User login
Medical record documentation: What to do, and what to avoid
Medical record documentation serves as a reminder of previous discussions with patients and what happened during their visits, a reimbursement justification for services, a communication tool to coordinate care with current and future clinicians, and a basis for defense in legal or regulatory matters.1,2 Documentation should be thorough, accurate, timely, and objective, with the ultimate goal of communicating our thoughts in an easily understood manner to other clinicians or attorneys.2 If we fail to achieve this goal, we may inadvertently give the impression that our care was hurried, incomplete, or thoughtless.2
Although not an exhaustive list, this article outlines strategies to employ and practices to avoid in our documentation efforts so we may enhance our defense in case of litigation and ensure the smooth transition of care for our patients.
Strategies to employ
Proper and accurate documentation details the course of patient care, and we should describe our thoughts in a clear and logical manner. Doing so minimizes the risk of misinterpretation by other clinicians or attorneys. Make sure the documentation of each appointment details the reason(s) for the patient’s visit, the effectiveness of treatment, possible treatment nonadherence, our clinical assessment, treatment consent, changes to the patient’s treatment plan, follow-up plans, reasons for not pursuing certain actions (eg, hospitalization), and a suicide risk assessment (and/or a violence risk assessment, if clinically indicated).2 Document missed or rescheduled appointments, and telephone and electronic contact with patients. Also be sure to use only commonly approved abbreviations.2 Document these items sooner rather than later because doing so improves the credibility of your charting.1 If you are handwriting notes, add the date and time to each encounter and make sure your handwriting is legible. Describe the behaviors of patients in objective and nonjudgmental terms.3 Documenting quotes from patients can convey crucial information about what was considered when making clinical decisions.1
Practices to avoid
If there is a need to make changes to previous entries, ensure these corrections are not mistaken for alterations. Each health care institution has its own policy for making corrections and addenda to medical records. Corrections to a patient’s medical record are acceptable, provided they are done appropriately, as I outlined in a previous Pearls article.4 Minimize or eliminate the copying and pasting of information; doing so can improve the efficiency of our documentation, but the practice can undermine the quality of the medical record, increase the risk of outdated and repetitive information being included, lead to clinical errors, and lead to overbilling of services.5 Finally, be sure to avoid speculation, personal commentary about patients and their family members, and language with negative connotations (unless such language is a direct quote from the patient).2,3
1. Mossman D. Tips to make documentation easier, faster, and more satisfying. Current Psychiatry. 2008;7(2):80,84-86.
2. Staus C. Documentation: your very best defense. Psychiatric News. 2022;57(4):7,19.
3. Nelson KJ. How to use patient-centered language in documentation. Current Psychiatry. 2011;10(10):70.
4. Joshi KG. Metadata, malpractice claims, and making changes to the EHR. Current Psychiatry. 2021;20(3):e1-e3. doi:10.12788/cp.0106
5. Neal D. Do’s and don’ts of electronic documentation. Psychiatric News. 2021;56(8):7.
Medical record documentation serves as a reminder of previous discussions with patients and what happened during their visits, a reimbursement justification for services, a communication tool to coordinate care with current and future clinicians, and a basis for defense in legal or regulatory matters.1,2 Documentation should be thorough, accurate, timely, and objective, with the ultimate goal of communicating our thoughts in an easily understood manner to other clinicians or attorneys.2 If we fail to achieve this goal, we may inadvertently give the impression that our care was hurried, incomplete, or thoughtless.2
Although not an exhaustive list, this article outlines strategies to employ and practices to avoid in our documentation efforts so we may enhance our defense in case of litigation and ensure the smooth transition of care for our patients.
Strategies to employ
Proper and accurate documentation details the course of patient care, and we should describe our thoughts in a clear and logical manner. Doing so minimizes the risk of misinterpretation by other clinicians or attorneys. Make sure the documentation of each appointment details the reason(s) for the patient’s visit, the effectiveness of treatment, possible treatment nonadherence, our clinical assessment, treatment consent, changes to the patient’s treatment plan, follow-up plans, reasons for not pursuing certain actions (eg, hospitalization), and a suicide risk assessment (and/or a violence risk assessment, if clinically indicated).2 Document missed or rescheduled appointments, and telephone and electronic contact with patients. Also be sure to use only commonly approved abbreviations.2 Document these items sooner rather than later because doing so improves the credibility of your charting.1 If you are handwriting notes, add the date and time to each encounter and make sure your handwriting is legible. Describe the behaviors of patients in objective and nonjudgmental terms.3 Documenting quotes from patients can convey crucial information about what was considered when making clinical decisions.1
Practices to avoid
If there is a need to make changes to previous entries, ensure these corrections are not mistaken for alterations. Each health care institution has its own policy for making corrections and addenda to medical records. Corrections to a patient’s medical record are acceptable, provided they are done appropriately, as I outlined in a previous Pearls article.4 Minimize or eliminate the copying and pasting of information; doing so can improve the efficiency of our documentation, but the practice can undermine the quality of the medical record, increase the risk of outdated and repetitive information being included, lead to clinical errors, and lead to overbilling of services.5 Finally, be sure to avoid speculation, personal commentary about patients and their family members, and language with negative connotations (unless such language is a direct quote from the patient).2,3
Medical record documentation serves as a reminder of previous discussions with patients and what happened during their visits, a reimbursement justification for services, a communication tool to coordinate care with current and future clinicians, and a basis for defense in legal or regulatory matters.1,2 Documentation should be thorough, accurate, timely, and objective, with the ultimate goal of communicating our thoughts in an easily understood manner to other clinicians or attorneys.2 If we fail to achieve this goal, we may inadvertently give the impression that our care was hurried, incomplete, or thoughtless.2
Although not an exhaustive list, this article outlines strategies to employ and practices to avoid in our documentation efforts so we may enhance our defense in case of litigation and ensure the smooth transition of care for our patients.
Strategies to employ
Proper and accurate documentation details the course of patient care, and we should describe our thoughts in a clear and logical manner. Doing so minimizes the risk of misinterpretation by other clinicians or attorneys. Make sure the documentation of each appointment details the reason(s) for the patient’s visit, the effectiveness of treatment, possible treatment nonadherence, our clinical assessment, treatment consent, changes to the patient’s treatment plan, follow-up plans, reasons for not pursuing certain actions (eg, hospitalization), and a suicide risk assessment (and/or a violence risk assessment, if clinically indicated).2 Document missed or rescheduled appointments, and telephone and electronic contact with patients. Also be sure to use only commonly approved abbreviations.2 Document these items sooner rather than later because doing so improves the credibility of your charting.1 If you are handwriting notes, add the date and time to each encounter and make sure your handwriting is legible. Describe the behaviors of patients in objective and nonjudgmental terms.3 Documenting quotes from patients can convey crucial information about what was considered when making clinical decisions.1
Practices to avoid
If there is a need to make changes to previous entries, ensure these corrections are not mistaken for alterations. Each health care institution has its own policy for making corrections and addenda to medical records. Corrections to a patient’s medical record are acceptable, provided they are done appropriately, as I outlined in a previous Pearls article.4 Minimize or eliminate the copying and pasting of information; doing so can improve the efficiency of our documentation, but the practice can undermine the quality of the medical record, increase the risk of outdated and repetitive information being included, lead to clinical errors, and lead to overbilling of services.5 Finally, be sure to avoid speculation, personal commentary about patients and their family members, and language with negative connotations (unless such language is a direct quote from the patient).2,3
1. Mossman D. Tips to make documentation easier, faster, and more satisfying. Current Psychiatry. 2008;7(2):80,84-86.
2. Staus C. Documentation: your very best defense. Psychiatric News. 2022;57(4):7,19.
3. Nelson KJ. How to use patient-centered language in documentation. Current Psychiatry. 2011;10(10):70.
4. Joshi KG. Metadata, malpractice claims, and making changes to the EHR. Current Psychiatry. 2021;20(3):e1-e3. doi:10.12788/cp.0106
5. Neal D. Do’s and don’ts of electronic documentation. Psychiatric News. 2021;56(8):7.
1. Mossman D. Tips to make documentation easier, faster, and more satisfying. Current Psychiatry. 2008;7(2):80,84-86.
2. Staus C. Documentation: your very best defense. Psychiatric News. 2022;57(4):7,19.
3. Nelson KJ. How to use patient-centered language in documentation. Current Psychiatry. 2011;10(10):70.
4. Joshi KG. Metadata, malpractice claims, and making changes to the EHR. Current Psychiatry. 2021;20(3):e1-e3. doi:10.12788/cp.0106
5. Neal D. Do’s and don’ts of electronic documentation. Psychiatric News. 2021;56(8):7.
The SCOTUS 2021–2022 Term: Decisions and analysis
The 2021–2022 US Supreme Court Term was a blockbuster medical Term. The bookends of the Term were COVID-19 vaccinations and abortion rights. Between the bookends were Medicare reimbursement, criminal liability for prescribing controlled substances, gun control, and carbon dioxide emissions. In this article, we focus on the significant medical issues, briefly note other important decisions, and consider the implications of this Term.
Abortion decisions
Dobbs v Jackson Women’s Health Organization1 was the most controversial decision and, for ObGyns, perhaps the most important decision in decades. The basic holding of the case can be stated simply: Roe v Wade2 and Planned Parenthood of Southeastern Pennsylvania v Casey3 (which essentially created a constitutional right to abortion) are overruled. The law related to abortion is for the states and Congress to determine, not federal courts. (For a review of earlier reproductive freedom cases in the Court, see our previous article, “The Supreme Court and reproductive rights.”4)
Dobbs arose from a Mississippi statute that made it illegal to perform abortions after 15 weeks of gestation, well before viability. Six members of the Court held that the Mississippi law was constitutional and 3 would have struck down the state law. There were 5 opinions, covering a total of 213 pages in the U.S. Reports. The Court fell into 4 camps, ranging from the most to the least protective of abortion rights, as follows:
- Three justices (Breyer, Kagan, and Sotomayor) voted to strike down the Mississippi statute and uphold Roe and Casey and wrote a joint dissent. They believe the Constitution makes abortion an issue “off limits to majority rule.” They also warned that other areas of “substantive due process” (discussed below), including contraception and same-sex marriage, might be under threat.
- The Chief Justice voted to uphold the statute but wanted an incremental approach; that is, not to overturn Roe and Casey entirely in this case because the Dobbs case required the Court only to determine the more limited question of whether the 15-week limit on abortion was constitutional. He found that the viability standard did not make sense, but he suggested that the Court “leave for another day” whether to overturn Roe.
- Five justices joined the opinion to uphold the statute and overturn Roe. Justice Alito wrote the decision joined by Justices Thomas, Kavanaugh, Gorsuch, and Barrett. They found that a right to abortion was not “deeply rooted in our Nation’s history,” as evidenced by the fact that when the 14th Amendment was adopted, abortion was a criminal offense in most states and not a protected right in any state. In 2 lengthy appendices, the Court reviewed the criminalization of abortion in the states in 1868 and in the territories that later became states. Even when Roe was decided in 1973, abortion was not “deeply rooted” because it was not generally legal in the states. Justice Kavanaugh joined this opinion and wrote separately to emphasize that the majority opinion does not outlaw abortion, but rather leaves the issue to “the people and their representatives.” He also emphasized that the case did not overturn all of the substantive due process cases.
- Justice Thomas would have gone further and abandoned “substantive due process” completely.
The constitutional issue
The majority said that the issue before the Court was not whether the law should permit or prohibit abortions—that is a question for the political branches. Rather, the question was only whether the Constitution precludes the political branches from allowing abortions. There is no mention of abortion in the Constitution and no specific reference to a right to privacy that includes medical decisions. A central constitutional question has been to identify where exactly in the Constitution the right to privacy resides. The Court has generally used “substantive due process” to locate privacy rights. The 14th Amendment provides, in part, that no state may “deprive any person of life, liberty, or property, without due process of law.” “Process” generally refers to procedural protections, but the Court sometimes has used it to encompass substantive rights (for example, privacy)—hence, “substantive due process.”
Over the decades, the legitimacy of substantive due process has remained controversial. Justice Thomas called it an “oxymoron” to turn “process” into substantive rights. And its use has a somewhat checkered history. For nearly 50 years (1890–1937), it was used to preclude states from protecting employees (for example, hour and wage laws violated “the right to contract”) and was discredited. More recently the Court has used substantive due process to protect contraception access, abortion, and same-sex marriages.
A critical question is knowing what rights substantive due process protects. The Court sometimes has said that it protects rights “deeply rooted in the Nation’s history and traditions” and “implicit in the concept of ordered liberty,”5 although in other cases suggested a more ambiguous definition.6 The next constitutional question is how to state or define the right to be protected. For example, is it the right to intimately personal decisions, bodily integrity, reproductive choice, abortion, or late-term abortion? Some of those may be deeply rooted in history and traditions (intimate decisions), and others not so much (late-term abortion). Finally, a question is whether a substantive right is defined at the time the 14th Amendment was adopted (1868) or now—is it a “living Constitution” that, without much guidance, means whatever 5 justices believe at the moment, or is it a Constitution grounded in the distant past?
The future of substantive due process is uncertain following Dobbs. Although the majority said it was not disclaiming substantive due process, the dissent said it doubted that claim because other rights are “part of the same constitutional fabric” (substantive due process). The Court might, in future cases, find some other constitutional provision in which to ground rights. The source of those rights might be the 9th Amendment (in addition to the Constitution’s enumerated rights, there are “others retained by the people”) or another provision of the 14th (“No State shall make or enforce any law which shall abridge the privileges or immunities of citizens of the United States…”). Each of these possibilities has its problems, many of which are similar to substantive due process, but they avoid the “oxymoron” issue.
Among the other important cases this Term, the Court made these determinations:
- Held that the 2nd Amendment, as applied to the states through the 14th Amendment, includes a general right to carry a gun for self-defense outside the home.1 It struck down a New York law that required people to show a special need to have and carry a gun.
- Determined that the US Environmental Protection Agency exceeded the authority Congress had granted it with a “Clean Power Plan” that was intended to reduce carbon dioxide emissions.2 It is up to Congress, not the agency, to expand agency authority.
- Gave trial courts discretion in determining whether (and under what conditions) children in international custody disputes must be returned to their home countries where there is a serious risk of harm to them.3
- Held that there is an implied right of action to sue medical providers for disability discrimination, but under the Rehabilitation Act and the Affordable Care Act the damages do not include emotional harm.4
- Decided several “free exercise of religion” cases, and in each found the state had violated religious rights, holding that: A state improperly prevented religious schools from being eligible for a state tuition grant system,5 a coach was wrongfully fired for kneeling in prayer following football games,6 Boston denied free speech in allowing other organizations to fly their flags but denying a Christian flag to be displayed,7 and a state must permit prisoners to have a spiritual advisor to be present and pray and touch them during their execution.8
- Held that the administration’s rescission of the “stay in Mexico” immigration policy was permitted by existing statutes.9
References
1. New York State Rifle & Pistol Association, Inc. v Bruen, 20-843, decided June 23, 2022. https://www.supremecourt.gov/opinions/21pdf/20-843_7j80.pdf
2. West Virginia v Environmental Protection Agency, 20-1530, decided June 30, 2022. https://www.supremecourt.gov/opinions/21pdf/20-1530_new_l537.pdf
3. Golan v Saada, 20-1034, decided June 15, 2022. https://www.supremecourt.gov/opinions/21pdf/20-1034_b8dg.pdf
4. Cummings v Premier Rehab Keller, 20-219, decided April 28, 2022. https://www.supremecourt.gov/opinions/21pdf/20-219_1b82.pdf
5. Carson v Makin, 20-1088, decided June 21, 2022. https://www.supremecourt.gov/opinions/21pdf/20-1088_dbfi.pdf
6. Kennedy v Bremerton School District., 21-418, decided June 27, 2022. https://www.supremecourt.gov/opinions/21pdf/21-418_new_onkq.pdf
7. Shurtleff v Boston, 20-1800, decided May 2, 2022. https://www.supremecourt.gov/opinions/21pdf/20-1800_7lho.pdf
8. Ramirez v Collier, 21-5592, decided March 24, 2022. https://www.supremecourt.gov/opinions/21pdf/21-5592_feah.pdf
9. Biden v Texas, 21-9 54, decided June 30, 2022. https://www.supremecourt.gov/opinions/21pdf/21-954_7l48.pdf
Continue to: ObGyn briefs in the case...
ObGyn briefs in the case
The medical profession filed several amicus curiae briefs in the Dobbs case. (These are “friends of the court” briefs filed by nonparties to the litigation. The purpose is to give a court a perspective on the case not presented by the parties.) The American College of Obstetricians and Gynecologists (ACOG) took the lead in filing an amicus brief.7 Nearly 2 dozen other medical organizations joined the brief, including the American Academy of Pediatrics, American College of Osteopathic Obstetricians and Gynecologists, American Gynecological and Obstetrical Society, American Society for Reproductive Medicine, Council of University Chairs of Obstetrics and Gynecology, North American Society for Pediatric and Adolescent Gynecology, Society for Academic Specialists in General Obstetrics and Gynecology, Society of Gynecologic Oncology, and Society of OB/GYN Hospitalists.
The brief argued that abortion is a safe procedure, an abortion ban would harm the health of pregnant patients, and it would undermine the physician-patient relationship and interfere with patient autonomy. It also discussed the issue of fetal pain,8 telling the Court that “Every major medical organization that has examined the issue of fetal pain and peer-reviewed studies on the matter have consistently concluded that pre-viability abortion does not result in fetal pain perception.”9 The brief was cited in the dissent for the fact that “About 18 percent of pregnancies in this country end in abortion, and about one-quarter of American women will have an abortion before the age of 45.”10
The Court received a different view from an amicus brief filed by the American Association of Pro-Life Obstetricians and Gynecologists.11 It told the Court that abortion, especially later-term, poses health risks: the abortion process itself may injure the woman, abortion puts women at risk for future preterm births, later-term abortion raises a woman’s risk of developing breast cancer, and abortions (especially those later in the pregnancy) are linked to a greater risk of psychological harm.12 The brief also noted that 93% of obstetrician-gynecologists do not perform abortions, and “abortion has been deemed contrary to sound medicine for thousands of years” (citing the Hippocratic oath).13 The brief was not cited by the Court.
Many other medical and pro-life medical groups presented amicus briefs. A list of and links to all the briefs is available on the SCOTUSblog website at https://www.scotusblog.com/case-files/cases/dobbs-v-jackson-womens-health-organization/.
Ramifications
The Court decision does not make abortion illegal but allows states (and possibly Congress) to decide whether, when, and how abortions may be performed. Some states may ban most abortions (making it illegal to have or to perform abortions). Thirteen states had “trigger laws” to go into effect limiting abortion if the Court permitted such limitations. Most of those states were almost immediately entangled in lawsuits challenging the state laws. Some states, for example, have privacy provisions in their state constitution that state courts could interpret as allowing abortion, thereby voiding the state statutes prohibiting abortion.
At least a few states have abortion laws still on the books that were passed decades ago (perhaps before Roe) and were never repealed. Those laws may once again be valid, although state courts might hold that those statutes were repealed by Roe and must be passed again to be valid. Some experts anticipate that 28 states will eventually have significant limitations on abortion.
The Guttmacher Institute maintains a frequently updated table on the abortion laws in each state.14 According to one estimate, 29 states are hostile to abortion rights (or lean that way), with about 40 million women aged 13 to 44 (58% of the United States) living in states with some hostility to abortion.15 Congress may pass some national abortion laws, but that seems unlikely and there may be some limits on its ability to control private medical practice within states.
An additional legal issue will arise from medication-induced abortions, generally through the use of mifepristone and misoprostol. They now account for the majority of abortions. These medications might be used for abortion, up to about 9 weeks of pregnancy, in states prohibiting abortion. The drugs once were available only with an in-person visit, but now the US Food and Drug Administration (FDA) permits mail-order delivery. The potential exists, therefore, to circumvent states’ prohibition on abortion through mail-order postal shipments. The FDA controls the licensing of pharmaceuticals in interstate commerce, but not the practice of medicine within a state. Therefore the ability of individuals (within a state) to possess or use drugs is unclear.
The abortion wars of the last 50 years gave rise to state laws related to abortion, including consent by minors, information to parents, special informed consent, and facilities requirements. If these laws were once struck down because they were inconsistent with Roe, but were never formally repealed, they may now become legal requirements.
In the foreseeable future, abortion laws generally will not be determined by federal courts but by state law, generally legislatures. In legislative hearings, town hall meetings, and conversations with lawmakers, ObGyns should engage the topic of abortion with scientific expertise, reason, openness, and humility. It will be impossible for the profession to speak with a single voice, as the briefs filed this Term demonstrate. Where there are honest differences in science, the reasons for the different interpretations should be explainable to lay decision makers. The profession, who are not being pseudo-lobbyists, can contribute a great deal to the rational consideration of this emotional topic.
On January 27, 2022, Justice Stephen Breyer informed President Biden of his intention to retire from the Court at the end of the Term. At age 84, he was the oldest member of the Court, but he continued to be among the most active of the justices and seemed to relish the work of the Court. He had been under pressure from liberal groups to retire earlier so a successor could be confirmed by a Democratic Senate. In many ways he was the Renaissance man of the Court: he spoke fluent French, wrote books, and famously sprinkled his questions with complex and funny hypotheticals.
Justice Breyer was a law professor before becoming a judge and enjoyed presentations to many groups, from children to law professors. He loved the Court and defended it—most recently against partisan attacks from both the right and the left. In the decisions of the Court, he was one of the more liberal justices. He had, for example, indicated that the death penalty is unconstitutional.
In his January retirement letter, he said that he would step down at the end of the Term if his replacement had been appointed and confirmed. She had. The new justice had clerked for Justice Breyer in 1999–2000.
Ketanji Brown Jackson was nominated by President Biden on February 28, confirmed by the Senate on April 7 by a 53–47 margin, and sworn in on June 30, 2022. Justice Jackson had previously been a federal district court judge and on the Court of Appeals for the D.C. Circuit. She attended Harvard-Radcliffe College and received her law degree from Harvard Law School. She worked as a criminal defense attorney and was active in the US Sentencing Commission.
Continue to: What is a practitioner to do?...
What is a practitioner to do?
For many practitioners, the Dobbs decision will have little effect because their state laws are consistent with Roe, and the legislature is not going to change the law. They may, of course, see an influx of patients from other states (that restrict abortion) seeking treatment. At the other extreme, in some states, most abortions will become prohibited. State courts may ease the restrictions. In many states, there will be an ongoing battle over when abortion is legal and when it is not, resulting in shifting laws and regulations. Keeping up with the shifts that affect practice will be a challenge.
All states are likely to permit abortions “to save the life of the mother,” and many will have a version of “to preserve the health of the mother.” Other exceptions may be for pregnancy resulting from rape or incest or in the case of serious fetal abnormality. ObGyns, of course, will be called on to certify that one of these exceptions exists. Determining that pregnancy resulted from rape or incest, of course, can be challenging. Before Roe, there was a cottage industry opining that pregnancy seriously affected the health of the mother, which often involved physical manifestations of mental health. ObGyns in some states may be asked once again to make such determinations.
Laws not directly related to abortions will, in some states, be changed as a way of discouraging abortion. For example, child abuse reporting laws may be modified to require reporting of any known or suspected abortion or attempted abortion, and medical licensing standards may make it a violation to participate in or facilitate abortion in any way.
Particularly in states where the rules keep shifting, practitioners must keep up with the current law. Professional organizations can help with that, but there is no substitute for practitioners having an ongoing professional relationship with an attorney who has expertise in health law.
Other abortion decisions this Term
In other abortion decisions this Term, the Court refused to suspend a Texas law that prohibited abortions after a fetal heartbeat could be detected.16 The law has remarkable enforcement mechanisms that preclude state officers from enforcing it; instead, it creates what amounts to a private attorney general (PAG) provision that allows private citizens to file suit against anyone performing or assisting in performing abortions. This PAG made pre-enforcement challenges to the law difficult.17
In a Kentucky case, the Court allowed the Kentucky attorney general to intervene in a case that challenged a Kentucky law that prohibits physicians from using dilation and evacuation procedures to end second-trimester pregnancies.18
Criminal convictions for physicians’ overprescription of controlled substances
Perhaps the least sympathetic of the physicians involved with the Court this Term were the 2 in Ruan v U.S.19 Their trials indicate that Dr. Ruan’s clinic issued more than 300,000 controlled substance prescriptions over 4 years and was one of the most frequent prescribers of fentanyl. Dr. Kahn prescribed controlled substances without an examination, falsified notes, and sold controlled substances for cash and guns.20
Both physicians were convicted of “knowingly or intentionally” dispensing a controlled substance without authorization.21 They were authorized to prescribe drugs, but only “for a legitimate medical purpose.”22 Appeals to their respective Circuit courts confirmed their convictions. The Supreme Court, however, held that to convict them, the government must prove that they knowingly or intentionally acted in an unauthorized manner. That proof can be by circumstantial evidence, but it must be beyond a reasonable doubt.
Health care reimbursement
Hospitals won one and lost one Medicare-Medicaid reimbursement case that involved payments for low-income patients.
In the loss, the Court held that the US Department of Health and Human Services (HHS) properly calculated the disproportionate share adjustments (DSH), or Medicare fraction,23 that provides a supplemental payment for hospitals with a large proportion of low-income patients. The lower DSH payments calculated by HHS were upheld, thereby reducing the number of hospitals receiving DSH payments and decreasing the amounts others will receive.
The win involved payments for prescription drugs that hospitals provide to outpatients in safety-net hospitals.24 HHS determined that it was overpaying hospitals for drugs and cut the reimbursement rate. The Court held that before HHS can change the drug rate, it must conduct a survey of hospitals regarding actual costs. It had not done that, so the rate reduction was not permitted by the law.
An accidental disincentive to (some) malpractice suits
Medicaid requires states to obtain part of a tort recovery that recipients obtain if Medicaid is covering medical expenses related to their injuries. In implementing that law, a state may provide a disincentive for injured beneficiaries to file malpractice cases. At issue was a Florida law that provided the Medicaid state would take 37.5% of the beneficiary’s total tort recovery (being one-half of the recovery after deducting 25% for attorney’s fees and costs). In a 7-2 decision, the Court upheld the Florida law.25
The disincentive to filing a lawsuit is that the state is taking 37.5%, plus contingency fee attorneys will typically take 33.3% (and there will be some fees). This is especially true when there is a state cap on noneconomic damages. In the case the Court decided, the plaintiff received a settlement of $850,000. If we assume a typical contingency fee, less the state’s Medicaid claim of $300,000, the plaintiff possibly received $266,667. That is not trivial, but it is only 31% of the settlement.
