User login
Restructuring health care delivery for the future: What we need to do post–COVID-19
Recently,
Barbara Levy, MD: The disruption of the COVID-19 pandemic has given us an opportunity to consider how we would recraft the delivery of health care for women if we could. My goal for this discussion is to talk about that and see if we can incentivize people to make changes.
Cindy, what are women looking for in health care that they are not getting now?
What women want in health care
Cynthia A. Pearson: Women, like men, want a sense of assurance that health care can be provided in a safe way, and that can’t be given completely right now.
Aside from that, women want a personal connection, ideally with the same provider. Many women are embracing telehealth, which came about because of this disruptive time, and that has potential that we can possibly mobilize around. One thing women don’t always find is consistency and contact, and they would like that.
Scott D. Hayworth, MD: Women want to be listened to, and they want their doctors to take a holistic and individualized approach to their care. In-person visits are the ideal setting for this, but during the pandemic we have had to adapt to new modalities for delivering care: government regulations restricting services, and the necessity to limit the flow of patients into offices, has meant that we have had to rely on remote visits. CareMount Medical has been in the forefront of telehealth with our “Virtual Visit” technology, so we were well prepared, and our patients have embraced this truly vital option. We’ve ramped up capabilities significantly to deal with the surge in volume.
While our practice has been able to provide consistent and convenient access to care, this isn’t the case in all areas of the country. Even before the pandemic, the cost of malpractice insurance has led to shortages of ObGyns; this deficit has been compounded by the closing of hospitals due to restrictions on services imposed to try to stem the spread of COVID-19. The affordability of care has also been jeopardized by job losses and therefore of employer-provided insurance, following months of lockdowns.
Continue to: Dr. Levy...
Dr. Levy: To balance that long-term relationship with access and cost, clearly we are not delivering what is needed. Janice, at UnitedHealth you have experimented with some products and some different ways of delivering care. What are beneficiaries looking for?
Janice Huckaby, MD: There is a real thirst for digital content—everybody consults with Dr. Google. They are looking for reliable sources of clinical content. Ideally, that comes from their physician, but people access it in other ways as well.
I agree that women desire a personalized relationship. That is why we are seeing more communities of women, such as virtual pregnancy support groups, that have cropped up in the age of COVID-19. Women are not content with the idea of “I’m going to see my doctor, get my tummy measured, listen to the heartbeat, and go home.” That model is done. Patients will look for practices that are accessible at convenient times and that can give them the personalized experience to make them feel well cared for and that offer them a long-term relationship.
One concern is that as more obstetric groups use laborists to do their deliveries at the hospital, I wonder whether we do a good job of forming that relationship on the front end, and when it comes to the delivery, will we drop the ball? The jury is out, but it’s worth watching.
Dr. Levy: How do we as obstetrician-gynecologists get patients to consider that we are providing reliable information? There is so much disinformation out there.
Errol R. Norwitz, MD, PhD, MBA: I echo the sentiments discussed and I’ll add that many women want care that is convenient, close to home, coordinated, and integrated—not fragmented. They want their providers and their office to anticipate and know who they are even before they arrive, to be prepared for the visit. And it’s not only care for them, but also care for their families. Women are the gatekeepers to the health care system. They want a health care system in place that will care not just for each member separately but also for the family as an integrated whole.
To answer your question, Barbara, we have all been overwhelmed with the amount of data coming at us, both providers and patients. Teaching providers how to synthesize and integrate the data and then present it to patients is quite a challenge. We have to instill this skill in our trainees, teach them how to absorb and present the data.
Consensus bodies can help in this regard, and ACOG (American College of Obstetricians and Gynecologists) has led the way in providing guidance around the management of pregnancy in the setting of COVID-19. Another reliable site for my trainees is UpToDate, which is easy to access. If a scientific paper comes out today, it will be covered in UpToDate tomorrow. Patients need someone who can synthesize the data and give it to them in little pieces, and keep it current.
Dr. Levy: We need to be a reliable source not only for medical information but also for referral to resources in the community for families and for women.
Continue to: ObGyn services...
ObGyn services: Primary care or specialty?
Dr. Norwitz: That begs the question, who are we? Are we primary care providers or are we a subspecialty, or are we both?
Ms. Pearson: Women, particularly in their younger, middle reproductive years, see their ObGyn as a primary care provider. The way forward for the profession is to embrace the call that Barbara articulated, to know what other referral sources are available beyond other clinicians. We need to be aware of the social determinants of health—that there are times when the primary care provider needs to know the community well enough to know what is available that would make a difference for that person and her family.
Dr. Levy: Scott, how do you manage that?
Dr. Hayworth: As reimbursement models move rapidly toward value, practices that can undertake risk are in the best position to thrive; specialty providers relying solely on fee-for-service may well be unable to survive. The key for any ObGyn practice is to be of sufficient size and scope that it can manage the primary care for a panel of patients, the more numerous the better; being in charge of those dollars allows maximum control. ObGyns who subspecialize should seek to become members of larger groups, whether comprehensive women’s health practices or multispecialty groups like ours at CareMount Medical, that manage the spectrum of care for their patients.
Dr. Levy: Janice, fill us in on some of the structures that exist now for ObGyns that they may be able to participate in—payment structures like the Women’s Medical Home. Does UnitedHealth have anything like that?
Dr. Huckaby: Probably 3 or 4 exist now, but I agree that risk arrangements are perhaps a wave of the future. Right now, UnitedHealth has accountable care organizations (ACOs) that include ObGyns, a number of them in the Northeast. We also rolled out bundled payment programs.
Our hospital contracts have always had metrics around infection rates and elective deliveries before 39 weeks, and we will probably start seeing some of that put into the provider contracts as well.
There is a desire to move people into a risk-sharing model for payment, but part of the concern there is the infrastructure, because if you are going to manage risk, you need to have staff that can do care coordination. Care coordinators can ensure, for example, that people have transportation to their appointments, and thus address some of the social determinants in ways that historically have not been done in obstetrics.
The ACOs sometimes have given seed money for practices to hire additional staff to do those kinds of things, and that can help get practices started. Probably the people best positioned are in large multispecialty groups that can leverage case management and maybe support other specialties.
I do think we are going to see a move to risk in the future. Obstetrics has moved at a slower pace than we have seen in internal medicine and some other specialties.
Dr. Hayworth: The value model for reimbursement can only be managed via care coordination, maximizing efficacy and efficiency at every level for every patient. Fortunately for ObGyns, we are familiar with the value concept via bundling for obstetrical services covering prenatal to postpartum, including delivery. ObGyn practices need to prepare for a future in which insurers will pay for patient panels in which providers take on the risk for the entirety of care.
At CareMount Medical, we have embraced the value model as one of 40 Next Generation Medicare Accountable Care Organizations across the country. We’ve put in place the infrastructure, from front desk through back office, to optimize resource utilization. Our team approach includes both patient advocates and care coordinators who extend the capabilities of our physicians and ensure that our patients’ needs, including well care, are met comprehensively.
Dr. Huckaby: One area that we sometimes leave out, whether we are talking about payment or a patient-centered medical home, is integration with behavioral health. Anxiety and depression are fairly rampant, fairly underdiagnosed, and woefully undertreated. I hope that our ObGyn practices of the future—and maybe this is the broadening into primary care—will engage and take the lead in addressing some of those issues, because women suffer. We need to embrace the behavioral aspect of care for the whole person more than we have.
Continue to: Physician training issues...
Physician training issues
Dr. Levy: I could not agree more. We have trained physicians to do illness care, not wellness care, and to be physician and practice centered, not patient centered. While we train medical students in hospital settings and in acute care, there’s not much training in how to manage people or in the factors that determine whether someone is truly well, such as housing security and food security. We are not training physicians in nutrition or in mental health.
Errol, how do we help an ObGyn or women’s health trainee to prepare for the ideal world we are trying to create?
Dr. Norwitz: It’s a challenging question. I like to reference a remarkable piece by Atul Gawande in The New Yorker, in which he interviewed the CEO of the Cheesecake Factory restaurant chain, who in effect said that we’ve got it all wrong; there’s no health in health care.1 We don’t manage health; we wait until people get sick and then we treat them. We have to put the health back into health care.
It has always been my passion to focus on preventative care. We need to reclaim our identity—I have never particularly liked the name “ObGyn,” the term “women’s health” may be more appropriate and help us focus on disease prevention—and we need to stand up for training programs that separate the O from the G.
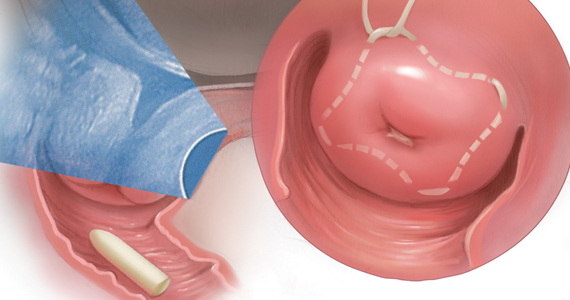
Low-volume surgeons, who may do only 1 or 2 hysterectomies per year, can’t maintain their proficiency, and many don’t do enough cases to maintain their robotics privileges. I can foresee a time where labor and delivery units are like ICUs, where the people who work there do nothing but manage labor and perform deliveries using standardized bundles of practice. Such an approach will decrease variability in management and lead to improved outcomes.
We need to completely reframe how we train our pipeline providers to provide care in women’s health. It would be difficult, take a lot of effort, and there would be pushback, I suspect, but that’s where the field needs to go.
The ideal system redesign
Dr. Levy: Cindy, if you could start from scratch and design an ideal comprehensive system to better deliver care for women of all ages, what would that look like?
Ms. Pearson: I would design a system in which people at any life stage met with providers who were less trained in dealing with disease and more trained in the holistic approach to maintaining health. That might be a nurse practitioner or maybe a version of what Errol describes as a new way of training ObGyns. That’s the initial interaction, and the person could be with someone for decades and deepen the relationship in that wonderful way. It would also have an avenue for the times when disease needed to be treated or when more specialized care would be provided. And the financing would be worked out to support consistency.
Dr. Norwitz: We can learn from other countries. Singapore, with only 5.5 million people, has the best health care system in the world. They have a great model. Costa Rica and Cuba have completely redesigned their health care systems. You go through medical school in 2 or 3 years, and then you get embedded in the community. So you have doctors living in the community responsible for the health of their neighbors. They get to know people in the context in which they live and refer them on only when they need more than basic care. These countries have vastly superior outcome measures, and they spend less money on health care.
Dr. Levy: My dream, as we reinvent things, is that we could create a comprehensive Women’s Medical Home where there’s a hub and an opportunity to be centered on patients so they could reach us when needed.
Ideally we could create a structure with a central contact person—a nurse practitioner, a midwife, someone in family medicine or internal medicine—someone focused on women’s health who has researched how inequities apply to women and women’s health and the areas where research doesn’t necessarily apply to women as just “smaller men.” Then we would have the hub, and the spokes—those would be mental health care providers, surgeons, and people to provide additional services when needed.
The only way I can figure how to make that work from a payment perspective is with a prospective payment system, a per member, per month capitated payment structure. That way, ancillary and other services would be available, and overtesting and such would be disincentivized.
Continue to: The question of payment...
The question of payment
Dr. Hayworth: I agree. For every practice, the two key considerations in addressing the challenges of capitation are, first, that the team approach is essential, and, second, that providers appreciate that everything they do for their patients is reimbursed in a global payment.
At CareMount Medical, our team system embeds advanced practice professionals in our primary care and ObGyn offices. Everyone—physicians, midwives, nurse practitioners—practices at the top of their license. Our care coordinators ensure that our patients’ health journeys are optimized from well care through specialized needs, engaging every member of the care team effectively.
To optimize our success in a risk model, we recognize that tasks and services that went without direct reimbursement in a fee-for-service arrangement are integral to producing the best outcomes for our patients. We examine everything we do from the perspective of how to provide the most advanced care in the most efficient manner. For example, we drive toward moving procedures from the hospital to the outpatient setting, and from the ambulatory surgical center to the office. This allows us maximal control of both quality and cost, with savings benefiting our group as well as the payers with whom we have contracts.
Dr. Norwitz: I have been fortunate to have trained and worked in 5 different countries on 3 continents. There’s no question there are better health care systems out there. Some form of capitation is needed, whether it’s value-based care or a risk-sharing arrangement. But how do you do it without a single payer? I don’t think you can, but I’m ready to listen.
Dr. Hayworth: You can have capitation without a single payer; in fact, it’s far better to have many payers compete to offer the greatest flexibility to both patients and providers. CareMount Medical has 650,000 patients who rely on us to provide their care with the utmost quality and affordability. In our Next Generation ACO, our Medicare patients have the benefit of care coordination in a team approach that saves our government money, and we are incentivized to do our best because some of those savings return to us.
The needs of Medicare patients, of course, are different from those in other age groups, and our contracts with other payers will reflect that distinction. There’s no inherent reason why capitation has to equal “single payer.” The benefits of the risk model are magnified by incentivizing all participants to provide maximum value.
Continue to: Ms. Pearson...
Ms. Pearson: I am going to comment on capitated care because I think educated consumers are well aware of the benefits of moving away from fee-for-service and bringing in some more sensible system. However, given the historical racial inequities and injustices, and lack of access and disparate treatment, capitation raises fear in the hearts of people whose communities have not gotten the care that they need.
The answer is not to avoid capitation, but to find a way for the profession to be seen more visibly as reflecting who they serve, and we know we can’t change the profession’s racial makeup overnight. That’s a generation-long effort.
Dr. Levy: For capitation to work, there has to be value, you have to meet the quality metrics. Having served on the National Quality Forum on multiple different committees, I am convinced that we measure what is easy to measure, and we are not measuring what really matters to people. My thought is to embrace the communities that have been underserved to help us design the metrics for a capitated system that is meaningful to the people that we serve.
Ms. Pearson: On the West Coast, some people are leading efforts to create patient-centered metrics for respectful maternity care led by Black, indigenous, and people of color communities that are validated with solid research tools.
Algorithms for care
Dr. Norwitz: Artificial intelligence (AI) may have a role to play. For example, I think we do a terrible job of caring for women in the postpartum period. We focus almost all of our care in the antepartum period and not postpartum. I am working with a group with a finance and banking background to try and risk-adjust patients in the antepartum, intrapartum, and postpartum period. We are developing algorithms using AI and deep learning technologies to risk-stratify patients and say, “This patient is low risk so can safely get obstetric care with a family medicine doctor or midwife. That patient requires consultation with a maternal-fetal medicine subspecialist or a general internist,” and so on.
Ms. Pearson: As policy advocates, we are trying to get Medicaid postpartum coverage expanded to 12 months. Too many women fall into a coverage gap shortly after delivery; continued coverage would help improve postpartum outcomes. I am curious how an algorithm might help take better care of women postpartum.
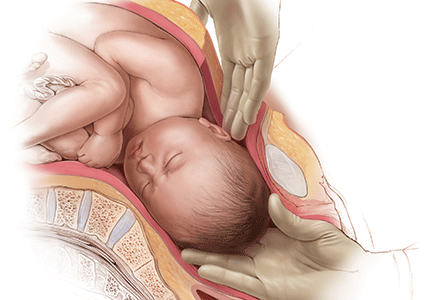
Dr. Norwitz: Postpartum care is one of the greatest areas of need. I love the Dutch model. In the Netherlands, when a woman goes home after giving birth, a designated nurse comes home with her, teaches her how to breastfeed and how to bathe the baby, and assists with routine activities such as cooking and washing. And the nurse remains engaged for a prolonged period of time, paid for by the government. There are also other social welfare packages, such as a full 4-year or more maternity leave.
The solution is part political and part medical. We need to rethink our care model, and I don’t think we provide enough postpartum care.
Continue to: Dr. Hayworth...
Dr. Hayworth: Errol made an excellent point about AI. There is a product that’s being used in Europe and in some other parts of the world that can provide 85% of care through an algorithm without a patient even having to speak to a nurse or doctor. The company that offers the product claims a high level of patient satisfaction and a very low error rate.
We are a long way from the point at which—and I don’t anticipate that we’ll ever get there—AI fully replaces human providers, but there’s enormous and growing potential for data aggregation and machine learning to enhance, exponentially, the capabilities and capacity of care teams.
The most immediate applications for AI in the United States are in diagnostics, pathology, and the mapping of protocols for patients with cancer who will benefit from access to investigational interventions and clinical trials. As we gain experience in those areas, acceptance and confidence will lead steadily to broader deployment of AI, enhancing the quality of care and the efficiency of delivery and saving costs.
Dr. Norwitz: AI is a tool to assist providers. It is not going to replace us, which is the fear.
Ms. Pearson: From the consumer perspective, again, there is concern that if not enough data are available from Black, indigenous, and people of color, the levels won’t start out in a good place. The criticism over mammography randomized controlled trials (RCTs) has existed for a long time. The big trials that got all the way out to mortality did not include enough women of color; and so women of color rightly say, “Why should we believe these guidelines developed on results of the RCTs?” My point is that because of historical inequity, logical solutions such as algorithms do not always work for communities that were previously excluded or mistreated.
Dr. Levy: Your point is incredibly well taken. That means that those of us researching and working with AI need to ensure that the data going in are representative, that we are not embedding implicit biases into the AI algorithms, which clearly has sometimes already happened. We have to be careful to embrace input from multiple sources that we have not thought of before.
As we look at an algorithm for managing a postpartum patient or a postoperative patient, have we thought about how she’s managing her children at home after she goes home? What else is happening in her life? How can we impact her recovery in a positive way? We need to hear the voices of the people that we are trying to serve as we develop those algorithms.
Perspectives on future health care delivery
Dr. Levy: To summarize so far, we are thinking about a Woman’s Medical Home, a capitated model of comprehensive care for women that includes mental health, social determinants, and home care. There are different models, but a payment structure where we would have the capital to invest in community services and in things that we think may make a difference.
Dr. Norwitz: I think the health care system of the future is not going to be based in large academic medical centers. It’s going to be in community hospitals close to home. It’s going to be in the home. And it will be provided by different types of practitioners, whose performances are tracked using more appropriate outcome metrics.
Dr. Levy: I also think we will have community health workers. While we haven’t talked about rural health and access to care, there are some structural things we can do to reach rural communities with really excellent care, such as training community health workers and using telemedicine. It does require thinking through a different payment structure, though, because there really isn’t money in the system to do that currently, at least to my knowledge.
Janice, do we have enough motivation to take care of women? Women are so underrepresented when we look at care models.
Dr. Huckaby: I do think there is hope, but it will truly take a village. While CMS (Centers for Medicare and Medicaid Services) has its innovation center in the Medicaid space, it’s almost like we have to have the payers, the government, the specialty societies, and so on say that we need to do something better. I mention the government because it is not only a payer but also a regulator. They can help create some of these things.
There are opportunities with payers to say, “Let’s move to this kind of model for that.” But still, we are implementing change but on a fairly minor scale.
We could have the people who care about issues, help deliver the care, pay the bills, and so on say, “This is what we want to do,” and then we could pilot them. It may be one type of pilot in a rural area and one type of pilot in an urban area, because they are going to differ, and do it that way and then scale it.
Telemedicine, or telehealth, is part of creating access. Even some nontraditional settings, such as retail store clinics, may work.
Continue to: Dr. Levy...
Dr. Levy: Cindy, is there any last thing you wanted to comment on?
Ms. Pearson: All the changes we have talked about require public policy change. Physicians become physicians to take care of people, not because they want to be policy wonks like us. We love policy because we see how it can benefit. To our readers I say be part of making this generational change in the profession and women’s health care, get involved in policy, because these things can’t happen without the policy changes.
Dr. Norwitz: That is so important. In most developed countries around the world, you get trained in medical school, the cost of training is subsidized, and in return you owe 2 years of service. In this country, if we subsidized the training of doctors and in return they owed us 2 years of primary care service based in the community or in an underserved area, they would get valuable clinical experience and wouldn’t have so many loans to pay back. I think it is a policy that could work and could profoundly change the health care landscape in time.
Dr. Levy: And it would save a great deal of money. The reality is that if we subsidize medical education and in return required service in a national public health service, we would move providers out into rural areas. That would to some extent solve our rural problem. We would train people to think about diagnostic options when the resources are not unlimited, so that they will perhaps not order quite so many tests.
That policy change would foundationally allow for more minority students to become physicians and health care workers. If there were one thing we could do to begin to drive this change, that would be it.
Who would have thought a disruptive pandemic could affect the way people receive care, in bad and good ways? Some carriers, for example, are now paying for telehealth visits who previously did not.
Final thoughts
Dr. Hayworth: It’s an exciting time to be in medicine and women’s health: We are ushering in a new era in which we can fulfill the vision of comprehensive care, patient-focused and seamlessly delivered by teams whose capabilities are optimized by ever-improving technology. ObGyns, with our foundation in the continuum of care, have the experience and the sensibilities to adapt to the challenges of the value model, in which our success will depend on fully embracing our role as primary care providers.
Dr. Levy: Circling back to the beginning of our discussion, we talked about relationships, and developing deep relationships with patients is the internal reward and the piece that prevents us from burnout. It makes you feel good at the end of the day—or sometimes bad at the end of the day when something didn’t go well. Restructuring the system in a way that gets us back to personalized relationship-centered care will benefit ObGyns and our patients.
I thank you all for participating in this thoughtful discussion. ●
- Gawande A. Big med. The New Yorker. August 13, 2012. https://www.newyorker.com/magazine/2012/08/13/big-med. Accessed July 24, 2020.
Recently,
Barbara Levy, MD: The disruption of the COVID-19 pandemic has given us an opportunity to consider how we would recraft the delivery of health care for women if we could. My goal for this discussion is to talk about that and see if we can incentivize people to make changes.
Cindy, what are women looking for in health care that they are not getting now?
What women want in health care
Cynthia A. Pearson: Women, like men, want a sense of assurance that health care can be provided in a safe way, and that can’t be given completely right now.
Aside from that, women want a personal connection, ideally with the same provider. Many women are embracing telehealth, which came about because of this disruptive time, and that has potential that we can possibly mobilize around. One thing women don’t always find is consistency and contact, and they would like that.
Scott D. Hayworth, MD: Women want to be listened to, and they want their doctors to take a holistic and individualized approach to their care. In-person visits are the ideal setting for this, but during the pandemic we have had to adapt to new modalities for delivering care: government regulations restricting services, and the necessity to limit the flow of patients into offices, has meant that we have had to rely on remote visits. CareMount Medical has been in the forefront of telehealth with our “Virtual Visit” technology, so we were well prepared, and our patients have embraced this truly vital option. We’ve ramped up capabilities significantly to deal with the surge in volume.
While our practice has been able to provide consistent and convenient access to care, this isn’t the case in all areas of the country. Even before the pandemic, the cost of malpractice insurance has led to shortages of ObGyns; this deficit has been compounded by the closing of hospitals due to restrictions on services imposed to try to stem the spread of COVID-19. The affordability of care has also been jeopardized by job losses and therefore of employer-provided insurance, following months of lockdowns.
Continue to: Dr. Levy...
