User login
Two Home Health Agencies Reduce Readmissions Among Heart Failure Patients Using a Quality Improvement Approach
From Collaborative Healthcare Strategies, Lexington, MA (Dr. Boutwell), and the National Home Health Corporation, Scarsdale, NY.
Abstract
- Objective: To describe a quality improvement initiative implemented by 2 home health care agencies to reduce readmissions.
- Methods: The agencies reviewed their data and identified best practices for reducing acute hospital transfers among their high-risk heart failure patients, focusing on the first 14 days of the care episode. Care intensity was increased during the first 3 days, and an active surveillance approach was used during the first 2 weeks. Training for staff, called “Heart Failure Boot Camp,” was introduced and made part of new employee orientation.
- Results: The 30-day rehospitalization rate was reduced from 31% to 17%.
- Conclusion: A data-driven transitional care model can lead to reductions in 30-day readmissions among high-risk patients receiving home health care.
Hospital readmissions are frequent, costly, and can be a marker of poorly coordinated postdischarge care [1]. Since the passage of the Affordable Care Act in 2010, reducing readmissions has become a national priority, as reflected in the emergence of accountable care organizations, bundled payments, and readmission penalties for hospitals, among other efforts. With the increasing attention on reducing readmissions, home health care agencies are under pressure to identify opportunities to improve performance. Two affiliated home health care agencies in Massachusetts and Connecticut made reducing their all-cause 30-day readmission rate a strategic priority. In this article, we describe their approach.
Setting
New England Home Care (NEHC, Cromwell, CT) is a regional agency that serves 7 of the 8 counties in Connecticut and over 7400 patients annually. Medical Resources Home Health (Newton, MA) is a regional agency that serves 8 of the 12 counties in Massachusetts and 2000 patients annually. These home health agencies are both owned by National Home Health Care Corporation (Scarsdale, NY) but are independently managed, with separate staff and regional market differences.
Data Analysis
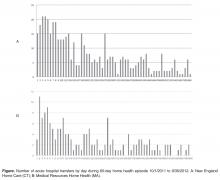
Opportunities for Improvement The data analysis highlighted several immediate opportunities for improvement. First, the data showed that the first 3 days of the home health episode are a period of increased risk. Thus, intensification of care—and successful first contacts—during the first 3 days of the home health episode was an important target goal. Similarly, the first 14 days were a period of increased risk, suggesting the potential benefit of home health staff proactively monitoring patients during this time to identify clinical or other needs early in the effort to avert a hospitalization. In addition, while respiratory symptoms were among the top reasons for acute care hospitalization within 30 days of episode initiation, many other diagnoses were also implicated. Nine conditions comprised 80% of coded reasons for hospitalization, suggesting that vigilance around respiratory complaints is important but cannot be the exclusive focus of symptom management in this population.
Approach The agencies started this performance improvement initiative by focusing on one patient subgroup (heart failure patients) served by one of the agencies (NEHC). New approaches were tried, and effective approaches were codified through training, on-the job coaching, and performance feedback to front-line clinicians. This approach facilitated the spread of these changes to the second agency, and subsequently both agencies expanded their focus beyond heart failure to other common diagnoses in the home health population.
