincter is also torn
Fourth degree: A third-degree anal tear with disruption of the anal epithelium (FIGURE 4).
If there is any ambiguity about grading of the injury, the higher grade should be selected. For example, if there is uncertainty between grades 3a and 3b, the injury should be classified as Grade 3b.
4. Is an operating room necessary?
OASIS should be repaired in the operating theater, where there is access to good lighting, appropriate equipment, and aseptic conditions. In our unit, we have a specially prepared instrument tray containing:
- a Weislander self-retaining retractor
- 4 Allis tissue forceps
- McIndoe scissors
- tooth forceps
- 4 artery forceps
- stitch scissors
- a needle holder.
In addition, deep retractors (e.g., Deavers) are useful when there are associated paravaginal tears.
5. What surgical technique is recommended?
Buttonhole injury
This type of injury can occur in the rectum without disrupting the anal sphincter or perineum. It is best repaired transvaginally using interrupted Vicryl (polyglactin) sutures.
To minimize the risk of persistent rectovaginal fistula, interpose a second layer of tissue between the rectum and vagina by approximating the rectovaginal fascia. A colostomy is rarely indicated unless a large tear extends above the pelvic floor or there is gross fecal contamination of the wound.
Fourth-degree tear
Repair torn anal epithelium with interrupted Vicryl 3-0 sutures, with the knots tied in the anal lumen. Proponents of this widely described technique argue that it reduces the quantity of foreign body (knots) within the tissue and lowers the risk of infection. Concern about a foreign body probably applies to the use of catgut, which dissolves by proteolysis, rather than to newer synthetic material such as Vicryl or Dexon (polyglycolic acid), which dissolves by hydrolysis.
Subcuticular repair of anal epithelium using a transvaginal approach has also been described and could be equally effective if the terminal knots are secure.10
Sphincter muscles
Repair these muscles using 3-0 polydioxanone (PDS) dyed sutures. Compared with braided sutures, monofilament sutures are believed to lessen the risk of infection, although a randomized controlled trial revealed no difference in suture-related morbidity between Vicryl and PDS at 6 weeks postpartum.11 Complete absorption of PDS takes longer than with Vicryl, with 50% tensile strength lasting more than 3 months, compared with 3 weeks for Vicryl.11 To minimize suture migration, cut suture ends short and ensure that they are covered by the overlying superficial perineal muscles.
Internal anal sphincter. Repair the IAS separately from the EAS. Grasp the ends of the torn muscle using Allis forceps and perform an end-to-end repair with interrupted or mattress 3-0 PDS sutures (FIGURE 5). Overlapping repair can be technically difficult.
There is some evidence that repair of an isolated IAS defect benefits patients with established anal incontinence.
External anal sphincter. Because the EAS is normally under tonic contraction, it tends to retract when torn. Therefore, repair requires identification and grasping of the torn ends using Allis tissue forceps (FIGURE 6).
When the EAS is only partially torn (Grade 3a and some cases of Grade 3b), perform an end-to end repair using 2 or 3 mattress sutures, similar to repair of IAS injury, instead of hemostatic “figure of eight” sutures.
For a full-thickness tear (some cases of Grade 3b or 3c, or Grade 4), overlapping repair may be preferable in experienced hands. The EAS may need to be mobilized by dissecting it free of the ischioanal fat laterally using a pair of McIndoe scissors. The torn ends of the EAS can then be overlapped in “double-breasted” fashion (FIGURE 7) using PDS 3-0 sutures. Proper overlap is possible only when the full length of the torn ends is identified.
Overlapping the ends of the sphincter allows for greater surface area of contact between muscle. In contrast, end-to-end repair can be performed without identifying the full length of the EAS and may give rise to incomplete apposition. Fernando and colleagues demonstrated that, in experienced hands, early primary overlap repair carries a lower risk of fecal urgency and anal incontinence than does immediate primary end-to-end repair.12,13
FIGURE 5 End-to-end repair
Internal anal sphincter (I) repair using mattress sutures, demonstrated on the latex Sultan model, used for training (www.perineum.net) (E, external sphincter; A, anal epithelium). SOURCE: Sultan AH, Thakar R2 (used with permission).
FIGURE 6 Locating the external anal sphincter
The external sphincter (E), grasped with Allis forceps, is surrounded by the capsule (C) and lies medial to the ischioanal fat. SOURCE: Sultan AH, Thakar R2 (used with permission).
FIGURE 7 Overlapping sphincter repair
Repair of a fourth degree tear (demonstrated on the Sultan model) using the overlap repair technique on the external sphincter (E). The anal epithelium (A) and the internal sphincter (I) have also been repaired. SOURCE: Sultan AH, Thakar R2 (used with permission).
Perineal muscles
After repair of the sphincter, suture the perineal muscles to reconstruct the perineal body and provide support to the repaired anal sphincter. A short, deficient perineum would leave the anal sphincter more vulnerable to trauma during a subsequent vaginal delivery.
Next, suture the vaginal skin and approximate the perineal skin using Vicryl Rapide 2-0 subcuticular suture.
Examine, and document, the repair
Perform a rectal and vaginal examination to confirm adequate repair and ensure that no other tears have been missed—and that all tampons or swabs have been removed.
Make detailed notes of the findings and repair. A pro forma pictorial representation of the tears proves very useful when notes are reviewed following complications or during audit or litigation.
6. What does postoperative care entail?
Prophylactic antibiotics are common
No randomized trials have substantiated the benefits of intraoperative and postoperative antibiotics after repair of OASIS. Nevertheless, these drugs are commonly prescribed, especially after fourth- degree tears, because infection and wound breakdown could jeopardize the repair and lead to incontinence or fistula.10,14
We prescribe intravenous broad-spectrum antibiotics such as cefuroxime and metronidazole intraoperatively and continue the drugs orally for 5 days.
Bladder catheterization is recommended
Severe perineal discomfort, especially after instrumental delivery, is a known cause of urinary retention. Moreover, after administration of regional anesthesia, it can take up to 12 hours before bladder sensation returns.
