User login
Malpractice Counsel: Cervical Spine Injury
| An 83-year-old man presented to the ED via emergency medical services (EMS) with a chief complaint of neck pain. He was the restrained driver of a car that was struck from behind by another vehicle. The patient denied any head injury, loss of consciousness, chest pain, shortness of breath, or abdominal pain. His medical history was significant for hypertension and coronary artery disease, for which he was taking several medications. Regarding his social history, the patient denied alcohol consumption or cigarette smoking. |
The patient’s physical examination was unremarkable. His vital signs were normal, and there was no obvious external evidence of trauma. The posterior cervical spine was tender to palpation in the midline, but no step-off signs were appreciated. The neurological examination, including strength and sensation in all four extremities, was normal.
Since the patient’s only complaint was neck pain and his physical examination and history were otherwise normal, the emergency physician (EP) ordered radiographs of the cervical spine. The imaging studies were interpreted as showing advanced degenerative changes but no fractures, and the patient was prescribed an analgesic and discharged home.
When the patient woke up the next morning, he was unable to move his extremities, and returned to the same ED via EMS. He was placed in a cervical collar and found to have flaccid extremities on examination. A computed tomography (CT) scan of the cervical spine revealed a transverse fracture through the C6 vertebra. Radiology services also reviewed the cervical spine X-rays from the previous day, noting the presence of fracture.
The patient was taken to the operating room by neurosurgery services but remained paralyzed postoperatively. He never recovered from his injury and died 6 months later. His family sued the EP and the hospital for missed diagnosis of cervical spine fracture at the first ED presentation and the resulting paralysis. The case was settled for $1.3 million prior to trial.
Discussion
The evaluation of suspected cervical spine injury secondary to blunt trauma is a frequent and important skill practiced by EPs. Motor vehicle accidents are the most common cause of spinal cord injury in the United States (42%), followed by falls (27%), acts of violence (15%), and sports-related injuries (8%).1 A review by Sekon and Fehlings2 showed that 55% of all spinal injuries involve the cervical spine. Interestingly, the majority of cervical spine injuries occur at the upper or lower ends of the cervical spine; C2 vertebral fractures account for 33%, while C6 and C7 vertebral fractures account for approximately 50%.1
There are two commonly used criteria to clinically clear the cervical spine (ie, no imaging studies necessary) in blunt-trauma patients. The first is the National Emergency X-Radiography Use Study (NEXUS), which has a sensitivity of 99.6% of identifying cervical spine fractures.1 According to the NEXUS criteria, no imaging studies are required if: (1) there is no midline cervical spine tenderness; (2) there are no focal neurological deficits; (3) the patient exhibits a normal level of alertness; (4) the patient is not intoxicated; and (5) there is no distracting injury.1
The other set of criteria used to clear the cervical spine is the Canadian Cervical Spine Rule. In these criteria, a patient is considered at very low risk for cervical spine fracture in the following cases: (1) the patient is fully alert with a Glasgow Coma scale of 15; (2) the patient has no high-risk factors (ie, age >65 years, dangerous mechanism of injury, fall greater than five stairs, axial load to the head, high-speed vehicular crash, bicycle or motorcycle crash, or the presence of paresthesias in the extremities); (3) the patient has low-risk factors (eg, simple vehicle crash, sitting position in the ED, ambulatory at any time, delayed onset of neck pain, and the absence of midline cervical tenderness); and (4) the patient can actively rotate his or her neck 45 degrees to the left and to the right. The Canadian group found the above criteria to have 100% sensitivity for predicting the absence of cervical spine injury.1
The patient in this case failed both sets of criteria (ie, presence of cervical spine tenderness and age >65 years) and therefore required imaging. Historically, cervical spine X-ray (three views, anteroposterior, lateral, and odontoid; or five views, three views plus obliques) has been the imaging study of choice for such patients. Unfortunately, however, cervical spine radiographs have severe limitations in identifying spinal injury. In a large retrospective review, Woodring and Lee,3 found that the standard three-view cervical spine series failed to demonstrate 61% of all fractures and 36% of all subluxation and dislocations. Similarly, in a prospective study of 1,006 patients with 72 injuries, Diaz et al,4 found a 52.3% missed fracture rate when five-view radiographs were used to identify cervical spine injury. In addition, radiographic evaluation of elderly patients was found to be even more challenging in identifying cervical spine injury due to age-related degenerative changes.
Given the abovementioned limitations associated with radiographic imaging, CT scan of the cervical spine has become the imaging study of choice in moderate-to-severe risk patients with blunt cervical spine trauma. This modality has been shown to have a higher sensitivity and specificity for evaluating cervical spine injury compared to plain X-ray films, with CT detecting 97% to 100% of cervical spine fractures.5
In addition to demonstrating a higher sensitivity, CT also has the advantage of speed—especially when the patient is undergoing other CT studies (eg, head, abdomen, pelvis). While some clinicians criticize the higher cost of CT versus plain films, CT has been shown to decrease institutional costs (when settlement costs are taken into account) due to the reduction of the incidence of paralysis resulting from false-negative imaging studies.6
Forgotten Tourniquet
| A 33-year-old woman presented to the ED with a chief complaint of left-sided abdominal and flank pain. She described the onset of pain as abrupt, severe, and lasting approximately 3 hours in duration. She admitted to nausea, but no vomiting. She also denied a history of any previous similar symptoms or recent trauma. The patient’s medical history was unremarkable. Her last menstrual period began 3 days prior to presentation. Regarding social history, she denied any tobacco or alcohol use. |
The patient’s vital signs were: blood pressure, 138/82 mm Hg; heart rate, 102 beats/minute; respiratory rate, 18 breaths/minute; temperature 98.6˚F. Oxygen saturation was 99% on room air.
The patient appeared uncomfortable overall. The physical examination was remarkable only for mild left-sided costovertebral angle tenderness. Her abdomen was soft, nontender, and without guarding or rebound.
The EP ordered the placement of an intravenous (IV) line, through which the patient was administered normal saline and morphine and promethazine, respectively, for pain and nausea. A complete blood count, basic metabolic panel, urinalysis, and urine pregnancy test were ordered. All of the laboratory bloodwork results were normal, and the urine pregnancy test was negative. The urinalysis was remarkable for 50 to 100 red blood cells.
A noncontrast CT scan of the abdomen and pelvis revealed a 3-mm ureteral stone on the left side. When the patient returned from radiology services, her pain was significantly decreased and she felt much improved. She was diagnosed with a kidney stone and discharged home with an analgesic and a strainer, along with instructions to follow-up with urology services. The patient was in the ED for a total of 5 hours.
The plaintiff sued the EP and hospital, claiming that the tourniquet used to start the IV line and draw blood was never removed, which in turn caused nerve damage resulting in reflex sympathetic dystrophy and complex regional pain syndrome. The defense denied all of these allegations, and the ED personnel testified that the tourniquet was removed as soon as the IV was established. The defense cited the plaintiff’s medical records, which contained documentation that the tourniquet had been removed. The defense further argued that if the tourniquet had been left on as the patient alleged, she would have experienced obvious physical signs, such as swelling, redness, infiltration of fluids, pain, and numbness. A defense verdict was returned.
Discussion
It is very tempting to simply dismiss this case as absurd, with nothing to be learned from it. It does defy common sense that no one would have noticed the tourniquet or, at the very least, that the patient would not have spoken up about it during her stay in the ED. While the jury clearly came to the correct conclusion, it does highlight a real problem: forgotten tourniquets.
According to the Pennsylvania Patient Safety Advisory (PPSA), there were 125 reports of tourniquets being left on patients in Pennsylvania healthcare facilities in 1 year alone.1 In 5% of these cases, the tourniquet was discovered within a half hour of application. In approximately 66% of cases, the tourniquet was left on for up to 2 hours, and the remaining were left in place for 2 to 18 hours.
