User login
Reforming prior authorization remains AGA’s top policy priority
Reforming prior authorization polices to reduce red tape for physicians and help patients get the care they need in a timely manner is the AGA’s number one policy priority as it impacts every gastroenterologist regardless of practice setting. We have seen an increase in prior authorization policies from every major insurer. The most recent prior authorization program to impact gastroenterologists was announced by UnitedHealthcare (UHC) in March for implementation on June 1, 2023 and will require prior authorization for most colonoscopy and upper GI endoscopy procedures with the exception of screening colonoscopy.1 This policy is a step back at a time when payers should be developing innovative policies in collaboration with health care providers to improve patient care.
UHC’s GI prior authorization policy
AGA met with UHC in March to discuss their plan to require prior authorization for most GI endoscopy procedures. We stressed how this change will cause care delays for high-risk individuals, deter patients from undergoing medically recommended procedures, exacerbate existing sociodemographic disparities in care and outcomes, and add unnecessary paperwork burden to physicians who have mounting rates of burnout.
Linda Lee, MD, medical director of endoscopy at Brigham and Women’s Hospital, Boston, recently spoke of the impact this policy will have on gastroenterologists and their patients. “We all know that requiring prior authorizations really only leads to more bureaucracy within the insurance company, as well as within each health care provider’s practice, because we need people to fill out these prior authorization forms, waste time trying to get through to their 1-800 number to speak with someone who has no clinical knowledge, then be told we need to speak with someone else who actually does have some medical knowledge about why these procedures are necessary.”
However, Dr. Lee stressed that “most importantly, this will lead to poorer patient care with delays in care as we are struggling to wade through the morass of prior authorization while patients are bleeding, not able to swallow, vomiting, and more while waiting for their insurance company to approve their potentially life-saving procedures.”
We were particularly troubled that UHC announced this policy during Colorectal Cancer Awareness Month, given the need to screen more Americans for colorectal cancer which remains the nation’s number two cancer killer. The UHC program would require a PA on surveillance colonoscopy for those patients who have previously had polyps removed and are at a higher risk for developing colorectal cancer.
“We know that patients with high-risk adenomas or advanced sessile serrated lesions have a higher risk of developing colorectal cancer and timely access to the necessary surveillance colonoscopy is critical,” said David Lieberman, MD, past president of the AGA and chair of the AGA Executive Committee on the Screening Continuum.
AGA plans to meet with UHC again to ask them to reconsider this policy, but we need your advocacy now to tell United how this will impact you and your patients.
How you can help stop UHC’s prior authorization program
Write to UHC: Tell UHC how this policy would impact you and your patients. Contact their CEO using our customizable letter2 that outlines the impact of United’s GI endoscopy prior authorization program on gastroenterologists and their patients available on the AGA Advocacy Action Center.
Use social media: Tag United (@UHC) on Twitter and tell them how this burdensome program will cause delays for high-risk individuals, deter patients from seeking treatment, and exacerbate existing disparities in care, all while saddling physicians with even more paperwork. Once you’ve tweeted, tag your colleagues and encourage them to get involved.
AGA is working to reform prior authorization
The AGA has supported federal legislation that would streamline prior authorization processes in Medicare Advantage (MA), the private insurance plans that contract with the Medicare program, given the explosion of these policies over the past several years. The Improving Seniors Timely Access to Care Act, bipartisan, bicameral legislation, would reduce prior authorization burdens by:
- Establishing an electronic prior authorization (ePA) program and require MA plans to adopt ePA capabilities.
- Requiring the Secretary of Health and Human Services to establish a list of items and services eligible for real-time decisions under an MA ePA program.
- Standardizing and streamlining the prior authorization process for routinely approved items and services.
- Ensuring prior authorization requests are reviewed by qualified medical personnel.
- Increasing transparency around MA prior authorization requirements and their use.
- Protecting beneficiaries from any disruptions in care due to prior authorization requirements as they transition between MA plans.
The Centers for Medicare & Medicaid Services (CMS) has also recognized the impact that prior authorization is having on physician wellness and how it is contributing to physician burnout. The agency recently proposed implementing many of the provisions that are outlined in the legislation, and AGA has expressed our support for moving forward with many of their proposals.