Dr. Levy: To balance that long-term relationship with access and cost, clearly we are not delivering what is needed. Janice, at UnitedHealth you have experimented with some products and some different ways of delivering care. What are beneficiaries looking for?
Janice Huckaby, MD: There is a real thirst for digital content—everybody consults with Dr. Google. They are looking for reliable sources of clinical content. Ideally, that comes from their physician, but people access it in other ways as well.
I agree that women desire a personalized relationship. That is why we are seeing more communities of women, such as virtual pregnancy support groups, that have cropped up in the age of COVID-19. Women are not content with the idea of “I’m going to see my doctor, get my tummy measured, listen to the heartbeat, and go home.” That model is done. Patients will look for practices that are accessible at convenient times and that can give them the personalized experience to make them feel well cared for and that offer them a long-term relationship.
One concern is that as more obstetric groups use laborists to do their deliveries at the hospital, I wonder whether we do a good job of forming that relationship on the front end, and when it comes to the delivery, will we drop the ball? The jury is out, but it’s worth watching.
Dr. Levy: How do we as obstetrician-gynecologists get patients to consider that we are providing reliable information? There is so much disinformation out there.
Errol R. Norwitz, MD, PhD, MBA: I echo the sentiments discussed and I’ll add that many women want care that is convenient, close to home, coordinated, and integrated—not fragmented. They want their providers and their office to anticipate and know who they are even before they arrive, to be prepared for the visit. And it’s not only care for them, but also care for their families. Women are the gatekeepers to the health care system. They want a health care system in place that will care not just for each member separately but also for the family as an integrated whole.
To answer your question, Barbara, we have all been overwhelmed with the amount of data coming at us, both providers and patients. Teaching providers how to synthesize and integrate the data and then present it to patients is quite a challenge. We have to instill this skill in our trainees, teach them how to absorb and present the data.
Consensus bodies can help in this regard, and ACOG (American College of Obstetricians and Gynecologists) has led the way in providing guidance around the management of pregnancy in the setting of COVID-19. Another reliable site for my trainees is UpToDate, which is easy to access. If a scientific paper comes out today, it will be covered in UpToDate tomorrow. Patients need someone who can synthesize the data and give it to them in little pieces, and keep it current.
Dr. Levy: We need to be a reliable source not only for medical information but also for referral to resources in the community for families and for women.
Continue to: ObGyn services...
ObGyn services: Primary care or specialty?
Dr. Norwitz: That begs the question, who are we? Are we primary care providers or are we a subspecialty, or are we both?
Ms. Pearson: Women, particularly in their younger, middle reproductive years, see their ObGyn as a primary care provider. The way forward for the profession is to embrace the call that Barbara articulated, to know what other referral sources are available beyond other clinicians. We need to be aware of the social determinants of health—that there are times when the primary care provider needs to know the community well enough to know what is available that would make a difference for that person and her family.
Dr. Levy: Scott, how do you manage that?
Dr. Hayworth: As reimbursement models move rapidly toward value, practices that can undertake risk are in the best position to thrive; specialty providers relying solely on fee-for-service may well be unable to survive. The key for any ObGyn practice is to be of sufficient size and scope that it can manage the primary care for a panel of patients, the more numerous the better; being in charge of those dollars allows maximum control. ObGyns who subspecialize should seek to become members of larger groups, whether comprehensive women’s health practices or multispecialty groups like ours at CareMount Medical, that manage the spectrum of care for their patients.
Dr. Levy: Janice, fill us in on some of the structures that exist now for ObGyns that they may be able to participate in—payment structures like the Women’s Medical Home. Does UnitedHealth have anything like that?
Dr. Huckaby: Probably 3 or 4 exist now, but I agree that risk arrangements are perhaps a wave of the future. Right now, UnitedHealth has accountable care organizations (ACOs) that include ObGyns, a number of them in the Northeast. We also rolled out bundled payment programs.
Our hospital contracts have always had metrics around infection rates and elective deliveries before 39 weeks, and we will probably start seeing some of that put into the provider contracts as well.
There is a desire to move people into a risk-sharing model for payment, but part of the concern there is the infrastructure, because if you are going to manage risk, you need to have staff that can do care coordination. Care coordinators can ensure, for example, that people have transportation to their appointments, and thus address some of the social determinants in ways that historically have not been done in obstetrics.
The ACOs sometimes have given seed money for practices to hire additional staff to do those kinds of things, and that can help get practices started. Probably the people best positioned are in large multispecialty groups that can leverage case management and maybe support other specialties.
I do think we are going to see a move to risk in the future. Obstetrics has moved at a slower pace than we have seen in internal medicine and some other specialties.
Dr. Hayworth: The value model for reimbursement can only be managed via care coordination, maximizing efficacy and efficiency at every level for every patient. Fortunately for ObGyns, we are familiar with the value concept via bundling for obstetrical services covering prenatal to postpartum, including delivery. ObGyn practices need to prepare for a future in which insurers will pay for patient panels in which providers take on the risk for the entirety of care.
At CareMount Medical, we have embraced the value model as one of 40 Next Generation Medicare Accountable Care Organizations across the country. We’ve put in place the infrastructure, from front desk through back office, to optimize resource utilization. Our team approach includes both patient advocates and care coordinators who extend the capabilities of our physicians and ensure that our patients’ needs, including well care, are met comprehensively.
Dr. Huckaby: One area that we sometimes leave out, whether we are talking about payment or a patient-centered medical home, is integration with behavioral health. Anxiety and depression are fairly rampant, fairly underdiagnosed, and woefully undertreated. I hope that our ObGyn practices of the future—and maybe this is the broadening into primary care—will engage and take the lead in addressing some of those issues, because women suffer. We need to embrace the behavioral aspect of care for the whole person more than we have.
Continue to: Physician training issues...
Physician training issues
Dr. Levy: I could not agree more. We have trained physicians to do illness care, not wellness care, and to be physician and practice centered, not patient centered. While we train medical students in hospital settings and in acute care, there’s not much training in how to manage people or in the factors that determine whether someone is truly well, such as housing security and food security. We are not training physicians in nutrition or in mental health.
Errol, how do we help an ObGyn or women’s health trainee to prepare for the ideal world we are trying to create?
Dr. Norwitz: It’s a challenging question. I like to reference a remarkable piece by Atul Gawande in The New Yorker, in which he interviewed the CEO of the Cheesecake Factory restaurant chain, who in effect said that we’ve got it all wrong; there’s no health in health care.1 We don’t manage health; we wait until people get sick and then we treat them. We have to put the health back into health care.
It has always been my passion to focus on preventative care. We need to reclaim our identity—I have never particularly liked the name “ObGyn,” the term “women’s health” may be more appropriate and help us focus on disease prevention—and we need to stand up for training programs that separate the O from the G.
Low-volume surgeons, who may do only 1 or 2 hysterectomies per year, can’t maintain their proficiency, and many don’t do enough cases to maintain their robotics privileges. I can foresee a time where labor and delivery units are like ICUs, where the people who work there do nothing but manage labor and perform deliveries using standardized bundles of practice. Such an approach will decrease variability in management and lead to improved outcomes.
We need to completely reframe how we train our pipeline providers to provide care in women’s health. It would be difficult, take a lot of effort, and there would be pushback, I suspect, but that’s where the field needs to go.
The ideal system redesign
Dr. Levy: Cindy, if you could start from scratch and design an ideal comprehensive system to better deliver care for women of all ages, what would that look like?
Ms. Pearson: I would design a system in which people at any life stage met with providers who were less trained in dealing with disease and more trained in the holistic approach to maintaining health. That might be a nurse practitioner or maybe a version of what Errol describes as a new way of training ObGyns. That’s the initial interaction, and the person could be with someone for decades and deepen the relationship in that wonderful way. It would also have an avenue for the times when disease needed to be treated or when more specialized care would be provided. And the financing would be worked out to support consistency.
Dr. Norwitz: We can learn from other countries. Singapore, with only 5.5 million people, has the best health care system in the world. They have a great model. Costa Rica and Cuba have completely redesigned their health care systems. You go through medical school in 2 or 3 years, and then you get embedded in the community. So you have doctors living in the community responsible for the health of their neighbors. They get to know people in the context in which they live and refer them on only when they need more than basic care. These countries have vastly superior outcome measures, and they spend less money on health care.
Dr. Levy: My dream, as we reinvent things, is that we could create a comprehensive Women’s Medical Home where there’s a hub and an opportunity to be centered on patients so they could reach us when needed.
Ideally we could create a structure with a central contact person—a nurse practitioner, a midwife, someone in family medicine or internal medicine—someone focused on women’s health who has researched how inequities apply to women and women’s health and the areas where research doesn’t necessarily apply to women as just “smaller men.” Then we would have the hub, and the spokes—those would be mental health care providers, surgeons, and people to provide additional services when needed.
The only way I can figure how to make that work from a payment perspective is with a prospective payment system, a per member, per month capitated payment structure. That way, ancillary and other services would be available, and overtesting and such would be disincentivized.
Continue to: The question of payment...
The question of payment
Dr. Hayworth: I agree. For every practice, the two key considerations in addressing the challenges of capitation are, first, that the team approach is essential, and, second, that providers appreciate that everything they do for their patients is reimbursed in a global payment.
At CareMount Medical, our team system embeds advanced practice professionals in our primary care and ObGyn offices. Everyone—physicians, midwives, nurse practitioners—practices at the top of their license. Our care coordinators ensure that our patients’ health journeys are optimized from well care through specialized needs, engaging every member of the care team effectively.
To optimize our success in a risk model, we recognize that tasks and services that went without direct reimbursement in a fee-for-service arrangement are integral to producing the best outcomes for our patients. We examine everything we do from the perspective of how to provide the most advanced care in the most efficient manner. For example, we drive toward moving procedures from the hospital to the outpatient setting, and from the ambulatory surgical center to the office. This allows us maximal control of both quality and cost, with savings benefiting our group as well as the payers with whom we have contracts.
Dr. Norwitz: I have been fortunate to have trained and worked in 5 different countries on 3 continents. There’s no question there are better health care systems out there. Some form of capitation is needed, whether it’s value-based care or a risk-sharing arrangement. But how do you do it without a single payer? I don’t think you can, but I’m ready to listen.
Dr. Hayworth: You can have capitation without a single payer; in fact, it’s far better to have many payers compete to offer the greatest flexibility to both patients and providers. CareMount Medical has 650,000 patients who rely on us to provide their care with the utmost quality and affordability. In our Next Generation ACO, our Medicare patients have the benefit of care coordination in a team approach that saves our government money, and we are incentivized to do our best because some of those savings return to us.
The needs of Medicare patients, of course, are different from those in other age groups, and our contracts with other payers will reflect that distinction. There’s no inherent reason why capitation has to equal “single payer.” The benefits of the risk model are magnified by incentivizing all participants to provide maximum value.
Continue to: Ms. Pearson...
Ms. Pearson: I am going to comment on capitated care because I think educated consumers are well aware of the benefits of moving away from fee-for-service and bringing in some more sensible system. However, given the historical racial inequities and injustices, and lack of access and disparate treatment, capitation raises fear in the hearts of people whose communities have not gotten the care that they need.
The answer is not to avoid capitation, but to find a way for the profession to be seen more visibly as reflecting who they serve, and we know we can’t change the profession’s racial makeup overnight. That’s a generation-long effort.
Dr. Levy: For capitation to work, there has to be value, you have to meet the quality metrics. Having served on the National Quality Forum on multiple different committees, I am convinced that we measure what is easy to measure, and we are not measuring what really matters to people. My thought is to embrace the communities that have been underserved to help us design the metrics for a capitated system that is meaningful to the people that we serve.
Ms. Pearson: On the West Coast, some people are leading efforts to create patient-centered metrics for respectful maternity care led by Black, indigenous, and people of color communities that are validated with solid research tools.
Algorithms for care
Dr. Norwitz: Artificial intelligence (AI) may have a role to play. For example, I think we do a terrible job of caring for women in the postpartum period. We focus almost all of our care in the antepartum period and not postpartum. I am working with a group with a finance and banking background to try and risk-adjust patients in the antepartum, intrapartum, and postpartum period. We are developing algorithms using AI and deep learning technologies to risk-stratify patients and say, “This patient is low risk so can safely get obstetric care with a family medicine doctor or midwife. That patient requires consultation with a maternal-fetal medicine subspecialist or a general internist,” and so on.
Ms. Pearson: As policy advocates, we are trying to get Medicaid postpartum coverage expanded to 12 months. Too many women fall into a coverage gap shortly after delivery; continued coverage would help improve postpartum outcomes. I am curious how an algorithm might help take better care of women postpartum.
Dr. Norwitz: Postpartum care is one of the greatest areas of need. I love the Dutch model. In the Netherlands, when a woman goes home after giving birth, a designated nurse comes home with her, teaches her how to breastfeed and how to bathe the baby, and assists with routine activities such as cooking and washing. And the nurse remains engaged for a prolonged period of time, paid for by the government. There are also other social welfare packages, such as a full 4-year or more maternity leave.
The solution is part political and part medical. We need to rethink our care model, and I don’t think we provide enough postpartum care.
Continue to: Dr. Hayworth...
Dr. Hayworth: Errol made an excellent point about AI. There is a product that’s being used in Europe and in some other parts of the world that can provide 85% of care through an algorithm without a patient even having to speak to a nurse or doctor. The company that offers the product claims a high level of patient satisfaction and a very low error rate.
We are a long way from the point at which—and I don’t anticipate that we’ll ever get there—AI fully replaces human providers, but there’s enormous and growing potential for data aggregation and machine learning to enhance, exponentially, the capabilities and capacity of care teams.
The most immediate applications for AI in the United States are in diagnostics, pathology, and the mapping of protocols for patients with cancer who will benefit from access to investigational interventions and clinical trials. As we gain experience in those areas, acceptance and confidence will lead steadily to broader deployment of AI, enhancing the quality of care and the efficiency of delivery and saving costs.
Dr. Norwitz: AI is a tool to assist providers. It is not going to replace us, which is the fear.
Ms. Pearson: From the consumer perspective, again, there is concern that if not enough data are available from Black, indigenous, and people of color, the levels won’t start out in a good place. The criticism over mammography randomized controlled trials (RCTs) has existed for a long time. The big trials that got all the way out to mortality did not include enough women of color; and so women of color rightly say, “Why should we believe these guidelines developed on results of the RCTs?” My point is that because of historical inequity, logical solutions such as algorithms do not always work for communities that were previously excluded or mistreated.
Dr. Levy: Your point is incredibly well taken. That means that those of us researching and working with AI need to ensure that the data going in are representative, that we are not embedding implicit biases into the AI algorithms, which clearly has sometimes already happened. We have to be careful to embrace input from multiple sources that we have not thought of before.
As we look at an algorithm for managing a postpartum patient or a postoperative patient, have we thought about how she’s managing her children at home after she goes home? What else is happening in her life? How can we impact her recovery in a positive way? We need to hear the voices of the people that we are trying to serve as we develop those algorithms.
Perspectives on future health care delivery
Dr. Levy: To summarize so far, we are thinking about a Woman’s Medical Home, a capitated model of comprehensive care for women that includes mental health, social determinants, and home care. There are different models, but a payment structure where we would have the capital to invest in community services and in things that we think may make a difference.
Dr. Norwitz: I think the health care system of the future is not going to be based in large academic medical centers. It’s going to be in community hospitals close to home. It’s going to be in the home. And it will be provided by different types of practitioners, whose performances are tracked using more appropriate outcome metrics.
Dr. Levy: I also think we will have community health workers. While we haven’t talked about rural health and access to care, there are some structural things we can do to reach rural communities with really excellent care, such as training community health workers and using telemedicine. It does require thinking through a different payment structure, though, because there really isn’t money in the system to do that currently, at least to my knowledge.
Janice, do we have enough motivation to take care of women? Women are so underrepresented when we look at care models.
Dr. Huckaby: I do think there is hope, but it will truly take a village. While CMS (Centers for Medicare and Medicaid Services) has its innovation center in the Medicaid space, it’s almost like we have to have the payers, the government, the specialty societies, and so on say that we need to do something better. I mention the government because it is not only a payer but also a regulator. They can help create some of these things.
There are opportunities with payers to say, “Let’s move to this kind of model for that.” But still, we are implementing change but on a fairly minor scale.
We could have the people who care about issues, help deliver the care, pay the bills, and so on say, “This is what we want to do,” and then we could pilot them. It may be one type of pilot in a rural area and one type of pilot in an urban area, because they are going to differ, and do it that way and then scale it.
Telemedicine, or telehealth, is part of creating access. Even some nontraditional settings, such as retail store clinics, may work.
Continue to: Dr. Levy...
Dr. Levy: Cindy, is there any last thing you wanted to comment on?
Ms. Pearson: All the changes we have talked about require public policy change. Physicians become physicians to take care of people, not because they want to be policy wonks like us. We love policy because we see how it can benefit. To our readers I say be part of making this generational change in the profession and women’s health care, get involved in policy, because these things can’t happen without the policy changes.
Dr. Norwitz: That is so important. In most developed countries around the world, you get trained in medical school, the cost of training is subsidized, and in return you owe 2 years of service. In this country, if we subsidized the training of doctors and in return they owed us 2 years of primary care service based in the community or in an underserved area, they would get valuable clinical experience and wouldn’t have so many loans to pay back. I think it is a policy that could work and could profoundly change the health care landscape in time.
Dr. Levy: And it would save a great deal of money. The reality is that if we subsidize medical education and in return required service in a national public health service, we would move providers out into rural areas. That would to some extent solve our rural problem. We would train people to think about diagnostic options when the resources are not unlimited, so that they will perhaps not order quite so many tests.
That policy change would foundationally allow for more minority students to become physicians and health care workers. If there were one thing we could do to begin to drive this change, that would be it.
Who would have thought a disruptive pandemic could affect the way people receive care, in bad and good ways? Some carriers, for example, are now paying for telehealth visits who previously did not.
Final thoughts
Dr. Hayworth: It’s an exciting time to be in medicine and women’s health: We are ushering in a new era in which we can fulfill the vision of comprehensive care, patient-focused and seamlessly delivered by teams whose capabilities are optimized by ever-improving technology. ObGyns, with our foundation in the continuum of care, have the experience and the sensibilities to adapt to the challenges of the value model, in which our success will depend on fully embracing our role as primary care providers.
Dr. Levy: Circling back to the beginning of our discussion, we talked about relationships, and developing deep relationships with patients is the internal reward and the piece that prevents us from burnout. It makes you feel good at the end of the day—or sometimes bad at the end of the day when something didn’t go well. Restructuring the system in a way that gets us back to personalized relationship-centered care will benefit ObGyns and our patients.
I thank you all for participating in this thoughtful discussion. ●
Recently,
Barbara Levy, MD: The disruption of the COVID-19 pandemic has given us an opportunity to consider how we would recraft the delivery of health care for women if we could. My goal for this discussion is to talk about that and see if we can incentivize people to make changes.
Cindy, what are women looking for in health care that they are not getting now?
What women want in health care
Cynthia A. Pearson: Women, like men, want a sense of assurance that health care can be provided in a safe way, and that can’t be given completely right now.
Aside from that, women want a personal connection, ideally with the same provider. Many women are embracing telehealth, which came about because of this disruptive time, and that has potential that we can possibly mobilize around. One thing women don’t always find is consistency and contact, and they would like that.
Scott D. Hayworth, MD: Women want to be listened to, and they want their doctors to take a holistic and individualized approach to their care. In-person visits are the ideal setting for this, but during the pandemic we have had to adapt to new modalities for delivering care: government regulations restricting services, and the necessity to limit the flow of patients into offices, has meant that we have had to rely on remote visits. CareMount Medical has been in the forefront of telehealth with our “Virtual Visit” technology, so we were well prepared, and our patients have embraced this truly vital option. We’ve ramped up capabilities significantly to deal with the surge in volume.
While our practice has been able to provide consistent and convenient access to care, this isn’t the case in all areas of the country. Even before the pandemic, the cost of malpractice insurance has led to shortages of ObGyns; this deficit has been compounded by the closing of hospitals due to restrictions on services imposed to try to stem the spread of COVID-19. The affordability of care has also been jeopardized by job losses and therefore of employer-provided insurance, following months of lockdowns.
Continue to: Dr. Levy...
Dr. Levy: To balance that long-term relationship with access and cost, clearly we are not delivering what is needed. Janice, at UnitedHealth you have experimented with some products and some different ways of delivering care. What are beneficiaries looking for?
Janice Huckaby, MD: There is a real thirst for digital content—everybody consults with Dr. Google. They are looking for reliable sources of clinical content. Ideally, that comes from their physician, but people access it in other ways as well.
I agree that women desire a personalized relationship. That is why we are seeing more communities of women, such as virtual pregnancy support groups, that have cropped up in the age of COVID-19. Women are not content with the idea of “I’m going to see my doctor, get my tummy measured, listen to the heartbeat, and go home.” That model is done. Patients will look for practices that are accessible at convenient times and that can give them the personalized experience to make them feel well cared for and that offer them a long-term relationship.
One concern is that as more obstetric groups use laborists to do their deliveries at the hospital, I wonder whether we do a good job of forming that relationship on the front end, and when it comes to the delivery, will we drop the ball? The jury is out, but it’s worth watching.
Dr. Levy: How do we as obstetrician-gynecologists get patients to consider that we are providing reliable information? There is so much disinformation out there.
Errol R. Norwitz, MD, PhD, MBA: I echo the sentiments discussed and I’ll add that many women want care that is convenient, close to home, coordinated, and integrated—not fragmented. They want their providers and their office to anticipate and know who they are even before they arrive, to be prepared for the visit. And it’s not only care for them, but also care for their families. Women are the gatekeepers to the health care system. They want a health care system in place that will care not just for each member separately but also for the family as an integrated whole.
To answer your question, Barbara, we have all been overwhelmed with the amount of data coming at us, both providers and patients. Teaching providers how to synthesize and integrate the data and then present it to patients is quite a challenge. We have to instill this skill in our trainees, teach them how to absorb and present the data.
Consensus bodies can help in this regard, and ACOG (American College of Obstetricians and Gynecologists) has led the way in providing guidance around the management of pregnancy in the setting of COVID-19. Another reliable site for my trainees is UpToDate, which is easy to access. If a scientific paper comes out today, it will be covered in UpToDate tomorrow. Patients need someone who can synthesize the data and give it to them in little pieces, and keep it current.
Dr. Levy: We need to be a reliable source not only for medical information but also for referral to resources in the community for families and for women.
Continue to: ObGyn services...
ObGyn services: Primary care or specialty?
Dr. Norwitz: That begs the question, who are we? Are we primary care providers or are we a subspecialty, or are we both?
Ms. Pearson: Women, particularly in their younger, middle reproductive years, see their ObGyn as a primary care provider. The way forward for the profession is to embrace the call that Barbara articulated, to know what other referral sources are available beyond other clinicians. We need to be aware of the social determinants of health—that there are times when the primary care provider needs to know the community well enough to know what is available that would make a difference for that person and her family.
