User login
A Pain He Can’t Walk Off
ANSWER
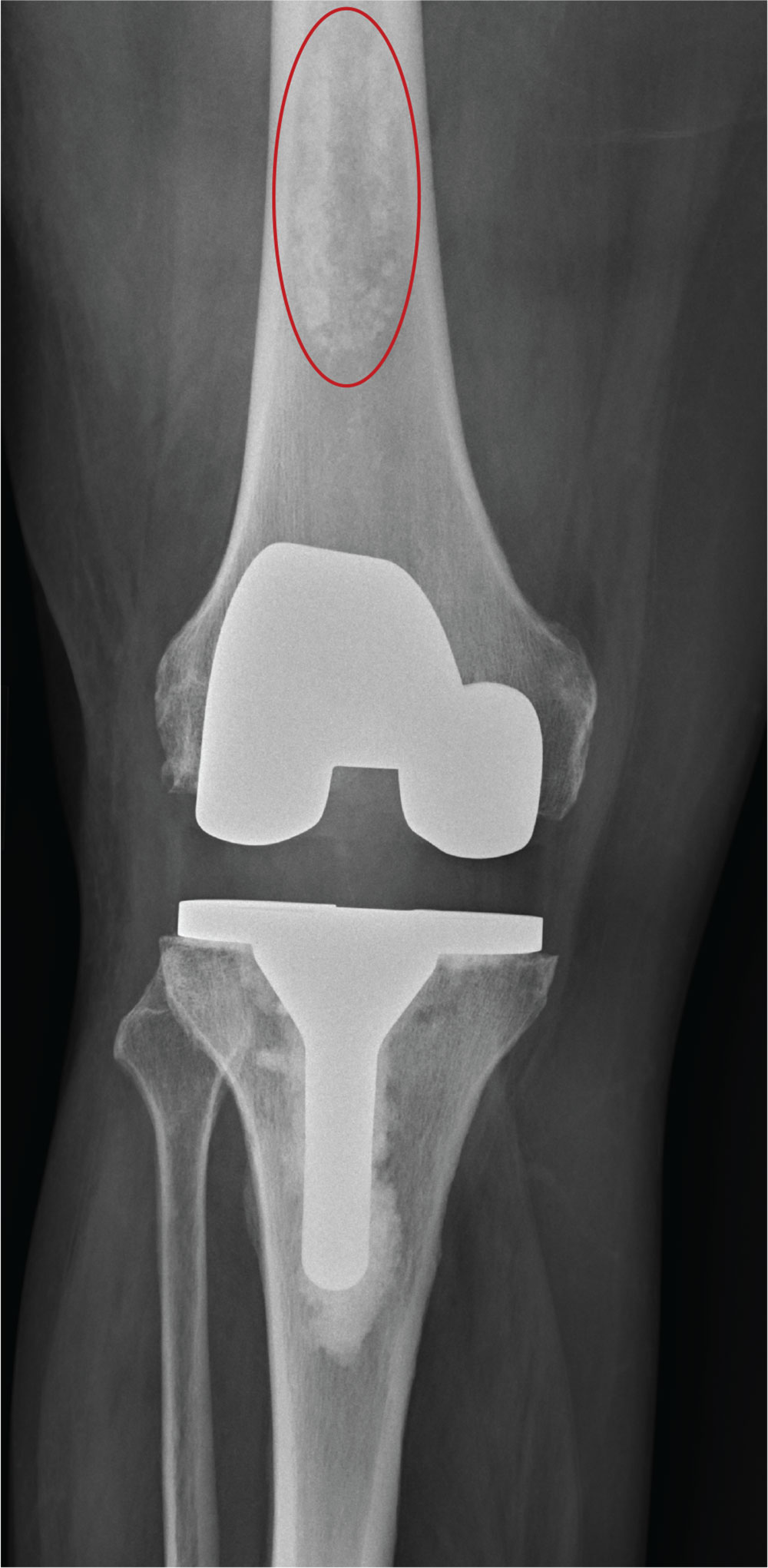
The radiograph shows a right knee prosthesis in place with no evidence of failure or displacement. Of note, there is a hyperdense, somewhat elongated lesion along the distal third of the femur. Radiographically, this is most likely consistent with an enchondroma. Enchondromas are typically benign bone lesions that originate from cartilage. They
The patient was referred to his orthopedist for follow-up.
ANSWER
The radiograph shows a right knee prosthesis in place with no evidence of failure or displacement. Of note, there is a hyperdense, somewhat elongated lesion along the distal third of the femur. Radiographically, this is most likely consistent with an enchondroma. Enchondromas are typically benign bone lesions that originate from cartilage. They
The patient was referred to his orthopedist for follow-up.
ANSWER
The radiograph shows a right knee prosthesis in place with no evidence of failure or displacement. Of note, there is a hyperdense, somewhat elongated lesion along the distal third of the femur. Radiographically, this is most likely consistent with an enchondroma. Enchondromas are typically benign bone lesions that originate from cartilage. They
The patient was referred to his orthopedist for follow-up.
A 70-year-old man presents to the urgent care clinic for evaluation of right knee pain. He denies any specific injury or trauma. For the past several months, he says, he has had a “deep aching pain” that is exacerbated by walking and weight bearing.
His medical history is significant for mild hypertension and diabetes. His surgical history is significant for remote right total knee arthroplasty.
On examination, you note an elderly male in no obvious distress. His vital signs are normal. Inspection of the right knee shows a well-healed incision with no obvious effusion or erythema. He demonstrates a fairly good active range of motion. There is no evidence of ligament laxity.
You obtain a radiograph of the knee (shown). What is your impression?
The Unintended Off-road Experience
ANSWER
A moderate amount of soft-tissue swelling is evident. There is also a fracture of the distal radius and an avulsion fracture of the triquetrum. The latter is the second most commonly fractured carpal bone after the scaphoid. Triquetral fractures usually result from a hyperflexion injury.
The patient’s wrist was immobilized in a splint, and referral to a hand surgeon was coordinated.
ANSWER
A moderate amount of soft-tissue swelling is evident. There is also a fracture of the distal radius and an avulsion fracture of the triquetrum. The latter is the second most commonly fractured carpal bone after the scaphoid. Triquetral fractures usually result from a hyperflexion injury.
The patient’s wrist was immobilized in a splint, and referral to a hand surgeon was coordinated.
ANSWER
A moderate amount of soft-tissue swelling is evident. There is also a fracture of the distal radius and an avulsion fracture of the triquetrum. The latter is the second most commonly fractured carpal bone after the scaphoid. Triquetral fractures usually result from a hyperflexion injury.
The patient’s wrist was immobilized in a splint, and referral to a hand surgeon was coordinated.
A 70-year-old woman is brought to the emergency department by EMS after being involved in a motor vehicle collision. She was a restrained driver in a vehicle that was hit by a tractor-trailer, causing her vehicle to go off the road and hit the guardrail. She does not recall if the airbag deployed, and she believes she momentarily lost consciousness. She is complaining of pain in the head and the right wrist.
Her medical history is significant for mild (controlled) hypertension. Primary survey reveals an elderly female who is awake, alert, and oriented and in mild distress. Her vital signs are stable.
