User login
Dear patients: Letters psychiatrists should and should not write
After several months of difficulty living in her current apartment complex, Ms. M asks you as her psychiatrist to write a letter to the management company requesting she be moved to an apartment on the opposite side of the maintenance closet because the noise aggravates her posttraumatic stress disorder. What should you consider when asked to write such a letter?
Psychiatric practice often extends beyond the treatment of mental illness to include addressing patients’ social well-being. Psychiatrists commonly inquire about a patient’s social situation to understand the impact of these environmental factors. Similarly, psychiatric illness may affect a patient’s ability to work or fulfill responsibilities. As a result, patients may ask their psychiatrists for assistance by requesting letters that address various aspects of their social well-being.1 These communications may address an array of topics, from a patient’s readiness to return to work to their ability to pay child support. This article focuses on the role psychiatrists have in writing patient-requested letters across a variety of topics, including the consideration of potential legal liability and ethical implications.
Types of letters
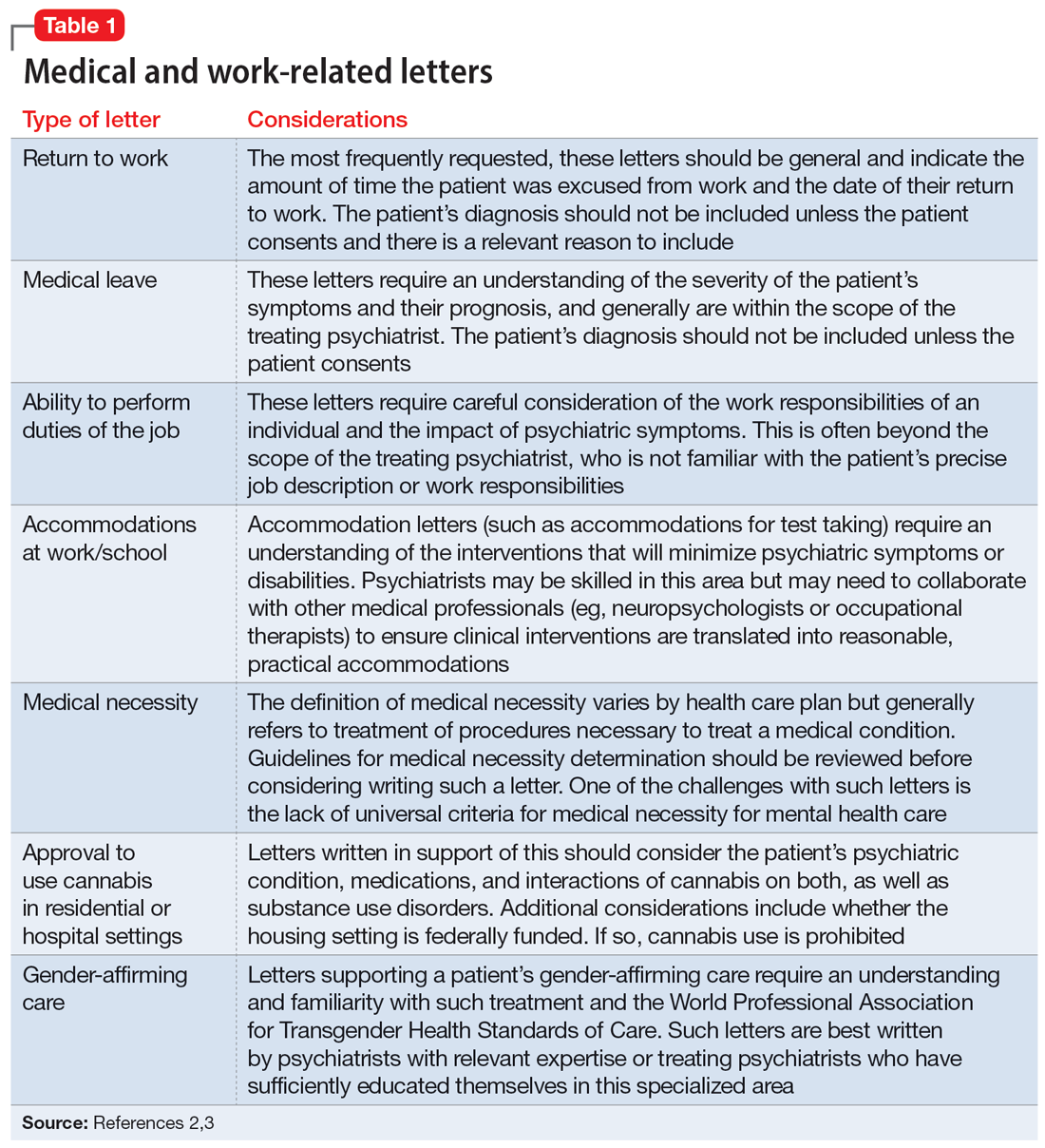
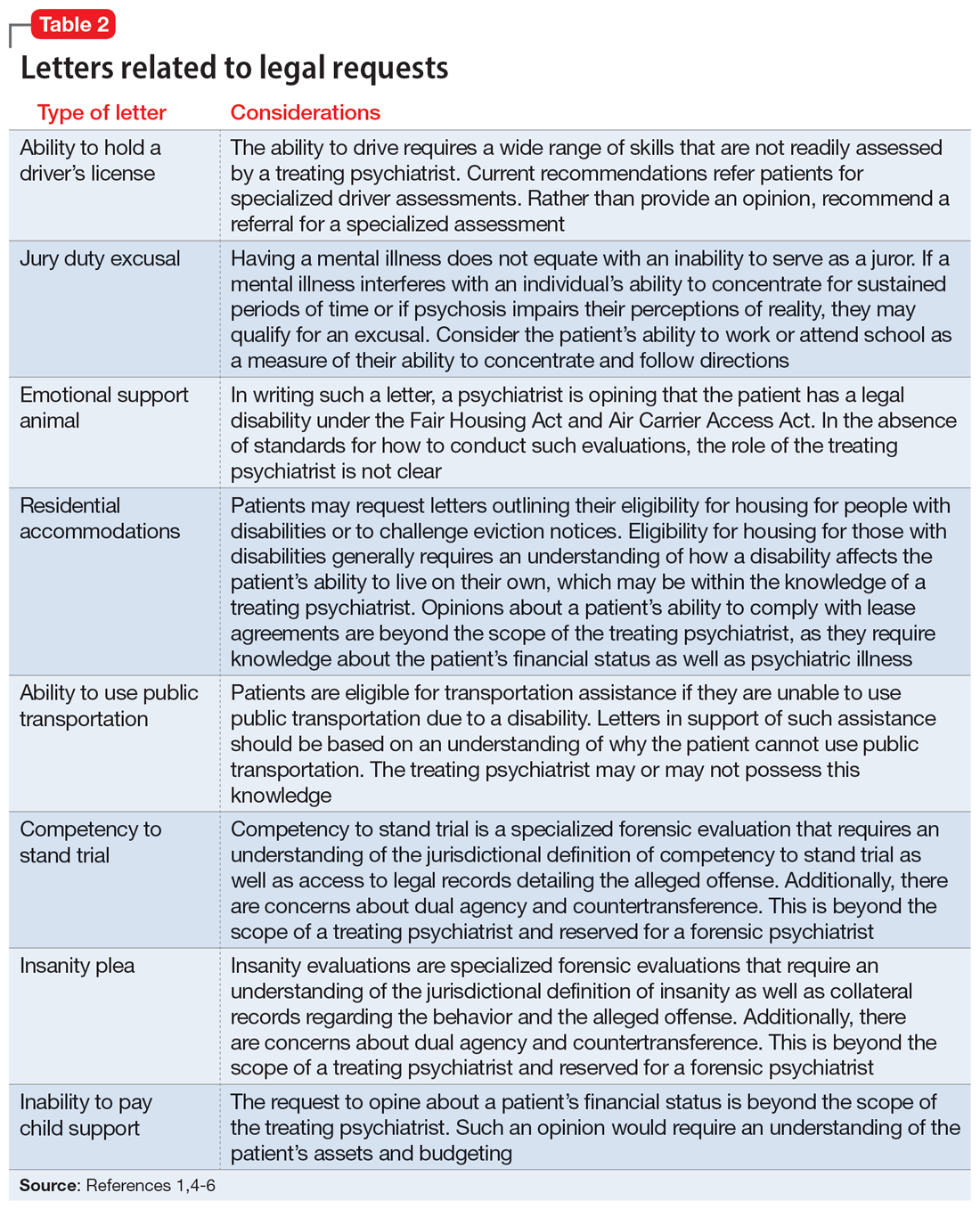
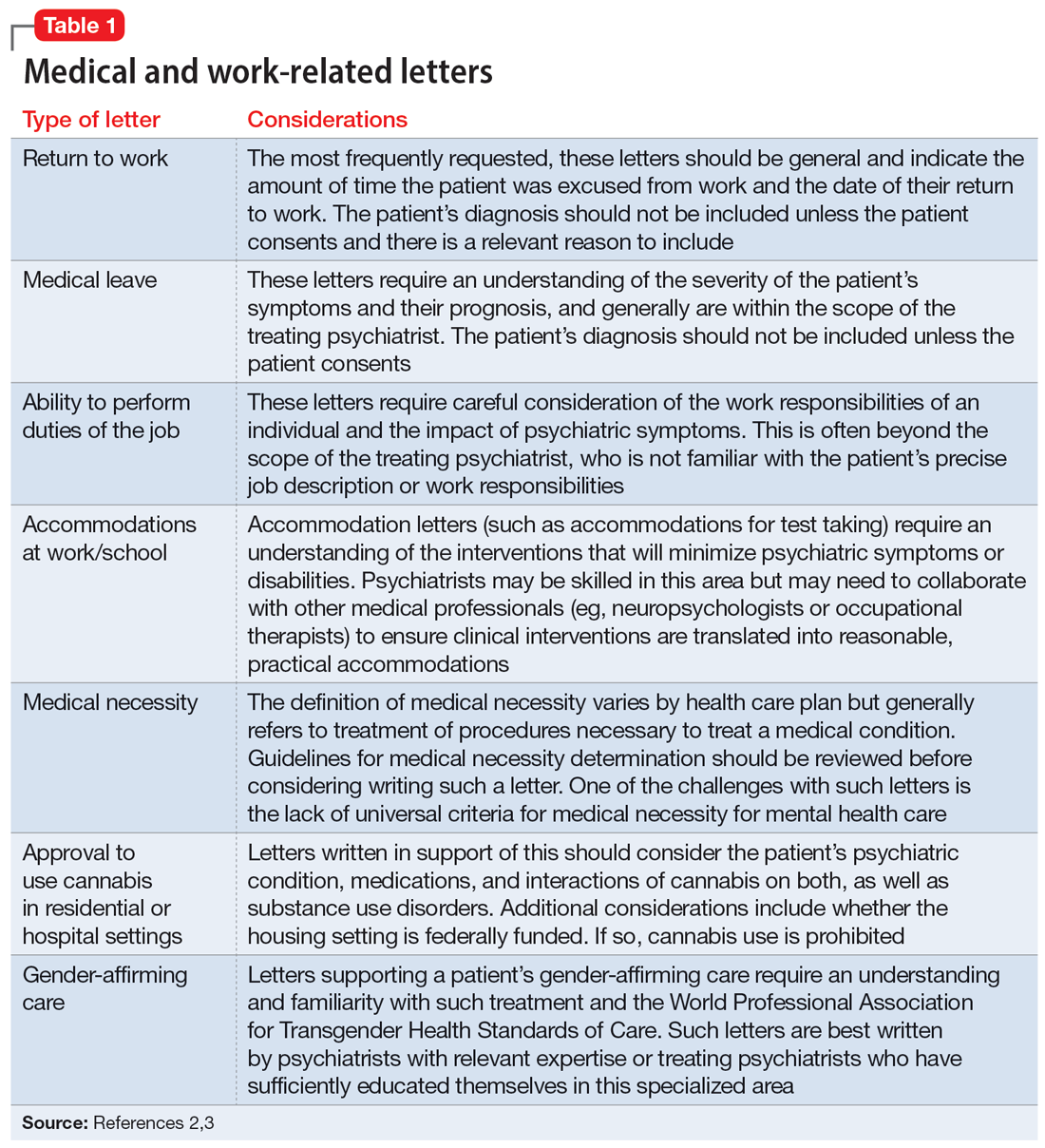
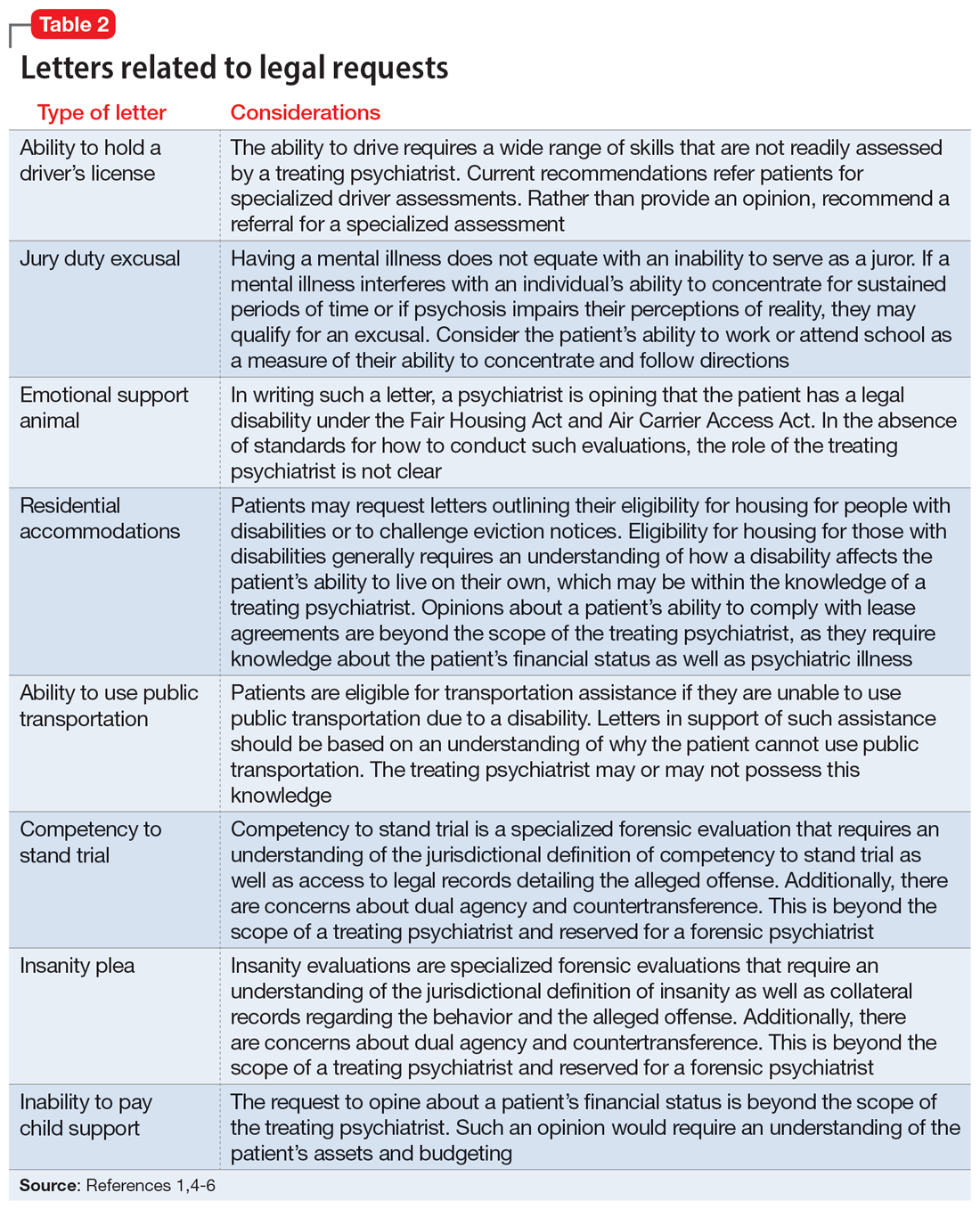
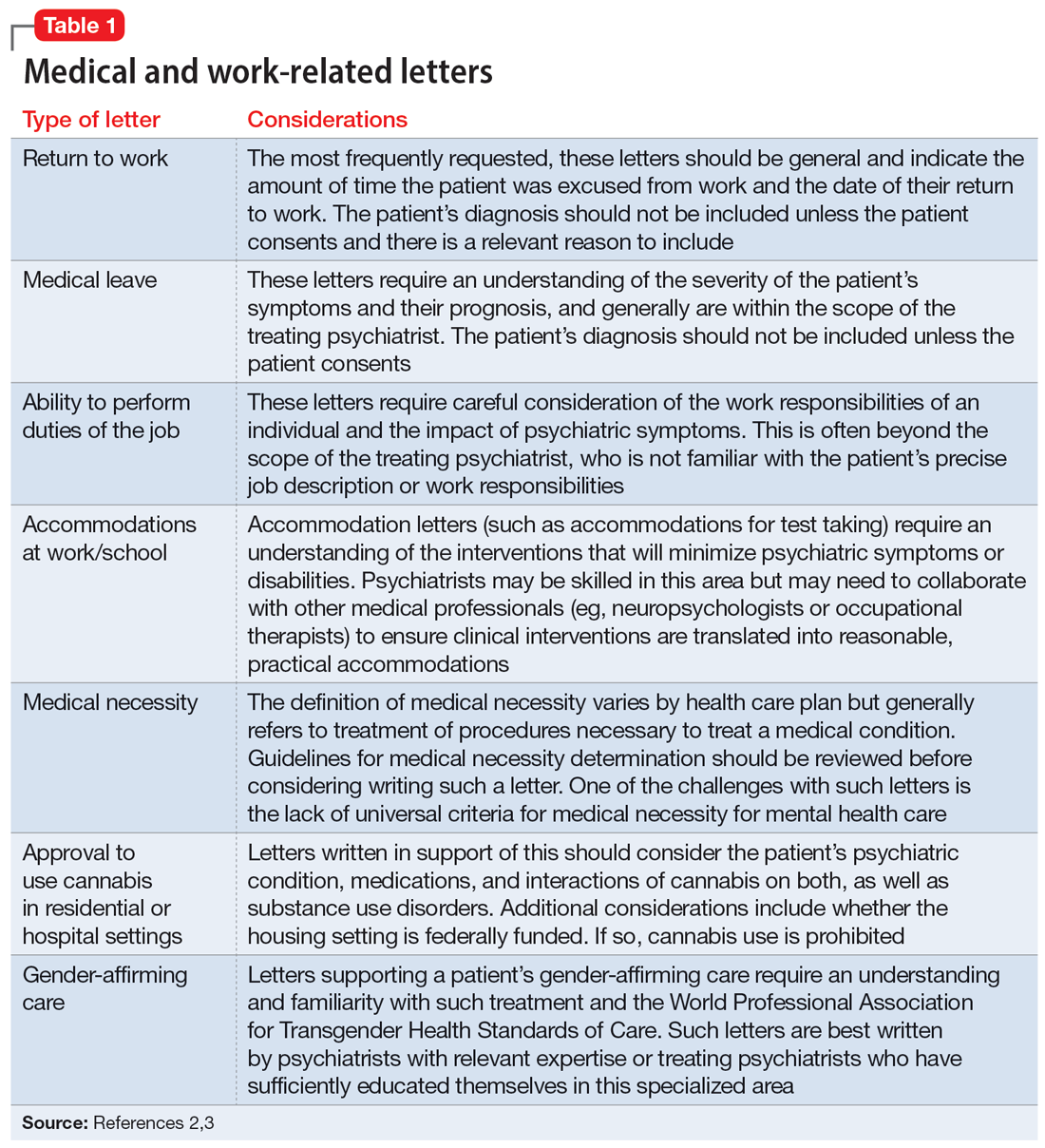
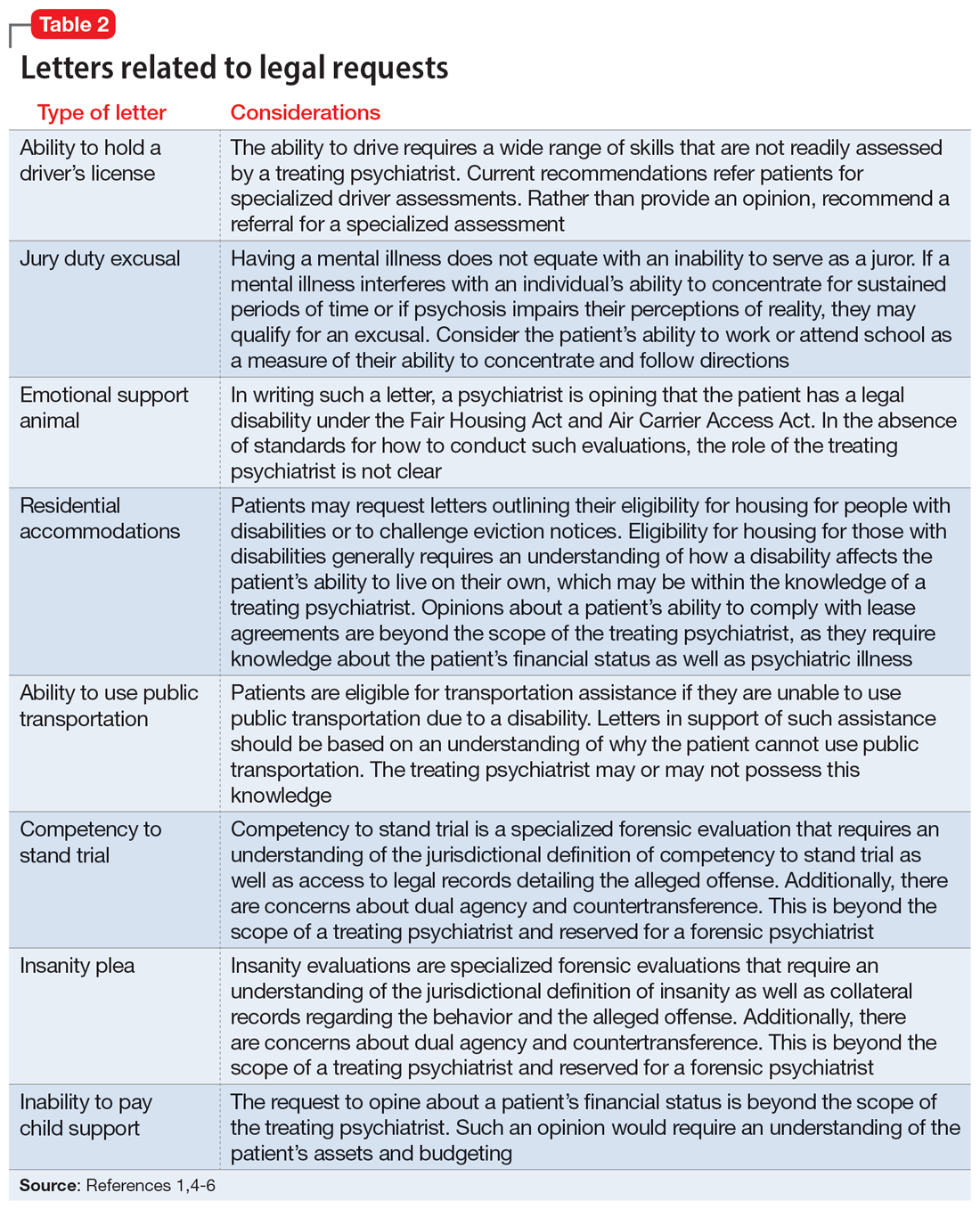
The categories of letters patients request can be divided into 2 groups. The first is comprised of letters relating to the patient’s medical needs (Table 12,3). These address the patient’s ability to work (eg, medical leave, return to work, or accommodations) or travel (eg, ability to drive or use public transportation), or need for specific medical treatment (ie, gender-affirming care or cannabis use in specific settings). The second group relates to legal requests such as excusal from jury duty, emotional support animals, or any other letter used specifically for legal purposes (in civil or criminal cases) (Table 21,4-6).
The decision to write a letter on behalf of a patient should be based on whether you have sufficient knowledge to answer the referral question, and whether the requested evaluation fits within your role as the treating psychiatrist. Many requests fall short of the first condition. For example, a request to opine about an individual’s ability to perform their job duties requires specific knowledge and careful consideration of the patient’s work responsibilities, knowledge of the impact of their psychiatric symptoms, and specialized knowledge about interventions that would ameliorate symptoms in the specialized work setting. Most psychiatrists are not sufficiently familiar with a specific workplace to provide opinions regarding reasonable accommodations.
The second condition refers to the role and responsibilities of the psychiatrist. Many letter requests are clearly within the scope of the clinical psychiatrist, such as a medical leave note due to a psychiatric decompensation or a jury duty excusal due to an unstable mental state. Other letters reach beyond the role of the general or treating psychiatrist, such as opinions about suitable housing or a patient’s competency to stand trial.
Components of letters
The decision to write or not to write a letter should be discussed with the patient. Identify the reasons for and against letter writing. If you decide to write a letter, the letter should have the following basic framework (Figure): the identity of the person who requested the letter, the referral question, and an answer to the referral question with a clear rationale. Describe the patient’s psychiatric diagnosis using DSM criteria. Any limitations to the answer should be identified. The letter should not go beyond the referral question and should not include information that was not requested. It also should be preserved in the medical record.
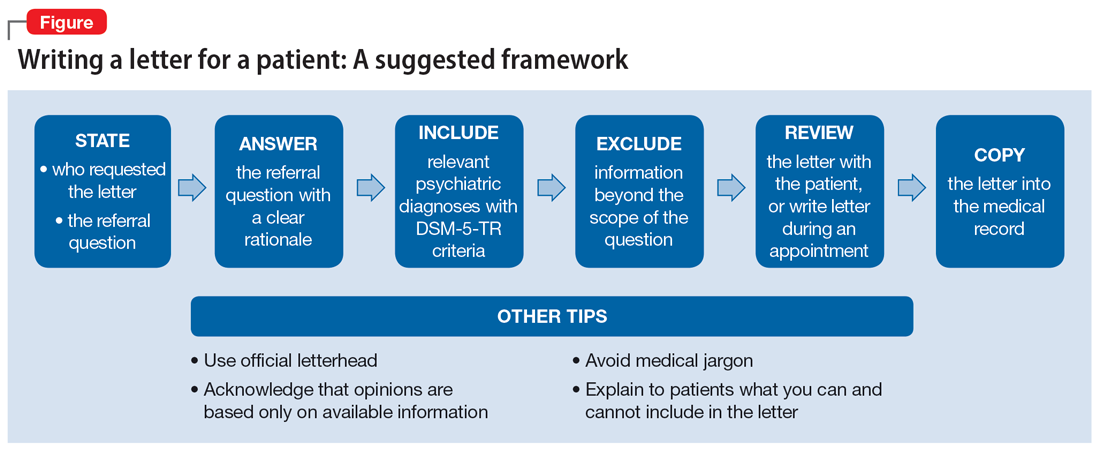
It is recommended to write or review the letter in the presence of the patient to discuss the contents of the letter and what the psychiatrist can or cannot write. As in forensic reports, conclusory statements are not helpful. Provide descriptive information instead of relying on psychiatric jargon, and a rationale for the opinion as opposed to stating an opinion as fact. In the letter, you must acknowledge that your opinion is based upon information provided by the patient (and the patient’s family, when accurate) and as a result, is not fully objective.
Continue to: Liability and dual agency
Liability and dual agency
Psychiatrists are familiar with clinical situations in which a duty to the patient is mitigated or superseded by a duty to a third party. As the Tarasoff court famously stated, “the protective privilege ends where the public peril begins.”7
To be liable to either a patient or a third party means to be “bound or obliged in law or equity; responsible; chargeable; answerable; compellable to make satisfaction, compensation, or restitution.”8 Liabilities related to clinical treatment are well-established; medical students learn the fundamentals before ever treating a patient, and physicians carry malpractice insurance throughout their careers.
Less well-established is the liability a treating psychiatrist owes a third party when forming an opinion that impacts both their patient and the third party (eg, an employer when writing a return-to-work letter, or a disability insurer when qualifying a patient for disability benefits). The American Academy of Psychiatry and the Law discourages treating psychiatrists from performing these types of evaluations of their patients based on the inherent conflict of serving as a dual agent, or acting both as an advocate for the patient and as an independent evaluator striving for objectivity.9 However, such requests commonly arise, and some may be unavoidable.