Earlier this year, Shivan Mehta, MD, MPH, met with CMS administrator Chiquita Brooks-LaSure and Surgeon General Vivek Murthy, MD, MBA, to express AGA’s support for prior authorization reform and discussed how it impacts how patients with chronic conditions like inflammatory bowel disease maintain continuity of care. He also stressed how prior authorization further exacerbates health inequities since it creates an additional barrier to care when barriers already exist.
AGA is taking a multi-pronged approach to advocating for prior authorization reform and reducing paperwork through legislative advocacy, regulatory advocacy with the CMS, and payer advocacy. We can’t do this alone. Join our AGA Advocacy Center3 and get involved in our AGA Congressional Advocates Program.4The authors have no conflicts to declare.
References
1. UnitedHealthcare (2023 Mar 01) New requirements for gastroenterology services.
2. American Gastroenterological Association (n.d.) AGA Advocacy Action Center. Tell United to Stop New Prior Auth Requirements!
3. American Gastroenterological Association (n.d.) AGA Advocacy Action Center. Advocacy & Policy. Get Involved.
4. American Gastroenterological Association (n.d.) AGA Congressional Advocates Program.
Reforming prior authorization polices to reduce red tape for physicians and help patients get the care they need in a timely manner is the AGA’s number one policy priority as it impacts every gastroenterologist regardless of practice setting. We have seen an increase in prior authorization policies from every major insurer. The most recent prior authorization program to impact gastroenterologists was announced by UnitedHealthcare (UHC) in March for implementation on June 1, 2023 and will require prior authorization for most colonoscopy and upper GI endoscopy procedures with the exception of screening colonoscopy.1 This policy is a step back at a time when payers should be developing innovative policies in collaboration with health care providers to improve patient care.
UHC’s GI prior authorization policy
AGA met with UHC in March to discuss their plan to require prior authorization for most GI endoscopy procedures. We stressed how this change will cause care delays for high-risk individuals, deter patients from undergoing medically recommended procedures, exacerbate existing sociodemographic disparities in care and outcomes, and add unnecessary paperwork burden to physicians who have mounting rates of burnout.
Linda Lee, MD, medical director of endoscopy at Brigham and Women’s Hospital, Boston, recently spoke of the impact this policy will have on gastroenterologists and their patients. “We all know that requiring prior authorizations really only leads to more bureaucracy within the insurance company, as well as within each health care provider’s practice, because we need people to fill out these prior authorization forms, waste time trying to get through to their 1-800 number to speak with someone who has no clinical knowledge, then be told we need to speak with someone else who actually does have some medical knowledge about why these procedures are necessary.”
However, Dr. Lee stressed that “most importantly, this will lead to poorer patient care with delays in care as we are struggling to wade through the morass of prior authorization while patients are bleeding, not able to swallow, vomiting, and more while waiting for their insurance company to approve their potentially life-saving procedures.”
We were particularly troubled that UHC announced this policy during Colorectal Cancer Awareness Month, given the need to screen more Americans for colorectal cancer which remains the nation’s number two cancer killer. The UHC program would require a PA on surveillance colonoscopy for those patients who have previously had polyps removed and are at a higher risk for developing colorectal cancer.
“We know that patients with high-risk adenomas or advanced sessile serrated lesions have a higher risk of developing colorectal cancer and timely access to the necessary surveillance colonoscopy is critical,” said David Lieberman, MD, past president of the AGA and chair of the AGA Executive Committee on the Screening Continuum.
AGA plans to meet with UHC again to ask them to reconsider this policy, but we need your advocacy now to tell United how this will impact you and your patients.
How you can help stop UHC’s prior authorization program
Write to UHC: Tell UHC how this policy would impact you and your patients. Contact their CEO using our customizable letter2 that outlines the impact of United’s GI endoscopy prior authorization program on gastroenterologists and their patients available on the AGA Advocacy Action Center.
Use social media: Tag United (@UHC) on Twitter and tell them how this burdensome program will cause delays for high-risk individuals, deter patients from seeking treatment, and exacerbate existing disparities in care, all while saddling physicians with even more paperwork. Once you’ve tweeted, tag your colleagues and encourage them to get involved.
