User login
How can we minimize recurrent ankle sprains?
USING EXTERNAL ANKLE SUPPORTS during physical activity significantly reduces the likelihood of primary and secondary sprains (strength of recommendation [SOR]: A, systematic review).
Proprioception rehabilitation substantially decreases further injury after an ankle sprain (SOR: A, 3 randomized control trials [RCTs] and 1 prospective cohort study).
Evidence summary
A Cochrane review of 14 randomized and quasi-randomized trials concluded that patients who used external ankle supports, such as semi-rigid orthotics or air cast braces, suffered significantly fewer ankle sprains than controls (relative risk [RR]=0.53; 95% confidence interval [CI], 0.40-0.69; number needed to treat [NNT]=22).1 Participants in the trials ranged in age from adolescence to middle age and were either at risk of injury or had suffered a previous ligament injury.
The benefits of ankle supports were most apparent in patients with previous injuries but still evident in patients who hadn’t been injured. External ankle support is recommended for sports with a high risk of ankle injury, such as soccer and basketball, but the decision to use it should be based on perceived risk of injury as opposed to perceived loss of performance.1
Research is insufficient to support wearing high-top shoes to prevent primary and secondary ankle sprains.
Also helpful: Balance and proprioceptive training
A systematic review of 2 RCTs with 703 and 1057 patients concluded that completing a minimum of 6 weeks of balance and coordination training after an acute injury substantially reduced the risk of recurrent ankle sprains for as long as a year (NNT=22; absolute risk reduction=4.5%).2
Proprioceptive training appears to effectively prevent primary and secondary ankle injuries but is more beneficial for patients with a previous ankle injury. A recent RCT that enrolled 522 active sports participants with recent ankle injuries found that those who completed an 8-week, self-guided, proprioceptive training program suffered significantly fewer recurrent sprains at 1 year than the control group (22% vs 33%; relative risk reduction=35%; NNT=9).3
Recommendations
The American Orthopaedic Society for Sports Medicine continues to endorse rest, ice, compression, and elevation for optimal initial care of ankle sprains.4 The American College of Sports Medicine suggests that rehabilitation after an ankle injury should include guided stretching and strengthening of the ankle joint as well as balance training to prevent future injuries.5 Both groups also recommend external ankle supports instead of taping to prevent ankle reinjury.4,5
1. Handoll HH, Rowe BH, Quinn KM, et al. Interventions for preventing ankle ligament injuries. Cochrane Database Syst Rev. 2009;(3):CD000018.-
2. Patrick OM, Hertel J. Systematic review of postural control and lateral ankle instability, part II: is balance training clinically effective? J Athletic Trng. 2008;43:305-315.
3. Hupperets MW, Verhagen EA, VanMechelen W. Effect of unsupervised home based proprioceptive training on recurrences of ankle sprain: randomised control trial. Available at: www.bmj.com/cgi/content/full/339/jul09_1/b2684?maxtoshow=&hits=10&RESULTFORMAT=&fulltext=hupperets&searchid=1&FIRSTINDEX=0&sortspec=date&resourcetype=HWCIT. Accessed July 29, 2010.
4. American Orthopaedic Society for Sports Medicine. Ankle sprains: how to speed your recovery. Available at: http://www.evanekman.com/pdfs/3ST%20Ankle%20Sprains%2008.pdf. Accessed October 10, 2011.
5. American College of Sports Medicine. Current comment: ankle sprains and the athlete. Available at: http://www.acsm.org/docs/current-comments/anklesprainstemp.pdf. Accessed on October 10, 2011.
USING EXTERNAL ANKLE SUPPORTS during physical activity significantly reduces the likelihood of primary and secondary sprains (strength of recommendation [SOR]: A, systematic review).
Proprioception rehabilitation substantially decreases further injury after an ankle sprain (SOR: A, 3 randomized control trials [RCTs] and 1 prospective cohort study).
Evidence summary
A Cochrane review of 14 randomized and quasi-randomized trials concluded that patients who used external ankle supports, such as semi-rigid orthotics or air cast braces, suffered significantly fewer ankle sprains than controls (relative risk [RR]=0.53; 95% confidence interval [CI], 0.40-0.69; number needed to treat [NNT]=22).1 Participants in the trials ranged in age from adolescence to middle age and were either at risk of injury or had suffered a previous ligament injury.
The benefits of ankle supports were most apparent in patients with previous injuries but still evident in patients who hadn’t been injured. External ankle support is recommended for sports with a high risk of ankle injury, such as soccer and basketball, but the decision to use it should be based on perceived risk of injury as opposed to perceived loss of performance.1
Research is insufficient to support wearing high-top shoes to prevent primary and secondary ankle sprains.