Dual-agency situations subject the treating psychiatrist to avenues of legal action arising from the patient-doctor relationship as well as the forensic evaluator relationship. If a letter is written during a clinical treatment, all duties owed to the patient continue to apply, and the relevant benchmarks of local statutes and principle of a standard of care are relevant. It is conceivable that a patient could bring a negligence lawsuit based on a standard of care allegation (eg, that writing certain types of letters is so ordinary that failure to write them would fall below the standard of care). Confidentiality is also of the utmost importance,10 and you should obtain a written release of information from the patient before releasing any letter with privileged information about the patient.11 Additional relevant legal causes of action the patient could include are torts such as defamation of character, invasion of privacy, breach of contract, and intentional infliction of emotional distress. There is limited case law supporting patients’ rights to sue psychiatrists for defamation.10
A psychiatrist writing a letter to a third party may also subject themselves to avenues of legal action occurring outside the physician-patient relationship. Importantly, damages resulting from these breaches would not be covered by your malpractice insurance. Extreme cases involve allegations of fraud or perjury, which could be pursued in criminal court. If a psychiatrist intentionally deceives a third party for the purpose of obtaining some benefit for the patient, this is clear grounds for civil or criminal action. Fraud is defined as “a false representation of a matter of fact, whether by words or by conduct, by false or misleading allegations, or by concealment of that which should have been disclosed, which deceives and is intended to deceive another so that he shall act upon it to his legal injury.”8 Negligence can also be grounds for liability if a third party suffers injury or loss. Although the liability is clearer if the third party retains an independent psychiatrist rather than soliciting an opinion from a patient’s treating psychiatrist, both parties are subject to the claim of negligence.10
Continue to: There are some important protections...
There are some important protections that limit psychiatrists’ good-faith opinions from litigation. The primary one is the “professional medical judgment rule,” which shields physicians from the consequences of erroneous opinions so long as the examination was competent, complete, and performed in an ordinary fashion.10 In some cases, psychiatrists writing a letter or report for a government agency may also qualify for quasi-judicial immunity or witness immunity, but case law shows significant variation in when and how these privileges apply and whether such privileges would be applied to a clinical psychiatrist in the context of a traditional physician-patient relationship.12 In general, these privileges are not absolute and may not be sufficiently well-established to discourage a plaintiff from filing suit or prompt early judicial dismissal of a case.
Like all aspects of practicing medicine, letter writing is subject to scrutiny and accountability. Think carefully about your obligations and the potential consequences of writing or not writing a letter to a third party.
Ethical considerations
The decision to write a letter for a patient must be carefully considered from multiple angles.6 In addition to liability concerns, various ethical considerations also arise. Guided by the principles of beneficence, nonmaleficence, autonomy, and justice,13 we recommend the following approaches.
Maintain objectivity
During letter writing, a conflict of interest may arise between your allegiance to the patient and the imperative to provide accurate information.14-16 If the conflict is overwhelming, the most appropriate approach is to recuse yourself from the case and refer the patient to a third party. When electing to write a letter, you accept the responsibility to provide an objective assessment of the relevant situation. This promotes a just outcome and may also serve to promote the patient’s or society’s well-being.
Encourage activity and overall function
Evidence suggests that participation in multiple aspects of life promotes positive health outcomes.17,18 As a physician, it is your duty to promote health and support and facilitate accommodations that allow patients to participate and flourish in society. By the same logic, when approached by patients with a request for letters in support of reduced activity, you should consider not only the benefits but also the potential detriments of such disruptions. This may entail recommending temporary restrictions or modifications, as appropriate.
Continue to: Think beyond the patient
Think beyond the patient
Letter writing, particularly when recommending accommodations, can have implications beyond the patient.16 Such letters may cause unintended societal harm. For example, others may have to assume additional responsibilities; competitive goods (eg, housing) may be rendered to the patient rather than to a person with greater needs; and workplace safety could be compromised due to absence. Consider not only the individual patient but also possible public health and societal effects of letter writing.
Deciding not to write
From an ethical perspective, a physician cannot be compelled to write a letter if such an undertaking violates a stronger moral obligation. An example of this is if writing a letter could cause significant harm to the patient or society, or if writing a letter might compromise a physician’s professionalism.19 When you elect to not write a letter, the ethical principles of autonomy and truth telling dictate that you must inform your patients of this choice.6 You should also provide an explanation to the patient as long as such information would not cause undue psychological or physical harm.20,21
Schedule time to write letters
Some physicians implement policies that all letters are to be completed during scheduled appointments. Others designate administrative time to complete requested letters. Finally, some physicians flexibly complete such requests between appointments or during other undedicated time slots. Any of these approaches are justifiable, though some urgent requests may require more immediate attention outside of appointments. Some physicians may choose to bill for the letter writing if completed outside an appointment and the patient is treated in private practice. Whatever your policy, inform patients of it at the beginning of care and remind them when appropriate, such as before completing a letter that may be billed.
Manage uncertainty
Always strive for objectivity in letter writing. However, some requests inherently hinge on subjective reports and assessments. For example, a patient may request an excuse letter due to feeling unwell. In the absence of objective findings, what should you do? We advise the following.
Acquire collateral information. Adequate information is essential when making any medical recommendation. The same is true for writing letters. With the patient’s permission, you may need to contact relevant parties to better understand the circumstance or activity about which you are being asked to write a letter. For example, a patient may request leave from work due to injury. If the specific parameters of the work impeded by the injury are unclear to you, refrain from writing the letter and explain the rationale to the patient.
Continue to: Integrate prior knowledge of the patient
Integrate prior knowledge of the patient. No letter writing request exists in a vacuum. If you know the patient, the letter should be contextualized within the patient’s prior behaviors.
Stay within your scope
Given the various dilemmas and challenges, you may want to consider whether some letter writing is out of your professional scope.14-16 One solution would be to leave such requests to other entities (eg, requiring employers to retain medical personnel with specialized skills in occupational evaluations) and make such recommendations to patients. Regardless, physicians should think carefully about their professional boundaries and scope regarding letter requests and adopt and implement a consistent standard for all patients.
Regarding the letter requested by Ms. M, you should consider whether the appeal is consistent with the patient’s psychiatric illness. You should also consider whether you have sufficient knowledge about the patient’s living environment to support their claim. Such a letter should be written only if you understand both considerations. Regardless of your decision, you should explain your rationale to the patient.
Bottom Line
Patients may ask their psychiatrists to write letters that address aspects of their social well-being. However, psychiatrists must be alert to requests that are outside their scope of practice or ethically or legally fraught. Carefully consider whether writing a letter is appropriate and if not, discuss with the patient the reasons you cannot write such a letter and any recommended alternative avenues to address their request.
Related Resources
- Riese A. Writing letters for transgender patients undergoing medical transition. Current Psychiatry. 2021;20(8):51-52. doi:10.12788/cp.0159
- Joshi KG. Service animals and emotional support animals: should you write that letter? Current Psychiatry. 2021;20(11):16-19,24. doi:10.12788/cp.0183
1. West S, Friedman SH. To be or not to be: treating psychiatrist and expert witness. Psychiatric Times. 2007;24(6). Accessed March 14, 2023. https://www.psychiatrictimes.com/view/be-or-not-be-treating-psychiatrist-and-expert-witness
2. Knoepflmacher D. ‘Medical necessity’ in psychiatry: whose definition is it anyway? Psychiatric News. 2016;51(18):12-14. https://psychnews.psychiatryonline.org/doi/10.1176/appi.pn.2016.9b14
3. Lampe JR. Recent developments in marijuana law (LSB10859). Congressional Research Service. 2022. Accessed October 25, 2023. https://crsreports.congress.gov/product/pdf/LSB/LSB10859/2
4. Brunnauer A, Buschert V, Segmiller F, et al. Mobility behaviour and driving status of patients with mental disorders – an exploratory study. Int J Psychiatry Clin Pract. 2016;20(1):40-46. doi:10.3109/13651501.2015.1089293
5. Chiu CW, Law CK, Cheng AS. Driver assessment service for people with mental illness. Hong Kong J Occup Ther. 2019;32(2):77-83. doi:10.1177/1569186119886773
6. Joshi KG. Service animals and emotional support animals: should you write that letter? Current Psychiatry. 2021;20(11):16-19. doi:10.12788/cp.0183
7. Tarasoff v Regents of University of California, 17 Cal 3d 425, 551 P2d 334, 131 Cal. Rptr. 14 (Cal 1976).
8. Black HC. Liability. Black’s Law Dictionary. Revised 4th ed. West Publishing; 1975:1060.
9. American Academy of Psychiatry and the Law. Ethics guidelines for the practice of forensic psychiatry. 2005. Accessed March 15, 2023. https://www.aapl.org/ethics.htm
10. Gold LH, Davidson JE. Do you understand your risk? Liability and third-party evaluations in civil litigation. J Am Acad Psychiatry Law. 2007;35(2):200-210.
11. Schouten R. Approach to the patient seeking disability benefits. In: Stern TA, Herman JB, Slavin PL, eds. The MGH Guide to Psychiatry in Primary Care. McGraw Hill; 1998:121-126.
12. Appelbaum PS. Law and psychiatry: liability for forensic evaluations: a word of caution. Psychiatr Serv. 2001;52(7):885-886. doi:10.1176/appi.ps.52.7.885
13. Varkey B. Principles of clinical ethics and their application to practice. Med Princ Pract. 2021;30(1):17-28. doi:10.1159/000509119
14. Mayhew HE, Nordlund DJ. Absenteeism certification: the physician’s role. J Fam Pract. 1988;26(6):651-655.
15. Younggren JN, Boisvert JA, Boness CL. Examining emotional support animals and role conflicts in professional psychology. Prof Psychol Res Pr. 2016;47(4):255-260. doi:10.1037/pro0000083
16. Carroll JD, Mohlenhoff BS, Kersten CM, et al. Laws and ethics related to emotional support animals. J Am Acad Psychiatry Law. 2020;48(4):509-518. doi:1-.29158/JAAPL.200047-20
17. Strully KW. Job loss and health in the U.S. labor market. Demography. 2009;46(2):221-246. doi:10.1353/dem.0.0050
18. Jurisic M, Bean M, Harbaugh J, et al. The personal physician’s role in helping patients with medical conditions stay at work or return to work. J Occup Environ Med. 2017;59(6):e125-131. doi:10.1097/JOM.0000000000001055
19. Munyaradzi M. Critical reflections on the principle of beneficence in biomedicine. Pan Afr Med J. 2012;11:29.
20. Beauchamp TL, Childress JF. Principles of Biomedical Ethics. 7th ed. Oxford University Press; 2012.
21. Gold M. Is honesty always the best policy? Ethical aspects of truth telling. Intern Med J. 2004;34(9-10):578-580. doi:10.1111/j.1445-5994.2004.00673.x
After several months of difficulty living in her current apartment complex, Ms. M asks you as her psychiatrist to write a letter to the management company requesting she be moved to an apartment on the opposite side of the maintenance closet because the noise aggravates her posttraumatic stress disorder. What should you consider when asked to write such a letter?
Psychiatric practice often extends beyond the treatment of mental illness to include addressing patients’ social well-being. Psychiatrists commonly inquire about a patient’s social situation to understand the impact of these environmental factors. Similarly, psychiatric illness may affect a patient’s ability to work or fulfill responsibilities. As a result, patients may ask their psychiatrists for assistance by requesting letters that address various aspects of their social well-being.1 These communications may address an array of topics, from a patient’s readiness to return to work to their ability to pay child support. This article focuses on the role psychiatrists have in writing patient-requested letters across a variety of topics, including the consideration of potential legal liability and ethical implications.
Types of letters
The categories of letters patients request can be divided into 2 groups. The first is comprised of letters relating to the patient’s medical needs (Table 12,3). These address the patient’s ability to work (eg, medical leave, return to work, or accommodations) or travel (eg, ability to drive or use public transportation), or need for specific medical treatment (ie, gender-affirming care or cannabis use in specific settings). The second group relates to legal requests such as excusal from jury duty, emotional support animals, or any other letter used specifically for legal purposes (in civil or criminal cases) (Table 21,4-6).
The decision to write a letter on behalf of a patient should be based on whether you have sufficient knowledge to answer the referral question, and whether the requested evaluation fits within your role as the treating psychiatrist. Many requests fall short of the first condition. For example, a request to opine about an individual’s ability to perform their job duties requires specific knowledge and careful consideration of the patient’s work responsibilities, knowledge of the impact of their psychiatric symptoms, and specialized knowledge about interventions that would ameliorate symptoms in the specialized work setting. Most psychiatrists are not sufficiently familiar with a specific workplace to provide opinions regarding reasonable accommodations.
The second condition refers to the role and responsibilities of the psychiatrist. Many letter requests are clearly within the scope of the clinical psychiatrist, such as a medical leave note due to a psychiatric decompensation or a jury duty excusal due to an unstable mental state. Other letters reach beyond the role of the general or treating psychiatrist, such as opinions about suitable housing or a patient’s competency to stand trial.
Components of letters
The decision to write or not to write a letter should be discussed with the patient. Identify the reasons for and against letter writing. If you decide to write a letter, the letter should have the following basic framework (Figure): the identity of the person who requested the letter, the referral question, and an answer to the referral question with a clear rationale. Describe the patient’s psychiatric diagnosis using DSM criteria. Any limitations to the answer should be identified. The letter should not go beyond the referral question and should not include information that was not requested. It also should be preserved in the medical record.
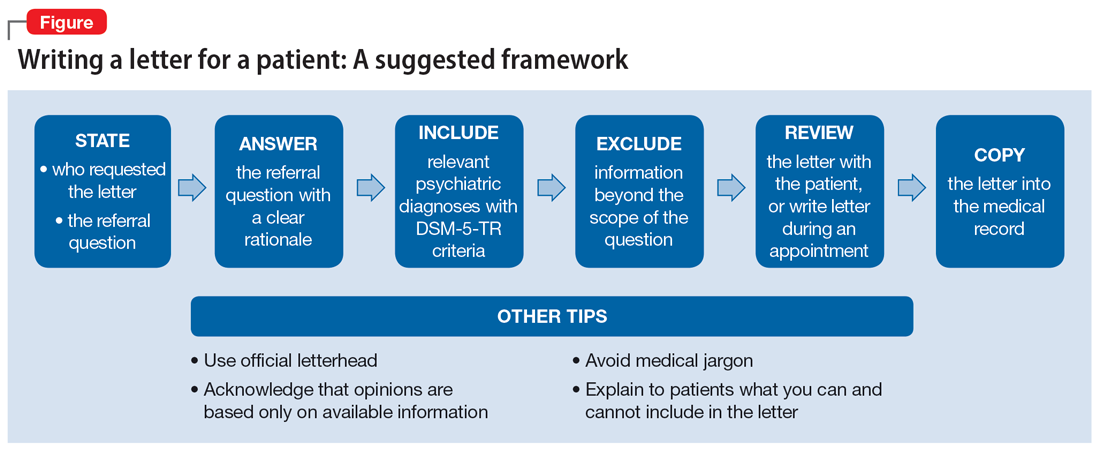
It is recommended to write or review the letter in the presence of the patient to discuss the contents of the letter and what the psychiatrist can or cannot write. As in forensic reports, conclusory statements are not helpful. Provide descriptive information instead of relying on psychiatric jargon, and a rationale for the opinion as opposed to stating an opinion as fact. In the letter, you must acknowledge that your opinion is based upon information provided by the patient (and the patient’s family, when accurate) and as a result, is not fully objective.
Continue to: Liability and dual agency
Liability and dual agency
Psychiatrists are familiar with clinical situations in which a duty to the patient is mitigated or superseded by a duty to a third party. As the Tarasoff court famously stated, “the protective privilege ends where the public peril begins.”7
To be liable to either a patient or a third party means to be “bound or obliged in law or equity; responsible; chargeable; answerable; compellable to make satisfaction, compensation, or restitution.”8 Liabilities related to clinical treatment are well-established; medical students learn the fundamentals before ever treating a patient, and physicians carry malpractice insurance throughout their careers.
Less well-established is the liability a treating psychiatrist owes a third party when forming an opinion that impacts both their patient and the third party (eg, an employer when writing a return-to-work letter, or a disability insurer when qualifying a patient for disability benefits). The American Academy of Psychiatry and the Law discourages treating psychiatrists from performing these types of evaluations of their patients based on the inherent conflict of serving as a dual agent, or acting both as an advocate for the patient and as an independent evaluator striving for objectivity.9 However, such requests commonly arise, and some may be unavoidable.
Dual-agency situations subject the treating psychiatrist to avenues of legal action arising from the patient-doctor relationship as well as the forensic evaluator relationship. If a letter is written during a clinical treatment, all duties owed to the patient continue to apply, and the relevant benchmarks of local statutes and principle of a standard of care are relevant. It is conceivable that a patient could bring a negligence lawsuit based on a standard of care allegation (eg, that writing certain types of letters is so ordinary that failure to write them would fall below the standard of care). Confidentiality is also of the utmost importance,10 and you should obtain a written release of information from the patient before releasing any letter with privileged information about the patient.11 Additional relevant legal causes of action the patient could include are torts such as defamation of character, invasion of privacy, breach of contract, and intentional infliction of emotional distress. There is limited case law supporting patients’ rights to sue psychiatrists for defamation.10
A psychiatrist writing a letter to a third party may also subject themselves to avenues of legal action occurring outside the physician-patient relationship. Importantly, damages resulting from these breaches would not be covered by your malpractice insurance. Extreme cases involve allegations of fraud or perjury, which could be pursued in criminal court. If a psychiatrist intentionally deceives a third party for the purpose of obtaining some benefit for the patient, this is clear grounds for civil or criminal action. Fraud is defined as “a false representation of a matter of fact, whether by words or by conduct, by false or misleading allegations, or by concealment of that which should have been disclosed, which deceives and is intended to deceive another so that he shall act upon it to his legal injury.”8 Negligence can also be grounds for liability if a third party suffers injury or loss. Although the liability is clearer if the third party retains an independent psychiatrist rather than soliciting an opinion from a patient’s treating psychiatrist, both parties are subject to the claim of negligence.10
Continue to: There are some important protections...
There are some important protections that limit psychiatrists’ good-faith opinions from litigation. The primary one is the “professional medical judgment rule,” which shields physicians from the consequences of erroneous opinions so long as the examination was competent, complete, and performed in an ordinary fashion.10 In some cases, psychiatrists writing a letter or report for a government agency may also qualify for quasi-judicial immunity or witness immunity, but case law shows significant variation in when and how these privileges apply and whether such privileges would be applied to a clinical psychiatrist in the context of a traditional physician-patient relationship.12 In general, these privileges are not absolute and may not be sufficiently well-established to discourage a plaintiff from filing suit or prompt early judicial dismissal of a case.
Like all aspects of practicing medicine, letter writing is subject to scrutiny and accountability. Think carefully about your obligations and the potential consequences of writing or not writing a letter to a third party.
Ethical considerations
The decision to write a letter for a patient must be carefully considered from multiple angles.6 In addition to liability concerns, various ethical considerations also arise. Guided by the principles of beneficence, nonmaleficence, autonomy, and justice,13 we recommend the following approaches.
Maintain objectivity
During letter writing, a conflict of interest may arise between your allegiance to the patient and the imperative to provide accurate information.14-16 If the conflict is overwhelming, the most appropriate approach is to recuse yourself from the case and refer the patient to a third party. When electing to write a letter, you accept the responsibility to provide an objective assessment of the relevant situation. This promotes a just outcome and may also serve to promote the patient’s or society’s well-being.
Encourage activity and overall function
Evidence suggests that participation in multiple aspects of life promotes positive health outcomes.17,18 As a physician, it is your duty to promote health and support and facilitate accommodations that allow patients to participate and flourish in society. By the same logic, when approached by patients with a request for letters in support of reduced activity, you should consider not only the benefits but also the potential detriments of such disruptions. This may entail recommending temporary restrictions or modifications, as appropriate.
Continue to: Think beyond the patient
Think beyond the patient
Letter writing, particularly when recommending accommodations, can have implications beyond the patient.16 Such letters may cause unintended societal harm. For example, others may have to assume additional responsibilities; competitive goods (eg, housing) may be rendered to the patient rather than to a person with greater needs; and workplace safety could be compromised due to absence. Consider not only the individual patient but also possible public health and societal effects of letter writing.
Deciding not to write
From an ethical perspective, a physician cannot be compelled to write a letter if such an undertaking violates a stronger moral obligation. An example of this is if writing a letter could cause significant harm to the patient or society, or if writing a letter might compromise a physician’s professionalism.19 When you elect to not write a letter, the ethical principles of autonomy and truth telling dictate that you must inform your patients of this choice.6 You should also provide an explanation to the patient as long as such information would not cause undue psychological or physical harm.20,21
Schedule time to write letters
Some physicians implement policies that all letters are to be completed during scheduled appointments. Others designate administrative time to complete requested letters. Finally, some physicians flexibly complete such requests between appointments or during other undedicated time slots. Any of these approaches are justifiable, though some urgent requests may require more immediate attention outside of appointments. Some physicians may choose to bill for the letter writing if completed outside an appointment and the patient is treated in private practice. Whatever your policy, inform patients of it at the beginning of care and remind them when appropriate, such as before completing a letter that may be billed.
Manage uncertainty
Always strive for objectivity in letter writing. However, some requests inherently hinge on subjective reports and assessments. For example, a patient may request an excuse letter due to feeling unwell. In the absence of objective findings, what should you do? We advise the following.
Acquire collateral information. Adequate information is essential when making any medical recommendation. The same is true for writing letters. With the patient’s permission, you may need to contact relevant parties to better understand the circumstance or activity about which you are being asked to write a letter. For example, a patient may request leave from work due to injury. If the specific parameters of the work impeded by the injury are unclear to you, refrain from writing the letter and explain the rationale to the patient.
Continue to: Integrate prior knowledge of the patient
Integrate prior knowledge of the patient. No letter writing request exists in a vacuum. If you know the patient, the letter should be contextualized within the patient’s prior behaviors.
Stay within your scope
Given the various dilemmas and challenges, you may want to consider whether some letter writing is out of your professional scope.14-16 One solution would be to leave such requests to other entities (eg, requiring employers to retain medical personnel with specialized skills in occupational evaluations) and make such recommendations to patients. Regardless, physicians should think carefully about their professional boundaries and scope regarding letter requests and adopt and implement a consistent standard for all patients.
Regarding the letter requested by Ms. M, you should consider whether the appeal is consistent with the patient’s psychiatric illness. You should also consider whether you have sufficient knowledge about the patient’s living environment to support their claim. Such a letter should be written only if you understand both considerations. Regardless of your decision, you should explain your rationale to the patient.
Bottom Line
Patients may ask their psychiatrists to write letters that address aspects of their social well-being. However, psychiatrists must be alert to requests that are outside their scope of practice or ethically or legally fraught. Carefully consider whether writing a letter is appropriate and if not, discuss with the patient the reasons you cannot write such a letter and any recommended alternative avenues to address their request.
Related Resources
- Riese A. Writing letters for transgender patients undergoing medical transition. Current Psychiatry. 2021;20(8):51-52. doi:10.12788/cp.0159
- Joshi KG. Service animals and emotional support animals: should you write that letter? Current Psychiatry. 2021;20(11):16-19,24. doi:10.12788/cp.0183
After several months of difficulty living in her current apartment complex, Ms. M asks you as her psychiatrist to write a letter to the management company requesting she be moved to an apartment on the opposite side of the maintenance closet because the noise aggravates her posttraumatic stress disorder. What should you consider when asked to write such a letter?
Psychiatric practice often extends beyond the treatment of mental illness to include addressing patients’ social well-being. Psychiatrists commonly inquire about a patient’s social situation to understand the impact of these environmental factors. Similarly, psychiatric illness may affect a patient’s ability to work or fulfill responsibilities. As a result, patients may ask their psychiatrists for assistance by requesting letters that address various aspects of their social well-being.1 These communications may address an array of topics, from a patient’s readiness to return to work to their ability to pay child support. This article focuses on the role psychiatrists have in writing patient-requested letters across a variety of topics, including the consideration of potential legal liability and ethical implications.
Types of letters
The categories of letters patients request can be divided into 2 groups. The first is comprised of letters relating to the patient’s medical needs (Table 12,3). These address the patient’s ability to work (eg, medical leave, return to work, or accommodations) or travel (eg, ability to drive or use public transportation), or need for specific medical treatment (ie, gender-affirming care or cannabis use in specific settings). The second group relates to legal requests such as excusal from jury duty, emotional support animals, or any other letter used specifically for legal purposes (in civil or criminal cases) (Table 21,4-6).
The decision to write a letter on behalf of a patient should be based on whether you have sufficient knowledge to answer the referral question, and whether the requested evaluation fits within your role as the treating psychiatrist. Many requests fall short of the first condition. For example, a request to opine about an individual’s ability to perform their job duties requires specific knowledge and careful consideration of the patient’s work responsibilities, knowledge of the impact of their psychiatric symptoms, and specialized knowledge about interventions that would ameliorate symptoms in the specialized work setting. Most psychiatrists are not sufficiently familiar with a specific workplace to provide opinions regarding reasonable accommodations.
The second condition refers to the role and responsibilities of the psychiatrist. Many letter requests are clearly within the scope of the clinical psychiatrist, such as a medical leave note due to a psychiatric decompensation or a jury duty excusal due to an unstable mental state. Other letters reach beyond the role of the general or treating psychiatrist, such as opinions about suitable housing or a patient’s competency to stand trial.
Components of letters
The decision to write or not to write a letter should be discussed with the patient. Identify the reasons for and against letter writing. If you decide to write a letter, the letter should have the following basic framework (Figure): the identity of the person who requested the letter, the referral question, and an answer to the referral question with a clear rationale. Describe the patient’s psychiatric diagnosis using DSM criteria. Any limitations to the answer should be identified. The letter should not go beyond the referral question and should not include information that was not requested. It also should be preserved in the medical record.
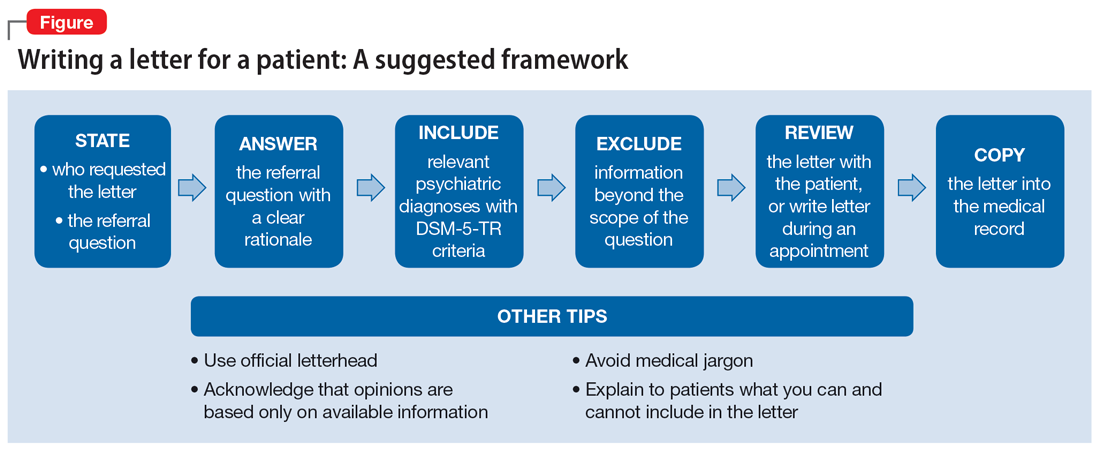
It is recommended to write or review the letter in the presence of the patient to discuss the contents of the letter and what the psychiatrist can or cannot write. As in forensic reports, conclusory statements are not helpful. Provide descriptive information instead of relying on psychiatric jargon, and a rationale for the opinion as opposed to stating an opinion as fact. In the letter, you must acknowledge that your opinion is based upon information provided by the patient (and the patient’s family, when accurate) and as a result, is not fully objective.
Continue to: Liability and dual agency
Liability and dual agency
Psychiatrists are familiar with clinical situations in which a duty to the patient is mitigated or superseded by a duty to a third party. As the Tarasoff court famously stated, “the protective privilege ends where the public peril begins.”7
To be liable to either a patient or a third party means to be “bound or obliged in law or equity; responsible; chargeable; answerable; compellable to make satisfaction, compensation, or restitution.”8 Liabilities related to clinical treatment are well-established; medical students learn the fundamentals before ever treating a patient, and physicians carry malpractice insurance throughout their careers.
