User login
Playing by the Rules: Using Decision Rules Wisely Part 2, Nontraumatic Conditions
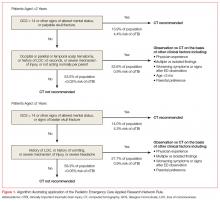
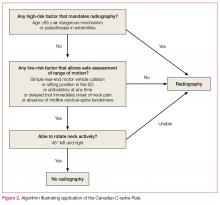
In this second part of “Playing by the Rules,” we will examine validated clinical decision rules that assist emergency physicians (EPs) in the diagnosis and treatment of nontraumatic conditions. Most trauma rules seek to answer a yes or no question regarding the utility of testing for specific disease states when the diagnosis is not clinically apparent.
For example, the Canadian CT Head Rule describes a number of conditions that, if met, can predict the absence of traumatic lesions requiring neurosurgical intervention in the alert patient with head injury, and thus obviate the need for imaging in those instances. In contrast, many medical rules are actually risk stratification scales for treatment and diagnosis, categorizing patients into low- to high-risk groups based on clinical factors. While traumatic conditions are linked to a specific inciting event or “trauma,” medical diseases may have multiple causative factors or may be delayed in presentation to the emergency department (ED), which subsequently increases the complexity of these decision instruments.
Rather than an exhaustive list of all clinical decision rules or risk stratification scales relevant to emergency medicine, this installment will provide EPs with a review of common instruments and the evidence behind them.
Central Nervous System
Ottawa Subarachnoid Hemorrhage Rule
The Ottawa Subarachnoid Hemorrhage Rule offers guidance for diagnosing atraumatic subarachnoid hemorrhage (SAH) in alert, neurologically intact adult patients presenting to the ED with a headache reaching maximal intensity within 1 hour of onset. The rule states that if none of the following conditions are present, then the diagnosis of SAH can be excluded without further testing:
Symptom of neck pain or stiffness
Age greater than 40 years old
Witnessed loss of consciousness
Onset during exertion
Thunderclap headache with peak pain instantly
Limited neck flexion on exam
The validation study prospectively enrolled 1153 adults of whom 67 had a positive workup for SAH (defined as subarachnoid blood visible on noncontrast CT scan of the head, xanthochromia of cerebrospinal fluid on visual inspection, or the presence of >1 million erythrocytes in the final tube of cerebrospinal fluid with an aneurysm or arteriovenous malformation confirmed on cerebral angiography).1 Of note, patients with prior history of cerebral aneurysm or SAH were excluded, as were patients with recurrent headaches similar to the presenting complaint, patients with focal neurologic deficits or papilledema, or patients with a history of brain neoplasm, ventricular shunt, or hydrocephalus. The authors found that the rule was 100% sensitive and 13% specific for detecting SAH, with a kappa of 0.82, which suggests good interrater reliability.1
Comment: It is important to note that the authors excluded patients with a history of cerebral aneurysm or prior SAH, and therefore the rule should not be applied to these patients in clinical practice. The utility of this rule is somewhat limited secondary to the age cutoff, as the incidence of aneurysmal SAH increases considerably after the fifth decade of life.2 Ultimately, this rule—combined with the authors’ previous work showing that CT performed within 6 hours of headache onset can rule out SAH—provides a powerful diagnostic tool for EPs considering SAH in the ED.3
ABCD2 Score
The ABCD2 score was developed to identify transient ischemic attack (TIA) patients at risk for early stroke, and thus inform decisions regarding admission and resource utilization in the ED and outpatient clinic setting.4 The score was created by combining elements of two previously existing rules, the California and the ABCD scales. Patients presenting with TIA symptoms are assigned points based on:
Age: 1 point if ≥ 60 years
Blood Pressure: 1 point if ≥ 140/90
Clinical Deficit: 2 points for unilateral weakness, 1 point for speech impairment without unilateral weakness
Duration: 2 points for ≥ 60 minutes, 1 point for 10 to 59 minutes
Diabetes: 1 point if diabetic
The greater the number of points, the higher the risk for imminent stroke, from low (0-3 points) to moderate (4-5 points) to high (6-7 points). The initial retrospective internal validation study found that the low, moderate, and high groups correlated to 7-day stroke risk of 1.2%, 5.9%, and 11.7%, respectively. Subsequently, the ABCD2 score was rapidly incorporated into institutional and national protocols for assessing risk for stroke and featured prominently in the 2009 American Heart Association guidelines on TIA, which recommend hospitalization for a score of 3 or greater.4,5
More recently, a multicenter prospective external validation study of more than 2000 TIA patients found that using the American Heart Association recommended cutoff of 3 or greater resulted in a sensitivity of 94.7% for detecting those patients who sustained a stroke within 7 days, but a specificity of only 12.5%.6 The investigators concluded that a specificity this low would require “almost all” of the TIA patients in their cohort (87.6%) to be admitted to the hospital—even though only 3.2% of their patients had a stroke within 90 days.6 Even when examined at other cutoff scores, the investigators found the ABCD2 score to have poor accuracy.6
Comment: Decreasing resource utilization is a laudable goal, but it does not appear that the ABCD2 score provides much guidance on which TIA patients can safely go home. Moreover, the increasing availability of advanced imaging and tele-neurology consultation in the ED have changed the landscape of TIA and stroke care. Many EPs have since argued that the ABCD2 score adds little to their evaluation.7
Abdomen
Alvarado Score
There are multiple clinical prediction rules for appendicitis. Among the most commonly utilized by EPs and surgical consultants are the Alvarado score and the Appendicitis Inflammatory Response Score. The Alvarado score was derived in 1986 based on a retrospective review of 305 abdominal pain patients of whom 227 (aged 4 to 80 years) had appendicitis.8 Factors were identified and weighted, which can be recalled through the mnemonic MANTRELS:
Migration of pain to the right lower quadrant: 1 point
Anorexia or acetone in urine: 1 point
Nausea or vomiting: 1 point
Tenderness in the right lower quadrant: 2 points
Rebound tenderness: 1 point
Elevation of the temperature > 37.3°C: 1 point
Leukocytosis >10K X 109/L: 2 points
Shift to the left of neutrophils (>75%): 1 point
The original article posited that a score of 5 or 6 was “compatible” with the diagnosis of acute appendicitis—necessitating further observation for possible appendicitis—and that higher scores indicated an increasing probability of disease.8 Of note, the rule has also been adapted for clinical settings where differentials are not easily obtainable with the left shift criterion removed; this is known as the modified Alvarado score and calculated out at a maximum of 9.9
Since the original Alvarado study was published, multiple small studies have attempted to validate or otherwise retrospectively assess the utility of this rule. A frequently cited systematic review of 42 prospective and retrospective studies by Ohle et al found that a score of <5 showed a sensitivity of 99% overall (96% in men, 99% in women, and 99% in children) for ruling out admission/observation of patient with suspected appendicitis, though the specificity for ruling in the diagnosis at scores 7 and higher was only 81% overall.10
However, a more recent prospective observational study of adult abdominal pain patients presenting to large American urban EDs found the modified Alvarado rule at cutoff levels of 3, 4, and 5 had sensitivities of only 72%, 55%, and 36%, respectively, of ruling out the diagnosis.11 In comparison, the study found that physicians’ clinical judgement of appendicitis being the first or second most likely diagnosis had a sensitivity of 93% for predicting appendicitis.11
Comment: The Alvarado score was developed to help rule out and rule in the diagnosis of appendicitis. However, with the increasing availability of CT scanning in EDs, the diagnostic pathway in unclear cases has shifted from admission/observation to CT scanning, which has the benefit of elucidating other pathology as well. The utility of the Alvarado rule has been called into question. Ultimately, there is data in support of the Alvarado rule from older articles and studies in resource-poor environments, and newer studies may reflect less rigorous application of the rule when CT scanning is the default clinical pathway. Further studies that focus specifically on the Alvarado score as a rule out test to decrease CT utilization may be instructive.
Appendicitis Inflammatory Response (AIR) score
The appendicitis inflammatory response (AIR) score was derived in a cohort of 316 patients and validated on a sample of 229 adults and children with suspected appendicitis.12 The authors specifically sought to create a rule that outperformed the Alvarado score; the criteria are:
Vomiting: 1 point
Right iliac fossa pain: 1 point
Rebound tenderness: 1 point for light, 2 for medium, 3 for strong
Temperature >38.5°C: 1 point
Polymorphonuclear leukocytes: 1 point for 70%-84%, 2 for 85% or greater
White blood cell count: 1 point for 10,000-14,900, 2 for 15,000 or greater
C-reactive protein level (mg/dL): 1 point for 10-49, 2 for 50 or greater
Patients with a score of 0-4 were classified as low risk, with recommendation for outpatient follow-up if general condition unchanged; a score of 5-8 as indeterminate risk, with recommendation for active observation with serial exams, imaging, or diagnostic laparoscopy; or a score of 9-12 as high risk, with recommendation for surgical exploration.12 In the validation cohort, the investigators found an AIR score or Alvarado score greater than 4 to have, respectively, 96% or 97% sensitivity and 73% or 61% specificity for detecting appendicitis.12 A high score of greater than 8 on either the AIR or Alvarado had respectively 37% or 28% sensitivity but specificity of 99% for detecting appendicitis with either instrument.12
In an external validation study, the AIR and Alvarado scores were calculated on a series of 941 patients (aged 1 to 97 years) being evaluated for possible appendicitis; 201 patients were younger than 18.13 At a cutoff of greater than 4, the sensitivity and specificity were found to be 93% and 85% for the AIR and 90% and 55% for Alvarado.13 In a cohort of 182 patients (aged 4 to 75 years), a score of 4 or greater on the AIR and Alvarado was found to have comparable sensitivity to that of a senior surgical consultant for detecting appendicitis—with sensitivities of 94%, 93%, and 90% respectively.14 Subsequently, the original investigators undertook a large multicenter implementation study of the AIR at 24 hospitals of patients (aged 5 to 96 years) with suspected appendicitis. As compared to the pre-implementation group, using AIR to categorize patients as low risk resulted in significantly fewer imaging studies, admissions, and surgical explorations.15
Comment: The AIR has the benefit of recent prospective studies that assess performance of the rule in settings that mirror the practice environments of most EPs today. The classification of rebound tenderness as light, medium, or strong may be difficult to ascertain. Ultimately, reductions in imaging, admissions, and surgical explorations are important goals and EPs might benefit from using this rule to guide imaging.
CHEST
HEART Score
The increasingly popular HEART score, first developed by physicians in the Netherlands in 2008, seeks to risk-stratify patients presenting to the ED with suspected cardiac chest pain without ST-elevation myocardial infarction (STEMI). It scores patients 0 to 2 on 5 different characteristics (with a total scored of 10 possible points):
History: 2 points for highly suspicious, 1 point for moderately suspicious
EKG: 2 points for significant ST deviation, 1 point for nonspecific repolarization disturbance
Age: 2 points for age 65 years or greater, 1 point for age 45-64 years
Risk Factors: 2 points for 3 or more risk factors or history of atherosclerotic disease, 1 point for 1 to 2 risk factors
Troponin: 2 points for troponin value >3 times the normal limit, 1 point for value 1-3 times the normal limit.
The authors developed these 5 categories “based on clinical experience and current medical literature,” and then applied the rule to 122 chest pain patients in the ED, finding a higher incidence of major adverse coronary events (MACE) with increasing score: 2.5% for low risk score of 0-3, 20.3% for intermediate risk score of 4-6, and 72.7% for score 7 or higher.16 The score has been retrospectively and prospectively validated.17,18 In a study of 2440 patients, the low risk group had a MACE of 1.7%, and the score had a c-statistic of 0.83, outperforming Thrombolysis in Myocardial Infarction (TIMI) and GRACE c-statistics of 0.75 and 0.70, respectively.18 In 2013, investigators calculated the HEART score on a multinational database of 2906 chest pain patients, finding a negative predictive value of 98.3% for MACE with HEART score less than or equal to 3.19
In the United States, Mahler et al have produced a series of 3 articles validating the HEART score and demonstrating its use in reducing cardiac testing and length of stay. In 1070 patients admitted to their observation unit, who were deemed low risk by physician assessment and TIMI <2, a score of less than or equal to 3 had a negative predictive value of 99.4% for MACE; the inclusion of serial troponins resulted in sensitivity of 100%, specificity of 83.1%, and negative predictive value of 100%.20 The team then conducted a secondary analysis of chest pain patients enrolled in a large multicenter trial (MIDAS) and compared HEART score, the North American Chest Pain Rule, and unstructured clinical assessment.21 Both rules had high sensitivities, but the HEART score identified 20% of patients suitable for early discharge, as compared to 4% for the North American Chest Pain Rule.21 Finally, Mahler’s team performed a randomized control trial of 282 patients investigating whether the HEART score with serial troponins compared with usual care could safely reduce cardiac testing.22 The HEART pathway resulted in an absolute reduction of 12.1% in cardiac testing, and median reduction in length of stay by 12 hours, with no missed MACE in discharged patients.22
Most recently, a stepped-wedge, cluster randomized trial across 9 hospitals published in 2017 investigated the utility of the HEART score. Despite enrolling only 3648 patients out of the statistically required sample size of 6600, they found that the HEART score was not inferior to usual care and there was no significant difference in median length of stay, but health care resources were typically lower in the HEART score group.23
Comment: While derived in a less conventional manner, the HEART score has held up in several validation studies and appears poised to safely decrease health care costs and increase ED efficiency and throughput. As more US EDs look to adopt high sensitivity troponin biomarkers, prospective studies will be needed to determine the role of the HEART score in this setting.
Thrombolysis in Myocardial Infarction (TIMI) score
The Thrombolysis in Myocardial Infarction (TIMI) score was developed in 2000 as a tool to risk-stratify patients with a diagnosis of unstable angina (UA) and non–ST-elevation myocardial infarction (NSTEMI). The score was derived from 1 arm (2047 patients) of a study comparing heparin with enoxaparin for treatment of NSTEMI, and validated in the other 3 arms of the study (5124 patients). Multivariate logistic regression was used to develop 7 variables of equal weight:
Age greater than or equal to 65yo
Three or more cardiac risk factors
Known coronary artery disease (with stenosis greater than or equal to 50%)
Aspirin use in the past 7 days
Severe angina (2 or more episodes in the past 24 hours)
EKG ST changes greater than or equal to 0.5 mm
Positive serum cardiac biomarkers
The investigators found that with a higher score, there was progressive increase in adverse cardiac outcomes, with a c-statistic of 0.65.24 This score was subsequently validated across several existing databases evaluating various therapeutic interventions for UA/NSTEMI and remained statistically significant, with increasing risk for MI and mortality with increasing score.25,26
Given the success in predicting patient outcomes and identifying patients who could benefit from more aggressive care, the TIMI risk score was then applied to unselected ED chest pain patients. In a secondary analysis of a prospective observational cohort of 3929 patient visits, the TIMI score correlated to the risk for adverse outcomes, with a risk of 2.1% at score 0.27
In a second prospective observational cohort of 1458 patient visits, a score of 0 correlated to a 1.7% incidence of adverse outcomes.28 In 2008, Body et al sought to increase the relative weight of EKG and biomarker factors to 5 (instead of 1) in a study of 796 patients, positing that these factors have more importance in the ED setting.29 Comparing the modified TIMI to the original, the modified instrument improved the area under curve (AUC) from 0.77 to 0.87.29 In follow-up validation studies, the modified score has an improved AUC, but the incidence of adverse outcomes at score 0 remains at about 2% for both modified and original score.30,31
In 2010, Hess et al performed a systematic review and meta-analysis of the studies that prospectively validated the TIMI score. They evaluated 10 validation studies, encompassing 17,265 patients across 5 countries, and found a strong linear relation between the TIMI score and adverse cardiac events.32 At TIMI score of 0, the incidence of cardiac events was 1.8%, with sensitivity of 97.2% and specificity of 25%. Subsequently, the ADAPT trial designed a diagnostic protocol consisting of TIMI risk assessment, EKG, and 0- and 2-hour troponin I biomarkers to find ED patients eligible for safe, early discharge.33 Of the 1975 patients, 20% were classified as low risk and eligible for early discharge, in that they had TIMI score of 0, a non-ischemic ECG, and negative troponins. Only one patient had a MACE at 30 days, giving the protocol a sensitivity of 99.7%, specificity of 23.4%, and negative predictive value of 99.7%.33
As the TIMI and HEART scores are both used to evaluate ED chest pain patients, several studies have sought to compare them. In 2015, Cartlon et al published a comparison of 5 established risk scores and 2 troponin assays in 963 patients: modified Goldman, TIMI, GRACE, HEART, and Vancouver Chest Pain Rule in combination with troponin T and I.34 The investigators found that a negative troponin T plus either TIMI score of 0 or a HEART score ≤3 gave a negative predictive value of greater than 99.5% with more than 30% of patients able to be discharged safely.34 In 2017, a comparison of the GRACE, HEART, and TIMI scores in 1833 chest pain patients found the HEART score identified more low risk patients than either of its comparators and had the highest AUC at 0.86.35 Other trials have similarly found HEART outperforming TIMI.36
Comment: The TIMI score was not specifically designed for ED use but has been adapted to serve this purpose. To the EP assessing the undifferentiated chest pain patient, the TIMI score uses clinical variables that may seem curious (eg, aspirin use) or impossible for EPs to ascertain (eg, presence or degree of stenosis). Even for patients with a score of 0, the risk for adverse outcomes remains stubbornly at the 2% level, similar to the original low risk HEART score findings.
Wells’ Criteria for Pulmonary Embolism
The diagnosis of pulmonary embolism (PE) is often challenging, requiring the use of multiple ED resources for timely diagnosis, and is therefore well suited for clinical decision instruments. The Wells’ Criteria were derived from a cohort of 1260 patients using logistic regression to identify 7 significant variables:
Clinical signs and symptoms of deep vein thrombosis (DVT): 3
PE is the most likely diagnosis: 3
Heart rate >100: 1.5
Immobilization or surgery in the previous 4 weeks: 1.5
Previously diagnosed DVT or PE: 1.5
Hemoptysis: 1
Malignancy with treatment within 6 months or palliative: 1
The investigators specifically linked the use of their instrument to the D-dimer assay, using their score to determine pretest probability and seeking to exclude the diagnosis in patients with low pretest probability and negative D-dimer result.37,38 They reported a three-tiered classification, with low risk at a score less than 2, moderate risk at scores from 2-6, and high risk at scores greater than 6. The risk for PE with a low risk score coupled with a negative D-dimer result were 1.5% and 2.7% in the derivation and validation cohorts. Using a two-tiered classification of PE unlikely at scores less than or equal to 4 and PE likely at scores 5 or greater, a PE unlikely score and a negative D-dimer had a 2.2% and 1.7% risk in the derivation and validation cohorts.
A subsequent study by Wells et al on 930 ED patients using the score plus D-dimer found a negative predictive value of 99.5% for a low risk score and a negative D-dimer.39 This allowed for reduced imaging in 53% of patients.39 Another external validation study found acceptable interrater agreement between physicians for the Wells’ score at kappa 0.62 for the three-tiered system and 0.7 for the two-tiered system.40 The Wells’ Criteria has been compared against the Geneva score with receiver operating characteristic curve analysis showing no difference between the two rules.41 In a large cohort of 3306 patients being evaluated for PE using the Wells’ score and D-dimer, for the 1028 patients with PE unlikely and a negative D-dimer, there was a 3-month incidence of venous thromboembolism (VTE) of 0.5%—none of which were fatal events.42
Comment: The Wells’ Criteria for pulmonary embolism combined with D-dimer is now the preferred approach for many EPs seeking to risk-stratify their patients for PE. Advances in age-adjusted cutoffs for D-dimer provide additional support for this powerful tool.
Pulmonary Embolism Rule-Out Criteria (PERC)
Given the low specificity of the D-dimer assay for VTE, researchers post–Wells’ Criteria have sought to further reduce unnecessary testing by reassessing the D-dimer’s role in the diagnostic pathway. The PERC rule was designed to reduce D-dimer use—and downstream CT scan testing—in low-risk patients. The investigators derived the rule from a population of patients for whom the pretest probability of PE was less than 15%, seeking a risk for PE less than 2% if the rule was satisfied. Using logistic regression in 3148 ED patients, 8 clinical criteria were obtained:
Age < 50 years Pulse <100
Pulse oximetry >94%
No unilateral leg swelling
No hemoptysis
No recent surgery
No prior PE/DVT
No hormone use
The variables were tested in 1427 low-risk and 382 very-low-risk patients (defined as being evaluated for dyspnea, but not part of the derivation or low-risk validation groups). In the low-risk group, the sensitivity, specificity, and false-negative rate was 96%, 27%, and 1.4% respectively. In the very-low-risk group, the sensitivity, specificity, and false-negative rate was 100%, 15%, and 0% respectively.43 The rule was further validated in a prospective multicenter study of 8138 patients; among patients with pretest probability less than 15% who were PERC negative, 1% had PE/DVT within 45 days.44 The large PERCEPIC trial on 1757 patients found low pretest probability patients who were PERC negative had a false-negative rate of 1.2% and estimated that the use of PERC could decrease the median length of stay in the ED by at least 2 hours.45 The PROPER study, a non-inferiority, crossover cluster-randomized trial in 14 EDs across France, found that use of the PERC rule was not inferior to conventional care and that it was associated with reduced ED length of stay and CT use.45,46
There has been criticism from some European studies that the PERC rule misses too many PEs. A provocatively titled multinational study from Hugli et al examined patients suspected to have PE in Switzerland, France, and Belgium. The investigators applied the PERC rule and then stratified the patients by pretest probability as defined by the Geneva score, which includes many of the same criteria as PERC. They found the PERC rule identified a small proportion of patients with suspected PE as very low risk (13.2%) and that the prevalence of PE among these patients was 5.4%. Critics of this study have noted that the PERC rule was designed to be applied in low-risk patients, not to define the low-risk population.47 Another study examined a retrospective cohort of patients in whom a D-dimer was ordered to exclude PE, and then calculated the Wells’ and PERC score from the medical record. The investigators found that the combination of Wells and PERC missed 2 PEs out of their population of 377 patients.48 However, a subsequent meta-analysis analyzed 11 studies—including the two negative studies—and found a pooled sensitivity of 97%, specificity of 23%, and negative likelihood ratio of 0.18, concluding that when the pretest probability is low, PERC is sensitive enough to exclude D-dimer testing.49
Comment: Given the number of disease states and sampling techniques that can cause nonspecific elevation in D-dimer assay, the PERC rule provides a useful tool in low-risk populations for excluding PE without laboratory testing. The key is applying the rule to the appropriate population, as stratified by gestalt or clinical score.
Infectious Disease
Mortality in Emergency Department Sepsis (MEDS) score
The Mortality in Emergency Department Sepsis (MEDS) score was developed as a risk stratification tool for patients presenting to the ED with concern for sepsis. This score was prospectively derived from a population of 3301 ED patient encounters during which a blood culture was ordered. Charts were reviewed and several data points extracted and analyzed to determine the following univariate predictors of 28-day mortality: terminal illness, tachypnea or hypoxia, septic shock, platelets <150,000/mm3, bands >5%, age >65 years, lower respiratory infection, nursing home residence, and altered mental status. These predictors were assigned point values based on their odds ratios, and points are added to generate a total score. Mortality risk was stratified into groups based on total score, with percentage mortality as follows: score 0-4: 0.9%; 5-7: 2.0%; 8-12: 7.8%; 13-15: 20.2%; >15: 50%. A separate validation cohort had the following mortality rates: score 0-4: 1.1%; 5-7: 4.4%; 8-12: 9.3%; 13-15: 16.1%; >15: 39%.50
The MEDS score was subsequently shown to also be predictive for 1-year mortality as well, with an area under receiver operating curve (AUROC) of 0.76 for 1-year mortality.51 A subsequent study showed similar mortality rates when expanding the patient population to include all patients with systemic inflammatory response syndrome (SIRS), potentially broadening the potential application of MEDS in ED risk stratification.52 However, the score was shown to be less predictive in patients with severe sepsis and septic shock, underestimating mortality in all MEDS score groups.53 Still, the MEDS score was demonstrated in multiple validation studies as a reliable risk stratification tool in patients with suspected infection or SIRS.54,55
Comment: The MEDS score is not as well studied in the literature as the SIRS criteria or QuickSOFA but is a validated risk stratification tool in patients with suspected infection and is ED specific. This tool, similar to Pneumonia Severity Index and CURB-65 (discussed below), can guide management of patients from the ED. Very-low-risk (score 0-4) patients can be treated as outpatients, low risk (score 5-7) patients warranting consideration of a short inpatient stay, and moderate to high risk (>8) requiring inpatient management. At present, there is insufficient evidence regarding the role of the MEDS score to guide inpatient disposition of floor vs. ICU in moderate to high-risk patients.
Pneumonia Severity Index
The Pneumonia Severity Index (PSI) was developed as a tool to predict mortality risk from pneumonia, allowing providers to appropriately manage care for these patients in the hospital or as outpatients. A derivation cohort of 14199 patients was utilized to create a prediction rule in two steps meant to parallel a clinician’s decision-making process. The first step identified a population of patients that were at low risk for death, which were assigned to class I. The second step quantified the risk for death in the remaining patients using weighted factors including demographics, comorbidities, exam findings, and clinical data. In all, 20 variables were used and assigned corresponding points, the sum of which would assign a patient to a particular risk for mortality (class II-V).56
Mortality risk was relatively low for patients in class I and II (0.4 and 0.7%, respectively). Class III carried a mortality risk of 2.8%. Mortality increased with class IV and class V classification: 8.5% and 31.1%, respectively. These data were replicated with a separate validation cohort of 38039 patients, with similar mortality rates in each class. This study concluded with the recommendation that patients diagnosed with pneumonia falling into class I and II mortality risk should be managed as outpatients, possible brief inpatient observation for class III, and class IV and V managed as inpatients.56
Subsequent trials evaluating the utility of the PSI score in the management of patients diagnosed with pneumonia randomized low-risk patients (class I-III PSI) to treatment as outpatients vs inpatients. There were no statistical differences in adverse outcomes (ICU admission, hospital readmission, mortality, complications), with notable improvements in hospital admission rates and patient satisfaction.57,58 A meta-analysis of 6 studies that used a clinical decision tools to identify low-risk patients to treat pneumonia as outpatients showed no significant difference in mortality, patient readmissions, or patient satisfaction. Low-risk patients that required admission often included comorbid illnesses not included in the PSI, inability to take oral medications, barriers to compliance, or hypoxemia.59
Though the PSI has been shown to successfully identify patients at low risk for mortality, it has been less accurate at predicting and stratifying classes of severe pneumonia. A meta-analysis by Loke et al showed that PSI class IV or V had pooled sensitivity of 0.90 and specificity 0.53 for 30-day mortality, which was significantly better than the CURB-65 rule (discussed below).60 However, a subsequent large meta-analysis showed that PSI class IV or V had a sensitivity of 75% and specificity 40% for requiring ICU intervention or admission, which are not sufficient to guide disposition decisions.61
CURB-65
One of the criticisms of PSI included its complexity, with inclusion of 20 factors making it impractical for use as a bedside tool. The CURB-65 score was developed with a similar goal of identifying low-risk patients with pneumonia who would be candidates for outpatient management, but also patients at high risk for mortality or ICU admission. Criteria for severe pneumonia published by the British Thoracic Society include: respiratory rate ≥ 30 breaths/min, diastolic blood pressure ≤60 mmHg, and blood urea nitrogen >7 mmol/L. The presence of 2 criteria was 88% sensitive and 72% specific for mortality or ICU admission.62 The CURB-65 tool was based on these criteria, with the addition of age ≥65 years, which was found to be a separate independent predictor of mortality. Thus, the 5 criteria making up the score are as follows (1 point each, 0-5 total):
Confusion, meaning Mental Test Score ≤8, or disorientation to person, place, or time
Urea >7 mmol/L (>19.6 mg/dL)
Respiratory rate ≥ 30 breaths/minute
Blood pressure (systolic < 90 mmHg or diastolic ≤ 60 mmHg)
Age ≥ 65 years
A score of 0-1 of these criteria characterized low mortality risk (<1.5%) in the test group, a score of 2 was intermediate mortality risk (9.2%), and a score of 3 or more associated with high mortality risk (22%). A score ≥ 2 was 93% sensitive and 49% specific for 30-day mortality.63
A subsequent prospective validation study by Aujesky et al that included 3181 patients with community-acquired pneumonia demonstrated slightly higher mortality rates for each CURB-65 score (0.6%, 3%, 6.1%, 13%, 17%, 43% mortality in scores of 0-5, respectively).64 In particular, the 3% mortality rate in CURB-65 scores of 1 is similar to PSI class III mortality rates, suggesting a lower threshold (CURB-65 ≥1) for consideration of admission for management. Another validation study by Capelastegui et al showed similar mortality rates to the derivation study for specific CURB-65 scores, but noted 53% of patients with a score of 1 also were found to have characteristics that were independent for a poor prognosis, and should be considered in the decision for outpatient or inpatient treatment.65 Furthermore, a recent study found that of patients in the ED with a CURB-65 score of 1, 8% still required critical care intervention.66 Thus, use of CURB-65 in screening for low-risk patients with community-acquired pneumonia is recommended to be limited to scores of 0. However, as with PSI, validation studies have yet to show predictive utility of scores suggesting severe pneumonia (CURB-65 ≥3) in predicting mortality or ICU requirement.60,61
As validation studies have suggested only patients with a CURB-65 score of 0 are screened low risk enough for outpatient treatment, greater weight may be placed on utility of CRB-65 as a tool. This rule, initially proposed in the same study as CURB-65, omits blood urea nitrogen as a factor to only rely on history and physical exam data with a score of 0 indicating low risk.63 In initial derivation and validation studies, this rule demonstrated <1.6% mortality risk with a score of 0, with risk increasing to 4-8.6% in scores of 1.63,65 Multiple studies have compared CRB-65 and CURB-65, with only marginal but not statistically significant improvement in prognostic utility of CURB-65.65,67 A meta-analysis of 1648 patients even showed only 0.5% mortality risk in CRB-65 ≤1; potentially including CRB-65 0-1 as low risk, though, would require further study.68 Although multiple validation studies have also successfully stratified low risk to similar mortality risk (<1.6%), accuracy wanes with higher CRB-65 scores.69
Several studies have directly compared CURB-65 and PSI both in terms of identifying low-risk patients and stratifying disease severity.60,61,64,68,70-72 Multiple studies have shown similar mortality risk in low-risk populations and have demonstrated sensitivities for mortality greater than 96% for CURB-65/CRB-65 = 0 and PSI class I-III, albeit with specificities ranging from 18-65%.64,68,70 In stratifying patients into different levels of severity (ward vs ICU patients), PSI has shown slightly better sensitivity/specificity for mortality and/or ICU intervention, though neither is strong enough to significantly stratify severe pneumonia to serve as tools for directing inpatient management.60,61
Comment: PSI, CRB-65, and CURB-65 have been well validated as screening tools for low-risk patients who should be treated as outpatients (CURB-65 or CRB-65 = 0, PSI class I and II). A moderate-risk population (CURB-65 = 1 or 2, PSI class III) may benefit from treatment as inpatient or outpatient at clinician judgement. Use of these tools for determining disease severity and possible ICU requirement is not as reliable, and other clinical factors should be considered.