AGA is working to reform prior authorization
The AGA has supported federal legislation that would streamline prior authorization processes in Medicare Advantage (MA), the private insurance plans that contract with the Medicare program, given the explosion of these policies over the past several years. The Improving Seniors Timely Access to Care Act, bipartisan, bicameral legislation, would reduce prior authorization burdens by:
- Establishing an electronic prior authorization (ePA) program and require MA plans to adopt ePA capabilities.
- Requiring the Secretary of Health and Human Services to establish a list of items and services eligible for real-time decisions under an MA ePA program.
- Standardizing and streamlining the prior authorization process for routinely approved items and services.
- Ensuring prior authorization requests are reviewed by qualified medical personnel.
- Increasing transparency around MA prior authorization requirements and their use.
- Protecting beneficiaries from any disruptions in care due to prior authorization requirements as they transition between MA plans.
The Centers for Medicare & Medicaid Services (CMS) has also recognized the impact that prior authorization is having on physician wellness and how it is contributing to physician burnout. The agency recently proposed implementing many of the provisions that are outlined in the legislation, and AGA has expressed our support for moving forward with many of their proposals.
Earlier this year, Shivan Mehta, MD, MPH, met with CMS administrator Chiquita Brooks-LaSure and Surgeon General Vivek Murthy, MD, MBA, to express AGA’s support for prior authorization reform and discussed how it impacts how patients with chronic conditions like inflammatory bowel disease maintain continuity of care. He also stressed how prior authorization further exacerbates health inequities since it creates an additional barrier to care when barriers already exist.
AGA is taking a multi-pronged approach to advocating for prior authorization reform and reducing paperwork through legislative advocacy, regulatory advocacy with the CMS, and payer advocacy. We can’t do this alone. Join our AGA Advocacy Center3 and get involved in our AGA Congressional Advocates Program.4The authors have no conflicts to declare.
References
1. UnitedHealthcare (2023 Mar 01) New requirements for gastroenterology services.
2. American Gastroenterological Association (n.d.) AGA Advocacy Action Center. Tell United to Stop New Prior Auth Requirements!
3. American Gastroenterological Association (n.d.) AGA Advocacy Action Center. Advocacy & Policy. Get Involved.
4. American Gastroenterological Association (n.d.) AGA Congressional Advocates Program.
Reforming prior authorization polices to reduce red tape for physicians and help patients get the care they need in a timely manner is the AGA’s number one policy priority as it impacts every gastroenterologist regardless of practice setting. We have seen an increase in prior authorization policies from every major insurer. The most recent prior authorization program to impact gastroenterologists was announced by UnitedHealthcare (UHC) in March for implementation on June 1, 2023 and will require prior authorization for most colonoscopy and upper GI endoscopy procedures with the exception of screening colonoscopy.1 This policy is a step back at a time when payers should be developing innovative policies in collaboration with health care providers to improve patient care.
UHC’s GI prior authorization policy
AGA met with UHC in March to discuss their plan to require prior authorization for most GI endoscopy procedures. We stressed how this change will cause care delays for high-risk individuals, deter patients from undergoing medically recommended procedures, exacerbate existing sociodemographic disparities in care and outcomes, and add unnecessary paperwork burden to physicians who have mounting rates of burnout.
Linda Lee, MD, medical director of endoscopy at Brigham and Women’s Hospital, Boston, recently spoke of the impact this policy will have on gastroenterologists and their patients. “We all know that requiring prior authorizations really only leads to more bureaucracy within the insurance company, as well as within each health care provider’s practice, because we need people to fill out these prior authorization forms, waste time trying to get through to their 1-800 number to speak with someone who has no clinical knowledge, then be told we need to speak with someone else who actually does have some medical knowledge about why these procedures are necessary.”
However, Dr. Lee stressed that “most importantly, this will lead to poorer patient care with delays in care as we are struggling to wade through the morass of prior authorization while patients are bleeding, not able to swallow, vomiting, and more while waiting for their insurance company to approve their potentially life-saving procedures.”
We were particularly troubled that UHC announced this policy during Colorectal Cancer Awareness Month, given the need to screen more Americans for colorectal cancer which remains the nation’s number two cancer killer. The UHC program would require a PA on surveillance colonoscopy for those patients who have previously had polyps removed and are at a higher risk for developing colorectal cancer.
