User login
Malpractice Counsel: Cervical Spine Injury
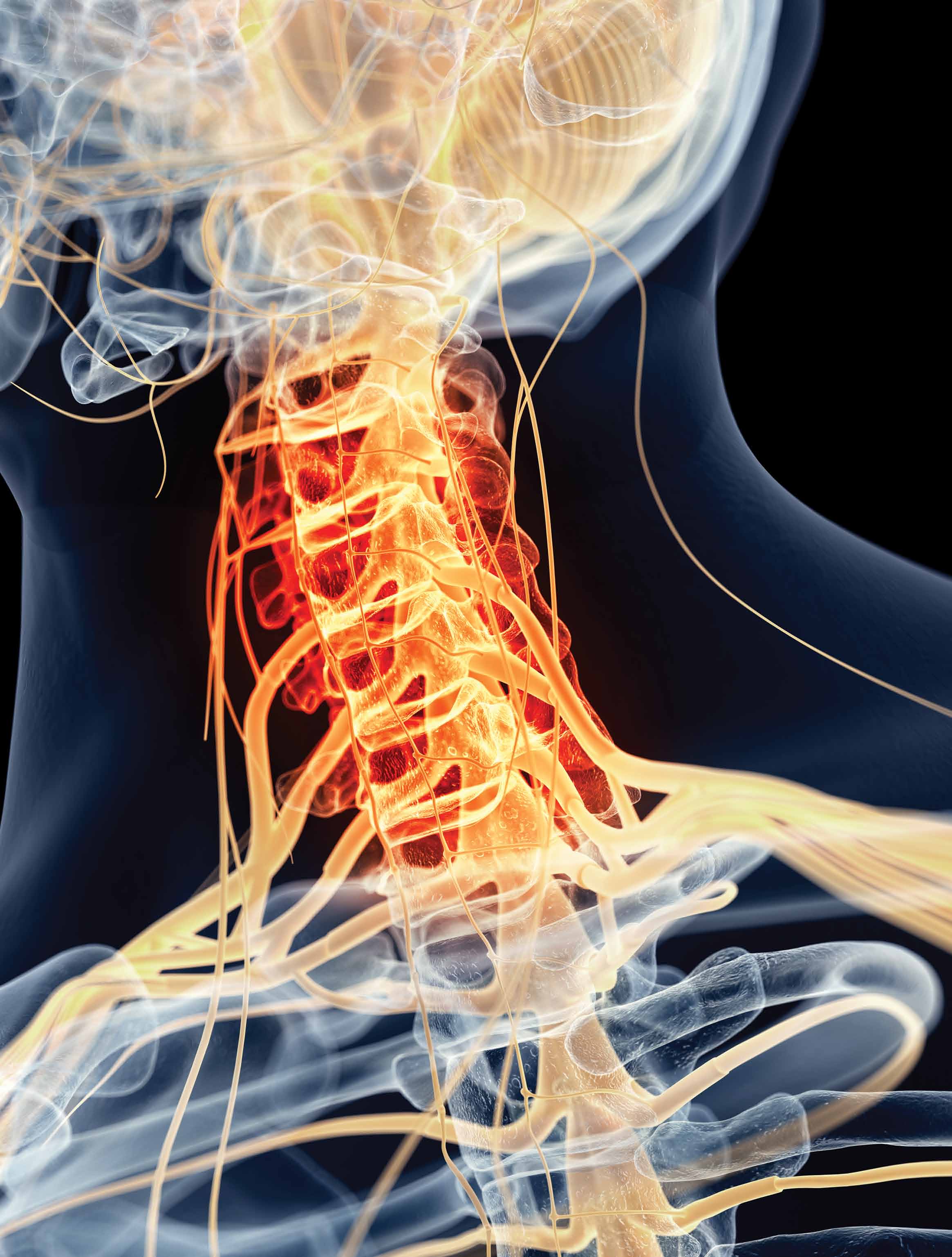
| An 83-year-old man presented to the ED via emergency medical services (EMS) with a chief complaint of neck pain. He was the restrained driver of a car that was struck from behind by another vehicle. The patient denied any head injury, loss of consciousness, chest pain, shortness of breath, or abdominal pain. His medical history was significant for hypertension and coronary artery disease, for which he was taking several medications. Regarding his social history, the patient denied alcohol consumption or cigarette smoking. |
The patient’s physical examination was unremarkable. His vital signs were normal, and there was no obvious external evidence of trauma. The posterior cervical spine was tender to palpation in the midline, but no step-off signs were appreciated. The neurological examination, including strength and sensation in all four extremities, was normal.
Since the patient’s only complaint was neck pain and his physical examination and history were otherwise normal, the emergency physician (EP) ordered radiographs of the cervical spine. The imaging studies were interpreted as showing advanced degenerative changes but no fractures, and the patient was prescribed an analgesic and discharged home.
When the patient woke up the next morning, he was unable to move his extremities, and returned to the same ED via EMS. He was placed in a cervical collar and found to have flaccid extremities on examination. A computed tomography (CT) scan of the cervical spine revealed a transverse fracture through the C6 vertebra. Radiology services also reviewed the cervical spine X-rays from the previous day, noting the presence of fracture.
The patient was taken to the operating room by neurosurgery services but remained paralyzed postoperatively. He never recovered from his injury and died 6 months later. His family sued the EP and the hospital for missed diagnosis of cervical spine fracture at the first ED presentation and the resulting paralysis. The case was settled for $1.3 million prior to trial.
Discussion
The evaluation of suspected cervical spine injury secondary to blunt trauma is a frequent and important skill practiced by EPs. Motor vehicle accidents are the most common cause of spinal cord injury in the United States (42%), followed by falls (27%), acts of violence (15%), and sports-related injuries (8%).1 A review by Sekon and Fehlings2 showed that 55% of all spinal injuries involve the cervical spine. Interestingly, the majority of cervical spine injuries occur at the upper or lower ends of the cervical spine; C2 vertebral fractures account for 33%, while C6 and C7 vertebral fractures account for approximately 50%.1
There are two commonly used criteria to clinically clear the cervical spine (ie, no imaging studies necessary) in blunt-trauma patients. The first is the National Emergency X-Radiography Use Study (NEXUS), which has a sensitivity of 99.6% of identifying cervical spine fractures.1 According to the NEXUS criteria, no imaging studies are required if: (1) there is no midline cervical spine tenderness; (2) there are no focal neurological deficits; (3) the patient exhibits a normal level of alertness; (4) the patient is not intoxicated; and (5) there is no distracting injury.1
The other set of criteria used to clear the cervical spine is the Canadian Cervical Spine Rule. In these criteria, a patient is considered at very low risk for cervical spine fracture in the following cases: (1) the patient is fully alert with a Glasgow Coma scale of 15; (2) the patient has no high-risk factors (ie, age >65 years, dangerous mechanism of injury, fall greater than five stairs, axial load to the head, high-speed vehicular crash, bicycle or motorcycle crash, or the presence of paresthesias in the extremities); (3) the patient has low-risk factors (eg, simple vehicle crash, sitting position in the ED, ambulatory at any time, delayed onset of neck pain, and the absence of midline cervical tenderness); and (4) the patient can actively rotate his or her neck 45 degrees to the left and to the right. The Canadian group found the above criteria to have 100% sensitivity for predicting the absence of cervical spine injury.1
The patient in this case failed both sets of criteria (ie, presence of cervical spine tenderness and age >65 years) and therefore required imaging. Historically, cervical spine X-ray (three views, anteroposterior, lateral, and odontoid; or five views, three views plus obliques) has been the imaging study of choice for such patients. Unfortunately, however, cervical spine radiographs have severe limitations in identifying spinal injury. In a large retrospective review, Woodring and Lee,3 found that the standard three-view cervical spine series failed to demonstrate 61% of all fractures and 36% of all subluxation and dislocations. Similarly, in a prospective study of 1,006 patients with 72 injuries, Diaz et al,4 found a 52.3% missed fracture rate when five-view radiographs were used to identify cervical spine injury. In addition, radiographic evaluation of elderly patients was found to be even more challenging in identifying cervical spine injury due to age-related degenerative changes.
Given the abovementioned limitations associated with radiographic imaging, CT scan of the cervical spine has become the imaging study of choice in moderate-to-severe risk patients with blunt cervical spine trauma. This modality has been shown to have a higher sensitivity and specificity for evaluating cervical spine injury compared to plain X-ray films, with CT detecting 97% to 100% of cervical spine fractures.5
In addition to demonstrating a higher sensitivity, CT also has the advantage of speed—especially when the patient is undergoing other CT studies (eg, head, abdomen, pelvis). While some clinicians criticize the higher cost of CT versus plain films, CT has been shown to decrease institutional costs (when settlement costs are taken into account) due to the reduction of the incidence of paralysis resulting from false-negative imaging studies.6
Forgotten Tourniquet
| A 33-year-old woman presented to the ED with a chief complaint of left-sided abdominal and flank pain. She described the onset of pain as abrupt, severe, and lasting approximately 3 hours in duration. She admitted to nausea, but no vomiting. She also denied a history of any previous similar symptoms or recent trauma. The patient’s medical history was unremarkable. Her last menstrual period began 3 days prior to presentation. Regarding social history, she denied any tobacco or alcohol use. |
The patient’s vital signs were: blood pressure, 138/82 mm Hg; heart rate, 102 beats/minute; respiratory rate, 18 breaths/minute; temperature 98.6˚F. Oxygen saturation was 99% on room air.
The patient appeared uncomfortable overall. The physical examination was remarkable only for mild left-sided costovertebral angle tenderness. Her abdomen was soft, nontender, and without guarding or rebound.
The EP ordered the placement of an intravenous (IV) line, through which the patient was administered normal saline and morphine and promethazine, respectively, for pain and nausea. A complete blood count, basic metabolic panel, urinalysis, and urine pregnancy test were ordered. All of the laboratory bloodwork results were normal, and the urine pregnancy test was negative. The urinalysis was remarkable for 50 to 100 red blood cells.
A noncontrast CT scan of the abdomen and pelvis revealed a 3-mm ureteral stone on the left side. When the patient returned from radiology services, her pain was significantly decreased and she felt much improved. She was diagnosed with a kidney stone and discharged home with an analgesic and a strainer, along with instructions to follow-up with urology services. The patient was in the ED for a total of 5 hours.
The plaintiff sued the EP and hospital, claiming that the tourniquet used to start the IV line and draw blood was never removed, which in turn caused nerve damage resulting in reflex sympathetic dystrophy and complex regional pain syndrome. The defense denied all of these allegations, and the ED personnel testified that the tourniquet was removed as soon as the IV was established. The defense cited the plaintiff’s medical records, which contained documentation that the tourniquet had been removed. The defense further argued that if the tourniquet had been left on as the patient alleged, she would have experienced obvious physical signs, such as swelling, redness, infiltration of fluids, pain, and numbness. A defense verdict was returned.
Discussion
It is very tempting to simply dismiss this case as absurd, with nothing to be learned from it. It does defy common sense that no one would have noticed the tourniquet or, at the very least, that the patient would not have spoken up about it during her stay in the ED. While the jury clearly came to the correct conclusion, it does highlight a real problem: forgotten tourniquets.
According to the Pennsylvania Patient Safety Advisory (PPSA), there were 125 reports of tourniquets being left on patients in Pennsylvania healthcare facilities in 1 year alone.1 In 5% of these cases, the tourniquet was discovered within a half hour of application. In approximately 66% of cases, the tourniquet was left on for up to 2 hours, and the remaining were left in place for 2 to 18 hours.
Few locations within the hospital are without risk for this type of accident. The PPSA further noted that approximately 30% of retained tourniquets occurred on medical/surgical units, 14% in the ED, and 14% on inpatient and ambulatory surgical services departments. Approximately 19% were discovered when patients were transferred from one department to another.1
In the analysis of these incidents, contributing factors to forgotten tourniquets included staff failing to follow proper procedures, inadequate staff proficiency, and staff distractions and/or interruptions.1 In addition, some patients appeared to be at increased risk of having a retained tourniquet than others. Sixty percent of 125 patients with a forgotten tourniquet were aged 70 years or older, whereas some patients were younger than age 2 years.1 Not surprisingly, patients who were unable to verbally communicate (eg, patients who were intubated, under anesthesia, had expressive aphasia, severe dementia), were at the highest risk.
In a review of recovery room incidents, Salman and Asfar2 identified two cases of forgotten tourniquets out of approximately 7,000 patients. Potential strategies to avoid this mistake include: (1) only documenting procedures after they have been completed (eg, tourniquet removal); (2) double-checking that the tourniquet has been removed prior to leaving patient bedside; and (3) the use of extra-long tourniquets so the ends are more clearly visible.
Reference - Missed Cervical Spine Injury
- Looby S, Flanders A. Spine trauma. Radiol Clin North Am. 2011;49(1):129-163.
- Sekon LH, Fehlings MG. Epidemiology, demographics, and pathophysiology of acute spinal cord injury. Spine (Phila Pa 1976). 2001;26(24 Suppl):S2-S12.
- Woodring JH, Lee C. Limitations of cervical radiography in the evaluation of acute cervical trauma. J Trauma. 1993;34(1):32-39.
- Diaz JJ Jr, Gillman C, Morris JA Jr, May AK, Carrillo YM, Guy J. Are five-view plain films of the cervical spine unreliable? A prospective evaluation in blunt trauma patients with altered mental status. J Trauma. 2003;55(4):658-663.
- Parizel PM, Zijden T, Gaudino S, et al. Trauma of the spine and spinal cord: imagining strategies. Eur Spine J. 2010;19(Suppl 1):S8-S17.
- Grogan EL, Morris JA Jr, Dittus RS, et al. Cervical spine evaluation in urban trauma centers: lowering institutional costs and complications through helical CT scan. J Am Coll Surg. 2005;200(2):160-165.
Reference - Forgotten Tourniquet
- Pennsylvania Safety Advisory. Forgotten but not gone: tourniquets left on patients. PA PSRS Patient Saf Advis. 2005;2(2):19-21.