We recommend insertion of a Foley catheter for approximately 24 hours, unless medical staff can ensure that spontaneous voiding occurs at least every 3 to 4 hours without bladder overdistension.
Pain may persist after severe injury
The degree of pain following perineal trauma is related to the extent of the injury. OASIS is frequently associated with other more extensive injuries such as paravaginal tears. In one study, 91% of women continued to complain of severe perineal pain 7 days after OASIS.15
In a systematic review, Hedayati and associates found rectal analgesia, such as diclofenac sodium, to be effective at reducing pain from perineal trauma within the first 24 hours after birth; they also found that women used less additional analgesia within the first 48 hours after birth.16 Diclofenac is almost completely bound to protein, so excretion in breast milk is negligible.17
In women who have undergone repair of a fourth-degree tear, administer oral diclofenac; suppositories may be uncomfortable, and there is a theoretical risk of poor healing associated with local anti-inflammatory agents.
Avoid codeine-based preparations because they may cause constipation and lead to excessive straining and disruption of the repair.
Recommend a stool softener
It is vital that constipation be avoided as the patient heals; passage of constipated stool or fecal impaction can disrupt the repair. We prescribe a stool softener (lactulose, 15 mL twice daily) for 10 to 14 days and have encountered no problem with bowel evacuation.18
We recommend that the patient telephone a healthcare provider 24 to 48 hours after hospital discharge to confirm that bowel evacuation has occurred. If it hasn’t, we add mineral oil, magnesium hydroxide, or another oral bowel stimulant to the stool softener and bulking agent.
Mahoney and colleagues conducted a randomized trial (n=105) of constipating versus laxative regimens and found the latter to be associated with earlier and less painful first bowel motion and earlier hospital discharge.19 Nineteen percent of women following the constipating regimen had troublesome constipation (two required hospitalization for fecal impaction), compared with 5% of women receiving a laxative. There were no significant differences in continence scores, anal manometry, and endoanal US findings.
Give the patient adequate information
Before the patient is discharged from the hospital, we give her a booklet that describes the implications of OASIS and explains when and where to seek help if symptoms of infection or incontinence develop. All women also complete a validated bowel-health and quality-of-life questionnaire regarding conditions prior to the delivery. We also recommend pelvic floor and anal sphincter exercises as soon as her discomfort resolves.
Perform a comprehensive follow-up exam
All women who sustain OASIS should be assessed by a senior obstetrician 6 to 8 weeks after delivery. In our practice, these women are seen in a dedicated perineal clinic.20 The clinic provides a supportive environment and increases the patient’s confidence in the team.21
At the clinic, each woman completes the same symptom questionnaire that she was given before hospital discharge. She then undergoes a genital examination in which the physician checks the degree of scarring, residual granulation tissue, and tenderness; ensures that the patient understands the circumstances surrounding the delivery and injury; and addresses any concerns. All women then undergo anal manometry and endoanal US (FIGURE 8). Each patient is encouraged to continue pelvic floor exercises. If she has minimal sphincter contractility, she may need electrical stimulation.
If a dedicated perineal clinic is unavailable, the patient should be given clear instructions, preferably in writing, before leaving the hospital. During the 6 weeks immediately after delivery, she should be instructed to look for signs of infection or wound dehiscence and to telephone the physician to report any increase in pain or swelling, rectal bleeding, or purulent discharge. Any incontinence of stool or flatus also should be reported.
FIGURE 8 Defect visible on US
Endoanal sonogram showing a defect in the external anal sphincter between 11 o’clock and 1 o’clock (between the yellow arrows) (S, subepithelium; E, external anal sphincter). SOURCE: Sultan AH, Thakar R2 (used with permission).
7. Is vaginal delivery advisable after OASIS?
No randomized trials have determined the most appropriate mode of delivery after a third- or fourth-degree tear. We base our counseling of the patient on a completed symptom questionnaire and findings from manometry and endoanal US (FIGURE 8). If vaginal delivery is contemplated, these tests should be performed during the current pregnancy unless they were abnormal at an earlier date. FIGURE 9 is a simple flow diagram from our unit that illustrates management of subsequent delivery after OASIS.
When determining the mode of delivery, thorough counseling and clear documentation of that counseling are extremely important.
FIGURE 9 How do you determine the mode of delivery after OASIS?
Vaginal delivery is possible unless anal sphincter function is impaired
One study found that when a large sonographic defect (more than one quadrant) is present, or the squeeze-pressure increment (above resting pressure) is less than 20 mm Hg, the risk of impaired continence after a subsequent delivery increases dramatically.22
Based on these findings, we conducted a prospective study that found no deterioration of sphincter function or increase in symptoms after vaginal delivery unless the patient had significant compromise of anal sphincter function before the pregnancy.23 Therefore, we encourage asymptomatic women who have minimal compromise of anal sphincter function to undergo vaginal delivery.
Routine episiotomy is not protective
There is no evidence that routine episiotomy prevents recurrent OASIS. If episiotomy is deemed to be necessary—e.g., for a thick inelastic or scarred perineum—mediolateral episiotomy is preferred.
High likelihood of success in some women
Women who have minimal compromise of anal sphincter function should be counseled that they have an 88% (in centers practicing midline episiotomy) to 95% (in centers practicing mediolateral episiotomy) chance of delivering without sustaining another OASIS.24,25 This should reassure them if they have misgivings about vaginal delivery.
Threshold for C-section is lower if additional risk factors are present
If traumatic delivery is anticipated, as in the presence of one or more additional risk factors (macrosomia, shoulder dystocia, prolonged labor, difficult instrumental delivery), cesarean section may be appropriate.
Consider emotional needs
Some women who have sustained OASIS may be scarred emotionally as well as physically and may find it difficult to cope with the thought of another vaginal delivery. These women deserve sympathy, psychological support, and consideration of their request for cesarean section.
