User login
John Bowlby and Heinz Kohut, meet Karl Friston
Attachment theory and object relations theory, meet neuroscience
The bonding process between individuals is essential to human life as we know it. The depth and strength of emotional bonds that we develop with other individuals are among the cardinal aspects of being human.
The strengths of the bonds that we form with others often are the most enduring aspects of our lives and can stretch back in time to include family members and friends who are no longer alive. The brain processes and neurochemicals involved in the bonding process are related to psychological processes using Bayesian theory. Abnormalities in attachment are described in terms of abnormal predictive models.
John Bowlby MD, and colleagues developed a psychological theory of early childhood attachment that shows the impact of different childhood experiences.1 Over many decades, they conducted painstaking observations, trials, and retrials that elucidated specific types of attachment that reflect the child’s internal representations of the parent.
Dr. Bowlby described the mental representations of attachment as “the internal working models of expectations” about the maternal-child relationship. This internal model guides the child’s behaviors, attitudes, and expectations, and is constantly being revised and expanded as the child matures in order to adapt to increasingly complex relationships. More current research has shown that adults who have experienced extreme early childhood adversity develop odd or deficient descriptions of primary attachment relationships, now refined into a low-coherence CC category.2 These children experience attachments that are characterized by feelings of emptiness, inconsistency, and fragmentation.
Object relations theory was created by Heinz Kohut, MD, to explain our internal models of others in psychoanalytic language.3 Dr. Kohut expands the concept of transference describing three new transferential relationships: mirroring, idealized, and twinship transferences. A mirroring transference describes the psychological mechanism whereby “the other” serves as a mirror that reflects back to the person a sense of self-worth and value. A mirroring transference uses the affirming and positive responses of others so that a person then can see positive traits within themselves. The idealizing transference refers to a person’s need for “another” who will make them feel calm and comfortable. The other is idealized as somebody who is calm and soothing when the person cannot provide that on their own. The twinship/alter ego transference occurs when a person feels a sense of likeness with “an other.” These advances in psychoanalytic theory advance our understanding of how we internalize aspects of other people and use these internalizations in our own development.
The neuroscience of attachment was revealed in the study of the children abandoned in Romanian orphanages before the 1989 revolution. These children were placed in orphanages that lacked adequate staff, and they were subjected to profound psychosocial neglect. In the Bucharest Early Intervention Project, the effects of neglect were seen in children aged less than 30-96 months, in EEG data.4 Abnormalities were found in two aberrantly connected brain networks: a hyperconnected parieto-occipital network and a hypoconnected network between left temporal and distributed bilateral regions. This study provides the first evidence of the adverse effects of early psychosocial neglect on the wiring of the developing brain.
Neurochemistry has suggested the impact of oxytocin on the promotion of attachment. Oxytocin has been called the “cuddle hormone,” as it is stimulated in mothers to promote bonding with their infant. Many studies have examined the introduction of intranasal oxytocin increases bonding and trust with others, but recent meta-analyses challenge those findings.5,6 Nevertheless, the process of bonding and attachment is thought to engage the mesocorticolimbic, nigrostriatal dopaminergic, and oxytocinergic systems. Tops and colleagues proposed that oxytocin facilitates a shift from ventral striatal “novelty processing” toward dorsal striatal “familiarity processing.”7 This shift to familiarity is thought to create secure internal working models. In addition, brain activity in specific regions, such as the right caudate, is correlated with romantic love.8 In summary, specific pathways and neurotransmitters underlie the emotional process of bonding and attachment.
However, it is Karl Friston, MD, who suggests a model of brain functioning that describes how we actually process our experiences of the world.9 Dr. Friston uses Bayesian modeling to describe how we interact and understand our world, describing the way we process information. Dr. Friston states that the process of inference that we use to discern our world is a process that uses Bayes’ theorem to update the probability for a specific hypothesis about our world. As more evidence or information becomes available, we update our internal models of the world. Predictive modeling is the term used in Bayesian terms to describe this process of continuous revision of our internal model of the world. Any new sensory input is compared to our current internal model, and if they do not match, our internal model of the world is updated and revised. Dr. Friston states: “As surprise is resolved, Bayesian model evidence is increased. This means that every living organism behaves as if it is a little statistician, analyzing its sensory data in exactly the same way that scientists evaluate the evidence for their hypotheses about how experimental data were caused. In this view, minimizing surprise is, literally, the search for evidence for one’s own existence.” This process of predictive modeling also can be applied to our internal models of other people, meaning that our internal model of another person is an iterative process that changes as the other person changes.
When our experience of the world and others fall into predictive patterns, we expect the “usual” responses from our world and from the people in it. This predictive processing makes it easier for us to understand our world, so that we do not have to continually analyze and reanalyze each event as a new experience. For example, a young child examines the waves as they crash on the shore. For a while, he will watch the waves but soon begins to recognize that there is a predictable pattern. With each ocean he visits, he will examine wave action and soon develop an internal model of what happens when the water reaches the shore. Similarly, when a young child has a secure and loving parent, he will expect security and love in his future relationships. On the other hand, the child who has been subjected to abuse and neglect has an internal working model of the other as nonreciprocal and perhaps irrelevant to their well-being. They will, therefore, have extreme difficulty in understanding the purpose or value of relationships. Their predictive model of the other reflects a lack of input in the case of neglect, or perverted input in the case of abuse. Their internal predictive model will require a great deal of therapeutic healthy inputs to be able to evolve to allow a healthy relationship with the other. This is the work of therapy.
When thinking about relationships, predictive processing makes clinical sense. In a committed partnership, each partner has a predictive model of their partner’s response to events/speech utterances/emotional displays. The prediction of the partner’s response is based on prior experience. This predictive model reduces the need to repeatedly reinterpret the partner’s actions. The partner is understood through an internal predictive model. When one partner changes their behavior, the other partner experiences the world/environment as disrupted or different. The couple, through an iterative process, can incorporate change and grow together. If the patient has an internalized model of a loving relationship, then they are more likely to find a partner who resonates with this internalized model. Using predictive modeling, we can understand how two people with their own internal models of each other interact. As one person approaches the other person, each internal model of the other person finds a “fit” with the behaviors of the other person. When a child with emotional deprivation approaches the other, the child perceives the other person in a way that fits with their prior experience of deprivation. It is an easy fit that requires little internal work, and the patient falls into a familiar relational pattern. This model of predictive processing explains why people repeatedly fall into similar familiar relationships: They recognize the relationship patterns. There is less predictive processing required, less emotional and cognitive work, and therefore less adjustment.
Psychotherapy helps patients by improving their understanding of the link between prior and current experience. Each piece of behavior is analyzed and compared with the patient’s internal model of the event. What neuroscience now provides is a deeper scientific understanding of this process.
In summary, the processes of attachment and bonding occur through oxytocin-mediated caudate–dorsal striatum pathways. Bayesian predictive modeling describes the processes by which our internal models of others are shaped and refined, and underscores the work of our psychotherapies. Neuroscience is beginning to delineate the “where” and “how” of attachment and bonding, thus advancing our understanding of the attachment process and giving us a new language to describe the work of psychotherapy.
References
1. Bowlby J. “A Secure Base: Parent-Child Attachment and Healthy Human Development.” New York: Basic Books, 1988.
2. Speranza AM et al. Attach Hum Dev. 2017 Dec;19(6):613-34.
3. Kohut H. “How Does Analysis Cure?” Chicago: University of Chicago Press, 1984.
4. Stamoulis C et al. J Neurophysiol. 2017 Oct 1;118(4):2275-88.
5. Leng G and Ludwig M.Biol Psychiatry. 2016 Feb 1;79(3):243-50.
6. Leppanen J et al. Neurosci Biobehav Rev. 2017 Jul;78:125-44.
7. Tops M et al. Pharmacol Biochem Behav. 2014 Apr;119:39-48.
8. Acevedo BP et al. Soc Cogn Affect Neurosci. 2012 Feb;7(2):145-59.
9. Friston K. Entropy (Basel). 2012 Nov;14(11):2100-21.
Attachment theory and object relations theory, meet neuroscience
Attachment theory and object relations theory, meet neuroscience
The bonding process between individuals is essential to human life as we know it. The depth and strength of emotional bonds that we develop with other individuals are among the cardinal aspects of being human.
The strengths of the bonds that we form with others often are the most enduring aspects of our lives and can stretch back in time to include family members and friends who are no longer alive. The brain processes and neurochemicals involved in the bonding process are related to psychological processes using Bayesian theory. Abnormalities in attachment are described in terms of abnormal predictive models.
John Bowlby MD, and colleagues developed a psychological theory of early childhood attachment that shows the impact of different childhood experiences.1 Over many decades, they conducted painstaking observations, trials, and retrials that elucidated specific types of attachment that reflect the child’s internal representations of the parent.
Dr. Bowlby described the mental representations of attachment as “the internal working models of expectations” about the maternal-child relationship. This internal model guides the child’s behaviors, attitudes, and expectations, and is constantly being revised and expanded as the child matures in order to adapt to increasingly complex relationships. More current research has shown that adults who have experienced extreme early childhood adversity develop odd or deficient descriptions of primary attachment relationships, now refined into a low-coherence CC category.2 These children experience attachments that are characterized by feelings of emptiness, inconsistency, and fragmentation.
Object relations theory was created by Heinz Kohut, MD, to explain our internal models of others in psychoanalytic language.3 Dr. Kohut expands the concept of transference describing three new transferential relationships: mirroring, idealized, and twinship transferences. A mirroring transference describes the psychological mechanism whereby “the other” serves as a mirror that reflects back to the person a sense of self-worth and value. A mirroring transference uses the affirming and positive responses of others so that a person then can see positive traits within themselves. The idealizing transference refers to a person’s need for “another” who will make them feel calm and comfortable. The other is idealized as somebody who is calm and soothing when the person cannot provide that on their own. The twinship/alter ego transference occurs when a person feels a sense of likeness with “an other.” These advances in psychoanalytic theory advance our understanding of how we internalize aspects of other people and use these internalizations in our own development.
The neuroscience of attachment was revealed in the study of the children abandoned in Romanian orphanages before the 1989 revolution. These children were placed in orphanages that lacked adequate staff, and they were subjected to profound psychosocial neglect. In the Bucharest Early Intervention Project, the effects of neglect were seen in children aged less than 30-96 months, in EEG data.4 Abnormalities were found in two aberrantly connected brain networks: a hyperconnected parieto-occipital network and a hypoconnected network between left temporal and distributed bilateral regions. This study provides the first evidence of the adverse effects of early psychosocial neglect on the wiring of the developing brain.
Neurochemistry has suggested the impact of oxytocin on the promotion of attachment. Oxytocin has been called the “cuddle hormone,” as it is stimulated in mothers to promote bonding with their infant. Many studies have examined the introduction of intranasal oxytocin increases bonding and trust with others, but recent meta-analyses challenge those findings.5,6 Nevertheless, the process of bonding and attachment is thought to engage the mesocorticolimbic, nigrostriatal dopaminergic, and oxytocinergic systems. Tops and colleagues proposed that oxytocin facilitates a shift from ventral striatal “novelty processing” toward dorsal striatal “familiarity processing.”7 This shift to familiarity is thought to create secure internal working models. In addition, brain activity in specific regions, such as the right caudate, is correlated with romantic love.8 In summary, specific pathways and neurotransmitters underlie the emotional process of bonding and attachment.
However, it is Karl Friston, MD, who suggests a model of brain functioning that describes how we actually process our experiences of the world.9 Dr. Friston uses Bayesian modeling to describe how we interact and understand our world, describing the way we process information. Dr. Friston states that the process of inference that we use to discern our world is a process that uses Bayes’ theorem to update the probability for a specific hypothesis about our world. As more evidence or information becomes available, we update our internal models of the world. Predictive modeling is the term used in Bayesian terms to describe this process of continuous revision of our internal model of the world. Any new sensory input is compared to our current internal model, and if they do not match, our internal model of the world is updated and revised. Dr. Friston states: “As surprise is resolved, Bayesian model evidence is increased. This means that every living organism behaves as if it is a little statistician, analyzing its sensory data in exactly the same way that scientists evaluate the evidence for their hypotheses about how experimental data were caused. In this view, minimizing surprise is, literally, the search for evidence for one’s own existence.” This process of predictive modeling also can be applied to our internal models of other people, meaning that our internal model of another person is an iterative process that changes as the other person changes.
When our experience of the world and others fall into predictive patterns, we expect the “usual” responses from our world and from the people in it. This predictive processing makes it easier for us to understand our world, so that we do not have to continually analyze and reanalyze each event as a new experience. For example, a young child examines the waves as they crash on the shore. For a while, he will watch the waves but soon begins to recognize that there is a predictable pattern. With each ocean he visits, he will examine wave action and soon develop an internal model of what happens when the water reaches the shore. Similarly, when a young child has a secure and loving parent, he will expect security and love in his future relationships. On the other hand, the child who has been subjected to abuse and neglect has an internal working model of the other as nonreciprocal and perhaps irrelevant to their well-being. They will, therefore, have extreme difficulty in understanding the purpose or value of relationships. Their predictive model of the other reflects a lack of input in the case of neglect, or perverted input in the case of abuse. Their internal predictive model will require a great deal of therapeutic healthy inputs to be able to evolve to allow a healthy relationship with the other. This is the work of therapy.
When thinking about relationships, predictive processing makes clinical sense. In a committed partnership, each partner has a predictive model of their partner’s response to events/speech utterances/emotional displays. The prediction of the partner’s response is based on prior experience. This predictive model reduces the need to repeatedly reinterpret the partner’s actions. The partner is understood through an internal predictive model. When one partner changes their behavior, the other partner experiences the world/environment as disrupted or different. The couple, through an iterative process, can incorporate change and grow together. If the patient has an internalized model of a loving relationship, then they are more likely to find a partner who resonates with this internalized model. Using predictive modeling, we can understand how two people with their own internal models of each other interact. As one person approaches the other person, each internal model of the other person finds a “fit” with the behaviors of the other person. When a child with emotional deprivation approaches the other, the child perceives the other person in a way that fits with their prior experience of deprivation. It is an easy fit that requires little internal work, and the patient falls into a familiar relational pattern. This model of predictive processing explains why people repeatedly fall into similar familiar relationships: They recognize the relationship patterns. There is less predictive processing required, less emotional and cognitive work, and therefore less adjustment.
Psychotherapy helps patients by improving their understanding of the link between prior and current experience. Each piece of behavior is analyzed and compared with the patient’s internal model of the event. What neuroscience now provides is a deeper scientific understanding of this process.
In summary, the processes of attachment and bonding occur through oxytocin-mediated caudate–dorsal striatum pathways. Bayesian predictive modeling describes the processes by which our internal models of others are shaped and refined, and underscores the work of our psychotherapies. Neuroscience is beginning to delineate the “where” and “how” of attachment and bonding, thus advancing our understanding of the attachment process and giving us a new language to describe the work of psychotherapy.
References
1. Bowlby J. “A Secure Base: Parent-Child Attachment and Healthy Human Development.” New York: Basic Books, 1988.
2. Speranza AM et al. Attach Hum Dev. 2017 Dec;19(6):613-34.
3. Kohut H. “How Does Analysis Cure?” Chicago: University of Chicago Press, 1984.
4. Stamoulis C et al. J Neurophysiol. 2017 Oct 1;118(4):2275-88.
5. Leng G and Ludwig M.Biol Psychiatry. 2016 Feb 1;79(3):243-50.
6. Leppanen J et al. Neurosci Biobehav Rev. 2017 Jul;78:125-44.
7. Tops M et al. Pharmacol Biochem Behav. 2014 Apr;119:39-48.
8. Acevedo BP et al. Soc Cogn Affect Neurosci. 2012 Feb;7(2):145-59.
9. Friston K. Entropy (Basel). 2012 Nov;14(11):2100-21.
The bonding process between individuals is essential to human life as we know it. The depth and strength of emotional bonds that we develop with other individuals are among the cardinal aspects of being human.
The strengths of the bonds that we form with others often are the most enduring aspects of our lives and can stretch back in time to include family members and friends who are no longer alive. The brain processes and neurochemicals involved in the bonding process are related to psychological processes using Bayesian theory. Abnormalities in attachment are described in terms of abnormal predictive models.
John Bowlby MD, and colleagues developed a psychological theory of early childhood attachment that shows the impact of different childhood experiences.1 Over many decades, they conducted painstaking observations, trials, and retrials that elucidated specific types of attachment that reflect the child’s internal representations of the parent.
Dr. Bowlby described the mental representations of attachment as “the internal working models of expectations” about the maternal-child relationship. This internal model guides the child’s behaviors, attitudes, and expectations, and is constantly being revised and expanded as the child matures in order to adapt to increasingly complex relationships. More current research has shown that adults who have experienced extreme early childhood adversity develop odd or deficient descriptions of primary attachment relationships, now refined into a low-coherence CC category.2 These children experience attachments that are characterized by feelings of emptiness, inconsistency, and fragmentation.
Object relations theory was created by Heinz Kohut, MD, to explain our internal models of others in psychoanalytic language.3 Dr. Kohut expands the concept of transference describing three new transferential relationships: mirroring, idealized, and twinship transferences. A mirroring transference describes the psychological mechanism whereby “the other” serves as a mirror that reflects back to the person a sense of self-worth and value. A mirroring transference uses the affirming and positive responses of others so that a person then can see positive traits within themselves. The idealizing transference refers to a person’s need for “another” who will make them feel calm and comfortable. The other is idealized as somebody who is calm and soothing when the person cannot provide that on their own. The twinship/alter ego transference occurs when a person feels a sense of likeness with “an other.” These advances in psychoanalytic theory advance our understanding of how we internalize aspects of other people and use these internalizations in our own development.
The neuroscience of attachment was revealed in the study of the children abandoned in Romanian orphanages before the 1989 revolution. These children were placed in orphanages that lacked adequate staff, and they were subjected to profound psychosocial neglect. In the Bucharest Early Intervention Project, the effects of neglect were seen in children aged less than 30-96 months, in EEG data.4 Abnormalities were found in two aberrantly connected brain networks: a hyperconnected parieto-occipital network and a hypoconnected network between left temporal and distributed bilateral regions. This study provides the first evidence of the adverse effects of early psychosocial neglect on the wiring of the developing brain.
Neurochemistry has suggested the impact of oxytocin on the promotion of attachment. Oxytocin has been called the “cuddle hormone,” as it is stimulated in mothers to promote bonding with their infant. Many studies have examined the introduction of intranasal oxytocin increases bonding and trust with others, but recent meta-analyses challenge those findings.5,6 Nevertheless, the process of bonding and attachment is thought to engage the mesocorticolimbic, nigrostriatal dopaminergic, and oxytocinergic systems. Tops and colleagues proposed that oxytocin facilitates a shift from ventral striatal “novelty processing” toward dorsal striatal “familiarity processing.”7 This shift to familiarity is thought to create secure internal working models. In addition, brain activity in specific regions, such as the right caudate, is correlated with romantic love.8 In summary, specific pathways and neurotransmitters underlie the emotional process of bonding and attachment.
However, it is Karl Friston, MD, who suggests a model of brain functioning that describes how we actually process our experiences of the world.9 Dr. Friston uses Bayesian modeling to describe how we interact and understand our world, describing the way we process information. Dr. Friston states that the process of inference that we use to discern our world is a process that uses Bayes’ theorem to update the probability for a specific hypothesis about our world. As more evidence or information becomes available, we update our internal models of the world. Predictive modeling is the term used in Bayesian terms to describe this process of continuous revision of our internal model of the world. Any new sensory input is compared to our current internal model, and if they do not match, our internal model of the world is updated and revised. Dr. Friston states: “As surprise is resolved, Bayesian model evidence is increased. This means that every living organism behaves as if it is a little statistician, analyzing its sensory data in exactly the same way that scientists evaluate the evidence for their hypotheses about how experimental data were caused. In this view, minimizing surprise is, literally, the search for evidence for one’s own existence.” This process of predictive modeling also can be applied to our internal models of other people, meaning that our internal model of another person is an iterative process that changes as the other person changes.
When our experience of the world and others fall into predictive patterns, we expect the “usual” responses from our world and from the people in it. This predictive processing makes it easier for us to understand our world, so that we do not have to continually analyze and reanalyze each event as a new experience. For example, a young child examines the waves as they crash on the shore. For a while, he will watch the waves but soon begins to recognize that there is a predictable pattern. With each ocean he visits, he will examine wave action and soon develop an internal model of what happens when the water reaches the shore. Similarly, when a young child has a secure and loving parent, he will expect security and love in his future relationships. On the other hand, the child who has been subjected to abuse and neglect has an internal working model of the other as nonreciprocal and perhaps irrelevant to their well-being. They will, therefore, have extreme difficulty in understanding the purpose or value of relationships. Their predictive model of the other reflects a lack of input in the case of neglect, or perverted input in the case of abuse. Their internal predictive model will require a great deal of therapeutic healthy inputs to be able to evolve to allow a healthy relationship with the other. This is the work of therapy.
When thinking about relationships, predictive processing makes clinical sense. In a committed partnership, each partner has a predictive model of their partner’s response to events/speech utterances/emotional displays. The prediction of the partner’s response is based on prior experience. This predictive model reduces the need to repeatedly reinterpret the partner’s actions. The partner is understood through an internal predictive model. When one partner changes their behavior, the other partner experiences the world/environment as disrupted or different. The couple, through an iterative process, can incorporate change and grow together. If the patient has an internalized model of a loving relationship, then they are more likely to find a partner who resonates with this internalized model. Using predictive modeling, we can understand how two people with their own internal models of each other interact. As one person approaches the other person, each internal model of the other person finds a “fit” with the behaviors of the other person. When a child with emotional deprivation approaches the other, the child perceives the other person in a way that fits with their prior experience of deprivation. It is an easy fit that requires little internal work, and the patient falls into a familiar relational pattern. This model of predictive processing explains why people repeatedly fall into similar familiar relationships: They recognize the relationship patterns. There is less predictive processing required, less emotional and cognitive work, and therefore less adjustment.
Psychotherapy helps patients by improving their understanding of the link between prior and current experience. Each piece of behavior is analyzed and compared with the patient’s internal model of the event. What neuroscience now provides is a deeper scientific understanding of this process.
In summary, the processes of attachment and bonding occur through oxytocin-mediated caudate–dorsal striatum pathways. Bayesian predictive modeling describes the processes by which our internal models of others are shaped and refined, and underscores the work of our psychotherapies. Neuroscience is beginning to delineate the “where” and “how” of attachment and bonding, thus advancing our understanding of the attachment process and giving us a new language to describe the work of psychotherapy.
References
1. Bowlby J. “A Secure Base: Parent-Child Attachment and Healthy Human Development.” New York: Basic Books, 1988.
2. Speranza AM et al. Attach Hum Dev. 2017 Dec;19(6):613-34.
3. Kohut H. “How Does Analysis Cure?” Chicago: University of Chicago Press, 1984.
4. Stamoulis C et al. J Neurophysiol. 2017 Oct 1;118(4):2275-88.
5. Leng G and Ludwig M.Biol Psychiatry. 2016 Feb 1;79(3):243-50.
6. Leppanen J et al. Neurosci Biobehav Rev. 2017 Jul;78:125-44.
7. Tops M et al. Pharmacol Biochem Behav. 2014 Apr;119:39-48.
8. Acevedo BP et al. Soc Cogn Affect Neurosci. 2012 Feb;7(2):145-59.
9. Friston K. Entropy (Basel). 2012 Nov;14(11):2100-21.
Antipsychotics, dopamine, and pain
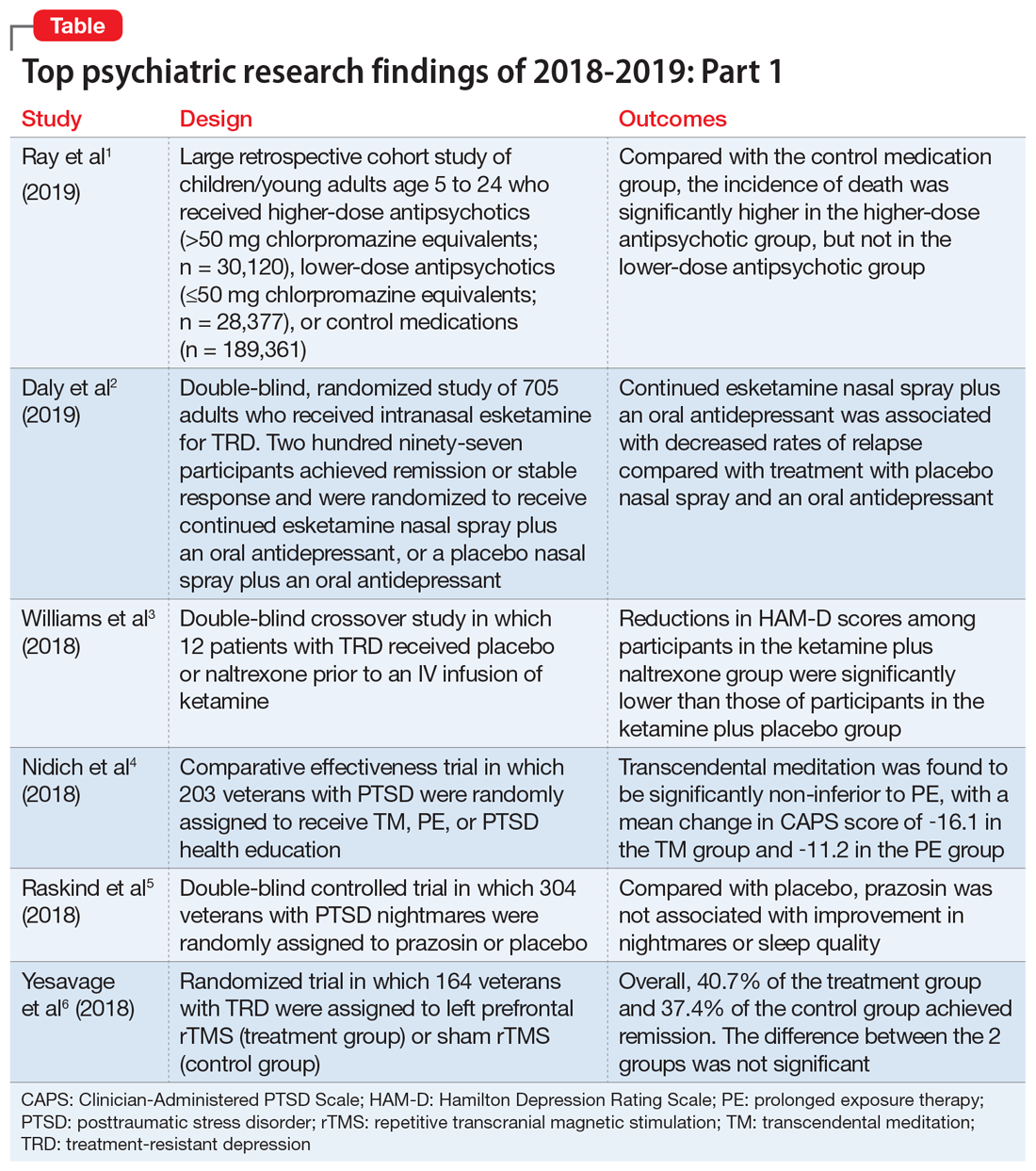
Our understanding of pain mechanisms continues to evolve and, accordingly, so do our treatment strategies. The fundamental differences between acute and chronic pain were only recently recognized; this lack of recognition led to the application of acute pain treatments to chronic pain, contributing to the opioid epidemic in the United States.