“We know that patients with high-risk adenomas or advanced sessile serrated lesions have a higher risk of developing colorectal cancer and timely access to the necessary surveillance colonoscopy is critical,” said David Lieberman, MD, past president of the AGA and chair of the AGA Executive Committee on the Screening Continuum.
AGA plans to meet with UHC again to ask them to reconsider this policy, but we need your advocacy now to tell United how this will impact you and your patients.
How you can help stop UHC’s prior authorization program
Write to UHC: Tell UHC how this policy would impact you and your patients. Contact their CEO using our customizable letter2 that outlines the impact of United’s GI endoscopy prior authorization program on gastroenterologists and their patients available on the AGA Advocacy Action Center.
Use social media: Tag United (@UHC) on Twitter and tell them how this burdensome program will cause delays for high-risk individuals, deter patients from seeking treatment, and exacerbate existing disparities in care, all while saddling physicians with even more paperwork. Once you’ve tweeted, tag your colleagues and encourage them to get involved.
AGA is working to reform prior authorization
The AGA has supported federal legislation that would streamline prior authorization processes in Medicare Advantage (MA), the private insurance plans that contract with the Medicare program, given the explosion of these policies over the past several years. The Improving Seniors Timely Access to Care Act, bipartisan, bicameral legislation, would reduce prior authorization burdens by:
- Establishing an electronic prior authorization (ePA) program and require MA plans to adopt ePA capabilities.
- Requiring the Secretary of Health and Human Services to establish a list of items and services eligible for real-time decisions under an MA ePA program.
- Standardizing and streamlining the prior authorization process for routinely approved items and services.
- Ensuring prior authorization requests are reviewed by qualified medical personnel.
- Increasing transparency around MA prior authorization requirements and their use.
- Protecting beneficiaries from any disruptions in care due to prior authorization requirements as they transition between MA plans.
The Centers for Medicare & Medicaid Services (CMS) has also recognized the impact that prior authorization is having on physician wellness and how it is contributing to physician burnout. The agency recently proposed implementing many of the provisions that are outlined in the legislation, and AGA has expressed our support for moving forward with many of their proposals.
Earlier this year, Shivan Mehta, MD, MPH, met with CMS administrator Chiquita Brooks-LaSure and Surgeon General Vivek Murthy, MD, MBA, to express AGA’s support for prior authorization reform and discussed how it impacts how patients with chronic conditions like inflammatory bowel disease maintain continuity of care. He also stressed how prior authorization further exacerbates health inequities since it creates an additional barrier to care when barriers already exist.
AGA is taking a multi-pronged approach to advocating for prior authorization reform and reducing paperwork through legislative advocacy, regulatory advocacy with the CMS, and payer advocacy. We can’t do this alone. Join our AGA Advocacy Center3 and get involved in our AGA Congressional Advocates Program.4The authors have no conflicts to declare.
References
1. UnitedHealthcare (2023 Mar 01) New requirements for gastroenterology services.
2. American Gastroenterological Association (n.d.) AGA Advocacy Action Center. Tell United to Stop New Prior Auth Requirements!
3. American Gastroenterological Association (n.d.) AGA Advocacy Action Center. Advocacy & Policy. Get Involved.
4. American Gastroenterological Association (n.d.) AGA Congressional Advocates Program.
New coding policies to prevent surprise billing for CRC screening
The Departments of Labor, Health & Human Services, and the Treasury issued guidance in 2022 that plans and insurers “must cover and may not impose cost sharing with respect to a colonoscopy conducted after a positive non-invasive stool-based screening test” for plan or policy years1 beginning on or after May 31, 2022, and, further, “may not impose cost-sharing with respect to a polyp removal during a colonoscopy performed as a screening procedure.”2 So why are so many patients still being charged fees for these screening services? In many cases, the answer comes down to missing code modifiers.