- Salman JM, Asfar SN. Recovery room incidents. Bas J Surg. 2007;24:3.
| An 83-year-old man presented to the ED via emergency medical services (EMS) with a chief complaint of neck pain. He was the restrained driver of a car that was struck from behind by another vehicle. The patient denied any head injury, loss of consciousness, chest pain, shortness of breath, or abdominal pain. His medical history was significant for hypertension and coronary artery disease, for which he was taking several medications. Regarding his social history, the patient denied alcohol consumption or cigarette smoking. |
The patient’s physical examination was unremarkable. His vital signs were normal, and there was no obvious external evidence of trauma. The posterior cervical spine was tender to palpation in the midline, but no step-off signs were appreciated. The neurological examination, including strength and sensation in all four extremities, was normal.
Since the patient’s only complaint was neck pain and his physical examination and history were otherwise normal, the emergency physician (EP) ordered radiographs of the cervical spine. The imaging studies were interpreted as showing advanced degenerative changes but no fractures, and the patient was prescribed an analgesic and discharged home.
When the patient woke up the next morning, he was unable to move his extremities, and returned to the same ED via EMS. He was placed in a cervical collar and found to have flaccid extremities on examination. A computed tomography (CT) scan of the cervical spine revealed a transverse fracture through the C6 vertebra. Radiology services also reviewed the cervical spine X-rays from the previous day, noting the presence of fracture.
The patient was taken to the operating room by neurosurgery services but remained paralyzed postoperatively. He never recovered from his injury and died 6 months later. His family sued the EP and the hospital for missed diagnosis of cervical spine fracture at the first ED presentation and the resulting paralysis. The case was settled for $1.3 million prior to trial.
Discussion
The evaluation of suspected cervical spine injury secondary to blunt trauma is a frequent and important skill practiced by EPs. Motor vehicle accidents are the most common cause of spinal cord injury in the United States (42%), followed by falls (27%), acts of violence (15%), and sports-related injuries (8%).1 A review by Sekon and Fehlings2 showed that 55% of all spinal injuries involve the cervical spine. Interestingly, the majority of cervical spine injuries occur at the upper or lower ends of the cervical spine; C2 vertebral fractures account for 33%, while C6 and C7 vertebral fractures account for approximately 50%.1
There are two commonly used criteria to clinically clear the cervical spine (ie, no imaging studies necessary) in blunt-trauma patients. The first is the National Emergency X-Radiography Use Study (NEXUS), which has a sensitivity of 99.6% of identifying cervical spine fractures.1 According to the NEXUS criteria, no imaging studies are required if: (1) there is no midline cervical spine tenderness; (2) there are no focal neurological deficits; (3) the patient exhibits a normal level of alertness; (4) the patient is not intoxicated; and (5) there is no distracting injury.1
The other set of criteria used to clear the cervical spine is the Canadian Cervical Spine Rule. In these criteria, a patient is considered at very low risk for cervical spine fracture in the following cases: (1) the patient is fully alert with a Glasgow Coma scale of 15; (2) the patient has no high-risk factors (ie, age >65 years, dangerous mechanism of injury, fall greater than five stairs, axial load to the head, high-speed vehicular crash, bicycle or motorcycle crash, or the presence of paresthesias in the extremities); (3) the patient has low-risk factors (eg, simple vehicle crash, sitting position in the ED, ambulatory at any time, delayed onset of neck pain, and the absence of midline cervical tenderness); and (4) the patient can actively rotate his or her neck 45 degrees to the left and to the right. The Canadian group found the above criteria to have 100% sensitivity for predicting the absence of cervical spine injury.1
The patient in this case failed both sets of criteria (ie, presence of cervical spine tenderness and age >65 years) and therefore required imaging. Historically, cervical spine X-ray (three views, anteroposterior, lateral, and odontoid; or five views, three views plus obliques) has been the imaging study of choice for such patients. Unfortunately, however, cervical spine radiographs have severe limitations in identifying spinal injury. In a large retrospective review, Woodring and Lee,3 found that the standard three-view cervical spine series failed to demonstrate 61% of all fractures and 36% of all subluxation and dislocations. Similarly, in a prospective study of 1,006 patients with 72 injuries, Diaz et al,4 found a 52.3% missed fracture rate when five-view radiographs were used to identify cervical spine injury. In addition, radiographic evaluation of elderly patients was found to be even more challenging in identifying cervical spine injury due to age-related degenerative changes.
Given the abovementioned limitations associated with radiographic imaging, CT scan of the cervical spine has become the imaging study of choice in moderate-to-severe risk patients with blunt cervical spine trauma. This modality has been shown to have a higher sensitivity and specificity for evaluating cervical spine injury compared to plain X-ray films, with CT detecting 97% to 100% of cervical spine fractures.5
In addition to demonstrating a higher sensitivity, CT also has the advantage of speed—especially when the patient is undergoing other CT studies (eg, head, abdomen, pelvis). While some clinicians criticize the higher cost of CT versus plain films, CT has been shown to decrease institutional costs (when settlement costs are taken into account) due to the reduction of the incidence of paralysis resulting from false-negative imaging studies.6
Forgotten Tourniquet
| A 33-year-old woman presented to the ED with a chief complaint of left-sided abdominal and flank pain. She described the onset of pain as abrupt, severe, and lasting approximately 3 hours in duration. She admitted to nausea, but no vomiting. She also denied a history of any previous similar symptoms or recent trauma. The patient’s medical history was unremarkable. Her last menstrual period began 3 days prior to presentation. Regarding social history, she denied any tobacco or alcohol use. |
The patient’s vital signs were: blood pressure, 138/82 mm Hg; heart rate, 102 beats/minute; respiratory rate, 18 breaths/minute; temperature 98.6˚F. Oxygen saturation was 99% on room air.
The patient appeared uncomfortable overall. The physical examination was remarkable only for mild left-sided costovertebral angle tenderness. Her abdomen was soft, nontender, and without guarding or rebound.
The EP ordered the placement of an intravenous (IV) line, through which the patient was administered normal saline and morphine and promethazine, respectively, for pain and nausea. A complete blood count, basic metabolic panel, urinalysis, and urine pregnancy test were ordered. All of the laboratory bloodwork results were normal, and the urine pregnancy test was negative. The urinalysis was remarkable for 50 to 100 red blood cells.
A noncontrast CT scan of the abdomen and pelvis revealed a 3-mm ureteral stone on the left side. When the patient returned from radiology services, her pain was significantly decreased and she felt much improved. She was diagnosed with a kidney stone and discharged home with an analgesic and a strainer, along with instructions to follow-up with urology services. The patient was in the ED for a total of 5 hours.
The plaintiff sued the EP and hospital, claiming that the tourniquet used to start the IV line and draw blood was never removed, which in turn caused nerve damage resulting in reflex sympathetic dystrophy and complex regional pain syndrome. The defense denied all of these allegations, and the ED personnel testified that the tourniquet was removed as soon as the IV was established. The defense cited the plaintiff’s medical records, which contained documentation that the tourniquet had been removed. The defense further argued that if the tourniquet had been left on as the patient alleged, she would have experienced obvious physical signs, such as swelling, redness, infiltration of fluids, pain, and numbness. A defense verdict was returned.
Discussion
It is very tempting to simply dismiss this case as absurd, with nothing to be learned from it. It does defy common sense that no one would have noticed the tourniquet or, at the very least, that the patient would not have spoken up about it during her stay in the ED. While the jury clearly came to the correct conclusion, it does highlight a real problem: forgotten tourniquets.
According to the Pennsylvania Patient Safety Advisory (PPSA), there were 125 reports of tourniquets being left on patients in Pennsylvania healthcare facilities in 1 year alone.1 In 5% of these cases, the tourniquet was discovered within a half hour of application. In approximately 66% of cases, the tourniquet was left on for up to 2 hours, and the remaining were left in place for 2 to 18 hours.
Few locations within the hospital are without risk for this type of accident. The PPSA further noted that approximately 30% of retained tourniquets occurred on medical/surgical units, 14% in the ED, and 14% on inpatient and ambulatory surgical services departments. Approximately 19% were discovered when patients were transferred from one department to another.1
In the analysis of these incidents, contributing factors to forgotten tourniquets included staff failing to follow proper procedures, inadequate staff proficiency, and staff distractions and/or interruptions.1 In addition, some patients appeared to be at increased risk of having a retained tourniquet than others. Sixty percent of 125 patients with a forgotten tourniquet were aged 70 years or older, whereas some patients were younger than age 2 years.1 Not surprisingly, patients who were unable to verbally communicate (eg, patients who were intubated, under anesthesia, had expressive aphasia, severe dementia), were at the highest risk.
In a review of recovery room incidents, Salman and Asfar2 identified two cases of forgotten tourniquets out of approximately 7,000 patients. Potential strategies to avoid this mistake include: (1) only documenting procedures after they have been completed (eg, tourniquet removal); (2) double-checking that the tourniquet has been removed prior to leaving patient bedside; and (3) the use of extra-long tourniquets so the ends are more clearly visible.
| An 83-year-old man presented to the ED via emergency medical services (EMS) with a chief complaint of neck pain. He was the restrained driver of a car that was struck from behind by another vehicle. The patient denied any head injury, loss of consciousness, chest pain, shortness of breath, or abdominal pain. His medical history was significant for hypertension and coronary artery disease, for which he was taking several medications. Regarding his social history, the patient denied alcohol consumption or cigarette smoking. |
The patient’s physical examination was unremarkable. His vital signs were normal, and there was no obvious external evidence of trauma. The posterior cervical spine was tender to palpation in the midline, but no step-off signs were appreciated. The neurological examination, including strength and sensation in all four extremities, was normal.
Since the patient’s only complaint was neck pain and his physical examination and history were otherwise normal, the emergency physician (EP) ordered radiographs of the cervical spine. The imaging studies were interpreted as showing advanced degenerative changes but no fractures, and the patient was prescribed an analgesic and discharged home.
When the patient woke up the next morning, he was unable to move his extremities, and returned to the same ED via EMS. He was placed in a cervical collar and found to have flaccid extremities on examination. A computed tomography (CT) scan of the cervical spine revealed a transverse fracture through the C6 vertebra. Radiology services also reviewed the cervical spine X-rays from the previous day, noting the presence of fracture.
The patient was taken to the operating room by neurosurgery services but remained paralyzed postoperatively. He never recovered from his injury and died 6 months later. His family sued the EP and the hospital for missed diagnosis of cervical spine fracture at the first ED presentation and the resulting paralysis. The case was settled for $1.3 million prior to trial.
Discussion
The evaluation of suspected cervical spine injury secondary to blunt trauma is a frequent and important skill practiced by EPs. Motor vehicle accidents are the most common cause of spinal cord injury in the United States (42%), followed by falls (27%), acts of violence (15%), and sports-related injuries (8%).1 A review by Sekon and Fehlings2 showed that 55% of all spinal injuries involve the cervical spine. Interestingly, the majority of cervical spine injuries occur at the upper or lower ends of the cervical spine; C2 vertebral fractures account for 33%, while C6 and C7 vertebral fractures account for approximately 50%.1
There are two commonly used criteria to clinically clear the cervical spine (ie, no imaging studies necessary) in blunt-trauma patients. The first is the National Emergency X-Radiography Use Study (NEXUS), which has a sensitivity of 99.6% of identifying cervical spine fractures.1 According to the NEXUS criteria, no imaging studies are required if: (1) there is no midline cervical spine tenderness; (2) there are no focal neurological deficits; (3) the patient exhibits a normal level of alertness; (4) the patient is not intoxicated; and (5) there is no distracting injury.1
The other set of criteria used to clear the cervical spine is the Canadian Cervical Spine Rule. In these criteria, a patient is considered at very low risk for cervical spine fracture in the following cases: (1) the patient is fully alert with a Glasgow Coma scale of 15; (2) the patient has no high-risk factors (ie, age >65 years, dangerous mechanism of injury, fall greater than five stairs, axial load to the head, high-speed vehicular crash, bicycle or motorcycle crash, or the presence of paresthesias in the extremities); (3) the patient has low-risk factors (eg, simple vehicle crash, sitting position in the ED, ambulatory at any time, delayed onset of neck pain, and the absence of midline cervical tenderness); and (4) the patient can actively rotate his or her neck 45 degrees to the left and to the right. The Canadian group found the above criteria to have 100% sensitivity for predicting the absence of cervical spine injury.1
The patient in this case failed both sets of criteria (ie, presence of cervical spine tenderness and age >65 years) and therefore required imaging. Historically, cervical spine X-ray (three views, anteroposterior, lateral, and odontoid; or five views, three views plus obliques) has been the imaging study of choice for such patients. Unfortunately, however, cervical spine radiographs have severe limitations in identifying spinal injury. In a large retrospective review, Woodring and Lee,3 found that the standard three-view cervical spine series failed to demonstrate 61% of all fractures and 36% of all subluxation and dislocations. Similarly, in a prospective study of 1,006 patients with 72 injuries, Diaz et al,4 found a 52.3% missed fracture rate when five-view radiographs were used to identify cervical spine injury. In addition, radiographic evaluation of elderly patients was found to be even more challenging in identifying cervical spine injury due to age-related degenerative changes.
Given the abovementioned limitations associated with radiographic imaging, CT scan of the cervical spine has become the imaging study of choice in moderate-to-severe risk patients with blunt cervical spine trauma. This modality has been shown to have a higher sensitivity and specificity for evaluating cervical spine injury compared to plain X-ray films, with CT detecting 97% to 100% of cervical spine fractures.5
In addition to demonstrating a higher sensitivity, CT also has the advantage of speed—especially when the patient is undergoing other CT studies (eg, head, abdomen, pelvis). While some clinicians criticize the higher cost of CT versus plain films, CT has been shown to decrease institutional costs (when settlement costs are taken into account) due to the reduction of the incidence of paralysis resulting from false-negative imaging studies.6
Forgotten Tourniquet
| A 33-year-old woman presented to the ED with a chief complaint of left-sided abdominal and flank pain. She described the onset of pain as abrupt, severe, and lasting approximately 3 hours in duration. She admitted to nausea, but no vomiting. She also denied a history of any previous similar symptoms or recent trauma. The patient’s medical history was unremarkable. Her last menstrual period began 3 days prior to presentation. Regarding social history, she denied any tobacco or alcohol use. |
The patient’s vital signs were: blood pressure, 138/82 mm Hg; heart rate, 102 beats/minute; respiratory rate, 18 breaths/minute; temperature 98.6˚F. Oxygen saturation was 99% on room air.