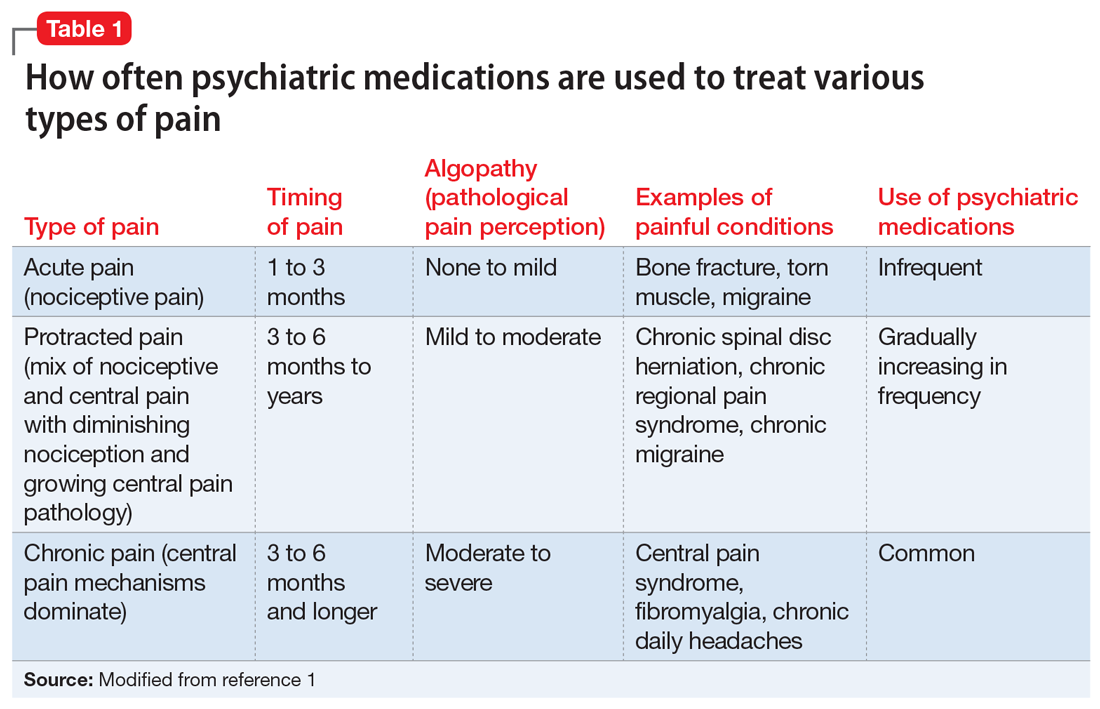
With the diminishing emphasis on opioid medications, researchers are exploring other pharmacologic modalities for treating pain. Many nonopioid psychiatric medications are used off-label for the treatment of pain. Psychiatric medications play a larger role in the management of pain as pain becomes more chronic (Table 11). For simplicity, acute pain may be seen as nociception colored by emotions, and chronic pain as emotions colored by nociception. Protracted pain connects those extremes with a diminishing role of nociception and an increasing role of emotion,1 which may increase the potential role of psychiatric medications, including antipsychotics.
In this article, I discuss the potential role of dopamine in the perception of pain, and review the potential use of first- and second-generation antipsychotics for treating various pain syndromes.
Role of dopamine in pain
There is increasing interest in exploring antipsychotics to treat chronic pain2 because dopamine dysfunction is part of pathological pain perception. Excess dopamine is associated with headaches (dopamine hypersensitivity hypothesis3,4) and dopamine dysfunction is a part of posttraumatic stress disorder (PTSD),5 dissociation,6 paranoia,7 and catastrophizing.8 Somatic psychosis, like any psychosis, can be based on dopamine pathology. Dopaminergic neurons affect nociceptive function in the spinal dorsal horn,9 and dopamine receptors are altered in atypical facial pain,10 burning mouth syndrome,11 and fibromyalgia.12
In normal circumstances, dopamine is fundamentally a protective neurotransmitter. In acute pain, dopamine is powerfully released, making the pain bearable. A patient may describe acute pain as seeming “like it was not happening to me” or “it was like a dream”; both are examples of dopamine-caused dissociation and a possible prediction of subsequent chronification. In chronic pain, pathological mechanisms settle in and take root; therefore, keeping protective dopamine levels high becomes a priority. This is especially common in patients who have experienced abuse or PTSD. The only natural way to keep dopamine up for prolonged periods of time is to decrease pain and stress thresholds. Both phenomena are readily observed in patients with pain. In extreme cases, self-mutilation and involvement in conflicts become pathologically gratifying.
The dopaminergic system is essential for pain control with a tissue injury.13 It becomes pathologically stimulated and increasingly dysfunctional as algopathy (a pathological pain perception) develops. At the same time, a flood or drought of any neurotransmitter is equally bad and may produce similar clinical pictures. Both a lack of and excess of dopamine are associated with pain.14 This is why opposite treatments may be beneficial in different patients with chronic pain. As an example, the use of stimulants15 and bupropion16 has been reported in the treatment of abdominal pain. And, reversely, antipsychotics, especially first-generation agents, may be associated with chronic (tardive) pain, including orofacial and genital pain.17
First-generation antipsychotics
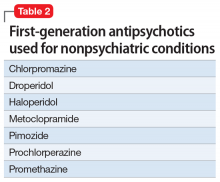
First-generation antipsychotics (FGAs) have been used to treat various nonpsychiatric conditions (Table 2). Although they are powerful D2 receptor inhibitors, FGAs lack the intrinsic ability to counteract the unwanted adverse effects of strong inhibition. As a result, movement disorders and prolactinemia are commonly induced by FGAs. The most dangerous consequence of treatment with these agents is neuroleptic malignant syndrome (NMS).
Continue to: Haloperidol
Haloperidol is prescribed widely by nonpsychiatrists, primarily to treat agitation. Intravenous haloperidol has been used for the abortive treatment of headaches.18 Paradoxically, IV haloperidol is less likely to induce extrapyramidal symptoms (EPS) than the oral formulation because of a more pronounced anticholinergic action in IV use. Haloperidol can help relieve gastroparesis and nausea, especially in IV administration,19 but prolonged oral administration is associated with unwanted movement problems and should be avoided.20
Chlorpromazine is more anticholinergic than haloperidol. It can be used in the abortive treatment of headaches (preferably via IV and IM administration), nausea, hiccups, porphyria, and serotonin syndrome, but it is very sedating and frequently produces hypotension, dangerous QT prolongation, and sensations of thought-blocking.21
Pimozide is reported to help with skin picking, trichotillomania, and somatic hallucinations.22
Droperidol, promethazine, and prochlorperazine are used off-label to treat nausea and headaches. Primary care clinicians may not be aware that these commonly used medications are antipsychotics. Similar to other FGAs, these 3 agents may produce NMS and tardive dyskinesia (TD). The same applies to the prokinetic drug metoclopramide.
Second-generation antipsychotics
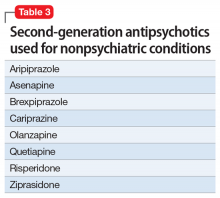
Second-generation antipsychotics (SGAs) work with various serotonin receptors, offsetting and enhancing the antipsychotic function of dopamine blockade. This diminishes but does not eliminate EPS and the risk of TD. Fortunately, the risk of NMS is lower with SGAs than with FGAs. Many SGAs are FDA-approved for treating schizophrenia and other psychiatric disorders, and some have relevance for pain management (Table 3). Many SGAs help with depressive symptoms and are powerful mood stabilizers. As such, they may diminish central over-firing of dopaminergic and serotonergic neurons involved in the pain cascade, which in turn decreases pain transmission and perception. The downside is that in general, SGAs increase the risk of diabetes and hyperlipidemia.
Continue to: Risperidone
Risperidone was the second FDA-approved SGA. Pain practitioners primarily prescribe it for treatmeant-resistant headaches, but patients with fibromyalgia and those with phantom and thalamic pain also may respond. Because risperidone’s properties are similar to that of many FGAs, it may potently cause EPS, TD, and prolactinemia. Neuroleptic malignant syndrome also has been reported.23
Ziprasidone is frequently overlooked by clinicians who treat pain. Although ziprasidone may be sedating, it is powerful as both a preventive and abortive (in an IM formulation) agent for treatment-resistant headaches. This might be attributed to its effects on the 5HT9 receptor. It is approved for treating bipolar depression and has been prescribed to effectively treat anxiety. For patients receiving ziprasidone, QT prolongation needs to be monitored closely.24
Olanzapine was modeled after clozapine and is effective as a mood stabilizer and an antianxiety, antipsychotic, and sleep-promoting medication. It has a useful “mellowing” effect and helps with central pain syndrome management. Patients with fibromyalgia respond well; in some cases, patients with phantom and thalamic pain also respond. Among SGAs prescribed to treat chronic pain, olanzapine has the most published studies. However, the downside is the risk of severe weight gain and diabetes. Usually, if a patient is already overweight, they gain less, but these patients typically are concerned about any additional weight gain.25
Aripiprazole is a partial dopamine agonist. It increases dopamine function in the prefrontal cortex, and by doing so it possibly improves cognition, mental acuity, goal-oriented activity, and attention. At the same time, it decreases dopamine activity in the basal ganglia and limbic system, improving catastrophizing, paranoia, abnormal pain perception, and multiple homeostasis functions. This combination of effects can be invaluable for some patients, but depending on individual susceptibility, aripiprazole might be too activating (causing agitation and akathisia) or too sedating.26
Brexpiprazole is a relative of aripiprazole, but for some patients it is better tolerated, and compliance with this medication usually is good. It partially antagonizes the D2 and 5HT1A receptors while antagonizing the 5HT2A receptors (which decreases the dopamine release in the striatum) and mimics the mechanism of action of an antidepressant. Through alpha-1-adrenergic receptor antagonism, it reduces EPS. All these effects are also part of the mechanisms of action of quetiapine, clozapine, and iloperidone, but brexpiprazole is considered to be the most alpha-1 antagonistic, which is a mechanism of action of other potential pain-controlling medications such as clonidine and tizanidine. In patients with pain who have an overactive noradrenergic system, this property may be beneficial. Its major problem stems from cytochrome P450 2D6 (CYP2D6) enzyme-dependent metabolism, which causes an approximately 5-fold increase in brexpiprazole blood level in poor CYP2D6 metabolizers. Therefore, combining brexpiprazole with CYP2D6 inhibitors such as fluoxetine, paroxetine, and duloxetine would be unwise. Aripiprazole and brexpiprazole are less associated with diabetes and sexual adverse effects than many other SGAs.27
Continue to: Asenapine
Asenapine is an underutilized antipsychotic. Its mechanism of action spans multiple receptors and is less specific in individual receptor activity than other dopamine blockers. It is administered under the tongue due to poor absorption when swallowed, and its molecule has an anesthetic property that causes mouth and tongue numbness/paresthesia. This function may help patients with orofacial pain. Significant somnolence and weight gain (although less than with olanzapine) limit its use. Some patients cannot tolerate the taste.28
Quetiapine is prescribed rather frequently due to its significant antianxiety effect. It is also reported to be beneficial in pain control.29 Weight gain may be severe. In doses smaller than typically administered to patients with bipolar disorder or schizophrenia, quetiapine is widely prescribed off-label for sleep. In lower doses, it acts primarily as an antihistamine (hence the sedation), but at an increased dose it activates the adrenergic system, which offsets sedation. Quetiapine antagonizes H1 histamine and 5HT2
Cariprazine is typically well tolerated because of its benign metabolic profile. It does not increase the QT interval and is not sedating. Cariprazine is a D2 and D3 partial receptor agonist. This allows the medication to inhibit overstimulated dopamine receptors (a desirable effect in pain management) and induces them when the endogenous dopamine level is low (helping with cognition, volition, and attention). Pro-cognitive effects are always beneficial for patients with pain. Cariprazine produces less EPS due to more ventral striatum vs dorsal striatum activity. Mood improvement caused by this medication is attributed to its 5HT2A, 5HT2B, and 5HT2C inverse agonism, which modulates the serotonergic system. Cariprazine will likely have a positive future in pain management because it has shown efficacy in the chronic stress model.33
A complex condition
No single medication or group of medications may be exclusively relied on for treating patients with chronic pain. Identifying alternatives to opioids for treating pain brings more attention to centrally-acting medications that may aid in the stabilization of the nervous system, which can decrease pathological pain perception and help patients cope with chronic painful conditions.
Bottom Line
Antipsychotics may be a valuable asset in the treatment of chronic pain, offering a potential alternative to prescribing opioids for pain. More research is needed to identify specific ways of using dopamine blockade or dopamine enhancement to help patients with chronic pain.
Continue to: Related Resource
Related Resource
- Tripathi A. Antipsychotics for migraines, cluster headaches, and nausea. Current Psychiatry. 2013;12(2):E1-E4.
Drug Brand Names
Aripiprazole • Abilify
Asenapine • Saphris
Brexpiprazole • Rexulti
Bupropion • Wellbutrin, Zyban
Cariprazine • Vraylar
Chlorpromazine • Thorazine
Clonidine • Catapres
Clozapine • Clozaril
Droperidol • Inapsine
Duloxetine • Cymbalta
Fluoxetine • Prozac
Haloperidol • Haldol
Iloperidone • Fanapt
Metoclopramide • Reglan
Olanzapine • Zyprexa
Paroxetine • Paxil
Pimozide • Orap
Prochlorperazine • Compazine
Promethazine • Phenergan
Quetiapine • Seroquel
Risperidone • Risperdal
Tizanidine • Zanaflex
Ziprasidone • Geodon
1. Arbuck D, Pergolizzi J. Algopathy—acknowledging the pathological process of pain chronification. Pract Pain Manag. 2017;17(4):4,26-32.
2. Shin SW, Lee JS, Abdi S, et al. Antipsychotics for patients with pain. Korean J Pain. 2019;32(1):3-11.
3. D’Andrea G, Leone M, Bussone G, et al. Abnormal tyrosine metabolism in chronic cluster headache. Cephalalgia. 2017;37(2):148-153.
4. D’Andrea G, Granella F, Perini F, et al. Platelet levels of dopamine are increased in migraine and cluster headache. Headache. 2006;46(4):585-591.
5. Wolf EJ, Mitchell KS, Logue MW, et al. The dopamine D3 receptor gene, and posttraumatic stress disorder. J Trauma Stress. 2014;27(4):379-387.
6. den Ouden HEM, Daw ND, Fernandez G, et al. Dissociable effects of dopamine and serotonin on reversal learning. Neuron. 2013;80(4):1090-1100.
7. Nour MM, Dahoun T, Schwartenbeck P, et al. Dopaminergic basis for signaling belief updates, but not surprise, and the link to paranoia. Proc Natl Acad Sci U S A. 2018;115(43):E10167-E10176.
8. Zhu H, Clemens S, Sawchuk M, et al. Expression and distribution of all dopamine receptor subtypes (D(1)-D(5)) in the mouse lumbar spinal cord: a real-time polymerase chain reaction and non-autoradiographic in situ hybridization study. Neuroscience. 2007;149:885-897.
9. Wood PB, Schweinhardt P, Jaeger E, et al. Fibromyalgia patients show an abnormal dopamine response to pain. Eur J Neurosci. 2007;25:3576-3582.
10. Hagelberg N, Fossell H, Aalto S, et al. Altered dopamine D2 receptor binding in atypical facial pain. Pain. 2003;106(1-2):43-48.
11. Hagelberg N, Fossell H, Rinne JD, et al. Striatal dopamine D1 and D2 receptors in burning mouth syndrome. Pain. 2003;101(1-2):149-154.
12. Elman I, Borsook D. Common brain mechanisms of chronic pain and addiction. Neuron. 2016;89(1):11-36.
13. Siahposht-Khachaki A, Pourreza P, Ezzatpanah S, et al. Nucleus accumbens dopamine receptors mediate hypothalamus-induced antinociception in the rat formalin test. Eur J Pain. 2017;21(7):1285-1294.
14. Thompson T, Gallop K, Correll CU, et al. Pain perception in Parkinson’s disease: a systematic review and meta-analysis of experimental studies. Aging Res Rev. 2017;35:74-86.
15. Check JH. Chronic unremitting lower abdominal pain quickly abrogated following treatment with amphetamine. Clin Exp Obstet Gynecol. 2016;43(1):109-111.
16. Wilkes S. Bupropion. Drugs Today (Barc). 2006;42(10):671-681.
17. Frei K, Truong DD, Fahn S, et al. The nosology of tardive syndromes. J Neurol Sci. 2018;389:10-16.
18. Honkaniemi J, Liimatainen S, Rainesalo S, et al. Haloperidol in the acute treatment of migraine: a randomized, double-blind, placebo-controlled study. Headache. 2006;46(5):781-787.
19. Murray-Brown F, Dorman S. Haloperidol for the treatment of nausea and vomiting in palliative care patients. Cochrane Database Syst Rev. 2015;(11):CD006271.
20. Gaffigan ME, Bruner DI, Wason C, et al. A randomized controlled trial of intravenous haloperidol vs. intravenous metoclopramide for acute migraine therapy in the emergency department. J Emerg Med. 2015;49(3):326-334.
21. Weinman D, Nicastro O, Akala O, et al. Parenteral treatment of episodic tension-type headache: a systematic review. Headache. 2014;54(2):260-268.
22. Arnold LM, Auchenbach MB, McElroy SL. Psychogenic excoriation. Clinical features, proposed diagnostic criteria, epidemiology, and approaches to treatment. CNS Drugs. 2001;15(5):351-359.
23. Khouzam HR. Psychopharmacology of chronic pain: a focus on antidepressants and atypical antipsychotics. Postgrad Med. 2016;128(3):323-330.
24. Landsness EC, Wang LH, Bucelli RC. Ziprasidone as a potential abortive therapy for status migrainosus. Neurohospitalist. 2016;6(4):151-156.
25. Jimenez XF, Sundararajan T, Covington EC. A systematic review of atypical antipsychotics in chronic pain management: olanzapine demonstrates potential in central sensitization, fibromyalgia, and headache/migraine. Clin J Pain. 2018;34(6):585-591.
26. Fei L, Abrardi L, Mediati RD. Unexpected effect of aripiprazole on nociceptive pain. Ther Adv Psychopharmacol. 2012;2(5):211-212.
27. Markovic M, Gallipani A, Patel KH, et al. Brexpiprazole. Ann Pharmacother. 2017;51(4):315-322.
28. Gerrits M, de Greef R, Peeters P. Effect of absorption site on the pharmacokinetics of sublingual asenapine in healthy male subjects. Biopharm Drug Dispos. 2010;31(5-6):351-357.
29. Heo MH, Kim JY, Hwang I, et al. Analgesic effect of quetiapine in a mouse model of cancer-induced bone pain. Korean J Intern Med. 2017;32(6):1069-1074.
30. Tamburello AC, Lieberman JA, Baum RM, et al. Successful removal of quetiapine from a correctional formulary. J Am Acad Psychiatry Law. 2012;40(4):502-508.
31. Fountoulakis KN, Iacovides A, Kaprinis SG, et al. Diffuse muscle pain with quetiapine. Br J Psychiatry. 2003;182:81.
32. Shintani F. Diminished pain perception in schizophrenia. Lancet. 2010;376(9735):87.
33. Duric V, Banasr M, Franklin T, et al. Cariprazine exhibits anxiolytic and dopamine D3 receptor-dependent antidepressant effects in the chronic stress model. Int J Neuropsychopharmacol. 2017;20(10):788-796
Our understanding of pain mechanisms continues to evolve and, accordingly, so do our treatment strategies. The fundamental differences between acute and chronic pain were only recently recognized; this lack of recognition led to the application of acute pain treatments to chronic pain, contributing to the opioid epidemic in the United States.
With the diminishing emphasis on opioid medications, researchers are exploring other pharmacologic modalities for treating pain. Many nonopioid psychiatric medications are used off-label for the treatment of pain. Psychiatric medications play a larger role in the management of pain as pain becomes more chronic (Table 11). For simplicity, acute pain may be seen as nociception colored by emotions, and chronic pain as emotions colored by nociception. Protracted pain connects those extremes with a diminishing role of nociception and an increasing role of emotion,1 which may increase the potential role of psychiatric medications, including antipsychotics.
In this article, I discuss the potential role of dopamine in the perception of pain, and review the potential use of first- and second-generation antipsychotics for treating various pain syndromes.
Role of dopamine in pain
There is increasing interest in exploring antipsychotics to treat chronic pain2 because dopamine dysfunction is part of pathological pain perception. Excess dopamine is associated with headaches (dopamine hypersensitivity hypothesis3,4) and dopamine dysfunction is a part of posttraumatic stress disorder (PTSD),5 dissociation,6 paranoia,7 and catastrophizing.8 Somatic psychosis, like any psychosis, can be based on dopamine pathology. Dopaminergic neurons affect nociceptive function in the spinal dorsal horn,9 and dopamine receptors are altered in atypical facial pain,10 burning mouth syndrome,11 and fibromyalgia.12
In normal circumstances, dopamine is fundamentally a protective neurotransmitter. In acute pain, dopamine is powerfully released, making the pain bearable. A patient may describe acute pain as seeming “like it was not happening to me” or “it was like a dream”; both are examples of dopamine-caused dissociation and a possible prediction of subsequent chronification. In chronic pain, pathological mechanisms settle in and take root; therefore, keeping protective dopamine levels high becomes a priority. This is especially common in patients who have experienced abuse or PTSD. The only natural way to keep dopamine up for prolonged periods of time is to decrease pain and stress thresholds. Both phenomena are readily observed in patients with pain. In extreme cases, self-mutilation and involvement in conflicts become pathologically gratifying.
The dopaminergic system is essential for pain control with a tissue injury.13 It becomes pathologically stimulated and increasingly dysfunctional as algopathy (a pathological pain perception) develops. At the same time, a flood or drought of any neurotransmitter is equally bad and may produce similar clinical pictures. Both a lack of and excess of dopamine are associated with pain.14 This is why opposite treatments may be beneficial in different patients with chronic pain. As an example, the use of stimulants15 and bupropion16 has been reported in the treatment of abdominal pain. And, reversely, antipsychotics, especially first-generation agents, may be associated with chronic (tardive) pain, including orofacial and genital pain.17
First-generation antipsychotics
First-generation antipsychotics (FGAs) have been used to treat various nonpsychiatric conditions (Table 2). Although they are powerful D2 receptor inhibitors, FGAs lack the intrinsic ability to counteract the unwanted adverse effects of strong inhibition. As a result, movement disorders and prolactinemia are commonly induced by FGAs. The most dangerous consequence of treatment with these agents is neuroleptic malignant syndrome (NMS).
Continue to: Haloperidol
Haloperidol is prescribed widely by nonpsychiatrists, primarily to treat agitation. Intravenous haloperidol has been used for the abortive treatment of headaches.18 Paradoxically, IV haloperidol is less likely to induce extrapyramidal symptoms (EPS) than the oral formulation because of a more pronounced anticholinergic action in IV use. Haloperidol can help relieve gastroparesis and nausea, especially in IV administration,19 but prolonged oral administration is associated with unwanted movement problems and should be avoided.20
Chlorpromazine is more anticholinergic than haloperidol. It can be used in the abortive treatment of headaches (preferably via IV and IM administration), nausea, hiccups, porphyria, and serotonin syndrome, but it is very sedating and frequently produces hypotension, dangerous QT prolongation, and sensations of thought-blocking.21
Pimozide is reported to help with skin picking, trichotillomania, and somatic hallucinations.22
Droperidol, promethazine, and prochlorperazine are used off-label to treat nausea and headaches. Primary care clinicians may not be aware that these commonly used medications are antipsychotics. Similar to other FGAs, these 3 agents may produce NMS and tardive dyskinesia (TD). The same applies to the prokinetic drug metoclopramide.
Second-generation antipsychotics
Second-generation antipsychotics (SGAs) work with various serotonin receptors, offsetting and enhancing the antipsychotic function of dopamine blockade. This diminishes but does not eliminate EPS and the risk of TD. Fortunately, the risk of NMS is lower with SGAs than with FGAs. Many SGAs are FDA-approved for treating schizophrenia and other psychiatric disorders, and some have relevance for pain management (Table 3). Many SGAs help with depressive symptoms and are powerful mood stabilizers. As such, they may diminish central over-firing of dopaminergic and serotonergic neurons involved in the pain cascade, which in turn decreases pain transmission and perception. The downside is that in general, SGAs increase the risk of diabetes and hyperlipidemia.
Continue to: Risperidone
Risperidone was the second FDA-approved SGA. Pain practitioners primarily prescribe it for treatmeant-resistant headaches, but patients with fibromyalgia and those with phantom and thalamic pain also may respond. Because risperidone’s properties are similar to that of many FGAs, it may potently cause EPS, TD, and prolactinemia. Neuroleptic malignant syndrome also has been reported.23
Ziprasidone is frequently overlooked by clinicians who treat pain. Although ziprasidone may be sedating, it is powerful as both a preventive and abortive (in an IM formulation) agent for treatment-resistant headaches. This might be attributed to its effects on the 5HT9 receptor. It is approved for treating bipolar depression and has been prescribed to effectively treat anxiety. For patients receiving ziprasidone, QT prolongation needs to be monitored closely.24
Olanzapine was modeled after clozapine and is effective as a mood stabilizer and an antianxiety, antipsychotic, and sleep-promoting medication. It has a useful “mellowing” effect and helps with central pain syndrome management. Patients with fibromyalgia respond well; in some cases, patients with phantom and thalamic pain also respond. Among SGAs prescribed to treat chronic pain, olanzapine has the most published studies. However, the downside is the risk of severe weight gain and diabetes. Usually, if a patient is already overweight, they gain less, but these patients typically are concerned about any additional weight gain.25
Aripiprazole is a partial dopamine agonist. It increases dopamine function in the prefrontal cortex, and by doing so it possibly improves cognition, mental acuity, goal-oriented activity, and attention. At the same time, it decreases dopamine activity in the basal ganglia and limbic system, improving catastrophizing, paranoia, abnormal pain perception, and multiple homeostasis functions. This combination of effects can be invaluable for some patients, but depending on individual susceptibility, aripiprazole might be too activating (causing agitation and akathisia) or too sedating.26
Brexpiprazole is a relative of aripiprazole, but for some patients it is better tolerated, and compliance with this medication usually is good. It partially antagonizes the D2 and 5HT1A receptors while antagonizing the 5HT2A receptors (which decreases the dopamine release in the striatum) and mimics the mechanism of action of an antidepressant. Through alpha-1-adrenergic receptor antagonism, it reduces EPS. All these effects are also part of the mechanisms of action of quetiapine, clozapine, and iloperidone, but brexpiprazole is considered to be the most alpha-1 antagonistic, which is a mechanism of action of other potential pain-controlling medications such as clonidine and tizanidine. In patients with pain who have an overactive noradrenergic system, this property may be beneficial. Its major problem stems from cytochrome P450 2D6 (CYP2D6) enzyme-dependent metabolism, which causes an approximately 5-fold increase in brexpiprazole blood level in poor CYP2D6 metabolizers. Therefore, combining brexpiprazole with CYP2D6 inhibitors such as fluoxetine, paroxetine, and duloxetine would be unwise. Aripiprazole and brexpiprazole are less associated with diabetes and sexual adverse effects than many other SGAs.27
Continue to: Asenapine
Asenapine is an underutilized antipsychotic. Its mechanism of action spans multiple receptors and is less specific in individual receptor activity than other dopamine blockers. It is administered under the tongue due to poor absorption when swallowed, and its molecule has an anesthetic property that causes mouth and tongue numbness/paresthesia. This function may help patients with orofacial pain. Significant somnolence and weight gain (although less than with olanzapine) limit its use. Some patients cannot tolerate the taste.28
Quetiapine is prescribed rather frequently due to its significant antianxiety effect. It is also reported to be beneficial in pain control.29 Weight gain may be severe. In doses smaller than typically administered to patients with bipolar disorder or schizophrenia, quetiapine is widely prescribed off-label for sleep. In lower doses, it acts primarily as an antihistamine (hence the sedation), but at an increased dose it activates the adrenergic system, which offsets sedation. Quetiapine antagonizes H1 histamine and 5HT2
Cariprazine is typically well tolerated because of its benign metabolic profile. It does not increase the QT interval and is not sedating. Cariprazine is a D2 and D3 partial receptor agonist. This allows the medication to inhibit overstimulated dopamine receptors (a desirable effect in pain management) and induces them when the endogenous dopamine level is low (helping with cognition, volition, and attention). Pro-cognitive effects are always beneficial for patients with pain. Cariprazine produces less EPS due to more ventral striatum vs dorsal striatum activity. Mood improvement caused by this medication is attributed to its 5HT2A, 5HT2B, and 5HT2C inverse agonism, which modulates the serotonergic system. Cariprazine will likely have a positive future in pain management because it has shown efficacy in the chronic stress model.33
A complex condition
No single medication or group of medications may be exclusively relied on for treating patients with chronic pain. Identifying alternatives to opioids for treating pain brings more attention to centrally-acting medications that may aid in the stabilization of the nervous system, which can decrease pathological pain perception and help patients cope with chronic painful conditions.