Less well-established is the liability a treating psychiatrist owes a third party when forming an opinion that impacts both their patient and the third party (eg, an employer when writing a return-to-work letter, or a disability insurer when qualifying a patient for disability benefits). The American Academy of Psychiatry and the Law discourages treating psychiatrists from performing these types of evaluations of their patients based on the inherent conflict of serving as a dual agent, or acting both as an advocate for the patient and as an independent evaluator striving for objectivity.9 However, such requests commonly arise, and some may be unavoidable.
Dual-agency situations subject the treating psychiatrist to avenues of legal action arising from the patient-doctor relationship as well as the forensic evaluator relationship. If a letter is written during a clinical treatment, all duties owed to the patient continue to apply, and the relevant benchmarks of local statutes and principle of a standard of care are relevant. It is conceivable that a patient could bring a negligence lawsuit based on a standard of care allegation (eg, that writing certain types of letters is so ordinary that failure to write them would fall below the standard of care). Confidentiality is also of the utmost importance,10 and you should obtain a written release of information from the patient before releasing any letter with privileged information about the patient.11 Additional relevant legal causes of action the patient could include are torts such as defamation of character, invasion of privacy, breach of contract, and intentional infliction of emotional distress. There is limited case law supporting patients’ rights to sue psychiatrists for defamation.10
A psychiatrist writing a letter to a third party may also subject themselves to avenues of legal action occurring outside the physician-patient relationship. Importantly, damages resulting from these breaches would not be covered by your malpractice insurance. Extreme cases involve allegations of fraud or perjury, which could be pursued in criminal court. If a psychiatrist intentionally deceives a third party for the purpose of obtaining some benefit for the patient, this is clear grounds for civil or criminal action. Fraud is defined as “a false representation of a matter of fact, whether by words or by conduct, by false or misleading allegations, or by concealment of that which should have been disclosed, which deceives and is intended to deceive another so that he shall act upon it to his legal injury.”8 Negligence can also be grounds for liability if a third party suffers injury or loss. Although the liability is clearer if the third party retains an independent psychiatrist rather than soliciting an opinion from a patient’s treating psychiatrist, both parties are subject to the claim of negligence.10
Continue to: There are some important protections...
There are some important protections that limit psychiatrists’ good-faith opinions from litigation. The primary one is the “professional medical judgment rule,” which shields physicians from the consequences of erroneous opinions so long as the examination was competent, complete, and performed in an ordinary fashion.10 In some cases, psychiatrists writing a letter or report for a government agency may also qualify for quasi-judicial immunity or witness immunity, but case law shows significant variation in when and how these privileges apply and whether such privileges would be applied to a clinical psychiatrist in the context of a traditional physician-patient relationship.12 In general, these privileges are not absolute and may not be sufficiently well-established to discourage a plaintiff from filing suit or prompt early judicial dismissal of a case.
Like all aspects of practicing medicine, letter writing is subject to scrutiny and accountability. Think carefully about your obligations and the potential consequences of writing or not writing a letter to a third party.
Ethical considerations
The decision to write a letter for a patient must be carefully considered from multiple angles.6 In addition to liability concerns, various ethical considerations also arise. Guided by the principles of beneficence, nonmaleficence, autonomy, and justice,13 we recommend the following approaches.
Maintain objectivity
During letter writing, a conflict of interest may arise between your allegiance to the patient and the imperative to provide accurate information.14-16 If the conflict is overwhelming, the most appropriate approach is to recuse yourself from the case and refer the patient to a third party. When electing to write a letter, you accept the responsibility to provide an objective assessment of the relevant situation. This promotes a just outcome and may also serve to promote the patient’s or society’s well-being.
Encourage activity and overall function
Evidence suggests that participation in multiple aspects of life promotes positive health outcomes.17,18 As a physician, it is your duty to promote health and support and facilitate accommodations that allow patients to participate and flourish in society. By the same logic, when approached by patients with a request for letters in support of reduced activity, you should consider not only the benefits but also the potential detriments of such disruptions. This may entail recommending temporary restrictions or modifications, as appropriate.
Continue to: Think beyond the patient
Think beyond the patient
Letter writing, particularly when recommending accommodations, can have implications beyond the patient.16 Such letters may cause unintended societal harm. For example, others may have to assume additional responsibilities; competitive goods (eg, housing) may be rendered to the patient rather than to a person with greater needs; and workplace safety could be compromised due to absence. Consider not only the individual patient but also possible public health and societal effects of letter writing.
Deciding not to write
From an ethical perspective, a physician cannot be compelled to write a letter if such an undertaking violates a stronger moral obligation. An example of this is if writing a letter could cause significant harm to the patient or society, or if writing a letter might compromise a physician’s professionalism.19 When you elect to not write a letter, the ethical principles of autonomy and truth telling dictate that you must inform your patients of this choice.6 You should also provide an explanation to the patient as long as such information would not cause undue psychological or physical harm.20,21
Schedule time to write letters
Some physicians implement policies that all letters are to be completed during scheduled appointments. Others designate administrative time to complete requested letters. Finally, some physicians flexibly complete such requests between appointments or during other undedicated time slots. Any of these approaches are justifiable, though some urgent requests may require more immediate attention outside of appointments. Some physicians may choose to bill for the letter writing if completed outside an appointment and the patient is treated in private practice. Whatever your policy, inform patients of it at the beginning of care and remind them when appropriate, such as before completing a letter that may be billed.
Manage uncertainty
Always strive for objectivity in letter writing. However, some requests inherently hinge on subjective reports and assessments. For example, a patient may request an excuse letter due to feeling unwell. In the absence of objective findings, what should you do? We advise the following.
Acquire collateral information. Adequate information is essential when making any medical recommendation. The same is true for writing letters. With the patient’s permission, you may need to contact relevant parties to better understand the circumstance or activity about which you are being asked to write a letter. For example, a patient may request leave from work due to injury. If the specific parameters of the work impeded by the injury are unclear to you, refrain from writing the letter and explain the rationale to the patient.
Continue to: Integrate prior knowledge of the patient
Integrate prior knowledge of the patient. No letter writing request exists in a vacuum. If you know the patient, the letter should be contextualized within the patient’s prior behaviors.
Stay within your scope
Given the various dilemmas and challenges, you may want to consider whether some letter writing is out of your professional scope.14-16 One solution would be to leave such requests to other entities (eg, requiring employers to retain medical personnel with specialized skills in occupational evaluations) and make such recommendations to patients. Regardless, physicians should think carefully about their professional boundaries and scope regarding letter requests and adopt and implement a consistent standard for all patients.
Regarding the letter requested by Ms. M, you should consider whether the appeal is consistent with the patient’s psychiatric illness. You should also consider whether you have sufficient knowledge about the patient’s living environment to support their claim. Such a letter should be written only if you understand both considerations. Regardless of your decision, you should explain your rationale to the patient.
Bottom Line
Patients may ask their psychiatrists to write letters that address aspects of their social well-being. However, psychiatrists must be alert to requests that are outside their scope of practice or ethically or legally fraught. Carefully consider whether writing a letter is appropriate and if not, discuss with the patient the reasons you cannot write such a letter and any recommended alternative avenues to address their request.
Related Resources
- Riese A. Writing letters for transgender patients undergoing medical transition. Current Psychiatry. 2021;20(8):51-52. doi:10.12788/cp.0159
- Joshi KG. Service animals and emotional support animals: should you write that letter? Current Psychiatry. 2021;20(11):16-19,24. doi:10.12788/cp.0183
1. West S, Friedman SH. To be or not to be: treating psychiatrist and expert witness. Psychiatric Times. 2007;24(6). Accessed March 14, 2023. https://www.psychiatrictimes.com/view/be-or-not-be-treating-psychiatrist-and-expert-witness
2. Knoepflmacher D. ‘Medical necessity’ in psychiatry: whose definition is it anyway? Psychiatric News. 2016;51(18):12-14. https://psychnews.psychiatryonline.org/doi/10.1176/appi.pn.2016.9b14
3. Lampe JR. Recent developments in marijuana law (LSB10859). Congressional Research Service. 2022. Accessed October 25, 2023. https://crsreports.congress.gov/product/pdf/LSB/LSB10859/2
4. Brunnauer A, Buschert V, Segmiller F, et al. Mobility behaviour and driving status of patients with mental disorders – an exploratory study. Int J Psychiatry Clin Pract. 2016;20(1):40-46. doi:10.3109/13651501.2015.1089293
5. Chiu CW, Law CK, Cheng AS. Driver assessment service for people with mental illness. Hong Kong J Occup Ther. 2019;32(2):77-83. doi:10.1177/1569186119886773
6. Joshi KG. Service animals and emotional support animals: should you write that letter? Current Psychiatry. 2021;20(11):16-19. doi:10.12788/cp.0183
7. Tarasoff v Regents of University of California, 17 Cal 3d 425, 551 P2d 334, 131 Cal. Rptr. 14 (Cal 1976).
8. Black HC. Liability. Black’s Law Dictionary. Revised 4th ed. West Publishing; 1975:1060.
9. American Academy of Psychiatry and the Law. Ethics guidelines for the practice of forensic psychiatry. 2005. Accessed March 15, 2023. https://www.aapl.org/ethics.htm
10. Gold LH, Davidson JE. Do you understand your risk? Liability and third-party evaluations in civil litigation. J Am Acad Psychiatry Law. 2007;35(2):200-210.
11. Schouten R. Approach to the patient seeking disability benefits. In: Stern TA, Herman JB, Slavin PL, eds. The MGH Guide to Psychiatry in Primary Care. McGraw Hill; 1998:121-126.
12. Appelbaum PS. Law and psychiatry: liability for forensic evaluations: a word of caution. Psychiatr Serv. 2001;52(7):885-886. doi:10.1176/appi.ps.52.7.885
13. Varkey B. Principles of clinical ethics and their application to practice. Med Princ Pract. 2021;30(1):17-28. doi:10.1159/000509119
14. Mayhew HE, Nordlund DJ. Absenteeism certification: the physician’s role. J Fam Pract. 1988;26(6):651-655.
15. Younggren JN, Boisvert JA, Boness CL. Examining emotional support animals and role conflicts in professional psychology. Prof Psychol Res Pr. 2016;47(4):255-260. doi:10.1037/pro0000083
16. Carroll JD, Mohlenhoff BS, Kersten CM, et al. Laws and ethics related to emotional support animals. J Am Acad Psychiatry Law. 2020;48(4):509-518. doi:1-.29158/JAAPL.200047-20
17. Strully KW. Job loss and health in the U.S. labor market. Demography. 2009;46(2):221-246. doi:10.1353/dem.0.0050
18. Jurisic M, Bean M, Harbaugh J, et al. The personal physician’s role in helping patients with medical conditions stay at work or return to work. J Occup Environ Med. 2017;59(6):e125-131. doi:10.1097/JOM.0000000000001055
19. Munyaradzi M. Critical reflections on the principle of beneficence in biomedicine. Pan Afr Med J. 2012;11:29.
20. Beauchamp TL, Childress JF. Principles of Biomedical Ethics. 7th ed. Oxford University Press; 2012.
21. Gold M. Is honesty always the best policy? Ethical aspects of truth telling. Intern Med J. 2004;34(9-10):578-580. doi:10.1111/j.1445-5994.2004.00673.x
1. West S, Friedman SH. To be or not to be: treating psychiatrist and expert witness. Psychiatric Times. 2007;24(6). Accessed March 14, 2023. https://www.psychiatrictimes.com/view/be-or-not-be-treating-psychiatrist-and-expert-witness
2. Knoepflmacher D. ‘Medical necessity’ in psychiatry: whose definition is it anyway? Psychiatric News. 2016;51(18):12-14. https://psychnews.psychiatryonline.org/doi/10.1176/appi.pn.2016.9b14
3. Lampe JR. Recent developments in marijuana law (LSB10859). Congressional Research Service. 2022. Accessed October 25, 2023. https://crsreports.congress.gov/product/pdf/LSB/LSB10859/2
4. Brunnauer A, Buschert V, Segmiller F, et al. Mobility behaviour and driving status of patients with mental disorders – an exploratory study. Int J Psychiatry Clin Pract. 2016;20(1):40-46. doi:10.3109/13651501.2015.1089293
5. Chiu CW, Law CK, Cheng AS. Driver assessment service for people with mental illness. Hong Kong J Occup Ther. 2019;32(2):77-83. doi:10.1177/1569186119886773
6. Joshi KG. Service animals and emotional support animals: should you write that letter? Current Psychiatry. 2021;20(11):16-19. doi:10.12788/cp.0183
7. Tarasoff v Regents of University of California, 17 Cal 3d 425, 551 P2d 334, 131 Cal. Rptr. 14 (Cal 1976).
8. Black HC. Liability. Black’s Law Dictionary. Revised 4th ed. West Publishing; 1975:1060.
9. American Academy of Psychiatry and the Law. Ethics guidelines for the practice of forensic psychiatry. 2005. Accessed March 15, 2023. https://www.aapl.org/ethics.htm
10. Gold LH, Davidson JE. Do you understand your risk? Liability and third-party evaluations in civil litigation. J Am Acad Psychiatry Law. 2007;35(2):200-210.
11. Schouten R. Approach to the patient seeking disability benefits. In: Stern TA, Herman JB, Slavin PL, eds. The MGH Guide to Psychiatry in Primary Care. McGraw Hill; 1998:121-126.
12. Appelbaum PS. Law and psychiatry: liability for forensic evaluations: a word of caution. Psychiatr Serv. 2001;52(7):885-886. doi:10.1176/appi.ps.52.7.885
13. Varkey B. Principles of clinical ethics and their application to practice. Med Princ Pract. 2021;30(1):17-28. doi:10.1159/000509119
14. Mayhew HE, Nordlund DJ. Absenteeism certification: the physician’s role. J Fam Pract. 1988;26(6):651-655.
15. Younggren JN, Boisvert JA, Boness CL. Examining emotional support animals and role conflicts in professional psychology. Prof Psychol Res Pr. 2016;47(4):255-260. doi:10.1037/pro0000083
16. Carroll JD, Mohlenhoff BS, Kersten CM, et al. Laws and ethics related to emotional support animals. J Am Acad Psychiatry Law. 2020;48(4):509-518. doi:1-.29158/JAAPL.200047-20
17. Strully KW. Job loss and health in the U.S. labor market. Demography. 2009;46(2):221-246. doi:10.1353/dem.0.0050
18. Jurisic M, Bean M, Harbaugh J, et al. The personal physician’s role in helping patients with medical conditions stay at work or return to work. J Occup Environ Med. 2017;59(6):e125-131. doi:10.1097/JOM.0000000000001055
19. Munyaradzi M. Critical reflections on the principle of beneficence in biomedicine. Pan Afr Med J. 2012;11:29.
20. Beauchamp TL, Childress JF. Principles of Biomedical Ethics. 7th ed. Oxford University Press; 2012.
21. Gold M. Is honesty always the best policy? Ethical aspects of truth telling. Intern Med J. 2004;34(9-10):578-580. doi:10.1111/j.1445-5994.2004.00673.x
The medical profession and the 2022 ̶ 2023 Term of the Supreme Court

The 2022-2023 Term of the Supreme Court illustrates how important the Court has become to health-related matters, including decisions regarding the selection and training of new professionals, the daily practice of medicine, and the future availability of new drugs. The importance of several cases is reinforced by the fact that major medical organizations filed amicus curiae (“friend of the court”) briefs in those cases.
Amicus briefs are filed by individuals or organizations with something significant to say about a case to the court—most often to present a point of view, make an argument, or provide information that the parties to the case may not have communicated. Amicus briefs are burdensome in terms of the time, energy, and cost of preparing and filing. Thus, they are not undertaken lightly. Medical organizations submitted amicus briefs in the first 3 cases we consider.
Admissions, race, and diversity
The case: Students for Fair Admissions v President and Fellows of Harvard College
The American College of Obstetricians and Gynecologists (ACOG) joined an amici curiae brief in Students for Fair Admissions v President and Fellows of Harvard College (and the University of North Carolina [UNC]).1 This case challenged the use of racial preferences in college admissions. The Association of American Medical Colleges (AAMC) was the lead organization; nearly 40 other health-related organizations joined the brief.
The legal claim. Those filing the suits asserted that racial preferences by public colleges violate the 14th Amendment’s Equal Protection Clause (“no state shall deny to any person … the equal protection of the law”). That is, if a state university gives racial preferences in selective admissions, it denies some other applicant the equal protection of the law. As for private schools (in this case, Harvard), Title VI of the Civil Rights Act of 1964 has the same standards as the Equal Protection Clause. Thus, the Court consolidated the cases and used the same legal standard in considering public and private colleges (with “colleges” including professional and graduate programs as well as undergraduate institutions).
Background. For nearly 50 years, the Supreme Court has allowed limited racial preferences in college admissions. Those preferences could only operate as a plus, however, and not a negative for applicants and be narrowly tailored. The measure was instituted temporarily; in a 2003 case, the Court said, “We expect that 25 years from now, the use of racial preferences will no longer be necessary.”2
Decision. In a 6-3 decision, the Court held (in the UNC case) that racial preferences generally violate the Constitution, and by a 6-2 decision (in the Harvard case) these preferences violate the Civil Rights Act of 1964. (Justice Jackson was recused in the Harvard case because of a conflict.) The opinion covered 237 pages in the US Reports, so any summary is incomplete.
The majority concluded, “The Harvard and UNC admissions programs cannot be reconciled with the guarantees of the Equal Protection Clause. Both programs lack sufficiently focused and measurable objectives warranting the use of race, unavoidably employ race in a negative manner, involve racial stereotyping, and lack meaningful end points. We have never permitted admissions programs to work in that way, and we will not do so today.”3
There were 3 concurring opinions and 2 dissents in the case. The concurrences reviewed the history of the Equal Protection Clause and the Civil Rights Act, the damage racial preferences can do, and the explicit limits the Court said there must be on racial preferences in higher education. The dissents had a different view of the legal history of the 14th Amendment. They said the majority was turning a blind eye to segregation in society and the race-based gap in America.
As a practical matter, this case means that colleges, including professional schools, cannot use racial preferences. The Court said that universities may consider essays and the like in which applicants describe how their own experiences as an individual (including race) have affected their own lives. However, the Court cautioned that “universities may not simply establish through application essays or other means the regime we hold unlawful today.”3
Continue to: The amici brief...
The amici brief
ACOG joined 40 other health-related organizations in filing an amici brief (multiple “friends”) in Students for Fair Admission. The AAMC led the brief, with the others signing as amici.4 The brief made 3 essential points: diversity in medical education “markedly improves health outcomes,” and a loss of diversity “threaten[s] patients’ health; medical schools engage in an intense “holistic” review of applicants for admission; and medical schools must consider applicants’ “full background” (including race) to achieve their educational and professional goals.4
A powerful part of the brief described the medical school admissions process, particularly the very “holistic” review that is not entirely dependent on admissions scores. The brief effectively weaves the consideration of race into this process, mentioning race (on page 22) only after discussing many other admissions factors.
Child custody decisions related to the Indian Child Welfare Act
The case: Haaland v Brackeen
The American Medical Association (AMA) and the American Academy of Pediatrics filed a brief in Haaland v Brackeen5 involving the constitutionality of the 1978 Indian Child Welfare Act (ICWA). The statute followed a terrible history of Indian children being removed from their families inappropriately, as detailed in a concurring opinion by Justice Gorsuch.5 The two purposes of the act were to promote raising Native American children in their culture and stem the downward trend in tribal membership.
The legal claim. The Court consolidated several cases. Essentially, a 10-month-old child (A.L.M.) was placed in foster care with the Brackeens in Texas. After more than 1 year, the Brackeens sought adoption; the biological father, mother, and grandparents all supported it. The Navajo and Cherokee Nations objected and informed the Texas court that they had found alternative placement with (nonrelative) tribal members in New Mexico. The “court-appointed guardian and a psychological expert … described the strong emotional bond between A.L.M. and his foster parents.” The court denied the adoption petition based on ICWA’s preference for tribe custody, and the Brackeens filed a lawsuit.
Decision. The constitutional claim in the case was that Congress lacked the authority to impose these substantial rules on states in making child custody decisions. The Supreme Court, in a 7-2 decision, upheld the constitutionality of the ICWA.
The amici brief
The joint amici brief of the American Academy of Pediatrics (AAP) and the AMA argued that tribes are “extended families” of Native American children.6 It noted the destructive history of removing Native American children from their families and suggested that kinship care improves children’s health. To its credit, the brief also honestly noted the serious mental health and suicide rates in some tribes, which suggest issues that might arise in child custody and adoption cases.
The Court did not, in this case, take up another constitutional issue that the parties raised—whether the strong preference for Native American over non ̶ Native American custody violates the Equal Protection Clause of the 14th Amendment. The Court said the parties to this case did not have standing to raise the issue. Justice Kavanaugh, concurring, said it was a “serious” issue and invited it to be raised in another case.5
False Claims Act cases
The case: Costs for SuperValu prescriptions
The legal claim. One FCA case this Term involved billings SuperValu made for outpatient prescriptions in Medicare-Medicaid programs. As its “usual and customary” costs, it essentially reported a list price that did not include the substantial discounts it commonly gave.
Background. Subjective knowledge (what the defendant actually knows) may seem impossible to prove—the defendant could just say, “I did not know I was doing wrong.” Over time the law has developed several ways of demonstrating “knowing.” Justice Thomas, writing for a unanimous Court, held that whistleblowers or the government might prove “knowing” in 3 ways:
1. defendants “actually knew that their reported prices were not their ‘usual and customary’ prices when they reported them”
2. were aware of a substantial risk that their higher, retail prices were not their “usual and customary” prices and intentionally avoided learning whether their reports were accurate
3. were aware of such a substantial and unjustifiable risk but submitted the claims anyway.9
Of course, records of the company, information from the whistleblower, and circumstantial evidence may be used to prove any of these; it does not require the company’s admission.
The Court said that if the government or whistleblowers make a showing of any of these 3 things, it is enough.
Decision. The case was returned to the lower court to apply these rules.
The amici brief
The American Hospital Association and America’s Health Insurance Plans filed an amici brief.10 It reminded the Court that many reimbursement regulations are unclear. Therefore, it is inappropriate to impose FCA liability for guessing incorrectly what the regulations mean. Having to check on every possible ambiguity was unworkable. The Court declined, however, the suggestion that defendants should be able to use any one of many “objectively” reasonable interpretations of regulations.
Continue to: The case: Polansky v Executive Health Resources...
The case: Polansky v Executive Health Resources
Health care providers who dislike the FCA may find solace this Term in this second FCA case.11
The legal claim. Polansky, a physician employed by a medical billing company, became an “intervenor” in a suit claiming the company assisted hospitals in false billing (inpatient claims for outpatient services). The government sought to dismiss the case, but Polansky refused.
Decision. The case eventually reached the Supreme Court, which held that the government may enter an FCA case at any time and move to dismiss the case even over the objection of a whistleblower. The government does not seek to enter a case in order to file dismissal motions often. When it does so, whistleblowers are protected by the fact that the dismissal motion requires a hearing before the federal court.
An important part of this case has escaped much attention. Justices Thomas, Kavanaugh, and Barrett invited litigation to determine if allowing private whistleblowers to represent the government’s interest is consistent with Article II of the Constitution.11 The invitation will likely be accepted. We expect to see cases challenging the place of “intervenors” pursuing claims when the government has declined to take up the case. The private intervenor is a crucial provision of the current FCA, and if such a challenge were successful, it could substantially reduce FCA cases.
Criminal false claims
Dubin overbilled Medicaid for psychological testing by saying the testing was done by a licensed psychologist rather than an assistant. The government claimed the “identity theft” was using the patient’s (actual) Medicaid number in submitting the bill.12 The Court unanimously held the overbilling was not aggravated identity theft as defined in federal law. Dubin could be convicted of fraudulent billing but not aggravated identity theft, thereby avoiding the mandatory prison term.
Patents of “genus” targets
The case: Amgen v Sanofi
Background. “Genus” patents allow a single pharmaceutical company to patent every antibody that binds to a specific amino acid on a naturally occurring protein. In this case, the patent office had granted a “genus” patent on “all antibodies” that bind to the naturally occurring protein PCSK9 and block it from hindering the body’s mechanism for removing low-density lipoprotein (LDL) cholesterol from the bloodstream,13 helping to reduce LDL cholesterol levels. These patents could involve millions of antibodies—and Amgen was claiming a patent on all of them. Amgen and Sanofi marketed their products, each with their own unique amino acid sequence.13 Amgen sued Sanofi for violating its patent rights.
Decision. The Court unanimously held that Amgen did not have a valid patent on all antibodies targeting PCSK9, only those that it had explicitly described in its patent application—a ruling based on a 150-year-old technical requirement for receiving a patent. An applicant for a patent must include “a written description of the invention, and of the manner and process of making and using it, in such full, clear, concise, and exact terms as to enable any person skilled in the art…to make and use the same.”13 Amgen’s patent provided the description for only a few of the antibodies, but from the description in its application others could not “make and use” all of the antibodies targeting PCSK9.
While the decision was vital for future pharmaceuticals, the patent principle on which it was based has an interesting history. The Court noted that it affected the telegraph (Morse lost part of his patent), electric lights (Edison won his case against other inventors), and the glue for wood veneering (Perkins Glue Company lost).13
Continue to: Other notable decisions...
Other notable decisions
Student loans
The Court struck down the Biden Administration’s student loan forgiveness program, which would have cost approximately $430 billion.14 The central issue was whether the administration had the authority for such massive loan forgiveness; that is, whether Congress had authorized the broad loan forgiveness. The administration claimed authority from the post ̶ 9/11 HEROES Act, which allows the Secretary of Education to “waive or modify” loan provisions during national emergencies.
Free speech and the wedding web designer
303 Creative v Elenis involved a creative website designer who did not want to be required to create a website for a gay wedding.15 The designer had strong beliefs against same-sex marriages, but Colorado sought to force her to do so under the state “public accommodations” law. In a 6-3 decision, the Court held that the designer had a “free speech” right. That is, the state could not compel her to undertake speech expressing things she did not believe. This was because the website design was an expressive, creative activity and therefore was “speech” under the First Amendment.
Wetlands and the Clean Water Act
The essential issue in Sackett v Environmental Protection Agency (EPA) was the definitions of waters of the United States and related wetlands. The broad definition the EPA used meant it had jurisdiction to regulate an extraordinary amount of territory. It had, for example, prevented the Sacketts from building a modest house claiming it was part of the “waters of the United States because they were near a ditch that fed into a creek, which fed into Priest Lake, a navigable, intrastate lake.” The Court held that the EPA exceeded its statutory authority to define “wetlands.”16
The Court held that under the Clean Water Act, for the EPA to establish jurisdiction over adjacent wetlands, it must demonstrate that16:
1. “the adjacent body of water constitutes waters of the United States (ie, a relatively permanent body of water connected to traditional interstate navigable waters)…”
2. “…the wetland has a continuous surface connection with that water, making it difficult to determine where the water ends, and the wetland begins.”
Under this definition, the Sacketts could build their house. This was a statutory interpretation case. Therefore, Congress can expand or otherwise change the EPA’s authority under the Clean Water Act and other legislation.
Conclusions: A new justice, “shadow docket,” and ethics rules
SCOTUS’ newest member. When the Marshall called the Court into session on October 3, 2022, it had a new member, Justice Ketanji Brown Jackson. She was sworn in on June 30, 2022, when her predecessor (Justice Breyer) officially retired. She had been a law clerk for Justice Breyer in 1999, as well as a district court judge and court of appeals judge. Those who count such things described her as the “chattiest justice.”17 She spoke more than any other justice—by one count, a total of 75,632 words (an average of 1,300 words in each of the 58 arguments).
A more balanced Court? Most commentators view the Court as more balanced or less conservative than the previous Term. For example, Justice Sotomayor was in the majority 40% last Term but 65% this Term. Justice Thomas was in the majority 75% last Term but 55% this Term. Put another way, this Term in the divided cases, the liberal justices were in the majority 64% of the time, compared with the conservative justices 73%.18 Of course, these differences may reflect a different set of cases rather than a change in the direction of the Court. There were 11 (or 12, depending on how 1 case is counted) 6-3 cases, but only 5 were considered ideological. That suggests that, in many cases, the coalitions were somewhat fluid.