Few locations within the hospital are without risk for this type of accident. The PPSA further noted that approximately 30% of retained tourniquets occurred on medical/surgical units, 14% in the ED, and 14% on inpatient and ambulatory surgical services departments. Approximately 19% were discovered when patients were transferred from one department to another.1
In the analysis of these incidents, contributing factors to forgotten tourniquets included staff failing to follow proper procedures, inadequate staff proficiency, and staff distractions and/or interruptions.1 In addition, some patients appeared to be at increased risk of having a retained tourniquet than others. Sixty percent of 125 patients with a forgotten tourniquet were aged 70 years or older, whereas some patients were younger than age 2 years.1 Not surprisingly, patients who were unable to verbally communicate (eg, patients who were intubated, under anesthesia, had expressive aphasia, severe dementia), were at the highest risk.
In a review of recovery room incidents, Salman and Asfar2 identified two cases of forgotten tourniquets out of approximately 7,000 patients. Potential strategies to avoid this mistake include: (1) only documenting procedures after they have been completed (eg, tourniquet removal); (2) double-checking that the tourniquet has been removed prior to leaving patient bedside; and (3) the use of extra-long tourniquets so the ends are more clearly visible.
Reference - Missed Cervical Spine Injury
- Looby S, Flanders A. Spine trauma. Radiol Clin North Am. 2011;49(1):129-163.
- Sekon LH, Fehlings MG. Epidemiology, demographics, and pathophysiology of acute spinal cord injury. Spine (Phila Pa 1976). 2001;26(24 Suppl):S2-S12.
- Woodring JH, Lee C. Limitations of cervical radiography in the evaluation of acute cervical trauma. J Trauma. 1993;34(1):32-39.
- Diaz JJ Jr, Gillman C, Morris JA Jr, May AK, Carrillo YM, Guy J. Are five-view plain films of the cervical spine unreliable? A prospective evaluation in blunt trauma patients with altered mental status. J Trauma. 2003;55(4):658-663.
- Parizel PM, Zijden T, Gaudino S, et al. Trauma of the spine and spinal cord: imagining strategies. Eur Spine J. 2010;19(Suppl 1):S8-S17.
- Grogan EL, Morris JA Jr, Dittus RS, et al. Cervical spine evaluation in urban trauma centers: lowering institutional costs and complications through helical CT scan. J Am Coll Surg. 2005;200(2):160-165.
Reference - Forgotten Tourniquet
- Pennsylvania Safety Advisory. Forgotten but not gone: tourniquets left on patients. PA PSRS Patient Saf Advis. 2005;2(2):19-21.
- Salman JM, Asfar SN. Recovery room incidents. Bas J Surg. 2007;24:3.
| An 83-year-old man presented to the ED via emergency medical services (EMS) with a chief complaint of neck pain. He was the restrained driver of a car that was struck from behind by another vehicle. The patient denied any head injury, loss of consciousness, chest pain, shortness of breath, or abdominal pain. His medical history was significant for hypertension and coronary artery disease, for which he was taking several medications. Regarding his social history, the patient denied alcohol consumption or cigarette smoking. |
The patient’s physical examination was unremarkable. His vital signs were normal, and there was no obvious external evidence of trauma. The posterior cervical spine was tender to palpation in the midline, but no step-off signs were appreciated. The neurological examination, including strength and sensation in all four extremities, was normal.
Since the patient’s only complaint was neck pain and his physical examination and history were otherwise normal, the emergency physician (EP) ordered radiographs of the cervical spine. The imaging studies were interpreted as showing advanced degenerative changes but no fractures, and the patient was prescribed an analgesic and discharged home.
When the patient woke up the next morning, he was unable to move his extremities, and returned to the same ED via EMS. He was placed in a cervical collar and found to have flaccid extremities on examination. A computed tomography (CT) scan of the cervical spine revealed a transverse fracture through the C6 vertebra. Radiology services also reviewed the cervical spine X-rays from the previous day, noting the presence of fracture.
The patient was taken to the operating room by neurosurgery services but remained paralyzed postoperatively. He never recovered from his injury and died 6 months later. His family sued the EP and the hospital for missed diagnosis of cervical spine fracture at the first ED presentation and the resulting paralysis. The case was settled for $1.3 million prior to trial.
Discussion
The evaluation of suspected cervical spine injury secondary to blunt trauma is a frequent and important skill practiced by EPs. Motor vehicle accidents are the most common cause of spinal cord injury in the United States (42%), followed by falls (27%), acts of violence (15%), and sports-related injuries (8%).1 A review by Sekon and Fehlings2 showed that 55% of all spinal injuries involve the cervical spine. Interestingly, the majority of cervical spine injuries occur at the upper or lower ends of the cervical spine; C2 vertebral fractures account for 33%, while C6 and C7 vertebral fractures account for approximately 50%.1
There are two commonly used criteria to clinically clear the cervical spine (ie, no imaging studies necessary) in blunt-trauma patients. The first is the National Emergency X-Radiography Use Study (NEXUS), which has a sensitivity of 99.6% of identifying cervical spine fractures.1 According to the NEXUS criteria, no imaging studies are required if: (1) there is no midline cervical spine tenderness; (2) there are no focal neurological deficits; (3) the patient exhibits a normal level of alertness; (4) the patient is not intoxicated; and (5) there is no distracting injury.1
The other set of criteria used to clear the cervical spine is the Canadian Cervical Spine Rule. In these criteria, a patient is considered at very low risk for cervical spine fracture in the following cases: (1) the patient is fully alert with a Glasgow Coma scale of 15; (2) the patient has no high-risk factors (ie, age >65 years, dangerous mechanism of injury, fall greater than five stairs, axial load to the head, high-speed vehicular crash, bicycle or motorcycle crash, or the presence of paresthesias in the extremities); (3) the patient has low-risk factors (eg, simple vehicle crash, sitting position in the ED, ambulatory at any time, delayed onset of neck pain, and the absence of midline cervical tenderness); and (4) the patient can actively rotate his or her neck 45 degrees to the left and to the right. The Canadian group found the above criteria to have 100% sensitivity for predicting the absence of cervical spine injury.1
The patient in this case failed both sets of criteria (ie, presence of cervical spine tenderness and age >65 years) and therefore required imaging. Historically, cervical spine X-ray (three views, anteroposterior, lateral, and odontoid; or five views, three views plus obliques) has been the imaging study of choice for such patients. Unfortunately, however, cervical spine radiographs have severe limitations in identifying spinal injury. In a large retrospective review, Woodring and Lee,3 found that the standard three-view cervical spine series failed to demonstrate 61% of all fractures and 36% of all subluxation and dislocations. Similarly, in a prospective study of 1,006 patients with 72 injuries, Diaz et al,4 found a 52.3% missed fracture rate when five-view radiographs were used to identify cervical spine injury. In addition, radiographic evaluation of elderly patients was found to be even more challenging in identifying cervical spine injury due to age-related degenerative changes.
Given the abovementioned limitations associated with radiographic imaging, CT scan of the cervical spine has become the imaging study of choice in moderate-to-severe risk patients with blunt cervical spine trauma. This modality has been shown to have a higher sensitivity and specificity for evaluating cervical spine injury compared to plain X-ray films, with CT detecting 97% to 100% of cervical spine fractures.5
In addition to demonstrating a higher sensitivity, CT also has the advantage of speed—especially when the patient is undergoing other CT studies (eg, head, abdomen, pelvis). While some clinicians criticize the higher cost of CT versus plain films, CT has been shown to decrease institutional costs (when settlement costs are taken into account) due to the reduction of the incidence of paralysis resulting from false-negative imaging studies.6
Forgotten Tourniquet
| A 33-year-old woman presented to the ED with a chief complaint of left-sided abdominal and flank pain. She described the onset of pain as abrupt, severe, and lasting approximately 3 hours in duration. She admitted to nausea, but no vomiting. She also denied a history of any previous similar symptoms or recent trauma. The patient’s medical history was unremarkable. Her last menstrual period began 3 days prior to presentation. Regarding social history, she denied any tobacco or alcohol use. |
The patient’s vital signs were: blood pressure, 138/82 mm Hg; heart rate, 102 beats/minute; respiratory rate, 18 breaths/minute; temperature 98.6˚F. Oxygen saturation was 99% on room air.
The patient appeared uncomfortable overall. The physical examination was remarkable only for mild left-sided costovertebral angle tenderness. Her abdomen was soft, nontender, and without guarding or rebound.