The Medicaid expectation of reimbursement and the Florida approach, however, impose heavy burdens on severely injured beneficiaries. The plaintiff had catastrophic injuries and was in a vegetative state. There are some things Medicaid does not pay for, as well as nonmedical expenses. The amount left for such expenses is likely well below what the family will need.
Continue to: COVID-19 vaccinations...
COVID-19 vaccinations
Had it not been for the abortion decisions, 2021–2022 might have been “the COVID Term.” Two of the most anticipated decisions involved mandatory vaccinations (or masking/testing instead). The question in each of these cases was whether Congress had authorized 2 federal agencies to issue the emergency regulations requiring vaccination. Emergency regulations are held to higher standards because they bypass the usual protections of the Administrative Procedure Act.
One case involved a regulation issued by the Occupational Safety and Health Administration (OSHA) that employers (with more than 100 employees) must require their employees to be vaccinated. In a 6-3 decision, the Court held that OSHA did not have the authority to enforce this as an emergency regulation. The other case was a regulation issued by HHS that health care institutions receiving Medicare and Medicaid funding must require all staff to be vaccinated.26 In a 5-4 decision, the Court upheld this emergency regulation because of the very broad authority Congress had given HHS to ensure the safety of patients and the quality of Medicare- and Medicaid-funded programs.27
In another case, in the shadow docket (orders and opinions in cases without full arguments), the Court struck down the Centers for Disease Control and Prevention’s eviction moratorium.28 The Court said the government claimed “a breathtaking amount of authority” that Congress did not intend. In other shadow docket cases, the Court refused to hold unconstitutional state laws that require COVID-19 vaccination but did not have religious exemptions.29
Analysis of this Term
It was an extraordinary Term. The Court decided 66 cases (excluding most cases in the shadow docket), a low number historically. Not only were there many seminal cases but also the Court appears to be shifting toward a new direction. That direction may be oriented more toward the original understanding of the words of the Constitution and statutes and less toward policy; Congress rather than administrative agencies; racial nondiscrimination rather than preferences; and the free exercise rather than the establishment of religion. Whether there is such a shift or not, of course, only time will tell.
Chief Justice Roberts and Justice Kavanaugh were in the majority most often (95% of the cases), followed by Justices Barrett (90%), Alito (85%), Thomas (80%), and Gorsuch (75%). Justices Kagan (69%) and Breyer (68%) were not far behind. Justice Sotomayor was in the majority 58%. The Court was unanimous 29% of the time, well below the decade average (43%), and 6-3 accounted for 30% of the decisions.
A major, potentially scarring, event this Term was the leak of an early draft of the majority opinion in Dobbs. Although leaks have occurred before, the early leak of an opinion was unprecedented. It will almost inevitably change the openness and candor within the Court and the justices’ clerks. Although not unprecedented, the attempt on the life of Justice Kavanaugh and the organized efforts to harass some justices in their homes are likely to have lasting impact. Almost certainly it means that justices and their families will have constant security and their movements and connection with the general public will become less frequent, which is sad for the justices and our democracy.
Looking toward the next Term
When the Court next convenes, Justice Ketanji Brown Jackson will take her seat on the left end of the Court (the traditional seat for a new justice, not a commentary on judicial philosophy). The Court has already taken many cases, including issues about university affirmative action programs, web designers and same-sex couples, redistricting and voting rights, DNA testing in criminal cases, and overtime pay for someone making over $200,000 per year. It begins Monday, October 3, and promises to be another interesting Term. ●
- Dobbs v Jackson Women’s Health Organization, 19-1392, decided June 24, 2022. https://www.supremecourt.gov /opinions/21pdf/19-1392_6j37.pdf
- Roe v Wade, 410 U.S. 113, 163 (1973).
- Planned Parenthood of Southeastern Pennsylvania v Casey, 505 U.S. 833 (1992).
- Smith SR, Sanfilippo JR. The Supreme Court and reproductive rights. OBG Manag. 2022;34(1):36-41, 46. https://cdn.mdedge. com/files/s3fs-public/issues/articles/obgm0340136_smith.pdf
- Washington v Glucksberg, 521 U.S. 702 (1997).
- Obergefell v Hodges, 576 U.S. 644, 654-70 (2015).
- Brief of amici curiae of American College of Obstetricians and Gynecologists, American Medical Association, et al, in Dobbs v Jackson Women’s Health Organization, in Support of Respondents (Sep. 2021). https://www.supremecourt .gov/DocketPDF/19/19-1392/193074/20210920174518042 _19-1392%20bsacACOGetal.pdf
- Id. at 8, 13-15.
- Id. at 14.
- Justices Breyer, Kagan, and Sotomayor, dissenting, at 48, note 22.
- Brief for American Association of Pro-Life Obstetricians And Gynecologists as Amicus Curiae, in Dobbs v Jackson Women’s Health Organization, in Support of Petitioners (July 2021). https://www.supremecourt.gov /DocketPDF/19/19-1392/185350/20210729163532595_No. %2019-1392%20-%20American%20Association%20of%20 Pro-Life%20Obstetricians%20and%20Gynecologists%20-%20 Amicus%20Brief%20in%20Support%20of%20Petitioner%20-%20 7-29-21.pdf
- Id. at 3-4, 7-29.
- Id. at 30.
- Guttmacher Institute. An overview of abortion laws. July 11, 2022. https://www.guttmacher.org/state-policy/explore/overview -abortion-laws
- Guttmacher Institute. State abortion policy landscape: from hostile to supportive. Dec. 2020. https://www .guttmacher.org/article/2019/08/state-abortion-policy -landscape-hostile-supportive
- Whole Woman’s Health v Jackson, 21-463, decided Dec. 10, 2021. https://www.supremecourt.gov/opinions/21pdf/21-463_ new_8o6b.pdf
- United States v Texas, 21-588, decided Dec. 10, 2021. (Per curiam, Sotomayor dissenting). https://www.supremecourt.gov /opinions/21pdf/21-588_c07d.pdf
- Cameron v EMW Women’s Surgical Center, 20-601, decided Mar. 3, 2022. https://www.supremecourt.gov/opinions/21pdf/20-601 _new_g20h.pdf
- Xiulu Ruan v United States, 20-1410, decided June 27, 2022. https:// www.supremecourt.gov/opinions/21pdf/20-1410_1an2.pdf
- Adam Liptak. Supreme Court sides with doctors accused of running pill mills. The New York Times. June 27, 2022. https://www .nytimes.com/2022/06/27/us/politics/supreme-court-controlled -substance-act.html
- 84 Stat. 1260, 21 U.S.C. §841(a).
- 21 CFR §1306.04(a) (2021).
- Becerra v Empire Health Foundation, For Valley Hospital Medical Center, 20-1312, decided June 24, 2022. https://www.supremecourt .gov/opinions/21pdf/20-1312_j42l.pdf
- American Hospital Association v Becerra, 20-1114, decided June 15, 2022. https://www.supremecourt.gov/opinions/21pdf/20 -1114_09m1.pdf
- Gallardo v Marstiller, 20-1263, decided June 6, 2022. https:// www.supremecourt.gov/opinions/21pdf/20-1263_new_hfci.pdf
- National Federation of Independent Business v Department of Labor, Occupational Safety and Health Administration, 21A244, decided Jan. 13, 2022. https://www.supremecourt.gov /opinions/21pdf/21a244_hgci.pdf
- Biden v Missouri, 21A240, decided Jan. 13, 2022. https://www .supremecourt.gov/opinions/21pdf/21a240_d18e.pdf
- Alabama Association of Realtors v Department of Health and Human Services, 21A23, decided Aug. 26, 2021. https://www .supremecourt.gov/opinions/20pdf/21a23_ap6c.pdf
- Does v Mills, 21A90, decided Oct. 29, 2021. https://www .supremecourt.gov/opinions/21pdf/21a90_6j37.pdf
The 2021–2022 US Supreme Court Term was a blockbuster medical Term. The bookends of the Term were COVID-19 vaccinations and abortion rights. Between the bookends were Medicare reimbursement, criminal liability for prescribing controlled substances, gun control, and carbon dioxide emissions. In this article, we focus on the significant medical issues, briefly note other important decisions, and consider the implications of this Term.
Abortion decisions
Dobbs v Jackson Women’s Health Organization1 was the most controversial decision and, for ObGyns, perhaps the most important decision in decades. The basic holding of the case can be stated simply: Roe v Wade2 and Planned Parenthood of Southeastern Pennsylvania v Casey3 (which essentially created a constitutional right to abortion) are overruled. The law related to abortion is for the states and Congress to determine, not federal courts. (For a review of earlier reproductive freedom cases in the Court, see our previous article, “The Supreme Court and reproductive rights.”4)
Dobbs arose from a Mississippi statute that made it illegal to perform abortions after 15 weeks of gestation, well before viability. Six members of the Court held that the Mississippi law was constitutional and 3 would have struck down the state law. There were 5 opinions, covering a total of 213 pages in the U.S. Reports. The Court fell into 4 camps, ranging from the most to the least protective of abortion rights, as follows:
- Three justices (Breyer, Kagan, and Sotomayor) voted to strike down the Mississippi statute and uphold Roe and Casey and wrote a joint dissent. They believe the Constitution makes abortion an issue “off limits to majority rule.” They also warned that other areas of “substantive due process” (discussed below), including contraception and same-sex marriage, might be under threat.
- The Chief Justice voted to uphold the statute but wanted an incremental approach; that is, not to overturn Roe and Casey entirely in this case because the Dobbs case required the Court only to determine the more limited question of whether the 15-week limit on abortion was constitutional. He found that the viability standard did not make sense, but he suggested that the Court “leave for another day” whether to overturn Roe.
- Five justices joined the opinion to uphold the statute and overturn Roe. Justice Alito wrote the decision joined by Justices Thomas, Kavanaugh, Gorsuch, and Barrett. They found that a right to abortion was not “deeply rooted in our Nation’s history,” as evidenced by the fact that when the 14th Amendment was adopted, abortion was a criminal offense in most states and not a protected right in any state. In 2 lengthy appendices, the Court reviewed the criminalization of abortion in the states in 1868 and in the territories that later became states. Even when Roe was decided in 1973, abortion was not “deeply rooted” because it was not generally legal in the states. Justice Kavanaugh joined this opinion and wrote separately to emphasize that the majority opinion does not outlaw abortion, but rather leaves the issue to “the people and their representatives.” He also emphasized that the case did not overturn all of the substantive due process cases.
- Justice Thomas would have gone further and abandoned “substantive due process” completely.
The constitutional issue
The majority said that the issue before the Court was not whether the law should permit or prohibit abortions—that is a question for the political branches. Rather, the question was only whether the Constitution precludes the political branches from allowing abortions. There is no mention of abortion in the Constitution and no specific reference to a right to privacy that includes medical decisions. A central constitutional question has been to identify where exactly in the Constitution the right to privacy resides. The Court has generally used “substantive due process” to locate privacy rights. The 14th Amendment provides, in part, that no state may “deprive any person of life, liberty, or property, without due process of law.” “Process” generally refers to procedural protections, but the Court sometimes has used it to encompass substantive rights (for example, privacy)—hence, “substantive due process.”
Over the decades, the legitimacy of substantive due process has remained controversial. Justice Thomas called it an “oxymoron” to turn “process” into substantive rights. And its use has a somewhat checkered history. For nearly 50 years (1890–1937), it was used to preclude states from protecting employees (for example, hour and wage laws violated “the right to contract”) and was discredited. More recently the Court has used substantive due process to protect contraception access, abortion, and same-sex marriages.
A critical question is knowing what rights substantive due process protects. The Court sometimes has said that it protects rights “deeply rooted in the Nation’s history and traditions” and “implicit in the concept of ordered liberty,”5 although in other cases suggested a more ambiguous definition.6 The next constitutional question is how to state or define the right to be protected. For example, is it the right to intimately personal decisions, bodily integrity, reproductive choice, abortion, or late-term abortion? Some of those may be deeply rooted in history and traditions (intimate decisions), and others not so much (late-term abortion). Finally, a question is whether a substantive right is defined at the time the 14th Amendment was adopted (1868) or now—is it a “living Constitution” that, without much guidance, means whatever 5 justices believe at the moment, or is it a Constitution grounded in the distant past?
The future of substantive due process is uncertain following Dobbs. Although the majority said it was not disclaiming substantive due process, the dissent said it doubted that claim because other rights are “part of the same constitutional fabric” (substantive due process). The Court might, in future cases, find some other constitutional provision in which to ground rights. The source of those rights might be the 9th Amendment (in addition to the Constitution’s enumerated rights, there are “others retained by the people”) or another provision of the 14th (“No State shall make or enforce any law which shall abridge the privileges or immunities of citizens of the United States…”). Each of these possibilities has its problems, many of which are similar to substantive due process, but they avoid the “oxymoron” issue.
Among the other important cases this Term, the Court made these determinations:
- Held that the 2nd Amendment, as applied to the states through the 14th Amendment, includes a general right to carry a gun for self-defense outside the home.1 It struck down a New York law that required people to show a special need to have and carry a gun.
- Determined that the US Environmental Protection Agency exceeded the authority Congress had granted it with a “Clean Power Plan” that was intended to reduce carbon dioxide emissions.2 It is up to Congress, not the agency, to expand agency authority.
- Gave trial courts discretion in determining whether (and under what conditions) children in international custody disputes must be returned to their home countries where there is a serious risk of harm to them.3
- Held that there is an implied right of action to sue medical providers for disability discrimination, but under the Rehabilitation Act and the Affordable Care Act the damages do not include emotional harm.4
- Decided several “free exercise of religion” cases, and in each found the state had violated religious rights, holding that: A state improperly prevented religious schools from being eligible for a state tuition grant system,5 a coach was wrongfully fired for kneeling in prayer following football games,6 Boston denied free speech in allowing other organizations to fly their flags but denying a Christian flag to be displayed,7 and a state must permit prisoners to have a spiritual advisor to be present and pray and touch them during their execution.8
- Held that the administration’s rescission of the “stay in Mexico” immigration policy was permitted by existing statutes.9
References
1. New York State Rifle & Pistol Association, Inc. v Bruen, 20-843, decided June 23, 2022. https://www.supremecourt.gov/opinions/21pdf/20-843_7j80.pdf
2. West Virginia v Environmental Protection Agency, 20-1530, decided June 30, 2022. https://www.supremecourt.gov/opinions/21pdf/20-1530_new_l537.pdf
3. Golan v Saada, 20-1034, decided June 15, 2022. https://www.supremecourt.gov/opinions/21pdf/20-1034_b8dg.pdf
4. Cummings v Premier Rehab Keller, 20-219, decided April 28, 2022. https://www.supremecourt.gov/opinions/21pdf/20-219_1b82.pdf
5. Carson v Makin, 20-1088, decided June 21, 2022. https://www.supremecourt.gov/opinions/21pdf/20-1088_dbfi.pdf
6. Kennedy v Bremerton School District., 21-418, decided June 27, 2022. https://www.supremecourt.gov/opinions/21pdf/21-418_new_onkq.pdf
7. Shurtleff v Boston, 20-1800, decided May 2, 2022. https://www.supremecourt.gov/opinions/21pdf/20-1800_7lho.pdf
8. Ramirez v Collier, 21-5592, decided March 24, 2022. https://www.supremecourt.gov/opinions/21pdf/21-5592_feah.pdf
9. Biden v Texas, 21-9 54, decided June 30, 2022. https://www.supremecourt.gov/opinions/21pdf/21-954_7l48.pdf
Continue to: ObGyn briefs in the case...
ObGyn briefs in the case
The medical profession filed several amicus curiae briefs in the Dobbs case. (These are “friends of the court” briefs filed by nonparties to the litigation. The purpose is to give a court a perspective on the case not presented by the parties.) The American College of Obstetricians and Gynecologists (ACOG) took the lead in filing an amicus brief.7 Nearly 2 dozen other medical organizations joined the brief, including the American Academy of Pediatrics, American College of Osteopathic Obstetricians and Gynecologists, American Gynecological and Obstetrical Society, American Society for Reproductive Medicine, Council of University Chairs of Obstetrics and Gynecology, North American Society for Pediatric and Adolescent Gynecology, Society for Academic Specialists in General Obstetrics and Gynecology, Society of Gynecologic Oncology, and Society of OB/GYN Hospitalists.
The brief argued that abortion is a safe procedure, an abortion ban would harm the health of pregnant patients, and it would undermine the physician-patient relationship and interfere with patient autonomy. It also discussed the issue of fetal pain,8 telling the Court that “Every major medical organization that has examined the issue of fetal pain and peer-reviewed studies on the matter have consistently concluded that pre-viability abortion does not result in fetal pain perception.”9 The brief was cited in the dissent for the fact that “About 18 percent of pregnancies in this country end in abortion, and about one-quarter of American women will have an abortion before the age of 45.”10
The Court received a different view from an amicus brief filed by the American Association of Pro-Life Obstetricians and Gynecologists.11 It told the Court that abortion, especially later-term, poses health risks: the abortion process itself may injure the woman, abortion puts women at risk for future preterm births, later-term abortion raises a woman’s risk of developing breast cancer, and abortions (especially those later in the pregnancy) are linked to a greater risk of psychological harm.12 The brief also noted that 93% of obstetrician-gynecologists do not perform abortions, and “abortion has been deemed contrary to sound medicine for thousands of years” (citing the Hippocratic oath).13 The brief was not cited by the Court.
Many other medical and pro-life medical groups presented amicus briefs. A list of and links to all the briefs is available on the SCOTUSblog website at https://www.scotusblog.com/case-files/cases/dobbs-v-jackson-womens-health-organization/.
Ramifications
The Court decision does not make abortion illegal but allows states (and possibly Congress) to decide whether, when, and how abortions may be performed. Some states may ban most abortions (making it illegal to have or to perform abortions). Thirteen states had “trigger laws” to go into effect limiting abortion if the Court permitted such limitations. Most of those states were almost immediately entangled in lawsuits challenging the state laws. Some states, for example, have privacy provisions in their state constitution that state courts could interpret as allowing abortion, thereby voiding the state statutes prohibiting abortion.
At least a few states have abortion laws still on the books that were passed decades ago (perhaps before Roe) and were never repealed. Those laws may once again be valid, although state courts might hold that those statutes were repealed by Roe and must be passed again to be valid. Some experts anticipate that 28 states will eventually have significant limitations on abortion.
The Guttmacher Institute maintains a frequently updated table on the abortion laws in each state.14 According to one estimate, 29 states are hostile to abortion rights (or lean that way), with about 40 million women aged 13 to 44 (58% of the United States) living in states with some hostility to abortion.15 Congress may pass some national abortion laws, but that seems unlikely and there may be some limits on its ability to control private medical practice within states.
An additional legal issue will arise from medication-induced abortions, generally through the use of mifepristone and misoprostol. They now account for the majority of abortions. These medications might be used for abortion, up to about 9 weeks of pregnancy, in states prohibiting abortion. The drugs once were available only with an in-person visit, but now the US Food and Drug Administration (FDA) permits mail-order delivery. The potential exists, therefore, to circumvent states’ prohibition on abortion through mail-order postal shipments. The FDA controls the licensing of pharmaceuticals in interstate commerce, but not the practice of medicine within a state. Therefore the ability of individuals (within a state) to possess or use drugs is unclear.
The abortion wars of the last 50 years gave rise to state laws related to abortion, including consent by minors, information to parents, special informed consent, and facilities requirements. If these laws were once struck down because they were inconsistent with Roe, but were never formally repealed, they may now become legal requirements.
In the foreseeable future, abortion laws generally will not be determined by federal courts but by state law, generally legislatures. In legislative hearings, town hall meetings, and conversations with lawmakers, ObGyns should engage the topic of abortion with scientific expertise, reason, openness, and humility. It will be impossible for the profession to speak with a single voice, as the briefs filed this Term demonstrate. Where there are honest differences in science, the reasons for the different interpretations should be explainable to lay decision makers. The profession, who are not being pseudo-lobbyists, can contribute a great deal to the rational consideration of this emotional topic.
On January 27, 2022, Justice Stephen Breyer informed President Biden of his intention to retire from the Court at the end of the Term. At age 84, he was the oldest member of the Court, but he continued to be among the most active of the justices and seemed to relish the work of the Court. He had been under pressure from liberal groups to retire earlier so a successor could be confirmed by a Democratic Senate. In many ways he was the Renaissance man of the Court: he spoke fluent French, wrote books, and famously sprinkled his questions with complex and funny hypotheticals.
Justice Breyer was a law professor before becoming a judge and enjoyed presentations to many groups, from children to law professors. He loved the Court and defended it—most recently against partisan attacks from both the right and the left. In the decisions of the Court, he was one of the more liberal justices. He had, for example, indicated that the death penalty is unconstitutional.
In his January retirement letter, he said that he would step down at the end of the Term if his replacement had been appointed and confirmed. She had. The new justice had clerked for Justice Breyer in 1999–2000.
Ketanji Brown Jackson was nominated by President Biden on February 28, confirmed by the Senate on April 7 by a 53–47 margin, and sworn in on June 30, 2022. Justice Jackson had previously been a federal district court judge and on the Court of Appeals for the D.C. Circuit. She attended Harvard-Radcliffe College and received her law degree from Harvard Law School. She worked as a criminal defense attorney and was active in the US Sentencing Commission.
Continue to: What is a practitioner to do?...
What is a practitioner to do?
For many practitioners, the Dobbs decision will have little effect because their state laws are consistent with Roe, and the legislature is not going to change the law. They may, of course, see an influx of patients from other states (that restrict abortion) seeking treatment. At the other extreme, in some states, most abortions will become prohibited. State courts may ease the restrictions. In many states, there will be an ongoing battle over when abortion is legal and when it is not, resulting in shifting laws and regulations. Keeping up with the shifts that affect practice will be a challenge.
All states are likely to permit abortions “to save the life of the mother,” and many will have a version of “to preserve the health of the mother.” Other exceptions may be for pregnancy resulting from rape or incest or in the case of serious fetal abnormality. ObGyns, of course, will be called on to certify that one of these exceptions exists. Determining that pregnancy resulted from rape or incest, of course, can be challenging. Before Roe, there was a cottage industry opining that pregnancy seriously affected the health of the mother, which often involved physical manifestations of mental health. ObGyns in some states may be asked once again to make such determinations.
Laws not directly related to abortions will, in some states, be changed as a way of discouraging abortion. For example, child abuse reporting laws may be modified to require reporting of any known or suspected abortion or attempted abortion, and medical licensing standards may make it a violation to participate in or facilitate abortion in any way.
Particularly in states where the rules keep shifting, practitioners must keep up with the current law. Professional organizations can help with that, but there is no substitute for practitioners having an ongoing professional relationship with an attorney who has expertise in health law.
Other abortion decisions this Term
In other abortion decisions this Term, the Court refused to suspend a Texas law that prohibited abortions after a fetal heartbeat could be detected.16 The law has remarkable enforcement mechanisms that preclude state officers from enforcing it; instead, it creates what amounts to a private attorney general (PAG) provision that allows private citizens to file suit against anyone performing or assisting in performing abortions. This PAG made pre-enforcement challenges to the law difficult.17
In a Kentucky case, the Court allowed the Kentucky attorney general to intervene in a case that challenged a Kentucky law that prohibits physicians from using dilation and evacuation procedures to end second-trimester pregnancies.18
Criminal convictions for physicians’ overprescription of controlled substances
Perhaps the least sympathetic of the physicians involved with the Court this Term were the 2 in Ruan v U.S.19 Their trials indicate that Dr. Ruan’s clinic issued more than 300,000 controlled substance prescriptions over 4 years and was one of the most frequent prescribers of fentanyl. Dr. Kahn prescribed controlled substances without an examination, falsified notes, and sold controlled substances for cash and guns.20
Both physicians were convicted of “knowingly or intentionally” dispensing a controlled substance without authorization.21 They were authorized to prescribe drugs, but only “for a legitimate medical purpose.”22 Appeals to their respective Circuit courts confirmed their convictions. The Supreme Court, however, held that to convict them, the government must prove that they knowingly or intentionally acted in an unauthorized manner. That proof can be by circumstantial evidence, but it must be beyond a reasonable doubt.
Health care reimbursement
Hospitals won one and lost one Medicare-Medicaid reimbursement case that involved payments for low-income patients.
In the loss, the Court held that the US Department of Health and Human Services (HHS) properly calculated the disproportionate share adjustments (DSH), or Medicare fraction,23 that provides a supplemental payment for hospitals with a large proportion of low-income patients. The lower DSH payments calculated by HHS were upheld, thereby reducing the number of hospitals receiving DSH payments and decreasing the amounts others will receive.
The win involved payments for prescription drugs that hospitals provide to outpatients in safety-net hospitals.24 HHS determined that it was overpaying hospitals for drugs and cut the reimbursement rate. The Court held that before HHS can change the drug rate, it must conduct a survey of hospitals regarding actual costs. It had not done that, so the rate reduction was not permitted by the law.
An accidental disincentive to (some) malpractice suits
Medicaid requires states to obtain part of a tort recovery that recipients obtain if Medicaid is covering medical expenses related to their injuries. In implementing that law, a state may provide a disincentive for injured beneficiaries to file malpractice cases. At issue was a Florida law that provided the Medicaid state would take 37.5% of the beneficiary’s total tort recovery (being one-half of the recovery after deducting 25% for attorney’s fees and costs). In a 7-2 decision, the Court upheld the Florida law.25
The disincentive to filing a lawsuit is that the state is taking 37.5%, plus contingency fee attorneys will typically take 33.3% (and there will be some fees). This is especially true when there is a state cap on noneconomic damages. In the case the Court decided, the plaintiff received a settlement of $850,000. If we assume a typical contingency fee, less the state’s Medicaid claim of $300,000, the plaintiff possibly received $266,667. That is not trivial, but it is only 31% of the settlement.
The Medicaid expectation of reimbursement and the Florida approach, however, impose heavy burdens on severely injured beneficiaries. The plaintiff had catastrophic injuries and was in a vegetative state. There are some things Medicaid does not pay for, as well as nonmedical expenses. The amount left for such expenses is likely well below what the family will need.