Changes to Standard Care Practices Based on identified opportunities for improvement, the agency incorporated modifications to standard care utilizing existing resources and within the construct of a certified Medicare home health episode (Medicare’s required specific services, assessments, and other activities that a home health agency must provide in order to bill for an episode). First, working with managers and front-line clinicians, they focused on establishing successful contact during the first 3 days of an episode of care. Front-line staff reported that some patients did not respond to the first attempt to establish contact, and staff thought that it indicated that the patient did not want home health care. The agency designed a new initial contact protocol to increase the likelihood of a successful first contact with the patient. Second, staff increased the frequency of contact in the first 3 days of the episode, either through home visits or phone calls. Increased contact served to allowed the home health staff to get to know the patient and have more points of reference upon which to identify whether symptoms were developing or changing. In addition, increase initial frequency served to increase the comfort and confidence that the patient and their family had in the agency. Third, in the context of increasing the frequency and effectiveness of contacts in the first 14 days, home care staff were trained to adopt an “active surveillance” approach. This staff development and re-training initiative instructed staff on practices to increase their awareness and recognition of patient needs or changing circumstances, outside the specific problem-defined focus area(s) of the home health episode. Frequent contact in the first 14 days creates an opportunity for home health staff to intervene proactively in the confusion or symptoms that lead patients or their families to call 911. Fourth, home care staff received professional development training specifically focused on heart failure, called “Heart Failure Boot Camp.” This training provided a review and update on the clinical management best practices for home care for heart failure patients. This training was conducted by the agency’s staff clinical educator at each local field office. Once all the agencies’ existing staff were trained, the training materials were included in new employee orientation. Rate of acute care hospitalizations was tracked and reports were provided to each local field office on a quarterly basis. Agency leadership included review of these data with local field office managers in their existing management meetings to reinforce the importance of this initiative for the agency at the highest levels. As the efforts to reduce hospitalizations evolved to include patients with conditions other than heart failure, the agencies developed a readmission risk assessment that included the number of medications ( < 5; 6–10; 11–15; 16–20; or > 20) and number of hospitalizations within the past 12 months. Staff could act upon the risk elements identified to reduce each individual patient’s risk of readmission.
Adding Enhanced Service to Standard Care: The Transitional Care Liaison
ollowing the implementation of the above changes to standard home health care practices, the agencies subsequently deployed full-time transitional care liaisons at local hospitals. This was a new role, requiring newly dedicated resources for the position. The role is modeled upon the Care Transitions Intervention [2],which emphasizes the value of initiating transitional care during the hospitalization. In this new role, the hospital-based home care liaisons establish a relationship with the patient, schedule immediate follow-up, review medications and the plan to obtain new medications, and review the plan of care in the hospital, prior to the transition home. On-site transitional care liaisons greatly facilitate clinical collaboration, allowing the “receiving” provider to request clarifications prior to discharge. On-site relationships also enable formal and informal mutual improvements in the transition process. An unanticipated benefit to this collaboration is that the agencies are able to identify some high-utilizing patients who are served by several area hospitals. Thus the agencies were able to add to the list of highest-risk patients for some hospitals that were otherwise unidentified.
Outcomes
The 30-day rehospitalization rate for NEHC was 31% during the baseline period (9/30/2008 to 6/30/2010). The quarterly variability in readmission rates was high, ranging from 20% to 42% in any given quarter. Following the start of the performance improvement initiative in Quarter 3 of 2010, and through the most recent quarter for which data are available (Quarter 3 2013) the quarterly 30-day readmission rates demonstrated decreased variability (15% to 22%) and the 30-day readmission rate was reduced to 17%—a 45% reduction in rehospitalizations. The agencies’ rehospitalization rates are lower than local benchmarks [1].
Lessons Learned
The agencies experience with this initiative has led to several lessons learned that may be of interest to other agencies and providers looking to design and implement care models to reduce rehospitalizations.
First, it was essential to supplement our knowledge of best practices from the literature and industry experts with an examination of our own data. In addition to examining rates of rehospitalization, we were able to identify patients at highest risk so we could intensify services early for this group.
Second, the 2 agencies participating in this effort are affiliated but independently managed, with separate staff and regional market differences. We were pleased to learn that a common service delivery model could be successfully implemented in both agencies. This suggests that this structured care delivery improvement approach can be replicated in other organizations and local contexts.
Third, by no means was the staff development and retraining a “one and done” effort; continuous reinforcement of the rationale for the practice change and the protocols for optimizing engagement to reduce rehospitalizations was required.