Dr. Levy: Scott, how do you manage that?
Dr. Hayworth: As reimbursement models move rapidly toward value, practices that can undertake risk are in the best position to thrive; specialty providers relying solely on fee-for-service may well be unable to survive. The key for any ObGyn practice is to be of sufficient size and scope that it can manage the primary care for a panel of patients, the more numerous the better; being in charge of those dollars allows maximum control. ObGyns who subspecialize should seek to become members of larger groups, whether comprehensive women’s health practices or multispecialty groups like ours at CareMount Medical, that manage the spectrum of care for their patients.
Dr. Levy: Janice, fill us in on some of the structures that exist now for ObGyns that they may be able to participate in—payment structures like the Women’s Medical Home. Does UnitedHealth have anything like that?
Dr. Huckaby: Probably 3 or 4 exist now, but I agree that risk arrangements are perhaps a wave of the future. Right now, UnitedHealth has accountable care organizations (ACOs) that include ObGyns, a number of them in the Northeast. We also rolled out bundled payment programs.
Our hospital contracts have always had metrics around infection rates and elective deliveries before 39 weeks, and we will probably start seeing some of that put into the provider contracts as well.
There is a desire to move people into a risk-sharing model for payment, but part of the concern there is the infrastructure, because if you are going to manage risk, you need to have staff that can do care coordination. Care coordinators can ensure, for example, that people have transportation to their appointments, and thus address some of the social determinants in ways that historically have not been done in obstetrics.
The ACOs sometimes have given seed money for practices to hire additional staff to do those kinds of things, and that can help get practices started. Probably the people best positioned are in large multispecialty groups that can leverage case management and maybe support other specialties.
I do think we are going to see a move to risk in the future. Obstetrics has moved at a slower pace than we have seen in internal medicine and some other specialties.
Dr. Hayworth: The value model for reimbursement can only be managed via care coordination, maximizing efficacy and efficiency at every level for every patient. Fortunately for ObGyns, we are familiar with the value concept via bundling for obstetrical services covering prenatal to postpartum, including delivery. ObGyn practices need to prepare for a future in which insurers will pay for patient panels in which providers take on the risk for the entirety of care.
At CareMount Medical, we have embraced the value model as one of 40 Next Generation Medicare Accountable Care Organizations across the country. We’ve put in place the infrastructure, from front desk through back office, to optimize resource utilization. Our team approach includes both patient advocates and care coordinators who extend the capabilities of our physicians and ensure that our patients’ needs, including well care, are met comprehensively.
Dr. Huckaby: One area that we sometimes leave out, whether we are talking about payment or a patient-centered medical home, is integration with behavioral health. Anxiety and depression are fairly rampant, fairly underdiagnosed, and woefully undertreated. I hope that our ObGyn practices of the future—and maybe this is the broadening into primary care—will engage and take the lead in addressing some of those issues, because women suffer. We need to embrace the behavioral aspect of care for the whole person more than we have.
Continue to: Physician training issues...
Physician training issues
Dr. Levy: I could not agree more. We have trained physicians to do illness care, not wellness care, and to be physician and practice centered, not patient centered. While we train medical students in hospital settings and in acute care, there’s not much training in how to manage people or in the factors that determine whether someone is truly well, such as housing security and food security. We are not training physicians in nutrition or in mental health.
Errol, how do we help an ObGyn or women’s health trainee to prepare for the ideal world we are trying to create?
Dr. Norwitz: It’s a challenging question. I like to reference a remarkable piece by Atul Gawande in The New Yorker, in which he interviewed the CEO of the Cheesecake Factory restaurant chain, who in effect said that we’ve got it all wrong; there’s no health in health care.1 We don’t manage health; we wait until people get sick and then we treat them. We have to put the health back into health care.
It has always been my passion to focus on preventative care. We need to reclaim our identity—I have never particularly liked the name “ObGyn,” the term “women’s health” may be more appropriate and help us focus on disease prevention—and we need to stand up for training programs that separate the O from the G.
Low-volume surgeons, who may do only 1 or 2 hysterectomies per year, can’t maintain their proficiency, and many don’t do enough cases to maintain their robotics privileges. I can foresee a time where labor and delivery units are like ICUs, where the people who work there do nothing but manage labor and perform deliveries using standardized bundles of practice. Such an approach will decrease variability in management and lead to improved outcomes.
We need to completely reframe how we train our pipeline providers to provide care in women’s health. It would be difficult, take a lot of effort, and there would be pushback, I suspect, but that’s where the field needs to go.
The ideal system redesign
Dr. Levy: Cindy, if you could start from scratch and design an ideal comprehensive system to better deliver care for women of all ages, what would that look like?
Ms. Pearson: I would design a system in which people at any life stage met with providers who were less trained in dealing with disease and more trained in the holistic approach to maintaining health. That might be a nurse practitioner or maybe a version of what Errol describes as a new way of training ObGyns. That’s the initial interaction, and the person could be with someone for decades and deepen the relationship in that wonderful way. It would also have an avenue for the times when disease needed to be treated or when more specialized care would be provided. And the financing would be worked out to support consistency.
Dr. Norwitz: We can learn from other countries. Singapore, with only 5.5 million people, has the best health care system in the world. They have a great model. Costa Rica and Cuba have completely redesigned their health care systems. You go through medical school in 2 or 3 years, and then you get embedded in the community. So you have doctors living in the community responsible for the health of their neighbors. They get to know people in the context in which they live and refer them on only when they need more than basic care. These countries have vastly superior outcome measures, and they spend less money on health care.
Dr. Levy: My dream, as we reinvent things, is that we could create a comprehensive Women’s Medical Home where there’s a hub and an opportunity to be centered on patients so they could reach us when needed.
Ideally we could create a structure with a central contact person—a nurse practitioner, a midwife, someone in family medicine or internal medicine—someone focused on women’s health who has researched how inequities apply to women and women’s health and the areas where research doesn’t necessarily apply to women as just “smaller men.” Then we would have the hub, and the spokes—those would be mental health care providers, surgeons, and people to provide additional services when needed.
The only way I can figure how to make that work from a payment perspective is with a prospective payment system, a per member, per month capitated payment structure. That way, ancillary and other services would be available, and overtesting and such would be disincentivized.
Continue to: The question of payment...
The question of payment
Dr. Hayworth: I agree. For every practice, the two key considerations in addressing the challenges of capitation are, first, that the team approach is essential, and, second, that providers appreciate that everything they do for their patients is reimbursed in a global payment.
At CareMount Medical, our team system embeds advanced practice professionals in our primary care and ObGyn offices. Everyone—physicians, midwives, nurse practitioners—practices at the top of their license. Our care coordinators ensure that our patients’ health journeys are optimized from well care through specialized needs, engaging every member of the care team effectively.
To optimize our success in a risk model, we recognize that tasks and services that went without direct reimbursement in a fee-for-service arrangement are integral to producing the best outcomes for our patients. We examine everything we do from the perspective of how to provide the most advanced care in the most efficient manner. For example, we drive toward moving procedures from the hospital to the outpatient setting, and from the ambulatory surgical center to the office. This allows us maximal control of both quality and cost, with savings benefiting our group as well as the payers with whom we have contracts.
Dr. Norwitz: I have been fortunate to have trained and worked in 5 different countries on 3 continents. There’s no question there are better health care systems out there. Some form of capitation is needed, whether it’s value-based care or a risk-sharing arrangement. But how do you do it without a single payer? I don’t think you can, but I’m ready to listen.
Dr. Hayworth: You can have capitation without a single payer; in fact, it’s far better to have many payers compete to offer the greatest flexibility to both patients and providers. CareMount Medical has 650,000 patients who rely on us to provide their care with the utmost quality and affordability. In our Next Generation ACO, our Medicare patients have the benefit of care coordination in a team approach that saves our government money, and we are incentivized to do our best because some of those savings return to us.
The needs of Medicare patients, of course, are different from those in other age groups, and our contracts with other payers will reflect that distinction. There’s no inherent reason why capitation has to equal “single payer.” The benefits of the risk model are magnified by incentivizing all participants to provide maximum value.
Continue to: Ms. Pearson...
Ms. Pearson: I am going to comment on capitated care because I think educated consumers are well aware of the benefits of moving away from fee-for-service and bringing in some more sensible system. However, given the historical racial inequities and injustices, and lack of access and disparate treatment, capitation raises fear in the hearts of people whose communities have not gotten the care that they need.
The answer is not to avoid capitation, but to find a way for the profession to be seen more visibly as reflecting who they serve, and we know we can’t change the profession’s racial makeup overnight. That’s a generation-long effort.
Dr. Levy: For capitation to work, there has to be value, you have to meet the quality metrics. Having served on the National Quality Forum on multiple different committees, I am convinced that we measure what is easy to measure, and we are not measuring what really matters to people. My thought is to embrace the communities that have been underserved to help us design the metrics for a capitated system that is meaningful to the people that we serve.
Ms. Pearson: On the West Coast, some people are leading efforts to create patient-centered metrics for respectful maternity care led by Black, indigenous, and people of color communities that are validated with solid research tools.
Algorithms for care
Dr. Norwitz: Artificial intelligence (AI) may have a role to play. For example, I think we do a terrible job of caring for women in the postpartum period. We focus almost all of our care in the antepartum period and not postpartum. I am working with a group with a finance and banking background to try and risk-adjust patients in the antepartum, intrapartum, and postpartum period. We are developing algorithms using AI and deep learning technologies to risk-stratify patients and say, “This patient is low risk so can safely get obstetric care with a family medicine doctor or midwife. That patient requires consultation with a maternal-fetal medicine subspecialist or a general internist,” and so on.
Ms. Pearson: As policy advocates, we are trying to get Medicaid postpartum coverage expanded to 12 months. Too many women fall into a coverage gap shortly after delivery; continued coverage would help improve postpartum outcomes. I am curious how an algorithm might help take better care of women postpartum.
Dr. Norwitz: Postpartum care is one of the greatest areas of need. I love the Dutch model. In the Netherlands, when a woman goes home after giving birth, a designated nurse comes home with her, teaches her how to breastfeed and how to bathe the baby, and assists with routine activities such as cooking and washing. And the nurse remains engaged for a prolonged period of time, paid for by the government. There are also other social welfare packages, such as a full 4-year or more maternity leave.
The solution is part political and part medical. We need to rethink our care model, and I don’t think we provide enough postpartum care.
Continue to: Dr. Hayworth...
Dr. Hayworth: Errol made an excellent point about AI. There is a product that’s being used in Europe and in some other parts of the world that can provide 85% of care through an algorithm without a patient even having to speak to a nurse or doctor. The company that offers the product claims a high level of patient satisfaction and a very low error rate.
We are a long way from the point at which—and I don’t anticipate that we’ll ever get there—AI fully replaces human providers, but there’s enormous and growing potential for data aggregation and machine learning to enhance, exponentially, the capabilities and capacity of care teams.
The most immediate applications for AI in the United States are in diagnostics, pathology, and the mapping of protocols for patients with cancer who will benefit from access to investigational interventions and clinical trials. As we gain experience in those areas, acceptance and confidence will lead steadily to broader deployment of AI, enhancing the quality of care and the efficiency of delivery and saving costs.
Dr. Norwitz: AI is a tool to assist providers. It is not going to replace us, which is the fear.
Ms. Pearson: From the consumer perspective, again, there is concern that if not enough data are available from Black, indigenous, and people of color, the levels won’t start out in a good place. The criticism over mammography randomized controlled trials (RCTs) has existed for a long time. The big trials that got all the way out to mortality did not include enough women of color; and so women of color rightly say, “Why should we believe these guidelines developed on results of the RCTs?” My point is that because of historical inequity, logical solutions such as algorithms do not always work for communities that were previously excluded or mistreated.
Dr. Levy: Your point is incredibly well taken. That means that those of us researching and working with AI need to ensure that the data going in are representative, that we are not embedding implicit biases into the AI algorithms, which clearly has sometimes already happened. We have to be careful to embrace input from multiple sources that we have not thought of before.
As we look at an algorithm for managing a postpartum patient or a postoperative patient, have we thought about how she’s managing her children at home after she goes home? What else is happening in her life? How can we impact her recovery in a positive way? We need to hear the voices of the people that we are trying to serve as we develop those algorithms.
Perspectives on future health care delivery
Dr. Levy: To summarize so far, we are thinking about a Woman’s Medical Home, a capitated model of comprehensive care for women that includes mental health, social determinants, and home care. There are different models, but a payment structure where we would have the capital to invest in community services and in things that we think may make a difference.
Dr. Norwitz: I think the health care system of the future is not going to be based in large academic medical centers. It’s going to be in community hospitals close to home. It’s going to be in the home. And it will be provided by different types of practitioners, whose performances are tracked using more appropriate outcome metrics.
Dr. Levy: I also think we will have community health workers. While we haven’t talked about rural health and access to care, there are some structural things we can do to reach rural communities with really excellent care, such as training community health workers and using telemedicine. It does require thinking through a different payment structure, though, because there really isn’t money in the system to do that currently, at least to my knowledge.
Janice, do we have enough motivation to take care of women? Women are so underrepresented when we look at care models.
Dr. Huckaby: I do think there is hope, but it will truly take a village. While CMS (Centers for Medicare and Medicaid Services) has its innovation center in the Medicaid space, it’s almost like we have to have the payers, the government, the specialty societies, and so on say that we need to do something better. I mention the government because it is not only a payer but also a regulator. They can help create some of these things.
There are opportunities with payers to say, “Let’s move to this kind of model for that.” But still, we are implementing change but on a fairly minor scale.
We could have the people who care about issues, help deliver the care, pay the bills, and so on say, “This is what we want to do,” and then we could pilot them. It may be one type of pilot in a rural area and one type of pilot in an urban area, because they are going to differ, and do it that way and then scale it.
Telemedicine, or telehealth, is part of creating access. Even some nontraditional settings, such as retail store clinics, may work.
Continue to: Dr. Levy...
Dr. Levy: Cindy, is there any last thing you wanted to comment on?
Ms. Pearson: All the changes we have talked about require public policy change. Physicians become physicians to take care of people, not because they want to be policy wonks like us. We love policy because we see how it can benefit. To our readers I say be part of making this generational change in the profession and women’s health care, get involved in policy, because these things can’t happen without the policy changes.
Dr. Norwitz: That is so important. In most developed countries around the world, you get trained in medical school, the cost of training is subsidized, and in return you owe 2 years of service. In this country, if we subsidized the training of doctors and in return they owed us 2 years of primary care service based in the community or in an underserved area, they would get valuable clinical experience and wouldn’t have so many loans to pay back. I think it is a policy that could work and could profoundly change the health care landscape in time.
Dr. Levy: And it would save a great deal of money. The reality is that if we subsidize medical education and in return required service in a national public health service, we would move providers out into rural areas. That would to some extent solve our rural problem. We would train people to think about diagnostic options when the resources are not unlimited, so that they will perhaps not order quite so many tests.
That policy change would foundationally allow for more minority students to become physicians and health care workers. If there were one thing we could do to begin to drive this change, that would be it.
Who would have thought a disruptive pandemic could affect the way people receive care, in bad and good ways? Some carriers, for example, are now paying for telehealth visits who previously did not.
Final thoughts
Dr. Hayworth: It’s an exciting time to be in medicine and women’s health: We are ushering in a new era in which we can fulfill the vision of comprehensive care, patient-focused and seamlessly delivered by teams whose capabilities are optimized by ever-improving technology. ObGyns, with our foundation in the continuum of care, have the experience and the sensibilities to adapt to the challenges of the value model, in which our success will depend on fully embracing our role as primary care providers.
Dr. Levy: Circling back to the beginning of our discussion, we talked about relationships, and developing deep relationships with patients is the internal reward and the piece that prevents us from burnout. It makes you feel good at the end of the day—or sometimes bad at the end of the day when something didn’t go well. Restructuring the system in a way that gets us back to personalized relationship-centered care will benefit ObGyns and our patients.
I thank you all for participating in this thoughtful discussion. ●
- Gawande A. Big med. The New Yorker. August 13, 2012. https://www.newyorker.com/magazine/2012/08/13/big-med. Accessed July 24, 2020.
- Gawande A. Big med. The New Yorker. August 13, 2012. https://www.newyorker.com/magazine/2012/08/13/big-med. Accessed July 24, 2020.
Learning to live with COVID-19: Postpandemic life will be reflected in how effectively we leverage this crisis
While often compared with the Spanish influenza contagion of 1918, the current COVID-19 pandemic is arguably unprecedented in scale and scope, global reach, and the rate at which it has spread across the world.
Unprecedented times
The United States now has the greatest burden of COVID-19 disease worldwide.1 Although Boston has thus far been spared the full force of the disease’s impact, it is likely only a matter of time before it reaches here. To prepare for the imminent surge, we at Tufts Medical Center defined 4 short-term strategic imperatives to help guide our COVID-19 preparedness. Having a single unified strategy across our organization has helped to maintain focus and consistency in the messaging amidst all of the uncertainty. Our focus areas are outlined below.
1 Flatten the curve
This term refers to the use of “social distancing” and community isolation measures to keep the number of disease cases at a manageable level. COVID-19 is spread almost exclusively through contact with contaminated respiratory droplets. While several categories of risk have been described, the US Centers for Disease Control and Prevention (CDC) defines disease “exposure” as face-to-face contact within 6 feet of an infected individual for more than 15 minutes without wearing a mask.2 Intervening at all 3 of these touchpoints effectively reduces transmission. Interventions include limiting in-person meetings, increasing the space between individuals (both providers and patients), and routinely using personal protective equipment (PPE).
Another effective strategy is to divide frontline providers into smaller units or teams to limit cross-contamination: the inpatient team versus the outpatient team, the day team versus the night team, the “on” team versus the “off” team. If the infection lays one team low, other providers can step in until they recover and return to work.
Visitor policies should be developed and strictly implemented. Many institutions do allow one support person in labor and delivery (L&D) regardless of the patient’s COVID-19 status, although that person should not be symptomatic or COVID-19 positive. Whether to test all patients and support persons for COVID-19 on arrival at L&D remains controversial.3 At a minimum, these individuals should be screened for symptoms. Although it was a major focus of initial preventative efforts, taking a travel and exposure history is no longer informative as the virus is now endemic and community spread is common.
Initial preventative efforts focused also on high-risk patients, but routine use of PPE for all encounters clearly is more effective because of the high rate of asymptomatic shedding. The virus can survive suspended in the air for up to 2 hours following an aerosol-generating procedure (AGP) and on surfaces for several hours or even days. Practices such as regular handwashing, cleaning of exposed work surfaces, and avoiding face touching should by now be part of our everyday routine.
Institutions throughout the United States have established inpatient COVID-19 units—so-called “dirty” units—with mixed success. As the pandemic spreads and the number of patients with asymptomatic shedding increases, it is harder to determine who is and who is not infected. Cross-contamination has rendered this approach largely ineffective. Whether this will change with the introduction of rapid point-of-care testing remains to be seen.
Continue to: 2 Preserve PPE...
2 Preserve PPE
PPE use is effective in reducing transmission. This includes tier 1 PPE with or without enhanced droplet precaution (surgical mask, eye protection, gloves, yellow gown) and tier 2 PPE (tier 1 plus N95 respirators or powered air-purifying respirators [PAPR]). Given the acute PPE shortage in many parts of the country, appropriate use of PPE is critical to maintain an adequate supply. For example, tier 2 PPE is required only in the setting of an AGP. This includes intubation and, in our determination, the second stage of labor for COVID-19–positive patients and patients under investigation (PUIs); we do not employ tier 2 PPE for all patients in the second stage of labor, although some hospitals endorse this practice.
Creative solutions to the impending PPE shortage abound, such as the use of 3D printers to make face shields and novel techniques to sterilize and reuse N95 respirators.
3 Create capacity
In the absence of effective treatment for COVID-19 and with a vaccine still many months away, supportive care is critical. The pulmonary sequelae with cytokine storm and acute hypoxemia can come on quickly, require urgent mechanical ventilatory support, and take several weeks to resolve.
Our ability to create inpatient capacity to accommodate ill patients, monitor them closely, and intubate early will likely be the most critical driver of the case fatality rate. This requires deferring outpatient visits (or doing them via telemedicine), expanding intensive care unit capabilities (especially ventilator beds), and canceling elective surgeries. What constitutes “elective surgery” is not always clear. Our institution, for example, regards abortion services as essential and not elective, but this is not the case throughout the United States.
Creating capacity also refers to staffing. Where necessary, providers should be retrained and redeployed. This may require emergency credentialing of providers in areas outside their usual clinical practice and permission may be needed from the Accreditation Council for Graduate Medical Education to engage trainees outside their usual duty hours.
4 Support and protect your workforce
Everyone is anxious, and people convey their anxiety in different ways. I have found it helpful to acknowledge those feelings and provide a forum for staff to express and share their anxieties. That said, hospitals are not a democracy. While staff members should be encouraged to ask questions and voice their opinions, everyone is expected to follow protocol regarding patient care.
Celebrating small successes and finding creative ways to alleviate the stress and inject humor can help. Most institutions are using electronic conferencing platforms (such as Zoom or Microsoft Teams) to stay in touch and to continue education initiatives through interactive didactic sessions, grand rounds, morbidity and mortality conferences, and e-journal clubs. These are also a great platform for social events, such as w(h)ine and book clubs and virtual karaoke.
Since many ObGyn providers are women, the closure of day-care centers and schools is particularly challenging. Share best practices among your staff on how to address this problem, such as alternating on-call shifts or matching providers needing day care with ‘furloughed’ college students who are looking to keep busy and make a little money.
Continue to: Avoid overcommunicating...
Avoid overcommunicating
Clear, concise, and timely communication is key. This can be challenging given the rapidly evolving science of COVID-19 and the daily barrage of information from both reliable and unreliable sources. Setting up regular online meetings with your faculty 2 or 3 times per week can keep people informed, promote engagement, and boost morale.
If an urgent e-mail announcement is needed, keep the message focused. Highlight only updated information and changes to existing policies and guidelines. And consider adding a brief anecdote to illustrate the staff’s creativity and resilience: a “best catch” story, for example, or a staff member who started a “commit to sit” program (spending time in the room with patients who want company but are not able to have their family in attendance).
Look to the future
COVID-19 will pass. Herd immunity will inevitably develop. The question is how quickly and at what cost. Children delivered today are being born into a society already profoundly altered by COVID-19. Some have started to call them Generation C.
Exactly what life will look like at the back end of this pandemic depends on how effectively we leverage this crisis. There are numerous opportunities to change the way we think about health care and educate the next generation of providers. These include increasing the use of telehealth and remote education, redesigning our traditional prenatal care paradigms, and reinforcing the importance of preventive medicine. This is an opportunity to put the “health” back into “health care.”
Look after yourself
Amid all the chaos and uncertainty, do not forget to take care of yourself and your family. Be calm, be kind, and be flexible. Stay safe.
- Kommenda N, Gutierrez P, Adolphe J. Coronavirus world map: which countries have the most cases and deaths? The Guardian. April 1, 2020. https://www.theguardian.com/world/2020/mar/31/coronavirus-mapped-which-countries-have-the-most-cases-and-deaths. Accessed April 1, 2020.