Continue to: COVID-19 vaccinations...
COVID-19 vaccinations
Had it not been for the abortion decisions, 2021–2022 might have been “the COVID Term.” Two of the most anticipated decisions involved mandatory vaccinations (or masking/testing instead). The question in each of these cases was whether Congress had authorized 2 federal agencies to issue the emergency regulations requiring vaccination. Emergency regulations are held to higher standards because they bypass the usual protections of the Administrative Procedure Act.
One case involved a regulation issued by the Occupational Safety and Health Administration (OSHA) that employers (with more than 100 employees) must require their employees to be vaccinated. In a 6-3 decision, the Court held that OSHA did not have the authority to enforce this as an emergency regulation. The other case was a regulation issued by HHS that health care institutions receiving Medicare and Medicaid funding must require all staff to be vaccinated.26 In a 5-4 decision, the Court upheld this emergency regulation because of the very broad authority Congress had given HHS to ensure the safety of patients and the quality of Medicare- and Medicaid-funded programs.27
In another case, in the shadow docket (orders and opinions in cases without full arguments), the Court struck down the Centers for Disease Control and Prevention’s eviction moratorium.28 The Court said the government claimed “a breathtaking amount of authority” that Congress did not intend. In other shadow docket cases, the Court refused to hold unconstitutional state laws that require COVID-19 vaccination but did not have religious exemptions.29
Analysis of this Term
It was an extraordinary Term. The Court decided 66 cases (excluding most cases in the shadow docket), a low number historically. Not only were there many seminal cases but also the Court appears to be shifting toward a new direction. That direction may be oriented more toward the original understanding of the words of the Constitution and statutes and less toward policy; Congress rather than administrative agencies; racial nondiscrimination rather than preferences; and the free exercise rather than the establishment of religion. Whether there is such a shift or not, of course, only time will tell.
Chief Justice Roberts and Justice Kavanaugh were in the majority most often (95% of the cases), followed by Justices Barrett (90%), Alito (85%), Thomas (80%), and Gorsuch (75%). Justices Kagan (69%) and Breyer (68%) were not far behind. Justice Sotomayor was in the majority 58%. The Court was unanimous 29% of the time, well below the decade average (43%), and 6-3 accounted for 30% of the decisions.
A major, potentially scarring, event this Term was the leak of an early draft of the majority opinion in Dobbs. Although leaks have occurred before, the early leak of an opinion was unprecedented. It will almost inevitably change the openness and candor within the Court and the justices’ clerks. Although not unprecedented, the attempt on the life of Justice Kavanaugh and the organized efforts to harass some justices in their homes are likely to have lasting impact. Almost certainly it means that justices and their families will have constant security and their movements and connection with the general public will become less frequent, which is sad for the justices and our democracy.
Looking toward the next Term
When the Court next convenes, Justice Ketanji Brown Jackson will take her seat on the left end of the Court (the traditional seat for a new justice, not a commentary on judicial philosophy). The Court has already taken many cases, including issues about university affirmative action programs, web designers and same-sex couples, redistricting and voting rights, DNA testing in criminal cases, and overtime pay for someone making over $200,000 per year. It begins Monday, October 3, and promises to be another interesting Term. ●
The 2021–2022 US Supreme Court Term was a blockbuster medical Term. The bookends of the Term were COVID-19 vaccinations and abortion rights. Between the bookends were Medicare reimbursement, criminal liability for prescribing controlled substances, gun control, and carbon dioxide emissions. In this article, we focus on the significant medical issues, briefly note other important decisions, and consider the implications of this Term.
Abortion decisions
Dobbs v Jackson Women’s Health Organization1 was the most controversial decision and, for ObGyns, perhaps the most important decision in decades. The basic holding of the case can be stated simply: Roe v Wade2 and Planned Parenthood of Southeastern Pennsylvania v Casey3 (which essentially created a constitutional right to abortion) are overruled. The law related to abortion is for the states and Congress to determine, not federal courts. (For a review of earlier reproductive freedom cases in the Court, see our previous article, “The Supreme Court and reproductive rights.”4)
Dobbs arose from a Mississippi statute that made it illegal to perform abortions after 15 weeks of gestation, well before viability. Six members of the Court held that the Mississippi law was constitutional and 3 would have struck down the state law. There were 5 opinions, covering a total of 213 pages in the U.S. Reports. The Court fell into 4 camps, ranging from the most to the least protective of abortion rights, as follows:
- Three justices (Breyer, Kagan, and Sotomayor) voted to strike down the Mississippi statute and uphold Roe and Casey and wrote a joint dissent. They believe the Constitution makes abortion an issue “off limits to majority rule.” They also warned that other areas of “substantive due process” (discussed below), including contraception and same-sex marriage, might be under threat.
- The Chief Justice voted to uphold the statute but wanted an incremental approach; that is, not to overturn Roe and Casey entirely in this case because the Dobbs case required the Court only to determine the more limited question of whether the 15-week limit on abortion was constitutional. He found that the viability standard did not make sense, but he suggested that the Court “leave for another day” whether to overturn Roe.
- Five justices joined the opinion to uphold the statute and overturn Roe. Justice Alito wrote the decision joined by Justices Thomas, Kavanaugh, Gorsuch, and Barrett. They found that a right to abortion was not “deeply rooted in our Nation’s history,” as evidenced by the fact that when the 14th Amendment was adopted, abortion was a criminal offense in most states and not a protected right in any state. In 2 lengthy appendices, the Court reviewed the criminalization of abortion in the states in 1868 and in the territories that later became states. Even when Roe was decided in 1973, abortion was not “deeply rooted” because it was not generally legal in the states. Justice Kavanaugh joined this opinion and wrote separately to emphasize that the majority opinion does not outlaw abortion, but rather leaves the issue to “the people and their representatives.” He also emphasized that the case did not overturn all of the substantive due process cases.
- Justice Thomas would have gone further and abandoned “substantive due process” completely.
The constitutional issue
The majority said that the issue before the Court was not whether the law should permit or prohibit abortions—that is a question for the political branches. Rather, the question was only whether the Constitution precludes the political branches from allowing abortions. There is no mention of abortion in the Constitution and no specific reference to a right to privacy that includes medical decisions. A central constitutional question has been to identify where exactly in the Constitution the right to privacy resides. The Court has generally used “substantive due process” to locate privacy rights. The 14th Amendment provides, in part, that no state may “deprive any person of life, liberty, or property, without due process of law.” “Process” generally refers to procedural protections, but the Court sometimes has used it to encompass substantive rights (for example, privacy)—hence, “substantive due process.”
Over the decades, the legitimacy of substantive due process has remained controversial. Justice Thomas called it an “oxymoron” to turn “process” into substantive rights. And its use has a somewhat checkered history. For nearly 50 years (1890–1937), it was used to preclude states from protecting employees (for example, hour and wage laws violated “the right to contract”) and was discredited. More recently the Court has used substantive due process to protect contraception access, abortion, and same-sex marriages.
A critical question is knowing what rights substantive due process protects. The Court sometimes has said that it protects rights “deeply rooted in the Nation’s history and traditions” and “implicit in the concept of ordered liberty,”5 although in other cases suggested a more ambiguous definition.6 The next constitutional question is how to state or define the right to be protected. For example, is it the right to intimately personal decisions, bodily integrity, reproductive choice, abortion, or late-term abortion? Some of those may be deeply rooted in history and traditions (intimate decisions), and others not so much (late-term abortion). Finally, a question is whether a substantive right is defined at the time the 14th Amendment was adopted (1868) or now—is it a “living Constitution” that, without much guidance, means whatever 5 justices believe at the moment, or is it a Constitution grounded in the distant past?
The future of substantive due process is uncertain following Dobbs. Although the majority said it was not disclaiming substantive due process, the dissent said it doubted that claim because other rights are “part of the same constitutional fabric” (substantive due process). The Court might, in future cases, find some other constitutional provision in which to ground rights. The source of those rights might be the 9th Amendment (in addition to the Constitution’s enumerated rights, there are “others retained by the people”) or another provision of the 14th (“No State shall make or enforce any law which shall abridge the privileges or immunities of citizens of the United States…”). Each of these possibilities has its problems, many of which are similar to substantive due process, but they avoid the “oxymoron” issue.
Among the other important cases this Term, the Court made these determinations:
- Held that the 2nd Amendment, as applied to the states through the 14th Amendment, includes a general right to carry a gun for self-defense outside the home.1 It struck down a New York law that required people to show a special need to have and carry a gun.
- Determined that the US Environmental Protection Agency exceeded the authority Congress had granted it with a “Clean Power Plan” that was intended to reduce carbon dioxide emissions.2 It is up to Congress, not the agency, to expand agency authority.
- Gave trial courts discretion in determining whether (and under what conditions) children in international custody disputes must be returned to their home countries where there is a serious risk of harm to them.3
- Held that there is an implied right of action to sue medical providers for disability discrimination, but under the Rehabilitation Act and the Affordable Care Act the damages do not include emotional harm.4
- Decided several “free exercise of religion” cases, and in each found the state had violated religious rights, holding that: A state improperly prevented religious schools from being eligible for a state tuition grant system,5 a coach was wrongfully fired for kneeling in prayer following football games,6 Boston denied free speech in allowing other organizations to fly their flags but denying a Christian flag to be displayed,7 and a state must permit prisoners to have a spiritual advisor to be present and pray and touch them during their execution.8
- Held that the administration’s rescission of the “stay in Mexico” immigration policy was permitted by existing statutes.9
References
1. New York State Rifle & Pistol Association, Inc. v Bruen, 20-843, decided June 23, 2022. https://www.supremecourt.gov/opinions/21pdf/20-843_7j80.pdf
2. West Virginia v Environmental Protection Agency, 20-1530, decided June 30, 2022. https://www.supremecourt.gov/opinions/21pdf/20-1530_new_l537.pdf
3. Golan v Saada, 20-1034, decided June 15, 2022. https://www.supremecourt.gov/opinions/21pdf/20-1034_b8dg.pdf
4. Cummings v Premier Rehab Keller, 20-219, decided April 28, 2022. https://www.supremecourt.gov/opinions/21pdf/20-219_1b82.pdf
5. Carson v Makin, 20-1088, decided June 21, 2022. https://www.supremecourt.gov/opinions/21pdf/20-1088_dbfi.pdf
6. Kennedy v Bremerton School District., 21-418, decided June 27, 2022. https://www.supremecourt.gov/opinions/21pdf/21-418_new_onkq.pdf
7. Shurtleff v Boston, 20-1800, decided May 2, 2022. https://www.supremecourt.gov/opinions/21pdf/20-1800_7lho.pdf
8. Ramirez v Collier, 21-5592, decided March 24, 2022. https://www.supremecourt.gov/opinions/21pdf/21-5592_feah.pdf
9. Biden v Texas, 21-9 54, decided June 30, 2022. https://www.supremecourt.gov/opinions/21pdf/21-954_7l48.pdf
Continue to: ObGyn briefs in the case...
ObGyn briefs in the case
The medical profession filed several amicus curiae briefs in the Dobbs case. (These are “friends of the court” briefs filed by nonparties to the litigation. The purpose is to give a court a perspective on the case not presented by the parties.) The American College of Obstetricians and Gynecologists (ACOG) took the lead in filing an amicus brief.7 Nearly 2 dozen other medical organizations joined the brief, including the American Academy of Pediatrics, American College of Osteopathic Obstetricians and Gynecologists, American Gynecological and Obstetrical Society, American Society for Reproductive Medicine, Council of University Chairs of Obstetrics and Gynecology, North American Society for Pediatric and Adolescent Gynecology, Society for Academic Specialists in General Obstetrics and Gynecology, Society of Gynecologic Oncology, and Society of OB/GYN Hospitalists.
The brief argued that abortion is a safe procedure, an abortion ban would harm the health of pregnant patients, and it would undermine the physician-patient relationship and interfere with patient autonomy. It also discussed the issue of fetal pain,8 telling the Court that “Every major medical organization that has examined the issue of fetal pain and peer-reviewed studies on the matter have consistently concluded that pre-viability abortion does not result in fetal pain perception.”9 The brief was cited in the dissent for the fact that “About 18 percent of pregnancies in this country end in abortion, and about one-quarter of American women will have an abortion before the age of 45.”10
The Court received a different view from an amicus brief filed by the American Association of Pro-Life Obstetricians and Gynecologists.11 It told the Court that abortion, especially later-term, poses health risks: the abortion process itself may injure the woman, abortion puts women at risk for future preterm births, later-term abortion raises a woman’s risk of developing breast cancer, and abortions (especially those later in the pregnancy) are linked to a greater risk of psychological harm.12 The brief also noted that 93% of obstetrician-gynecologists do not perform abortions, and “abortion has been deemed contrary to sound medicine for thousands of years” (citing the Hippocratic oath).13 The brief was not cited by the Court.
Many other medical and pro-life medical groups presented amicus briefs. A list of and links to all the briefs is available on the SCOTUSblog website at https://www.scotusblog.com/case-files/cases/dobbs-v-jackson-womens-health-organization/.
Ramifications
The Court decision does not make abortion illegal but allows states (and possibly Congress) to decide whether, when, and how abortions may be performed. Some states may ban most abortions (making it illegal to have or to perform abortions). Thirteen states had “trigger laws” to go into effect limiting abortion if the Court permitted such limitations. Most of those states were almost immediately entangled in lawsuits challenging the state laws. Some states, for example, have privacy provisions in their state constitution that state courts could interpret as allowing abortion, thereby voiding the state statutes prohibiting abortion.
At least a few states have abortion laws still on the books that were passed decades ago (perhaps before Roe) and were never repealed. Those laws may once again be valid, although state courts might hold that those statutes were repealed by Roe and must be passed again to be valid. Some experts anticipate that 28 states will eventually have significant limitations on abortion.
The Guttmacher Institute maintains a frequently updated table on the abortion laws in each state.14 According to one estimate, 29 states are hostile to abortion rights (or lean that way), with about 40 million women aged 13 to 44 (58% of the United States) living in states with some hostility to abortion.15 Congress may pass some national abortion laws, but that seems unlikely and there may be some limits on its ability to control private medical practice within states.
An additional legal issue will arise from medication-induced abortions, generally through the use of mifepristone and misoprostol. They now account for the majority of abortions. These medications might be used for abortion, up to about 9 weeks of pregnancy, in states prohibiting abortion. The drugs once were available only with an in-person visit, but now the US Food and Drug Administration (FDA) permits mail-order delivery. The potential exists, therefore, to circumvent states’ prohibition on abortion through mail-order postal shipments. The FDA controls the licensing of pharmaceuticals in interstate commerce, but not the practice of medicine within a state. Therefore the ability of individuals (within a state) to possess or use drugs is unclear.
The abortion wars of the last 50 years gave rise to state laws related to abortion, including consent by minors, information to parents, special informed consent, and facilities requirements. If these laws were once struck down because they were inconsistent with Roe, but were never formally repealed, they may now become legal requirements.
In the foreseeable future, abortion laws generally will not be determined by federal courts but by state law, generally legislatures. In legislative hearings, town hall meetings, and conversations with lawmakers, ObGyns should engage the topic of abortion with scientific expertise, reason, openness, and humility. It will be impossible for the profession to speak with a single voice, as the briefs filed this Term demonstrate. Where there are honest differences in science, the reasons for the different interpretations should be explainable to lay decision makers. The profession, who are not being pseudo-lobbyists, can contribute a great deal to the rational consideration of this emotional topic.
On January 27, 2022, Justice Stephen Breyer informed President Biden of his intention to retire from the Court at the end of the Term. At age 84, he was the oldest member of the Court, but he continued to be among the most active of the justices and seemed to relish the work of the Court. He had been under pressure from liberal groups to retire earlier so a successor could be confirmed by a Democratic Senate. In many ways he was the Renaissance man of the Court: he spoke fluent French, wrote books, and famously sprinkled his questions with complex and funny hypotheticals.
Justice Breyer was a law professor before becoming a judge and enjoyed presentations to many groups, from children to law professors. He loved the Court and defended it—most recently against partisan attacks from both the right and the left. In the decisions of the Court, he was one of the more liberal justices. He had, for example, indicated that the death penalty is unconstitutional.
In his January retirement letter, he said that he would step down at the end of the Term if his replacement had been appointed and confirmed. She had. The new justice had clerked for Justice Breyer in 1999–2000.
Ketanji Brown Jackson was nominated by President Biden on February 28, confirmed by the Senate on April 7 by a 53–47 margin, and sworn in on June 30, 2022. Justice Jackson had previously been a federal district court judge and on the Court of Appeals for the D.C. Circuit. She attended Harvard-Radcliffe College and received her law degree from Harvard Law School. She worked as a criminal defense attorney and was active in the US Sentencing Commission.
Continue to: What is a practitioner to do?...
What is a practitioner to do?
For many practitioners, the Dobbs decision will have little effect because their state laws are consistent with Roe, and the legislature is not going to change the law. They may, of course, see an influx of patients from other states (that restrict abortion) seeking treatment. At the other extreme, in some states, most abortions will become prohibited. State courts may ease the restrictions. In many states, there will be an ongoing battle over when abortion is legal and when it is not, resulting in shifting laws and regulations. Keeping up with the shifts that affect practice will be a challenge.
All states are likely to permit abortions “to save the life of the mother,” and many will have a version of “to preserve the health of the mother.” Other exceptions may be for pregnancy resulting from rape or incest or in the case of serious fetal abnormality. ObGyns, of course, will be called on to certify that one of these exceptions exists. Determining that pregnancy resulted from rape or incest, of course, can be challenging. Before Roe, there was a cottage industry opining that pregnancy seriously affected the health of the mother, which often involved physical manifestations of mental health. ObGyns in some states may be asked once again to make such determinations.
Laws not directly related to abortions will, in some states, be changed as a way of discouraging abortion. For example, child abuse reporting laws may be modified to require reporting of any known or suspected abortion or attempted abortion, and medical licensing standards may make it a violation to participate in or facilitate abortion in any way.
Particularly in states where the rules keep shifting, practitioners must keep up with the current law. Professional organizations can help with that, but there is no substitute for practitioners having an ongoing professional relationship with an attorney who has expertise in health law.
Other abortion decisions this Term
In other abortion decisions this Term, the Court refused to suspend a Texas law that prohibited abortions after a fetal heartbeat could be detected.16 The law has remarkable enforcement mechanisms that preclude state officers from enforcing it; instead, it creates what amounts to a private attorney general (PAG) provision that allows private citizens to file suit against anyone performing or assisting in performing abortions. This PAG made pre-enforcement challenges to the law difficult.17
In a Kentucky case, the Court allowed the Kentucky attorney general to intervene in a case that challenged a Kentucky law that prohibits physicians from using dilation and evacuation procedures to end second-trimester pregnancies.18
Criminal convictions for physicians’ overprescription of controlled substances
Perhaps the least sympathetic of the physicians involved with the Court this Term were the 2 in Ruan v U.S.19 Their trials indicate that Dr. Ruan’s clinic issued more than 300,000 controlled substance prescriptions over 4 years and was one of the most frequent prescribers of fentanyl. Dr. Kahn prescribed controlled substances without an examination, falsified notes, and sold controlled substances for cash and guns.20
Both physicians were convicted of “knowingly or intentionally” dispensing a controlled substance without authorization.21 They were authorized to prescribe drugs, but only “for a legitimate medical purpose.”22 Appeals to their respective Circuit courts confirmed their convictions. The Supreme Court, however, held that to convict them, the government must prove that they knowingly or intentionally acted in an unauthorized manner. That proof can be by circumstantial evidence, but it must be beyond a reasonable doubt.
Health care reimbursement
Hospitals won one and lost one Medicare-Medicaid reimbursement case that involved payments for low-income patients.
In the loss, the Court held that the US Department of Health and Human Services (HHS) properly calculated the disproportionate share adjustments (DSH), or Medicare fraction,23 that provides a supplemental payment for hospitals with a large proportion of low-income patients. The lower DSH payments calculated by HHS were upheld, thereby reducing the number of hospitals receiving DSH payments and decreasing the amounts others will receive.
The win involved payments for prescription drugs that hospitals provide to outpatients in safety-net hospitals.24 HHS determined that it was overpaying hospitals for drugs and cut the reimbursement rate. The Court held that before HHS can change the drug rate, it must conduct a survey of hospitals regarding actual costs. It had not done that, so the rate reduction was not permitted by the law.
An accidental disincentive to (some) malpractice suits
Medicaid requires states to obtain part of a tort recovery that recipients obtain if Medicaid is covering medical expenses related to their injuries. In implementing that law, a state may provide a disincentive for injured beneficiaries to file malpractice cases. At issue was a Florida law that provided the Medicaid state would take 37.5% of the beneficiary’s total tort recovery (being one-half of the recovery after deducting 25% for attorney’s fees and costs). In a 7-2 decision, the Court upheld the Florida law.25
The disincentive to filing a lawsuit is that the state is taking 37.5%, plus contingency fee attorneys will typically take 33.3% (and there will be some fees). This is especially true when there is a state cap on noneconomic damages. In the case the Court decided, the plaintiff received a settlement of $850,000. If we assume a typical contingency fee, less the state’s Medicaid claim of $300,000, the plaintiff possibly received $266,667. That is not trivial, but it is only 31% of the settlement.
The Medicaid expectation of reimbursement and the Florida approach, however, impose heavy burdens on severely injured beneficiaries. The plaintiff had catastrophic injuries and was in a vegetative state. There are some things Medicaid does not pay for, as well as nonmedical expenses. The amount left for such expenses is likely well below what the family will need.
Continue to: COVID-19 vaccinations...
COVID-19 vaccinations
Had it not been for the abortion decisions, 2021–2022 might have been “the COVID Term.” Two of the most anticipated decisions involved mandatory vaccinations (or masking/testing instead). The question in each of these cases was whether Congress had authorized 2 federal agencies to issue the emergency regulations requiring vaccination. Emergency regulations are held to higher standards because they bypass the usual protections of the Administrative Procedure Act.
One case involved a regulation issued by the Occupational Safety and Health Administration (OSHA) that employers (with more than 100 employees) must require their employees to be vaccinated. In a 6-3 decision, the Court held that OSHA did not have the authority to enforce this as an emergency regulation. The other case was a regulation issued by HHS that health care institutions receiving Medicare and Medicaid funding must require all staff to be vaccinated.26 In a 5-4 decision, the Court upheld this emergency regulation because of the very broad authority Congress had given HHS to ensure the safety of patients and the quality of Medicare- and Medicaid-funded programs.27
In another case, in the shadow docket (orders and opinions in cases without full arguments), the Court struck down the Centers for Disease Control and Prevention’s eviction moratorium.28 The Court said the government claimed “a breathtaking amount of authority” that Congress did not intend. In other shadow docket cases, the Court refused to hold unconstitutional state laws that require COVID-19 vaccination but did not have religious exemptions.29
Analysis of this Term
It was an extraordinary Term. The Court decided 66 cases (excluding most cases in the shadow docket), a low number historically. Not only were there many seminal cases but also the Court appears to be shifting toward a new direction. That direction may be oriented more toward the original understanding of the words of the Constitution and statutes and less toward policy; Congress rather than administrative agencies; racial nondiscrimination rather than preferences; and the free exercise rather than the establishment of religion. Whether there is such a shift or not, of course, only time will tell.
Chief Justice Roberts and Justice Kavanaugh were in the majority most often (95% of the cases), followed by Justices Barrett (90%), Alito (85%), Thomas (80%), and Gorsuch (75%). Justices Kagan (69%) and Breyer (68%) were not far behind. Justice Sotomayor was in the majority 58%. The Court was unanimous 29% of the time, well below the decade average (43%), and 6-3 accounted for 30% of the decisions.
A major, potentially scarring, event this Term was the leak of an early draft of the majority opinion in Dobbs. Although leaks have occurred before, the early leak of an opinion was unprecedented. It will almost inevitably change the openness and candor within the Court and the justices’ clerks. Although not unprecedented, the attempt on the life of Justice Kavanaugh and the organized efforts to harass some justices in their homes are likely to have lasting impact. Almost certainly it means that justices and their families will have constant security and their movements and connection with the general public will become less frequent, which is sad for the justices and our democracy.
Looking toward the next Term
When the Court next convenes, Justice Ketanji Brown Jackson will take her seat on the left end of the Court (the traditional seat for a new justice, not a commentary on judicial philosophy). The Court has already taken many cases, including issues about university affirmative action programs, web designers and same-sex couples, redistricting and voting rights, DNA testing in criminal cases, and overtime pay for someone making over $200,000 per year. It begins Monday, October 3, and promises to be another interesting Term. ●
- Dobbs v Jackson Women’s Health Organization, 19-1392, decided June 24, 2022. https://www.supremecourt.gov /opinions/21pdf/19-1392_6j37.pdf
- Roe v Wade, 410 U.S. 113, 163 (1973).
- Planned Parenthood of Southeastern Pennsylvania v Casey, 505 U.S. 833 (1992).
- Smith SR, Sanfilippo JR. The Supreme Court and reproductive rights. OBG Manag. 2022;34(1):36-41, 46. https://cdn.mdedge. com/files/s3fs-public/issues/articles/obgm0340136_smith.pdf
- Washington v Glucksberg, 521 U.S. 702 (1997).
- Obergefell v Hodges, 576 U.S. 644, 654-70 (2015).
- Brief of amici curiae of American College of Obstetricians and Gynecologists, American Medical Association, et al, in Dobbs v Jackson Women’s Health Organization, in Support of Respondents (Sep. 2021). https://www.supremecourt .gov/DocketPDF/19/19-1392/193074/20210920174518042 _19-1392%20bsacACOGetal.pdf
- Id. at 8, 13-15.
- Id. at 14.
- Justices Breyer, Kagan, and Sotomayor, dissenting, at 48, note 22.
- Brief for American Association of Pro-Life Obstetricians And Gynecologists as Amicus Curiae, in Dobbs v Jackson Women’s Health Organization, in Support of Petitioners (July 2021). https://www.supremecourt.gov /DocketPDF/19/19-1392/185350/20210729163532595_No. %2019-1392%20-%20American%20Association%20of%20 Pro-Life%20Obstetricians%20and%20Gynecologists%20-%20 Amicus%20Brief%20in%20Support%20of%20Petitioner%20-%20 7-29-21.pdf
- Id. at 3-4, 7-29.
- Id. at 30.