Also helpful: Balance and proprioceptive training
A systematic review of 2 RCTs with 703 and 1057 patients concluded that completing a minimum of 6 weeks of balance and coordination training after an acute injury substantially reduced the risk of recurrent ankle sprains for as long as a year (NNT=22; absolute risk reduction=4.5%).2
Proprioceptive training appears to effectively prevent primary and secondary ankle injuries but is more beneficial for patients with a previous ankle injury. A recent RCT that enrolled 522 active sports participants with recent ankle injuries found that those who completed an 8-week, self-guided, proprioceptive training program suffered significantly fewer recurrent sprains at 1 year than the control group (22% vs 33%; relative risk reduction=35%; NNT=9).3
Recommendations
The American Orthopaedic Society for Sports Medicine continues to endorse rest, ice, compression, and elevation for optimal initial care of ankle sprains.4 The American College of Sports Medicine suggests that rehabilitation after an ankle injury should include guided stretching and strengthening of the ankle joint as well as balance training to prevent future injuries.5 Both groups also recommend external ankle supports instead of taping to prevent ankle reinjury.4,5
USING EXTERNAL ANKLE SUPPORTS during physical activity significantly reduces the likelihood of primary and secondary sprains (strength of recommendation [SOR]: A, systematic review).
Proprioception rehabilitation substantially decreases further injury after an ankle sprain (SOR: A, 3 randomized control trials [RCTs] and 1 prospective cohort study).
Evidence summary
A Cochrane review of 14 randomized and quasi-randomized trials concluded that patients who used external ankle supports, such as semi-rigid orthotics or air cast braces, suffered significantly fewer ankle sprains than controls (relative risk [RR]=0.53; 95% confidence interval [CI], 0.40-0.69; number needed to treat [NNT]=22).1 Participants in the trials ranged in age from adolescence to middle age and were either at risk of injury or had suffered a previous ligament injury.
The benefits of ankle supports were most apparent in patients with previous injuries but still evident in patients who hadn’t been injured. External ankle support is recommended for sports with a high risk of ankle injury, such as soccer and basketball, but the decision to use it should be based on perceived risk of injury as opposed to perceived loss of performance.1
Research is insufficient to support wearing high-top shoes to prevent primary and secondary ankle sprains.
Also helpful: Balance and proprioceptive training
A systematic review of 2 RCTs with 703 and 1057 patients concluded that completing a minimum of 6 weeks of balance and coordination training after an acute injury substantially reduced the risk of recurrent ankle sprains for as long as a year (NNT=22; absolute risk reduction=4.5%).2
Proprioceptive training appears to effectively prevent primary and secondary ankle injuries but is more beneficial for patients with a previous ankle injury. A recent RCT that enrolled 522 active sports participants with recent ankle injuries found that those who completed an 8-week, self-guided, proprioceptive training program suffered significantly fewer recurrent sprains at 1 year than the control group (22% vs 33%; relative risk reduction=35%; NNT=9).3
Recommendations
The American Orthopaedic Society for Sports Medicine continues to endorse rest, ice, compression, and elevation for optimal initial care of ankle sprains.4 The American College of Sports Medicine suggests that rehabilitation after an ankle injury should include guided stretching and strengthening of the ankle joint as well as balance training to prevent future injuries.5 Both groups also recommend external ankle supports instead of taping to prevent ankle reinjury.4,5
1. Handoll HH, Rowe BH, Quinn KM, et al. Interventions for preventing ankle ligament injuries. Cochrane Database Syst Rev. 2009;(3):CD000018.-
2. Patrick OM, Hertel J. Systematic review of postural control and lateral ankle instability, part II: is balance training clinically effective? J Athletic Trng. 2008;43:305-315.
3. Hupperets MW, Verhagen EA, VanMechelen W. Effect of unsupervised home based proprioceptive training on recurrences of ankle sprain: randomised control trial. Available at: www.bmj.com/cgi/content/full/339/jul09_1/b2684?maxtoshow=&hits=10&RESULTFORMAT=&fulltext=hupperets&searchid=1&FIRSTINDEX=0&sortspec=date&resourcetype=HWCIT. Accessed July 29, 2010.
4. American Orthopaedic Society for Sports Medicine. Ankle sprains: how to speed your recovery. Available at: http://www.evanekman.com/pdfs/3ST%20Ankle%20Sprains%2008.pdf. Accessed October 10, 2011.
5. American College of Sports Medicine. Current comment: ankle sprains and the athlete. Available at: http://www.acsm.org/docs/current-comments/anklesprainstemp.pdf. Accessed on October 10, 2011.
1. Handoll HH, Rowe BH, Quinn KM, et al. Interventions for preventing ankle ligament injuries. Cochrane Database Syst Rev. 2009;(3):CD000018.-
2. Patrick OM, Hertel J. Systematic review of postural control and lateral ankle instability, part II: is balance training clinically effective? J Athletic Trng. 2008;43:305-315.
3. Hupperets MW, Verhagen EA, VanMechelen W. Effect of unsupervised home based proprioceptive training on recurrences of ankle sprain: randomised control trial. Available at: www.bmj.com/cgi/content/full/339/jul09_1/b2684?maxtoshow=&hits=10&RESULTFORMAT=&fulltext=hupperets&searchid=1&FIRSTINDEX=0&sortspec=date&resourcetype=HWCIT. Accessed July 29, 2010.
4. American Orthopaedic Society for Sports Medicine. Ankle sprains: how to speed your recovery. Available at: http://www.evanekman.com/pdfs/3ST%20Ankle%20Sprains%2008.pdf. Accessed October 10, 2011.