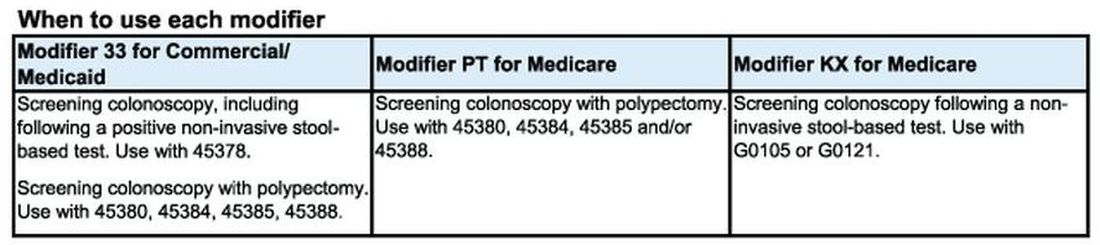
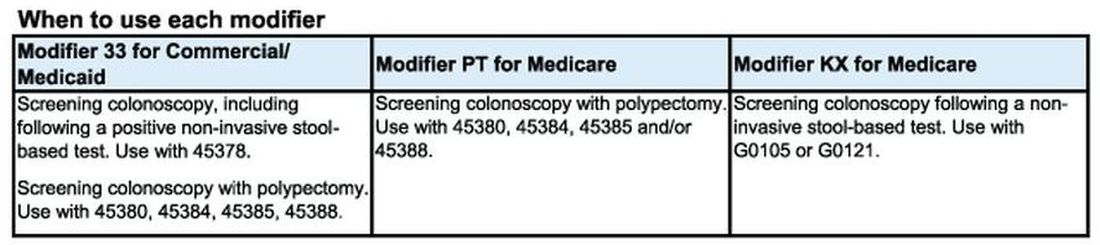
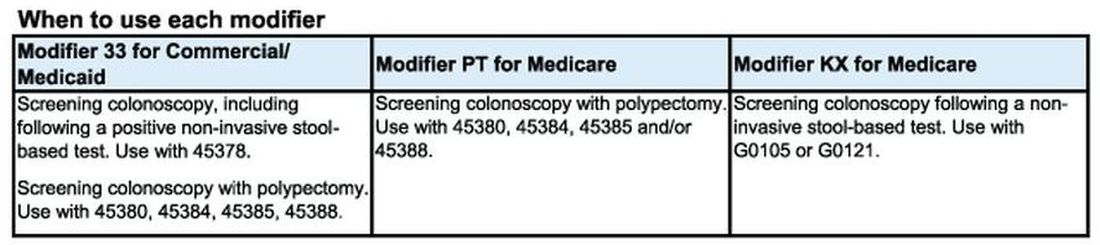
Commercial insurers want you to use modifier 33
AGA spoke to Elevance (formerly Anthem), Cigna, Aetna, and Blue Cross Blue Shield Association about how physicians should report colorectal cancer screening procedures and tests. They said using the 33 modifier (preventive service) is essential for their systems to trigger the screening benefits for beneficiaries. Without the 33 modifier, the claim will be processed as a diagnostic service, and coinsurance may apply.
According to the CPT manual, modifier 33 should be used “when the primary purpose of the service is the delivery of an evidence-based service in accordance with a U.S. Preventive Services Task Force A or B rating in effect and other preventive services identified in preventive mandates (legislative or regulatory) ...” Use modifier 33 with colonoscopies that start out as screening procedures and with colonoscopies following a positive non-invasive stool-based test, like fecal immunochemical test (FIT) or Cologuard™ multi-target stool DNA test.
It is important to note that modifier 33 won’t ensure all screening colonoscopy claims are paid, because not all commercial plans are required to cover 100 percent of the costs of CRC screening tests and procedures. For example, employer-sponsored insurance plans and legacy plans can choose not to adopt the expanded CRC benefits. Patients who are covered under these plans may not be aware that their CRC test or procedure will not be fully covered. These patients may still receive a “surprise” bill if their screening colonoscopy requires removal of polyps or if they have a colonoscopy following a positive non-invasive CRC test.
Medicare wants you to use modifiers PT and KX, but not together
CMS uses Healthcare Common Procedural Coding System (HCPCS) codes to differentiate between screening and diagnostic colonoscopies to apply screening benefits. For Medicare beneficiaries who choose colonoscopy as their CRC screening, use HCPCS code G0105 (Colorectal cancer screening; colonoscopy on individual at high risk) or G0121 (Colorectal cancer screening; colonoscopy on individual not meeting the criteria for high risk) for screening colonoscopies as appropriate. No modifier is necessary with G0105 or G0121.