Finally, the performance improvement initiative started with an initial focus on heart failure patients. Over the course of the Initiative we named the series of practice changes our “Healthy@Home” model of care. As we expanded our focus to all patients at high risk of readmission (as identified by our risk assessment score), we learned that staff thought the Healthy@Home practice changes only applied to heart failure patients. This required re-messaging with the staff and regional supervisors.
Conclusion
As rehospitalizations continue to be a prominent measure of quality, cost, and patient experience and a measure for which hospitals and post-acute and community-based providers are either penalized or rewarded, there is a growing awareness of the many factors outside the walls of the hospital that determine whether a patient will return within a defined period of time. Many home health agencies see this as an opportune moment to highlight the critical role they play in care transitions across settings and over time. In this article, we describe the experience of 2 affiliated regional home health care agencies as they engaged in a structured performance improvement effort to reduce readmissions among their high-risk patients. This effort involving data analysis, identification of locally relevant opportunities for improvement, modifications to standard care utilizing existing resources, adding a new service, and expansion beyond the initial target population to all patients at high risk of readmission. This 3-year effort has resulted in a substantial and sustained reduction in rehospitalization rates.
1. Masspro, Massachusetts’ Quality Improvement Organization. State of the state: readmissions in Massachusetts January 1 2009-September 30 2013. Accessed 14 April 2014 at www.masspro.org/files/tools/12_13_state_of_the_state.pdf.
2. Coleman EA, Parry C, Chalmers S, Min S. The care transitions intervention. Arch Intern Med 2006;166:1822–8.
From Collaborative Healthcare Strategies, Lexington, MA (Dr. Boutwell), and the National Home Health Corporation, Scarsdale, NY.
Abstract
- Objective: To describe a quality improvement initiative implemented by 2 home health care agencies to reduce readmissions.
- Methods: The agencies reviewed their data and identified best practices for reducing acute hospital transfers among their high-risk heart failure patients, focusing on the first 14 days of the care episode. Care intensity was increased during the first 3 days, and an active surveillance approach was used during the first 2 weeks. Training for staff, called “Heart Failure Boot Camp,” was introduced and made part of new employee orientation.
- Results: The 30-day rehospitalization rate was reduced from 31% to 17%.
- Conclusion: A data-driven transitional care model can lead to reductions in 30-day readmissions among high-risk patients receiving home health care.
Hospital readmissions are frequent, costly, and can be a marker of poorly coordinated postdischarge care [1]. Since the passage of the Affordable Care Act in 2010, reducing readmissions has become a national priority, as reflected in the emergence of accountable care organizations, bundled payments, and readmission penalties for hospitals, among other efforts. With the increasing attention on reducing readmissions, home health care agencies are under pressure to identify opportunities to improve performance. Two affiliated home health care agencies in Massachusetts and Connecticut made reducing their all-cause 30-day readmission rate a strategic priority. In this article, we describe their approach.
Setting
New England Home Care (NEHC, Cromwell, CT) is a regional agency that serves 7 of the 8 counties in Connecticut and over 7400 patients annually. Medical Resources Home Health (Newton, MA) is a regional agency that serves 8 of the 12 counties in Massachusetts and 2000 patients annually. These home health agencies are both owned by National Home Health Care Corporation (Scarsdale, NY) but are independently managed, with separate staff and regional market differences.
Data Analysis
Opportunities for Improvement The data analysis highlighted several immediate opportunities for improvement. First, the data showed that the first 3 days of the home health episode are a period of increased risk. Thus, intensification of care—and successful first contacts—during the first 3 days of the home health episode was an important target goal. Similarly, the first 14 days were a period of increased risk, suggesting the potential benefit of home health staff proactively monitoring patients during this time to identify clinical or other needs early in the effort to avert a hospitalization. In addition, while respiratory symptoms were among the top reasons for acute care hospitalization within 30 days of episode initiation, many other diagnoses were also implicated. Nine conditions comprised 80% of coded reasons for hospitalization, suggesting that vigilance around respiratory complaints is important but cannot be the exclusive focus of symptom management in this population.