5. American College of Sports Medicine. Current comment: ankle sprains and the athlete. Available at: http://www.acsm.org/docs/current-comments/anklesprainstemp.pdf. Accessed on October 10, 2011.
Evidence-based answers from the Family Physicians Inquiries Network
What's the best way to monitor low-risk patients with a history of differentiated thyroid cancer?
A recombinant human thyrotropin (rhTSH)-stimulated serum thyroglobulin (Tg) level alone is sufficient to monitor for recurrent disease in low-risk patients with a history of differentiated thyroid cancer (DTC) (strength of recommendation [SOR] A, meta-analysis). Low-risk patients are defined as patients who have undergone total thyroidectomy and radioactive iodine (I131) remnant ablation therapy and show no clinical evidence of recurrent disease.
Evidence summary
An estimated 37,340 new cases of thyroid cancer are diagnosed annually in the United States, typically in people between 20 and 55 years of age. The most common type of thyroid cancer is DTC, which includes papillary and follicular carcinoma. Papillary carcinoma accounts for 80% of all thyroid cancers, and follicular carcinoma accounts for 10%.
The 5-year survival rate for all cases of DTC is 97%. Although the disease has a favorable prognosis, an estimated 1630 patients were expected to die of it in 2009 because of its prevalence.1
The goal: Find recurrent disease early
The purpose of surveillance protocols in thyroid cancer is early detection of recurrent disease. Expert debate about DTC surveillance centers on the disease’s low incidence and prolonged clinical course, as well as a lack of prospective randomized clinical trials. Current guidelines were developed from large retrospective cohort studies of patients observed over several decades.
rhTSH-stimulated Tg is the new surveillance standard
All major professional organizations support the consensus that an rhTSH-stimulated serum Tg is adequate to follow-up low-risk patients. This test replaces the previous accepted standard of thyroid hormone withdrawal (THW)-stimulated measurements. Moreover, rhTSH-stimulated serum Tg is comparable to a THW-stimulated measurement for detecting recurrent disease, when a cutoff value of 2 mcg/L is used.2
rhTSH testing has similar sensitivity to THW
A 2004 meta-analysis examined 46 studies with a total of 9094 patients. THW-stimulated Tg measurements after thyroid remnant ablation had a sensitivity of 96% (95% confidence interval [CI], 93.5%-98.7%) and a specificity of 94% (95% CI, 93.3%-96.1%). For rhTSH-stimulated serum Tg measurements, sensitivity and specificity were 92% (95% CI, 88.9%-96.1%) and 88% (95% CI, 85.4%-90.6%), respectively.
Because the difference in sensitivity between THW-stimulated and rhTSH-stimulated serum Tg isn’t statistically significant, rhTSH can be used for Tg testing without significantly decreasing detection of DTC recurrence. The slightly lower specificity of rhTSH may lead to unnecessary additional testing because of a few more false-positive results. However, this risk should be weighed against the benefits of reducing morbidity by avoiding the need to withhold thyroid hormone replacement therapy before testing.3
Thyroglobulin measurements: How they compare to body scanning
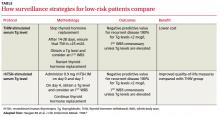
A 1999 prospective cohort study of 229 patients with DTC compared the accuracy of I131 whole body scanning with serum Tg measurement after both rhTSH and THW stimulation (TABLE). The results of the whole body scan were concordant with the rhTSH-stimulated and THW-stimulated Tg measurements in 89% of the patients (P=.108).
Using a cutoff value of ≥2 mcg/L for recurrent disease, an elevated Tg level was detected in 52% of patients with localized thyroid bed disease after rhTSH stimulation and in 56% of patients after THW stimulation. An elevated Tg level after rhTSH stimulation was found in 100% of patients with metastatic disease. Symptoms of hypothyroidism, including overall quality-of-life scores, were significantly better in the rhTSH group than the THW group (P<.01).4
rhTSH-stimulated Tg: Accuracy with a lower cost
A retrospective cohort study of 107 patients determined that rhTSH-stimulated serum Tg levels alone are sensitive enough to identify recurrent disease in low-risk patients. Levels greater than 2 mcg/L had a sensitivity and negative predictive value of 100% and a false-positive rate of 9%—a statistically and clinically significant improvement in accuracy over a whole body scan obtained after rhTSH stimulation, which had a sensitivity of only 27%, negative predictive value of 92%, and false-positive rate of 9% (P<.05). In low-risk patients, rhTSH-stimulated serum Tg measurement is the most accurate and least costly method of surveillance because of its high negative predictive value.5
Whole body scanning doesn’t enhance surveillance accuracy
This conclusion is supported by a cohort study that prospectively followed 99 patients with a history of DTC who underwent serum Tg measurement and an I131 whole body scan obtained after rhTSH stimulation and were followed by neck ultrasound 6 to 12 months after ablation treatment. The whole body scan was negative in 95% of the patients, with a sensitivity of 0%. Serum Tg was positive in 19 of these patients. Neck ultrasound confirmed positive lymph nodes in 7 patients, of whom 5 were Tg-positive. The I131 whole body scan added no benefit to the accuracy of surveillance.6
Recommendations
The British Thyroid Association and the American Thyroid Association recommend performing a physical examination with serum TSH, Tg, and antithyroglobulin antibodies at 6 and 12 months postablation, then annually if the patient is disease free.7,8
In low-risk patients, stimulated serum Tg measurement alone is an acceptable initial follow-up; a value of ≥2 mcg/L indicates a need for further evaluation. If serum Tg is undetectable under TSH stimulation, subsequent long-term follow-up by serum Tg levels alone while under TSH suppression is sufficient. TSH stimulation can be achieved by THW or rhTSH.7-9
A whole body scan rarely adds valuable additional information. Periodic neck ultrasound should be performed, however.7-9
Acknowledgement
The opinions and assertions contained herein are the private views of the authors and not to be construed as official or as reflecting the views of the US Air Force Medical Service or the US Air Force at large.