“Shadow docket” controversy continues.19 Shadow docket refers to orders the Court makes that do not follow oral arguments and often do not have written opinions. The orders are all publicly available. This Term a close examination of the approximately 30 shadow docket opinions shows that the overwhelming majority were dissents or explanations about denials of certiorari. The Court ordered only a few stays or injunctions via the shadow docket. One shadow docket stay (that prevented a lower court order from going into effect) is particularly noteworthy. A federal judge had ordered the suspension of the distribution of mifepristone while courts considered claims that the US Food and Drug Administration (FDA) had improperly approved the drug. In a shadow docket order, the Court issued the stay to allow mifepristone to be sold while the case challenging its approval was heard.20 The only opinion was a dissent from Justice Alito. But it also demonstrates the importance of the shadow docket. Without this intervention, in at least part of the country, the distribution of mifepristone would have been interrupted pending the outcome of the FDA cases.
In August, the Court delayed a settlement in the Purdue Pharma liability bankruptcy case.21 It also stayed an injunction of a lower court, thereby permitting federal “ghost guns” regulations to go into effect at least temporarily.22
More ethics rules to come? Another area in which the Court faced criticism was formal ethics rules. The justices make financial disclosures, but these are somewhat ambiguous. There is likely to be increasing pressure for a more complete disclosure of non-financial relationships and more formal ethics rules. ●
The Court had, by September 1, 2023, accepted 22 cases for hearing next Term.1 The cases include a challenge to the extraordinary funding provision for the Consumer Financial Protection Bureau, another racial challenge to congressional districts (South Carolina), the status of Americans with Disability Act “testers” who look for violations without ever intending to use the facilities, the level of deference courts should give to interpreting federal statutes (so-called “Chevron” deference), the opioid (OxyContin ) bankruptcy, and limitations on gun ownership. This represents less than half of the cases the Court will likely hear next Term, so the Court will add many more cases to the docket. It promises to be an appealing Term.
Reference
1. October Term 2023. SCOTUSblog website. Accessed August 29, 2023. https://www.scotusblog.com/case-files/terms/ot2023/
When the Court adjourned on June 30, 2023, it had considered 60 cases, plus hundreds of petitions asking it to hear cases. Most commentators count 55 cases decided after briefing and oral argument and where there was a signed opinion. The information below uses 55 cases unless otherwise noted. During the 2022-2023 Term, the Court:
- upheld liability for the involuntary administration of psychotropic drugs in nursing home1
- permitted disabled students, in some instances, both to make Individuals with Disabilities Education Act (IDEA) claims for services and to file Americans with Disabilities Act (ADA) lawsuits against their schools2
- upheld a statute that makes it illegal to “encourage or induce an alien to come to, enter, or reside in the United States, knowing or in reckless disregard of the fact that such coming to, entry, or residence is or will be in violation of law.” The defendant had used a scam promising noncitizens “adult adoptions” (of which there is no such thing) making it legal for them to come to and stay in the United States.3
- narrowed the “fair use” of copyrighted works. It held that Andy Warhol’s use of a copyrighted photograph in his famous Prince prints was not “transformative” in a legal sense largely because the photo and prints “share the same use”—magazine illustrations.4
- in another intellectual property case, held that Jack Daniel’s might sue a dog toy maker for a rubber dog toy that looked like a Jack Daniel’s bottle5
- further expanded the Federal Arbitration Act by holding that a federal district court must immediately stay court proceedings if one party is appealing a decision not to require arbitration6
- held that two social media companies were not responsible for terrorists using their platforms to recruit others to their cause. It did not, however, decide whether §230 of the Communication Decency Act protects companies from liability.7
- made it easier for employees to receive accommodation for their religious practices and beliefs. Employers must make religious accommodations unless the employer can show that “the burden of granting an accommodation would result in substantial increased [financial and other] costs in relation to the conduct of its particular business.”8
- declined to hear an appeal from Johnson & Johnson (through a subsidiary, Ethicon) about pelvic mesh. In this case, the California Attorney General filed a lawsuit against Ethicon for false advertising by failing to detail the risks of pelvic mesh. The lower courts estimated 240,000 written violations of the law by Ethicon between 2008 and 2017. The trial and appeal to California courts resulted in a judgment of $302 million against Johnson & Johnson. The company asked the Court to review that judgment, but the Court denied certiorari. That likely means the $302 million is final.
References
1. Health and Hospital Corporation of Marion Cty. v Talevski, Docket no. 21-806; June 8, 2023.
2. Luna Perez v Sturgis Public Schools, Docket no. 21-887; March 21, 2023.
3. United States v Hansen, Docket no. 22-179; June 23, 2023.
4. Andy Warhol Foundation for Visual Arts, Inc. v Goldsmith, Docket no. 21-869; May 18, 2023.
5. Jack Daniel’s Properties, Inc. v VIP Products LLC, Docket no. 22-148; June 8, 2023.
6. Coinbase, Inc. v Bielski, Docket no. 22-105; June 23, 2023.
7. Gonzalez v Google LLC, Docket no. 21-1333; May 18, 2023.
8. Groff v DeJoy, Docket no. 22-273; June 29, 2023.
- Students for Fair Admissions, Inc. v President and Fellows of Harvard College, 600 US ___ (2023).
- Grutter v Bollinger, 539 US 306, 326 (2003).
- Students for Fair Admissions, Inc. v President and Fellows of Harvard College, 600 US ___, 39 (2023).
- Brief for Amici Curiae Association of American Medical Colleges et al. in Support of Respondents, Students for Fair Admissions v University of North Carolina (July 28, 2022). Accessed August 18, 2023. https://www.supremecourt.gov /DocketPDF/21/21-707/232120/20220728171307159_20 -1199%20and%2021-707%20Amicus%20Brief%20for%20 Association%20of%20American%20Medical%20Colleges%20 et%20al.pdf
- Haaland v Brackeen, Docket no. 21-376; June 15, 2023.
- Brief of American Academy of Pediatrics and American Medical Association as Amici Curiae in Support of Respondents, in Haaland v Brackeen. August 19, 2022. Accessed August 18, 2023. https://www.supremecourt.gov /DocketPDF/21/21-376/234042/20220819140750948_21-376 .amics.brief.FINAL.pdf
- Justice Department’s False Claims Act Settlements and Judgments Exceed $5.6 Billion in Fiscal Year 2021. US Department of Justice website. February 1, 2022. Accessed August 18, 2023. https://www.justice.gov/opa/pr/justice -department-s-false-claims-act-settlements-and-judgments -exceed-56-billion-fiscal-year
- False Claims Act Settlements and Judgments Exceed $2 Billion in Fiscal Year 2022. US Department of Justice website. February 7, 2023. Accessed August 18, 2023. https://www .justice.gov/opa/pr/false-claims-act-settlements-and -judgments-exceed-2-billion-fiscal-year-2022
- United States ex rel. Schutte v Supervalu Inc., Docket no. 21-1326; June 1, 2023.
- Brief of American Hospital Association and America’s Health Insurance Plans as Amici Curiae in Support of Respondents, in Schutte v Supervalu. March 2023. Accessed August 18, 2023. https://www.supremecourt.gov/DocketPDF/21/21-1326 /262428/20230331113854936_3-31-23%20AHA_AHIP _Amicus_Brief.pdf
- United States ex rel. Polansky v Executive Health Resources, Inc., Docket no. 21-1052; June 16, 2023.
- Dubin v United States, Docket no. 22-10; June 8, 2023.
- Amgen v Sanofi, 598 US ___ (2023).
- Biden v Nebraska, 600 US ___ (2023).
- 303 Creative LLC v Elenis, 600 US ___ (2023).
- Sackett v Environmental Protection Agency, Docket no. 21454; May 25, 2023.
- Krochtengel J. Jackson debuts as chattiest Justice. Law360. July 3, 2023. https://www.law360.com/articles/1692839 /jackson-debuts-as-chattiest-justice
- Feldman A. Another One Bites the Dust: End of 2022/2023 Supreme Court Term Statistics. EmpiricalScotus website. 30, 2023. Accessed August 18, 2023. https://empiricalscotus .com/2023/06/30/another-one-bites-2022/
- Vladeck S. The Shadow Docket: How the Supreme Court Uses Stealth Rulings to Amass Power and Undermine the Republic. New York, New York; Basic Books; 2023.
- Danco Laboratories, LLC v Alliance for Hippocratic Medicine. Docket no. 22A902; April 21, 2023.
- Harrington v Purdue Pharma, 23-124 (23A87).
- Garland v Vanderstok, 23-10718 (August 8, 2023).

The 2022-2023 Term of the Supreme Court illustrates how important the Court has become to health-related matters, including decisions regarding the selection and training of new professionals, the daily practice of medicine, and the future availability of new drugs. The importance of several cases is reinforced by the fact that major medical organizations filed amicus curiae (“friend of the court”) briefs in those cases.
Amicus briefs are filed by individuals or organizations with something significant to say about a case to the court—most often to present a point of view, make an argument, or provide information that the parties to the case may not have communicated. Amicus briefs are burdensome in terms of the time, energy, and cost of preparing and filing. Thus, they are not undertaken lightly. Medical organizations submitted amicus briefs in the first 3 cases we consider.
Admissions, race, and diversity
The case: Students for Fair Admissions v President and Fellows of Harvard College
The American College of Obstetricians and Gynecologists (ACOG) joined an amici curiae brief in Students for Fair Admissions v President and Fellows of Harvard College (and the University of North Carolina [UNC]).1 This case challenged the use of racial preferences in college admissions. The Association of American Medical Colleges (AAMC) was the lead organization; nearly 40 other health-related organizations joined the brief.
The legal claim. Those filing the suits asserted that racial preferences by public colleges violate the 14th Amendment’s Equal Protection Clause (“no state shall deny to any person … the equal protection of the law”). That is, if a state university gives racial preferences in selective admissions, it denies some other applicant the equal protection of the law. As for private schools (in this case, Harvard), Title VI of the Civil Rights Act of 1964 has the same standards as the Equal Protection Clause. Thus, the Court consolidated the cases and used the same legal standard in considering public and private colleges (with “colleges” including professional and graduate programs as well as undergraduate institutions).
Background. For nearly 50 years, the Supreme Court has allowed limited racial preferences in college admissions. Those preferences could only operate as a plus, however, and not a negative for applicants and be narrowly tailored. The measure was instituted temporarily; in a 2003 case, the Court said, “We expect that 25 years from now, the use of racial preferences will no longer be necessary.”2
Decision. In a 6-3 decision, the Court held (in the UNC case) that racial preferences generally violate the Constitution, and by a 6-2 decision (in the Harvard case) these preferences violate the Civil Rights Act of 1964. (Justice Jackson was recused in the Harvard case because of a conflict.) The opinion covered 237 pages in the US Reports, so any summary is incomplete.
The majority concluded, “The Harvard and UNC admissions programs cannot be reconciled with the guarantees of the Equal Protection Clause. Both programs lack sufficiently focused and measurable objectives warranting the use of race, unavoidably employ race in a negative manner, involve racial stereotyping, and lack meaningful end points. We have never permitted admissions programs to work in that way, and we will not do so today.”3
There were 3 concurring opinions and 2 dissents in the case. The concurrences reviewed the history of the Equal Protection Clause and the Civil Rights Act, the damage racial preferences can do, and the explicit limits the Court said there must be on racial preferences in higher education. The dissents had a different view of the legal history of the 14th Amendment. They said the majority was turning a blind eye to segregation in society and the race-based gap in America.
As a practical matter, this case means that colleges, including professional schools, cannot use racial preferences. The Court said that universities may consider essays and the like in which applicants describe how their own experiences as an individual (including race) have affected their own lives. However, the Court cautioned that “universities may not simply establish through application essays or other means the regime we hold unlawful today.”3
Continue to: The amici brief...
The amici brief
ACOG joined 40 other health-related organizations in filing an amici brief (multiple “friends”) in Students for Fair Admission. The AAMC led the brief, with the others signing as amici.4 The brief made 3 essential points: diversity in medical education “markedly improves health outcomes,” and a loss of diversity “threaten[s] patients’ health; medical schools engage in an intense “holistic” review of applicants for admission; and medical schools must consider applicants’ “full background” (including race) to achieve their educational and professional goals.4
A powerful part of the brief described the medical school admissions process, particularly the very “holistic” review that is not entirely dependent on admissions scores. The brief effectively weaves the consideration of race into this process, mentioning race (on page 22) only after discussing many other admissions factors.
Child custody decisions related to the Indian Child Welfare Act
The case: Haaland v Brackeen
The American Medical Association (AMA) and the American Academy of Pediatrics filed a brief in Haaland v Brackeen5 involving the constitutionality of the 1978 Indian Child Welfare Act (ICWA). The statute followed a terrible history of Indian children being removed from their families inappropriately, as detailed in a concurring opinion by Justice Gorsuch.5 The two purposes of the act were to promote raising Native American children in their culture and stem the downward trend in tribal membership.
The legal claim. The Court consolidated several cases. Essentially, a 10-month-old child (A.L.M.) was placed in foster care with the Brackeens in Texas. After more than 1 year, the Brackeens sought adoption; the biological father, mother, and grandparents all supported it. The Navajo and Cherokee Nations objected and informed the Texas court that they had found alternative placement with (nonrelative) tribal members in New Mexico. The “court-appointed guardian and a psychological expert … described the strong emotional bond between A.L.M. and his foster parents.” The court denied the adoption petition based on ICWA’s preference for tribe custody, and the Brackeens filed a lawsuit.
Decision. The constitutional claim in the case was that Congress lacked the authority to impose these substantial rules on states in making child custody decisions. The Supreme Court, in a 7-2 decision, upheld the constitutionality of the ICWA.
The amici brief
The joint amici brief of the American Academy of Pediatrics (AAP) and the AMA argued that tribes are “extended families” of Native American children.6 It noted the destructive history of removing Native American children from their families and suggested that kinship care improves children’s health. To its credit, the brief also honestly noted the serious mental health and suicide rates in some tribes, which suggest issues that might arise in child custody and adoption cases.
The Court did not, in this case, take up another constitutional issue that the parties raised—whether the strong preference for Native American over non ̶ Native American custody violates the Equal Protection Clause of the 14th Amendment. The Court said the parties to this case did not have standing to raise the issue. Justice Kavanaugh, concurring, said it was a “serious” issue and invited it to be raised in another case.5
False Claims Act cases
The case: Costs for SuperValu prescriptions
The legal claim. One FCA case this Term involved billings SuperValu made for outpatient prescriptions in Medicare-Medicaid programs. As its “usual and customary” costs, it essentially reported a list price that did not include the substantial discounts it commonly gave.
Background. Subjective knowledge (what the defendant actually knows) may seem impossible to prove—the defendant could just say, “I did not know I was doing wrong.” Over time the law has developed several ways of demonstrating “knowing.” Justice Thomas, writing for a unanimous Court, held that whistleblowers or the government might prove “knowing” in 3 ways:
1. defendants “actually knew that their reported prices were not their ‘usual and customary’ prices when they reported them”
2. were aware of a substantial risk that their higher, retail prices were not their “usual and customary” prices and intentionally avoided learning whether their reports were accurate
3. were aware of such a substantial and unjustifiable risk but submitted the claims anyway.9
Of course, records of the company, information from the whistleblower, and circumstantial evidence may be used to prove any of these; it does not require the company’s admission.
The Court said that if the government or whistleblowers make a showing of any of these 3 things, it is enough.
Decision. The case was returned to the lower court to apply these rules.
The amici brief
The American Hospital Association and America’s Health Insurance Plans filed an amici brief.10 It reminded the Court that many reimbursement regulations are unclear. Therefore, it is inappropriate to impose FCA liability for guessing incorrectly what the regulations mean. Having to check on every possible ambiguity was unworkable. The Court declined, however, the suggestion that defendants should be able to use any one of many “objectively” reasonable interpretations of regulations.
Continue to: The case: Polansky v Executive Health Resources...
The case: Polansky v Executive Health Resources
Health care providers who dislike the FCA may find solace this Term in this second FCA case.11
The legal claim. Polansky, a physician employed by a medical billing company, became an “intervenor” in a suit claiming the company assisted hospitals in false billing (inpatient claims for outpatient services). The government sought to dismiss the case, but Polansky refused.
Decision. The case eventually reached the Supreme Court, which held that the government may enter an FCA case at any time and move to dismiss the case even over the objection of a whistleblower. The government does not seek to enter a case in order to file dismissal motions often. When it does so, whistleblowers are protected by the fact that the dismissal motion requires a hearing before the federal court.
An important part of this case has escaped much attention. Justices Thomas, Kavanaugh, and Barrett invited litigation to determine if allowing private whistleblowers to represent the government’s interest is consistent with Article II of the Constitution.11 The invitation will likely be accepted. We expect to see cases challenging the place of “intervenors” pursuing claims when the government has declined to take up the case. The private intervenor is a crucial provision of the current FCA, and if such a challenge were successful, it could substantially reduce FCA cases.
Criminal false claims
Dubin overbilled Medicaid for psychological testing by saying the testing was done by a licensed psychologist rather than an assistant. The government claimed the “identity theft” was using the patient’s (actual) Medicaid number in submitting the bill.12 The Court unanimously held the overbilling was not aggravated identity theft as defined in federal law. Dubin could be convicted of fraudulent billing but not aggravated identity theft, thereby avoiding the mandatory prison term.
Patents of “genus” targets
The case: Amgen v Sanofi
Background. “Genus” patents allow a single pharmaceutical company to patent every antibody that binds to a specific amino acid on a naturally occurring protein. In this case, the patent office had granted a “genus” patent on “all antibodies” that bind to the naturally occurring protein PCSK9 and block it from hindering the body’s mechanism for removing low-density lipoprotein (LDL) cholesterol from the bloodstream,13 helping to reduce LDL cholesterol levels. These patents could involve millions of antibodies—and Amgen was claiming a patent on all of them. Amgen and Sanofi marketed their products, each with their own unique amino acid sequence.13 Amgen sued Sanofi for violating its patent rights.
Decision. The Court unanimously held that Amgen did not have a valid patent on all antibodies targeting PCSK9, only those that it had explicitly described in its patent application—a ruling based on a 150-year-old technical requirement for receiving a patent. An applicant for a patent must include “a written description of the invention, and of the manner and process of making and using it, in such full, clear, concise, and exact terms as to enable any person skilled in the art…to make and use the same.”13 Amgen’s patent provided the description for only a few of the antibodies, but from the description in its application others could not “make and use” all of the antibodies targeting PCSK9.
While the decision was vital for future pharmaceuticals, the patent principle on which it was based has an interesting history. The Court noted that it affected the telegraph (Morse lost part of his patent), electric lights (Edison won his case against other inventors), and the glue for wood veneering (Perkins Glue Company lost).13
Continue to: Other notable decisions...
Other notable decisions
Student loans
The Court struck down the Biden Administration’s student loan forgiveness program, which would have cost approximately $430 billion.14 The central issue was whether the administration had the authority for such massive loan forgiveness; that is, whether Congress had authorized the broad loan forgiveness. The administration claimed authority from the post ̶ 9/11 HEROES Act, which allows the Secretary of Education to “waive or modify” loan provisions during national emergencies.
Free speech and the wedding web designer
303 Creative v Elenis involved a creative website designer who did not want to be required to create a website for a gay wedding.15 The designer had strong beliefs against same-sex marriages, but Colorado sought to force her to do so under the state “public accommodations” law. In a 6-3 decision, the Court held that the designer had a “free speech” right. That is, the state could not compel her to undertake speech expressing things she did not believe. This was because the website design was an expressive, creative activity and therefore was “speech” under the First Amendment.
Wetlands and the Clean Water Act
The essential issue in Sackett v Environmental Protection Agency (EPA) was the definitions of waters of the United States and related wetlands. The broad definition the EPA used meant it had jurisdiction to regulate an extraordinary amount of territory. It had, for example, prevented the Sacketts from building a modest house claiming it was part of the “waters of the United States because they were near a ditch that fed into a creek, which fed into Priest Lake, a navigable, intrastate lake.” The Court held that the EPA exceeded its statutory authority to define “wetlands.”16
The Court held that under the Clean Water Act, for the EPA to establish jurisdiction over adjacent wetlands, it must demonstrate that16:
1. “the adjacent body of water constitutes waters of the United States (ie, a relatively permanent body of water connected to traditional interstate navigable waters)…”
2. “…the wetland has a continuous surface connection with that water, making it difficult to determine where the water ends, and the wetland begins.”
Under this definition, the Sacketts could build their house. This was a statutory interpretation case. Therefore, Congress can expand or otherwise change the EPA’s authority under the Clean Water Act and other legislation.
Conclusions: A new justice, “shadow docket,” and ethics rules
SCOTUS’ newest member. When the Marshall called the Court into session on October 3, 2022, it had a new member, Justice Ketanji Brown Jackson. She was sworn in on June 30, 2022, when her predecessor (Justice Breyer) officially retired. She had been a law clerk for Justice Breyer in 1999, as well as a district court judge and court of appeals judge. Those who count such things described her as the “chattiest justice.”17 She spoke more than any other justice—by one count, a total of 75,632 words (an average of 1,300 words in each of the 58 arguments).
A more balanced Court? Most commentators view the Court as more balanced or less conservative than the previous Term. For example, Justice Sotomayor was in the majority 40% last Term but 65% this Term. Justice Thomas was in the majority 75% last Term but 55% this Term. Put another way, this Term in the divided cases, the liberal justices were in the majority 64% of the time, compared with the conservative justices 73%.18 Of course, these differences may reflect a different set of cases rather than a change in the direction of the Court. There were 11 (or 12, depending on how 1 case is counted) 6-3 cases, but only 5 were considered ideological. That suggests that, in many cases, the coalitions were somewhat fluid.
“Shadow docket” controversy continues.19 Shadow docket refers to orders the Court makes that do not follow oral arguments and often do not have written opinions. The orders are all publicly available. This Term a close examination of the approximately 30 shadow docket opinions shows that the overwhelming majority were dissents or explanations about denials of certiorari. The Court ordered only a few stays or injunctions via the shadow docket. One shadow docket stay (that prevented a lower court order from going into effect) is particularly noteworthy. A federal judge had ordered the suspension of the distribution of mifepristone while courts considered claims that the US Food and Drug Administration (FDA) had improperly approved the drug. In a shadow docket order, the Court issued the stay to allow mifepristone to be sold while the case challenging its approval was heard.20 The only opinion was a dissent from Justice Alito. But it also demonstrates the importance of the shadow docket. Without this intervention, in at least part of the country, the distribution of mifepristone would have been interrupted pending the outcome of the FDA cases.
In August, the Court delayed a settlement in the Purdue Pharma liability bankruptcy case.21 It also stayed an injunction of a lower court, thereby permitting federal “ghost guns” regulations to go into effect at least temporarily.22
More ethics rules to come? Another area in which the Court faced criticism was formal ethics rules. The justices make financial disclosures, but these are somewhat ambiguous. There is likely to be increasing pressure for a more complete disclosure of non-financial relationships and more formal ethics rules. ●
The Court had, by September 1, 2023, accepted 22 cases for hearing next Term.1 The cases include a challenge to the extraordinary funding provision for the Consumer Financial Protection Bureau, another racial challenge to congressional districts (South Carolina), the status of Americans with Disability Act “testers” who look for violations without ever intending to use the facilities, the level of deference courts should give to interpreting federal statutes (so-called “Chevron” deference), the opioid (OxyContin ) bankruptcy, and limitations on gun ownership. This represents less than half of the cases the Court will likely hear next Term, so the Court will add many more cases to the docket. It promises to be an appealing Term.
Reference
1. October Term 2023. SCOTUSblog website. Accessed August 29, 2023. https://www.scotusblog.com/case-files/terms/ot2023/
When the Court adjourned on June 30, 2023, it had considered 60 cases, plus hundreds of petitions asking it to hear cases. Most commentators count 55 cases decided after briefing and oral argument and where there was a signed opinion. The information below uses 55 cases unless otherwise noted. During the 2022-2023 Term, the Court:
- upheld liability for the involuntary administration of psychotropic drugs in nursing home1
- permitted disabled students, in some instances, both to make Individuals with Disabilities Education Act (IDEA) claims for services and to file Americans with Disabilities Act (ADA) lawsuits against their schools2
- upheld a statute that makes it illegal to “encourage or induce an alien to come to, enter, or reside in the United States, knowing or in reckless disregard of the fact that such coming to, entry, or residence is or will be in violation of law.” The defendant had used a scam promising noncitizens “adult adoptions” (of which there is no such thing) making it legal for them to come to and stay in the United States.3
- narrowed the “fair use” of copyrighted works. It held that Andy Warhol’s use of a copyrighted photograph in his famous Prince prints was not “transformative” in a legal sense largely because the photo and prints “share the same use”—magazine illustrations.4
- in another intellectual property case, held that Jack Daniel’s might sue a dog toy maker for a rubber dog toy that looked like a Jack Daniel’s bottle5
- further expanded the Federal Arbitration Act by holding that a federal district court must immediately stay court proceedings if one party is appealing a decision not to require arbitration6
- held that two social media companies were not responsible for terrorists using their platforms to recruit others to their cause. It did not, however, decide whether §230 of the Communication Decency Act protects companies from liability.7
- made it easier for employees to receive accommodation for their religious practices and beliefs. Employers must make religious accommodations unless the employer can show that “the burden of granting an accommodation would result in substantial increased [financial and other] costs in relation to the conduct of its particular business.”8
- declined to hear an appeal from Johnson & Johnson (through a subsidiary, Ethicon) about pelvic mesh. In this case, the California Attorney General filed a lawsuit against Ethicon for false advertising by failing to detail the risks of pelvic mesh. The lower courts estimated 240,000 written violations of the law by Ethicon between 2008 and 2017. The trial and appeal to California courts resulted in a judgment of $302 million against Johnson & Johnson. The company asked the Court to review that judgment, but the Court denied certiorari. That likely means the $302 million is final.
References
1. Health and Hospital Corporation of Marion Cty. v Talevski, Docket no. 21-806; June 8, 2023.
2. Luna Perez v Sturgis Public Schools, Docket no. 21-887; March 21, 2023.
3. United States v Hansen, Docket no. 22-179; June 23, 2023.
4. Andy Warhol Foundation for Visual Arts, Inc. v Goldsmith, Docket no. 21-869; May 18, 2023.
5. Jack Daniel’s Properties, Inc. v VIP Products LLC, Docket no. 22-148; June 8, 2023.
6. Coinbase, Inc. v Bielski, Docket no. 22-105; June 23, 2023.
7. Gonzalez v Google LLC, Docket no. 21-1333; May 18, 2023.
8. Groff v DeJoy, Docket no. 22-273; June 29, 2023.

The 2022-2023 Term of the Supreme Court illustrates how important the Court has become to health-related matters, including decisions regarding the selection and training of new professionals, the daily practice of medicine, and the future availability of new drugs. The importance of several cases is reinforced by the fact that major medical organizations filed amicus curiae (“friend of the court”) briefs in those cases.
Amicus briefs are filed by individuals or organizations with something significant to say about a case to the court—most often to present a point of view, make an argument, or provide information that the parties to the case may not have communicated. Amicus briefs are burdensome in terms of the time, energy, and cost of preparing and filing. Thus, they are not undertaken lightly. Medical organizations submitted amicus briefs in the first 3 cases we consider.
Admissions, race, and diversity
The case: Students for Fair Admissions v President and Fellows of Harvard College
The American College of Obstetricians and Gynecologists (ACOG) joined an amici curiae brief in Students for Fair Admissions v President and Fellows of Harvard College (and the University of North Carolina [UNC]).1 This case challenged the use of racial preferences in college admissions. The Association of American Medical Colleges (AAMC) was the lead organization; nearly 40 other health-related organizations joined the brief.
The legal claim. Those filing the suits asserted that racial preferences by public colleges violate the 14th Amendment’s Equal Protection Clause (“no state shall deny to any person … the equal protection of the law”). That is, if a state university gives racial preferences in selective admissions, it denies some other applicant the equal protection of the law. As for private schools (in this case, Harvard), Title VI of the Civil Rights Act of 1964 has the same standards as the Equal Protection Clause. Thus, the Court consolidated the cases and used the same legal standard in considering public and private colleges (with “colleges” including professional and graduate programs as well as undergraduate institutions).
Background. For nearly 50 years, the Supreme Court has allowed limited racial preferences in college admissions. Those preferences could only operate as a plus, however, and not a negative for applicants and be narrowly tailored. The measure was instituted temporarily; in a 2003 case, the Court said, “We expect that 25 years from now, the use of racial preferences will no longer be necessary.”2
Decision. In a 6-3 decision, the Court held (in the UNC case) that racial preferences generally violate the Constitution, and by a 6-2 decision (in the Harvard case) these preferences violate the Civil Rights Act of 1964. (Justice Jackson was recused in the Harvard case because of a conflict.) The opinion covered 237 pages in the US Reports, so any summary is incomplete.