Conclusion
This article provides an overview of several common clinical decision instruments and the evidence behind them. Ultimately, many institutions have incorporated clinical decision rules directly into the electronic medical record, and this strategy will not only increase their use, but hopefully collect further data on whether the instruments truly perform better than unstructured clinical judgement.
1. Perry JJ, Sivilotti MLA, Sutherland J, et al. Validation of the Ottawa Subarachnoid Hemorrhage Rule in patients with acute headache. CMAJ. 2017;189(45):E1379-E1385.
2. de Rooij NK, Linn FH, van der Plas JA, Algra A, Rinkel GJ. Incidence of subarachnoid haemorrhage: a systematic review with emphasis on region, age, gender and time trends. J Neurol Neurosurg Psychiatry. 2007;78(12):1365-1372.
3. Perry JJ, Stiell IG, Sivilotti ML, et al. Sensitivity of computed tomography performed within six hours of onset of headache for diagnosis of subarachnoid haemorrhage: prospective cohort study. BMJ. 2011;343:d4277.
4. Johnston SC, Rothwell PM, Nguyen-Huynh MN, et al. Validation and refinement of scores to predict very early stroke risk after transient ischaemic attack. Lancet. 2007;369(9558):283-292.
5. Easton JD, Saver JL, Albers GW, et al. Definition and evaluation of transient ischemic attack: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association Stroke Council; Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; and the Interdisciplinary Council on Peripheral Vascular Disease. The American Academy of Neurology affirms the value of this statement as an educational tool for neurologists. Stroke. 2009;40:2276-2293
6. Perry JJ, Sharma M, Sivilotti ML, et al. Prospective validation of the ABCD2 score for patients in the emergency department with transient ischemic attack. CMAJ. 2011;183(10):1137-1145.
7. Stead LG, Suravaram S, Bellolio MF, et al. An assessment of the incremental value of the ABCD2 score in the emergeny department evaluation of transient ischemic attack. Ann Emerg Med. 2011;57(1):46-51.
8. Alvarado A. A practical score for the early diagnosis of acute appendicitis. Ann Emerg Med. 1986;15(5):557-564.
9. Kalan M, Talbot D, Cunliffe WJ, Rich AJ. Evaluation of the modified Alvarado score in the diagnosis of acute appendicitis: a prospective study. Ann R Coll Surg Engl. 1994;76(6):418-419.
10. Ohle R, O'Reilly F, O'Brien KK, Fahey T, Dimitrov BD. The Alvarado score for predicting acute appendicitis: a systematic review. BMC Med. 2011;9:139.
11. Meltzer AC, Baumann BM, Chen EH, Shofer FS, Mills AM. Poor sensitivity of a modified Alvarado score in adults with suspected appendicitis. Ann Emerg Med. 2013;62(2):126-31.
12. Andersson M, Andersson RE. The appendicitis inflammatory response score: a tool for the diagnosis of acute appendicitis that outperforms the Alvarado score. World J Surg. 2008;32(8):1843-1849.
13. de Castro SM, Ünlü C, Steller EP, van Wagensveld BA, Vrouenraets BC. Evaluation of the appendicitis inflammatory response score for patients with acute appendicitis. World J Surg. 2012;36(7):1540-1545.
14. Kollár D, McCartan DP, Bourke M, Cross KS, Dowdall J. Predicting acute appendicitis? A comparison of the Alvarado score, the Appendicitis Inflammatory Response Score and clinical assessment. World J Surg. 2015;39(1):104-109.
15. Andersson M, Kolodziej B, Andersson RE; STRAPPSCORE Study Group. Randomized clinical trial of Appendicitis Inflammatory Response score-based management of patients with suspected appendicitis. Br J Surg. 2017;104(11):1451-1461.
16. Six AJ, Backus BE, Kelder JC. Chest pain in the emergency room: value of the HEART score. Netherlands Heart J. 2008;16(6):191-196.
17. Backus BE, Six AJ, Kelder JC, et al. Chest Pain in the Emergency Room. A Multicenter Validation of the HEART Score. Crit Pathways Cardiol. 2010;9:164-169.
18. Backus BE, Six AJ, Kelder JC, et al. A prospective validation of the HEART score for chest pain patients at the emergency department. In J Cardiol. 2013;168:2153-2158.
19. Six AJ, Cullen L, Backus BE, et al. The HEART score for the assessment of patients with chest pain in the emergency department. Crit Pathways Cardiol. 2013;12:121-126.
20. Mahler SA, Hiestand BC, Goff DC, Hoekstra JW, Miller CD. Can the HEART score safely reduce stress testing and cardiac imaging in patients at low risk for acute coronary syndrome? Crit Pathw Cardiol. 2011:10(3):128-133.
21. Mahler SA, Miller CD, Hollander JE, et al. Identifying patients for early discharge: performance of decision rules among patients with acute chest pain. Int J Cardiol. 2013;168(2):795-802.
22. Mahler SA, Riley RF, Hiestand BC, et al. The HEART Pathway Randomized Trial: identifying emergency department patients with acute chest pain for early discharge. Circ Cardiovasc Qual Outcomes. 2015;8(2):195-203.
23. Poldervaart JM, Reitsma JB, Backus BE, et al. Effect of using the HEART score in patients with chest pain in the emergency department: a stepped-wedge, cluster randomized trial. Ann Intern Med. 2017;166:687-697.
24. Antman EM, Cohen M, Bernink PJLM, et al. The TIMI risk score for unstable angina/non-ST eevation MI. JAMA. 2000;284:835-842.
25. Scirica BM, Cannon CP, Antman EM, et al. Validation of the Thrombolysis In Myocardial Infarction (TIMI) risk score for unstable angina pectoris and non-ST-elevation myocardial infarction in the TIMI III registry. Am J Cardiol. 2002;90:303-305.
26. Morrow DA, Antman EM, Snapinn SM, McCabe CH, Theroux P, Braunwald E. An integrated clinical approach to predicting the benefit of tirofiban in non-ST elevation acute coronary syndromes. Eur Heart J. 2002;23:223-229.
27. Pollack CV, Sites FD, Shofer FS, Sease KL, Hollander JE. Application of the TIMI risk score for unstable angina and non–ST-elevation acute coronary syndrome to an unselected emergency department chest pain population. Acad Emerg Med. 2006:13(1):13-18.
28. Chase M, Robey JL, Zogby KE, Sease KL, Shofer FS, Hollander JE. Prospective validation of the Thrombolysis in Myocardial Infarction risk score in the emergency department chest pain population. Ann Emerg Med. 2006;48(3):252-259.
29. Body R, Carley S, McDowell G, Ferguson J, Mackway-Jones K. Can a modified thrombolysis in myocardial infarction risk score outperform the original for risk stratifying emergency department patients with chest pain? Emerg Med J. 2009;26:95-99.
30. Hess EP, Perry JJ, Calder LA, et al. Prospective validation of a modified Thrombolysis In Myocardial Infarction risk score in emergency department patients with chest pain and possible acute coronary syndrome. Acad Emerg Med. 2010;17(4):368-375.
31. Macdonald SPJ, Nagree Y, Fatovich DM, ad Brown SGA. Modified TIMI risk score cannot be used to identify low-risk chest pain in the emergency department: a multicenter validation study. Emerg Med J. 2014;31:281-285.
32. Hess EP, Agarwal D, Chandra S, et al. Diagnostic accuracy of the TIMI risk score in patients with chest pain in the emergency department: a meta-analysis. CMAJ. 2010;182(10):1039-1044.
33. Than, M, Cullen L, Aldous S, et al. 2-Hour accelerated diagnostic protocol to assess patients with chest pain symptoms using contemporary troponins as the only biomarker: the ADAPT trial. JACC. 2012;59(23):2091-2098.
34. Carlton EW, Khattab A, Greaves K. Identifying patients suitable for discharge after a single-presentation high-sensitivity Troponin result: a comparison of five established risk scores and two high-sensitivity assays. Ann Emerg Med. 2015;66(6):635-645.
35. Poldervaart JM, Langedijk M, Backus BE, et al. Comparison of the GRACE, HEART and TIMI score to predict major adverse cardiac events in chest pain patients at the emergency department. Int J Cardiol. 2017;227:656-661.
36. Nieuwets A, Poldervaart JM, Reitsma JB, et al. Medical consumption compared for TIMI and HEART score in chest pain patients at the emergency department: a retrospective cost analysis. BMJ Open. 2016;6:e010694.
37. Wells PS, Ginsberg JS, Anderson DR, et al. Use of a clinical model for safe management of patients with suspected pulmonary embolism. Ann Intern Med. 1998;129:997-1005.
38. Wells PS, Anderson DR, Rodger M, et al. Derivation of a simple clinical model to categorize patients’ probability of pulmonary embolism: increasing the model’s utility with the SimpliRED D-dimer. Thromb Haemost. 2000;83(3):416-420.
39. Wells PS, Anderson DR, Rodger M, et al. Excluding pulmonary embolism at the bedside without diagnostic imaging: management of patients with suspected pulmonary embolism presenting to the emergency department by using a simple clinical model and D-dimer. Ann Intern Med. 2001;135:98-107.
40. Wolf SJ, McCubbin TR, Feldhaus KM, Faragher JP, Adcock DM. Prospective validation of Wells’ criteria in the evaluation of patients with suspected pulmonary embolism. Ann Emerg Med. 2004;44:503-510.
41. Chagnon I, Bounameaux H, Aujesky D, et al. Comparison of two clinical prediction rules and implicit assessment among patients with suspected pulmonary embolism. Am J Med. 2002;113:269-275.
42. Christopher Study Investigators. Effectiveness of managing suspected pulmonary embolism using an algorithm combining clinical probability, D-dimer testing, and computed tomography. JAMA. 2006;295:172-179.
43. Kline JA, Mitchell AM, Kabrhel C, Richman PB, Courtney DM. Clinical criteria to prevent unnecessary diagnostic testing in emergency department patients with suspected pulmonary embolism. J Thromb Haemost. 2004;2:1247-1255.
44. Kline JA, Courtney DM, Kabrhel C, et al. Propsective multicenter evaluation of the pulmonary embolism rule-out criteria. J Thromb Haemost. 2008;6:772-780.
45. Penaloza A, Soulie C, Moumneh T, et al. Pulmonary embolism rule-out criteria (PERC) rule in European patients with low implicit clinical probability (PERCEPIC): a multicenter, prospective, observational study. Lancet Haematol. 2017;4:e615-e621.
46. Freund Y, Cachanado M, Aubry A, et al. Effect of the Pulmonary Embolism Rule-Out Criteria on subsequent thromboembolic events among low-risk emergency department patients. The PROPER randomized clinical trial. JAMA. 2018;319(6):559-566.
47. Hugli O, Righini M, Le Gal G, et al. The pulmonary embolism rule-out criteria (PERC) rule does not safely exclude pulmonary embolism. J Thromb Haemost. 2011;9:300-4.
48. Theunissen JMG, Scholing C, van Hasselt WE, van der Maten J, ter Avest E. A retrospective analysis of the combined use of PERC rule and Wells score to exclude pulmonary embolism in the Emergency Department. Emerg Med J. 2016;33:696-701.
49. Singh B, Parsaik AK, Aharwal D, Surana A, Mascarenhas SS, Chandra S. Diagnostic accuracy of Pulmonary Embolism Rule-Out Criteria: a systematic review and meta-analysis. Ann Emerg Med. 2012;59(6):517-520.
50. Shapiro NI, Wolfe RE, Moore RB, Smith E, Burdick E, Bates DW. Mortality in Emergency Department Sepsis (MEDS) score: a prospectively derived and validated clinical prediction rule. Crit Care Med. 2003;31(3):670-675.
51. Shapiro NI, Howell MD, Talmor D, Donnino M, Ngo L, Bates DW. Mortality in Emergency Department Sepsis (MEDS) score predicts 1-year mortality. Crit Care Med. 2007;35(1):192-198.
52. Sankoff JD, Goyal M, Gaieski DF, et al. Validation of the Mortality in Emergency Department Sepsis (MEDS) score in patients with the systemic inflammatory response syndrome (SIRS). Crit Care Med. 2008;36(2):421-26.
53. Jones AE, Saak K, Kline JA. Performance of the Mortality in Emergency Department Sepsis score for predicting hospital mortality among patients with severe sepsis and septic shock. Am J Emerg Med. 2008;26(6):689-692.
54. Carpenter CR., Keim SM, Upadhye S, Nguyen HB. Risk stratification of the potentially septic patient in the emergency department: the Mortality in the Emergency Department Sepsis (MEDS) score. J Emerg Med. 2009;37(3):319-327.
55. Hermans MAW, Leffers P, Jansen LM, Keulemans YC, Stassen PM. The value of the Mortality in Emergency Department Sepsis (MEDS) score, C reactive protein and lactate in predicting 28-day mortality of sepsis in a Dutch emergency department. Emerg Med J. 2012;29(4):295–300.
56. Fine MJ, Auble TE, Yealy DM, et al. A Prediction Rule to Identify Low-Risk Patients with Community Acquired Pneumonia. N Engl J Med. 1997;326(4):243-250.
57. Marrie TJ, Lau CY, Wheeler SL, et al. A controlled trial of a critical pathway for treatment of community-acquired pneumonia. JAMA. 2000;283(6):749-755. doi:10.1001/jama.283.6.749.
58. Carratalà J, Fernandez-Sabe N. Outpatient care compared with hospitalization for community-acquired pneumonia: a randomized trial in low-risk patients . Ann Intern Med. 2005;142:165-172. doi:10.7326/0003-4819-142-3-200502010-00006.
59. Chalmers JD, Akram AR, Hill AT. Increasing outpatient treatment of mild community-acquired pneumonia: Systematic review and meta-analysis. Eur Respir J. 2011;37(4):858-864. doi:10.1183/09031936.00065610.
60. Loke YK, Kwok CS, Niruban A, Myint PK. Value of severity scales in predicting mortality from community-acquired pneumonia: systematic review and meta-analysis. Thorax. 2010;65(10):884-890. doi:10.1136/thx.2009.134072.
61. Marti C, Garin N, Grosgurin O, et al. Prediction of severe community-acquired pneumonia: A systematic review and meta-analysis. Crit Care. 2012;16(4):R141. doi:10.1186/cc11447.
62. Neill AM, Martin IR, Weir R, et al. Community-acquired pneumonia: aetiology and usefulness of severity criteria on admission. Thorax. 1996;51(10):1010-1016. doi:10.1136/thx.51.10.1010.
63. Lim WS, Van Der Eerden MM, Laing R, et al. Defining community acquired pneumonia severity on presentation to hospital: An international derivation and validation study. Thorax. 2003;58(5):377-382. doi:10.1136/thorax.58.5.377.
64. Aujesky D, Auble TE, Yealy DM, et al. Prospective comparison of three validated prediction rules for prognosis in community-acquired pneumonia. Am J Med. 2005;118(4):384-392. doi:10.1016/j.amjmed.2005.01.006.
65. Capelastegui A, España PP, Quintana JM, et al. Validation of a predictive rule for the management of community-acquired pneumonia. Eur Respir J. 2006;27(1):151-157. doi:10.1183/09031936.06.00062505.
66. Ilg A, Moskowitz A, Konanki V, et al. Performance of the CURB-65 score in predicting critical care interventions in patients admitted with community-acquired pneumonia. Ann Emerg Med. 2018. doi:10.1016/j.annemergmed.2018.06.017.
67. Bauer TT, Ewig S, Marre R, Suttorp N, Welte T. CRB-65 predicts death from community-acquired pneumonia. J Intern Med. 2006;260(1):93-101. doi:10.1111/j.1365-2796.2006.01657.x.
68. Akram AR, Chalmers JD, Hill AT. Predicting mortality with severity assessment tools in out-patients with community-acquired pneumonia. QJM. 2011;104(10):871-879. doi:10.1093/qjmed/hcr088.
69. McNally M, Curtain J, O’Brien KK, Dimitrov BD, Fahey T. Validity of British Thoracic Society guidance (the CRB-65 rule) for predicting the severity of pneumonia in general practice: Systematic review and meta-analysis. Br J Gen Pract. 2010;60(579):423-433. doi:10.3399/bjgp10X532422.
70. Shah BA, Ahmed W, Dhobi GN, Shah NN, Khursheed SQ, Haq I. Validity of Pneumonia Severity Index and CURB-65 severity scoring systems in community acquired pneumonia in an Indian Setting. Indian J Chest Dis Allied Sci. 2010;52(1):9-17.
71. Noguchi S, Yatera K, Kawanami T, et al. Pneumonia severity assessment tools for predicting mortality in patients with cealthcare-associated pneumonia: a systematic review and meta-analysis. Respiration. 2017;93(6):441-450. doi:10.1159/000470915.
72. Kolditz M, Braeken D, Ewig S, Rohde G. Severity assessment and the immediate and long-term prognosis in community-acquired pneumonia. Semin Respir Crit Care Med. 2016;37(6):886-896. doi:http://dx.doi.org/10.1055/s-0036-1592127.
In this second part of “Playing by the Rules,” we will examine validated clinical decision rules that assist emergency physicians (EPs) in the diagnosis and treatment of nontraumatic conditions. Most trauma rules seek to answer a yes or no question regarding the utility of testing for specific disease states when the diagnosis is not clinically apparent.
For example, the Canadian CT Head Rule describes a number of conditions that, if met, can predict the absence of traumatic lesions requiring neurosurgical intervention in the alert patient with head injury, and thus obviate the need for imaging in those instances. In contrast, many medical rules are actually risk stratification scales for treatment and diagnosis, categorizing patients into low- to high-risk groups based on clinical factors. While traumatic conditions are linked to a specific inciting event or “trauma,” medical diseases may have multiple causative factors or may be delayed in presentation to the emergency department (ED), which subsequently increases the complexity of these decision instruments.
Rather than an exhaustive list of all clinical decision rules or risk stratification scales relevant to emergency medicine, this installment will provide EPs with a review of common instruments and the evidence behind them.
Central Nervous System
Ottawa Subarachnoid Hemorrhage Rule
The Ottawa Subarachnoid Hemorrhage Rule offers guidance for diagnosing atraumatic subarachnoid hemorrhage (SAH) in alert, neurologically intact adult patients presenting to the ED with a headache reaching maximal intensity within 1 hour of onset. The rule states that if none of the following conditions are present, then the diagnosis of SAH can be excluded without further testing:
Symptom of neck pain or stiffness
Age greater than 40 years old
Witnessed loss of consciousness
Onset during exertion
Thunderclap headache with peak pain instantly
Limited neck flexion on exam
The validation study prospectively enrolled 1153 adults of whom 67 had a positive workup for SAH (defined as subarachnoid blood visible on noncontrast CT scan of the head, xanthochromia of cerebrospinal fluid on visual inspection, or the presence of >1 million erythrocytes in the final tube of cerebrospinal fluid with an aneurysm or arteriovenous malformation confirmed on cerebral angiography).1 Of note, patients with prior history of cerebral aneurysm or SAH were excluded, as were patients with recurrent headaches similar to the presenting complaint, patients with focal neurologic deficits or papilledema, or patients with a history of brain neoplasm, ventricular shunt, or hydrocephalus. The authors found that the rule was 100% sensitive and 13% specific for detecting SAH, with a kappa of 0.82, which suggests good interrater reliability.1
Comment: It is important to note that the authors excluded patients with a history of cerebral aneurysm or prior SAH, and therefore the rule should not be applied to these patients in clinical practice. The utility of this rule is somewhat limited secondary to the age cutoff, as the incidence of aneurysmal SAH increases considerably after the fifth decade of life.2 Ultimately, this rule—combined with the authors’ previous work showing that CT performed within 6 hours of headache onset can rule out SAH—provides a powerful diagnostic tool for EPs considering SAH in the ED.3
ABCD2 Score
The ABCD2 score was developed to identify transient ischemic attack (TIA) patients at risk for early stroke, and thus inform decisions regarding admission and resource utilization in the ED and outpatient clinic setting.4 The score was created by combining elements of two previously existing rules, the California and the ABCD scales. Patients presenting with TIA symptoms are assigned points based on:
Age: 1 point if ≥ 60 years
Blood Pressure: 1 point if ≥ 140/90
Clinical Deficit: 2 points for unilateral weakness, 1 point for speech impairment without unilateral weakness
Duration: 2 points for ≥ 60 minutes, 1 point for 10 to 59 minutes
Diabetes: 1 point if diabetic
The greater the number of points, the higher the risk for imminent stroke, from low (0-3 points) to moderate (4-5 points) to high (6-7 points). The initial retrospective internal validation study found that the low, moderate, and high groups correlated to 7-day stroke risk of 1.2%, 5.9%, and 11.7%, respectively. Subsequently, the ABCD2 score was rapidly incorporated into institutional and national protocols for assessing risk for stroke and featured prominently in the 2009 American Heart Association guidelines on TIA, which recommend hospitalization for a score of 3 or greater.4,5
More recently, a multicenter prospective external validation study of more than 2000 TIA patients found that using the American Heart Association recommended cutoff of 3 or greater resulted in a sensitivity of 94.7% for detecting those patients who sustained a stroke within 7 days, but a specificity of only 12.5%.6 The investigators concluded that a specificity this low would require “almost all” of the TIA patients in their cohort (87.6%) to be admitted to the hospital—even though only 3.2% of their patients had a stroke within 90 days.6 Even when examined at other cutoff scores, the investigators found the ABCD2 score to have poor accuracy.6
Comment: Decreasing resource utilization is a laudable goal, but it does not appear that the ABCD2 score provides much guidance on which TIA patients can safely go home. Moreover, the increasing availability of advanced imaging and tele-neurology consultation in the ED have changed the landscape of TIA and stroke care. Many EPs have since argued that the ABCD2 score adds little to their evaluation.7
Abdomen
Alvarado Score
There are multiple clinical prediction rules for appendicitis. Among the most commonly utilized by EPs and surgical consultants are the Alvarado score and the Appendicitis Inflammatory Response Score. The Alvarado score was derived in 1986 based on a retrospective review of 305 abdominal pain patients of whom 227 (aged 4 to 80 years) had appendicitis.8 Factors were identified and weighted, which can be recalled through the mnemonic MANTRELS:
Migration of pain to the right lower quadrant: 1 point
Anorexia or acetone in urine: 1 point
Nausea or vomiting: 1 point
Tenderness in the right lower quadrant: 2 points
Rebound tenderness: 1 point
Elevation of the temperature > 37.3°C: 1 point
Leukocytosis >10K X 109/L: 2 points
Shift to the left of neutrophils (>75%): 1 point
The original article posited that a score of 5 or 6 was “compatible” with the diagnosis of acute appendicitis—necessitating further observation for possible appendicitis—and that higher scores indicated an increasing probability of disease.8 Of note, the rule has also been adapted for clinical settings where differentials are not easily obtainable with the left shift criterion removed; this is known as the modified Alvarado score and calculated out at a maximum of 9.9
Since the original Alvarado study was published, multiple small studies have attempted to validate or otherwise retrospectively assess the utility of this rule. A frequently cited systematic review of 42 prospective and retrospective studies by Ohle et al found that a score of <5 showed a sensitivity of 99% overall (96% in men, 99% in women, and 99% in children) for ruling out admission/observation of patient with suspected appendicitis, though the specificity for ruling in the diagnosis at scores 7 and higher was only 81% overall.10
However, a more recent prospective observational study of adult abdominal pain patients presenting to large American urban EDs found the modified Alvarado rule at cutoff levels of 3, 4, and 5 had sensitivities of only 72%, 55%, and 36%, respectively, of ruling out the diagnosis.11 In comparison, the study found that physicians’ clinical judgement of appendicitis being the first or second most likely diagnosis had a sensitivity of 93% for predicting appendicitis.11
Comment: The Alvarado score was developed to help rule out and rule in the diagnosis of appendicitis. However, with the increasing availability of CT scanning in EDs, the diagnostic pathway in unclear cases has shifted from admission/observation to CT scanning, which has the benefit of elucidating other pathology as well. The utility of the Alvarado rule has been called into question. Ultimately, there is data in support of the Alvarado rule from older articles and studies in resource-poor environments, and newer studies may reflect less rigorous application of the rule when CT scanning is the default clinical pathway. Further studies that focus specifically on the Alvarado score as a rule out test to decrease CT utilization may be instructive.
Appendicitis Inflammatory Response (AIR) score
The appendicitis inflammatory response (AIR) score was derived in a cohort of 316 patients and validated on a sample of 229 adults and children with suspected appendicitis.12 The authors specifically sought to create a rule that outperformed the Alvarado score; the criteria are:
Vomiting: 1 point
Right iliac fossa pain: 1 point
Rebound tenderness: 1 point for light, 2 for medium, 3 for strong
Temperature >38.5°C: 1 point
Polymorphonuclear leukocytes: 1 point for 70%-84%, 2 for 85% or greater
White blood cell count: 1 point for 10,000-14,900, 2 for 15,000 or greater
C-reactive protein level (mg/dL): 1 point for 10-49, 2 for 50 or greater
Patients with a score of 0-4 were classified as low risk, with recommendation for outpatient follow-up if general condition unchanged; a score of 5-8 as indeterminate risk, with recommendation for active observation with serial exams, imaging, or diagnostic laparoscopy; or a score of 9-12 as high risk, with recommendation for surgical exploration.12 In the validation cohort, the investigators found an AIR score or Alvarado score greater than 4 to have, respectively, 96% or 97% sensitivity and 73% or 61% specificity for detecting appendicitis.12 A high score of greater than 8 on either the AIR or Alvarado had respectively 37% or 28% sensitivity but specificity of 99% for detecting appendicitis with either instrument.12
In an external validation study, the AIR and Alvarado scores were calculated on a series of 941 patients (aged 1 to 97 years) being evaluated for possible appendicitis; 201 patients were younger than 18.13 At a cutoff of greater than 4, the sensitivity and specificity were found to be 93% and 85% for the AIR and 90% and 55% for Alvarado.13 In a cohort of 182 patients (aged 4 to 75 years), a score of 4 or greater on the AIR and Alvarado was found to have comparable sensitivity to that of a senior surgical consultant for detecting appendicitis—with sensitivities of 94%, 93%, and 90% respectively.14 Subsequently, the original investigators undertook a large multicenter implementation study of the AIR at 24 hospitals of patients (aged 5 to 96 years) with suspected appendicitis. As compared to the pre-implementation group, using AIR to categorize patients as low risk resulted in significantly fewer imaging studies, admissions, and surgical explorations.15
Comment: The AIR has the benefit of recent prospective studies that assess performance of the rule in settings that mirror the practice environments of most EPs today. The classification of rebound tenderness as light, medium, or strong may be difficult to ascertain. Ultimately, reductions in imaging, admissions, and surgical explorations are important goals and EPs might benefit from using this rule to guide imaging.