The EP ordered the placement of an intravenous (IV) line, through which the patient was administered normal saline and morphine and promethazine, respectively, for pain and nausea. A complete blood count, basic metabolic panel, urinalysis, and urine pregnancy test were ordered. All of the laboratory bloodwork results were normal, and the urine pregnancy test was negative. The urinalysis was remarkable for 50 to 100 red blood cells.
A noncontrast CT scan of the abdomen and pelvis revealed a 3-mm ureteral stone on the left side. When the patient returned from radiology services, her pain was significantly decreased and she felt much improved. She was diagnosed with a kidney stone and discharged home with an analgesic and a strainer, along with instructions to follow-up with urology services. The patient was in the ED for a total of 5 hours.
The plaintiff sued the EP and hospital, claiming that the tourniquet used to start the IV line and draw blood was never removed, which in turn caused nerve damage resulting in reflex sympathetic dystrophy and complex regional pain syndrome. The defense denied all of these allegations, and the ED personnel testified that the tourniquet was removed as soon as the IV was established. The defense cited the plaintiff’s medical records, which contained documentation that the tourniquet had been removed. The defense further argued that if the tourniquet had been left on as the patient alleged, she would have experienced obvious physical signs, such as swelling, redness, infiltration of fluids, pain, and numbness. A defense verdict was returned.
Discussion
It is very tempting to simply dismiss this case as absurd, with nothing to be learned from it. It does defy common sense that no one would have noticed the tourniquet or, at the very least, that the patient would not have spoken up about it during her stay in the ED. While the jury clearly came to the correct conclusion, it does highlight a real problem: forgotten tourniquets.
According to the Pennsylvania Patient Safety Advisory (PPSA), there were 125 reports of tourniquets being left on patients in Pennsylvania healthcare facilities in 1 year alone.1 In 5% of these cases, the tourniquet was discovered within a half hour of application. In approximately 66% of cases, the tourniquet was left on for up to 2 hours, and the remaining were left in place for 2 to 18 hours.
Few locations within the hospital are without risk for this type of accident. The PPSA further noted that approximately 30% of retained tourniquets occurred on medical/surgical units, 14% in the ED, and 14% on inpatient and ambulatory surgical services departments. Approximately 19% were discovered when patients were transferred from one department to another.1
In the analysis of these incidents, contributing factors to forgotten tourniquets included staff failing to follow proper procedures, inadequate staff proficiency, and staff distractions and/or interruptions.1 In addition, some patients appeared to be at increased risk of having a retained tourniquet than others. Sixty percent of 125 patients with a forgotten tourniquet were aged 70 years or older, whereas some patients were younger than age 2 years.1 Not surprisingly, patients who were unable to verbally communicate (eg, patients who were intubated, under anesthesia, had expressive aphasia, severe dementia), were at the highest risk.
In a review of recovery room incidents, Salman and Asfar2 identified two cases of forgotten tourniquets out of approximately 7,000 patients. Potential strategies to avoid this mistake include: (1) only documenting procedures after they have been completed (eg, tourniquet removal); (2) double-checking that the tourniquet has been removed prior to leaving patient bedside; and (3) the use of extra-long tourniquets so the ends are more clearly visible.
| An 83-year-old man presented to the ED via emergency medical services (EMS) with a chief complaint of neck pain. He was the restrained driver of a car that was struck from behind by another vehicle. The patient denied any head injury, loss of consciousness, chest pain, shortness of breath, or abdominal pain. His medical history was significant for hypertension and coronary artery disease, for which he was taking several medications. Regarding his social history, the patient denied alcohol consumption or cigarette smoking. |
The patient’s physical examination was unremarkable. His vital signs were normal, and there was no obvious external evidence of trauma. The posterior cervical spine was tender to palpation in the midline, but no step-off signs were appreciated. The neurological examination, including strength and sensation in all four extremities, was normal.
Since the patient’s only complaint was neck pain and his physical examination and history were otherwise normal, the emergency physician (EP) ordered radiographs of the cervical spine. The imaging studies were interpreted as showing advanced degenerative changes but no fractures, and the patient was prescribed an analgesic and discharged home.
When the patient woke up the next morning, he was unable to move his extremities, and returned to the same ED via EMS. He was placed in a cervical collar and found to have flaccid extremities on examination. A computed tomography (CT) scan of the cervical spine revealed a transverse fracture through the C6 vertebra. Radiology services also reviewed the cervical spine X-rays from the previous day, noting the presence of fracture.
The patient was taken to the operating room by neurosurgery services but remained paralyzed postoperatively. He never recovered from his injury and died 6 months later. His family sued the EP and the hospital for missed diagnosis of cervical spine fracture at the first ED presentation and the resulting paralysis. The case was settled for $1.3 million prior to trial.
Discussion
The evaluation of suspected cervical spine injury secondary to blunt trauma is a frequent and important skill practiced by EPs. Motor vehicle accidents are the most common cause of spinal cord injury in the United States (42%), followed by falls (27%), acts of violence (15%), and sports-related injuries (8%).1 A review by Sekon and Fehlings2 showed that 55% of all spinal injuries involve the cervical spine. Interestingly, the majority of cervical spine injuries occur at the upper or lower ends of the cervical spine; C2 vertebral fractures account for 33%, while C6 and C7 vertebral fractures account for approximately 50%.1
There are two commonly used criteria to clinically clear the cervical spine (ie, no imaging studies necessary) in blunt-trauma patients. The first is the National Emergency X-Radiography Use Study (NEXUS), which has a sensitivity of 99.6% of identifying cervical spine fractures.1 According to the NEXUS criteria, no imaging studies are required if: (1) there is no midline cervical spine tenderness; (2) there are no focal neurological deficits; (3) the patient exhibits a normal level of alertness; (4) the patient is not intoxicated; and (5) there is no distracting injury.1
The other set of criteria used to clear the cervical spine is the Canadian Cervical Spine Rule. In these criteria, a patient is considered at very low risk for cervical spine fracture in the following cases: (1) the patient is fully alert with a Glasgow Coma scale of 15; (2) the patient has no high-risk factors (ie, age >65 years, dangerous mechanism of injury, fall greater than five stairs, axial load to the head, high-speed vehicular crash, bicycle or motorcycle crash, or the presence of paresthesias in the extremities); (3) the patient has low-risk factors (eg, simple vehicle crash, sitting position in the ED, ambulatory at any time, delayed onset of neck pain, and the absence of midline cervical tenderness); and (4) the patient can actively rotate his or her neck 45 degrees to the left and to the right. The Canadian group found the above criteria to have 100% sensitivity for predicting the absence of cervical spine injury.1
The patient in this case failed both sets of criteria (ie, presence of cervical spine tenderness and age >65 years) and therefore required imaging. Historically, cervical spine X-ray (three views, anteroposterior, lateral, and odontoid; or five views, three views plus obliques) has been the imaging study of choice for such patients. Unfortunately, however, cervical spine radiographs have severe limitations in identifying spinal injury. In a large retrospective review, Woodring and Lee,3 found that the standard three-view cervical spine series failed to demonstrate 61% of all fractures and 36% of all subluxation and dislocations. Similarly, in a prospective study of 1,006 patients with 72 injuries, Diaz et al,4 found a 52.3% missed fracture rate when five-view radiographs were used to identify cervical spine injury. In addition, radiographic evaluation of elderly patients was found to be even more challenging in identifying cervical spine injury due to age-related degenerative changes.
Given the abovementioned limitations associated with radiographic imaging, CT scan of the cervical spine has become the imaging study of choice in moderate-to-severe risk patients with blunt cervical spine trauma. This modality has been shown to have a higher sensitivity and specificity for evaluating cervical spine injury compared to plain X-ray films, with CT detecting 97% to 100% of cervical spine fractures.5
In addition to demonstrating a higher sensitivity, CT also has the advantage of speed—especially when the patient is undergoing other CT studies (eg, head, abdomen, pelvis). While some clinicians criticize the higher cost of CT versus plain films, CT has been shown to decrease institutional costs (when settlement costs are taken into account) due to the reduction of the incidence of paralysis resulting from false-negative imaging studies.6
Forgotten Tourniquet
| A 33-year-old woman presented to the ED with a chief complaint of left-sided abdominal and flank pain. She described the onset of pain as abrupt, severe, and lasting approximately 3 hours in duration. She admitted to nausea, but no vomiting. She also denied a history of any previous similar symptoms or recent trauma. The patient’s medical history was unremarkable. Her last menstrual period began 3 days prior to presentation. Regarding social history, she denied any tobacco or alcohol use. |
The patient’s vital signs were: blood pressure, 138/82 mm Hg; heart rate, 102 beats/minute; respiratory rate, 18 breaths/minute; temperature 98.6˚F. Oxygen saturation was 99% on room air.