The majority concluded, “The Harvard and UNC admissions programs cannot be reconciled with the guarantees of the Equal Protection Clause. Both programs lack sufficiently focused and measurable objectives warranting the use of race, unavoidably employ race in a negative manner, involve racial stereotyping, and lack meaningful end points. We have never permitted admissions programs to work in that way, and we will not do so today.”3
There were 3 concurring opinions and 2 dissents in the case. The concurrences reviewed the history of the Equal Protection Clause and the Civil Rights Act, the damage racial preferences can do, and the explicit limits the Court said there must be on racial preferences in higher education. The dissents had a different view of the legal history of the 14th Amendment. They said the majority was turning a blind eye to segregation in society and the race-based gap in America.
As a practical matter, this case means that colleges, including professional schools, cannot use racial preferences. The Court said that universities may consider essays and the like in which applicants describe how their own experiences as an individual (including race) have affected their own lives. However, the Court cautioned that “universities may not simply establish through application essays or other means the regime we hold unlawful today.”3
Continue to: The amici brief...
The amici brief
ACOG joined 40 other health-related organizations in filing an amici brief (multiple “friends”) in Students for Fair Admission. The AAMC led the brief, with the others signing as amici.4 The brief made 3 essential points: diversity in medical education “markedly improves health outcomes,” and a loss of diversity “threaten[s] patients’ health; medical schools engage in an intense “holistic” review of applicants for admission; and medical schools must consider applicants’ “full background” (including race) to achieve their educational and professional goals.4
A powerful part of the brief described the medical school admissions process, particularly the very “holistic” review that is not entirely dependent on admissions scores. The brief effectively weaves the consideration of race into this process, mentioning race (on page 22) only after discussing many other admissions factors.
Child custody decisions related to the Indian Child Welfare Act
The case: Haaland v Brackeen
The American Medical Association (AMA) and the American Academy of Pediatrics filed a brief in Haaland v Brackeen5 involving the constitutionality of the 1978 Indian Child Welfare Act (ICWA). The statute followed a terrible history of Indian children being removed from their families inappropriately, as detailed in a concurring opinion by Justice Gorsuch.5 The two purposes of the act were to promote raising Native American children in their culture and stem the downward trend in tribal membership.
The legal claim. The Court consolidated several cases. Essentially, a 10-month-old child (A.L.M.) was placed in foster care with the Brackeens in Texas. After more than 1 year, the Brackeens sought adoption; the biological father, mother, and grandparents all supported it. The Navajo and Cherokee Nations objected and informed the Texas court that they had found alternative placement with (nonrelative) tribal members in New Mexico. The “court-appointed guardian and a psychological expert … described the strong emotional bond between A.L.M. and his foster parents.” The court denied the adoption petition based on ICWA’s preference for tribe custody, and the Brackeens filed a lawsuit.
Decision. The constitutional claim in the case was that Congress lacked the authority to impose these substantial rules on states in making child custody decisions. The Supreme Court, in a 7-2 decision, upheld the constitutionality of the ICWA.
The amici brief
The joint amici brief of the American Academy of Pediatrics (AAP) and the AMA argued that tribes are “extended families” of Native American children.6 It noted the destructive history of removing Native American children from their families and suggested that kinship care improves children’s health. To its credit, the brief also honestly noted the serious mental health and suicide rates in some tribes, which suggest issues that might arise in child custody and adoption cases.
The Court did not, in this case, take up another constitutional issue that the parties raised—whether the strong preference for Native American over non ̶ Native American custody violates the Equal Protection Clause of the 14th Amendment. The Court said the parties to this case did not have standing to raise the issue. Justice Kavanaugh, concurring, said it was a “serious” issue and invited it to be raised in another case.5
False Claims Act cases
The case: Costs for SuperValu prescriptions
The legal claim. One FCA case this Term involved billings SuperValu made for outpatient prescriptions in Medicare-Medicaid programs. As its “usual and customary” costs, it essentially reported a list price that did not include the substantial discounts it commonly gave.
Background. Subjective knowledge (what the defendant actually knows) may seem impossible to prove—the defendant could just say, “I did not know I was doing wrong.” Over time the law has developed several ways of demonstrating “knowing.” Justice Thomas, writing for a unanimous Court, held that whistleblowers or the government might prove “knowing” in 3 ways:
1. defendants “actually knew that their reported prices were not their ‘usual and customary’ prices when they reported them”
2. were aware of a substantial risk that their higher, retail prices were not their “usual and customary” prices and intentionally avoided learning whether their reports were accurate
3. were aware of such a substantial and unjustifiable risk but submitted the claims anyway.9
Of course, records of the company, information from the whistleblower, and circumstantial evidence may be used to prove any of these; it does not require the company’s admission.
The Court said that if the government or whistleblowers make a showing of any of these 3 things, it is enough.
Decision. The case was returned to the lower court to apply these rules.
The amici brief
The American Hospital Association and America’s Health Insurance Plans filed an amici brief.10 It reminded the Court that many reimbursement regulations are unclear. Therefore, it is inappropriate to impose FCA liability for guessing incorrectly what the regulations mean. Having to check on every possible ambiguity was unworkable. The Court declined, however, the suggestion that defendants should be able to use any one of many “objectively” reasonable interpretations of regulations.
Continue to: The case: Polansky v Executive Health Resources...
The case: Polansky v Executive Health Resources
Health care providers who dislike the FCA may find solace this Term in this second FCA case.11
The legal claim. Polansky, a physician employed by a medical billing company, became an “intervenor” in a suit claiming the company assisted hospitals in false billing (inpatient claims for outpatient services). The government sought to dismiss the case, but Polansky refused.
Decision. The case eventually reached the Supreme Court, which held that the government may enter an FCA case at any time and move to dismiss the case even over the objection of a whistleblower. The government does not seek to enter a case in order to file dismissal motions often. When it does so, whistleblowers are protected by the fact that the dismissal motion requires a hearing before the federal court.
An important part of this case has escaped much attention. Justices Thomas, Kavanaugh, and Barrett invited litigation to determine if allowing private whistleblowers to represent the government’s interest is consistent with Article II of the Constitution.11 The invitation will likely be accepted. We expect to see cases challenging the place of “intervenors” pursuing claims when the government has declined to take up the case. The private intervenor is a crucial provision of the current FCA, and if such a challenge were successful, it could substantially reduce FCA cases.
Criminal false claims
Dubin overbilled Medicaid for psychological testing by saying the testing was done by a licensed psychologist rather than an assistant. The government claimed the “identity theft” was using the patient’s (actual) Medicaid number in submitting the bill.12 The Court unanimously held the overbilling was not aggravated identity theft as defined in federal law. Dubin could be convicted of fraudulent billing but not aggravated identity theft, thereby avoiding the mandatory prison term.
Patents of “genus” targets
The case: Amgen v Sanofi
Background. “Genus” patents allow a single pharmaceutical company to patent every antibody that binds to a specific amino acid on a naturally occurring protein. In this case, the patent office had granted a “genus” patent on “all antibodies” that bind to the naturally occurring protein PCSK9 and block it from hindering the body’s mechanism for removing low-density lipoprotein (LDL) cholesterol from the bloodstream,13 helping to reduce LDL cholesterol levels. These patents could involve millions of antibodies—and Amgen was claiming a patent on all of them. Amgen and Sanofi marketed their products, each with their own unique amino acid sequence.13 Amgen sued Sanofi for violating its patent rights.
Decision. The Court unanimously held that Amgen did not have a valid patent on all antibodies targeting PCSK9, only those that it had explicitly described in its patent application—a ruling based on a 150-year-old technical requirement for receiving a patent. An applicant for a patent must include “a written description of the invention, and of the manner and process of making and using it, in such full, clear, concise, and exact terms as to enable any person skilled in the art…to make and use the same.”13 Amgen’s patent provided the description for only a few of the antibodies, but from the description in its application others could not “make and use” all of the antibodies targeting PCSK9.
While the decision was vital for future pharmaceuticals, the patent principle on which it was based has an interesting history. The Court noted that it affected the telegraph (Morse lost part of his patent), electric lights (Edison won his case against other inventors), and the glue for wood veneering (Perkins Glue Company lost).13
Continue to: Other notable decisions...
Other notable decisions
Student loans
The Court struck down the Biden Administration’s student loan forgiveness program, which would have cost approximately $430 billion.14 The central issue was whether the administration had the authority for such massive loan forgiveness; that is, whether Congress had authorized the broad loan forgiveness. The administration claimed authority from the post ̶ 9/11 HEROES Act, which allows the Secretary of Education to “waive or modify” loan provisions during national emergencies.
Free speech and the wedding web designer
303 Creative v Elenis involved a creative website designer who did not want to be required to create a website for a gay wedding.15 The designer had strong beliefs against same-sex marriages, but Colorado sought to force her to do so under the state “public accommodations” law. In a 6-3 decision, the Court held that the designer had a “free speech” right. That is, the state could not compel her to undertake speech expressing things she did not believe. This was because the website design was an expressive, creative activity and therefore was “speech” under the First Amendment.
Wetlands and the Clean Water Act
The essential issue in Sackett v Environmental Protection Agency (EPA) was the definitions of waters of the United States and related wetlands. The broad definition the EPA used meant it had jurisdiction to regulate an extraordinary amount of territory. It had, for example, prevented the Sacketts from building a modest house claiming it was part of the “waters of the United States because they were near a ditch that fed into a creek, which fed into Priest Lake, a navigable, intrastate lake.” The Court held that the EPA exceeded its statutory authority to define “wetlands.”16
The Court held that under the Clean Water Act, for the EPA to establish jurisdiction over adjacent wetlands, it must demonstrate that16:
1. “the adjacent body of water constitutes waters of the United States (ie, a relatively permanent body of water connected to traditional interstate navigable waters)…”
2. “…the wetland has a continuous surface connection with that water, making it difficult to determine where the water ends, and the wetland begins.”
Under this definition, the Sacketts could build their house. This was a statutory interpretation case. Therefore, Congress can expand or otherwise change the EPA’s authority under the Clean Water Act and other legislation.
Conclusions: A new justice, “shadow docket,” and ethics rules
SCOTUS’ newest member. When the Marshall called the Court into session on October 3, 2022, it had a new member, Justice Ketanji Brown Jackson. She was sworn in on June 30, 2022, when her predecessor (Justice Breyer) officially retired. She had been a law clerk for Justice Breyer in 1999, as well as a district court judge and court of appeals judge. Those who count such things described her as the “chattiest justice.”17 She spoke more than any other justice—by one count, a total of 75,632 words (an average of 1,300 words in each of the 58 arguments).
A more balanced Court? Most commentators view the Court as more balanced or less conservative than the previous Term. For example, Justice Sotomayor was in the majority 40% last Term but 65% this Term. Justice Thomas was in the majority 75% last Term but 55% this Term. Put another way, this Term in the divided cases, the liberal justices were in the majority 64% of the time, compared with the conservative justices 73%.18 Of course, these differences may reflect a different set of cases rather than a change in the direction of the Court. There were 11 (or 12, depending on how 1 case is counted) 6-3 cases, but only 5 were considered ideological. That suggests that, in many cases, the coalitions were somewhat fluid.
“Shadow docket” controversy continues.19 Shadow docket refers to orders the Court makes that do not follow oral arguments and often do not have written opinions. The orders are all publicly available. This Term a close examination of the approximately 30 shadow docket opinions shows that the overwhelming majority were dissents or explanations about denials of certiorari. The Court ordered only a few stays or injunctions via the shadow docket. One shadow docket stay (that prevented a lower court order from going into effect) is particularly noteworthy. A federal judge had ordered the suspension of the distribution of mifepristone while courts considered claims that the US Food and Drug Administration (FDA) had improperly approved the drug. In a shadow docket order, the Court issued the stay to allow mifepristone to be sold while the case challenging its approval was heard.20 The only opinion was a dissent from Justice Alito. But it also demonstrates the importance of the shadow docket. Without this intervention, in at least part of the country, the distribution of mifepristone would have been interrupted pending the outcome of the FDA cases.
In August, the Court delayed a settlement in the Purdue Pharma liability bankruptcy case.21 It also stayed an injunction of a lower court, thereby permitting federal “ghost guns” regulations to go into effect at least temporarily.22
More ethics rules to come? Another area in which the Court faced criticism was formal ethics rules. The justices make financial disclosures, but these are somewhat ambiguous. There is likely to be increasing pressure for a more complete disclosure of non-financial relationships and more formal ethics rules. ●
The Court had, by September 1, 2023, accepted 22 cases for hearing next Term.1 The cases include a challenge to the extraordinary funding provision for the Consumer Financial Protection Bureau, another racial challenge to congressional districts (South Carolina), the status of Americans with Disability Act “testers” who look for violations without ever intending to use the facilities, the level of deference courts should give to interpreting federal statutes (so-called “Chevron” deference), the opioid (OxyContin ) bankruptcy, and limitations on gun ownership. This represents less than half of the cases the Court will likely hear next Term, so the Court will add many more cases to the docket. It promises to be an appealing Term.
Reference
1. October Term 2023. SCOTUSblog website. Accessed August 29, 2023. https://www.scotusblog.com/case-files/terms/ot2023/
When the Court adjourned on June 30, 2023, it had considered 60 cases, plus hundreds of petitions asking it to hear cases. Most commentators count 55 cases decided after briefing and oral argument and where there was a signed opinion. The information below uses 55 cases unless otherwise noted. During the 2022-2023 Term, the Court:
- upheld liability for the involuntary administration of psychotropic drugs in nursing home1
- permitted disabled students, in some instances, both to make Individuals with Disabilities Education Act (IDEA) claims for services and to file Americans with Disabilities Act (ADA) lawsuits against their schools2
- upheld a statute that makes it illegal to “encourage or induce an alien to come to, enter, or reside in the United States, knowing or in reckless disregard of the fact that such coming to, entry, or residence is or will be in violation of law.” The defendant had used a scam promising noncitizens “adult adoptions” (of which there is no such thing) making it legal for them to come to and stay in the United States.3
- narrowed the “fair use” of copyrighted works. It held that Andy Warhol’s use of a copyrighted photograph in his famous Prince prints was not “transformative” in a legal sense largely because the photo and prints “share the same use”—magazine illustrations.4
- in another intellectual property case, held that Jack Daniel’s might sue a dog toy maker for a rubber dog toy that looked like a Jack Daniel’s bottle5
- further expanded the Federal Arbitration Act by holding that a federal district court must immediately stay court proceedings if one party is appealing a decision not to require arbitration6
- held that two social media companies were not responsible for terrorists using their platforms to recruit others to their cause. It did not, however, decide whether §230 of the Communication Decency Act protects companies from liability.7
- made it easier for employees to receive accommodation for their religious practices and beliefs. Employers must make religious accommodations unless the employer can show that “the burden of granting an accommodation would result in substantial increased [financial and other] costs in relation to the conduct of its particular business.”8
- declined to hear an appeal from Johnson & Johnson (through a subsidiary, Ethicon) about pelvic mesh. In this case, the California Attorney General filed a lawsuit against Ethicon for false advertising by failing to detail the risks of pelvic mesh. The lower courts estimated 240,000 written violations of the law by Ethicon between 2008 and 2017. The trial and appeal to California courts resulted in a judgment of $302 million against Johnson & Johnson. The company asked the Court to review that judgment, but the Court denied certiorari. That likely means the $302 million is final.
References
1. Health and Hospital Corporation of Marion Cty. v Talevski, Docket no. 21-806; June 8, 2023.
2. Luna Perez v Sturgis Public Schools, Docket no. 21-887; March 21, 2023.
3. United States v Hansen, Docket no. 22-179; June 23, 2023.
4. Andy Warhol Foundation for Visual Arts, Inc. v Goldsmith, Docket no. 21-869; May 18, 2023.
5. Jack Daniel’s Properties, Inc. v VIP Products LLC, Docket no. 22-148; June 8, 2023.
6. Coinbase, Inc. v Bielski, Docket no. 22-105; June 23, 2023.
7. Gonzalez v Google LLC, Docket no. 21-1333; May 18, 2023.
8. Groff v DeJoy, Docket no. 22-273; June 29, 2023.
- Students for Fair Admissions, Inc. v President and Fellows of Harvard College, 600 US ___ (2023).
- Grutter v Bollinger, 539 US 306, 326 (2003).
- Students for Fair Admissions, Inc. v President and Fellows of Harvard College, 600 US ___, 39 (2023).
- Brief for Amici Curiae Association of American Medical Colleges et al. in Support of Respondents, Students for Fair Admissions v University of North Carolina (July 28, 2022). Accessed August 18, 2023. https://www.supremecourt.gov /DocketPDF/21/21-707/232120/20220728171307159_20 -1199%20and%2021-707%20Amicus%20Brief%20for%20 Association%20of%20American%20Medical%20Colleges%20 et%20al.pdf
- Haaland v Brackeen, Docket no. 21-376; June 15, 2023.
- Brief of American Academy of Pediatrics and American Medical Association as Amici Curiae in Support of Respondents, in Haaland v Brackeen. August 19, 2022. Accessed August 18, 2023. https://www.supremecourt.gov /DocketPDF/21/21-376/234042/20220819140750948_21-376 .amics.brief.FINAL.pdf
- Justice Department’s False Claims Act Settlements and Judgments Exceed $5.6 Billion in Fiscal Year 2021. US Department of Justice website. February 1, 2022. Accessed August 18, 2023. https://www.justice.gov/opa/pr/justice -department-s-false-claims-act-settlements-and-judgments -exceed-56-billion-fiscal-year
- False Claims Act Settlements and Judgments Exceed $2 Billion in Fiscal Year 2022. US Department of Justice website. February 7, 2023. Accessed August 18, 2023. https://www .justice.gov/opa/pr/false-claims-act-settlements-and -judgments-exceed-2-billion-fiscal-year-2022
- United States ex rel. Schutte v Supervalu Inc., Docket no. 21-1326; June 1, 2023.
- Brief of American Hospital Association and America’s Health Insurance Plans as Amici Curiae in Support of Respondents, in Schutte v Supervalu. March 2023. Accessed August 18, 2023. https://www.supremecourt.gov/DocketPDF/21/21-1326 /262428/20230331113854936_3-31-23%20AHA_AHIP _Amicus_Brief.pdf
- United States ex rel. Polansky v Executive Health Resources, Inc., Docket no. 21-1052; June 16, 2023.
- Dubin v United States, Docket no. 22-10; June 8, 2023.
- Amgen v Sanofi, 598 US ___ (2023).
- Biden v Nebraska, 600 US ___ (2023).
- 303 Creative LLC v Elenis, 600 US ___ (2023).
- Sackett v Environmental Protection Agency, Docket no. 21454; May 25, 2023.
- Krochtengel J. Jackson debuts as chattiest Justice. Law360. July 3, 2023. https://www.law360.com/articles/1692839 /jackson-debuts-as-chattiest-justice
- Feldman A. Another One Bites the Dust: End of 2022/2023 Supreme Court Term Statistics. EmpiricalScotus website. 30, 2023. Accessed August 18, 2023. https://empiricalscotus .com/2023/06/30/another-one-bites-2022/
- Vladeck S. The Shadow Docket: How the Supreme Court Uses Stealth Rulings to Amass Power and Undermine the Republic. New York, New York; Basic Books; 2023.
- Danco Laboratories, LLC v Alliance for Hippocratic Medicine. Docket no. 22A902; April 21, 2023.
- Harrington v Purdue Pharma, 23-124 (23A87).
- Garland v Vanderstok, 23-10718 (August 8, 2023).
- Students for Fair Admissions, Inc. v President and Fellows of Harvard College, 600 US ___ (2023).
- Grutter v Bollinger, 539 US 306, 326 (2003).
- Students for Fair Admissions, Inc. v President and Fellows of Harvard College, 600 US ___, 39 (2023).
- Brief for Amici Curiae Association of American Medical Colleges et al. in Support of Respondents, Students for Fair Admissions v University of North Carolina (July 28, 2022). Accessed August 18, 2023. https://www.supremecourt.gov /DocketPDF/21/21-707/232120/20220728171307159_20 -1199%20and%2021-707%20Amicus%20Brief%20for%20 Association%20of%20American%20Medical%20Colleges%20 et%20al.pdf
- Haaland v Brackeen, Docket no. 21-376; June 15, 2023.
- Brief of American Academy of Pediatrics and American Medical Association as Amici Curiae in Support of Respondents, in Haaland v Brackeen. August 19, 2022. Accessed August 18, 2023. https://www.supremecourt.gov /DocketPDF/21/21-376/234042/20220819140750948_21-376 .amics.brief.FINAL.pdf
- Justice Department’s False Claims Act Settlements and Judgments Exceed $5.6 Billion in Fiscal Year 2021. US Department of Justice website. February 1, 2022. Accessed August 18, 2023. https://www.justice.gov/opa/pr/justice -department-s-false-claims-act-settlements-and-judgments -exceed-56-billion-fiscal-year
- False Claims Act Settlements and Judgments Exceed $2 Billion in Fiscal Year 2022. US Department of Justice website. February 7, 2023. Accessed August 18, 2023. https://www .justice.gov/opa/pr/false-claims-act-settlements-and -judgments-exceed-2-billion-fiscal-year-2022
- United States ex rel. Schutte v Supervalu Inc., Docket no. 21-1326; June 1, 2023.
- Brief of American Hospital Association and America’s Health Insurance Plans as Amici Curiae in Support of Respondents, in Schutte v Supervalu. March 2023. Accessed August 18, 2023. https://www.supremecourt.gov/DocketPDF/21/21-1326 /262428/20230331113854936_3-31-23%20AHA_AHIP _Amicus_Brief.pdf
- United States ex rel. Polansky v Executive Health Resources, Inc., Docket no. 21-1052; June 16, 2023.
- Dubin v United States, Docket no. 22-10; June 8, 2023.
- Amgen v Sanofi, 598 US ___ (2023).
- Biden v Nebraska, 600 US ___ (2023).
- 303 Creative LLC v Elenis, 600 US ___ (2023).
- Sackett v Environmental Protection Agency, Docket no. 21454; May 25, 2023.
- Krochtengel J. Jackson debuts as chattiest Justice. Law360. July 3, 2023. https://www.law360.com/articles/1692839 /jackson-debuts-as-chattiest-justice
- Feldman A. Another One Bites the Dust: End of 2022/2023 Supreme Court Term Statistics. EmpiricalScotus website. 30, 2023. Accessed August 18, 2023. https://empiricalscotus .com/2023/06/30/another-one-bites-2022/
- Vladeck S. The Shadow Docket: How the Supreme Court Uses Stealth Rulings to Amass Power and Undermine the Republic. New York, New York; Basic Books; 2023.
- Danco Laboratories, LLC v Alliance for Hippocratic Medicine. Docket no. 22A902; April 21, 2023.
- Harrington v Purdue Pharma, 23-124 (23A87).
- Garland v Vanderstok, 23-10718 (August 8, 2023).
How to avoid abandonment claims when terminating care
Psychiatric clinicians may unilaterally decide to end a treatment relationship with a patient when the relationship is no longer therapeutic, such as when the patient does not adhere to treatment, repeatedly misses appointments, exhibits abusive behaviors, or fails to pay for treatment.1 Claims of abandonment can arise if ending the treatment relationship is not executed properly. Abandonment is the termination of a treatment relationship with a patient who remains in need of treatment, has no suitable substitute treatment, and subsequently experiences damages as a result of the termination.2 When a patient terminates a treatment relationship, there are no legal bases for abandonment claims.3 In this article, I provide a few practical tips for properly terminating the doctor-patient relationship to limit the likelihood of claims of abandonment.
Know your jurisdiction’s requirements for terminating the relationship. Each state has its own legal definition of a doctor-patient relationship as well as requirements for ending it. Abandonment claims are unfounded in the absence of a doctor-patient relationship.3 Contact the appropriate licensing board to determine what your state’s regulatory requirements are. If necessary, consult with your attorney or a risk management professional for guidance.4
Communicate clearly. Communicate with your patient about the end of the treatment relationship in a clear and consistent manner, both verbally and in writing, because a termination should be viewed as a formal, documented event.3 Except in situations requiring immediate termination, psychiatric clinicians should inform the patient about the reason(s) for termination,4 the need for continued treatment,3 and the type of recommended treatment.3 This discussion should be summarized in a termination letter given to the patient that includes termination language, referral sources, the end date of treatment, and a request for authorization to release a copy of the patient’s medical records to their new clinician.3,4
Give adequate time, set boundaries, and document. Thirty days is generally considered adequate time for a patient to find a new clinician,5 unless the patient lives in an area where there is a shortage of psychiatric clinicians, in which case a longer time period would be appropriate.3 Ensure your patient has a sufficient supply of medication(s) until they establish care with a new clinician.4 Offer to provide emergency care for a reasonable period of time during the termination process unless a safety concern requires immediate termination.4 Avoid situations in which the patient attempts to re-enter your care. Document the reason for the termination in your progress notes and keep a copy of the termination letter in the patient’s medical record.4
1. Mossman D. ‘Firing’ a patient: may a psychiatrist unilaterally terminate care? Current Psychiatry. 2010;9(12):18,20,22,29.
2. Van Susteren L. Psychiatric abandonment: pitfalls and prevention. Psychiatric Times. 2001;18(8). Accessed April 30, 2023. https://www.psychiatrictimes.com/view/psychiatric-abandonment-pitfalls-and-prevention
3. Stankowski J, Sorrentino R. Abandonment and unnecessary commitment. In: Ash P, Frierson RL, Hatters Friedman S, eds. Malpractice and Liability in Psychiatry. Springer Nature Publishing; 2022:129-135.
4. Funicelli A. Avoiding abandonment claim: how to properly terminate patients from your practice. Psychiatric News. 2022;57(12):13,41. https://psychnews.psychiatryonline.org/doi/10.1176/appi.pn.2022.12.12.23
5. American Psychiatric Association. APA Quick Practice Guide: Ending the Physician/Patient Relationship. 2014. Accessed April 30, 2023. https://www.psychiatry.org/File%20Library/Psychiatrists/Practice/Practice-Management/Practice-Management-Guides/GeneralIssues-terminating-patient-relationships.pdf
Psychiatric clinicians may unilaterally decide to end a treatment relationship with a patient when the relationship is no longer therapeutic, such as when the patient does not adhere to treatment, repeatedly misses appointments, exhibits abusive behaviors, or fails to pay for treatment.1 Claims of abandonment can arise if ending the treatment relationship is not executed properly. Abandonment is the termination of a treatment relationship with a patient who remains in need of treatment, has no suitable substitute treatment, and subsequently experiences damages as a result of the termination.2 When a patient terminates a treatment relationship, there are no legal bases for abandonment claims.3 In this article, I provide a few practical tips for properly terminating the doctor-patient relationship to limit the likelihood of claims of abandonment.
Know your jurisdiction’s requirements for terminating the relationship. Each state has its own legal definition of a doctor-patient relationship as well as requirements for ending it. Abandonment claims are unfounded in the absence of a doctor-patient relationship.3 Contact the appropriate licensing board to determine what your state’s regulatory requirements are. If necessary, consult with your attorney or a risk management professional for guidance.4
Communicate clearly. Communicate with your patient about the end of the treatment relationship in a clear and consistent manner, both verbally and in writing, because a termination should be viewed as a formal, documented event.3 Except in situations requiring immediate termination, psychiatric clinicians should inform the patient about the reason(s) for termination,4 the need for continued treatment,3 and the type of recommended treatment.3 This discussion should be summarized in a termination letter given to the patient that includes termination language, referral sources, the end date of treatment, and a request for authorization to release a copy of the patient’s medical records to their new clinician.3,4
Give adequate time, set boundaries, and document. Thirty days is generally considered adequate time for a patient to find a new clinician,5 unless the patient lives in an area where there is a shortage of psychiatric clinicians, in which case a longer time period would be appropriate.3 Ensure your patient has a sufficient supply of medication(s) until they establish care with a new clinician.4 Offer to provide emergency care for a reasonable period of time during the termination process unless a safety concern requires immediate termination.4 Avoid situations in which the patient attempts to re-enter your care. Document the reason for the termination in your progress notes and keep a copy of the termination letter in the patient’s medical record.4
Psychiatric clinicians may unilaterally decide to end a treatment relationship with a patient when the relationship is no longer therapeutic, such as when the patient does not adhere to treatment, repeatedly misses appointments, exhibits abusive behaviors, or fails to pay for treatment.1 Claims of abandonment can arise if ending the treatment relationship is not executed properly. Abandonment is the termination of a treatment relationship with a patient who remains in need of treatment, has no suitable substitute treatment, and subsequently experiences damages as a result of the termination.2 When a patient terminates a treatment relationship, there are no legal bases for abandonment claims.3 In this article, I provide a few practical tips for properly terminating the doctor-patient relationship to limit the likelihood of claims of abandonment.