A recombinant human thyrotropin (rhTSH)-stimulated serum thyroglobulin (Tg) level alone is sufficient to monitor for recurrent disease in low-risk patients with a history of differentiated thyroid cancer (DTC) (strength of recommendation [SOR] A, meta-analysis). Low-risk patients are defined as patients who have undergone total thyroidectomy and radioactive iodine (I131) remnant ablation therapy and show no clinical evidence of recurrent disease.
Evidence summary
An estimated 37,340 new cases of thyroid cancer are diagnosed annually in the United States, typically in people between 20 and 55 years of age. The most common type of thyroid cancer is DTC, which includes papillary and follicular carcinoma. Papillary carcinoma accounts for 80% of all thyroid cancers, and follicular carcinoma accounts for 10%.
The 5-year survival rate for all cases of DTC is 97%. Although the disease has a favorable prognosis, an estimated 1630 patients were expected to die of it in 2009 because of its prevalence.1
The goal: Find recurrent disease early
The purpose of surveillance protocols in thyroid cancer is early detection of recurrent disease. Expert debate about DTC surveillance centers on the disease’s low incidence and prolonged clinical course, as well as a lack of prospective randomized clinical trials. Current guidelines were developed from large retrospective cohort studies of patients observed over several decades.
rhTSH-stimulated Tg is the new surveillance standard
All major professional organizations support the consensus that an rhTSH-stimulated serum Tg is adequate to follow-up low-risk patients. This test replaces the previous accepted standard of thyroid hormone withdrawal (THW)-stimulated measurements. Moreover, rhTSH-stimulated serum Tg is comparable to a THW-stimulated measurement for detecting recurrent disease, when a cutoff value of 2 mcg/L is used.2
rhTSH testing has similar sensitivity to THW
A 2004 meta-analysis examined 46 studies with a total of 9094 patients. THW-stimulated Tg measurements after thyroid remnant ablation had a sensitivity of 96% (95% confidence interval [CI], 93.5%-98.7%) and a specificity of 94% (95% CI, 93.3%-96.1%). For rhTSH-stimulated serum Tg measurements, sensitivity and specificity were 92% (95% CI, 88.9%-96.1%) and 88% (95% CI, 85.4%-90.6%), respectively.
Because the difference in sensitivity between THW-stimulated and rhTSH-stimulated serum Tg isn’t statistically significant, rhTSH can be used for Tg testing without significantly decreasing detection of DTC recurrence. The slightly lower specificity of rhTSH may lead to unnecessary additional testing because of a few more false-positive results. However, this risk should be weighed against the benefits of reducing morbidity by avoiding the need to withhold thyroid hormone replacement therapy before testing.3
Thyroglobulin measurements: How they compare to body scanning
A 1999 prospective cohort study of 229 patients with DTC compared the accuracy of I131 whole body scanning with serum Tg measurement after both rhTSH and THW stimulation (TABLE). The results of the whole body scan were concordant with the rhTSH-stimulated and THW-stimulated Tg measurements in 89% of the patients (P=.108).