The patient appeared uncomfortable overall. The physical examination was remarkable only for mild left-sided costovertebral angle tenderness. Her abdomen was soft, nontender, and without guarding or rebound.
The EP ordered the placement of an intravenous (IV) line, through which the patient was administered normal saline and morphine and promethazine, respectively, for pain and nausea. A complete blood count, basic metabolic panel, urinalysis, and urine pregnancy test were ordered. All of the laboratory bloodwork results were normal, and the urine pregnancy test was negative. The urinalysis was remarkable for 50 to 100 red blood cells.
A noncontrast CT scan of the abdomen and pelvis revealed a 3-mm ureteral stone on the left side. When the patient returned from radiology services, her pain was significantly decreased and she felt much improved. She was diagnosed with a kidney stone and discharged home with an analgesic and a strainer, along with instructions to follow-up with urology services. The patient was in the ED for a total of 5 hours.
The plaintiff sued the EP and hospital, claiming that the tourniquet used to start the IV line and draw blood was never removed, which in turn caused nerve damage resulting in reflex sympathetic dystrophy and complex regional pain syndrome. The defense denied all of these allegations, and the ED personnel testified that the tourniquet was removed as soon as the IV was established. The defense cited the plaintiff’s medical records, which contained documentation that the tourniquet had been removed. The defense further argued that if the tourniquet had been left on as the patient alleged, she would have experienced obvious physical signs, such as swelling, redness, infiltration of fluids, pain, and numbness. A defense verdict was returned.
Discussion
It is very tempting to simply dismiss this case as absurd, with nothing to be learned from it. It does defy common sense that no one would have noticed the tourniquet or, at the very least, that the patient would not have spoken up about it during her stay in the ED. While the jury clearly came to the correct conclusion, it does highlight a real problem: forgotten tourniquets.
According to the Pennsylvania Patient Safety Advisory (PPSA), there were 125 reports of tourniquets being left on patients in Pennsylvania healthcare facilities in 1 year alone.1 In 5% of these cases, the tourniquet was discovered within a half hour of application. In approximately 66% of cases, the tourniquet was left on for up to 2 hours, and the remaining were left in place for 2 to 18 hours.
Few locations within the hospital are without risk for this type of accident. The PPSA further noted that approximately 30% of retained tourniquets occurred on medical/surgical units, 14% in the ED, and 14% on inpatient and ambulatory surgical services departments. Approximately 19% were discovered when patients were transferred from one department to another.1
In the analysis of these incidents, contributing factors to forgotten tourniquets included staff failing to follow proper procedures, inadequate staff proficiency, and staff distractions and/or interruptions.1 In addition, some patients appeared to be at increased risk of having a retained tourniquet than others. Sixty percent of 125 patients with a forgotten tourniquet were aged 70 years or older, whereas some patients were younger than age 2 years.1 Not surprisingly, patients who were unable to verbally communicate (eg, patients who were intubated, under anesthesia, had expressive aphasia, severe dementia), were at the highest risk.
In a review of recovery room incidents, Salman and Asfar2 identified two cases of forgotten tourniquets out of approximately 7,000 patients. Potential strategies to avoid this mistake include: (1) only documenting procedures after they have been completed (eg, tourniquet removal); (2) double-checking that the tourniquet has been removed prior to leaving patient bedside; and (3) the use of extra-long tourniquets so the ends are more clearly visible.
Reference - Missed Cervical Spine Injury
- Looby S, Flanders A. Spine trauma. Radiol Clin North Am. 2011;49(1):129-163.
- Sekon LH, Fehlings MG. Epidemiology, demographics, and pathophysiology of acute spinal cord injury. Spine (Phila Pa 1976). 2001;26(24 Suppl):S2-S12.
- Woodring JH, Lee C. Limitations of cervical radiography in the evaluation of acute cervical trauma. J Trauma. 1993;34(1):32-39.
- Diaz JJ Jr, Gillman C, Morris JA Jr, May AK, Carrillo YM, Guy J. Are five-view plain films of the cervical spine unreliable? A prospective evaluation in blunt trauma patients with altered mental status. J Trauma. 2003;55(4):658-663.
- Parizel PM, Zijden T, Gaudino S, et al. Trauma of the spine and spinal cord: imagining strategies. Eur Spine J. 2010;19(Suppl 1):S8-S17.
- Grogan EL, Morris JA Jr, Dittus RS, et al. Cervical spine evaluation in urban trauma centers: lowering institutional costs and complications through helical CT scan. J Am Coll Surg. 2005;200(2):160-165.
Reference - Forgotten Tourniquet
- Pennsylvania Safety Advisory. Forgotten but not gone: tourniquets left on patients. PA PSRS Patient Saf Advis. 2005;2(2):19-21.
- Salman JM, Asfar SN. Recovery room incidents. Bas J Surg. 2007;24:3.
Reference - Missed Cervical Spine Injury
- Looby S, Flanders A. Spine trauma. Radiol Clin North Am. 2011;49(1):129-163.
- Sekon LH, Fehlings MG. Epidemiology, demographics, and pathophysiology of acute spinal cord injury. Spine (Phila Pa 1976). 2001;26(24 Suppl):S2-S12.
- Woodring JH, Lee C. Limitations of cervical radiography in the evaluation of acute cervical trauma. J Trauma. 1993;34(1):32-39.
- Diaz JJ Jr, Gillman C, Morris JA Jr, May AK, Carrillo YM, Guy J. Are five-view plain films of the cervical spine unreliable? A prospective evaluation in blunt trauma patients with altered mental status. J Trauma. 2003;55(4):658-663.
- Parizel PM, Zijden T, Gaudino S, et al. Trauma of the spine and spinal cord: imagining strategies. Eur Spine J. 2010;19(Suppl 1):S8-S17.
- Grogan EL, Morris JA Jr, Dittus RS, et al. Cervical spine evaluation in urban trauma centers: lowering institutional costs and complications through helical CT scan. J Am Coll Surg. 2005;200(2):160-165.
Reference - Forgotten Tourniquet
- Pennsylvania Safety Advisory. Forgotten but not gone: tourniquets left on patients. PA PSRS Patient Saf Advis. 2005;2(2):19-21.
- Salman JM, Asfar SN. Recovery room incidents. Bas J Surg. 2007;24:3.
Malpractice Counsel: Missed Preeclampsia
Missed Preeclampsia
| A 24-year-old woman, gravida 1, para 1, aborta 0, presented to the ED complaining of a 1-day history of shortness of breath. Four days earlier, she had delivered a healthy baby boy via normal vaginal delivery and without complication. She denied chest pain, fever, or abdominal pain. She was otherwise in good health, stating that she was not taking any medications. She also denied smoking cigarettes. |
On physical examination, the patient’s vital signs were remarkable for the following: heart rate (HR), 86 beats/minute; blood pressure (BP), 164/94 mm Hg; respiratory rate, 18 breaths/minute; temperature, 98.6oF. Oxygen saturation was 96% on room air. The head, eye, ear, nose and throat examination was unremarkable. The lungs were clear to auscultation bilaterally, and HR and heart rhythm were normal. The abdomen was soft and nontender without guarding or rebound. The lower extremities were remarkable for 1+ pedal and pretibial edema bilaterally.
The patient presented to the same ED 2 days later, again with the chief complaint of shortness of breath. On examination, her BP was noted to be elevated and she had 1+ dependent edema bilaterally. Again, the EP was concerned for a PE and ordered a repeat CTA scan of the chest. This study, similar to the first, was read as normal, and showed no evidence of PE. The patient was diagnosed again with “shortness of breath of unknown etiology” and discharged home. The patient’s obstetrician-gynecologist (Ob/Gyn) was not consulted; however, the patient was encouraged to follow up with him.