- Guttmacher Institute. An overview of abortion laws. July 11, 2022. https://www.guttmacher.org/state-policy/explore/overview -abortion-laws
- Guttmacher Institute. State abortion policy landscape: from hostile to supportive. Dec. 2020. https://www .guttmacher.org/article/2019/08/state-abortion-policy -landscape-hostile-supportive
- Whole Woman’s Health v Jackson, 21-463, decided Dec. 10, 2021. https://www.supremecourt.gov/opinions/21pdf/21-463_ new_8o6b.pdf
- United States v Texas, 21-588, decided Dec. 10, 2021. (Per curiam, Sotomayor dissenting). https://www.supremecourt.gov /opinions/21pdf/21-588_c07d.pdf
- Cameron v EMW Women’s Surgical Center, 20-601, decided Mar. 3, 2022. https://www.supremecourt.gov/opinions/21pdf/20-601 _new_g20h.pdf
- Xiulu Ruan v United States, 20-1410, decided June 27, 2022. https:// www.supremecourt.gov/opinions/21pdf/20-1410_1an2.pdf
- Adam Liptak. Supreme Court sides with doctors accused of running pill mills. The New York Times. June 27, 2022. https://www .nytimes.com/2022/06/27/us/politics/supreme-court-controlled -substance-act.html
- 84 Stat. 1260, 21 U.S.C. §841(a).
- 21 CFR §1306.04(a) (2021).
- Becerra v Empire Health Foundation, For Valley Hospital Medical Center, 20-1312, decided June 24, 2022. https://www.supremecourt .gov/opinions/21pdf/20-1312_j42l.pdf
- American Hospital Association v Becerra, 20-1114, decided June 15, 2022. https://www.supremecourt.gov/opinions/21pdf/20 -1114_09m1.pdf
- Gallardo v Marstiller, 20-1263, decided June 6, 2022. https:// www.supremecourt.gov/opinions/21pdf/20-1263_new_hfci.pdf
- National Federation of Independent Business v Department of Labor, Occupational Safety and Health Administration, 21A244, decided Jan. 13, 2022. https://www.supremecourt.gov /opinions/21pdf/21a244_hgci.pdf
- Biden v Missouri, 21A240, decided Jan. 13, 2022. https://www .supremecourt.gov/opinions/21pdf/21a240_d18e.pdf
- Alabama Association of Realtors v Department of Health and Human Services, 21A23, decided Aug. 26, 2021. https://www .supremecourt.gov/opinions/20pdf/21a23_ap6c.pdf
- Does v Mills, 21A90, decided Oct. 29, 2021. https://www .supremecourt.gov/opinions/21pdf/21a90_6j37.pdf
- Dobbs v Jackson Women’s Health Organization, 19-1392, decided June 24, 2022. https://www.supremecourt.gov /opinions/21pdf/19-1392_6j37.pdf
- Roe v Wade, 410 U.S. 113, 163 (1973).
- Planned Parenthood of Southeastern Pennsylvania v Casey, 505 U.S. 833 (1992).
- Smith SR, Sanfilippo JR. The Supreme Court and reproductive rights. OBG Manag. 2022;34(1):36-41, 46. https://cdn.mdedge. com/files/s3fs-public/issues/articles/obgm0340136_smith.pdf
- Washington v Glucksberg, 521 U.S. 702 (1997).
- Obergefell v Hodges, 576 U.S. 644, 654-70 (2015).
- Brief of amici curiae of American College of Obstetricians and Gynecologists, American Medical Association, et al, in Dobbs v Jackson Women’s Health Organization, in Support of Respondents (Sep. 2021). https://www.supremecourt .gov/DocketPDF/19/19-1392/193074/20210920174518042 _19-1392%20bsacACOGetal.pdf
- Id. at 8, 13-15.
- Id. at 14.
- Justices Breyer, Kagan, and Sotomayor, dissenting, at 48, note 22.
- Brief for American Association of Pro-Life Obstetricians And Gynecologists as Amicus Curiae, in Dobbs v Jackson Women’s Health Organization, in Support of Petitioners (July 2021). https://www.supremecourt.gov /DocketPDF/19/19-1392/185350/20210729163532595_No. %2019-1392%20-%20American%20Association%20of%20 Pro-Life%20Obstetricians%20and%20Gynecologists%20-%20 Amicus%20Brief%20in%20Support%20of%20Petitioner%20-%20 7-29-21.pdf
- Id. at 3-4, 7-29.
- Id. at 30.
- Guttmacher Institute. An overview of abortion laws. July 11, 2022. https://www.guttmacher.org/state-policy/explore/overview -abortion-laws
- Guttmacher Institute. State abortion policy landscape: from hostile to supportive. Dec. 2020. https://www .guttmacher.org/article/2019/08/state-abortion-policy -landscape-hostile-supportive
- Whole Woman’s Health v Jackson, 21-463, decided Dec. 10, 2021. https://www.supremecourt.gov/opinions/21pdf/21-463_ new_8o6b.pdf
- United States v Texas, 21-588, decided Dec. 10, 2021. (Per curiam, Sotomayor dissenting). https://www.supremecourt.gov /opinions/21pdf/21-588_c07d.pdf
- Cameron v EMW Women’s Surgical Center, 20-601, decided Mar. 3, 2022. https://www.supremecourt.gov/opinions/21pdf/20-601 _new_g20h.pdf
- Xiulu Ruan v United States, 20-1410, decided June 27, 2022. https:// www.supremecourt.gov/opinions/21pdf/20-1410_1an2.pdf
- Adam Liptak. Supreme Court sides with doctors accused of running pill mills. The New York Times. June 27, 2022. https://www .nytimes.com/2022/06/27/us/politics/supreme-court-controlled -substance-act.html
- 84 Stat. 1260, 21 U.S.C. §841(a).
- 21 CFR §1306.04(a) (2021).
- Becerra v Empire Health Foundation, For Valley Hospital Medical Center, 20-1312, decided June 24, 2022. https://www.supremecourt .gov/opinions/21pdf/20-1312_j42l.pdf
- American Hospital Association v Becerra, 20-1114, decided June 15, 2022. https://www.supremecourt.gov/opinions/21pdf/20 -1114_09m1.pdf
- Gallardo v Marstiller, 20-1263, decided June 6, 2022. https:// www.supremecourt.gov/opinions/21pdf/20-1263_new_hfci.pdf
- National Federation of Independent Business v Department of Labor, Occupational Safety and Health Administration, 21A244, decided Jan. 13, 2022. https://www.supremecourt.gov /opinions/21pdf/21a244_hgci.pdf
- Biden v Missouri, 21A240, decided Jan. 13, 2022. https://www .supremecourt.gov/opinions/21pdf/21a240_d18e.pdf
- Alabama Association of Realtors v Department of Health and Human Services, 21A23, decided Aug. 26, 2021. https://www .supremecourt.gov/opinions/20pdf/21a23_ap6c.pdf
- Does v Mills, 21A90, decided Oct. 29, 2021. https://www .supremecourt.gov/opinions/21pdf/21a90_6j37.pdf
Hold or not to hold: Navigating involuntary commitment
CASE Depressed and suicidal
Police arrive at the home of Mr. H, age 50, after his wife calls 911. She reports he has depression and she saw him in bed brandishing a firearm as if he wanted to hurt himself. Upon arrival, the officers enter the house and find Mr. H in bed without a firearm. Mr. H says little to the officers about the alleged events, but acknowledges he has depression and is willing to go the hospital for further evaluation. Neither his wife nor the officers locate a firearm in the home.
EVALUATION Emergency detention
In the emergency department (ED), Mr. H’s laboratory results and physical examination findings are normal. He acknowledges feeling depressed over the past 2 weeks. Though he cannot identify any precipitants, he says he has experienced anhedonia, lack of appetite, decreased energy, and changes in his sleep patterns. When asked about the day’s events concerning the firearm, Mr. H becomes guarded and does not give a clear answer regarding having thoughts of suicide.
The evaluating psychiatrist obtains collateral from Mr. H’s wife and reviews his medical records. There are no active prescriptions on file and the psychiatrist notices that last year there was a suicide attempt involving a firearm. Following that episode, Mr. H was hospitalized, treated with sertraline 50 mg/d, and discharged with a diagnosis of major depressive disorder. There was no legal or substance abuse history.
In the ED, the psychiatrist conducts a psychiatric evaluation, including a suicide risk assessment, and determines Mr. H is at imminent risk of ending his life. Mr. H’s psychiatrist explains there are 2 treatment options: to be admitted to the hospital or to be discharged. The psychiatrist recommends hospital admission to Mr. H for his safety and stabilization. Mr. H says he prefers to return home.
Because the psychiatrist believes Mr. H is at imminent risk of ending his life and there is no less restrictive setting for treatment, he implements an emergency detention. In Ohio, this allows Mr. H to be held in the hospital for no more than 3 court days in accordance with state law. Before Mr. H’s emergency detention periods ends, the psychiatrist will need to decide whether Mr. H can be safely discharged. If the psychiatrist determines that Mr. H still needs treatment, the court will be petitioned for a civil commitment hearing.
[polldaddy:11189291]
The author’s observations
In some cases, courts allow information a psychiatrist does not directly obtain from a patient to be admitted as testimony in a civil commitment hearing. However, some jurisdictions consider sources of information not obtained directly from the patient as hearsay and thus inadmissible.1 Though each source listed may provide credible information that could be presented at a hearing, the psychiatrist should discuss with the patient the information obtained from these sources to ensure it is admissable.2 A discussion with Mr. H about the factors that led to his hospital arrival will avoid the psychiatrist’s reliance on what another person has heard or seen when providing testimony. Even when a psychiatrist is not faced with an issue of admissibility, caution must be taken with third-party reports.3
TREATMENT Civil commitment hearing
Before the emergency detention period expires, Mr. H’s psychiatrist determines that he remains at imminent risk of self-harm. To continue hospitalization, the psychiatrist files a petition for civil commitment and testifies at the commitment hearing. He reports that Mr. H suffers from a substantial mood disorder that grossly impairs his judgment and behavior. The psychiatrist also testifies that the least restrictive environment for treatment continues to be inpatient hospitalization, because Mr. H is still at imminent risk of harming himself.
Continue to: Following the psychiatrist's...
Following the psychiatrist’s testimony, the magistrate finds that Mr. H is a mentally ill person subject to hospitalization given his mood disorder that grossly impairs his judgment and behavior. The magistrate orders that Mr. H be civilly committed to the hospital.
[polldaddy:11189293]
The author’s observations
The psychiatrist’s testimony mirrors the language regarding civil commitment in the Ohio Revised Code.4 Other elements considered for mental illness in Ohio are a substantial disorder of memory, thought, orientation, or perception that grossly impairs one’s capacity to recognize reality or meet the demands of life.4 The definition of what constitutes a mental disorder varies by state, but the burden of persuasion—the standard by which the court must be convinced—is generally uniform.5 In the 1979 case Addington v Texas, the United States Supreme Court concluded that in a civil commitment hearing, the minimum standard of proof for involuntary commitment must be clear and convincing evidence.6 Neither medical certainty nor substantial probability are burdens of persuasions.6 Instead, these terms may be presented in a forensic report when an examiner outlines their opinion. Table 1 and the Figure provide more detail on burdens of persuasion.
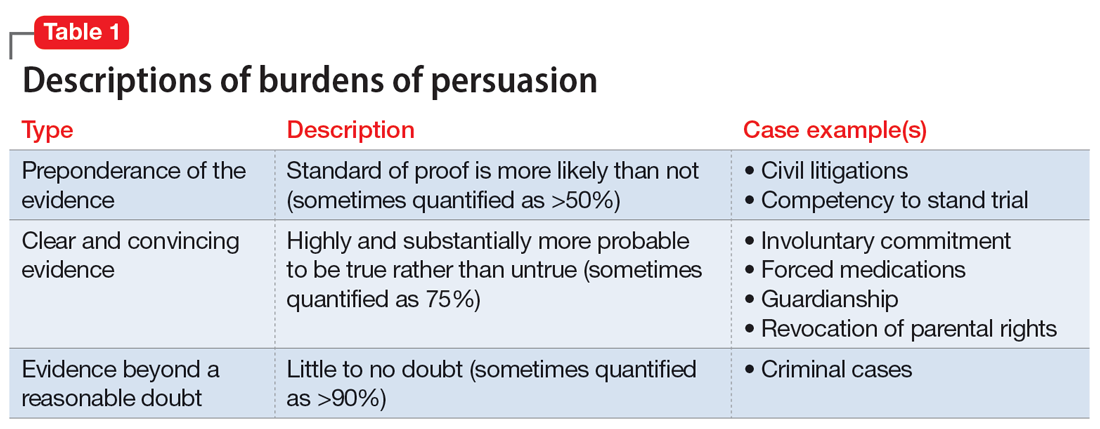
TREATMENT Civil commitment and patient rights
At a regularly scheduled treatment team meeting, the team informs Mr. H that he has been civilly committed for further treatment. Mr. H becomes upset and tells the team the decision is a complete violation of his rights. After a long rant, Mr. H walks out of the room, saying, “I did not even know when this hearing was.” A member of the treatment team becomes concerned that Mr. H may not have been notified of the hearing.
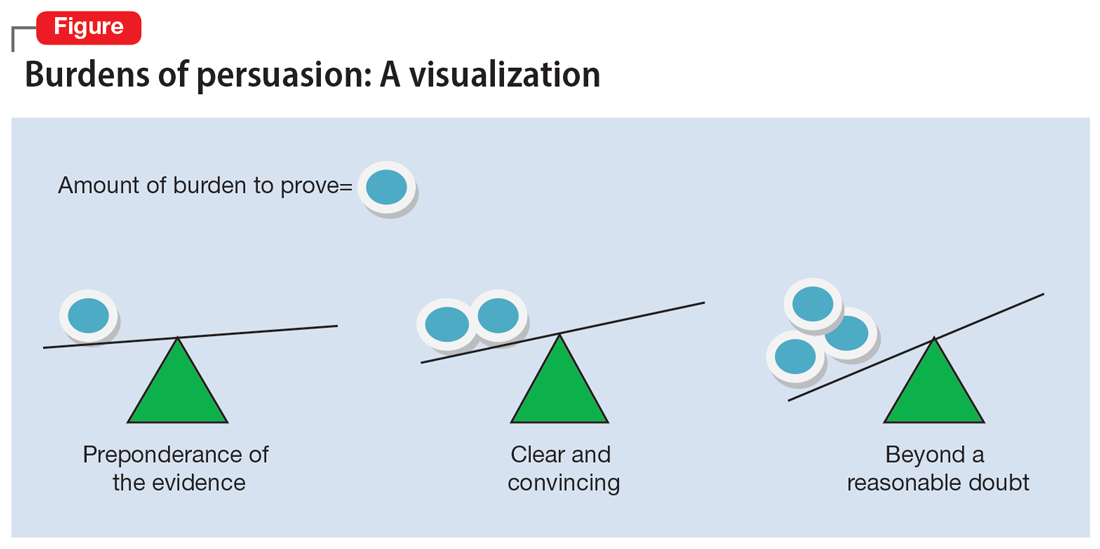
[polldaddy:11189294]
The author’s observations
It is not clear if Mr. H had been notified of his civil commitment hearing. If Mr. H had not been notified, his rights would have been compromised. Lessard v Schmidt (1972) outlined that individuals involved in a civil commitment hearing should be afforded the same rights as those involved in criminal proceedings.7 Mr. H should have been notified of his hearing and afforded the opportunity to have the assignment of counsel, the right to appear, the right to testify, the right to present witnesses and other evidence, and the right to confront witnesses.
Without notification of the hearing, the only right that would have remained intact for Mr. H would have been the assignment of counsel in his absence and without his knowledge. If Mr. H had been notified of the hearing and did not want to attend, yet still desired legal counsel, he could have waived his presence voluntarily after discussing this option with his attorney.8,9
Continue to: OUTCOME Stabilization and discharge
OUTCOME Stabilization and discharge
During his 10-day stay, Mr. H is treated with sertraline 50 mg/d and engages in individual and group therapy. He shows noticeable improvement in his depressive symptoms and reports having no thoughts of suicide or self-harm. The treatment team determines it is appropriate to discharge him home (the firearm was never found) and involves his wife in safety planning and follow-up care. On the day of his discharge, Mr. H reflects on his treatment and civil commitment. He says, “I did not know a judge could order me to be hospitalized.”
[polldaddy:11189297]
The author’s observations
The physician’s decision to pursue civil commitment is best described by the legal doctrines of police powers and parens patriae. Other relevant ethical principles are described in Table 2.10
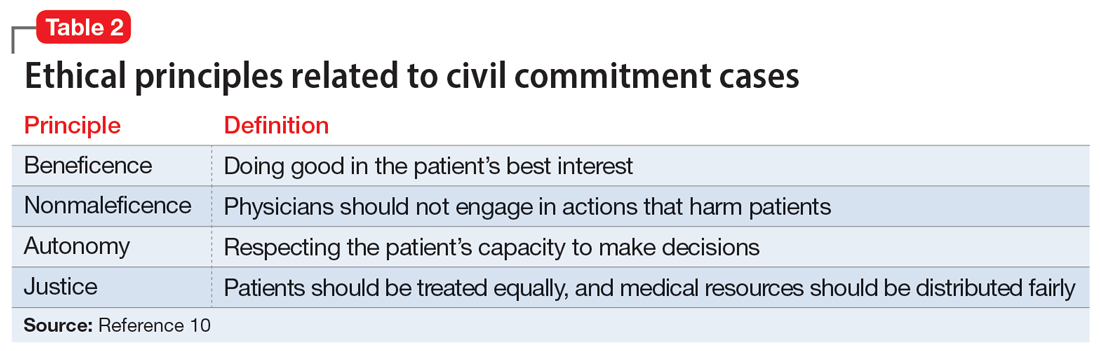
Though ethical principles may play a role in civil commitment, parens patriae and police powers is the answer with respect to the State.11Parens patriae is Latin for the “parent of the country” and grants the State the power to protect those residents who are most vulnerable. Police power is the authority of the State to enact and enforce rules that limit the rights of individuals for the greater good of ensuring health, safety, and welfare of all citizens.
Bottom Line
Psychiatrists are entrusted with recognizing when a patient, due to mental illness, is a danger to themselves or others and in need of treatment. After an emergency detention period, if the patient remains a danger to themselves or others and does not want to voluntarily receive treatment, a court hearing is required. As an expert witness, the treating psychiatrist should know the factors of law in their jurisdiction that determine civil commitment.
Related Resources
- Extreme Risk Protection Orders. Johns Hopkins Bloomberg School of Public Health. https://www.jhsph.edu/research/ centers-and-institutes/johns-hopkins-center-for-gun-violenceprevention-and-policy/research/extreme-risk-protectionorders/
- Gutheil TG. The Psychiatrist as Expert Witness. 2nd ed. American Psychiatric Association Publishing; 2009.
- Landmark Cases 2014. American Academy of Psychiatry and the Law. https://www.aapl.org/landmark-cases
Drug Brand Names
Sertraline • Zoloft
1. Pinals DA, Mossman D. Evaluation for Civil Commitment. Oxford University Press; 2012.
2. Thatcher BT, Mossman D. Testifying for civil commitment: help unwilling patients get the treatment they need. Current Psychiatry. 2009;8(11):51-56.
3. Marett CP, Mossman D. What is your liability for involuntary commitment based on faulty information? Current Psychiatry. 2017;16(3):21-25,33.
4. Ohio Rev Code § 5122.01 (2018).
5. The Burden of Proof. University of Minnesota. Accessed January 23, 2022. https://open.lib.umn.edu/criminallaw/chapter/2-4-the-burden-of-proof/
6. Gold LH, Frierson RL, eds. The American Psychiatric Association Publishing Textbook of Forensic Psychiatry. 3rd ed. American Psychiatric Association Publishing; 2018.
7. Gold LH, Frierson RL, eds. The American Psychiatric Association Publishing Textbook of Suicide Assessment and Management. 3rd ed. American Psychiatric Association Publishing; 2020.
8. Cook J. Good lawyering and bad role models: the role of respondent’s counsel in a civil commitment hearing. Georgetown Journal of Legal Ethics. 2000;14(1):179-195.
9. Ferris CE. The search for due process in civil commitment hearings: how procedural realities have altered substantive standards. Vanderbilt Law Rev. 2008;61(3):959-981.
10. Substance Abuse and Mental Health Services Administration. Civil Commitment and the Mental Health Care Continuum: Historical Trends and Principles for Law and Practice. 2019. Accessed January 23, 2022. https://www.samhsa.gov/resource/ebp/civil-commitment-mental-health-care-continuum-historical-trends-principles-law
11. Melton GB, Petrila J, Poythress NG, et al. Psychological Evaluations for the Courts: A Handbook for Mental Health Profession. 4th ed. Guilford Press; 2018.
CASE Depressed and suicidal
Police arrive at the home of Mr. H, age 50, after his wife calls 911. She reports he has depression and she saw him in bed brandishing a firearm as if he wanted to hurt himself. Upon arrival, the officers enter the house and find Mr. H in bed without a firearm. Mr. H says little to the officers about the alleged events, but acknowledges he has depression and is willing to go the hospital for further evaluation. Neither his wife nor the officers locate a firearm in the home.
EVALUATION Emergency detention
In the emergency department (ED), Mr. H’s laboratory results and physical examination findings are normal. He acknowledges feeling depressed over the past 2 weeks. Though he cannot identify any precipitants, he says he has experienced anhedonia, lack of appetite, decreased energy, and changes in his sleep patterns. When asked about the day’s events concerning the firearm, Mr. H becomes guarded and does not give a clear answer regarding having thoughts of suicide.
The evaluating psychiatrist obtains collateral from Mr. H’s wife and reviews his medical records. There are no active prescriptions on file and the psychiatrist notices that last year there was a suicide attempt involving a firearm. Following that episode, Mr. H was hospitalized, treated with sertraline 50 mg/d, and discharged with a diagnosis of major depressive disorder. There was no legal or substance abuse history.
In the ED, the psychiatrist conducts a psychiatric evaluation, including a suicide risk assessment, and determines Mr. H is at imminent risk of ending his life. Mr. H’s psychiatrist explains there are 2 treatment options: to be admitted to the hospital or to be discharged. The psychiatrist recommends hospital admission to Mr. H for his safety and stabilization. Mr. H says he prefers to return home.
Because the psychiatrist believes Mr. H is at imminent risk of ending his life and there is no less restrictive setting for treatment, he implements an emergency detention. In Ohio, this allows Mr. H to be held in the hospital for no more than 3 court days in accordance with state law. Before Mr. H’s emergency detention periods ends, the psychiatrist will need to decide whether Mr. H can be safely discharged. If the psychiatrist determines that Mr. H still needs treatment, the court will be petitioned for a civil commitment hearing.
[polldaddy:11189291]
The author’s observations
In some cases, courts allow information a psychiatrist does not directly obtain from a patient to be admitted as testimony in a civil commitment hearing. However, some jurisdictions consider sources of information not obtained directly from the patient as hearsay and thus inadmissible.1 Though each source listed may provide credible information that could be presented at a hearing, the psychiatrist should discuss with the patient the information obtained from these sources to ensure it is admissable.2 A discussion with Mr. H about the factors that led to his hospital arrival will avoid the psychiatrist’s reliance on what another person has heard or seen when providing testimony. Even when a psychiatrist is not faced with an issue of admissibility, caution must be taken with third-party reports.3
TREATMENT Civil commitment hearing
Before the emergency detention period expires, Mr. H’s psychiatrist determines that he remains at imminent risk of self-harm. To continue hospitalization, the psychiatrist files a petition for civil commitment and testifies at the commitment hearing. He reports that Mr. H suffers from a substantial mood disorder that grossly impairs his judgment and behavior. The psychiatrist also testifies that the least restrictive environment for treatment continues to be inpatient hospitalization, because Mr. H is still at imminent risk of harming himself.
Continue to: Following the psychiatrist's...
Following the psychiatrist’s testimony, the magistrate finds that Mr. H is a mentally ill person subject to hospitalization given his mood disorder that grossly impairs his judgment and behavior. The magistrate orders that Mr. H be civilly committed to the hospital.
[polldaddy:11189293]
The author’s observations
The psychiatrist’s testimony mirrors the language regarding civil commitment in the Ohio Revised Code.4 Other elements considered for mental illness in Ohio are a substantial disorder of memory, thought, orientation, or perception that grossly impairs one’s capacity to recognize reality or meet the demands of life.4 The definition of what constitutes a mental disorder varies by state, but the burden of persuasion—the standard by which the court must be convinced—is generally uniform.5 In the 1979 case Addington v Texas, the United States Supreme Court concluded that in a civil commitment hearing, the minimum standard of proof for involuntary commitment must be clear and convincing evidence.6 Neither medical certainty nor substantial probability are burdens of persuasions.6 Instead, these terms may be presented in a forensic report when an examiner outlines their opinion. Table 1 and the Figure provide more detail on burdens of persuasion.
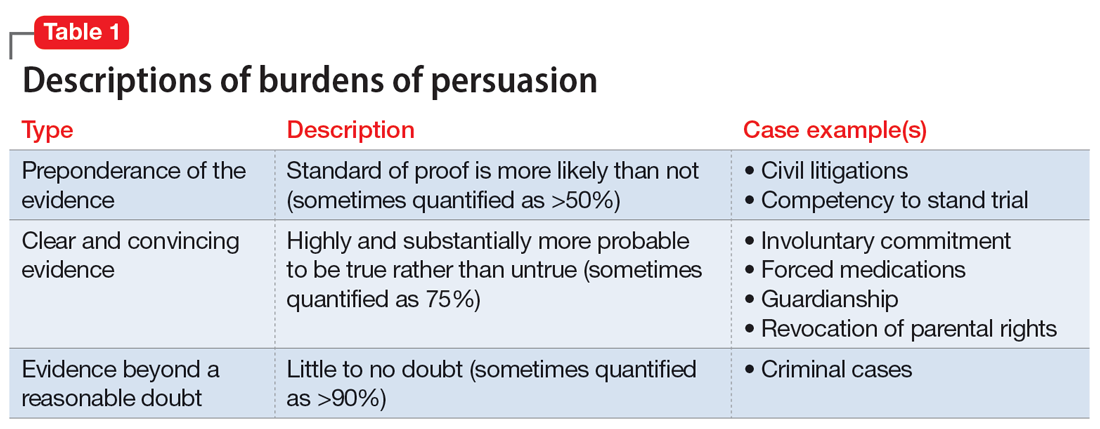
TREATMENT Civil commitment and patient rights
At a regularly scheduled treatment team meeting, the team informs Mr. H that he has been civilly committed for further treatment. Mr. H becomes upset and tells the team the decision is a complete violation of his rights. After a long rant, Mr. H walks out of the room, saying, “I did not even know when this hearing was.” A member of the treatment team becomes concerned that Mr. H may not have been notified of the hearing.