The patient has a small laceration on her face. Her right wrist is moderately swollen, and she has decreased range of motion. There is also moderate tenderness to palpation. Pulses are good, as is capillary refill time in the fingernail bed.
Radiograph of the right wrist is obtained (oblique view shown). What is your impression?
There’s No Patellin’ What Happened
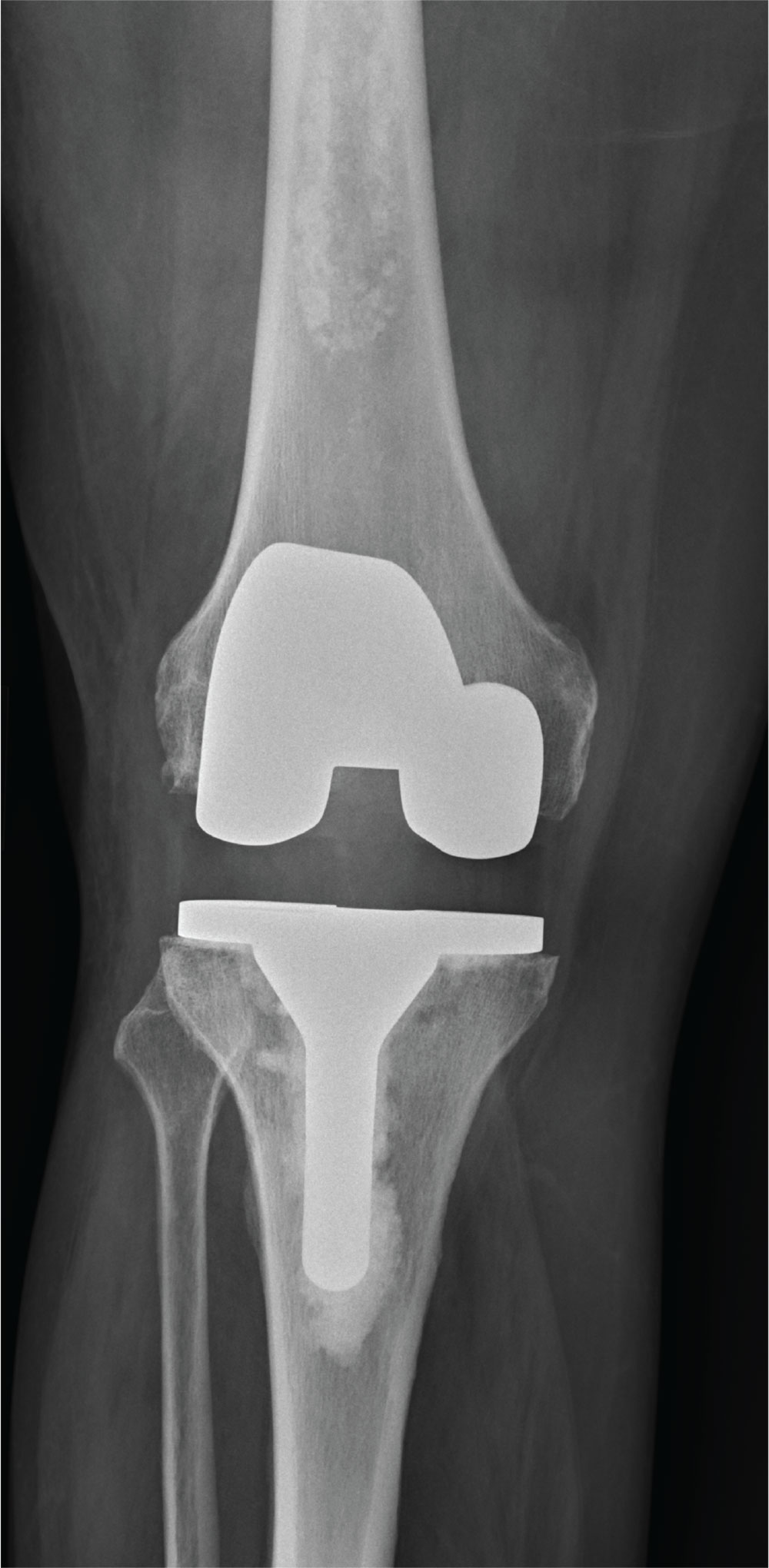
ANSWER
The radiograph demonstrates an abnormal-appearing patella; there is a longitudinal lucency along the lateral portion. There is some mild soft-tissue swelling but no evidence of a definite joint effusion. The lucency could represent a fracture, especially in the setting of trauma. The other possibility is that the patient has a bipartite patella. This is a rare congenital condition in which the patella does not completely fuse; it remains two separate bones. CT of the knee for further evaluation, as well as orthopedic consultation, were ordered.
ANSWER
The radiograph demonstrates an abnormal-appearing patella; there is a longitudinal lucency along the lateral portion. There is some mild soft-tissue swelling but no evidence of a definite joint effusion. The lucency could represent a fracture, especially in the setting of trauma. The other possibility is that the patient has a bipartite patella. This is a rare congenital condition in which the patella does not completely fuse; it remains two separate bones. CT of the knee for further evaluation, as well as orthopedic consultation, were ordered.
ANSWER
The radiograph demonstrates an abnormal-appearing patella; there is a longitudinal lucency along the lateral portion. There is some mild soft-tissue swelling but no evidence of a definite joint effusion. The lucency could represent a fracture, especially in the setting of trauma. The other possibility is that the patient has a bipartite patella. This is a rare congenital condition in which the patella does not completely fuse; it remains two separate bones. CT of the knee for further evaluation, as well as orthopedic consultation, were ordered.
A 30-year-old man is transported by ambulance to your emergency department from the scene of a motor vehicle collision. He was a restrained driver who lost control of his vehicle and hit the back of a tractor-trailer. His airbag deployed, and he thinks he had a brief loss of consciousness. He complains of pain in his neck, right-side chest wall, and right knee.
He denies any significant medical history and takes no medications regularly. He reports smoking a half-pack of cigarettes per day and consuming alcohol socially; he denies drinking this evening.
Primary survey shows a male in no obvious distress who is currently awake, alert, and oriented. His Glasgow Coma Scale score is 15. Primary exam is stable except for some neck pain and right-side rib pain.
During secondary survey, examination of his right knee shows a superficial laceration with controlled bleeding. No significant swelling is present. The patient does have decreased range of motion secondary to a moderate amount of pain. Distal pulses are present, and there is no neurovascular compromise.
You obtain a portable radiograph of the knee (shown). What is your impression?
Taking a Stab in the Dark
ANSWER
The radiograph shows an obvious metallic foreign body that appears to be lodged within the first and second lumbar disc space. This is likely the tip of the knife, which presumably broke off when the patient was stabbed.
The patient was promptly transferred to a trauma center with neurosurgery coverage. Subsequent CT showed that the blade had penetrated the spinal canal, but remarkably, the patient remained neurologically intact. He underwent successful removal without any neurologic compromise.
This case highlights several points for clinicians: First, provider-to-provider sign-out of patients should be complete and detailed. Second, obtaining a thorough history is essential. And third, you should maintain a low threshold for obtaining radiographs of wounds, to rule out a foreign body.
ANSWER
The radiograph shows an obvious metallic foreign body that appears to be lodged within the first and second lumbar disc space. This is likely the tip of the knife, which presumably broke off when the patient was stabbed.