The patient appeared uncomfortable overall. The physical examination was remarkable only for mild left-sided costovertebral angle tenderness. Her abdomen was soft, nontender, and without guarding or rebound.
The EP ordered the placement of an intravenous (IV) line, through which the patient was administered normal saline and morphine and promethazine, respectively, for pain and nausea. A complete blood count, basic metabolic panel, urinalysis, and urine pregnancy test were ordered. All of the laboratory bloodwork results were normal, and the urine pregnancy test was negative. The urinalysis was remarkable for 50 to 100 red blood cells.
A noncontrast CT scan of the abdomen and pelvis revealed a 3-mm ureteral stone on the left side. When the patient returned from radiology services, her pain was significantly decreased and she felt much improved. She was diagnosed with a kidney stone and discharged home with an analgesic and a strainer, along with instructions to follow-up with urology services. The patient was in the ED for a total of 5 hours.
The plaintiff sued the EP and hospital, claiming that the tourniquet used to start the IV line and draw blood was never removed, which in turn caused nerve damage resulting in reflex sympathetic dystrophy and complex regional pain syndrome. The defense denied all of these allegations, and the ED personnel testified that the tourniquet was removed as soon as the IV was established. The defense cited the plaintiff’s medical records, which contained documentation that the tourniquet had been removed. The defense further argued that if the tourniquet had been left on as the patient alleged, she would have experienced obvious physical signs, such as swelling, redness, infiltration of fluids, pain, and numbness. A defense verdict was returned.
Discussion
It is very tempting to simply dismiss this case as absurd, with nothing to be learned from it. It does defy common sense that no one would have noticed the tourniquet or, at the very least, that the patient would not have spoken up about it during her stay in the ED. While the jury clearly came to the correct conclusion, it does highlight a real problem: forgotten tourniquets.
According to the Pennsylvania Patient Safety Advisory (PPSA), there were 125 reports of tourniquets being left on patients in Pennsylvania healthcare facilities in 1 year alone.1 In 5% of these cases, the tourniquet was discovered within a half hour of application. In approximately 66% of cases, the tourniquet was left on for up to 2 hours, and the remaining were left in place for 2 to 18 hours.
Few locations within the hospital are without risk for this type of accident. The PPSA further noted that approximately 30% of retained tourniquets occurred on medical/surgical units, 14% in the ED, and 14% on inpatient and ambulatory surgical services departments. Approximately 19% were discovered when patients were transferred from one department to another.1
In the analysis of these incidents, contributing factors to forgotten tourniquets included staff failing to follow proper procedures, inadequate staff proficiency, and staff distractions and/or interruptions.1 In addition, some patients appeared to be at increased risk of having a retained tourniquet than others. Sixty percent of 125 patients with a forgotten tourniquet were aged 70 years or older, whereas some patients were younger than age 2 years.1 Not surprisingly, patients who were unable to verbally communicate (eg, patients who were intubated, under anesthesia, had expressive aphasia, severe dementia), were at the highest risk.
In a review of recovery room incidents, Salman and Asfar2 identified two cases of forgotten tourniquets out of approximately 7,000 patients. Potential strategies to avoid this mistake include: (1) only documenting procedures after they have been completed (eg, tourniquet removal); (2) double-checking that the tourniquet has been removed prior to leaving patient bedside; and (3) the use of extra-long tourniquets so the ends are more clearly visible.
Reference - Missed Cervical Spine Injury
- Looby S, Flanders A. Spine trauma. Radiol Clin North Am. 2011;49(1):129-163.
- Sekon LH, Fehlings MG. Epidemiology, demographics, and pathophysiology of acute spinal cord injury. Spine (Phila Pa 1976). 2001;26(24 Suppl):S2-S12.
- Woodring JH, Lee C. Limitations of cervical radiography in the evaluation of acute cervical trauma. J Trauma. 1993;34(1):32-39.
- Diaz JJ Jr, Gillman C, Morris JA Jr, May AK, Carrillo YM, Guy J. Are five-view plain films of the cervical spine unreliable? A prospective evaluation in blunt trauma patients with altered mental status. J Trauma. 2003;55(4):658-663.
- Parizel PM, Zijden T, Gaudino S, et al. Trauma of the spine and spinal cord: imagining strategies. Eur Spine J. 2010;19(Suppl 1):S8-S17.
- Grogan EL, Morris JA Jr, Dittus RS, et al. Cervical spine evaluation in urban trauma centers: lowering institutional costs and complications through helical CT scan. J Am Coll Surg. 2005;200(2):160-165.
Reference - Forgotten Tourniquet
- Pennsylvania Safety Advisory. Forgotten but not gone: tourniquets left on patients. PA PSRS Patient Saf Advis. 2005;2(2):19-21.
- Salman JM, Asfar SN. Recovery room incidents. Bas J Surg. 2007;24:3.
Reference - Missed Cervical Spine Injury
- Looby S, Flanders A. Spine trauma. Radiol Clin North Am. 2011;49(1):129-163.
- Sekon LH, Fehlings MG. Epidemiology, demographics, and pathophysiology of acute spinal cord injury. Spine (Phila Pa 1976). 2001;26(24 Suppl):S2-S12.
- Woodring JH, Lee C. Limitations of cervical radiography in the evaluation of acute cervical trauma. J Trauma. 1993;34(1):32-39.
- Diaz JJ Jr, Gillman C, Morris JA Jr, May AK, Carrillo YM, Guy J. Are five-view plain films of the cervical spine unreliable? A prospective evaluation in blunt trauma patients with altered mental status. J Trauma. 2003;55(4):658-663.
- Parizel PM, Zijden T, Gaudino S, et al. Trauma of the spine and spinal cord: imagining strategies. Eur Spine J. 2010;19(Suppl 1):S8-S17.
- Grogan EL, Morris JA Jr, Dittus RS, et al. Cervical spine evaluation in urban trauma centers: lowering institutional costs and complications through helical CT scan. J Am Coll Surg. 2005;200(2):160-165.
Reference - Forgotten Tourniquet
- Pennsylvania Safety Advisory. Forgotten but not gone: tourniquets left on patients. PA PSRS Patient Saf Advis. 2005;2(2):19-21.
- Salman JM, Asfar SN. Recovery room incidents. Bas J Surg. 2007;24:3.
Malpractice Counsel: Missed Preeclampsia
Missed Preeclampsia
| A 24-year-old woman, gravida 1, para 1, aborta 0, presented to the ED complaining of a 1-day history of shortness of breath. Four days earlier, she had delivered a healthy baby boy via normal vaginal delivery and without complication. She denied chest pain, fever, or abdominal pain. She was otherwise in good health, stating that she was not taking any medications. She also denied smoking cigarettes. |
On physical examination, the patient’s vital signs were remarkable for the following: heart rate (HR), 86 beats/minute; blood pressure (BP), 164/94 mm Hg; respiratory rate, 18 breaths/minute; temperature, 98.6oF. Oxygen saturation was 96% on room air. The head, eye, ear, nose and throat examination was unremarkable. The lungs were clear to auscultation bilaterally, and HR and heart rhythm were normal. The abdomen was soft and nontender without guarding or rebound. The lower extremities were remarkable for 1+ pedal and pretibial edema bilaterally.
The patient presented to the same ED 2 days later, again with the chief complaint of shortness of breath. On examination, her BP was noted to be elevated and she had 1+ dependent edema bilaterally. Again, the EP was concerned for a PE and ordered a repeat CTA scan of the chest. This study, similar to the first, was read as normal, and showed no evidence of PE. The patient was diagnosed again with “shortness of breath of unknown etiology” and discharged home. The patient’s obstetrician-gynecologist (Ob/Gyn) was not consulted; however, the patient was encouraged to follow up with him.
The next day, the patient presented to the same ED via emergency medical services, this time with seizures; she had no prior history of a seizure disorder. On presentation to the ED, she was noted to be postictal, with an elevated BP and tachycardic with an HR of 104 beats/minute. On examination, the lungs were clear to auscultation and the lower extremities exhibited 1+ pedal and pretibial edema. A urinalysis revealed proteinuria. The patient was given 4 g of magnesium sulfate intravenously (IV) and her Ob/Gyn was consulted.
The patient was admitted to the hospital with a diagnosis of eclampsia. She was given an IV drip of magnesium and labetalol for the high BP. Unfortunately, the patient apparently had suffered an anoxic brain injury from the previous seizures and died on hospital day 3.
The family sued the treating EPs and the hospital for failure to diagnose preeclampsia on two separate ED presentations. They noted the patient’s Ob/Gyn was never consulted; no action was taken to treat the hypertension; and no urinalysis was ordered on either visit. The EPs and hospital settled the case prior to trial for several million dollars.
Discussion
This is an incredibly sad case, and the EPs and hospital were right to settle and not go to trial. While PE was a reasonable diagnosis to consider in this patient on her first ED visit, it should not have been the only one in the differential diagnosis. The EP became anchored to this single diagnosis and refused to consider other alternative diagnoses—even after the CTA scan of the chest ruled out PE. Moreover, it appears the EP either never considered the significance of the elevated BP and dependent edema or just ignored these findings. To repeat essentially the same exact workup on the second visit does not make sense—one should “cast a wider net, not the same net.”
The diagnosis of “shortness of breath of unknown etiology” is similarly unacceptable. While this is a common and accepted diagnosis when it pertains to abdominal pain, the same is not true for dyspnea.
Preeclampsia is characterized by hypertension (BP >140/90 mm Hg) and proteinuria; associated symptoms include edema and hyperreflexia. Postpartum preeclampsia occurs infrequently and can develop up to 4 weeks after delivery.1 In one 10-year retrospective case series, the incidence of preeclampsia in the postpartum period was 5.7%, and nearly 16% went on to develop eclampsia.2 In a retrospective study of 22 postpartum preeclamptic patients, the median time to presentation was 5 days postpartum.1 In a similar retrospective study of 152 patients, 90% of such patients presented within 7 days.3 The patient in this case initially presented on postpartum day 4.
Interestingly, in a study by Al-Safi et al,3 63% of postpartum preeclamptic patients had no antecedent diagnosis of hypertensive disease during pregnancy. These findings are consistent with the findings of others that 33% to 69% of such patients show no evidence of preeclampsia in the ante- or peripartum period.
The clinical presentation of postpartum preeclampsia is similar to preeclampsia complicating pregnancy after gestation week 20. In the study by Al-Safi et al,3 headache was the most common presenting symptom (69%), followed by shortness of breath (30%), blurry vision (21%), nausea (12.5%), and epigastric abdominal pain (5%). Similarly, Yancey et al1 found headache (82%) to be the most common presenting symptom in their series. Unfortunately, it is not known whether the patient in this case complained of headache or blurred vision as the published records note neither their presence nor absence.
The management of patients with preeclampsia includes IV magnesium to prevent seizures (ie, eclampsia) and BP control.1 A bolus of 4 to 6 g IV magnesium sulfate over 15 to 30 minutes is recommended, followed by an infusion of 2 g/h IV. Historically, IV hydralazine has been used to manage preeclamptic patients with a BP greater than 160/110 mm Hg. More recently, however, IV labetalol has become popular.5 All such patients require admission to the hospital with Ob/Gyn involvement.
Missed Subdural Hematoma
A 59-year-old man presented to the ED with a chief complaint of headache, the onset of which he stated started gradually 2 days prior. He noted the headache was worse than normal but without associated nausea, vomiting, fever, chills, or change in vision. His past medical history was significant for a lower extremity deep vein thrombosis 3 months prior, for which he was taking warfarin.
The patient’s vital signs were all normal. The physical examination, including a thorough neurological examination, was also normal. The EP ordered a prothrombin time (PT), an international normalized ratio (INR), and a noncontrast CT scan of the head. The PT/INR results were therapeutic at 22 seconds and 2.3. The CT scan was interpreted by radiology services as normal. The patient’s headache was treated with IV prochlorperazine and diphenhydramine. After treatment, the patient reported feeling better and was discharged home with instructions to follow up with his primary care physician.
Over the next several months, the patient presented to the same ED on seven different occasions, each time with the chief complaint of headache. At each of these presentations, the history and physical examination were documented as unremarkable, with no history of trauma. The thoroughness, however, of the documentation varied considerably for each ED encounter. No head CT scan was ordered on the subsequent seven visits, and at each presentation, the patient was treated symptomatically and discharged home.
Two days after his eighth visit to the same hospital ED, the patient presented to a different ED, again with a chief complaint of headache. The EP at this ED ordered a noncontrast CT of the head, which demonstrated a left subdural hematoma. The patient was admitted to the hospital, given IV vitamin K and fresh frozen plasma, and underwent evacuation of the hematoma by neurosurgery. The patient’s hospital course was unremarkable, and he was discharged home without any focal weakness.
The patient, however, claimed that he suffered cognitive impairment as a result of the missed diagnosis. He sued treating EPs at the first ED as well as the hospital for failure to timely diagnose the subdural hematoma, stating that a CT scan should have been performed at each of his ED visits since he was on warfarin. The defense claimed that a CT scan was not warranted for each visit, and that the timing of when and how the brain bleed started was uncertain. At trial, a defense verdict was returned.
Discussion
It is well known that patients receiving warfarin are at an increased risk for intracranial hemorrhage (ICH) following blunt head trauma.1 The recommendation is that all such patients have a noncontrast CT scan of the head to rule out intracranial bleeding. This is due to the fact that 60% of patients presenting with an immediate traumatic intracranial hemorrhage will have a normal mental status on examination; and 11% will have no history of loss of consciousness, a normal mental status examination, and no physical evidence of trauma above the clavicles.1 In a study by Hart et al,2 subdural hematoma accounted for 44% of all ICH in these types of patients.
More controversial is how to manage patients on warfarin who experience blunt head trauma and have a normal CT scan of the head. Because of the fear for delayed traumatic ICH, many clinicians recommend admitting such patients for neurological observation and repeat head CT scan the next morning.3 Additionally, some clinicians even recommend reversing the warfarin anticoagulation in such patients. 4 These recommendations, though, are based on expert consensus rather than on rigorous, prospective multicenter studies.1 These strategies are also problematic, since such multiple repeat CT scans would not only be incredibly expensive but also would expose the patient to high doses of radiation to the brain. Moreover, the Centers for Medicare and Medicaid Services has now made CT brain scan imaging of patients presenting to the ED with complaint of nontraumatic headache a quality measure they follow. Their goal is to decrease the number of “unnecessary” head CT scans.