Approach The agencies started this performance improvement initiative by focusing on one patient subgroup (heart failure patients) served by one of the agencies (NEHC). New approaches were tried, and effective approaches were codified through training, on-the job coaching, and performance feedback to front-line clinicians. This approach facilitated the spread of these changes to the second agency, and subsequently both agencies expanded their focus beyond heart failure to other common diagnoses in the home health population.
Changes to Standard Care Practices Based on identified opportunities for improvement, the agency incorporated modifications to standard care utilizing existing resources and within the construct of a certified Medicare home health episode (Medicare’s required specific services, assessments, and other activities that a home health agency must provide in order to bill for an episode). First, working with managers and front-line clinicians, they focused on establishing successful contact during the first 3 days of an episode of care. Front-line staff reported that some patients did not respond to the first attempt to establish contact, and staff thought that it indicated that the patient did not want home health care. The agency designed a new initial contact protocol to increase the likelihood of a successful first contact with the patient. Second, staff increased the frequency of contact in the first 3 days of the episode, either through home visits or phone calls. Increased contact served to allowed the home health staff to get to know the patient and have more points of reference upon which to identify whether symptoms were developing or changing. In addition, increase initial frequency served to increase the comfort and confidence that the patient and their family had in the agency. Third, in the context of increasing the frequency and effectiveness of contacts in the first 14 days, home care staff were trained to adopt an “active surveillance” approach. This staff development and re-training initiative instructed staff on practices to increase their awareness and recognition of patient needs or changing circumstances, outside the specific problem-defined focus area(s) of the home health episode. Frequent contact in the first 14 days creates an opportunity for home health staff to intervene proactively in the confusion or symptoms that lead patients or their families to call 911. Fourth, home care staff received professional development training specifically focused on heart failure, called “Heart Failure Boot Camp.” This training provided a review and update on the clinical management best practices for home care for heart failure patients. This training was conducted by the agency’s staff clinical educator at each local field office. Once all the agencies’ existing staff were trained, the training materials were included in new employee orientation. Rate of acute care hospitalizations was tracked and reports were provided to each local field office on a quarterly basis. Agency leadership included review of these data with local field office managers in their existing management meetings to reinforce the importance of this initiative for the agency at the highest levels. As the efforts to reduce hospitalizations evolved to include patients with conditions other than heart failure, the agencies developed a readmission risk assessment that included the number of medications ( < 5; 6–10; 11–15; 16–20; or > 20) and number of hospitalizations within the past 12 months. Staff could act upon the risk elements identified to reduce each individual patient’s risk of readmission.
Adding Enhanced Service to Standard Care: The Transitional Care Liaison
ollowing the implementation of the above changes to standard home health care practices, the agencies subsequently deployed full-time transitional care liaisons at local hospitals. This was a new role, requiring newly dedicated resources for the position. The role is modeled upon the Care Transitions Intervention [2],which emphasizes the value of initiating transitional care during the hospitalization. In this new role, the hospital-based home care liaisons establish a relationship with the patient, schedule immediate follow-up, review medications and the plan to obtain new medications, and review the plan of care in the hospital, prior to the transition home. On-site transitional care liaisons greatly facilitate clinical collaboration, allowing the “receiving” provider to request clarifications prior to discharge. On-site relationships also enable formal and informal mutual improvements in the transition process. An unanticipated benefit to this collaboration is that the agencies are able to identify some high-utilizing patients who are served by several area hospitals. Thus the agencies were able to add to the list of highest-risk patients for some hospitals that were otherwise unidentified.