Effective for claims with dates of service on or after 1/1/2023, use the appropriate HCPCS codes G0105 or G0121 with the KX modifier for colonoscopy following a positive result for any of the following non-invasive stool-based CRC screening tests:
• Screening guaiac-based fecal occult blood test (gFOBT) (CPT 82270)
• Screening immunoassay-based fecal occult blood test (iFOBT) (HCPCS G0328)
• Cologuard™ – multi-target stool DNA (sDNA) test (CPT 81528)
According to the guidance in the CMS Manual System, if modifier KX is not added to G0105 or G0121 for colonoscopy following a positive non-invasive stool-based test, Medicare will return the screening colonoscopy claim as “unprocessable.”3 If this happens, add modifier KX and resubmit the claim.
If polyps are removed during a screening colonoscopy, use the appropriate CPT code (45380, 45384, 45385, 45388) and add modifier PT (colorectal cancer screening test; converted to diagnostic test or other procedure) to each CPT code for Medicare. However, it is important to note that if a polyp is removed during a screening colonoscopy, the Medicare beneficiary is responsible for 15% of the cost from 2023 to 2026. This falls to 10% of the cost from 2027 to 2029, and by 2030 it will be covered 100% by Medicare. Some Medicare beneficiaries are not aware that Medicare has not fully eliminated the coinsurance responsibility yet.
What to do if your patient gets an unexpected bill
If your patient gets an unexpected bill and you coded the procedure correctly with the correct modifier, direct them to the AGA GI Patient Care Center’s “Colorectal cancer screening: what to expect when paying” resource for help with next steps.4
The authors have no conflicts to declare.
References
1. U.S. Department of Labor (2022, Jan. 10) FAQs About Affordable Care Act Implementation Part 51. https://www.dol.gov/sites/dolgov/files/EBSA/about-ebsa/our-activities/resource-center/faqs/aca-part-51.pdf
2. Centers for Medicare and Medicaid Services (n.d.) Affordable Care Act Implementation FAQs - Set 12. https://www.cms.gov/CCIIO/Resources/Fact-Sheets-and-FAQs/aca_implementation_faqs12.
3. Centers for Medicare and Medicaid Services (2023, Jan. 27) CMS Manual System Pub 100-03 Medicare National Coverage Determinations Transmittal 11824. https://www.cms.gov/files/document/r11824ncd.pdf.
4. American Gastroenterological Association (2023, Feb. 21) AGA GI Patient Center Colorectal Cancer Screening: What to expect when paying. https://patient.gastro.org/paying-for-your-colonoscopy/.
The Departments of Labor, Health & Human Services, and the Treasury issued guidance in 2022 that plans and insurers “must cover and may not impose cost sharing with respect to a colonoscopy conducted after a positive non-invasive stool-based screening test” for plan or policy years1 beginning on or after May 31, 2022, and, further, “may not impose cost-sharing with respect to a polyp removal during a colonoscopy performed as a screening procedure.”2 So why are so many patients still being charged fees for these screening services? In many cases, the answer comes down to missing code modifiers.
Commercial insurers want you to use modifier 33
AGA spoke to Elevance (formerly Anthem), Cigna, Aetna, and Blue Cross Blue Shield Association about how physicians should report colorectal cancer screening procedures and tests. They said using the 33 modifier (preventive service) is essential for their systems to trigger the screening benefits for beneficiaries. Without the 33 modifier, the claim will be processed as a diagnostic service, and coinsurance may apply.
According to the CPT manual, modifier 33 should be used “when the primary purpose of the service is the delivery of an evidence-based service in accordance with a U.S. Preventive Services Task Force A or B rating in effect and other preventive services identified in preventive mandates (legislative or regulatory) ...” Use modifier 33 with colonoscopies that start out as screening procedures and with colonoscopies following a positive non-invasive stool-based test, like fecal immunochemical test (FIT) or Cologuard™ multi-target stool DNA test.