The patient in this case denied any history of trauma on the subsequent seven ED visits. Unfortunately, as pointed out, even minor trauma can result in ICH, and patients may not recall the occurrence of the event.
For patients on warfarin who present with headache, a very careful history must be taken—including inquiring about minor traumatic events. Even then, as has been shown, patients may have not experienced a loss of consciousness, have a normal mental status examination, and exhibit no external evidence of head trauma. The clinician is forced to use her or his own best judgment when evaluating such patients in the ED.
Interestingly, the risk of ICH secondary to blunt head trauma in patients on warfarin is increased if they are on concomitant aspirin therapy.2 Similarly, the risk of ICH following head trauma in patients on clopidogrel is greater than for those patients taking warfarin,1 and the risk of ICH in patients taking dabigatran is less than if taking warfarin.2
Reference - Missed Preeclampsia
- Yancey LM, Withers E, Barnes K, Abbott J. Postpartum preeclampsia: emergency department presentation and management. J Emerg Med. 2011;40(4):380-384.
- Matthys LA, Coppage KH, Lambers DS, Barton JR, Sibai BM. Delayed postpartum preeclampsia: an experience of 151 cases. Am J Obstet Gynecol. 2004;190(5):1464-1466.
- Al-Safi Z, Imudia AN, Filetti LC, Hobson DT, Bahado-Singh RO, Awonuga AO. Delayed postpartum preeclampsia and eclampsia: demographics, clinical course, and complications. Obstet Gynecol. 2011;118(5):1102-1107.
- Chames MC, Livingston JC, Ivester TS, Barton JR, Sibai BM. Late postpartum eclampsia: a preventable disease? Am J Obstet Gynecol. 2002;186(6):1174-1177.
- Graeber B, Vanderwal T, Stiller RJ, Werdmann MJ. Late postpartum eclampsia as an obstetric complication seen in the ED. Am J Emerg Med. 2005;23(2):168-170.
Reference - Missed Subdural Hematoma
- Nishijima DK, Offerman SR, Ballard DW, et al; Clinical Research in Emergency Services and Treatment (CREST) Network. Immediate and delayed traumatic intracranial hemorrhage in patients with head trauma and preinjury warfarin or clopidogrel use. Ann Emerg Med. 2012;59(6):460-468.
- Hart RG, Diener HC, Yang S, Connolly SJ, Wallentin L, et al. Intracranial hemorrhage in atrial fibrillation patients during anticoagulation with warfarin or dabigatran: the RE-LY trial. Stroke. 2012;43(6): 1511-1517.
- Vos PE, Battistin L, Birbamer G, et al; European Federation of Neurological Societies. EFNS guideline on mild traumatic brain injury: report of an EFNS task force. Eur J Neurol. 2002;9(3):207-219.
- Coimbra R, Hoyt DB, Anjaria DJ, Potenza BM, Fortlage D, Hollingsworth-Fridlund P. Reversal of anticoagulation in trauma: a North-American survey on clinical practices among trauma surgeons. J Trauma. 2005;59(2):375-382.
Missed Preeclampsia
| A 24-year-old woman, gravida 1, para 1, aborta 0, presented to the ED complaining of a 1-day history of shortness of breath. Four days earlier, she had delivered a healthy baby boy via normal vaginal delivery and without complication. She denied chest pain, fever, or abdominal pain. She was otherwise in good health, stating that she was not taking any medications. She also denied smoking cigarettes. |
On physical examination, the patient’s vital signs were remarkable for the following: heart rate (HR), 86 beats/minute; blood pressure (BP), 164/94 mm Hg; respiratory rate, 18 breaths/minute; temperature, 98.6oF. Oxygen saturation was 96% on room air. The head, eye, ear, nose and throat examination was unremarkable. The lungs were clear to auscultation bilaterally, and HR and heart rhythm were normal. The abdomen was soft and nontender without guarding or rebound. The lower extremities were remarkable for 1+ pedal and pretibial edema bilaterally.
The patient presented to the same ED 2 days later, again with the chief complaint of shortness of breath. On examination, her BP was noted to be elevated and she had 1+ dependent edema bilaterally. Again, the EP was concerned for a PE and ordered a repeat CTA scan of the chest. This study, similar to the first, was read as normal, and showed no evidence of PE. The patient was diagnosed again with “shortness of breath of unknown etiology” and discharged home. The patient’s obstetrician-gynecologist (Ob/Gyn) was not consulted; however, the patient was encouraged to follow up with him.
The next day, the patient presented to the same ED via emergency medical services, this time with seizures; she had no prior history of a seizure disorder. On presentation to the ED, she was noted to be postictal, with an elevated BP and tachycardic with an HR of 104 beats/minute. On examination, the lungs were clear to auscultation and the lower extremities exhibited 1+ pedal and pretibial edema. A urinalysis revealed proteinuria. The patient was given 4 g of magnesium sulfate intravenously (IV) and her Ob/Gyn was consulted.
The patient was admitted to the hospital with a diagnosis of eclampsia. She was given an IV drip of magnesium and labetalol for the high BP. Unfortunately, the patient apparently had suffered an anoxic brain injury from the previous seizures and died on hospital day 3.
The family sued the treating EPs and the hospital for failure to diagnose preeclampsia on two separate ED presentations. They noted the patient’s Ob/Gyn was never consulted; no action was taken to treat the hypertension; and no urinalysis was ordered on either visit. The EPs and hospital settled the case prior to trial for several million dollars.
Discussion
This is an incredibly sad case, and the EPs and hospital were right to settle and not go to trial. While PE was a reasonable diagnosis to consider in this patient on her first ED visit, it should not have been the only one in the differential diagnosis. The EP became anchored to this single diagnosis and refused to consider other alternative diagnoses—even after the CTA scan of the chest ruled out PE. Moreover, it appears the EP either never considered the significance of the elevated BP and dependent edema or just ignored these findings. To repeat essentially the same exact workup on the second visit does not make sense—one should “cast a wider net, not the same net.”
The diagnosis of “shortness of breath of unknown etiology” is similarly unacceptable. While this is a common and accepted diagnosis when it pertains to abdominal pain, the same is not true for dyspnea.
Preeclampsia is characterized by hypertension (BP >140/90 mm Hg) and proteinuria; associated symptoms include edema and hyperreflexia. Postpartum preeclampsia occurs infrequently and can develop up to 4 weeks after delivery.1 In one 10-year retrospective case series, the incidence of preeclampsia in the postpartum period was 5.7%, and nearly 16% went on to develop eclampsia.2 In a retrospective study of 22 postpartum preeclamptic patients, the median time to presentation was 5 days postpartum.1 In a similar retrospective study of 152 patients, 90% of such patients presented within 7 days.3 The patient in this case initially presented on postpartum day 4.
Interestingly, in a study by Al-Safi et al,3 63% of postpartum preeclamptic patients had no antecedent diagnosis of hypertensive disease during pregnancy. These findings are consistent with the findings of others that 33% to 69% of such patients show no evidence of preeclampsia in the ante- or peripartum period.
The clinical presentation of postpartum preeclampsia is similar to preeclampsia complicating pregnancy after gestation week 20. In the study by Al-Safi et al,3 headache was the most common presenting symptom (69%), followed by shortness of breath (30%), blurry vision (21%), nausea (12.5%), and epigastric abdominal pain (5%). Similarly, Yancey et al1 found headache (82%) to be the most common presenting symptom in their series. Unfortunately, it is not known whether the patient in this case complained of headache or blurred vision as the published records note neither their presence nor absence.
The management of patients with preeclampsia includes IV magnesium to prevent seizures (ie, eclampsia) and BP control.1 A bolus of 4 to 6 g IV magnesium sulfate over 15 to 30 minutes is recommended, followed by an infusion of 2 g/h IV. Historically, IV hydralazine has been used to manage preeclamptic patients with a BP greater than 160/110 mm Hg. More recently, however, IV labetalol has become popular.5 All such patients require admission to the hospital with Ob/Gyn involvement.
Missed Subdural Hematoma
A 59-year-old man presented to the ED with a chief complaint of headache, the onset of which he stated started gradually 2 days prior. He noted the headache was worse than normal but without associated nausea, vomiting, fever, chills, or change in vision. His past medical history was significant for a lower extremity deep vein thrombosis 3 months prior, for which he was taking warfarin.
The patient’s vital signs were all normal. The physical examination, including a thorough neurological examination, was also normal. The EP ordered a prothrombin time (PT), an international normalized ratio (INR), and a noncontrast CT scan of the head. The PT/INR results were therapeutic at 22 seconds and 2.3. The CT scan was interpreted by radiology services as normal. The patient’s headache was treated with IV prochlorperazine and diphenhydramine. After treatment, the patient reported feeling better and was discharged home with instructions to follow up with his primary care physician.
Over the next several months, the patient presented to the same ED on seven different occasions, each time with the chief complaint of headache. At each of these presentations, the history and physical examination were documented as unremarkable, with no history of trauma. The thoroughness, however, of the documentation varied considerably for each ED encounter. No head CT scan was ordered on the subsequent seven visits, and at each presentation, the patient was treated symptomatically and discharged home.
Two days after his eighth visit to the same hospital ED, the patient presented to a different ED, again with a chief complaint of headache. The EP at this ED ordered a noncontrast CT of the head, which demonstrated a left subdural hematoma. The patient was admitted to the hospital, given IV vitamin K and fresh frozen plasma, and underwent evacuation of the hematoma by neurosurgery. The patient’s hospital course was unremarkable, and he was discharged home without any focal weakness.
The patient, however, claimed that he suffered cognitive impairment as a result of the missed diagnosis. He sued treating EPs at the first ED as well as the hospital for failure to timely diagnose the subdural hematoma, stating that a CT scan should have been performed at each of his ED visits since he was on warfarin. The defense claimed that a CT scan was not warranted for each visit, and that the timing of when and how the brain bleed started was uncertain. At trial, a defense verdict was returned.
Discussion
It is well known that patients receiving warfarin are at an increased risk for intracranial hemorrhage (ICH) following blunt head trauma.1 The recommendation is that all such patients have a noncontrast CT scan of the head to rule out intracranial bleeding. This is due to the fact that 60% of patients presenting with an immediate traumatic intracranial hemorrhage will have a normal mental status on examination; and 11% will have no history of loss of consciousness, a normal mental status examination, and no physical evidence of trauma above the clavicles.1 In a study by Hart et al,2 subdural hematoma accounted for 44% of all ICH in these types of patients.
More controversial is how to manage patients on warfarin who experience blunt head trauma and have a normal CT scan of the head. Because of the fear for delayed traumatic ICH, many clinicians recommend admitting such patients for neurological observation and repeat head CT scan the next morning.3 Additionally, some clinicians even recommend reversing the warfarin anticoagulation in such patients. 4 These recommendations, though, are based on expert consensus rather than on rigorous, prospective multicenter studies.1 These strategies are also problematic, since such multiple repeat CT scans would not only be incredibly expensive but also would expose the patient to high doses of radiation to the brain. Moreover, the Centers for Medicare and Medicaid Services has now made CT brain scan imaging of patients presenting to the ED with complaint of nontraumatic headache a quality measure they follow. Their goal is to decrease the number of “unnecessary” head CT scans.
The patient in this case denied any history of trauma on the subsequent seven ED visits. Unfortunately, as pointed out, even minor trauma can result in ICH, and patients may not recall the occurrence of the event.
For patients on warfarin who present with headache, a very careful history must be taken—including inquiring about minor traumatic events. Even then, as has been shown, patients may have not experienced a loss of consciousness, have a normal mental status examination, and exhibit no external evidence of head trauma. The clinician is forced to use her or his own best judgment when evaluating such patients in the ED.
Interestingly, the risk of ICH secondary to blunt head trauma in patients on warfarin is increased if they are on concomitant aspirin therapy.2 Similarly, the risk of ICH following head trauma in patients on clopidogrel is greater than for those patients taking warfarin,1 and the risk of ICH in patients taking dabigatran is less than if taking warfarin.2
Missed Preeclampsia
| A 24-year-old woman, gravida 1, para 1, aborta 0, presented to the ED complaining of a 1-day history of shortness of breath. Four days earlier, she had delivered a healthy baby boy via normal vaginal delivery and without complication. She denied chest pain, fever, or abdominal pain. She was otherwise in good health, stating that she was not taking any medications. She also denied smoking cigarettes. |
On physical examination, the patient’s vital signs were remarkable for the following: heart rate (HR), 86 beats/minute; blood pressure (BP), 164/94 mm Hg; respiratory rate, 18 breaths/minute; temperature, 98.6oF. Oxygen saturation was 96% on room air. The head, eye, ear, nose and throat examination was unremarkable. The lungs were clear to auscultation bilaterally, and HR and heart rhythm were normal. The abdomen was soft and nontender without guarding or rebound. The lower extremities were remarkable for 1+ pedal and pretibial edema bilaterally.
The patient presented to the same ED 2 days later, again with the chief complaint of shortness of breath. On examination, her BP was noted to be elevated and she had 1+ dependent edema bilaterally. Again, the EP was concerned for a PE and ordered a repeat CTA scan of the chest. This study, similar to the first, was read as normal, and showed no evidence of PE. The patient was diagnosed again with “shortness of breath of unknown etiology” and discharged home. The patient’s obstetrician-gynecologist (Ob/Gyn) was not consulted; however, the patient was encouraged to follow up with him.
The next day, the patient presented to the same ED via emergency medical services, this time with seizures; she had no prior history of a seizure disorder. On presentation to the ED, she was noted to be postictal, with an elevated BP and tachycardic with an HR of 104 beats/minute. On examination, the lungs were clear to auscultation and the lower extremities exhibited 1+ pedal and pretibial edema. A urinalysis revealed proteinuria. The patient was given 4 g of magnesium sulfate intravenously (IV) and her Ob/Gyn was consulted.
The patient was admitted to the hospital with a diagnosis of eclampsia. She was given an IV drip of magnesium and labetalol for the high BP. Unfortunately, the patient apparently had suffered an anoxic brain injury from the previous seizures and died on hospital day 3.
The family sued the treating EPs and the hospital for failure to diagnose preeclampsia on two separate ED presentations. They noted the patient’s Ob/Gyn was never consulted; no action was taken to treat the hypertension; and no urinalysis was ordered on either visit. The EPs and hospital settled the case prior to trial for several million dollars.