CHEST
HEART Score
The increasingly popular HEART score, first developed by physicians in the Netherlands in 2008, seeks to risk-stratify patients presenting to the ED with suspected cardiac chest pain without ST-elevation myocardial infarction (STEMI). It scores patients 0 to 2 on 5 different characteristics (with a total scored of 10 possible points):
History: 2 points for highly suspicious, 1 point for moderately suspicious
EKG: 2 points for significant ST deviation, 1 point for nonspecific repolarization disturbance
Age: 2 points for age 65 years or greater, 1 point for age 45-64 years
Risk Factors: 2 points for 3 or more risk factors or history of atherosclerotic disease, 1 point for 1 to 2 risk factors
Troponin: 2 points for troponin value >3 times the normal limit, 1 point for value 1-3 times the normal limit.
The authors developed these 5 categories “based on clinical experience and current medical literature,” and then applied the rule to 122 chest pain patients in the ED, finding a higher incidence of major adverse coronary events (MACE) with increasing score: 2.5% for low risk score of 0-3, 20.3% for intermediate risk score of 4-6, and 72.7% for score 7 or higher.16 The score has been retrospectively and prospectively validated.17,18 In a study of 2440 patients, the low risk group had a MACE of 1.7%, and the score had a c-statistic of 0.83, outperforming Thrombolysis in Myocardial Infarction (TIMI) and GRACE c-statistics of 0.75 and 0.70, respectively.18 In 2013, investigators calculated the HEART score on a multinational database of 2906 chest pain patients, finding a negative predictive value of 98.3% for MACE with HEART score less than or equal to 3.19
In the United States, Mahler et al have produced a series of 3 articles validating the HEART score and demonstrating its use in reducing cardiac testing and length of stay. In 1070 patients admitted to their observation unit, who were deemed low risk by physician assessment and TIMI <2, a score of less than or equal to 3 had a negative predictive value of 99.4% for MACE; the inclusion of serial troponins resulted in sensitivity of 100%, specificity of 83.1%, and negative predictive value of 100%.20 The team then conducted a secondary analysis of chest pain patients enrolled in a large multicenter trial (MIDAS) and compared HEART score, the North American Chest Pain Rule, and unstructured clinical assessment.21 Both rules had high sensitivities, but the HEART score identified 20% of patients suitable for early discharge, as compared to 4% for the North American Chest Pain Rule.21 Finally, Mahler’s team performed a randomized control trial of 282 patients investigating whether the HEART score with serial troponins compared with usual care could safely reduce cardiac testing.22 The HEART pathway resulted in an absolute reduction of 12.1% in cardiac testing, and median reduction in length of stay by 12 hours, with no missed MACE in discharged patients.22
Most recently, a stepped-wedge, cluster randomized trial across 9 hospitals published in 2017 investigated the utility of the HEART score. Despite enrolling only 3648 patients out of the statistically required sample size of 6600, they found that the HEART score was not inferior to usual care and there was no significant difference in median length of stay, but health care resources were typically lower in the HEART score group.23
Comment: While derived in a less conventional manner, the HEART score has held up in several validation studies and appears poised to safely decrease health care costs and increase ED efficiency and throughput. As more US EDs look to adopt high sensitivity troponin biomarkers, prospective studies will be needed to determine the role of the HEART score in this setting.
Thrombolysis in Myocardial Infarction (TIMI) score
The Thrombolysis in Myocardial Infarction (TIMI) score was developed in 2000 as a tool to risk-stratify patients with a diagnosis of unstable angina (UA) and non–ST-elevation myocardial infarction (NSTEMI). The score was derived from 1 arm (2047 patients) of a study comparing heparin with enoxaparin for treatment of NSTEMI, and validated in the other 3 arms of the study (5124 patients). Multivariate logistic regression was used to develop 7 variables of equal weight:
Age greater than or equal to 65yo
Three or more cardiac risk factors
Known coronary artery disease (with stenosis greater than or equal to 50%)
Aspirin use in the past 7 days
Severe angina (2 or more episodes in the past 24 hours)
EKG ST changes greater than or equal to 0.5 mm
Positive serum cardiac biomarkers
The investigators found that with a higher score, there was progressive increase in adverse cardiac outcomes, with a c-statistic of 0.65.24 This score was subsequently validated across several existing databases evaluating various therapeutic interventions for UA/NSTEMI and remained statistically significant, with increasing risk for MI and mortality with increasing score.25,26
Given the success in predicting patient outcomes and identifying patients who could benefit from more aggressive care, the TIMI risk score was then applied to unselected ED chest pain patients. In a secondary analysis of a prospective observational cohort of 3929 patient visits, the TIMI score correlated to the risk for adverse outcomes, with a risk of 2.1% at score 0.27
In a second prospective observational cohort of 1458 patient visits, a score of 0 correlated to a 1.7% incidence of adverse outcomes.28 In 2008, Body et al sought to increase the relative weight of EKG and biomarker factors to 5 (instead of 1) in a study of 796 patients, positing that these factors have more importance in the ED setting.29 Comparing the modified TIMI to the original, the modified instrument improved the area under curve (AUC) from 0.77 to 0.87.29 In follow-up validation studies, the modified score has an improved AUC, but the incidence of adverse outcomes at score 0 remains at about 2% for both modified and original score.30,31
In 2010, Hess et al performed a systematic review and meta-analysis of the studies that prospectively validated the TIMI score. They evaluated 10 validation studies, encompassing 17,265 patients across 5 countries, and found a strong linear relation between the TIMI score and adverse cardiac events.32 At TIMI score of 0, the incidence of cardiac events was 1.8%, with sensitivity of 97.2% and specificity of 25%. Subsequently, the ADAPT trial designed a diagnostic protocol consisting of TIMI risk assessment, EKG, and 0- and 2-hour troponin I biomarkers to find ED patients eligible for safe, early discharge.33 Of the 1975 patients, 20% were classified as low risk and eligible for early discharge, in that they had TIMI score of 0, a non-ischemic ECG, and negative troponins. Only one patient had a MACE at 30 days, giving the protocol a sensitivity of 99.7%, specificity of 23.4%, and negative predictive value of 99.7%.33
As the TIMI and HEART scores are both used to evaluate ED chest pain patients, several studies have sought to compare them. In 2015, Cartlon et al published a comparison of 5 established risk scores and 2 troponin assays in 963 patients: modified Goldman, TIMI, GRACE, HEART, and Vancouver Chest Pain Rule in combination with troponin T and I.34 The investigators found that a negative troponin T plus either TIMI score of 0 or a HEART score ≤3 gave a negative predictive value of greater than 99.5% with more than 30% of patients able to be discharged safely.34 In 2017, a comparison of the GRACE, HEART, and TIMI scores in 1833 chest pain patients found the HEART score identified more low risk patients than either of its comparators and had the highest AUC at 0.86.35 Other trials have similarly found HEART outperforming TIMI.36
Comment: The TIMI score was not specifically designed for ED use but has been adapted to serve this purpose. To the EP assessing the undifferentiated chest pain patient, the TIMI score uses clinical variables that may seem curious (eg, aspirin use) or impossible for EPs to ascertain (eg, presence or degree of stenosis). Even for patients with a score of 0, the risk for adverse outcomes remains stubbornly at the 2% level, similar to the original low risk HEART score findings.
Wells’ Criteria for Pulmonary Embolism
The diagnosis of pulmonary embolism (PE) is often challenging, requiring the use of multiple ED resources for timely diagnosis, and is therefore well suited for clinical decision instruments. The Wells’ Criteria were derived from a cohort of 1260 patients using logistic regression to identify 7 significant variables:
Clinical signs and symptoms of deep vein thrombosis (DVT): 3
PE is the most likely diagnosis: 3
Heart rate >100: 1.5
Immobilization or surgery in the previous 4 weeks: 1.5
Previously diagnosed DVT or PE: 1.5
Hemoptysis: 1
Malignancy with treatment within 6 months or palliative: 1
The investigators specifically linked the use of their instrument to the D-dimer assay, using their score to determine pretest probability and seeking to exclude the diagnosis in patients with low pretest probability and negative D-dimer result.37,38 They reported a three-tiered classification, with low risk at a score less than 2, moderate risk at scores from 2-6, and high risk at scores greater than 6. The risk for PE with a low risk score coupled with a negative D-dimer result were 1.5% and 2.7% in the derivation and validation cohorts. Using a two-tiered classification of PE unlikely at scores less than or equal to 4 and PE likely at scores 5 or greater, a PE unlikely score and a negative D-dimer had a 2.2% and 1.7% risk in the derivation and validation cohorts.
A subsequent study by Wells et al on 930 ED patients using the score plus D-dimer found a negative predictive value of 99.5% for a low risk score and a negative D-dimer.39 This allowed for reduced imaging in 53% of patients.39 Another external validation study found acceptable interrater agreement between physicians for the Wells’ score at kappa 0.62 for the three-tiered system and 0.7 for the two-tiered system.40 The Wells’ Criteria has been compared against the Geneva score with receiver operating characteristic curve analysis showing no difference between the two rules.41 In a large cohort of 3306 patients being evaluated for PE using the Wells’ score and D-dimer, for the 1028 patients with PE unlikely and a negative D-dimer, there was a 3-month incidence of venous thromboembolism (VTE) of 0.5%—none of which were fatal events.42
Comment: The Wells’ Criteria for pulmonary embolism combined with D-dimer is now the preferred approach for many EPs seeking to risk-stratify their patients for PE. Advances in age-adjusted cutoffs for D-dimer provide additional support for this powerful tool.
Pulmonary Embolism Rule-Out Criteria (PERC)
Given the low specificity of the D-dimer assay for VTE, researchers post–Wells’ Criteria have sought to further reduce unnecessary testing by reassessing the D-dimer’s role in the diagnostic pathway. The PERC rule was designed to reduce D-dimer use—and downstream CT scan testing—in low-risk patients. The investigators derived the rule from a population of patients for whom the pretest probability of PE was less than 15%, seeking a risk for PE less than 2% if the rule was satisfied. Using logistic regression in 3148 ED patients, 8 clinical criteria were obtained:
Age < 50 years Pulse <100
Pulse oximetry >94%
No unilateral leg swelling
No hemoptysis
No recent surgery
No prior PE/DVT
No hormone use
The variables were tested in 1427 low-risk and 382 very-low-risk patients (defined as being evaluated for dyspnea, but not part of the derivation or low-risk validation groups). In the low-risk group, the sensitivity, specificity, and false-negative rate was 96%, 27%, and 1.4% respectively. In the very-low-risk group, the sensitivity, specificity, and false-negative rate was 100%, 15%, and 0% respectively.43 The rule was further validated in a prospective multicenter study of 8138 patients; among patients with pretest probability less than 15% who were PERC negative, 1% had PE/DVT within 45 days.44 The large PERCEPIC trial on 1757 patients found low pretest probability patients who were PERC negative had a false-negative rate of 1.2% and estimated that the use of PERC could decrease the median length of stay in the ED by at least 2 hours.45 The PROPER study, a non-inferiority, crossover cluster-randomized trial in 14 EDs across France, found that use of the PERC rule was not inferior to conventional care and that it was associated with reduced ED length of stay and CT use.45,46
There has been criticism from some European studies that the PERC rule misses too many PEs. A provocatively titled multinational study from Hugli et al examined patients suspected to have PE in Switzerland, France, and Belgium. The investigators applied the PERC rule and then stratified the patients by pretest probability as defined by the Geneva score, which includes many of the same criteria as PERC. They found the PERC rule identified a small proportion of patients with suspected PE as very low risk (13.2%) and that the prevalence of PE among these patients was 5.4%. Critics of this study have noted that the PERC rule was designed to be applied in low-risk patients, not to define the low-risk population.47 Another study examined a retrospective cohort of patients in whom a D-dimer was ordered to exclude PE, and then calculated the Wells’ and PERC score from the medical record. The investigators found that the combination of Wells and PERC missed 2 PEs out of their population of 377 patients.48 However, a subsequent meta-analysis analyzed 11 studies—including the two negative studies—and found a pooled sensitivity of 97%, specificity of 23%, and negative likelihood ratio of 0.18, concluding that when the pretest probability is low, PERC is sensitive enough to exclude D-dimer testing.49
Comment: Given the number of disease states and sampling techniques that can cause nonspecific elevation in D-dimer assay, the PERC rule provides a useful tool in low-risk populations for excluding PE without laboratory testing. The key is applying the rule to the appropriate population, as stratified by gestalt or clinical score.
Infectious Disease
Mortality in Emergency Department Sepsis (MEDS) score
The Mortality in Emergency Department Sepsis (MEDS) score was developed as a risk stratification tool for patients presenting to the ED with concern for sepsis. This score was prospectively derived from a population of 3301 ED patient encounters during which a blood culture was ordered. Charts were reviewed and several data points extracted and analyzed to determine the following univariate predictors of 28-day mortality: terminal illness, tachypnea or hypoxia, septic shock, platelets <150,000/mm3, bands >5%, age >65 years, lower respiratory infection, nursing home residence, and altered mental status. These predictors were assigned point values based on their odds ratios, and points are added to generate a total score. Mortality risk was stratified into groups based on total score, with percentage mortality as follows: score 0-4: 0.9%; 5-7: 2.0%; 8-12: 7.8%; 13-15: 20.2%; >15: 50%. A separate validation cohort had the following mortality rates: score 0-4: 1.1%; 5-7: 4.4%; 8-12: 9.3%; 13-15: 16.1%; >15: 39%.50
The MEDS score was subsequently shown to also be predictive for 1-year mortality as well, with an area under receiver operating curve (AUROC) of 0.76 for 1-year mortality.51 A subsequent study showed similar mortality rates when expanding the patient population to include all patients with systemic inflammatory response syndrome (SIRS), potentially broadening the potential application of MEDS in ED risk stratification.52 However, the score was shown to be less predictive in patients with severe sepsis and septic shock, underestimating mortality in all MEDS score groups.53 Still, the MEDS score was demonstrated in multiple validation studies as a reliable risk stratification tool in patients with suspected infection or SIRS.54,55
Comment: The MEDS score is not as well studied in the literature as the SIRS criteria or QuickSOFA but is a validated risk stratification tool in patients with suspected infection and is ED specific. This tool, similar to Pneumonia Severity Index and CURB-65 (discussed below), can guide management of patients from the ED. Very-low-risk (score 0-4) patients can be treated as outpatients, low risk (score 5-7) patients warranting consideration of a short inpatient stay, and moderate to high risk (>8) requiring inpatient management. At present, there is insufficient evidence regarding the role of the MEDS score to guide inpatient disposition of floor vs. ICU in moderate to high-risk patients.
Pneumonia Severity Index
The Pneumonia Severity Index (PSI) was developed as a tool to predict mortality risk from pneumonia, allowing providers to appropriately manage care for these patients in the hospital or as outpatients. A derivation cohort of 14199 patients was utilized to create a prediction rule in two steps meant to parallel a clinician’s decision-making process. The first step identified a population of patients that were at low risk for death, which were assigned to class I. The second step quantified the risk for death in the remaining patients using weighted factors including demographics, comorbidities, exam findings, and clinical data. In all, 20 variables were used and assigned corresponding points, the sum of which would assign a patient to a particular risk for mortality (class II-V).56
Mortality risk was relatively low for patients in class I and II (0.4 and 0.7%, respectively). Class III carried a mortality risk of 2.8%. Mortality increased with class IV and class V classification: 8.5% and 31.1%, respectively. These data were replicated with a separate validation cohort of 38039 patients, with similar mortality rates in each class. This study concluded with the recommendation that patients diagnosed with pneumonia falling into class I and II mortality risk should be managed as outpatients, possible brief inpatient observation for class III, and class IV and V managed as inpatients.56
Subsequent trials evaluating the utility of the PSI score in the management of patients diagnosed with pneumonia randomized low-risk patients (class I-III PSI) to treatment as outpatients vs inpatients. There were no statistical differences in adverse outcomes (ICU admission, hospital readmission, mortality, complications), with notable improvements in hospital admission rates and patient satisfaction.57,58 A meta-analysis of 6 studies that used a clinical decision tools to identify low-risk patients to treat pneumonia as outpatients showed no significant difference in mortality, patient readmissions, or patient satisfaction. Low-risk patients that required admission often included comorbid illnesses not included in the PSI, inability to take oral medications, barriers to compliance, or hypoxemia.59
Though the PSI has been shown to successfully identify patients at low risk for mortality, it has been less accurate at predicting and stratifying classes of severe pneumonia. A meta-analysis by Loke et al showed that PSI class IV or V had pooled sensitivity of 0.90 and specificity 0.53 for 30-day mortality, which was significantly better than the CURB-65 rule (discussed below).60 However, a subsequent large meta-analysis showed that PSI class IV or V had a sensitivity of 75% and specificity 40% for requiring ICU intervention or admission, which are not sufficient to guide disposition decisions.61
CURB-65
One of the criticisms of PSI included its complexity, with inclusion of 20 factors making it impractical for use as a bedside tool. The CURB-65 score was developed with a similar goal of identifying low-risk patients with pneumonia who would be candidates for outpatient management, but also patients at high risk for mortality or ICU admission. Criteria for severe pneumonia published by the British Thoracic Society include: respiratory rate ≥ 30 breaths/min, diastolic blood pressure ≤60 mmHg, and blood urea nitrogen >7 mmol/L. The presence of 2 criteria was 88% sensitive and 72% specific for mortality or ICU admission.62 The CURB-65 tool was based on these criteria, with the addition of age ≥65 years, which was found to be a separate independent predictor of mortality. Thus, the 5 criteria making up the score are as follows (1 point each, 0-5 total):
Confusion, meaning Mental Test Score ≤8, or disorientation to person, place, or time
Urea >7 mmol/L (>19.6 mg/dL)
Respiratory rate ≥ 30 breaths/minute
Blood pressure (systolic < 90 mmHg or diastolic ≤ 60 mmHg)
Age ≥ 65 years
A score of 0-1 of these criteria characterized low mortality risk (<1.5%) in the test group, a score of 2 was intermediate mortality risk (9.2%), and a score of 3 or more associated with high mortality risk (22%). A score ≥ 2 was 93% sensitive and 49% specific for 30-day mortality.63
A subsequent prospective validation study by Aujesky et al that included 3181 patients with community-acquired pneumonia demonstrated slightly higher mortality rates for each CURB-65 score (0.6%, 3%, 6.1%, 13%, 17%, 43% mortality in scores of 0-5, respectively).64 In particular, the 3% mortality rate in CURB-65 scores of 1 is similar to PSI class III mortality rates, suggesting a lower threshold (CURB-65 ≥1) for consideration of admission for management. Another validation study by Capelastegui et al showed similar mortality rates to the derivation study for specific CURB-65 scores, but noted 53% of patients with a score of 1 also were found to have characteristics that were independent for a poor prognosis, and should be considered in the decision for outpatient or inpatient treatment.65 Furthermore, a recent study found that of patients in the ED with a CURB-65 score of 1, 8% still required critical care intervention.66 Thus, use of CURB-65 in screening for low-risk patients with community-acquired pneumonia is recommended to be limited to scores of 0. However, as with PSI, validation studies have yet to show predictive utility of scores suggesting severe pneumonia (CURB-65 ≥3) in predicting mortality or ICU requirement.60,61
As validation studies have suggested only patients with a CURB-65 score of 0 are screened low risk enough for outpatient treatment, greater weight may be placed on utility of CRB-65 as a tool. This rule, initially proposed in the same study as CURB-65, omits blood urea nitrogen as a factor to only rely on history and physical exam data with a score of 0 indicating low risk.63 In initial derivation and validation studies, this rule demonstrated <1.6% mortality risk with a score of 0, with risk increasing to 4-8.6% in scores of 1.63,65 Multiple studies have compared CRB-65 and CURB-65, with only marginal but not statistically significant improvement in prognostic utility of CURB-65.65,67 A meta-analysis of 1648 patients even showed only 0.5% mortality risk in CRB-65 ≤1; potentially including CRB-65 0-1 as low risk, though, would require further study.68 Although multiple validation studies have also successfully stratified low risk to similar mortality risk (<1.6%), accuracy wanes with higher CRB-65 scores.69
Several studies have directly compared CURB-65 and PSI both in terms of identifying low-risk patients and stratifying disease severity.60,61,64,68,70-72 Multiple studies have shown similar mortality risk in low-risk populations and have demonstrated sensitivities for mortality greater than 96% for CURB-65/CRB-65 = 0 and PSI class I-III, albeit with specificities ranging from 18-65%.64,68,70 In stratifying patients into different levels of severity (ward vs ICU patients), PSI has shown slightly better sensitivity/specificity for mortality and/or ICU intervention, though neither is strong enough to significantly stratify severe pneumonia to serve as tools for directing inpatient management.60,61
Comment: PSI, CRB-65, and CURB-65 have been well validated as screening tools for low-risk patients who should be treated as outpatients (CURB-65 or CRB-65 = 0, PSI class I and II). A moderate-risk population (CURB-65 = 1 or 2, PSI class III) may benefit from treatment as inpatient or outpatient at clinician judgement. Use of these tools for determining disease severity and possible ICU requirement is not as reliable, and other clinical factors should be considered.
Conclusion
This article provides an overview of several common clinical decision instruments and the evidence behind them. Ultimately, many institutions have incorporated clinical decision rules directly into the electronic medical record, and this strategy will not only increase their use, but hopefully collect further data on whether the instruments truly perform better than unstructured clinical judgement.
In this second part of “Playing by the Rules,” we will examine validated clinical decision rules that assist emergency physicians (EPs) in the diagnosis and treatment of nontraumatic conditions. Most trauma rules seek to answer a yes or no question regarding the utility of testing for specific disease states when the diagnosis is not clinically apparent.
For example, the Canadian CT Head Rule describes a number of conditions that, if met, can predict the absence of traumatic lesions requiring neurosurgical intervention in the alert patient with head injury, and thus obviate the need for imaging in those instances. In contrast, many medical rules are actually risk stratification scales for treatment and diagnosis, categorizing patients into low- to high-risk groups based on clinical factors. While traumatic conditions are linked to a specific inciting event or “trauma,” medical diseases may have multiple causative factors or may be delayed in presentation to the emergency department (ED), which subsequently increases the complexity of these decision instruments.
Rather than an exhaustive list of all clinical decision rules or risk stratification scales relevant to emergency medicine, this installment will provide EPs with a review of common instruments and the evidence behind them.
Central Nervous System
Ottawa Subarachnoid Hemorrhage Rule
The Ottawa Subarachnoid Hemorrhage Rule offers guidance for diagnosing atraumatic subarachnoid hemorrhage (SAH) in alert, neurologically intact adult patients presenting to the ED with a headache reaching maximal intensity within 1 hour of onset. The rule states that if none of the following conditions are present, then the diagnosis of SAH can be excluded without further testing:
Symptom of neck pain or stiffness
Age greater than 40 years old
Witnessed loss of consciousness
Onset during exertion
Thunderclap headache with peak pain instantly
Limited neck flexion on exam
The validation study prospectively enrolled 1153 adults of whom 67 had a positive workup for SAH (defined as subarachnoid blood visible on noncontrast CT scan of the head, xanthochromia of cerebrospinal fluid on visual inspection, or the presence of >1 million erythrocytes in the final tube of cerebrospinal fluid with an aneurysm or arteriovenous malformation confirmed on cerebral angiography).1 Of note, patients with prior history of cerebral aneurysm or SAH were excluded, as were patients with recurrent headaches similar to the presenting complaint, patients with focal neurologic deficits or papilledema, or patients with a history of brain neoplasm, ventricular shunt, or hydrocephalus. The authors found that the rule was 100% sensitive and 13% specific for detecting SAH, with a kappa of 0.82, which suggests good interrater reliability.1
Comment: It is important to note that the authors excluded patients with a history of cerebral aneurysm or prior SAH, and therefore the rule should not be applied to these patients in clinical practice. The utility of this rule is somewhat limited secondary to the age cutoff, as the incidence of aneurysmal SAH increases considerably after the fifth decade of life.2 Ultimately, this rule—combined with the authors’ previous work showing that CT performed within 6 hours of headache onset can rule out SAH—provides a powerful diagnostic tool for EPs considering SAH in the ED.3
ABCD2 Score
The ABCD2 score was developed to identify transient ischemic attack (TIA) patients at risk for early stroke, and thus inform decisions regarding admission and resource utilization in the ED and outpatient clinic setting.4 The score was created by combining elements of two previously existing rules, the California and the ABCD scales. Patients presenting with TIA symptoms are assigned points based on:
Age: 1 point if ≥ 60 years
Blood Pressure: 1 point if ≥ 140/90
Clinical Deficit: 2 points for unilateral weakness, 1 point for speech impairment without unilateral weakness
Duration: 2 points for ≥ 60 minutes, 1 point for 10 to 59 minutes
Diabetes: 1 point if diabetic
The greater the number of points, the higher the risk for imminent stroke, from low (0-3 points) to moderate (4-5 points) to high (6-7 points). The initial retrospective internal validation study found that the low, moderate, and high groups correlated to 7-day stroke risk of 1.2%, 5.9%, and 11.7%, respectively. Subsequently, the ABCD2 score was rapidly incorporated into institutional and national protocols for assessing risk for stroke and featured prominently in the 2009 American Heart Association guidelines on TIA, which recommend hospitalization for a score of 3 or greater.4,5
More recently, a multicenter prospective external validation study of more than 2000 TIA patients found that using the American Heart Association recommended cutoff of 3 or greater resulted in a sensitivity of 94.7% for detecting those patients who sustained a stroke within 7 days, but a specificity of only 12.5%.6 The investigators concluded that a specificity this low would require “almost all” of the TIA patients in their cohort (87.6%) to be admitted to the hospital—even though only 3.2% of their patients had a stroke within 90 days.6 Even when examined at other cutoff scores, the investigators found the ABCD2 score to have poor accuracy.6
Comment: Decreasing resource utilization is a laudable goal, but it does not appear that the ABCD2 score provides much guidance on which TIA patients can safely go home. Moreover, the increasing availability of advanced imaging and tele-neurology consultation in the ED have changed the landscape of TIA and stroke care. Many EPs have since argued that the ABCD2 score adds little to their evaluation.7
Abdomen
Alvarado Score
There are multiple clinical prediction rules for appendicitis. Among the most commonly utilized by EPs and surgical consultants are the Alvarado score and the Appendicitis Inflammatory Response Score. The Alvarado score was derived in 1986 based on a retrospective review of 305 abdominal pain patients of whom 227 (aged 4 to 80 years) had appendicitis.8 Factors were identified and weighted, which can be recalled through the mnemonic MANTRELS:
Migration of pain to the right lower quadrant: 1 point
Anorexia or acetone in urine: 1 point
Nausea or vomiting: 1 point
Tenderness in the right lower quadrant: 2 points
Rebound tenderness: 1 point
Elevation of the temperature > 37.3°C: 1 point
Leukocytosis >10K X 109/L: 2 points
Shift to the left of neutrophils (>75%): 1 point
The original article posited that a score of 5 or 6 was “compatible” with the diagnosis of acute appendicitis—necessitating further observation for possible appendicitis—and that higher scores indicated an increasing probability of disease.8 Of note, the rule has also been adapted for clinical settings where differentials are not easily obtainable with the left shift criterion removed; this is known as the modified Alvarado score and calculated out at a maximum of 9.9
Since the original Alvarado study was published, multiple small studies have attempted to validate or otherwise retrospectively assess the utility of this rule. A frequently cited systematic review of 42 prospective and retrospective studies by Ohle et al found that a score of <5 showed a sensitivity of 99% overall (96% in men, 99% in women, and 99% in children) for ruling out admission/observation of patient with suspected appendicitis, though the specificity for ruling in the diagnosis at scores 7 and higher was only 81% overall.10
However, a more recent prospective observational study of adult abdominal pain patients presenting to large American urban EDs found the modified Alvarado rule at cutoff levels of 3, 4, and 5 had sensitivities of only 72%, 55%, and 36%, respectively, of ruling out the diagnosis.11 In comparison, the study found that physicians’ clinical judgement of appendicitis being the first or second most likely diagnosis had a sensitivity of 93% for predicting appendicitis.11
Comment: The Alvarado score was developed to help rule out and rule in the diagnosis of appendicitis. However, with the increasing availability of CT scanning in EDs, the diagnostic pathway in unclear cases has shifted from admission/observation to CT scanning, which has the benefit of elucidating other pathology as well. The utility of the Alvarado rule has been called into question. Ultimately, there is data in support of the Alvarado rule from older articles and studies in resource-poor environments, and newer studies may reflect less rigorous application of the rule when CT scanning is the default clinical pathway. Further studies that focus specifically on the Alvarado score as a rule out test to decrease CT utilization may be instructive.