Bottom Line
Antipsychotics may be a valuable asset in the treatment of chronic pain, offering a potential alternative to prescribing opioids for pain. More research is needed to identify specific ways of using dopamine blockade or dopamine enhancement to help patients with chronic pain.
Continue to: Related Resource
Related Resource
- Tripathi A. Antipsychotics for migraines, cluster headaches, and nausea. Current Psychiatry. 2013;12(2):E1-E4.
Drug Brand Names
Aripiprazole • Abilify
Asenapine • Saphris
Brexpiprazole • Rexulti
Bupropion • Wellbutrin, Zyban
Cariprazine • Vraylar
Chlorpromazine • Thorazine
Clonidine • Catapres
Clozapine • Clozaril
Droperidol • Inapsine
Duloxetine • Cymbalta
Fluoxetine • Prozac
Haloperidol • Haldol
Iloperidone • Fanapt
Metoclopramide • Reglan
Olanzapine • Zyprexa
Paroxetine • Paxil
Pimozide • Orap
Prochlorperazine • Compazine
Promethazine • Phenergan
Quetiapine • Seroquel
Risperidone • Risperdal
Tizanidine • Zanaflex
Ziprasidone • Geodon
Our understanding of pain mechanisms continues to evolve and, accordingly, so do our treatment strategies. The fundamental differences between acute and chronic pain were only recently recognized; this lack of recognition led to the application of acute pain treatments to chronic pain, contributing to the opioid epidemic in the United States.
With the diminishing emphasis on opioid medications, researchers are exploring other pharmacologic modalities for treating pain. Many nonopioid psychiatric medications are used off-label for the treatment of pain. Psychiatric medications play a larger role in the management of pain as pain becomes more chronic (Table 11). For simplicity, acute pain may be seen as nociception colored by emotions, and chronic pain as emotions colored by nociception. Protracted pain connects those extremes with a diminishing role of nociception and an increasing role of emotion,1 which may increase the potential role of psychiatric medications, including antipsychotics.
In this article, I discuss the potential role of dopamine in the perception of pain, and review the potential use of first- and second-generation antipsychotics for treating various pain syndromes.
Role of dopamine in pain
There is increasing interest in exploring antipsychotics to treat chronic pain2 because dopamine dysfunction is part of pathological pain perception. Excess dopamine is associated with headaches (dopamine hypersensitivity hypothesis3,4) and dopamine dysfunction is a part of posttraumatic stress disorder (PTSD),5 dissociation,6 paranoia,7 and catastrophizing.8 Somatic psychosis, like any psychosis, can be based on dopamine pathology. Dopaminergic neurons affect nociceptive function in the spinal dorsal horn,9 and dopamine receptors are altered in atypical facial pain,10 burning mouth syndrome,11 and fibromyalgia.12
In normal circumstances, dopamine is fundamentally a protective neurotransmitter. In acute pain, dopamine is powerfully released, making the pain bearable. A patient may describe acute pain as seeming “like it was not happening to me” or “it was like a dream”; both are examples of dopamine-caused dissociation and a possible prediction of subsequent chronification. In chronic pain, pathological mechanisms settle in and take root; therefore, keeping protective dopamine levels high becomes a priority. This is especially common in patients who have experienced abuse or PTSD. The only natural way to keep dopamine up for prolonged periods of time is to decrease pain and stress thresholds. Both phenomena are readily observed in patients with pain. In extreme cases, self-mutilation and involvement in conflicts become pathologically gratifying.
The dopaminergic system is essential for pain control with a tissue injury.13 It becomes pathologically stimulated and increasingly dysfunctional as algopathy (a pathological pain perception) develops. At the same time, a flood or drought of any neurotransmitter is equally bad and may produce similar clinical pictures. Both a lack of and excess of dopamine are associated with pain.14 This is why opposite treatments may be beneficial in different patients with chronic pain. As an example, the use of stimulants15 and bupropion16 has been reported in the treatment of abdominal pain. And, reversely, antipsychotics, especially first-generation agents, may be associated with chronic (tardive) pain, including orofacial and genital pain.17
First-generation antipsychotics
First-generation antipsychotics (FGAs) have been used to treat various nonpsychiatric conditions (Table 2). Although they are powerful D2 receptor inhibitors, FGAs lack the intrinsic ability to counteract the unwanted adverse effects of strong inhibition. As a result, movement disorders and prolactinemia are commonly induced by FGAs. The most dangerous consequence of treatment with these agents is neuroleptic malignant syndrome (NMS).
Continue to: Haloperidol
Haloperidol is prescribed widely by nonpsychiatrists, primarily to treat agitation. Intravenous haloperidol has been used for the abortive treatment of headaches.18 Paradoxically, IV haloperidol is less likely to induce extrapyramidal symptoms (EPS) than the oral formulation because of a more pronounced anticholinergic action in IV use. Haloperidol can help relieve gastroparesis and nausea, especially in IV administration,19 but prolonged oral administration is associated with unwanted movement problems and should be avoided.20
Chlorpromazine is more anticholinergic than haloperidol. It can be used in the abortive treatment of headaches (preferably via IV and IM administration), nausea, hiccups, porphyria, and serotonin syndrome, but it is very sedating and frequently produces hypotension, dangerous QT prolongation, and sensations of thought-blocking.21
Pimozide is reported to help with skin picking, trichotillomania, and somatic hallucinations.22
Droperidol, promethazine, and prochlorperazine are used off-label to treat nausea and headaches. Primary care clinicians may not be aware that these commonly used medications are antipsychotics. Similar to other FGAs, these 3 agents may produce NMS and tardive dyskinesia (TD). The same applies to the prokinetic drug metoclopramide.
Second-generation antipsychotics
Second-generation antipsychotics (SGAs) work with various serotonin receptors, offsetting and enhancing the antipsychotic function of dopamine blockade. This diminishes but does not eliminate EPS and the risk of TD. Fortunately, the risk of NMS is lower with SGAs than with FGAs. Many SGAs are FDA-approved for treating schizophrenia and other psychiatric disorders, and some have relevance for pain management (Table 3). Many SGAs help with depressive symptoms and are powerful mood stabilizers. As such, they may diminish central over-firing of dopaminergic and serotonergic neurons involved in the pain cascade, which in turn decreases pain transmission and perception. The downside is that in general, SGAs increase the risk of diabetes and hyperlipidemia.
Continue to: Risperidone
Risperidone was the second FDA-approved SGA. Pain practitioners primarily prescribe it for treatmeant-resistant headaches, but patients with fibromyalgia and those with phantom and thalamic pain also may respond. Because risperidone’s properties are similar to that of many FGAs, it may potently cause EPS, TD, and prolactinemia. Neuroleptic malignant syndrome also has been reported.23
Ziprasidone is frequently overlooked by clinicians who treat pain. Although ziprasidone may be sedating, it is powerful as both a preventive and abortive (in an IM formulation) agent for treatment-resistant headaches. This might be attributed to its effects on the 5HT9 receptor. It is approved for treating bipolar depression and has been prescribed to effectively treat anxiety. For patients receiving ziprasidone, QT prolongation needs to be monitored closely.24
Olanzapine was modeled after clozapine and is effective as a mood stabilizer and an antianxiety, antipsychotic, and sleep-promoting medication. It has a useful “mellowing” effect and helps with central pain syndrome management. Patients with fibromyalgia respond well; in some cases, patients with phantom and thalamic pain also respond. Among SGAs prescribed to treat chronic pain, olanzapine has the most published studies. However, the downside is the risk of severe weight gain and diabetes. Usually, if a patient is already overweight, they gain less, but these patients typically are concerned about any additional weight gain.25
Aripiprazole is a partial dopamine agonist. It increases dopamine function in the prefrontal cortex, and by doing so it possibly improves cognition, mental acuity, goal-oriented activity, and attention. At the same time, it decreases dopamine activity in the basal ganglia and limbic system, improving catastrophizing, paranoia, abnormal pain perception, and multiple homeostasis functions. This combination of effects can be invaluable for some patients, but depending on individual susceptibility, aripiprazole might be too activating (causing agitation and akathisia) or too sedating.26
Brexpiprazole is a relative of aripiprazole, but for some patients it is better tolerated, and compliance with this medication usually is good. It partially antagonizes the D2 and 5HT1A receptors while antagonizing the 5HT2A receptors (which decreases the dopamine release in the striatum) and mimics the mechanism of action of an antidepressant. Through alpha-1-adrenergic receptor antagonism, it reduces EPS. All these effects are also part of the mechanisms of action of quetiapine, clozapine, and iloperidone, but brexpiprazole is considered to be the most alpha-1 antagonistic, which is a mechanism of action of other potential pain-controlling medications such as clonidine and tizanidine. In patients with pain who have an overactive noradrenergic system, this property may be beneficial. Its major problem stems from cytochrome P450 2D6 (CYP2D6) enzyme-dependent metabolism, which causes an approximately 5-fold increase in brexpiprazole blood level in poor CYP2D6 metabolizers. Therefore, combining brexpiprazole with CYP2D6 inhibitors such as fluoxetine, paroxetine, and duloxetine would be unwise. Aripiprazole and brexpiprazole are less associated with diabetes and sexual adverse effects than many other SGAs.27
Continue to: Asenapine
Asenapine is an underutilized antipsychotic. Its mechanism of action spans multiple receptors and is less specific in individual receptor activity than other dopamine blockers. It is administered under the tongue due to poor absorption when swallowed, and its molecule has an anesthetic property that causes mouth and tongue numbness/paresthesia. This function may help patients with orofacial pain. Significant somnolence and weight gain (although less than with olanzapine) limit its use. Some patients cannot tolerate the taste.28
Quetiapine is prescribed rather frequently due to its significant antianxiety effect. It is also reported to be beneficial in pain control.29 Weight gain may be severe. In doses smaller than typically administered to patients with bipolar disorder or schizophrenia, quetiapine is widely prescribed off-label for sleep. In lower doses, it acts primarily as an antihistamine (hence the sedation), but at an increased dose it activates the adrenergic system, which offsets sedation. Quetiapine antagonizes H1 histamine and 5HT2
Cariprazine is typically well tolerated because of its benign metabolic profile. It does not increase the QT interval and is not sedating. Cariprazine is a D2 and D3 partial receptor agonist. This allows the medication to inhibit overstimulated dopamine receptors (a desirable effect in pain management) and induces them when the endogenous dopamine level is low (helping with cognition, volition, and attention). Pro-cognitive effects are always beneficial for patients with pain. Cariprazine produces less EPS due to more ventral striatum vs dorsal striatum activity. Mood improvement caused by this medication is attributed to its 5HT2A, 5HT2B, and 5HT2C inverse agonism, which modulates the serotonergic system. Cariprazine will likely have a positive future in pain management because it has shown efficacy in the chronic stress model.33
A complex condition
No single medication or group of medications may be exclusively relied on for treating patients with chronic pain. Identifying alternatives to opioids for treating pain brings more attention to centrally-acting medications that may aid in the stabilization of the nervous system, which can decrease pathological pain perception and help patients cope with chronic painful conditions.
Bottom Line
Antipsychotics may be a valuable asset in the treatment of chronic pain, offering a potential alternative to prescribing opioids for pain. More research is needed to identify specific ways of using dopamine blockade or dopamine enhancement to help patients with chronic pain.
Continue to: Related Resource
Related Resource
- Tripathi A. Antipsychotics for migraines, cluster headaches, and nausea. Current Psychiatry. 2013;12(2):E1-E4.
Drug Brand Names
Aripiprazole • Abilify
Asenapine • Saphris
Brexpiprazole • Rexulti
Bupropion • Wellbutrin, Zyban
Cariprazine • Vraylar
Chlorpromazine • Thorazine
Clonidine • Catapres
Clozapine • Clozaril
Droperidol • Inapsine
Duloxetine • Cymbalta
Fluoxetine • Prozac
Haloperidol • Haldol
Iloperidone • Fanapt
Metoclopramide • Reglan
Olanzapine • Zyprexa
Paroxetine • Paxil
Pimozide • Orap
Prochlorperazine • Compazine
Promethazine • Phenergan
Quetiapine • Seroquel
Risperidone • Risperdal
Tizanidine • Zanaflex
Ziprasidone • Geodon
1. Arbuck D, Pergolizzi J. Algopathy—acknowledging the pathological process of pain chronification. Pract Pain Manag. 2017;17(4):4,26-32.
2. Shin SW, Lee JS, Abdi S, et al. Antipsychotics for patients with pain. Korean J Pain. 2019;32(1):3-11.
3. D’Andrea G, Leone M, Bussone G, et al. Abnormal tyrosine metabolism in chronic cluster headache. Cephalalgia. 2017;37(2):148-153.
4. D’Andrea G, Granella F, Perini F, et al. Platelet levels of dopamine are increased in migraine and cluster headache. Headache. 2006;46(4):585-591.
5. Wolf EJ, Mitchell KS, Logue MW, et al. The dopamine D3 receptor gene, and posttraumatic stress disorder. J Trauma Stress. 2014;27(4):379-387.
6. den Ouden HEM, Daw ND, Fernandez G, et al. Dissociable effects of dopamine and serotonin on reversal learning. Neuron. 2013;80(4):1090-1100.
7. Nour MM, Dahoun T, Schwartenbeck P, et al. Dopaminergic basis for signaling belief updates, but not surprise, and the link to paranoia. Proc Natl Acad Sci U S A. 2018;115(43):E10167-E10176.
8. Zhu H, Clemens S, Sawchuk M, et al. Expression and distribution of all dopamine receptor subtypes (D(1)-D(5)) in the mouse lumbar spinal cord: a real-time polymerase chain reaction and non-autoradiographic in situ hybridization study. Neuroscience. 2007;149:885-897.
9. Wood PB, Schweinhardt P, Jaeger E, et al. Fibromyalgia patients show an abnormal dopamine response to pain. Eur J Neurosci. 2007;25:3576-3582.
10. Hagelberg N, Fossell H, Aalto S, et al. Altered dopamine D2 receptor binding in atypical facial pain. Pain. 2003;106(1-2):43-48.
11. Hagelberg N, Fossell H, Rinne JD, et al. Striatal dopamine D1 and D2 receptors in burning mouth syndrome. Pain. 2003;101(1-2):149-154.
12. Elman I, Borsook D. Common brain mechanisms of chronic pain and addiction. Neuron. 2016;89(1):11-36.
13. Siahposht-Khachaki A, Pourreza P, Ezzatpanah S, et al. Nucleus accumbens dopamine receptors mediate hypothalamus-induced antinociception in the rat formalin test. Eur J Pain. 2017;21(7):1285-1294.
14. Thompson T, Gallop K, Correll CU, et al. Pain perception in Parkinson’s disease: a systematic review and meta-analysis of experimental studies. Aging Res Rev. 2017;35:74-86.
15. Check JH. Chronic unremitting lower abdominal pain quickly abrogated following treatment with amphetamine. Clin Exp Obstet Gynecol. 2016;43(1):109-111.
16. Wilkes S. Bupropion. Drugs Today (Barc). 2006;42(10):671-681.
17. Frei K, Truong DD, Fahn S, et al. The nosology of tardive syndromes. J Neurol Sci. 2018;389:10-16.
18. Honkaniemi J, Liimatainen S, Rainesalo S, et al. Haloperidol in the acute treatment of migraine: a randomized, double-blind, placebo-controlled study. Headache. 2006;46(5):781-787.
19. Murray-Brown F, Dorman S. Haloperidol for the treatment of nausea and vomiting in palliative care patients. Cochrane Database Syst Rev. 2015;(11):CD006271.
20. Gaffigan ME, Bruner DI, Wason C, et al. A randomized controlled trial of intravenous haloperidol vs. intravenous metoclopramide for acute migraine therapy in the emergency department. J Emerg Med. 2015;49(3):326-334.
21. Weinman D, Nicastro O, Akala O, et al. Parenteral treatment of episodic tension-type headache: a systematic review. Headache. 2014;54(2):260-268.
22. Arnold LM, Auchenbach MB, McElroy SL. Psychogenic excoriation. Clinical features, proposed diagnostic criteria, epidemiology, and approaches to treatment. CNS Drugs. 2001;15(5):351-359.
23. Khouzam HR. Psychopharmacology of chronic pain: a focus on antidepressants and atypical antipsychotics. Postgrad Med. 2016;128(3):323-330.
24. Landsness EC, Wang LH, Bucelli RC. Ziprasidone as a potential abortive therapy for status migrainosus. Neurohospitalist. 2016;6(4):151-156.
25. Jimenez XF, Sundararajan T, Covington EC. A systematic review of atypical antipsychotics in chronic pain management: olanzapine demonstrates potential in central sensitization, fibromyalgia, and headache/migraine. Clin J Pain. 2018;34(6):585-591.
26. Fei L, Abrardi L, Mediati RD. Unexpected effect of aripiprazole on nociceptive pain. Ther Adv Psychopharmacol. 2012;2(5):211-212.
27. Markovic M, Gallipani A, Patel KH, et al. Brexpiprazole. Ann Pharmacother. 2017;51(4):315-322.
28. Gerrits M, de Greef R, Peeters P. Effect of absorption site on the pharmacokinetics of sublingual asenapine in healthy male subjects. Biopharm Drug Dispos. 2010;31(5-6):351-357.
29. Heo MH, Kim JY, Hwang I, et al. Analgesic effect of quetiapine in a mouse model of cancer-induced bone pain. Korean J Intern Med. 2017;32(6):1069-1074.
30. Tamburello AC, Lieberman JA, Baum RM, et al. Successful removal of quetiapine from a correctional formulary. J Am Acad Psychiatry Law. 2012;40(4):502-508.
31. Fountoulakis KN, Iacovides A, Kaprinis SG, et al. Diffuse muscle pain with quetiapine. Br J Psychiatry. 2003;182:81.
32. Shintani F. Diminished pain perception in schizophrenia. Lancet. 2010;376(9735):87.
33. Duric V, Banasr M, Franklin T, et al. Cariprazine exhibits anxiolytic and dopamine D3 receptor-dependent antidepressant effects in the chronic stress model. Int J Neuropsychopharmacol. 2017;20(10):788-796
1. Arbuck D, Pergolizzi J. Algopathy—acknowledging the pathological process of pain chronification. Pract Pain Manag. 2017;17(4):4,26-32.
2. Shin SW, Lee JS, Abdi S, et al. Antipsychotics for patients with pain. Korean J Pain. 2019;32(1):3-11.
3. D’Andrea G, Leone M, Bussone G, et al. Abnormal tyrosine metabolism in chronic cluster headache. Cephalalgia. 2017;37(2):148-153.
4. D’Andrea G, Granella F, Perini F, et al. Platelet levels of dopamine are increased in migraine and cluster headache. Headache. 2006;46(4):585-591.
5. Wolf EJ, Mitchell KS, Logue MW, et al. The dopamine D3 receptor gene, and posttraumatic stress disorder. J Trauma Stress. 2014;27(4):379-387.
6. den Ouden HEM, Daw ND, Fernandez G, et al. Dissociable effects of dopamine and serotonin on reversal learning. Neuron. 2013;80(4):1090-1100.
7. Nour MM, Dahoun T, Schwartenbeck P, et al. Dopaminergic basis for signaling belief updates, but not surprise, and the link to paranoia. Proc Natl Acad Sci U S A. 2018;115(43):E10167-E10176.
8. Zhu H, Clemens S, Sawchuk M, et al. Expression and distribution of all dopamine receptor subtypes (D(1)-D(5)) in the mouse lumbar spinal cord: a real-time polymerase chain reaction and non-autoradiographic in situ hybridization study. Neuroscience. 2007;149:885-897.
9. Wood PB, Schweinhardt P, Jaeger E, et al. Fibromyalgia patients show an abnormal dopamine response to pain. Eur J Neurosci. 2007;25:3576-3582.
10. Hagelberg N, Fossell H, Aalto S, et al. Altered dopamine D2 receptor binding in atypical facial pain. Pain. 2003;106(1-2):43-48.
11. Hagelberg N, Fossell H, Rinne JD, et al. Striatal dopamine D1 and D2 receptors in burning mouth syndrome. Pain. 2003;101(1-2):149-154.
12. Elman I, Borsook D. Common brain mechanisms of chronic pain and addiction. Neuron. 2016;89(1):11-36.
13. Siahposht-Khachaki A, Pourreza P, Ezzatpanah S, et al. Nucleus accumbens dopamine receptors mediate hypothalamus-induced antinociception in the rat formalin test. Eur J Pain. 2017;21(7):1285-1294.
14. Thompson T, Gallop K, Correll CU, et al. Pain perception in Parkinson’s disease: a systematic review and meta-analysis of experimental studies. Aging Res Rev. 2017;35:74-86.
15. Check JH. Chronic unremitting lower abdominal pain quickly abrogated following treatment with amphetamine. Clin Exp Obstet Gynecol. 2016;43(1):109-111.
16. Wilkes S. Bupropion. Drugs Today (Barc). 2006;42(10):671-681.
17. Frei K, Truong DD, Fahn S, et al. The nosology of tardive syndromes. J Neurol Sci. 2018;389:10-16.
18. Honkaniemi J, Liimatainen S, Rainesalo S, et al. Haloperidol in the acute treatment of migraine: a randomized, double-blind, placebo-controlled study. Headache. 2006;46(5):781-787.
19. Murray-Brown F, Dorman S. Haloperidol for the treatment of nausea and vomiting in palliative care patients. Cochrane Database Syst Rev. 2015;(11):CD006271.
20. Gaffigan ME, Bruner DI, Wason C, et al. A randomized controlled trial of intravenous haloperidol vs. intravenous metoclopramide for acute migraine therapy in the emergency department. J Emerg Med. 2015;49(3):326-334.
21. Weinman D, Nicastro O, Akala O, et al. Parenteral treatment of episodic tension-type headache: a systematic review. Headache. 2014;54(2):260-268.
22. Arnold LM, Auchenbach MB, McElroy SL. Psychogenic excoriation. Clinical features, proposed diagnostic criteria, epidemiology, and approaches to treatment. CNS Drugs. 2001;15(5):351-359.
23. Khouzam HR. Psychopharmacology of chronic pain: a focus on antidepressants and atypical antipsychotics. Postgrad Med. 2016;128(3):323-330.
24. Landsness EC, Wang LH, Bucelli RC. Ziprasidone as a potential abortive therapy for status migrainosus. Neurohospitalist. 2016;6(4):151-156.
25. Jimenez XF, Sundararajan T, Covington EC. A systematic review of atypical antipsychotics in chronic pain management: olanzapine demonstrates potential in central sensitization, fibromyalgia, and headache/migraine. Clin J Pain. 2018;34(6):585-591.
26. Fei L, Abrardi L, Mediati RD. Unexpected effect of aripiprazole on nociceptive pain. Ther Adv Psychopharmacol. 2012;2(5):211-212.
27. Markovic M, Gallipani A, Patel KH, et al. Brexpiprazole. Ann Pharmacother. 2017;51(4):315-322.
28. Gerrits M, de Greef R, Peeters P. Effect of absorption site on the pharmacokinetics of sublingual asenapine in healthy male subjects. Biopharm Drug Dispos. 2010;31(5-6):351-357.
29. Heo MH, Kim JY, Hwang I, et al. Analgesic effect of quetiapine in a mouse model of cancer-induced bone pain. Korean J Intern Med. 2017;32(6):1069-1074.
30. Tamburello AC, Lieberman JA, Baum RM, et al. Successful removal of quetiapine from a correctional formulary. J Am Acad Psychiatry Law. 2012;40(4):502-508.
31. Fountoulakis KN, Iacovides A, Kaprinis SG, et al. Diffuse muscle pain with quetiapine. Br J Psychiatry. 2003;182:81.
32. Shintani F. Diminished pain perception in schizophrenia. Lancet. 2010;376(9735):87.
33. Duric V, Banasr M, Franklin T, et al. Cariprazine exhibits anxiolytic and dopamine D3 receptor-dependent antidepressant effects in the chronic stress model. Int J Neuropsychopharmacol. 2017;20(10):788-796
Buspirone: A forgotten friend
In general, when a medication goes off patent, marketing for it significantly slows down or comes to a halt. Studies have shown that physicians’ prescribing habits are influenced by pharmaceutical representatives and companies.1 This phenomenon may have an unforeseen adverse effect: once an effective and inexpensive medication “goes generic,” its use may fall out of favor. Additionally, physicians may have concerns about prescribing generic medications, such as perceiving them as less effective and conferring more adverse effects compared with brand-name formulations.2 One such generic medication is buspirone, which originally was branded as BuSpar.
Anxiety disorders are the most common psychiatric diagnoses, and at times are the most challenging to treat.3 Anecdotally, we often see benzodiazepines prescribed as first-line monotherapy for acute and chronic anxiety, but because these agents can cause physical dependence and a withdrawal reaction, alternative anxiolytic medications should be strongly considered. Despite its age, buspirone still plays a role in the treatment of anxiety, and its off-label use can also be useful in certain populations and scenarios. In this article, we delve into buspirone’s mechanism of action, discuss its advantages and challenges, and what you need to know when prescribing it.
How buspirone works
Buspirone was originally described as an anxiolytic agent that was pharmacologically unrelated to traditional anxiety-reducing medications (ie, benzodiazepines and barbiturates).4
The antidepressants vortioxetine and vilazodone exhibit dual-action at both serotonin reuptake transporters and 5HT1A receptors; thus, they work like an SSRI and buspirone combined.6 Although some patients may find it more convenient to take a dual-action pill over 2 separate ones, some insurance companies do not cover these newer agents. Additionally, prescribing buspirone separately allows for more precise dosing, which may lower the risk of adverse effects.
Buspirone is a major substrate for cytochrome P450 (CYP) 3A4 and a minor for CYP2D6, so caution must be advised if considering buspirone for a patient receiving any CYP3A4 inducers and/or inhibitors,7 including grapefruit juice.8
Dose adjustments are not necessary for age and sex, which allows for highly consistent dosing.4 However, as with prescribing medications in any geriatric population, lower starting doses and slower titration of buspirone may be necessary to avoid potential adverse effects due to the alterations of pharmacodynamic and pharmacokinetic processes that occur as patients age.9
Advantages of buspirone
Works well as an add-on to other medications. While buspirone in adequate doses may be helpful as monotherapy in GAD, it can also be helpful in other, more complex psychiatric scenarios. Sumiyoshi et al10 observed improvement in scores on the Digit Symbol Substitution Test when buspirone was added to a second-generation antipsychotic (SGA), which suggests buspirone may help improve attention in patients with schizophrenia. It has been postulated that buspirone may also be helpful for cognitive dysfunction in patients with Alzheimer’s disease.11 Buspirone has been used to treat comorbid anxiety and alcohol use disorder, resulting in reduced anxiety, longer latency to relapse, and fewer drinking days during a 12-week treatment program.12 Buspirone has been more effective than placebo for treating post-stroke anxiety.13
Continue to: Patients who receive...
Patients who receive an SSRI, such as citalopram, but are not able to achieve a substantial improvement in their depressive and/or anxious symptoms may benefit from the addition of buspirone to their treatment regimen.14,15
A favorable adverse-effect profile. There are no absolute contraindications to buspirone except a history of hypersensitivity.4 Buspirone generally is well tolerated and carries a low risk of adverse effects. The most common adverse effects are dizziness and nausea.6 Buspirone is not sedating.