Discussion
This is an incredibly sad case, and the EPs and hospital were right to settle and not go to trial. While PE was a reasonable diagnosis to consider in this patient on her first ED visit, it should not have been the only one in the differential diagnosis. The EP became anchored to this single diagnosis and refused to consider other alternative diagnoses—even after the CTA scan of the chest ruled out PE. Moreover, it appears the EP either never considered the significance of the elevated BP and dependent edema or just ignored these findings. To repeat essentially the same exact workup on the second visit does not make sense—one should “cast a wider net, not the same net.”
The diagnosis of “shortness of breath of unknown etiology” is similarly unacceptable. While this is a common and accepted diagnosis when it pertains to abdominal pain, the same is not true for dyspnea.
Preeclampsia is characterized by hypertension (BP >140/90 mm Hg) and proteinuria; associated symptoms include edema and hyperreflexia. Postpartum preeclampsia occurs infrequently and can develop up to 4 weeks after delivery.1 In one 10-year retrospective case series, the incidence of preeclampsia in the postpartum period was 5.7%, and nearly 16% went on to develop eclampsia.2 In a retrospective study of 22 postpartum preeclamptic patients, the median time to presentation was 5 days postpartum.1 In a similar retrospective study of 152 patients, 90% of such patients presented within 7 days.3 The patient in this case initially presented on postpartum day 4.
Interestingly, in a study by Al-Safi et al,3 63% of postpartum preeclamptic patients had no antecedent diagnosis of hypertensive disease during pregnancy. These findings are consistent with the findings of others that 33% to 69% of such patients show no evidence of preeclampsia in the ante- or peripartum period.
The clinical presentation of postpartum preeclampsia is similar to preeclampsia complicating pregnancy after gestation week 20. In the study by Al-Safi et al,3 headache was the most common presenting symptom (69%), followed by shortness of breath (30%), blurry vision (21%), nausea (12.5%), and epigastric abdominal pain (5%). Similarly, Yancey et al1 found headache (82%) to be the most common presenting symptom in their series. Unfortunately, it is not known whether the patient in this case complained of headache or blurred vision as the published records note neither their presence nor absence.
The management of patients with preeclampsia includes IV magnesium to prevent seizures (ie, eclampsia) and BP control.1 A bolus of 4 to 6 g IV magnesium sulfate over 15 to 30 minutes is recommended, followed by an infusion of 2 g/h IV. Historically, IV hydralazine has been used to manage preeclamptic patients with a BP greater than 160/110 mm Hg. More recently, however, IV labetalol has become popular.5 All such patients require admission to the hospital with Ob/Gyn involvement.
Missed Subdural Hematoma
A 59-year-old man presented to the ED with a chief complaint of headache, the onset of which he stated started gradually 2 days prior. He noted the headache was worse than normal but without associated nausea, vomiting, fever, chills, or change in vision. His past medical history was significant for a lower extremity deep vein thrombosis 3 months prior, for which he was taking warfarin.
The patient’s vital signs were all normal. The physical examination, including a thorough neurological examination, was also normal. The EP ordered a prothrombin time (PT), an international normalized ratio (INR), and a noncontrast CT scan of the head. The PT/INR results were therapeutic at 22 seconds and 2.3. The CT scan was interpreted by radiology services as normal. The patient’s headache was treated with IV prochlorperazine and diphenhydramine. After treatment, the patient reported feeling better and was discharged home with instructions to follow up with his primary care physician.
Over the next several months, the patient presented to the same ED on seven different occasions, each time with the chief complaint of headache. At each of these presentations, the history and physical examination were documented as unremarkable, with no history of trauma. The thoroughness, however, of the documentation varied considerably for each ED encounter. No head CT scan was ordered on the subsequent seven visits, and at each presentation, the patient was treated symptomatically and discharged home.
Two days after his eighth visit to the same hospital ED, the patient presented to a different ED, again with a chief complaint of headache. The EP at this ED ordered a noncontrast CT of the head, which demonstrated a left subdural hematoma. The patient was admitted to the hospital, given IV vitamin K and fresh frozen plasma, and underwent evacuation of the hematoma by neurosurgery. The patient’s hospital course was unremarkable, and he was discharged home without any focal weakness.
The patient, however, claimed that he suffered cognitive impairment as a result of the missed diagnosis. He sued treating EPs at the first ED as well as the hospital for failure to timely diagnose the subdural hematoma, stating that a CT scan should have been performed at each of his ED visits since he was on warfarin. The defense claimed that a CT scan was not warranted for each visit, and that the timing of when and how the brain bleed started was uncertain. At trial, a defense verdict was returned.
Discussion
It is well known that patients receiving warfarin are at an increased risk for intracranial hemorrhage (ICH) following blunt head trauma.1 The recommendation is that all such patients have a noncontrast CT scan of the head to rule out intracranial bleeding. This is due to the fact that 60% of patients presenting with an immediate traumatic intracranial hemorrhage will have a normal mental status on examination; and 11% will have no history of loss of consciousness, a normal mental status examination, and no physical evidence of trauma above the clavicles.1 In a study by Hart et al,2 subdural hematoma accounted for 44% of all ICH in these types of patients.
More controversial is how to manage patients on warfarin who experience blunt head trauma and have a normal CT scan of the head. Because of the fear for delayed traumatic ICH, many clinicians recommend admitting such patients for neurological observation and repeat head CT scan the next morning.3 Additionally, some clinicians even recommend reversing the warfarin anticoagulation in such patients. 4 These recommendations, though, are based on expert consensus rather than on rigorous, prospective multicenter studies.1 These strategies are also problematic, since such multiple repeat CT scans would not only be incredibly expensive but also would expose the patient to high doses of radiation to the brain. Moreover, the Centers for Medicare and Medicaid Services has now made CT brain scan imaging of patients presenting to the ED with complaint of nontraumatic headache a quality measure they follow. Their goal is to decrease the number of “unnecessary” head CT scans.
The patient in this case denied any history of trauma on the subsequent seven ED visits. Unfortunately, as pointed out, even minor trauma can result in ICH, and patients may not recall the occurrence of the event.
For patients on warfarin who present with headache, a very careful history must be taken—including inquiring about minor traumatic events. Even then, as has been shown, patients may have not experienced a loss of consciousness, have a normal mental status examination, and exhibit no external evidence of head trauma. The clinician is forced to use her or his own best judgment when evaluating such patients in the ED.
Interestingly, the risk of ICH secondary to blunt head trauma in patients on warfarin is increased if they are on concomitant aspirin therapy.2 Similarly, the risk of ICH following head trauma in patients on clopidogrel is greater than for those patients taking warfarin,1 and the risk of ICH in patients taking dabigatran is less than if taking warfarin.2
Reference - Missed Preeclampsia
- Yancey LM, Withers E, Barnes K, Abbott J. Postpartum preeclampsia: emergency department presentation and management. J Emerg Med. 2011;40(4):380-384.
- Matthys LA, Coppage KH, Lambers DS, Barton JR, Sibai BM. Delayed postpartum preeclampsia: an experience of 151 cases. Am J Obstet Gynecol. 2004;190(5):1464-1466.
- Al-Safi Z, Imudia AN, Filetti LC, Hobson DT, Bahado-Singh RO, Awonuga AO. Delayed postpartum preeclampsia and eclampsia: demographics, clinical course, and complications. Obstet Gynecol. 2011;118(5):1102-1107.
- Chames MC, Livingston JC, Ivester TS, Barton JR, Sibai BM. Late postpartum eclampsia: a preventable disease? Am J Obstet Gynecol. 2002;186(6):1174-1177.
- Graeber B, Vanderwal T, Stiller RJ, Werdmann MJ. Late postpartum eclampsia as an obstetric complication seen in the ED. Am J Emerg Med. 2005;23(2):168-170.
Reference - Missed Subdural Hematoma
- Nishijima DK, Offerman SR, Ballard DW, et al; Clinical Research in Emergency Services and Treatment (CREST) Network. Immediate and delayed traumatic intracranial hemorrhage in patients with head trauma and preinjury warfarin or clopidogrel use. Ann Emerg Med. 2012;59(6):460-468.
- Hart RG, Diener HC, Yang S, Connolly SJ, Wallentin L, et al. Intracranial hemorrhage in atrial fibrillation patients during anticoagulation with warfarin or dabigatran: the RE-LY trial. Stroke. 2012;43(6): 1511-1517.
- Vos PE, Battistin L, Birbamer G, et al; European Federation of Neurological Societies. EFNS guideline on mild traumatic brain injury: report of an EFNS task force. Eur J Neurol. 2002;9(3):207-219.
- Coimbra R, Hoyt DB, Anjaria DJ, Potenza BM, Fortlage D, Hollingsworth-Fridlund P. Reversal of anticoagulation in trauma: a North-American survey on clinical practices among trauma surgeons. J Trauma. 2005;59(2):375-382.
Reference - Missed Preeclampsia
- Yancey LM, Withers E, Barnes K, Abbott J. Postpartum preeclampsia: emergency department presentation and management. J Emerg Med. 2011;40(4):380-384.
- Matthys LA, Coppage KH, Lambers DS, Barton JR, Sibai BM. Delayed postpartum preeclampsia: an experience of 151 cases. Am J Obstet Gynecol. 2004;190(5):1464-1466.
- Al-Safi Z, Imudia AN, Filetti LC, Hobson DT, Bahado-Singh RO, Awonuga AO. Delayed postpartum preeclampsia and eclampsia: demographics, clinical course, and complications. Obstet Gynecol. 2011;118(5):1102-1107.
- Chames MC, Livingston JC, Ivester TS, Barton JR, Sibai BM. Late postpartum eclampsia: a preventable disease? Am J Obstet Gynecol. 2002;186(6):1174-1177.
- Graeber B, Vanderwal T, Stiller RJ, Werdmann MJ. Late postpartum eclampsia as an obstetric complication seen in the ED. Am J Emerg Med. 2005;23(2):168-170.
Reference - Missed Subdural Hematoma
- Nishijima DK, Offerman SR, Ballard DW, et al; Clinical Research in Emergency Services and Treatment (CREST) Network. Immediate and delayed traumatic intracranial hemorrhage in patients with head trauma and preinjury warfarin or clopidogrel use. Ann Emerg Med. 2012;59(6):460-468.
- Hart RG, Diener HC, Yang S, Connolly SJ, Wallentin L, et al. Intracranial hemorrhage in atrial fibrillation patients during anticoagulation with warfarin or dabigatran: the RE-LY trial. Stroke. 2012;43(6): 1511-1517.
- Vos PE, Battistin L, Birbamer G, et al; European Federation of Neurological Societies. EFNS guideline on mild traumatic brain injury: report of an EFNS task force. Eur J Neurol. 2002;9(3):207-219.
- Coimbra R, Hoyt DB, Anjaria DJ, Potenza BM, Fortlage D, Hollingsworth-Fridlund P. Reversal of anticoagulation in trauma: a North-American survey on clinical practices among trauma surgeons. J Trauma. 2005;59(2):375-382.
Malpractice Counsel: Child abuse, methadone overdose
Missed Child Abuse
A 7-year-old girl was brought to the ED by her mother for discomfort with urination. The patient was otherwise healthy, up-to-date on all of her immunizations, and without any other complaints. Her vital signs were normal, and the physical examination was unremarkable. Although the chart did not reflect that a genitourinary examination was performed, the emergency physician (EP) stated that he had performed one.
A urinalysis was obtained, which was consistent with a bacterial infection. The patient was diagnosed with a urinary tract infection (UTI), prescribed an antibiotic, and discharged home with appropriate instructions.
Approximately 11 months later, it was discovered that the patient and her older sister were victims of sexual abuse by their 17-year-old stepbrother. Apparently, the abuse had started several months prior to the patient’s ED visit. The mother sued the EP and hospital for failure to recognize the signs and symptoms of sexual abuse. The plaintiff argued the child and mother should have been questioned about the possibility of sexual abuse, and that a more detailed physical examination would have shown evidence of abuse. The defense argued that the child’s presentation did not suggest sexual abuse; a defense verdict was returned.
Discussion
There are no reliable estimates of the incidence of pediatric sexual abuse in the United States. According to the most recent US Department of Health and Human Services Child Maltreatment Report, approximately 62,936 cases of child sexual abuse were reported in the United States in 2012, representing 9.3% of the total number of reported maltreatment cases that year.1 A meta-analysis of 22 US-based studies using national, local, and regional sampling found a much higher rate. This data suggest that 30% to 40% of girls and 13% of boys experienced sexual abuse during childhood.2
For EPs, sexually abused pediatric patients usually present in one of two ways: they are presented by a caregiver based on a suspicion or a disclosure of sexual abuse; or, in the more difficult presentation, they are brought in for evaluation of symptoms related to the genitourinary system or rectum. Such symptoms include vaginal discharge or anal or vaginal bleeding, and the presence of a sexually transmitted infection or UTI. While UTI is frequently listed as a potential sign of sexual abuse in children, there are no good data to demonstrate its frequency. Compounding this problem is that approximately 3% of girls and 1% of boys in the general population are diagnosed with a UTI prior to the onset of puberty.3 Interestingly, though most texts and articles discussing pediatric sexual abuse usually include UTI as a potential sign of abuse, reviews of UTIs in pediatric patients seldom include a discussion of sexual abuse as a potential etiology.
Emergency physicians must therefore maintain a high index of suspicion when evaluating a pediatric patient with a genitourinary or rectal complaint. If the child is old enough to give a history, the caregiver(s) should be asked to leave the room and the patient questioned directly about improper touching, physical activity, etc. The genital and perianal areas should be visually inspected. In general, a speculum examination is not necessary unless vaginal penetration is suspected or the patient is an older adolescent. The majority of pediatric patients can simply be examined in the supine, frog-leg position.
Physical signs of penetration include the presence of concavities (hymen notches), especially at the 6 o’clock position. In addition, irregularities in the hymen contour may be associated with prior injury. More obvious signs of sexual abuse include the presence of warts (condyloma acuminata or lata), vesicles, ulcers, bruising, or vaginal discharge.4 It is important to remember that the absence of physical findings does not exclude sexual abuse.
Laboratory testing of suspected victims of sexual abuse should include cultures of the vagina and rectum for gonorrhea and chlamydia, and throat cultures for gonorrhea.4 Additional testing should be based on the history and physical examination.
