User login
Reducing Lost-to-Follow-Up Rates in Patients Discharged from an Early Psychosis Intervention Program
From the Early Psychosis Intervention Program, Institute of Mental Health, Singapore.
Abstract
- Objective: To develop and apply interventions to reduce lost-to-follow-up rates in patients discharged from an early psychosis intervention program.
- Methods: A team comprising clinical staff, case managers, and patients was formed to carry out a clinical practice improvement project. Tools such as brainstorming and root cause analysis were used to derive causes of patient loss to follow-up and interventions to address them were implemented. Plan, Do, Study, and Act cycles were used to evaluate the effectiveness of identified interventions.
- Results: After the 3 interventions were implemented, there was a decrease in the default rate, and the target default rate of 0% was achieved in less than 6 months.
- Conclusion: Easily implemented program changes led to rapid and sustained improvement in reducing lost-to-follow-up rates in patients discharged from an early psychosis intervention program.
Key words: Transfusion; red blood cells; plasma; platelets; veterans.
Psychosis is a mental illness in which affected individuals lose contact with reality. The lifetime prevalence of all psychotic disorders is 3.06% [1]. The typical symptoms consist of hallucinations, delusions, disorganized speech and thinking and negative symptoms (apathy, avolition, alogia, affective flattening, and anhedonia). Treatment is primarily with antipsychotics and psychological and social therapies.
The key to better prognosis is shortening the duration of untreated psychoses (DUP), defined as the period of time between the onset of psychosis and initiation of adequate treatment [2]. Longer DUP is one of the poorer prognostic factors in the outcome of first episode psychosis patients [3]. Over the past 2 decades, there has been considerable interest in developing and implementing specialized treatment programs for first episode psychosis [4], and early intervention is now a well-established therapeutic approach [5]. Early intervention has 2 elements that are distinct from standard care: early detection and phase-specific treatment (phase-specific treatment is a psychological, social, or physical treatment developed, or modified, specifically for use with people at an early stage of the illness). It is not only the initial care that is important, but regular follow up in the stable phase is necessary to reduce chances of relapse.
The Early Psychosis Intervention Programme (EPIP) in Singapore is a national program whose mission is early detection of young people with early psychosis or at risk of developing a psychotic illness and engagement with these individuals and families with the aim of providing accessible, empowering, individualized, evidence-based care in a least restrictive environment. The program was initiated in April 2001 under the auspices of the Ministry of Health, Singapore. EPIP has a multidisciplinary team of doctors, case managers, occupational therapists, psychologists, family therapists, social workers, and nurses to provide a comprehensive and personalized client-centered service across inpatient, outpatient, and community settings. The program spans 3 years and has 3 phases, beginning with acute intervention, followed by the stabilization phase, and then the stable phase, which focuses on relapse prevention, healthy lifestyle, stress management and plan for transition to downstream care. The frequency of visits and interaction with the team is tailored to suit individual patient needs and phase of care and can range from every day to once every 3 months. Following the 3-year program, clients are discharged from EPIP to continuity care (community psychiatry teams).
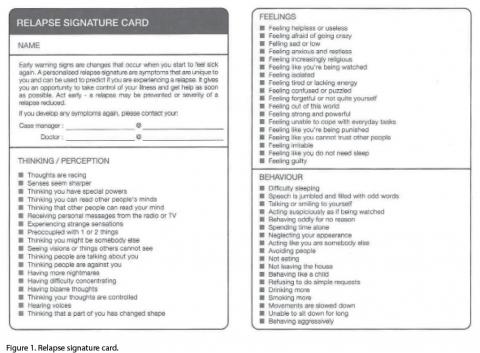
The relapse signature card was used every 2 months in the last 6 months during the period that the improvement project was ongoing. As it was found effective, now we use it every 6 months until 30 months and then every 2 months until conclusion of the 3-year program.
In addition, an appreciation card (Figure 2) was designed that is given to patients who keep their first downstream appointment. The card highlights independence and responsibility for one’s own care.
3. Provide a designated contact person
To ensure a smooth transition to the new service, we provided a designated person to contact for continuity care. Arrangement was made to transfer care to a specific community team of specific doctors and case managers, and their hospital contact details were provided on a card that was given to patients. Of the 8 patients who were transferred, 1 defaulted, 1 went overseas, 1 followed up with a private psychiatrist and the remaining 5 came for their first visit appointments.
Results
shown).