Potentially safe for patients who are pregnant. Unlike many other first-line agents for anxiety, such as SSRIs, buspirone has an FDA Category B classification, meaning animal studies have shown no adverse events during pregnancy.4 The FDA Pregnancy and Lactation Labeling Rule applies only to medications that entered the market on or after June 30, 2001; unfortunately, buspirone is excluded from this updated categorization.16 As with any medication being considered for pregnant or lactating women, the prescriber and patient must weigh the benefits vs the risks to determine if buspirone is appropriate for any individual patient.
No adverse events have been reported from abrupt discontinuation of buspirone.17
Inexpensive. Buspirone is generic and extremely inexpensive. According to GoodRx.com, a 30-day supply of 5-mg tablets for twice-daily dosing can cost $4.18 A maximum daily dose (prescribed as 2 pills, 15 mg twice daily) may cost approximately $18/month.18 Thus, buspirone is a good option for uninsured or underinsured patients, for whom this would be more affordable than other anxiolytic medications.
Continue to: May offset certain adverse effects
May offset certain adverse effects. Sexual dysfunction is a common adverse effect of SSRIs. One strategy to offset this phenomenon is to add bupropion. However, in a randomized controlled trial, Landén et al19 found that sexual adverse effects induced by SSRIs were greatly mitigated by adding buspirone, even within the first week of treatment. This improvement was more marked in women than in men, which is helpful because sexual dysfunction in women is generally resistant to other interventions.20 Unlike
Unlikely to cause extrapyramidal symptoms (EPS). Because of its central D2 antagonism, buspirone has a low potential (<1%) to produce EPS. Buspirone has even been shown to reverse
The Table4 highlights key points to bear in mind when prescribing buspirone.
Challenges with buspirone
Response is not immediate. Unlike benzodiazepines, buspirone does not have an immediate onset of action.22 With buspirone monotherapy, response may be seen in approximately 2 to 4 weeks.23 Therefore, patients transitioning from a quick-onset benzodiazepine to buspirone may not report a good response. However, as noted above, when using buspirone to treat SSRI-induced sexual dysfunction, response may emerge within 1 week.19 Buspirone also lacks the euphoric and sedative qualities of benzodiazepines that patients may prefer.
Not for patients with hepatic and renal impairment. Because plasma levels of buspirone are elevated in patients with hepatic and renal impairment, this medication is not ideal for use in these populations.4
Continue to: Contraindicated in patients receiving MAOIs
Contraindicated in patients receiving MAOIs. Buspirone should not be prescribed to patients with depression who are receiving treatment with a monoamine oxidase inhibitor (MAOI) because the combination may precipitate a hypertensive reaction.4 A minimum washout period of 14 days from the MAOI is necessary before initiating buspirone.9
Idiosyncratic adverse effects. As with all pharmaceuticals, buspirone may produce idiosyncratic adverse effects. Faber and Sansone24 reported a case of a woman who experienced hair loss 3 months into treatment with buspirone. After cessation, her alopecia resolved.
Questionable efficacy for some anxiety subtypes. Buspirone has been studied as a treatment of other common psychiatric conditions, such as social phobia and anxiety in the setting of smoking cessation. However, it has not proven to be effective over placebo in treating these anxiety subtypes.25,26
Short half-life. Because of its relatively short half-life (2 to 3 hours), buspirone requires dosing 2 to 3 times a day, which could increase the risk of noncompliance.4 However, some patients might prefer multiple dosing throughout the day due to perceived better coverage of their anxiety symptoms.
Limited incentive for future research. Because buspirone is available only as a generic formulation, there is little financial incentive for pharmaceutical companies and other interested parties to study what may be valuable uses for buspirone. For example, there is no data available on comparative augmentation of buspirone and SGAs with antidepressants for depression and/or anxiety. There is also little data available about buspirone prescribing trends or why buspirone may be underutilized in clinical practice today.
Continue to: Unfortunately, historical and longitudinal...
Unfortunately, historical and longitudinal data on the prescribing practices of buspirone is limited because the original branded medication, BuSpar, is no longer on the market. However, this medication offers multiple advantages over other agents used to treat anxiety, and it should not be forgotten when formulating a treatment regimen for patients with anxiety and/or depression.
Bottom Line
Buspirone is a safe, low-cost, effective treatment option for patients with anxiety and may be helpful as an augmenting agent for depression. Because of its efficacy and high degree of tolerability, it should be prioritized higher in our treatment algorithms and be a part of our routine pharmacologic armamentarium.
Related Resources
- Howland RH. Buspirone: Back to the future. J Psychosoc Nurs Ment Health Serv. 2015;53(11):21-24.
- Strawn JR, Mills JA, Cornwall GJ, et al. Buspirone in children and adolescents with anxiety: a review and Bayesian analysis of abandoned randomized controlled trials. J Child Adolesc Psychopharmacol. 2018;28(1):2-9.
Drug Brand Names
Bupropion • Wellbutrin, Zyban
Buspirone • BuSpar
Citalopram • Celexa
Haloperidol • Haldol
Vilazodone • Viibryd
Vortioxetine • Trintellix
1. Fickweiler F, Fickweiler W, Urbach E. Interactions between physicians and the pharmaceutical industry generally and sales representatives specifically and their association with physicians’ attitudes and prescribing habits: a systematic review. BMJ Open. 2017;7(9):e016408. doi: 10.1136/bmjopen-2017-016408.
2. Haque M. Generic medicine and prescribing: a quick assessment. Adv Hum Biol. 2017;7(3):101-108.
3. National Alliance on Mental Illness. Anxiety disorders. https://www.nami.org/Learn-More/Mental-Health-Conditions/Anxiety-Disorders. Published December 2017. Accessed November 26, 2019.
4. Buspar [package insert]. Princeton, NJ: Bristol-Myers Squibb Company; 2000.
5. Hjorth S, Carlsson A. Buspirone: effects on central monoaminergic transmission-possible relevance to animal experimental and clinical findings. Eur J Pharmacol. 1982:83;299-303.
6. Stahl SM. Stahl’s essential psychopharmacology: neuroscientific basis and practical applications, 4th ed. Cambridge, United Kingdom: Cambridge University Press; 2013.
7. Buspirone tablets [package insert]. East Brunswick, NJ: Strides Pharma Inc; 2017.
8. Lilja JJ, Kivistö KT, Backman, JT, et al. Grapefruit juice substantially increases plasma concentrations of buspirone. Clin Pharmacol Ther. 1998;64:655-660.
9. Stahl SM. Stahl’s essential psychopharmacology: prescriber’s guide, 6th ed. Cambridge, United Kingdom: Cambridge University Press; 2017.
10. Sumiyoshi T, Park S, Jayathilake K. Effect of buspirone, a serotonin1A partial agonist, on cognitive function in schizophrenia: a randomized, double-blind, placebo-controlled study. Schizophr Res. 2007;95(1-3):158-168.
11. Schechter LE, Dawson LA, Harder JA. The potential utility of 5-HT1A receptor antagonists in the treatment of cognitive dysfunction associated with Alzheimer’s disease. Curr Pharm Des. 2002;8(2):139-145.
12. Kranzler HR, Burleson JA, Del Boca FK. Buspirone treatment of anxious alcoholics: a placebo-controlled trial. Arch Gen Psychiatry. 1994;51(9):720-731.
13. Burton CA, Holmes J, Murray J, et al. Interventions for treating anxiety after stroke. Cochrane Database Syst Rev. 2011;12:1-25.
14. Appelberg BG, Syvälahti EK, Koskinen TE, et al. Patients with severe depression may benefit from buspirone augmentation of selective serotonin reuptake inhibitors: results from a placebo-controlled, randomized, double-blind, placebo wash-in study. J Clin Psychiatry. 2001; 62(6):448-452.
15. American Psychiatric Association. Practice guideline for the treatment of patients with major depressive disorder. 3rd edition. https://psychiatryonline.org/pb/assets/raw/sitewide/practice_guidelines/guidelines/mdd.pdf. Published May 2010. Accessed November 2019.
16. U.S. Food and Drug Administration. Pregnancy and lactation labeling (drugs) final rule. https://www.fda.gov/drugs/labeling/pregnancy-and-lactation-labeling-drugs-final-rule. Published September 11, 2019. Accessed November 26, 2019.
17. Goa KL, Ward A. Buspirone. A preliminary review of its pharmacological properties and therapeutic efficacy as an anxiolytic. Drugs. 1986;32(2):114-129.
18. GoodRx. Buspar prices, coupons, & savings tips in U.S. area code 08054. https://www.goodrx.com/buspar. Accessed June 6, 2019.
19. Landén M, Eriksson E, Agren H, et al. Effect of buspirone on sexual dysfunction in depressed patients treated with selective serotonin reuptake inhibitors. J Clin Psychopharmacol. 1999;19(3):268-271.
20. Hensley PL, Nurnberg HG. SSRI sexual dysfunction: a female perspective. J Sex Marital Ther. 2002;28(suppl 1):143-153.
21. Haleem DJ, Samad N, Haleem MA. Reversal of haloperidol-induced extrapyramidal symptoms by buspirone: a time-related study. Behav Pharmacol. 2007;18(2):147-153.
22. Kaplan SS, Saddock BJ, Grebb JA. Synopsis of psychiatry. 11th ed. Philadelphia, PA: Wolters Kluwer; 2014.
23. National Alliance on Mental Health. Buspirone (BuSpar). https://www.nami.org/Learn-More/Treatment/Mental-Health-Medications/Types-of-Medication/Buspirone-(BuSpar). Published January 2019. Accessed November 26, 2019.
24. Faber J, Sansone RA. Buspirone: a possible cause of alopecia. Innov Clin Neurosci. 2013;10(1):13.
25. Van Vliet IM, Den Boer JA, Westenberg HGM, et al. Clinical effects of buspirone in social phobia, a double-blind placebo controlled study. J Clin Psychiatry. 1997;58(4):164-168.
26. Schneider NG, Olmstead RE, Steinberg C, et al. Efficacy of buspirone in smoking cessation: a placebo‐controlled trial. Clin Pharmacol Ther. 1996;60(5):568-575.
In general, when a medication goes off patent, marketing for it significantly slows down or comes to a halt. Studies have shown that physicians’ prescribing habits are influenced by pharmaceutical representatives and companies.1 This phenomenon may have an unforeseen adverse effect: once an effective and inexpensive medication “goes generic,” its use may fall out of favor. Additionally, physicians may have concerns about prescribing generic medications, such as perceiving them as less effective and conferring more adverse effects compared with brand-name formulations.2 One such generic medication is buspirone, which originally was branded as BuSpar.
Anxiety disorders are the most common psychiatric diagnoses, and at times are the most challenging to treat.3 Anecdotally, we often see benzodiazepines prescribed as first-line monotherapy for acute and chronic anxiety, but because these agents can cause physical dependence and a withdrawal reaction, alternative anxiolytic medications should be strongly considered. Despite its age, buspirone still plays a role in the treatment of anxiety, and its off-label use can also be useful in certain populations and scenarios. In this article, we delve into buspirone’s mechanism of action, discuss its advantages and challenges, and what you need to know when prescribing it.
How buspirone works
Buspirone was originally described as an anxiolytic agent that was pharmacologically unrelated to traditional anxiety-reducing medications (ie, benzodiazepines and barbiturates).4
The antidepressants vortioxetine and vilazodone exhibit dual-action at both serotonin reuptake transporters and 5HT1A receptors; thus, they work like an SSRI and buspirone combined.6 Although some patients may find it more convenient to take a dual-action pill over 2 separate ones, some insurance companies do not cover these newer agents. Additionally, prescribing buspirone separately allows for more precise dosing, which may lower the risk of adverse effects.
Buspirone is a major substrate for cytochrome P450 (CYP) 3A4 and a minor for CYP2D6, so caution must be advised if considering buspirone for a patient receiving any CYP3A4 inducers and/or inhibitors,7 including grapefruit juice.8
Dose adjustments are not necessary for age and sex, which allows for highly consistent dosing.4 However, as with prescribing medications in any geriatric population, lower starting doses and slower titration of buspirone may be necessary to avoid potential adverse effects due to the alterations of pharmacodynamic and pharmacokinetic processes that occur as patients age.9
Advantages of buspirone
Works well as an add-on to other medications. While buspirone in adequate doses may be helpful as monotherapy in GAD, it can also be helpful in other, more complex psychiatric scenarios. Sumiyoshi et al10 observed improvement in scores on the Digit Symbol Substitution Test when buspirone was added to a second-generation antipsychotic (SGA), which suggests buspirone may help improve attention in patients with schizophrenia. It has been postulated that buspirone may also be helpful for cognitive dysfunction in patients with Alzheimer’s disease.11 Buspirone has been used to treat comorbid anxiety and alcohol use disorder, resulting in reduced anxiety, longer latency to relapse, and fewer drinking days during a 12-week treatment program.12 Buspirone has been more effective than placebo for treating post-stroke anxiety.13
Continue to: Patients who receive...
Patients who receive an SSRI, such as citalopram, but are not able to achieve a substantial improvement in their depressive and/or anxious symptoms may benefit from the addition of buspirone to their treatment regimen.14,15
A favorable adverse-effect profile. There are no absolute contraindications to buspirone except a history of hypersensitivity.4 Buspirone generally is well tolerated and carries a low risk of adverse effects. The most common adverse effects are dizziness and nausea.6 Buspirone is not sedating.
Potentially safe for patients who are pregnant. Unlike many other first-line agents for anxiety, such as SSRIs, buspirone has an FDA Category B classification, meaning animal studies have shown no adverse events during pregnancy.4 The FDA Pregnancy and Lactation Labeling Rule applies only to medications that entered the market on or after June 30, 2001; unfortunately, buspirone is excluded from this updated categorization.16 As with any medication being considered for pregnant or lactating women, the prescriber and patient must weigh the benefits vs the risks to determine if buspirone is appropriate for any individual patient.
No adverse events have been reported from abrupt discontinuation of buspirone.17
Inexpensive. Buspirone is generic and extremely inexpensive. According to GoodRx.com, a 30-day supply of 5-mg tablets for twice-daily dosing can cost $4.18 A maximum daily dose (prescribed as 2 pills, 15 mg twice daily) may cost approximately $18/month.18 Thus, buspirone is a good option for uninsured or underinsured patients, for whom this would be more affordable than other anxiolytic medications.
Continue to: May offset certain adverse effects
May offset certain adverse effects. Sexual dysfunction is a common adverse effect of SSRIs. One strategy to offset this phenomenon is to add bupropion. However, in a randomized controlled trial, Landén et al19 found that sexual adverse effects induced by SSRIs were greatly mitigated by adding buspirone, even within the first week of treatment. This improvement was more marked in women than in men, which is helpful because sexual dysfunction in women is generally resistant to other interventions.20 Unlike
Unlikely to cause extrapyramidal symptoms (EPS). Because of its central D2 antagonism, buspirone has a low potential (<1%) to produce EPS. Buspirone has even been shown to reverse
The Table4 highlights key points to bear in mind when prescribing buspirone.
Challenges with buspirone
Response is not immediate. Unlike benzodiazepines, buspirone does not have an immediate onset of action.22 With buspirone monotherapy, response may be seen in approximately 2 to 4 weeks.23 Therefore, patients transitioning from a quick-onset benzodiazepine to buspirone may not report a good response. However, as noted above, when using buspirone to treat SSRI-induced sexual dysfunction, response may emerge within 1 week.19 Buspirone also lacks the euphoric and sedative qualities of benzodiazepines that patients may prefer.
Not for patients with hepatic and renal impairment. Because plasma levels of buspirone are elevated in patients with hepatic and renal impairment, this medication is not ideal for use in these populations.4
Continue to: Contraindicated in patients receiving MAOIs
Contraindicated in patients receiving MAOIs. Buspirone should not be prescribed to patients with depression who are receiving treatment with a monoamine oxidase inhibitor (MAOI) because the combination may precipitate a hypertensive reaction.4 A minimum washout period of 14 days from the MAOI is necessary before initiating buspirone.9
Idiosyncratic adverse effects. As with all pharmaceuticals, buspirone may produce idiosyncratic adverse effects. Faber and Sansone24 reported a case of a woman who experienced hair loss 3 months into treatment with buspirone. After cessation, her alopecia resolved.
Questionable efficacy for some anxiety subtypes. Buspirone has been studied as a treatment of other common psychiatric conditions, such as social phobia and anxiety in the setting of smoking cessation. However, it has not proven to be effective over placebo in treating these anxiety subtypes.25,26
Short half-life. Because of its relatively short half-life (2 to 3 hours), buspirone requires dosing 2 to 3 times a day, which could increase the risk of noncompliance.4 However, some patients might prefer multiple dosing throughout the day due to perceived better coverage of their anxiety symptoms.
Limited incentive for future research. Because buspirone is available only as a generic formulation, there is little financial incentive for pharmaceutical companies and other interested parties to study what may be valuable uses for buspirone. For example, there is no data available on comparative augmentation of buspirone and SGAs with antidepressants for depression and/or anxiety. There is also little data available about buspirone prescribing trends or why buspirone may be underutilized in clinical practice today.
Continue to: Unfortunately, historical and longitudinal...
Unfortunately, historical and longitudinal data on the prescribing practices of buspirone is limited because the original branded medication, BuSpar, is no longer on the market. However, this medication offers multiple advantages over other agents used to treat anxiety, and it should not be forgotten when formulating a treatment regimen for patients with anxiety and/or depression.
Bottom Line
Buspirone is a safe, low-cost, effective treatment option for patients with anxiety and may be helpful as an augmenting agent for depression. Because of its efficacy and high degree of tolerability, it should be prioritized higher in our treatment algorithms and be a part of our routine pharmacologic armamentarium.
Related Resources
- Howland RH. Buspirone: Back to the future. J Psychosoc Nurs Ment Health Serv. 2015;53(11):21-24.
- Strawn JR, Mills JA, Cornwall GJ, et al. Buspirone in children and adolescents with anxiety: a review and Bayesian analysis of abandoned randomized controlled trials. J Child Adolesc Psychopharmacol. 2018;28(1):2-9.
Drug Brand Names
Bupropion • Wellbutrin, Zyban
Buspirone • BuSpar
Citalopram • Celexa
Haloperidol • Haldol
Vilazodone • Viibryd
Vortioxetine • Trintellix
In general, when a medication goes off patent, marketing for it significantly slows down or comes to a halt. Studies have shown that physicians’ prescribing habits are influenced by pharmaceutical representatives and companies.1 This phenomenon may have an unforeseen adverse effect: once an effective and inexpensive medication “goes generic,” its use may fall out of favor. Additionally, physicians may have concerns about prescribing generic medications, such as perceiving them as less effective and conferring more adverse effects compared with brand-name formulations.2 One such generic medication is buspirone, which originally was branded as BuSpar.
Anxiety disorders are the most common psychiatric diagnoses, and at times are the most challenging to treat.3 Anecdotally, we often see benzodiazepines prescribed as first-line monotherapy for acute and chronic anxiety, but because these agents can cause physical dependence and a withdrawal reaction, alternative anxiolytic medications should be strongly considered. Despite its age, buspirone still plays a role in the treatment of anxiety, and its off-label use can also be useful in certain populations and scenarios. In this article, we delve into buspirone’s mechanism of action, discuss its advantages and challenges, and what you need to know when prescribing it.
How buspirone works
Buspirone was originally described as an anxiolytic agent that was pharmacologically unrelated to traditional anxiety-reducing medications (ie, benzodiazepines and barbiturates).4
The antidepressants vortioxetine and vilazodone exhibit dual-action at both serotonin reuptake transporters and 5HT1A receptors; thus, they work like an SSRI and buspirone combined.6 Although some patients may find it more convenient to take a dual-action pill over 2 separate ones, some insurance companies do not cover these newer agents. Additionally, prescribing buspirone separately allows for more precise dosing, which may lower the risk of adverse effects.
Buspirone is a major substrate for cytochrome P450 (CYP) 3A4 and a minor for CYP2D6, so caution must be advised if considering buspirone for a patient receiving any CYP3A4 inducers and/or inhibitors,7 including grapefruit juice.8
Dose adjustments are not necessary for age and sex, which allows for highly consistent dosing.4 However, as with prescribing medications in any geriatric population, lower starting doses and slower titration of buspirone may be necessary to avoid potential adverse effects due to the alterations of pharmacodynamic and pharmacokinetic processes that occur as patients age.9
Advantages of buspirone
Works well as an add-on to other medications. While buspirone in adequate doses may be helpful as monotherapy in GAD, it can also be helpful in other, more complex psychiatric scenarios. Sumiyoshi et al10 observed improvement in scores on the Digit Symbol Substitution Test when buspirone was added to a second-generation antipsychotic (SGA), which suggests buspirone may help improve attention in patients with schizophrenia. It has been postulated that buspirone may also be helpful for cognitive dysfunction in patients with Alzheimer’s disease.11 Buspirone has been used to treat comorbid anxiety and alcohol use disorder, resulting in reduced anxiety, longer latency to relapse, and fewer drinking days during a 12-week treatment program.12 Buspirone has been more effective than placebo for treating post-stroke anxiety.13
Continue to: Patients who receive...
Patients who receive an SSRI, such as citalopram, but are not able to achieve a substantial improvement in their depressive and/or anxious symptoms may benefit from the addition of buspirone to their treatment regimen.14,15
A favorable adverse-effect profile. There are no absolute contraindications to buspirone except a history of hypersensitivity.4 Buspirone generally is well tolerated and carries a low risk of adverse effects. The most common adverse effects are dizziness and nausea.6 Buspirone is not sedating.
Potentially safe for patients who are pregnant. Unlike many other first-line agents for anxiety, such as SSRIs, buspirone has an FDA Category B classification, meaning animal studies have shown no adverse events during pregnancy.4 The FDA Pregnancy and Lactation Labeling Rule applies only to medications that entered the market on or after June 30, 2001; unfortunately, buspirone is excluded from this updated categorization.16 As with any medication being considered for pregnant or lactating women, the prescriber and patient must weigh the benefits vs the risks to determine if buspirone is appropriate for any individual patient.
No adverse events have been reported from abrupt discontinuation of buspirone.17
Inexpensive. Buspirone is generic and extremely inexpensive. According to GoodRx.com, a 30-day supply of 5-mg tablets for twice-daily dosing can cost $4.18 A maximum daily dose (prescribed as 2 pills, 15 mg twice daily) may cost approximately $18/month.18 Thus, buspirone is a good option for uninsured or underinsured patients, for whom this would be more affordable than other anxiolytic medications.
Continue to: May offset certain adverse effects
May offset certain adverse effects. Sexual dysfunction is a common adverse effect of SSRIs. One strategy to offset this phenomenon is to add bupropion. However, in a randomized controlled trial, Landén et al19 found that sexual adverse effects induced by SSRIs were greatly mitigated by adding buspirone, even within the first week of treatment. This improvement was more marked in women than in men, which is helpful because sexual dysfunction in women is generally resistant to other interventions.20 Unlike
Unlikely to cause extrapyramidal symptoms (EPS). Because of its central D2 antagonism, buspirone has a low potential (<1%) to produce EPS. Buspirone has even been shown to reverse
The Table4 highlights key points to bear in mind when prescribing buspirone.
Challenges with buspirone
Response is not immediate. Unlike benzodiazepines, buspirone does not have an immediate onset of action.22 With buspirone monotherapy, response may be seen in approximately 2 to 4 weeks.23 Therefore, patients transitioning from a quick-onset benzodiazepine to buspirone may not report a good response. However, as noted above, when using buspirone to treat SSRI-induced sexual dysfunction, response may emerge within 1 week.19 Buspirone also lacks the euphoric and sedative qualities of benzodiazepines that patients may prefer.
Not for patients with hepatic and renal impairment. Because plasma levels of buspirone are elevated in patients with hepatic and renal impairment, this medication is not ideal for use in these populations.4
Continue to: Contraindicated in patients receiving MAOIs
Contraindicated in patients receiving MAOIs. Buspirone should not be prescribed to patients with depression who are receiving treatment with a monoamine oxidase inhibitor (MAOI) because the combination may precipitate a hypertensive reaction.4 A minimum washout period of 14 days from the MAOI is necessary before initiating buspirone.9
Idiosyncratic adverse effects. As with all pharmaceuticals, buspirone may produce idiosyncratic adverse effects. Faber and Sansone24 reported a case of a woman who experienced hair loss 3 months into treatment with buspirone. After cessation, her alopecia resolved.
Questionable efficacy for some anxiety subtypes. Buspirone has been studied as a treatment of other common psychiatric conditions, such as social phobia and anxiety in the setting of smoking cessation. However, it has not proven to be effective over placebo in treating these anxiety subtypes.25,26
Short half-life. Because of its relatively short half-life (2 to 3 hours), buspirone requires dosing 2 to 3 times a day, which could increase the risk of noncompliance.4 However, some patients might prefer multiple dosing throughout the day due to perceived better coverage of their anxiety symptoms.
Limited incentive for future research. Because buspirone is available only as a generic formulation, there is little financial incentive for pharmaceutical companies and other interested parties to study what may be valuable uses for buspirone. For example, there is no data available on comparative augmentation of buspirone and SGAs with antidepressants for depression and/or anxiety. There is also little data available about buspirone prescribing trends or why buspirone may be underutilized in clinical practice today.
Continue to: Unfortunately, historical and longitudinal...
Unfortunately, historical and longitudinal data on the prescribing practices of buspirone is limited because the original branded medication, BuSpar, is no longer on the market. However, this medication offers multiple advantages over other agents used to treat anxiety, and it should not be forgotten when formulating a treatment regimen for patients with anxiety and/or depression.
Bottom Line
Buspirone is a safe, low-cost, effective treatment option for patients with anxiety and may be helpful as an augmenting agent for depression. Because of its efficacy and high degree of tolerability, it should be prioritized higher in our treatment algorithms and be a part of our routine pharmacologic armamentarium.
Related Resources
- Howland RH. Buspirone: Back to the future. J Psychosoc Nurs Ment Health Serv. 2015;53(11):21-24.
- Strawn JR, Mills JA, Cornwall GJ, et al. Buspirone in children and adolescents with anxiety: a review and Bayesian analysis of abandoned randomized controlled trials. J Child Adolesc Psychopharmacol. 2018;28(1):2-9.
Drug Brand Names
Bupropion • Wellbutrin, Zyban
Buspirone • BuSpar
Citalopram • Celexa
Haloperidol • Haldol
Vilazodone • Viibryd
Vortioxetine • Trintellix
1. Fickweiler F, Fickweiler W, Urbach E. Interactions between physicians and the pharmaceutical industry generally and sales representatives specifically and their association with physicians’ attitudes and prescribing habits: a systematic review. BMJ Open. 2017;7(9):e016408. doi: 10.1136/bmjopen-2017-016408.
2. Haque M. Generic medicine and prescribing: a quick assessment. Adv Hum Biol. 2017;7(3):101-108.
3. National Alliance on Mental Illness. Anxiety disorders. https://www.nami.org/Learn-More/Mental-Health-Conditions/Anxiety-Disorders. Published December 2017. Accessed November 26, 2019.
4. Buspar [package insert]. Princeton, NJ: Bristol-Myers Squibb Company; 2000.
5. Hjorth S, Carlsson A. Buspirone: effects on central monoaminergic transmission-possible relevance to animal experimental and clinical findings. Eur J Pharmacol. 1982:83;299-303.
6. Stahl SM. Stahl’s essential psychopharmacology: neuroscientific basis and practical applications, 4th ed. Cambridge, United Kingdom: Cambridge University Press; 2013.
7. Buspirone tablets [package insert]. East Brunswick, NJ: Strides Pharma Inc; 2017.
8. Lilja JJ, Kivistö KT, Backman, JT, et al. Grapefruit juice substantially increases plasma concentrations of buspirone. Clin Pharmacol Ther. 1998;64:655-660.