Appendicitis Inflammatory Response (AIR) score
The appendicitis inflammatory response (AIR) score was derived in a cohort of 316 patients and validated on a sample of 229 adults and children with suspected appendicitis.12 The authors specifically sought to create a rule that outperformed the Alvarado score; the criteria are:
Vomiting: 1 point
Right iliac fossa pain: 1 point
Rebound tenderness: 1 point for light, 2 for medium, 3 for strong
Temperature >38.5°C: 1 point
Polymorphonuclear leukocytes: 1 point for 70%-84%, 2 for 85% or greater
White blood cell count: 1 point for 10,000-14,900, 2 for 15,000 or greater
C-reactive protein level (mg/dL): 1 point for 10-49, 2 for 50 or greater
Patients with a score of 0-4 were classified as low risk, with recommendation for outpatient follow-up if general condition unchanged; a score of 5-8 as indeterminate risk, with recommendation for active observation with serial exams, imaging, or diagnostic laparoscopy; or a score of 9-12 as high risk, with recommendation for surgical exploration.12 In the validation cohort, the investigators found an AIR score or Alvarado score greater than 4 to have, respectively, 96% or 97% sensitivity and 73% or 61% specificity for detecting appendicitis.12 A high score of greater than 8 on either the AIR or Alvarado had respectively 37% or 28% sensitivity but specificity of 99% for detecting appendicitis with either instrument.12
In an external validation study, the AIR and Alvarado scores were calculated on a series of 941 patients (aged 1 to 97 years) being evaluated for possible appendicitis; 201 patients were younger than 18.13 At a cutoff of greater than 4, the sensitivity and specificity were found to be 93% and 85% for the AIR and 90% and 55% for Alvarado.13 In a cohort of 182 patients (aged 4 to 75 years), a score of 4 or greater on the AIR and Alvarado was found to have comparable sensitivity to that of a senior surgical consultant for detecting appendicitis—with sensitivities of 94%, 93%, and 90% respectively.14 Subsequently, the original investigators undertook a large multicenter implementation study of the AIR at 24 hospitals of patients (aged 5 to 96 years) with suspected appendicitis. As compared to the pre-implementation group, using AIR to categorize patients as low risk resulted in significantly fewer imaging studies, admissions, and surgical explorations.15
Comment: The AIR has the benefit of recent prospective studies that assess performance of the rule in settings that mirror the practice environments of most EPs today. The classification of rebound tenderness as light, medium, or strong may be difficult to ascertain. Ultimately, reductions in imaging, admissions, and surgical explorations are important goals and EPs might benefit from using this rule to guide imaging.
CHEST
HEART Score
The increasingly popular HEART score, first developed by physicians in the Netherlands in 2008, seeks to risk-stratify patients presenting to the ED with suspected cardiac chest pain without ST-elevation myocardial infarction (STEMI). It scores patients 0 to 2 on 5 different characteristics (with a total scored of 10 possible points):
History: 2 points for highly suspicious, 1 point for moderately suspicious
EKG: 2 points for significant ST deviation, 1 point for nonspecific repolarization disturbance
Age: 2 points for age 65 years or greater, 1 point for age 45-64 years
Risk Factors: 2 points for 3 or more risk factors or history of atherosclerotic disease, 1 point for 1 to 2 risk factors
Troponin: 2 points for troponin value >3 times the normal limit, 1 point for value 1-3 times the normal limit.
The authors developed these 5 categories “based on clinical experience and current medical literature,” and then applied the rule to 122 chest pain patients in the ED, finding a higher incidence of major adverse coronary events (MACE) with increasing score: 2.5% for low risk score of 0-3, 20.3% for intermediate risk score of 4-6, and 72.7% for score 7 or higher.16 The score has been retrospectively and prospectively validated.17,18 In a study of 2440 patients, the low risk group had a MACE of 1.7%, and the score had a c-statistic of 0.83, outperforming Thrombolysis in Myocardial Infarction (TIMI) and GRACE c-statistics of 0.75 and 0.70, respectively.18 In 2013, investigators calculated the HEART score on a multinational database of 2906 chest pain patients, finding a negative predictive value of 98.3% for MACE with HEART score less than or equal to 3.19
In the United States, Mahler et al have produced a series of 3 articles validating the HEART score and demonstrating its use in reducing cardiac testing and length of stay. In 1070 patients admitted to their observation unit, who were deemed low risk by physician assessment and TIMI <2, a score of less than or equal to 3 had a negative predictive value of 99.4% for MACE; the inclusion of serial troponins resulted in sensitivity of 100%, specificity of 83.1%, and negative predictive value of 100%.20 The team then conducted a secondary analysis of chest pain patients enrolled in a large multicenter trial (MIDAS) and compared HEART score, the North American Chest Pain Rule, and unstructured clinical assessment.21 Both rules had high sensitivities, but the HEART score identified 20% of patients suitable for early discharge, as compared to 4% for the North American Chest Pain Rule.21 Finally, Mahler’s team performed a randomized control trial of 282 patients investigating whether the HEART score with serial troponins compared with usual care could safely reduce cardiac testing.22 The HEART pathway resulted in an absolute reduction of 12.1% in cardiac testing, and median reduction in length of stay by 12 hours, with no missed MACE in discharged patients.22
Most recently, a stepped-wedge, cluster randomized trial across 9 hospitals published in 2017 investigated the utility of the HEART score. Despite enrolling only 3648 patients out of the statistically required sample size of 6600, they found that the HEART score was not inferior to usual care and there was no significant difference in median length of stay, but health care resources were typically lower in the HEART score group.23
Comment: While derived in a less conventional manner, the HEART score has held up in several validation studies and appears poised to safely decrease health care costs and increase ED efficiency and throughput. As more US EDs look to adopt high sensitivity troponin biomarkers, prospective studies will be needed to determine the role of the HEART score in this setting.
Thrombolysis in Myocardial Infarction (TIMI) score
The Thrombolysis in Myocardial Infarction (TIMI) score was developed in 2000 as a tool to risk-stratify patients with a diagnosis of unstable angina (UA) and non–ST-elevation myocardial infarction (NSTEMI). The score was derived from 1 arm (2047 patients) of a study comparing heparin with enoxaparin for treatment of NSTEMI, and validated in the other 3 arms of the study (5124 patients). Multivariate logistic regression was used to develop 7 variables of equal weight:
Age greater than or equal to 65yo
Three or more cardiac risk factors
Known coronary artery disease (with stenosis greater than or equal to 50%)
Aspirin use in the past 7 days
Severe angina (2 or more episodes in the past 24 hours)
EKG ST changes greater than or equal to 0.5 mm
Positive serum cardiac biomarkers
The investigators found that with a higher score, there was progressive increase in adverse cardiac outcomes, with a c-statistic of 0.65.24 This score was subsequently validated across several existing databases evaluating various therapeutic interventions for UA/NSTEMI and remained statistically significant, with increasing risk for MI and mortality with increasing score.25,26
Given the success in predicting patient outcomes and identifying patients who could benefit from more aggressive care, the TIMI risk score was then applied to unselected ED chest pain patients. In a secondary analysis of a prospective observational cohort of 3929 patient visits, the TIMI score correlated to the risk for adverse outcomes, with a risk of 2.1% at score 0.27
In a second prospective observational cohort of 1458 patient visits, a score of 0 correlated to a 1.7% incidence of adverse outcomes.28 In 2008, Body et al sought to increase the relative weight of EKG and biomarker factors to 5 (instead of 1) in a study of 796 patients, positing that these factors have more importance in the ED setting.29 Comparing the modified TIMI to the original, the modified instrument improved the area under curve (AUC) from 0.77 to 0.87.29 In follow-up validation studies, the modified score has an improved AUC, but the incidence of adverse outcomes at score 0 remains at about 2% for both modified and original score.30,31
In 2010, Hess et al performed a systematic review and meta-analysis of the studies that prospectively validated the TIMI score. They evaluated 10 validation studies, encompassing 17,265 patients across 5 countries, and found a strong linear relation between the TIMI score and adverse cardiac events.32 At TIMI score of 0, the incidence of cardiac events was 1.8%, with sensitivity of 97.2% and specificity of 25%. Subsequently, the ADAPT trial designed a diagnostic protocol consisting of TIMI risk assessment, EKG, and 0- and 2-hour troponin I biomarkers to find ED patients eligible for safe, early discharge.33 Of the 1975 patients, 20% were classified as low risk and eligible for early discharge, in that they had TIMI score of 0, a non-ischemic ECG, and negative troponins. Only one patient had a MACE at 30 days, giving the protocol a sensitivity of 99.7%, specificity of 23.4%, and negative predictive value of 99.7%.33
As the TIMI and HEART scores are both used to evaluate ED chest pain patients, several studies have sought to compare them. In 2015, Cartlon et al published a comparison of 5 established risk scores and 2 troponin assays in 963 patients: modified Goldman, TIMI, GRACE, HEART, and Vancouver Chest Pain Rule in combination with troponin T and I.34 The investigators found that a negative troponin T plus either TIMI score of 0 or a HEART score ≤3 gave a negative predictive value of greater than 99.5% with more than 30% of patients able to be discharged safely.34 In 2017, a comparison of the GRACE, HEART, and TIMI scores in 1833 chest pain patients found the HEART score identified more low risk patients than either of its comparators and had the highest AUC at 0.86.35 Other trials have similarly found HEART outperforming TIMI.36
Comment: The TIMI score was not specifically designed for ED use but has been adapted to serve this purpose. To the EP assessing the undifferentiated chest pain patient, the TIMI score uses clinical variables that may seem curious (eg, aspirin use) or impossible for EPs to ascertain (eg, presence or degree of stenosis). Even for patients with a score of 0, the risk for adverse outcomes remains stubbornly at the 2% level, similar to the original low risk HEART score findings.
Wells’ Criteria for Pulmonary Embolism
The diagnosis of pulmonary embolism (PE) is often challenging, requiring the use of multiple ED resources for timely diagnosis, and is therefore well suited for clinical decision instruments. The Wells’ Criteria were derived from a cohort of 1260 patients using logistic regression to identify 7 significant variables:
Clinical signs and symptoms of deep vein thrombosis (DVT): 3
PE is the most likely diagnosis: 3
Heart rate >100: 1.5
Immobilization or surgery in the previous 4 weeks: 1.5
Previously diagnosed DVT or PE: 1.5
Hemoptysis: 1
Malignancy with treatment within 6 months or palliative: 1
The investigators specifically linked the use of their instrument to the D-dimer assay, using their score to determine pretest probability and seeking to exclude the diagnosis in patients with low pretest probability and negative D-dimer result.37,38 They reported a three-tiered classification, with low risk at a score less than 2, moderate risk at scores from 2-6, and high risk at scores greater than 6. The risk for PE with a low risk score coupled with a negative D-dimer result were 1.5% and 2.7% in the derivation and validation cohorts. Using a two-tiered classification of PE unlikely at scores less than or equal to 4 and PE likely at scores 5 or greater, a PE unlikely score and a negative D-dimer had a 2.2% and 1.7% risk in the derivation and validation cohorts.
A subsequent study by Wells et al on 930 ED patients using the score plus D-dimer found a negative predictive value of 99.5% for a low risk score and a negative D-dimer.39 This allowed for reduced imaging in 53% of patients.39 Another external validation study found acceptable interrater agreement between physicians for the Wells’ score at kappa 0.62 for the three-tiered system and 0.7 for the two-tiered system.40 The Wells’ Criteria has been compared against the Geneva score with receiver operating characteristic curve analysis showing no difference between the two rules.41 In a large cohort of 3306 patients being evaluated for PE using the Wells’ score and D-dimer, for the 1028 patients with PE unlikely and a negative D-dimer, there was a 3-month incidence of venous thromboembolism (VTE) of 0.5%—none of which were fatal events.42
Comment: The Wells’ Criteria for pulmonary embolism combined with D-dimer is now the preferred approach for many EPs seeking to risk-stratify their patients for PE. Advances in age-adjusted cutoffs for D-dimer provide additional support for this powerful tool.
Pulmonary Embolism Rule-Out Criteria (PERC)
Given the low specificity of the D-dimer assay for VTE, researchers post–Wells’ Criteria have sought to further reduce unnecessary testing by reassessing the D-dimer’s role in the diagnostic pathway. The PERC rule was designed to reduce D-dimer use—and downstream CT scan testing—in low-risk patients. The investigators derived the rule from a population of patients for whom the pretest probability of PE was less than 15%, seeking a risk for PE less than 2% if the rule was satisfied. Using logistic regression in 3148 ED patients, 8 clinical criteria were obtained:
Age < 50 years Pulse <100
Pulse oximetry >94%
No unilateral leg swelling
No hemoptysis
No recent surgery
No prior PE/DVT
No hormone use
The variables were tested in 1427 low-risk and 382 very-low-risk patients (defined as being evaluated for dyspnea, but not part of the derivation or low-risk validation groups). In the low-risk group, the sensitivity, specificity, and false-negative rate was 96%, 27%, and 1.4% respectively. In the very-low-risk group, the sensitivity, specificity, and false-negative rate was 100%, 15%, and 0% respectively.43 The rule was further validated in a prospective multicenter study of 8138 patients; among patients with pretest probability less than 15% who were PERC negative, 1% had PE/DVT within 45 days.44 The large PERCEPIC trial on 1757 patients found low pretest probability patients who were PERC negative had a false-negative rate of 1.2% and estimated that the use of PERC could decrease the median length of stay in the ED by at least 2 hours.45 The PROPER study, a non-inferiority, crossover cluster-randomized trial in 14 EDs across France, found that use of the PERC rule was not inferior to conventional care and that it was associated with reduced ED length of stay and CT use.45,46
There has been criticism from some European studies that the PERC rule misses too many PEs. A provocatively titled multinational study from Hugli et al examined patients suspected to have PE in Switzerland, France, and Belgium. The investigators applied the PERC rule and then stratified the patients by pretest probability as defined by the Geneva score, which includes many of the same criteria as PERC. They found the PERC rule identified a small proportion of patients with suspected PE as very low risk (13.2%) and that the prevalence of PE among these patients was 5.4%. Critics of this study have noted that the PERC rule was designed to be applied in low-risk patients, not to define the low-risk population.47 Another study examined a retrospective cohort of patients in whom a D-dimer was ordered to exclude PE, and then calculated the Wells’ and PERC score from the medical record. The investigators found that the combination of Wells and PERC missed 2 PEs out of their population of 377 patients.48 However, a subsequent meta-analysis analyzed 11 studies—including the two negative studies—and found a pooled sensitivity of 97%, specificity of 23%, and negative likelihood ratio of 0.18, concluding that when the pretest probability is low, PERC is sensitive enough to exclude D-dimer testing.49
Comment: Given the number of disease states and sampling techniques that can cause nonspecific elevation in D-dimer assay, the PERC rule provides a useful tool in low-risk populations for excluding PE without laboratory testing. The key is applying the rule to the appropriate population, as stratified by gestalt or clinical score.
Infectious Disease
Mortality in Emergency Department Sepsis (MEDS) score
The Mortality in Emergency Department Sepsis (MEDS) score was developed as a risk stratification tool for patients presenting to the ED with concern for sepsis. This score was prospectively derived from a population of 3301 ED patient encounters during which a blood culture was ordered. Charts were reviewed and several data points extracted and analyzed to determine the following univariate predictors of 28-day mortality: terminal illness, tachypnea or hypoxia, septic shock, platelets <150,000/mm3, bands >5%, age >65 years, lower respiratory infection, nursing home residence, and altered mental status. These predictors were assigned point values based on their odds ratios, and points are added to generate a total score. Mortality risk was stratified into groups based on total score, with percentage mortality as follows: score 0-4: 0.9%; 5-7: 2.0%; 8-12: 7.8%; 13-15: 20.2%; >15: 50%. A separate validation cohort had the following mortality rates: score 0-4: 1.1%; 5-7: 4.4%; 8-12: 9.3%; 13-15: 16.1%; >15: 39%.50
The MEDS score was subsequently shown to also be predictive for 1-year mortality as well, with an area under receiver operating curve (AUROC) of 0.76 for 1-year mortality.51 A subsequent study showed similar mortality rates when expanding the patient population to include all patients with systemic inflammatory response syndrome (SIRS), potentially broadening the potential application of MEDS in ED risk stratification.52 However, the score was shown to be less predictive in patients with severe sepsis and septic shock, underestimating mortality in all MEDS score groups.53 Still, the MEDS score was demonstrated in multiple validation studies as a reliable risk stratification tool in patients with suspected infection or SIRS.54,55
Comment: The MEDS score is not as well studied in the literature as the SIRS criteria or QuickSOFA but is a validated risk stratification tool in patients with suspected infection and is ED specific. This tool, similar to Pneumonia Severity Index and CURB-65 (discussed below), can guide management of patients from the ED. Very-low-risk (score 0-4) patients can be treated as outpatients, low risk (score 5-7) patients warranting consideration of a short inpatient stay, and moderate to high risk (>8) requiring inpatient management. At present, there is insufficient evidence regarding the role of the MEDS score to guide inpatient disposition of floor vs. ICU in moderate to high-risk patients.
Pneumonia Severity Index
The Pneumonia Severity Index (PSI) was developed as a tool to predict mortality risk from pneumonia, allowing providers to appropriately manage care for these patients in the hospital or as outpatients. A derivation cohort of 14199 patients was utilized to create a prediction rule in two steps meant to parallel a clinician’s decision-making process. The first step identified a population of patients that were at low risk for death, which were assigned to class I. The second step quantified the risk for death in the remaining patients using weighted factors including demographics, comorbidities, exam findings, and clinical data. In all, 20 variables were used and assigned corresponding points, the sum of which would assign a patient to a particular risk for mortality (class II-V).56
Mortality risk was relatively low for patients in class I and II (0.4 and 0.7%, respectively). Class III carried a mortality risk of 2.8%. Mortality increased with class IV and class V classification: 8.5% and 31.1%, respectively. These data were replicated with a separate validation cohort of 38039 patients, with similar mortality rates in each class. This study concluded with the recommendation that patients diagnosed with pneumonia falling into class I and II mortality risk should be managed as outpatients, possible brief inpatient observation for class III, and class IV and V managed as inpatients.56
Subsequent trials evaluating the utility of the PSI score in the management of patients diagnosed with pneumonia randomized low-risk patients (class I-III PSI) to treatment as outpatients vs inpatients. There were no statistical differences in adverse outcomes (ICU admission, hospital readmission, mortality, complications), with notable improvements in hospital admission rates and patient satisfaction.57,58 A meta-analysis of 6 studies that used a clinical decision tools to identify low-risk patients to treat pneumonia as outpatients showed no significant difference in mortality, patient readmissions, or patient satisfaction. Low-risk patients that required admission often included comorbid illnesses not included in the PSI, inability to take oral medications, barriers to compliance, or hypoxemia.59
Though the PSI has been shown to successfully identify patients at low risk for mortality, it has been less accurate at predicting and stratifying classes of severe pneumonia. A meta-analysis by Loke et al showed that PSI class IV or V had pooled sensitivity of 0.90 and specificity 0.53 for 30-day mortality, which was significantly better than the CURB-65 rule (discussed below).60 However, a subsequent large meta-analysis showed that PSI class IV or V had a sensitivity of 75% and specificity 40% for requiring ICU intervention or admission, which are not sufficient to guide disposition decisions.61
CURB-65
One of the criticisms of PSI included its complexity, with inclusion of 20 factors making it impractical for use as a bedside tool. The CURB-65 score was developed with a similar goal of identifying low-risk patients with pneumonia who would be candidates for outpatient management, but also patients at high risk for mortality or ICU admission. Criteria for severe pneumonia published by the British Thoracic Society include: respiratory rate ≥ 30 breaths/min, diastolic blood pressure ≤60 mmHg, and blood urea nitrogen >7 mmol/L. The presence of 2 criteria was 88% sensitive and 72% specific for mortality or ICU admission.62 The CURB-65 tool was based on these criteria, with the addition of age ≥65 years, which was found to be a separate independent predictor of mortality. Thus, the 5 criteria making up the score are as follows (1 point each, 0-5 total):
Confusion, meaning Mental Test Score ≤8, or disorientation to person, place, or time
Urea >7 mmol/L (>19.6 mg/dL)
Respiratory rate ≥ 30 breaths/minute
Blood pressure (systolic < 90 mmHg or diastolic ≤ 60 mmHg)
Age ≥ 65 years
A score of 0-1 of these criteria characterized low mortality risk (<1.5%) in the test group, a score of 2 was intermediate mortality risk (9.2%), and a score of 3 or more associated with high mortality risk (22%). A score ≥ 2 was 93% sensitive and 49% specific for 30-day mortality.63
A subsequent prospective validation study by Aujesky et al that included 3181 patients with community-acquired pneumonia demonstrated slightly higher mortality rates for each CURB-65 score (0.6%, 3%, 6.1%, 13%, 17%, 43% mortality in scores of 0-5, respectively).64 In particular, the 3% mortality rate in CURB-65 scores of 1 is similar to PSI class III mortality rates, suggesting a lower threshold (CURB-65 ≥1) for consideration of admission for management. Another validation study by Capelastegui et al showed similar mortality rates to the derivation study for specific CURB-65 scores, but noted 53% of patients with a score of 1 also were found to have characteristics that were independent for a poor prognosis, and should be considered in the decision for outpatient or inpatient treatment.65 Furthermore, a recent study found that of patients in the ED with a CURB-65 score of 1, 8% still required critical care intervention.66 Thus, use of CURB-65 in screening for low-risk patients with community-acquired pneumonia is recommended to be limited to scores of 0. However, as with PSI, validation studies have yet to show predictive utility of scores suggesting severe pneumonia (CURB-65 ≥3) in predicting mortality or ICU requirement.60,61
As validation studies have suggested only patients with a CURB-65 score of 0 are screened low risk enough for outpatient treatment, greater weight may be placed on utility of CRB-65 as a tool. This rule, initially proposed in the same study as CURB-65, omits blood urea nitrogen as a factor to only rely on history and physical exam data with a score of 0 indicating low risk.63 In initial derivation and validation studies, this rule demonstrated <1.6% mortality risk with a score of 0, with risk increasing to 4-8.6% in scores of 1.63,65 Multiple studies have compared CRB-65 and CURB-65, with only marginal but not statistically significant improvement in prognostic utility of CURB-65.65,67 A meta-analysis of 1648 patients even showed only 0.5% mortality risk in CRB-65 ≤1; potentially including CRB-65 0-1 as low risk, though, would require further study.68 Although multiple validation studies have also successfully stratified low risk to similar mortality risk (<1.6%), accuracy wanes with higher CRB-65 scores.69
Several studies have directly compared CURB-65 and PSI both in terms of identifying low-risk patients and stratifying disease severity.60,61,64,68,70-72 Multiple studies have shown similar mortality risk in low-risk populations and have demonstrated sensitivities for mortality greater than 96% for CURB-65/CRB-65 = 0 and PSI class I-III, albeit with specificities ranging from 18-65%.64,68,70 In stratifying patients into different levels of severity (ward vs ICU patients), PSI has shown slightly better sensitivity/specificity for mortality and/or ICU intervention, though neither is strong enough to significantly stratify severe pneumonia to serve as tools for directing inpatient management.60,61
Comment: PSI, CRB-65, and CURB-65 have been well validated as screening tools for low-risk patients who should be treated as outpatients (CURB-65 or CRB-65 = 0, PSI class I and II). A moderate-risk population (CURB-65 = 1 or 2, PSI class III) may benefit from treatment as inpatient or outpatient at clinician judgement. Use of these tools for determining disease severity and possible ICU requirement is not as reliable, and other clinical factors should be considered.
Conclusion
This article provides an overview of several common clinical decision instruments and the evidence behind them. Ultimately, many institutions have incorporated clinical decision rules directly into the electronic medical record, and this strategy will not only increase their use, but hopefully collect further data on whether the instruments truly perform better than unstructured clinical judgement.
1. Perry JJ, Sivilotti MLA, Sutherland J, et al. Validation of the Ottawa Subarachnoid Hemorrhage Rule in patients with acute headache. CMAJ. 2017;189(45):E1379-E1385.
2. de Rooij NK, Linn FH, van der Plas JA, Algra A, Rinkel GJ. Incidence of subarachnoid haemorrhage: a systematic review with emphasis on region, age, gender and time trends. J Neurol Neurosurg Psychiatry. 2007;78(12):1365-1372.
3. Perry JJ, Stiell IG, Sivilotti ML, et al. Sensitivity of computed tomography performed within six hours of onset of headache for diagnosis of subarachnoid haemorrhage: prospective cohort study. BMJ. 2011;343:d4277.
4. Johnston SC, Rothwell PM, Nguyen-Huynh MN, et al. Validation and refinement of scores to predict very early stroke risk after transient ischaemic attack. Lancet. 2007;369(9558):283-292.
5. Easton JD, Saver JL, Albers GW, et al. Definition and evaluation of transient ischemic attack: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association Stroke Council; Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; and the Interdisciplinary Council on Peripheral Vascular Disease. The American Academy of Neurology affirms the value of this statement as an educational tool for neurologists. Stroke. 2009;40:2276-2293
6. Perry JJ, Sharma M, Sivilotti ML, et al. Prospective validation of the ABCD2 score for patients in the emergency department with transient ischemic attack. CMAJ. 2011;183(10):1137-1145.
7. Stead LG, Suravaram S, Bellolio MF, et al. An assessment of the incremental value of the ABCD2 score in the emergeny department evaluation of transient ischemic attack. Ann Emerg Med. 2011;57(1):46-51.
8. Alvarado A. A practical score for the early diagnosis of acute appendicitis. Ann Emerg Med. 1986;15(5):557-564.
9. Kalan M, Talbot D, Cunliffe WJ, Rich AJ. Evaluation of the modified Alvarado score in the diagnosis of acute appendicitis: a prospective study. Ann R Coll Surg Engl. 1994;76(6):418-419.
10. Ohle R, O'Reilly F, O'Brien KK, Fahey T, Dimitrov BD. The Alvarado score for predicting acute appendicitis: a systematic review. BMC Med. 2011;9:139.
11. Meltzer AC, Baumann BM, Chen EH, Shofer FS, Mills AM. Poor sensitivity of a modified Alvarado score in adults with suspected appendicitis. Ann Emerg Med. 2013;62(2):126-31.
12. Andersson M, Andersson RE. The appendicitis inflammatory response score: a tool for the diagnosis of acute appendicitis that outperforms the Alvarado score. World J Surg. 2008;32(8):1843-1849.
13. de Castro SM, Ünlü C, Steller EP, van Wagensveld BA, Vrouenraets BC. Evaluation of the appendicitis inflammatory response score for patients with acute appendicitis. World J Surg. 2012;36(7):1540-1545.
14. Kollár D, McCartan DP, Bourke M, Cross KS, Dowdall J. Predicting acute appendicitis? A comparison of the Alvarado score, the Appendicitis Inflammatory Response Score and clinical assessment. World J Surg. 2015;39(1):104-109.
15. Andersson M, Kolodziej B, Andersson RE; STRAPPSCORE Study Group. Randomized clinical trial of Appendicitis Inflammatory Response score-based management of patients with suspected appendicitis. Br J Surg. 2017;104(11):1451-1461.
16. Six AJ, Backus BE, Kelder JC. Chest pain in the emergency room: value of the HEART score. Netherlands Heart J. 2008;16(6):191-196.
17. Backus BE, Six AJ, Kelder JC, et al. Chest Pain in the Emergency Room. A Multicenter Validation of the HEART Score. Crit Pathways Cardiol. 2010;9:164-169.
18. Backus BE, Six AJ, Kelder JC, et al. A prospective validation of the HEART score for chest pain patients at the emergency department. In J Cardiol. 2013;168:2153-2158.
19. Six AJ, Cullen L, Backus BE, et al. The HEART score for the assessment of patients with chest pain in the emergency department. Crit Pathways Cardiol. 2013;12:121-126.
20. Mahler SA, Hiestand BC, Goff DC, Hoekstra JW, Miller CD. Can the HEART score safely reduce stress testing and cardiac imaging in patients at low risk for acute coronary syndrome? Crit Pathw Cardiol. 2011:10(3):128-133.
21. Mahler SA, Miller CD, Hollander JE, et al. Identifying patients for early discharge: performance of decision rules among patients with acute chest pain. Int J Cardiol. 2013;168(2):795-802.
22. Mahler SA, Riley RF, Hiestand BC, et al. The HEART Pathway Randomized Trial: identifying emergency department patients with acute chest pain for early discharge. Circ Cardiovasc Qual Outcomes. 2015;8(2):195-203.