Outcomes
The 30-day rehospitalization rate for NEHC was 31% during the baseline period (9/30/2008 to 6/30/2010). The quarterly variability in readmission rates was high, ranging from 20% to 42% in any given quarter. Following the start of the performance improvement initiative in Quarter 3 of 2010, and through the most recent quarter for which data are available (Quarter 3 2013) the quarterly 30-day readmission rates demonstrated decreased variability (15% to 22%) and the 30-day readmission rate was reduced to 17%—a 45% reduction in rehospitalizations. The agencies’ rehospitalization rates are lower than local benchmarks [1].
Lessons Learned
The agencies experience with this initiative has led to several lessons learned that may be of interest to other agencies and providers looking to design and implement care models to reduce rehospitalizations.
First, it was essential to supplement our knowledge of best practices from the literature and industry experts with an examination of our own data. In addition to examining rates of rehospitalization, we were able to identify patients at highest risk so we could intensify services early for this group.
Second, the 2 agencies participating in this effort are affiliated but independently managed, with separate staff and regional market differences. We were pleased to learn that a common service delivery model could be successfully implemented in both agencies. This suggests that this structured care delivery improvement approach can be replicated in other organizations and local contexts.
Third, by no means was the staff development and retraining a “one and done” effort; continuous reinforcement of the rationale for the practice change and the protocols for optimizing engagement to reduce rehospitalizations was required.
Finally, the performance improvement initiative started with an initial focus on heart failure patients. Over the course of the Initiative we named the series of practice changes our “Healthy@Home” model of care. As we expanded our focus to all patients at high risk of readmission (as identified by our risk assessment score), we learned that staff thought the Healthy@Home practice changes only applied to heart failure patients. This required re-messaging with the staff and regional supervisors.
Conclusion
As rehospitalizations continue to be a prominent measure of quality, cost, and patient experience and a measure for which hospitals and post-acute and community-based providers are either penalized or rewarded, there is a growing awareness of the many factors outside the walls of the hospital that determine whether a patient will return within a defined period of time. Many home health agencies see this as an opportune moment to highlight the critical role they play in care transitions across settings and over time. In this article, we describe the experience of 2 affiliated regional home health care agencies as they engaged in a structured performance improvement effort to reduce readmissions among their high-risk patients. This effort involving data analysis, identification of locally relevant opportunities for improvement, modifications to standard care utilizing existing resources, adding a new service, and expansion beyond the initial target population to all patients at high risk of readmission. This 3-year effort has resulted in a substantial and sustained reduction in rehospitalization rates.
From Collaborative Healthcare Strategies, Lexington, MA (Dr. Boutwell), and the National Home Health Corporation, Scarsdale, NY.
Abstract
- Objective: To describe a quality improvement initiative implemented by 2 home health care agencies to reduce readmissions.
- Methods: The agencies reviewed their data and identified best practices for reducing acute hospital transfers among their high-risk heart failure patients, focusing on the first 14 days of the care episode. Care intensity was increased during the first 3 days, and an active surveillance approach was used during the first 2 weeks. Training for staff, called “Heart Failure Boot Camp,” was introduced and made part of new employee orientation.
- Results: The 30-day rehospitalization rate was reduced from 31% to 17%.
- Conclusion: A data-driven transitional care model can lead to reductions in 30-day readmissions among high-risk patients receiving home health care.
Hospital readmissions are frequent, costly, and can be a marker of poorly coordinated postdischarge care [1]. Since the passage of the Affordable Care Act in 2010, reducing readmissions has become a national priority, as reflected in the emergence of accountable care organizations, bundled payments, and readmission penalties for hospitals, among other efforts. With the increasing attention on reducing readmissions, home health care agencies are under pressure to identify opportunities to improve performance. Two affiliated home health care agencies in Massachusetts and Connecticut made reducing their all-cause 30-day readmission rate a strategic priority. In this article, we describe their approach.
Setting
New England Home Care (NEHC, Cromwell, CT) is a regional agency that serves 7 of the 8 counties in Connecticut and over 7400 patients annually. Medical Resources Home Health (Newton, MA) is a regional agency that serves 8 of the 12 counties in Massachusetts and 2000 patients annually. These home health agencies are both owned by National Home Health Care Corporation (Scarsdale, NY) but are independently managed, with separate staff and regional market differences.