When cesarean is a good idea
Women who have a minor degree of incontinence (e.g., fecal urgency or flatus incontinence) may be managed with dietary advice, constipating agents (loperamide or codeine phosphate), and physiotherapy or biofeedback. These women who have some degree of anal sphincter compromise but whose symptoms are controlled should be counseled that cesarean delivery is recommended (FIGURE 9).
Women who have sustained a previous third- or fourth-degree tear with subsequent severe incontinence should be offered secondary sphincter repair by a colorectal surgeon or urogynecologist with expertise in secondary sphincter repair. All subsequent deliveries by these women should be by cesarean section.
Some women with fecal incontinence may choose to complete their family before embarking on anal sphincter surgery. It remains unclear whether these women should be allowed a vaginal delivery, but it is likely that most damage has already occurred and that the risk of further injury is minimal and possibly insignificant. The benefit of cesarean delivery, if any, should be weighed against its risks for all subsequent pregnancies.
Women who have undergone a previous successful secondary sphincter repair for fecal incontinence should be delivered by cesarean delivery.9
Not all women fit neatly into one category
There are going to be women who do not entirely fit any of the categories described—such as those who have isolated internal sphincter defects or irritable bowel syndrome. Management of these women should be individualized, with the mode of delivery determined by mutual agreement after taking into account symptoms and clinical and other findings.
If there are no facilities for anal manometry and US, the physician should base management on symptoms and clinical evaluation. Asymptomatic women who do not have clinical evidence of sphincter compromise during anal tone assessment may be allowed to undergo vaginal delivery. All women who are symptomatic should be referred to a center with facilities for anorectal assessment to establish the ideal management and mode of delivery.
Pay attention to modifiable risk factors
In the case described at the beginning of this article, two risk factors could have been modified to minimize the patient’s risk of OASIS—namely, midline episiotomy and forceps delivery. In a quasirandomized study by Coats, involving 407 nulliparous women, which compared mediolateral and midline episiotomy (when episiotomy was necessary), tears into or through the anal sphincter occurred in 12% of women undergoing midline episiotomy and 2% of those undergoing mediolateral episiotomy.26
If operative vaginal delivery is required, vacuum extraction is preferred. In a meta-analysis of randomized studies, Thakar and Eason found that fewer women have anal sphincter trauma with vacuum delivery than with forceps.27 One anal sphincter tear is avoided for every 18 women delivered by vacuum extraction instead of forceps. A randomized trial conducted in the United Kingdom involving mediolateral episiotomy found severe vaginal laceration in 17% of forceps deliveries and 11% of vacuum deliveries.28 A randomized controlled trial in Canada involving midline episiotomy found third- or fourth-degree tears in 29% of forceps deliveries, versus 12% of vacuum deliveries.29
Q. What is the proper code for reporting an anal sphincter injury incurred in pregnancy?
A. That depends—on when the tear occurred, whether the patient is currently pregnant, and whether there were additional lacerations of the perineum.
ICD-9-CM offers four codes in this setting. Choose one, as follows:
- If you note an anal tear at the time of, or after, delivery but there is no perineal laceration, report 664.6×. This code takes a fifth digit: “1,” for the patient who has just delivered, or “4,” if you are treating the tear after she has been discharged.
- If the tear is noted in addition to a third-degree perineal tear, report 664.2× instead; fifth-digit choices for this code are also “1” and “4.”
- If the patient had an anal tear before delivery, from a prior pregnancy, code 654.8× [congenital or acquired abnormality of the vulva].
- Last, if you are treating the patient for an old anal tear and she is not pregnant at the moment, report 569.43 and add any additional codes that have resulted from the tear, such as fecal incontinence (787.6).
—Melanie Witt, RN, CPC-OGS, MA
The authors report no financial relationships relevant to this article.
CASE Large baby, extensive tear
A 28-year-old primigravida undergoes a forceps delivery with a midline episiotomy for failure to progress in the second stage of labor. At birth, the infant weighs 4 kg (8.8 lb), and the episiotomy extends to the anal verge. The resident who delivered the child is uncertain whether the anal sphincter is involved in the injury and asks a consultant to examine the perineum.
What should this examination entail?
The obstetrician is rarely culpable when a third- or fourth-degree obstetric anal sphincter injury (OASIS) occurs—but there is little excuse for letting one go undetected.
To minimize the risk of undiagnosed OASIS, a digital anorectal examination is warranted—before any suturing—in every woman who delivers vaginally. This practice can help you avoid missing isolated tears, such as “buttonhole” of the rectal mucosa, which can occur even when the anal sphincter remains intact (FIGURE 1), or a third- or fourth-degree tear that can sometimes be present behind apparently intact perineal skin (FIGURE 2).1
Clinical training of physicians and midwives also needs to improve.
Every labor room should have a protocol for management of anal sphincter injury2; this article describes detection, diagnosis, and management, focusing on seven critical questions.
Only a physician formally trained in primary anal sphincter repair (or under supervision) should repair OASIS.
FIGURE 1 Buttonhole tear
A buttonhole tear of the rectal mucosa (arrow) with an intact external anal sphincter (EAS) demonstrated during a digital rectal examination. SOURCE: Sultan AH3 (used with permission).
FIGURE 2 Injury obscured by intact skin
(A) Intact perineum on visual examination. (B) Anal sphincter trauma detected after rectal examination. SOURCE: Sultan AH, Kettle C1 (used with permission).
1. When (and how) should the torn perineum be examined?
The first requisite is informed consent for vaginal and rectal examination immediately after delivery. Also vital are adequate exposure of the perineum, good lighting, and, if necessary, sufficient analgesia to prevent pain-related restriction of the evaluation. It may be advisable to place the patient in the lithotomy position to improve exposure.
After visual examination of the perineum, part the labia and examine the vagina to establish the full extent of the tear. Always identify the apex of the vaginal laceration.
Next, perform a rectal examination to exclude injury to the anorectal mucosa and anal sphincter.3
Palpation is necessary to confirm OASIS
Insert the index finger into the anal canal and the thumb into the vagina and perform a pill-rolling motion to palpate the anal sphincter. If this technique is inconclusive, ask the woman to contract her anal sphincter with your fingers still in place. When the sphincter is disrupted, you feel a distinct gap anteriorly. If the perineal skin is intact, there may be an absence of puckering on the perianal skin over any underlying defect that may not be evident under regional or general anesthesia.