- Centers for Disease Control and Prevention. Coronavirus disease 2019 (COVID-19).Interim US guidance for risk assessment and public health management of healthcare personnel with potential exposure in a healthcare setting to patients with coronavirus disease (COVID-19). https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-risk-assesment-hcp.html. Accessed April 1, 2020.
- Centers for Disease Control and Prevention. Coronavirus disease 2019 (COVID-19). Evaluating and testing persons for coronavirus disease 2020 (COVID-19). https://www.cdc.gov/coronavirus/2019-nCoV/hcp/clinical-criteria.html. Accessed April 1, 2020.
While often compared with the Spanish influenza contagion of 1918, the current COVID-19 pandemic is arguably unprecedented in scale and scope, global reach, and the rate at which it has spread across the world.
Unprecedented times
The United States now has the greatest burden of COVID-19 disease worldwide.1 Although Boston has thus far been spared the full force of the disease’s impact, it is likely only a matter of time before it reaches here. To prepare for the imminent surge, we at Tufts Medical Center defined 4 short-term strategic imperatives to help guide our COVID-19 preparedness. Having a single unified strategy across our organization has helped to maintain focus and consistency in the messaging amidst all of the uncertainty. Our focus areas are outlined below.
1 Flatten the curve
This term refers to the use of “social distancing” and community isolation measures to keep the number of disease cases at a manageable level. COVID-19 is spread almost exclusively through contact with contaminated respiratory droplets. While several categories of risk have been described, the US Centers for Disease Control and Prevention (CDC) defines disease “exposure” as face-to-face contact within 6 feet of an infected individual for more than 15 minutes without wearing a mask.2 Intervening at all 3 of these touchpoints effectively reduces transmission. Interventions include limiting in-person meetings, increasing the space between individuals (both providers and patients), and routinely using personal protective equipment (PPE).
Another effective strategy is to divide frontline providers into smaller units or teams to limit cross-contamination: the inpatient team versus the outpatient team, the day team versus the night team, the “on” team versus the “off” team. If the infection lays one team low, other providers can step in until they recover and return to work.
Visitor policies should be developed and strictly implemented. Many institutions do allow one support person in labor and delivery (L&D) regardless of the patient’s COVID-19 status, although that person should not be symptomatic or COVID-19 positive. Whether to test all patients and support persons for COVID-19 on arrival at L&D remains controversial.3 At a minimum, these individuals should be screened for symptoms. Although it was a major focus of initial preventative efforts, taking a travel and exposure history is no longer informative as the virus is now endemic and community spread is common.
Initial preventative efforts focused also on high-risk patients, but routine use of PPE for all encounters clearly is more effective because of the high rate of asymptomatic shedding. The virus can survive suspended in the air for up to 2 hours following an aerosol-generating procedure (AGP) and on surfaces for several hours or even days. Practices such as regular handwashing, cleaning of exposed work surfaces, and avoiding face touching should by now be part of our everyday routine.
Institutions throughout the United States have established inpatient COVID-19 units—so-called “dirty” units—with mixed success. As the pandemic spreads and the number of patients with asymptomatic shedding increases, it is harder to determine who is and who is not infected. Cross-contamination has rendered this approach largely ineffective. Whether this will change with the introduction of rapid point-of-care testing remains to be seen.
Continue to: 2 Preserve PPE...
2 Preserve PPE
PPE use is effective in reducing transmission. This includes tier 1 PPE with or without enhanced droplet precaution (surgical mask, eye protection, gloves, yellow gown) and tier 2 PPE (tier 1 plus N95 respirators or powered air-purifying respirators [PAPR]). Given the acute PPE shortage in many parts of the country, appropriate use of PPE is critical to maintain an adequate supply. For example, tier 2 PPE is required only in the setting of an AGP. This includes intubation and, in our determination, the second stage of labor for COVID-19–positive patients and patients under investigation (PUIs); we do not employ tier 2 PPE for all patients in the second stage of labor, although some hospitals endorse this practice.
Creative solutions to the impending PPE shortage abound, such as the use of 3D printers to make face shields and novel techniques to sterilize and reuse N95 respirators.
3 Create capacity
In the absence of effective treatment for COVID-19 and with a vaccine still many months away, supportive care is critical. The pulmonary sequelae with cytokine storm and acute hypoxemia can come on quickly, require urgent mechanical ventilatory support, and take several weeks to resolve.
Our ability to create inpatient capacity to accommodate ill patients, monitor them closely, and intubate early will likely be the most critical driver of the case fatality rate. This requires deferring outpatient visits (or doing them via telemedicine), expanding intensive care unit capabilities (especially ventilator beds), and canceling elective surgeries. What constitutes “elective surgery” is not always clear. Our institution, for example, regards abortion services as essential and not elective, but this is not the case throughout the United States.
Creating capacity also refers to staffing. Where necessary, providers should be retrained and redeployed. This may require emergency credentialing of providers in areas outside their usual clinical practice and permission may be needed from the Accreditation Council for Graduate Medical Education to engage trainees outside their usual duty hours.
4 Support and protect your workforce
Everyone is anxious, and people convey their anxiety in different ways. I have found it helpful to acknowledge those feelings and provide a forum for staff to express and share their anxieties. That said, hospitals are not a democracy. While staff members should be encouraged to ask questions and voice their opinions, everyone is expected to follow protocol regarding patient care.
Celebrating small successes and finding creative ways to alleviate the stress and inject humor can help. Most institutions are using electronic conferencing platforms (such as Zoom or Microsoft Teams) to stay in touch and to continue education initiatives through interactive didactic sessions, grand rounds, morbidity and mortality conferences, and e-journal clubs. These are also a great platform for social events, such as w(h)ine and book clubs and virtual karaoke.
Since many ObGyn providers are women, the closure of day-care centers and schools is particularly challenging. Share best practices among your staff on how to address this problem, such as alternating on-call shifts or matching providers needing day care with ‘furloughed’ college students who are looking to keep busy and make a little money.
Continue to: Avoid overcommunicating...
Avoid overcommunicating
Clear, concise, and timely communication is key. This can be challenging given the rapidly evolving science of COVID-19 and the daily barrage of information from both reliable and unreliable sources. Setting up regular online meetings with your faculty 2 or 3 times per week can keep people informed, promote engagement, and boost morale.
If an urgent e-mail announcement is needed, keep the message focused. Highlight only updated information and changes to existing policies and guidelines. And consider adding a brief anecdote to illustrate the staff’s creativity and resilience: a “best catch” story, for example, or a staff member who started a “commit to sit” program (spending time in the room with patients who want company but are not able to have their family in attendance).
Look to the future
COVID-19 will pass. Herd immunity will inevitably develop. The question is how quickly and at what cost. Children delivered today are being born into a society already profoundly altered by COVID-19. Some have started to call them Generation C.
Exactly what life will look like at the back end of this pandemic depends on how effectively we leverage this crisis. There are numerous opportunities to change the way we think about health care and educate the next generation of providers. These include increasing the use of telehealth and remote education, redesigning our traditional prenatal care paradigms, and reinforcing the importance of preventive medicine. This is an opportunity to put the “health” back into “health care.”
Look after yourself
Amid all the chaos and uncertainty, do not forget to take care of yourself and your family. Be calm, be kind, and be flexible. Stay safe.
While often compared with the Spanish influenza contagion of 1918, the current COVID-19 pandemic is arguably unprecedented in scale and scope, global reach, and the rate at which it has spread across the world.
Unprecedented times
The United States now has the greatest burden of COVID-19 disease worldwide.1 Although Boston has thus far been spared the full force of the disease’s impact, it is likely only a matter of time before it reaches here. To prepare for the imminent surge, we at Tufts Medical Center defined 4 short-term strategic imperatives to help guide our COVID-19 preparedness. Having a single unified strategy across our organization has helped to maintain focus and consistency in the messaging amidst all of the uncertainty. Our focus areas are outlined below.
1 Flatten the curve
This term refers to the use of “social distancing” and community isolation measures to keep the number of disease cases at a manageable level. COVID-19 is spread almost exclusively through contact with contaminated respiratory droplets. While several categories of risk have been described, the US Centers for Disease Control and Prevention (CDC) defines disease “exposure” as face-to-face contact within 6 feet of an infected individual for more than 15 minutes without wearing a mask.2 Intervening at all 3 of these touchpoints effectively reduces transmission. Interventions include limiting in-person meetings, increasing the space between individuals (both providers and patients), and routinely using personal protective equipment (PPE).
Another effective strategy is to divide frontline providers into smaller units or teams to limit cross-contamination: the inpatient team versus the outpatient team, the day team versus the night team, the “on” team versus the “off” team. If the infection lays one team low, other providers can step in until they recover and return to work.
Visitor policies should be developed and strictly implemented. Many institutions do allow one support person in labor and delivery (L&D) regardless of the patient’s COVID-19 status, although that person should not be symptomatic or COVID-19 positive. Whether to test all patients and support persons for COVID-19 on arrival at L&D remains controversial.3 At a minimum, these individuals should be screened for symptoms. Although it was a major focus of initial preventative efforts, taking a travel and exposure history is no longer informative as the virus is now endemic and community spread is common.
Initial preventative efforts focused also on high-risk patients, but routine use of PPE for all encounters clearly is more effective because of the high rate of asymptomatic shedding. The virus can survive suspended in the air for up to 2 hours following an aerosol-generating procedure (AGP) and on surfaces for several hours or even days. Practices such as regular handwashing, cleaning of exposed work surfaces, and avoiding face touching should by now be part of our everyday routine.
Institutions throughout the United States have established inpatient COVID-19 units—so-called “dirty” units—with mixed success. As the pandemic spreads and the number of patients with asymptomatic shedding increases, it is harder to determine who is and who is not infected. Cross-contamination has rendered this approach largely ineffective. Whether this will change with the introduction of rapid point-of-care testing remains to be seen.
Continue to: 2 Preserve PPE...
2 Preserve PPE
PPE use is effective in reducing transmission. This includes tier 1 PPE with or without enhanced droplet precaution (surgical mask, eye protection, gloves, yellow gown) and tier 2 PPE (tier 1 plus N95 respirators or powered air-purifying respirators [PAPR]). Given the acute PPE shortage in many parts of the country, appropriate use of PPE is critical to maintain an adequate supply. For example, tier 2 PPE is required only in the setting of an AGP. This includes intubation and, in our determination, the second stage of labor for COVID-19–positive patients and patients under investigation (PUIs); we do not employ tier 2 PPE for all patients in the second stage of labor, although some hospitals endorse this practice.
Creative solutions to the impending PPE shortage abound, such as the use of 3D printers to make face shields and novel techniques to sterilize and reuse N95 respirators.
3 Create capacity
In the absence of effective treatment for COVID-19 and with a vaccine still many months away, supportive care is critical. The pulmonary sequelae with cytokine storm and acute hypoxemia can come on quickly, require urgent mechanical ventilatory support, and take several weeks to resolve.
Our ability to create inpatient capacity to accommodate ill patients, monitor them closely, and intubate early will likely be the most critical driver of the case fatality rate. This requires deferring outpatient visits (or doing them via telemedicine), expanding intensive care unit capabilities (especially ventilator beds), and canceling elective surgeries. What constitutes “elective surgery” is not always clear. Our institution, for example, regards abortion services as essential and not elective, but this is not the case throughout the United States.
Creating capacity also refers to staffing. Where necessary, providers should be retrained and redeployed. This may require emergency credentialing of providers in areas outside their usual clinical practice and permission may be needed from the Accreditation Council for Graduate Medical Education to engage trainees outside their usual duty hours.
4 Support and protect your workforce
Everyone is anxious, and people convey their anxiety in different ways. I have found it helpful to acknowledge those feelings and provide a forum for staff to express and share their anxieties. That said, hospitals are not a democracy. While staff members should be encouraged to ask questions and voice their opinions, everyone is expected to follow protocol regarding patient care.
Celebrating small successes and finding creative ways to alleviate the stress and inject humor can help. Most institutions are using electronic conferencing platforms (such as Zoom or Microsoft Teams) to stay in touch and to continue education initiatives through interactive didactic sessions, grand rounds, morbidity and mortality conferences, and e-journal clubs. These are also a great platform for social events, such as w(h)ine and book clubs and virtual karaoke.
Since many ObGyn providers are women, the closure of day-care centers and schools is particularly challenging. Share best practices among your staff on how to address this problem, such as alternating on-call shifts or matching providers needing day care with ‘furloughed’ college students who are looking to keep busy and make a little money.
Continue to: Avoid overcommunicating...
Avoid overcommunicating
Clear, concise, and timely communication is key. This can be challenging given the rapidly evolving science of COVID-19 and the daily barrage of information from both reliable and unreliable sources. Setting up regular online meetings with your faculty 2 or 3 times per week can keep people informed, promote engagement, and boost morale.
If an urgent e-mail announcement is needed, keep the message focused. Highlight only updated information and changes to existing policies and guidelines. And consider adding a brief anecdote to illustrate the staff’s creativity and resilience: a “best catch” story, for example, or a staff member who started a “commit to sit” program (spending time in the room with patients who want company but are not able to have their family in attendance).
Look to the future
COVID-19 will pass. Herd immunity will inevitably develop. The question is how quickly and at what cost. Children delivered today are being born into a society already profoundly altered by COVID-19. Some have started to call them Generation C.
Exactly what life will look like at the back end of this pandemic depends on how effectively we leverage this crisis. There are numerous opportunities to change the way we think about health care and educate the next generation of providers. These include increasing the use of telehealth and remote education, redesigning our traditional prenatal care paradigms, and reinforcing the importance of preventive medicine. This is an opportunity to put the “health” back into “health care.”
Look after yourself
Amid all the chaos and uncertainty, do not forget to take care of yourself and your family. Be calm, be kind, and be flexible. Stay safe.
- Kommenda N, Gutierrez P, Adolphe J. Coronavirus world map: which countries have the most cases and deaths? The Guardian. April 1, 2020. https://www.theguardian.com/world/2020/mar/31/coronavirus-mapped-which-countries-have-the-most-cases-and-deaths. Accessed April 1, 2020.
- Centers for Disease Control and Prevention. Coronavirus disease 2019 (COVID-19).Interim US guidance for risk assessment and public health management of healthcare personnel with potential exposure in a healthcare setting to patients with coronavirus disease (COVID-19). https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-risk-assesment-hcp.html. Accessed April 1, 2020.
- Centers for Disease Control and Prevention. Coronavirus disease 2019 (COVID-19). Evaluating and testing persons for coronavirus disease 2020 (COVID-19). https://www.cdc.gov/coronavirus/2019-nCoV/hcp/clinical-criteria.html. Accessed April 1, 2020.
- Kommenda N, Gutierrez P, Adolphe J. Coronavirus world map: which countries have the most cases and deaths? The Guardian. April 1, 2020. https://www.theguardian.com/world/2020/mar/31/coronavirus-mapped-which-countries-have-the-most-cases-and-deaths. Accessed April 1, 2020.
- Centers for Disease Control and Prevention. Coronavirus disease 2019 (COVID-19).Interim US guidance for risk assessment and public health management of healthcare personnel with potential exposure in a healthcare setting to patients with coronavirus disease (COVID-19). https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-risk-assesment-hcp.html. Accessed April 1, 2020.
- Centers for Disease Control and Prevention. Coronavirus disease 2019 (COVID-19). Evaluating and testing persons for coronavirus disease 2020 (COVID-19). https://www.cdc.gov/coronavirus/2019-nCoV/hcp/clinical-criteria.html. Accessed April 1, 2020.
Progesterone supplementation does not PROLONG pregnancy in women at risk for preterm birth: What do we do now?
Preterm birth (PTB) remains a significant public health concern and a major cause of newborn morbidity and mortality. In the United States, 1 in 10 babies are born preterm (< 37 weeks), and this rate has changed little in 30 years.1
In 2011, the US Food and Drug Administration (FDA) approved progesterone supplementation—specifically, α-hydroxyprogesterone caproate (17P) injection (Makena)—to prevent recurrent PTB in women with a singleton pregnancy at high risk by virtue of a prior spontaneous PTB.2 This was the first-ever FDA-approved drug for PTB prevention, and it was the first drug approved by the FDA for use in pregnancy in more than 15 years. The approval of 17P utilized the FDA's Subpart H Accelerated Approval Pathway, which applies to therapies that: 1) treat serious conditions with unmet need, and 2) demonstrate safety and efficacy on surrogate end points reasonably likely to predict clinical benefit.3
By voting their approval of 17P in 2011, the FDA affirmed that PTB was a serious condition with unmet need, that birth < 37 weeks was an accepted surrogate end point, and that there was compelling evidence of safety and benefit. The compelling evidence presented was a single, randomized, vehicle-controlled clinical trial conducted by the Maternal-Fetal Medicine Units (MFMU) Network, which showed significant reduction in recurrent PTB < 37 weeks (from 54.9% in the placebo group to 36.3% in the 17P group; P<.001; relative risk [RR], 0.66; 95% confidence interval [CI], 0.54-0.81).4
In 2017, the Society for Maternal-Fetal Medicine (SMFM) reaffirmed the use of 17P to prevent recurrent PTB and, that same year, it was estimated that 75% of eligible patients received 17P.5,6 Importantly, Subpart H approval requires one or more follow-up clinical trials confirming safety and efficacy. And the FDA has the right—the responsibility—to revisit approval if such trials are either not performed or are unfavorable.
The recently published PROLONG study by Blackwell and colleagues is this required postapproval confirmatory trial conducted to verify the clinical benefit of 17P supplementation.7
Continue to: Study design, and stunning results...
Study design, and stunning results
PROLONG (Progestin's Role in Optimizing Neonatal Gestation) was a randomized (2:1), double-blind, vehicle-controlled, multicenter international trial (2009-2018) conducted to assess the safety and efficacy of 17P injection in 1,708 women with a singleton pregnancy and one or more prior spontaneous PTBs.7 Women in the active treatment group (n = 1,130) received weekly intramuscular injections of 17P, while those in the control group (n = 578) received weekly injections of inert oil vehicle.
Results of the trial showed no significant reduction in the co-primary end points, which were PTB < 35 weeks (11.0% in the 17P group vs 11.5% in the placebo group; RR, 0.95; 95% CI, 0.71-1.26) and neonatal morbidity index (5.6% in the 17P group vs 5.0% in the placebo group; RR, 1.12; 95% CI, 0.68-1.61). There was no evidence of benefit for any subpopulation (geographic region, race, or other PTB risk factor). Maternal outcomes also were similar between the groups. No significant safety concerns were identified.
Important differences between MFMU and PROLONG trials
Strengths of the PROLONG trial include its randomized, placebo-controlled design, excellent follow-up rate, and use of a protocol that mirrored that of the MFMU trial. The primary limitation of PROLONG is that participants experienced a lower rate of PTB compared with those in the MFMU trial. The rate of PTB < 37 weeks was 54.9% in the control group of the MFMU trial compared with 21.9% in PROLONG.
Given the low rate of PTB in PROLONG, the study was underpowered for the co-primary outcomes. In addition, lower rates of PTB in PROLONG compared with in the MFMU trial likely reflected different patient populations.8 Moreover, PROLONG was an international trial. Of the 1,708 participants, most were recruited in Russia (36%) and Ukraine (25%); only 23% were from the United States. By contrast, participants in the MFMU trial were recruited from US academic medical centers. Also, participants in the MFMU trial were significantly more likely to have a short cervix, to have a history of more than one PTB, and to be African American.
Discrepant trial results create clinical quandary
In October 2019, the FDA's Bone, Reproductive and Urologic Drugs Advisory Committee voted 9-7 to withdraw approval for 17P. Committee members struggled with the conflicting data between the 2 trials and hesitated to remove a medication whose use has become standard practice. Ultimately, however, it was lack of substantial evidence of effectiveness of 17P that swayed the committee's vote. While the FDA generally follows the recommendation of an advisory committee, it is not bound to do so.
Societies' perspectives
So what are physicians and patients to do? It is possible that a small subgroup of women at extremely high risk for early PTB may benefit from 17P administration. SMFM stated: "...it is reasonable for providers to use 17-OHPC [17P] in women with a profile more representative of the very high-risk population reported in the Meis [MFMU] trial."8 Further, the American College of Obstetricians and Gynecologists (ACOG) stated in a Practice Advisory dated October 25, 2019, that "ACOG is not changing our clinical recommendations at this time... [We] will be reviewing subsequent forthcoming analyses and will issue updated clinical guidance as appropriate."9
Where we stand on 17P use going forward
17P should be available to women who previously may have benefited from its use. However, 17P should not be recommended routinely to prevent recurrent spontaneous PTB in women with one prior PTB and no other risk factors. Of note, the PROLONG trial does not change recommendations for cervical length screening. Women with a history of a prior spontaneous PTB should undergo cervical length screening to identify those individuals who may benefit from an ultrasound-indicated cerclage.
- American College of Obstetricians and Gynecologists Committee on Practice Bulletins--Obstetrics. ACOG practice bulletin no. 127: Management of preterm labor. Obstet Gynecol. 2012;119:1308-1317.
- Makena [package insert]. Waltham, MA: AMAG Pharmaceuticals, Inc; 2018. https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/021945s012lbl.pdf. Accessed November 10, 2019.
- US Food and Drug Administration. Code of Federal Regulations Title 21. Subpart H--Acceleratedapproval of new drugs for serious or life-threatening illnesses. April 1, 2019. https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?CFRPart=314&showFR=1&subpartNode=21:5.0.1.1.4.8. Accessed November 10, 2019.
- Meis PJ, Klebanoff M, Thom E, et al; for the National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Prevention of recurrent preterm delivery by 17 alpha-hydroxyprogesterone caproate. N Engl J Med. 2003;348:2379-2385.
- Society for Maternal-Fetal Medicine Publications Committee. The choice of progestogen for the prevention of preterm birth in women with singleton pregnancy and prior preterm birth. Am J Obstet Gynecol. 2017;216:B11-B13.
- Gallagher JR, Gudeman J, Heap K, et al. Understanding if, how, and why women with prior spontaneous preterm births are treated with progestogens: a national survey of obstetrician practice patterns. AJP Rep. 2018;8:e315-e324.
- Blackwell SC, Gyamfi-Bannerman C, Biggio JR Jr, et al. 17-OHPC to prevent recurrent preterm birth in singleton gestations (PROLONG study): a multicenter, international, randomized double-blind trial. Am J Perinatol. 2019. doi:10.1055/s-0039-3400227.
- Society for Maternal-Fetal Medicine Publications Committee. SMFM statement: Use of 17-alpha hydroxyprogesterone caproate for prevention of recurrent preterm birth. https://els-jbs-prod-cdn.literatumonline.com/pb/assets/raw/Health%20Advance/journals/ymob/SMFM_Statement_PRO LONG-1572023839767.pdf. Accessed November 10, 2019.