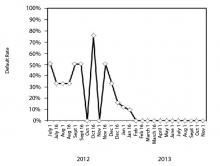
Figure 3. Run chart showing percentage of patients who failed to attend their first appointment with continuity care following transfer out of the program. Pre-intervention, default rates ranged from 9% to 75%. In the first 2 months after all the interventions were instituted (Dec 1 2012–March 1 2013), 2 patients defaulted, after which the default rate decreased to 0%.
Discussion
Making 3 small changes in our early psychosis intervention program led to rewarding gains in improving our patients’ follow-up with continuity care and the changes have become part of our standard operating procedure. In reviewing our processes to identify the root causes for loss of patients to follow-up, we found that obtaining the patient’s perspective was invaluable. It was interesting to learn that the word “discharge” might be impacting the way patients thought about follow-up after completion of the early intervention program. The interventions have become part of our standard operating procedure and we continue to audit the results every month to ensure that 0% default is being maintained. We are also looking into improving out psychoeducational materials for patients and caregivers and using more visual and interactive materials.
Corresponding author: Basu Sutapa, MD, Institute of Mental Health, Buangkok Green Medical Park, 10 Buangkok View, Singapore, S539747, Sutapa_Basu@imh.co.sg.
Financial disclosures: None.
1. Yung AR, Yuen HP, McGorry PD, et al. Mapping the onset of psychosis: the Comprehensive Assessment of At-Risk Mental States. Aust NZJ Psychiatry 2005;39:964–71.
2. Chang WC, Chan GH, Jim OT, et al. Optimal duration of an early intervention programme for first-episode psychosis: randomised controlled trial. Br J Psychiatry. 2015;206:
492–500.
3. Koch A, Gillis LS. Non-attendance of psychiatric outpatients. S Afr Med J 1991;80:289–91.
4. Mueser KT, Penn DL, Addington J, et al. The NAVIGATE Program for first-episode psychosis: rationale, overview, and description of psychosocial components. Psychiatr Serv 2015;66:680–90.
5. Marshall M, Rathbone J. Early intervention for psychosis. Cochrane Database Syst Rev 2011;(6):CD004718.
6. Mitchell AJ, Selmes T. Why don’t patients attend their appointments? Maintaining engagement with psychiatric services. Adv Psychiatr Treat 2007;13:423–34.
7. Magnes RM. Outpatient appointments: a necessary evil? A literature review and survey of patient attendance records. Psychiatr Bull 2008;32:458–60.
8. Appleby L, Shaw J, Amos T, et al. Suicide within 12 months of contact with mental health services: national clinical survey. Br Med J 1999;318:1235–39.
9. Chen A. Noncompliance in community psychiatry: a review of clinical interventions. Hosp Community Psychiatry 1991;
42:282–7.
10. Killaspy H, Banerjee S, King M, et al. Prospective controlled study of psychiatric outpatient nonattendance: characteristics and outcome. Br J Psych 2000;176:160–5.
11. Nelson EA, Maruish ME, Axler JL. Effects of discharge planning and compliance with outpatient appointments on readmission rates. Psychiatr Serv 2000;51:885–9.
12. Gutiérrez-Maldonado J, Caqueo-Urízar A, Kavanagh D. Burden of care and general health in families of patients with schizophrenia. Soc Psychiatr Epidemiol 2005;40:899–904.
13. Skarsholm H, Stoevring H, Nielsen B. Effect of a system-oriented intervention on compliance problems in schizophrenia: a pragmatic controlled trial. Schiz Res Treat 2014;
2014:789403.
14. The Clinical Practice Improvement Programme (CPIP), Institute of Healthcare Quality, National Healthcare Group 2002.
From the Early Psychosis Intervention Program, Institute of Mental Health, Singapore.
Abstract
- Objective: To develop and apply interventions to reduce lost-to-follow-up rates in patients discharged from an early psychosis intervention program.
- Methods: A team comprising clinical staff, case managers, and patients was formed to carry out a clinical practice improvement project. Tools such as brainstorming and root cause analysis were used to derive causes of patient loss to follow-up and interventions to address them were implemented. Plan, Do, Study, and Act cycles were used to evaluate the effectiveness of identified interventions.
- Results: After the 3 interventions were implemented, there was a decrease in the default rate, and the target default rate of 0% was achieved in less than 6 months.
- Conclusion: Easily implemented program changes led to rapid and sustained improvement in reducing lost-to-follow-up rates in patients discharged from an early psychosis intervention program.
Key words: Transfusion; red blood cells; plasma; platelets; veterans.