The next day, the patient presented to the same ED via emergency medical services, this time with seizures; she had no prior history of a seizure disorder. On presentation to the ED, she was noted to be postictal, with an elevated BP and tachycardic with an HR of 104 beats/minute. On examination, the lungs were clear to auscultation and the lower extremities exhibited 1+ pedal and pretibial edema. A urinalysis revealed proteinuria. The patient was given 4 g of magnesium sulfate intravenously (IV) and her Ob/Gyn was consulted.
The patient was admitted to the hospital with a diagnosis of eclampsia. She was given an IV drip of magnesium and labetalol for the high BP. Unfortunately, the patient apparently had suffered an anoxic brain injury from the previous seizures and died on hospital day 3.
The family sued the treating EPs and the hospital for failure to diagnose preeclampsia on two separate ED presentations. They noted the patient’s Ob/Gyn was never consulted; no action was taken to treat the hypertension; and no urinalysis was ordered on either visit. The EPs and hospital settled the case prior to trial for several million dollars.
Discussion
This is an incredibly sad case, and the EPs and hospital were right to settle and not go to trial. While PE was a reasonable diagnosis to consider in this patient on her first ED visit, it should not have been the only one in the differential diagnosis. The EP became anchored to this single diagnosis and refused to consider other alternative diagnoses—even after the CTA scan of the chest ruled out PE. Moreover, it appears the EP either never considered the significance of the elevated BP and dependent edema or just ignored these findings. To repeat essentially the same exact workup on the second visit does not make sense—one should “cast a wider net, not the same net.”
The diagnosis of “shortness of breath of unknown etiology” is similarly unacceptable. While this is a common and accepted diagnosis when it pertains to abdominal pain, the same is not true for dyspnea.
Preeclampsia is characterized by hypertension (BP >140/90 mm Hg) and proteinuria; associated symptoms include edema and hyperreflexia. Postpartum preeclampsia occurs infrequently and can develop up to 4 weeks after delivery.1 In one 10-year retrospective case series, the incidence of preeclampsia in the postpartum period was 5.7%, and nearly 16% went on to develop eclampsia.2 In a retrospective study of 22 postpartum preeclamptic patients, the median time to presentation was 5 days postpartum.1 In a similar retrospective study of 152 patients, 90% of such patients presented within 7 days.3 The patient in this case initially presented on postpartum day 4.
Interestingly, in a study by Al-Safi et al,3 63% of postpartum preeclamptic patients had no antecedent diagnosis of hypertensive disease during pregnancy. These findings are consistent with the findings of others that 33% to 69% of such patients show no evidence of preeclampsia in the ante- or peripartum period.
The clinical presentation of postpartum preeclampsia is similar to preeclampsia complicating pregnancy after gestation week 20. In the study by Al-Safi et al,3 headache was the most common presenting symptom (69%), followed by shortness of breath (30%), blurry vision (21%), nausea (12.5%), and epigastric abdominal pain (5%). Similarly, Yancey et al1 found headache (82%) to be the most common presenting symptom in their series. Unfortunately, it is not known whether the patient in this case complained of headache or blurred vision as the published records note neither their presence nor absence.
The management of patients with preeclampsia includes IV magnesium to prevent seizures (ie, eclampsia) and BP control.1 A bolus of 4 to 6 g IV magnesium sulfate over 15 to 30 minutes is recommended, followed by an infusion of 2 g/h IV. Historically, IV hydralazine has been used to manage preeclamptic patients with a BP greater than 160/110 mm Hg. More recently, however, IV labetalol has become popular.5 All such patients require admission to the hospital with Ob/Gyn involvement.
Missed Subdural Hematoma
A 59-year-old man presented to the ED with a chief complaint of headache, the onset of which he stated started gradually 2 days prior. He noted the headache was worse than normal but without associated nausea, vomiting, fever, chills, or change in vision. His past medical history was significant for a lower extremity deep vein thrombosis 3 months prior, for which he was taking warfarin.
The patient’s vital signs were all normal. The physical examination, including a thorough neurological examination, was also normal. The EP ordered a prothrombin time (PT), an international normalized ratio (INR), and a noncontrast CT scan of the head. The PT/INR results were therapeutic at 22 seconds and 2.3. The CT scan was interpreted by radiology services as normal. The patient’s headache was treated with IV prochlorperazine and diphenhydramine. After treatment, the patient reported feeling better and was discharged home with instructions to follow up with his primary care physician.
Over the next several months, the patient presented to the same ED on seven different occasions, each time with the chief complaint of headache. At each of these presentations, the history and physical examination were documented as unremarkable, with no history of trauma. The thoroughness, however, of the documentation varied considerably for each ED encounter. No head CT scan was ordered on the subsequent seven visits, and at each presentation, the patient was treated symptomatically and discharged home.
Two days after his eighth visit to the same hospital ED, the patient presented to a different ED, again with a chief complaint of headache. The EP at this ED ordered a noncontrast CT of the head, which demonstrated a left subdural hematoma. The patient was admitted to the hospital, given IV vitamin K and fresh frozen plasma, and underwent evacuation of the hematoma by neurosurgery. The patient’s hospital course was unremarkable, and he was discharged home without any focal weakness.
The patient, however, claimed that he suffered cognitive impairment as a result of the missed diagnosis. He sued treating EPs at the first ED as well as the hospital for failure to timely diagnose the subdural hematoma, stating that a CT scan should have been performed at each of his ED visits since he was on warfarin. The defense claimed that a CT scan was not warranted for each visit, and that the timing of when and how the brain bleed started was uncertain. At trial, a defense verdict was returned.
Discussion
It is well known that patients receiving warfarin are at an increased risk for intracranial hemorrhage (ICH) following blunt head trauma.1 The recommendation is that all such patients have a noncontrast CT scan of the head to rule out intracranial bleeding. This is due to the fact that 60% of patients presenting with an immediate traumatic intracranial hemorrhage will have a normal mental status on examination; and 11% will have no history of loss of consciousness, a normal mental status examination, and no physical evidence of trauma above the clavicles.1 In a study by Hart et al,2 subdural hematoma accounted for 44% of all ICH in these types of patients.
More controversial is how to manage patients on warfarin who experience blunt head trauma and have a normal CT scan of the head. Because of the fear for delayed traumatic ICH, many clinicians recommend admitting such patients for neurological observation and repeat head CT scan the next morning.3 Additionally, some clinicians even recommend reversing the warfarin anticoagulation in such patients. 4 These recommendations, though, are based on expert consensus rather than on rigorous, prospective multicenter studies.1 These strategies are also problematic, since such multiple repeat CT scans would not only be incredibly expensive but also would expose the patient to high doses of radiation to the brain. Moreover, the Centers for Medicare and Medicaid Services has now made CT brain scan imaging of patients presenting to the ED with complaint of nontraumatic headache a quality measure they follow. Their goal is to decrease the number of “unnecessary” head CT scans.
The patient in this case denied any history of trauma on the subsequent seven ED visits. Unfortunately, as pointed out, even minor trauma can result in ICH, and patients may not recall the occurrence of the event.
For patients on warfarin who present with headache, a very careful history must be taken—including inquiring about minor traumatic events. Even then, as has been shown, patients may have not experienced a loss of consciousness, have a normal mental status examination, and exhibit no external evidence of head trauma. The clinician is forced to use her or his own best judgment when evaluating such patients in the ED.
Interestingly, the risk of ICH secondary to blunt head trauma in patients on warfarin is increased if they are on concomitant aspirin therapy.2 Similarly, the risk of ICH following head trauma in patients on clopidogrel is greater than for those patients taking warfarin,1 and the risk of ICH in patients taking dabigatran is less than if taking warfarin.2
Reference - Missed Preeclampsia
- Yancey LM, Withers E, Barnes K, Abbott J. Postpartum preeclampsia: emergency department presentation and management. J Emerg Med. 2011;40(4):380-384.