Know your jurisdiction’s requirements for terminating the relationship. Each state has its own legal definition of a doctor-patient relationship as well as requirements for ending it. Abandonment claims are unfounded in the absence of a doctor-patient relationship.3 Contact the appropriate licensing board to determine what your state’s regulatory requirements are. If necessary, consult with your attorney or a risk management professional for guidance.4
Communicate clearly. Communicate with your patient about the end of the treatment relationship in a clear and consistent manner, both verbally and in writing, because a termination should be viewed as a formal, documented event.3 Except in situations requiring immediate termination, psychiatric clinicians should inform the patient about the reason(s) for termination,4 the need for continued treatment,3 and the type of recommended treatment.3 This discussion should be summarized in a termination letter given to the patient that includes termination language, referral sources, the end date of treatment, and a request for authorization to release a copy of the patient’s medical records to their new clinician.3,4
Give adequate time, set boundaries, and document. Thirty days is generally considered adequate time for a patient to find a new clinician,5 unless the patient lives in an area where there is a shortage of psychiatric clinicians, in which case a longer time period would be appropriate.3 Ensure your patient has a sufficient supply of medication(s) until they establish care with a new clinician.4 Offer to provide emergency care for a reasonable period of time during the termination process unless a safety concern requires immediate termination.4 Avoid situations in which the patient attempts to re-enter your care. Document the reason for the termination in your progress notes and keep a copy of the termination letter in the patient’s medical record.4
1. Mossman D. ‘Firing’ a patient: may a psychiatrist unilaterally terminate care? Current Psychiatry. 2010;9(12):18,20,22,29.
2. Van Susteren L. Psychiatric abandonment: pitfalls and prevention. Psychiatric Times. 2001;18(8). Accessed April 30, 2023. https://www.psychiatrictimes.com/view/psychiatric-abandonment-pitfalls-and-prevention
3. Stankowski J, Sorrentino R. Abandonment and unnecessary commitment. In: Ash P, Frierson RL, Hatters Friedman S, eds. Malpractice and Liability in Psychiatry. Springer Nature Publishing; 2022:129-135.
4. Funicelli A. Avoiding abandonment claim: how to properly terminate patients from your practice. Psychiatric News. 2022;57(12):13,41. https://psychnews.psychiatryonline.org/doi/10.1176/appi.pn.2022.12.12.23
5. American Psychiatric Association. APA Quick Practice Guide: Ending the Physician/Patient Relationship. 2014. Accessed April 30, 2023. https://www.psychiatry.org/File%20Library/Psychiatrists/Practice/Practice-Management/Practice-Management-Guides/GeneralIssues-terminating-patient-relationships.pdf
1. Mossman D. ‘Firing’ a patient: may a psychiatrist unilaterally terminate care? Current Psychiatry. 2010;9(12):18,20,22,29.
2. Van Susteren L. Psychiatric abandonment: pitfalls and prevention. Psychiatric Times. 2001;18(8). Accessed April 30, 2023. https://www.psychiatrictimes.com/view/psychiatric-abandonment-pitfalls-and-prevention
3. Stankowski J, Sorrentino R. Abandonment and unnecessary commitment. In: Ash P, Frierson RL, Hatters Friedman S, eds. Malpractice and Liability in Psychiatry. Springer Nature Publishing; 2022:129-135.
4. Funicelli A. Avoiding abandonment claim: how to properly terminate patients from your practice. Psychiatric News. 2022;57(12):13,41. https://psychnews.psychiatryonline.org/doi/10.1176/appi.pn.2022.12.12.23
5. American Psychiatric Association. APA Quick Practice Guide: Ending the Physician/Patient Relationship. 2014. Accessed April 30, 2023. https://www.psychiatry.org/File%20Library/Psychiatrists/Practice/Practice-Management/Practice-Management-Guides/GeneralIssues-terminating-patient-relationships.pdf
Criminal liability: What are the risks for medical professionals?
Medical professionals are well aware that civil liability (malpractice) may incur when a patient is harmed because of carelessness (negligence). Recent criminal charges against physicians and a nurse, however, have called medical professionals’ attention to the fact that they also may face criminal charges for inappropriate practice.
We cite 2 cases in which criminal liability resulted from bad medical practice. In both instances, there was considerable concern among medical professionals that criminal charges for making a mistake would make it difficult to practice without fear of criminal charges. One concern is that criminal charges could drive good people out of the profession or make them too cautious.1
We look more closely at those 2 cases in which criminal liability was imposed. These cases are outliers. Relatively few criminal cases against medical professionals are based on the quality of care. (There are, however, more criminal charges related to fraudulent billing and other insurance fraud, kickbacks, Medicare and Medicaid abuse, and the like.2) At the same time, the criminal law does not stop at the front door of a clinic or hospital.3 When medical professionals engage in seriously inappropriate health care conduct that directly harms someone, criminal liability may result.4
Anatomy of a crime
Crimes generally require a specific mental state (mens rea) and an act (actus reus). The law specifies the mental state required for conviction. It can range from premeditation—once commonly called “malice aforethought”—to negligence. The mens rea requirement is an essential element of the crime—as we will see in the discussion of the prescription drug cases. A few offenses do not require even negligence, but overwhelmingly, crimes require something more than simple negligence.5
The act requirement is generally obvious, such as firing a gun, driving while intoxicated, or recklessly giving inappropriate medication to a patient. It may include “attempts,” crimes where an act was not completed. For example, attempted murder or conspiracy to commit do not require a completed offense, only intent plus overt acts toward carrying out the crime. Similarly, the wrongful act usually has to produce some harm, but again there are exceptions (attempts). To obtain a conviction, the prosecution must prove all of the elements of the crime, including the required mens rea, beyond a reasonable doubt.6
With this general background, we turn to the first case, in which the charge was a form of homicide. Please note that the following case description was derived from news descriptions of the case, because juries do not publish opinions concerning their conclusions and court documents are unavailable. The public reports therefore may contain factual gaps and errors.
CASE 1 Patient dies after nurse administers wrong drug
RaDonda Vaught, a 38-year-old experienced registered nurse employed at Vanderbilt University Medical Center (VUMC) in the intensive care unit (ICU), was providing care for a 76-year-old patient who was admitted to VUMC’s ICU in December 2017 in association with a brain injury. The brain injury involved a fall with resultant subdural hematoma. In preparation for a positron emission tomography (PET) scan to assess the patient’s injury, the physician team prescribed the sedative Versed (midazolam) because of the patient’s claustrophobia. During the course of treatment, Ms. Vaught inadvertently administered the wrong drug, a fatal dose of the muscle relaxant vecuronium, to the patient, which resulted in the patient being unable to breathe. Apparently, Ms. Vaught had been unable to find the midazolam and disengaged a safeguard, proceeding into override mode, and thus vecuronium was dispensed. By the time the error was noticed, the patient was already in cardiac arrest with resultant brain damage (partial brain death). The patient died soon thereafter.
How this medication error occurred
The medication error occurred when Ms. Vaught overrode a computer in the medical system when she could not find the “Versed” entry and typed in “VE,” which was the abbreviation for vecuronium. The prosecutors in the case stated that she failed to distinguish that vecuronium is dispensed as a powder and Versed as a liquid formula. The vecuronium has a red cap, which warns that it is a paralyzing agent. Ms. Vaught ignored these red flags, according to the prosecutors. Furthermore, the lawsuit filing documented her discussion that she was “distracted with something” at the time and admitted to overriding the medication warning.
Continue to: The charges in this case...
The charges in this case
The charges revolved around “criminally negligent homicide and gross neglect of an impaired adult,” the most notable charge being criminally negligent homicide. Potential consequences were up to an 8 years’ prison sentence.7
Furthermore, the Tennessee Board of Nursing revoked Ms. Vaught’s license in July 2021.8 The Board also reportedly fined her $3,000.9
The criminal proceedings were filed in Davidson County Criminal Court, with Judge Jennifer Smith presiding. Ms. Vaught repeatedly manifested remorse for the event. The patient’s family, including her son Michael and her daughters-in-law, provided tearful testimonies at the hearing. Ms. Vaught repeatedly cried during the testimonies. The nurse did not provide an apology, according to one daughter-in-law. The news media reported that the family did not want jail time for Ms. Vaught.7 Nurses across the country were “jolted,” as expressed by the news media.10
Why the controversy?
The entire issue of medical errors continues to be discussed among both the medical and the legal professions. To have a nursing personnel held to the level of criminal liability is unusual.
It was clear that Ms. Vaught took responsibility for her actions, and neither the prosecutors nor defendant attorneys sensed any evidence of malice on her part. On the other hand, there was enough evidence and concern for District Attorney Glenn Funk to proceed with prosecution-related action. Ms. Vaught was facing years in prison if convicted.
WHAT’S THE VERDICT?
In March 2022, the jury convicted Ms. Vaught of criminally negligent homicide—but not of reckless homicide, a more serious offense.
Judge Smith granted a judicial diversion, that is, the conviction would be expunged from the record if Ms. Vaught completed a 3-year probation. Judge Smith noted the “credible remorse expressed by Nurse Vaught” and went on to state, “this is a terrible, terrible, mistake and there have been consequences to the defendant.” In the courtroom, Ms. Vaught apologized to the patient’s family and conveyed that she will “forever be haunted by her role in the (patient’s) passing.”
Overall, this served as an opportunity for health care workers to address oftentimes poor working conditions, which have been exacerbated by the COVID-19 pandemic.
The Davidson County District Attorney’s office conveyed that this was one case of a careless nurse and not a reflection of the nursing profession. The prosecutors were in accord with a probation verdict. The family felt that their mother, the patient, would not want to see the nurse serve a jail sentence: “Mom was a very forgiving person.”
The patient’s cause of death was listed as “intracerebral hemorrhage and cardiac arrest.” One year later, a new death certificate was issued and noted vecuronium intoxication as the cause of death.
Continue to: The health care institution’s involvement...
The health care institution’s involvement
Approximately 1 year after an apparent anonymous tip was made to health care officials, an unscheduled state and federal investigation, with the threat of possible sanctions, occurred at the VUMC. This was predicated on the criminal indictment related to Ms. Vaught. In the end, her nursing license was revoked, as noted earlier. The family earlier reached an out-of-court settlement with the hospital and there were a number of problems identified at the university medical center.11
Legal principles in the case
Most criminal cases are state cases. Crimes are defined in state statutes, and the trial takes place in state courts. Thus, crimes are defined a little differently from state to state. Ms. Vaught, for example, was tried in Tennessee under the laws of that state.
Homicide involves the killing of a human being. It may not be a crime. For example, there is “justifiable homicide,” such as self-defense. At the other extreme is first-degree murder, an intentional and planned killing. In this case, Ms. Vaught was charged with criminally negligent homicide, which is usually the least serious of criminal homicides but is still a felony. (Some states have misdemeanor manslaughter, which was not an issue in this case.) In some states, criminally negligent homicide is sometimes referred to as involuntary manslaughter. The mens rea for involuntary manslaughter is generally recklessness or “criminal negligence.” This crime goes by various names depending on the state, but involuntary manslaughter and criminally negligent homicide are common names.
Ordinary negligence versus criminal negligence. Criminal negligence is usually considered a more serious mistake than ordinary negligence. This is where there is a difference between civil malpractice negligence and criminal negligence. Criminal negligence is somewhat more careless than ordinary negligence. To use a driving example, if Dr. A was driving home from the hospital, missed seeing a red light, and killed Joe Pedestrian, it could be ordinary negligence. If, however, Dr. B was texting or drinking while driving, causing Dr. B to be distracted and miss seeing the red light, killing a pedestrian, it could be criminal negligence and result in the conviction for the homicide. Of course, in either case there could be civil liability for causing the death.
Applying these legal principles to the reported facts in Ms. Vaught’s case, it appears there was more than simple negligence. That is, the nurse was more than careless. Using “VE” for the wrong drug might have been negligent. In addition, however, she disengaged a safeguard meant to prevent wrongful use of the drug, failed to notice that the drug was a powder instead of a liquid, and ignored the red cap warning that the drug was a paralyzing agent. It becomes apparent why the jury could have found aggravated or criminal negligence.
It is worth emphasizing that in this case, the criminal charges were unusual. For years, studies have suggested that many deaths result from medical errors. The Institute of Medicine famously said that the number of deaths from medical errors was equivalent to that of a 747 airplane crashing every day.12,13 These events result in a relatively small number of malpractice actions but an infinitesimally small number of homicide charges. Among other things, prosecutors are reluctant to pursue such cases regarding acts carried out as part of clinical duties unless there is strong evidence, and grand juries may be reluctant to indict medical professionals.14
Nonetheless, medical professionals ultimately can be criminally responsible for deaths resulting from intentional, or criminally negligent, careless practice. Such liability should not dissuade nurses or others from medical practice any more than the much more common homicide charges that can occur from driving an automobile carelessly that results in someone’s death. A fundamental purpose of the criminal law is to disincentivize unnecessarily harmful (deadly) conduct, whether it is distracted driving or distracted nursing.
Continue to: The drug-prescribing crimes...
The drug-prescribing crimes
The US Supreme Court considered a much different kind of criminal medical practice in 2 (consolidated) cases in its 2021–2022 Term. Physicians in 2 states were each tried and convicted of federal charges of illegally dispensing or distributing (prescribing) controlled substances.15 A federal statute makes it a felony for a physician, or others, “except as authorized” to “knowingly or intentionally distribute, or dispense a controlled substance.”16 Federal regulations clarify the statute. The regulation provides that a prescription is authorized only if a doctor issues it “for a legitimate medical purpose . . . acting in the usual course of professional practice.”17
CASE 2 Physicians charged with overprescribing controlled substances
In these 2 drug-prescribing cases, the physicians had grossly overprescribed the opioids. One reportedly wrote prescriptions in 2 states in exchange for payments in cash or, infrequently, firearms, approximating the cost of the prescriptions to street drugs. The other had a clinic that, over about 4 years, issued 300,000 prescriptions for controlled substances and was a significant source for some kinds of fentanyl.18
WHAT’S THE VERDICT?
In each trial, the juries found the defendant guilty of improper distribution of controlled substances. Although the charges were not homicides, the sentencing judges were much more severe than the court had been in the nursing case discussed above. One physician received a prison term of 20 years, the other, a 25-year term. These undoubtedly reflect both the outrageous conduct and the likely great harm the defendants did.
The Supreme Court heard the cases
The Supreme Court reversed these physicians’ convictions. The Court held that the lower courts had not correctly described for the juries the mens rea required for a conviction under these charges. The Supreme Court held that to be convicted of these offenses, the government had to prove “beyond a reasonable doubt that the defendant [physician] knew that he or she was acting in an unauthorized manner.”19 Both can be retried and probably will be unless they reach a plea agreement with the federal government. Nonetheless, the Court established a very high standard. Carelessness is not enough, but rather “knowingly” acting in an unauthorized way is required. Although these physicians were prosecuted under federal law, other physicians have been prosecuted under state laws limiting the distribution of controlled substances.20
Some physicians have expressed concern that the Supreme Court, in these cases, made the practice of medicine more dangerous for physicians (the threat of criminal sanctions) and patients (making it more difficult to obtain pain control, for example).21,22 That view may be overly pessimistic for 2 reasons. First, the Court actually made it more difficult to convict physicians of writing excessive prescriptions. It did so by setting a higher mens rea standard than lower courts were using, that is, the physician had to “knowingly” act in an unauthorized way. Because “knowingly” can be implied by the circumstances, taking guns or cash would be evidence that the physician knowingly misprescribed.
More fundamentally, the actions of these physicians appear to be well outside even a generous legitimate level of controlled substance prescription. These convictions should not be misunderstood as a way of federal courts to crack down on pain medications. However, the original convictions are a warning to the small handful who grossly overprescribe controlled substances.
Lessons about criminal law and the practice of medicine
Medical professionals’ strong reaction to criminal charges is understandable. Criminal charges can result in jail time (the physicians involved in the controlled substance case were sentenced to 20 years or more) and hefty fines; bring social and professional disapprobation; may lead to license discipline; and are terribly disruptive even for those found not guilty. To make matters worse, malpractice insurance ordinarily does not cover criminal charges, so any fines and the cost of defense are likely out of pocket for those charged—and that can be very expensive. Therefore, the strong reaction to the cases we have described is understandable.
At the same time, the probability of criminal charges against medical personnel for their medical treatment is very low compared with, for example, fraudulent billing, their driving habits, or tax avoidance. Criminal charges are much more likely to arise from insurance fraud, Medicare or Medicaid dishonesty, kickbacks, false statements, and similar corruption crimes rather than inadequate practice. In the cases we examined here, there is an enhanced or aggravated negligence in one case and grossly inappropriate prescribing in the others (which the Supreme Court held must be “knowingly” wrong).
Finally, there is an irony. Medical professionals worried about practice-related criminal charges should be thankful for the malpractice system. Civil malpractice is, as a practical matter, an alternative for patients who believe they were mistreated or harmed by physicians or other providers. They have the option of finding a private attorney to file a civil complaint. In the absence of that system, they would be much more likely to take their grievance and complaint to the prosecutor to seek answers and retribution. Criminal law and civil liability are each a way of allowing someone harmed by another to seek redress. Both are intended to deter harmful conduct and provide some individual and social retribution for such behavior. The civil system, of course, also provides the potential for compensation to those injured. An injured patient without the possibility of a civil suit sometimes would turn to the criminal system for satisfaction. This way, the malpractice system is a better alternative to criminal charges. ●
- Kelman B. As a nurse faces prison for a deadly error, her colleagues worry: could I be next? NPR. March 22, 2022. Accessed November 7, 2022. https://www.npr.org/sections/health-shots/2022/03/22/1087903348/as-a-nurse-faces-prison-for-a-deadly-error-her-colleagues-worry-could-i-be-next
- US Department of Justice. National health care fraud enforcement action results in charges involving over $1.4 billion in alleged losses. September 17, 2021. Accessed November 7, 2022. https://www.justice.gov/opa/pr/national-health-care-fraud-enforcement-action-results-charges-involving-over-14-billion
- Steinman G. Stuff of nightmares: criminal prosecution for malpractice. OBG Manag. 2008;20(8):35-45.
- Maher V, Cwiek M. Criminal liability for nursing and medical harm. Hosp Top. 2022 July 13;1-8.
- Singer RG. The resurgence of mens rea: III—the rise and fall of strict criminal liability. Boston Coll Law Rev. 1989;30:337-408. Accessed November 7, 2022. https://lawdigitalcommons.bc.edu/cgi/viewcontent.cgi?article=2431&context=bclr
- Sarch AF. Knowledge, recklessness and the connection requirement between actus reus and mens rea. Penn State Law Rev. 2015;120:1-51. Accessed November 7, 2022. https://ideas.dickinsonlaw.psu.edu/cgi/viewcontent.cgi?article=4120&context=dlra
- Timms M, Gluck F, Wegner R, et al. RaDonda Vaught sentenced to three years probation on a diverted sentence, could see record wiped. Tennessean. May 13, 2022. Accessed November 7, 2022. http://www.tennessean.com/story/news/crime/2022/05/13/radonda-vaught-sentened-vanderbilt-nurse/9717529002/
- Tennessee Board of Nursing. Disciplinary hearing: RaDonda Vaught, RN #205702, minutes. July 22-23, 2021. Accessed November 7, 2022. https://www.tn.gov/content/dam/tn/health/healthprofboards/nursing/meeting-minutes/Nursing%20Meeting%20Minutes%20July%2022-23,%202021.pdf
- Institute for Safe Medication Practices. TN Board of Nursing’s unjust decision to revoke nurse’s license: travesty on top of tragedy! August 12, 2021. Accessed November 7, 2022. https://www.ismp.org/resources/tn-board-nursings-unjust-decision-revoke-nurses-license-travesty-top-tragedy
- Medina E. Ex-nurse convicted in fatal medication error gets probation. New York Times. May 15, 2022. Accessed November 7, 2022. https://www.nytimes.com/2022/05/15/us/tennessee-nurse-sentencing.html
- Kelman B. In nurse’s trial, investigator says hospital bears ‘heavy’ responsibility for patient death. KHN. March 24, 2022. Accessed November 15, 2022. https://khn.org/news/article/radonda-vaught-fatal-drug-error-vanderbilt-hospital-responsibility/
- Institute of Medicine (US) Committee on Quality of Health Care in America; Kohn LT, Corrigan JM, Donaldson MS, ed. To Err Is Human: Building a Safer Health System. National Academies Press; 2000.
- Bates DW, Singh H. Two decades since To Err Is Human: an assessment of progress and emerging priorities in patient safety. Health Affairs. 2018;37:1736-1743.
- Eisenberg RL, Berlin L. When does malpractice become manslaughter? Am J Roentgenol. 2002;179:331-335.
- Xiulu Ruan v United States, 20-1410, decided June 27, 2022. https://www.supremecourt.gov/opinions/21pdf/20 -1410_1an2.pdf
- 84 Stat. 1260, 21 U. S. C. §841(a).
- 21 CFR §1306.04(a) (2021).
- Liptak A. Supreme Court sides with doctors accused of running pill mills. The New York Times. June 27, 2022.
- Xiulu Ruan v United States, at 2 (slip opinion).
- Pedemonte S. State v. Christensen: criminalizing medical malpractice. Montana Law Rev. 2022;83(1):183-193. Accessed November 7, 2022. https://scholarworks.umt.edu/cgi/view content.cgi?article=2497&context=mlr
- Szalavitz M. A recent Supreme Court ruling will help people in pain. Scientific American. September 19, 2022. Accessed November 15, 2022. https://www.scientificamerican.com/ article/a-recent-supreme-court-ruling-will-help-people-in -pain/
- Lopez I. Opioid pill peddling case threatens future of pain treatment. Bloomberg Law. March 29, 2022. Accessed November 15, 2022. https://news.bloomberglaw.com/health -law-and-business/opioid-pill-peddling-case-threatens -future-of-pain-treatment
Medical professionals are well aware that civil liability (malpractice) may incur when a patient is harmed because of carelessness (negligence). Recent criminal charges against physicians and a nurse, however, have called medical professionals’ attention to the fact that they also may face criminal charges for inappropriate practice.
We cite 2 cases in which criminal liability resulted from bad medical practice. In both instances, there was considerable concern among medical professionals that criminal charges for making a mistake would make it difficult to practice without fear of criminal charges. One concern is that criminal charges could drive good people out of the profession or make them too cautious.1
We look more closely at those 2 cases in which criminal liability was imposed. These cases are outliers. Relatively few criminal cases against medical professionals are based on the quality of care. (There are, however, more criminal charges related to fraudulent billing and other insurance fraud, kickbacks, Medicare and Medicaid abuse, and the like.2) At the same time, the criminal law does not stop at the front door of a clinic or hospital.3 When medical professionals engage in seriously inappropriate health care conduct that directly harms someone, criminal liability may result.4
Anatomy of a crime
Crimes generally require a specific mental state (mens rea) and an act (actus reus). The law specifies the mental state required for conviction. It can range from premeditation—once commonly called “malice aforethought”—to negligence. The mens rea requirement is an essential element of the crime—as we will see in the discussion of the prescription drug cases. A few offenses do not require even negligence, but overwhelmingly, crimes require something more than simple negligence.5
The act requirement is generally obvious, such as firing a gun, driving while intoxicated, or recklessly giving inappropriate medication to a patient. It may include “attempts,” crimes where an act was not completed. For example, attempted murder or conspiracy to commit do not require a completed offense, only intent plus overt acts toward carrying out the crime. Similarly, the wrongful act usually has to produce some harm, but again there are exceptions (attempts). To obtain a conviction, the prosecution must prove all of the elements of the crime, including the required mens rea, beyond a reasonable doubt.6
With this general background, we turn to the first case, in which the charge was a form of homicide. Please note that the following case description was derived from news descriptions of the case, because juries do not publish opinions concerning their conclusions and court documents are unavailable. The public reports therefore may contain factual gaps and errors.
CASE 1 Patient dies after nurse administers wrong drug
RaDonda Vaught, a 38-year-old experienced registered nurse employed at Vanderbilt University Medical Center (VUMC) in the intensive care unit (ICU), was providing care for a 76-year-old patient who was admitted to VUMC’s ICU in December 2017 in association with a brain injury. The brain injury involved a fall with resultant subdural hematoma. In preparation for a positron emission tomography (PET) scan to assess the patient’s injury, the physician team prescribed the sedative Versed (midazolam) because of the patient’s claustrophobia. During the course of treatment, Ms. Vaught inadvertently administered the wrong drug, a fatal dose of the muscle relaxant vecuronium, to the patient, which resulted in the patient being unable to breathe. Apparently, Ms. Vaught had been unable to find the midazolam and disengaged a safeguard, proceeding into override mode, and thus vecuronium was dispensed. By the time the error was noticed, the patient was already in cardiac arrest with resultant brain damage (partial brain death). The patient died soon thereafter.
How this medication error occurred
The medication error occurred when Ms. Vaught overrode a computer in the medical system when she could not find the “Versed” entry and typed in “VE,” which was the abbreviation for vecuronium. The prosecutors in the case stated that she failed to distinguish that vecuronium is dispensed as a powder and Versed as a liquid formula. The vecuronium has a red cap, which warns that it is a paralyzing agent. Ms. Vaught ignored these red flags, according to the prosecutors. Furthermore, the lawsuit filing documented her discussion that she was “distracted with something” at the time and admitted to overriding the medication warning.
Continue to: The charges in this case...
The charges in this case
The charges revolved around “criminally negligent homicide and gross neglect of an impaired adult,” the most notable charge being criminally negligent homicide. Potential consequences were up to an 8 years’ prison sentence.7
Furthermore, the Tennessee Board of Nursing revoked Ms. Vaught’s license in July 2021.8 The Board also reportedly fined her $3,000.9
The criminal proceedings were filed in Davidson County Criminal Court, with Judge Jennifer Smith presiding. Ms. Vaught repeatedly manifested remorse for the event. The patient’s family, including her son Michael and her daughters-in-law, provided tearful testimonies at the hearing. Ms. Vaught repeatedly cried during the testimonies. The nurse did not provide an apology, according to one daughter-in-law. The news media reported that the family did not want jail time for Ms. Vaught.7 Nurses across the country were “jolted,” as expressed by the news media.10
Why the controversy?
The entire issue of medical errors continues to be discussed among both the medical and the legal professions. To have a nursing personnel held to the level of criminal liability is unusual.
It was clear that Ms. Vaught took responsibility for her actions, and neither the prosecutors nor defendant attorneys sensed any evidence of malice on her part. On the other hand, there was enough evidence and concern for District Attorney Glenn Funk to proceed with prosecution-related action. Ms. Vaught was facing years in prison if convicted.
WHAT’S THE VERDICT?
In March 2022, the jury convicted Ms. Vaught of criminally negligent homicide—but not of reckless homicide, a more serious offense.
Judge Smith granted a judicial diversion, that is, the conviction would be expunged from the record if Ms. Vaught completed a 3-year probation. Judge Smith noted the “credible remorse expressed by Nurse Vaught” and went on to state, “this is a terrible, terrible, mistake and there have been consequences to the defendant.” In the courtroom, Ms. Vaught apologized to the patient’s family and conveyed that she will “forever be haunted by her role in the (patient’s) passing.”
Overall, this served as an opportunity for health care workers to address oftentimes poor working conditions, which have been exacerbated by the COVID-19 pandemic.
The Davidson County District Attorney’s office conveyed that this was one case of a careless nurse and not a reflection of the nursing profession. The prosecutors were in accord with a probation verdict. The family felt that their mother, the patient, would not want to see the nurse serve a jail sentence: “Mom was a very forgiving person.”
The patient’s cause of death was listed as “intracerebral hemorrhage and cardiac arrest.” One year later, a new death certificate was issued and noted vecuronium intoxication as the cause of death.
Continue to: The health care institution’s involvement...
The health care institution’s involvement
Approximately 1 year after an apparent anonymous tip was made to health care officials, an unscheduled state and federal investigation, with the threat of possible sanctions, occurred at the VUMC. This was predicated on the criminal indictment related to Ms. Vaught. In the end, her nursing license was revoked, as noted earlier. The family earlier reached an out-of-court settlement with the hospital and there were a number of problems identified at the university medical center.11
Legal principles in the case
Most criminal cases are state cases. Crimes are defined in state statutes, and the trial takes place in state courts. Thus, crimes are defined a little differently from state to state. Ms. Vaught, for example, was tried in Tennessee under the laws of that state.