- American College of Obstetricians and Gynecologists. Practice advisory: Clinical guidance for integration of the findings of the PROLONG study: progestin's role in optimizing neonatal gestation. https://www.acog.org/Clinical-Guidance-and-Publications/Practice-Advisories/Clinical-guidance-for-integration-of-the-findings-of-The-PROLONG-study-Progestins-Role-in-Optimizing?IsMobileSet=false. Accessed November 10, 2019.
Preterm birth (PTB) remains a significant public health concern and a major cause of newborn morbidity and mortality. In the United States, 1 in 10 babies are born preterm (< 37 weeks), and this rate has changed little in 30 years.1
In 2011, the US Food and Drug Administration (FDA) approved progesterone supplementation—specifically, α-hydroxyprogesterone caproate (17P) injection (Makena)—to prevent recurrent PTB in women with a singleton pregnancy at high risk by virtue of a prior spontaneous PTB.2 This was the first-ever FDA-approved drug for PTB prevention, and it was the first drug approved by the FDA for use in pregnancy in more than 15 years. The approval of 17P utilized the FDA's Subpart H Accelerated Approval Pathway, which applies to therapies that: 1) treat serious conditions with unmet need, and 2) demonstrate safety and efficacy on surrogate end points reasonably likely to predict clinical benefit.3
By voting their approval of 17P in 2011, the FDA affirmed that PTB was a serious condition with unmet need, that birth < 37 weeks was an accepted surrogate end point, and that there was compelling evidence of safety and benefit. The compelling evidence presented was a single, randomized, vehicle-controlled clinical trial conducted by the Maternal-Fetal Medicine Units (MFMU) Network, which showed significant reduction in recurrent PTB < 37 weeks (from 54.9% in the placebo group to 36.3% in the 17P group; P<.001; relative risk [RR], 0.66; 95% confidence interval [CI], 0.54-0.81).4
In 2017, the Society for Maternal-Fetal Medicine (SMFM) reaffirmed the use of 17P to prevent recurrent PTB and, that same year, it was estimated that 75% of eligible patients received 17P.5,6 Importantly, Subpart H approval requires one or more follow-up clinical trials confirming safety and efficacy. And the FDA has the right—the responsibility—to revisit approval if such trials are either not performed or are unfavorable.
The recently published PROLONG study by Blackwell and colleagues is this required postapproval confirmatory trial conducted to verify the clinical benefit of 17P supplementation.7
Continue to: Study design, and stunning results...
Study design, and stunning results
PROLONG (Progestin's Role in Optimizing Neonatal Gestation) was a randomized (2:1), double-blind, vehicle-controlled, multicenter international trial (2009-2018) conducted to assess the safety and efficacy of 17P injection in 1,708 women with a singleton pregnancy and one or more prior spontaneous PTBs.7 Women in the active treatment group (n = 1,130) received weekly intramuscular injections of 17P, while those in the control group (n = 578) received weekly injections of inert oil vehicle.
Results of the trial showed no significant reduction in the co-primary end points, which were PTB < 35 weeks (11.0% in the 17P group vs 11.5% in the placebo group; RR, 0.95; 95% CI, 0.71-1.26) and neonatal morbidity index (5.6% in the 17P group vs 5.0% in the placebo group; RR, 1.12; 95% CI, 0.68-1.61). There was no evidence of benefit for any subpopulation (geographic region, race, or other PTB risk factor). Maternal outcomes also were similar between the groups. No significant safety concerns were identified.
Important differences between MFMU and PROLONG trials
Strengths of the PROLONG trial include its randomized, placebo-controlled design, excellent follow-up rate, and use of a protocol that mirrored that of the MFMU trial. The primary limitation of PROLONG is that participants experienced a lower rate of PTB compared with those in the MFMU trial. The rate of PTB < 37 weeks was 54.9% in the control group of the MFMU trial compared with 21.9% in PROLONG.
Given the low rate of PTB in PROLONG, the study was underpowered for the co-primary outcomes. In addition, lower rates of PTB in PROLONG compared with in the MFMU trial likely reflected different patient populations.8 Moreover, PROLONG was an international trial. Of the 1,708 participants, most were recruited in Russia (36%) and Ukraine (25%); only 23% were from the United States. By contrast, participants in the MFMU trial were recruited from US academic medical centers. Also, participants in the MFMU trial were significantly more likely to have a short cervix, to have a history of more than one PTB, and to be African American.
Discrepant trial results create clinical quandary
In October 2019, the FDA's Bone, Reproductive and Urologic Drugs Advisory Committee voted 9-7 to withdraw approval for 17P. Committee members struggled with the conflicting data between the 2 trials and hesitated to remove a medication whose use has become standard practice. Ultimately, however, it was lack of substantial evidence of effectiveness of 17P that swayed the committee's vote. While the FDA generally follows the recommendation of an advisory committee, it is not bound to do so.
Societies' perspectives
So what are physicians and patients to do? It is possible that a small subgroup of women at extremely high risk for early PTB may benefit from 17P administration. SMFM stated: "...it is reasonable for providers to use 17-OHPC [17P] in women with a profile more representative of the very high-risk population reported in the Meis [MFMU] trial."8 Further, the American College of Obstetricians and Gynecologists (ACOG) stated in a Practice Advisory dated October 25, 2019, that "ACOG is not changing our clinical recommendations at this time... [We] will be reviewing subsequent forthcoming analyses and will issue updated clinical guidance as appropriate."9
Where we stand on 17P use going forward
17P should be available to women who previously may have benefited from its use. However, 17P should not be recommended routinely to prevent recurrent spontaneous PTB in women with one prior PTB and no other risk factors. Of note, the PROLONG trial does not change recommendations for cervical length screening. Women with a history of a prior spontaneous PTB should undergo cervical length screening to identify those individuals who may benefit from an ultrasound-indicated cerclage.
Preterm birth (PTB) remains a significant public health concern and a major cause of newborn morbidity and mortality. In the United States, 1 in 10 babies are born preterm (< 37 weeks), and this rate has changed little in 30 years.1
In 2011, the US Food and Drug Administration (FDA) approved progesterone supplementation—specifically, α-hydroxyprogesterone caproate (17P) injection (Makena)—to prevent recurrent PTB in women with a singleton pregnancy at high risk by virtue of a prior spontaneous PTB.2 This was the first-ever FDA-approved drug for PTB prevention, and it was the first drug approved by the FDA for use in pregnancy in more than 15 years. The approval of 17P utilized the FDA's Subpart H Accelerated Approval Pathway, which applies to therapies that: 1) treat serious conditions with unmet need, and 2) demonstrate safety and efficacy on surrogate end points reasonably likely to predict clinical benefit.3
By voting their approval of 17P in 2011, the FDA affirmed that PTB was a serious condition with unmet need, that birth < 37 weeks was an accepted surrogate end point, and that there was compelling evidence of safety and benefit. The compelling evidence presented was a single, randomized, vehicle-controlled clinical trial conducted by the Maternal-Fetal Medicine Units (MFMU) Network, which showed significant reduction in recurrent PTB < 37 weeks (from 54.9% in the placebo group to 36.3% in the 17P group; P<.001; relative risk [RR], 0.66; 95% confidence interval [CI], 0.54-0.81).4
In 2017, the Society for Maternal-Fetal Medicine (SMFM) reaffirmed the use of 17P to prevent recurrent PTB and, that same year, it was estimated that 75% of eligible patients received 17P.5,6 Importantly, Subpart H approval requires one or more follow-up clinical trials confirming safety and efficacy. And the FDA has the right—the responsibility—to revisit approval if such trials are either not performed or are unfavorable.
The recently published PROLONG study by Blackwell and colleagues is this required postapproval confirmatory trial conducted to verify the clinical benefit of 17P supplementation.7
Continue to: Study design, and stunning results...
Study design, and stunning results
PROLONG (Progestin's Role in Optimizing Neonatal Gestation) was a randomized (2:1), double-blind, vehicle-controlled, multicenter international trial (2009-2018) conducted to assess the safety and efficacy of 17P injection in 1,708 women with a singleton pregnancy and one or more prior spontaneous PTBs.7 Women in the active treatment group (n = 1,130) received weekly intramuscular injections of 17P, while those in the control group (n = 578) received weekly injections of inert oil vehicle.
Results of the trial showed no significant reduction in the co-primary end points, which were PTB < 35 weeks (11.0% in the 17P group vs 11.5% in the placebo group; RR, 0.95; 95% CI, 0.71-1.26) and neonatal morbidity index (5.6% in the 17P group vs 5.0% in the placebo group; RR, 1.12; 95% CI, 0.68-1.61). There was no evidence of benefit for any subpopulation (geographic region, race, or other PTB risk factor). Maternal outcomes also were similar between the groups. No significant safety concerns were identified.
Important differences between MFMU and PROLONG trials
Strengths of the PROLONG trial include its randomized, placebo-controlled design, excellent follow-up rate, and use of a protocol that mirrored that of the MFMU trial. The primary limitation of PROLONG is that participants experienced a lower rate of PTB compared with those in the MFMU trial. The rate of PTB < 37 weeks was 54.9% in the control group of the MFMU trial compared with 21.9% in PROLONG.
Given the low rate of PTB in PROLONG, the study was underpowered for the co-primary outcomes. In addition, lower rates of PTB in PROLONG compared with in the MFMU trial likely reflected different patient populations.8 Moreover, PROLONG was an international trial. Of the 1,708 participants, most were recruited in Russia (36%) and Ukraine (25%); only 23% were from the United States. By contrast, participants in the MFMU trial were recruited from US academic medical centers. Also, participants in the MFMU trial were significantly more likely to have a short cervix, to have a history of more than one PTB, and to be African American.
Discrepant trial results create clinical quandary
In October 2019, the FDA's Bone, Reproductive and Urologic Drugs Advisory Committee voted 9-7 to withdraw approval for 17P. Committee members struggled with the conflicting data between the 2 trials and hesitated to remove a medication whose use has become standard practice. Ultimately, however, it was lack of substantial evidence of effectiveness of 17P that swayed the committee's vote. While the FDA generally follows the recommendation of an advisory committee, it is not bound to do so.
Societies' perspectives
So what are physicians and patients to do? It is possible that a small subgroup of women at extremely high risk for early PTB may benefit from 17P administration. SMFM stated: "...it is reasonable for providers to use 17-OHPC [17P] in women with a profile more representative of the very high-risk population reported in the Meis [MFMU] trial."8 Further, the American College of Obstetricians and Gynecologists (ACOG) stated in a Practice Advisory dated October 25, 2019, that "ACOG is not changing our clinical recommendations at this time... [We] will be reviewing subsequent forthcoming analyses and will issue updated clinical guidance as appropriate."9
Where we stand on 17P use going forward
17P should be available to women who previously may have benefited from its use. However, 17P should not be recommended routinely to prevent recurrent spontaneous PTB in women with one prior PTB and no other risk factors. Of note, the PROLONG trial does not change recommendations for cervical length screening. Women with a history of a prior spontaneous PTB should undergo cervical length screening to identify those individuals who may benefit from an ultrasound-indicated cerclage.
- American College of Obstetricians and Gynecologists Committee on Practice Bulletins--Obstetrics. ACOG practice bulletin no. 127: Management of preterm labor. Obstet Gynecol. 2012;119:1308-1317.
- Makena [package insert]. Waltham, MA: AMAG Pharmaceuticals, Inc; 2018. https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/021945s012lbl.pdf. Accessed November 10, 2019.
- US Food and Drug Administration. Code of Federal Regulations Title 21. Subpart H--Acceleratedapproval of new drugs for serious or life-threatening illnesses. April 1, 2019. https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?CFRPart=314&showFR=1&subpartNode=21:5.0.1.1.4.8. Accessed November 10, 2019.
- Meis PJ, Klebanoff M, Thom E, et al; for the National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Prevention of recurrent preterm delivery by 17 alpha-hydroxyprogesterone caproate. N Engl J Med. 2003;348:2379-2385.
- Society for Maternal-Fetal Medicine Publications Committee. The choice of progestogen for the prevention of preterm birth in women with singleton pregnancy and prior preterm birth. Am J Obstet Gynecol. 2017;216:B11-B13.
- Gallagher JR, Gudeman J, Heap K, et al. Understanding if, how, and why women with prior spontaneous preterm births are treated with progestogens: a national survey of obstetrician practice patterns. AJP Rep. 2018;8:e315-e324.
- Blackwell SC, Gyamfi-Bannerman C, Biggio JR Jr, et al. 17-OHPC to prevent recurrent preterm birth in singleton gestations (PROLONG study): a multicenter, international, randomized double-blind trial. Am J Perinatol. 2019. doi:10.1055/s-0039-3400227.
- Society for Maternal-Fetal Medicine Publications Committee. SMFM statement: Use of 17-alpha hydroxyprogesterone caproate for prevention of recurrent preterm birth. https://els-jbs-prod-cdn.literatumonline.com/pb/assets/raw/Health%20Advance/journals/ymob/SMFM_Statement_PRO LONG-1572023839767.pdf. Accessed November 10, 2019.
- American College of Obstetricians and Gynecologists. Practice advisory: Clinical guidance for integration of the findings of the PROLONG study: progestin's role in optimizing neonatal gestation. https://www.acog.org/Clinical-Guidance-and-Publications/Practice-Advisories/Clinical-guidance-for-integration-of-the-findings-of-The-PROLONG-study-Progestins-Role-in-Optimizing?IsMobileSet=false. Accessed November 10, 2019.
- American College of Obstetricians and Gynecologists Committee on Practice Bulletins--Obstetrics. ACOG practice bulletin no. 127: Management of preterm labor. Obstet Gynecol. 2012;119:1308-1317.
- Makena [package insert]. Waltham, MA: AMAG Pharmaceuticals, Inc; 2018. https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/021945s012lbl.pdf. Accessed November 10, 2019.
- US Food and Drug Administration. Code of Federal Regulations Title 21. Subpart H--Acceleratedapproval of new drugs for serious or life-threatening illnesses. April 1, 2019. https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?CFRPart=314&showFR=1&subpartNode=21:5.0.1.1.4.8. Accessed November 10, 2019.
- Meis PJ, Klebanoff M, Thom E, et al; for the National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Prevention of recurrent preterm delivery by 17 alpha-hydroxyprogesterone caproate. N Engl J Med. 2003;348:2379-2385.
- Society for Maternal-Fetal Medicine Publications Committee. The choice of progestogen for the prevention of preterm birth in women with singleton pregnancy and prior preterm birth. Am J Obstet Gynecol. 2017;216:B11-B13.
- Gallagher JR, Gudeman J, Heap K, et al. Understanding if, how, and why women with prior spontaneous preterm births are treated with progestogens: a national survey of obstetrician practice patterns. AJP Rep. 2018;8:e315-e324.
- Blackwell SC, Gyamfi-Bannerman C, Biggio JR Jr, et al. 17-OHPC to prevent recurrent preterm birth in singleton gestations (PROLONG study): a multicenter, international, randomized double-blind trial. Am J Perinatol. 2019. doi:10.1055/s-0039-3400227.
- Society for Maternal-Fetal Medicine Publications Committee. SMFM statement: Use of 17-alpha hydroxyprogesterone caproate for prevention of recurrent preterm birth. https://els-jbs-prod-cdn.literatumonline.com/pb/assets/raw/Health%20Advance/journals/ymob/SMFM_Statement_PRO LONG-1572023839767.pdf. Accessed November 10, 2019.
- American College of Obstetricians and Gynecologists. Practice advisory: Clinical guidance for integration of the findings of the PROLONG study: progestin's role in optimizing neonatal gestation. https://www.acog.org/Clinical-Guidance-and-Publications/Practice-Advisories/Clinical-guidance-for-integration-of-the-findings-of-The-PROLONG-study-Progestins-Role-in-Optimizing?IsMobileSet=false. Accessed November 10, 2019.
To AROM or not to AROM: Does early amniotomy during induction of labor increase the risk of cesarean delivery?
De Vivo V, Carbone L, Saccone G, et al. Early amniotomy after cervical ripening for induction of labor: a systematic review and meta-analysis of randomized controlled trials. Am J Obstet Gynecol. 2019. doi: 10.1016/j.ajog.2019.07.049.
EXPERT COMMENTARY
Induction of labor has doubled over the past 2 decades, with almost 25% of parturients currently undergoing induction in the United States.1 Labor induction at term is associated with perinatal outcomes similar to those with spontaneous labor, without an increase in the CD rate.1-3 Although numerous methods for cervical ripening have been evaluated, the safest and most effective method has yet to be determined.2
Amniotomy—or artificial rupture of membranes (AROM)—has long been used as a technique for labor induction and for augmentation in women in spontaneous labor. Purported benefits include an increased responsiveness to exogenous oxytocin, decreased interval to delivery, and an increased likelihood of spontaneous vaginal delivery. Risks of amniotomy include injury to the fetus or surrounding tissues, bleeding, nonreassuring fetal testing, cord prolapse, and prolonged rupture of membranes (defined as longer than 18 hours), which is a risk factor for intra-amniotic infection.
The optimal timing of amniotomy is not known. The recent study by De Vivo and colleagues was designed to better understand the risk/benefit ratio of early amniotomy after cervical ripening in women undergoing induction of labor.
Details of the study
The authors conducted a systematic review and meta-analysis that included 1,273 women in 4 randomized controlled trials to determine the effectiveness of routine early amniotomy versus late amniotomy/spontaneous rupture of membranes after cervical ripening (with either a Foley catheter or prostaglandins) in women with a singleton vertex fetus undergoing induction of labor in the term or late preterm period.
Early amniotomy was defined as AROM “soon after cervical ripening” (cases); late amniotomy was defined as AROM after the active phase of labor or spontaneous rupture of membranes (controls).
The primary outcome was the incidence of CD. Secondary outcomes included the overall length of labor, latency from induction to delivery, and neonatal morbidity (a composite of birth weight, Apgar scores, meconium-stained amniotic fluid, neonatal sepsis, need for resuscitation, and admission to the neonatal intensive care unit).
Continue to: Findings...
Findings. Women randomly assigned to early amniotomy had a similar risk of CD compared with controls (31.1% vs 30.9% [relative risk (RR), 1.05; 95% confidence interval (CI), 0.71–1.56]) and a shorter interval from induction to delivery of about 5 hours (mean difference, -4.95 hours [95% CI, -8.12 to -1.78]).
There was no difference in any of the secondary outcome measures, although the number of events was small. Specifically, there was no significant difference in rates of chorioamnionitis between the early and late amniotomy cohorts (7.3% vs 4.8% [RR, 1.47; 95% CI, 0.95–2.28]).
Study strengths and limitations
This is the first systematic review to evaluate early versus late amniotomy after cervical ripening for induction of labor. “Systematic review and meta-analysis” is not synonymous with a review of the literature. It has its own methodology and is regarded as original research. A strength of this study is that it was performed by a highly credible team who followed established Cochrane and PRISMA methodological and reporting guidelines.
Study weaknesses include the fact that the meta-analysis contained a relatively small number of trials and study participants. It was significantly underpowered to address issues related to neonatal outcome. The 4 trials included were highly variable in terms of maternal parity and indications for labor induction and CD. The definition of “early amniotomy” was inconsistent, and the overall rate of CD varied greatly among the studies (7.9%–41.1%). Multiple pregnancies were excluded. Taken together, these findings may have limited generalizability.
This is the first systematic review to evaluate early versus late amniotomy/spontaneous rupture of membranes after cervical ripening for induction of labor. The study results suggest that amniotomy soon after cervical ripening does not change the likelihood of CD, but it does shorten the induction-to-delivery interval by around 5 hours. Prior studies have shown that early amniotomy in women in spontaneous labor decreases time to delivery by an average of 3 hours.4 Now we know that this is true also of early amniotomy following cervical ripening for induction of labor.
A number of questions still remain before early amniotomy is introduced into routine practice: Does group B streptococcus colonization status matter? Does this practice increase the risk of chorioamnionitis? At this time, it seems most prudent to individualize amniotomy timing based on a woman's obstetric history, indication for induction, and response to cervical ripening.
ERROL R. NORWITZ, MD, PHD, MBA, AND DIANA KOLETTIS, MD
- American College of Obstetricians and Gynecologists Committee on Practice Bulletins--Obstetrics. ACOG practice bulletin no. 107: Induction of labor. Obstet Gynecol. 2009;114(2 pt 1):386-397.
- Saccone G, Berghella V. Induction of labor at full term in uncomplicated singleton gestations: a systematic review and metaanalysis of randomized controlled trials. Am J Obstet Gynecol. 2015;213:629-636.
- Grobman WA, Rice MM, Reddy UM, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Labor induction versus expectant management in low-risk nulliparous women. N Engl J Med. 2018;379:513-523.
- Frigoletto FD Jr, Lieberman E, Lang JM, et al. A clinical trial of active management of labor. N Engl J Med. 1995;333:745-750.
De Vivo V, Carbone L, Saccone G, et al. Early amniotomy after cervical ripening for induction of labor: a systematic review and meta-analysis of randomized controlled trials. Am J Obstet Gynecol. 2019. doi: 10.1016/j.ajog.2019.07.049.
EXPERT COMMENTARY
Induction of labor has doubled over the past 2 decades, with almost 25% of parturients currently undergoing induction in the United States.1 Labor induction at term is associated with perinatal outcomes similar to those with spontaneous labor, without an increase in the CD rate.1-3 Although numerous methods for cervical ripening have been evaluated, the safest and most effective method has yet to be determined.2
Amniotomy—or artificial rupture of membranes (AROM)—has long been used as a technique for labor induction and for augmentation in women in spontaneous labor. Purported benefits include an increased responsiveness to exogenous oxytocin, decreased interval to delivery, and an increased likelihood of spontaneous vaginal delivery. Risks of amniotomy include injury to the fetus or surrounding tissues, bleeding, nonreassuring fetal testing, cord prolapse, and prolonged rupture of membranes (defined as longer than 18 hours), which is a risk factor for intra-amniotic infection.
The optimal timing of amniotomy is not known. The recent study by De Vivo and colleagues was designed to better understand the risk/benefit ratio of early amniotomy after cervical ripening in women undergoing induction of labor.
Details of the study
The authors conducted a systematic review and meta-analysis that included 1,273 women in 4 randomized controlled trials to determine the effectiveness of routine early amniotomy versus late amniotomy/spontaneous rupture of membranes after cervical ripening (with either a Foley catheter or prostaglandins) in women with a singleton vertex fetus undergoing induction of labor in the term or late preterm period.
Early amniotomy was defined as AROM “soon after cervical ripening” (cases); late amniotomy was defined as AROM after the active phase of labor or spontaneous rupture of membranes (controls).
The primary outcome was the incidence of CD. Secondary outcomes included the overall length of labor, latency from induction to delivery, and neonatal morbidity (a composite of birth weight, Apgar scores, meconium-stained amniotic fluid, neonatal sepsis, need for resuscitation, and admission to the neonatal intensive care unit).
Continue to: Findings...
Findings. Women randomly assigned to early amniotomy had a similar risk of CD compared with controls (31.1% vs 30.9% [relative risk (RR), 1.05; 95% confidence interval (CI), 0.71–1.56]) and a shorter interval from induction to delivery of about 5 hours (mean difference, -4.95 hours [95% CI, -8.12 to -1.78]).