- Matthys LA, Coppage KH, Lambers DS, Barton JR, Sibai BM. Delayed postpartum preeclampsia: an experience of 151 cases. Am J Obstet Gynecol. 2004;190(5):1464-1466.
- Al-Safi Z, Imudia AN, Filetti LC, Hobson DT, Bahado-Singh RO, Awonuga AO. Delayed postpartum preeclampsia and eclampsia: demographics, clinical course, and complications. Obstet Gynecol. 2011;118(5):1102-1107.
- Chames MC, Livingston JC, Ivester TS, Barton JR, Sibai BM. Late postpartum eclampsia: a preventable disease? Am J Obstet Gynecol. 2002;186(6):1174-1177.
- Graeber B, Vanderwal T, Stiller RJ, Werdmann MJ. Late postpartum eclampsia as an obstetric complication seen in the ED. Am J Emerg Med. 2005;23(2):168-170.
Reference - Missed Subdural Hematoma
- Nishijima DK, Offerman SR, Ballard DW, et al; Clinical Research in Emergency Services and Treatment (CREST) Network. Immediate and delayed traumatic intracranial hemorrhage in patients with head trauma and preinjury warfarin or clopidogrel use. Ann Emerg Med. 2012;59(6):460-468.
- Hart RG, Diener HC, Yang S, Connolly SJ, Wallentin L, et al. Intracranial hemorrhage in atrial fibrillation patients during anticoagulation with warfarin or dabigatran: the RE-LY trial. Stroke. 2012;43(6): 1511-1517.
- Vos PE, Battistin L, Birbamer G, et al; European Federation of Neurological Societies. EFNS guideline on mild traumatic brain injury: report of an EFNS task force. Eur J Neurol. 2002;9(3):207-219.
- Coimbra R, Hoyt DB, Anjaria DJ, Potenza BM, Fortlage D, Hollingsworth-Fridlund P. Reversal of anticoagulation in trauma: a North-American survey on clinical practices among trauma surgeons. J Trauma. 2005;59(2):375-382.
Missed Preeclampsia
| A 24-year-old woman, gravida 1, para 1, aborta 0, presented to the ED complaining of a 1-day history of shortness of breath. Four days earlier, she had delivered a healthy baby boy via normal vaginal delivery and without complication. She denied chest pain, fever, or abdominal pain. She was otherwise in good health, stating that she was not taking any medications. She also denied smoking cigarettes. |
On physical examination, the patient’s vital signs were remarkable for the following: heart rate (HR), 86 beats/minute; blood pressure (BP), 164/94 mm Hg; respiratory rate, 18 breaths/minute; temperature, 98.6oF. Oxygen saturation was 96% on room air. The head, eye, ear, nose and throat examination was unremarkable. The lungs were clear to auscultation bilaterally, and HR and heart rhythm were normal. The abdomen was soft and nontender without guarding or rebound. The lower extremities were remarkable for 1+ pedal and pretibial edema bilaterally.
The patient presented to the same ED 2 days later, again with the chief complaint of shortness of breath. On examination, her BP was noted to be elevated and she had 1+ dependent edema bilaterally. Again, the EP was concerned for a PE and ordered a repeat CTA scan of the chest. This study, similar to the first, was read as normal, and showed no evidence of PE. The patient was diagnosed again with “shortness of breath of unknown etiology” and discharged home. The patient’s obstetrician-gynecologist (Ob/Gyn) was not consulted; however, the patient was encouraged to follow up with him.
The next day, the patient presented to the same ED via emergency medical services, this time with seizures; she had no prior history of a seizure disorder. On presentation to the ED, she was noted to be postictal, with an elevated BP and tachycardic with an HR of 104 beats/minute. On examination, the lungs were clear to auscultation and the lower extremities exhibited 1+ pedal and pretibial edema. A urinalysis revealed proteinuria. The patient was given 4 g of magnesium sulfate intravenously (IV) and her Ob/Gyn was consulted.
The patient was admitted to the hospital with a diagnosis of eclampsia. She was given an IV drip of magnesium and labetalol for the high BP. Unfortunately, the patient apparently had suffered an anoxic brain injury from the previous seizures and died on hospital day 3.
The family sued the treating EPs and the hospital for failure to diagnose preeclampsia on two separate ED presentations. They noted the patient’s Ob/Gyn was never consulted; no action was taken to treat the hypertension; and no urinalysis was ordered on either visit. The EPs and hospital settled the case prior to trial for several million dollars.
Discussion
This is an incredibly sad case, and the EPs and hospital were right to settle and not go to trial. While PE was a reasonable diagnosis to consider in this patient on her first ED visit, it should not have been the only one in the differential diagnosis. The EP became anchored to this single diagnosis and refused to consider other alternative diagnoses—even after the CTA scan of the chest ruled out PE. Moreover, it appears the EP either never considered the significance of the elevated BP and dependent edema or just ignored these findings. To repeat essentially the same exact workup on the second visit does not make sense—one should “cast a wider net, not the same net.”
The diagnosis of “shortness of breath of unknown etiology” is similarly unacceptable. While this is a common and accepted diagnosis when it pertains to abdominal pain, the same is not true for dyspnea.
Preeclampsia is characterized by hypertension (BP >140/90 mm Hg) and proteinuria; associated symptoms include edema and hyperreflexia. Postpartum preeclampsia occurs infrequently and can develop up to 4 weeks after delivery.1 In one 10-year retrospective case series, the incidence of preeclampsia in the postpartum period was 5.7%, and nearly 16% went on to develop eclampsia.2 In a retrospective study of 22 postpartum preeclamptic patients, the median time to presentation was 5 days postpartum.1 In a similar retrospective study of 152 patients, 90% of such patients presented within 7 days.3 The patient in this case initially presented on postpartum day 4.
Interestingly, in a study by Al-Safi et al,3 63% of postpartum preeclamptic patients had no antecedent diagnosis of hypertensive disease during pregnancy. These findings are consistent with the findings of others that 33% to 69% of such patients show no evidence of preeclampsia in the ante- or peripartum period.
The clinical presentation of postpartum preeclampsia is similar to preeclampsia complicating pregnancy after gestation week 20. In the study by Al-Safi et al,3 headache was the most common presenting symptom (69%), followed by shortness of breath (30%), blurry vision (21%), nausea (12.5%), and epigastric abdominal pain (5%). Similarly, Yancey et al1 found headache (82%) to be the most common presenting symptom in their series. Unfortunately, it is not known whether the patient in this case complained of headache or blurred vision as the published records note neither their presence nor absence.
The management of patients with preeclampsia includes IV magnesium to prevent seizures (ie, eclampsia) and BP control.1 A bolus of 4 to 6 g IV magnesium sulfate over 15 to 30 minutes is recommended, followed by an infusion of 2 g/h IV. Historically, IV hydralazine has been used to manage preeclamptic patients with a BP greater than 160/110 mm Hg. More recently, however, IV labetalol has become popular.5 All such patients require admission to the hospital with Ob/Gyn involvement.
Missed Subdural Hematoma
A 59-year-old man presented to the ED with a chief complaint of headache, the onset of which he stated started gradually 2 days prior. He noted the headache was worse than normal but without associated nausea, vomiting, fever, chills, or change in vision. His past medical history was significant for a lower extremity deep vein thrombosis 3 months prior, for which he was taking warfarin.
The patient’s vital signs were all normal. The physical examination, including a thorough neurological examination, was also normal. The EP ordered a prothrombin time (PT), an international normalized ratio (INR), and a noncontrast CT scan of the head. The PT/INR results were therapeutic at 22 seconds and 2.3. The CT scan was interpreted by radiology services as normal. The patient’s headache was treated with IV prochlorperazine and diphenhydramine. After treatment, the patient reported feeling better and was discharged home with instructions to follow up with his primary care physician.
Over the next several months, the patient presented to the same ED on seven different occasions, each time with the chief complaint of headache. At each of these presentations, the history and physical examination were documented as unremarkable, with no history of trauma. The thoroughness, however, of the documentation varied considerably for each ED encounter. No head CT scan was ordered on the subsequent seven visits, and at each presentation, the patient was treated symptomatically and discharged home.