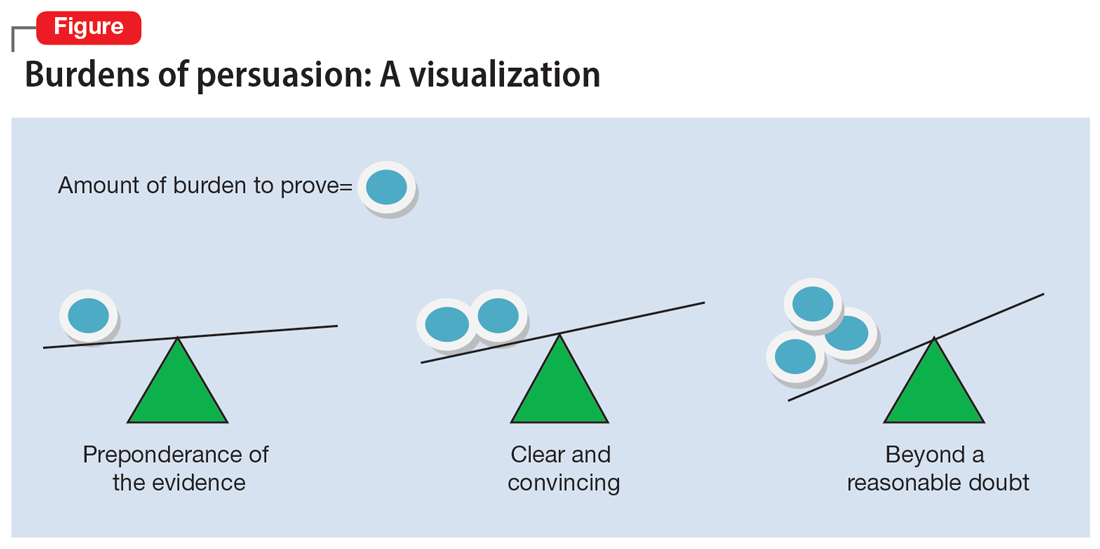
[polldaddy:11189294]
The author’s observations
It is not clear if Mr. H had been notified of his civil commitment hearing. If Mr. H had not been notified, his rights would have been compromised. Lessard v Schmidt (1972) outlined that individuals involved in a civil commitment hearing should be afforded the same rights as those involved in criminal proceedings.7 Mr. H should have been notified of his hearing and afforded the opportunity to have the assignment of counsel, the right to appear, the right to testify, the right to present witnesses and other evidence, and the right to confront witnesses.
Without notification of the hearing, the only right that would have remained intact for Mr. H would have been the assignment of counsel in his absence and without his knowledge. If Mr. H had been notified of the hearing and did not want to attend, yet still desired legal counsel, he could have waived his presence voluntarily after discussing this option with his attorney.8,9
Continue to: OUTCOME Stabilization and discharge
OUTCOME Stabilization and discharge
During his 10-day stay, Mr. H is treated with sertraline 50 mg/d and engages in individual and group therapy. He shows noticeable improvement in his depressive symptoms and reports having no thoughts of suicide or self-harm. The treatment team determines it is appropriate to discharge him home (the firearm was never found) and involves his wife in safety planning and follow-up care. On the day of his discharge, Mr. H reflects on his treatment and civil commitment. He says, “I did not know a judge could order me to be hospitalized.”
[polldaddy:11189297]
The author’s observations
The physician’s decision to pursue civil commitment is best described by the legal doctrines of police powers and parens patriae. Other relevant ethical principles are described in Table 2.10
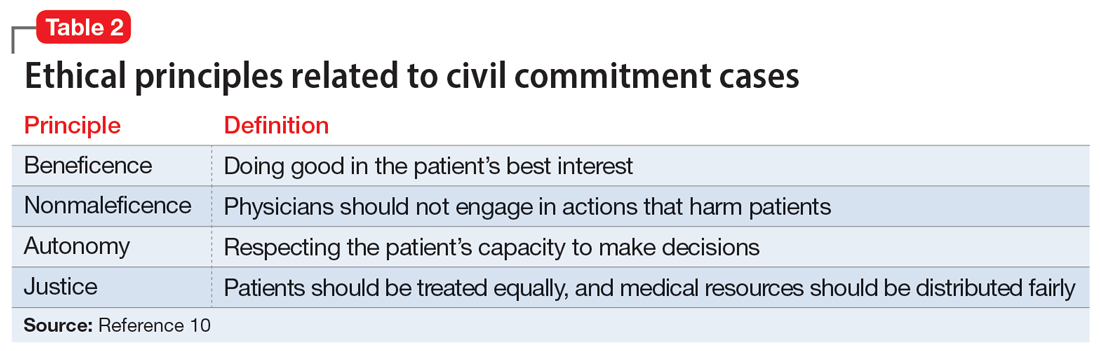
Though ethical principles may play a role in civil commitment, parens patriae and police powers is the answer with respect to the State.11Parens patriae is Latin for the “parent of the country” and grants the State the power to protect those residents who are most vulnerable. Police power is the authority of the State to enact and enforce rules that limit the rights of individuals for the greater good of ensuring health, safety, and welfare of all citizens.
Bottom Line
Psychiatrists are entrusted with recognizing when a patient, due to mental illness, is a danger to themselves or others and in need of treatment. After an emergency detention period, if the patient remains a danger to themselves or others and does not want to voluntarily receive treatment, a court hearing is required. As an expert witness, the treating psychiatrist should know the factors of law in their jurisdiction that determine civil commitment.
Related Resources
- Extreme Risk Protection Orders. Johns Hopkins Bloomberg School of Public Health. https://www.jhsph.edu/research/ centers-and-institutes/johns-hopkins-center-for-gun-violenceprevention-and-policy/research/extreme-risk-protectionorders/
- Gutheil TG. The Psychiatrist as Expert Witness. 2nd ed. American Psychiatric Association Publishing; 2009.
- Landmark Cases 2014. American Academy of Psychiatry and the Law. https://www.aapl.org/landmark-cases
Drug Brand Names
Sertraline • Zoloft
CASE Depressed and suicidal
Police arrive at the home of Mr. H, age 50, after his wife calls 911. She reports he has depression and she saw him in bed brandishing a firearm as if he wanted to hurt himself. Upon arrival, the officers enter the house and find Mr. H in bed without a firearm. Mr. H says little to the officers about the alleged events, but acknowledges he has depression and is willing to go the hospital for further evaluation. Neither his wife nor the officers locate a firearm in the home.
EVALUATION Emergency detention
In the emergency department (ED), Mr. H’s laboratory results and physical examination findings are normal. He acknowledges feeling depressed over the past 2 weeks. Though he cannot identify any precipitants, he says he has experienced anhedonia, lack of appetite, decreased energy, and changes in his sleep patterns. When asked about the day’s events concerning the firearm, Mr. H becomes guarded and does not give a clear answer regarding having thoughts of suicide.
The evaluating psychiatrist obtains collateral from Mr. H’s wife and reviews his medical records. There are no active prescriptions on file and the psychiatrist notices that last year there was a suicide attempt involving a firearm. Following that episode, Mr. H was hospitalized, treated with sertraline 50 mg/d, and discharged with a diagnosis of major depressive disorder. There was no legal or substance abuse history.
In the ED, the psychiatrist conducts a psychiatric evaluation, including a suicide risk assessment, and determines Mr. H is at imminent risk of ending his life. Mr. H’s psychiatrist explains there are 2 treatment options: to be admitted to the hospital or to be discharged. The psychiatrist recommends hospital admission to Mr. H for his safety and stabilization. Mr. H says he prefers to return home.
Because the psychiatrist believes Mr. H is at imminent risk of ending his life and there is no less restrictive setting for treatment, he implements an emergency detention. In Ohio, this allows Mr. H to be held in the hospital for no more than 3 court days in accordance with state law. Before Mr. H’s emergency detention periods ends, the psychiatrist will need to decide whether Mr. H can be safely discharged. If the psychiatrist determines that Mr. H still needs treatment, the court will be petitioned for a civil commitment hearing.
[polldaddy:11189291]
The author’s observations
In some cases, courts allow information a psychiatrist does not directly obtain from a patient to be admitted as testimony in a civil commitment hearing. However, some jurisdictions consider sources of information not obtained directly from the patient as hearsay and thus inadmissible.1 Though each source listed may provide credible information that could be presented at a hearing, the psychiatrist should discuss with the patient the information obtained from these sources to ensure it is admissable.2 A discussion with Mr. H about the factors that led to his hospital arrival will avoid the psychiatrist’s reliance on what another person has heard or seen when providing testimony. Even when a psychiatrist is not faced with an issue of admissibility, caution must be taken with third-party reports.3
TREATMENT Civil commitment hearing
Before the emergency detention period expires, Mr. H’s psychiatrist determines that he remains at imminent risk of self-harm. To continue hospitalization, the psychiatrist files a petition for civil commitment and testifies at the commitment hearing. He reports that Mr. H suffers from a substantial mood disorder that grossly impairs his judgment and behavior. The psychiatrist also testifies that the least restrictive environment for treatment continues to be inpatient hospitalization, because Mr. H is still at imminent risk of harming himself.
Continue to: Following the psychiatrist's...
Following the psychiatrist’s testimony, the magistrate finds that Mr. H is a mentally ill person subject to hospitalization given his mood disorder that grossly impairs his judgment and behavior. The magistrate orders that Mr. H be civilly committed to the hospital.
[polldaddy:11189293]
The author’s observations
The psychiatrist’s testimony mirrors the language regarding civil commitment in the Ohio Revised Code.4 Other elements considered for mental illness in Ohio are a substantial disorder of memory, thought, orientation, or perception that grossly impairs one’s capacity to recognize reality or meet the demands of life.4 The definition of what constitutes a mental disorder varies by state, but the burden of persuasion—the standard by which the court must be convinced—is generally uniform.5 In the 1979 case Addington v Texas, the United States Supreme Court concluded that in a civil commitment hearing, the minimum standard of proof for involuntary commitment must be clear and convincing evidence.6 Neither medical certainty nor substantial probability are burdens of persuasions.6 Instead, these terms may be presented in a forensic report when an examiner outlines their opinion. Table 1 and the Figure provide more detail on burdens of persuasion.
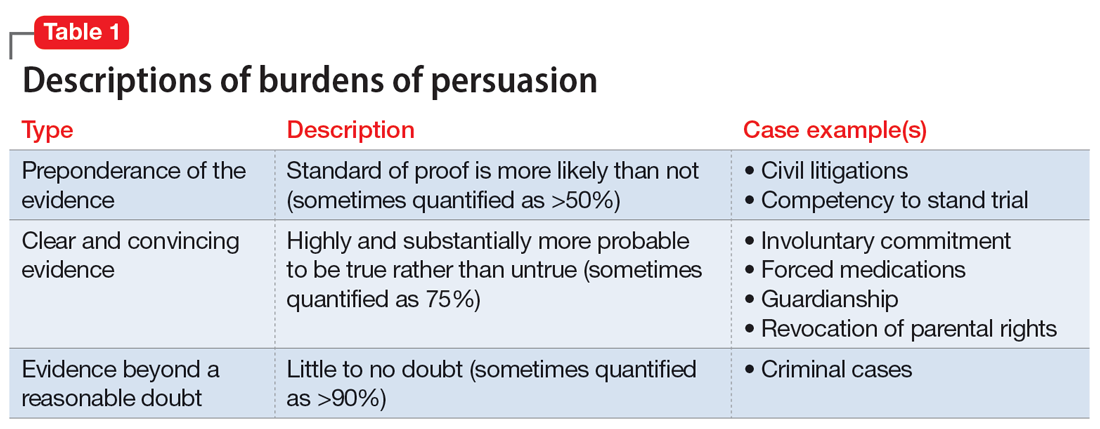
TREATMENT Civil commitment and patient rights
At a regularly scheduled treatment team meeting, the team informs Mr. H that he has been civilly committed for further treatment. Mr. H becomes upset and tells the team the decision is a complete violation of his rights. After a long rant, Mr. H walks out of the room, saying, “I did not even know when this hearing was.” A member of the treatment team becomes concerned that Mr. H may not have been notified of the hearing.
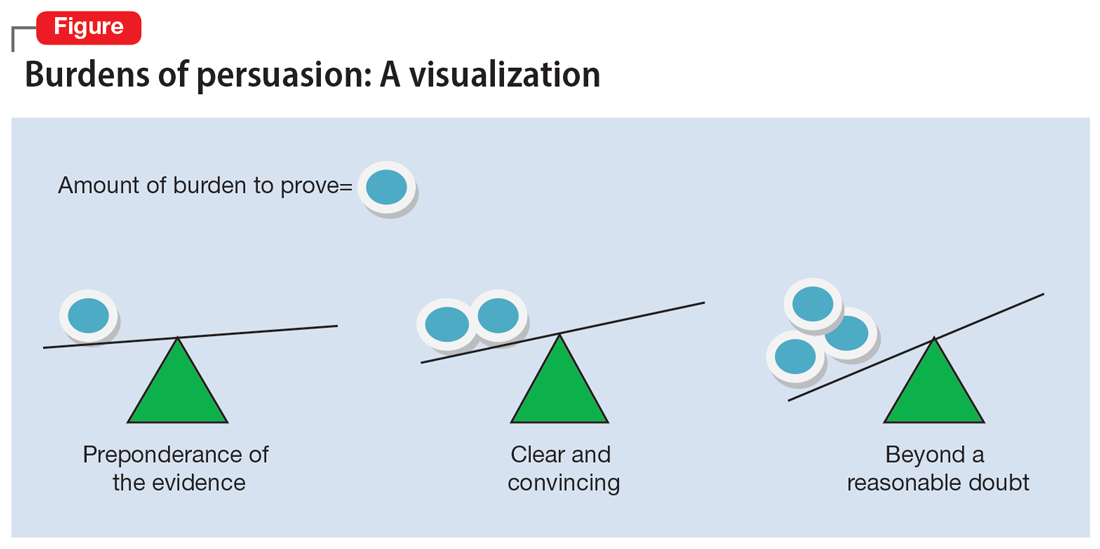
[polldaddy:11189294]
The author’s observations
It is not clear if Mr. H had been notified of his civil commitment hearing. If Mr. H had not been notified, his rights would have been compromised. Lessard v Schmidt (1972) outlined that individuals involved in a civil commitment hearing should be afforded the same rights as those involved in criminal proceedings.7 Mr. H should have been notified of his hearing and afforded the opportunity to have the assignment of counsel, the right to appear, the right to testify, the right to present witnesses and other evidence, and the right to confront witnesses.
Without notification of the hearing, the only right that would have remained intact for Mr. H would have been the assignment of counsel in his absence and without his knowledge. If Mr. H had been notified of the hearing and did not want to attend, yet still desired legal counsel, he could have waived his presence voluntarily after discussing this option with his attorney.8,9
Continue to: OUTCOME Stabilization and discharge
OUTCOME Stabilization and discharge
During his 10-day stay, Mr. H is treated with sertraline 50 mg/d and engages in individual and group therapy. He shows noticeable improvement in his depressive symptoms and reports having no thoughts of suicide or self-harm. The treatment team determines it is appropriate to discharge him home (the firearm was never found) and involves his wife in safety planning and follow-up care. On the day of his discharge, Mr. H reflects on his treatment and civil commitment. He says, “I did not know a judge could order me to be hospitalized.”
[polldaddy:11189297]
The author’s observations
The physician’s decision to pursue civil commitment is best described by the legal doctrines of police powers and parens patriae. Other relevant ethical principles are described in Table 2.10
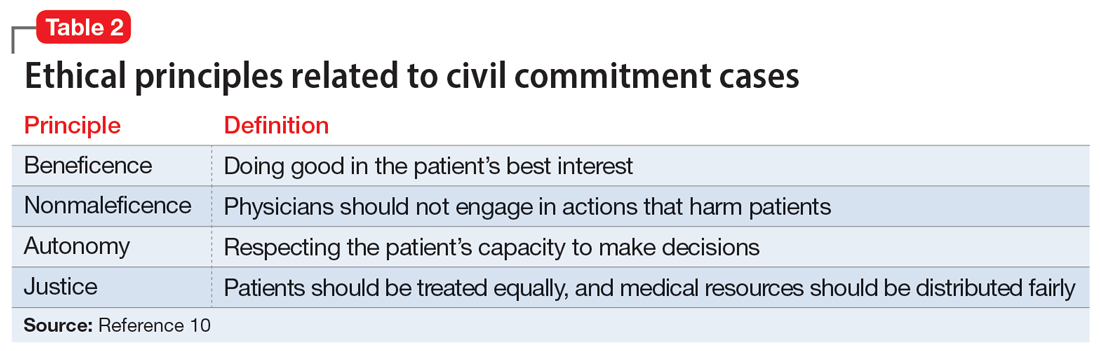
Though ethical principles may play a role in civil commitment, parens patriae and police powers is the answer with respect to the State.11Parens patriae is Latin for the “parent of the country” and grants the State the power to protect those residents who are most vulnerable. Police power is the authority of the State to enact and enforce rules that limit the rights of individuals for the greater good of ensuring health, safety, and welfare of all citizens.
Bottom Line
Psychiatrists are entrusted with recognizing when a patient, due to mental illness, is a danger to themselves or others and in need of treatment. After an emergency detention period, if the patient remains a danger to themselves or others and does not want to voluntarily receive treatment, a court hearing is required. As an expert witness, the treating psychiatrist should know the factors of law in their jurisdiction that determine civil commitment.
Related Resources
- Extreme Risk Protection Orders. Johns Hopkins Bloomberg School of Public Health. https://www.jhsph.edu/research/ centers-and-institutes/johns-hopkins-center-for-gun-violenceprevention-and-policy/research/extreme-risk-protectionorders/
- Gutheil TG. The Psychiatrist as Expert Witness. 2nd ed. American Psychiatric Association Publishing; 2009.
- Landmark Cases 2014. American Academy of Psychiatry and the Law. https://www.aapl.org/landmark-cases
Drug Brand Names
Sertraline • Zoloft
1. Pinals DA, Mossman D. Evaluation for Civil Commitment. Oxford University Press; 2012.
2. Thatcher BT, Mossman D. Testifying for civil commitment: help unwilling patients get the treatment they need. Current Psychiatry. 2009;8(11):51-56.
3. Marett CP, Mossman D. What is your liability for involuntary commitment based on faulty information? Current Psychiatry. 2017;16(3):21-25,33.
4. Ohio Rev Code § 5122.01 (2018).
5. The Burden of Proof. University of Minnesota. Accessed January 23, 2022. https://open.lib.umn.edu/criminallaw/chapter/2-4-the-burden-of-proof/
6. Gold LH, Frierson RL, eds. The American Psychiatric Association Publishing Textbook of Forensic Psychiatry. 3rd ed. American Psychiatric Association Publishing; 2018.
7. Gold LH, Frierson RL, eds. The American Psychiatric Association Publishing Textbook of Suicide Assessment and Management. 3rd ed. American Psychiatric Association Publishing; 2020.
8. Cook J. Good lawyering and bad role models: the role of respondent’s counsel in a civil commitment hearing. Georgetown Journal of Legal Ethics. 2000;14(1):179-195.
9. Ferris CE. The search for due process in civil commitment hearings: how procedural realities have altered substantive standards. Vanderbilt Law Rev. 2008;61(3):959-981.
10. Substance Abuse and Mental Health Services Administration. Civil Commitment and the Mental Health Care Continuum: Historical Trends and Principles for Law and Practice. 2019. Accessed January 23, 2022. https://www.samhsa.gov/resource/ebp/civil-commitment-mental-health-care-continuum-historical-trends-principles-law
11. Melton GB, Petrila J, Poythress NG, et al. Psychological Evaluations for the Courts: A Handbook for Mental Health Profession. 4th ed. Guilford Press; 2018.
1. Pinals DA, Mossman D. Evaluation for Civil Commitment. Oxford University Press; 2012.
2. Thatcher BT, Mossman D. Testifying for civil commitment: help unwilling patients get the treatment they need. Current Psychiatry. 2009;8(11):51-56.
3. Marett CP, Mossman D. What is your liability for involuntary commitment based on faulty information? Current Psychiatry. 2017;16(3):21-25,33.
4. Ohio Rev Code § 5122.01 (2018).
5. The Burden of Proof. University of Minnesota. Accessed January 23, 2022. https://open.lib.umn.edu/criminallaw/chapter/2-4-the-burden-of-proof/
6. Gold LH, Frierson RL, eds. The American Psychiatric Association Publishing Textbook of Forensic Psychiatry. 3rd ed. American Psychiatric Association Publishing; 2018.
7. Gold LH, Frierson RL, eds. The American Psychiatric Association Publishing Textbook of Suicide Assessment and Management. 3rd ed. American Psychiatric Association Publishing; 2020.
8. Cook J. Good lawyering and bad role models: the role of respondent’s counsel in a civil commitment hearing. Georgetown Journal of Legal Ethics. 2000;14(1):179-195.
9. Ferris CE. The search for due process in civil commitment hearings: how procedural realities have altered substantive standards. Vanderbilt Law Rev. 2008;61(3):959-981.
10. Substance Abuse and Mental Health Services Administration. Civil Commitment and the Mental Health Care Continuum: Historical Trends and Principles for Law and Practice. 2019. Accessed January 23, 2022. https://www.samhsa.gov/resource/ebp/civil-commitment-mental-health-care-continuum-historical-trends-principles-law
11. Melton GB, Petrila J, Poythress NG, et al. Psychological Evaluations for the Courts: A Handbook for Mental Health Profession. 4th ed. Guilford Press; 2018.
‘Med check’ appointments: How to minimize your malpractice risk
Medical malpractice claims can arise in any type of health care setting. The purpose of this article is to discuss the risk of medical malpractice suits in the context of brief “med checks,” which are 15- to 20-minute follow-up appointments for psychiatric outpatient medication management. Similar issues arise in brief new patient and transfer visits.
Malpractice hinges on ‘reasonableness’
Malpractice is an allegation of professional negligence.1 More specifically, it is an allegation that a clinician violated an existing duty by deviating from the standard of care, and that deviation caused damages.2 Medical malpractice claims involve questions about whether there was a deviation from the standard of care (whether the clinician failed to exercise a reasonable degree of skill and care given the context of the situation) and whether there was causation (whether a deviation caused a patient’s damages).3 These are fact-based determinations. Thus, the legal resolution of a malpractice claim is based on the facts of each specific case.
The advisability of 15-minute med checks and the associated limitation on a clinician’s ability to provide talk therapy are beyond the scope of this article. What is clear, however, is that not all brief med check appointments are created equal. Their safety and efficacy are dictated by the milieu in which they exist.
Practically speaking, although many factors need to be considered, the standard of care in a medical malpractice lawsuit is based on reasonableness.4-6 One strategy to proactively manage your malpractice risk is to consider—either for your existing job or before accepting a new position—whether your agency’s setup for brief med checks will allow you to practice reasonably. This article provides information to help you answer this question and describes a hypothetical case vignette to illustrate how certain factors might help lower the chances of facing a malpractice suit.
Established patients
In med check appointments for established patients, consider the patient population, the availability of pre- and postvisit support services, and contingency plans (Table).
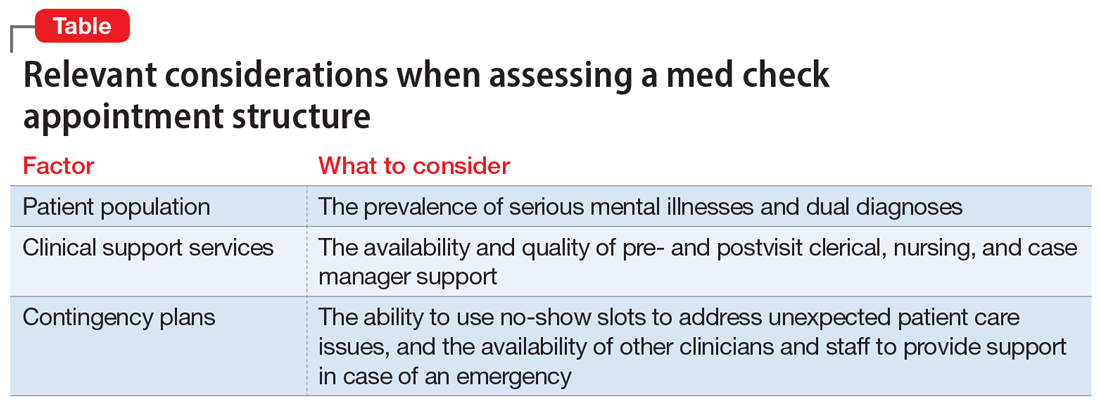
Different patient populations require different levels of treatment. Consider, for example, a patient with anxiety and trauma who is actively engaged with a therapist who works at the same agency as their psychiatrist, where the medication management appointments are solely for selective serotonin reuptake inhibitor refills. Compare that to a dual-diagnosis patient—with a psychotic and substance use disorder—who has had poor medication compliance and frequent rehospitalizations. The first patient is more likely to be reasonably managed in a 15-minute med check. The second patient would need significantly more pre- and postvisit support services. This consideration is relevant from a clinical perspective, and if a bad outcome occurs, from a malpractice perspective. Patient populations are not homogeneous; the reasonableness of a clinician’s actions during a brief med check visit depends on the specific patient.
Pre- and postvisit support services vary greatly from clinic to clinic. They range from clerical support (eg, calling a pharmacy to ensure that a patient’s medication is available for same-day pickup) to nursing support (eg, an injection nurse who is on site and can immediately provide a patient with a missed injection) to case manager support (eg, a case manager to facilitate coordination of care, such as by having a patient fill out record releases and then working to ensure that relevant hospital records are received prior to the next visit). The real-world availability of these services can determine the feasibility of safely conducting a 15-minute med check visit.
Continue to: Regardless of the patient population...