The patient was promptly transferred to a trauma center with neurosurgery coverage. Subsequent CT showed that the blade had penetrated the spinal canal, but remarkably, the patient remained neurologically intact. He underwent successful removal without any neurologic compromise.
This case highlights several points for clinicians: First, provider-to-provider sign-out of patients should be complete and detailed. Second, obtaining a thorough history is essential. And third, you should maintain a low threshold for obtaining radiographs of wounds, to rule out a foreign body.
ANSWER
The radiograph shows an obvious metallic foreign body that appears to be lodged within the first and second lumbar disc space. This is likely the tip of the knife, which presumably broke off when the patient was stabbed.
The patient was promptly transferred to a trauma center with neurosurgery coverage. Subsequent CT showed that the blade had penetrated the spinal canal, but remarkably, the patient remained neurologically intact. He underwent successful removal without any neurologic compromise.
This case highlights several points for clinicians: First, provider-to-provider sign-out of patients should be complete and detailed. Second, obtaining a thorough history is essential. And third, you should maintain a low threshold for obtaining radiographs of wounds, to rule out a foreign body.
As you arrive for your shift in the emergency department, the outgoing provider asks if you would mind checking a laceration that his student is stapling. “The discharge paperwork is all done,” he says, as he waves goodbye and walks out the door.
You find that the student has just about completed his task: sterilely stapling a 2.5-cm laceration on the left lumbar area of a man in his early 40s.
You ask the student for the basic history, and he informs you that the patient was drinking with friends and “accidentally got cut” when they started roughhousing. You turn your attention to the patient, who appears intoxicated but in no obvious distress; he confirms the story as presented.
A quick review of the chart shows no significant medial history, stable vital signs, and up-to-date tetanus status. The patient can move all extremities well and appears neurovascularly intact. But some instinct prompts you to probe further.
On additional questioning, the patient reveals that he was accidentally stabbed. When you inquire about the object he was stabbed with, he describes it as a knife, “pretty long, sort of like a dagger.”
With this information, you decide to order some laboratory studies and abdominal radiographs (lateral view shown). What is your impression?
Everything’s Fine … Except His Spine
ANSWER
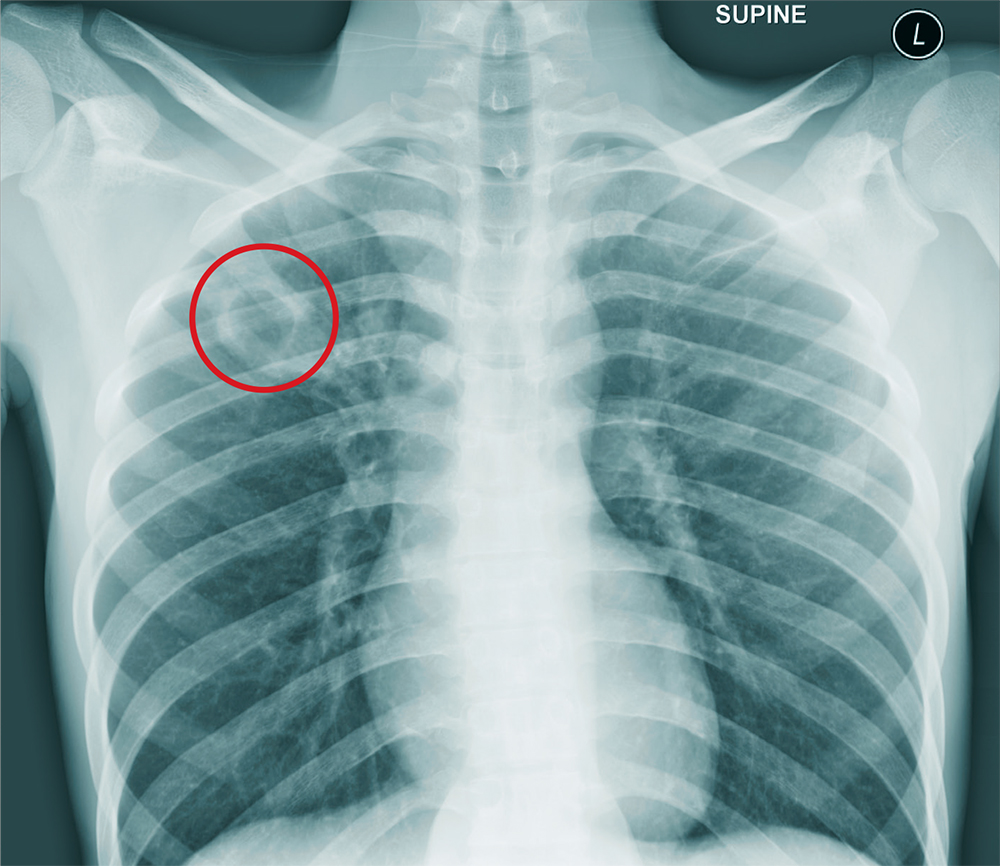
The chest radiograph shows an approximately 3-cm cavitary lesion in the right upper lobe. Such a lesion can indicate lung abscess, neoplasm, or tuberculosis.
Subsequent workup determined that he did, in fact, have tuberculosis, with involvement in his spine (known as Pott disease).
ANSWER
The chest radiograph shows an approximately 3-cm cavitary lesion in the right upper lobe. Such a lesion can indicate lung abscess, neoplasm, or tuberculosis.
Subsequent workup determined that he did, in fact, have tuberculosis, with involvement in his spine (known as Pott disease).
ANSWER
The chest radiograph shows an approximately 3-cm cavitary lesion in the right upper lobe. Such a lesion can indicate lung abscess, neoplasm, or tuberculosis.
Subsequent workup determined that he did, in fact, have tuberculosis, with involvement in his spine (known as Pott disease).
A 25-year-old man is admitted to your facility for a possible infection in his spine. He reports a two-week history of severe back pain with no history of injury or trauma. Imaging performed at an outside facility suggested compression and erosion of his vertebral bodies at the thoracolumbar junction, and the radiologist raised concern for possible osteomyelitis and diskitis.
The patient is otherwise healthy and denies any medical problems. He denies drug use of any form. Review of systems is significant for a three-month history of anorexia and night sweats but no fever.
Physical exam reveals a healthy-appearing male with normal vital signs. His heart and lung sounds are normal.
A chest radiograph is obtained (shown). What is your impression?