There was no difference in any of the secondary outcome measures, although the number of events was small. Specifically, there was no significant difference in rates of chorioamnionitis between the early and late amniotomy cohorts (7.3% vs 4.8% [RR, 1.47; 95% CI, 0.95–2.28]).
Study strengths and limitations
This is the first systematic review to evaluate early versus late amniotomy after cervical ripening for induction of labor. “Systematic review and meta-analysis” is not synonymous with a review of the literature. It has its own methodology and is regarded as original research. A strength of this study is that it was performed by a highly credible team who followed established Cochrane and PRISMA methodological and reporting guidelines.
Study weaknesses include the fact that the meta-analysis contained a relatively small number of trials and study participants. It was significantly underpowered to address issues related to neonatal outcome. The 4 trials included were highly variable in terms of maternal parity and indications for labor induction and CD. The definition of “early amniotomy” was inconsistent, and the overall rate of CD varied greatly among the studies (7.9%–41.1%). Multiple pregnancies were excluded. Taken together, these findings may have limited generalizability.
This is the first systematic review to evaluate early versus late amniotomy/spontaneous rupture of membranes after cervical ripening for induction of labor. The study results suggest that amniotomy soon after cervical ripening does not change the likelihood of CD, but it does shorten the induction-to-delivery interval by around 5 hours. Prior studies have shown that early amniotomy in women in spontaneous labor decreases time to delivery by an average of 3 hours.4 Now we know that this is true also of early amniotomy following cervical ripening for induction of labor.
A number of questions still remain before early amniotomy is introduced into routine practice: Does group B streptococcus colonization status matter? Does this practice increase the risk of chorioamnionitis? At this time, it seems most prudent to individualize amniotomy timing based on a woman's obstetric history, indication for induction, and response to cervical ripening.
ERROL R. NORWITZ, MD, PHD, MBA, AND DIANA KOLETTIS, MD
De Vivo V, Carbone L, Saccone G, et al. Early amniotomy after cervical ripening for induction of labor: a systematic review and meta-analysis of randomized controlled trials. Am J Obstet Gynecol. 2019. doi: 10.1016/j.ajog.2019.07.049.
EXPERT COMMENTARY
Induction of labor has doubled over the past 2 decades, with almost 25% of parturients currently undergoing induction in the United States.1 Labor induction at term is associated with perinatal outcomes similar to those with spontaneous labor, without an increase in the CD rate.1-3 Although numerous methods for cervical ripening have been evaluated, the safest and most effective method has yet to be determined.2
Amniotomy—or artificial rupture of membranes (AROM)—has long been used as a technique for labor induction and for augmentation in women in spontaneous labor. Purported benefits include an increased responsiveness to exogenous oxytocin, decreased interval to delivery, and an increased likelihood of spontaneous vaginal delivery. Risks of amniotomy include injury to the fetus or surrounding tissues, bleeding, nonreassuring fetal testing, cord prolapse, and prolonged rupture of membranes (defined as longer than 18 hours), which is a risk factor for intra-amniotic infection.
The optimal timing of amniotomy is not known. The recent study by De Vivo and colleagues was designed to better understand the risk/benefit ratio of early amniotomy after cervical ripening in women undergoing induction of labor.
Details of the study
The authors conducted a systematic review and meta-analysis that included 1,273 women in 4 randomized controlled trials to determine the effectiveness of routine early amniotomy versus late amniotomy/spontaneous rupture of membranes after cervical ripening (with either a Foley catheter or prostaglandins) in women with a singleton vertex fetus undergoing induction of labor in the term or late preterm period.
Early amniotomy was defined as AROM “soon after cervical ripening” (cases); late amniotomy was defined as AROM after the active phase of labor or spontaneous rupture of membranes (controls).
The primary outcome was the incidence of CD. Secondary outcomes included the overall length of labor, latency from induction to delivery, and neonatal morbidity (a composite of birth weight, Apgar scores, meconium-stained amniotic fluid, neonatal sepsis, need for resuscitation, and admission to the neonatal intensive care unit).
Continue to: Findings...
Findings. Women randomly assigned to early amniotomy had a similar risk of CD compared with controls (31.1% vs 30.9% [relative risk (RR), 1.05; 95% confidence interval (CI), 0.71–1.56]) and a shorter interval from induction to delivery of about 5 hours (mean difference, -4.95 hours [95% CI, -8.12 to -1.78]).
There was no difference in any of the secondary outcome measures, although the number of events was small. Specifically, there was no significant difference in rates of chorioamnionitis between the early and late amniotomy cohorts (7.3% vs 4.8% [RR, 1.47; 95% CI, 0.95–2.28]).
Study strengths and limitations
This is the first systematic review to evaluate early versus late amniotomy after cervical ripening for induction of labor. “Systematic review and meta-analysis” is not synonymous with a review of the literature. It has its own methodology and is regarded as original research. A strength of this study is that it was performed by a highly credible team who followed established Cochrane and PRISMA methodological and reporting guidelines.
Study weaknesses include the fact that the meta-analysis contained a relatively small number of trials and study participants. It was significantly underpowered to address issues related to neonatal outcome. The 4 trials included were highly variable in terms of maternal parity and indications for labor induction and CD. The definition of “early amniotomy” was inconsistent, and the overall rate of CD varied greatly among the studies (7.9%–41.1%). Multiple pregnancies were excluded. Taken together, these findings may have limited generalizability.
This is the first systematic review to evaluate early versus late amniotomy/spontaneous rupture of membranes after cervical ripening for induction of labor. The study results suggest that amniotomy soon after cervical ripening does not change the likelihood of CD, but it does shorten the induction-to-delivery interval by around 5 hours. Prior studies have shown that early amniotomy in women in spontaneous labor decreases time to delivery by an average of 3 hours.4 Now we know that this is true also of early amniotomy following cervical ripening for induction of labor.
A number of questions still remain before early amniotomy is introduced into routine practice: Does group B streptococcus colonization status matter? Does this practice increase the risk of chorioamnionitis? At this time, it seems most prudent to individualize amniotomy timing based on a woman's obstetric history, indication for induction, and response to cervical ripening.
ERROL R. NORWITZ, MD, PHD, MBA, AND DIANA KOLETTIS, MD
- American College of Obstetricians and Gynecologists Committee on Practice Bulletins--Obstetrics. ACOG practice bulletin no. 107: Induction of labor. Obstet Gynecol. 2009;114(2 pt 1):386-397.
- Saccone G, Berghella V. Induction of labor at full term in uncomplicated singleton gestations: a systematic review and metaanalysis of randomized controlled trials. Am J Obstet Gynecol. 2015;213:629-636.
- Grobman WA, Rice MM, Reddy UM, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Labor induction versus expectant management in low-risk nulliparous women. N Engl J Med. 2018;379:513-523.
- Frigoletto FD Jr, Lieberman E, Lang JM, et al. A clinical trial of active management of labor. N Engl J Med. 1995;333:745-750.
- American College of Obstetricians and Gynecologists Committee on Practice Bulletins--Obstetrics. ACOG practice bulletin no. 107: Induction of labor. Obstet Gynecol. 2009;114(2 pt 1):386-397.
- Saccone G, Berghella V. Induction of labor at full term in uncomplicated singleton gestations: a systematic review and metaanalysis of randomized controlled trials. Am J Obstet Gynecol. 2015;213:629-636.
- Grobman WA, Rice MM, Reddy UM, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Labor induction versus expectant management in low-risk nulliparous women. N Engl J Med. 2018;379:513-523.
- Frigoletto FD Jr, Lieberman E, Lang JM, et al. A clinical trial of active management of labor. N Engl J Med. 1995;333:745-750.
Is the vaginal or buccal route more effective when administering prostaglandins for cervical ripening at term?
Haas DM, Daggy J, Flannery KM, et al. A comparison of vaginal versus buccal misoprostol for cervical ripening in women for labor induction at term (the IMPROVE trial): a triple masked randomized controlled trial. Am J Obstet Gynecol. 2019. doi:10.1016/j.ajog.2019.04.037.
EXPERT COMMENTARY
Cervical ripening is routine practice in women undergoing induction of labor who have an unfavorable cervical examination.1 This is because generating contractions against a long thick cervix is more likely to lead to failed induction and cesarean delivery. Cervical ripening can be achieved using mechanical or pharmacologic methods.
Misoprostol (a prostaglandin E1 [PGE1] analog) is approved by the US Food and Drug Administration for the treatment of peptic ulcer disease, but it also is widely used off-label for cervical ripening, partly due to its low cost. Misoprostol’s optimal dosing regimen and route of administration are not known. The IMPROVE trial was designed to address this knowledge gap, specifically to compare the efficacy and safety of VM versus BM in women undergoing labor induction at term.
Details of the study
The IMPROVE trial was a prospective, randomized, noninferiority, triple-masked, placebo-controlled trial of 300 women with a singleton vertex fetus requiring cervical ripening for induction of labor at term.2 Enrolled women were randomly assigned to VM or BM (same dosing regimen) and to a matching placebo administered via the opposite route.
Primary outcomes included time-to-vaginal-delivery from first dose, which was reduced in VM vs BM (20.1 vs 28.1 hours; P = .006), and urgent cesarean delivery for nonreassuring fetal testing, which was similarly reduced in VM (3.3% vs 9.5%; P = .33). These differences persisted after controlling for covariates. There was also a greater difference seen in multiparous versus nulliparous women.
Secondary outcomes also favored VM over BM, including more vaginal deliverieswithin 24 hours, fewer doses to achieve active labor, and a lower maximum dose of oxytocin.
Overall cesarean delivery rates were similar in the 2 groups (VM, 15.8%; BM, 22.3%; P = .15). There were no significant differences in other delivery characteristics or in maternal or fetal adverse events.
While a number of studies have evaluated the risk of cesarean delivery (CD) with the use of cervical ripening agents by different routes of administration, Handal-Orefice and colleagues studied this outcome specifically in a predominantly overweight population at a tertiary care center.1
The retrospective study included 276 women, of whom 91% had a body mass index (BMI) of 25 kg/m2 or more and 61% had a BMI of 30 kg/m2 or more at the time of delivery.
For cervical ripening, 138 women received vaginal misoprostol (25 µg) and 138 received oral misoprostol (50 µg). The frequency of CD (the primary study outcome) was significantly higher with oral compared with vaginal misoprostol use (32% vs 21%; P = .04). When the analysis was adjusted for age, BMI, parity, indication for induction, and Foley catheter use, the risk of CD remained significantly higher for the oral misoprostol group (adjusted odds ratio [aOR], 2.01; 95% confidence interval [CI], 1.07-3.76).
Other key findings:
- frequency of CD among nulliparous women: 41% in the oral misoprostol group, 28% in the vaginal misoprostol group (aOR, 2.79; 95% CI, 1.26-6.19)
- time to vaginal delivery: 41 hours for the oral misoprostol group, 31 hours for the vaginal misoprostol group (P = .01)
- uterine tachysystole: 11% in the oral misoprostol group, 20% in the vaginal misoprostol group (P = .04).
The authors noted that the strengths of the study, including the racial and ethnic diversity of the population (72% of women were of either black or Hispanic race or ethnicity), the commonly used doses of misoprostol, and the performance of inductions outside a research protocol, add to the generalizability of the results.
Reference
1. Handal-Orefice R, Friedman AM, Chouinard SM, et al. Oral or vaginal misoprostol for labor induction and cesarean delivery risk. Obstet Gynecol. 2019. doi:10.1097/AOG.0000000000003274.
Continue to: Study strengths and limitations...
Study strengths and limitations
The IMPROVE trial had a triple-blinded study design with an intention-to-treat paradigm and good follow-up. There was also standardization of PGE1 administration criteria, which was consistent with the American College of Obstetricians and Gynecologists standards of care. Results were similar to those of prior studies regarding rates of tachysystole, urgent cesarean delivery, and vaginal delivery.
The study has good generalizability as it included both elective and medically indicated inductions; however, patients with ruptured membranes were excluded. Although there was no difference in the overall cesarean delivery rates, the study was underpowered to look at this outcome. The authors included a patient satisfaction survey, but this is hard to interpret since study participants all received tablets orally and vaginally. The study did not address efficacy of VM versus BM administration at different doses or time intervals.
Labor induction has doubled over the past 2 decades, with almost 25% of parturients currently undergoing induction in the United States.3 This number is likely to increase given recent data suggesting that routine induction at 39 weeks may significantly decrease cesarean delivery rates.4 It is critical, therefore, that we identify the optimal technique for cervical ripening, including the ideal dosing regimen and route of administration. Results of the IMPROVE trial suggest that vaginal administration of misoprostol (25 μg initial dose, 50 μg subsequent doses) may be superior to the buccal route, with more rapid vaginal delivery, more vaginal deliveries within 24 hours, and fewer urgent cesareans for nonreassuring fetal testing (although the overall cesarean delivery rate was not significantly different).
ERROL R. NORWITZ, MD, PHD, MBA; JULIE M. STONE, MD
- American College of Obstetricians and Gynecologists. ACOG practice bulletin no. 107. Induction of labor. Obstet Gynecol. 2009;114(2 pt 1):386-397.
- Haas DM, Daggy J, Flannery KM, et al. A comparison of vaginal versus buccal misoprostol for cervical ripening in women for labor induction at term (the IMPROVE trial): a triple masked randomized controlled trial. Am J Obstet Gynecol. 2019. doi:10.1016/j.ajog.2019.04.037.
- Martin JA, Hamilton BE, Osterman M, et al. Births: final data for 2016. Nat Vital Stat Rep. 2018;67:1-55.
- Grobman WA, Rice MM, Reddy UM, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal–Fetal Medicine Units Network. Labor induction versus expectant management in low-risk nulliparous women. N Engl J Med. 2018;379:513-523.
Haas DM, Daggy J, Flannery KM, et al. A comparison of vaginal versus buccal misoprostol for cervical ripening in women for labor induction at term (the IMPROVE trial): a triple masked randomized controlled trial. Am J Obstet Gynecol. 2019. doi:10.1016/j.ajog.2019.04.037.
EXPERT COMMENTARY
Cervical ripening is routine practice in women undergoing induction of labor who have an unfavorable cervical examination.1 This is because generating contractions against a long thick cervix is more likely to lead to failed induction and cesarean delivery. Cervical ripening can be achieved using mechanical or pharmacologic methods.
Misoprostol (a prostaglandin E1 [PGE1] analog) is approved by the US Food and Drug Administration for the treatment of peptic ulcer disease, but it also is widely used off-label for cervical ripening, partly due to its low cost. Misoprostol’s optimal dosing regimen and route of administration are not known. The IMPROVE trial was designed to address this knowledge gap, specifically to compare the efficacy and safety of VM versus BM in women undergoing labor induction at term.
Details of the study
The IMPROVE trial was a prospective, randomized, noninferiority, triple-masked, placebo-controlled trial of 300 women with a singleton vertex fetus requiring cervical ripening for induction of labor at term.2 Enrolled women were randomly assigned to VM or BM (same dosing regimen) and to a matching placebo administered via the opposite route.
Primary outcomes included time-to-vaginal-delivery from first dose, which was reduced in VM vs BM (20.1 vs 28.1 hours; P = .006), and urgent cesarean delivery for nonreassuring fetal testing, which was similarly reduced in VM (3.3% vs 9.5%; P = .33). These differences persisted after controlling for covariates. There was also a greater difference seen in multiparous versus nulliparous women.
Secondary outcomes also favored VM over BM, including more vaginal deliverieswithin 24 hours, fewer doses to achieve active labor, and a lower maximum dose of oxytocin.
Overall cesarean delivery rates were similar in the 2 groups (VM, 15.8%; BM, 22.3%; P = .15). There were no significant differences in other delivery characteristics or in maternal or fetal adverse events.
While a number of studies have evaluated the risk of cesarean delivery (CD) with the use of cervical ripening agents by different routes of administration, Handal-Orefice and colleagues studied this outcome specifically in a predominantly overweight population at a tertiary care center.1
The retrospective study included 276 women, of whom 91% had a body mass index (BMI) of 25 kg/m2 or more and 61% had a BMI of 30 kg/m2 or more at the time of delivery.
For cervical ripening, 138 women received vaginal misoprostol (25 µg) and 138 received oral misoprostol (50 µg). The frequency of CD (the primary study outcome) was significantly higher with oral compared with vaginal misoprostol use (32% vs 21%; P = .04). When the analysis was adjusted for age, BMI, parity, indication for induction, and Foley catheter use, the risk of CD remained significantly higher for the oral misoprostol group (adjusted odds ratio [aOR], 2.01; 95% confidence interval [CI], 1.07-3.76).
Other key findings:
- frequency of CD among nulliparous women: 41% in the oral misoprostol group, 28% in the vaginal misoprostol group (aOR, 2.79; 95% CI, 1.26-6.19)
- time to vaginal delivery: 41 hours for the oral misoprostol group, 31 hours for the vaginal misoprostol group (P = .01)
- uterine tachysystole: 11% in the oral misoprostol group, 20% in the vaginal misoprostol group (P = .04).
The authors noted that the strengths of the study, including the racial and ethnic diversity of the population (72% of women were of either black or Hispanic race or ethnicity), the commonly used doses of misoprostol, and the performance of inductions outside a research protocol, add to the generalizability of the results.
Reference
1. Handal-Orefice R, Friedman AM, Chouinard SM, et al. Oral or vaginal misoprostol for labor induction and cesarean delivery risk. Obstet Gynecol. 2019. doi:10.1097/AOG.0000000000003274.
Continue to: Study strengths and limitations...
Study strengths and limitations
The IMPROVE trial had a triple-blinded study design with an intention-to-treat paradigm and good follow-up. There was also standardization of PGE1 administration criteria, which was consistent with the American College of Obstetricians and Gynecologists standards of care. Results were similar to those of prior studies regarding rates of tachysystole, urgent cesarean delivery, and vaginal delivery.
The study has good generalizability as it included both elective and medically indicated inductions; however, patients with ruptured membranes were excluded. Although there was no difference in the overall cesarean delivery rates, the study was underpowered to look at this outcome. The authors included a patient satisfaction survey, but this is hard to interpret since study participants all received tablets orally and vaginally. The study did not address efficacy of VM versus BM administration at different doses or time intervals.
Labor induction has doubled over the past 2 decades, with almost 25% of parturients currently undergoing induction in the United States.3 This number is likely to increase given recent data suggesting that routine induction at 39 weeks may significantly decrease cesarean delivery rates.4 It is critical, therefore, that we identify the optimal technique for cervical ripening, including the ideal dosing regimen and route of administration. Results of the IMPROVE trial suggest that vaginal administration of misoprostol (25 μg initial dose, 50 μg subsequent doses) may be superior to the buccal route, with more rapid vaginal delivery, more vaginal deliveries within 24 hours, and fewer urgent cesareans for nonreassuring fetal testing (although the overall cesarean delivery rate was not significantly different).
ERROL R. NORWITZ, MD, PHD, MBA; JULIE M. STONE, MD
Haas DM, Daggy J, Flannery KM, et al. A comparison of vaginal versus buccal misoprostol for cervical ripening in women for labor induction at term (the IMPROVE trial): a triple masked randomized controlled trial. Am J Obstet Gynecol. 2019. doi:10.1016/j.ajog.2019.04.037.
EXPERT COMMENTARY
Cervical ripening is routine practice in women undergoing induction of labor who have an unfavorable cervical examination.1 This is because generating contractions against a long thick cervix is more likely to lead to failed induction and cesarean delivery. Cervical ripening can be achieved using mechanical or pharmacologic methods.
Misoprostol (a prostaglandin E1 [PGE1] analog) is approved by the US Food and Drug Administration for the treatment of peptic ulcer disease, but it also is widely used off-label for cervical ripening, partly due to its low cost. Misoprostol’s optimal dosing regimen and route of administration are not known. The IMPROVE trial was designed to address this knowledge gap, specifically to compare the efficacy and safety of VM versus BM in women undergoing labor induction at term.
Details of the study
The IMPROVE trial was a prospective, randomized, noninferiority, triple-masked, placebo-controlled trial of 300 women with a singleton vertex fetus requiring cervical ripening for induction of labor at term.2 Enrolled women were randomly assigned to VM or BM (same dosing regimen) and to a matching placebo administered via the opposite route.
Primary outcomes included time-to-vaginal-delivery from first dose, which was reduced in VM vs BM (20.1 vs 28.1 hours; P = .006), and urgent cesarean delivery for nonreassuring fetal testing, which was similarly reduced in VM (3.3% vs 9.5%; P = .33). These differences persisted after controlling for covariates. There was also a greater difference seen in multiparous versus nulliparous women.
Secondary outcomes also favored VM over BM, including more vaginal deliverieswithin 24 hours, fewer doses to achieve active labor, and a lower maximum dose of oxytocin.
Overall cesarean delivery rates were similar in the 2 groups (VM, 15.8%; BM, 22.3%; P = .15). There were no significant differences in other delivery characteristics or in maternal or fetal adverse events.
While a number of studies have evaluated the risk of cesarean delivery (CD) with the use of cervical ripening agents by different routes of administration, Handal-Orefice and colleagues studied this outcome specifically in a predominantly overweight population at a tertiary care center.1
The retrospective study included 276 women, of whom 91% had a body mass index (BMI) of 25 kg/m2 or more and 61% had a BMI of 30 kg/m2 or more at the time of delivery.
For cervical ripening, 138 women received vaginal misoprostol (25 µg) and 138 received oral misoprostol (50 µg). The frequency of CD (the primary study outcome) was significantly higher with oral compared with vaginal misoprostol use (32% vs 21%; P = .04). When the analysis was adjusted for age, BMI, parity, indication for induction, and Foley catheter use, the risk of CD remained significantly higher for the oral misoprostol group (adjusted odds ratio [aOR], 2.01; 95% confidence interval [CI], 1.07-3.76).
Other key findings:
- frequency of CD among nulliparous women: 41% in the oral misoprostol group, 28% in the vaginal misoprostol group (aOR, 2.79; 95% CI, 1.26-6.19)
- time to vaginal delivery: 41 hours for the oral misoprostol group, 31 hours for the vaginal misoprostol group (P = .01)
- uterine tachysystole: 11% in the oral misoprostol group, 20% in the vaginal misoprostol group (P = .04).
The authors noted that the strengths of the study, including the racial and ethnic diversity of the population (72% of women were of either black or Hispanic race or ethnicity), the commonly used doses of misoprostol, and the performance of inductions outside a research protocol, add to the generalizability of the results.
Reference
1. Handal-Orefice R, Friedman AM, Chouinard SM, et al. Oral or vaginal misoprostol for labor induction and cesarean delivery risk. Obstet Gynecol. 2019. doi:10.1097/AOG.0000000000003274.
Continue to: Study strengths and limitations...
Study strengths and limitations
The IMPROVE trial had a triple-blinded study design with an intention-to-treat paradigm and good follow-up. There was also standardization of PGE1 administration criteria, which was consistent with the American College of Obstetricians and Gynecologists standards of care. Results were similar to those of prior studies regarding rates of tachysystole, urgent cesarean delivery, and vaginal delivery.