Because the external anal sphincter (EAS) is in a state of tonic contraction, the sphincter ends will retract when it is disrupted. These ends need to be grasped and retrieved at the time of repair.
Also identify the internal anal sphincter (IAS). It is a circular smooth muscle (FIGURE 3) that is paler in appearance (similar to the flesh of raw fish) than the striated EAS (similar to raw red meat).4 Under normal circumstances, the distal end of the IAS lies a few millimeters proximal to the distal end of the EAS (FIGURE 4). However, if the EAS is relaxed due to regional or general anesthesia, the distal end of the IAS will appear to be at a lower level. If the IAS or anal epithelium is torn, the EAS is, invariably, torn, too.
General or regional (spinal, epidural, caudal) anesthesia provides analgesia and muscle relaxation and enables proper evaluation of the full extent of the injury.
FIGURE 3 Grade 3b tear
Grade 3b tear with an intact internal anal sphincter (IAS). The external sphincter (EAS) is being grasped with Allis forceps. Note the difference in appearance of the paler IAS and darker EAS. SOURCE: Sultan AH, Kettle C1 (used with permission).
FIGURE 4 Classification of anal sphincter injury
First- and second-degree injuries are described below.
2. Is endoanal US helpful to detect OASIS?
Endoanal ultrasonography (US) to identify OASIS requires specific expertise, particularly in the immediate postpartum period, when the anal canal is lax (especially after an epidural). Ultimately, however, the diagnosis rests on clinical assessment and a rectal examination because, even if a defect is seen on US, it has to be clinically apparent to be repaired.
In a study by Faltin and colleagues, in which routine postpartum endoanal US was used as the gold standard for diagnosis of OASIS, five of 21 women had unnecessary intervention because the sonographic defect was not clinically visible despite exploration of the anal sphincter.5 As a result of this unnecessary exploration based on endoanal US, 20% of these women developed severe fecal incontinence. Therefore, we believe that OASIS is best detected clinically immediately after delivery, provided the physician performs a careful examination with palpation of the anal sphincter.6 In such a scenario, endoanal US is of limited value.
3. How is obstetric anal sphincter trauma classified?
To standardize the classification of perineal trauma, Sultan proposed the following system, which has been adopted by the Royal College of Obstetricians and Gynaecologists and internationally7-9:
First degree: Laceration of the vaginal epithelium or perineal skin only
Second degree: Involvement of the perineal muscles, but not the anal sphincter
Third degree: Disruption of the anal sphincter muscles (FIGURE 4):
- 3a: Less than 50% thickness of the external sphincter is torn
- 3b: More than 50% thickness of the external sphincter is torn
- 3c: Internal sphincter is also torn
Fourth degree: A third-degree anal tear with disruption of the anal epithelium (FIGURE 4).
If there is any ambiguity about grading of the injury, the higher grade should be selected. For example, if there is uncertainty between grades 3a and 3b, the injury should be classified as Grade 3b.
4. Is an operating room necessary?
OASIS should be repaired in the operating theater, where there is access to good lighting, appropriate equipment, and aseptic conditions. In our unit, we have a specially prepared instrument tray containing:
- a Weislander self-retaining retractor
- 4 Allis tissue forceps
- McIndoe scissors
- tooth forceps
- 4 artery forceps
- stitch scissors
- a needle holder.
In addition, deep retractors (e.g., Deavers) are useful when there are associated paravaginal tears.
5. What surgical technique is recommended?
Buttonhole injury
This type of injury can occur in the rectum without disrupting the anal sphincter or perineum. It is best repaired transvaginally using interrupted Vicryl (polyglactin) sutures.
To minimize the risk of persistent rectovaginal fistula, interpose a second layer of tissue between the rectum and vagina by approximating the rectovaginal fascia. A colostomy is rarely indicated unless a large tear extends above the pelvic floor or there is gross fecal contamination of the wound.
Fourth-degree tear
Repair torn anal epithelium with interrupted Vicryl 3-0 sutures, with the knots tied in the anal lumen. Proponents of this widely described technique argue that it reduces the quantity of foreign body (knots) within the tissue and lowers the risk of infection. Concern about a foreign body probably applies to the use of catgut, which dissolves by proteolysis, rather than to newer synthetic material such as Vicryl or Dexon (polyglycolic acid), which dissolves by hydrolysis.
Subcuticular repair of anal epithelium using a transvaginal approach has also been described and could be equally effective if the terminal knots are secure.10
Sphincter muscles
Repair these muscles using 3-0 polydioxanone (PDS) dyed sutures. Compared with braided sutures, monofilament sutures are believed to lessen the risk of infection, although a randomized controlled trial revealed no difference in suture-related morbidity between Vicryl and PDS at 6 weeks postpartum.11 Complete absorption of PDS takes longer than with Vicryl, with 50% tensile strength lasting more than 3 months, compared with 3 weeks for Vicryl.11 To minimize suture migration, cut suture ends short and ensure that they are covered by the overlying superficial perineal muscles.
Internal anal sphincter. Repair the IAS separately from the EAS. Grasp the ends of the torn muscle using Allis forceps and perform an end-to-end repair with interrupted or mattress 3-0 PDS sutures (FIGURE 5). Overlapping repair can be technically difficult.
There is some evidence that repair of an isolated IAS defect benefits patients with established anal incontinence.
External anal sphincter. Because the EAS is normally under tonic contraction, it tends to retract when torn. Therefore, repair requires identification and grasping of the torn ends using Allis tissue forceps (FIGURE 6).
When the EAS is only partially torn (Grade 3a and some cases of Grade 3b), perform an end-to end repair using 2 or 3 mattress sutures, similar to repair of IAS injury, instead of hemostatic “figure of eight” sutures.