The Pop That Stopped the Soccer Game
ANSWER
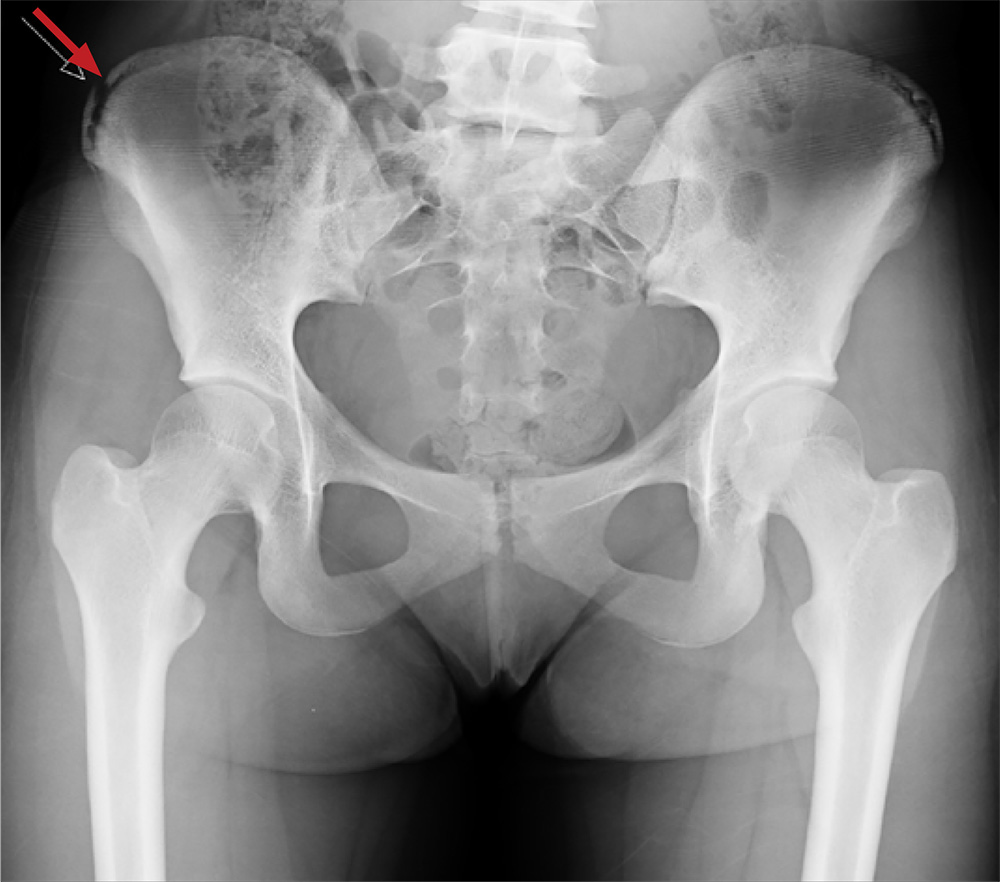
The radiograph shows an avulsion fracture of the right iliac crest. While the patient does have a growth plate in this location, there is asymmetry between the right and left sides.
Pelvic avulsion fractures can be easy to overlook and are often misdiagnosed as strains. Providers must remember that the pelvis serves as an insertion site for multiple muscles; in both adolescent and adult patients, certain activities (eg, sprinting, jumping, kicking) can increase tension and result in a bone avulsion. Affected patients typically report a popping sensation, pain with range of motion, and point tenderness over the fracture.
Avulsion fractures can usually be identified on x-ray; CT and MRI are used only when definitive diagnosis is unclear. Treatment consists of conservative management—rest, protected weight bearing, and physical therapy. Surgery is typically reserved for those with > 2 cm displacement of the fracture fragment.
In athletes, a gradual return to sports is advised, with full participation at four to 12 weeks postinjury. Possible complications include recurrent symptoms, prolonged healing time, nonunion, malunion, or hip weakness.
This patient was placed on crutches with non-weight-bearing status for one week. She used OTC pain medication as needed. The patient completed a four-week course of physical therapy and returned to full weight-bearing status. After six weeks, the patient had returned to full activity with pain-free range of motion and full strength.
ANSWER
The radiograph shows an avulsion fracture of the right iliac crest. While the patient does have a growth plate in this location, there is asymmetry between the right and left sides.
Pelvic avulsion fractures can be easy to overlook and are often misdiagnosed as strains. Providers must remember that the pelvis serves as an insertion site for multiple muscles; in both adolescent and adult patients, certain activities (eg, sprinting, jumping, kicking) can increase tension and result in a bone avulsion. Affected patients typically report a popping sensation, pain with range of motion, and point tenderness over the fracture.
Avulsion fractures can usually be identified on x-ray; CT and MRI are used only when definitive diagnosis is unclear. Treatment consists of conservative management—rest, protected weight bearing, and physical therapy. Surgery is typically reserved for those with > 2 cm displacement of the fracture fragment.
In athletes, a gradual return to sports is advised, with full participation at four to 12 weeks postinjury. Possible complications include recurrent symptoms, prolonged healing time, nonunion, malunion, or hip weakness.
This patient was placed on crutches with non-weight-bearing status for one week. She used OTC pain medication as needed. The patient completed a four-week course of physical therapy and returned to full weight-bearing status. After six weeks, the patient had returned to full activity with pain-free range of motion and full strength.
ANSWER
The radiograph shows an avulsion fracture of the right iliac crest. While the patient does have a growth plate in this location, there is asymmetry between the right and left sides.
Pelvic avulsion fractures can be easy to overlook and are often misdiagnosed as strains. Providers must remember that the pelvis serves as an insertion site for multiple muscles; in both adolescent and adult patients, certain activities (eg, sprinting, jumping, kicking) can increase tension and result in a bone avulsion. Affected patients typically report a popping sensation, pain with range of motion, and point tenderness over the fracture.
Avulsion fractures can usually be identified on x-ray; CT and MRI are used only when definitive diagnosis is unclear. Treatment consists of conservative management—rest, protected weight bearing, and physical therapy. Surgery is typically reserved for those with > 2 cm displacement of the fracture fragment.
In athletes, a gradual return to sports is advised, with full participation at four to 12 weeks postinjury. Possible complications include recurrent symptoms, prolonged healing time, nonunion, malunion, or hip weakness.
This patient was placed on crutches with non-weight-bearing status for one week. She used OTC pain medication as needed. The patient completed a four-week course of physical therapy and returned to full weight-bearing status. After six weeks, the patient had returned to full activity with pain-free range of motion and full strength.
A 13-year-old girl presents with her mother for evaluation of right hip pain following a soccer game two days ago. The patient says she felt a “pop” in her right hip while running and kicking the ball. She was escorted off the field, unable to finish the game.
Since then, she has had pain over the right superior pelvic region. She rates the pain as a 1/10 at rest but 7/10 with ambulation. She is unwilling to bear weight secondary to discomfort and has been using crutches provided by her trainer. She has been using ice and ibuprofen without relief. Her medical history is unremarkable.
On physical exam, you note a well-developed, well-nourished female in no acute distress. No ecchymosis, erythema, or abrasions can be seen on skin exam. The patient has point tenderness over the right iliac crest. She has mild pain and weakness with hip flexion and significant pain with abduction. The extremity is neurovascularly intact.
A pelvic radiograph is obtained. What is your impression?