9. Stahl SM. Stahl’s essential psychopharmacology: prescriber’s guide, 6th ed. Cambridge, United Kingdom: Cambridge University Press; 2017.
10. Sumiyoshi T, Park S, Jayathilake K. Effect of buspirone, a serotonin1A partial agonist, on cognitive function in schizophrenia: a randomized, double-blind, placebo-controlled study. Schizophr Res. 2007;95(1-3):158-168.
11. Schechter LE, Dawson LA, Harder JA. The potential utility of 5-HT1A receptor antagonists in the treatment of cognitive dysfunction associated with Alzheimer’s disease. Curr Pharm Des. 2002;8(2):139-145.
12. Kranzler HR, Burleson JA, Del Boca FK. Buspirone treatment of anxious alcoholics: a placebo-controlled trial. Arch Gen Psychiatry. 1994;51(9):720-731.
13. Burton CA, Holmes J, Murray J, et al. Interventions for treating anxiety after stroke. Cochrane Database Syst Rev. 2011;12:1-25.
14. Appelberg BG, Syvälahti EK, Koskinen TE, et al. Patients with severe depression may benefit from buspirone augmentation of selective serotonin reuptake inhibitors: results from a placebo-controlled, randomized, double-blind, placebo wash-in study. J Clin Psychiatry. 2001; 62(6):448-452.
15. American Psychiatric Association. Practice guideline for the treatment of patients with major depressive disorder. 3rd edition. https://psychiatryonline.org/pb/assets/raw/sitewide/practice_guidelines/guidelines/mdd.pdf. Published May 2010. Accessed November 2019.
16. U.S. Food and Drug Administration. Pregnancy and lactation labeling (drugs) final rule. https://www.fda.gov/drugs/labeling/pregnancy-and-lactation-labeling-drugs-final-rule. Published September 11, 2019. Accessed November 26, 2019.
17. Goa KL, Ward A. Buspirone. A preliminary review of its pharmacological properties and therapeutic efficacy as an anxiolytic. Drugs. 1986;32(2):114-129.
18. GoodRx. Buspar prices, coupons, & savings tips in U.S. area code 08054. https://www.goodrx.com/buspar. Accessed June 6, 2019.
19. Landén M, Eriksson E, Agren H, et al. Effect of buspirone on sexual dysfunction in depressed patients treated with selective serotonin reuptake inhibitors. J Clin Psychopharmacol. 1999;19(3):268-271.
20. Hensley PL, Nurnberg HG. SSRI sexual dysfunction: a female perspective. J Sex Marital Ther. 2002;28(suppl 1):143-153.
21. Haleem DJ, Samad N, Haleem MA. Reversal of haloperidol-induced extrapyramidal symptoms by buspirone: a time-related study. Behav Pharmacol. 2007;18(2):147-153.
22. Kaplan SS, Saddock BJ, Grebb JA. Synopsis of psychiatry. 11th ed. Philadelphia, PA: Wolters Kluwer; 2014.
23. National Alliance on Mental Health. Buspirone (BuSpar). https://www.nami.org/Learn-More/Treatment/Mental-Health-Medications/Types-of-Medication/Buspirone-(BuSpar). Published January 2019. Accessed November 26, 2019.
24. Faber J, Sansone RA. Buspirone: a possible cause of alopecia. Innov Clin Neurosci. 2013;10(1):13.
25. Van Vliet IM, Den Boer JA, Westenberg HGM, et al. Clinical effects of buspirone in social phobia, a double-blind placebo controlled study. J Clin Psychiatry. 1997;58(4):164-168.
26. Schneider NG, Olmstead RE, Steinberg C, et al. Efficacy of buspirone in smoking cessation: a placebo‐controlled trial. Clin Pharmacol Ther. 1996;60(5):568-575.
1. Fickweiler F, Fickweiler W, Urbach E. Interactions between physicians and the pharmaceutical industry generally and sales representatives specifically and their association with physicians’ attitudes and prescribing habits: a systematic review. BMJ Open. 2017;7(9):e016408. doi: 10.1136/bmjopen-2017-016408.
2. Haque M. Generic medicine and prescribing: a quick assessment. Adv Hum Biol. 2017;7(3):101-108.
3. National Alliance on Mental Illness. Anxiety disorders. https://www.nami.org/Learn-More/Mental-Health-Conditions/Anxiety-Disorders. Published December 2017. Accessed November 26, 2019.
4. Buspar [package insert]. Princeton, NJ: Bristol-Myers Squibb Company; 2000.
5. Hjorth S, Carlsson A. Buspirone: effects on central monoaminergic transmission-possible relevance to animal experimental and clinical findings. Eur J Pharmacol. 1982:83;299-303.
6. Stahl SM. Stahl’s essential psychopharmacology: neuroscientific basis and practical applications, 4th ed. Cambridge, United Kingdom: Cambridge University Press; 2013.
7. Buspirone tablets [package insert]. East Brunswick, NJ: Strides Pharma Inc; 2017.
8. Lilja JJ, Kivistö KT, Backman, JT, et al. Grapefruit juice substantially increases plasma concentrations of buspirone. Clin Pharmacol Ther. 1998;64:655-660.
9. Stahl SM. Stahl’s essential psychopharmacology: prescriber’s guide, 6th ed. Cambridge, United Kingdom: Cambridge University Press; 2017.
10. Sumiyoshi T, Park S, Jayathilake K. Effect of buspirone, a serotonin1A partial agonist, on cognitive function in schizophrenia: a randomized, double-blind, placebo-controlled study. Schizophr Res. 2007;95(1-3):158-168.
11. Schechter LE, Dawson LA, Harder JA. The potential utility of 5-HT1A receptor antagonists in the treatment of cognitive dysfunction associated with Alzheimer’s disease. Curr Pharm Des. 2002;8(2):139-145.
12. Kranzler HR, Burleson JA, Del Boca FK. Buspirone treatment of anxious alcoholics: a placebo-controlled trial. Arch Gen Psychiatry. 1994;51(9):720-731.
13. Burton CA, Holmes J, Murray J, et al. Interventions for treating anxiety after stroke. Cochrane Database Syst Rev. 2011;12:1-25.
14. Appelberg BG, Syvälahti EK, Koskinen TE, et al. Patients with severe depression may benefit from buspirone augmentation of selective serotonin reuptake inhibitors: results from a placebo-controlled, randomized, double-blind, placebo wash-in study. J Clin Psychiatry. 2001; 62(6):448-452.
15. American Psychiatric Association. Practice guideline for the treatment of patients with major depressive disorder. 3rd edition. https://psychiatryonline.org/pb/assets/raw/sitewide/practice_guidelines/guidelines/mdd.pdf. Published May 2010. Accessed November 2019.
16. U.S. Food and Drug Administration. Pregnancy and lactation labeling (drugs) final rule. https://www.fda.gov/drugs/labeling/pregnancy-and-lactation-labeling-drugs-final-rule. Published September 11, 2019. Accessed November 26, 2019.
17. Goa KL, Ward A. Buspirone. A preliminary review of its pharmacological properties and therapeutic efficacy as an anxiolytic. Drugs. 1986;32(2):114-129.
18. GoodRx. Buspar prices, coupons, & savings tips in U.S. area code 08054. https://www.goodrx.com/buspar. Accessed June 6, 2019.
19. Landén M, Eriksson E, Agren H, et al. Effect of buspirone on sexual dysfunction in depressed patients treated with selective serotonin reuptake inhibitors. J Clin Psychopharmacol. 1999;19(3):268-271.
20. Hensley PL, Nurnberg HG. SSRI sexual dysfunction: a female perspective. J Sex Marital Ther. 2002;28(suppl 1):143-153.
21. Haleem DJ, Samad N, Haleem MA. Reversal of haloperidol-induced extrapyramidal symptoms by buspirone: a time-related study. Behav Pharmacol. 2007;18(2):147-153.
22. Kaplan SS, Saddock BJ, Grebb JA. Synopsis of psychiatry. 11th ed. Philadelphia, PA: Wolters Kluwer; 2014.
23. National Alliance on Mental Health. Buspirone (BuSpar). https://www.nami.org/Learn-More/Treatment/Mental-Health-Medications/Types-of-Medication/Buspirone-(BuSpar). Published January 2019. Accessed November 26, 2019.
24. Faber J, Sansone RA. Buspirone: a possible cause of alopecia. Innov Clin Neurosci. 2013;10(1):13.
25. Van Vliet IM, Den Boer JA, Westenberg HGM, et al. Clinical effects of buspirone in social phobia, a double-blind placebo controlled study. J Clin Psychiatry. 1997;58(4):164-168.
26. Schneider NG, Olmstead RE, Steinberg C, et al. Efficacy of buspirone in smoking cessation: a placebo‐controlled trial. Clin Pharmacol Ther. 1996;60(5):568-575.
Top research findings of 2018-2019 for clinical practice
Medical knowledge is growing faster than ever, as is the challenge of keeping up with this ever-growing body of information. Clinicians need a system or method to help them sort and evaluate the quality of new information before they can apply it to clinical care. Without such a system, when facing an overload of information, most of us tend to take the first or the most easily accessed information, without considering the quality of such information. As a result, the use of poor-quality information affects the quality and outcome of care we provide, and costs billions of dollars annually in problems associated with underuse, overuse, and misuse of treatments.
In an effort to sort and evaluate recently published research that is ready for clinical use, the first author (SAS) used the following 3-step methodology:
1. Searched literature for research findings suggesting readiness for clinical utilization published between July 1, 2018 and June 30, 2019.
2. Surveyed members of the American Association of Chairs of Departments of Psychiatry, the American Association of Community Psychiatrists, the American Association of Psychiatric Administrators, the North Carolina Psychiatric Association, the Group for the Advancement of Psychiatry, and many other colleagues by asking them: “Among the articles published from July 1, 2018 to June 30, 2019, which ones in your opinion have (or are likely to have or should have) affected/changed the clinical practice of psychiatry?”
3. Looked for appraisals in post-publication reviews such as NEJM Journal Watch, F1000 Prime, Evidence-Based Mental Health, commentaries in peer-reviewed journals, and other sources (see Related Resources).
We chose 12 articles based on their clinical relevance/applicability. Here in Part 1 we present brief descriptions of the 6 of top 12 papers chosen by this methodology; these studies are summarized in the Table.1-6 The order in which they appear in this article is arbitrary. The remaining 6 studies will be reviewed in Part 2 in the February 2020 issue of
1. Ray WA, Stein CM, Murray KT, et al. Association of antipsychotic treatment with risk of unexpected death among children and youths. JAMA Psychiatry. 2019;76(2):162-171.
Children and young adults are increasingly being prescribed antipsychotic medications. Studies have suggested that when these medications are used in adults and older patients, they are associated with an increased risk of death.7-9 Whether or not these medications are associated with an increased risk of death in children and youth has been unknown. Ray et al1 compared the risk of unexpected death among children and youths who were beginning treatment with an antipsychotic or control medications.
Study design
- This retrospective cohort study evaluated children and young adults age 5 to 24 who were enrolled in Medicaid in Tennessee between 1999 and 2014.
- New antipsychotic use at both a higher dose (>50 mg chlorpromazine equivalents) and a lower dose (≤50 mg chlorpromazine equivalents) was compared with new use of a control medication, including attention-deficit/hyperactivity disorder medications, antidepressants, and mood stabilizers.
- There were 189,361 participants in the control group, 28,377 participants in the lower-dose antipsychotic group, and 30,120 participants in the higher-dose antipsychotic group.
Outcomes
- The primary outcome was death due to injury or suicide or unexpected death occurring during study follow-up.
- The incidence of death in the higher-dose antipsychotic group (146.2 per 100,000 person-years) was significantly higher (P < .001) than the incidence of death in the control medications group (54.5 per 100,000 person years).
- There was no similar significant difference between the lower-dose antipsychotic group and the control medications group.
Continue to: Conclusion
Conclusion
- Higher-dose antipsychotic use is associated with increased rates of unexpected deaths in children and young adults.
- As with all association studies, no direct line connected cause and effect. However, these results reinforce recommendations for careful prescribing and monitoring of antipsychotic regimens for children and youths, and the need for larger antipsychotic safety studies in this population.
- Examining risks associated with specific antipsychotics will require larger datasets, but will be critical for our understanding of the risks and benefits.
2. Daly EJ, Trivedi MH, Janik A, et al. Efficacy of esketamine nasal spray plus oral antidepressant treatment for relapse prevention in patients with treatment-resistant depression: a randomized clinical trial. JAMA Psychiatry. 2019;76(9):893-903.
Controlled studies have shown esketamine has efficacy for treatment-resistant depression (TRD), but these studies have been only short-term, and the long-term effects of esketamine for TRD have not been established. To fill that gap, Daly et al2 assessed the efficacy of esketamine nasal spray plus an oral antidepressant vs a placebo nasal spray plus an oral antidepressant in delaying relapse of depressive symptoms in patients with TRD. All patients were in stable remission after an optimization course of esketamine nasal spray plus an oral antidepressant.
Study design
- Between October 2015 and February 2018, researchers conducted a phase III, multicenter, double-blind, randomized withdrawal study to evaluate the effect of continuation of esketamine on rates of relapse in patients with TRD who had responded to initial treatment with esketamine.
- Initially, 705 adults were enrolled. Of these participants, 455 proceeded to the optimization phase, in which they were treated with esketamine nasal spray plus an oral antidepressant.
- After 16 weeks of optimization treatment, 297 participants achieved remission or stable response and were randomized to a treatment group, which received continued esketamine nasal spray plus an oral antidepressant, or to a control group, which received a placebo nasal spray plus an oral antidepressant.
Outcomes
- Treatment with esketamine nasal spray and an oral antidepressant was associated with decreased rates of relapse compared with treatment with placebo nasal spray and an oral antidepressant. This was the case among patients who had achieved remission as well as those who had achieved stable response.
- Continued treatment with esketamine decreased the risk of relapse by 51%, with 40 participants in the treatment group experiencing relapse compared with 73 participants in the placebo group.
Continue to: Conclusion
Conclusion
- In patients with TRD who responded to initial treatment with esketamine, continuing esketamine plus an oral antidepressant resulted in clinically meaningful superiority in preventing relapse compared with a placebo nasal spray plus an oral antidepressant.
3. Williams NR, Heifets BD, Blasey C, et al. Attenuation of antidepressant effects of ketamine by opioid receptor antagonism. Am J Psychiatry. 2018;175(12):1205-1215.
Many studies have documented the efficacy of ketamine as a rapid-onset antidepressant. Studies investigating the mechanism of this effect have focused on antagonism of N-methyl-
Study design
- This double-blind crossover study evaluated if opioid receptor activation is necessary for ketamine to have an antidepressant effect in patients with TRD.
- Twelve participants completed both sides of the study in a randomized order. Participants received placebo or naltrexone prior to an IV infusion of ketamine.
- Researchers measured patients’ scores on the Hamilton Depression Rating Scale (HAM-D) at baseline and 1 day after infusion. Response was defined as a ≥50% reduction in HAM-D score.
Outcomes
- Reductions in HAM-D scores among participants in the ketamine plus naltrexone group were significantly lower than those of participants in the ketamine plus placebo group.
- Dissociation related to ketamine use did not differ significantly between the naltrexone group and the placebo group.
Continue to: Conclusion
Conclusion
- This small study found a significant decrease in the antidepressant effect of ketamine infusion in patients with TRD when opioid receptors are blocked with naltrexone prior to infusion, which suggests opioid receptor activation is necessary for ketamine to be effective as an antidepressant.
- This appears to be consistent with observations of buprenorphine’s antidepressant effects. Caution is indicated until additional studies can further elucidate the mechanism of action of ketamine’s antidepressant effects (see "Ketamine/esketamine: Putative mechanism of action," page 32).
4. Nidich S, Mills PJ, Rainforth M, et al. Non-trauma-focused meditation versus exposure therapy in veterans with post-traumatic stress disorder: a randomised controlled trial. Lancet Psychiatry. 2018;5(12):975-986.
Posttraumatic stress disorder (PTSD) is a common and important public health problem. Evidence-based treatments for PTSD include trauma-focused therapies such as prolonged exposure therapy (PE). However, some patients may not respond to PE, drop out, or elect not to pursue it. Researchers continue to explore treatments that are non-trauma-focused, such as mindfulness meditation and interpersonal psychotherapy. In a 3-group comparative effectiveness trial, Nidich et al4 examined the efficacy of a non-trauma-focused intervention, transcendental meditation (TM), in reducing PTSD symptom severity and depression in veterans.
Study design
- Researchers recruited 203 veterans with PTSD from the Department of Veterans Affairs (VA) San Diego Healthcare System between June 2013 and October 2016.
- Participants were randomly assigned to 1 of 3 groups: 68 to TM, 68 to PE, and 67 to PTSD health education (HE).
- Each group received 12 sessions over 12 weeks. In addition to group and individual sessions, all participants received daily practice or assignments.
- The Clinician-Administered PTSD Scale (CAPS) was used to assess symptoms before and after treatment.
Outcomes
- The primary outcome assessed was change in PTSD symptom severity at the end of the study compared with baseline as measured by change in CAPS score.
- Transcendental meditation was found to be significantly non-inferior to PE, with a mean change in CAPS score of −16.1 in the TM group and −11.2 in the PE group.
- Both the TM and PE groups also had significant reductions in CAPS scores compared with the HE group, which had a mean change in CAPS score of −2.5.
Continue to: Conclusion
Conclusion
- Transcendental meditation is significantly not inferior to PE in the treatment of veterans with PTSD.
- The findings from this first comparative effectiveness trial comparing TM with an established psychotherapy for PTSD suggests the feasibility and efficacy of TM as an alternative therapy for veterans with PTSD.
- Because TM is self-administered after an initial expert training, it may offer an easy-to-implement approach that may be more accessible to veterans than other treatments.
5. Raskind MA, Peskind ER, Chow B, et al. Trial of prazosin for post-traumatic stress disorder in military veterans. N Engl J Med. 2018;378(6):507-517.
Several smaller randomized trials of prazosin involving a total of 283 active-duty service members, veterans, and civilian participants have shown efficacy of prazosin for PTSD-related nightmares, sleep disturbance, and overall clinical functioning. However, in a recent trial, Raskind et al5 failed to demonstrate such efficacy.
Study design
- Veterans with chronic PTSD nightmares were recruited from 13 VA medical centers to participate in a 26-week, double-blind, randomized controlled trial.
- A total of 304 participants were randomized to a prazosin treatment group (n = 152) or a placebo control group (n = 152).
- During the first 10 weeks, prazosin or placebo were administered in an escalating fashion up to a maximum dose.
- The CAPS, Pittsburgh Sleep Quality Index (PSQI), and Clinical Global Impressions of Change (CGIC) scores were measured at baseline, after 10 weeks, and after 26 weeks.
Outcomes
- Three primary outcomes measures were assessed: change in score from baseline to 10 weeks on CAPS item B2, the PSQI, and the CGIC.
- A secondary measure was change in score from baseline of the same measures at 26 weeks.
- There was no significant difference between the prazosin group and the placebo group in any of the primary or secondary measures.
Continue to: Conclusion
Conclusion
- Compared with placebo, prazosin was not associated with improvement in nightmares or sleep quality for veterans with chronic PTSD nightmares.
- Because psychosocial instability was an exclusion criterion, it is possible that a selection bias resulting from recruitment of patients who were mainly in clinically stable condition accounted for these negative results, since symptoms in such patients were less likely to be ameliorated with antiadrenergic treatment.
Treatment-resistant depression in veterans is a major clinical challenge because of these patients’ increased risk of suicide. Repetitive transcranial magnetic stimulation (rTMS) has shown promising results for TRD. In a randomized trial, Yesavage et al6 compared rTMS vs sham rTMS in veterans with TRD.
Study design
- Veterans with TRD were recruited from 9 VA medical centers throughout the United States between September 2012 and May 2016.
- Researchers randomized 164 participants into 1 of 2 groups in a double-blind fashion. The treatment group (n = 81) received left prefrontal rTMS, and the control group (n = 83) received sham rTMS.
Outcomes
- In an intention-to-treat analysis, remission rate (defined as a HAM-D score of ≤10) was assessed as the primary outcome measure.
- Remission was seen in both groups, with 40.7% of the treatment group achieving remission and 37.4% of the control group achieving remission. However, the difference between the 2 groups was not significant (P = .67), with an odds ratio of 1.16.
Continue to: Conclusion
Conclusion
- In this study, treatment with rTMS did not show a statistically significant difference in rates of remission from TRD in veterans compared with sham rTMS. This differs from previous rTMS trials in non-veteran patients.
- The findings of this study also differed from those of other rTMS research in terms of the high remission rates that were seen in both the active and sham groups.
Bottom Line
The risk of death might be increased in children and young adults who receive highdose antipsychotics. Continued treatment with intranasal esketamine may help prevent relapse in patients with treatment-resistant depression (TRD) who initially respond to esketamine. The antidepressant effects of ketamine might be associated with opioid receptor activation. Transcendental meditation may be helpful for patients with posttraumatic stress disorder (PTSD), while prazosin might not improve nightmares or sleep quality in patients with PTSD. Repetitive transcranial magnetic stimulation (rTMS) might not be any more effective than sham rTMS for veterans with TRD.
Related Resources
- NEJM Journal Watch. www.jwatch.org.
- F1000 Prime. https://f1000.com/prime/home.
- BMJ Journals Evidence-Based Mental Health. https://ebmh.bmj.com.
Drug Brand Names
Buprenorphine • Subutex
Chlorpromazine • Thorazine
Esketamine nasal spray • Spravato
Ketamine • Ketalar
Naltrexone • Narcan
Prazosin • Minipress
1. Ray WA, Stein CM, Murray KT, et al. Association of antipsychotic treatment with risk of unexpected death among children and youths. JAMA Psychiatry. 2019;76(2):162-171.
2. Daly EJ, Trivedi MH, Janik A, et al. Efficacy of esketamine nasal spray plus oral antidepressant treatment for relapse prevention in patients with treatment-resistant depression: a randomized clinical trial. JAMA Psychiatry. 2019;76(9):893-903.
3. Williams NR, Heifets BD, Blasey C, et al. Attenuation of antidepressant effects of ketamine by opioid receptor antagonism. Am J Psychiatry. 2018;175(12):1205-1215.
4. Nidich S, Mills PJ, Rainforth M, et al. Non-trauma-focused meditation versus exposure therapy in veterans with post-traumatic stress disorder: a randomized controlled trial. Lancet Psychiatry. 2018;5(12):975-986.
5. Raskind MA, Peskind ER, Chow B, et al. Trial of prazosin for post-traumatic stress disorder in military veterans. N Engl J Med. 2018;378(6):507-517.
6. Yesavage JA, Fairchild JK, Mi Z, et al. Effect of repetitive transcranial magnetic stimulation on treatment-resistant major depression in US veterans: a randomized clinical trial. JAMA Psychiatry. 2018;75(9):884-893.
7. Ray WA, Meredith S, Thapa PB, et al. Antipsychotics and the risk of sudden cardiac death. Arch Gen Psychiatry. 2001;58(12):1161-1167.
8. Ray WA, Chung CP, Murray KT, Hall K, Stein CM. Atypical antipsychotic drugs and the risk of sudden cardiac death. N Engl J Med. 2009;360(3):225-235.
9. Jeste DV, Blazer D, Casey D, et al. ACNP White Paper: update on use of antipsychotic drugs in elderly persons with dementia. Neuropsychopharmacology. 2008;33(5):957-970.
Medical knowledge is growing faster than ever, as is the challenge of keeping up with this ever-growing body of information. Clinicians need a system or method to help them sort and evaluate the quality of new information before they can apply it to clinical care. Without such a system, when facing an overload of information, most of us tend to take the first or the most easily accessed information, without considering the quality of such information. As a result, the use of poor-quality information affects the quality and outcome of care we provide, and costs billions of dollars annually in problems associated with underuse, overuse, and misuse of treatments.
In an effort to sort and evaluate recently published research that is ready for clinical use, the first author (SAS) used the following 3-step methodology:
1. Searched literature for research findings suggesting readiness for clinical utilization published between July 1, 2018 and June 30, 2019.
2. Surveyed members of the American Association of Chairs of Departments of Psychiatry, the American Association of Community Psychiatrists, the American Association of Psychiatric Administrators, the North Carolina Psychiatric Association, the Group for the Advancement of Psychiatry, and many other colleagues by asking them: “Among the articles published from July 1, 2018 to June 30, 2019, which ones in your opinion have (or are likely to have or should have) affected/changed the clinical practice of psychiatry?”
3. Looked for appraisals in post-publication reviews such as NEJM Journal Watch, F1000 Prime, Evidence-Based Mental Health, commentaries in peer-reviewed journals, and other sources (see Related Resources).
We chose 12 articles based on their clinical relevance/applicability. Here in Part 1 we present brief descriptions of the 6 of top 12 papers chosen by this methodology; these studies are summarized in the Table.1-6 The order in which they appear in this article is arbitrary. The remaining 6 studies will be reviewed in Part 2 in the February 2020 issue of
1. Ray WA, Stein CM, Murray KT, et al. Association of antipsychotic treatment with risk of unexpected death among children and youths. JAMA Psychiatry. 2019;76(2):162-171.
Children and young adults are increasingly being prescribed antipsychotic medications. Studies have suggested that when these medications are used in adults and older patients, they are associated with an increased risk of death.7-9 Whether or not these medications are associated with an increased risk of death in children and youth has been unknown. Ray et al1 compared the risk of unexpected death among children and youths who were beginning treatment with an antipsychotic or control medications.
Study design
- This retrospective cohort study evaluated children and young adults age 5 to 24 who were enrolled in Medicaid in Tennessee between 1999 and 2014.
- New antipsychotic use at both a higher dose (>50 mg chlorpromazine equivalents) and a lower dose (≤50 mg chlorpromazine equivalents) was compared with new use of a control medication, including attention-deficit/hyperactivity disorder medications, antidepressants, and mood stabilizers.
- There were 189,361 participants in the control group, 28,377 participants in the lower-dose antipsychotic group, and 30,120 participants in the higher-dose antipsychotic group.
Outcomes
- The primary outcome was death due to injury or suicide or unexpected death occurring during study follow-up.
- The incidence of death in the higher-dose antipsychotic group (146.2 per 100,000 person-years) was significantly higher (P < .001) than the incidence of death in the control medications group (54.5 per 100,000 person years).
- There was no similar significant difference between the lower-dose antipsychotic group and the control medications group.
Continue to: Conclusion
Conclusion
- Higher-dose antipsychotic use is associated with increased rates of unexpected deaths in children and young adults.
- As with all association studies, no direct line connected cause and effect. However, these results reinforce recommendations for careful prescribing and monitoring of antipsychotic regimens for children and youths, and the need for larger antipsychotic safety studies in this population.
- Examining risks associated with specific antipsychotics will require larger datasets, but will be critical for our understanding of the risks and benefits.
2. Daly EJ, Trivedi MH, Janik A, et al. Efficacy of esketamine nasal spray plus oral antidepressant treatment for relapse prevention in patients with treatment-resistant depression: a randomized clinical trial. JAMA Psychiatry. 2019;76(9):893-903.
Controlled studies have shown esketamine has efficacy for treatment-resistant depression (TRD), but these studies have been only short-term, and the long-term effects of esketamine for TRD have not been established. To fill that gap, Daly et al2 assessed the efficacy of esketamine nasal spray plus an oral antidepressant vs a placebo nasal spray plus an oral antidepressant in delaying relapse of depressive symptoms in patients with TRD. All patients were in stable remission after an optimization course of esketamine nasal spray plus an oral antidepressant.
Study design
- Between October 2015 and February 2018, researchers conducted a phase III, multicenter, double-blind, randomized withdrawal study to evaluate the effect of continuation of esketamine on rates of relapse in patients with TRD who had responded to initial treatment with esketamine.
- Initially, 705 adults were enrolled. Of these participants, 455 proceeded to the optimization phase, in which they were treated with esketamine nasal spray plus an oral antidepressant.