For a full-thickness tear (some cases of Grade 3b or 3c, or Grade 4), overlapping repair may be preferable in experienced hands. The EAS may need to be mobilized by dissecting it free of the ischioanal fat laterally using a pair of McIndoe scissors. The torn ends of the EAS can then be overlapped in “double-breasted” fashion (FIGURE 7) using PDS 3-0 sutures. Proper overlap is possible only when the full length of the torn ends is identified.
Overlapping the ends of the sphincter allows for greater surface area of contact between muscle. In contrast, end-to-end repair can be performed without identifying the full length of the EAS and may give rise to incomplete apposition. Fernando and colleagues demonstrated that, in experienced hands, early primary overlap repair carries a lower risk of fecal urgency and anal incontinence than does immediate primary end-to-end repair.12,13
FIGURE 5 End-to-end repair
Internal anal sphincter (I) repair using mattress sutures, demonstrated on the latex Sultan model, used for training (www.perineum.net) (E, external sphincter; A, anal epithelium). SOURCE: Sultan AH, Thakar R2 (used with permission).
FIGURE 6 Locating the external anal sphincter
The external sphincter (E), grasped with Allis forceps, is surrounded by the capsule (C) and lies medial to the ischioanal fat. SOURCE: Sultan AH, Thakar R2 (used with permission).
FIGURE 7 Overlapping sphincter repair
Repair of a fourth degree tear (demonstrated on the Sultan model) using the overlap repair technique on the external sphincter (E). The anal epithelium (A) and the internal sphincter (I) have also been repaired. SOURCE: Sultan AH, Thakar R2 (used with permission).
Perineal muscles
After repair of the sphincter, suture the perineal muscles to reconstruct the perineal body and provide support to the repaired anal sphincter. A short, deficient perineum would leave the anal sphincter more vulnerable to trauma during a subsequent vaginal delivery.
Next, suture the vaginal skin and approximate the perineal skin using Vicryl Rapide 2-0 subcuticular suture.
Examine, and document, the repair
Perform a rectal and vaginal examination to confirm adequate repair and ensure that no other tears have been missed—and that all tampons or swabs have been removed.
Make detailed notes of the findings and repair. A pro forma pictorial representation of the tears proves very useful when notes are reviewed following complications or during audit or litigation.
6. What does postoperative care entail?
Prophylactic antibiotics are common
No randomized trials have substantiated the benefits of intraoperative and postoperative antibiotics after repair of OASIS. Nevertheless, these drugs are commonly prescribed, especially after fourth- degree tears, because infection and wound breakdown could jeopardize the repair and lead to incontinence or fistula.10,14
We prescribe intravenous broad-spectrum antibiotics such as cefuroxime and metronidazole intraoperatively and continue the drugs orally for 5 days.
Bladder catheterization is recommended
Severe perineal discomfort, especially after instrumental delivery, is a known cause of urinary retention. Moreover, after administration of regional anesthesia, it can take up to 12 hours before bladder sensation returns.
We recommend insertion of a Foley catheter for approximately 24 hours, unless medical staff can ensure that spontaneous voiding occurs at least every 3 to 4 hours without bladder overdistension.
Pain may persist after severe injury
The degree of pain following perineal trauma is related to the extent of the injury. OASIS is frequently associated with other more extensive injuries such as paravaginal tears. In one study, 91% of women continued to complain of severe perineal pain 7 days after OASIS.15
In a systematic review, Hedayati and associates found rectal analgesia, such as diclofenac sodium, to be effective at reducing pain from perineal trauma within the first 24 hours after birth; they also found that women used less additional analgesia within the first 48 hours after birth.16 Diclofenac is almost completely bound to protein, so excretion in breast milk is negligible.17
In women who have undergone repair of a fourth-degree tear, administer oral diclofenac; suppositories may be uncomfortable, and there is a theoretical risk of poor healing associated with local anti-inflammatory agents.
Avoid codeine-based preparations because they may cause constipation and lead to excessive straining and disruption of the repair.
Recommend a stool softener
It is vital that constipation be avoided as the patient heals; passage of constipated stool or fecal impaction can disrupt the repair. We prescribe a stool softener (lactulose, 15 mL twice daily) for 10 to 14 days and have encountered no problem with bowel evacuation.18
We recommend that the patient telephone a healthcare provider 24 to 48 hours after hospital discharge to confirm that bowel evacuation has occurred. If it hasn’t, we add mineral oil, magnesium hydroxide, or another oral bowel stimulant to the stool softener and bulking agent.
Mahoney and colleagues conducted a randomized trial (n=105) of constipating versus laxative regimens and found the latter to be associated with earlier and less painful first bowel motion and earlier hospital discharge.19 Nineteen percent of women following the constipating regimen had troublesome constipation (two required hospitalization for fecal impaction), compared with 5% of women receiving a laxative. There were no significant differences in continence scores, anal manometry, and endoanal US findings.
Give the patient adequate information
Before the patient is discharged from the hospital, we give her a booklet that describes the implications of OASIS and explains when and where to seek help if symptoms of infection or incontinence develop. All women also complete a validated bowel-health and quality-of-life questionnaire regarding conditions prior to the delivery. We also recommend pelvic floor and anal sphincter exercises as soon as her discomfort resolves.
Perform a comprehensive follow-up exam
All women who sustain OASIS should be assessed by a senior obstetrician 6 to 8 weeks after delivery. In our practice, these women are seen in a dedicated perineal clinic.20 The clinic provides a supportive environment and increases the patient’s confidence in the team.21
At the clinic, each woman completes the same symptom questionnaire that she was given before hospital discharge. She then undergoes a genital examination in which the physician checks the degree of scarring, residual granulation tissue, and tenderness; ensures that the patient understands the circumstances surrounding the delivery and injury; and addresses any concerns. All women then undergo anal manometry and endoanal US (FIGURE 8). Each patient is encouraged to continue pelvic floor exercises. If she has minimal sphincter contractility, she may need electrical stimulation.