Thrown Off Track
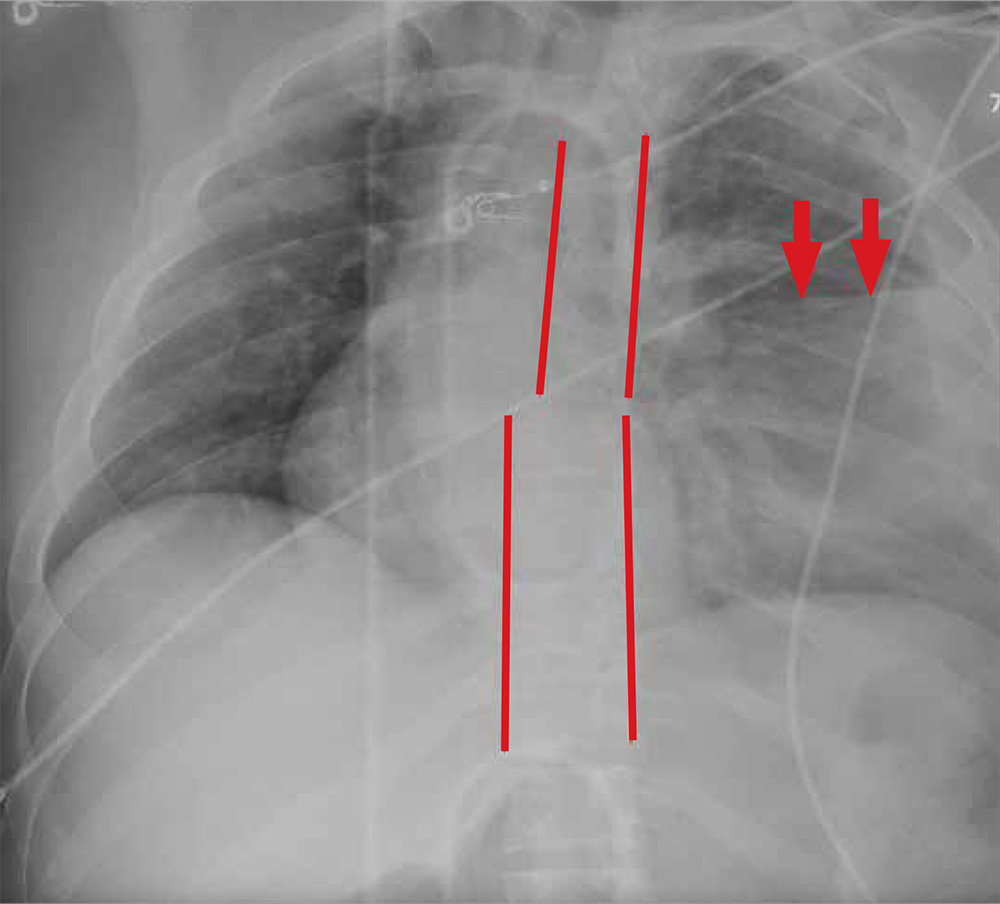
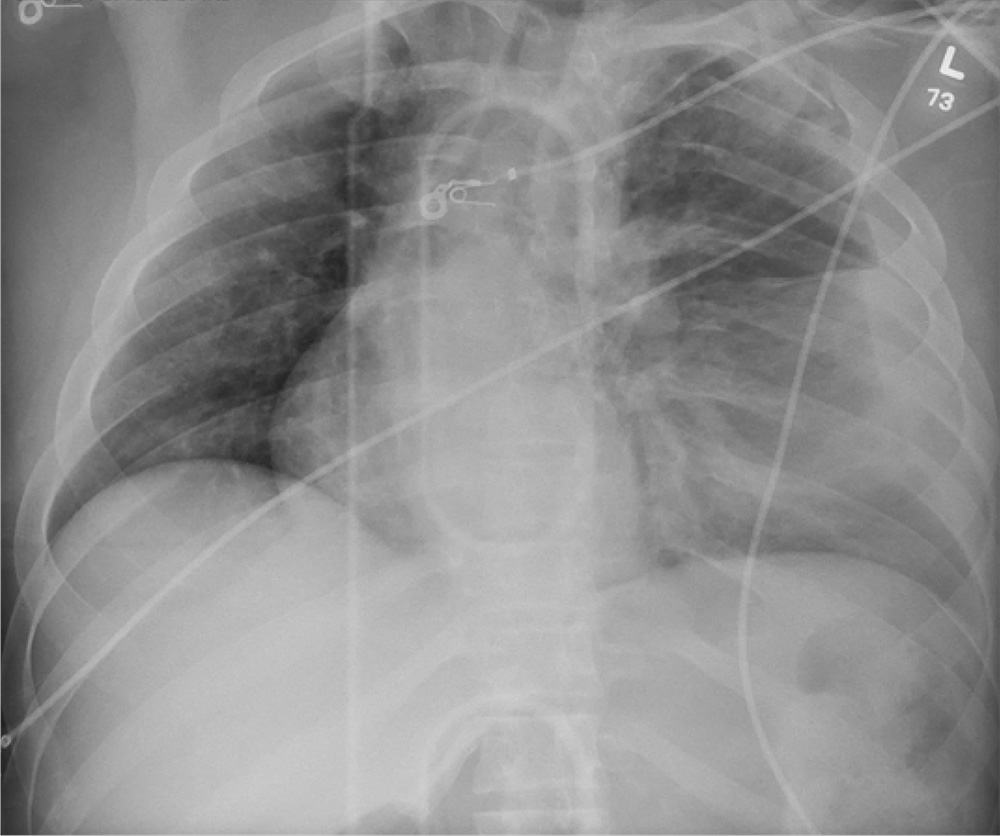
ANSWER
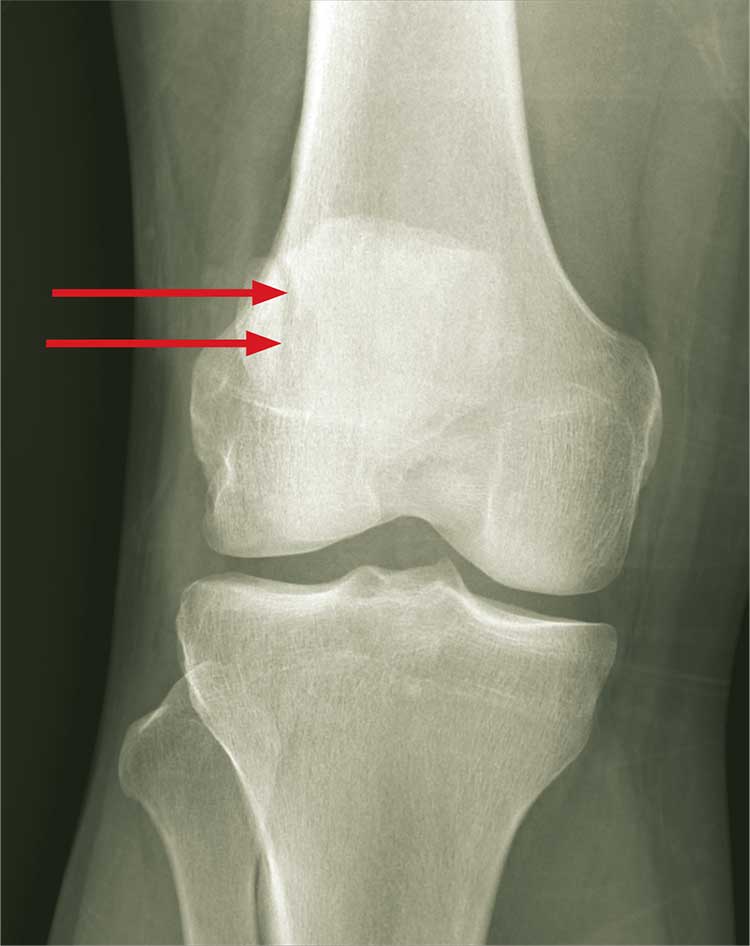
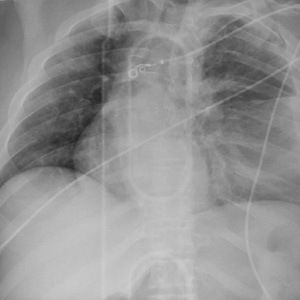
The radiograph shows rib fractures on the left side (arrows); on the same side, there is a moderate-sized pleural effusion—presumably a hemothorax from the trauma.