Homicide involves the killing of a human being. It may not be a crime. For example, there is “justifiable homicide,” such as self-defense. At the other extreme is first-degree murder, an intentional and planned killing. In this case, Ms. Vaught was charged with criminally negligent homicide, which is usually the least serious of criminal homicides but is still a felony. (Some states have misdemeanor manslaughter, which was not an issue in this case.) In some states, criminally negligent homicide is sometimes referred to as involuntary manslaughter. The mens rea for involuntary manslaughter is generally recklessness or “criminal negligence.” This crime goes by various names depending on the state, but involuntary manslaughter and criminally negligent homicide are common names.
Ordinary negligence versus criminal negligence. Criminal negligence is usually considered a more serious mistake than ordinary negligence. This is where there is a difference between civil malpractice negligence and criminal negligence. Criminal negligence is somewhat more careless than ordinary negligence. To use a driving example, if Dr. A was driving home from the hospital, missed seeing a red light, and killed Joe Pedestrian, it could be ordinary negligence. If, however, Dr. B was texting or drinking while driving, causing Dr. B to be distracted and miss seeing the red light, killing a pedestrian, it could be criminal negligence and result in the conviction for the homicide. Of course, in either case there could be civil liability for causing the death.
Applying these legal principles to the reported facts in Ms. Vaught’s case, it appears there was more than simple negligence. That is, the nurse was more than careless. Using “VE” for the wrong drug might have been negligent. In addition, however, she disengaged a safeguard meant to prevent wrongful use of the drug, failed to notice that the drug was a powder instead of a liquid, and ignored the red cap warning that the drug was a paralyzing agent. It becomes apparent why the jury could have found aggravated or criminal negligence.
It is worth emphasizing that in this case, the criminal charges were unusual. For years, studies have suggested that many deaths result from medical errors. The Institute of Medicine famously said that the number of deaths from medical errors was equivalent to that of a 747 airplane crashing every day.12,13 These events result in a relatively small number of malpractice actions but an infinitesimally small number of homicide charges. Among other things, prosecutors are reluctant to pursue such cases regarding acts carried out as part of clinical duties unless there is strong evidence, and grand juries may be reluctant to indict medical professionals.14
Nonetheless, medical professionals ultimately can be criminally responsible for deaths resulting from intentional, or criminally negligent, careless practice. Such liability should not dissuade nurses or others from medical practice any more than the much more common homicide charges that can occur from driving an automobile carelessly that results in someone’s death. A fundamental purpose of the criminal law is to disincentivize unnecessarily harmful (deadly) conduct, whether it is distracted driving or distracted nursing.
Continue to: The drug-prescribing crimes...
The drug-prescribing crimes
The US Supreme Court considered a much different kind of criminal medical practice in 2 (consolidated) cases in its 2021–2022 Term. Physicians in 2 states were each tried and convicted of federal charges of illegally dispensing or distributing (prescribing) controlled substances.15 A federal statute makes it a felony for a physician, or others, “except as authorized” to “knowingly or intentionally distribute, or dispense a controlled substance.”16 Federal regulations clarify the statute. The regulation provides that a prescription is authorized only if a doctor issues it “for a legitimate medical purpose . . . acting in the usual course of professional practice.”17
CASE 2 Physicians charged with overprescribing controlled substances
In these 2 drug-prescribing cases, the physicians had grossly overprescribed the opioids. One reportedly wrote prescriptions in 2 states in exchange for payments in cash or, infrequently, firearms, approximating the cost of the prescriptions to street drugs. The other had a clinic that, over about 4 years, issued 300,000 prescriptions for controlled substances and was a significant source for some kinds of fentanyl.18
WHAT’S THE VERDICT?
In each trial, the juries found the defendant guilty of improper distribution of controlled substances. Although the charges were not homicides, the sentencing judges were much more severe than the court had been in the nursing case discussed above. One physician received a prison term of 20 years, the other, a 25-year term. These undoubtedly reflect both the outrageous conduct and the likely great harm the defendants did.
The Supreme Court heard the cases
The Supreme Court reversed these physicians’ convictions. The Court held that the lower courts had not correctly described for the juries the mens rea required for a conviction under these charges. The Supreme Court held that to be convicted of these offenses, the government had to prove “beyond a reasonable doubt that the defendant [physician] knew that he or she was acting in an unauthorized manner.”19 Both can be retried and probably will be unless they reach a plea agreement with the federal government. Nonetheless, the Court established a very high standard. Carelessness is not enough, but rather “knowingly” acting in an unauthorized way is required. Although these physicians were prosecuted under federal law, other physicians have been prosecuted under state laws limiting the distribution of controlled substances.20
Some physicians have expressed concern that the Supreme Court, in these cases, made the practice of medicine more dangerous for physicians (the threat of criminal sanctions) and patients (making it more difficult to obtain pain control, for example).21,22 That view may be overly pessimistic for 2 reasons. First, the Court actually made it more difficult to convict physicians of writing excessive prescriptions. It did so by setting a higher mens rea standard than lower courts were using, that is, the physician had to “knowingly” act in an unauthorized way. Because “knowingly” can be implied by the circumstances, taking guns or cash would be evidence that the physician knowingly misprescribed.
More fundamentally, the actions of these physicians appear to be well outside even a generous legitimate level of controlled substance prescription. These convictions should not be misunderstood as a way of federal courts to crack down on pain medications. However, the original convictions are a warning to the small handful who grossly overprescribe controlled substances.
Lessons about criminal law and the practice of medicine
Medical professionals’ strong reaction to criminal charges is understandable. Criminal charges can result in jail time (the physicians involved in the controlled substance case were sentenced to 20 years or more) and hefty fines; bring social and professional disapprobation; may lead to license discipline; and are terribly disruptive even for those found not guilty. To make matters worse, malpractice insurance ordinarily does not cover criminal charges, so any fines and the cost of defense are likely out of pocket for those charged—and that can be very expensive. Therefore, the strong reaction to the cases we have described is understandable.
At the same time, the probability of criminal charges against medical personnel for their medical treatment is very low compared with, for example, fraudulent billing, their driving habits, or tax avoidance. Criminal charges are much more likely to arise from insurance fraud, Medicare or Medicaid dishonesty, kickbacks, false statements, and similar corruption crimes rather than inadequate practice. In the cases we examined here, there is an enhanced or aggravated negligence in one case and grossly inappropriate prescribing in the others (which the Supreme Court held must be “knowingly” wrong).
Finally, there is an irony. Medical professionals worried about practice-related criminal charges should be thankful for the malpractice system. Civil malpractice is, as a practical matter, an alternative for patients who believe they were mistreated or harmed by physicians or other providers. They have the option of finding a private attorney to file a civil complaint. In the absence of that system, they would be much more likely to take their grievance and complaint to the prosecutor to seek answers and retribution. Criminal law and civil liability are each a way of allowing someone harmed by another to seek redress. Both are intended to deter harmful conduct and provide some individual and social retribution for such behavior. The civil system, of course, also provides the potential for compensation to those injured. An injured patient without the possibility of a civil suit sometimes would turn to the criminal system for satisfaction. This way, the malpractice system is a better alternative to criminal charges. ●
Medical professionals are well aware that civil liability (malpractice) may incur when a patient is harmed because of carelessness (negligence). Recent criminal charges against physicians and a nurse, however, have called medical professionals’ attention to the fact that they also may face criminal charges for inappropriate practice.
We cite 2 cases in which criminal liability resulted from bad medical practice. In both instances, there was considerable concern among medical professionals that criminal charges for making a mistake would make it difficult to practice without fear of criminal charges. One concern is that criminal charges could drive good people out of the profession or make them too cautious.1
We look more closely at those 2 cases in which criminal liability was imposed. These cases are outliers. Relatively few criminal cases against medical professionals are based on the quality of care. (There are, however, more criminal charges related to fraudulent billing and other insurance fraud, kickbacks, Medicare and Medicaid abuse, and the like.2) At the same time, the criminal law does not stop at the front door of a clinic or hospital.3 When medical professionals engage in seriously inappropriate health care conduct that directly harms someone, criminal liability may result.4
Anatomy of a crime
Crimes generally require a specific mental state (mens rea) and an act (actus reus). The law specifies the mental state required for conviction. It can range from premeditation—once commonly called “malice aforethought”—to negligence. The mens rea requirement is an essential element of the crime—as we will see in the discussion of the prescription drug cases. A few offenses do not require even negligence, but overwhelmingly, crimes require something more than simple negligence.5
The act requirement is generally obvious, such as firing a gun, driving while intoxicated, or recklessly giving inappropriate medication to a patient. It may include “attempts,” crimes where an act was not completed. For example, attempted murder or conspiracy to commit do not require a completed offense, only intent plus overt acts toward carrying out the crime. Similarly, the wrongful act usually has to produce some harm, but again there are exceptions (attempts). To obtain a conviction, the prosecution must prove all of the elements of the crime, including the required mens rea, beyond a reasonable doubt.6
With this general background, we turn to the first case, in which the charge was a form of homicide. Please note that the following case description was derived from news descriptions of the case, because juries do not publish opinions concerning their conclusions and court documents are unavailable. The public reports therefore may contain factual gaps and errors.
CASE 1 Patient dies after nurse administers wrong drug
RaDonda Vaught, a 38-year-old experienced registered nurse employed at Vanderbilt University Medical Center (VUMC) in the intensive care unit (ICU), was providing care for a 76-year-old patient who was admitted to VUMC’s ICU in December 2017 in association with a brain injury. The brain injury involved a fall with resultant subdural hematoma. In preparation for a positron emission tomography (PET) scan to assess the patient’s injury, the physician team prescribed the sedative Versed (midazolam) because of the patient’s claustrophobia. During the course of treatment, Ms. Vaught inadvertently administered the wrong drug, a fatal dose of the muscle relaxant vecuronium, to the patient, which resulted in the patient being unable to breathe. Apparently, Ms. Vaught had been unable to find the midazolam and disengaged a safeguard, proceeding into override mode, and thus vecuronium was dispensed. By the time the error was noticed, the patient was already in cardiac arrest with resultant brain damage (partial brain death). The patient died soon thereafter.
How this medication error occurred
The medication error occurred when Ms. Vaught overrode a computer in the medical system when she could not find the “Versed” entry and typed in “VE,” which was the abbreviation for vecuronium. The prosecutors in the case stated that she failed to distinguish that vecuronium is dispensed as a powder and Versed as a liquid formula. The vecuronium has a red cap, which warns that it is a paralyzing agent. Ms. Vaught ignored these red flags, according to the prosecutors. Furthermore, the lawsuit filing documented her discussion that she was “distracted with something” at the time and admitted to overriding the medication warning.
Continue to: The charges in this case...
The charges in this case
The charges revolved around “criminally negligent homicide and gross neglect of an impaired adult,” the most notable charge being criminally negligent homicide. Potential consequences were up to an 8 years’ prison sentence.7
Furthermore, the Tennessee Board of Nursing revoked Ms. Vaught’s license in July 2021.8 The Board also reportedly fined her $3,000.9
The criminal proceedings were filed in Davidson County Criminal Court, with Judge Jennifer Smith presiding. Ms. Vaught repeatedly manifested remorse for the event. The patient’s family, including her son Michael and her daughters-in-law, provided tearful testimonies at the hearing. Ms. Vaught repeatedly cried during the testimonies. The nurse did not provide an apology, according to one daughter-in-law. The news media reported that the family did not want jail time for Ms. Vaught.7 Nurses across the country were “jolted,” as expressed by the news media.10
Why the controversy?
The entire issue of medical errors continues to be discussed among both the medical and the legal professions. To have a nursing personnel held to the level of criminal liability is unusual.
It was clear that Ms. Vaught took responsibility for her actions, and neither the prosecutors nor defendant attorneys sensed any evidence of malice on her part. On the other hand, there was enough evidence and concern for District Attorney Glenn Funk to proceed with prosecution-related action. Ms. Vaught was facing years in prison if convicted.
WHAT’S THE VERDICT?
In March 2022, the jury convicted Ms. Vaught of criminally negligent homicide—but not of reckless homicide, a more serious offense.
Judge Smith granted a judicial diversion, that is, the conviction would be expunged from the record if Ms. Vaught completed a 3-year probation. Judge Smith noted the “credible remorse expressed by Nurse Vaught” and went on to state, “this is a terrible, terrible, mistake and there have been consequences to the defendant.” In the courtroom, Ms. Vaught apologized to the patient’s family and conveyed that she will “forever be haunted by her role in the (patient’s) passing.”
Overall, this served as an opportunity for health care workers to address oftentimes poor working conditions, which have been exacerbated by the COVID-19 pandemic.
The Davidson County District Attorney’s office conveyed that this was one case of a careless nurse and not a reflection of the nursing profession. The prosecutors were in accord with a probation verdict. The family felt that their mother, the patient, would not want to see the nurse serve a jail sentence: “Mom was a very forgiving person.”
The patient’s cause of death was listed as “intracerebral hemorrhage and cardiac arrest.” One year later, a new death certificate was issued and noted vecuronium intoxication as the cause of death.
Continue to: The health care institution’s involvement...
The health care institution’s involvement
Approximately 1 year after an apparent anonymous tip was made to health care officials, an unscheduled state and federal investigation, with the threat of possible sanctions, occurred at the VUMC. This was predicated on the criminal indictment related to Ms. Vaught. In the end, her nursing license was revoked, as noted earlier. The family earlier reached an out-of-court settlement with the hospital and there were a number of problems identified at the university medical center.11
Legal principles in the case
Most criminal cases are state cases. Crimes are defined in state statutes, and the trial takes place in state courts. Thus, crimes are defined a little differently from state to state. Ms. Vaught, for example, was tried in Tennessee under the laws of that state.
Homicide involves the killing of a human being. It may not be a crime. For example, there is “justifiable homicide,” such as self-defense. At the other extreme is first-degree murder, an intentional and planned killing. In this case, Ms. Vaught was charged with criminally negligent homicide, which is usually the least serious of criminal homicides but is still a felony. (Some states have misdemeanor manslaughter, which was not an issue in this case.) In some states, criminally negligent homicide is sometimes referred to as involuntary manslaughter. The mens rea for involuntary manslaughter is generally recklessness or “criminal negligence.” This crime goes by various names depending on the state, but involuntary manslaughter and criminally negligent homicide are common names.
Ordinary negligence versus criminal negligence. Criminal negligence is usually considered a more serious mistake than ordinary negligence. This is where there is a difference between civil malpractice negligence and criminal negligence. Criminal negligence is somewhat more careless than ordinary negligence. To use a driving example, if Dr. A was driving home from the hospital, missed seeing a red light, and killed Joe Pedestrian, it could be ordinary negligence. If, however, Dr. B was texting or drinking while driving, causing Dr. B to be distracted and miss seeing the red light, killing a pedestrian, it could be criminal negligence and result in the conviction for the homicide. Of course, in either case there could be civil liability for causing the death.
Applying these legal principles to the reported facts in Ms. Vaught’s case, it appears there was more than simple negligence. That is, the nurse was more than careless. Using “VE” for the wrong drug might have been negligent. In addition, however, she disengaged a safeguard meant to prevent wrongful use of the drug, failed to notice that the drug was a powder instead of a liquid, and ignored the red cap warning that the drug was a paralyzing agent. It becomes apparent why the jury could have found aggravated or criminal negligence.
It is worth emphasizing that in this case, the criminal charges were unusual. For years, studies have suggested that many deaths result from medical errors. The Institute of Medicine famously said that the number of deaths from medical errors was equivalent to that of a 747 airplane crashing every day.12,13 These events result in a relatively small number of malpractice actions but an infinitesimally small number of homicide charges. Among other things, prosecutors are reluctant to pursue such cases regarding acts carried out as part of clinical duties unless there is strong evidence, and grand juries may be reluctant to indict medical professionals.14
Nonetheless, medical professionals ultimately can be criminally responsible for deaths resulting from intentional, or criminally negligent, careless practice. Such liability should not dissuade nurses or others from medical practice any more than the much more common homicide charges that can occur from driving an automobile carelessly that results in someone’s death. A fundamental purpose of the criminal law is to disincentivize unnecessarily harmful (deadly) conduct, whether it is distracted driving or distracted nursing.
Continue to: The drug-prescribing crimes...
The drug-prescribing crimes
The US Supreme Court considered a much different kind of criminal medical practice in 2 (consolidated) cases in its 2021–2022 Term. Physicians in 2 states were each tried and convicted of federal charges of illegally dispensing or distributing (prescribing) controlled substances.15 A federal statute makes it a felony for a physician, or others, “except as authorized” to “knowingly or intentionally distribute, or dispense a controlled substance.”16 Federal regulations clarify the statute. The regulation provides that a prescription is authorized only if a doctor issues it “for a legitimate medical purpose . . . acting in the usual course of professional practice.”17
CASE 2 Physicians charged with overprescribing controlled substances
In these 2 drug-prescribing cases, the physicians had grossly overprescribed the opioids. One reportedly wrote prescriptions in 2 states in exchange for payments in cash or, infrequently, firearms, approximating the cost of the prescriptions to street drugs. The other had a clinic that, over about 4 years, issued 300,000 prescriptions for controlled substances and was a significant source for some kinds of fentanyl.18
WHAT’S THE VERDICT?
In each trial, the juries found the defendant guilty of improper distribution of controlled substances. Although the charges were not homicides, the sentencing judges were much more severe than the court had been in the nursing case discussed above. One physician received a prison term of 20 years, the other, a 25-year term. These undoubtedly reflect both the outrageous conduct and the likely great harm the defendants did.
The Supreme Court heard the cases
The Supreme Court reversed these physicians’ convictions. The Court held that the lower courts had not correctly described for the juries the mens rea required for a conviction under these charges. The Supreme Court held that to be convicted of these offenses, the government had to prove “beyond a reasonable doubt that the defendant [physician] knew that he or she was acting in an unauthorized manner.”19 Both can be retried and probably will be unless they reach a plea agreement with the federal government. Nonetheless, the Court established a very high standard. Carelessness is not enough, but rather “knowingly” acting in an unauthorized way is required. Although these physicians were prosecuted under federal law, other physicians have been prosecuted under state laws limiting the distribution of controlled substances.20
Some physicians have expressed concern that the Supreme Court, in these cases, made the practice of medicine more dangerous for physicians (the threat of criminal sanctions) and patients (making it more difficult to obtain pain control, for example).21,22 That view may be overly pessimistic for 2 reasons. First, the Court actually made it more difficult to convict physicians of writing excessive prescriptions. It did so by setting a higher mens rea standard than lower courts were using, that is, the physician had to “knowingly” act in an unauthorized way. Because “knowingly” can be implied by the circumstances, taking guns or cash would be evidence that the physician knowingly misprescribed.
More fundamentally, the actions of these physicians appear to be well outside even a generous legitimate level of controlled substance prescription. These convictions should not be misunderstood as a way of federal courts to crack down on pain medications. However, the original convictions are a warning to the small handful who grossly overprescribe controlled substances.
Lessons about criminal law and the practice of medicine
Medical professionals’ strong reaction to criminal charges is understandable. Criminal charges can result in jail time (the physicians involved in the controlled substance case were sentenced to 20 years or more) and hefty fines; bring social and professional disapprobation; may lead to license discipline; and are terribly disruptive even for those found not guilty. To make matters worse, malpractice insurance ordinarily does not cover criminal charges, so any fines and the cost of defense are likely out of pocket for those charged—and that can be very expensive. Therefore, the strong reaction to the cases we have described is understandable.
At the same time, the probability of criminal charges against medical personnel for their medical treatment is very low compared with, for example, fraudulent billing, their driving habits, or tax avoidance. Criminal charges are much more likely to arise from insurance fraud, Medicare or Medicaid dishonesty, kickbacks, false statements, and similar corruption crimes rather than inadequate practice. In the cases we examined here, there is an enhanced or aggravated negligence in one case and grossly inappropriate prescribing in the others (which the Supreme Court held must be “knowingly” wrong).
Finally, there is an irony. Medical professionals worried about practice-related criminal charges should be thankful for the malpractice system. Civil malpractice is, as a practical matter, an alternative for patients who believe they were mistreated or harmed by physicians or other providers. They have the option of finding a private attorney to file a civil complaint. In the absence of that system, they would be much more likely to take their grievance and complaint to the prosecutor to seek answers and retribution. Criminal law and civil liability are each a way of allowing someone harmed by another to seek redress. Both are intended to deter harmful conduct and provide some individual and social retribution for such behavior. The civil system, of course, also provides the potential for compensation to those injured. An injured patient without the possibility of a civil suit sometimes would turn to the criminal system for satisfaction. This way, the malpractice system is a better alternative to criminal charges. ●
- Kelman B. As a nurse faces prison for a deadly error, her colleagues worry: could I be next? NPR. March 22, 2022. Accessed November 7, 2022. https://www.npr.org/sections/health-shots/2022/03/22/1087903348/as-a-nurse-faces-prison-for-a-deadly-error-her-colleagues-worry-could-i-be-next
- US Department of Justice. National health care fraud enforcement action results in charges involving over $1.4 billion in alleged losses. September 17, 2021. Accessed November 7, 2022. https://www.justice.gov/opa/pr/national-health-care-fraud-enforcement-action-results-charges-involving-over-14-billion
- Steinman G. Stuff of nightmares: criminal prosecution for malpractice. OBG Manag. 2008;20(8):35-45.
- Maher V, Cwiek M. Criminal liability for nursing and medical harm. Hosp Top. 2022 July 13;1-8.
- Singer RG. The resurgence of mens rea: III—the rise and fall of strict criminal liability. Boston Coll Law Rev. 1989;30:337-408. Accessed November 7, 2022. https://lawdigitalcommons.bc.edu/cgi/viewcontent.cgi?article=2431&context=bclr
- Sarch AF. Knowledge, recklessness and the connection requirement between actus reus and mens rea. Penn State Law Rev. 2015;120:1-51. Accessed November 7, 2022. https://ideas.dickinsonlaw.psu.edu/cgi/viewcontent.cgi?article=4120&context=dlra
- Timms M, Gluck F, Wegner R, et al. RaDonda Vaught sentenced to three years probation on a diverted sentence, could see record wiped. Tennessean. May 13, 2022. Accessed November 7, 2022. http://www.tennessean.com/story/news/crime/2022/05/13/radonda-vaught-sentened-vanderbilt-nurse/9717529002/
- Tennessee Board of Nursing. Disciplinary hearing: RaDonda Vaught, RN #205702, minutes. July 22-23, 2021. Accessed November 7, 2022. https://www.tn.gov/content/dam/tn/health/healthprofboards/nursing/meeting-minutes/Nursing%20Meeting%20Minutes%20July%2022-23,%202021.pdf
- Institute for Safe Medication Practices. TN Board of Nursing’s unjust decision to revoke nurse’s license: travesty on top of tragedy! August 12, 2021. Accessed November 7, 2022. https://www.ismp.org/resources/tn-board-nursings-unjust-decision-revoke-nurses-license-travesty-top-tragedy
- Medina E. Ex-nurse convicted in fatal medication error gets probation. New York Times. May 15, 2022. Accessed November 7, 2022. https://www.nytimes.com/2022/05/15/us/tennessee-nurse-sentencing.html
- Kelman B. In nurse’s trial, investigator says hospital bears ‘heavy’ responsibility for patient death. KHN. March 24, 2022. Accessed November 15, 2022. https://khn.org/news/article/radonda-vaught-fatal-drug-error-vanderbilt-hospital-responsibility/
- Institute of Medicine (US) Committee on Quality of Health Care in America; Kohn LT, Corrigan JM, Donaldson MS, ed. To Err Is Human: Building a Safer Health System. National Academies Press; 2000.
- Bates DW, Singh H. Two decades since To Err Is Human: an assessment of progress and emerging priorities in patient safety. Health Affairs. 2018;37:1736-1743.
- Eisenberg RL, Berlin L. When does malpractice become manslaughter? Am J Roentgenol. 2002;179:331-335.
- Xiulu Ruan v United States, 20-1410, decided June 27, 2022. https://www.supremecourt.gov/opinions/21pdf/20 -1410_1an2.pdf
- 84 Stat. 1260, 21 U. S. C. §841(a).
- 21 CFR §1306.04(a) (2021).
- Liptak A. Supreme Court sides with doctors accused of running pill mills. The New York Times. June 27, 2022.
- Xiulu Ruan v United States, at 2 (slip opinion).
- Pedemonte S. State v. Christensen: criminalizing medical malpractice. Montana Law Rev. 2022;83(1):183-193. Accessed November 7, 2022. https://scholarworks.umt.edu/cgi/view content.cgi?article=2497&context=mlr
- Szalavitz M. A recent Supreme Court ruling will help people in pain. Scientific American. September 19, 2022. Accessed November 15, 2022. https://www.scientificamerican.com/ article/a-recent-supreme-court-ruling-will-help-people-in -pain/
- Lopez I. Opioid pill peddling case threatens future of pain treatment. Bloomberg Law. March 29, 2022. Accessed November 15, 2022. https://news.bloomberglaw.com/health -law-and-business/opioid-pill-peddling-case-threatens -future-of-pain-treatment
- Kelman B. As a nurse faces prison for a deadly error, her colleagues worry: could I be next? NPR. March 22, 2022. Accessed November 7, 2022. https://www.npr.org/sections/health-shots/2022/03/22/1087903348/as-a-nurse-faces-prison-for-a-deadly-error-her-colleagues-worry-could-i-be-next
- US Department of Justice. National health care fraud enforcement action results in charges involving over $1.4 billion in alleged losses. September 17, 2021. Accessed November 7, 2022. https://www.justice.gov/opa/pr/national-health-care-fraud-enforcement-action-results-charges-involving-over-14-billion
- Steinman G. Stuff of nightmares: criminal prosecution for malpractice. OBG Manag. 2008;20(8):35-45.
- Maher V, Cwiek M. Criminal liability for nursing and medical harm. Hosp Top. 2022 July 13;1-8.
- Singer RG. The resurgence of mens rea: III—the rise and fall of strict criminal liability. Boston Coll Law Rev. 1989;30:337-408. Accessed November 7, 2022. https://lawdigitalcommons.bc.edu/cgi/viewcontent.cgi?article=2431&context=bclr
- Sarch AF. Knowledge, recklessness and the connection requirement between actus reus and mens rea. Penn State Law Rev. 2015;120:1-51. Accessed November 7, 2022. https://ideas.dickinsonlaw.psu.edu/cgi/viewcontent.cgi?article=4120&context=dlra
- Timms M, Gluck F, Wegner R, et al. RaDonda Vaught sentenced to three years probation on a diverted sentence, could see record wiped. Tennessean. May 13, 2022. Accessed November 7, 2022. http://www.tennessean.com/story/news/crime/2022/05/13/radonda-vaught-sentened-vanderbilt-nurse/9717529002/
- Tennessee Board of Nursing. Disciplinary hearing: RaDonda Vaught, RN #205702, minutes. July 22-23, 2021. Accessed November 7, 2022. https://www.tn.gov/content/dam/tn/health/healthprofboards/nursing/meeting-minutes/Nursing%20Meeting%20Minutes%20July%2022-23,%202021.pdf
- Institute for Safe Medication Practices. TN Board of Nursing’s unjust decision to revoke nurse’s license: travesty on top of tragedy! August 12, 2021. Accessed November 7, 2022. https://www.ismp.org/resources/tn-board-nursings-unjust-decision-revoke-nurses-license-travesty-top-tragedy
- Medina E. Ex-nurse convicted in fatal medication error gets probation. New York Times. May 15, 2022. Accessed November 7, 2022. https://www.nytimes.com/2022/05/15/us/tennessee-nurse-sentencing.html
- Kelman B. In nurse’s trial, investigator says hospital bears ‘heavy’ responsibility for patient death. KHN. March 24, 2022. Accessed November 15, 2022. https://khn.org/news/article/radonda-vaught-fatal-drug-error-vanderbilt-hospital-responsibility/
- Institute of Medicine (US) Committee on Quality of Health Care in America; Kohn LT, Corrigan JM, Donaldson MS, ed. To Err Is Human: Building a Safer Health System. National Academies Press; 2000.
- Bates DW, Singh H. Two decades since To Err Is Human: an assessment of progress and emerging priorities in patient safety. Health Affairs. 2018;37:1736-1743.
- Eisenberg RL, Berlin L. When does malpractice become manslaughter? Am J Roentgenol. 2002;179:331-335.