Psychosis is a mental illness in which affected individuals lose contact with reality. The lifetime prevalence of all psychotic disorders is 3.06% [1]. The typical symptoms consist of hallucinations, delusions, disorganized speech and thinking and negative symptoms (apathy, avolition, alogia, affective flattening, and anhedonia). Treatment is primarily with antipsychotics and psychological and social therapies.
The key to better prognosis is shortening the duration of untreated psychoses (DUP), defined as the period of time between the onset of psychosis and initiation of adequate treatment [2]. Longer DUP is one of the poorer prognostic factors in the outcome of first episode psychosis patients [3]. Over the past 2 decades, there has been considerable interest in developing and implementing specialized treatment programs for first episode psychosis [4], and early intervention is now a well-established therapeutic approach [5]. Early intervention has 2 elements that are distinct from standard care: early detection and phase-specific treatment (phase-specific treatment is a psychological, social, or physical treatment developed, or modified, specifically for use with people at an early stage of the illness). It is not only the initial care that is important, but regular follow up in the stable phase is necessary to reduce chances of relapse.
The Early Psychosis Intervention Programme (EPIP) in Singapore is a national program whose mission is early detection of young people with early psychosis or at risk of developing a psychotic illness and engagement with these individuals and families with the aim of providing accessible, empowering, individualized, evidence-based care in a least restrictive environment. The program was initiated in April 2001 under the auspices of the Ministry of Health, Singapore. EPIP has a multidisciplinary team of doctors, case managers, occupational therapists, psychologists, family therapists, social workers, and nurses to provide a comprehensive and personalized client-centered service across inpatient, outpatient, and community settings. The program spans 3 years and has 3 phases, beginning with acute intervention, followed by the stabilization phase, and then the stable phase, which focuses on relapse prevention, healthy lifestyle, stress management and plan for transition to downstream care. The frequency of visits and interaction with the team is tailored to suit individual patient needs and phase of care and can range from every day to once every 3 months. Following the 3-year program, clients are discharged from EPIP to continuity care (community psychiatry teams).
The relapse signature card was used every 2 months in the last 6 months during the period that the improvement project was ongoing. As it was found effective, now we use it every 6 months until 30 months and then every 2 months until conclusion of the 3-year program.
In addition, an appreciation card (Figure 2) was designed that is given to patients who keep their first downstream appointment. The card highlights independence and responsibility for one’s own care.
3. Provide a designated contact person
To ensure a smooth transition to the new service, we provided a designated person to contact for continuity care. Arrangement was made to transfer care to a specific community team of specific doctors and case managers, and their hospital contact details were provided on a card that was given to patients. Of the 8 patients who were transferred, 1 defaulted, 1 went overseas, 1 followed up with a private psychiatrist and the remaining 5 came for their first visit appointments.
Results
shown).
Figure 3. Run chart showing percentage of patients who failed to attend their first appointment with continuity care following transfer out of the program. Pre-intervention, default rates ranged from 9% to 75%. In the first 2 months after all the interventions were instituted (Dec 1 2012–March 1 2013), 2 patients defaulted, after which the default rate decreased to 0%.
Discussion
Making 3 small changes in our early psychosis intervention program led to rewarding gains in improving our patients’ follow-up with continuity care and the changes have become part of our standard operating procedure. In reviewing our processes to identify the root causes for loss of patients to follow-up, we found that obtaining the patient’s perspective was invaluable. It was interesting to learn that the word “discharge” might be impacting the way patients thought about follow-up after completion of the early intervention program. The interventions have become part of our standard operating procedure and we continue to audit the results every month to ensure that 0% default is being maintained. We are also looking into improving out psychoeducational materials for patients and caregivers and using more visual and interactive materials.
Corresponding author: Basu Sutapa, MD, Institute of Mental Health, Buangkok Green Medical Park, 10 Buangkok View, Singapore, S539747, Sutapa_Basu@imh.co.sg.
Financial disclosures: None.
From the Early Psychosis Intervention Program, Institute of Mental Health, Singapore.
Abstract
- Objective: To develop and apply interventions to reduce lost-to-follow-up rates in patients discharged from an early psychosis intervention program.
- Methods: A team comprising clinical staff, case managers, and patients was formed to carry out a clinical practice improvement project. Tools such as brainstorming and root cause analysis were used to derive causes of patient loss to follow-up and interventions to address them were implemented. Plan, Do, Study, and Act cycles were used to evaluate the effectiveness of identified interventions.
- Results: After the 3 interventions were implemented, there was a decrease in the default rate, and the target default rate of 0% was achieved in less than 6 months.