If a dedicated perineal clinic is unavailable, the patient should be given clear instructions, preferably in writing, before leaving the hospital. During the 6 weeks immediately after delivery, she should be instructed to look for signs of infection or wound dehiscence and to telephone the physician to report any increase in pain or swelling, rectal bleeding, or purulent discharge. Any incontinence of stool or flatus also should be reported.
FIGURE 8 Defect visible on US
Endoanal sonogram showing a defect in the external anal sphincter between 11 o’clock and 1 o’clock (between the yellow arrows) (S, subepithelium; E, external anal sphincter). SOURCE: Sultan AH, Thakar R2 (used with permission).
7. Is vaginal delivery advisable after OASIS?
No randomized trials have determined the most appropriate mode of delivery after a third- or fourth-degree tear. We base our counseling of the patient on a completed symptom questionnaire and findings from manometry and endoanal US (FIGURE 8). If vaginal delivery is contemplated, these tests should be performed during the current pregnancy unless they were abnormal at an earlier date. FIGURE 9 is a simple flow diagram from our unit that illustrates management of subsequent delivery after OASIS.
When determining the mode of delivery, thorough counseling and clear documentation of that counseling are extremely important.
FIGURE 9 How do you determine the mode of delivery after OASIS?
Vaginal delivery is possible unless anal sphincter function is impaired
One study found that when a large sonographic defect (more than one quadrant) is present, or the squeeze-pressure increment (above resting pressure) is less than 20 mm Hg, the risk of impaired continence after a subsequent delivery increases dramatically.22
Based on these findings, we conducted a prospective study that found no deterioration of sphincter function or increase in symptoms after vaginal delivery unless the patient had significant compromise of anal sphincter function before the pregnancy.23 Therefore, we encourage asymptomatic women who have minimal compromise of anal sphincter function to undergo vaginal delivery.
Routine episiotomy is not protective
There is no evidence that routine episiotomy prevents recurrent OASIS. If episiotomy is deemed to be necessary—e.g., for a thick inelastic or scarred perineum—mediolateral episiotomy is preferred.
High likelihood of success in some women
Women who have minimal compromise of anal sphincter function should be counseled that they have an 88% (in centers practicing midline episiotomy) to 95% (in centers practicing mediolateral episiotomy) chance of delivering without sustaining another OASIS.24,25 This should reassure them if they have misgivings about vaginal delivery.
Threshold for C-section is lower if additional risk factors are present
If traumatic delivery is anticipated, as in the presence of one or more additional risk factors (macrosomia, shoulder dystocia, prolonged labor, difficult instrumental delivery), cesarean section may be appropriate.
Consider emotional needs
Some women who have sustained OASIS may be scarred emotionally as well as physically and may find it difficult to cope with the thought of another vaginal delivery. These women deserve sympathy, psychological support, and consideration of their request for cesarean section.
When cesarean is a good idea
Women who have a minor degree of incontinence (e.g., fecal urgency or flatus incontinence) may be managed with dietary advice, constipating agents (loperamide or codeine phosphate), and physiotherapy or biofeedback. These women who have some degree of anal sphincter compromise but whose symptoms are controlled should be counseled that cesarean delivery is recommended (FIGURE 9).
Women who have sustained a previous third- or fourth-degree tear with subsequent severe incontinence should be offered secondary sphincter repair by a colorectal surgeon or urogynecologist with expertise in secondary sphincter repair. All subsequent deliveries by these women should be by cesarean section.
Some women with fecal incontinence may choose to complete their family before embarking on anal sphincter surgery. It remains unclear whether these women should be allowed a vaginal delivery, but it is likely that most damage has already occurred and that the risk of further injury is minimal and possibly insignificant. The benefit of cesarean delivery, if any, should be weighed against its risks for all subsequent pregnancies.
Women who have undergone a previous successful secondary sphincter repair for fecal incontinence should be delivered by cesarean delivery.9
Not all women fit neatly into one category
There are going to be women who do not entirely fit any of the categories described—such as those who have isolated internal sphincter defects or irritable bowel syndrome. Management of these women should be individualized, with the mode of delivery determined by mutual agreement after taking into account symptoms and clinical and other findings.
If there are no facilities for anal manometry and US, the physician should base management on symptoms and clinical evaluation. Asymptomatic women who do not have clinical evidence of sphincter compromise during anal tone assessment may be allowed to undergo vaginal delivery. All women who are symptomatic should be referred to a center with facilities for anorectal assessment to establish the ideal management and mode of delivery.
Pay attention to modifiable risk factors
In the case described at the beginning of this article, two risk factors could have been modified to minimize the patient’s risk of OASIS—namely, midline episiotomy and forceps delivery. In a quasirandomized study by Coats, involving 407 nulliparous women, which compared mediolateral and midline episiotomy (when episiotomy was necessary), tears into or through the anal sphincter occurred in 12% of women undergoing midline episiotomy and 2% of those undergoing mediolateral episiotomy.26
If operative vaginal delivery is required, vacuum extraction is preferred. In a meta-analysis of randomized studies, Thakar and Eason found that fewer women have anal sphincter trauma with vacuum delivery than with forceps.27 One anal sphincter tear is avoided for every 18 women delivered by vacuum extraction instead of forceps. A randomized trial conducted in the United Kingdom involving mediolateral episiotomy found severe vaginal laceration in 17% of forceps deliveries and 11% of vacuum deliveries.28 A randomized controlled trial in Canada involving midline episiotomy found third- or fourth-degree tears in 29% of forceps deliveries, versus 12% of vacuum deliveries.29
Q. What is the proper code for reporting an anal sphincter injury incurred in pregnancy?
A. That depends—on when the tear occurred, whether the patient is currently pregnant, and whether there were additional lacerations of the perineum.
ICD-9-CM offers four codes in this setting. Choose one, as follows:
- If you note an anal tear at the time of, or after, delivery but there is no perineal laceration, report 664.6×. This code takes a fifth digit: “1,” for the patient who has just delivered, or “4,” if you are treating the tear after she has been discharged.
- If the tear is noted in addition to a third-degree perineal tear, report 664.2× instead; fifth-digit choices for this code are also “1” and “4.”