The study has good generalizability as it included both elective and medically indicated inductions; however, patients with ruptured membranes were excluded. Although there was no difference in the overall cesarean delivery rates, the study was underpowered to look at this outcome. The authors included a patient satisfaction survey, but this is hard to interpret since study participants all received tablets orally and vaginally. The study did not address efficacy of VM versus BM administration at different doses or time intervals.
Labor induction has doubled over the past 2 decades, with almost 25% of parturients currently undergoing induction in the United States.3 This number is likely to increase given recent data suggesting that routine induction at 39 weeks may significantly decrease cesarean delivery rates.4 It is critical, therefore, that we identify the optimal technique for cervical ripening, including the ideal dosing regimen and route of administration. Results of the IMPROVE trial suggest that vaginal administration of misoprostol (25 μg initial dose, 50 μg subsequent doses) may be superior to the buccal route, with more rapid vaginal delivery, more vaginal deliveries within 24 hours, and fewer urgent cesareans for nonreassuring fetal testing (although the overall cesarean delivery rate was not significantly different).
ERROL R. NORWITZ, MD, PHD, MBA; JULIE M. STONE, MD
- American College of Obstetricians and Gynecologists. ACOG practice bulletin no. 107. Induction of labor. Obstet Gynecol. 2009;114(2 pt 1):386-397.
- Haas DM, Daggy J, Flannery KM, et al. A comparison of vaginal versus buccal misoprostol for cervical ripening in women for labor induction at term (the IMPROVE trial): a triple masked randomized controlled trial. Am J Obstet Gynecol. 2019. doi:10.1016/j.ajog.2019.04.037.
- Martin JA, Hamilton BE, Osterman M, et al. Births: final data for 2016. Nat Vital Stat Rep. 2018;67:1-55.
- Grobman WA, Rice MM, Reddy UM, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal–Fetal Medicine Units Network. Labor induction versus expectant management in low-risk nulliparous women. N Engl J Med. 2018;379:513-523.
- American College of Obstetricians and Gynecologists. ACOG practice bulletin no. 107. Induction of labor. Obstet Gynecol. 2009;114(2 pt 1):386-397.
- Haas DM, Daggy J, Flannery KM, et al. A comparison of vaginal versus buccal misoprostol for cervical ripening in women for labor induction at term (the IMPROVE trial): a triple masked randomized controlled trial. Am J Obstet Gynecol. 2019. doi:10.1016/j.ajog.2019.04.037.
- Martin JA, Hamilton BE, Osterman M, et al. Births: final data for 2016. Nat Vital Stat Rep. 2018;67:1-55.
- Grobman WA, Rice MM, Reddy UM, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal–Fetal Medicine Units Network. Labor induction versus expectant management in low-risk nulliparous women. N Engl J Med. 2018;379:513-523.
Are sweeping efforts to reduce primary CD rates associated with an increase in maternal or neonatal AEs?
EXPERT COMMENTARY
Main EK, Chang SC, Cape V, et al. Safety assessment of a large-scale improvement collaborative to reduce nulliparous cesarean delivery rates. Obstet Gynecol. 2019;133:613-623.
Cesarean delivery can be lifesaving for both mother and infant. When compared with successful vaginal delivery, however, CD is associated with higher maternal complication rates (including excessive blood loss requiring blood product transfusion, infectious morbidity, and venous thromboembolic events), longer hospital length of stay, and higher cost. While the optimal CD rate is not well defined, it is generally accepted that the CD rate in the United States is excessively high. As such, efforts to reduce the CD rate should be encouraged, but not at the expense of patient safety.
Details about the study
In keeping with the dictum that the most important CD to prevent is the first one, the California Maternal Quality Care Collaborative (CMQCC) in 2016 introduced a large-scale quality improvement project designed to reduce nulliparous, term, singleton, vertex (NTSV) CDs across the state. This bundle included education around joint guidelines issued by the American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine on reducing primary CDs,1 introduction of a CMQCC toolkit, increased nursing labor support, and monthly meetings to share best practices across all collaborating sites. The NTSV CD rate in these hospitals did decrease from 29.3% in 2015 to 25.0% in 2017 (adjusted odds ratio, 0.76; 95% confidence interval, 0.73–0.78).
Whether or not implementation of the bundle resulted in an inappropriate delay in indicated CDs and, as such, in an increase in maternal or neonatal morbidity is not known. To address this issue, Main and colleagues collected cross-sectional data from more than 50 hospitals with more than 119,000 deliveries throughout California and measured rates of chorioamnionitis, blood transfusions, third- or fourth-degree perineal lacerations, operative vaginal delivery, severe unexpected newborn complications, and 5-minute Apgar scores of less than 5. None of the 6 safety measures showed any difference when comparing 2017 (after implementation of the CMQCC bundle) to 2015 (before implementation), suggesting that patient safety was not compromised significantly.
Study strengths and weaknesses
Strengths of this study include its large sample size and multicenter design with inclusion of a variety of collaborating hospitals. Earlier studies examining the effect of standardized protocols to reduce CD rates have been largely underpowered and conducted at single institutions.2-6 Moreover, results have been mixed, with some studies reporting an increase in maternal/neonatal adverse events,2-4 while others suggesting an improvement in select newborn quality outcome metrics.5 The current study provides reassurance to providers and institutions employing strategies to reduce NTSV CD rates that such efforts are safe.
Continue to: This study has several limitations...
This study has several limitations. Data collection relied on birth certificate and discharge diagnoses without a robust quality audit. As such, ascertainment bias, random error, and undercounting cannot be excluded. Although the population was heterogeneous, most women had more than a high school education and private insurance, and only 1 in 5 were obese. Whether these findings are generalizable to other areas within the United States is not known.
All reasonable efforts to decrease the CD rate in the United States should be encouraged, with particular attention paid to avoiding the first CD. However, this should not be done at the expense of patient safety. Large-scale quality improvement initiatives, similar to CMQCC efforts in California in 2016, appear to be one such strategy. Other successful strategies may include, for example, routine induction of labor for all low-risk nulliparous women at 39 weeks' gestation.7 The current report suggests that implementing a large-scale quality improvement initiative to reduce the primary CD rate can likely be done safely, without a significant increase in maternal or neonatal morbidity.
- American College of Obstetricians and Gynecologists; Society for Maternal-Fetal Medicine. ACOG Obstetric care consensus no. 1: safe prevention of the primary cesarean delivery. Obstet Gynecol. 2014;123:693-711.
- Rosenbloom JI, Stout MJ, Tuuli MG, et al. New labor management guidelines and changes in cesarean delivery patterns. Am J Obstet Gynecol. 2017;217:689.e1-689.e8.
- Vadnais MA, Hacker MR, Shah NT, et al. Quality improvement initiatives lead to reduction in nulliparous term singleton vertex cesarean delivery rate. Jt Comm J Qual Patient Saf. 2017;43:53-61.
- Zipori Y, Grunwald O, Ginsberg Y, et al. The impact of extending the second stage of labor to prevent primary cesarean delivery on maternal and neonatal outcomes. Am J Obstet Gynecol. 2019; 220:191.e1-191.e7.
- Thuillier C, Roy S, Peyronnet V, et al. Impact of recommended changes in labor management for prevention of the primary cesarean delivery. Am J Obstet Gynecol. 2018;218:341.e1-341.e9.
- Gimovsky AC, Berghella V. Randomized controlled trial of prolonged second stage: extending the time limit vs usual guidelines. Am J Obstet Gynecol. 2016;214:361.e1-361.e6.
- Grobman WA, Rice MM, Reddy UM, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Labor induction versus expectant management in low-risk nulliparous women. N Engl J Med. 2018;379:513-523.
EXPERT COMMENTARY
Main EK, Chang SC, Cape V, et al. Safety assessment of a large-scale improvement collaborative to reduce nulliparous cesarean delivery rates. Obstet Gynecol. 2019;133:613-623.
Cesarean delivery can be lifesaving for both mother and infant. When compared with successful vaginal delivery, however, CD is associated with higher maternal complication rates (including excessive blood loss requiring blood product transfusion, infectious morbidity, and venous thromboembolic events), longer hospital length of stay, and higher cost. While the optimal CD rate is not well defined, it is generally accepted that the CD rate in the United States is excessively high. As such, efforts to reduce the CD rate should be encouraged, but not at the expense of patient safety.
Details about the study
In keeping with the dictum that the most important CD to prevent is the first one, the California Maternal Quality Care Collaborative (CMQCC) in 2016 introduced a large-scale quality improvement project designed to reduce nulliparous, term, singleton, vertex (NTSV) CDs across the state. This bundle included education around joint guidelines issued by the American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine on reducing primary CDs,1 introduction of a CMQCC toolkit, increased nursing labor support, and monthly meetings to share best practices across all collaborating sites. The NTSV CD rate in these hospitals did decrease from 29.3% in 2015 to 25.0% in 2017 (adjusted odds ratio, 0.76; 95% confidence interval, 0.73–0.78).
Whether or not implementation of the bundle resulted in an inappropriate delay in indicated CDs and, as such, in an increase in maternal or neonatal morbidity is not known. To address this issue, Main and colleagues collected cross-sectional data from more than 50 hospitals with more than 119,000 deliveries throughout California and measured rates of chorioamnionitis, blood transfusions, third- or fourth-degree perineal lacerations, operative vaginal delivery, severe unexpected newborn complications, and 5-minute Apgar scores of less than 5. None of the 6 safety measures showed any difference when comparing 2017 (after implementation of the CMQCC bundle) to 2015 (before implementation), suggesting that patient safety was not compromised significantly.
Study strengths and weaknesses
Strengths of this study include its large sample size and multicenter design with inclusion of a variety of collaborating hospitals. Earlier studies examining the effect of standardized protocols to reduce CD rates have been largely underpowered and conducted at single institutions.2-6 Moreover, results have been mixed, with some studies reporting an increase in maternal/neonatal adverse events,2-4 while others suggesting an improvement in select newborn quality outcome metrics.5 The current study provides reassurance to providers and institutions employing strategies to reduce NTSV CD rates that such efforts are safe.
Continue to: This study has several limitations...
This study has several limitations. Data collection relied on birth certificate and discharge diagnoses without a robust quality audit. As such, ascertainment bias, random error, and undercounting cannot be excluded. Although the population was heterogeneous, most women had more than a high school education and private insurance, and only 1 in 5 were obese. Whether these findings are generalizable to other areas within the United States is not known.
All reasonable efforts to decrease the CD rate in the United States should be encouraged, with particular attention paid to avoiding the first CD. However, this should not be done at the expense of patient safety. Large-scale quality improvement initiatives, similar to CMQCC efforts in California in 2016, appear to be one such strategy. Other successful strategies may include, for example, routine induction of labor for all low-risk nulliparous women at 39 weeks' gestation.7 The current report suggests that implementing a large-scale quality improvement initiative to reduce the primary CD rate can likely be done safely, without a significant increase in maternal or neonatal morbidity.
EXPERT COMMENTARY
Main EK, Chang SC, Cape V, et al. Safety assessment of a large-scale improvement collaborative to reduce nulliparous cesarean delivery rates. Obstet Gynecol. 2019;133:613-623.
Cesarean delivery can be lifesaving for both mother and infant. When compared with successful vaginal delivery, however, CD is associated with higher maternal complication rates (including excessive blood loss requiring blood product transfusion, infectious morbidity, and venous thromboembolic events), longer hospital length of stay, and higher cost. While the optimal CD rate is not well defined, it is generally accepted that the CD rate in the United States is excessively high. As such, efforts to reduce the CD rate should be encouraged, but not at the expense of patient safety.
Details about the study
In keeping with the dictum that the most important CD to prevent is the first one, the California Maternal Quality Care Collaborative (CMQCC) in 2016 introduced a large-scale quality improvement project designed to reduce nulliparous, term, singleton, vertex (NTSV) CDs across the state. This bundle included education around joint guidelines issued by the American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine on reducing primary CDs,1 introduction of a CMQCC toolkit, increased nursing labor support, and monthly meetings to share best practices across all collaborating sites. The NTSV CD rate in these hospitals did decrease from 29.3% in 2015 to 25.0% in 2017 (adjusted odds ratio, 0.76; 95% confidence interval, 0.73–0.78).
Whether or not implementation of the bundle resulted in an inappropriate delay in indicated CDs and, as such, in an increase in maternal or neonatal morbidity is not known. To address this issue, Main and colleagues collected cross-sectional data from more than 50 hospitals with more than 119,000 deliveries throughout California and measured rates of chorioamnionitis, blood transfusions, third- or fourth-degree perineal lacerations, operative vaginal delivery, severe unexpected newborn complications, and 5-minute Apgar scores of less than 5. None of the 6 safety measures showed any difference when comparing 2017 (after implementation of the CMQCC bundle) to 2015 (before implementation), suggesting that patient safety was not compromised significantly.
Study strengths and weaknesses
Strengths of this study include its large sample size and multicenter design with inclusion of a variety of collaborating hospitals. Earlier studies examining the effect of standardized protocols to reduce CD rates have been largely underpowered and conducted at single institutions.2-6 Moreover, results have been mixed, with some studies reporting an increase in maternal/neonatal adverse events,2-4 while others suggesting an improvement in select newborn quality outcome metrics.5 The current study provides reassurance to providers and institutions employing strategies to reduce NTSV CD rates that such efforts are safe.
Continue to: This study has several limitations...
This study has several limitations. Data collection relied on birth certificate and discharge diagnoses without a robust quality audit. As such, ascertainment bias, random error, and undercounting cannot be excluded. Although the population was heterogeneous, most women had more than a high school education and private insurance, and only 1 in 5 were obese. Whether these findings are generalizable to other areas within the United States is not known.
All reasonable efforts to decrease the CD rate in the United States should be encouraged, with particular attention paid to avoiding the first CD. However, this should not be done at the expense of patient safety. Large-scale quality improvement initiatives, similar to CMQCC efforts in California in 2016, appear to be one such strategy. Other successful strategies may include, for example, routine induction of labor for all low-risk nulliparous women at 39 weeks' gestation.7 The current report suggests that implementing a large-scale quality improvement initiative to reduce the primary CD rate can likely be done safely, without a significant increase in maternal or neonatal morbidity.
- American College of Obstetricians and Gynecologists; Society for Maternal-Fetal Medicine. ACOG Obstetric care consensus no. 1: safe prevention of the primary cesarean delivery. Obstet Gynecol. 2014;123:693-711.
- Rosenbloom JI, Stout MJ, Tuuli MG, et al. New labor management guidelines and changes in cesarean delivery patterns. Am J Obstet Gynecol. 2017;217:689.e1-689.e8.
- Vadnais MA, Hacker MR, Shah NT, et al. Quality improvement initiatives lead to reduction in nulliparous term singleton vertex cesarean delivery rate. Jt Comm J Qual Patient Saf. 2017;43:53-61.
- Zipori Y, Grunwald O, Ginsberg Y, et al. The impact of extending the second stage of labor to prevent primary cesarean delivery on maternal and neonatal outcomes. Am J Obstet Gynecol. 2019; 220:191.e1-191.e7.
- Thuillier C, Roy S, Peyronnet V, et al. Impact of recommended changes in labor management for prevention of the primary cesarean delivery. Am J Obstet Gynecol. 2018;218:341.e1-341.e9.
- Gimovsky AC, Berghella V. Randomized controlled trial of prolonged second stage: extending the time limit vs usual guidelines. Am J Obstet Gynecol. 2016;214:361.e1-361.e6.
- Grobman WA, Rice MM, Reddy UM, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Labor induction versus expectant management in low-risk nulliparous women. N Engl J Med. 2018;379:513-523.
- American College of Obstetricians and Gynecologists; Society for Maternal-Fetal Medicine. ACOG Obstetric care consensus no. 1: safe prevention of the primary cesarean delivery. Obstet Gynecol. 2014;123:693-711.
- Rosenbloom JI, Stout MJ, Tuuli MG, et al. New labor management guidelines and changes in cesarean delivery patterns. Am J Obstet Gynecol. 2017;217:689.e1-689.e8.
- Vadnais MA, Hacker MR, Shah NT, et al. Quality improvement initiatives lead to reduction in nulliparous term singleton vertex cesarean delivery rate. Jt Comm J Qual Patient Saf. 2017;43:53-61.
- Zipori Y, Grunwald O, Ginsberg Y, et al. The impact of extending the second stage of labor to prevent primary cesarean delivery on maternal and neonatal outcomes. Am J Obstet Gynecol. 2019; 220:191.e1-191.e7.
- Thuillier C, Roy S, Peyronnet V, et al. Impact of recommended changes in labor management for prevention of the primary cesarean delivery. Am J Obstet Gynecol. 2018;218:341.e1-341.e9.
- Gimovsky AC, Berghella V. Randomized controlled trial of prolonged second stage: extending the time limit vs usual guidelines. Am J Obstet Gynecol. 2016;214:361.e1-361.e6.
- Grobman WA, Rice MM, Reddy UM, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Labor induction versus expectant management in low-risk nulliparous women. N Engl J Med. 2018;379:513-523.
STOP using instruments to assist with delivery of the head at cesarean
Rates of cesarean delivery in the second stage of labor have increased dramatically over the past few years.1 Compared with cesarean delivery prior to labor, second-stage labor cesarean is associated with a higher risk to both the mother and the fetus; risks include excessive bleeding, lower uterine segment extensions, injuries to the maternal ureters or bladder, and injury to the fetus.2−4 The risk is increased even further if the fetal head is deeply impacted in the pelvis. What can we do to avoid and manage such situations?
Anticipate an impacted fetal headThe true incidence of an impacted fetal head at the time of cesarean is not known, although a number of risk factors have been described (TABLE). Obstetric care providers should be aware of these risk factors and anticipate the likelihood of a difficult delivery of the fetal head at cesarean.
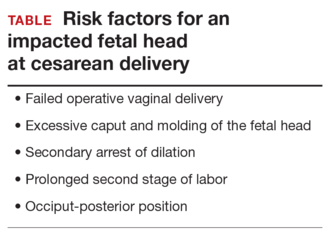
Options for managing an impacted fetal head at cesareanSeveral techniques have been reported in the literature for managing the delivery of a deeply engaged head, including:
Using an assistant to push the fetus’s head up using a hand in the vagina (“push” technique). This can cause trauma to the fetus, since the force required to push the fetus up from below is uncontrolled.5,6
The reverse breech extraction (“pull” technique) involves pulling the infant out feet first through the uterine incision.7
Use of an instrument. The most common instrument used is a vacuum extractor,8 although a number of other devices have been developed, including the Murless fetal head extractor (an instrument with a hinged shaft and sliding collar lock),9 the C-Snorkel impacted fetal head release device (the device’s tip contains ventilation ports to facilitate airflow and release of the vacuum/suction created by the impacted fetal head),10 and the Fetal Pillow (a balloon device inserted in the vagina and inflated with sterile saline to disimpact an engaged fetal head before cesarean delivery).11
While all of these techniques can cause injury to the mother and the fetus, available data favor use of the reverse breech extraction (pull) technique, since it is associated with fewer maternal risks, including lower rates of uterine incision extension, infection, and postpartum hemorrhage and a shorter operative time.12−18
Stop use of vacuum to deliver the fetal head at cesarean
Placement of a vacuum can be effective in assisting with delivery of the fetal head at cesarean. For this reason, vacuum-assisted deliveries at cesarean are becoming more common. While the rate of complications caused by vacuum extraction of the fetal head at cesarean is not known, injuries have been reported.19,20 As such, routine use of vacuum extraction at the time of cesarean delivery cannot be recommended.
Start disengaging the fetal head prior to cesarean
One useful technique in planning a cesarean in the second stage of labor or when an impacted fetal head is anticipated is to disengage the fetal head vaginally prior to skin incision. This can be done in the delivery room or in the operating room immediately prior to surgery with the help of an assistant.
While supporting the patient’s legs, the assistant inserts a hand into the vagina and pushes upward on the fetal head with gentle, sustained effort. The assistant should use a cupped hand or the palm of the hand while attempting to both elevate and flex the fetal head. It is best to avoid using 1 or 2 fingers to elevate the head, as this may cause excessive pressure at a single point and lead to injury, such as a skull fracture (FIGURE). The assistant should disengage his or her hand only when the operating surgeon is able to reach down and secure the fetal head from above.
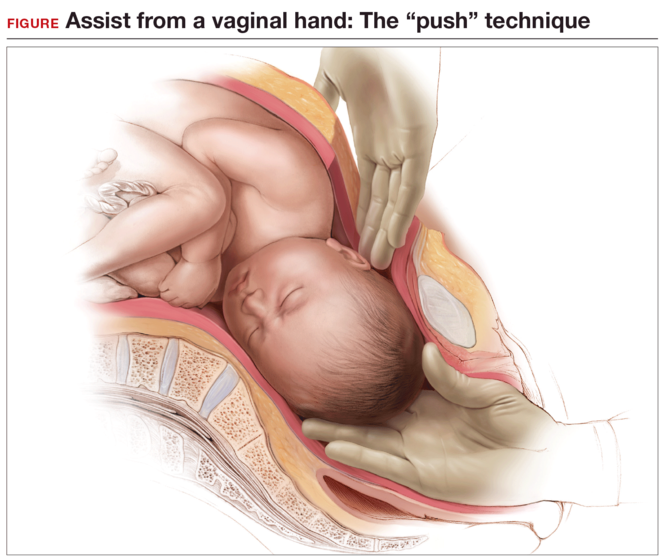
Elevating the fetal head prior to skin incision offers 3 major advantages:
- It avoids the embarrassing situation of having the fetus deliver vaginally before it can be pulled out through the abdominal incision. Although rare, this has been known to happen, because the dense regional anesthesia further relaxes the pelvic floor musculature, leading to flexion and rotation of the fetal head, which then descends and delivers. Performing a final bimanual examination in the operating room after the establishment of surgical level anesthesia and immediately prior to skin incision will avoid this situation.
- It elevates the fetal head, thereby creating additional space between the bony pelvis and fetal presenting part for the provider’s hand to fit. This helps minimize injury to the fetus and to the maternal soft tissues at the time of cesarean.
- Lastly, it provides additional information about the extent to which the fetal head is impacted in the pelvis and may influence decision making around the time of cesarean. For example, if the fetal head were deeply impacted in the pelvis and could not be disimpacted vaginally, the surgeon may choose to make a different uterine incision (such as a low vertical hysterotomy), administer a uterine relaxant (an inhaled anesthetic agent or nitric oxide), ask for additional instrumentation, and/or ask an assistant to be ready to elevate the fetal head vaginally should this be necessary.21
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Spencer C, Murphy D, Bewley S. Caesarean delivery in the second stage of labour. BMJ. 2006;333(7569):613–614.
- Häger RM, Daltviet AK, Hofoss D, et al. Complications of cesarean deliveries: rates and risk factors. Am J Obstet Gynecol. 2004;190(2):428–434.
- Murphy DJ, Liebling RE, Verity L, Swingler R, Patel R. Early maternal and neonatal morbidity associated with operative delivery in second stage of labour: a cohort study. Lancet. 2001;358(9289):1203–1207.