Using a cutoff value of ≥2 mcg/L for recurrent disease, an elevated Tg level was detected in 52% of patients with localized thyroid bed disease after rhTSH stimulation and in 56% of patients after THW stimulation. An elevated Tg level after rhTSH stimulation was found in 100% of patients with metastatic disease. Symptoms of hypothyroidism, including overall quality-of-life scores, were significantly better in the rhTSH group than the THW group (P<.01).4
rhTSH-stimulated Tg: Accuracy with a lower cost
A retrospective cohort study of 107 patients determined that rhTSH-stimulated serum Tg levels alone are sensitive enough to identify recurrent disease in low-risk patients. Levels greater than 2 mcg/L had a sensitivity and negative predictive value of 100% and a false-positive rate of 9%—a statistically and clinically significant improvement in accuracy over a whole body scan obtained after rhTSH stimulation, which had a sensitivity of only 27%, negative predictive value of 92%, and false-positive rate of 9% (P<.05). In low-risk patients, rhTSH-stimulated serum Tg measurement is the most accurate and least costly method of surveillance because of its high negative predictive value.5
Whole body scanning doesn’t enhance surveillance accuracy
This conclusion is supported by a cohort study that prospectively followed 99 patients with a history of DTC who underwent serum Tg measurement and an I131 whole body scan obtained after rhTSH stimulation and were followed by neck ultrasound 6 to 12 months after ablation treatment. The whole body scan was negative in 95% of the patients, with a sensitivity of 0%. Serum Tg was positive in 19 of these patients. Neck ultrasound confirmed positive lymph nodes in 7 patients, of whom 5 were Tg-positive. The I131 whole body scan added no benefit to the accuracy of surveillance.6
Recommendations
The British Thyroid Association and the American Thyroid Association recommend performing a physical examination with serum TSH, Tg, and antithyroglobulin antibodies at 6 and 12 months postablation, then annually if the patient is disease free.7,8
In low-risk patients, stimulated serum Tg measurement alone is an acceptable initial follow-up; a value of ≥2 mcg/L indicates a need for further evaluation. If serum Tg is undetectable under TSH stimulation, subsequent long-term follow-up by serum Tg levels alone while under TSH suppression is sufficient. TSH stimulation can be achieved by THW or rhTSH.7-9
A whole body scan rarely adds valuable additional information. Periodic neck ultrasound should be performed, however.7-9
Acknowledgement
The opinions and assertions contained herein are the private views of the authors and not to be construed as official or as reflecting the views of the US Air Force Medical Service or the US Air Force at large.
A recombinant human thyrotropin (rhTSH)-stimulated serum thyroglobulin (Tg) level alone is sufficient to monitor for recurrent disease in low-risk patients with a history of differentiated thyroid cancer (DTC) (strength of recommendation [SOR] A, meta-analysis). Low-risk patients are defined as patients who have undergone total thyroidectomy and radioactive iodine (I131) remnant ablation therapy and show no clinical evidence of recurrent disease.
Evidence summary
An estimated 37,340 new cases of thyroid cancer are diagnosed annually in the United States, typically in people between 20 and 55 years of age. The most common type of thyroid cancer is DTC, which includes papillary and follicular carcinoma. Papillary carcinoma accounts for 80% of all thyroid cancers, and follicular carcinoma accounts for 10%.
The 5-year survival rate for all cases of DTC is 97%. Although the disease has a favorable prognosis, an estimated 1630 patients were expected to die of it in 2009 because of its prevalence.1
The goal: Find recurrent disease early
The purpose of surveillance protocols in thyroid cancer is early detection of recurrent disease. Expert debate about DTC surveillance centers on the disease’s low incidence and prolonged clinical course, as well as a lack of prospective randomized clinical trials. Current guidelines were developed from large retrospective cohort studies of patients observed over several decades.
rhTSH-stimulated Tg is the new surveillance standard
All major professional organizations support the consensus that an rhTSH-stimulated serum Tg is adequate to follow-up low-risk patients. This test replaces the previous accepted standard of thyroid hormone withdrawal (THW)-stimulated measurements. Moreover, rhTSH-stimulated serum Tg is comparable to a THW-stimulated measurement for detecting recurrent disease, when a cutoff value of 2 mcg/L is used.2
rhTSH testing has similar sensitivity to THW
A 2004 meta-analysis examined 46 studies with a total of 9094 patients. THW-stimulated Tg measurements after thyroid remnant ablation had a sensitivity of 96% (95% confidence interval [CI], 93.5%-98.7%) and a specificity of 94% (95% CI, 93.3%-96.1%). For rhTSH-stimulated serum Tg measurements, sensitivity and specificity were 92% (95% CI, 88.9%-96.1%) and 88% (95% CI, 85.4%-90.6%), respectively.
Because the difference in sensitivity between THW-stimulated and rhTSH-stimulated serum Tg isn’t statistically significant, rhTSH can be used for Tg testing without significantly decreasing detection of DTC recurrence. The slightly lower specificity of rhTSH may lead to unnecessary additional testing because of a few more false-positive results. However, this risk should be weighed against the benefits of reducing morbidity by avoiding the need to withhold thyroid hormone replacement therapy before testing.3
Thyroglobulin measurements: How they compare to body scanning
A 1999 prospective cohort study of 229 patients with DTC compared the accuracy of I131 whole body scanning with serum Tg measurement after both rhTSH and THW stimulation (TABLE). The results of the whole body scan were concordant with the rhTSH-stimulated and THW-stimulated Tg measurements in 89% of the patients (P=.108).