- After 16 weeks of optimization treatment, 297 participants achieved remission or stable response and were randomized to a treatment group, which received continued esketamine nasal spray plus an oral antidepressant, or to a control group, which received a placebo nasal spray plus an oral antidepressant.
Outcomes
- Treatment with esketamine nasal spray and an oral antidepressant was associated with decreased rates of relapse compared with treatment with placebo nasal spray and an oral antidepressant. This was the case among patients who had achieved remission as well as those who had achieved stable response.
- Continued treatment with esketamine decreased the risk of relapse by 51%, with 40 participants in the treatment group experiencing relapse compared with 73 participants in the placebo group.
Continue to: Conclusion
Conclusion
- In patients with TRD who responded to initial treatment with esketamine, continuing esketamine plus an oral antidepressant resulted in clinically meaningful superiority in preventing relapse compared with a placebo nasal spray plus an oral antidepressant.
3. Williams NR, Heifets BD, Blasey C, et al. Attenuation of antidepressant effects of ketamine by opioid receptor antagonism. Am J Psychiatry. 2018;175(12):1205-1215.
Many studies have documented the efficacy of ketamine as a rapid-onset antidepressant. Studies investigating the mechanism of this effect have focused on antagonism of N-methyl-
Study design
- This double-blind crossover study evaluated if opioid receptor activation is necessary for ketamine to have an antidepressant effect in patients with TRD.
- Twelve participants completed both sides of the study in a randomized order. Participants received placebo or naltrexone prior to an IV infusion of ketamine.
- Researchers measured patients’ scores on the Hamilton Depression Rating Scale (HAM-D) at baseline and 1 day after infusion. Response was defined as a ≥50% reduction in HAM-D score.
Outcomes
- Reductions in HAM-D scores among participants in the ketamine plus naltrexone group were significantly lower than those of participants in the ketamine plus placebo group.
- Dissociation related to ketamine use did not differ significantly between the naltrexone group and the placebo group.
Continue to: Conclusion
Conclusion
- This small study found a significant decrease in the antidepressant effect of ketamine infusion in patients with TRD when opioid receptors are blocked with naltrexone prior to infusion, which suggests opioid receptor activation is necessary for ketamine to be effective as an antidepressant.
- This appears to be consistent with observations of buprenorphine’s antidepressant effects. Caution is indicated until additional studies can further elucidate the mechanism of action of ketamine’s antidepressant effects (see "Ketamine/esketamine: Putative mechanism of action," page 32).
4. Nidich S, Mills PJ, Rainforth M, et al. Non-trauma-focused meditation versus exposure therapy in veterans with post-traumatic stress disorder: a randomised controlled trial. Lancet Psychiatry. 2018;5(12):975-986.
Posttraumatic stress disorder (PTSD) is a common and important public health problem. Evidence-based treatments for PTSD include trauma-focused therapies such as prolonged exposure therapy (PE). However, some patients may not respond to PE, drop out, or elect not to pursue it. Researchers continue to explore treatments that are non-trauma-focused, such as mindfulness meditation and interpersonal psychotherapy. In a 3-group comparative effectiveness trial, Nidich et al4 examined the efficacy of a non-trauma-focused intervention, transcendental meditation (TM), in reducing PTSD symptom severity and depression in veterans.
Study design
- Researchers recruited 203 veterans with PTSD from the Department of Veterans Affairs (VA) San Diego Healthcare System between June 2013 and October 2016.
- Participants were randomly assigned to 1 of 3 groups: 68 to TM, 68 to PE, and 67 to PTSD health education (HE).
- Each group received 12 sessions over 12 weeks. In addition to group and individual sessions, all participants received daily practice or assignments.
- The Clinician-Administered PTSD Scale (CAPS) was used to assess symptoms before and after treatment.
Outcomes
- The primary outcome assessed was change in PTSD symptom severity at the end of the study compared with baseline as measured by change in CAPS score.
- Transcendental meditation was found to be significantly non-inferior to PE, with a mean change in CAPS score of −16.1 in the TM group and −11.2 in the PE group.
- Both the TM and PE groups also had significant reductions in CAPS scores compared with the HE group, which had a mean change in CAPS score of −2.5.
Continue to: Conclusion
Conclusion
- Transcendental meditation is significantly not inferior to PE in the treatment of veterans with PTSD.
- The findings from this first comparative effectiveness trial comparing TM with an established psychotherapy for PTSD suggests the feasibility and efficacy of TM as an alternative therapy for veterans with PTSD.
- Because TM is self-administered after an initial expert training, it may offer an easy-to-implement approach that may be more accessible to veterans than other treatments.
5. Raskind MA, Peskind ER, Chow B, et al. Trial of prazosin for post-traumatic stress disorder in military veterans. N Engl J Med. 2018;378(6):507-517.
Several smaller randomized trials of prazosin involving a total of 283 active-duty service members, veterans, and civilian participants have shown efficacy of prazosin for PTSD-related nightmares, sleep disturbance, and overall clinical functioning. However, in a recent trial, Raskind et al5 failed to demonstrate such efficacy.
Study design
- Veterans with chronic PTSD nightmares were recruited from 13 VA medical centers to participate in a 26-week, double-blind, randomized controlled trial.
- A total of 304 participants were randomized to a prazosin treatment group (n = 152) or a placebo control group (n = 152).
- During the first 10 weeks, prazosin or placebo were administered in an escalating fashion up to a maximum dose.
- The CAPS, Pittsburgh Sleep Quality Index (PSQI), and Clinical Global Impressions of Change (CGIC) scores were measured at baseline, after 10 weeks, and after 26 weeks.
Outcomes
- Three primary outcomes measures were assessed: change in score from baseline to 10 weeks on CAPS item B2, the PSQI, and the CGIC.
- A secondary measure was change in score from baseline of the same measures at 26 weeks.
- There was no significant difference between the prazosin group and the placebo group in any of the primary or secondary measures.
Continue to: Conclusion
Conclusion
- Compared with placebo, prazosin was not associated with improvement in nightmares or sleep quality for veterans with chronic PTSD nightmares.
- Because psychosocial instability was an exclusion criterion, it is possible that a selection bias resulting from recruitment of patients who were mainly in clinically stable condition accounted for these negative results, since symptoms in such patients were less likely to be ameliorated with antiadrenergic treatment.
Treatment-resistant depression in veterans is a major clinical challenge because of these patients’ increased risk of suicide. Repetitive transcranial magnetic stimulation (rTMS) has shown promising results for TRD. In a randomized trial, Yesavage et al6 compared rTMS vs sham rTMS in veterans with TRD.
Study design
- Veterans with TRD were recruited from 9 VA medical centers throughout the United States between September 2012 and May 2016.
- Researchers randomized 164 participants into 1 of 2 groups in a double-blind fashion. The treatment group (n = 81) received left prefrontal rTMS, and the control group (n = 83) received sham rTMS.
Outcomes
- In an intention-to-treat analysis, remission rate (defined as a HAM-D score of ≤10) was assessed as the primary outcome measure.
- Remission was seen in both groups, with 40.7% of the treatment group achieving remission and 37.4% of the control group achieving remission. However, the difference between the 2 groups was not significant (P = .67), with an odds ratio of 1.16.
Continue to: Conclusion
Conclusion
- In this study, treatment with rTMS did not show a statistically significant difference in rates of remission from TRD in veterans compared with sham rTMS. This differs from previous rTMS trials in non-veteran patients.
- The findings of this study also differed from those of other rTMS research in terms of the high remission rates that were seen in both the active and sham groups.
Bottom Line
The risk of death might be increased in children and young adults who receive highdose antipsychotics. Continued treatment with intranasal esketamine may help prevent relapse in patients with treatment-resistant depression (TRD) who initially respond to esketamine. The antidepressant effects of ketamine might be associated with opioid receptor activation. Transcendental meditation may be helpful for patients with posttraumatic stress disorder (PTSD), while prazosin might not improve nightmares or sleep quality in patients with PTSD. Repetitive transcranial magnetic stimulation (rTMS) might not be any more effective than sham rTMS for veterans with TRD.
Related Resources
- NEJM Journal Watch. www.jwatch.org.
- F1000 Prime. https://f1000.com/prime/home.
- BMJ Journals Evidence-Based Mental Health. https://ebmh.bmj.com.
Drug Brand Names
Buprenorphine • Subutex
Chlorpromazine • Thorazine
Esketamine nasal spray • Spravato
Ketamine • Ketalar
Naltrexone • Narcan
Prazosin • Minipress
Medical knowledge is growing faster than ever, as is the challenge of keeping up with this ever-growing body of information. Clinicians need a system or method to help them sort and evaluate the quality of new information before they can apply it to clinical care. Without such a system, when facing an overload of information, most of us tend to take the first or the most easily accessed information, without considering the quality of such information. As a result, the use of poor-quality information affects the quality and outcome of care we provide, and costs billions of dollars annually in problems associated with underuse, overuse, and misuse of treatments.
In an effort to sort and evaluate recently published research that is ready for clinical use, the first author (SAS) used the following 3-step methodology:
1. Searched literature for research findings suggesting readiness for clinical utilization published between July 1, 2018 and June 30, 2019.
2. Surveyed members of the American Association of Chairs of Departments of Psychiatry, the American Association of Community Psychiatrists, the American Association of Psychiatric Administrators, the North Carolina Psychiatric Association, the Group for the Advancement of Psychiatry, and many other colleagues by asking them: “Among the articles published from July 1, 2018 to June 30, 2019, which ones in your opinion have (or are likely to have or should have) affected/changed the clinical practice of psychiatry?”
3. Looked for appraisals in post-publication reviews such as NEJM Journal Watch, F1000 Prime, Evidence-Based Mental Health, commentaries in peer-reviewed journals, and other sources (see Related Resources).
We chose 12 articles based on their clinical relevance/applicability. Here in Part 1 we present brief descriptions of the 6 of top 12 papers chosen by this methodology; these studies are summarized in the Table.1-6 The order in which they appear in this article is arbitrary. The remaining 6 studies will be reviewed in Part 2 in the February 2020 issue of
1. Ray WA, Stein CM, Murray KT, et al. Association of antipsychotic treatment with risk of unexpected death among children and youths. JAMA Psychiatry. 2019;76(2):162-171.
Children and young adults are increasingly being prescribed antipsychotic medications. Studies have suggested that when these medications are used in adults and older patients, they are associated with an increased risk of death.7-9 Whether or not these medications are associated with an increased risk of death in children and youth has been unknown. Ray et al1 compared the risk of unexpected death among children and youths who were beginning treatment with an antipsychotic or control medications.
Study design
- This retrospective cohort study evaluated children and young adults age 5 to 24 who were enrolled in Medicaid in Tennessee between 1999 and 2014.
- New antipsychotic use at both a higher dose (>50 mg chlorpromazine equivalents) and a lower dose (≤50 mg chlorpromazine equivalents) was compared with new use of a control medication, including attention-deficit/hyperactivity disorder medications, antidepressants, and mood stabilizers.
- There were 189,361 participants in the control group, 28,377 participants in the lower-dose antipsychotic group, and 30,120 participants in the higher-dose antipsychotic group.
Outcomes
- The primary outcome was death due to injury or suicide or unexpected death occurring during study follow-up.
- The incidence of death in the higher-dose antipsychotic group (146.2 per 100,000 person-years) was significantly higher (P < .001) than the incidence of death in the control medications group (54.5 per 100,000 person years).
- There was no similar significant difference between the lower-dose antipsychotic group and the control medications group.
Continue to: Conclusion
Conclusion
- Higher-dose antipsychotic use is associated with increased rates of unexpected deaths in children and young adults.
- As with all association studies, no direct line connected cause and effect. However, these results reinforce recommendations for careful prescribing and monitoring of antipsychotic regimens for children and youths, and the need for larger antipsychotic safety studies in this population.
- Examining risks associated with specific antipsychotics will require larger datasets, but will be critical for our understanding of the risks and benefits.
2. Daly EJ, Trivedi MH, Janik A, et al. Efficacy of esketamine nasal spray plus oral antidepressant treatment for relapse prevention in patients with treatment-resistant depression: a randomized clinical trial. JAMA Psychiatry. 2019;76(9):893-903.
Controlled studies have shown esketamine has efficacy for treatment-resistant depression (TRD), but these studies have been only short-term, and the long-term effects of esketamine for TRD have not been established. To fill that gap, Daly et al2 assessed the efficacy of esketamine nasal spray plus an oral antidepressant vs a placebo nasal spray plus an oral antidepressant in delaying relapse of depressive symptoms in patients with TRD. All patients were in stable remission after an optimization course of esketamine nasal spray plus an oral antidepressant.
Study design
- Between October 2015 and February 2018, researchers conducted a phase III, multicenter, double-blind, randomized withdrawal study to evaluate the effect of continuation of esketamine on rates of relapse in patients with TRD who had responded to initial treatment with esketamine.
- Initially, 705 adults were enrolled. Of these participants, 455 proceeded to the optimization phase, in which they were treated with esketamine nasal spray plus an oral antidepressant.
- After 16 weeks of optimization treatment, 297 participants achieved remission or stable response and were randomized to a treatment group, which received continued esketamine nasal spray plus an oral antidepressant, or to a control group, which received a placebo nasal spray plus an oral antidepressant.
Outcomes
- Treatment with esketamine nasal spray and an oral antidepressant was associated with decreased rates of relapse compared with treatment with placebo nasal spray and an oral antidepressant. This was the case among patients who had achieved remission as well as those who had achieved stable response.
- Continued treatment with esketamine decreased the risk of relapse by 51%, with 40 participants in the treatment group experiencing relapse compared with 73 participants in the placebo group.
Continue to: Conclusion
Conclusion
- In patients with TRD who responded to initial treatment with esketamine, continuing esketamine plus an oral antidepressant resulted in clinically meaningful superiority in preventing relapse compared with a placebo nasal spray plus an oral antidepressant.
3. Williams NR, Heifets BD, Blasey C, et al. Attenuation of antidepressant effects of ketamine by opioid receptor antagonism. Am J Psychiatry. 2018;175(12):1205-1215.
Many studies have documented the efficacy of ketamine as a rapid-onset antidepressant. Studies investigating the mechanism of this effect have focused on antagonism of N-methyl-
Study design
- This double-blind crossover study evaluated if opioid receptor activation is necessary for ketamine to have an antidepressant effect in patients with TRD.
- Twelve participants completed both sides of the study in a randomized order. Participants received placebo or naltrexone prior to an IV infusion of ketamine.
- Researchers measured patients’ scores on the Hamilton Depression Rating Scale (HAM-D) at baseline and 1 day after infusion. Response was defined as a ≥50% reduction in HAM-D score.
Outcomes
- Reductions in HAM-D scores among participants in the ketamine plus naltrexone group were significantly lower than those of participants in the ketamine plus placebo group.
- Dissociation related to ketamine use did not differ significantly between the naltrexone group and the placebo group.
Continue to: Conclusion
Conclusion
- This small study found a significant decrease in the antidepressant effect of ketamine infusion in patients with TRD when opioid receptors are blocked with naltrexone prior to infusion, which suggests opioid receptor activation is necessary for ketamine to be effective as an antidepressant.
- This appears to be consistent with observations of buprenorphine’s antidepressant effects. Caution is indicated until additional studies can further elucidate the mechanism of action of ketamine’s antidepressant effects (see "Ketamine/esketamine: Putative mechanism of action," page 32).
4. Nidich S, Mills PJ, Rainforth M, et al. Non-trauma-focused meditation versus exposure therapy in veterans with post-traumatic stress disorder: a randomised controlled trial. Lancet Psychiatry. 2018;5(12):975-986.
Posttraumatic stress disorder (PTSD) is a common and important public health problem. Evidence-based treatments for PTSD include trauma-focused therapies such as prolonged exposure therapy (PE). However, some patients may not respond to PE, drop out, or elect not to pursue it. Researchers continue to explore treatments that are non-trauma-focused, such as mindfulness meditation and interpersonal psychotherapy. In a 3-group comparative effectiveness trial, Nidich et al4 examined the efficacy of a non-trauma-focused intervention, transcendental meditation (TM), in reducing PTSD symptom severity and depression in veterans.
Study design
- Researchers recruited 203 veterans with PTSD from the Department of Veterans Affairs (VA) San Diego Healthcare System between June 2013 and October 2016.
- Participants were randomly assigned to 1 of 3 groups: 68 to TM, 68 to PE, and 67 to PTSD health education (HE).
- Each group received 12 sessions over 12 weeks. In addition to group and individual sessions, all participants received daily practice or assignments.
- The Clinician-Administered PTSD Scale (CAPS) was used to assess symptoms before and after treatment.
Outcomes
- The primary outcome assessed was change in PTSD symptom severity at the end of the study compared with baseline as measured by change in CAPS score.
- Transcendental meditation was found to be significantly non-inferior to PE, with a mean change in CAPS score of −16.1 in the TM group and −11.2 in the PE group.
- Both the TM and PE groups also had significant reductions in CAPS scores compared with the HE group, which had a mean change in CAPS score of −2.5.
Continue to: Conclusion
Conclusion
- Transcendental meditation is significantly not inferior to PE in the treatment of veterans with PTSD.
- The findings from this first comparative effectiveness trial comparing TM with an established psychotherapy for PTSD suggests the feasibility and efficacy of TM as an alternative therapy for veterans with PTSD.
- Because TM is self-administered after an initial expert training, it may offer an easy-to-implement approach that may be more accessible to veterans than other treatments.
5. Raskind MA, Peskind ER, Chow B, et al. Trial of prazosin for post-traumatic stress disorder in military veterans. N Engl J Med. 2018;378(6):507-517.
Several smaller randomized trials of prazosin involving a total of 283 active-duty service members, veterans, and civilian participants have shown efficacy of prazosin for PTSD-related nightmares, sleep disturbance, and overall clinical functioning. However, in a recent trial, Raskind et al5 failed to demonstrate such efficacy.
Study design
- Veterans with chronic PTSD nightmares were recruited from 13 VA medical centers to participate in a 26-week, double-blind, randomized controlled trial.
- A total of 304 participants were randomized to a prazosin treatment group (n = 152) or a placebo control group (n = 152).
- During the first 10 weeks, prazosin or placebo were administered in an escalating fashion up to a maximum dose.
- The CAPS, Pittsburgh Sleep Quality Index (PSQI), and Clinical Global Impressions of Change (CGIC) scores were measured at baseline, after 10 weeks, and after 26 weeks.
Outcomes
- Three primary outcomes measures were assessed: change in score from baseline to 10 weeks on CAPS item B2, the PSQI, and the CGIC.
- A secondary measure was change in score from baseline of the same measures at 26 weeks.
- There was no significant difference between the prazosin group and the placebo group in any of the primary or secondary measures.
Continue to: Conclusion
Conclusion
- Compared with placebo, prazosin was not associated with improvement in nightmares or sleep quality for veterans with chronic PTSD nightmares.
- Because psychosocial instability was an exclusion criterion, it is possible that a selection bias resulting from recruitment of patients who were mainly in clinically stable condition accounted for these negative results, since symptoms in such patients were less likely to be ameliorated with antiadrenergic treatment.
Treatment-resistant depression in veterans is a major clinical challenge because of these patients’ increased risk of suicide. Repetitive transcranial magnetic stimulation (rTMS) has shown promising results for TRD. In a randomized trial, Yesavage et al6 compared rTMS vs sham rTMS in veterans with TRD.
Study design
- Veterans with TRD were recruited from 9 VA medical centers throughout the United States between September 2012 and May 2016.
- Researchers randomized 164 participants into 1 of 2 groups in a double-blind fashion. The treatment group (n = 81) received left prefrontal rTMS, and the control group (n = 83) received sham rTMS.
Outcomes
- In an intention-to-treat analysis, remission rate (defined as a HAM-D score of ≤10) was assessed as the primary outcome measure.
- Remission was seen in both groups, with 40.7% of the treatment group achieving remission and 37.4% of the control group achieving remission. However, the difference between the 2 groups was not significant (P = .67), with an odds ratio of 1.16.
Continue to: Conclusion
Conclusion
- In this study, treatment with rTMS did not show a statistically significant difference in rates of remission from TRD in veterans compared with sham rTMS. This differs from previous rTMS trials in non-veteran patients.
- The findings of this study also differed from those of other rTMS research in terms of the high remission rates that were seen in both the active and sham groups.
Bottom Line
The risk of death might be increased in children and young adults who receive highdose antipsychotics. Continued treatment with intranasal esketamine may help prevent relapse in patients with treatment-resistant depression (TRD) who initially respond to esketamine. The antidepressant effects of ketamine might be associated with opioid receptor activation. Transcendental meditation may be helpful for patients with posttraumatic stress disorder (PTSD), while prazosin might not improve nightmares or sleep quality in patients with PTSD. Repetitive transcranial magnetic stimulation (rTMS) might not be any more effective than sham rTMS for veterans with TRD.
Related Resources
- NEJM Journal Watch. www.jwatch.org.
- F1000 Prime. https://f1000.com/prime/home.
- BMJ Journals Evidence-Based Mental Health. https://ebmh.bmj.com.
Drug Brand Names
Buprenorphine • Subutex
Chlorpromazine • Thorazine
Esketamine nasal spray • Spravato
Ketamine • Ketalar
Naltrexone • Narcan
Prazosin • Minipress
1. Ray WA, Stein CM, Murray KT, et al. Association of antipsychotic treatment with risk of unexpected death among children and youths. JAMA Psychiatry. 2019;76(2):162-171.
2. Daly EJ, Trivedi MH, Janik A, et al. Efficacy of esketamine nasal spray plus oral antidepressant treatment for relapse prevention in patients with treatment-resistant depression: a randomized clinical trial. JAMA Psychiatry. 2019;76(9):893-903.
3. Williams NR, Heifets BD, Blasey C, et al. Attenuation of antidepressant effects of ketamine by opioid receptor antagonism. Am J Psychiatry. 2018;175(12):1205-1215.
4. Nidich S, Mills PJ, Rainforth M, et al. Non-trauma-focused meditation versus exposure therapy in veterans with post-traumatic stress disorder: a randomized controlled trial. Lancet Psychiatry. 2018;5(12):975-986.
5. Raskind MA, Peskind ER, Chow B, et al. Trial of prazosin for post-traumatic stress disorder in military veterans. N Engl J Med. 2018;378(6):507-517.
6. Yesavage JA, Fairchild JK, Mi Z, et al. Effect of repetitive transcranial magnetic stimulation on treatment-resistant major depression in US veterans: a randomized clinical trial. JAMA Psychiatry. 2018;75(9):884-893.
7. Ray WA, Meredith S, Thapa PB, et al. Antipsychotics and the risk of sudden cardiac death. Arch Gen Psychiatry. 2001;58(12):1161-1167.
8. Ray WA, Chung CP, Murray KT, Hall K, Stein CM. Atypical antipsychotic drugs and the risk of sudden cardiac death. N Engl J Med. 2009;360(3):225-235.
9. Jeste DV, Blazer D, Casey D, et al. ACNP White Paper: update on use of antipsychotic drugs in elderly persons with dementia. Neuropsychopharmacology. 2008;33(5):957-970.
1. Ray WA, Stein CM, Murray KT, et al. Association of antipsychotic treatment with risk of unexpected death among children and youths. JAMA Psychiatry. 2019;76(2):162-171.
2. Daly EJ, Trivedi MH, Janik A, et al. Efficacy of esketamine nasal spray plus oral antidepressant treatment for relapse prevention in patients with treatment-resistant depression: a randomized clinical trial. JAMA Psychiatry. 2019;76(9):893-903.
3. Williams NR, Heifets BD, Blasey C, et al. Attenuation of antidepressant effects of ketamine by opioid receptor antagonism. Am J Psychiatry. 2018;175(12):1205-1215.
4. Nidich S, Mills PJ, Rainforth M, et al. Non-trauma-focused meditation versus exposure therapy in veterans with post-traumatic stress disorder: a randomized controlled trial. Lancet Psychiatry. 2018;5(12):975-986.
5. Raskind MA, Peskind ER, Chow B, et al. Trial of prazosin for post-traumatic stress disorder in military veterans. N Engl J Med. 2018;378(6):507-517.
6. Yesavage JA, Fairchild JK, Mi Z, et al. Effect of repetitive transcranial magnetic stimulation on treatment-resistant major depression in US veterans: a randomized clinical trial. JAMA Psychiatry. 2018;75(9):884-893.
7. Ray WA, Meredith S, Thapa PB, et al. Antipsychotics and the risk of sudden cardiac death. Arch Gen Psychiatry. 2001;58(12):1161-1167.
8. Ray WA, Chung CP, Murray KT, Hall K, Stein CM. Atypical antipsychotic drugs and the risk of sudden cardiac death. N Engl J Med. 2009;360(3):225-235.
9. Jeste DV, Blazer D, Casey D, et al. ACNP White Paper: update on use of antipsychotic drugs in elderly persons with dementia. Neuropsychopharmacology. 2008;33(5):957-970.
Hematology News welcomes Dr. Ify Osunkwo as editor in chief
Hematology News welcomes Ifeyinwa (Ify) Osunkwo, MD, MPH, as the new editor in chief.
Dr. Osunkwo is a professor of medicine at Atrium Health and the director of the Sickle Cell Enterprise at the Levine Cancer Institute, part of Atrium Health, in Charlotte, N.C.
She has made it her personal mission to improve the quality of life for patients with sickle cell disease, a passion that began during time spent in Nigeria as a child, where 150,000 children are born each year with the condition. In 2014, Dr. Osunkwo created a comprehensive sickle cell center in Charlotte with a multidisciplinary team of providers that includes physicians, nurses, social workers, psychologists, and nurse managers. She has also been an instrumental part of the Carolinas Sickle Cell Collaborative, which seeks to match sickle cell patients in the community with blood donors who have similar blood characteristics.
“As a practicing hematologist and researcher, I have a deep appreciation for the timely and relevant content provided by Hematology News,” Dr. Osunkwo said. “I hope to use my experience to help make this publication even better.”
She is a member of the National Adult Sickle Cell Provider Network and leads the Transition/Medical Home Committee for the Southeast Regional Genetics Network. Her interests include health literacy, adolescent transition of care, and chronic pain management.
Dr. Osunkwo graduated from medical school at the University of Nigeria, Enugu, performed her residency at the New Jersey Medical School, Newark, and completed her fellowship training at Columbia University, New York.
Dr. Osunkwo takes the reigns at Hematology News from Matt Kalaycio, MD, of the Cleveland Clinic Taussig Cancer Center. Dr. Kalaycio was the first editor in chief of Hematology News and held the post for 3 years.
Hematology News welcomes Ifeyinwa (Ify) Osunkwo, MD, MPH, as the new editor in chief.
Dr. Osunkwo is a professor of medicine at Atrium Health and the director of the Sickle Cell Enterprise at the Levine Cancer Institute, part of Atrium Health, in Charlotte, N.C.
She has made it her personal mission to improve the quality of life for patients with sickle cell disease, a passion that began during time spent in Nigeria as a child, where 150,000 children are born each year with the condition. In 2014, Dr. Osunkwo created a comprehensive sickle cell center in Charlotte with a multidisciplinary team of providers that includes physicians, nurses, social workers, psychologists, and nurse managers. She has also been an instrumental part of the Carolinas Sickle Cell Collaborative, which seeks to match sickle cell patients in the community with blood donors who have similar blood characteristics.
“As a practicing hematologist and researcher, I have a deep appreciation for the timely and relevant content provided by Hematology News,” Dr. Osunkwo said. “I hope to use my experience to help make this publication even better.”
She is a member of the National Adult Sickle Cell Provider Network and leads the Transition/Medical Home Committee for the Southeast Regional Genetics Network. Her interests include health literacy, adolescent transition of care, and chronic pain management.
Dr. Osunkwo graduated from medical school at the University of Nigeria, Enugu, performed her residency at the New Jersey Medical School, Newark, and completed her fellowship training at Columbia University, New York.
Dr. Osunkwo takes the reigns at Hematology News from Matt Kalaycio, MD, of the Cleveland Clinic Taussig Cancer Center. Dr. Kalaycio was the first editor in chief of Hematology News and held the post for 3 years.