- If the patient had an anal tear before delivery, from a prior pregnancy, code 654.8× [congenital or acquired abnormality of the vulva].
- Last, if you are treating the patient for an old anal tear and she is not pregnant at the moment, report 569.43 and add any additional codes that have resulted from the tear, such as fecal incontinence (787.6).
—Melanie Witt, RN, CPC-OGS, MA
1. Sultan AH, Kettle C. Diagnosis of perineal trauma. In: Sultan AH, Thakar R, Fenner DE, eds. Perineal and Anal Sphincter Trauma. London: Springer; 2007:13-19.
2. Sultan AH, Thakar R. Third and fourth degree tears. In: Sultan AH, Thakar R, Fenner DE, eds. Perineal and Anal Sphincter Trauma. London: Springer; 2007:33-51.
3. Sultan AH. Primary repair of obstetric anal sphincter injury. In: Staskin DR, Cardozo L, ed. Textbook of Female Urology and Urogynaecology. London: ISIS Medical Media; 2006.
4. Thakar R, Fenner DE. Anatomy of the perineum and the anal sphincter. In: Sultan AH, Thakar R, Fenner DE, eds. Perineal and Anal Sphincter Trauma. London: Springer; 2007:1-12.
5. Faltin DL, Boulvain M, Floris LA, Irion O. Diagnosis of anal sphincter tears to prevent fecal incontinence: a randomized controlled trial. Obstet Gynecol. 2005;106:6-13.
6. Andrews V, Thakar R, Sultan AH. Occult anal sphincter injuries—myth or reality. Br J Obstet Gynaecol. 2006;113:195-200.
7. Sultan AH. Obstetric perineal injury and anal incontinence. Clin Risk. 1999;5:193-196.
8. Royal College of Obstetricians and Gynaecologists. Management of third and fourth degree perineal tears following vaginal delivery. Guideline 29. London: RCOG Press; 2001.
9. Norton C, Christensen J, Butler U, et al. Anal Incontinence. 2nd ed. Plymouth: Health Publication Ltd; 2005:985-1044.
10. Sultan AH, Thakar R. Lower genital tract and anal sphincter trauma. Best Pract Res Clin Obstet Gynaecol. 2002;16:99-116.
11. Williams A, Adams EJ, Tincello DG, Alfirevic Z, Walkinshaw SA, Richmond DH. How to repair an anal sphincter injury after vaginal delivery: results of a randomised controlled trial. BJOG. 2006;113:201-207.
12. Fernando RJ, Sultan AH, Kettle C, Radley S, Jones P, O’Brien PMS. Repair techniques for obstetric anal sphincter injuries. A randomized controlled trial. Obstet Gynecol. 2006;107:1261-1268.
13. Fernando R, Sultan AH, Kettle C, Thakar R, Radley S. Methods of repair for obstetric anal sphincter injury. Cochrane Database Syst Rev. 2006;3:CD002866.-
14. Fernando RJ, Sultan AH, Radley S, Jones PW, Johanson RB. Management of obstetric anal sphincter injury: a systematic review and national practice survey. BMC Health Serv Res. 2002;2:9.-
15. MacArthur AJ, MacArthur C. Incidence, severity, and determinants of perineal pain after vaginal delivery: a prospective cohort study. Am J Obstet Gynecol. 2004;191:1199-1204.
16. Hedayati H, Parsons J, Crowther CA. Rectal analgesia for pain from perineal trauma following childbirth. Cochrane Database Syst Rev. 2003;(3):CD003931.-
17. Kettle C, Hills RK, Jones P, Darby L, Gray R, Johanson R. Continuous versus interrupted perineal repair with standard or rapidly absorbed sutures after spontaneous vaginal birth: a randomised controlled trial. Lancet. 2002;359:2217-2223.
18. Sultan AH, Monga AK, Kumar D, Stanton SL. Primary repair of obstetric anal sphincter rupture using the overlap technique. Br J Obstet Gynaecol. 1999;106:318-323.
19. Mahony R, Behan M, O’Herlihy C, O’Connell PR. Randomized, clinical trial of bowel confinement vs. laxative use after primary repair of a third-degree obstetric anal sphincter tear. Dis Colon Rectum. 2004;47:12-17.
20. Thakar R, Sultan A. Postpartum problems and the role of a perineal clinic. In: Sultan AH, Thakar R, Fenner DE, eds. Perineal and Anal Sphincter Trauma. London: Springer; 2007:65-79.
21. Williams A, Lavender T, Richmond DH, Tincello DG. Women’s experiences after a third-degree obstetric anal sphincter tear: a qualitative study. Birth. 2005;32:129-136.
22. Fynes M, Donnelly V, Behan M, O’Connell PR, O’Herlihy C. Effect of second vaginal delivery on anorectal physiology and faecal continence: a prospective study. Lancet. 1999;354:983-986.
23. Scheer I, Thakar R, Sultan A. Should women who sustained obstetric anal sphincter injuries be allowed a vaginal delivery? Neurourol Urodynam. 2006;25:512-513.
24. Peleg D, Kennedy CM, Merrill D, Zlatnik FJ. Risk of repetition of a severe perineal laceration. Obstet Gynecol. 1999;93:1021-1024.
25. Harkin R, Fitzpatrick M, O’Connell PR, O’Herlihy C. Anal sphincter disruption at vaginal delivery: is recurrence predictable? Eur J Obstet Gynaecol Reprod Biol. 2003;109:149-152.
26. Coats PM, Chan KK, Wilkins M, Beard RJ. A comparison between midline and mediolateral episiotomies. Br J Obstet Gynaecol. 1980;87:408-412.
27. Thakar R, Eason E. Prevention of perineal trauma. In: Sultan AH, Thakar R, Fenner DE, eds. Perineal and Anal Sphincter Trauma. London: Springer; 2007:52-64.
28. Johanson RB, Rice C, Doyle M. A randomised prospective study comparing the new vacuum extractor policy with forceps delivery. Br J Obstet Gynaecol. 1993;100:524-530.