When an EP suspects child abuse, he or she must contact child protective services and/or law enforcement agencies, as required by law. It is imperative that the child be placed in a protected environment immediately; on occasion, this may require hospital admission.
This case emphasizes the need for EPs to at least consider sexual abuse in the pediatric patient with a genitourinary or rectal complaint.
Methadone Overdose: Intentional or Not
A 19-year-old woman presented to the ED via emergency medical services (EMS) unresponsive with shallow respirations. She had been found in her home by her grandmother. The paramedics brought the patient’s prescription medications to the ED, which included methadone, morphine, and naproxen. Reportedly, these medications had been prescribed by the patient’s family practitioner for chronic neck pain.
The patient was given intravenous naloxone (Narcan) and rapidly returned to her usual baseline. Her vital signs were normal and the physical examination was unremarkable. She told the EP that she had mistakenly taken the wrong dose of methadone, and vehemently denied any suicidal ideations or past attempts; she did not want to be admitted to the hospital. After several hours of observation, the patient remained in stable condition and without complaint. She was discharged home in the company of her grandmother, with instructions to continue her methadone, morphine, and naproxen, but to pay special attention to the dosage and frequency of use for each drug.
Four days later, the patient was found dead at home by her grandmother; the death was attributed to an overdose of methadone. The EP and hospital were sued by the plaintiff because of the discharge instructions to continue the same medication which had resulted in her first ED visit. The family practitioner was also sued for prescribing these medications to a patient with a history of drug abuse. At trial, it came to light that the patient had also probably ingested some illegally obtained hydrocodone/acetaminophen tablets (Vicodin). A defense verdict was returned.
Discussion
Deaths due to methadone overdose are becoming an increasing problem in the United States. In 2009 alone, more than 4 million prescriptions for methadone were written for pain patients.1 To place this figure in perspective, between 1997 and 2007 the number of grams of methadone prescribed in the United States increased more than 1,200%.2 According to US Centers for Disease Control and Prevention data from 2009, although methadone comprises approximately 2% of all analgesic prescription medications, it has been linked to more than 30% of overdose-related deaths due to prescription analgesics.1
Two factors contribute to this problem. Since methadone is so inexpensive, many states and insurance companies list it as the preferred opioid medication on their formularies. In addition, there is also the increased emphasis on physicians to adequately control pain. This helps explain, in part, for the dramatic increase in its use.
The second factor involves the toxicokinetics of methadone. This drug has a long and often unpredictable half-life, which can lead to toxic levels resulting in respiratory depression and death.1 Thus, methadone should only be prescribed by physicians well versed in its pharmacotherapy. Combined with the fact that there is very limited evidence supporting the use of methadone to treat acute or chronic pain unrelated to cancer, most experts agree there are better and safer alternatives.
This patient was treated appropriately in the ED regarding her resuscitation and observation. The real problem lies with the two narcotic medications she was prescribed for chronic pain. The combination of methadone and morphine in an otherwise healthy young woman probably should have raised a red flag. A conversation with the prescribing physician might have been helpful and resulted in a decrease in the dosage of one or both medications. Abrupt discontinuation, however, would not have been appropriate, since this would have resulted in opiate withdrawal and the associated effects of attending nausea, vomiting, diarrhea, diaphoresis, and abdominal cramping.
This patient was not a missed opportunity for psychiatric intervention and prevention of a suicide as there was no evidence she was ever depressed or suicidal. Rather, this was the case of a drug abuser accidently overdosing from multiple prescribed narcotic medications. It is going to take a multipronged effort to reverse this trend, including improved physician education regarding narcotic prescribing, additional resources to treat narcotic addiction, and improved identification of those at risk.
(Missed Child Abuse)
- U.S. Department of Health & Human Services. Administration on Children, Youth and Families, Administration for Children and Families Web site. Child maltreatment 2012. http://www.acf.hhs.gov/sites/default/files/cb/cm2012.pdf. Accessed October 23, 2014.
- Bolen RM, Scannapieco M. Presentation of child sexual abuse: a corrective meta-analysis. Social Serv Rev. 1999; 73(3): 281-313.
- Byerley JS, Steiner MJ: Urinary tract infection in infants and children. In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 7th ed. New York, NY: McGraw Hill Medical; 2011:854-860.
- Berkowitz CD, Claudius I, Tieder JS. Child abuse and neglect. In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 7th ed. New York, NY: McGraw Hill Medical; 2011:1976-1978.
(Methadone Overdose: Intentional or Not)
- Kuehn BM. Methadone overdose deaths rise with increased prescribing for pain. JAMA. 2012; 308(8):749-750.
- U.S. Department of Justice. Drug Enforcement Administration Office of Diversion Control Web site. Automation of reports and consolidation order system (ARCOS). http://www.deadiversion.usdoj.gov/arcos/index.html. Accessed October 23, 2014.
Missed Child Abuse
A 7-year-old girl was brought to the ED by her mother for discomfort with urination. The patient was otherwise healthy, up-to-date on all of her immunizations, and without any other complaints. Her vital signs were normal, and the physical examination was unremarkable. Although the chart did not reflect that a genitourinary examination was performed, the emergency physician (EP) stated that he had performed one.
A urinalysis was obtained, which was consistent with a bacterial infection. The patient was diagnosed with a urinary tract infection (UTI), prescribed an antibiotic, and discharged home with appropriate instructions.
Approximately 11 months later, it was discovered that the patient and her older sister were victims of sexual abuse by their 17-year-old stepbrother. Apparently, the abuse had started several months prior to the patient’s ED visit. The mother sued the EP and hospital for failure to recognize the signs and symptoms of sexual abuse. The plaintiff argued the child and mother should have been questioned about the possibility of sexual abuse, and that a more detailed physical examination would have shown evidence of abuse. The defense argued that the child’s presentation did not suggest sexual abuse; a defense verdict was returned.
Discussion
There are no reliable estimates of the incidence of pediatric sexual abuse in the United States. According to the most recent US Department of Health and Human Services Child Maltreatment Report, approximately 62,936 cases of child sexual abuse were reported in the United States in 2012, representing 9.3% of the total number of reported maltreatment cases that year.1 A meta-analysis of 22 US-based studies using national, local, and regional sampling found a much higher rate. This data suggest that 30% to 40% of girls and 13% of boys experienced sexual abuse during childhood.2
For EPs, sexually abused pediatric patients usually present in one of two ways: they are presented by a caregiver based on a suspicion or a disclosure of sexual abuse; or, in the more difficult presentation, they are brought in for evaluation of symptoms related to the genitourinary system or rectum. Such symptoms include vaginal discharge or anal or vaginal bleeding, and the presence of a sexually transmitted infection or UTI. While UTI is frequently listed as a potential sign of sexual abuse in children, there are no good data to demonstrate its frequency. Compounding this problem is that approximately 3% of girls and 1% of boys in the general population are diagnosed with a UTI prior to the onset of puberty.3 Interestingly, though most texts and articles discussing pediatric sexual abuse usually include UTI as a potential sign of abuse, reviews of UTIs in pediatric patients seldom include a discussion of sexual abuse as a potential etiology.
Emergency physicians must therefore maintain a high index of suspicion when evaluating a pediatric patient with a genitourinary or rectal complaint. If the child is old enough to give a history, the caregiver(s) should be asked to leave the room and the patient questioned directly about improper touching, physical activity, etc. The genital and perianal areas should be visually inspected. In general, a speculum examination is not necessary unless vaginal penetration is suspected or the patient is an older adolescent. The majority of pediatric patients can simply be examined in the supine, frog-leg position.
Physical signs of penetration include the presence of concavities (hymen notches), especially at the 6 o’clock position. In addition, irregularities in the hymen contour may be associated with prior injury. More obvious signs of sexual abuse include the presence of warts (condyloma acuminata or lata), vesicles, ulcers, bruising, or vaginal discharge.4 It is important to remember that the absence of physical findings does not exclude sexual abuse.
Laboratory testing of suspected victims of sexual abuse should include cultures of the vagina and rectum for gonorrhea and chlamydia, and throat cultures for gonorrhea.4 Additional testing should be based on the history and physical examination.
When an EP suspects child abuse, he or she must contact child protective services and/or law enforcement agencies, as required by law. It is imperative that the child be placed in a protected environment immediately; on occasion, this may require hospital admission.
This case emphasizes the need for EPs to at least consider sexual abuse in the pediatric patient with a genitourinary or rectal complaint.
Methadone Overdose: Intentional or Not
A 19-year-old woman presented to the ED via emergency medical services (EMS) unresponsive with shallow respirations. She had been found in her home by her grandmother. The paramedics brought the patient’s prescription medications to the ED, which included methadone, morphine, and naproxen. Reportedly, these medications had been prescribed by the patient’s family practitioner for chronic neck pain.
The patient was given intravenous naloxone (Narcan) and rapidly returned to her usual baseline. Her vital signs were normal and the physical examination was unremarkable. She told the EP that she had mistakenly taken the wrong dose of methadone, and vehemently denied any suicidal ideations or past attempts; she did not want to be admitted to the hospital. After several hours of observation, the patient remained in stable condition and without complaint. She was discharged home in the company of her grandmother, with instructions to continue her methadone, morphine, and naproxen, but to pay special attention to the dosage and frequency of use for each drug.
Four days later, the patient was found dead at home by her grandmother; the death was attributed to an overdose of methadone. The EP and hospital were sued by the plaintiff because of the discharge instructions to continue the same medication which had resulted in her first ED visit. The family practitioner was also sued for prescribing these medications to a patient with a history of drug abuse. At trial, it came to light that the patient had also probably ingested some illegally obtained hydrocodone/acetaminophen tablets (Vicodin). A defense verdict was returned.
Discussion
Deaths due to methadone overdose are becoming an increasing problem in the United States. In 2009 alone, more than 4 million prescriptions for methadone were written for pain patients.1 To place this figure in perspective, between 1997 and 2007 the number of grams of methadone prescribed in the United States increased more than 1,200%.2 According to US Centers for Disease Control and Prevention data from 2009, although methadone comprises approximately 2% of all analgesic prescription medications, it has been linked to more than 30% of overdose-related deaths due to prescription analgesics.1
Two factors contribute to this problem. Since methadone is so inexpensive, many states and insurance companies list it as the preferred opioid medication on their formularies. In addition, there is also the increased emphasis on physicians to adequately control pain. This helps explain, in part, for the dramatic increase in its use.
The second factor involves the toxicokinetics of methadone. This drug has a long and often unpredictable half-life, which can lead to toxic levels resulting in respiratory depression and death.1 Thus, methadone should only be prescribed by physicians well versed in its pharmacotherapy. Combined with the fact that there is very limited evidence supporting the use of methadone to treat acute or chronic pain unrelated to cancer, most experts agree there are better and safer alternatives.
This patient was treated appropriately in the ED regarding her resuscitation and observation. The real problem lies with the two narcotic medications she was prescribed for chronic pain. The combination of methadone and morphine in an otherwise healthy young woman probably should have raised a red flag. A conversation with the prescribing physician might have been helpful and resulted in a decrease in the dosage of one or both medications. Abrupt discontinuation, however, would not have been appropriate, since this would have resulted in opiate withdrawal and the associated effects of attending nausea, vomiting, diarrhea, diaphoresis, and abdominal cramping.
This patient was not a missed opportunity for psychiatric intervention and prevention of a suicide as there was no evidence she was ever depressed or suicidal. Rather, this was the case of a drug abuser accidently overdosing from multiple prescribed narcotic medications. It is going to take a multipronged effort to reverse this trend, including improved physician education regarding narcotic prescribing, additional resources to treat narcotic addiction, and improved identification of those at risk.
Missed Child Abuse
A 7-year-old girl was brought to the ED by her mother for discomfort with urination. The patient was otherwise healthy, up-to-date on all of her immunizations, and without any other complaints. Her vital signs were normal, and the physical examination was unremarkable. Although the chart did not reflect that a genitourinary examination was performed, the emergency physician (EP) stated that he had performed one.
A urinalysis was obtained, which was consistent with a bacterial infection. The patient was diagnosed with a urinary tract infection (UTI), prescribed an antibiotic, and discharged home with appropriate instructions.
Approximately 11 months later, it was discovered that the patient and her older sister were victims of sexual abuse by their 17-year-old stepbrother. Apparently, the abuse had started several months prior to the patient’s ED visit. The mother sued the EP and hospital for failure to recognize the signs and symptoms of sexual abuse. The plaintiff argued the child and mother should have been questioned about the possibility of sexual abuse, and that a more detailed physical examination would have shown evidence of abuse. The defense argued that the child’s presentation did not suggest sexual abuse; a defense verdict was returned.
Discussion
There are no reliable estimates of the incidence of pediatric sexual abuse in the United States. According to the most recent US Department of Health and Human Services Child Maltreatment Report, approximately 62,936 cases of child sexual abuse were reported in the United States in 2012, representing 9.3% of the total number of reported maltreatment cases that year.1 A meta-analysis of 22 US-based studies using national, local, and regional sampling found a much higher rate. This data suggest that 30% to 40% of girls and 13% of boys experienced sexual abuse during childhood.2
For EPs, sexually abused pediatric patients usually present in one of two ways: they are presented by a caregiver based on a suspicion or a disclosure of sexual abuse; or, in the more difficult presentation, they are brought in for evaluation of symptoms related to the genitourinary system or rectum. Such symptoms include vaginal discharge or anal or vaginal bleeding, and the presence of a sexually transmitted infection or UTI. While UTI is frequently listed as a potential sign of sexual abuse in children, there are no good data to demonstrate its frequency. Compounding this problem is that approximately 3% of girls and 1% of boys in the general population are diagnosed with a UTI prior to the onset of puberty.3 Interestingly, though most texts and articles discussing pediatric sexual abuse usually include UTI as a potential sign of abuse, reviews of UTIs in pediatric patients seldom include a discussion of sexual abuse as a potential etiology.
Emergency physicians must therefore maintain a high index of suspicion when evaluating a pediatric patient with a genitourinary or rectal complaint. If the child is old enough to give a history, the caregiver(s) should be asked to leave the room and the patient questioned directly about improper touching, physical activity, etc. The genital and perianal areas should be visually inspected. In general, a speculum examination is not necessary unless vaginal penetration is suspected or the patient is an older adolescent. The majority of pediatric patients can simply be examined in the supine, frog-leg position.