Two days after his eighth visit to the same hospital ED, the patient presented to a different ED, again with a chief complaint of headache. The EP at this ED ordered a noncontrast CT of the head, which demonstrated a left subdural hematoma. The patient was admitted to the hospital, given IV vitamin K and fresh frozen plasma, and underwent evacuation of the hematoma by neurosurgery. The patient’s hospital course was unremarkable, and he was discharged home without any focal weakness.
The patient, however, claimed that he suffered cognitive impairment as a result of the missed diagnosis. He sued treating EPs at the first ED as well as the hospital for failure to timely diagnose the subdural hematoma, stating that a CT scan should have been performed at each of his ED visits since he was on warfarin. The defense claimed that a CT scan was not warranted for each visit, and that the timing of when and how the brain bleed started was uncertain. At trial, a defense verdict was returned.
Discussion
It is well known that patients receiving warfarin are at an increased risk for intracranial hemorrhage (ICH) following blunt head trauma.1 The recommendation is that all such patients have a noncontrast CT scan of the head to rule out intracranial bleeding. This is due to the fact that 60% of patients presenting with an immediate traumatic intracranial hemorrhage will have a normal mental status on examination; and 11% will have no history of loss of consciousness, a normal mental status examination, and no physical evidence of trauma above the clavicles.1 In a study by Hart et al,2 subdural hematoma accounted for 44% of all ICH in these types of patients.
More controversial is how to manage patients on warfarin who experience blunt head trauma and have a normal CT scan of the head. Because of the fear for delayed traumatic ICH, many clinicians recommend admitting such patients for neurological observation and repeat head CT scan the next morning.3 Additionally, some clinicians even recommend reversing the warfarin anticoagulation in such patients. 4 These recommendations, though, are based on expert consensus rather than on rigorous, prospective multicenter studies.1 These strategies are also problematic, since such multiple repeat CT scans would not only be incredibly expensive but also would expose the patient to high doses of radiation to the brain. Moreover, the Centers for Medicare and Medicaid Services has now made CT brain scan imaging of patients presenting to the ED with complaint of nontraumatic headache a quality measure they follow. Their goal is to decrease the number of “unnecessary” head CT scans.
The patient in this case denied any history of trauma on the subsequent seven ED visits. Unfortunately, as pointed out, even minor trauma can result in ICH, and patients may not recall the occurrence of the event.
For patients on warfarin who present with headache, a very careful history must be taken—including inquiring about minor traumatic events. Even then, as has been shown, patients may have not experienced a loss of consciousness, have a normal mental status examination, and exhibit no external evidence of head trauma. The clinician is forced to use her or his own best judgment when evaluating such patients in the ED.
Interestingly, the risk of ICH secondary to blunt head trauma in patients on warfarin is increased if they are on concomitant aspirin therapy.2 Similarly, the risk of ICH following head trauma in patients on clopidogrel is greater than for those patients taking warfarin,1 and the risk of ICH in patients taking dabigatran is less than if taking warfarin.2
Missed Preeclampsia
| A 24-year-old woman, gravida 1, para 1, aborta 0, presented to the ED complaining of a 1-day history of shortness of breath. Four days earlier, she had delivered a healthy baby boy via normal vaginal delivery and without complication. She denied chest pain, fever, or abdominal pain. She was otherwise in good health, stating that she was not taking any medications. She also denied smoking cigarettes. |
On physical examination, the patient’s vital signs were remarkable for the following: heart rate (HR), 86 beats/minute; blood pressure (BP), 164/94 mm Hg; respiratory rate, 18 breaths/minute; temperature, 98.6oF. Oxygen saturation was 96% on room air. The head, eye, ear, nose and throat examination was unremarkable. The lungs were clear to auscultation bilaterally, and HR and heart rhythm were normal. The abdomen was soft and nontender without guarding or rebound. The lower extremities were remarkable for 1+ pedal and pretibial edema bilaterally.
The patient presented to the same ED 2 days later, again with the chief complaint of shortness of breath. On examination, her BP was noted to be elevated and she had 1+ dependent edema bilaterally. Again, the EP was concerned for a PE and ordered a repeat CTA scan of the chest. This study, similar to the first, was read as normal, and showed no evidence of PE. The patient was diagnosed again with “shortness of breath of unknown etiology” and discharged home. The patient’s obstetrician-gynecologist (Ob/Gyn) was not consulted; however, the patient was encouraged to follow up with him.
The next day, the patient presented to the same ED via emergency medical services, this time with seizures; she had no prior history of a seizure disorder. On presentation to the ED, she was noted to be postictal, with an elevated BP and tachycardic with an HR of 104 beats/minute. On examination, the lungs were clear to auscultation and the lower extremities exhibited 1+ pedal and pretibial edema. A urinalysis revealed proteinuria. The patient was given 4 g of magnesium sulfate intravenously (IV) and her Ob/Gyn was consulted.
The patient was admitted to the hospital with a diagnosis of eclampsia. She was given an IV drip of magnesium and labetalol for the high BP. Unfortunately, the patient apparently had suffered an anoxic brain injury from the previous seizures and died on hospital day 3.
The family sued the treating EPs and the hospital for failure to diagnose preeclampsia on two separate ED presentations. They noted the patient’s Ob/Gyn was never consulted; no action was taken to treat the hypertension; and no urinalysis was ordered on either visit. The EPs and hospital settled the case prior to trial for several million dollars.
Discussion
This is an incredibly sad case, and the EPs and hospital were right to settle and not go to trial. While PE was a reasonable diagnosis to consider in this patient on her first ED visit, it should not have been the only one in the differential diagnosis. The EP became anchored to this single diagnosis and refused to consider other alternative diagnoses—even after the CTA scan of the chest ruled out PE. Moreover, it appears the EP either never considered the significance of the elevated BP and dependent edema or just ignored these findings. To repeat essentially the same exact workup on the second visit does not make sense—one should “cast a wider net, not the same net.”
The diagnosis of “shortness of breath of unknown etiology” is similarly unacceptable. While this is a common and accepted diagnosis when it pertains to abdominal pain, the same is not true for dyspnea.
Preeclampsia is characterized by hypertension (BP >140/90 mm Hg) and proteinuria; associated symptoms include edema and hyperreflexia. Postpartum preeclampsia occurs infrequently and can develop up to 4 weeks after delivery.1 In one 10-year retrospective case series, the incidence of preeclampsia in the postpartum period was 5.7%, and nearly 16% went on to develop eclampsia.2 In a retrospective study of 22 postpartum preeclamptic patients, the median time to presentation was 5 days postpartum.1 In a similar retrospective study of 152 patients, 90% of such patients presented within 7 days.3 The patient in this case initially presented on postpartum day 4.
Interestingly, in a study by Al-Safi et al,3 63% of postpartum preeclamptic patients had no antecedent diagnosis of hypertensive disease during pregnancy. These findings are consistent with the findings of others that 33% to 69% of such patients show no evidence of preeclampsia in the ante- or peripartum period.
The clinical presentation of postpartum preeclampsia is similar to preeclampsia complicating pregnancy after gestation week 20. In the study by Al-Safi et al,3 headache was the most common presenting symptom (69%), followed by shortness of breath (30%), blurry vision (21%), nausea (12.5%), and epigastric abdominal pain (5%). Similarly, Yancey et al1 found headache (82%) to be the most common presenting symptom in their series. Unfortunately, it is not known whether the patient in this case complained of headache or blurred vision as the published records note neither their presence nor absence.
The management of patients with preeclampsia includes IV magnesium to prevent seizures (ie, eclampsia) and BP control.1 A bolus of 4 to 6 g IV magnesium sulfate over 15 to 30 minutes is recommended, followed by an infusion of 2 g/h IV. Historically, IV hydralazine has been used to manage preeclamptic patients with a BP greater than 160/110 mm Hg. More recently, however, IV labetalol has become popular.5 All such patients require admission to the hospital with Ob/Gyn involvement.
Missed Subdural Hematoma
A 59-year-old man presented to the ED with a chief complaint of headache, the onset of which he stated started gradually 2 days prior. He noted the headache was worse than normal but without associated nausea, vomiting, fever, chills, or change in vision. His past medical history was significant for a lower extremity deep vein thrombosis 3 months prior, for which he was taking warfarin.