- Conclusion: Easily implemented program changes led to rapid and sustained improvement in reducing lost-to-follow-up rates in patients discharged from an early psychosis intervention program.
Key words: Transfusion; red blood cells; plasma; platelets; veterans.
Psychosis is a mental illness in which affected individuals lose contact with reality. The lifetime prevalence of all psychotic disorders is 3.06% [1]. The typical symptoms consist of hallucinations, delusions, disorganized speech and thinking and negative symptoms (apathy, avolition, alogia, affective flattening, and anhedonia). Treatment is primarily with antipsychotics and psychological and social therapies.
The key to better prognosis is shortening the duration of untreated psychoses (DUP), defined as the period of time between the onset of psychosis and initiation of adequate treatment [2]. Longer DUP is one of the poorer prognostic factors in the outcome of first episode psychosis patients [3]. Over the past 2 decades, there has been considerable interest in developing and implementing specialized treatment programs for first episode psychosis [4], and early intervention is now a well-established therapeutic approach [5]. Early intervention has 2 elements that are distinct from standard care: early detection and phase-specific treatment (phase-specific treatment is a psychological, social, or physical treatment developed, or modified, specifically for use with people at an early stage of the illness). It is not only the initial care that is important, but regular follow up in the stable phase is necessary to reduce chances of relapse.
The Early Psychosis Intervention Programme (EPIP) in Singapore is a national program whose mission is early detection of young people with early psychosis or at risk of developing a psychotic illness and engagement with these individuals and families with the aim of providing accessible, empowering, individualized, evidence-based care in a least restrictive environment. The program was initiated in April 2001 under the auspices of the Ministry of Health, Singapore. EPIP has a multidisciplinary team of doctors, case managers, occupational therapists, psychologists, family therapists, social workers, and nurses to provide a comprehensive and personalized client-centered service across inpatient, outpatient, and community settings. The program spans 3 years and has 3 phases, beginning with acute intervention, followed by the stabilization phase, and then the stable phase, which focuses on relapse prevention, healthy lifestyle, stress management and plan for transition to downstream care. The frequency of visits and interaction with the team is tailored to suit individual patient needs and phase of care and can range from every day to once every 3 months. Following the 3-year program, clients are discharged from EPIP to continuity care (community psychiatry teams).
The relapse signature card was used every 2 months in the last 6 months during the period that the improvement project was ongoing. As it was found effective, now we use it every 6 months until 30 months and then every 2 months until conclusion of the 3-year program.
In addition, an appreciation card (Figure 2) was designed that is given to patients who keep their first downstream appointment. The card highlights independence and responsibility for one’s own care.
3. Provide a designated contact person
To ensure a smooth transition to the new service, we provided a designated person to contact for continuity care. Arrangement was made to transfer care to a specific community team of specific doctors and case managers, and their hospital contact details were provided on a card that was given to patients. Of the 8 patients who were transferred, 1 defaulted, 1 went overseas, 1 followed up with a private psychiatrist and the remaining 5 came for their first visit appointments.
Results
shown).
Figure 3. Run chart showing percentage of patients who failed to attend their first appointment with continuity care following transfer out of the program. Pre-intervention, default rates ranged from 9% to 75%. In the first 2 months after all the interventions were instituted (Dec 1 2012–March 1 2013), 2 patients defaulted, after which the default rate decreased to 0%.
Discussion
Making 3 small changes in our early psychosis intervention program led to rewarding gains in improving our patients’ follow-up with continuity care and the changes have become part of our standard operating procedure. In reviewing our processes to identify the root causes for loss of patients to follow-up, we found that obtaining the patient’s perspective was invaluable. It was interesting to learn that the word “discharge” might be impacting the way patients thought about follow-up after completion of the early intervention program. The interventions have become part of our standard operating procedure and we continue to audit the results every month to ensure that 0% default is being maintained. We are also looking into improving out psychoeducational materials for patients and caregivers and using more visual and interactive materials.
Corresponding author: Basu Sutapa, MD, Institute of Mental Health, Buangkok Green Medical Park, 10 Buangkok View, Singapore, S539747, Sutapa_Basu@imh.co.sg.
Financial disclosures: None.
1. Yung AR, Yuen HP, McGorry PD, et al. Mapping the onset of psychosis: the Comprehensive Assessment of At-Risk Mental States. Aust NZJ Psychiatry 2005;39:964–71.