A closer look at the mid-thoracic spine reveals some irregularity and possible deformity—note the slight offset. This finding is strongly suspicious for a fracture.
A subsequent CT revealed a thoracic burst fracture with retropulsion into the spinal canal.
ANSWER
The radiograph shows rib fractures on the left side (arrows); on the same side, there is a moderate-sized pleural effusion—presumably a hemothorax from the trauma.
A closer look at the mid-thoracic spine reveals some irregularity and possible deformity—note the slight offset. This finding is strongly suspicious for a fracture.
A subsequent CT revealed a thoracic burst fracture with retropulsion into the spinal canal.
ANSWER
The radiograph shows rib fractures on the left side (arrows); on the same side, there is a moderate-sized pleural effusion—presumably a hemothorax from the trauma.
A closer look at the mid-thoracic spine reveals some irregularity and possible deformity—note the slight offset. This finding is strongly suspicious for a fracture.
A subsequent CT revealed a thoracic burst fracture with retropulsion into the spinal canal.
A 20-year-old man is riding a four-wheel all-terrain vehicle at a high rate of speed when he loses control and is thrown off. He is not wearin
As you begin your primary survey, you note a young male who is anxious but awake and able to converse. He is receiving 100% oxygen via a non-rebreather mask. His heart rate is 130 beats/min and his blood pressure, 80/40 mm Hg. Breath sounds are somewhat decreased on the left side. The patient can move both arms, and his strength is normal. However, he is insensate from his mid-chest down and is unable to move his legs at all.
Portable radiographs are obtained, including a chest radiograph (shown). What is your impression?
Getting Ahead of the Pain
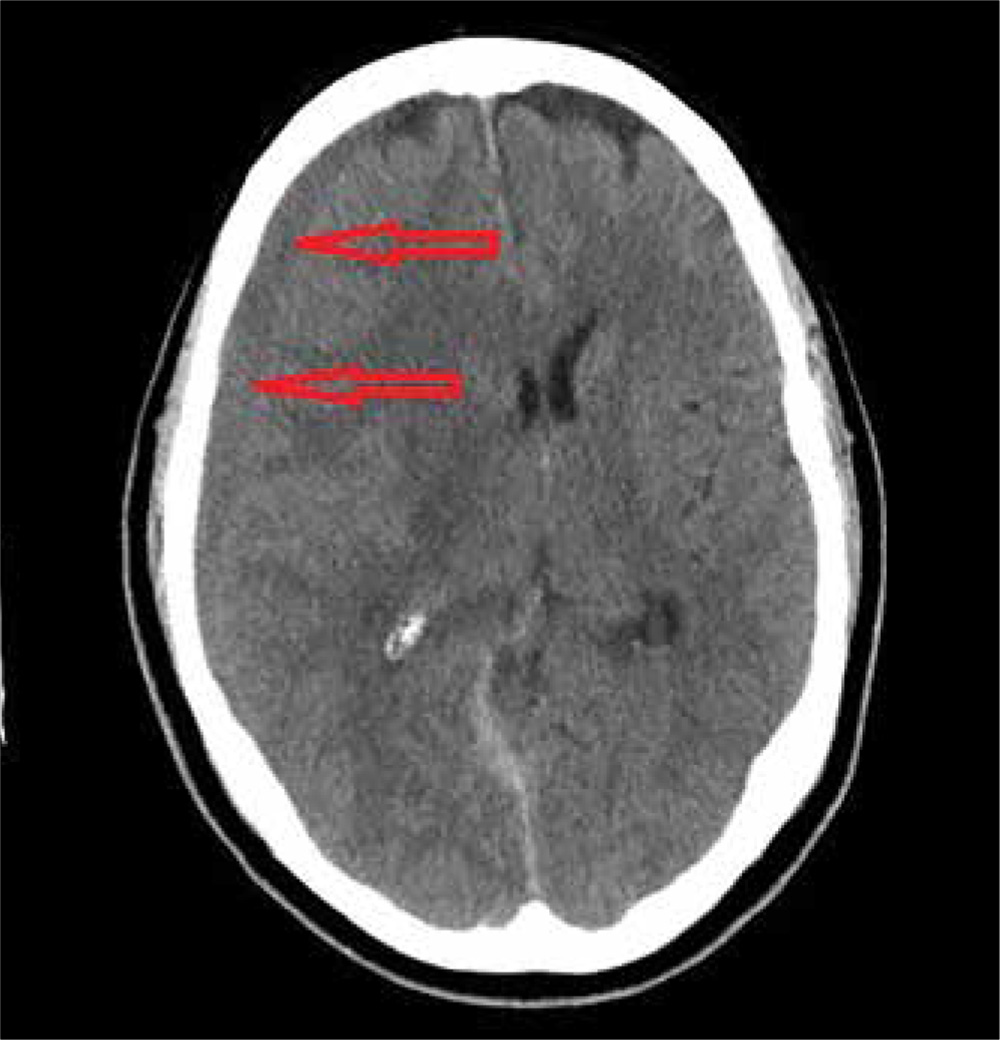
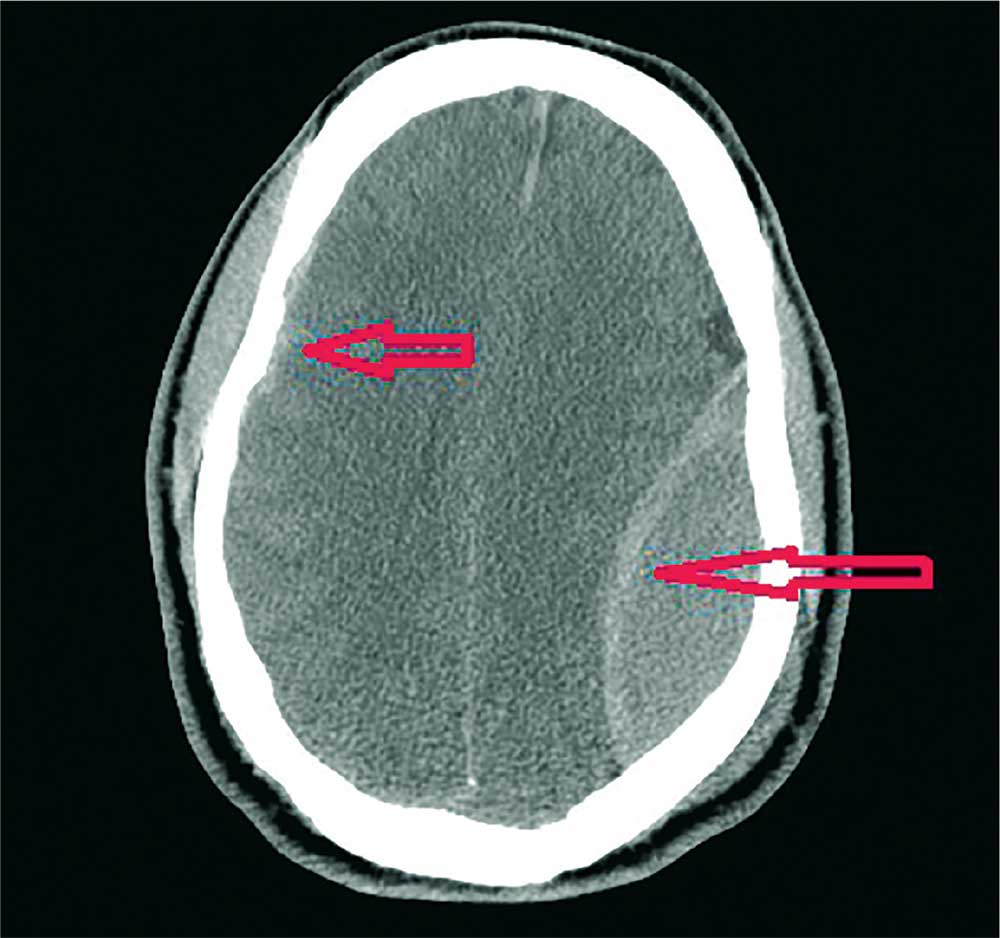
ANSWER
The image reveals a hypodense extra-axial fluid collection in the right frontoparietal region, measuring 8 to 10 mm in diameter. There is some mass effect and evidence of right-to-left shift. These findings are consistent with a subacute subdural hematoma, possibly secondary to the patient’s anticoagulant use. (The patient later recalled bumping his head a couple of months prior—but that may have been incidental.)