Hematology News welcomes Ifeyinwa (Ify) Osunkwo, MD, MPH, as the new editor in chief.
Dr. Osunkwo is a professor of medicine at Atrium Health and the director of the Sickle Cell Enterprise at the Levine Cancer Institute, part of Atrium Health, in Charlotte, N.C.
She has made it her personal mission to improve the quality of life for patients with sickle cell disease, a passion that began during time spent in Nigeria as a child, where 150,000 children are born each year with the condition. In 2014, Dr. Osunkwo created a comprehensive sickle cell center in Charlotte with a multidisciplinary team of providers that includes physicians, nurses, social workers, psychologists, and nurse managers. She has also been an instrumental part of the Carolinas Sickle Cell Collaborative, which seeks to match sickle cell patients in the community with blood donors who have similar blood characteristics.
“As a practicing hematologist and researcher, I have a deep appreciation for the timely and relevant content provided by Hematology News,” Dr. Osunkwo said. “I hope to use my experience to help make this publication even better.”
She is a member of the National Adult Sickle Cell Provider Network and leads the Transition/Medical Home Committee for the Southeast Regional Genetics Network. Her interests include health literacy, adolescent transition of care, and chronic pain management.
Dr. Osunkwo graduated from medical school at the University of Nigeria, Enugu, performed her residency at the New Jersey Medical School, Newark, and completed her fellowship training at Columbia University, New York.
Dr. Osunkwo takes the reigns at Hematology News from Matt Kalaycio, MD, of the Cleveland Clinic Taussig Cancer Center. Dr. Kalaycio was the first editor in chief of Hematology News and held the post for 3 years.
Worry Loves Company, but Unnecessary Consultations May Harm the Patients We Comanage
“Never worry alone” is a common mantra that most of us have heard throughout medical training. The premise is simple and well meaning. If a patient has an issue that concerns you, ask someone for help. As a student, this can be a resident; as a resident, this can be an attending. However, for hospitalists, the answer is often a subspecialty consultation. Asking for help never seems to be wrong, but what happens when our worry delays appropriate care with unnecessary consultations? In this month’s issue of the Journal of Hospital Medicine, authors Bellas et al. have investigated this issue through the lens of subspecialty preoperative consultation for patients admitted to a hospitalist comanagement service with a fragility hip fracture requiring surgery.1
Morbidity and mortality for patients who experience hip fractures are high, and time to appropriate surgery is one of the few modifiable risk factors that may reduce morbidity and mortality.2,3 Bellas et al. conducted a retrospective cohort study to test the association between preoperative subspecialty consultation and multiple clinically relevant outcomes in patients admitted with an acute hip fracture.1 All patients were comanaged by a hospitalist and orthopedic surgery, and “consultation” was defined as any preoperative subspecialty consultation requested by the hospitalist. Outcome measures included time to surgery, length of stay, readmission rate, perioperative complications, and 30-day mortality. In total, 36% (177/491) of patients who underwent surgery received a subspecialty preoperative consultation. Unsurprisingly, these patients were older with higher rates of comorbidity. After controlling for age and Charlson Comorbidity Index, preoperative consultation was associated with dramatic delays and increased rates of time to surgery >24 hours (adjusted odds ratio, 4.2; 95% CI: 2.8-6.6). The authors classified 90% of consultations as appropriate, either because of an active condition (eg, acute coronary syndrome) or because admitting physicians documented a perception that patients were at increased risk. However, 73% of consultations had only minor recommendations, such as ordering an ECG or changing the dose of an existing medication, and only 37% of the time did consultations lead to an identifiable change in management as a result of the consultation.
Although striking, integrating these findings into clinical practice is complex. As a retrospective study, patients who received consultations were obviously different from those who did not. The authors attempted to adjust for this but used only age and Charlson Comorbidity Index. Other factors that are both associated with consultations and known to increase mortality—such as frailty and functional status—were not included in their adjustment. Such unmeasured confounders possibly explain at least some, if not all, of the findings that consultations were associated with a doubling of the likelihood of 30-day mortality. In addition, although the authors assessed the appropriateness of consultation and degree of recommendations, their methods for this deserve scrutiny. Two independent providers adjudicated the consultations with excellent agreement (kappa 0.96 for indication, 0.95 for degree of recommendation), but this reliability assessment was done on previously extracted chart data, probably inflating their agreement statistics. Finally, the adjudication of consultant recommendations into minor, moderate, and major categories may oversimplify the outcome of each consultation. For example, all medication recommendations, regardless of type, were considered as minor, and recommendations were considered as major only if they resulted in invasive testing or procedures. This approach may underrepresent the impact of consultations as in clinical practice not all high-impact recommendations result in invasive testing or procedures. Despite these important limitations, Bellas et al. present a compelling case for preoperative consultation being associated with delays in surgery.
How then should this study change practice? The authors’ findings tell two separate but intertwined stories. The first is that preoperative consultation leads to delays in surgery. As patients who received preoperative consultation were obviously sicker, and because delays caused by consultation may lead to increased morbidity and mortality, perhaps the solution is to simply fix the delays. However, this approach ignores the more compelling story the authors tell. More important than the delays was the surprising lack of impact of preoperative consultations. Bellas et al. found that the majority of consultations resulted in only minor recommendations, and more importantly, hospitalists rarely changed treatment as a result. Although patients who received consultations were more ill, consultation rarely changed their care or decreased the risk posed by surgery. Bellas et al. found that only patients with active medical conditions had consultations, which resulted in moderate or major recommendations. These findings highlight an opportunity to better identify patients for whom consultation might be helpful and to prevent delays by avoiding consultation for those unlikely to benefit. There have been several efforts in the orthopedic literature to use guidelines for preoperative cardiac testing to guide cardiology consultation.4,5,6 One study using this approach reported findings that were extremely similar to those reported by Bellas et al. in that 71% of preoperative cardiology consultations in their institution did not meet the guideline criteria for invasive cardiac testing.7 The primary difference between the findings of Bellas et al. and the studies in the orthopedic literature is the presence of the comanaging hospitalist. As more and more patients receive hospitalist comanagement prior to inpatient surgery, it is well within the scope of the hospitalist to differentiate chronic risk factors from active or decompensated medical disease requiring a subspecialist. This is in fact much of the value that a hospitalist adds. Avoiding consultation for patients with only elevated chronic risk factors is an important first step in avoiding unnecessary delays to surgery and an opportunity for hospitalists to improve the care of the patients they comanage.
The goal of teaching trainees to “never worry alone” is to harness the feelings of uncertainty that all providers face to improve patient care. Knowing when to worry is a valuable lesson, but as with all skills, it should be applied thoughtfully and informed by evidence. Appreciating the risks that surgery poses is quintessential to safe perioperative care, but equally important is understanding that inappropriate consultations can create risks from needless delays and testing. Only in balancing these two concerns, and appreciating when it is appropriate to worry, can we provide the highest quality of care to our patients.
1. Bellas N, Stohler S, Staff I, et al. Impact of preoperative consults and hospitalist comanagement in hip fracture patients. J Hosp Med. 2020;15(1):16-21. https:doi.org/jhm.3264.
2. Goldacre MJ, Roberts SE, Yeates D. Mortality after admission to hospital with fractured neck of femur: database study. BMJ 2002;325(7369):868-869. https://doi.org/10.1136/bmj.325.7369.868.
3. Shiga T, Wajima Z, Ohe Y. Is operative delay associated with increased mortality of hip fracture patients? Systematic review, meta-analysis, and meta-regression. Can J Anaesth. 2008;55(3):146-154. https://doi.org/10.1007/BF03016088.
4. Cluett J, Caplan J, Yu W. Preoperative cardiac evaluation of patients with acute hip fracture. Am J Orthop. 2008;37(1):32-36.
5. Smeets SJ, Poeze M, Verbruggen JP. Preoperative cardiac evaluation of geriatric patients with hip fracture. Injury. 2012;43(12):2146-2151. https://doi.org/10.1016/j.injury.2012.08.007.
6. Siu CW, Sun NC, Lau TW, Yiu KH, Leung F, Tse HF. Preoperative cardiac risk assessment in geriatric patients with hip fractures: an orthopedic surgeons’ perspective. Osteoporos Int. 2010;21(Suppl 4):S587-S591. https://doi.org/10.1007/s00198-010-1393-0.
7. Stitgen A, Poludnianyk K, Dulaney-Cripe E, Markert R, Prayson M. Adherence to preoperative cardiac clearance guidelines in hip fracture patients. J Orthop Trauma 2015;29(11):500-503. https://doi.org/10.1097/BOT.0000000000000381.
“Never worry alone” is a common mantra that most of us have heard throughout medical training. The premise is simple and well meaning. If a patient has an issue that concerns you, ask someone for help. As a student, this can be a resident; as a resident, this can be an attending. However, for hospitalists, the answer is often a subspecialty consultation. Asking for help never seems to be wrong, but what happens when our worry delays appropriate care with unnecessary consultations? In this month’s issue of the Journal of Hospital Medicine, authors Bellas et al. have investigated this issue through the lens of subspecialty preoperative consultation for patients admitted to a hospitalist comanagement service with a fragility hip fracture requiring surgery.1
Morbidity and mortality for patients who experience hip fractures are high, and time to appropriate surgery is one of the few modifiable risk factors that may reduce morbidity and mortality.2,3 Bellas et al. conducted a retrospective cohort study to test the association between preoperative subspecialty consultation and multiple clinically relevant outcomes in patients admitted with an acute hip fracture.1 All patients were comanaged by a hospitalist and orthopedic surgery, and “consultation” was defined as any preoperative subspecialty consultation requested by the hospitalist. Outcome measures included time to surgery, length of stay, readmission rate, perioperative complications, and 30-day mortality. In total, 36% (177/491) of patients who underwent surgery received a subspecialty preoperative consultation. Unsurprisingly, these patients were older with higher rates of comorbidity. After controlling for age and Charlson Comorbidity Index, preoperative consultation was associated with dramatic delays and increased rates of time to surgery >24 hours (adjusted odds ratio, 4.2; 95% CI: 2.8-6.6). The authors classified 90% of consultations as appropriate, either because of an active condition (eg, acute coronary syndrome) or because admitting physicians documented a perception that patients were at increased risk. However, 73% of consultations had only minor recommendations, such as ordering an ECG or changing the dose of an existing medication, and only 37% of the time did consultations lead to an identifiable change in management as a result of the consultation.
Although striking, integrating these findings into clinical practice is complex. As a retrospective study, patients who received consultations were obviously different from those who did not. The authors attempted to adjust for this but used only age and Charlson Comorbidity Index. Other factors that are both associated with consultations and known to increase mortality—such as frailty and functional status—were not included in their adjustment. Such unmeasured confounders possibly explain at least some, if not all, of the findings that consultations were associated with a doubling of the likelihood of 30-day mortality. In addition, although the authors assessed the appropriateness of consultation and degree of recommendations, their methods for this deserve scrutiny. Two independent providers adjudicated the consultations with excellent agreement (kappa 0.96 for indication, 0.95 for degree of recommendation), but this reliability assessment was done on previously extracted chart data, probably inflating their agreement statistics. Finally, the adjudication of consultant recommendations into minor, moderate, and major categories may oversimplify the outcome of each consultation. For example, all medication recommendations, regardless of type, were considered as minor, and recommendations were considered as major only if they resulted in invasive testing or procedures. This approach may underrepresent the impact of consultations as in clinical practice not all high-impact recommendations result in invasive testing or procedures. Despite these important limitations, Bellas et al. present a compelling case for preoperative consultation being associated with delays in surgery.
How then should this study change practice? The authors’ findings tell two separate but intertwined stories. The first is that preoperative consultation leads to delays in surgery. As patients who received preoperative consultation were obviously sicker, and because delays caused by consultation may lead to increased morbidity and mortality, perhaps the solution is to simply fix the delays. However, this approach ignores the more compelling story the authors tell. More important than the delays was the surprising lack of impact of preoperative consultations. Bellas et al. found that the majority of consultations resulted in only minor recommendations, and more importantly, hospitalists rarely changed treatment as a result. Although patients who received consultations were more ill, consultation rarely changed their care or decreased the risk posed by surgery. Bellas et al. found that only patients with active medical conditions had consultations, which resulted in moderate or major recommendations. These findings highlight an opportunity to better identify patients for whom consultation might be helpful and to prevent delays by avoiding consultation for those unlikely to benefit. There have been several efforts in the orthopedic literature to use guidelines for preoperative cardiac testing to guide cardiology consultation.4,5,6 One study using this approach reported findings that were extremely similar to those reported by Bellas et al. in that 71% of preoperative cardiology consultations in their institution did not meet the guideline criteria for invasive cardiac testing.7 The primary difference between the findings of Bellas et al. and the studies in the orthopedic literature is the presence of the comanaging hospitalist. As more and more patients receive hospitalist comanagement prior to inpatient surgery, it is well within the scope of the hospitalist to differentiate chronic risk factors from active or decompensated medical disease requiring a subspecialist. This is in fact much of the value that a hospitalist adds. Avoiding consultation for patients with only elevated chronic risk factors is an important first step in avoiding unnecessary delays to surgery and an opportunity for hospitalists to improve the care of the patients they comanage.
The goal of teaching trainees to “never worry alone” is to harness the feelings of uncertainty that all providers face to improve patient care. Knowing when to worry is a valuable lesson, but as with all skills, it should be applied thoughtfully and informed by evidence. Appreciating the risks that surgery poses is quintessential to safe perioperative care, but equally important is understanding that inappropriate consultations can create risks from needless delays and testing. Only in balancing these two concerns, and appreciating when it is appropriate to worry, can we provide the highest quality of care to our patients.
“Never worry alone” is a common mantra that most of us have heard throughout medical training. The premise is simple and well meaning. If a patient has an issue that concerns you, ask someone for help. As a student, this can be a resident; as a resident, this can be an attending. However, for hospitalists, the answer is often a subspecialty consultation. Asking for help never seems to be wrong, but what happens when our worry delays appropriate care with unnecessary consultations? In this month’s issue of the Journal of Hospital Medicine, authors Bellas et al. have investigated this issue through the lens of subspecialty preoperative consultation for patients admitted to a hospitalist comanagement service with a fragility hip fracture requiring surgery.1
Morbidity and mortality for patients who experience hip fractures are high, and time to appropriate surgery is one of the few modifiable risk factors that may reduce morbidity and mortality.2,3 Bellas et al. conducted a retrospective cohort study to test the association between preoperative subspecialty consultation and multiple clinically relevant outcomes in patients admitted with an acute hip fracture.1 All patients were comanaged by a hospitalist and orthopedic surgery, and “consultation” was defined as any preoperative subspecialty consultation requested by the hospitalist. Outcome measures included time to surgery, length of stay, readmission rate, perioperative complications, and 30-day mortality. In total, 36% (177/491) of patients who underwent surgery received a subspecialty preoperative consultation. Unsurprisingly, these patients were older with higher rates of comorbidity. After controlling for age and Charlson Comorbidity Index, preoperative consultation was associated with dramatic delays and increased rates of time to surgery >24 hours (adjusted odds ratio, 4.2; 95% CI: 2.8-6.6). The authors classified 90% of consultations as appropriate, either because of an active condition (eg, acute coronary syndrome) or because admitting physicians documented a perception that patients were at increased risk. However, 73% of consultations had only minor recommendations, such as ordering an ECG or changing the dose of an existing medication, and only 37% of the time did consultations lead to an identifiable change in management as a result of the consultation.
Although striking, integrating these findings into clinical practice is complex. As a retrospective study, patients who received consultations were obviously different from those who did not. The authors attempted to adjust for this but used only age and Charlson Comorbidity Index. Other factors that are both associated with consultations and known to increase mortality—such as frailty and functional status—were not included in their adjustment. Such unmeasured confounders possibly explain at least some, if not all, of the findings that consultations were associated with a doubling of the likelihood of 30-day mortality. In addition, although the authors assessed the appropriateness of consultation and degree of recommendations, their methods for this deserve scrutiny. Two independent providers adjudicated the consultations with excellent agreement (kappa 0.96 for indication, 0.95 for degree of recommendation), but this reliability assessment was done on previously extracted chart data, probably inflating their agreement statistics. Finally, the adjudication of consultant recommendations into minor, moderate, and major categories may oversimplify the outcome of each consultation. For example, all medication recommendations, regardless of type, were considered as minor, and recommendations were considered as major only if they resulted in invasive testing or procedures. This approach may underrepresent the impact of consultations as in clinical practice not all high-impact recommendations result in invasive testing or procedures. Despite these important limitations, Bellas et al. present a compelling case for preoperative consultation being associated with delays in surgery.
How then should this study change practice? The authors’ findings tell two separate but intertwined stories. The first is that preoperative consultation leads to delays in surgery. As patients who received preoperative consultation were obviously sicker, and because delays caused by consultation may lead to increased morbidity and mortality, perhaps the solution is to simply fix the delays. However, this approach ignores the more compelling story the authors tell. More important than the delays was the surprising lack of impact of preoperative consultations. Bellas et al. found that the majority of consultations resulted in only minor recommendations, and more importantly, hospitalists rarely changed treatment as a result. Although patients who received consultations were more ill, consultation rarely changed their care or decreased the risk posed by surgery. Bellas et al. found that only patients with active medical conditions had consultations, which resulted in moderate or major recommendations. These findings highlight an opportunity to better identify patients for whom consultation might be helpful and to prevent delays by avoiding consultation for those unlikely to benefit. There have been several efforts in the orthopedic literature to use guidelines for preoperative cardiac testing to guide cardiology consultation.4,5,6 One study using this approach reported findings that were extremely similar to those reported by Bellas et al. in that 71% of preoperative cardiology consultations in their institution did not meet the guideline criteria for invasive cardiac testing.7 The primary difference between the findings of Bellas et al. and the studies in the orthopedic literature is the presence of the comanaging hospitalist. As more and more patients receive hospitalist comanagement prior to inpatient surgery, it is well within the scope of the hospitalist to differentiate chronic risk factors from active or decompensated medical disease requiring a subspecialist. This is in fact much of the value that a hospitalist adds. Avoiding consultation for patients with only elevated chronic risk factors is an important first step in avoiding unnecessary delays to surgery and an opportunity for hospitalists to improve the care of the patients they comanage.
The goal of teaching trainees to “never worry alone” is to harness the feelings of uncertainty that all providers face to improve patient care. Knowing when to worry is a valuable lesson, but as with all skills, it should be applied thoughtfully and informed by evidence. Appreciating the risks that surgery poses is quintessential to safe perioperative care, but equally important is understanding that inappropriate consultations can create risks from needless delays and testing. Only in balancing these two concerns, and appreciating when it is appropriate to worry, can we provide the highest quality of care to our patients.
1. Bellas N, Stohler S, Staff I, et al. Impact of preoperative consults and hospitalist comanagement in hip fracture patients. J Hosp Med. 2020;15(1):16-21. https:doi.org/jhm.3264.
2. Goldacre MJ, Roberts SE, Yeates D. Mortality after admission to hospital with fractured neck of femur: database study. BMJ 2002;325(7369):868-869. https://doi.org/10.1136/bmj.325.7369.868.
3. Shiga T, Wajima Z, Ohe Y. Is operative delay associated with increased mortality of hip fracture patients? Systematic review, meta-analysis, and meta-regression. Can J Anaesth. 2008;55(3):146-154. https://doi.org/10.1007/BF03016088.
4. Cluett J, Caplan J, Yu W. Preoperative cardiac evaluation of patients with acute hip fracture. Am J Orthop. 2008;37(1):32-36.
5. Smeets SJ, Poeze M, Verbruggen JP. Preoperative cardiac evaluation of geriatric patients with hip fracture. Injury. 2012;43(12):2146-2151. https://doi.org/10.1016/j.injury.2012.08.007.
6. Siu CW, Sun NC, Lau TW, Yiu KH, Leung F, Tse HF. Preoperative cardiac risk assessment in geriatric patients with hip fractures: an orthopedic surgeons’ perspective. Osteoporos Int. 2010;21(Suppl 4):S587-S591. https://doi.org/10.1007/s00198-010-1393-0.
7. Stitgen A, Poludnianyk K, Dulaney-Cripe E, Markert R, Prayson M. Adherence to preoperative cardiac clearance guidelines in hip fracture patients. J Orthop Trauma 2015;29(11):500-503. https://doi.org/10.1097/BOT.0000000000000381.
1. Bellas N, Stohler S, Staff I, et al. Impact of preoperative consults and hospitalist comanagement in hip fracture patients. J Hosp Med. 2020;15(1):16-21. https:doi.org/jhm.3264.
2. Goldacre MJ, Roberts SE, Yeates D. Mortality after admission to hospital with fractured neck of femur: database study. BMJ 2002;325(7369):868-869. https://doi.org/10.1136/bmj.325.7369.868.
3. Shiga T, Wajima Z, Ohe Y. Is operative delay associated with increased mortality of hip fracture patients? Systematic review, meta-analysis, and meta-regression. Can J Anaesth. 2008;55(3):146-154. https://doi.org/10.1007/BF03016088.
4. Cluett J, Caplan J, Yu W. Preoperative cardiac evaluation of patients with acute hip fracture. Am J Orthop. 2008;37(1):32-36.
5. Smeets SJ, Poeze M, Verbruggen JP. Preoperative cardiac evaluation of geriatric patients with hip fracture. Injury. 2012;43(12):2146-2151. https://doi.org/10.1016/j.injury.2012.08.007.
6. Siu CW, Sun NC, Lau TW, Yiu KH, Leung F, Tse HF. Preoperative cardiac risk assessment in geriatric patients with hip fractures: an orthopedic surgeons’ perspective. Osteoporos Int. 2010;21(Suppl 4):S587-S591. https://doi.org/10.1007/s00198-010-1393-0.
7. Stitgen A, Poludnianyk K, Dulaney-Cripe E, Markert R, Prayson M. Adherence to preoperative cardiac clearance guidelines in hip fracture patients. J Orthop Trauma 2015;29(11):500-503. https://doi.org/10.1097/BOT.0000000000000381.
© 2020 Society of Hospital Medicine
Quantifying the Risks of Hospitalization—Is It Really as Safe as We Believe?
Even though I could not remember her name, I remembered her story, and I would bet that my colleagues did as well. She was someone that we had all cared for at one time or another. She frequently presented to the hospital with chest pain or shortness of breath attributable to a combination of longstanding congestive heart failure, chronic obstructive pulmonary disease, and cocaine abuse. But most tragic of all, she was homeless, which meant that she was frequently hospitalized not only for medical complaints but also for a night’s shelter and a bite of food. Even though she often refused medical treatment and social workers’ efforts to stabilize her housing situation, the staff in the emergency room and observation unit all knew her by name and greeted her like an old friend. And then one day she stopped showing up to the hospital. Sitting in the emergency department (ED), I overheard that she was found outside of a storefront and had passed away. Saddened by her death, which was not unexpected given her medical issues, I still wondered if we had done right by her during the hundreds of times that she had come to our hospital. Clinicians at busy safety-net hospitals face these questions every day, and it would seem beyond doubt that our duty is to address both medical and nonmedical determinants of health of everyone that walks through our door. But is this in fact the right thing to do? Is it possible that we unwittingly expose these vulnerable patients to risks from hospitalization alone?
In this month’s Journal of Hospital Medicine, Sekijima et al. sought to quantify precisely the risks of hospitalization, particularly among the subset of patients whose “severity” of medical problems alone might not have warranted hospital admission, a scenario known colloquially as a “social” admission.1 In real time, an inhouse triage physician classified patients as being admitted with or without “definite medical acuity.” Investigators retrospectively identified adverse events and illness acuity using standardized instruments, the Institute for Healthcare Improvement Global Trigger Tool and Emergency Severity Index, respectively. Despite the acknowledged differences in the patient population and the inherent subjectivity within the designation process, Sekijima et al. found no statistically significant difference in the percentage of admissions with an adverse event nor in the rate of adverse events per 1,000 patient days. Falls, oversedation/hypotension and code/arrest/rapid response activation were the most frequently encountered adverse events.
Delving deeper into the origin of admissions without definite medical acuity, the authors identified homelessness, lack of outpatient social support, substance use disorder, and lack of outpatient medical support as the most common reasons for “nonmedical” admissions. As healthcare providers, we recognize that these factors are generally long-term, chronic socioeconomic determinants of health. Despite our objective knowledge that we are limited in our ability to fix these problems on a short-term basis, the authors’ observations reflect our compulsion to try and help in any way possible. Patients admitted without definite medical acuity were more vulnerable and had higher rates of public insurance and housing insecurity. However, they were less acutely ill, as indicated by lower Emergency Severity Index scores. These factors were not associated with statistically significant differences in either 48-hour ED readmission or 30-day hospital readmission rates.
The process of appropriately triaging patients to an inpatient setting is challenging because of wide variability in both patients and ED providers. Hospitalists are increasingly recognized as an additional resource to assist in the triage process, as we are uniquely in a position to view the patient’s clinical presentation within the context of their anticipated clinical trajectory, promote effective utilization of inpatient bed availability, and anticipate potential barriers to discharge. Graduate medical education now identifies the triage process as a specific milestone within the transitions of care competency, as it requires mastery of interpersonal communication, professionalism, systems-based thinking, and patient-centered care.2 However, many institutions lack a dedicated faculty member to perform the triage role. Our institution recently examined the feasibility of instituting a daily “huddle” between the admitting hospitalist and the ED to facilitate interdepartmental communication to create care plans in patient triage and to promote patient throughput. Available admission beds are valuable commodities, and one challenge is that the ED makes disposition decisions without knowledge of the number of available beds in the hospital. The goal of the huddle was to quickly discuss all patients potentially requiring admission prior to the final disposition decision and to address any modifiable factors to potentially prevent a “social” admission with social work early in the day. Further work is in progress to determine if introducing flexibility within existing provider roles can improve the triage process in a measurable and efficient manner.
Many challenges remain as we balance the medical needs of patients with any potential social drivers that necessitate admission to the inpatient hospital setting. From an ED perspective, social support and community follow-up were “universally considered powerful influences on admission,” and other factors such as time of day, clinical volume, and the four-hour waiting time target also played a significant role in the decision to admit.3 Hunter et al. found that admissions with moderate to low acuity may be shorter or less costly,4 which presents an interesting question of cost-effectiveness as an avenue for further study. As clinicians, we are intuitively aware of the subjective risk of hospitalization itself, and this work provides new objective evidence that hospitalization confers specific and quantifiable risks. Though we can undoubtedly use this knowledge to guide internal decisions about admissions and discharges, do we also have an obligation to inform our patients about these risks in real time? Ultimately, hospitalization itself might be viewed as a “procedure” or intervention that has inherent risks for all who receive it, regardless of the individual patient or hospital characteristics. As hospitalists, we should continue to strive to reduce these risks, but we should also initiate a conversation about the risks and benefits of hospitalization similarly to how we discuss other procedures with patients and their families.
1. Sekijima A, Sunga C, Bann M. Adverse events experienced by patients hospitalized without definite medical acuity: A retrospective cohort study. J Hosp Med. 2020;15(1):42-45. https://doi.org/10.12788/jhm.3235.
2. Wang ES, Velásquez ST, Smith CJ, et al. Triaging inpatient admissions : An opportunity for resident education. J Gen Intern Med. 2019;34(5):754-757. https://doi.org/10.1007/s11606-019-04882-2.
3. Pope I, Burn H, Ismail SA, et al. A qualitative study exploring the factors influencing admission to hospital from the emergency department. BMJ Open. 2017;7(8):e011543. https://doi.org/10.1136/bmjopen-2016-011543.
4. Lewis Hunter AE, Spatz ES, Bernstein SL, Rosenthal MS. Factors influencing hospital admission of non-critically ill patients presenting to the emergency department: a cross-sectional study. J Gen Intern Med. 2016;31(1):37-44. https://doi.org/10.1007/s11606-015-3438-8.