It is important to note that modifier 33 won’t ensure all screening colonoscopy claims are paid, because not all commercial plans are required to cover 100 percent of the costs of CRC screening tests and procedures. For example, employer-sponsored insurance plans and legacy plans can choose not to adopt the expanded CRC benefits. Patients who are covered under these plans may not be aware that their CRC test or procedure will not be fully covered. These patients may still receive a “surprise” bill if their screening colonoscopy requires removal of polyps or if they have a colonoscopy following a positive non-invasive CRC test.
Medicare wants you to use modifiers PT and KX, but not together
CMS uses Healthcare Common Procedural Coding System (HCPCS) codes to differentiate between screening and diagnostic colonoscopies to apply screening benefits. For Medicare beneficiaries who choose colonoscopy as their CRC screening, use HCPCS code G0105 (Colorectal cancer screening; colonoscopy on individual at high risk) or G0121 (Colorectal cancer screening; colonoscopy on individual not meeting the criteria for high risk) for screening colonoscopies as appropriate. No modifier is necessary with G0105 or G0121.
Effective for claims with dates of service on or after 1/1/2023, use the appropriate HCPCS codes G0105 or G0121 with the KX modifier for colonoscopy following a positive result for any of the following non-invasive stool-based CRC screening tests:
• Screening guaiac-based fecal occult blood test (gFOBT) (CPT 82270)
• Screening immunoassay-based fecal occult blood test (iFOBT) (HCPCS G0328)
• Cologuard™ – multi-target stool DNA (sDNA) test (CPT 81528)
According to the guidance in the CMS Manual System, if modifier KX is not added to G0105 or G0121 for colonoscopy following a positive non-invasive stool-based test, Medicare will return the screening colonoscopy claim as “unprocessable.”3 If this happens, add modifier KX and resubmit the claim.
If polyps are removed during a screening colonoscopy, use the appropriate CPT code (45380, 45384, 45385, 45388) and add modifier PT (colorectal cancer screening test; converted to diagnostic test or other procedure) to each CPT code for Medicare. However, it is important to note that if a polyp is removed during a screening colonoscopy, the Medicare beneficiary is responsible for 15% of the cost from 2023 to 2026. This falls to 10% of the cost from 2027 to 2029, and by 2030 it will be covered 100% by Medicare. Some Medicare beneficiaries are not aware that Medicare has not fully eliminated the coinsurance responsibility yet.
What to do if your patient gets an unexpected bill
If your patient gets an unexpected bill and you coded the procedure correctly with the correct modifier, direct them to the AGA GI Patient Care Center’s “Colorectal cancer screening: what to expect when paying” resource for help with next steps.4
The authors have no conflicts to declare.
References
1. U.S. Department of Labor (2022, Jan. 10) FAQs About Affordable Care Act Implementation Part 51. https://www.dol.gov/sites/dolgov/files/EBSA/about-ebsa/our-activities/resource-center/faqs/aca-part-51.pdf
2. Centers for Medicare and Medicaid Services (n.d.) Affordable Care Act Implementation FAQs - Set 12. https://www.cms.gov/CCIIO/Resources/Fact-Sheets-and-FAQs/aca_implementation_faqs12.
3. Centers for Medicare and Medicaid Services (2023, Jan. 27) CMS Manual System Pub 100-03 Medicare National Coverage Determinations Transmittal 11824. https://www.cms.gov/files/document/r11824ncd.pdf.
4. American Gastroenterological Association (2023, Feb. 21) AGA GI Patient Center Colorectal Cancer Screening: What to expect when paying. https://patient.gastro.org/paying-for-your-colonoscopy/.
The Departments of Labor, Health & Human Services, and the Treasury issued guidance in 2022 that plans and insurers “must cover and may not impose cost sharing with respect to a colonoscopy conducted after a positive non-invasive stool-based screening test” for plan or policy years1 beginning on or after May 31, 2022, and, further, “may not impose cost-sharing with respect to a polyp removal during a colonoscopy performed as a screening procedure.”2 So why are so many patients still being charged fees for these screening services? In many cases, the answer comes down to missing code modifiers.
Commercial insurers want you to use modifier 33
AGA spoke to Elevance (formerly Anthem), Cigna, Aetna, and Blue Cross Blue Shield Association about how physicians should report colorectal cancer screening procedures and tests. They said using the 33 modifier (preventive service) is essential for their systems to trigger the screening benefits for beneficiaries. Without the 33 modifier, the claim will be processed as a diagnostic service, and coinsurance may apply.