Physical signs of penetration include the presence of concavities (hymen notches), especially at the 6 o’clock position. In addition, irregularities in the hymen contour may be associated with prior injury. More obvious signs of sexual abuse include the presence of warts (condyloma acuminata or lata), vesicles, ulcers, bruising, or vaginal discharge.4 It is important to remember that the absence of physical findings does not exclude sexual abuse.
Laboratory testing of suspected victims of sexual abuse should include cultures of the vagina and rectum for gonorrhea and chlamydia, and throat cultures for gonorrhea.4 Additional testing should be based on the history and physical examination.
When an EP suspects child abuse, he or she must contact child protective services and/or law enforcement agencies, as required by law. It is imperative that the child be placed in a protected environment immediately; on occasion, this may require hospital admission.
This case emphasizes the need for EPs to at least consider sexual abuse in the pediatric patient with a genitourinary or rectal complaint.
Methadone Overdose: Intentional or Not
A 19-year-old woman presented to the ED via emergency medical services (EMS) unresponsive with shallow respirations. She had been found in her home by her grandmother. The paramedics brought the patient’s prescription medications to the ED, which included methadone, morphine, and naproxen. Reportedly, these medications had been prescribed by the patient’s family practitioner for chronic neck pain.
The patient was given intravenous naloxone (Narcan) and rapidly returned to her usual baseline. Her vital signs were normal and the physical examination was unremarkable. She told the EP that she had mistakenly taken the wrong dose of methadone, and vehemently denied any suicidal ideations or past attempts; she did not want to be admitted to the hospital. After several hours of observation, the patient remained in stable condition and without complaint. She was discharged home in the company of her grandmother, with instructions to continue her methadone, morphine, and naproxen, but to pay special attention to the dosage and frequency of use for each drug.
Four days later, the patient was found dead at home by her grandmother; the death was attributed to an overdose of methadone. The EP and hospital were sued by the plaintiff because of the discharge instructions to continue the same medication which had resulted in her first ED visit. The family practitioner was also sued for prescribing these medications to a patient with a history of drug abuse. At trial, it came to light that the patient had also probably ingested some illegally obtained hydrocodone/acetaminophen tablets (Vicodin). A defense verdict was returned.
Discussion
Deaths due to methadone overdose are becoming an increasing problem in the United States. In 2009 alone, more than 4 million prescriptions for methadone were written for pain patients.1 To place this figure in perspective, between 1997 and 2007 the number of grams of methadone prescribed in the United States increased more than 1,200%.2 According to US Centers for Disease Control and Prevention data from 2009, although methadone comprises approximately 2% of all analgesic prescription medications, it has been linked to more than 30% of overdose-related deaths due to prescription analgesics.1
Two factors contribute to this problem. Since methadone is so inexpensive, many states and insurance companies list it as the preferred opioid medication on their formularies. In addition, there is also the increased emphasis on physicians to adequately control pain. This helps explain, in part, for the dramatic increase in its use.
The second factor involves the toxicokinetics of methadone. This drug has a long and often unpredictable half-life, which can lead to toxic levels resulting in respiratory depression and death.1 Thus, methadone should only be prescribed by physicians well versed in its pharmacotherapy. Combined with the fact that there is very limited evidence supporting the use of methadone to treat acute or chronic pain unrelated to cancer, most experts agree there are better and safer alternatives.
This patient was treated appropriately in the ED regarding her resuscitation and observation. The real problem lies with the two narcotic medications she was prescribed for chronic pain. The combination of methadone and morphine in an otherwise healthy young woman probably should have raised a red flag. A conversation with the prescribing physician might have been helpful and resulted in a decrease in the dosage of one or both medications. Abrupt discontinuation, however, would not have been appropriate, since this would have resulted in opiate withdrawal and the associated effects of attending nausea, vomiting, diarrhea, diaphoresis, and abdominal cramping.
This patient was not a missed opportunity for psychiatric intervention and prevention of a suicide as there was no evidence she was ever depressed or suicidal. Rather, this was the case of a drug abuser accidently overdosing from multiple prescribed narcotic medications. It is going to take a multipronged effort to reverse this trend, including improved physician education regarding narcotic prescribing, additional resources to treat narcotic addiction, and improved identification of those at risk.
(Missed Child Abuse)
- U.S. Department of Health & Human Services. Administration on Children, Youth and Families, Administration for Children and Families Web site. Child maltreatment 2012. http://www.acf.hhs.gov/sites/default/files/cb/cm2012.pdf. Accessed October 23, 2014.
- Bolen RM, Scannapieco M. Presentation of child sexual abuse: a corrective meta-analysis. Social Serv Rev. 1999; 73(3): 281-313.
- Byerley JS, Steiner MJ: Urinary tract infection in infants and children. In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 7th ed. New York, NY: McGraw Hill Medical; 2011:854-860.
- Berkowitz CD, Claudius I, Tieder JS. Child abuse and neglect. In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 7th ed. New York, NY: McGraw Hill Medical; 2011:1976-1978.
(Methadone Overdose: Intentional or Not)
- Kuehn BM. Methadone overdose deaths rise with increased prescribing for pain. JAMA. 2012; 308(8):749-750.
- U.S. Department of Justice. Drug Enforcement Administration Office of Diversion Control Web site. Automation of reports and consolidation order system (ARCOS). http://www.deadiversion.usdoj.gov/arcos/index.html. Accessed October 23, 2014.
(Missed Child Abuse)
- U.S. Department of Health & Human Services. Administration on Children, Youth and Families, Administration for Children and Families Web site. Child maltreatment 2012. http://www.acf.hhs.gov/sites/default/files/cb/cm2012.pdf. Accessed October 23, 2014.
- Bolen RM, Scannapieco M. Presentation of child sexual abuse: a corrective meta-analysis. Social Serv Rev. 1999; 73(3): 281-313.
- Byerley JS, Steiner MJ: Urinary tract infection in infants and children. In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 7th ed. New York, NY: McGraw Hill Medical; 2011:854-860.
- Berkowitz CD, Claudius I, Tieder JS. Child abuse and neglect. In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 7th ed. New York, NY: McGraw Hill Medical; 2011:1976-1978.
(Methadone Overdose: Intentional or Not)
- Kuehn BM. Methadone overdose deaths rise with increased prescribing for pain. JAMA. 2012; 308(8):749-750.
- U.S. Department of Justice. Drug Enforcement Administration Office of Diversion Control Web site. Automation of reports and consolidation order system (ARCOS). http://www.deadiversion.usdoj.gov/arcos/index.html. Accessed October 23, 2014.
Malpractice Counsel
Aortic Rupture
A 59-year-old woman involved in a motor vehicle crash presented to the ED via emergency medical services. The patient had been the front-seat passenger and was wearing a seat belt. She complained of chest wall pain, but denied head injury, loss of consciousness, neck pain, abdominal pain, or shortness of breath. Her past medical history was unremarkable.
A chest X-ray was performed and interpreted as normal by the attending radiologist. Laboratory studies were normal except for mild anemia. The patient was discharged from the hospital with a diagnosis of chest wall contusion. She died 36 hours later from a ruptured thoracic aorta. The family of the patient brought a malpractice suit against the emergency physician (EP) for failing to diagnose and treat acute aortic rupture. At trial, a defense verdict was returned.
Discussion
Aortic rupture from blunt trauma is a devastating injury. More than 90% of patients who have sustained this type of injury in a motor vehicle crash die at the scene.1 For the remaining 10%, 50% die within the following 24 hours.1 The injury occurs in the proximal descending aorta, secondary to the fixation of the vessels between the left subclavian artery and the ligamentum arteriosum; the cause in approximately 80% to 90% of cases is due to blunt trauma. Involvement of the ascending aorta is much less common. Many patients, such as the one in this case, exhibit no external physical findings of injury. Chest pain is the most frequent complaint, followed by dyspnea—both fairly nonspecific symptoms. Physical findings that should raise a suspicion for a thoracic aortic injury include hypotension, hypertension in the upper extremity and hypotension in the lower extremity, unequal BPs in the extremities, external evidence of chest wall trauma, and palpable fractures of the sternum and ribs.2 While it is unclear if this patient had unequal extremity BPs, she did not have any of the other classic findings of aortic rupture. Associated neurological, abdominal, or orthopedic injuries are frequently present as well, and can mask the subtle signs of aortic rupture.
A chest radiograph is often the initial screening test used to evaluate for possible thoracic aortic injury. Suspicious findings include a widened mediastinum (greater than 8 cm), right-sided deviation of the esophagus, depression of the left mainstem bronchus, loss of the aortic knob, and an apical pleural cap. Unfortunately, chest X-ray can be normal, and a normal mediastinum on the radiograph does not exclude the diagnosis.
For patients with suspected thoracic aortic injury, helical computed tomography with angiography is the study of choice. It can accurately identify operative and nonoperative lesions, as well as associated injuries (eg, small pneumothorax, rib fractures). Magnetic resonance angiography provides similar sensitivity and specificity, but is not practical for the majority of trauma patients. Occasionally, aortography can be considered when the CT scan results are indeterminate and when thought to be needed to plan operative intervention. Finally, transesophageal echocardiography can be considered in hemodynamically unstable patients unable to be transferred to the radiology suite.
For most patients, immediate operative intervention is the definitive treatment. For patients with suspected thoracic aortic injury and hypertension, shear forces need to be decreased just as they are for patients with aortic dissection. A short-acting β-blocker like intravenous (IV) esmolol can be used initially to slow HR. Then, an IV arterial vasodilator can be given to decrease BP. To prevent rebound tachycardia and increased shear forces, the β-blocker should always be initiated before the vasodilator is given. Vital-sign targets include an HR of 60 beats/minute and a systolic BP in the range of 100 to 120 mm Hg.
This was a very atypical presentation of a devastating injury. Given the benign presentation, lack of associated injuries, and the normal chest X-ray, a defense verdict appears to be the correct one in this very unfortunate case.
Foot Drop
A 20-year-old woman presented to the ED complaining of severe numbness, tingling, and pain in her left calf. According to the patient, she had attended a New Year’s Eve party, where she spent much of the time dancing. She was awakened by calf pain on the following morning and sought treatment at the ED.
On physical examination, the patient’s vital signs were normal. Examination of the left calf revealed tenderness to palpation; no swelling was noted. The patient was unable to lift her left foot or bear weight on the left leg. She had normal dorsalis pedis and posterior tibial pulses in the affected leg. The remainder of her examination was normal and no testing was performed. The patient was diagnosed with “floppy foot syndrome” and discharged home with a prescription for a nonsteroidal anti-inflammatory drug.
The next day, the patient presented to a different ED because of worsening pain and swelling of the calf. She was admitted to the hospital and the orthopedic service was consulted. The patient was diagnosed with compartment syndrome; however, by that time her condition was complicated by rhabdomyolysis, resulting in acute renal failure.
The patient underwent a fasciotomy. After surgery, she required hemodialysis until her kidney function returned. She had damage to the nerves in her left calf and leg resulting in a permanent foot drop that required prolonged physical therapy following her hospitalization.
The patient sued the initial EP for failure to diagnose compartment syndrome, which resulted in permanent nerve damage and foot drop. A $750,000 settlement was reached.
Discussion
The EP did not appear to have taken this case seriously, as “floppy foot syndrome” is not a recognized diagnosis. No significance was attached to the presence of the foot drop, which is an objective and concerning physical finding.
The differential diagnoses of foot drop are relatively small: a nerve injury, which is the most common cause; a central nervous system event, such as a stroke; or a muscular disorder.3 An injury or problem with the peroneal nerve is the most common cause of foot drop.
While the patient’s history was not typical for the development of compartment syndrome, she potentially participated in strenuous physical activity, which can result in muscle swelling and subsequent compartment syndrome.4 The pain from compartment syndrome is typically described as out of proportion to physical findings; this seems to have been the case for this patient.
The symptoms and findings of compartment syndrome are classically taught as the five “Ps”: pain, paresthesias, paralysis, pallor, and pulselessness, with the symptoms typically presenting in this order. The patient had the first three symptoms, but they were not appreciated in the initial evaluation. Pulselessness is usually the last finding to develop, and tissue damage is frequently present at that point.
Interestingly, approximately 40% of compartment syndromes occur at the level of the tibia and fibula. The lower leg has four compartments: the anterior, which contains the anterior tibial artery and deep peroneal nerve; the lateral, which contains the superficial peroneal nerve; the superficial posterior, which contains the sural nerve; and the deep posterior, which contains the posterior tibial artery and nerve.
As pressure within the enclosed space increases due to swelling, hemorrhage, fracture, etc, the blood supply as well as nerve and muscle functions become compromised. Left untreated, the increased pressure can result in permanent tissue and nerve damage.
Compartment syndrome is a time sensitive diagnosis because of the need for surgical intervention to open the compartment. The EP can measure compartment pressures if he or she has the right equipment and training. A normal compartment pressure is less than 10 mm Hg. When the compartment pressure begins to exceed 30 mm Hg, tissue damage can occur. If unable to measure compartment pressure, an emergent orthopedic consult is indicated.
- Chiesa R, de Moura MR, Lucci C, et al. Traumatic rupture of the thoracic aorta. Acta Chir Belq. 2003;103(4):364-374.
- Ross C, Schwab TM. Cardiac trauma. In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD. Ross C. In: Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 7th ed. New York, NY: McGraw Hill Medical; 2011:1758-1765.
- Ricarte IF, Figueiredo MM, Fukuda TG, Pedroso JL, Silva GS. Acute foot drop syndrome mimicking peroneal nerve injury: an atypical presentation of ischemic stroke. J Stroke Cerebrovasc Dis. 2014:23(5):1229-1231.
- Aliano K, Gulati S, Stavrides S, Davenport T, Hines G. Low-impact trauma causing acute compartment syndrome of the lower extremities. Am J Emerg Med. 2013;31(5):890.e3-e4.
Aortic Rupture
A 59-year-old woman involved in a motor vehicle crash presented to the ED via emergency medical services. The patient had been the front-seat passenger and was wearing a seat belt. She complained of chest wall pain, but denied head injury, loss of consciousness, neck pain, abdominal pain, or shortness of breath. Her past medical history was unremarkable.