Using a cutoff value of ≥2 mcg/L for recurrent disease, an elevated Tg level was detected in 52% of patients with localized thyroid bed disease after rhTSH stimulation and in 56% of patients after THW stimulation. An elevated Tg level after rhTSH stimulation was found in 100% of patients with metastatic disease. Symptoms of hypothyroidism, including overall quality-of-life scores, were significantly better in the rhTSH group than the THW group (P<.01).4
rhTSH-stimulated Tg: Accuracy with a lower cost
A retrospective cohort study of 107 patients determined that rhTSH-stimulated serum Tg levels alone are sensitive enough to identify recurrent disease in low-risk patients. Levels greater than 2 mcg/L had a sensitivity and negative predictive value of 100% and a false-positive rate of 9%—a statistically and clinically significant improvement in accuracy over a whole body scan obtained after rhTSH stimulation, which had a sensitivity of only 27%, negative predictive value of 92%, and false-positive rate of 9% (P<.05). In low-risk patients, rhTSH-stimulated serum Tg measurement is the most accurate and least costly method of surveillance because of its high negative predictive value.5
Whole body scanning doesn’t enhance surveillance accuracy
This conclusion is supported by a cohort study that prospectively followed 99 patients with a history of DTC who underwent serum Tg measurement and an I131 whole body scan obtained after rhTSH stimulation and were followed by neck ultrasound 6 to 12 months after ablation treatment. The whole body scan was negative in 95% of the patients, with a sensitivity of 0%. Serum Tg was positive in 19 of these patients. Neck ultrasound confirmed positive lymph nodes in 7 patients, of whom 5 were Tg-positive. The I131 whole body scan added no benefit to the accuracy of surveillance.6
Recommendations
The British Thyroid Association and the American Thyroid Association recommend performing a physical examination with serum TSH, Tg, and antithyroglobulin antibodies at 6 and 12 months postablation, then annually if the patient is disease free.7,8
In low-risk patients, stimulated serum Tg measurement alone is an acceptable initial follow-up; a value of ≥2 mcg/L indicates a need for further evaluation. If serum Tg is undetectable under TSH stimulation, subsequent long-term follow-up by serum Tg levels alone while under TSH suppression is sufficient. TSH stimulation can be achieved by THW or rhTSH.7-9
A whole body scan rarely adds valuable additional information. Periodic neck ultrasound should be performed, however.7-9
Acknowledgement
The opinions and assertions contained herein are the private views of the authors and not to be construed as official or as reflecting the views of the US Air Force Medical Service or the US Air Force at large.
Evidence-based answers from the Family Physicians Inquiries Network
Does heat or cold work better for acute muscle strain?
Cryotherapy is better than heat for treating acute muscle strain (strength of recommendation [SOR]: C, consensus, usual practice, and expert opinion). Insufficient patient-oriented evidence exists regarding use of heat to treat acute soft-tissue injuries.
Evidence summary
A comprehensive review of the literature revealed no studies that compare heat and cryotherapy to treat acute soft-tissue injury. Well-designed human trials of general management of acute soft-tissue injury are rare.1
Cryotherapy has been the recommended initial treatment for muscle strain for more than 30 years, based generally on expert opinion and physiological models, not clinical trials.2 Theoretically, cryotherapy controls hemorrhage and tissue edema, whereas heat enhances the inflammatory response.2
One human RCT and animal studies find benefits from cold
A 2007 review evaluated 66 publications and found only 1 randomized controlled trial conducted on humans.3 The intervention in this trial involved applying cold gel 4 times a day for the first 14 days after the injury. The control group received a room-temperature gel application; neither group was aware of the temperature differential.
The study found significant reduction in pain at rest, pain with movement, and functional disability at intervals of 7, 14, and 28 days postinjury (P<.001) among patients receiving cold-gel applications. Patients receiving cold-gel treatment also reported increased satisfaction with treatment compared with the controls. At 28 days, cold-gel treatment patients scored 71 on a 100-point satisfaction scale compared with 44 for controls (P<.001).3 Inconclusive results or significant design flaws limited the validity of all other trials cited in this review.3
Laboratory studies on rats have also demonstrated beneficial effects of cryotherapy after simulated soft-tissue injuries.4,5 One study cited a significant reduction in inflammatory cells, based on histologic examination, in 43 rats between 6 and 24 hours after trauma.4 A second study of 21 rats showed improvement in associated physiological components with cryotherapy, but no statistically significant improvement in edema.5
How cold is too cold?
Most authorities recommend empiric treatment with cryotherapy during the acute inflammatory phase—the first 24 to 48 hours after injury.6 Although not rigorously studied, some sources recommend applying cold to the involved muscle for the first 4 hours after injury at intervals of 10 to 20 minutes every 30 to 60 minutes.6
The literature focuses more on the optimal temperature for cryotherapy than on the duration and frequency of therapy.7 Temperatures below 15°to 25°C may actually result in vasodilatation rather than vasoconstriction.7
Evidence for heat is limited
A 2006 Cochrane review that addressed treatment of lower back muscular strain, not soft-tissue injuries in general, found moderate evidence that heat therapy reduces pain by 17% and disability in the acute setting (P=.001).8 The review also cited 2 head-to-head trials that compared heat and cryotherapy; however, the study designs were poor and the results were contradictory.8
Recommendations
Authoritative textbooks consistently recommend applying ice for initial treatment of musculoskeletal and soft-tissue strains.9
Acknowledgments
The opinions and assertions contained herein are the private views of the authors and not to be construed as official or as reflecting the views of the United States Air Force Medical Service or the United States Air Force at large.