Regardless of the patient population, unexpected situations will arise. It could be a patient with posttraumatic stress disorder who was recently retraumatized and is in the midst of disclosing this new trauma at the end of a 15-minute visit. Or it could be a patient with dual diagnoses who comes to the agency intoxicated and manic, describing a plan to kill his neighbor with a shotgun. A clinician’s ability to meet the standard of care, and act reasonably within the confines of a brief med check structure, can thus depend on whether there are means of adequately managing such emergent situations.
Some clinics have fairly high no-show rates. Leaving no-show slots open for administrative time can provide a means of managing emergent situations. If, however, they are automatically rebooked with walk-ins, brief visits become more challenging. Thus, when assessing contingency plan logistics, consider the no-show rate, what happens when there are no-shows, how many other clinicians are available on a given day, and whether staff is available to provide support (eg, sitting with a patient while waiting for an ambulance).
New and transfer patients
Brief visits for new or transfer patients require the same assessment described above. However, there are additional considerations regarding previsit support services. Some clinics use clinical social workers to perform intake evaluations before a new patient sees the psychiatrist. A high-quality intake evaluation can allow a psychiatrist to focus, in a shorter amount of time, on a patient’s medication needs. An additional time saver is having support staff who will obtain relevant medical records before a patient’s first psychiatric visit. Such actions can greatly increase the efficacy of a new patient appointment for the prescribing clinician.
The reliability of and level of detail assessed in prior evaluations can be particularly relevant when considering a job providing coverage as locum tenens, when all patients will be new to you. Unfortunately, if you are not employed at a clinic, it can be hard to assess this ahead of time. If you know colleagues in the area where you are considering taking a locum position, ask for their opinions about the quality of work at the agency.
Case vignette
Mr. J is a 30-year-old man with schizoaffective disorder. For several years, he has been followed once every 4 weeks at the local clinic. During the first year of treatment, he had numerous hospitalizations due to medication noncompliance, psychotic episodes, and threats of violence against his mother. For the past year, he had been stable on the same dose of an oral antipsychotic medication (risperidone 2 mg twice a day). Then he stopped taking his medication, became increasingly psychotic, and, while holding a butcher knife, threatened to kill his mother. His mother called 911 and Mr. J was hospitalized.
Continue to: While in the hospital...
While in the hospital, Mr. J was restarted on risperidone 2 mg twice a day, and lithium 600 mg twice a day was added. As part of discharge planning, the hospital social worker set up an outpatient appointment with Dr. R, Mr. J’s treating psychiatrist at the clinic. That appointment was scheduled as a 15-minute med check. At the visit, Dr. R did not have or try to obtain a copy of the hospital discharge summary. Mr. J told Dr. R that he had been hospitalized because he had run out of his oral antipsychotic, and that it had been restarted during the hospitalization. Dr. R—who did not know about the recent incident involving a butcher knife or the subsequent medication changes—continued Mr. J’s risperidone, but did not continue his lithium because she did not know it had been added.
Dr. R scheduled a 4-week follow-up visit for Mr. J. Then she went on maternity leave. Because the agency was short-staffed, they hired Dr. C—a locum tenens—to see all of Dr. R’s established patients in 15-minute time slots.
At their first visit, Mr. J told Dr. C that he was gaining too much weight from his antipsychotic and wanted to know if it would be OK to decrease the dose. Dr. C reviewed Dr. R’s last office note but, due to limited time, did not review any other notes. Although Dr. C had 2 no-shows that day, the clinic had a policy that required Dr. C to see walk-ins whenever there was a no-show.
Dr. C did not know of Mr. J’s threats of violence or the medication changes associated with his recent hospitalization (they were not referenced in Dr. R’s last note). Dr. C decreased the dose of Mr. J’s risperidone from 2 mg twice a day to 0.5 mg twice a day. He did not do a violence risk assessment. Two weeks after the visit with Dr. C, Mr. J, who had become increasingly depressed and psychotic, killed his mother and died by suicide.
The estates of Mr. J and his mother filed a medical malpractice lawsuit against Dr. R and Dr. C. Both psychiatrists had a duty to Mr. J. Whether there was a duty to Mr. J’s mother would depend in part on the state’s duty to protect laws. Either way, the malpractice case would hinge on whether the psychiatrists’ conduct fell below the standard of care.
Continue to: In this case...
In this case, the critical issues were Dr. R’s failure to obtain and review the recent hospital records and Dr. C’s decision to decrease the antipsychotic dose. Of particular concern is Dr. C’s decision to decrease the antipsychotic dose without reviewing more information from past records, and the resultant failure to perform a violence risk assessment. These deviations cannot be blamed entirely on the brevity of the med check appointment. They could happen in a clinic that allotted longer time periods for follow-up visits, but they are, however, more likely to occur in a short med check appointment due to time constraints.
The likelihood of these errors could have been reduced by additional support services, as well as more time for Dr. C to see each patient who was new to him. For example, if there had been a support person available to obtain hospital records prior to the postdischarge appointment, Dr. R and Dr. C would have been more likely to be aware of the violent threat associated with Mr. J’s hospitalization. Additionally, if the busy clinicians had contingency plans to assess complicated patients, such as the ability to use no-show time to deal with difficult situations, Dr. C could have taken more time to review past records.
Bottom Line
When working in a setting that involves brief med check appointments, assess the agency structure, and whether it will allow you to practice reasonably. This will be relevant clinically and may reduce the risk of malpractice lawsuits. Reasonableness of a clinician’s actions is a fact-specific question and is influenced by multiple factors, including the patient population, the availability and quality of an agency’s support services, and contingency plans.
Related Resources
- Mossman D. Successfully navigating the 15-minute ‘med check.’ Current Psychiatry. 2010;9(6):40-43.
- Olfson M, Marcus SC. National trends in outpatient psychotherapy. Am J Psychiatry. 2010;167(12):1456-1463.
Drug Brand Names
Lithium • Eskalith, Lithobid
Risperidone • Risperdal
1. Malpractice. In: Garner BA, ed. Black’s Law Dictionary. 11th ed. Thomson West; 2019:1148.
2. Frierson RL, Joshi KG. Malpractice law and psychiatry: an overview. Focus. 2019;17:332-336. doi:10.1176/appi.focus.20190017
3. Negligence Based Claims. In: Boumil MM, Hattis PA, eds. Medical Liability in a Nutshell. 4th ed. West Academic Publishing; 2017:43-88
4. Peters PG. The quiet demise of deference to custom: malpractice law at the millennium. Washington and Lee Law Review. 2000;57(1):163-205. Accessed July 8, 2022. https://scholarlycommons.law.wlu.edu/wlulr/vol57/iss1/5
5. Simon RI. Standard-of-care testimony: best practices or reasonable care? J Am Acad Psychiatry Law. 2005;33(1):8-11. Accessed July 8, 2022. http://jaapl.org/content/33/1/8
6. Behrens SA. Call in Houdini: the time has come to be released from the geographic straightjacket known as the locality rule. Drake Law Review. 2008; 56(3):753-790. Accessed June 20, 2022. https://lawreviewdrake.files.wordpress.com/2015/06/lrvol56-3_behrens.pdf
Medical malpractice claims can arise in any type of health care setting. The purpose of this article is to discuss the risk of medical malpractice suits in the context of brief “med checks,” which are 15- to 20-minute follow-up appointments for psychiatric outpatient medication management. Similar issues arise in brief new patient and transfer visits.
Malpractice hinges on ‘reasonableness’
Malpractice is an allegation of professional negligence.1 More specifically, it is an allegation that a clinician violated an existing duty by deviating from the standard of care, and that deviation caused damages.2 Medical malpractice claims involve questions about whether there was a deviation from the standard of care (whether the clinician failed to exercise a reasonable degree of skill and care given the context of the situation) and whether there was causation (whether a deviation caused a patient’s damages).3 These are fact-based determinations. Thus, the legal resolution of a malpractice claim is based on the facts of each specific case.
The advisability of 15-minute med checks and the associated limitation on a clinician’s ability to provide talk therapy are beyond the scope of this article. What is clear, however, is that not all brief med check appointments are created equal. Their safety and efficacy are dictated by the milieu in which they exist.
Practically speaking, although many factors need to be considered, the standard of care in a medical malpractice lawsuit is based on reasonableness.4-6 One strategy to proactively manage your malpractice risk is to consider—either for your existing job or before accepting a new position—whether your agency’s setup for brief med checks will allow you to practice reasonably. This article provides information to help you answer this question and describes a hypothetical case vignette to illustrate how certain factors might help lower the chances of facing a malpractice suit.
Established patients
In med check appointments for established patients, consider the patient population, the availability of pre- and postvisit support services, and contingency plans (Table).
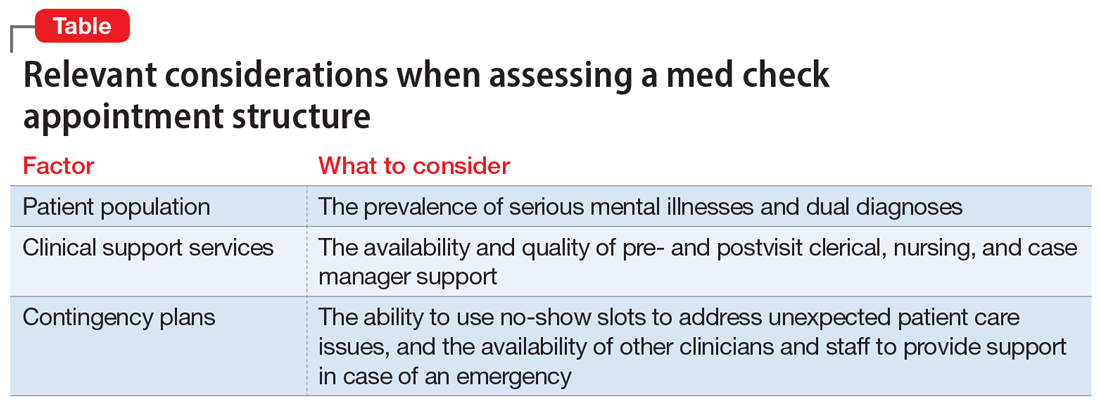
Different patient populations require different levels of treatment. Consider, for example, a patient with anxiety and trauma who is actively engaged with a therapist who works at the same agency as their psychiatrist, where the medication management appointments are solely for selective serotonin reuptake inhibitor refills. Compare that to a dual-diagnosis patient—with a psychotic and substance use disorder—who has had poor medication compliance and frequent rehospitalizations. The first patient is more likely to be reasonably managed in a 15-minute med check. The second patient would need significantly more pre- and postvisit support services. This consideration is relevant from a clinical perspective, and if a bad outcome occurs, from a malpractice perspective. Patient populations are not homogeneous; the reasonableness of a clinician’s actions during a brief med check visit depends on the specific patient.
Pre- and postvisit support services vary greatly from clinic to clinic. They range from clerical support (eg, calling a pharmacy to ensure that a patient’s medication is available for same-day pickup) to nursing support (eg, an injection nurse who is on site and can immediately provide a patient with a missed injection) to case manager support (eg, a case manager to facilitate coordination of care, such as by having a patient fill out record releases and then working to ensure that relevant hospital records are received prior to the next visit). The real-world availability of these services can determine the feasibility of safely conducting a 15-minute med check visit.
Continue to: Regardless of the patient population...
Regardless of the patient population, unexpected situations will arise. It could be a patient with posttraumatic stress disorder who was recently retraumatized and is in the midst of disclosing this new trauma at the end of a 15-minute visit. Or it could be a patient with dual diagnoses who comes to the agency intoxicated and manic, describing a plan to kill his neighbor with a shotgun. A clinician’s ability to meet the standard of care, and act reasonably within the confines of a brief med check structure, can thus depend on whether there are means of adequately managing such emergent situations.
Some clinics have fairly high no-show rates. Leaving no-show slots open for administrative time can provide a means of managing emergent situations. If, however, they are automatically rebooked with walk-ins, brief visits become more challenging. Thus, when assessing contingency plan logistics, consider the no-show rate, what happens when there are no-shows, how many other clinicians are available on a given day, and whether staff is available to provide support (eg, sitting with a patient while waiting for an ambulance).
New and transfer patients
Brief visits for new or transfer patients require the same assessment described above. However, there are additional considerations regarding previsit support services. Some clinics use clinical social workers to perform intake evaluations before a new patient sees the psychiatrist. A high-quality intake evaluation can allow a psychiatrist to focus, in a shorter amount of time, on a patient’s medication needs. An additional time saver is having support staff who will obtain relevant medical records before a patient’s first psychiatric visit. Such actions can greatly increase the efficacy of a new patient appointment for the prescribing clinician.
The reliability of and level of detail assessed in prior evaluations can be particularly relevant when considering a job providing coverage as locum tenens, when all patients will be new to you. Unfortunately, if you are not employed at a clinic, it can be hard to assess this ahead of time. If you know colleagues in the area where you are considering taking a locum position, ask for their opinions about the quality of work at the agency.
Case vignette
Mr. J is a 30-year-old man with schizoaffective disorder. For several years, he has been followed once every 4 weeks at the local clinic. During the first year of treatment, he had numerous hospitalizations due to medication noncompliance, psychotic episodes, and threats of violence against his mother. For the past year, he had been stable on the same dose of an oral antipsychotic medication (risperidone 2 mg twice a day). Then he stopped taking his medication, became increasingly psychotic, and, while holding a butcher knife, threatened to kill his mother. His mother called 911 and Mr. J was hospitalized.
Continue to: While in the hospital...
While in the hospital, Mr. J was restarted on risperidone 2 mg twice a day, and lithium 600 mg twice a day was added. As part of discharge planning, the hospital social worker set up an outpatient appointment with Dr. R, Mr. J’s treating psychiatrist at the clinic. That appointment was scheduled as a 15-minute med check. At the visit, Dr. R did not have or try to obtain a copy of the hospital discharge summary. Mr. J told Dr. R that he had been hospitalized because he had run out of his oral antipsychotic, and that it had been restarted during the hospitalization. Dr. R—who did not know about the recent incident involving a butcher knife or the subsequent medication changes—continued Mr. J’s risperidone, but did not continue his lithium because she did not know it had been added.
Dr. R scheduled a 4-week follow-up visit for Mr. J. Then she went on maternity leave. Because the agency was short-staffed, they hired Dr. C—a locum tenens—to see all of Dr. R’s established patients in 15-minute time slots.
At their first visit, Mr. J told Dr. C that he was gaining too much weight from his antipsychotic and wanted to know if it would be OK to decrease the dose. Dr. C reviewed Dr. R’s last office note but, due to limited time, did not review any other notes. Although Dr. C had 2 no-shows that day, the clinic had a policy that required Dr. C to see walk-ins whenever there was a no-show.
Dr. C did not know of Mr. J’s threats of violence or the medication changes associated with his recent hospitalization (they were not referenced in Dr. R’s last note). Dr. C decreased the dose of Mr. J’s risperidone from 2 mg twice a day to 0.5 mg twice a day. He did not do a violence risk assessment. Two weeks after the visit with Dr. C, Mr. J, who had become increasingly depressed and psychotic, killed his mother and died by suicide.
The estates of Mr. J and his mother filed a medical malpractice lawsuit against Dr. R and Dr. C. Both psychiatrists had a duty to Mr. J. Whether there was a duty to Mr. J’s mother would depend in part on the state’s duty to protect laws. Either way, the malpractice case would hinge on whether the psychiatrists’ conduct fell below the standard of care.
Continue to: In this case...
In this case, the critical issues were Dr. R’s failure to obtain and review the recent hospital records and Dr. C’s decision to decrease the antipsychotic dose. Of particular concern is Dr. C’s decision to decrease the antipsychotic dose without reviewing more information from past records, and the resultant failure to perform a violence risk assessment. These deviations cannot be blamed entirely on the brevity of the med check appointment. They could happen in a clinic that allotted longer time periods for follow-up visits, but they are, however, more likely to occur in a short med check appointment due to time constraints.
The likelihood of these errors could have been reduced by additional support services, as well as more time for Dr. C to see each patient who was new to him. For example, if there had been a support person available to obtain hospital records prior to the postdischarge appointment, Dr. R and Dr. C would have been more likely to be aware of the violent threat associated with Mr. J’s hospitalization. Additionally, if the busy clinicians had contingency plans to assess complicated patients, such as the ability to use no-show time to deal with difficult situations, Dr. C could have taken more time to review past records.
Bottom Line
When working in a setting that involves brief med check appointments, assess the agency structure, and whether it will allow you to practice reasonably. This will be relevant clinically and may reduce the risk of malpractice lawsuits. Reasonableness of a clinician’s actions is a fact-specific question and is influenced by multiple factors, including the patient population, the availability and quality of an agency’s support services, and contingency plans.
Related Resources
- Mossman D. Successfully navigating the 15-minute ‘med check.’ Current Psychiatry. 2010;9(6):40-43.
- Olfson M, Marcus SC. National trends in outpatient psychotherapy. Am J Psychiatry. 2010;167(12):1456-1463.
Drug Brand Names
Lithium • Eskalith, Lithobid
Risperidone • Risperdal
Medical malpractice claims can arise in any type of health care setting. The purpose of this article is to discuss the risk of medical malpractice suits in the context of brief “med checks,” which are 15- to 20-minute follow-up appointments for psychiatric outpatient medication management. Similar issues arise in brief new patient and transfer visits.
Malpractice hinges on ‘reasonableness’
Malpractice is an allegation of professional negligence.1 More specifically, it is an allegation that a clinician violated an existing duty by deviating from the standard of care, and that deviation caused damages.2 Medical malpractice claims involve questions about whether there was a deviation from the standard of care (whether the clinician failed to exercise a reasonable degree of skill and care given the context of the situation) and whether there was causation (whether a deviation caused a patient’s damages).3 These are fact-based determinations. Thus, the legal resolution of a malpractice claim is based on the facts of each specific case.
The advisability of 15-minute med checks and the associated limitation on a clinician’s ability to provide talk therapy are beyond the scope of this article. What is clear, however, is that not all brief med check appointments are created equal. Their safety and efficacy are dictated by the milieu in which they exist.
Practically speaking, although many factors need to be considered, the standard of care in a medical malpractice lawsuit is based on reasonableness.4-6 One strategy to proactively manage your malpractice risk is to consider—either for your existing job or before accepting a new position—whether your agency’s setup for brief med checks will allow you to practice reasonably. This article provides information to help you answer this question and describes a hypothetical case vignette to illustrate how certain factors might help lower the chances of facing a malpractice suit.
Established patients
In med check appointments for established patients, consider the patient population, the availability of pre- and postvisit support services, and contingency plans (Table).
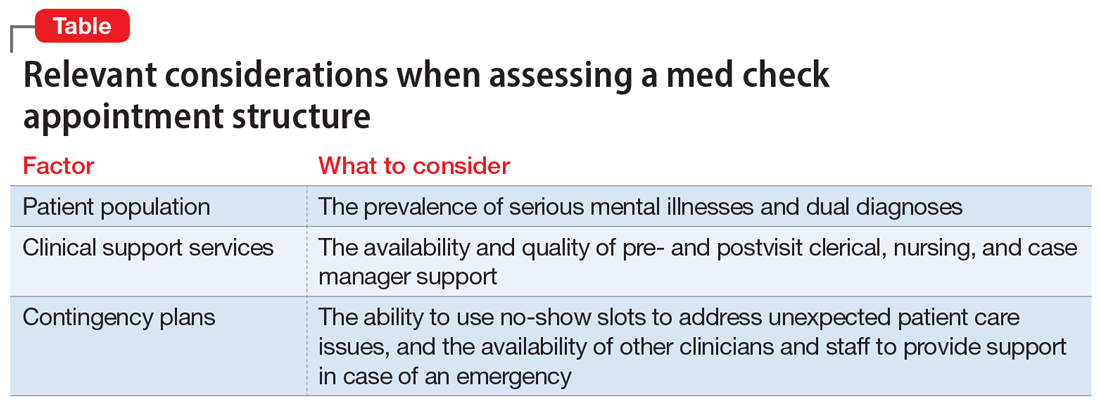
Different patient populations require different levels of treatment. Consider, for example, a patient with anxiety and trauma who is actively engaged with a therapist who works at the same agency as their psychiatrist, where the medication management appointments are solely for selective serotonin reuptake inhibitor refills. Compare that to a dual-diagnosis patient—with a psychotic and substance use disorder—who has had poor medication compliance and frequent rehospitalizations. The first patient is more likely to be reasonably managed in a 15-minute med check. The second patient would need significantly more pre- and postvisit support services. This consideration is relevant from a clinical perspective, and if a bad outcome occurs, from a malpractice perspective. Patient populations are not homogeneous; the reasonableness of a clinician’s actions during a brief med check visit depends on the specific patient.
Pre- and postvisit support services vary greatly from clinic to clinic. They range from clerical support (eg, calling a pharmacy to ensure that a patient’s medication is available for same-day pickup) to nursing support (eg, an injection nurse who is on site and can immediately provide a patient with a missed injection) to case manager support (eg, a case manager to facilitate coordination of care, such as by having a patient fill out record releases and then working to ensure that relevant hospital records are received prior to the next visit). The real-world availability of these services can determine the feasibility of safely conducting a 15-minute med check visit.
Continue to: Regardless of the patient population...
Regardless of the patient population, unexpected situations will arise. It could be a patient with posttraumatic stress disorder who was recently retraumatized and is in the midst of disclosing this new trauma at the end of a 15-minute visit. Or it could be a patient with dual diagnoses who comes to the agency intoxicated and manic, describing a plan to kill his neighbor with a shotgun. A clinician’s ability to meet the standard of care, and act reasonably within the confines of a brief med check structure, can thus depend on whether there are means of adequately managing such emergent situations.
Some clinics have fairly high no-show rates. Leaving no-show slots open for administrative time can provide a means of managing emergent situations. If, however, they are automatically rebooked with walk-ins, brief visits become more challenging. Thus, when assessing contingency plan logistics, consider the no-show rate, what happens when there are no-shows, how many other clinicians are available on a given day, and whether staff is available to provide support (eg, sitting with a patient while waiting for an ambulance).
New and transfer patients
Brief visits for new or transfer patients require the same assessment described above. However, there are additional considerations regarding previsit support services. Some clinics use clinical social workers to perform intake evaluations before a new patient sees the psychiatrist. A high-quality intake evaluation can allow a psychiatrist to focus, in a shorter amount of time, on a patient’s medication needs. An additional time saver is having support staff who will obtain relevant medical records before a patient’s first psychiatric visit. Such actions can greatly increase the efficacy of a new patient appointment for the prescribing clinician.
The reliability of and level of detail assessed in prior evaluations can be particularly relevant when considering a job providing coverage as locum tenens, when all patients will be new to you. Unfortunately, if you are not employed at a clinic, it can be hard to assess this ahead of time. If you know colleagues in the area where you are considering taking a locum position, ask for their opinions about the quality of work at the agency.
Case vignette
Mr. J is a 30-year-old man with schizoaffective disorder. For several years, he has been followed once every 4 weeks at the local clinic. During the first year of treatment, he had numerous hospitalizations due to medication noncompliance, psychotic episodes, and threats of violence against his mother. For the past year, he had been stable on the same dose of an oral antipsychotic medication (risperidone 2 mg twice a day). Then he stopped taking his medication, became increasingly psychotic, and, while holding a butcher knife, threatened to kill his mother. His mother called 911 and Mr. J was hospitalized.
Continue to: While in the hospital...
While in the hospital, Mr. J was restarted on risperidone 2 mg twice a day, and lithium 600 mg twice a day was added. As part of discharge planning, the hospital social worker set up an outpatient appointment with Dr. R, Mr. J’s treating psychiatrist at the clinic. That appointment was scheduled as a 15-minute med check. At the visit, Dr. R did not have or try to obtain a copy of the hospital discharge summary. Mr. J told Dr. R that he had been hospitalized because he had run out of his oral antipsychotic, and that it had been restarted during the hospitalization. Dr. R—who did not know about the recent incident involving a butcher knife or the subsequent medication changes—continued Mr. J’s risperidone, but did not continue his lithium because she did not know it had been added.
Dr. R scheduled a 4-week follow-up visit for Mr. J. Then she went on maternity leave. Because the agency was short-staffed, they hired Dr. C—a locum tenens—to see all of Dr. R’s established patients in 15-minute time slots.
At their first visit, Mr. J told Dr. C that he was gaining too much weight from his antipsychotic and wanted to know if it would be OK to decrease the dose. Dr. C reviewed Dr. R’s last office note but, due to limited time, did not review any other notes. Although Dr. C had 2 no-shows that day, the clinic had a policy that required Dr. C to see walk-ins whenever there was a no-show.
Dr. C did not know of Mr. J’s threats of violence or the medication changes associated with his recent hospitalization (they were not referenced in Dr. R’s last note). Dr. C decreased the dose of Mr. J’s risperidone from 2 mg twice a day to 0.5 mg twice a day. He did not do a violence risk assessment. Two weeks after the visit with Dr. C, Mr. J, who had become increasingly depressed and psychotic, killed his mother and died by suicide.
The estates of Mr. J and his mother filed a medical malpractice lawsuit against Dr. R and Dr. C. Both psychiatrists had a duty to Mr. J. Whether there was a duty to Mr. J’s mother would depend in part on the state’s duty to protect laws. Either way, the malpractice case would hinge on whether the psychiatrists’ conduct fell below the standard of care.
Continue to: In this case...
In this case, the critical issues were Dr. R’s failure to obtain and review the recent hospital records and Dr. C’s decision to decrease the antipsychotic dose. Of particular concern is Dr. C’s decision to decrease the antipsychotic dose without reviewing more information from past records, and the resultant failure to perform a violence risk assessment. These deviations cannot be blamed entirely on the brevity of the med check appointment. They could happen in a clinic that allotted longer time periods for follow-up visits, but they are, however, more likely to occur in a short med check appointment due to time constraints.
The likelihood of these errors could have been reduced by additional support services, as well as more time for Dr. C to see each patient who was new to him. For example, if there had been a support person available to obtain hospital records prior to the postdischarge appointment, Dr. R and Dr. C would have been more likely to be aware of the violent threat associated with Mr. J’s hospitalization. Additionally, if the busy clinicians had contingency plans to assess complicated patients, such as the ability to use no-show time to deal with difficult situations, Dr. C could have taken more time to review past records.
Bottom Line
When working in a setting that involves brief med check appointments, assess the agency structure, and whether it will allow you to practice reasonably. This will be relevant clinically and may reduce the risk of malpractice lawsuits. Reasonableness of a clinician’s actions is a fact-specific question and is influenced by multiple factors, including the patient population, the availability and quality of an agency’s support services, and contingency plans.