23. Poldervaart JM, Reitsma JB, Backus BE, et al. Effect of using the HEART score in patients with chest pain in the emergency department: a stepped-wedge, cluster randomized trial. Ann Intern Med. 2017;166:687-697.
24. Antman EM, Cohen M, Bernink PJLM, et al. The TIMI risk score for unstable angina/non-ST eevation MI. JAMA. 2000;284:835-842.
25. Scirica BM, Cannon CP, Antman EM, et al. Validation of the Thrombolysis In Myocardial Infarction (TIMI) risk score for unstable angina pectoris and non-ST-elevation myocardial infarction in the TIMI III registry. Am J Cardiol. 2002;90:303-305.
26. Morrow DA, Antman EM, Snapinn SM, McCabe CH, Theroux P, Braunwald E. An integrated clinical approach to predicting the benefit of tirofiban in non-ST elevation acute coronary syndromes. Eur Heart J. 2002;23:223-229.
27. Pollack CV, Sites FD, Shofer FS, Sease KL, Hollander JE. Application of the TIMI risk score for unstable angina and non–ST-elevation acute coronary syndrome to an unselected emergency department chest pain population. Acad Emerg Med. 2006:13(1):13-18.
28. Chase M, Robey JL, Zogby KE, Sease KL, Shofer FS, Hollander JE. Prospective validation of the Thrombolysis in Myocardial Infarction risk score in the emergency department chest pain population. Ann Emerg Med. 2006;48(3):252-259.
29. Body R, Carley S, McDowell G, Ferguson J, Mackway-Jones K. Can a modified thrombolysis in myocardial infarction risk score outperform the original for risk stratifying emergency department patients with chest pain? Emerg Med J. 2009;26:95-99.
30. Hess EP, Perry JJ, Calder LA, et al. Prospective validation of a modified Thrombolysis In Myocardial Infarction risk score in emergency department patients with chest pain and possible acute coronary syndrome. Acad Emerg Med. 2010;17(4):368-375.
31. Macdonald SPJ, Nagree Y, Fatovich DM, ad Brown SGA. Modified TIMI risk score cannot be used to identify low-risk chest pain in the emergency department: a multicenter validation study. Emerg Med J. 2014;31:281-285.
32. Hess EP, Agarwal D, Chandra S, et al. Diagnostic accuracy of the TIMI risk score in patients with chest pain in the emergency department: a meta-analysis. CMAJ. 2010;182(10):1039-1044.
33. Than, M, Cullen L, Aldous S, et al. 2-Hour accelerated diagnostic protocol to assess patients with chest pain symptoms using contemporary troponins as the only biomarker: the ADAPT trial. JACC. 2012;59(23):2091-2098.
34. Carlton EW, Khattab A, Greaves K. Identifying patients suitable for discharge after a single-presentation high-sensitivity Troponin result: a comparison of five established risk scores and two high-sensitivity assays. Ann Emerg Med. 2015;66(6):635-645.
35. Poldervaart JM, Langedijk M, Backus BE, et al. Comparison of the GRACE, HEART and TIMI score to predict major adverse cardiac events in chest pain patients at the emergency department. Int J Cardiol. 2017;227:656-661.
36. Nieuwets A, Poldervaart JM, Reitsma JB, et al. Medical consumption compared for TIMI and HEART score in chest pain patients at the emergency department: a retrospective cost analysis. BMJ Open. 2016;6:e010694.
37. Wells PS, Ginsberg JS, Anderson DR, et al. Use of a clinical model for safe management of patients with suspected pulmonary embolism. Ann Intern Med. 1998;129:997-1005.
38. Wells PS, Anderson DR, Rodger M, et al. Derivation of a simple clinical model to categorize patients’ probability of pulmonary embolism: increasing the model’s utility with the SimpliRED D-dimer. Thromb Haemost. 2000;83(3):416-420.
39. Wells PS, Anderson DR, Rodger M, et al. Excluding pulmonary embolism at the bedside without diagnostic imaging: management of patients with suspected pulmonary embolism presenting to the emergency department by using a simple clinical model and D-dimer. Ann Intern Med. 2001;135:98-107.
40. Wolf SJ, McCubbin TR, Feldhaus KM, Faragher JP, Adcock DM. Prospective validation of Wells’ criteria in the evaluation of patients with suspected pulmonary embolism. Ann Emerg Med. 2004;44:503-510.
41. Chagnon I, Bounameaux H, Aujesky D, et al. Comparison of two clinical prediction rules and implicit assessment among patients with suspected pulmonary embolism. Am J Med. 2002;113:269-275.
42. Christopher Study Investigators. Effectiveness of managing suspected pulmonary embolism using an algorithm combining clinical probability, D-dimer testing, and computed tomography. JAMA. 2006;295:172-179.
43. Kline JA, Mitchell AM, Kabrhel C, Richman PB, Courtney DM. Clinical criteria to prevent unnecessary diagnostic testing in emergency department patients with suspected pulmonary embolism. J Thromb Haemost. 2004;2:1247-1255.
44. Kline JA, Courtney DM, Kabrhel C, et al. Propsective multicenter evaluation of the pulmonary embolism rule-out criteria. J Thromb Haemost. 2008;6:772-780.
45. Penaloza A, Soulie C, Moumneh T, et al. Pulmonary embolism rule-out criteria (PERC) rule in European patients with low implicit clinical probability (PERCEPIC): a multicenter, prospective, observational study. Lancet Haematol. 2017;4:e615-e621.
46. Freund Y, Cachanado M, Aubry A, et al. Effect of the Pulmonary Embolism Rule-Out Criteria on subsequent thromboembolic events among low-risk emergency department patients. The PROPER randomized clinical trial. JAMA. 2018;319(6):559-566.
47. Hugli O, Righini M, Le Gal G, et al. The pulmonary embolism rule-out criteria (PERC) rule does not safely exclude pulmonary embolism. J Thromb Haemost. 2011;9:300-4.
48. Theunissen JMG, Scholing C, van Hasselt WE, van der Maten J, ter Avest E. A retrospective analysis of the combined use of PERC rule and Wells score to exclude pulmonary embolism in the Emergency Department. Emerg Med J. 2016;33:696-701.
49. Singh B, Parsaik AK, Aharwal D, Surana A, Mascarenhas SS, Chandra S. Diagnostic accuracy of Pulmonary Embolism Rule-Out Criteria: a systematic review and meta-analysis. Ann Emerg Med. 2012;59(6):517-520.
50. Shapiro NI, Wolfe RE, Moore RB, Smith E, Burdick E, Bates DW. Mortality in Emergency Department Sepsis (MEDS) score: a prospectively derived and validated clinical prediction rule. Crit Care Med. 2003;31(3):670-675.
51. Shapiro NI, Howell MD, Talmor D, Donnino M, Ngo L, Bates DW. Mortality in Emergency Department Sepsis (MEDS) score predicts 1-year mortality. Crit Care Med. 2007;35(1):192-198.
52. Sankoff JD, Goyal M, Gaieski DF, et al. Validation of the Mortality in Emergency Department Sepsis (MEDS) score in patients with the systemic inflammatory response syndrome (SIRS). Crit Care Med. 2008;36(2):421-26.
53. Jones AE, Saak K, Kline JA. Performance of the Mortality in Emergency Department Sepsis score for predicting hospital mortality among patients with severe sepsis and septic shock. Am J Emerg Med. 2008;26(6):689-692.
54. Carpenter CR., Keim SM, Upadhye S, Nguyen HB. Risk stratification of the potentially septic patient in the emergency department: the Mortality in the Emergency Department Sepsis (MEDS) score. J Emerg Med. 2009;37(3):319-327.
55. Hermans MAW, Leffers P, Jansen LM, Keulemans YC, Stassen PM. The value of the Mortality in Emergency Department Sepsis (MEDS) score, C reactive protein and lactate in predicting 28-day mortality of sepsis in a Dutch emergency department. Emerg Med J. 2012;29(4):295–300.
56. Fine MJ, Auble TE, Yealy DM, et al. A Prediction Rule to Identify Low-Risk Patients with Community Acquired Pneumonia. N Engl J Med. 1997;326(4):243-250.
57. Marrie TJ, Lau CY, Wheeler SL, et al. A controlled trial of a critical pathway for treatment of community-acquired pneumonia. JAMA. 2000;283(6):749-755. doi:10.1001/jama.283.6.749.
58. Carratalà J, Fernandez-Sabe N. Outpatient care compared with hospitalization for community-acquired pneumonia: a randomized trial in low-risk patients . Ann Intern Med. 2005;142:165-172. doi:10.7326/0003-4819-142-3-200502010-00006.
59. Chalmers JD, Akram AR, Hill AT. Increasing outpatient treatment of mild community-acquired pneumonia: Systematic review and meta-analysis. Eur Respir J. 2011;37(4):858-864. doi:10.1183/09031936.00065610.
60. Loke YK, Kwok CS, Niruban A, Myint PK. Value of severity scales in predicting mortality from community-acquired pneumonia: systematic review and meta-analysis. Thorax. 2010;65(10):884-890. doi:10.1136/thx.2009.134072.
61. Marti C, Garin N, Grosgurin O, et al. Prediction of severe community-acquired pneumonia: A systematic review and meta-analysis. Crit Care. 2012;16(4):R141. doi:10.1186/cc11447.
62. Neill AM, Martin IR, Weir R, et al. Community-acquired pneumonia: aetiology and usefulness of severity criteria on admission. Thorax. 1996;51(10):1010-1016. doi:10.1136/thx.51.10.1010.
63. Lim WS, Van Der Eerden MM, Laing R, et al. Defining community acquired pneumonia severity on presentation to hospital: An international derivation and validation study. Thorax. 2003;58(5):377-382. doi:10.1136/thorax.58.5.377.
64. Aujesky D, Auble TE, Yealy DM, et al. Prospective comparison of three validated prediction rules for prognosis in community-acquired pneumonia. Am J Med. 2005;118(4):384-392. doi:10.1016/j.amjmed.2005.01.006.
65. Capelastegui A, España PP, Quintana JM, et al. Validation of a predictive rule for the management of community-acquired pneumonia. Eur Respir J. 2006;27(1):151-157. doi:10.1183/09031936.06.00062505.
66. Ilg A, Moskowitz A, Konanki V, et al. Performance of the CURB-65 score in predicting critical care interventions in patients admitted with community-acquired pneumonia. Ann Emerg Med. 2018. doi:10.1016/j.annemergmed.2018.06.017.
67. Bauer TT, Ewig S, Marre R, Suttorp N, Welte T. CRB-65 predicts death from community-acquired pneumonia. J Intern Med. 2006;260(1):93-101. doi:10.1111/j.1365-2796.2006.01657.x.
68. Akram AR, Chalmers JD, Hill AT. Predicting mortality with severity assessment tools in out-patients with community-acquired pneumonia. QJM. 2011;104(10):871-879. doi:10.1093/qjmed/hcr088.
69. McNally M, Curtain J, O’Brien KK, Dimitrov BD, Fahey T. Validity of British Thoracic Society guidance (the CRB-65 rule) for predicting the severity of pneumonia in general practice: Systematic review and meta-analysis. Br J Gen Pract. 2010;60(579):423-433. doi:10.3399/bjgp10X532422.
70. Shah BA, Ahmed W, Dhobi GN, Shah NN, Khursheed SQ, Haq I. Validity of Pneumonia Severity Index and CURB-65 severity scoring systems in community acquired pneumonia in an Indian Setting. Indian J Chest Dis Allied Sci. 2010;52(1):9-17.
71. Noguchi S, Yatera K, Kawanami T, et al. Pneumonia severity assessment tools for predicting mortality in patients with cealthcare-associated pneumonia: a systematic review and meta-analysis. Respiration. 2017;93(6):441-450. doi:10.1159/000470915.
72. Kolditz M, Braeken D, Ewig S, Rohde G. Severity assessment and the immediate and long-term prognosis in community-acquired pneumonia. Semin Respir Crit Care Med. 2016;37(6):886-896. doi:http://dx.doi.org/10.1055/s-0036-1592127.
1. Perry JJ, Sivilotti MLA, Sutherland J, et al. Validation of the Ottawa Subarachnoid Hemorrhage Rule in patients with acute headache. CMAJ. 2017;189(45):E1379-E1385.
2. de Rooij NK, Linn FH, van der Plas JA, Algra A, Rinkel GJ. Incidence of subarachnoid haemorrhage: a systematic review with emphasis on region, age, gender and time trends. J Neurol Neurosurg Psychiatry. 2007;78(12):1365-1372.
3. Perry JJ, Stiell IG, Sivilotti ML, et al. Sensitivity of computed tomography performed within six hours of onset of headache for diagnosis of subarachnoid haemorrhage: prospective cohort study. BMJ. 2011;343:d4277.
4. Johnston SC, Rothwell PM, Nguyen-Huynh MN, et al. Validation and refinement of scores to predict very early stroke risk after transient ischaemic attack. Lancet. 2007;369(9558):283-292.
5. Easton JD, Saver JL, Albers GW, et al. Definition and evaluation of transient ischemic attack: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association Stroke Council; Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; and the Interdisciplinary Council on Peripheral Vascular Disease. The American Academy of Neurology affirms the value of this statement as an educational tool for neurologists. Stroke. 2009;40:2276-2293
6. Perry JJ, Sharma M, Sivilotti ML, et al. Prospective validation of the ABCD2 score for patients in the emergency department with transient ischemic attack. CMAJ. 2011;183(10):1137-1145.
7. Stead LG, Suravaram S, Bellolio MF, et al. An assessment of the incremental value of the ABCD2 score in the emergeny department evaluation of transient ischemic attack. Ann Emerg Med. 2011;57(1):46-51.
8. Alvarado A. A practical score for the early diagnosis of acute appendicitis. Ann Emerg Med. 1986;15(5):557-564.
9. Kalan M, Talbot D, Cunliffe WJ, Rich AJ. Evaluation of the modified Alvarado score in the diagnosis of acute appendicitis: a prospective study. Ann R Coll Surg Engl. 1994;76(6):418-419.
10. Ohle R, O'Reilly F, O'Brien KK, Fahey T, Dimitrov BD. The Alvarado score for predicting acute appendicitis: a systematic review. BMC Med. 2011;9:139.
11. Meltzer AC, Baumann BM, Chen EH, Shofer FS, Mills AM. Poor sensitivity of a modified Alvarado score in adults with suspected appendicitis. Ann Emerg Med. 2013;62(2):126-31.
12. Andersson M, Andersson RE. The appendicitis inflammatory response score: a tool for the diagnosis of acute appendicitis that outperforms the Alvarado score. World J Surg. 2008;32(8):1843-1849.
13. de Castro SM, Ünlü C, Steller EP, van Wagensveld BA, Vrouenraets BC. Evaluation of the appendicitis inflammatory response score for patients with acute appendicitis. World J Surg. 2012;36(7):1540-1545.
14. Kollár D, McCartan DP, Bourke M, Cross KS, Dowdall J. Predicting acute appendicitis? A comparison of the Alvarado score, the Appendicitis Inflammatory Response Score and clinical assessment. World J Surg. 2015;39(1):104-109.
15. Andersson M, Kolodziej B, Andersson RE; STRAPPSCORE Study Group. Randomized clinical trial of Appendicitis Inflammatory Response score-based management of patients with suspected appendicitis. Br J Surg. 2017;104(11):1451-1461.
16. Six AJ, Backus BE, Kelder JC. Chest pain in the emergency room: value of the HEART score. Netherlands Heart J. 2008;16(6):191-196.
17. Backus BE, Six AJ, Kelder JC, et al. Chest Pain in the Emergency Room. A Multicenter Validation of the HEART Score. Crit Pathways Cardiol. 2010;9:164-169.
18. Backus BE, Six AJ, Kelder JC, et al. A prospective validation of the HEART score for chest pain patients at the emergency department. In J Cardiol. 2013;168:2153-2158.
19. Six AJ, Cullen L, Backus BE, et al. The HEART score for the assessment of patients with chest pain in the emergency department. Crit Pathways Cardiol. 2013;12:121-126.
20. Mahler SA, Hiestand BC, Goff DC, Hoekstra JW, Miller CD. Can the HEART score safely reduce stress testing and cardiac imaging in patients at low risk for acute coronary syndrome? Crit Pathw Cardiol. 2011:10(3):128-133.
21. Mahler SA, Miller CD, Hollander JE, et al. Identifying patients for early discharge: performance of decision rules among patients with acute chest pain. Int J Cardiol. 2013;168(2):795-802.
22. Mahler SA, Riley RF, Hiestand BC, et al. The HEART Pathway Randomized Trial: identifying emergency department patients with acute chest pain for early discharge. Circ Cardiovasc Qual Outcomes. 2015;8(2):195-203.
23. Poldervaart JM, Reitsma JB, Backus BE, et al. Effect of using the HEART score in patients with chest pain in the emergency department: a stepped-wedge, cluster randomized trial. Ann Intern Med. 2017;166:687-697.
24. Antman EM, Cohen M, Bernink PJLM, et al. The TIMI risk score for unstable angina/non-ST eevation MI. JAMA. 2000;284:835-842.
25. Scirica BM, Cannon CP, Antman EM, et al. Validation of the Thrombolysis In Myocardial Infarction (TIMI) risk score for unstable angina pectoris and non-ST-elevation myocardial infarction in the TIMI III registry. Am J Cardiol. 2002;90:303-305.
26. Morrow DA, Antman EM, Snapinn SM, McCabe CH, Theroux P, Braunwald E. An integrated clinical approach to predicting the benefit of tirofiban in non-ST elevation acute coronary syndromes. Eur Heart J. 2002;23:223-229.
27. Pollack CV, Sites FD, Shofer FS, Sease KL, Hollander JE. Application of the TIMI risk score for unstable angina and non–ST-elevation acute coronary syndrome to an unselected emergency department chest pain population. Acad Emerg Med. 2006:13(1):13-18.
28. Chase M, Robey JL, Zogby KE, Sease KL, Shofer FS, Hollander JE. Prospective validation of the Thrombolysis in Myocardial Infarction risk score in the emergency department chest pain population. Ann Emerg Med. 2006;48(3):252-259.
29. Body R, Carley S, McDowell G, Ferguson J, Mackway-Jones K. Can a modified thrombolysis in myocardial infarction risk score outperform the original for risk stratifying emergency department patients with chest pain? Emerg Med J. 2009;26:95-99.
30. Hess EP, Perry JJ, Calder LA, et al. Prospective validation of a modified Thrombolysis In Myocardial Infarction risk score in emergency department patients with chest pain and possible acute coronary syndrome. Acad Emerg Med. 2010;17(4):368-375.
31. Macdonald SPJ, Nagree Y, Fatovich DM, ad Brown SGA. Modified TIMI risk score cannot be used to identify low-risk chest pain in the emergency department: a multicenter validation study. Emerg Med J. 2014;31:281-285.
32. Hess EP, Agarwal D, Chandra S, et al. Diagnostic accuracy of the TIMI risk score in patients with chest pain in the emergency department: a meta-analysis. CMAJ. 2010;182(10):1039-1044.
33. Than, M, Cullen L, Aldous S, et al. 2-Hour accelerated diagnostic protocol to assess patients with chest pain symptoms using contemporary troponins as the only biomarker: the ADAPT trial. JACC. 2012;59(23):2091-2098.
34. Carlton EW, Khattab A, Greaves K. Identifying patients suitable for discharge after a single-presentation high-sensitivity Troponin result: a comparison of five established risk scores and two high-sensitivity assays. Ann Emerg Med. 2015;66(6):635-645.
35. Poldervaart JM, Langedijk M, Backus BE, et al. Comparison of the GRACE, HEART and TIMI score to predict major adverse cardiac events in chest pain patients at the emergency department. Int J Cardiol. 2017;227:656-661.
36. Nieuwets A, Poldervaart JM, Reitsma JB, et al. Medical consumption compared for TIMI and HEART score in chest pain patients at the emergency department: a retrospective cost analysis. BMJ Open. 2016;6:e010694.
37. Wells PS, Ginsberg JS, Anderson DR, et al. Use of a clinical model for safe management of patients with suspected pulmonary embolism. Ann Intern Med. 1998;129:997-1005.
38. Wells PS, Anderson DR, Rodger M, et al. Derivation of a simple clinical model to categorize patients’ probability of pulmonary embolism: increasing the model’s utility with the SimpliRED D-dimer. Thromb Haemost. 2000;83(3):416-420.
39. Wells PS, Anderson DR, Rodger M, et al. Excluding pulmonary embolism at the bedside without diagnostic imaging: management of patients with suspected pulmonary embolism presenting to the emergency department by using a simple clinical model and D-dimer. Ann Intern Med. 2001;135:98-107.
40. Wolf SJ, McCubbin TR, Feldhaus KM, Faragher JP, Adcock DM. Prospective validation of Wells’ criteria in the evaluation of patients with suspected pulmonary embolism. Ann Emerg Med. 2004;44:503-510.
41. Chagnon I, Bounameaux H, Aujesky D, et al. Comparison of two clinical prediction rules and implicit assessment among patients with suspected pulmonary embolism. Am J Med. 2002;113:269-275.
42. Christopher Study Investigators. Effectiveness of managing suspected pulmonary embolism using an algorithm combining clinical probability, D-dimer testing, and computed tomography. JAMA. 2006;295:172-179.
43. Kline JA, Mitchell AM, Kabrhel C, Richman PB, Courtney DM. Clinical criteria to prevent unnecessary diagnostic testing in emergency department patients with suspected pulmonary embolism. J Thromb Haemost. 2004;2:1247-1255.
44. Kline JA, Courtney DM, Kabrhel C, et al. Propsective multicenter evaluation of the pulmonary embolism rule-out criteria. J Thromb Haemost. 2008;6:772-780.
45. Penaloza A, Soulie C, Moumneh T, et al. Pulmonary embolism rule-out criteria (PERC) rule in European patients with low implicit clinical probability (PERCEPIC): a multicenter, prospective, observational study. Lancet Haematol. 2017;4:e615-e621.
46. Freund Y, Cachanado M, Aubry A, et al. Effect of the Pulmonary Embolism Rule-Out Criteria on subsequent thromboembolic events among low-risk emergency department patients. The PROPER randomized clinical trial. JAMA. 2018;319(6):559-566.
47. Hugli O, Righini M, Le Gal G, et al. The pulmonary embolism rule-out criteria (PERC) rule does not safely exclude pulmonary embolism. J Thromb Haemost. 2011;9:300-4.
48. Theunissen JMG, Scholing C, van Hasselt WE, van der Maten J, ter Avest E. A retrospective analysis of the combined use of PERC rule and Wells score to exclude pulmonary embolism in the Emergency Department. Emerg Med J. 2016;33:696-701.
49. Singh B, Parsaik AK, Aharwal D, Surana A, Mascarenhas SS, Chandra S. Diagnostic accuracy of Pulmonary Embolism Rule-Out Criteria: a systematic review and meta-analysis. Ann Emerg Med. 2012;59(6):517-520.
50. Shapiro NI, Wolfe RE, Moore RB, Smith E, Burdick E, Bates DW. Mortality in Emergency Department Sepsis (MEDS) score: a prospectively derived and validated clinical prediction rule. Crit Care Med. 2003;31(3):670-675.
51. Shapiro NI, Howell MD, Talmor D, Donnino M, Ngo L, Bates DW. Mortality in Emergency Department Sepsis (MEDS) score predicts 1-year mortality. Crit Care Med. 2007;35(1):192-198.
52. Sankoff JD, Goyal M, Gaieski DF, et al. Validation of the Mortality in Emergency Department Sepsis (MEDS) score in patients with the systemic inflammatory response syndrome (SIRS). Crit Care Med. 2008;36(2):421-26.
53. Jones AE, Saak K, Kline JA. Performance of the Mortality in Emergency Department Sepsis score for predicting hospital mortality among patients with severe sepsis and septic shock. Am J Emerg Med. 2008;26(6):689-692.
54. Carpenter CR., Keim SM, Upadhye S, Nguyen HB. Risk stratification of the potentially septic patient in the emergency department: the Mortality in the Emergency Department Sepsis (MEDS) score. J Emerg Med. 2009;37(3):319-327.
55. Hermans MAW, Leffers P, Jansen LM, Keulemans YC, Stassen PM. The value of the Mortality in Emergency Department Sepsis (MEDS) score, C reactive protein and lactate in predicting 28-day mortality of sepsis in a Dutch emergency department. Emerg Med J. 2012;29(4):295–300.
56. Fine MJ, Auble TE, Yealy DM, et al. A Prediction Rule to Identify Low-Risk Patients with Community Acquired Pneumonia. N Engl J Med. 1997;326(4):243-250.
57. Marrie TJ, Lau CY, Wheeler SL, et al. A controlled trial of a critical pathway for treatment of community-acquired pneumonia. JAMA. 2000;283(6):749-755. doi:10.1001/jama.283.6.749.
58. Carratalà J, Fernandez-Sabe N. Outpatient care compared with hospitalization for community-acquired pneumonia: a randomized trial in low-risk patients . Ann Intern Med. 2005;142:165-172. doi:10.7326/0003-4819-142-3-200502010-00006.
59. Chalmers JD, Akram AR, Hill AT. Increasing outpatient treatment of mild community-acquired pneumonia: Systematic review and meta-analysis. Eur Respir J. 2011;37(4):858-864. doi:10.1183/09031936.00065610.
60. Loke YK, Kwok CS, Niruban A, Myint PK. Value of severity scales in predicting mortality from community-acquired pneumonia: systematic review and meta-analysis. Thorax. 2010;65(10):884-890. doi:10.1136/thx.2009.134072.
61. Marti C, Garin N, Grosgurin O, et al. Prediction of severe community-acquired pneumonia: A systematic review and meta-analysis. Crit Care. 2012;16(4):R141. doi:10.1186/cc11447.
62. Neill AM, Martin IR, Weir R, et al. Community-acquired pneumonia: aetiology and usefulness of severity criteria on admission. Thorax. 1996;51(10):1010-1016. doi:10.1136/thx.51.10.1010.
63. Lim WS, Van Der Eerden MM, Laing R, et al. Defining community acquired pneumonia severity on presentation to hospital: An international derivation and validation study. Thorax. 2003;58(5):377-382. doi:10.1136/thorax.58.5.377.
64. Aujesky D, Auble TE, Yealy DM, et al. Prospective comparison of three validated prediction rules for prognosis in community-acquired pneumonia. Am J Med. 2005;118(4):384-392. doi:10.1016/j.amjmed.2005.01.006.
65. Capelastegui A, España PP, Quintana JM, et al. Validation of a predictive rule for the management of community-acquired pneumonia. Eur Respir J. 2006;27(1):151-157. doi:10.1183/09031936.06.00062505.
66. Ilg A, Moskowitz A, Konanki V, et al. Performance of the CURB-65 score in predicting critical care interventions in patients admitted with community-acquired pneumonia. Ann Emerg Med. 2018. doi:10.1016/j.annemergmed.2018.06.017.
67. Bauer TT, Ewig S, Marre R, Suttorp N, Welte T. CRB-65 predicts death from community-acquired pneumonia. J Intern Med. 2006;260(1):93-101. doi:10.1111/j.1365-2796.2006.01657.x.
68. Akram AR, Chalmers JD, Hill AT. Predicting mortality with severity assessment tools in out-patients with community-acquired pneumonia. QJM. 2011;104(10):871-879. doi:10.1093/qjmed/hcr088.
69. McNally M, Curtain J, O’Brien KK, Dimitrov BD, Fahey T. Validity of British Thoracic Society guidance (the CRB-65 rule) for predicting the severity of pneumonia in general practice: Systematic review and meta-analysis. Br J Gen Pract. 2010;60(579):423-433. doi:10.3399/bjgp10X532422.
70. Shah BA, Ahmed W, Dhobi GN, Shah NN, Khursheed SQ, Haq I. Validity of Pneumonia Severity Index and CURB-65 severity scoring systems in community acquired pneumonia in an Indian Setting. Indian J Chest Dis Allied Sci. 2010;52(1):9-17.
71. Noguchi S, Yatera K, Kawanami T, et al. Pneumonia severity assessment tools for predicting mortality in patients with cealthcare-associated pneumonia: a systematic review and meta-analysis. Respiration. 2017;93(6):441-450. doi:10.1159/000470915.
72. Kolditz M, Braeken D, Ewig S, Rohde G. Severity assessment and the immediate and long-term prognosis in community-acquired pneumonia. Semin Respir Crit Care Med. 2016;37(6):886-896. doi:http://dx.doi.org/10.1055/s-0036-1592127.