1. Hubbard TJ, Denegar CR. Does cryotherapy improve outcomes with soft tissue injury? J Athl Train. 2004;39:278-279.
2. Kalenak A, Medlar CE, Fleagle SB, Hochberg WJ. Athletic injuries: heat vs cold. Am Fam Physician. 1975;12:131-134.
3. Collins NC. Is ice right? Does cryotherapy improve outcome for acute soft tissue injury? Emerg Med J. 2008;25:65-68.
4. Hurme T, Rantanen J, Kalimo H. Effects of early cryotherapy in experimental skeletal muscle injury. Scand J Med Sci Sports. 1993;3:46-51.
5. Schaser K, Disch AC, Stover JF, et al. Prolonged superficial local cryotherapy attenuates microcirculatory impairment, regional inflammation, and muscle necrosis after closed soft tissue injury in rats. Am J Sports Med. 2007;35:93-102.
6. Kellett J. Acute soft tissue injuries—a review of the literature. Med Sci Sports Exerc. 1986;18:489-500.
7. McMaster WC, Liddle S, Waugh TR. Laboratory evaluation of various cold therapy modalities. Am J Sports Med. 1978;6:291-294.
8. French SD, Cameron M, Walker BF, Reggars JW, Esterman AJ. A Cochrane review of superficial heat or cold for low back pain. Spine. 2006;31:998-1006.
9. Griffin LY. Essentials of Musculoskeletal Care. 3rd ed. Rosemont, Ill: American Academy of Orthopaedic Surgeons; 2005:134.
Cryotherapy is better than heat for treating acute muscle strain (strength of recommendation [SOR]: C, consensus, usual practice, and expert opinion). Insufficient patient-oriented evidence exists regarding use of heat to treat acute soft-tissue injuries.
Evidence summary
A comprehensive review of the literature revealed no studies that compare heat and cryotherapy to treat acute soft-tissue injury. Well-designed human trials of general management of acute soft-tissue injury are rare.1
Cryotherapy has been the recommended initial treatment for muscle strain for more than 30 years, based generally on expert opinion and physiological models, not clinical trials.2 Theoretically, cryotherapy controls hemorrhage and tissue edema, whereas heat enhances the inflammatory response.2
One human RCT and animal studies find benefits from cold
A 2007 review evaluated 66 publications and found only 1 randomized controlled trial conducted on humans.3 The intervention in this trial involved applying cold gel 4 times a day for the first 14 days after the injury. The control group received a room-temperature gel application; neither group was aware of the temperature differential.
The study found significant reduction in pain at rest, pain with movement, and functional disability at intervals of 7, 14, and 28 days postinjury (P<.001) among patients receiving cold-gel applications. Patients receiving cold-gel treatment also reported increased satisfaction with treatment compared with the controls. At 28 days, cold-gel treatment patients scored 71 on a 100-point satisfaction scale compared with 44 for controls (P<.001).3 Inconclusive results or significant design flaws limited the validity of all other trials cited in this review.3
Laboratory studies on rats have also demonstrated beneficial effects of cryotherapy after simulated soft-tissue injuries.4,5 One study cited a significant reduction in inflammatory cells, based on histologic examination, in 43 rats between 6 and 24 hours after trauma.4 A second study of 21 rats showed improvement in associated physiological components with cryotherapy, but no statistically significant improvement in edema.5
How cold is too cold?
Most authorities recommend empiric treatment with cryotherapy during the acute inflammatory phase—the first 24 to 48 hours after injury.6 Although not rigorously studied, some sources recommend applying cold to the involved muscle for the first 4 hours after injury at intervals of 10 to 20 minutes every 30 to 60 minutes.6
The literature focuses more on the optimal temperature for cryotherapy than on the duration and frequency of therapy.7 Temperatures below 15°to 25°C may actually result in vasodilatation rather than vasoconstriction.7
Evidence for heat is limited
A 2006 Cochrane review that addressed treatment of lower back muscular strain, not soft-tissue injuries in general, found moderate evidence that heat therapy reduces pain by 17% and disability in the acute setting (P=.001).8 The review also cited 2 head-to-head trials that compared heat and cryotherapy; however, the study designs were poor and the results were contradictory.8
Recommendations
Authoritative textbooks consistently recommend applying ice for initial treatment of musculoskeletal and soft-tissue strains.9
Acknowledgments
The opinions and assertions contained herein are the private views of the authors and not to be construed as official or as reflecting the views of the United States Air Force Medical Service or the United States Air Force at large.
Cryotherapy is better than heat for treating acute muscle strain (strength of recommendation [SOR]: C, consensus, usual practice, and expert opinion). Insufficient patient-oriented evidence exists regarding use of heat to treat acute soft-tissue injuries.
Evidence summary
A comprehensive review of the literature revealed no studies that compare heat and cryotherapy to treat acute soft-tissue injury. Well-designed human trials of general management of acute soft-tissue injury are rare.1
Cryotherapy has been the recommended initial treatment for muscle strain for more than 30 years, based generally on expert opinion and physiological models, not clinical trials.2 Theoretically, cryotherapy controls hemorrhage and tissue edema, whereas heat enhances the inflammatory response.2
One human RCT and animal studies find benefits from cold
A 2007 review evaluated 66 publications and found only 1 randomized controlled trial conducted on humans.3 The intervention in this trial involved applying cold gel 4 times a day for the first 14 days after the injury. The control group received a room-temperature gel application; neither group was aware of the temperature differential.