Related Resources
- Mossman D. Successfully navigating the 15-minute ‘med check.’ Current Psychiatry. 2010;9(6):40-43.
- Olfson M, Marcus SC. National trends in outpatient psychotherapy. Am J Psychiatry. 2010;167(12):1456-1463.
Drug Brand Names
Lithium • Eskalith, Lithobid
Risperidone • Risperdal
1. Malpractice. In: Garner BA, ed. Black’s Law Dictionary. 11th ed. Thomson West; 2019:1148.
2. Frierson RL, Joshi KG. Malpractice law and psychiatry: an overview. Focus. 2019;17:332-336. doi:10.1176/appi.focus.20190017
3. Negligence Based Claims. In: Boumil MM, Hattis PA, eds. Medical Liability in a Nutshell. 4th ed. West Academic Publishing; 2017:43-88
4. Peters PG. The quiet demise of deference to custom: malpractice law at the millennium. Washington and Lee Law Review. 2000;57(1):163-205. Accessed July 8, 2022. https://scholarlycommons.law.wlu.edu/wlulr/vol57/iss1/5
5. Simon RI. Standard-of-care testimony: best practices or reasonable care? J Am Acad Psychiatry Law. 2005;33(1):8-11. Accessed July 8, 2022. http://jaapl.org/content/33/1/8
6. Behrens SA. Call in Houdini: the time has come to be released from the geographic straightjacket known as the locality rule. Drake Law Review. 2008; 56(3):753-790. Accessed June 20, 2022. https://lawreviewdrake.files.wordpress.com/2015/06/lrvol56-3_behrens.pdf
1. Malpractice. In: Garner BA, ed. Black’s Law Dictionary. 11th ed. Thomson West; 2019:1148.
2. Frierson RL, Joshi KG. Malpractice law and psychiatry: an overview. Focus. 2019;17:332-336. doi:10.1176/appi.focus.20190017
3. Negligence Based Claims. In: Boumil MM, Hattis PA, eds. Medical Liability in a Nutshell. 4th ed. West Academic Publishing; 2017:43-88
4. Peters PG. The quiet demise of deference to custom: malpractice law at the millennium. Washington and Lee Law Review. 2000;57(1):163-205. Accessed July 8, 2022. https://scholarlycommons.law.wlu.edu/wlulr/vol57/iss1/5
5. Simon RI. Standard-of-care testimony: best practices or reasonable care? J Am Acad Psychiatry Law. 2005;33(1):8-11. Accessed July 8, 2022. http://jaapl.org/content/33/1/8
6. Behrens SA. Call in Houdini: the time has come to be released from the geographic straightjacket known as the locality rule. Drake Law Review. 2008; 56(3):753-790. Accessed June 20, 2022. https://lawreviewdrake.files.wordpress.com/2015/06/lrvol56-3_behrens.pdf
Paraphilic disorders and sexual criminality
Mr. J, age 23, presents to an outpatient mental health clinic for treatment of anxiety. He has no psychiatric history, is dressed neatly, and recently finished graduate school with a degree in accounting. Mr. J is reserved during the initial psychiatric evaluation and provides only basic facts about his developmental history.
Mr. J comes from a middle-class household with no history of trauma or substance use. He does not report any symptoms consistent with anxiety, but discloses a history of sexual preoccupations. Mr. J says that during adolescence he developed a predilection for observing others engage in sexual activity. In his late teens, he began following couples to their homes in the hope of witnessing sexual intimacy. In the rare instance that his voyeuristic fantasy comes to fruition, he masturbates and achieves sexual gratification he is incapable of experiencing otherwise. Mr. J notes that he has not yet been caught, but he expresses concern and embarrassment related to his actions. He concludes by noting that he seeks help because the frequency of this behavior has steadily increased.
How would you treat Mr. J? Where does the line exist between a normophilic sexual interest, fantasy or urge, and a paraphilia? Does Mr. J qualify as a sexually violent predator?
From The Rocky Horror Picture Show to Fifty Shades of Grey, sensationalized portrayals of sexual deviancy have long been present in popular culture. The continued popularity of serial killers years after their crimes seems in part related to the extreme sexual torture their victims often endure. However, a sexual offense does not always qualify as a paraphilic disorder.1 In fact, many individuals with paraphilic disorders never engage in illegal activity. Additionally, experiencing sexually deviant thoughts alone does not qualify as a paraphilic disorder.1
A thorough psychiatric evaluation should include a discussion of the patient’s sexual history, including the potential of sexual dysfunction and abnormal desires or behaviors. Most individuals with sexual dysfunction do not have a paraphilic disorder.2 DSM-5 and ICD-11 classify sexual dysfunction and paraphilic disorders in different categories. However, previous editions grouped them together under sexual and gender identity disorders. Individuals with paraphilic disorders may not originally present to the outpatient setting for a paraphilic disorder, but instead may first seek treatment for a more common comorbid disorder, such as a mood disorder, personality disorder, or substance use disorder.3
Diagnostically speaking, if individuals do not experience distress or issues with functionality and lack legal charges (suggesting that they have not violated the rights of others), they are categorized as having an atypical sexual interest but do not necessarily meet the criteria for a disorder.4 This article provides an overview of paraphilic disorders as well as forensic considerations when examining individuals with sexually deviant behaviors.
Overview of paraphilic disorders
DSM-5 characterizes a paraphilic disorder as “recurrent, intense sexually arousing fantasies, sexual urges, or behaviors generally involving nonhuman objects or nonconsenting partners for at least 6 months. The individual must have acted on the thought and/or it caused clinically significant distress or impairment in social, occupational, or other important areas of functioning.” DSM-5 outlines 9 categories of paraphilic disorders, which are described in Table 1.4,5
Continue to: Paraphilic disorders are more common...
Paraphilic disorders are more common in men than in women; the 2 most prevalent are voyeuristic disorder and frotteuristic disorder.6 The incidence of paraphilias in the general outpatient setting varies by disorder. Approximately 45% of individuals with pedophilic disorder seek treatment, whereas only 1% of individuals with zoophilia seek treatment.6 The incidence of paraphilic acts also varies drastically; individuals with exhibitionistic disorder engaged in an average of 50 acts vs only 3 for individuals with sexual sadism.6 Not all individuals with paraphilic disorders commit crimes. Approximately 58% of sexual offenders meet the criteria for a paraphilic disorder, but antisocial personality disorder is a far more common diagnosis.7
Sexual psychopath statutes: Phase 1
In 1937, Michigan became the first state to enact sexual psychopath statutes, allowing for indeterminate sentencing and the civil commitment/treatment of sex offenders with repeated convictions. By the 1970s, more than 30 states had enacted similar statutes. It was not until 1967, in Specht v Patterson,8 that the United States Supreme Court unanimously ruled that the Fourteenth Amendment Due Process Clause was violated when Francis Eddie Specht faced life in prison following his conviction for indecent liberties under the Colorado Sex Offenders Act.
Specht was convicted in 1959 for indecent liberties after pleading guilty to enticing a child younger than age 16 into an office and engaging in sexual activities with them. At the time of Specht’s conviction, the crime of indecent liberties carried a punishment of 10 years. However, Specht was sentenced under the Sexual Offenders Act, which allowed for an indeterminate sentence of 1 day to life in prison. The Supreme Court noted that Specht was denied the right to be present with counsel, to confront the evidence against him, to cross-examine witnesses, and to offer his own evidence, which was a violation of his constitutionally guaranteed Fourteenth Amendment right to Procedural Due Process. The decision led most states to repeal early sexual psychopath statutes.8
Sexually violent predator laws: Phase 2
After early sexual psychopath statutes were repealed, many states pushed to update sex offender laws in response to the Earl Shriner case.9 In 1989, Shriner was released from prison after serving a 10-year sentence for sexually assaulting 2 teenage girls. At the time, he did not meet the criteria for civil commitment in the state of Washington. On the day he was released, Shriner cut off a young boy’s penis and left him to die. Washington subsequently became the first of many states to enact sexually violent predator (SVP) laws. Table 210 shows states and districts that have SVP civil commitment laws.
A series of United States Supreme Court cases solidified current sexual offender civil commitment laws (Table 38,11-15).
Continue to: Allen v Illinois
Allen v Illinois (1986).11 The Court ruled that forcing an individual to participate in a psychiatric evaluation prior to a sexually dangerous person’s commitment hearing did not violate the individual’s Fifth Amendment right against self-incrimination because the purpose of the evaluation was to provide treatment, not punishment.
Kansas v Hendricks (1997).12 The Court upheld that the Kansas Sexually Violent Predator Act was constitutional and noted that the use of the broad term “mental abnormality” (in lieu of the more specific term “mental illness”) does not violate an individual’s Fourteenth Amendment right to substantive due process. Additionally, the Court opined that the constitutional ban on double jeopardy and ex post facto lawmaking does not apply because the procedures are civil, not criminal.
Kansas v Crane (2002).13 The Court upheld the Kansas Sexually Violent Predator Act, stating that mental illness and dangerousness are essential elements to meet the criteria for civil commitment. The Court added that proof of partial (not total) “volitional impairment” is all that is required to meet the threshold of sexual dangerousness.
McKune v Lile (2002).14 The Court ruled that a policy requiring participation in polygraph testing, which would lead to the disclosure of sexual crimes (even those that have not been prosecuted), does not violate an individual’s Fifth Amendment rights because it serves a vital penological purpose.
Adam Walsh Child Protection and Safety Act of 200616; United States v Comstock (2010).15 This act and subsequent case reinforced the federal government’s right to civilly commit sexually dangerous persons approaching the end of their prison sentences.
Continue to: What is requiried for civil commitment?
What is required for civil commitment?
SVP laws require 4 conditions to be met for the civil commitment of sexual offenders (Table 417). In criteria 1, “charges” is a key word, because this allows individuals found Not Guilty by Reason of Insanity or Incompetent to Stand Trial to be civilly committed. Criteria 2 defines “mental abnormality” as a “congenital or acquired condition affecting the emotional or volitional capacity which predisposes the person to commit criminal sexual acts in a degree constituting such person a menace to the health and safety of others.”18 This is a broad definition, and allows individuals with personality disorders to be civilly committed (although most sexual offenders are committed for having a paraphilic disorder). To determine risk, various actuarial instruments are used to assess for sexually violent recidivism, including (but not limited to) the Static-99R, Sexual Violence Risk-20, and the Sex Offender Risk Appraisal Guide.19
Although the percentages vary, sex offenders rarely are civilly committed following their criminal sentence. In California, approximately 1.5% of sex offenders are civilly committed.17 The standard of proof for civil commitment varies by state between “clear and convincing evidence” and “beyond a reasonable doubt.” As sex offenders approach the end of their sentence, sexually violent offenders are identified to the general population and referred for a psychiatric evaluation. If the individual meets the 4 criteria for commitment (Table 417), their case is sent to the prosecuting attorney’s office. If accepted, the court holds a probable cause hearing, followed by a full trial.
Pornography and sex offenders
Pornography has long been considered a risk factor for sexual offending, and the role of pornography in influencing sexual behavior has drawn recent interest in research towards predicting future offenses. However, a 2019 systematic review by Mellor et al20 on the relationship between pornography and sexual offending suggested that early exposure to pornography is not a risk factor for sexual offending, nor is the risk of offending increased shortly after pornography exposure. Additionally, pornography use did not predict recidivism in low-risk sexual offenders, but did in high-risk offenders.
The use of child pornography presents a set of new risk factors. Prohibited by federal and state law, child pornography is defined under Section 2256 of Title 18, United States Code, as any visual depiction of sexually explicit conduct involving a minor (someone <age 18). Visual depictions include photographs, videos, digital or computer-generated images indistinguishable from an actual minor, and images created to depict a minor. The law does not require an image of a child engaging in sexual activity for the image to be characterized as child pornography. Offenders are also commonly charged with the distribution of child pornography. A conviction of child pornography possession carries a 15- to 30-year sentence, and distribution carries a 5- to 20-year sentence.21 The individual must also file for the sex offender registry, which may restrict their employment and place of residency.
It is unclear what percentage of individuals charged with child pornography have a history of prior sexual offenses. Numerous studies suggest there is a low risk of online offenders without prior offenses becoming contact offenders. Characteristics of online-only offenders include being White, a single male, age 20 to 30, well-educated, and employed, and having antisocial traits and a history of sexual deviancy.22 Contact offenders tend to be married with easy access to children, unemployed, uneducated, and to have a history of mental illness or criminal offenses.22
Continue to: Recidivism and treatment
Recidivism and treatment
The recidivism rate among sexual offenders averages 13.7% at 3- to 6-year follow-up,although rates vary by type of sexual offense.23 Individuals who committed rape have the highest rate of recidivism, while those who engaged in incest have the lowest. Three key points about sexual offender recidivism are:
- it declines over time and with increased age.
- sexual offenders are more like to commit a nonsexual offense than a sexual offense.
- sexual offenders who have undergone treatment are 26.3% less likely to reoffend.23
Although there is no standard of treatment, current interventions include external control, reduction of sexual drive, treatment of comorbid conditions, cognitive-behavioral therapy (CBT), and dynamic psychotherapy. External control relies on an outside entity that affects the individual’s behavior. For sexually deviant behaviors, simply making the act illegal or involving the law may inhibit many individuals from acting on a thought. Additional external control may include pharmacotherapy, which ranges from nonhormonal options such as selective serotonin reuptake inhibitors (SSRIs) to hormonal options. Therapy tends to focus on social skills training, sex education, cognitive restructuring, and identifying triggers, as well as victim empathy. The best indicators for successful treatment include an absence of comorbidities, increased age, and adult interpersonal relationships.24
Treatment choice may be predicated on the severity of the paraphilia. Psychotherapy alone is recommended for individuals able to maintain functioning if it does not affect their conventional sexual activity. Common treatment for low-risk individuals is psychotherapy and an SSRI. As risk increases, so does treatment with pharmacologic agents. Beyond SSRIs, moderate offenders may be treated with an SSRI and a low-dose antiandrogen. This is escalated in high-risk violent offenders to long-acting gonadotropin-releasing hormone analogs and synthetic steroidal analogs.25
An evolving class of disorders
With the evolution and accessibility of pornography, uncommon sexual practices have become more common, gaining notoriety and increased social acceptance. As a result, mental health professionals may be tasked with evaluating patients for possible paraphilic disorders. A common misconception is that individuals with sexually deviant thoughts, sexual offenders, and patients with paraphilic disorders are all the same. However, more commonly, sexual offenders do not have a paraphilic disorder. In the case of SVPs, outside of imprisonment, civil commitment remains a consideration for possible treatment. To meet the threshold of civil commitment, a sexual offender must have a “mental abnormality,” which is most commonly a paraphilic disorder. The treatment of paraphilic disorders remains a difficult task and includes a mixture of psychotherapy and medication options.
CASE CONTINUED
Mr. J begins weekly CBT to gain control of his voyeuristic fantasies without impacting his conventional sexual activity and desire. He responds well to treatment, and after 18 months, begins a typical sexual relationship with a woman. Although his voyeuristic thoughts remain, the urge to act on the thoughts decreases as Mr. J develops coping mechanisms. He does not require pharmacologic treatment.
Bottom Line
Individuals with paraphilic disorders are too often portrayed as sexual deviants or criminals. Psychiatrists must review each case with careful consideration of individual risk factors, such as the patient’s sexual history, to evaluate potential treatment options while determining if they pose a threat to the public.
Related Resources
- Sorrentino R, Abramowitz J. Minor-attracted persons: a neglected population. Current Psychiatry. 2021;20(7):21-27. doi:10.12788/cp.0149
- Berlin FS. Paraphilic disorders: a better understanding. Current Psychiatry. 2019;18(4):22-26,28.
1. Federoff JP. The paraphilias. In: Gelder MG, Andreasen NC, López-Ibor JJ Jr, Geddes JR, eds. New Oxford Textbook of Psychiatry. 2nd ed. Oxford University Press; 2012:832-842.
2. Grubin D. Medical models and interventions in sexual deviance. In: Laws R, O’Donohue WT, eds. Sexual Deviance: Theory, Assessment and Treatment. 2nd ed. Guilford Press; 2008:594-610.
3. Guidry LL, Saleh FM. Clinical considerations of paraphilic sex offenders with comorbid psychiatric conditions. Sex Addict Compulsivity. 2004;11(1-2):21-34.
4. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013.
5. Balon R. Paraphilic disorders. In: Roberts LW, Hales RE, Yudofsky SC, eds. The American Psychiatric Association Publishing Textbook of Psychiatry. 7th ed. American Psychiatric Association Publishing; 2019:749-770.
6. Sadock BJ, Sadock VA, Ruiz P. Paraphilic disorders. Kaplan and Sadock’s Synopsis of Psychiatry. 11th ed. Wolters Kluwer; 2015:593-599.
7. First MB, Halon RL. Use of DSM paraphilia diagnosis in sexually violent predator commitment cases. J Am Acad Psychiatry Law. 2008;36(4):443-454.
8. Specht v Patterson, 386 US 605 (1967).
9. Ra EP. The civil confinement of sexual predators: a delicate balance. J Civ Rts Econ Dev. 2007;22(1):335-372.
10. Felthous AR, Ko J. Sexually violent predator law in the United States. East Asian Arch Psychiatry. 2018;28(4):159-173.
11. Allen v Illinois, 478 US 364 (1986).
12. Kansas v Hendricks, 521 US 346 (1997).
13. Kansas v Crane, 534 US 407 (2002).
14. McKune v Lile, 536 US 24 (2002).
15. United States v Comstock, 560 US 126 (2010).
16. Adam Walsh Child Protection and Safety Act of 2006, HR 4472, 109th Cong (2006). Accessed April 25, 2022. https://www.congress.gov/bill/109th-congress/house-bill/4472
17. Tucker DE, Brakel SJ. Sexually violent predator laws. In: Rosner R, Scott C, eds. Principles and Practice of Forensic Psychiatry. 3rd ed. CRC Press; 2017:823-831.
18. Wash. Rev. Code. Ann. §71.09.020(8)
19. Bradford J, de Amorim Levin GV, Booth BD, et al. Forensic assessment of sex offenders. In: Gold LH, Frierson RL, eds. The American Psychiatric Association Publishing Textbook of Forensic Psychiatry. 3rd ed. American Psychiatric Association Publishing; 2017:382-397.
20. Mellor E, Duff S. The use of pornography and the relationship between pornography exposure and sexual offending in males: a systematic review. Aggress Violent Beh. 2019;46:116-126.
21. Failure To Register, 18 USC § 2250 (2012). Accessed April 25, 2022. https://www.govinfo.gov/app/details/USCODE-2011-title18/USCODE-2011-title18-partI-chap109B-sec2250
22. Hirschtritt ME, Tucker D, Binder RL. Risk assessment of online child sexual exploitation offenders. J Am Acad Psychiatry Law. 2019;47(2):155-164.
23. Blasko BL. Overview of sexual offender typologies, recidivism, and treatment. In: Jeglic EL, Calkins C, eds. Sexual Violence: Evidence Based Policy and Prevention. Springer; 2016:11-29.
24. Thibaut F, Cosyns P, Fedoroff JP, et al; WFSBP Task Force on Paraphilias. The World Federation of Societies of Biological Psychiatry (WFSBP) 2020 guidelines for the pharmacological treatment of paraphilic disorders. World J Biol Psychiatry. 2020;21(6):412-490.
25. Holoyda B. Paraphilias: from diagnosis to treatment. Psychiatric Times. 2019;36(12).
Mr. J, age 23, presents to an outpatient mental health clinic for treatment of anxiety. He has no psychiatric history, is dressed neatly, and recently finished graduate school with a degree in accounting. Mr. J is reserved during the initial psychiatric evaluation and provides only basic facts about his developmental history.
Mr. J comes from a middle-class household with no history of trauma or substance use. He does not report any symptoms consistent with anxiety, but discloses a history of sexual preoccupations. Mr. J says that during adolescence he developed a predilection for observing others engage in sexual activity. In his late teens, he began following couples to their homes in the hope of witnessing sexual intimacy. In the rare instance that his voyeuristic fantasy comes to fruition, he masturbates and achieves sexual gratification he is incapable of experiencing otherwise. Mr. J notes that he has not yet been caught, but he expresses concern and embarrassment related to his actions. He concludes by noting that he seeks help because the frequency of this behavior has steadily increased.
How would you treat Mr. J? Where does the line exist between a normophilic sexual interest, fantasy or urge, and a paraphilia? Does Mr. J qualify as a sexually violent predator?
From The Rocky Horror Picture Show to Fifty Shades of Grey, sensationalized portrayals of sexual deviancy have long been present in popular culture. The continued popularity of serial killers years after their crimes seems in part related to the extreme sexual torture their victims often endure. However, a sexual offense does not always qualify as a paraphilic disorder.1 In fact, many individuals with paraphilic disorders never engage in illegal activity. Additionally, experiencing sexually deviant thoughts alone does not qualify as a paraphilic disorder.1
A thorough psychiatric evaluation should include a discussion of the patient’s sexual history, including the potential of sexual dysfunction and abnormal desires or behaviors. Most individuals with sexual dysfunction do not have a paraphilic disorder.2 DSM-5 and ICD-11 classify sexual dysfunction and paraphilic disorders in different categories. However, previous editions grouped them together under sexual and gender identity disorders. Individuals with paraphilic disorders may not originally present to the outpatient setting for a paraphilic disorder, but instead may first seek treatment for a more common comorbid disorder, such as a mood disorder, personality disorder, or substance use disorder.3
Diagnostically speaking, if individuals do not experience distress or issues with functionality and lack legal charges (suggesting that they have not violated the rights of others), they are categorized as having an atypical sexual interest but do not necessarily meet the criteria for a disorder.4 This article provides an overview of paraphilic disorders as well as forensic considerations when examining individuals with sexually deviant behaviors.
Overview of paraphilic disorders
DSM-5 characterizes a paraphilic disorder as “recurrent, intense sexually arousing fantasies, sexual urges, or behaviors generally involving nonhuman objects or nonconsenting partners for at least 6 months. The individual must have acted on the thought and/or it caused clinically significant distress or impairment in social, occupational, or other important areas of functioning.” DSM-5 outlines 9 categories of paraphilic disorders, which are described in Table 1.4,5
Continue to: Paraphilic disorders are more common...
Paraphilic disorders are more common in men than in women; the 2 most prevalent are voyeuristic disorder and frotteuristic disorder.6 The incidence of paraphilias in the general outpatient setting varies by disorder. Approximately 45% of individuals with pedophilic disorder seek treatment, whereas only 1% of individuals with zoophilia seek treatment.6 The incidence of paraphilic acts also varies drastically; individuals with exhibitionistic disorder engaged in an average of 50 acts vs only 3 for individuals with sexual sadism.6 Not all individuals with paraphilic disorders commit crimes. Approximately 58% of sexual offenders meet the criteria for a paraphilic disorder, but antisocial personality disorder is a far more common diagnosis.7
Sexual psychopath statutes: Phase 1
In 1937, Michigan became the first state to enact sexual psychopath statutes, allowing for indeterminate sentencing and the civil commitment/treatment of sex offenders with repeated convictions. By the 1970s, more than 30 states had enacted similar statutes. It was not until 1967, in Specht v Patterson,8 that the United States Supreme Court unanimously ruled that the Fourteenth Amendment Due Process Clause was violated when Francis Eddie Specht faced life in prison following his conviction for indecent liberties under the Colorado Sex Offenders Act.
Specht was convicted in 1959 for indecent liberties after pleading guilty to enticing a child younger than age 16 into an office and engaging in sexual activities with them. At the time of Specht’s conviction, the crime of indecent liberties carried a punishment of 10 years. However, Specht was sentenced under the Sexual Offenders Act, which allowed for an indeterminate sentence of 1 day to life in prison. The Supreme Court noted that Specht was denied the right to be present with counsel, to confront the evidence against him, to cross-examine witnesses, and to offer his own evidence, which was a violation of his constitutionally guaranteed Fourteenth Amendment right to Procedural Due Process. The decision led most states to repeal early sexual psychopath statutes.8
Sexually violent predator laws: Phase 2
After early sexual psychopath statutes were repealed, many states pushed to update sex offender laws in response to the Earl Shriner case.9 In 1989, Shriner was released from prison after serving a 10-year sentence for sexually assaulting 2 teenage girls. At the time, he did not meet the criteria for civil commitment in the state of Washington. On the day he was released, Shriner cut off a young boy’s penis and left him to die. Washington subsequently became the first of many states to enact sexually violent predator (SVP) laws. Table 210 shows states and districts that have SVP civil commitment laws.
A series of United States Supreme Court cases solidified current sexual offender civil commitment laws (Table 38,11-15).
Continue to: Allen v Illinois
Allen v Illinois (1986).11 The Court ruled that forcing an individual to participate in a psychiatric evaluation prior to a sexually dangerous person’s commitment hearing did not violate the individual’s Fifth Amendment right against self-incrimination because the purpose of the evaluation was to provide treatment, not punishment.
Kansas v Hendricks (1997).12 The Court upheld that the Kansas Sexually Violent Predator Act was constitutional and noted that the use of the broad term “mental abnormality” (in lieu of the more specific term “mental illness”) does not violate an individual’s Fourteenth Amendment right to substantive due process. Additionally, the Court opined that the constitutional ban on double jeopardy and ex post facto lawmaking does not apply because the procedures are civil, not criminal.
Kansas v Crane (2002).13 The Court upheld the Kansas Sexually Violent Predator Act, stating that mental illness and dangerousness are essential elements to meet the criteria for civil commitment. The Court added that proof of partial (not total) “volitional impairment” is all that is required to meet the threshold of sexual dangerousness.
McKune v Lile (2002).14 The Court ruled that a policy requiring participation in polygraph testing, which would lead to the disclosure of sexual crimes (even those that have not been prosecuted), does not violate an individual’s Fifth Amendment rights because it serves a vital penological purpose.
Adam Walsh Child Protection and Safety Act of 200616; United States v Comstock (2010).15 This act and subsequent case reinforced the federal government’s right to civilly commit sexually dangerous persons approaching the end of their prison sentences.
Continue to: What is requiried for civil commitment?
What is required for civil commitment?