Playing by the Rules: Using Decision Rules Wisely Part 1, Trauma
Emergency physicians (EPs) rely on rapid diagnostic testing to help screen patients for illnesses. While the decision to order a test for a patient should be driven by an objective assessment of pretest probability, other factors such as fear of litigation, clinical inexperience, or desire for increased patient satisfaction can prompt testing even when the likelihood of disease is low. This in turn leads to practice variability, increased cost, and decreased ED throughput, as well as other risks attendant to overtesting and overtreatment. Conversely, practitioners may fail to order necessary tests despite the presence of high-risk clinical features, which in turn may lead to misdiagnoses and delay in initiating life-saving treatments.
Development of Decision Rules
Clinical decision rules seek to decrease resource utilization in instances of low probability of disease and to identify high-risk features that should prompt further investigation. The formation of clinical decision rules entails at least three steps, which Ian Stiell, MD, emergency medicine’s (EM’s) most prolific author of these instruments, describes as follows:
- Creation of the rule or derivation;
- Prospective assessment of the reliability, accuracy, and impact of the rule in a validation study; and
- Gauging the effect of the rule on patient care through an implementation study.1
In addition to these three steps, many clinicians argue that there should also be an important fourth step included in this process: the external validation or assessment of the rule outside of the original study site(s), to assure reliability of the rule across a variety of populations for which its use was intended.2
Critiques and Caveats
A common critique of clinical decision rules is that they may not necessarily outperform subjective physician judgment, and that those who create these rules often do not explicitly compare their instruments against independent unassisted decision-making by clinicians.2,3
Another drawback is that the misapplication of these rules can lead to increased testing, something particularly problematic for one-way rules, which only guide the provider in a single clinical direction. An example of a one-way rule is the Pulmonary Embolism Rule-Out Criteria (PERC), which advises that a low-risk patient who does not have any of the PERC factors will not require any further testing. This, however, does not necessarily mean that further testing is indicated in patients who have one of the PERC factors present.2 Thus, applying PERC and other one-way decision-making rules in a two-way fashion can prompt testing that would not be ordered based on clinician gestalt. Rules that are designed to help determine when testing is necessary and when it is unnecessary are referred to as two-way rules, an example of which is the Ottawa Ankle Rule.
Controversies aside, the incorporation of clinical decision rules in the electronic medical record of many institutions and the proliferation of smartphone applications utilizing these instruments have further cemented their place in EM. This article describes the more commonly used ED clinical decision rules, as well as pearls and pitfalls pertaining to their use. Part 1 that follows covers important validated rules related to trauma patients in the ED. Part 2, which will appear in an upcoming 2018 issue, will cover nontrauma medical-diagnosis decision rules, including pulmonary embolism, and pneumonia.
Head Trauma
The increased utilization of computed tomography (CT) studies to assess for minor blunt head trauma spurred the development of clinical decision rules. In adult patients, the most popular and well-studied instruments are the New Orleans Criteria (NOC), the Canadian CT Head Rule (CCHR), and the National Emergency X-Radiography Utilization Study (NEXUS) CT Head Rule.
New Orleans Criteria
The NOC validation cohort examined over 900 cases at a single trauma center, enrolling all patients 3 years of age and older who had suffered minor head trauma (defined as loss of consciousness (LOC) in a patient with grossly normal neurological examination and a Glasgow Coma Scale [GCS] score of 15), in the preceding 24 hours.4 Patients who experienced no LOC, had focal neurological deficit (except isolated short-term memory deficits), or who did not have any CT study performed, were excluded.
The NOC describes seven factors for consideration:
- Short-term memory deficits;
- Intoxication with drugs or alcohol;
- Physical evidence of trauma above the clavicles;
- Patients older than age 60 years;
- Seizure;
- Headache; and
- Vomiting.
The presence of at least one of these factors was found to be 100% sensitive and 25% specific for the presence of any traumatic intracranial abnormality on CT, though only 6.5% of patients in the derivation and validation cohorts had positive CT scans, and ultimately less than 1% had lesions that required surgery.4
Canadian CT Head Rule
The CCHR validation study assessed over 2,700 patients at nine Canadian EDs, enrolling all patients aged 16 years and older who sustained a blunt head trauma less than 24 hours prior to presentation and who had a GCS score of 13 or higher. The investigators of the CCHR study specified that included patients should have suffered a witnessed LOC, definite amnesia, or a witnessed disorientation.5 Patients who did not have any of these factors were deemed to have minimal head trauma and were excluded from the study. Also excluded from this study were patients who had seizure prior to ED arrival, had a coagulopathy or used oral anticoagulants, had acute focal neurological deficit or obvious depressed skull fracture, had unstable vitals associated with a major trauma, or were pregnant.5 The CCHR was not designed to be applied to these excluded populations. Of note, patients with drug and alcohol intoxication were included in their validation.6
The CCHR describes five high-risk factors that increase the likelihood of requiring acute neurosurgical intervention:
- A GCS score of less than 15 at 2 hours after injury;
- Suspected open or depressed skull fracture;
- Any sign of basal skull fracture (eg, hemotympanum, raccoon eyes, cerebrospinal fluid otorrhea/rhinorrhea, Battle’s sign;
- Two or more episodes of vomiting; or
- Patients aged 65 years or older.
In addition to these five high-risk factors, the CCHR also describes two medium risk criteria for finding any traumatic lesion on CT that would not necessitate acute neurosurgical intervention: amnesia of greater than 30 minutes before impact; and injury resulting from a dangerous mechanism such as a pedestrian struck by motor vehicle, occupant ejected from a motor vehicle, or a fall from a height greater than 3 feet or from over 5 stair-steps.
The presence of any one or more of the five high-risk factors was 100% sensitive for predicting the need for neurosurgical intervention, and taken together, having one or more of the seven factors was 100% sensitive for predicting clinically important brain injury.5
NEXUS CT Head Rule
The NEXUS CT Head Rule validation cohort included over 11,000 pediatric and adult blunt head trauma patients undergoing CT imaging at four hospital EDs, and excluded patients with penetrating injuries or presentation greater than 24 hours after injury.7 Patients were considered to be low risk if none of the following criteria were present:
- Age 65 years or older;
- Evidence of significant skull fracture;
- Scalp hematoma;
- Neurological deficit;
- Altered level of alertness;
- Abnormal behavior;
- Coagulopathy; and
- Recurrent vomiting.
Patients who have one or more of these factors were considered as high risk. The presence of one of these factors was 100% sensitive for detecting patients with lesions requiring neurosurgery and 99% sensitive for detecting any significant intracranial injury, with specificity for either condition at 25%.7
Decision-Rule Sensitivity Comparison
Though the CCHR, NOC, and NEXUS rules differ in their inclusion/exclusion criteria, they have been compared to each other in different populations in the medical literature. A subgroup of the CCHR validation cohort and an accompanying external validation study of over 3,000 patients both found that the CCHR and the NOC were at least as sensitive (100%) in detecting lesions requiring neurosurgical intervention, but the CCHR was more specific and had greater potential to reduce imaging rates.5,8 Another study examined the performance of NEXUS, CCHR, NOC, and other decision instruments in a database of nearly 8,000 adolescent and adult head trauma patients. The authors of this study found the three rules to have similarly high sensitivities (97% to 99%) for detecting clinically important findings, but felt NEXUS to have the best combination of sensitivity and specificity compared to CCHR and NOC.9
Comment: A decision rule to decrease CT utilization in intoxicated head trauma patients is particularly useful, but only the CCHR can help potentially avoid imaging a drug or alcohol-intoxicated patient with abnormal behavior or altered level of alertness. Similarly, distinguishing superficial scalp trauma from more worrisome signs of intracranial injury is important, but the NOC and NEXUS rules recommend imaging for any trauma above the clavicles and
Though the rules have similar sensitivities, the CCHR appears to have the greatest potential for aiding clinical decision-making. Of note, all of the adult decision rules consider patients older than age 60 or 65 years to be a high-risk feature. An instrument with better specificity for geriatric patients would be immensely helpful as our population continues to age.
The Pediatric Population: The PECARN Rule
The CCHR, NEXUS, and NOC have been variously applied to pediatric populations, and the NEXUS and NOC included children (patients aged 3 years and older in the NOC) in their validation cohorts. Perhaps the most widely utilized validated rule for pediatric head trauma in the United States is the Pediatric Emergency Care Applied Research Network (PECARN) rule.
The PECARN rule is an age-specific instrument for assessing pediatric blunt head trauma patients for clinically important traumatic brain injury (TBI)—ie, brain injuries resulting in death, neurosurgery, intubation longer than 24 hours, or hospital admission length of more than two nights.10 The PECARN algorithm as described in its validation study is reproduced in Figure 1.
Patients with trivial injury mechanisms such as ground level falls or running into stationary objects and no signs or symptoms of head trauma other than scalp abrasions or lacerations were excluded from the PECARN analysis, as were patients with pre-existing neurological disorders, including ventricular shunts and brain tumors, patients with penetrating trauma, and those with bleeding disorders. The validation study of over 8,000 children found the presence of any of the criteria to be 100% and 96.8% sensitive in detecting clinically important TBI in children aged less than 2 years and children aged 2 years or older, respectively.
The PECARN rule was recently assessed in a large prospective cohort against two less extensively studied clinical decision rules: the Children’s Head Injury Algorithm for the Prediction of Important Clinical Events (CHALICE) and the Canadian Assessment of Tomography for Childhood Head Injury (CATCH). Though the sample size was over 20,000 patients, only less than 1% required neurosurgery or died. The PECARN rule was determined to have the highest validation sensitivities (100% for <2 years, 99% for ≥2 years) of all of the rules; however, it has been noted by some clinicians that the strict application of the PECARN rule to the study population would have increased the rate of CT scanning 5-fold without providing any clear benefit over clinical judgment in detecting injury.11,12
Comment: The PECARN tool is by far the most robust instrument for pediatric head trauma, but striking a balance between finding otherwise clinically occult injury and reducing unnecessary testing/irradiation remains difficult in this vulnerable population.
Cervical Spine Trauma
Though the incidence of serious cervical spine injury in blunt trauma is low, the potentially devastating consequences of a missed lesion is a potent driver of radiographic testing.13 The Nexus Criteria and Canadian C-Spine Rule were developed to assist the clinician in determining when radiographic imaging is indicated in patients presenting with a blunt-trauma-related injury. The NEXUS criteria were developed to decrease cervical spine X-ray use based on five low-risk factors:
- No posterior midline tenderness;
- No focal neurological deficit;
- Normal level of alertness;
- No evidence of intoxication; and
- No clinically apparent pain that could distract the patient from the pain of a cervical spine injury.13
Patients meeting these low-risk criteria were considered to not have a clinically significant cervical spine injury. Of note, the NEXUS investigators deemed several isolated radiographic lesions to be clinically insignificant in their analysis, including spinous process fractures, simple wedge-compression fractures without loss of 25% or more of vertebral body height, isolated avulsion fractures without ligamentous injury, type 1 odontoid fractures, transverse process fractures, end-plate fractures, trabecular bony injuries, and osteophyte fractures, except corner or teardrop fractures.13
The NEXUS validation study included 34,000 blunt trauma patients, including 3,000 patients aged 1 to 17 years and nearly 3,000 elderly patients, all of whom received at least 3-view X-rays (cross-table lateral, anteroposterior view, and open-mouth odontoid view) unless CT or magnetic resonance imaging was performed because X-rays were deemed impractical or impossible.13-15
The five low-risk features of NEXUS had a sensitivity of 99% in excluding clinically significant cervical spine trauma, and the authors determined that X-rays could have been avoided in more than 12% of the study population.
The NEXUS criteria have been criticized as being less reliable at the extremes of age, and the study authors have specifically urged caution in the use of this rule for infants and toddlers given the small number of these patients in the validation cohort.14
There have been multiple case reports and studies suggesting that the NEXUS rule does not perform well in elderly patients.15,16 Recent research has suggested that substituting “deviation from baseline mental status” for “normal level of alertness” and signs of head and neck trauma for distracting injury may improve specificity for detecting clinically significant injuries in geriatric fall patients, though the sample size does not approach the numbers from the original validation cohort.15,17
Canadian C-Spine Rule
The Canadian C-spine Rule (CCR), described in Figure 2, is more complex than the NEXUS criteria, but there are data to suggest it performs better in head-to-head evaluations.18
Patients were assessed primarily on the basis of the three-view X-rays used in the NEXUS validation, however, only 71.7% of patients received radiographs and the remainder of patients were assessed using a telephone survey the authors had created during the derivation phase.18 Some lesions were deemed to be clinically unimportant, including isolated osteophyte avulsion, isolated fracture of a transverse process not involving a facet joint, isolated fracture of a spinous process not involving the lamina, or simple compression fracture involving less than 25% of the vertebral body height.18
Unfortunately, the CCR validation study was limited by incomplete evaluation in 10% of cases, though multiple subgroup analyses consistently demonstrated the CCR was 95% sensitive or higher for detecting clinically important cervical spine injury, outperforming NEXUS. Subsequently, a large systematic review of 15 studies shows sensitivity of the CCR to be 90% to 100% and NEXUS to be 83% to 100%.19
Comment: The NEXUS criteria were validated in a larger and more heterogeneous cohort than CCR, and also have the advantage of being easier to remember. Using either rule, clinicians must consider that “clinically unimportant” cervical spine fractures are not excluded. Ultimately, the landscape of cervical spine assessment has shifted to performing CT over plain radiographs, and these rules should be re-evaluated in this context.20
Blunt Chest Trauma
NEXUS Chest Guidelines
The NEXUS chest guidelines are more recent developments to help assess the need for chest imaging in the patient presenting with a blunt trauma. The first rule derived and validated by the investigators examined the utility of seven clinical criteria in predicting the need for chest imaging—either X-ray or CT:
- Patients older than age 60 years;
- Rapid deceleration mechanism defined as fall greater than 20 feet or motor vehicle crash greater than 40 mph;
- Chest pain;
- Intoxication;
- Abnormal alertness/mental status;
- Painful distracting injury; and
- Chest wall tenderness to palpation, with the exception of isolated clavicular tenderness to palpation.21
Of note, pericardial tamponade and cardiac contusion were not studied as they “are not primarily diagnosed by chest X-ray (CXR) or chest CT.”21 The NEXUS chest validation cohort included over 9,000 blunt trauma patients older than age 14 years receiving a variety of imaging modalities, but 43% received only a single CXR. The presence of one or more of the criteria had a sensitivity of 98.8% for detecting any traumatic injury on chest imaging, as well as a sensitivity of 99.7% for any major injury.
CT-All Rule and CT-Major Rule
Subsequently, the investigators of the NEXUS chest rule focused on creating a decision rule to decrease chest CT utilization in blunt trauma, as they found chest CT after a normal CXR to be low-yield.22 After classifying injuries as major or minor based on the necessity of procedural intervention, the authors derived two rules: CT-All, designed to not miss any injuries; and CT-Major, to identify major injuries requiring procedural intervention.
Hemothorax, pneumothorax, pneumomediastinum, or pulmonary contusion that were found on CT but did not require inpatient observation, intervention, or mechanical ventilation were considered clinically insignificant.23
The CT-Major includes six factors:
- Abnormal CXR showing any thoracic injury including clavicle fracture or widened mediastinum;
- Distracting injury;
- Any chest wall tenderness;
- Sternum tenderness;
- Thoracic spine tenderness; or
- Scapular tenderness.
The CT-All includes all of the CT-Major criteria and the additional criteria of rapid deceleration mechanism as defined previously. The validation cohort included over 5,000 patients aged 14 years and older. Having one or more of the major criteria was found to be 99.2% sensitive for major injury, and meeting one or more of the CT-All criteria were found to be 95.4% sensitive for any clinically significant injury. Both CT-Major and CT-All rules identified all 21 aortic/great vessel injuries in their study; the authors assert that vigilance for these types of injuries is often the primary justification for ordering CT imaging.23
Comment: Given the ubiquity and utility of the CXR, it seems unlikely that one would forgo a simple film on the basis of these rules. The presence of an abnormal CXR was by far the best screening criterion for major injury seen on subsequent chest CT, with sensitivity and specificity of 74.7% and 83.9%, respectively.24 Of note, focused assessment with sonography for trauma (FAST) or eFAST (extended FAST) examinations were reported in only 63% or fewer patients in the derivation phase, so the rules did not incorporate point of care ultrasound findings as a criterion despite the growing influence of this modality on trauma decision-making.23
Knee Trauma
Ottawa Knee Rules
The Ottawa Knee Rules state that X-rays are only indicated if patients present with the following:
- Age older than 55 years;
- Isolated tenderness of the patella or fibular head;
- Inability to flex the knee to 90°; or
- Inability to bear weight (limping is allowed) for four steps both immediately following injury and at the ED.
In a prospective validation cohort of 1,096 adult patients, the rule was found to be 100% sensitive for detecting clinically important fractures—defined as any bone fragment at least 5 mm or avulsion if associated with complete disruption as tendons or ligaments—with a potential reduction in radiography use by 28%.25 Though the rule was designed for adult patients, it was validated in 750 children aged 2 to 16 years and found to be 100% sensitive with a 31% potential reduction in radiographs.26
Pittsburgh Knee Rules
The Pittsburgh Knee Rules only apply to patients with blunt trauma or fall to the knee—not twisting injury—and state X-rays are indicated if patients are younger than age 12 years or older than age 50 years, and are unable to bear weight fully on toe pads and heels for four steps (limping is not allowed).
An initial validation of 133 patients demonstrating 100% sensitivity was followed by a larger external validation study.27 That study prospectively applied the Pittsburgh and the Ottawa rules in over 700 patients and found the sensitivity and specificity of the rules to be 99% and 60% for Pittsburgh and 97% and 27% for Ottawa.28
Comment: The ability to apply a rule to “all-comers” is important to EPs. The Ottawa instrument is more broadly applicable and has even been assessed in pediatric populations.
Foot and Ankle Trauma
Ottawa Foot and Ankle Rule
The most well-studied clinical decision rule in this category is the Ottawa Foot and Ankle Rule.29 This rule states that an ankle X-ray is only required if there is pain in the malleolar zone and bony tenderness to palpation at the posterior edge or tip of either the lateral or medial malleolus, or the inability to bear weight both immediately after injury and in the ED. The anatomic landmarks are shown in Figure 3.
- Pain in the midfoot zone and either tenderness at the base of the fifth metatarsal;
- Tenderness over the navicular; or
- Inability to bear weight both immediately after the injury and at the ED.
The prospective validation study included over 1,400 adult patients with blunt trauma or twisting injury within 10 days of presentation. Clinically significant fractures were defined as malleolar or midfoot fractures with bone fragments greater than 3 mm. The rule was found to be 100% sensitive for detecting both ankle and midfoot fractures, and would lead to a reduction of radiographs by 34% for the ankle and 30% for the foot.29 These results have borne out in multiple studies including a recent meta-analysis comparing six different decision instruments where the Ottawa rule was found to be superior.30
Though the initial validation cohort of the Ottawa rule did not include pediatric patients, it has subsequently been applied to this population. The initial validation study in the pediatric population included 670 patients aged 2 to 16 years. In addition to the criteria for clinically significant injuries in the original validation study, Salter Harris type I fractures, though treated with immobilization, were not deemed to be clinically significant injuries in this cohort.
Although the Ottawa rules were determined to be 100% sensitive for detecting significant ankle and midfoot fractures in the pediatric cohort, one of the study sites experienced an increase rather than a decrease in X-rays when this rule was applied.31
Low Risk Ankle Rule
Investigators for the pediatric specific Low Risk Ankle Rule posited that many pediatric patients with mild ankle injury refuse to bear weight on the extremity. Also, the most common fracture among preadolescent patients is a Salter-Harris type I fracture of the distal fibular epiphysis, which the investigators felt was commonly a clinical diagnosis with little to be gained from X-ray.32 These factors would prompt clinicians using the Ottawa rule to order imaging that may not be necessary in pediatric patients.
The Low Risk Ankle Rule states that if a patient has a low-risk examination, which is defined as tenderness and swelling isolated to the distal fibula and/or adjacent lateral ligaments distal to the tibial anterior joint line, then X-rays may not be necessary to exclude a high-risk ankle injury.
High-risk injuries were defined as any injury leading to an unstable ankle, and do not include avulsion, buckle, and nondisplaced Salter-Harris types I and II fractures of the distal fibula. In the validation study of nearly 600 children, the sensitivity for detecting a high risk fracture was 100% and X-rays could have been reduced in 62.8% of children with low-risk examinations compared to only 12% with the Ottawa Ankle Rule.
Comment: Although the Low Risk Ankle Rule was shown to reduce radiographic imaging by almost 63%, it omits many patients who would require splinting or subspecialty follow-up. Even the Salter-Harris type I fractures in the pediatric validation of the Ottawa rule were treated with splinting, though they were not regarded as “significant” injuries. Clinicians applying these rules, especially to a pediatric population, should have a good sense of what type of injuries these rules are designed to detect.
Conclusion
In the midst of a busy shift, clinical decision rules can help save time and expense. However, few of the rules described are meant to be applied to “all-comers,” and practitioners should be careful to not apply these rules to populations that were excluded in the validation cohorts. While clinical decision rules can help identify high-risk features, they are not a substitute for performing a thorough history and physical examination. Further studies should focus on whether these rules truly outperform unaided clinical decision-making.
Part 2 of “Playing by the Rules” will examine the use of clinician decision rules for nontraumatic conditions.
1. Stiell IG, Bennett C. Implementation of clinical decision rules in the emergency department. Acad Emerg Med. 2007;14(11):955-959. doi:10.1197/j.aem.2007.06.039.
2. Green SM. When do clinical decision rules improve patient care? Ann Emerg Med. 2013;62(2):132-135. doi:10.1016/j.annemergmed.2013.02.006.
3. Schriger DL, Elder JW, Cooper RJ. Structured clinical decision aids are seldom compared with subjective physician judgment, and are seldom superior. Ann Emerg Med. 2017;70(3):338-344.e3. doi:10.1016/j.annemergmed.2016.12.004.
4. Haydel MJ, Preston CA, Mills TJ, et al. Indications for computed tomography in patients with minor head injury. N Engl J Med. 2000;343(2):100-105. doi:10.1056/NEJM200007133430204.
5. Stiell IG, Clement CM, Rowe BH, et al. Comparison of the Canadian CT head rule and the New Orleans criteria in patients with minor head injury. JAMA. 2005;294(12):1511-1518. doi:10.1001/jama.294.12.1511
6. Stiell IG, Perry JJ. Traumatic intracranial injury in intoxicate patients with minor head trauma. Acad Emerg Med. 2014;21(2):221. doi:10.1111/acem.12306.
7. Mower WR, Gupta M, Rodriguez R, Hendey GW. Validation of the sensitivity of the National Emergency X-Radiography Utilization Study (NEXUS) head computed tomographic (CT) decision instrument for selective imaging of blunt head injury patients: An observational study. PLoS Med. 2017;14(7):e1002313. doi:10.1371/journal.pmed.1002313.
8. Smits M, Dippel DW, de Haan GG, et al. External validation of the Canadian CT head rule and the New Orleans criteria for CT scanning in patients with minor head injury. JAMA. 2005;294(12):1519-1525. doi:10.1001/jama.294.12.1519.
9. Stein SC, Fabbri A, Servadei F, Glick HA. A critical comparison of clinical decision instruments for computed tomographic scanning in mild closed traumatic brain injury in adolescents and adults. Ann Emerg Med. 2009;53(2):180-188. doi:10.1016/j.annemergmed.2008.01.002.
10. Kuppermann N, Holmes JF, Dayan PS, et al. Identification of children at very low risk of clinically-important brain injuries after head trauma: a prospective cohort study. Lancet. 2009;374(9696):1160-1170. doi:10.1016/S0140-6736(09)61558-0.
11. Babi FE, Borland ML, Phillips N, et al. Accuracy of PECARN, CATCH, and CHALICE head injury decision rules in children: a prospective cohort study. Lancet. 2017;389(10087):2393-2402. doi:10.1016/S0140-6736(17)30555-X.
12. Mower WR. Paediatric head imaging decisions are not child’s play. Lancet. 2017;389(10087):2354-2355. doi:10.1016/S0140-6736(17)30932-7.
13. Hoffman JR, Mower WR, Wolfson AB, Todd KH, Zucker MI. Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. National Emergency X-Radiography Utilization Study Group. N Engl J Med. 2000;343(2):94-99. doi:10.1056/NEJM200007133430203.
14. Viccellio P, Simon H, Pressman BD, Shah NM, Mower WR, Hoffman JR; NEXUS Group. A prospective multicenter study of cervical spine injury in children. Pediatrics. 2001;108(2):20.
15. Tran J, Jeanmonod D, Agresti D, Hamden K, Jeanmonod RK. Prospective validation of modified NEXUS cervical spine injury criteria in low-risk elderly fall patients. West J Emerg Med. 2016;17(3):252-257. doi:10.5811/westjem.2016.3.29702.
16. Paykin G, O’Reilly G, Ackland HM, Mitra B. The NEXUS criteria are insufficient to exclude cervical spine fractures in older blunt trauma patients. Injury. 2017;48(5):1020-1024. doi:10.1016/j.injury.2017.02.013.
17. Evans D, Vera L, Jeanmonod D, Pester J, Jeanmonod R. Application of National Emergency X-Ray Utilizations Study low-risk c-spine criteria in high-risk geriatric falls. Am J Emerg Med. 2015;33(9):1184-1187. doi:10.1016/j.ajem.2015.05.031.
18. Stiell IG, Clement CM, McKnight RD, et al. The Canadian C-spine rule versus the NEXUS low-risk criteria in patients with trauma. N Engl J Med. 2003;349(26):2510-2518.
19. Michaleff ZA, Maher CG, Verhagen AP, Rebbeck T, Lin CW. Accuracy of the Canadian C-spine rule and NEXUS to screen for clinically important cervical spine injury in patients following blunt trauma: A systematic review. CMAJ. 2012;184(16):E867-E876. doi:10.1503/cmaj.120675.
20. Gale SC, Gracias VH, Reilly PM, Schwab CW. The inefficiency of plain radiography to evaluate the cervical spine after blunt trauma. J Trauma. 2005;59(5):1121-1125.
21. Rodriguez RM, Anglin D, Langdorf MI, et al. NEXUS chest: validation of a decision instrument for selective chest imaging in blunt trauma. JAMA Surg. 2013;148(10):940-946. doi:10.1001/jamasurg.2013.2757.
22. Rodriguez RM, Baumann BM, Raja AS, et al. Diagnostic yields, charges, and radiation dose of chest imaging in blunt trauma evaluations. Acad Emerg Med. 2014;21(6):644-650. doi:10.1111/acem.12396.
23. Rodriguez RM, Langdorf MI, Nishijima D, et al. Derivation and validation of two decision instruments for selective chest CT in blunt trauma: a multicenter prospective observational study (NEXUS Chest CT). PLoS Med. 2015;12(10):e1001883. doi:10.1371/journal.pmed.1001883.
24. Rodriguez RM, Hendey GW, Mower WR, et al. Selective chest imaging for blunt trauma patients: The national emergency X-ray utilization studies (NEXUS-chest algorithm). Am J Emerg Med. 2017;35(1):164-170. doi:10.1016/j.ajem.2016.10.066.
25. Stiell IG, Greenberg GH, Wells GA, et al. Prospective validation of a decision rule for the use of radiography in acute knee injuries. JAMA. 1996;275(8):611-615.
26. Bulloch B, Neto G, Plint A, et al. Validation of the Ottawa Knee Rule in children: a multicenter study. Ann Emerg Med. 2003;42(1):48-55. doi:10.1067/mem.2003.196.
27. Seaberg DC, Jackson R. Clinical decision rule for knee radiographs. Am J Emerg Med. 1994;12(5):541-543.
28. Seaberg DC, Yealy DM, Lukens T, Auble T, Mathias S. Multicenter comparison of two clinical decision rules for the use of radiography in acute, high-risk knee injuries. Ann Emerg Med. 1998;32(1):8-13.
29. Stiell IG, Greenberg GH, McKnight RD, et al. Decision rules for the use of radiography in acute ankle injuries. Refinement and prospective validation. JAMA. 1993;269(9):1127-1132.
30. Barelds I, Krijnen WP, van de Leur JP, van der Schans CP, Goddard RJ. Diagnostic accuracy of clinical decision rules to exclude fractures in acute ankle injuries: Systematic review and meta-analysis. J Emerg Med. 2017;53(3):353-368. doi:10.1016/j.jemermed.2017.04.035.
31. Plint AC, Bulloch B, Osmond MH, et al. Validation of the Ottawa Ankle Rules in children with ankle injuries. Acad Emerg Med. 1999;6(10):1005-1009.
32. Boutis K, Komar L, Jaramillo D, et al. Sensitivity of a clinical examination to predict need for radiography in children with ankle injuries: a prospective study. Lancet. 2001;358(9299):2118-2121. doi:10.1016/S0140-6736(01)07218-X.