According to the CPT manual, modifier 33 should be used “when the primary purpose of the service is the delivery of an evidence-based service in accordance with a U.S. Preventive Services Task Force A or B rating in effect and other preventive services identified in preventive mandates (legislative or regulatory) ...” Use modifier 33 with colonoscopies that start out as screening procedures and with colonoscopies following a positive non-invasive stool-based test, like fecal immunochemical test (FIT) or Cologuard™ multi-target stool DNA test.
It is important to note that modifier 33 won’t ensure all screening colonoscopy claims are paid, because not all commercial plans are required to cover 100 percent of the costs of CRC screening tests and procedures. For example, employer-sponsored insurance plans and legacy plans can choose not to adopt the expanded CRC benefits. Patients who are covered under these plans may not be aware that their CRC test or procedure will not be fully covered. These patients may still receive a “surprise” bill if their screening colonoscopy requires removal of polyps or if they have a colonoscopy following a positive non-invasive CRC test.
Medicare wants you to use modifiers PT and KX, but not together
CMS uses Healthcare Common Procedural Coding System (HCPCS) codes to differentiate between screening and diagnostic colonoscopies to apply screening benefits. For Medicare beneficiaries who choose colonoscopy as their CRC screening, use HCPCS code G0105 (Colorectal cancer screening; colonoscopy on individual at high risk) or G0121 (Colorectal cancer screening; colonoscopy on individual not meeting the criteria for high risk) for screening colonoscopies as appropriate. No modifier is necessary with G0105 or G0121.
Effective for claims with dates of service on or after 1/1/2023, use the appropriate HCPCS codes G0105 or G0121 with the KX modifier for colonoscopy following a positive result for any of the following non-invasive stool-based CRC screening tests:
• Screening guaiac-based fecal occult blood test (gFOBT) (CPT 82270)
• Screening immunoassay-based fecal occult blood test (iFOBT) (HCPCS G0328)
• Cologuard™ – multi-target stool DNA (sDNA) test (CPT 81528)
According to the guidance in the CMS Manual System, if modifier KX is not added to G0105 or G0121 for colonoscopy following a positive non-invasive stool-based test, Medicare will return the screening colonoscopy claim as “unprocessable.”3 If this happens, add modifier KX and resubmit the claim.
If polyps are removed during a screening colonoscopy, use the appropriate CPT code (45380, 45384, 45385, 45388) and add modifier PT (colorectal cancer screening test; converted to diagnostic test or other procedure) to each CPT code for Medicare. However, it is important to note that if a polyp is removed during a screening colonoscopy, the Medicare beneficiary is responsible for 15% of the cost from 2023 to 2026. This falls to 10% of the cost from 2027 to 2029, and by 2030 it will be covered 100% by Medicare. Some Medicare beneficiaries are not aware that Medicare has not fully eliminated the coinsurance responsibility yet.
What to do if your patient gets an unexpected bill
If your patient gets an unexpected bill and you coded the procedure correctly with the correct modifier, direct them to the AGA GI Patient Care Center’s “Colorectal cancer screening: what to expect when paying” resource for help with next steps.4
The authors have no conflicts to declare.
References
1. U.S. Department of Labor (2022, Jan. 10) FAQs About Affordable Care Act Implementation Part 51. https://www.dol.gov/sites/dolgov/files/EBSA/about-ebsa/our-activities/resource-center/faqs/aca-part-51.pdf
2. Centers for Medicare and Medicaid Services (n.d.) Affordable Care Act Implementation FAQs - Set 12. https://www.cms.gov/CCIIO/Resources/Fact-Sheets-and-FAQs/aca_implementation_faqs12.
3. Centers for Medicare and Medicaid Services (2023, Jan. 27) CMS Manual System Pub 100-03 Medicare National Coverage Determinations Transmittal 11824. https://www.cms.gov/files/document/r11824ncd.pdf.
4. American Gastroenterological Association (2023, Feb. 21) AGA GI Patient Center Colorectal Cancer Screening: What to expect when paying. https://patient.gastro.org/paying-for-your-colonoscopy/.