Arrangements were made for him at a local hospital where neurosurgical services were available. He underwent successful evacuation and was subsequently symptom free.
ANSWER
The image reveals a hypodense extra-axial fluid collection in the right frontoparietal region, measuring 8 to 10 mm in diameter. There is some mass effect and evidence of right-to-left shift. These findings are consistent with a subacute subdural hematoma, possibly secondary to the patient’s anticoagulant use. (The patient later recalled bumping his head a couple of months prior—but that may have been incidental.)
Arrangements were made for him at a local hospital where neurosurgical services were available. He underwent successful evacuation and was subsequently symptom free.
ANSWER
The image reveals a hypodense extra-axial fluid collection in the right frontoparietal region, measuring 8 to 10 mm in diameter. There is some mass effect and evidence of right-to-left shift. These findings are consistent with a subacute subdural hematoma, possibly secondary to the patient’s anticoagulant use. (The patient later recalled bumping his head a couple of months prior—but that may have been incidental.)
Arrangements were made for him at a local hospital where neurosurgical services were available. He underwent successful evacuation and was subsequently symptom free.
An 80-year-old man presents to urgent care for intermittent severe headaches. The pain is reportedly bifrontal, slightly worse on the right side than the left. He denies any recent injury or trauma, as well as symptoms including fever, chills, nausea, vomiting, and visual disturbance.
His medical history is significant for hypertension and hyperlipidemia. His current medications include prasugrel and aspirin.
On examination, you note an elderly male who is awake, alert, and oriented x 3. His vital signs are normal. His physical exam is overall normal, with no focal findings or neurologic deficits.
Noncontrast CT of the head is obtained at a local hospital. As you review the images, you see the following cut (shown). What is your impression?
All-Terrain, No Control
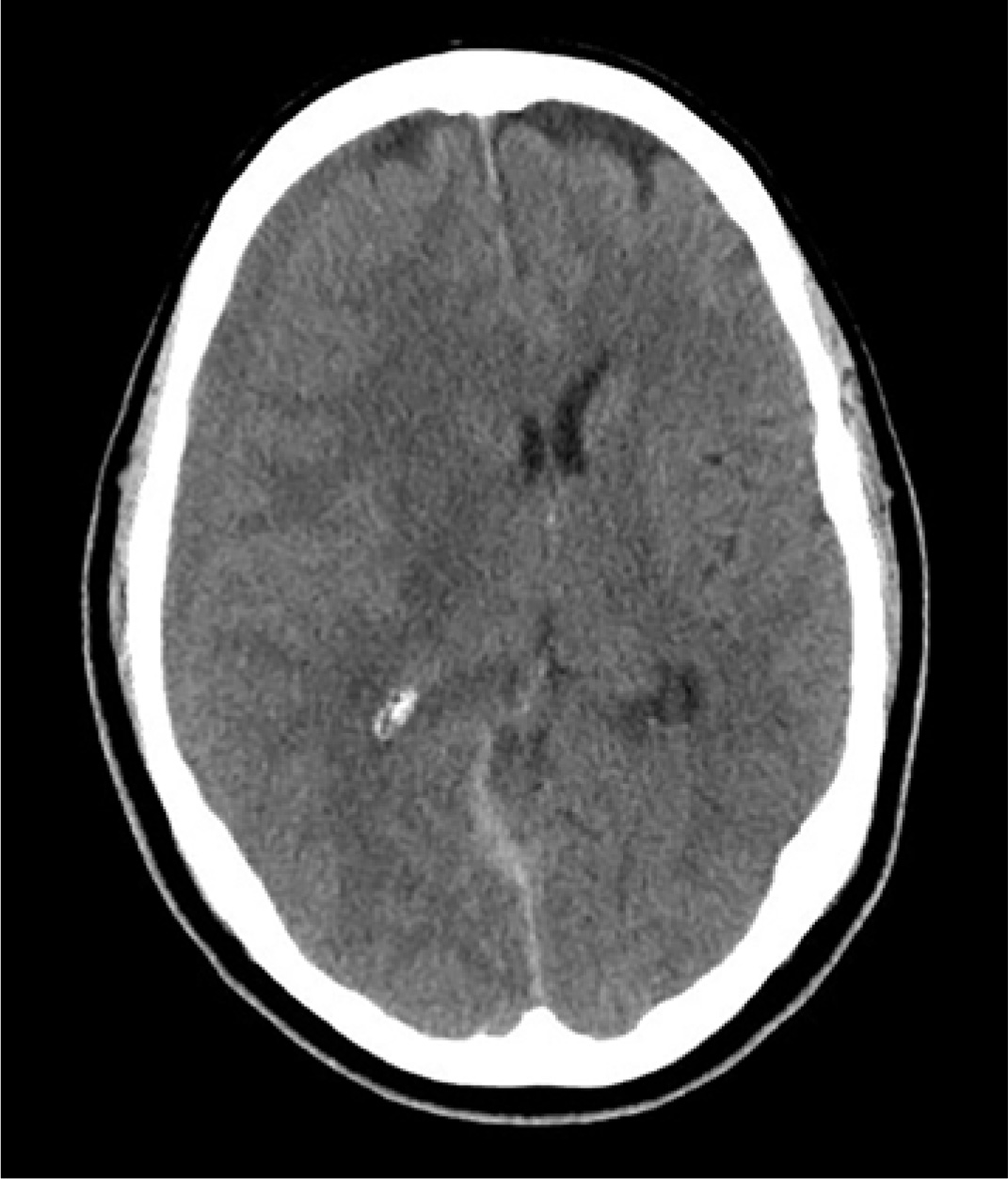
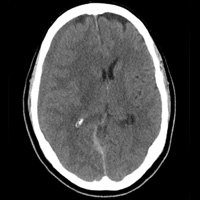
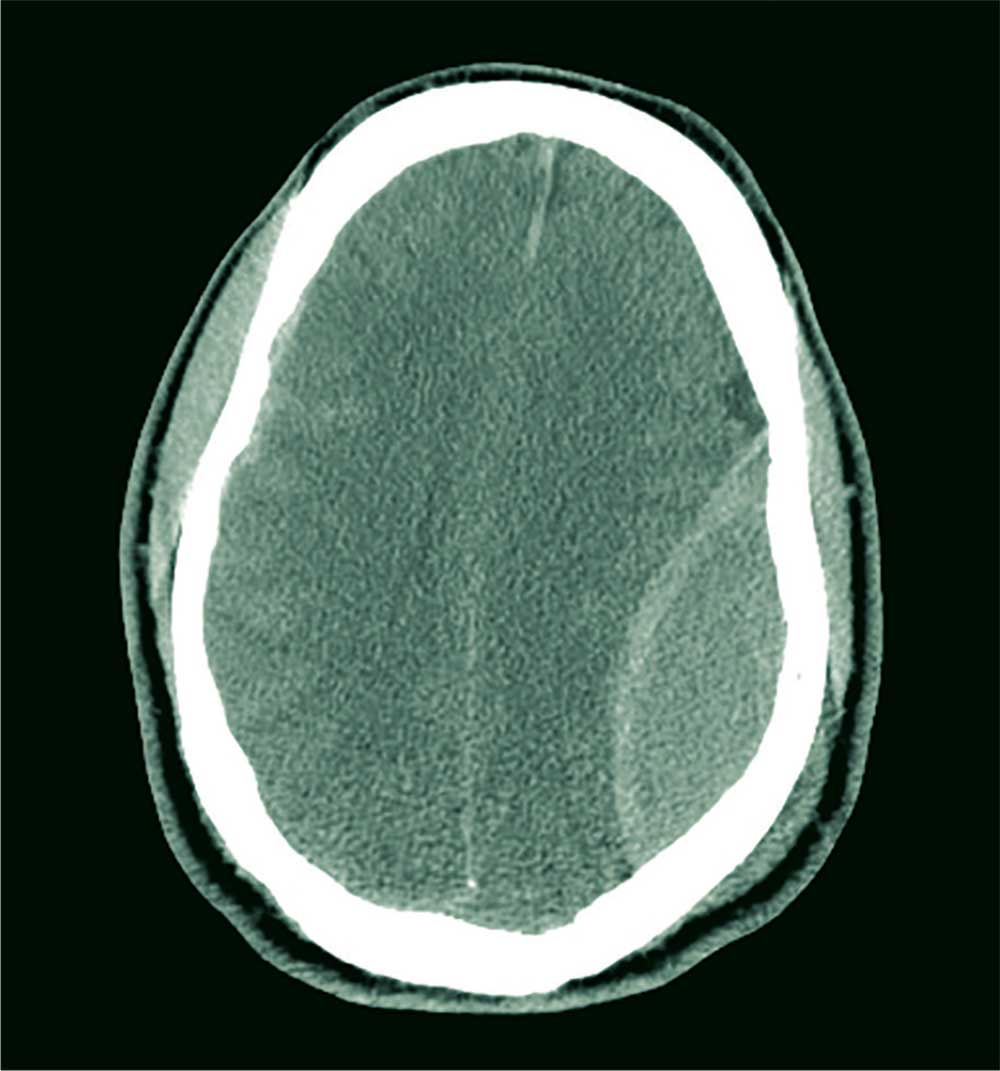
ANSWER
The image shows a large, convex hyperdensity within the left parietal region. This is a textbook image of an acute epidural hematoma. There is considerable mass effect and evidence of left-to-right shift. Windowing shows an underlying fracture, which is typically associated with these types of hemorrhages.
There is also evidence of a right-side concave hyperdensity, consistent with an acute subdural hematoma. Typically, this is referred to as a contrecoup injury.
The patient was transported to the operating room for an emergent left craniotomy for epidural evacuation; he recovered uneventfully.
ANSWER
The image shows a large, convex hyperdensity within the left parietal region. This is a textbook image of an acute epidural hematoma. There is considerable mass effect and evidence of left-to-right shift. Windowing shows an underlying fracture, which is typically associated with these types of hemorrhages.