- Pergialiotis V, Vlachos DG, Rodolakis A, Haidopoulos D, Thomakos N, Vlachos GD. First versus second stage C/S maternal and neonatal morbidity: a systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2014;175:15–24.
- Lippert TH. Bimanual delivery of the fetal head at cesarean section with the fetal head in the midcavity. Arch Gynecol. 1983;234(1):59–60.
- Landesman R, Graber EA. Abdominovaginal delivery: modification of the cesarean section operation to facilitate delivery of the impacted head. Am J Obstet Gynecol. 1984;148(6):707–710.
- Fong YF, Arulkumaran S. Breech extraction—an alternative method of delivering a deeply engaged head at cesarean section. Int J Gynaecol Obstet. 1997;56(2):183–184.
- Arad I, Linder N, Bercovici B. Vacuum extraction at cesarean section—neonatal outcome. J Perinat Med. 1986;14(2):137–140.
- Murless BC. Lower-segment caesarean section; a new head extractor. BMJ. 1948;1(4564):1234.
- C-Snorkle impacted fetal head release device. Clinical Innovations website. http://clinicalinnovations.com /portfolio-items/c-snorkel/. Accessed July 22, 2016.
- Seal SL, Dey A, Barman SC, Kamilya G, Mukherji J, Onwude JL. Randomized controlled trial of elevation of the fetal head with a fetal pillow during cesarean delivery at full cervical dilatation. Int J Gynaecol Obstet. 2016;133(2):178–182.
- Fasubaa OB, Ezechi OC, Orji EO, et al. Delivery of the impacted head of the fetus at caesarean section after prolonged obstructed labour: a randomised comparative study of two methods. J Obstet Gynaecol. 2002;22(4):375–378.
- Levy R, Chernomoretz T, Appelman Z, Levin D, Or Y, Hagay ZJ. Head pushing versus reverse breech extraction in cases of impacted fetal head during Cesarean section. Eur J Obstet Gynecol Reprod Biol. 2005;121(1):24–26.
- Chopra S, Bagga R, Keepanasseril A, Jain V, Kalra J, Suri V. Disengagement of the deeply engaged fetal head during cesarean section in advanced labor: conventional method versus reverse breech extraction. Acta Obstet Gynecol Scand. 2009;88(10):1163–1166.
- Veisi F, Zangeneh M, Malekkhosravi S, Rezavand N. Comparison of “push” and “pull” methods for impacted fetal head extraction during cesarean delivery. Int J Gynaecol Obstet. 2012;118(1):4–6.
- Bastani P, Pourabolghasem S, Abbasalizadeh F, Motvalli L. ComparisonColor/Black of neonatal and maternal outcomes associated with head-pushing and head-pulling methods for impacted fetal head extraction during cesarean delivery. Int J Gynaecol Obstet. 2012;118(1):1–3.
- Waterfall H, Grivell RM, Dodd JM. Techniques for assisting difficult delivery at caesarean section. Cochrane Database Syst Rev. 2016;1:CD004944.
- Jeve YB, Navti OB, Konje JC. Comparison of techniques used to deliver a deeply impacted fetal head at full dilation: a systematic review and meta-analysis. BJOG. 2016;123(3): 337–345.
- Clark SL, Vines VL, Belfort MA. Fetal injury associated with routine vacuum use during cesarean delivery. Am J Obstet Gynecol. 2008;198(4):e4.
- Fareeduddin R, Schifrin BS. Subgaleal hemorrhage after the use of a vacuum extractor during elective cesarean delivery: a case report. J Reprod Med. 2008;53(10):809–810.
- Barbieri RL. Difficult fetal extraction at cesarean delivery: What should you do? OBG Manag. 2012;24(1):8–12.
Rates of cesarean delivery in the second stage of labor have increased dramatically over the past few years.1 Compared with cesarean delivery prior to labor, second-stage labor cesarean is associated with a higher risk to both the mother and the fetus; risks include excessive bleeding, lower uterine segment extensions, injuries to the maternal ureters or bladder, and injury to the fetus.2−4 The risk is increased even further if the fetal head is deeply impacted in the pelvis. What can we do to avoid and manage such situations?
Anticipate an impacted fetal headThe true incidence of an impacted fetal head at the time of cesarean is not known, although a number of risk factors have been described (TABLE). Obstetric care providers should be aware of these risk factors and anticipate the likelihood of a difficult delivery of the fetal head at cesarean.
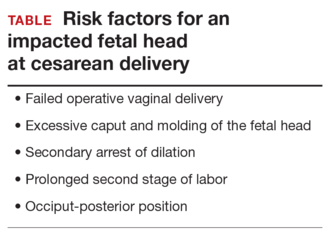
Options for managing an impacted fetal head at cesareanSeveral techniques have been reported in the literature for managing the delivery of a deeply engaged head, including:
Using an assistant to push the fetus’s head up using a hand in the vagina (“push” technique). This can cause trauma to the fetus, since the force required to push the fetus up from below is uncontrolled.5,6
The reverse breech extraction (“pull” technique) involves pulling the infant out feet first through the uterine incision.7
Use of an instrument. The most common instrument used is a vacuum extractor,8 although a number of other devices have been developed, including the Murless fetal head extractor (an instrument with a hinged shaft and sliding collar lock),9 the C-Snorkel impacted fetal head release device (the device’s tip contains ventilation ports to facilitate airflow and release of the vacuum/suction created by the impacted fetal head),10 and the Fetal Pillow (a balloon device inserted in the vagina and inflated with sterile saline to disimpact an engaged fetal head before cesarean delivery).11
While all of these techniques can cause injury to the mother and the fetus, available data favor use of the reverse breech extraction (pull) technique, since it is associated with fewer maternal risks, including lower rates of uterine incision extension, infection, and postpartum hemorrhage and a shorter operative time.12−18
Stop use of vacuum to deliver the fetal head at cesarean
Placement of a vacuum can be effective in assisting with delivery of the fetal head at cesarean. For this reason, vacuum-assisted deliveries at cesarean are becoming more common. While the rate of complications caused by vacuum extraction of the fetal head at cesarean is not known, injuries have been reported.19,20 As such, routine use of vacuum extraction at the time of cesarean delivery cannot be recommended.
Start disengaging the fetal head prior to cesarean
One useful technique in planning a cesarean in the second stage of labor or when an impacted fetal head is anticipated is to disengage the fetal head vaginally prior to skin incision. This can be done in the delivery room or in the operating room immediately prior to surgery with the help of an assistant.
While supporting the patient’s legs, the assistant inserts a hand into the vagina and pushes upward on the fetal head with gentle, sustained effort. The assistant should use a cupped hand or the palm of the hand while attempting to both elevate and flex the fetal head. It is best to avoid using 1 or 2 fingers to elevate the head, as this may cause excessive pressure at a single point and lead to injury, such as a skull fracture (FIGURE). The assistant should disengage his or her hand only when the operating surgeon is able to reach down and secure the fetal head from above.
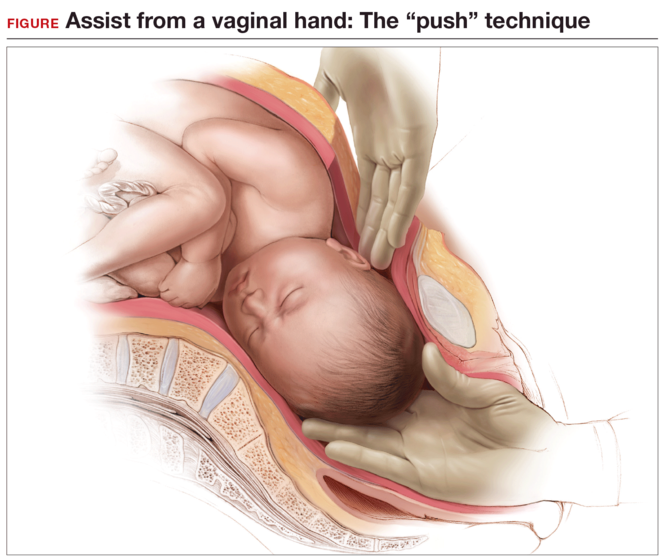
Elevating the fetal head prior to skin incision offers 3 major advantages:
- It avoids the embarrassing situation of having the fetus deliver vaginally before it can be pulled out through the abdominal incision. Although rare, this has been known to happen, because the dense regional anesthesia further relaxes the pelvic floor musculature, leading to flexion and rotation of the fetal head, which then descends and delivers. Performing a final bimanual examination in the operating room after the establishment of surgical level anesthesia and immediately prior to skin incision will avoid this situation.
- It elevates the fetal head, thereby creating additional space between the bony pelvis and fetal presenting part for the provider’s hand to fit. This helps minimize injury to the fetus and to the maternal soft tissues at the time of cesarean.
- Lastly, it provides additional information about the extent to which the fetal head is impacted in the pelvis and may influence decision making around the time of cesarean. For example, if the fetal head were deeply impacted in the pelvis and could not be disimpacted vaginally, the surgeon may choose to make a different uterine incision (such as a low vertical hysterotomy), administer a uterine relaxant (an inhaled anesthetic agent or nitric oxide), ask for additional instrumentation, and/or ask an assistant to be ready to elevate the fetal head vaginally should this be necessary.21
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Rates of cesarean delivery in the second stage of labor have increased dramatically over the past few years.1 Compared with cesarean delivery prior to labor, second-stage labor cesarean is associated with a higher risk to both the mother and the fetus; risks include excessive bleeding, lower uterine segment extensions, injuries to the maternal ureters or bladder, and injury to the fetus.2−4 The risk is increased even further if the fetal head is deeply impacted in the pelvis. What can we do to avoid and manage such situations?
Anticipate an impacted fetal headThe true incidence of an impacted fetal head at the time of cesarean is not known, although a number of risk factors have been described (TABLE). Obstetric care providers should be aware of these risk factors and anticipate the likelihood of a difficult delivery of the fetal head at cesarean.
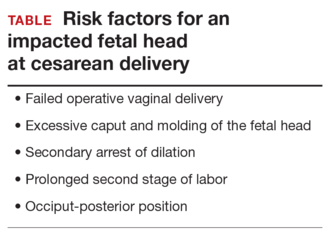
Options for managing an impacted fetal head at cesareanSeveral techniques have been reported in the literature for managing the delivery of a deeply engaged head, including:
Using an assistant to push the fetus’s head up using a hand in the vagina (“push” technique). This can cause trauma to the fetus, since the force required to push the fetus up from below is uncontrolled.5,6
The reverse breech extraction (“pull” technique) involves pulling the infant out feet first through the uterine incision.7
Use of an instrument. The most common instrument used is a vacuum extractor,8 although a number of other devices have been developed, including the Murless fetal head extractor (an instrument with a hinged shaft and sliding collar lock),9 the C-Snorkel impacted fetal head release device (the device’s tip contains ventilation ports to facilitate airflow and release of the vacuum/suction created by the impacted fetal head),10 and the Fetal Pillow (a balloon device inserted in the vagina and inflated with sterile saline to disimpact an engaged fetal head before cesarean delivery).11
While all of these techniques can cause injury to the mother and the fetus, available data favor use of the reverse breech extraction (pull) technique, since it is associated with fewer maternal risks, including lower rates of uterine incision extension, infection, and postpartum hemorrhage and a shorter operative time.12−18
Stop use of vacuum to deliver the fetal head at cesarean
Placement of a vacuum can be effective in assisting with delivery of the fetal head at cesarean. For this reason, vacuum-assisted deliveries at cesarean are becoming more common. While the rate of complications caused by vacuum extraction of the fetal head at cesarean is not known, injuries have been reported.19,20 As such, routine use of vacuum extraction at the time of cesarean delivery cannot be recommended.
Start disengaging the fetal head prior to cesarean
One useful technique in planning a cesarean in the second stage of labor or when an impacted fetal head is anticipated is to disengage the fetal head vaginally prior to skin incision. This can be done in the delivery room or in the operating room immediately prior to surgery with the help of an assistant.
While supporting the patient’s legs, the assistant inserts a hand into the vagina and pushes upward on the fetal head with gentle, sustained effort. The assistant should use a cupped hand or the palm of the hand while attempting to both elevate and flex the fetal head. It is best to avoid using 1 or 2 fingers to elevate the head, as this may cause excessive pressure at a single point and lead to injury, such as a skull fracture (FIGURE). The assistant should disengage his or her hand only when the operating surgeon is able to reach down and secure the fetal head from above.
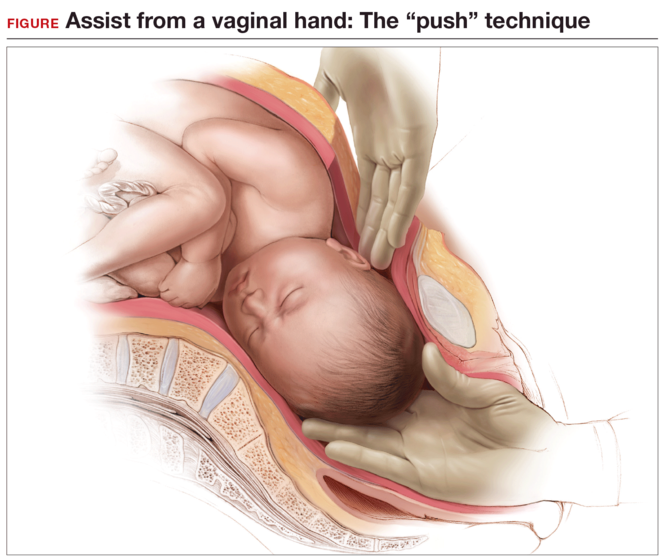
Elevating the fetal head prior to skin incision offers 3 major advantages:
- It avoids the embarrassing situation of having the fetus deliver vaginally before it can be pulled out through the abdominal incision. Although rare, this has been known to happen, because the dense regional anesthesia further relaxes the pelvic floor musculature, leading to flexion and rotation of the fetal head, which then descends and delivers. Performing a final bimanual examination in the operating room after the establishment of surgical level anesthesia and immediately prior to skin incision will avoid this situation.
- It elevates the fetal head, thereby creating additional space between the bony pelvis and fetal presenting part for the provider’s hand to fit. This helps minimize injury to the fetus and to the maternal soft tissues at the time of cesarean.
- Lastly, it provides additional information about the extent to which the fetal head is impacted in the pelvis and may influence decision making around the time of cesarean. For example, if the fetal head were deeply impacted in the pelvis and could not be disimpacted vaginally, the surgeon may choose to make a different uterine incision (such as a low vertical hysterotomy), administer a uterine relaxant (an inhaled anesthetic agent or nitric oxide), ask for additional instrumentation, and/or ask an assistant to be ready to elevate the fetal head vaginally should this be necessary.21
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Spencer C, Murphy D, Bewley S. Caesarean delivery in the second stage of labour. BMJ. 2006;333(7569):613–614.
- Häger RM, Daltviet AK, Hofoss D, et al. Complications of cesarean deliveries: rates and risk factors. Am J Obstet Gynecol. 2004;190(2):428–434.
- Murphy DJ, Liebling RE, Verity L, Swingler R, Patel R. Early maternal and neonatal morbidity associated with operative delivery in second stage of labour: a cohort study. Lancet. 2001;358(9289):1203–1207.
- Pergialiotis V, Vlachos DG, Rodolakis A, Haidopoulos D, Thomakos N, Vlachos GD. First versus second stage C/S maternal and neonatal morbidity: a systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2014;175:15–24.
- Lippert TH. Bimanual delivery of the fetal head at cesarean section with the fetal head in the midcavity. Arch Gynecol. 1983;234(1):59–60.
- Landesman R, Graber EA. Abdominovaginal delivery: modification of the cesarean section operation to facilitate delivery of the impacted head. Am J Obstet Gynecol. 1984;148(6):707–710.
- Fong YF, Arulkumaran S. Breech extraction—an alternative method of delivering a deeply engaged head at cesarean section. Int J Gynaecol Obstet. 1997;56(2):183–184.
- Arad I, Linder N, Bercovici B. Vacuum extraction at cesarean section—neonatal outcome. J Perinat Med. 1986;14(2):137–140.
- Murless BC. Lower-segment caesarean section; a new head extractor. BMJ. 1948;1(4564):1234.
- C-Snorkle impacted fetal head release device. Clinical Innovations website. http://clinicalinnovations.com /portfolio-items/c-snorkel/. Accessed July 22, 2016.
- Seal SL, Dey A, Barman SC, Kamilya G, Mukherji J, Onwude JL. Randomized controlled trial of elevation of the fetal head with a fetal pillow during cesarean delivery at full cervical dilatation. Int J Gynaecol Obstet. 2016;133(2):178–182.
- Fasubaa OB, Ezechi OC, Orji EO, et al. Delivery of the impacted head of the fetus at caesarean section after prolonged obstructed labour: a randomised comparative study of two methods. J Obstet Gynaecol. 2002;22(4):375–378.
- Levy R, Chernomoretz T, Appelman Z, Levin D, Or Y, Hagay ZJ. Head pushing versus reverse breech extraction in cases of impacted fetal head during Cesarean section. Eur J Obstet Gynecol Reprod Biol. 2005;121(1):24–26.
- Chopra S, Bagga R, Keepanasseril A, Jain V, Kalra J, Suri V. Disengagement of the deeply engaged fetal head during cesarean section in advanced labor: conventional method versus reverse breech extraction. Acta Obstet Gynecol Scand. 2009;88(10):1163–1166.
- Veisi F, Zangeneh M, Malekkhosravi S, Rezavand N. Comparison of “push” and “pull” methods for impacted fetal head extraction during cesarean delivery. Int J Gynaecol Obstet. 2012;118(1):4–6.
- Bastani P, Pourabolghasem S, Abbasalizadeh F, Motvalli L. ComparisonColor/Black of neonatal and maternal outcomes associated with head-pushing and head-pulling methods for impacted fetal head extraction during cesarean delivery. Int J Gynaecol Obstet. 2012;118(1):1–3.
- Waterfall H, Grivell RM, Dodd JM. Techniques for assisting difficult delivery at caesarean section. Cochrane Database Syst Rev. 2016;1:CD004944.
- Jeve YB, Navti OB, Konje JC. Comparison of techniques used to deliver a deeply impacted fetal head at full dilation: a systematic review and meta-analysis. BJOG. 2016;123(3): 337–345.
- Clark SL, Vines VL, Belfort MA. Fetal injury associated with routine vacuum use during cesarean delivery. Am J Obstet Gynecol. 2008;198(4):e4.
- Fareeduddin R, Schifrin BS. Subgaleal hemorrhage after the use of a vacuum extractor during elective cesarean delivery: a case report. J Reprod Med. 2008;53(10):809–810.
- Barbieri RL. Difficult fetal extraction at cesarean delivery: What should you do? OBG Manag. 2012;24(1):8–12.
- Spencer C, Murphy D, Bewley S. Caesarean delivery in the second stage of labour. BMJ. 2006;333(7569):613–614.
- Häger RM, Daltviet AK, Hofoss D, et al. Complications of cesarean deliveries: rates and risk factors. Am J Obstet Gynecol. 2004;190(2):428–434.
- Murphy DJ, Liebling RE, Verity L, Swingler R, Patel R. Early maternal and neonatal morbidity associated with operative delivery in second stage of labour: a cohort study. Lancet. 2001;358(9289):1203–1207.
- Pergialiotis V, Vlachos DG, Rodolakis A, Haidopoulos D, Thomakos N, Vlachos GD. First versus second stage C/S maternal and neonatal morbidity: a systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2014;175:15–24.
- Lippert TH. Bimanual delivery of the fetal head at cesarean section with the fetal head in the midcavity. Arch Gynecol. 1983;234(1):59–60.
- Landesman R, Graber EA. Abdominovaginal delivery: modification of the cesarean section operation to facilitate delivery of the impacted head. Am J Obstet Gynecol. 1984;148(6):707–710.
- Fong YF, Arulkumaran S. Breech extraction—an alternative method of delivering a deeply engaged head at cesarean section. Int J Gynaecol Obstet. 1997;56(2):183–184.
- Arad I, Linder N, Bercovici B. Vacuum extraction at cesarean section—neonatal outcome. J Perinat Med. 1986;14(2):137–140.
- Murless BC. Lower-segment caesarean section; a new head extractor. BMJ. 1948;1(4564):1234.
- C-Snorkle impacted fetal head release device. Clinical Innovations website. http://clinicalinnovations.com /portfolio-items/c-snorkel/. Accessed July 22, 2016.
- Seal SL, Dey A, Barman SC, Kamilya G, Mukherji J, Onwude JL. Randomized controlled trial of elevation of the fetal head with a fetal pillow during cesarean delivery at full cervical dilatation. Int J Gynaecol Obstet. 2016;133(2):178–182.
- Fasubaa OB, Ezechi OC, Orji EO, et al. Delivery of the impacted head of the fetus at caesarean section after prolonged obstructed labour: a randomised comparative study of two methods. J Obstet Gynaecol. 2002;22(4):375–378.
- Levy R, Chernomoretz T, Appelman Z, Levin D, Or Y, Hagay ZJ. Head pushing versus reverse breech extraction in cases of impacted fetal head during Cesarean section. Eur J Obstet Gynecol Reprod Biol. 2005;121(1):24–26.
- Chopra S, Bagga R, Keepanasseril A, Jain V, Kalra J, Suri V. Disengagement of the deeply engaged fetal head during cesarean section in advanced labor: conventional method versus reverse breech extraction. Acta Obstet Gynecol Scand. 2009;88(10):1163–1166.
- Veisi F, Zangeneh M, Malekkhosravi S, Rezavand N. Comparison of “push” and “pull” methods for impacted fetal head extraction during cesarean delivery. Int J Gynaecol Obstet. 2012;118(1):4–6.
- Bastani P, Pourabolghasem S, Abbasalizadeh F, Motvalli L. ComparisonColor/Black of neonatal and maternal outcomes associated with head-pushing and head-pulling methods for impacted fetal head extraction during cesarean delivery. Int J Gynaecol Obstet. 2012;118(1):1–3.
- Waterfall H, Grivell RM, Dodd JM. Techniques for assisting difficult delivery at caesarean section. Cochrane Database Syst Rev. 2016;1:CD004944.
- Jeve YB, Navti OB, Konje JC. Comparison of techniques used to deliver a deeply impacted fetal head at full dilation: a systematic review and meta-analysis. BJOG. 2016;123(3): 337–345.
- Clark SL, Vines VL, Belfort MA. Fetal injury associated with routine vacuum use during cesarean delivery. Am J Obstet Gynecol. 2008;198(4):e4.
- Fareeduddin R, Schifrin BS. Subgaleal hemorrhage after the use of a vacuum extractor during elective cesarean delivery: a case report. J Reprod Med. 2008;53(10):809–810.
- Barbieri RL. Difficult fetal extraction at cesarean delivery: What should you do? OBG Manag. 2012;24(1):8–12.
In this Article
- Risk factors for impacted fetal head
- Advantages to elevating fetal head