Data Analysis
Opportunities for Improvement The data analysis highlighted several immediate opportunities for improvement. First, the data showed that the first 3 days of the home health episode are a period of increased risk. Thus, intensification of care—and successful first contacts—during the first 3 days of the home health episode was an important target goal. Similarly, the first 14 days were a period of increased risk, suggesting the potential benefit of home health staff proactively monitoring patients during this time to identify clinical or other needs early in the effort to avert a hospitalization. In addition, while respiratory symptoms were among the top reasons for acute care hospitalization within 30 days of episode initiation, many other diagnoses were also implicated. Nine conditions comprised 80% of coded reasons for hospitalization, suggesting that vigilance around respiratory complaints is important but cannot be the exclusive focus of symptom management in this population.
Approach The agencies started this performance improvement initiative by focusing on one patient subgroup (heart failure patients) served by one of the agencies (NEHC). New approaches were tried, and effective approaches were codified through training, on-the job coaching, and performance feedback to front-line clinicians. This approach facilitated the spread of these changes to the second agency, and subsequently both agencies expanded their focus beyond heart failure to other common diagnoses in the home health population.
Changes to Standard Care Practices Based on identified opportunities for improvement, the agency incorporated modifications to standard care utilizing existing resources and within the construct of a certified Medicare home health episode (Medicare’s required specific services, assessments, and other activities that a home health agency must provide in order to bill for an episode). First, working with managers and front-line clinicians, they focused on establishing successful contact during the first 3 days of an episode of care. Front-line staff reported that some patients did not respond to the first attempt to establish contact, and staff thought that it indicated that the patient did not want home health care. The agency designed a new initial contact protocol to increase the likelihood of a successful first contact with the patient. Second, staff increased the frequency of contact in the first 3 days of the episode, either through home visits or phone calls. Increased contact served to allowed the home health staff to get to know the patient and have more points of reference upon which to identify whether symptoms were developing or changing. In addition, increase initial frequency served to increase the comfort and confidence that the patient and their family had in the agency. Third, in the context of increasing the frequency and effectiveness of contacts in the first 14 days, home care staff were trained to adopt an “active surveillance” approach. This staff development and re-training initiative instructed staff on practices to increase their awareness and recognition of patient needs or changing circumstances, outside the specific problem-defined focus area(s) of the home health episode. Frequent contact in the first 14 days creates an opportunity for home health staff to intervene proactively in the confusion or symptoms that lead patients or their families to call 911. Fourth, home care staff received professional development training specifically focused on heart failure, called “Heart Failure Boot Camp.” This training provided a review and update on the clinical management best practices for home care for heart failure patients. This training was conducted by the agency’s staff clinical educator at each local field office. Once all the agencies’ existing staff were trained, the training materials were included in new employee orientation. Rate of acute care hospitalizations was tracked and reports were provided to each local field office on a quarterly basis. Agency leadership included review of these data with local field office managers in their existing management meetings to reinforce the importance of this initiative for the agency at the highest levels. As the efforts to reduce hospitalizations evolved to include patients with conditions other than heart failure, the agencies developed a readmission risk assessment that included the number of medications ( < 5; 6–10; 11–15; 16–20; or > 20) and number of hospitalizations within the past 12 months. Staff could act upon the risk elements identified to reduce each individual patient’s risk of readmission.