Emergency physicians (EPs) rely on rapid diagnostic testing to help screen patients for illnesses. While the decision to order a test for a patient should be driven by an objective assessment of pretest probability, other factors such as fear of litigation, clinical inexperience, or desire for increased patient satisfaction can prompt testing even when the likelihood of disease is low. This in turn leads to practice variability, increased cost, and decreased ED throughput, as well as other risks attendant to overtesting and overtreatment. Conversely, practitioners may fail to order necessary tests despite the presence of high-risk clinical features, which in turn may lead to misdiagnoses and delay in initiating life-saving treatments.
Development of Decision Rules
Clinical decision rules seek to decrease resource utilization in instances of low probability of disease and to identify high-risk features that should prompt further investigation. The formation of clinical decision rules entails at least three steps, which Ian Stiell, MD, emergency medicine’s (EM’s) most prolific author of these instruments, describes as follows:
- Creation of the rule or derivation;
- Prospective assessment of the reliability, accuracy, and impact of the rule in a validation study; and
- Gauging the effect of the rule on patient care through an implementation study.1
In addition to these three steps, many clinicians argue that there should also be an important fourth step included in this process: the external validation or assessment of the rule outside of the original study site(s), to assure reliability of the rule across a variety of populations for which its use was intended.2
Critiques and Caveats
A common critique of clinical decision rules is that they may not necessarily outperform subjective physician judgment, and that those who create these rules often do not explicitly compare their instruments against independent unassisted decision-making by clinicians.2,3
Another drawback is that the misapplication of these rules can lead to increased testing, something particularly problematic for one-way rules, which only guide the provider in a single clinical direction. An example of a one-way rule is the Pulmonary Embolism Rule-Out Criteria (PERC), which advises that a low-risk patient who does not have any of the PERC factors will not require any further testing. This, however, does not necessarily mean that further testing is indicated in patients who have one of the PERC factors present.2 Thus, applying PERC and other one-way decision-making rules in a two-way fashion can prompt testing that would not be ordered based on clinician gestalt. Rules that are designed to help determine when testing is necessary and when it is unnecessary are referred to as two-way rules, an example of which is the Ottawa Ankle Rule.
Controversies aside, the incorporation of clinical decision rules in the electronic medical record of many institutions and the proliferation of smartphone applications utilizing these instruments have further cemented their place in EM. This article describes the more commonly used ED clinical decision rules, as well as pearls and pitfalls pertaining to their use. Part 1 that follows covers important validated rules related to trauma patients in the ED. Part 2, which will appear in an upcoming 2018 issue, will cover nontrauma medical-diagnosis decision rules, including pulmonary embolism, and pneumonia.
Head Trauma
The increased utilization of computed tomography (CT) studies to assess for minor blunt head trauma spurred the development of clinical decision rules. In adult patients, the most popular and well-studied instruments are the New Orleans Criteria (NOC), the Canadian CT Head Rule (CCHR), and the National Emergency X-Radiography Utilization Study (NEXUS) CT Head Rule.
New Orleans Criteria
The NOC validation cohort examined over 900 cases at a single trauma center, enrolling all patients 3 years of age and older who had suffered minor head trauma (defined as loss of consciousness (LOC) in a patient with grossly normal neurological examination and a Glasgow Coma Scale [GCS] score of 15), in the preceding 24 hours.4 Patients who experienced no LOC, had focal neurological deficit (except isolated short-term memory deficits), or who did not have any CT study performed, were excluded.
The NOC describes seven factors for consideration:
- Short-term memory deficits;
- Intoxication with drugs or alcohol;
- Physical evidence of trauma above the clavicles;
- Patients older than age 60 years;
- Seizure;
- Headache; and
- Vomiting.
The presence of at least one of these factors was found to be 100% sensitive and 25% specific for the presence of any traumatic intracranial abnormality on CT, though only 6.5% of patients in the derivation and validation cohorts had positive CT scans, and ultimately less than 1% had lesions that required surgery.4
Canadian CT Head Rule
The CCHR validation study assessed over 2,700 patients at nine Canadian EDs, enrolling all patients aged 16 years and older who sustained a blunt head trauma less than 24 hours prior to presentation and who had a GCS score of 13 or higher. The investigators of the CCHR study specified that included patients should have suffered a witnessed LOC, definite amnesia, or a witnessed disorientation.5 Patients who did not have any of these factors were deemed to have minimal head trauma and were excluded from the study. Also excluded from this study were patients who had seizure prior to ED arrival, had a coagulopathy or used oral anticoagulants, had acute focal neurological deficit or obvious depressed skull fracture, had unstable vitals associated with a major trauma, or were pregnant.5 The CCHR was not designed to be applied to these excluded populations. Of note, patients with drug and alcohol intoxication were included in their validation.6
The CCHR describes five high-risk factors that increase the likelihood of requiring acute neurosurgical intervention:
- A GCS score of less than 15 at 2 hours after injury;
- Suspected open or depressed skull fracture;
- Any sign of basal skull fracture (eg, hemotympanum, raccoon eyes, cerebrospinal fluid otorrhea/rhinorrhea, Battle’s sign;
- Two or more episodes of vomiting; or
- Patients aged 65 years or older.
In addition to these five high-risk factors, the CCHR also describes two medium risk criteria for finding any traumatic lesion on CT that would not necessitate acute neurosurgical intervention: amnesia of greater than 30 minutes before impact; and injury resulting from a dangerous mechanism such as a pedestrian struck by motor vehicle, occupant ejected from a motor vehicle, or a fall from a height greater than 3 feet or from over 5 stair-steps.
The presence of any one or more of the five high-risk factors was 100% sensitive for predicting the need for neurosurgical intervention, and taken together, having one or more of the seven factors was 100% sensitive for predicting clinically important brain injury.5
NEXUS CT Head Rule
The NEXUS CT Head Rule validation cohort included over 11,000 pediatric and adult blunt head trauma patients undergoing CT imaging at four hospital EDs, and excluded patients with penetrating injuries or presentation greater than 24 hours after injury.7 Patients were considered to be low risk if none of the following criteria were present:
- Age 65 years or older;
- Evidence of significant skull fracture;
- Scalp hematoma;
- Neurological deficit;
- Altered level of alertness;
- Abnormal behavior;
- Coagulopathy; and
- Recurrent vomiting.
Patients who have one or more of these factors were considered as high risk. The presence of one of these factors was 100% sensitive for detecting patients with lesions requiring neurosurgery and 99% sensitive for detecting any significant intracranial injury, with specificity for either condition at 25%.7
Decision-Rule Sensitivity Comparison
Though the CCHR, NOC, and NEXUS rules differ in their inclusion/exclusion criteria, they have been compared to each other in different populations in the medical literature. A subgroup of the CCHR validation cohort and an accompanying external validation study of over 3,000 patients both found that the CCHR and the NOC were at least as sensitive (100%) in detecting lesions requiring neurosurgical intervention, but the CCHR was more specific and had greater potential to reduce imaging rates.5,8 Another study examined the performance of NEXUS, CCHR, NOC, and other decision instruments in a database of nearly 8,000 adolescent and adult head trauma patients. The authors of this study found the three rules to have similarly high sensitivities (97% to 99%) for detecting clinically important findings, but felt NEXUS to have the best combination of sensitivity and specificity compared to CCHR and NOC.9
Comment: A decision rule to decrease CT utilization in intoxicated head trauma patients is particularly useful, but only the CCHR can help potentially avoid imaging a drug or alcohol-intoxicated patient with abnormal behavior or altered level of alertness. Similarly, distinguishing superficial scalp trauma from more worrisome signs of intracranial injury is important, but the NOC and NEXUS rules recommend imaging for any trauma above the clavicles and
Though the rules have similar sensitivities, the CCHR appears to have the greatest potential for aiding clinical decision-making. Of note, all of the adult decision rules consider patients older than age 60 or 65 years to be a high-risk feature. An instrument with better specificity for geriatric patients would be immensely helpful as our population continues to age.
The Pediatric Population: The PECARN Rule
The CCHR, NEXUS, and NOC have been variously applied to pediatric populations, and the NEXUS and NOC included children (patients aged 3 years and older in the NOC) in their validation cohorts. Perhaps the most widely utilized validated rule for pediatric head trauma in the United States is the Pediatric Emergency Care Applied Research Network (PECARN) rule.
The PECARN rule is an age-specific instrument for assessing pediatric blunt head trauma patients for clinically important traumatic brain injury (TBI)—ie, brain injuries resulting in death, neurosurgery, intubation longer than 24 hours, or hospital admission length of more than two nights.10 The PECARN algorithm as described in its validation study is reproduced in Figure 1.
Patients with trivial injury mechanisms such as ground level falls or running into stationary objects and no signs or symptoms of head trauma other than scalp abrasions or lacerations were excluded from the PECARN analysis, as were patients with pre-existing neurological disorders, including ventricular shunts and brain tumors, patients with penetrating trauma, and those with bleeding disorders. The validation study of over 8,000 children found the presence of any of the criteria to be 100% and 96.8% sensitive in detecting clinically important TBI in children aged less than 2 years and children aged 2 years or older, respectively.
The PECARN rule was recently assessed in a large prospective cohort against two less extensively studied clinical decision rules: the Children’s Head Injury Algorithm for the Prediction of Important Clinical Events (CHALICE) and the Canadian Assessment of Tomography for Childhood Head Injury (CATCH). Though the sample size was over 20,000 patients, only less than 1% required neurosurgery or died. The PECARN rule was determined to have the highest validation sensitivities (100% for <2 years, 99% for ≥2 years) of all of the rules; however, it has been noted by some clinicians that the strict application of the PECARN rule to the study population would have increased the rate of CT scanning 5-fold without providing any clear benefit over clinical judgment in detecting injury.11,12
Comment: The PECARN tool is by far the most robust instrument for pediatric head trauma, but striking a balance between finding otherwise clinically occult injury and reducing unnecessary testing/irradiation remains difficult in this vulnerable population.
Cervical Spine Trauma
Though the incidence of serious cervical spine injury in blunt trauma is low, the potentially devastating consequences of a missed lesion is a potent driver of radiographic testing.13 The Nexus Criteria and Canadian C-Spine Rule were developed to assist the clinician in determining when radiographic imaging is indicated in patients presenting with a blunt-trauma-related injury. The NEXUS criteria were developed to decrease cervical spine X-ray use based on five low-risk factors:
- No posterior midline tenderness;
- No focal neurological deficit;
- Normal level of alertness;
- No evidence of intoxication; and
- No clinically apparent pain that could distract the patient from the pain of a cervical spine injury.13
Patients meeting these low-risk criteria were considered to not have a clinically significant cervical spine injury. Of note, the NEXUS investigators deemed several isolated radiographic lesions to be clinically insignificant in their analysis, including spinous process fractures, simple wedge-compression fractures without loss of 25% or more of vertebral body height, isolated avulsion fractures without ligamentous injury, type 1 odontoid fractures, transverse process fractures, end-plate fractures, trabecular bony injuries, and osteophyte fractures, except corner or teardrop fractures.13
The NEXUS validation study included 34,000 blunt trauma patients, including 3,000 patients aged 1 to 17 years and nearly 3,000 elderly patients, all of whom received at least 3-view X-rays (cross-table lateral, anteroposterior view, and open-mouth odontoid view) unless CT or magnetic resonance imaging was performed because X-rays were deemed impractical or impossible.13-15
The five low-risk features of NEXUS had a sensitivity of 99% in excluding clinically significant cervical spine trauma, and the authors determined that X-rays could have been avoided in more than 12% of the study population.
The NEXUS criteria have been criticized as being less reliable at the extremes of age, and the study authors have specifically urged caution in the use of this rule for infants and toddlers given the small number of these patients in the validation cohort.14
There have been multiple case reports and studies suggesting that the NEXUS rule does not perform well in elderly patients.15,16 Recent research has suggested that substituting “deviation from baseline mental status” for “normal level of alertness” and signs of head and neck trauma for distracting injury may improve specificity for detecting clinically significant injuries in geriatric fall patients, though the sample size does not approach the numbers from the original validation cohort.15,17
Canadian C-Spine Rule
The Canadian C-spine Rule (CCR), described in Figure 2, is more complex than the NEXUS criteria, but there are data to suggest it performs better in head-to-head evaluations.18
Patients were assessed primarily on the basis of the three-view X-rays used in the NEXUS validation, however, only 71.7% of patients received radiographs and the remainder of patients were assessed using a telephone survey the authors had created during the derivation phase.18 Some lesions were deemed to be clinically unimportant, including isolated osteophyte avulsion, isolated fracture of a transverse process not involving a facet joint, isolated fracture of a spinous process not involving the lamina, or simple compression fracture involving less than 25% of the vertebral body height.18
Unfortunately, the CCR validation study was limited by incomplete evaluation in 10% of cases, though multiple subgroup analyses consistently demonstrated the CCR was 95% sensitive or higher for detecting clinically important cervical spine injury, outperforming NEXUS. Subsequently, a large systematic review of 15 studies shows sensitivity of the CCR to be 90% to 100% and NEXUS to be 83% to 100%.19
Comment: The NEXUS criteria were validated in a larger and more heterogeneous cohort than CCR, and also have the advantage of being easier to remember. Using either rule, clinicians must consider that “clinically unimportant” cervical spine fractures are not excluded. Ultimately, the landscape of cervical spine assessment has shifted to performing CT over plain radiographs, and these rules should be re-evaluated in this context.20
Blunt Chest Trauma
NEXUS Chest Guidelines
The NEXUS chest guidelines are more recent developments to help assess the need for chest imaging in the patient presenting with a blunt trauma. The first rule derived and validated by the investigators examined the utility of seven clinical criteria in predicting the need for chest imaging—either X-ray or CT:
- Patients older than age 60 years;
- Rapid deceleration mechanism defined as fall greater than 20 feet or motor vehicle crash greater than 40 mph;
- Chest pain;
- Intoxication;
- Abnormal alertness/mental status;
- Painful distracting injury; and
- Chest wall tenderness to palpation, with the exception of isolated clavicular tenderness to palpation.21
Of note, pericardial tamponade and cardiac contusion were not studied as they “are not primarily diagnosed by chest X-ray (CXR) or chest CT.”21 The NEXUS chest validation cohort included over 9,000 blunt trauma patients older than age 14 years receiving a variety of imaging modalities, but 43% received only a single CXR. The presence of one or more of the criteria had a sensitivity of 98.8% for detecting any traumatic injury on chest imaging, as well as a sensitivity of 99.7% for any major injury.
CT-All Rule and CT-Major Rule
Subsequently, the investigators of the NEXUS chest rule focused on creating a decision rule to decrease chest CT utilization in blunt trauma, as they found chest CT after a normal CXR to be low-yield.22 After classifying injuries as major or minor based on the necessity of procedural intervention, the authors derived two rules: CT-All, designed to not miss any injuries; and CT-Major, to identify major injuries requiring procedural intervention.
Hemothorax, pneumothorax, pneumomediastinum, or pulmonary contusion that were found on CT but did not require inpatient observation, intervention, or mechanical ventilation were considered clinically insignificant.23
The CT-Major includes six factors:
- Abnormal CXR showing any thoracic injury including clavicle fracture or widened mediastinum;
- Distracting injury;
- Any chest wall tenderness;
- Sternum tenderness;
- Thoracic spine tenderness; or
- Scapular tenderness.
The CT-All includes all of the CT-Major criteria and the additional criteria of rapid deceleration mechanism as defined previously. The validation cohort included over 5,000 patients aged 14 years and older. Having one or more of the major criteria was found to be 99.2% sensitive for major injury, and meeting one or more of the CT-All criteria were found to be 95.4% sensitive for any clinically significant injury. Both CT-Major and CT-All rules identified all 21 aortic/great vessel injuries in their study; the authors assert that vigilance for these types of injuries is often the primary justification for ordering CT imaging.23
Comment: Given the ubiquity and utility of the CXR, it seems unlikely that one would forgo a simple film on the basis of these rules. The presence of an abnormal CXR was by far the best screening criterion for major injury seen on subsequent chest CT, with sensitivity and specificity of 74.7% and 83.9%, respectively.24 Of note, focused assessment with sonography for trauma (FAST) or eFAST (extended FAST) examinations were reported in only 63% or fewer patients in the derivation phase, so the rules did not incorporate point of care ultrasound findings as a criterion despite the growing influence of this modality on trauma decision-making.23
Knee Trauma
Ottawa Knee Rules
The Ottawa Knee Rules state that X-rays are only indicated if patients present with the following:
- Age older than 55 years;
- Isolated tenderness of the patella or fibular head;
- Inability to flex the knee to 90°; or
- Inability to bear weight (limping is allowed) for four steps both immediately following injury and at the ED.
In a prospective validation cohort of 1,096 adult patients, the rule was found to be 100% sensitive for detecting clinically important fractures—defined as any bone fragment at least 5 mm or avulsion if associated with complete disruption as tendons or ligaments—with a potential reduction in radiography use by 28%.25 Though the rule was designed for adult patients, it was validated in 750 children aged 2 to 16 years and found to be 100% sensitive with a 31% potential reduction in radiographs.26
Pittsburgh Knee Rules
The Pittsburgh Knee Rules only apply to patients with blunt trauma or fall to the knee—not twisting injury—and state X-rays are indicated if patients are younger than age 12 years or older than age 50 years, and are unable to bear weight fully on toe pads and heels for four steps (limping is not allowed).
An initial validation of 133 patients demonstrating 100% sensitivity was followed by a larger external validation study.27 That study prospectively applied the Pittsburgh and the Ottawa rules in over 700 patients and found the sensitivity and specificity of the rules to be 99% and 60% for Pittsburgh and 97% and 27% for Ottawa.28
Comment: The ability to apply a rule to “all-comers” is important to EPs. The Ottawa instrument is more broadly applicable and has even been assessed in pediatric populations.
Foot and Ankle Trauma
Ottawa Foot and Ankle Rule
The most well-studied clinical decision rule in this category is the Ottawa Foot and Ankle Rule.29 This rule states that an ankle X-ray is only required if there is pain in the malleolar zone and bony tenderness to palpation at the posterior edge or tip of either the lateral or medial malleolus, or the inability to bear weight both immediately after injury and in the ED. The anatomic landmarks are shown in Figure 3.
- Pain in the midfoot zone and either tenderness at the base of the fifth metatarsal;
- Tenderness over the navicular; or
- Inability to bear weight both immediately after the injury and at the ED.
The prospective validation study included over 1,400 adult patients with blunt trauma or twisting injury within 10 days of presentation. Clinically significant fractures were defined as malleolar or midfoot fractures with bone fragments greater than 3 mm. The rule was found to be 100% sensitive for detecting both ankle and midfoot fractures, and would lead to a reduction of radiographs by 34% for the ankle and 30% for the foot.29 These results have borne out in multiple studies including a recent meta-analysis comparing six different decision instruments where the Ottawa rule was found to be superior.30
Though the initial validation cohort of the Ottawa rule did not include pediatric patients, it has subsequently been applied to this population. The initial validation study in the pediatric population included 670 patients aged 2 to 16 years. In addition to the criteria for clinically significant injuries in the original validation study, Salter Harris type I fractures, though treated with immobilization, were not deemed to be clinically significant injuries in this cohort.
Although the Ottawa rules were determined to be 100% sensitive for detecting significant ankle and midfoot fractures in the pediatric cohort, one of the study sites experienced an increase rather than a decrease in X-rays when this rule was applied.31
Low Risk Ankle Rule
Investigators for the pediatric specific Low Risk Ankle Rule posited that many pediatric patients with mild ankle injury refuse to bear weight on the extremity. Also, the most common fracture among preadolescent patients is a Salter-Harris type I fracture of the distal fibular epiphysis, which the investigators felt was commonly a clinical diagnosis with little to be gained from X-ray.32 These factors would prompt clinicians using the Ottawa rule to order imaging that may not be necessary in pediatric patients.
The Low Risk Ankle Rule states that if a patient has a low-risk examination, which is defined as tenderness and swelling isolated to the distal fibula and/or adjacent lateral ligaments distal to the tibial anterior joint line, then X-rays may not be necessary to exclude a high-risk ankle injury.
High-risk injuries were defined as any injury leading to an unstable ankle, and do not include avulsion, buckle, and nondisplaced Salter-Harris types I and II fractures of the distal fibula. In the validation study of nearly 600 children, the sensitivity for detecting a high risk fracture was 100% and X-rays could have been reduced in 62.8% of children with low-risk examinations compared to only 12% with the Ottawa Ankle Rule.
Comment: Although the Low Risk Ankle Rule was shown to reduce radiographic imaging by almost 63%, it omits many patients who would require splinting or subspecialty follow-up. Even the Salter-Harris type I fractures in the pediatric validation of the Ottawa rule were treated with splinting, though they were not regarded as “significant” injuries. Clinicians applying these rules, especially to a pediatric population, should have a good sense of what type of injuries these rules are designed to detect.
Conclusion
In the midst of a busy shift, clinical decision rules can help save time and expense. However, few of the rules described are meant to be applied to “all-comers,” and practitioners should be careful to not apply these rules to populations that were excluded in the validation cohorts. While clinical decision rules can help identify high-risk features, they are not a substitute for performing a thorough history and physical examination. Further studies should focus on whether these rules truly outperform unaided clinical decision-making.
Part 2 of “Playing by the Rules” will examine the use of clinician decision rules for nontraumatic conditions.
Emergency physicians (EPs) rely on rapid diagnostic testing to help screen patients for illnesses. While the decision to order a test for a patient should be driven by an objective assessment of pretest probability, other factors such as fear of litigation, clinical inexperience, or desire for increased patient satisfaction can prompt testing even when the likelihood of disease is low. This in turn leads to practice variability, increased cost, and decreased ED throughput, as well as other risks attendant to overtesting and overtreatment. Conversely, practitioners may fail to order necessary tests despite the presence of high-risk clinical features, which in turn may lead to misdiagnoses and delay in initiating life-saving treatments.
Development of Decision Rules
Clinical decision rules seek to decrease resource utilization in instances of low probability of disease and to identify high-risk features that should prompt further investigation. The formation of clinical decision rules entails at least three steps, which Ian Stiell, MD, emergency medicine’s (EM’s) most prolific author of these instruments, describes as follows:
- Creation of the rule or derivation;
- Prospective assessment of the reliability, accuracy, and impact of the rule in a validation study; and
- Gauging the effect of the rule on patient care through an implementation study.1
In addition to these three steps, many clinicians argue that there should also be an important fourth step included in this process: the external validation or assessment of the rule outside of the original study site(s), to assure reliability of the rule across a variety of populations for which its use was intended.2
Critiques and Caveats
A common critique of clinical decision rules is that they may not necessarily outperform subjective physician judgment, and that those who create these rules often do not explicitly compare their instruments against independent unassisted decision-making by clinicians.2,3
Another drawback is that the misapplication of these rules can lead to increased testing, something particularly problematic for one-way rules, which only guide the provider in a single clinical direction. An example of a one-way rule is the Pulmonary Embolism Rule-Out Criteria (PERC), which advises that a low-risk patient who does not have any of the PERC factors will not require any further testing. This, however, does not necessarily mean that further testing is indicated in patients who have one of the PERC factors present.2 Thus, applying PERC and other one-way decision-making rules in a two-way fashion can prompt testing that would not be ordered based on clinician gestalt. Rules that are designed to help determine when testing is necessary and when it is unnecessary are referred to as two-way rules, an example of which is the Ottawa Ankle Rule.
Controversies aside, the incorporation of clinical decision rules in the electronic medical record of many institutions and the proliferation of smartphone applications utilizing these instruments have further cemented their place in EM. This article describes the more commonly used ED clinical decision rules, as well as pearls and pitfalls pertaining to their use. Part 1 that follows covers important validated rules related to trauma patients in the ED. Part 2, which will appear in an upcoming 2018 issue, will cover nontrauma medical-diagnosis decision rules, including pulmonary embolism, and pneumonia.
Head Trauma
The increased utilization of computed tomography (CT) studies to assess for minor blunt head trauma spurred the development of clinical decision rules. In adult patients, the most popular and well-studied instruments are the New Orleans Criteria (NOC), the Canadian CT Head Rule (CCHR), and the National Emergency X-Radiography Utilization Study (NEXUS) CT Head Rule.
New Orleans Criteria
The NOC validation cohort examined over 900 cases at a single trauma center, enrolling all patients 3 years of age and older who had suffered minor head trauma (defined as loss of consciousness (LOC) in a patient with grossly normal neurological examination and a Glasgow Coma Scale [GCS] score of 15), in the preceding 24 hours.4 Patients who experienced no LOC, had focal neurological deficit (except isolated short-term memory deficits), or who did not have any CT study performed, were excluded.
The NOC describes seven factors for consideration:
- Short-term memory deficits;
- Intoxication with drugs or alcohol;
- Physical evidence of trauma above the clavicles;
- Patients older than age 60 years;
- Seizure;
- Headache; and
- Vomiting.
The presence of at least one of these factors was found to be 100% sensitive and 25% specific for the presence of any traumatic intracranial abnormality on CT, though only 6.5% of patients in the derivation and validation cohorts had positive CT scans, and ultimately less than 1% had lesions that required surgery.4
Canadian CT Head Rule
The CCHR validation study assessed over 2,700 patients at nine Canadian EDs, enrolling all patients aged 16 years and older who sustained a blunt head trauma less than 24 hours prior to presentation and who had a GCS score of 13 or higher. The investigators of the CCHR study specified that included patients should have suffered a witnessed LOC, definite amnesia, or a witnessed disorientation.5 Patients who did not have any of these factors were deemed to have minimal head trauma and were excluded from the study. Also excluded from this study were patients who had seizure prior to ED arrival, had a coagulopathy or used oral anticoagulants, had acute focal neurological deficit or obvious depressed skull fracture, had unstable vitals associated with a major trauma, or were pregnant.5 The CCHR was not designed to be applied to these excluded populations. Of note, patients with drug and alcohol intoxication were included in their validation.6
The CCHR describes five high-risk factors that increase the likelihood of requiring acute neurosurgical intervention:
- A GCS score of less than 15 at 2 hours after injury;
- Suspected open or depressed skull fracture;
- Any sign of basal skull fracture (eg, hemotympanum, raccoon eyes, cerebrospinal fluid otorrhea/rhinorrhea, Battle’s sign;
- Two or more episodes of vomiting; or
- Patients aged 65 years or older.
In addition to these five high-risk factors, the CCHR also describes two medium risk criteria for finding any traumatic lesion on CT that would not necessitate acute neurosurgical intervention: amnesia of greater than 30 minutes before impact; and injury resulting from a dangerous mechanism such as a pedestrian struck by motor vehicle, occupant ejected from a motor vehicle, or a fall from a height greater than 3 feet or from over 5 stair-steps.
The presence of any one or more of the five high-risk factors was 100% sensitive for predicting the need for neurosurgical intervention, and taken together, having one or more of the seven factors was 100% sensitive for predicting clinically important brain injury.5
NEXUS CT Head Rule
The NEXUS CT Head Rule validation cohort included over 11,000 pediatric and adult blunt head trauma patients undergoing CT imaging at four hospital EDs, and excluded patients with penetrating injuries or presentation greater than 24 hours after injury.7 Patients were considered to be low risk if none of the following criteria were present:
- Age 65 years or older;
- Evidence of significant skull fracture;
- Scalp hematoma;
- Neurological deficit;
- Altered level of alertness;
- Abnormal behavior;
- Coagulopathy; and
- Recurrent vomiting.
Patients who have one or more of these factors were considered as high risk. The presence of one of these factors was 100% sensitive for detecting patients with lesions requiring neurosurgery and 99% sensitive for detecting any significant intracranial injury, with specificity for either condition at 25%.7
Decision-Rule Sensitivity Comparison
Though the CCHR, NOC, and NEXUS rules differ in their inclusion/exclusion criteria, they have been compared to each other in different populations in the medical literature. A subgroup of the CCHR validation cohort and an accompanying external validation study of over 3,000 patients both found that the CCHR and the NOC were at least as sensitive (100%) in detecting lesions requiring neurosurgical intervention, but the CCHR was more specific and had greater potential to reduce imaging rates.5,8 Another study examined the performance of NEXUS, CCHR, NOC, and other decision instruments in a database of nearly 8,000 adolescent and adult head trauma patients. The authors of this study found the three rules to have similarly high sensitivities (97% to 99%) for detecting clinically important findings, but felt NEXUS to have the best combination of sensitivity and specificity compared to CCHR and NOC.9
Comment: A decision rule to decrease CT utilization in intoxicated head trauma patients is particularly useful, but only the CCHR can help potentially avoid imaging a drug or alcohol-intoxicated patient with abnormal behavior or altered level of alertness. Similarly, distinguishing superficial scalp trauma from more worrisome signs of intracranial injury is important, but the NOC and NEXUS rules recommend imaging for any trauma above the clavicles and
Though the rules have similar sensitivities, the CCHR appears to have the greatest potential for aiding clinical decision-making. Of note, all of the adult decision rules consider patients older than age 60 or 65 years to be a high-risk feature. An instrument with better specificity for geriatric patients would be immensely helpful as our population continues to age.