29. Bofill JA, Rust OA, Schorr SJ, et al. A randomized prospective trial of the obstetric forceps versus the M-cup vacuum extractor. Am J Obstet Gynecol. 1996;175:1325-1330.
1. Sultan AH, Kettle C. Diagnosis of perineal trauma. In: Sultan AH, Thakar R, Fenner DE, eds. Perineal and Anal Sphincter Trauma. London: Springer; 2007:13-19.
2. Sultan AH, Thakar R. Third and fourth degree tears. In: Sultan AH, Thakar R, Fenner DE, eds. Perineal and Anal Sphincter Trauma. London: Springer; 2007:33-51.
3. Sultan AH. Primary repair of obstetric anal sphincter injury. In: Staskin DR, Cardozo L, ed. Textbook of Female Urology and Urogynaecology. London: ISIS Medical Media; 2006.
4. Thakar R, Fenner DE. Anatomy of the perineum and the anal sphincter. In: Sultan AH, Thakar R, Fenner DE, eds. Perineal and Anal Sphincter Trauma. London: Springer; 2007:1-12.
5. Faltin DL, Boulvain M, Floris LA, Irion O. Diagnosis of anal sphincter tears to prevent fecal incontinence: a randomized controlled trial. Obstet Gynecol. 2005;106:6-13.
6. Andrews V, Thakar R, Sultan AH. Occult anal sphincter injuries—myth or reality. Br J Obstet Gynaecol. 2006;113:195-200.
7. Sultan AH. Obstetric perineal injury and anal incontinence. Clin Risk. 1999;5:193-196.
8. Royal College of Obstetricians and Gynaecologists. Management of third and fourth degree perineal tears following vaginal delivery. Guideline 29. London: RCOG Press; 2001.
9. Norton C, Christensen J, Butler U, et al. Anal Incontinence. 2nd ed. Plymouth: Health Publication Ltd; 2005:985-1044.
10. Sultan AH, Thakar R. Lower genital tract and anal sphincter trauma. Best Pract Res Clin Obstet Gynaecol. 2002;16:99-116.
11. Williams A, Adams EJ, Tincello DG, Alfirevic Z, Walkinshaw SA, Richmond DH. How to repair an anal sphincter injury after vaginal delivery: results of a randomised controlled trial. BJOG. 2006;113:201-207.
12. Fernando RJ, Sultan AH, Kettle C, Radley S, Jones P, O’Brien PMS. Repair techniques for obstetric anal sphincter injuries. A randomized controlled trial. Obstet Gynecol. 2006;107:1261-1268.
13. Fernando R, Sultan AH, Kettle C, Thakar R, Radley S. Methods of repair for obstetric anal sphincter injury. Cochrane Database Syst Rev. 2006;3:CD002866.-
14. Fernando RJ, Sultan AH, Radley S, Jones PW, Johanson RB. Management of obstetric anal sphincter injury: a systematic review and national practice survey. BMC Health Serv Res. 2002;2:9.-
15. MacArthur AJ, MacArthur C. Incidence, severity, and determinants of perineal pain after vaginal delivery: a prospective cohort study. Am J Obstet Gynecol. 2004;191:1199-1204.
16. Hedayati H, Parsons J, Crowther CA. Rectal analgesia for pain from perineal trauma following childbirth. Cochrane Database Syst Rev. 2003;(3):CD003931.-
17. Kettle C, Hills RK, Jones P, Darby L, Gray R, Johanson R. Continuous versus interrupted perineal repair with standard or rapidly absorbed sutures after spontaneous vaginal birth: a randomised controlled trial. Lancet. 2002;359:2217-2223.
18. Sultan AH, Monga AK, Kumar D, Stanton SL. Primary repair of obstetric anal sphincter rupture using the overlap technique. Br J Obstet Gynaecol. 1999;106:318-323.
19. Mahony R, Behan M, O’Herlihy C, O’Connell PR. Randomized, clinical trial of bowel confinement vs. laxative use after primary repair of a third-degree obstetric anal sphincter tear. Dis Colon Rectum. 2004;47:12-17.
20. Thakar R, Sultan A. Postpartum problems and the role of a perineal clinic. In: Sultan AH, Thakar R, Fenner DE, eds. Perineal and Anal Sphincter Trauma. London: Springer; 2007:65-79.
21. Williams A, Lavender T, Richmond DH, Tincello DG. Women’s experiences after a third-degree obstetric anal sphincter tear: a qualitative study. Birth. 2005;32:129-136.
22. Fynes M, Donnelly V, Behan M, O’Connell PR, O’Herlihy C. Effect of second vaginal delivery on anorectal physiology and faecal continence: a prospective study. Lancet. 1999;354:983-986.
23. Scheer I, Thakar R, Sultan A. Should women who sustained obstetric anal sphincter injuries be allowed a vaginal delivery? Neurourol Urodynam. 2006;25:512-513.
24. Peleg D, Kennedy CM, Merrill D, Zlatnik FJ. Risk of repetition of a severe perineal laceration. Obstet Gynecol. 1999;93:1021-1024.
25. Harkin R, Fitzpatrick M, O’Connell PR, O’Herlihy C. Anal sphincter disruption at vaginal delivery: is recurrence predictable? Eur J Obstet Gynaecol Reprod Biol. 2003;109:149-152.
26. Coats PM, Chan KK, Wilkins M, Beard RJ. A comparison between midline and mediolateral episiotomies. Br J Obstet Gynaecol. 1980;87:408-412.
27. Thakar R, Eason E. Prevention of perineal trauma. In: Sultan AH, Thakar R, Fenner DE, eds. Perineal and Anal Sphincter Trauma. London: Springer; 2007:52-64.
28. Johanson RB, Rice C, Doyle M. A randomised prospective study comparing the new vacuum extractor policy with forceps delivery. Br J Obstet Gynaecol. 1993;100:524-530.
29. Bofill JA, Rust OA, Schorr SJ, et al. A randomized prospective trial of the obstetric forceps versus the M-cup vacuum extractor. Am J Obstet Gynecol. 1996;175:1325-1330.