2. Chang WC, Chan GH, Jim OT, et al. Optimal duration of an early intervention programme for first-episode psychosis: randomised controlled trial. Br J Psychiatry. 2015;206:
492–500.
3. Koch A, Gillis LS. Non-attendance of psychiatric outpatients. S Afr Med J 1991;80:289–91.
4. Mueser KT, Penn DL, Addington J, et al. The NAVIGATE Program for first-episode psychosis: rationale, overview, and description of psychosocial components. Psychiatr Serv 2015;66:680–90.
5. Marshall M, Rathbone J. Early intervention for psychosis. Cochrane Database Syst Rev 2011;(6):CD004718.
6. Mitchell AJ, Selmes T. Why don’t patients attend their appointments? Maintaining engagement with psychiatric services. Adv Psychiatr Treat 2007;13:423–34.
7. Magnes RM. Outpatient appointments: a necessary evil? A literature review and survey of patient attendance records. Psychiatr Bull 2008;32:458–60.
8. Appleby L, Shaw J, Amos T, et al. Suicide within 12 months of contact with mental health services: national clinical survey. Br Med J 1999;318:1235–39.
9. Chen A. Noncompliance in community psychiatry: a review of clinical interventions. Hosp Community Psychiatry 1991;
42:282–7.
10. Killaspy H, Banerjee S, King M, et al. Prospective controlled study of psychiatric outpatient nonattendance: characteristics and outcome. Br J Psych 2000;176:160–5.
11. Nelson EA, Maruish ME, Axler JL. Effects of discharge planning and compliance with outpatient appointments on readmission rates. Psychiatr Serv 2000;51:885–9.
12. Gutiérrez-Maldonado J, Caqueo-Urízar A, Kavanagh D. Burden of care and general health in families of patients with schizophrenia. Soc Psychiatr Epidemiol 2005;40:899–904.
13. Skarsholm H, Stoevring H, Nielsen B. Effect of a system-oriented intervention on compliance problems in schizophrenia: a pragmatic controlled trial. Schiz Res Treat 2014;
2014:789403.
14. The Clinical Practice Improvement Programme (CPIP), Institute of Healthcare Quality, National Healthcare Group 2002.
1. Yung AR, Yuen HP, McGorry PD, et al. Mapping the onset of psychosis: the Comprehensive Assessment of At-Risk Mental States. Aust NZJ Psychiatry 2005;39:964–71.
2. Chang WC, Chan GH, Jim OT, et al. Optimal duration of an early intervention programme for first-episode psychosis: randomised controlled trial. Br J Psychiatry. 2015;206:
492–500.
3. Koch A, Gillis LS. Non-attendance of psychiatric outpatients. S Afr Med J 1991;80:289–91.
4. Mueser KT, Penn DL, Addington J, et al. The NAVIGATE Program for first-episode psychosis: rationale, overview, and description of psychosocial components. Psychiatr Serv 2015;66:680–90.
5. Marshall M, Rathbone J. Early intervention for psychosis. Cochrane Database Syst Rev 2011;(6):CD004718.
6. Mitchell AJ, Selmes T. Why don’t patients attend their appointments? Maintaining engagement with psychiatric services. Adv Psychiatr Treat 2007;13:423–34.
7. Magnes RM. Outpatient appointments: a necessary evil? A literature review and survey of patient attendance records. Psychiatr Bull 2008;32:458–60.
8. Appleby L, Shaw J, Amos T, et al. Suicide within 12 months of contact with mental health services: national clinical survey. Br Med J 1999;318:1235–39.
9. Chen A. Noncompliance in community psychiatry: a review of clinical interventions. Hosp Community Psychiatry 1991;
42:282–7.
10. Killaspy H, Banerjee S, King M, et al. Prospective controlled study of psychiatric outpatient nonattendance: characteristics and outcome. Br J Psych 2000;176:160–5.
11. Nelson EA, Maruish ME, Axler JL. Effects of discharge planning and compliance with outpatient appointments on readmission rates. Psychiatr Serv 2000;51:885–9.
12. Gutiérrez-Maldonado J, Caqueo-Urízar A, Kavanagh D. Burden of care and general health in families of patients with schizophrenia. Soc Psychiatr Epidemiol 2005;40:899–904.
13. Skarsholm H, Stoevring H, Nielsen B. Effect of a system-oriented intervention on compliance problems in schizophrenia: a pragmatic controlled trial. Schiz Res Treat 2014;
2014:789403.
14. The Clinical Practice Improvement Programme (CPIP), Institute of Healthcare Quality, National Healthcare Group 2002.