A chest X-ray was performed and interpreted as normal by the attending radiologist. Laboratory studies were normal except for mild anemia. The patient was discharged from the hospital with a diagnosis of chest wall contusion. She died 36 hours later from a ruptured thoracic aorta. The family of the patient brought a malpractice suit against the emergency physician (EP) for failing to diagnose and treat acute aortic rupture. At trial, a defense verdict was returned.
Discussion
Aortic rupture from blunt trauma is a devastating injury. More than 90% of patients who have sustained this type of injury in a motor vehicle crash die at the scene.1 For the remaining 10%, 50% die within the following 24 hours.1 The injury occurs in the proximal descending aorta, secondary to the fixation of the vessels between the left subclavian artery and the ligamentum arteriosum; the cause in approximately 80% to 90% of cases is due to blunt trauma. Involvement of the ascending aorta is much less common. Many patients, such as the one in this case, exhibit no external physical findings of injury. Chest pain is the most frequent complaint, followed by dyspnea—both fairly nonspecific symptoms. Physical findings that should raise a suspicion for a thoracic aortic injury include hypotension, hypertension in the upper extremity and hypotension in the lower extremity, unequal BPs in the extremities, external evidence of chest wall trauma, and palpable fractures of the sternum and ribs.2 While it is unclear if this patient had unequal extremity BPs, she did not have any of the other classic findings of aortic rupture. Associated neurological, abdominal, or orthopedic injuries are frequently present as well, and can mask the subtle signs of aortic rupture.
A chest radiograph is often the initial screening test used to evaluate for possible thoracic aortic injury. Suspicious findings include a widened mediastinum (greater than 8 cm), right-sided deviation of the esophagus, depression of the left mainstem bronchus, loss of the aortic knob, and an apical pleural cap. Unfortunately, chest X-ray can be normal, and a normal mediastinum on the radiograph does not exclude the diagnosis.
For patients with suspected thoracic aortic injury, helical computed tomography with angiography is the study of choice. It can accurately identify operative and nonoperative lesions, as well as associated injuries (eg, small pneumothorax, rib fractures). Magnetic resonance angiography provides similar sensitivity and specificity, but is not practical for the majority of trauma patients. Occasionally, aortography can be considered when the CT scan results are indeterminate and when thought to be needed to plan operative intervention. Finally, transesophageal echocardiography can be considered in hemodynamically unstable patients unable to be transferred to the radiology suite.
For most patients, immediate operative intervention is the definitive treatment. For patients with suspected thoracic aortic injury and hypertension, shear forces need to be decreased just as they are for patients with aortic dissection. A short-acting β-blocker like intravenous (IV) esmolol can be used initially to slow HR. Then, an IV arterial vasodilator can be given to decrease BP. To prevent rebound tachycardia and increased shear forces, the β-blocker should always be initiated before the vasodilator is given. Vital-sign targets include an HR of 60 beats/minute and a systolic BP in the range of 100 to 120 mm Hg.
This was a very atypical presentation of a devastating injury. Given the benign presentation, lack of associated injuries, and the normal chest X-ray, a defense verdict appears to be the correct one in this very unfortunate case.
Foot Drop
A 20-year-old woman presented to the ED complaining of severe numbness, tingling, and pain in her left calf. According to the patient, she had attended a New Year’s Eve party, where she spent much of the time dancing. She was awakened by calf pain on the following morning and sought treatment at the ED.
On physical examination, the patient’s vital signs were normal. Examination of the left calf revealed tenderness to palpation; no swelling was noted. The patient was unable to lift her left foot or bear weight on the left leg. She had normal dorsalis pedis and posterior tibial pulses in the affected leg. The remainder of her examination was normal and no testing was performed. The patient was diagnosed with “floppy foot syndrome” and discharged home with a prescription for a nonsteroidal anti-inflammatory drug.
The next day, the patient presented to a different ED because of worsening pain and swelling of the calf. She was admitted to the hospital and the orthopedic service was consulted. The patient was diagnosed with compartment syndrome; however, by that time her condition was complicated by rhabdomyolysis, resulting in acute renal failure.
The patient underwent a fasciotomy. After surgery, she required hemodialysis until her kidney function returned. She had damage to the nerves in her left calf and leg resulting in a permanent foot drop that required prolonged physical therapy following her hospitalization.
The patient sued the initial EP for failure to diagnose compartment syndrome, which resulted in permanent nerve damage and foot drop. A $750,000 settlement was reached.
Discussion
The EP did not appear to have taken this case seriously, as “floppy foot syndrome” is not a recognized diagnosis. No significance was attached to the presence of the foot drop, which is an objective and concerning physical finding.
The differential diagnoses of foot drop are relatively small: a nerve injury, which is the most common cause; a central nervous system event, such as a stroke; or a muscular disorder.3 An injury or problem with the peroneal nerve is the most common cause of foot drop.
While the patient’s history was not typical for the development of compartment syndrome, she potentially participated in strenuous physical activity, which can result in muscle swelling and subsequent compartment syndrome.4 The pain from compartment syndrome is typically described as out of proportion to physical findings; this seems to have been the case for this patient.
The symptoms and findings of compartment syndrome are classically taught as the five “Ps”: pain, paresthesias, paralysis, pallor, and pulselessness, with the symptoms typically presenting in this order. The patient had the first three symptoms, but they were not appreciated in the initial evaluation. Pulselessness is usually the last finding to develop, and tissue damage is frequently present at that point.
Interestingly, approximately 40% of compartment syndromes occur at the level of the tibia and fibula. The lower leg has four compartments: the anterior, which contains the anterior tibial artery and deep peroneal nerve; the lateral, which contains the superficial peroneal nerve; the superficial posterior, which contains the sural nerve; and the deep posterior, which contains the posterior tibial artery and nerve.
As pressure within the enclosed space increases due to swelling, hemorrhage, fracture, etc, the blood supply as well as nerve and muscle functions become compromised. Left untreated, the increased pressure can result in permanent tissue and nerve damage.
Compartment syndrome is a time sensitive diagnosis because of the need for surgical intervention to open the compartment. The EP can measure compartment pressures if he or she has the right equipment and training. A normal compartment pressure is less than 10 mm Hg. When the compartment pressure begins to exceed 30 mm Hg, tissue damage can occur. If unable to measure compartment pressure, an emergent orthopedic consult is indicated.
Aortic Rupture
A 59-year-old woman involved in a motor vehicle crash presented to the ED via emergency medical services. The patient had been the front-seat passenger and was wearing a seat belt. She complained of chest wall pain, but denied head injury, loss of consciousness, neck pain, abdominal pain, or shortness of breath. Her past medical history was unremarkable.
A chest X-ray was performed and interpreted as normal by the attending radiologist. Laboratory studies were normal except for mild anemia. The patient was discharged from the hospital with a diagnosis of chest wall contusion. She died 36 hours later from a ruptured thoracic aorta. The family of the patient brought a malpractice suit against the emergency physician (EP) for failing to diagnose and treat acute aortic rupture. At trial, a defense verdict was returned.
Discussion
Aortic rupture from blunt trauma is a devastating injury. More than 90% of patients who have sustained this type of injury in a motor vehicle crash die at the scene.1 For the remaining 10%, 50% die within the following 24 hours.1 The injury occurs in the proximal descending aorta, secondary to the fixation of the vessels between the left subclavian artery and the ligamentum arteriosum; the cause in approximately 80% to 90% of cases is due to blunt trauma. Involvement of the ascending aorta is much less common. Many patients, such as the one in this case, exhibit no external physical findings of injury. Chest pain is the most frequent complaint, followed by dyspnea—both fairly nonspecific symptoms. Physical findings that should raise a suspicion for a thoracic aortic injury include hypotension, hypertension in the upper extremity and hypotension in the lower extremity, unequal BPs in the extremities, external evidence of chest wall trauma, and palpable fractures of the sternum and ribs.2 While it is unclear if this patient had unequal extremity BPs, she did not have any of the other classic findings of aortic rupture. Associated neurological, abdominal, or orthopedic injuries are frequently present as well, and can mask the subtle signs of aortic rupture.
A chest radiograph is often the initial screening test used to evaluate for possible thoracic aortic injury. Suspicious findings include a widened mediastinum (greater than 8 cm), right-sided deviation of the esophagus, depression of the left mainstem bronchus, loss of the aortic knob, and an apical pleural cap. Unfortunately, chest X-ray can be normal, and a normal mediastinum on the radiograph does not exclude the diagnosis.
For patients with suspected thoracic aortic injury, helical computed tomography with angiography is the study of choice. It can accurately identify operative and nonoperative lesions, as well as associated injuries (eg, small pneumothorax, rib fractures). Magnetic resonance angiography provides similar sensitivity and specificity, but is not practical for the majority of trauma patients. Occasionally, aortography can be considered when the CT scan results are indeterminate and when thought to be needed to plan operative intervention. Finally, transesophageal echocardiography can be considered in hemodynamically unstable patients unable to be transferred to the radiology suite.
For most patients, immediate operative intervention is the definitive treatment. For patients with suspected thoracic aortic injury and hypertension, shear forces need to be decreased just as they are for patients with aortic dissection. A short-acting β-blocker like intravenous (IV) esmolol can be used initially to slow HR. Then, an IV arterial vasodilator can be given to decrease BP. To prevent rebound tachycardia and increased shear forces, the β-blocker should always be initiated before the vasodilator is given. Vital-sign targets include an HR of 60 beats/minute and a systolic BP in the range of 100 to 120 mm Hg.
This was a very atypical presentation of a devastating injury. Given the benign presentation, lack of associated injuries, and the normal chest X-ray, a defense verdict appears to be the correct one in this very unfortunate case.
Foot Drop
A 20-year-old woman presented to the ED complaining of severe numbness, tingling, and pain in her left calf. According to the patient, she had attended a New Year’s Eve party, where she spent much of the time dancing. She was awakened by calf pain on the following morning and sought treatment at the ED.
On physical examination, the patient’s vital signs were normal. Examination of the left calf revealed tenderness to palpation; no swelling was noted. The patient was unable to lift her left foot or bear weight on the left leg. She had normal dorsalis pedis and posterior tibial pulses in the affected leg. The remainder of her examination was normal and no testing was performed. The patient was diagnosed with “floppy foot syndrome” and discharged home with a prescription for a nonsteroidal anti-inflammatory drug.
The next day, the patient presented to a different ED because of worsening pain and swelling of the calf. She was admitted to the hospital and the orthopedic service was consulted. The patient was diagnosed with compartment syndrome; however, by that time her condition was complicated by rhabdomyolysis, resulting in acute renal failure.
The patient underwent a fasciotomy. After surgery, she required hemodialysis until her kidney function returned. She had damage to the nerves in her left calf and leg resulting in a permanent foot drop that required prolonged physical therapy following her hospitalization.
The patient sued the initial EP for failure to diagnose compartment syndrome, which resulted in permanent nerve damage and foot drop. A $750,000 settlement was reached.
Discussion
The EP did not appear to have taken this case seriously, as “floppy foot syndrome” is not a recognized diagnosis. No significance was attached to the presence of the foot drop, which is an objective and concerning physical finding.
The differential diagnoses of foot drop are relatively small: a nerve injury, which is the most common cause; a central nervous system event, such as a stroke; or a muscular disorder.3 An injury or problem with the peroneal nerve is the most common cause of foot drop.
While the patient’s history was not typical for the development of compartment syndrome, she potentially participated in strenuous physical activity, which can result in muscle swelling and subsequent compartment syndrome.4 The pain from compartment syndrome is typically described as out of proportion to physical findings; this seems to have been the case for this patient.
The symptoms and findings of compartment syndrome are classically taught as the five “Ps”: pain, paresthesias, paralysis, pallor, and pulselessness, with the symptoms typically presenting in this order. The patient had the first three symptoms, but they were not appreciated in the initial evaluation. Pulselessness is usually the last finding to develop, and tissue damage is frequently present at that point.
Interestingly, approximately 40% of compartment syndromes occur at the level of the tibia and fibula. The lower leg has four compartments: the anterior, which contains the anterior tibial artery and deep peroneal nerve; the lateral, which contains the superficial peroneal nerve; the superficial posterior, which contains the sural nerve; and the deep posterior, which contains the posterior tibial artery and nerve.
As pressure within the enclosed space increases due to swelling, hemorrhage, fracture, etc, the blood supply as well as nerve and muscle functions become compromised. Left untreated, the increased pressure can result in permanent tissue and nerve damage.
Compartment syndrome is a time sensitive diagnosis because of the need for surgical intervention to open the compartment. The EP can measure compartment pressures if he or she has the right equipment and training. A normal compartment pressure is less than 10 mm Hg. When the compartment pressure begins to exceed 30 mm Hg, tissue damage can occur. If unable to measure compartment pressure, an emergent orthopedic consult is indicated.
- Chiesa R, de Moura MR, Lucci C, et al. Traumatic rupture of the thoracic aorta. Acta Chir Belq. 2003;103(4):364-374.
- Ross C, Schwab TM. Cardiac trauma. In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD. Ross C. In: Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 7th ed. New York, NY: McGraw Hill Medical; 2011:1758-1765.
- Ricarte IF, Figueiredo MM, Fukuda TG, Pedroso JL, Silva GS. Acute foot drop syndrome mimicking peroneal nerve injury: an atypical presentation of ischemic stroke. J Stroke Cerebrovasc Dis. 2014:23(5):1229-1231.
- Aliano K, Gulati S, Stavrides S, Davenport T, Hines G. Low-impact trauma causing acute compartment syndrome of the lower extremities. Am J Emerg Med. 2013;31(5):890.e3-e4.
- Chiesa R, de Moura MR, Lucci C, et al. Traumatic rupture of the thoracic aorta. Acta Chir Belq. 2003;103(4):364-374.
- Ross C, Schwab TM. Cardiac trauma. In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD. Ross C. In: Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 7th ed. New York, NY: McGraw Hill Medical; 2011:1758-1765.
- Ricarte IF, Figueiredo MM, Fukuda TG, Pedroso JL, Silva GS. Acute foot drop syndrome mimicking peroneal nerve injury: an atypical presentation of ischemic stroke. J Stroke Cerebrovasc Dis. 2014:23(5):1229-1231.
- Aliano K, Gulati S, Stavrides S, Davenport T, Hines G. Low-impact trauma causing acute compartment syndrome of the lower extremities. Am J Emerg Med. 2013;31(5):890.e3-e4.