Adding Enhanced Service to Standard Care: The Transitional Care Liaison
ollowing the implementation of the above changes to standard home health care practices, the agencies subsequently deployed full-time transitional care liaisons at local hospitals. This was a new role, requiring newly dedicated resources for the position. The role is modeled upon the Care Transitions Intervention [2],which emphasizes the value of initiating transitional care during the hospitalization. In this new role, the hospital-based home care liaisons establish a relationship with the patient, schedule immediate follow-up, review medications and the plan to obtain new medications, and review the plan of care in the hospital, prior to the transition home. On-site transitional care liaisons greatly facilitate clinical collaboration, allowing the “receiving” provider to request clarifications prior to discharge. On-site relationships also enable formal and informal mutual improvements in the transition process. An unanticipated benefit to this collaboration is that the agencies are able to identify some high-utilizing patients who are served by several area hospitals. Thus the agencies were able to add to the list of highest-risk patients for some hospitals that were otherwise unidentified.
Outcomes
The 30-day rehospitalization rate for NEHC was 31% during the baseline period (9/30/2008 to 6/30/2010). The quarterly variability in readmission rates was high, ranging from 20% to 42% in any given quarter. Following the start of the performance improvement initiative in Quarter 3 of 2010, and through the most recent quarter for which data are available (Quarter 3 2013) the quarterly 30-day readmission rates demonstrated decreased variability (15% to 22%) and the 30-day readmission rate was reduced to 17%—a 45% reduction in rehospitalizations. The agencies’ rehospitalization rates are lower than local benchmarks [1].
Lessons Learned
The agencies experience with this initiative has led to several lessons learned that may be of interest to other agencies and providers looking to design and implement care models to reduce rehospitalizations.
First, it was essential to supplement our knowledge of best practices from the literature and industry experts with an examination of our own data. In addition to examining rates of rehospitalization, we were able to identify patients at highest risk so we could intensify services early for this group.
Second, the 2 agencies participating in this effort are affiliated but independently managed, with separate staff and regional market differences. We were pleased to learn that a common service delivery model could be successfully implemented in both agencies. This suggests that this structured care delivery improvement approach can be replicated in other organizations and local contexts.
Third, by no means was the staff development and retraining a “one and done” effort; continuous reinforcement of the rationale for the practice change and the protocols for optimizing engagement to reduce rehospitalizations was required.
Finally, the performance improvement initiative started with an initial focus on heart failure patients. Over the course of the Initiative we named the series of practice changes our “Healthy@Home” model of care. As we expanded our focus to all patients at high risk of readmission (as identified by our risk assessment score), we learned that staff thought the Healthy@Home practice changes only applied to heart failure patients. This required re-messaging with the staff and regional supervisors.
Conclusion
As rehospitalizations continue to be a prominent measure of quality, cost, and patient experience and a measure for which hospitals and post-acute and community-based providers are either penalized or rewarded, there is a growing awareness of the many factors outside the walls of the hospital that determine whether a patient will return within a defined period of time. Many home health agencies see this as an opportune moment to highlight the critical role they play in care transitions across settings and over time. In this article, we describe the experience of 2 affiliated regional home health care agencies as they engaged in a structured performance improvement effort to reduce readmissions among their high-risk patients. This effort involving data analysis, identification of locally relevant opportunities for improvement, modifications to standard care utilizing existing resources, adding a new service, and expansion beyond the initial target population to all patients at high risk of readmission. This 3-year effort has resulted in a substantial and sustained reduction in rehospitalization rates.
1. Masspro, Massachusetts’ Quality Improvement Organization. State of the state: readmissions in Massachusetts January 1 2009-September 30 2013. Accessed 14 April 2014 at www.masspro.org/files/tools/12_13_state_of_the_state.pdf.
2. Coleman EA, Parry C, Chalmers S, Min S. The care transitions intervention. Arch Intern Med 2006;166:1822–8.
1. Masspro, Massachusetts’ Quality Improvement Organization. State of the state: readmissions in Massachusetts January 1 2009-September 30 2013. Accessed 14 April 2014 at www.masspro.org/files/tools/12_13_state_of_the_state.pdf.
2. Coleman EA, Parry C, Chalmers S, Min S. The care transitions intervention. Arch Intern Med 2006;166:1822–8.