- Xiulu Ruan v United States, 20-1410, decided June 27, 2022. https://www.supremecourt.gov/opinions/21pdf/20 -1410_1an2.pdf
- 84 Stat. 1260, 21 U. S. C. §841(a).
- 21 CFR §1306.04(a) (2021).
- Liptak A. Supreme Court sides with doctors accused of running pill mills. The New York Times. June 27, 2022.
- Xiulu Ruan v United States, at 2 (slip opinion).
- Pedemonte S. State v. Christensen: criminalizing medical malpractice. Montana Law Rev. 2022;83(1):183-193. Accessed November 7, 2022. https://scholarworks.umt.edu/cgi/view content.cgi?article=2497&context=mlr
- Szalavitz M. A recent Supreme Court ruling will help people in pain. Scientific American. September 19, 2022. Accessed November 15, 2022. https://www.scientificamerican.com/ article/a-recent-supreme-court-ruling-will-help-people-in -pain/
- Lopez I. Opioid pill peddling case threatens future of pain treatment. Bloomberg Law. March 29, 2022. Accessed November 15, 2022. https://news.bloomberglaw.com/health -law-and-business/opioid-pill-peddling-case-threatens -future-of-pain-treatment
Disjointed states of America: The medical is political

Like many of you, I am an obstetrician-gynecologist who provides full-spectrum reproductive health care. Our jobs demand great intimacy—we are with patients as they meet their first born, learn of a miscarriage diagnosis, or decide to end their pregnancy. I have performed an uncomplicated, joyful vaginal delivery, then within an hour rushed a different patient’s gurney to the intensive care unit as she became acutely hypotensive and hypoxic, developing ARDS after a stillbirth. The care we provide is uniquely personal, and in that, has become deeply political. We have spent a long time here—news pundits, members of our family, even us—viewing abortion and reproductive health as something innately political. Although abortion is at the forefront of legislative interference and politicization, more than 1,300 abortion restrictions have been passed in the United States since Roe v Wade in 1973. It is not the only medical care affected by political interference.1 The United States ranks last in maternal mortality among industrialized nations, and Black women are more than twice as likely to die.2 As we grapple with the fallout of the Dobbs v Jackson Women’s Health Organization opinion and begin to recognize how fractured medical care has become—based on zip code—we should take stock of the way legislation and politics have already dictated reproductive health care. Abortion is the salient example, but state policy and legislation have unjustly been determining medical care available to women and other patients on a broader scale for decades. Here are just a few examples.
Postpartum care
The postpartum period is critical for maternal health; it is the time period in which many comorbidities emerge, including hypertensive disorders, postpartum thyroiditis, and mood disorders. Fifty percent of maternal deaths in the United States occur postpartum. Despite the importance of this care, Medicaid coverage for longer than 60 days postpartum varies greatly state to state. After the Affordable Care Act was implemented, it was assumed that all states would expand their Medicaid programs to include parents in their coverage plans beyond the guaranteed 60 days, negating the need for a specific postpartum coverage time period. However, the 2012 Supreme Court decision in National Federation of Independent Business v Sebelius allowed states to opt out of Medicaid expansion.3 In many states, postpartum patients lose their Medicaid insurance after 60 days if they do not meet the stringent income criteria.
The income level that makes patients ineligible for Medicaid coverage at day 61 postpartum varies widely. In Maryland, a patient can extend their Medicaid coverage for 12 months postpartum if their family of 4 earns less than $73,260 annually (264% of the federal poverty level). However, in Mississippi, an income of more than $6,936 per year for a family of 4 (approximately 25% of the federal poverty level) renders mothers who are 61 days postpartum ineligible for Medicaid coverage.4 Thus, many low-income postpartum patients (who are at twice the risk of maternal mortality as affluent patients) find themselves without access to this critical care depending on the decisions of their state legislatures.5 The American Rescue Plan Act of 2021 (known as the COVID-19 Stimulus Package) included a provision that allows states to expand their postpartum Medicaid coverage from 60 days to 12 months; currently, 10 additional states are planning to expand postpartum Medicaid for 12 months. While encouraging, 14 states still have not announced plans to utilize this provision or apply for a waiver to extend Medicaid coverage in the postpartum period.6
Treatment for substance use
Drug overdose is a leading cause of pregnancy-related death from unintentional causes.7 Overdose deaths in the general population climbed between 2020 and 2021, reaching historic highs of more than 100,000 deaths in a 12-month period.8 Given the impact of substance use and overdose on maternal mortality, health systems should be maximizing efforts to respond to this public health crisis by implementing effective screening and treatment interventions and establishing clinics and hospitals as safe places to seek care. However, many states have criminalized substance use in pregnant patients and mandate that clinicians report patients who use substances, creating an ethical dilemma for clinicians seeking to screen and treat patients for substance use disorder. Twenty-three states consider substance use in pregnancy to be child abuse, and 3 states consider substance use in pregnancy to be grounds for civil commitment. In Wisconsin, a patient can be detained against their will for the duration of the pregnancy. Twenty-five states require health care professionals to report suspected substance abuse in pregnancy to child protective services or a similar state office.9 Even when universal substance use screening is implemented, it has disparate impact on patients of color; Black women who screened positive for substance use in pregnancy were more likely to be reported to child protective services than their White counterparts.10 The criminalization of pregnant bodies does not lead to improvements in individual, community, or public health, it infringes on the ethical principle of bodily autonomy and puts clinicians at odds with what is best for their patients.
Gender-affirming care
Gender-affirming care is supported by major medical organizations and reduces the risk of depression and suicidality in transgender youth.11 Despite this evidence, several states have passed legislation restricting or banning this care, criminalizing the doctors who provide it. Idaho’s house of representatives passed House Bill 675,12 which would make providing gender-affirming care a felony, punishable by up to a life sentence. This would extend to parents trying to access care for their children as well as clinicians.
Although abortion is the medical care most conspicuously manipulated by politics and legislation, it is far from the only example. No area of medicine will be untouched by eliminating access to reproductive health care and by the regulation and criminalization of health care workers who provide it. This is a sea change, although state legislative interference and disparities in reproductive health care have been a tocsin of such change for years. We can no longer afford to believe there is a separation between politics and medicine; this directly interferes with our Hippocratic oath to do no harm. A politician in Ohio should not decide whether or not a 13-year-old patient should have to carry a pregnancy to term; the house of representatives in Idaho should not put someone’s transgender child at increased risk of depression and suicidality by making their medical care a felony. Colleagues in Texas should not be punishable by life in prison for providing abortion care.13 As a physician, I cannot stand by when, facing a maternal mortality crisis, state politicians decide whether a patient living below the poverty line should have access to postpartum care.
I am neither a politician nor a legal scholar. I am a physician who takes care of people in this intimate and powerful space of healing and support between doctor and patient. What should we do? We need to come together to find the answers. We need to vote if we haven’t before. And we need to vote differently if we have elected lawmakers who politicize and dangerously interfere with medicine, the well-being of our patients, and our ability to carry out our duty as physicians in our patients’ best interests. We need to tell our stories—to each other, to our newspapers, to our neighbors, and to our legislatures. If we are leading organizations, we can use the power held in our institutions to commit to providing care to the fullest extent possible, commit to protecting our clinicians providing evidence-based care, and encourage legislators who use medicine as a political bargaining chip to reverse course. Medicine is not an apolitical field, and we can no longer uphold that paradigm. Our patients lives, and our livelihood as healers and caretakers, depends on our collective action against it. ●
Acknowledgement
The author would like to thank Lauren Sobel, DO, MPH, for her contributions to a presentation on this subject.
- Nash E, Ephross P. State policy trends at midyear 2022: with Roe about to be overturned, some states double down on abortion restrictions. Guttmacher Institute. June 22, 2022. https://live. guttmacher.org/article/2022/06/state-policy -trends-midyear-2022-roe-about-be-overturnedsome-states-double-down. Accessed September 12, 2022.
- Declercq E, Zephyrin L. Maternal mortality in the United States: a primer. Commonwealth Fund; 2020. https://www.commonwealthfund .org/publications/issue-brief-report/2020 /dec/maternal-mortality-united-states-primer. Accessed September 12, 2022.
- Santa Clara Law Digital Communications website. Supreme Court of the United States. National Federation of Independent Business v Sebelius. (2012). Patient Protection and Affordable Care Act Litigation. 333. https://digitalcommons.law.scu.edu /aca/333. Accessed September 13, 2022.
- Ranji U, Salganicoff A, Gomez I. Postpartum coverage extension in the American Rescue Plan Act of 2021. San Francisco, CA: Kaiser Family Foundation; 2021.
- Singh GK, Lee H. Trends and racial/ethnic, socioeconomic, and geographic disparities in maternal mortality from indirect obstetric causes in the United States, 1999-2017. Int J MCH AIDS. 2021;10:43.
- Kaiser Family Foundation. Medicaid Postpartum Coverage Extension Tracker. https://www.kff. org/medicaid/issue-brief/medicaid-postpartum -coverage-extension-tracker/. Accessed September 7, 2022.
- Mehta PK, Bachhuber MA, Hoffman R, et al. Deaths from unintentional injury, homicide, and suicide during or within 1 year of pregnancy in Philadelphia. Am J Public Health. 2016;106: 2208-2210.
- O’Donnell J, Tanz LJ, Gladden RM, et al. Trends in and characteristics of drug overdose deaths involving illicitly manufactured fentanyls— United States, 2019–2020. MMWR Morb Mortal Wkly Rep. 2021;70:1740.
- State laws and policies: substance use during pregnancy. Guttmacher Institute. https://www .guttmacher.org/state-policy/explore/substance -use-during-pregnancy. August 1, 2022. Accessed September 13, 2022.
- Roberts S, Nuru-Jeter A. Universal screening for alcohol and drug use and racial disparities in child protective services reporting. J Behav Health Serv Res. 2012;39;3-16.
- Tordoff DM, Wanta JW, Collin, et al. (2022). Mental health outcomes in transgender and nonbinary youths receiving gender-affirming care. JAMA Network Open. 2022;5:e220978. doi: 10.1001/jamanetworkopen.2022.0978.
- House Bill 675. Idaho Legislature web site. https:// legislature.idaho.gov/sessioninfo/2022/legislation/h0675/. Accessed September 9, 2022.
- Simon S. New Texas trigger law makes abortion a felony. NPR. August 27, 2022. https://www.npr. org/2022/08/27/1119795665/new-texas-trigger -law-makes-abortion-a-felony. Accessed September 13, 2022.

Like many of you, I am an obstetrician-gynecologist who provides full-spectrum reproductive health care. Our jobs demand great intimacy—we are with patients as they meet their first born, learn of a miscarriage diagnosis, or decide to end their pregnancy. I have performed an uncomplicated, joyful vaginal delivery, then within an hour rushed a different patient’s gurney to the intensive care unit as she became acutely hypotensive and hypoxic, developing ARDS after a stillbirth. The care we provide is uniquely personal, and in that, has become deeply political. We have spent a long time here—news pundits, members of our family, even us—viewing abortion and reproductive health as something innately political. Although abortion is at the forefront of legislative interference and politicization, more than 1,300 abortion restrictions have been passed in the United States since Roe v Wade in 1973. It is not the only medical care affected by political interference.1 The United States ranks last in maternal mortality among industrialized nations, and Black women are more than twice as likely to die.2 As we grapple with the fallout of the Dobbs v Jackson Women’s Health Organization opinion and begin to recognize how fractured medical care has become—based on zip code—we should take stock of the way legislation and politics have already dictated reproductive health care. Abortion is the salient example, but state policy and legislation have unjustly been determining medical care available to women and other patients on a broader scale for decades. Here are just a few examples.
Postpartum care
The postpartum period is critical for maternal health; it is the time period in which many comorbidities emerge, including hypertensive disorders, postpartum thyroiditis, and mood disorders. Fifty percent of maternal deaths in the United States occur postpartum. Despite the importance of this care, Medicaid coverage for longer than 60 days postpartum varies greatly state to state. After the Affordable Care Act was implemented, it was assumed that all states would expand their Medicaid programs to include parents in their coverage plans beyond the guaranteed 60 days, negating the need for a specific postpartum coverage time period. However, the 2012 Supreme Court decision in National Federation of Independent Business v Sebelius allowed states to opt out of Medicaid expansion.3 In many states, postpartum patients lose their Medicaid insurance after 60 days if they do not meet the stringent income criteria.
The income level that makes patients ineligible for Medicaid coverage at day 61 postpartum varies widely. In Maryland, a patient can extend their Medicaid coverage for 12 months postpartum if their family of 4 earns less than $73,260 annually (264% of the federal poverty level). However, in Mississippi, an income of more than $6,936 per year for a family of 4 (approximately 25% of the federal poverty level) renders mothers who are 61 days postpartum ineligible for Medicaid coverage.4 Thus, many low-income postpartum patients (who are at twice the risk of maternal mortality as affluent patients) find themselves without access to this critical care depending on the decisions of their state legislatures.5 The American Rescue Plan Act of 2021 (known as the COVID-19 Stimulus Package) included a provision that allows states to expand their postpartum Medicaid coverage from 60 days to 12 months; currently, 10 additional states are planning to expand postpartum Medicaid for 12 months. While encouraging, 14 states still have not announced plans to utilize this provision or apply for a waiver to extend Medicaid coverage in the postpartum period.6
Treatment for substance use
Drug overdose is a leading cause of pregnancy-related death from unintentional causes.7 Overdose deaths in the general population climbed between 2020 and 2021, reaching historic highs of more than 100,000 deaths in a 12-month period.8 Given the impact of substance use and overdose on maternal mortality, health systems should be maximizing efforts to respond to this public health crisis by implementing effective screening and treatment interventions and establishing clinics and hospitals as safe places to seek care. However, many states have criminalized substance use in pregnant patients and mandate that clinicians report patients who use substances, creating an ethical dilemma for clinicians seeking to screen and treat patients for substance use disorder. Twenty-three states consider substance use in pregnancy to be child abuse, and 3 states consider substance use in pregnancy to be grounds for civil commitment. In Wisconsin, a patient can be detained against their will for the duration of the pregnancy. Twenty-five states require health care professionals to report suspected substance abuse in pregnancy to child protective services or a similar state office.9 Even when universal substance use screening is implemented, it has disparate impact on patients of color; Black women who screened positive for substance use in pregnancy were more likely to be reported to child protective services than their White counterparts.10 The criminalization of pregnant bodies does not lead to improvements in individual, community, or public health, it infringes on the ethical principle of bodily autonomy and puts clinicians at odds with what is best for their patients.
Gender-affirming care
Gender-affirming care is supported by major medical organizations and reduces the risk of depression and suicidality in transgender youth.11 Despite this evidence, several states have passed legislation restricting or banning this care, criminalizing the doctors who provide it. Idaho’s house of representatives passed House Bill 675,12 which would make providing gender-affirming care a felony, punishable by up to a life sentence. This would extend to parents trying to access care for their children as well as clinicians.
Although abortion is the medical care most conspicuously manipulated by politics and legislation, it is far from the only example. No area of medicine will be untouched by eliminating access to reproductive health care and by the regulation and criminalization of health care workers who provide it. This is a sea change, although state legislative interference and disparities in reproductive health care have been a tocsin of such change for years. We can no longer afford to believe there is a separation between politics and medicine; this directly interferes with our Hippocratic oath to do no harm. A politician in Ohio should not decide whether or not a 13-year-old patient should have to carry a pregnancy to term; the house of representatives in Idaho should not put someone’s transgender child at increased risk of depression and suicidality by making their medical care a felony. Colleagues in Texas should not be punishable by life in prison for providing abortion care.13 As a physician, I cannot stand by when, facing a maternal mortality crisis, state politicians decide whether a patient living below the poverty line should have access to postpartum care.
I am neither a politician nor a legal scholar. I am a physician who takes care of people in this intimate and powerful space of healing and support between doctor and patient. What should we do? We need to come together to find the answers. We need to vote if we haven’t before. And we need to vote differently if we have elected lawmakers who politicize and dangerously interfere with medicine, the well-being of our patients, and our ability to carry out our duty as physicians in our patients’ best interests. We need to tell our stories—to each other, to our newspapers, to our neighbors, and to our legislatures. If we are leading organizations, we can use the power held in our institutions to commit to providing care to the fullest extent possible, commit to protecting our clinicians providing evidence-based care, and encourage legislators who use medicine as a political bargaining chip to reverse course. Medicine is not an apolitical field, and we can no longer uphold that paradigm. Our patients lives, and our livelihood as healers and caretakers, depends on our collective action against it. ●
Acknowledgement
The author would like to thank Lauren Sobel, DO, MPH, for her contributions to a presentation on this subject.

Like many of you, I am an obstetrician-gynecologist who provides full-spectrum reproductive health care. Our jobs demand great intimacy—we are with patients as they meet their first born, learn of a miscarriage diagnosis, or decide to end their pregnancy. I have performed an uncomplicated, joyful vaginal delivery, then within an hour rushed a different patient’s gurney to the intensive care unit as she became acutely hypotensive and hypoxic, developing ARDS after a stillbirth. The care we provide is uniquely personal, and in that, has become deeply political. We have spent a long time here—news pundits, members of our family, even us—viewing abortion and reproductive health as something innately political. Although abortion is at the forefront of legislative interference and politicization, more than 1,300 abortion restrictions have been passed in the United States since Roe v Wade in 1973. It is not the only medical care affected by political interference.1 The United States ranks last in maternal mortality among industrialized nations, and Black women are more than twice as likely to die.2 As we grapple with the fallout of the Dobbs v Jackson Women’s Health Organization opinion and begin to recognize how fractured medical care has become—based on zip code—we should take stock of the way legislation and politics have already dictated reproductive health care. Abortion is the salient example, but state policy and legislation have unjustly been determining medical care available to women and other patients on a broader scale for decades. Here are just a few examples.
Postpartum care
The postpartum period is critical for maternal health; it is the time period in which many comorbidities emerge, including hypertensive disorders, postpartum thyroiditis, and mood disorders. Fifty percent of maternal deaths in the United States occur postpartum. Despite the importance of this care, Medicaid coverage for longer than 60 days postpartum varies greatly state to state. After the Affordable Care Act was implemented, it was assumed that all states would expand their Medicaid programs to include parents in their coverage plans beyond the guaranteed 60 days, negating the need for a specific postpartum coverage time period. However, the 2012 Supreme Court decision in National Federation of Independent Business v Sebelius allowed states to opt out of Medicaid expansion.3 In many states, postpartum patients lose their Medicaid insurance after 60 days if they do not meet the stringent income criteria.
The income level that makes patients ineligible for Medicaid coverage at day 61 postpartum varies widely. In Maryland, a patient can extend their Medicaid coverage for 12 months postpartum if their family of 4 earns less than $73,260 annually (264% of the federal poverty level). However, in Mississippi, an income of more than $6,936 per year for a family of 4 (approximately 25% of the federal poverty level) renders mothers who are 61 days postpartum ineligible for Medicaid coverage.4 Thus, many low-income postpartum patients (who are at twice the risk of maternal mortality as affluent patients) find themselves without access to this critical care depending on the decisions of their state legislatures.5 The American Rescue Plan Act of 2021 (known as the COVID-19 Stimulus Package) included a provision that allows states to expand their postpartum Medicaid coverage from 60 days to 12 months; currently, 10 additional states are planning to expand postpartum Medicaid for 12 months. While encouraging, 14 states still have not announced plans to utilize this provision or apply for a waiver to extend Medicaid coverage in the postpartum period.6
Treatment for substance use
Drug overdose is a leading cause of pregnancy-related death from unintentional causes.7 Overdose deaths in the general population climbed between 2020 and 2021, reaching historic highs of more than 100,000 deaths in a 12-month period.8 Given the impact of substance use and overdose on maternal mortality, health systems should be maximizing efforts to respond to this public health crisis by implementing effective screening and treatment interventions and establishing clinics and hospitals as safe places to seek care. However, many states have criminalized substance use in pregnant patients and mandate that clinicians report patients who use substances, creating an ethical dilemma for clinicians seeking to screen and treat patients for substance use disorder. Twenty-three states consider substance use in pregnancy to be child abuse, and 3 states consider substance use in pregnancy to be grounds for civil commitment. In Wisconsin, a patient can be detained against their will for the duration of the pregnancy. Twenty-five states require health care professionals to report suspected substance abuse in pregnancy to child protective services or a similar state office.9 Even when universal substance use screening is implemented, it has disparate impact on patients of color; Black women who screened positive for substance use in pregnancy were more likely to be reported to child protective services than their White counterparts.10 The criminalization of pregnant bodies does not lead to improvements in individual, community, or public health, it infringes on the ethical principle of bodily autonomy and puts clinicians at odds with what is best for their patients.
Gender-affirming care
Gender-affirming care is supported by major medical organizations and reduces the risk of depression and suicidality in transgender youth.11 Despite this evidence, several states have passed legislation restricting or banning this care, criminalizing the doctors who provide it. Idaho’s house of representatives passed House Bill 675,12 which would make providing gender-affirming care a felony, punishable by up to a life sentence. This would extend to parents trying to access care for their children as well as clinicians.
Although abortion is the medical care most conspicuously manipulated by politics and legislation, it is far from the only example. No area of medicine will be untouched by eliminating access to reproductive health care and by the regulation and criminalization of health care workers who provide it. This is a sea change, although state legislative interference and disparities in reproductive health care have been a tocsin of such change for years. We can no longer afford to believe there is a separation between politics and medicine; this directly interferes with our Hippocratic oath to do no harm. A politician in Ohio should not decide whether or not a 13-year-old patient should have to carry a pregnancy to term; the house of representatives in Idaho should not put someone’s transgender child at increased risk of depression and suicidality by making their medical care a felony. Colleagues in Texas should not be punishable by life in prison for providing abortion care.13 As a physician, I cannot stand by when, facing a maternal mortality crisis, state politicians decide whether a patient living below the poverty line should have access to postpartum care.
I am neither a politician nor a legal scholar. I am a physician who takes care of people in this intimate and powerful space of healing and support between doctor and patient. What should we do? We need to come together to find the answers. We need to vote if we haven’t before. And we need to vote differently if we have elected lawmakers who politicize and dangerously interfere with medicine, the well-being of our patients, and our ability to carry out our duty as physicians in our patients’ best interests. We need to tell our stories—to each other, to our newspapers, to our neighbors, and to our legislatures. If we are leading organizations, we can use the power held in our institutions to commit to providing care to the fullest extent possible, commit to protecting our clinicians providing evidence-based care, and encourage legislators who use medicine as a political bargaining chip to reverse course. Medicine is not an apolitical field, and we can no longer uphold that paradigm. Our patients lives, and our livelihood as healers and caretakers, depends on our collective action against it. ●
Acknowledgement
The author would like to thank Lauren Sobel, DO, MPH, for her contributions to a presentation on this subject.
- Nash E, Ephross P. State policy trends at midyear 2022: with Roe about to be overturned, some states double down on abortion restrictions. Guttmacher Institute. June 22, 2022. https://live. guttmacher.org/article/2022/06/state-policy -trends-midyear-2022-roe-about-be-overturnedsome-states-double-down. Accessed September 12, 2022.
- Declercq E, Zephyrin L. Maternal mortality in the United States: a primer. Commonwealth Fund; 2020. https://www.commonwealthfund .org/publications/issue-brief-report/2020 /dec/maternal-mortality-united-states-primer. Accessed September 12, 2022.
- Santa Clara Law Digital Communications website. Supreme Court of the United States. National Federation of Independent Business v Sebelius. (2012). Patient Protection and Affordable Care Act Litigation. 333. https://digitalcommons.law.scu.edu /aca/333. Accessed September 13, 2022.
- Ranji U, Salganicoff A, Gomez I. Postpartum coverage extension in the American Rescue Plan Act of 2021. San Francisco, CA: Kaiser Family Foundation; 2021.
- Singh GK, Lee H. Trends and racial/ethnic, socioeconomic, and geographic disparities in maternal mortality from indirect obstetric causes in the United States, 1999-2017. Int J MCH AIDS. 2021;10:43.
- Kaiser Family Foundation. Medicaid Postpartum Coverage Extension Tracker. https://www.kff. org/medicaid/issue-brief/medicaid-postpartum -coverage-extension-tracker/. Accessed September 7, 2022.
- Mehta PK, Bachhuber MA, Hoffman R, et al. Deaths from unintentional injury, homicide, and suicide during or within 1 year of pregnancy in Philadelphia. Am J Public Health. 2016;106: 2208-2210.
- O’Donnell J, Tanz LJ, Gladden RM, et al. Trends in and characteristics of drug overdose deaths involving illicitly manufactured fentanyls— United States, 2019–2020. MMWR Morb Mortal Wkly Rep. 2021;70:1740.
- State laws and policies: substance use during pregnancy. Guttmacher Institute. https://www .guttmacher.org/state-policy/explore/substance -use-during-pregnancy. August 1, 2022. Accessed September 13, 2022.
- Roberts S, Nuru-Jeter A. Universal screening for alcohol and drug use and racial disparities in child protective services reporting. J Behav Health Serv Res. 2012;39;3-16.
- Tordoff DM, Wanta JW, Collin, et al. (2022). Mental health outcomes in transgender and nonbinary youths receiving gender-affirming care. JAMA Network Open. 2022;5:e220978. doi: 10.1001/jamanetworkopen.2022.0978.
- House Bill 675. Idaho Legislature web site. https:// legislature.idaho.gov/sessioninfo/2022/legislation/h0675/. Accessed September 9, 2022.
- Simon S. New Texas trigger law makes abortion a felony. NPR. August 27, 2022. https://www.npr. org/2022/08/27/1119795665/new-texas-trigger -law-makes-abortion-a-felony. Accessed September 13, 2022.
- Nash E, Ephross P. State policy trends at midyear 2022: with Roe about to be overturned, some states double down on abortion restrictions. Guttmacher Institute. June 22, 2022. https://live. guttmacher.org/article/2022/06/state-policy -trends-midyear-2022-roe-about-be-overturnedsome-states-double-down. Accessed September 12, 2022.
- Declercq E, Zephyrin L. Maternal mortality in the United States: a primer. Commonwealth Fund; 2020. https://www.commonwealthfund .org/publications/issue-brief-report/2020 /dec/maternal-mortality-united-states-primer. Accessed September 12, 2022.
- Santa Clara Law Digital Communications website. Supreme Court of the United States. National Federation of Independent Business v Sebelius. (2012). Patient Protection and Affordable Care Act Litigation. 333. https://digitalcommons.law.scu.edu /aca/333. Accessed September 13, 2022.
- Ranji U, Salganicoff A, Gomez I. Postpartum coverage extension in the American Rescue Plan Act of 2021. San Francisco, CA: Kaiser Family Foundation; 2021.
- Singh GK, Lee H. Trends and racial/ethnic, socioeconomic, and geographic disparities in maternal mortality from indirect obstetric causes in the United States, 1999-2017. Int J MCH AIDS. 2021;10:43.
- Kaiser Family Foundation. Medicaid Postpartum Coverage Extension Tracker. https://www.kff. org/medicaid/issue-brief/medicaid-postpartum -coverage-extension-tracker/. Accessed September 7, 2022.
- Mehta PK, Bachhuber MA, Hoffman R, et al. Deaths from unintentional injury, homicide, and suicide during or within 1 year of pregnancy in Philadelphia. Am J Public Health. 2016;106: 2208-2210.
- O’Donnell J, Tanz LJ, Gladden RM, et al. Trends in and characteristics of drug overdose deaths involving illicitly manufactured fentanyls— United States, 2019–2020. MMWR Morb Mortal Wkly Rep. 2021;70:1740.
- State laws and policies: substance use during pregnancy. Guttmacher Institute. https://www .guttmacher.org/state-policy/explore/substance -use-during-pregnancy. August 1, 2022. Accessed September 13, 2022.
- Roberts S, Nuru-Jeter A. Universal screening for alcohol and drug use and racial disparities in child protective services reporting. J Behav Health Serv Res. 2012;39;3-16.
- Tordoff DM, Wanta JW, Collin, et al. (2022). Mental health outcomes in transgender and nonbinary youths receiving gender-affirming care. JAMA Network Open. 2022;5:e220978. doi: 10.1001/jamanetworkopen.2022.0978.
- House Bill 675. Idaho Legislature web site. https:// legislature.idaho.gov/sessioninfo/2022/legislation/h0675/. Accessed September 9, 2022.
- Simon S. New Texas trigger law makes abortion a felony. NPR. August 27, 2022. https://www.npr. org/2022/08/27/1119795665/new-texas-trigger -law-makes-abortion-a-felony. Accessed September 13, 2022.