There is also evidence of a right-side concave hyperdensity, consistent with an acute subdural hematoma. Typically, this is referred to as a contrecoup injury.
The patient was transported to the operating room for an emergent left craniotomy for epidural evacuation; he recovered uneventfully.
ANSWER
The image shows a large, convex hyperdensity within the left parietal region. This is a textbook image of an acute epidural hematoma. There is considerable mass effect and evidence of left-to-right shift. Windowing shows an underlying fracture, which is typically associated with these types of hemorrhages.
There is also evidence of a right-side concave hyperdensity, consistent with an acute subdural hematoma. Typically, this is referred to as a contrecoup injury.
The patient was transported to the operating room for an emergent left craniotomy for epidural evacuation; he recovered uneventfully.
A 40-year-old man is brought to the emergency department (ED) with a suspected intracranial hemorrhage after being thrown off an all-terrain vehicle. He was reportedly riding the vehicle without a helmet when he somehow lost control; the accident itself was unwitnessed.
En route to the ED, he was reportedly confused but hemodynamically stable, with a Glasgow Coma Scale score of 13-14. He lost consciousness while in the CT scanner, requiring emergent intubation for airway protection.
When you arrive to assess him, you note an intubated male with stable vital signs. The pupils display slight anisocoria but equally react. The patient withdraws in all four extremities secondary to pain, with slight posturing.
Noncontrast CT of the head is obtained, a static image from which is shown. What is your impression?
From Local Bar to Police Car
ANSWER
The radiograph demonstrates no acute injury to the wrist. There is, however, a subtle nondisplaced fracture of the distal fifth metacarpal joint. The patient was given a wrist splint for symptomatic relief, and orthopedic follow-up was coordinated.
ANSWER
The radiograph demonstrates no acute injury to the wrist. There is, however, a subtle nondisplaced fracture of the distal fifth metacarpal joint. The patient was given a wrist splint for symptomatic relief, and orthopedic follow-up was coordinated.
ANSWER
The radiograph demonstrates no acute injury to the wrist. There is, however, a subtle nondisplaced fracture of the distal fifth metacarpal joint. The patient was given a wrist splint for symptomatic relief, and orthopedic follow-up was coordinated.
A 31-year-old man is brought to your facility by local law enforcement for evaluation of left wrist pain following an altercation. The patient was reportedly at a local bar; as he was leaving, he started arguing with some other patrons. A fight ensued.
The patient believes he was struck by something on his left wrist. He denies any other injuries or complaints. His medical history is unremarkable, and vital signs are stable.
Physical examination of his left wrist shows no obvious deformity. There is some mild swelling over the dorsal aspect of his wrist. Range of motion is painful and limited. Good capillary refill is noted in the fingers, and sensation is intact. Good pulses are present.
Radiograph of the left wrist is obtained. What is your impression?