The study found significant reduction in pain at rest, pain with movement, and functional disability at intervals of 7, 14, and 28 days postinjury (P<.001) among patients receiving cold-gel applications. Patients receiving cold-gel treatment also reported increased satisfaction with treatment compared with the controls. At 28 days, cold-gel treatment patients scored 71 on a 100-point satisfaction scale compared with 44 for controls (P<.001).3 Inconclusive results or significant design flaws limited the validity of all other trials cited in this review.3
Laboratory studies on rats have also demonstrated beneficial effects of cryotherapy after simulated soft-tissue injuries.4,5 One study cited a significant reduction in inflammatory cells, based on histologic examination, in 43 rats between 6 and 24 hours after trauma.4 A second study of 21 rats showed improvement in associated physiological components with cryotherapy, but no statistically significant improvement in edema.5
How cold is too cold?
Most authorities recommend empiric treatment with cryotherapy during the acute inflammatory phase—the first 24 to 48 hours after injury.6 Although not rigorously studied, some sources recommend applying cold to the involved muscle for the first 4 hours after injury at intervals of 10 to 20 minutes every 30 to 60 minutes.6
The literature focuses more on the optimal temperature for cryotherapy than on the duration and frequency of therapy.7 Temperatures below 15°to 25°C may actually result in vasodilatation rather than vasoconstriction.7
Evidence for heat is limited
A 2006 Cochrane review that addressed treatment of lower back muscular strain, not soft-tissue injuries in general, found moderate evidence that heat therapy reduces pain by 17% and disability in the acute setting (P=.001).8 The review also cited 2 head-to-head trials that compared heat and cryotherapy; however, the study designs were poor and the results were contradictory.8
Recommendations
Authoritative textbooks consistently recommend applying ice for initial treatment of musculoskeletal and soft-tissue strains.9
Acknowledgments
The opinions and assertions contained herein are the private views of the authors and not to be construed as official or as reflecting the views of the United States Air Force Medical Service or the United States Air Force at large.
1. Hubbard TJ, Denegar CR. Does cryotherapy improve outcomes with soft tissue injury? J Athl Train. 2004;39:278-279.
2. Kalenak A, Medlar CE, Fleagle SB, Hochberg WJ. Athletic injuries: heat vs cold. Am Fam Physician. 1975;12:131-134.
3. Collins NC. Is ice right? Does cryotherapy improve outcome for acute soft tissue injury? Emerg Med J. 2008;25:65-68.
4. Hurme T, Rantanen J, Kalimo H. Effects of early cryotherapy in experimental skeletal muscle injury. Scand J Med Sci Sports. 1993;3:46-51.
5. Schaser K, Disch AC, Stover JF, et al. Prolonged superficial local cryotherapy attenuates microcirculatory impairment, regional inflammation, and muscle necrosis after closed soft tissue injury in rats. Am J Sports Med. 2007;35:93-102.
6. Kellett J. Acute soft tissue injuries—a review of the literature. Med Sci Sports Exerc. 1986;18:489-500.
7. McMaster WC, Liddle S, Waugh TR. Laboratory evaluation of various cold therapy modalities. Am J Sports Med. 1978;6:291-294.
8. French SD, Cameron M, Walker BF, Reggars JW, Esterman AJ. A Cochrane review of superficial heat or cold for low back pain. Spine. 2006;31:998-1006.
9. Griffin LY. Essentials of Musculoskeletal Care. 3rd ed. Rosemont, Ill: American Academy of Orthopaedic Surgeons; 2005:134.
1. Hubbard TJ, Denegar CR. Does cryotherapy improve outcomes with soft tissue injury? J Athl Train. 2004;39:278-279.
2. Kalenak A, Medlar CE, Fleagle SB, Hochberg WJ. Athletic injuries: heat vs cold. Am Fam Physician. 1975;12:131-134.
3. Collins NC. Is ice right? Does cryotherapy improve outcome for acute soft tissue injury? Emerg Med J. 2008;25:65-68.
4. Hurme T, Rantanen J, Kalimo H. Effects of early cryotherapy in experimental skeletal muscle injury. Scand J Med Sci Sports. 1993;3:46-51.
5. Schaser K, Disch AC, Stover JF, et al. Prolonged superficial local cryotherapy attenuates microcirculatory impairment, regional inflammation, and muscle necrosis after closed soft tissue injury in rats. Am J Sports Med. 2007;35:93-102.
6. Kellett J. Acute soft tissue injuries—a review of the literature. Med Sci Sports Exerc. 1986;18:489-500.
7. McMaster WC, Liddle S, Waugh TR. Laboratory evaluation of various cold therapy modalities. Am J Sports Med. 1978;6:291-294.
8. French SD, Cameron M, Walker BF, Reggars JW, Esterman AJ. A Cochrane review of superficial heat or cold for low back pain. Spine. 2006;31:998-1006.
9. Griffin LY. Essentials of Musculoskeletal Care. 3rd ed. Rosemont, Ill: American Academy of Orthopaedic Surgeons; 2005:134.
Evidence-based answers from the Family Physicians Inquiries Network