Even though I could not remember her name, I remembered her story, and I would bet that my colleagues did as well. She was someone that we had all cared for at one time or another. She frequently presented to the hospital with chest pain or shortness of breath attributable to a combination of longstanding congestive heart failure, chronic obstructive pulmonary disease, and cocaine abuse. But most tragic of all, she was homeless, which meant that she was frequently hospitalized not only for medical complaints but also for a night’s shelter and a bite of food. Even though she often refused medical treatment and social workers’ efforts to stabilize her housing situation, the staff in the emergency room and observation unit all knew her by name and greeted her like an old friend. And then one day she stopped showing up to the hospital. Sitting in the emergency department (ED), I overheard that she was found outside of a storefront and had passed away. Saddened by her death, which was not unexpected given her medical issues, I still wondered if we had done right by her during the hundreds of times that she had come to our hospital. Clinicians at busy safety-net hospitals face these questions every day, and it would seem beyond doubt that our duty is to address both medical and nonmedical determinants of health of everyone that walks through our door. But is this in fact the right thing to do? Is it possible that we unwittingly expose these vulnerable patients to risks from hospitalization alone?
In this month’s Journal of Hospital Medicine, Sekijima et al. sought to quantify precisely the risks of hospitalization, particularly among the subset of patients whose “severity” of medical problems alone might not have warranted hospital admission, a scenario known colloquially as a “social” admission.1 In real time, an inhouse triage physician classified patients as being admitted with or without “definite medical acuity.” Investigators retrospectively identified adverse events and illness acuity using standardized instruments, the Institute for Healthcare Improvement Global Trigger Tool and Emergency Severity Index, respectively. Despite the acknowledged differences in the patient population and the inherent subjectivity within the designation process, Sekijima et al. found no statistically significant difference in the percentage of admissions with an adverse event nor in the rate of adverse events per 1,000 patient days. Falls, oversedation/hypotension and code/arrest/rapid response activation were the most frequently encountered adverse events.
Delving deeper into the origin of admissions without definite medical acuity, the authors identified homelessness, lack of outpatient social support, substance use disorder, and lack of outpatient medical support as the most common reasons for “nonmedical” admissions. As healthcare providers, we recognize that these factors are generally long-term, chronic socioeconomic determinants of health. Despite our objective knowledge that we are limited in our ability to fix these problems on a short-term basis, the authors’ observations reflect our compulsion to try and help in any way possible. Patients admitted without definite medical acuity were more vulnerable and had higher rates of public insurance and housing insecurity. However, they were less acutely ill, as indicated by lower Emergency Severity Index scores. These factors were not associated with statistically significant differences in either 48-hour ED readmission or 30-day hospital readmission rates.
The process of appropriately triaging patients to an inpatient setting is challenging because of wide variability in both patients and ED providers. Hospitalists are increasingly recognized as an additional resource to assist in the triage process, as we are uniquely in a position to view the patient’s clinical presentation within the context of their anticipated clinical trajectory, promote effective utilization of inpatient bed availability, and anticipate potential barriers to discharge. Graduate medical education now identifies the triage process as a specific milestone within the transitions of care competency, as it requires mastery of interpersonal communication, professionalism, systems-based thinking, and patient-centered care.2 However, many institutions lack a dedicated faculty member to perform the triage role. Our institution recently examined the feasibility of instituting a daily “huddle” between the admitting hospitalist and the ED to facilitate interdepartmental communication to create care plans in patient triage and to promote patient throughput. Available admission beds are valuable commodities, and one challenge is that the ED makes disposition decisions without knowledge of the number of available beds in the hospital. The goal of the huddle was to quickly discuss all patients potentially requiring admission prior to the final disposition decision and to address any modifiable factors to potentially prevent a “social” admission with social work early in the day. Further work is in progress to determine if introducing flexibility within existing provider roles can improve the triage process in a measurable and efficient manner.
Many challenges remain as we balance the medical needs of patients with any potential social drivers that necessitate admission to the inpatient hospital setting. From an ED perspective, social support and community follow-up were “universally considered powerful influences on admission,” and other factors such as time of day, clinical volume, and the four-hour waiting time target also played a significant role in the decision to admit.3 Hunter et al. found that admissions with moderate to low acuity may be shorter or less costly,4 which presents an interesting question of cost-effectiveness as an avenue for further study. As clinicians, we are intuitively aware of the subjective risk of hospitalization itself, and this work provides new objective evidence that hospitalization confers specific and quantifiable risks. Though we can undoubtedly use this knowledge to guide internal decisions about admissions and discharges, do we also have an obligation to inform our patients about these risks in real time? Ultimately, hospitalization itself might be viewed as a “procedure” or intervention that has inherent risks for all who receive it, regardless of the individual patient or hospital characteristics. As hospitalists, we should continue to strive to reduce these risks, but we should also initiate a conversation about the risks and benefits of hospitalization similarly to how we discuss other procedures with patients and their families.
Even though I could not remember her name, I remembered her story, and I would bet that my colleagues did as well. She was someone that we had all cared for at one time or another. She frequently presented to the hospital with chest pain or shortness of breath attributable to a combination of longstanding congestive heart failure, chronic obstructive pulmonary disease, and cocaine abuse. But most tragic of all, she was homeless, which meant that she was frequently hospitalized not only for medical complaints but also for a night’s shelter and a bite of food. Even though she often refused medical treatment and social workers’ efforts to stabilize her housing situation, the staff in the emergency room and observation unit all knew her by name and greeted her like an old friend. And then one day she stopped showing up to the hospital. Sitting in the emergency department (ED), I overheard that she was found outside of a storefront and had passed away. Saddened by her death, which was not unexpected given her medical issues, I still wondered if we had done right by her during the hundreds of times that she had come to our hospital. Clinicians at busy safety-net hospitals face these questions every day, and it would seem beyond doubt that our duty is to address both medical and nonmedical determinants of health of everyone that walks through our door. But is this in fact the right thing to do? Is it possible that we unwittingly expose these vulnerable patients to risks from hospitalization alone?
In this month’s Journal of Hospital Medicine, Sekijima et al. sought to quantify precisely the risks of hospitalization, particularly among the subset of patients whose “severity” of medical problems alone might not have warranted hospital admission, a scenario known colloquially as a “social” admission.1 In real time, an inhouse triage physician classified patients as being admitted with or without “definite medical acuity.” Investigators retrospectively identified adverse events and illness acuity using standardized instruments, the Institute for Healthcare Improvement Global Trigger Tool and Emergency Severity Index, respectively. Despite the acknowledged differences in the patient population and the inherent subjectivity within the designation process, Sekijima et al. found no statistically significant difference in the percentage of admissions with an adverse event nor in the rate of adverse events per 1,000 patient days. Falls, oversedation/hypotension and code/arrest/rapid response activation were the most frequently encountered adverse events.
Delving deeper into the origin of admissions without definite medical acuity, the authors identified homelessness, lack of outpatient social support, substance use disorder, and lack of outpatient medical support as the most common reasons for “nonmedical” admissions. As healthcare providers, we recognize that these factors are generally long-term, chronic socioeconomic determinants of health. Despite our objective knowledge that we are limited in our ability to fix these problems on a short-term basis, the authors’ observations reflect our compulsion to try and help in any way possible. Patients admitted without definite medical acuity were more vulnerable and had higher rates of public insurance and housing insecurity. However, they were less acutely ill, as indicated by lower Emergency Severity Index scores. These factors were not associated with statistically significant differences in either 48-hour ED readmission or 30-day hospital readmission rates.
The process of appropriately triaging patients to an inpatient setting is challenging because of wide variability in both patients and ED providers. Hospitalists are increasingly recognized as an additional resource to assist in the triage process, as we are uniquely in a position to view the patient’s clinical presentation within the context of their anticipated clinical trajectory, promote effective utilization of inpatient bed availability, and anticipate potential barriers to discharge. Graduate medical education now identifies the triage process as a specific milestone within the transitions of care competency, as it requires mastery of interpersonal communication, professionalism, systems-based thinking, and patient-centered care.2 However, many institutions lack a dedicated faculty member to perform the triage role. Our institution recently examined the feasibility of instituting a daily “huddle” between the admitting hospitalist and the ED to facilitate interdepartmental communication to create care plans in patient triage and to promote patient throughput. Available admission beds are valuable commodities, and one challenge is that the ED makes disposition decisions without knowledge of the number of available beds in the hospital. The goal of the huddle was to quickly discuss all patients potentially requiring admission prior to the final disposition decision and to address any modifiable factors to potentially prevent a “social” admission with social work early in the day. Further work is in progress to determine if introducing flexibility within existing provider roles can improve the triage process in a measurable and efficient manner.
Many challenges remain as we balance the medical needs of patients with any potential social drivers that necessitate admission to the inpatient hospital setting. From an ED perspective, social support and community follow-up were “universally considered powerful influences on admission,” and other factors such as time of day, clinical volume, and the four-hour waiting time target also played a significant role in the decision to admit.3 Hunter et al. found that admissions with moderate to low acuity may be shorter or less costly,4 which presents an interesting question of cost-effectiveness as an avenue for further study. As clinicians, we are intuitively aware of the subjective risk of hospitalization itself, and this work provides new objective evidence that hospitalization confers specific and quantifiable risks. Though we can undoubtedly use this knowledge to guide internal decisions about admissions and discharges, do we also have an obligation to inform our patients about these risks in real time? Ultimately, hospitalization itself might be viewed as a “procedure” or intervention that has inherent risks for all who receive it, regardless of the individual patient or hospital characteristics. As hospitalists, we should continue to strive to reduce these risks, but we should also initiate a conversation about the risks and benefits of hospitalization similarly to how we discuss other procedures with patients and their families.
1. Sekijima A, Sunga C, Bann M. Adverse events experienced by patients hospitalized without definite medical acuity: A retrospective cohort study. J Hosp Med. 2020;15(1):42-45. https://doi.org/10.12788/jhm.3235.
2. Wang ES, Velásquez ST, Smith CJ, et al. Triaging inpatient admissions : An opportunity for resident education. J Gen Intern Med. 2019;34(5):754-757. https://doi.org/10.1007/s11606-019-04882-2.
3. Pope I, Burn H, Ismail SA, et al. A qualitative study exploring the factors influencing admission to hospital from the emergency department. BMJ Open. 2017;7(8):e011543. https://doi.org/10.1136/bmjopen-2016-011543.
4. Lewis Hunter AE, Spatz ES, Bernstein SL, Rosenthal MS. Factors influencing hospital admission of non-critically ill patients presenting to the emergency department: a cross-sectional study. J Gen Intern Med. 2016;31(1):37-44. https://doi.org/10.1007/s11606-015-3438-8.
1. Sekijima A, Sunga C, Bann M. Adverse events experienced by patients hospitalized without definite medical acuity: A retrospective cohort study. J Hosp Med. 2020;15(1):42-45. https://doi.org/10.12788/jhm.3235.
2. Wang ES, Velásquez ST, Smith CJ, et al. Triaging inpatient admissions : An opportunity for resident education. J Gen Intern Med. 2019;34(5):754-757. https://doi.org/10.1007/s11606-019-04882-2.
3. Pope I, Burn H, Ismail SA, et al. A qualitative study exploring the factors influencing admission to hospital from the emergency department. BMJ Open. 2017;7(8):e011543. https://doi.org/10.1136/bmjopen-2016-011543.
4. Lewis Hunter AE, Spatz ES, Bernstein SL, Rosenthal MS. Factors influencing hospital admission of non-critically ill patients presenting to the emergency department: a cross-sectional study. J Gen Intern Med. 2016;31(1):37-44. https://doi.org/10.1007/s11606-015-3438-8.
© 2020 Society of Hospital Medicine
Leadership & Professional Development: Make the Most of Your Oranges
“If you define the problem correctly, you almost have the solution.”
—Steve Jobs
In the classic tale of a chaotic kitchen before an important dinner, two feuding chefs urgently need the only remaining orange in the pantry for their respective dishes. The first chef asserts its necessity for his prized sauce. The second chef retorts that her dessert will be ruined without it. After an emotion-laden battle, they finally agree to compromise, cutting the orange in half. The first chef squeezes the juice out of his half of the orange for his sauce, while the second grates half the zest she needs for her cake. Each chef had less of the orange than their recipe needed, but figured this was the best they could do given the dispute.1
Conflict frequently occurs for hospitalists leading change efforts, managing service lines, and caring for patients. Often conflict can help clarify a decision or course of action. However, when navigated poorly, disputes can also consume precious energy and sap the goodwill and cooperation needed to effectively lead change and ensure excellent clinical care. Worse yet, ineffective conversations can result in begrudging and ultimately value-destroying agreements, as the chefs above demonstrate.
Instead of focusing on someone’s position (the need for the orange), successful leaders first seek to understand all discernible underlying interests (zest, juice) and motivations (creating a signature dish) of each party.1 Essential to this process is swift recognition of the conflict and self-regulation. Rather than succumbing to strong fight-or-flight reactions, the wise hospitalist first takes inventory of their own interests and calmly applies a known schema, similar to their approach to common clinical scenarios.
So how can you get to the underlying interests effectively? We use a three-step process reminding us of the benefits of the orange’s ACID.2
ASK TO DISCOVER INTERESTS
Ask open-ended questions and closely listen to their responses. Listening more than talking is critical to this process. When facing conflict, it is common to listen only to refute the other’s position. Instead, actively suppress your instinct to “reload” and seek to genuinely understand the other’s perspective. Continue to ask clarifying questions until you feel you understand their interests.
A new hire requests a higher salary than offered. Ask with curiosity: “Can you tell me more about some of your financial priorities? Even if I can’t do much about the dollar figure, there may be benefits and other helpful tips I can suggest.”
CHECK YOUR UNDERSTANDING
Restate your understanding of their interests from listening. This critical step serves to confirm your good-faith effort to address a common problem and to demonstrate that you have heard their perspective accurately. Even if you ultimately cannot agree on a solution to the dispute at hand, demonstrating an understanding of their perspective helps to preserve the relationship, which can be useful for future conflicts.
“I am hearing that you are hoping to save money for the future, to pay down outstanding loans, and to expand your family. Is that right?”
IDENTIFY SOLUTIONS TOGETHER
Accurately defining interests and demonstrating your understanding will maximize the possibility of mutually acceptable solutions. Share your own perspective, being careful to describe your underlying interests, not positions. What mutual goals do you share? What potential solutions were not immediately evident based on positions alone? During this process, remain open to arriving at a solution that you had not anticipated.
“While I unfortunately have little wiggle room on annual salary, there are some options for loan repayment, housing down payment assistance, and low-cost childcare at the health system, which is where my kids went.”
Whether you are a chef or a hospitalist and whether you are dividing oranges or clinical shifts, understanding the interests buried within the conflict will help define and potentially solve the problem. When you encounter an orange, remember the value of its ACID.
Acknowledgement
The authors wish to thank Charlie Wray, DO, Division of Hospital Medicine, San Francisco VA, for assistance with revisions of early drafts.
1. Fisher RL., Ury A, Patton B. Getting to Yes. Penguin Books, 2011.
2. Adapted from: Chou CL, Cooley L. Communication Rx. McGraw Hill, 2018.
“If you define the problem correctly, you almost have the solution.”
—Steve Jobs
In the classic tale of a chaotic kitchen before an important dinner, two feuding chefs urgently need the only remaining orange in the pantry for their respective dishes. The first chef asserts its necessity for his prized sauce. The second chef retorts that her dessert will be ruined without it. After an emotion-laden battle, they finally agree to compromise, cutting the orange in half. The first chef squeezes the juice out of his half of the orange for his sauce, while the second grates half the zest she needs for her cake. Each chef had less of the orange than their recipe needed, but figured this was the best they could do given the dispute.1
Conflict frequently occurs for hospitalists leading change efforts, managing service lines, and caring for patients. Often conflict can help clarify a decision or course of action. However, when navigated poorly, disputes can also consume precious energy and sap the goodwill and cooperation needed to effectively lead change and ensure excellent clinical care. Worse yet, ineffective conversations can result in begrudging and ultimately value-destroying agreements, as the chefs above demonstrate.
Instead of focusing on someone’s position (the need for the orange), successful leaders first seek to understand all discernible underlying interests (zest, juice) and motivations (creating a signature dish) of each party.1 Essential to this process is swift recognition of the conflict and self-regulation. Rather than succumbing to strong fight-or-flight reactions, the wise hospitalist first takes inventory of their own interests and calmly applies a known schema, similar to their approach to common clinical scenarios.
So how can you get to the underlying interests effectively? We use a three-step process reminding us of the benefits of the orange’s ACID.2
ASK TO DISCOVER INTERESTS
Ask open-ended questions and closely listen to their responses. Listening more than talking is critical to this process. When facing conflict, it is common to listen only to refute the other’s position. Instead, actively suppress your instinct to “reload” and seek to genuinely understand the other’s perspective. Continue to ask clarifying questions until you feel you understand their interests.
A new hire requests a higher salary than offered. Ask with curiosity: “Can you tell me more about some of your financial priorities? Even if I can’t do much about the dollar figure, there may be benefits and other helpful tips I can suggest.”
CHECK YOUR UNDERSTANDING
Restate your understanding of their interests from listening. This critical step serves to confirm your good-faith effort to address a common problem and to demonstrate that you have heard their perspective accurately. Even if you ultimately cannot agree on a solution to the dispute at hand, demonstrating an understanding of their perspective helps to preserve the relationship, which can be useful for future conflicts.
“I am hearing that you are hoping to save money for the future, to pay down outstanding loans, and to expand your family. Is that right?”
IDENTIFY SOLUTIONS TOGETHER
Accurately defining interests and demonstrating your understanding will maximize the possibility of mutually acceptable solutions. Share your own perspective, being careful to describe your underlying interests, not positions. What mutual goals do you share? What potential solutions were not immediately evident based on positions alone? During this process, remain open to arriving at a solution that you had not anticipated.
“While I unfortunately have little wiggle room on annual salary, there are some options for loan repayment, housing down payment assistance, and low-cost childcare at the health system, which is where my kids went.”
Whether you are a chef or a hospitalist and whether you are dividing oranges or clinical shifts, understanding the interests buried within the conflict will help define and potentially solve the problem. When you encounter an orange, remember the value of its ACID.
Acknowledgement
The authors wish to thank Charlie Wray, DO, Division of Hospital Medicine, San Francisco VA, for assistance with revisions of early drafts.
“If you define the problem correctly, you almost have the solution.”
—Steve Jobs
In the classic tale of a chaotic kitchen before an important dinner, two feuding chefs urgently need the only remaining orange in the pantry for their respective dishes. The first chef asserts its necessity for his prized sauce. The second chef retorts that her dessert will be ruined without it. After an emotion-laden battle, they finally agree to compromise, cutting the orange in half. The first chef squeezes the juice out of his half of the orange for his sauce, while the second grates half the zest she needs for her cake. Each chef had less of the orange than their recipe needed, but figured this was the best they could do given the dispute.1
Conflict frequently occurs for hospitalists leading change efforts, managing service lines, and caring for patients. Often conflict can help clarify a decision or course of action. However, when navigated poorly, disputes can also consume precious energy and sap the goodwill and cooperation needed to effectively lead change and ensure excellent clinical care. Worse yet, ineffective conversations can result in begrudging and ultimately value-destroying agreements, as the chefs above demonstrate.
Instead of focusing on someone’s position (the need for the orange), successful leaders first seek to understand all discernible underlying interests (zest, juice) and motivations (creating a signature dish) of each party.1 Essential to this process is swift recognition of the conflict and self-regulation. Rather than succumbing to strong fight-or-flight reactions, the wise hospitalist first takes inventory of their own interests and calmly applies a known schema, similar to their approach to common clinical scenarios.
So how can you get to the underlying interests effectively? We use a three-step process reminding us of the benefits of the orange’s ACID.2
ASK TO DISCOVER INTERESTS
Ask open-ended questions and closely listen to their responses. Listening more than talking is critical to this process. When facing conflict, it is common to listen only to refute the other’s position. Instead, actively suppress your instinct to “reload” and seek to genuinely understand the other’s perspective. Continue to ask clarifying questions until you feel you understand their interests.
A new hire requests a higher salary than offered. Ask with curiosity: “Can you tell me more about some of your financial priorities? Even if I can’t do much about the dollar figure, there may be benefits and other helpful tips I can suggest.”
CHECK YOUR UNDERSTANDING
Restate your understanding of their interests from listening. This critical step serves to confirm your good-faith effort to address a common problem and to demonstrate that you have heard their perspective accurately. Even if you ultimately cannot agree on a solution to the dispute at hand, demonstrating an understanding of their perspective helps to preserve the relationship, which can be useful for future conflicts.
“I am hearing that you are hoping to save money for the future, to pay down outstanding loans, and to expand your family. Is that right?”
IDENTIFY SOLUTIONS TOGETHER
Accurately defining interests and demonstrating your understanding will maximize the possibility of mutually acceptable solutions. Share your own perspective, being careful to describe your underlying interests, not positions. What mutual goals do you share? What potential solutions were not immediately evident based on positions alone? During this process, remain open to arriving at a solution that you had not anticipated.
“While I unfortunately have little wiggle room on annual salary, there are some options for loan repayment, housing down payment assistance, and low-cost childcare at the health system, which is where my kids went.”
Whether you are a chef or a hospitalist and whether you are dividing oranges or clinical shifts, understanding the interests buried within the conflict will help define and potentially solve the problem. When you encounter an orange, remember the value of its ACID.
Acknowledgement
The authors wish to thank Charlie Wray, DO, Division of Hospital Medicine, San Francisco VA, for assistance with revisions of early drafts.
1. Fisher RL., Ury A, Patton B. Getting to Yes. Penguin Books, 2011.
2. Adapted from: Chou CL, Cooley L. Communication Rx. McGraw Hill, 2018.
1. Fisher RL., Ury A, Patton B. Getting to Yes. Penguin Books, 2011.
2. Adapted from: Chou CL, Cooley L. Communication Rx. McGraw Hill, 2018.
© 2020 Society of Hospital Medicine
In Reply to “Be Careful What We Call It”
I appreciate the input from Dr. Rauch regarding the terminology of “fellowship” in regards to APP postgraduate training programs.1 When researching these programs, the overwhelming majority we surveyed described themselves as fellowships. Because of this, we chose to use the same nomenclature. The survey we used was meant to explore and quantify certain discreet components of program creation and execution, and further study would be needed to shed light on how they name themselves.
While it is not known if the term “fellowship” in this context would be confusing to patients, it does seem that the ideal terminology has not yet been clarified. In 2014, the American Association of Nurse Practitioners released a position statement that, for NP postgraduate training programs, the term “fellowship” should be used above other terms.2 We were unable to find a similar position statement regarding postgraduate physician assistant training, but did note that the Association of Post-Graduate PA Programs website uses the terms “residency” and “fellowship” seemingly interchangeably.3 As most of the programs that we surveyed train mixed groups of nurse practitioners and physician assistants, developing unified language will be an important step in the future.
1. Rauch D. Be Careful What We Call it. J Hosp Med. 2019;15(1):64. https://doi.org/10.12788/jhm.3297.
2. AANP and the NP Roundtable Joint Statements (2014). Nurse Practitioner Perspective on Education a nd Post-Graduate Training. [online] Available at: https://storage.aanp.org/www/documents/advocacy/nproundtablestatementmay6th.pdf Accessed August 27, 2019.
3. Home - APPAP. APPAP. https://appap.org. Published 2019. Accessed August 27, 2019.
I appreciate the input from Dr. Rauch regarding the terminology of “fellowship” in regards to APP postgraduate training programs.1 When researching these programs, the overwhelming majority we surveyed described themselves as fellowships. Because of this, we chose to use the same nomenclature. The survey we used was meant to explore and quantify certain discreet components of program creation and execution, and further study would be needed to shed light on how they name themselves.
While it is not known if the term “fellowship” in this context would be confusing to patients, it does seem that the ideal terminology has not yet been clarified. In 2014, the American Association of Nurse Practitioners released a position statement that, for NP postgraduate training programs, the term “fellowship” should be used above other terms.2 We were unable to find a similar position statement regarding postgraduate physician assistant training, but did note that the Association of Post-Graduate PA Programs website uses the terms “residency” and “fellowship” seemingly interchangeably.3 As most of the programs that we surveyed train mixed groups of nurse practitioners and physician assistants, developing unified language will be an important step in the future.
I appreciate the input from Dr. Rauch regarding the terminology of “fellowship” in regards to APP postgraduate training programs.1 When researching these programs, the overwhelming majority we surveyed described themselves as fellowships. Because of this, we chose to use the same nomenclature. The survey we used was meant to explore and quantify certain discreet components of program creation and execution, and further study would be needed to shed light on how they name themselves.
While it is not known if the term “fellowship” in this context would be confusing to patients, it does seem that the ideal terminology has not yet been clarified. In 2014, the American Association of Nurse Practitioners released a position statement that, for NP postgraduate training programs, the term “fellowship” should be used above other terms.2 We were unable to find a similar position statement regarding postgraduate physician assistant training, but did note that the Association of Post-Graduate PA Programs website uses the terms “residency” and “fellowship” seemingly interchangeably.3 As most of the programs that we surveyed train mixed groups of nurse practitioners and physician assistants, developing unified language will be an important step in the future.
1. Rauch D. Be Careful What We Call it. J Hosp Med. 2019;15(1):64. https://doi.org/10.12788/jhm.3297.
2. AANP and the NP Roundtable Joint Statements (2014). Nurse Practitioner Perspective on Education a nd Post-Graduate Training. [online] Available at: https://storage.aanp.org/www/documents/advocacy/nproundtablestatementmay6th.pdf Accessed August 27, 2019.
3. Home - APPAP. APPAP. https://appap.org. Published 2019. Accessed August 27, 2019.
1. Rauch D. Be Careful What We Call it. J Hosp Med. 2019;15(1):64. https://doi.org/10.12788/jhm.3297.
2. AANP and the NP Roundtable Joint Statements (2014). Nurse Practitioner Perspective on Education a nd Post-Graduate Training. [online] Available at: https://storage.aanp.org/www/documents/advocacy/nproundtablestatementmay6th.pdf Accessed August 27, 2019.
3. Home - APPAP. APPAP. https://appap.org. Published 2019. Accessed August 27, 2019.
© 2020 Society of Hospital Medicine
In Reference to: “The Current State of Advanced Practice Provider Fellowships in Hospital Medicine: A Survey of Program Directors.” Be Careful What We Call It
I read with interest the recent article by Klimpl et al. “The Current State of Advanced Practice provider Fellowships in Hospital Medicine: A Survey of Program Directors.”1 I appreciate the description of the variation in training as well as the discussion points about the driving forces behind
1. Klimpl D, Franco T, Tackett S, Cardin TE, Wolfe B, Wright S, Kisuule F. The current state of advanced practice provider fellowships in hospital medicine: a survey of program directors. J Hosp Med. 2019;14(7):401-406. https://doi.org/10.12788/jhm.3191.
I read with interest the recent article by Klimpl et al. “The Current State of Advanced Practice provider Fellowships in Hospital Medicine: A Survey of Program Directors.”1 I appreciate the description of the variation in training as well as the discussion points about the driving forces behind
I read with interest the recent article by Klimpl et al. “The Current State of Advanced Practice provider Fellowships in Hospital Medicine: A Survey of Program Directors.”1 I appreciate the description of the variation in training as well as the discussion points about the driving forces behind
1. Klimpl D, Franco T, Tackett S, Cardin TE, Wolfe B, Wright S, Kisuule F. The current state of advanced practice provider fellowships in hospital medicine: a survey of program directors. J Hosp Med. 2019;14(7):401-406. https://doi.org/10.12788/jhm.3191.
1. Klimpl D, Franco T, Tackett S, Cardin TE, Wolfe B, Wright S, Kisuule F. The current state of advanced practice provider fellowships in hospital medicine: a survey of program directors. J Hosp Med. 2019;14(7):401-406. https://doi.org/10.12788/jhm.3191.
© 2020 Society of Hospital Medicine