The Pediatric Population: The PECARN Rule
The CCHR, NEXUS, and NOC have been variously applied to pediatric populations, and the NEXUS and NOC included children (patients aged 3 years and older in the NOC) in their validation cohorts. Perhaps the most widely utilized validated rule for pediatric head trauma in the United States is the Pediatric Emergency Care Applied Research Network (PECARN) rule.
The PECARN rule is an age-specific instrument for assessing pediatric blunt head trauma patients for clinically important traumatic brain injury (TBI)—ie, brain injuries resulting in death, neurosurgery, intubation longer than 24 hours, or hospital admission length of more than two nights.10 The PECARN algorithm as described in its validation study is reproduced in Figure 1.
Patients with trivial injury mechanisms such as ground level falls or running into stationary objects and no signs or symptoms of head trauma other than scalp abrasions or lacerations were excluded from the PECARN analysis, as were patients with pre-existing neurological disorders, including ventricular shunts and brain tumors, patients with penetrating trauma, and those with bleeding disorders. The validation study of over 8,000 children found the presence of any of the criteria to be 100% and 96.8% sensitive in detecting clinically important TBI in children aged less than 2 years and children aged 2 years or older, respectively.
The PECARN rule was recently assessed in a large prospective cohort against two less extensively studied clinical decision rules: the Children’s Head Injury Algorithm for the Prediction of Important Clinical Events (CHALICE) and the Canadian Assessment of Tomography for Childhood Head Injury (CATCH). Though the sample size was over 20,000 patients, only less than 1% required neurosurgery or died. The PECARN rule was determined to have the highest validation sensitivities (100% for <2 years, 99% for ≥2 years) of all of the rules; however, it has been noted by some clinicians that the strict application of the PECARN rule to the study population would have increased the rate of CT scanning 5-fold without providing any clear benefit over clinical judgment in detecting injury.11,12
Comment: The PECARN tool is by far the most robust instrument for pediatric head trauma, but striking a balance between finding otherwise clinically occult injury and reducing unnecessary testing/irradiation remains difficult in this vulnerable population.
Cervical Spine Trauma
Though the incidence of serious cervical spine injury in blunt trauma is low, the potentially devastating consequences of a missed lesion is a potent driver of radiographic testing.13 The Nexus Criteria and Canadian C-Spine Rule were developed to assist the clinician in determining when radiographic imaging is indicated in patients presenting with a blunt-trauma-related injury. The NEXUS criteria were developed to decrease cervical spine X-ray use based on five low-risk factors:
- No posterior midline tenderness;
- No focal neurological deficit;
- Normal level of alertness;
- No evidence of intoxication; and
- No clinically apparent pain that could distract the patient from the pain of a cervical spine injury.13
Patients meeting these low-risk criteria were considered to not have a clinically significant cervical spine injury. Of note, the NEXUS investigators deemed several isolated radiographic lesions to be clinically insignificant in their analysis, including spinous process fractures, simple wedge-compression fractures without loss of 25% or more of vertebral body height, isolated avulsion fractures without ligamentous injury, type 1 odontoid fractures, transverse process fractures, end-plate fractures, trabecular bony injuries, and osteophyte fractures, except corner or teardrop fractures.13
The NEXUS validation study included 34,000 blunt trauma patients, including 3,000 patients aged 1 to 17 years and nearly 3,000 elderly patients, all of whom received at least 3-view X-rays (cross-table lateral, anteroposterior view, and open-mouth odontoid view) unless CT or magnetic resonance imaging was performed because X-rays were deemed impractical or impossible.13-15
The five low-risk features of NEXUS had a sensitivity of 99% in excluding clinically significant cervical spine trauma, and the authors determined that X-rays could have been avoided in more than 12% of the study population.
The NEXUS criteria have been criticized as being less reliable at the extremes of age, and the study authors have specifically urged caution in the use of this rule for infants and toddlers given the small number of these patients in the validation cohort.14
There have been multiple case reports and studies suggesting that the NEXUS rule does not perform well in elderly patients.15,16 Recent research has suggested that substituting “deviation from baseline mental status” for “normal level of alertness” and signs of head and neck trauma for distracting injury may improve specificity for detecting clinically significant injuries in geriatric fall patients, though the sample size does not approach the numbers from the original validation cohort.15,17
Canadian C-Spine Rule
The Canadian C-spine Rule (CCR), described in Figure 2, is more complex than the NEXUS criteria, but there are data to suggest it performs better in head-to-head evaluations.18
Patients were assessed primarily on the basis of the three-view X-rays used in the NEXUS validation, however, only 71.7% of patients received radiographs and the remainder of patients were assessed using a telephone survey the authors had created during the derivation phase.18 Some lesions were deemed to be clinically unimportant, including isolated osteophyte avulsion, isolated fracture of a transverse process not involving a facet joint, isolated fracture of a spinous process not involving the lamina, or simple compression fracture involving less than 25% of the vertebral body height.18
Unfortunately, the CCR validation study was limited by incomplete evaluation in 10% of cases, though multiple subgroup analyses consistently demonstrated the CCR was 95% sensitive or higher for detecting clinically important cervical spine injury, outperforming NEXUS. Subsequently, a large systematic review of 15 studies shows sensitivity of the CCR to be 90% to 100% and NEXUS to be 83% to 100%.19
Comment: The NEXUS criteria were validated in a larger and more heterogeneous cohort than CCR, and also have the advantage of being easier to remember. Using either rule, clinicians must consider that “clinically unimportant” cervical spine fractures are not excluded. Ultimately, the landscape of cervical spine assessment has shifted to performing CT over plain radiographs, and these rules should be re-evaluated in this context.20
Blunt Chest Trauma
NEXUS Chest Guidelines
The NEXUS chest guidelines are more recent developments to help assess the need for chest imaging in the patient presenting with a blunt trauma. The first rule derived and validated by the investigators examined the utility of seven clinical criteria in predicting the need for chest imaging—either X-ray or CT:
- Patients older than age 60 years;
- Rapid deceleration mechanism defined as fall greater than 20 feet or motor vehicle crash greater than 40 mph;
- Chest pain;
- Intoxication;
- Abnormal alertness/mental status;
- Painful distracting injury; and
- Chest wall tenderness to palpation, with the exception of isolated clavicular tenderness to palpation.21
Of note, pericardial tamponade and cardiac contusion were not studied as they “are not primarily diagnosed by chest X-ray (CXR) or chest CT.”21 The NEXUS chest validation cohort included over 9,000 blunt trauma patients older than age 14 years receiving a variety of imaging modalities, but 43% received only a single CXR. The presence of one or more of the criteria had a sensitivity of 98.8% for detecting any traumatic injury on chest imaging, as well as a sensitivity of 99.7% for any major injury.
CT-All Rule and CT-Major Rule
Subsequently, the investigators of the NEXUS chest rule focused on creating a decision rule to decrease chest CT utilization in blunt trauma, as they found chest CT after a normal CXR to be low-yield.22 After classifying injuries as major or minor based on the necessity of procedural intervention, the authors derived two rules: CT-All, designed to not miss any injuries; and CT-Major, to identify major injuries requiring procedural intervention.
Hemothorax, pneumothorax, pneumomediastinum, or pulmonary contusion that were found on CT but did not require inpatient observation, intervention, or mechanical ventilation were considered clinically insignificant.23
The CT-Major includes six factors:
- Abnormal CXR showing any thoracic injury including clavicle fracture or widened mediastinum;
- Distracting injury;
- Any chest wall tenderness;
- Sternum tenderness;
- Thoracic spine tenderness; or
- Scapular tenderness.
The CT-All includes all of the CT-Major criteria and the additional criteria of rapid deceleration mechanism as defined previously. The validation cohort included over 5,000 patients aged 14 years and older. Having one or more of the major criteria was found to be 99.2% sensitive for major injury, and meeting one or more of the CT-All criteria were found to be 95.4% sensitive for any clinically significant injury. Both CT-Major and CT-All rules identified all 21 aortic/great vessel injuries in their study; the authors assert that vigilance for these types of injuries is often the primary justification for ordering CT imaging.23
Comment: Given the ubiquity and utility of the CXR, it seems unlikely that one would forgo a simple film on the basis of these rules. The presence of an abnormal CXR was by far the best screening criterion for major injury seen on subsequent chest CT, with sensitivity and specificity of 74.7% and 83.9%, respectively.24 Of note, focused assessment with sonography for trauma (FAST) or eFAST (extended FAST) examinations were reported in only 63% or fewer patients in the derivation phase, so the rules did not incorporate point of care ultrasound findings as a criterion despite the growing influence of this modality on trauma decision-making.23
Knee Trauma
Ottawa Knee Rules
The Ottawa Knee Rules state that X-rays are only indicated if patients present with the following:
- Age older than 55 years;
- Isolated tenderness of the patella or fibular head;
- Inability to flex the knee to 90°; or
- Inability to bear weight (limping is allowed) for four steps both immediately following injury and at the ED.
In a prospective validation cohort of 1,096 adult patients, the rule was found to be 100% sensitive for detecting clinically important fractures—defined as any bone fragment at least 5 mm or avulsion if associated with complete disruption as tendons or ligaments—with a potential reduction in radiography use by 28%.25 Though the rule was designed for adult patients, it was validated in 750 children aged 2 to 16 years and found to be 100% sensitive with a 31% potential reduction in radiographs.26
Pittsburgh Knee Rules
The Pittsburgh Knee Rules only apply to patients with blunt trauma or fall to the knee—not twisting injury—and state X-rays are indicated if patients are younger than age 12 years or older than age 50 years, and are unable to bear weight fully on toe pads and heels for four steps (limping is not allowed).
An initial validation of 133 patients demonstrating 100% sensitivity was followed by a larger external validation study.27 That study prospectively applied the Pittsburgh and the Ottawa rules in over 700 patients and found the sensitivity and specificity of the rules to be 99% and 60% for Pittsburgh and 97% and 27% for Ottawa.28
Comment: The ability to apply a rule to “all-comers” is important to EPs. The Ottawa instrument is more broadly applicable and has even been assessed in pediatric populations.
Foot and Ankle Trauma
Ottawa Foot and Ankle Rule
The most well-studied clinical decision rule in this category is the Ottawa Foot and Ankle Rule.29 This rule states that an ankle X-ray is only required if there is pain in the malleolar zone and bony tenderness to palpation at the posterior edge or tip of either the lateral or medial malleolus, or the inability to bear weight both immediately after injury and in the ED. The anatomic landmarks are shown in Figure 3.
- Pain in the midfoot zone and either tenderness at the base of the fifth metatarsal;
- Tenderness over the navicular; or
- Inability to bear weight both immediately after the injury and at the ED.
The prospective validation study included over 1,400 adult patients with blunt trauma or twisting injury within 10 days of presentation. Clinically significant fractures were defined as malleolar or midfoot fractures with bone fragments greater than 3 mm. The rule was found to be 100% sensitive for detecting both ankle and midfoot fractures, and would lead to a reduction of radiographs by 34% for the ankle and 30% for the foot.29 These results have borne out in multiple studies including a recent meta-analysis comparing six different decision instruments where the Ottawa rule was found to be superior.30
Though the initial validation cohort of the Ottawa rule did not include pediatric patients, it has subsequently been applied to this population. The initial validation study in the pediatric population included 670 patients aged 2 to 16 years. In addition to the criteria for clinically significant injuries in the original validation study, Salter Harris type I fractures, though treated with immobilization, were not deemed to be clinically significant injuries in this cohort.
Although the Ottawa rules were determined to be 100% sensitive for detecting significant ankle and midfoot fractures in the pediatric cohort, one of the study sites experienced an increase rather than a decrease in X-rays when this rule was applied.31
Low Risk Ankle Rule
Investigators for the pediatric specific Low Risk Ankle Rule posited that many pediatric patients with mild ankle injury refuse to bear weight on the extremity. Also, the most common fracture among preadolescent patients is a Salter-Harris type I fracture of the distal fibular epiphysis, which the investigators felt was commonly a clinical diagnosis with little to be gained from X-ray.32 These factors would prompt clinicians using the Ottawa rule to order imaging that may not be necessary in pediatric patients.
The Low Risk Ankle Rule states that if a patient has a low-risk examination, which is defined as tenderness and swelling isolated to the distal fibula and/or adjacent lateral ligaments distal to the tibial anterior joint line, then X-rays may not be necessary to exclude a high-risk ankle injury.
High-risk injuries were defined as any injury leading to an unstable ankle, and do not include avulsion, buckle, and nondisplaced Salter-Harris types I and II fractures of the distal fibula. In the validation study of nearly 600 children, the sensitivity for detecting a high risk fracture was 100% and X-rays could have been reduced in 62.8% of children with low-risk examinations compared to only 12% with the Ottawa Ankle Rule.
Comment: Although the Low Risk Ankle Rule was shown to reduce radiographic imaging by almost 63%, it omits many patients who would require splinting or subspecialty follow-up. Even the Salter-Harris type I fractures in the pediatric validation of the Ottawa rule were treated with splinting, though they were not regarded as “significant” injuries. Clinicians applying these rules, especially to a pediatric population, should have a good sense of what type of injuries these rules are designed to detect.
Conclusion
In the midst of a busy shift, clinical decision rules can help save time and expense. However, few of the rules described are meant to be applied to “all-comers,” and practitioners should be careful to not apply these rules to populations that were excluded in the validation cohorts. While clinical decision rules can help identify high-risk features, they are not a substitute for performing a thorough history and physical examination. Further studies should focus on whether these rules truly outperform unaided clinical decision-making.
Part 2 of “Playing by the Rules” will examine the use of clinician decision rules for nontraumatic conditions.
1. Stiell IG, Bennett C. Implementation of clinical decision rules in the emergency department. Acad Emerg Med. 2007;14(11):955-959. doi:10.1197/j.aem.2007.06.039.
2. Green SM. When do clinical decision rules improve patient care? Ann Emerg Med. 2013;62(2):132-135. doi:10.1016/j.annemergmed.2013.02.006.
3. Schriger DL, Elder JW, Cooper RJ. Structured clinical decision aids are seldom compared with subjective physician judgment, and are seldom superior. Ann Emerg Med. 2017;70(3):338-344.e3. doi:10.1016/j.annemergmed.2016.12.004.
4. Haydel MJ, Preston CA, Mills TJ, et al. Indications for computed tomography in patients with minor head injury. N Engl J Med. 2000;343(2):100-105. doi:10.1056/NEJM200007133430204.
5. Stiell IG, Clement CM, Rowe BH, et al. Comparison of the Canadian CT head rule and the New Orleans criteria in patients with minor head injury. JAMA. 2005;294(12):1511-1518. doi:10.1001/jama.294.12.1511
6. Stiell IG, Perry JJ. Traumatic intracranial injury in intoxicate patients with minor head trauma. Acad Emerg Med. 2014;21(2):221. doi:10.1111/acem.12306.
7. Mower WR, Gupta M, Rodriguez R, Hendey GW. Validation of the sensitivity of the National Emergency X-Radiography Utilization Study (NEXUS) head computed tomographic (CT) decision instrument for selective imaging of blunt head injury patients: An observational study. PLoS Med. 2017;14(7):e1002313. doi:10.1371/journal.pmed.1002313.
8. Smits M, Dippel DW, de Haan GG, et al. External validation of the Canadian CT head rule and the New Orleans criteria for CT scanning in patients with minor head injury. JAMA. 2005;294(12):1519-1525. doi:10.1001/jama.294.12.1519.
9. Stein SC, Fabbri A, Servadei F, Glick HA. A critical comparison of clinical decision instruments for computed tomographic scanning in mild closed traumatic brain injury in adolescents and adults. Ann Emerg Med. 2009;53(2):180-188. doi:10.1016/j.annemergmed.2008.01.002.
10. Kuppermann N, Holmes JF, Dayan PS, et al. Identification of children at very low risk of clinically-important brain injuries after head trauma: a prospective cohort study. Lancet. 2009;374(9696):1160-1170. doi:10.1016/S0140-6736(09)61558-0.
11. Babi FE, Borland ML, Phillips N, et al. Accuracy of PECARN, CATCH, and CHALICE head injury decision rules in children: a prospective cohort study. Lancet. 2017;389(10087):2393-2402. doi:10.1016/S0140-6736(17)30555-X.
12. Mower WR. Paediatric head imaging decisions are not child’s play. Lancet. 2017;389(10087):2354-2355. doi:10.1016/S0140-6736(17)30932-7.
13. Hoffman JR, Mower WR, Wolfson AB, Todd KH, Zucker MI. Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. National Emergency X-Radiography Utilization Study Group. N Engl J Med. 2000;343(2):94-99. doi:10.1056/NEJM200007133430203.
14. Viccellio P, Simon H, Pressman BD, Shah NM, Mower WR, Hoffman JR; NEXUS Group. A prospective multicenter study of cervical spine injury in children. Pediatrics. 2001;108(2):20.
15. Tran J, Jeanmonod D, Agresti D, Hamden K, Jeanmonod RK. Prospective validation of modified NEXUS cervical spine injury criteria in low-risk elderly fall patients. West J Emerg Med. 2016;17(3):252-257. doi:10.5811/westjem.2016.3.29702.
16. Paykin G, O’Reilly G, Ackland HM, Mitra B. The NEXUS criteria are insufficient to exclude cervical spine fractures in older blunt trauma patients. Injury. 2017;48(5):1020-1024. doi:10.1016/j.injury.2017.02.013.
17. Evans D, Vera L, Jeanmonod D, Pester J, Jeanmonod R. Application of National Emergency X-Ray Utilizations Study low-risk c-spine criteria in high-risk geriatric falls. Am J Emerg Med. 2015;33(9):1184-1187. doi:10.1016/j.ajem.2015.05.031.
18. Stiell IG, Clement CM, McKnight RD, et al. The Canadian C-spine rule versus the NEXUS low-risk criteria in patients with trauma. N Engl J Med. 2003;349(26):2510-2518.
19. Michaleff ZA, Maher CG, Verhagen AP, Rebbeck T, Lin CW. Accuracy of the Canadian C-spine rule and NEXUS to screen for clinically important cervical spine injury in patients following blunt trauma: A systematic review. CMAJ. 2012;184(16):E867-E876. doi:10.1503/cmaj.120675.
20. Gale SC, Gracias VH, Reilly PM, Schwab CW. The inefficiency of plain radiography to evaluate the cervical spine after blunt trauma. J Trauma. 2005;59(5):1121-1125.
21. Rodriguez RM, Anglin D, Langdorf MI, et al. NEXUS chest: validation of a decision instrument for selective chest imaging in blunt trauma. JAMA Surg. 2013;148(10):940-946. doi:10.1001/jamasurg.2013.2757.
22. Rodriguez RM, Baumann BM, Raja AS, et al. Diagnostic yields, charges, and radiation dose of chest imaging in blunt trauma evaluations. Acad Emerg Med. 2014;21(6):644-650. doi:10.1111/acem.12396.
23. Rodriguez RM, Langdorf MI, Nishijima D, et al. Derivation and validation of two decision instruments for selective chest CT in blunt trauma: a multicenter prospective observational study (NEXUS Chest CT). PLoS Med. 2015;12(10):e1001883. doi:10.1371/journal.pmed.1001883.
24. Rodriguez RM, Hendey GW, Mower WR, et al. Selective chest imaging for blunt trauma patients: The national emergency X-ray utilization studies (NEXUS-chest algorithm). Am J Emerg Med. 2017;35(1):164-170. doi:10.1016/j.ajem.2016.10.066.
25. Stiell IG, Greenberg GH, Wells GA, et al. Prospective validation of a decision rule for the use of radiography in acute knee injuries. JAMA. 1996;275(8):611-615.
26. Bulloch B, Neto G, Plint A, et al. Validation of the Ottawa Knee Rule in children: a multicenter study. Ann Emerg Med. 2003;42(1):48-55. doi:10.1067/mem.2003.196.
27. Seaberg DC, Jackson R. Clinical decision rule for knee radiographs. Am J Emerg Med. 1994;12(5):541-543.
28. Seaberg DC, Yealy DM, Lukens T, Auble T, Mathias S. Multicenter comparison of two clinical decision rules for the use of radiography in acute, high-risk knee injuries. Ann Emerg Med. 1998;32(1):8-13.
29. Stiell IG, Greenberg GH, McKnight RD, et al. Decision rules for the use of radiography in acute ankle injuries. Refinement and prospective validation. JAMA. 1993;269(9):1127-1132.
30. Barelds I, Krijnen WP, van de Leur JP, van der Schans CP, Goddard RJ. Diagnostic accuracy of clinical decision rules to exclude fractures in acute ankle injuries: Systematic review and meta-analysis. J Emerg Med. 2017;53(3):353-368. doi:10.1016/j.jemermed.2017.04.035.
31. Plint AC, Bulloch B, Osmond MH, et al. Validation of the Ottawa Ankle Rules in children with ankle injuries. Acad Emerg Med. 1999;6(10):1005-1009.
32. Boutis K, Komar L, Jaramillo D, et al. Sensitivity of a clinical examination to predict need for radiography in children with ankle injuries: a prospective study. Lancet. 2001;358(9299):2118-2121. doi:10.1016/S0140-6736(01)07218-X.
1. Stiell IG, Bennett C. Implementation of clinical decision rules in the emergency department. Acad Emerg Med. 2007;14(11):955-959. doi:10.1197/j.aem.2007.06.039.
2. Green SM. When do clinical decision rules improve patient care? Ann Emerg Med. 2013;62(2):132-135. doi:10.1016/j.annemergmed.2013.02.006.
3. Schriger DL, Elder JW, Cooper RJ. Structured clinical decision aids are seldom compared with subjective physician judgment, and are seldom superior. Ann Emerg Med. 2017;70(3):338-344.e3. doi:10.1016/j.annemergmed.2016.12.004.
4. Haydel MJ, Preston CA, Mills TJ, et al. Indications for computed tomography in patients with minor head injury. N Engl J Med. 2000;343(2):100-105. doi:10.1056/NEJM200007133430204.
5. Stiell IG, Clement CM, Rowe BH, et al. Comparison of the Canadian CT head rule and the New Orleans criteria in patients with minor head injury. JAMA. 2005;294(12):1511-1518. doi:10.1001/jama.294.12.1511
6. Stiell IG, Perry JJ. Traumatic intracranial injury in intoxicate patients with minor head trauma. Acad Emerg Med. 2014;21(2):221. doi:10.1111/acem.12306.
7. Mower WR, Gupta M, Rodriguez R, Hendey GW. Validation of the sensitivity of the National Emergency X-Radiography Utilization Study (NEXUS) head computed tomographic (CT) decision instrument for selective imaging of blunt head injury patients: An observational study. PLoS Med. 2017;14(7):e1002313. doi:10.1371/journal.pmed.1002313.
8. Smits M, Dippel DW, de Haan GG, et al. External validation of the Canadian CT head rule and the New Orleans criteria for CT scanning in patients with minor head injury. JAMA. 2005;294(12):1519-1525. doi:10.1001/jama.294.12.1519.
9. Stein SC, Fabbri A, Servadei F, Glick HA. A critical comparison of clinical decision instruments for computed tomographic scanning in mild closed traumatic brain injury in adolescents and adults. Ann Emerg Med. 2009;53(2):180-188. doi:10.1016/j.annemergmed.2008.01.002.
10. Kuppermann N, Holmes JF, Dayan PS, et al. Identification of children at very low risk of clinically-important brain injuries after head trauma: a prospective cohort study. Lancet. 2009;374(9696):1160-1170. doi:10.1016/S0140-6736(09)61558-0.
11. Babi FE, Borland ML, Phillips N, et al. Accuracy of PECARN, CATCH, and CHALICE head injury decision rules in children: a prospective cohort study. Lancet. 2017;389(10087):2393-2402. doi:10.1016/S0140-6736(17)30555-X.
12. Mower WR. Paediatric head imaging decisions are not child’s play. Lancet. 2017;389(10087):2354-2355. doi:10.1016/S0140-6736(17)30932-7.
13. Hoffman JR, Mower WR, Wolfson AB, Todd KH, Zucker MI. Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. National Emergency X-Radiography Utilization Study Group. N Engl J Med. 2000;343(2):94-99. doi:10.1056/NEJM200007133430203.
14. Viccellio P, Simon H, Pressman BD, Shah NM, Mower WR, Hoffman JR; NEXUS Group. A prospective multicenter study of cervical spine injury in children. Pediatrics. 2001;108(2):20.
15. Tran J, Jeanmonod D, Agresti D, Hamden K, Jeanmonod RK. Prospective validation of modified NEXUS cervical spine injury criteria in low-risk elderly fall patients. West J Emerg Med. 2016;17(3):252-257. doi:10.5811/westjem.2016.3.29702.
16. Paykin G, O’Reilly G, Ackland HM, Mitra B. The NEXUS criteria are insufficient to exclude cervical spine fractures in older blunt trauma patients. Injury. 2017;48(5):1020-1024. doi:10.1016/j.injury.2017.02.013.
17. Evans D, Vera L, Jeanmonod D, Pester J, Jeanmonod R. Application of National Emergency X-Ray Utilizations Study low-risk c-spine criteria in high-risk geriatric falls. Am J Emerg Med. 2015;33(9):1184-1187. doi:10.1016/j.ajem.2015.05.031.
18. Stiell IG, Clement CM, McKnight RD, et al. The Canadian C-spine rule versus the NEXUS low-risk criteria in patients with trauma. N Engl J Med. 2003;349(26):2510-2518.
19. Michaleff ZA, Maher CG, Verhagen AP, Rebbeck T, Lin CW. Accuracy of the Canadian C-spine rule and NEXUS to screen for clinically important cervical spine injury in patients following blunt trauma: A systematic review. CMAJ. 2012;184(16):E867-E876. doi:10.1503/cmaj.120675.
20. Gale SC, Gracias VH, Reilly PM, Schwab CW. The inefficiency of plain radiography to evaluate the cervical spine after blunt trauma. J Trauma. 2005;59(5):1121-1125.
21. Rodriguez RM, Anglin D, Langdorf MI, et al. NEXUS chest: validation of a decision instrument for selective chest imaging in blunt trauma. JAMA Surg. 2013;148(10):940-946. doi:10.1001/jamasurg.2013.2757.
22. Rodriguez RM, Baumann BM, Raja AS, et al. Diagnostic yields, charges, and radiation dose of chest imaging in blunt trauma evaluations. Acad Emerg Med. 2014;21(6):644-650. doi:10.1111/acem.12396.
23. Rodriguez RM, Langdorf MI, Nishijima D, et al. Derivation and validation of two decision instruments for selective chest CT in blunt trauma: a multicenter prospective observational study (NEXUS Chest CT). PLoS Med. 2015;12(10):e1001883. doi:10.1371/journal.pmed.1001883.
24. Rodriguez RM, Hendey GW, Mower WR, et al. Selective chest imaging for blunt trauma patients: The national emergency X-ray utilization studies (NEXUS-chest algorithm). Am J Emerg Med. 2017;35(1):164-170. doi:10.1016/j.ajem.2016.10.066.
25. Stiell IG, Greenberg GH, Wells GA, et al. Prospective validation of a decision rule for the use of radiography in acute knee injuries. JAMA. 1996;275(8):611-615.
26. Bulloch B, Neto G, Plint A, et al. Validation of the Ottawa Knee Rule in children: a multicenter study. Ann Emerg Med. 2003;42(1):48-55. doi:10.1067/mem.2003.196.
27. Seaberg DC, Jackson R. Clinical decision rule for knee radiographs. Am J Emerg Med. 1994;12(5):541-543.
28. Seaberg DC, Yealy DM, Lukens T, Auble T, Mathias S. Multicenter comparison of two clinical decision rules for the use of radiography in acute, high-risk knee injuries. Ann Emerg Med. 1998;32(1):8-13.
29. Stiell IG, Greenberg GH, McKnight RD, et al. Decision rules for the use of radiography in acute ankle injuries. Refinement and prospective validation. JAMA. 1993;269(9):1127-1132.
30. Barelds I, Krijnen WP, van de Leur JP, van der Schans CP, Goddard RJ. Diagnostic accuracy of clinical decision rules to exclude fractures in acute ankle injuries: Systematic review and meta-analysis. J Emerg Med. 2017;53(3):353-368. doi:10.1016/j.jemermed.2017.04.035.
31. Plint AC, Bulloch B, Osmond MH, et al. Validation of the Ottawa Ankle Rules in children with ankle injuries. Acad Emerg Med. 1999;6(10):1005-1009.
32. Boutis K, Komar L, Jaramillo D, et al. Sensitivity of a clinical examination to predict need for radiography in children with ankle injuries: a prospective study. Lancet. 2001;358(9299):2118-2121. doi:10.1016/S0140-6736(01)07218-X.