SVP laws require 4 conditions to be met for the civil commitment of sexual offenders (Table 417). In criteria 1, “charges” is a key word, because this allows individuals found Not Guilty by Reason of Insanity or Incompetent to Stand Trial to be civilly committed. Criteria 2 defines “mental abnormality” as a “congenital or acquired condition affecting the emotional or volitional capacity which predisposes the person to commit criminal sexual acts in a degree constituting such person a menace to the health and safety of others.”18 This is a broad definition, and allows individuals with personality disorders to be civilly committed (although most sexual offenders are committed for having a paraphilic disorder). To determine risk, various actuarial instruments are used to assess for sexually violent recidivism, including (but not limited to) the Static-99R, Sexual Violence Risk-20, and the Sex Offender Risk Appraisal Guide.19
Although the percentages vary, sex offenders rarely are civilly committed following their criminal sentence. In California, approximately 1.5% of sex offenders are civilly committed.17 The standard of proof for civil commitment varies by state between “clear and convincing evidence” and “beyond a reasonable doubt.” As sex offenders approach the end of their sentence, sexually violent offenders are identified to the general population and referred for a psychiatric evaluation. If the individual meets the 4 criteria for commitment (Table 417), their case is sent to the prosecuting attorney’s office. If accepted, the court holds a probable cause hearing, followed by a full trial.
Pornography and sex offenders
Pornography has long been considered a risk factor for sexual offending, and the role of pornography in influencing sexual behavior has drawn recent interest in research towards predicting future offenses. However, a 2019 systematic review by Mellor et al20 on the relationship between pornography and sexual offending suggested that early exposure to pornography is not a risk factor for sexual offending, nor is the risk of offending increased shortly after pornography exposure. Additionally, pornography use did not predict recidivism in low-risk sexual offenders, but did in high-risk offenders.
The use of child pornography presents a set of new risk factors. Prohibited by federal and state law, child pornography is defined under Section 2256 of Title 18, United States Code, as any visual depiction of sexually explicit conduct involving a minor (someone <age 18). Visual depictions include photographs, videos, digital or computer-generated images indistinguishable from an actual minor, and images created to depict a minor. The law does not require an image of a child engaging in sexual activity for the image to be characterized as child pornography. Offenders are also commonly charged with the distribution of child pornography. A conviction of child pornography possession carries a 15- to 30-year sentence, and distribution carries a 5- to 20-year sentence.21 The individual must also file for the sex offender registry, which may restrict their employment and place of residency.
It is unclear what percentage of individuals charged with child pornography have a history of prior sexual offenses. Numerous studies suggest there is a low risk of online offenders without prior offenses becoming contact offenders. Characteristics of online-only offenders include being White, a single male, age 20 to 30, well-educated, and employed, and having antisocial traits and a history of sexual deviancy.22 Contact offenders tend to be married with easy access to children, unemployed, uneducated, and to have a history of mental illness or criminal offenses.22
Continue to: Recidivism and treatment
Recidivism and treatment
The recidivism rate among sexual offenders averages 13.7% at 3- to 6-year follow-up,although rates vary by type of sexual offense.23 Individuals who committed rape have the highest rate of recidivism, while those who engaged in incest have the lowest. Three key points about sexual offender recidivism are:
- it declines over time and with increased age.
- sexual offenders are more like to commit a nonsexual offense than a sexual offense.
- sexual offenders who have undergone treatment are 26.3% less likely to reoffend.23
Although there is no standard of treatment, current interventions include external control, reduction of sexual drive, treatment of comorbid conditions, cognitive-behavioral therapy (CBT), and dynamic psychotherapy. External control relies on an outside entity that affects the individual’s behavior. For sexually deviant behaviors, simply making the act illegal or involving the law may inhibit many individuals from acting on a thought. Additional external control may include pharmacotherapy, which ranges from nonhormonal options such as selective serotonin reuptake inhibitors (SSRIs) to hormonal options. Therapy tends to focus on social skills training, sex education, cognitive restructuring, and identifying triggers, as well as victim empathy. The best indicators for successful treatment include an absence of comorbidities, increased age, and adult interpersonal relationships.24
Treatment choice may be predicated on the severity of the paraphilia. Psychotherapy alone is recommended for individuals able to maintain functioning if it does not affect their conventional sexual activity. Common treatment for low-risk individuals is psychotherapy and an SSRI. As risk increases, so does treatment with pharmacologic agents. Beyond SSRIs, moderate offenders may be treated with an SSRI and a low-dose antiandrogen. This is escalated in high-risk violent offenders to long-acting gonadotropin-releasing hormone analogs and synthetic steroidal analogs.25
An evolving class of disorders
With the evolution and accessibility of pornography, uncommon sexual practices have become more common, gaining notoriety and increased social acceptance. As a result, mental health professionals may be tasked with evaluating patients for possible paraphilic disorders. A common misconception is that individuals with sexually deviant thoughts, sexual offenders, and patients with paraphilic disorders are all the same. However, more commonly, sexual offenders do not have a paraphilic disorder. In the case of SVPs, outside of imprisonment, civil commitment remains a consideration for possible treatment. To meet the threshold of civil commitment, a sexual offender must have a “mental abnormality,” which is most commonly a paraphilic disorder. The treatment of paraphilic disorders remains a difficult task and includes a mixture of psychotherapy and medication options.
CASE CONTINUED
Mr. J begins weekly CBT to gain control of his voyeuristic fantasies without impacting his conventional sexual activity and desire. He responds well to treatment, and after 18 months, begins a typical sexual relationship with a woman. Although his voyeuristic thoughts remain, the urge to act on the thoughts decreases as Mr. J develops coping mechanisms. He does not require pharmacologic treatment.
Bottom Line
Individuals with paraphilic disorders are too often portrayed as sexual deviants or criminals. Psychiatrists must review each case with careful consideration of individual risk factors, such as the patient’s sexual history, to evaluate potential treatment options while determining if they pose a threat to the public.
Related Resources
- Sorrentino R, Abramowitz J. Minor-attracted persons: a neglected population. Current Psychiatry. 2021;20(7):21-27. doi:10.12788/cp.0149
- Berlin FS. Paraphilic disorders: a better understanding. Current Psychiatry. 2019;18(4):22-26,28.
Mr. J, age 23, presents to an outpatient mental health clinic for treatment of anxiety. He has no psychiatric history, is dressed neatly, and recently finished graduate school with a degree in accounting. Mr. J is reserved during the initial psychiatric evaluation and provides only basic facts about his developmental history.
Mr. J comes from a middle-class household with no history of trauma or substance use. He does not report any symptoms consistent with anxiety, but discloses a history of sexual preoccupations. Mr. J says that during adolescence he developed a predilection for observing others engage in sexual activity. In his late teens, he began following couples to their homes in the hope of witnessing sexual intimacy. In the rare instance that his voyeuristic fantasy comes to fruition, he masturbates and achieves sexual gratification he is incapable of experiencing otherwise. Mr. J notes that he has not yet been caught, but he expresses concern and embarrassment related to his actions. He concludes by noting that he seeks help because the frequency of this behavior has steadily increased.
How would you treat Mr. J? Where does the line exist between a normophilic sexual interest, fantasy or urge, and a paraphilia? Does Mr. J qualify as a sexually violent predator?
From The Rocky Horror Picture Show to Fifty Shades of Grey, sensationalized portrayals of sexual deviancy have long been present in popular culture. The continued popularity of serial killers years after their crimes seems in part related to the extreme sexual torture their victims often endure. However, a sexual offense does not always qualify as a paraphilic disorder.1 In fact, many individuals with paraphilic disorders never engage in illegal activity. Additionally, experiencing sexually deviant thoughts alone does not qualify as a paraphilic disorder.1
A thorough psychiatric evaluation should include a discussion of the patient’s sexual history, including the potential of sexual dysfunction and abnormal desires or behaviors. Most individuals with sexual dysfunction do not have a paraphilic disorder.2 DSM-5 and ICD-11 classify sexual dysfunction and paraphilic disorders in different categories. However, previous editions grouped them together under sexual and gender identity disorders. Individuals with paraphilic disorders may not originally present to the outpatient setting for a paraphilic disorder, but instead may first seek treatment for a more common comorbid disorder, such as a mood disorder, personality disorder, or substance use disorder.3
Diagnostically speaking, if individuals do not experience distress or issues with functionality and lack legal charges (suggesting that they have not violated the rights of others), they are categorized as having an atypical sexual interest but do not necessarily meet the criteria for a disorder.4 This article provides an overview of paraphilic disorders as well as forensic considerations when examining individuals with sexually deviant behaviors.
Overview of paraphilic disorders
DSM-5 characterizes a paraphilic disorder as “recurrent, intense sexually arousing fantasies, sexual urges, or behaviors generally involving nonhuman objects or nonconsenting partners for at least 6 months. The individual must have acted on the thought and/or it caused clinically significant distress or impairment in social, occupational, or other important areas of functioning.” DSM-5 outlines 9 categories of paraphilic disorders, which are described in Table 1.4,5
Continue to: Paraphilic disorders are more common...
Paraphilic disorders are more common in men than in women; the 2 most prevalent are voyeuristic disorder and frotteuristic disorder.6 The incidence of paraphilias in the general outpatient setting varies by disorder. Approximately 45% of individuals with pedophilic disorder seek treatment, whereas only 1% of individuals with zoophilia seek treatment.6 The incidence of paraphilic acts also varies drastically; individuals with exhibitionistic disorder engaged in an average of 50 acts vs only 3 for individuals with sexual sadism.6 Not all individuals with paraphilic disorders commit crimes. Approximately 58% of sexual offenders meet the criteria for a paraphilic disorder, but antisocial personality disorder is a far more common diagnosis.7
Sexual psychopath statutes: Phase 1
In 1937, Michigan became the first state to enact sexual psychopath statutes, allowing for indeterminate sentencing and the civil commitment/treatment of sex offenders with repeated convictions. By the 1970s, more than 30 states had enacted similar statutes. It was not until 1967, in Specht v Patterson,8 that the United States Supreme Court unanimously ruled that the Fourteenth Amendment Due Process Clause was violated when Francis Eddie Specht faced life in prison following his conviction for indecent liberties under the Colorado Sex Offenders Act.
Specht was convicted in 1959 for indecent liberties after pleading guilty to enticing a child younger than age 16 into an office and engaging in sexual activities with them. At the time of Specht’s conviction, the crime of indecent liberties carried a punishment of 10 years. However, Specht was sentenced under the Sexual Offenders Act, which allowed for an indeterminate sentence of 1 day to life in prison. The Supreme Court noted that Specht was denied the right to be present with counsel, to confront the evidence against him, to cross-examine witnesses, and to offer his own evidence, which was a violation of his constitutionally guaranteed Fourteenth Amendment right to Procedural Due Process. The decision led most states to repeal early sexual psychopath statutes.8
Sexually violent predator laws: Phase 2
After early sexual psychopath statutes were repealed, many states pushed to update sex offender laws in response to the Earl Shriner case.9 In 1989, Shriner was released from prison after serving a 10-year sentence for sexually assaulting 2 teenage girls. At the time, he did not meet the criteria for civil commitment in the state of Washington. On the day he was released, Shriner cut off a young boy’s penis and left him to die. Washington subsequently became the first of many states to enact sexually violent predator (SVP) laws. Table 210 shows states and districts that have SVP civil commitment laws.
A series of United States Supreme Court cases solidified current sexual offender civil commitment laws (Table 38,11-15).
Continue to: Allen v Illinois
Allen v Illinois (1986).11 The Court ruled that forcing an individual to participate in a psychiatric evaluation prior to a sexually dangerous person’s commitment hearing did not violate the individual’s Fifth Amendment right against self-incrimination because the purpose of the evaluation was to provide treatment, not punishment.
Kansas v Hendricks (1997).12 The Court upheld that the Kansas Sexually Violent Predator Act was constitutional and noted that the use of the broad term “mental abnormality” (in lieu of the more specific term “mental illness”) does not violate an individual’s Fourteenth Amendment right to substantive due process. Additionally, the Court opined that the constitutional ban on double jeopardy and ex post facto lawmaking does not apply because the procedures are civil, not criminal.
Kansas v Crane (2002).13 The Court upheld the Kansas Sexually Violent Predator Act, stating that mental illness and dangerousness are essential elements to meet the criteria for civil commitment. The Court added that proof of partial (not total) “volitional impairment” is all that is required to meet the threshold of sexual dangerousness.
McKune v Lile (2002).14 The Court ruled that a policy requiring participation in polygraph testing, which would lead to the disclosure of sexual crimes (even those that have not been prosecuted), does not violate an individual’s Fifth Amendment rights because it serves a vital penological purpose.
Adam Walsh Child Protection and Safety Act of 200616; United States v Comstock (2010).15 This act and subsequent case reinforced the federal government’s right to civilly commit sexually dangerous persons approaching the end of their prison sentences.
Continue to: What is requiried for civil commitment?
What is required for civil commitment?
SVP laws require 4 conditions to be met for the civil commitment of sexual offenders (Table 417). In criteria 1, “charges” is a key word, because this allows individuals found Not Guilty by Reason of Insanity or Incompetent to Stand Trial to be civilly committed. Criteria 2 defines “mental abnormality” as a “congenital or acquired condition affecting the emotional or volitional capacity which predisposes the person to commit criminal sexual acts in a degree constituting such person a menace to the health and safety of others.”18 This is a broad definition, and allows individuals with personality disorders to be civilly committed (although most sexual offenders are committed for having a paraphilic disorder). To determine risk, various actuarial instruments are used to assess for sexually violent recidivism, including (but not limited to) the Static-99R, Sexual Violence Risk-20, and the Sex Offender Risk Appraisal Guide.19
Although the percentages vary, sex offenders rarely are civilly committed following their criminal sentence. In California, approximately 1.5% of sex offenders are civilly committed.17 The standard of proof for civil commitment varies by state between “clear and convincing evidence” and “beyond a reasonable doubt.” As sex offenders approach the end of their sentence, sexually violent offenders are identified to the general population and referred for a psychiatric evaluation. If the individual meets the 4 criteria for commitment (Table 417), their case is sent to the prosecuting attorney’s office. If accepted, the court holds a probable cause hearing, followed by a full trial.
Pornography and sex offenders
Pornography has long been considered a risk factor for sexual offending, and the role of pornography in influencing sexual behavior has drawn recent interest in research towards predicting future offenses. However, a 2019 systematic review by Mellor et al20 on the relationship between pornography and sexual offending suggested that early exposure to pornography is not a risk factor for sexual offending, nor is the risk of offending increased shortly after pornography exposure. Additionally, pornography use did not predict recidivism in low-risk sexual offenders, but did in high-risk offenders.
The use of child pornography presents a set of new risk factors. Prohibited by federal and state law, child pornography is defined under Section 2256 of Title 18, United States Code, as any visual depiction of sexually explicit conduct involving a minor (someone <age 18). Visual depictions include photographs, videos, digital or computer-generated images indistinguishable from an actual minor, and images created to depict a minor. The law does not require an image of a child engaging in sexual activity for the image to be characterized as child pornography. Offenders are also commonly charged with the distribution of child pornography. A conviction of child pornography possession carries a 15- to 30-year sentence, and distribution carries a 5- to 20-year sentence.21 The individual must also file for the sex offender registry, which may restrict their employment and place of residency.
It is unclear what percentage of individuals charged with child pornography have a history of prior sexual offenses. Numerous studies suggest there is a low risk of online offenders without prior offenses becoming contact offenders. Characteristics of online-only offenders include being White, a single male, age 20 to 30, well-educated, and employed, and having antisocial traits and a history of sexual deviancy.22 Contact offenders tend to be married with easy access to children, unemployed, uneducated, and to have a history of mental illness or criminal offenses.22
Continue to: Recidivism and treatment
Recidivism and treatment
The recidivism rate among sexual offenders averages 13.7% at 3- to 6-year follow-up,although rates vary by type of sexual offense.23 Individuals who committed rape have the highest rate of recidivism, while those who engaged in incest have the lowest. Three key points about sexual offender recidivism are:
- it declines over time and with increased age.
- sexual offenders are more like to commit a nonsexual offense than a sexual offense.
- sexual offenders who have undergone treatment are 26.3% less likely to reoffend.23
Although there is no standard of treatment, current interventions include external control, reduction of sexual drive, treatment of comorbid conditions, cognitive-behavioral therapy (CBT), and dynamic psychotherapy. External control relies on an outside entity that affects the individual’s behavior. For sexually deviant behaviors, simply making the act illegal or involving the law may inhibit many individuals from acting on a thought. Additional external control may include pharmacotherapy, which ranges from nonhormonal options such as selective serotonin reuptake inhibitors (SSRIs) to hormonal options. Therapy tends to focus on social skills training, sex education, cognitive restructuring, and identifying triggers, as well as victim empathy. The best indicators for successful treatment include an absence of comorbidities, increased age, and adult interpersonal relationships.24
Treatment choice may be predicated on the severity of the paraphilia. Psychotherapy alone is recommended for individuals able to maintain functioning if it does not affect their conventional sexual activity. Common treatment for low-risk individuals is psychotherapy and an SSRI. As risk increases, so does treatment with pharmacologic agents. Beyond SSRIs, moderate offenders may be treated with an SSRI and a low-dose antiandrogen. This is escalated in high-risk violent offenders to long-acting gonadotropin-releasing hormone analogs and synthetic steroidal analogs.25
An evolving class of disorders
With the evolution and accessibility of pornography, uncommon sexual practices have become more common, gaining notoriety and increased social acceptance. As a result, mental health professionals may be tasked with evaluating patients for possible paraphilic disorders. A common misconception is that individuals with sexually deviant thoughts, sexual offenders, and patients with paraphilic disorders are all the same. However, more commonly, sexual offenders do not have a paraphilic disorder. In the case of SVPs, outside of imprisonment, civil commitment remains a consideration for possible treatment. To meet the threshold of civil commitment, a sexual offender must have a “mental abnormality,” which is most commonly a paraphilic disorder. The treatment of paraphilic disorders remains a difficult task and includes a mixture of psychotherapy and medication options.
CASE CONTINUED
Mr. J begins weekly CBT to gain control of his voyeuristic fantasies without impacting his conventional sexual activity and desire. He responds well to treatment, and after 18 months, begins a typical sexual relationship with a woman. Although his voyeuristic thoughts remain, the urge to act on the thoughts decreases as Mr. J develops coping mechanisms. He does not require pharmacologic treatment.
Bottom Line
Individuals with paraphilic disorders are too often portrayed as sexual deviants or criminals. Psychiatrists must review each case with careful consideration of individual risk factors, such as the patient’s sexual history, to evaluate potential treatment options while determining if they pose a threat to the public.
Related Resources
- Sorrentino R, Abramowitz J. Minor-attracted persons: a neglected population. Current Psychiatry. 2021;20(7):21-27. doi:10.12788/cp.0149
- Berlin FS. Paraphilic disorders: a better understanding. Current Psychiatry. 2019;18(4):22-26,28.
1. Federoff JP. The paraphilias. In: Gelder MG, Andreasen NC, López-Ibor JJ Jr, Geddes JR, eds. New Oxford Textbook of Psychiatry. 2nd ed. Oxford University Press; 2012:832-842.
2. Grubin D. Medical models and interventions in sexual deviance. In: Laws R, O’Donohue WT, eds. Sexual Deviance: Theory, Assessment and Treatment. 2nd ed. Guilford Press; 2008:594-610.
3. Guidry LL, Saleh FM. Clinical considerations of paraphilic sex offenders with comorbid psychiatric conditions. Sex Addict Compulsivity. 2004;11(1-2):21-34.
4. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013.
5. Balon R. Paraphilic disorders. In: Roberts LW, Hales RE, Yudofsky SC, eds. The American Psychiatric Association Publishing Textbook of Psychiatry. 7th ed. American Psychiatric Association Publishing; 2019:749-770.
6. Sadock BJ, Sadock VA, Ruiz P. Paraphilic disorders. Kaplan and Sadock’s Synopsis of Psychiatry. 11th ed. Wolters Kluwer; 2015:593-599.
7. First MB, Halon RL. Use of DSM paraphilia diagnosis in sexually violent predator commitment cases. J Am Acad Psychiatry Law. 2008;36(4):443-454.
8. Specht v Patterson, 386 US 605 (1967).
9. Ra EP. The civil confinement of sexual predators: a delicate balance. J Civ Rts Econ Dev. 2007;22(1):335-372.
10. Felthous AR, Ko J. Sexually violent predator law in the United States. East Asian Arch Psychiatry. 2018;28(4):159-173.
11. Allen v Illinois, 478 US 364 (1986).
12. Kansas v Hendricks, 521 US 346 (1997).
13. Kansas v Crane, 534 US 407 (2002).
14. McKune v Lile, 536 US 24 (2002).
15. United States v Comstock, 560 US 126 (2010).
16. Adam Walsh Child Protection and Safety Act of 2006, HR 4472, 109th Cong (2006). Accessed April 25, 2022. https://www.congress.gov/bill/109th-congress/house-bill/4472
17. Tucker DE, Brakel SJ. Sexually violent predator laws. In: Rosner R, Scott C, eds. Principles and Practice of Forensic Psychiatry. 3rd ed. CRC Press; 2017:823-831.
18. Wash. Rev. Code. Ann. §71.09.020(8)
19. Bradford J, de Amorim Levin GV, Booth BD, et al. Forensic assessment of sex offenders. In: Gold LH, Frierson RL, eds. The American Psychiatric Association Publishing Textbook of Forensic Psychiatry. 3rd ed. American Psychiatric Association Publishing; 2017:382-397.
20. Mellor E, Duff S. The use of pornography and the relationship between pornography exposure and sexual offending in males: a systematic review. Aggress Violent Beh. 2019;46:116-126.
21. Failure To Register, 18 USC § 2250 (2012). Accessed April 25, 2022. https://www.govinfo.gov/app/details/USCODE-2011-title18/USCODE-2011-title18-partI-chap109B-sec2250
22. Hirschtritt ME, Tucker D, Binder RL. Risk assessment of online child sexual exploitation offenders. J Am Acad Psychiatry Law. 2019;47(2):155-164.
23. Blasko BL. Overview of sexual offender typologies, recidivism, and treatment. In: Jeglic EL, Calkins C, eds. Sexual Violence: Evidence Based Policy and Prevention. Springer; 2016:11-29.
24. Thibaut F, Cosyns P, Fedoroff JP, et al; WFSBP Task Force on Paraphilias. The World Federation of Societies of Biological Psychiatry (WFSBP) 2020 guidelines for the pharmacological treatment of paraphilic disorders. World J Biol Psychiatry. 2020;21(6):412-490.
25. Holoyda B. Paraphilias: from diagnosis to treatment. Psychiatric Times. 2019;36(12).
1. Federoff JP. The paraphilias. In: Gelder MG, Andreasen NC, López-Ibor JJ Jr, Geddes JR, eds. New Oxford Textbook of Psychiatry. 2nd ed. Oxford University Press; 2012:832-842.
2. Grubin D. Medical models and interventions in sexual deviance. In: Laws R, O’Donohue WT, eds. Sexual Deviance: Theory, Assessment and Treatment. 2nd ed. Guilford Press; 2008:594-610.
3. Guidry LL, Saleh FM. Clinical considerations of paraphilic sex offenders with comorbid psychiatric conditions. Sex Addict Compulsivity. 2004;11(1-2):21-34.
4. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013.
5. Balon R. Paraphilic disorders. In: Roberts LW, Hales RE, Yudofsky SC, eds. The American Psychiatric Association Publishing Textbook of Psychiatry. 7th ed. American Psychiatric Association Publishing; 2019:749-770.
6. Sadock BJ, Sadock VA, Ruiz P. Paraphilic disorders. Kaplan and Sadock’s Synopsis of Psychiatry. 11th ed. Wolters Kluwer; 2015:593-599.
7. First MB, Halon RL. Use of DSM paraphilia diagnosis in sexually violent predator commitment cases. J Am Acad Psychiatry Law. 2008;36(4):443-454.
8. Specht v Patterson, 386 US 605 (1967).
9. Ra EP. The civil confinement of sexual predators: a delicate balance. J Civ Rts Econ Dev. 2007;22(1):335-372.
10. Felthous AR, Ko J. Sexually violent predator law in the United States. East Asian Arch Psychiatry. 2018;28(4):159-173.
11. Allen v Illinois, 478 US 364 (1986).
12. Kansas v Hendricks, 521 US 346 (1997).
13. Kansas v Crane, 534 US 407 (2002).
14. McKune v Lile, 536 US 24 (2002).
15. United States v Comstock, 560 US 126 (2010).
16. Adam Walsh Child Protection and Safety Act of 2006, HR 4472, 109th Cong (2006). Accessed April 25, 2022. https://www.congress.gov/bill/109th-congress/house-bill/4472
17. Tucker DE, Brakel SJ. Sexually violent predator laws. In: Rosner R, Scott C, eds. Principles and Practice of Forensic Psychiatry. 3rd ed. CRC Press; 2017:823-831.
18. Wash. Rev. Code. Ann. §71.09.020(8)
19. Bradford J, de Amorim Levin GV, Booth BD, et al. Forensic assessment of sex offenders. In: Gold LH, Frierson RL, eds. The American Psychiatric Association Publishing Textbook of Forensic Psychiatry. 3rd ed. American Psychiatric Association Publishing; 2017:382-397.
20. Mellor E, Duff S. The use of pornography and the relationship between pornography exposure and sexual offending in males: a systematic review. Aggress Violent Beh. 2019;46:116-126.
21. Failure To Register, 18 USC § 2250 (2012). Accessed April 25, 2022. https://www.govinfo.gov/app/details/USCODE-2011-title18/USCODE-2011-title18-partI-chap109B-sec2250
22. Hirschtritt ME, Tucker D, Binder RL. Risk assessment of online child sexual exploitation offenders. J Am Acad Psychiatry Law. 2019;47(2):155-164.
23. Blasko BL. Overview of sexual offender typologies, recidivism, and treatment. In: Jeglic EL, Calkins C, eds. Sexual Violence: Evidence Based Policy and Prevention. Springer; 2016:11-29.
24. Thibaut F, Cosyns P, Fedoroff JP, et al; WFSBP Task Force on Paraphilias. The World Federation of Societies of Biological Psychiatry (WFSBP) 2020 guidelines for the pharmacological treatment of paraphilic disorders. World J Biol Psychiatry. 2020;21(6):412-490.
25. Holoyda B. Paraphilias: from diagnosis to treatment. Psychiatric Times. 2019;36(12).