The patient’s vital signs were all normal. The physical examination, including a thorough neurological examination, was also normal. The EP ordered a prothrombin time (PT), an international normalized ratio (INR), and a noncontrast CT scan of the head. The PT/INR results were therapeutic at 22 seconds and 2.3. The CT scan was interpreted by radiology services as normal. The patient’s headache was treated with IV prochlorperazine and diphenhydramine. After treatment, the patient reported feeling better and was discharged home with instructions to follow up with his primary care physician.
Over the next several months, the patient presented to the same ED on seven different occasions, each time with the chief complaint of headache. At each of these presentations, the history and physical examination were documented as unremarkable, with no history of trauma. The thoroughness, however, of the documentation varied considerably for each ED encounter. No head CT scan was ordered on the subsequent seven visits, and at each presentation, the patient was treated symptomatically and discharged home.
Two days after his eighth visit to the same hospital ED, the patient presented to a different ED, again with a chief complaint of headache. The EP at this ED ordered a noncontrast CT of the head, which demonstrated a left subdural hematoma. The patient was admitted to the hospital, given IV vitamin K and fresh frozen plasma, and underwent evacuation of the hematoma by neurosurgery. The patient’s hospital course was unremarkable, and he was discharged home without any focal weakness.
The patient, however, claimed that he suffered cognitive impairment as a result of the missed diagnosis. He sued treating EPs at the first ED as well as the hospital for failure to timely diagnose the subdural hematoma, stating that a CT scan should have been performed at each of his ED visits since he was on warfarin. The defense claimed that a CT scan was not warranted for each visit, and that the timing of when and how the brain bleed started was uncertain. At trial, a defense verdict was returned.
Discussion
It is well known that patients receiving warfarin are at an increased risk for intracranial hemorrhage (ICH) following blunt head trauma.1 The recommendation is that all such patients have a noncontrast CT scan of the head to rule out intracranial bleeding. This is due to the fact that 60% of patients presenting with an immediate traumatic intracranial hemorrhage will have a normal mental status on examination; and 11% will have no history of loss of consciousness, a normal mental status examination, and no physical evidence of trauma above the clavicles.1 In a study by Hart et al,2 subdural hematoma accounted for 44% of all ICH in these types of patients.
More controversial is how to manage patients on warfarin who experience blunt head trauma and have a normal CT scan of the head. Because of the fear for delayed traumatic ICH, many clinicians recommend admitting such patients for neurological observation and repeat head CT scan the next morning.3 Additionally, some clinicians even recommend reversing the warfarin anticoagulation in such patients. 4 These recommendations, though, are based on expert consensus rather than on rigorous, prospective multicenter studies.1 These strategies are also problematic, since such multiple repeat CT scans would not only be incredibly expensive but also would expose the patient to high doses of radiation to the brain. Moreover, the Centers for Medicare and Medicaid Services has now made CT brain scan imaging of patients presenting to the ED with complaint of nontraumatic headache a quality measure they follow. Their goal is to decrease the number of “unnecessary” head CT scans.
The patient in this case denied any history of trauma on the subsequent seven ED visits. Unfortunately, as pointed out, even minor trauma can result in ICH, and patients may not recall the occurrence of the event.
For patients on warfarin who present with headache, a very careful history must be taken—including inquiring about minor traumatic events. Even then, as has been shown, patients may have not experienced a loss of consciousness, have a normal mental status examination, and exhibit no external evidence of head trauma. The clinician is forced to use her or his own best judgment when evaluating such patients in the ED.
Interestingly, the risk of ICH secondary to blunt head trauma in patients on warfarin is increased if they are on concomitant aspirin therapy.2 Similarly, the risk of ICH following head trauma in patients on clopidogrel is greater than for those patients taking warfarin,1 and the risk of ICH in patients taking dabigatran is less than if taking warfarin.2
Reference - Missed Preeclampsia
- Yancey LM, Withers E, Barnes K, Abbott J. Postpartum preeclampsia: emergency department presentation and management. J Emerg Med. 2011;40(4):380-384.
- Matthys LA, Coppage KH, Lambers DS, Barton JR, Sibai BM. Delayed postpartum preeclampsia: an experience of 151 cases. Am J Obstet Gynecol. 2004;190(5):1464-1466.
- Al-Safi Z, Imudia AN, Filetti LC, Hobson DT, Bahado-Singh RO, Awonuga AO. Delayed postpartum preeclampsia and eclampsia: demographics, clinical course, and complications. Obstet Gynecol. 2011;118(5):1102-1107.
- Chames MC, Livingston JC, Ivester TS, Barton JR, Sibai BM. Late postpartum eclampsia: a preventable disease? Am J Obstet Gynecol. 2002;186(6):1174-1177.
- Graeber B, Vanderwal T, Stiller RJ, Werdmann MJ. Late postpartum eclampsia as an obstetric complication seen in the ED. Am J Emerg Med. 2005;23(2):168-170.
Reference - Missed Subdural Hematoma
- Nishijima DK, Offerman SR, Ballard DW, et al; Clinical Research in Emergency Services and Treatment (CREST) Network. Immediate and delayed traumatic intracranial hemorrhage in patients with head trauma and preinjury warfarin or clopidogrel use. Ann Emerg Med. 2012;59(6):460-468.
- Hart RG, Diener HC, Yang S, Connolly SJ, Wallentin L, et al. Intracranial hemorrhage in atrial fibrillation patients during anticoagulation with warfarin or dabigatran: the RE-LY trial. Stroke. 2012;43(6): 1511-1517.
- Vos PE, Battistin L, Birbamer G, et al; European Federation of Neurological Societies. EFNS guideline on mild traumatic brain injury: report of an EFNS task force. Eur J Neurol. 2002;9(3):207-219.
- Coimbra R, Hoyt DB, Anjaria DJ, Potenza BM, Fortlage D, Hollingsworth-Fridlund P. Reversal of anticoagulation in trauma: a North-American survey on clinical practices among trauma surgeons. J Trauma. 2005;59(2):375-382.
Reference - Missed Preeclampsia
- Yancey LM, Withers E, Barnes K, Abbott J. Postpartum preeclampsia: emergency department presentation and management. J Emerg Med. 2011;40(4):380-384.
- Matthys LA, Coppage KH, Lambers DS, Barton JR, Sibai BM. Delayed postpartum preeclampsia: an experience of 151 cases. Am J Obstet Gynecol. 2004;190(5):1464-1466.
- Al-Safi Z, Imudia AN, Filetti LC, Hobson DT, Bahado-Singh RO, Awonuga AO. Delayed postpartum preeclampsia and eclampsia: demographics, clinical course, and complications. Obstet Gynecol. 2011;118(5):1102-1107.
- Chames MC, Livingston JC, Ivester TS, Barton JR, Sibai BM. Late postpartum eclampsia: a preventable disease? Am J Obstet Gynecol. 2002;186(6):1174-1177.
- Graeber B, Vanderwal T, Stiller RJ, Werdmann MJ. Late postpartum eclampsia as an obstetric complication seen in the ED. Am J Emerg Med. 2005;23(2):168-170.
Reference - Missed Subdural Hematoma
- Nishijima DK, Offerman SR, Ballard DW, et al; Clinical Research in Emergency Services and Treatment (CREST) Network. Immediate and delayed traumatic intracranial hemorrhage in patients with head trauma and preinjury warfarin or clopidogrel use. Ann Emerg Med. 2012;59(6):460-468.
- Hart RG, Diener HC, Yang S, Connolly SJ, Wallentin L, et al. Intracranial hemorrhage in atrial fibrillation patients during anticoagulation with warfarin or dabigatran: the RE-LY trial. Stroke. 2012;43(6): 1511-1517.
- Vos PE, Battistin L, Birbamer G, et al; European Federation of Neurological Societies. EFNS guideline on mild traumatic brain injury: report of an EFNS task force. Eur J Neurol. 2002;9(3):207-219.
- Coimbra R, Hoyt DB, Anjaria DJ, Potenza BM, Fortlage D, Hollingsworth-Fridlund P. Reversal of anticoagulation in trauma: a North-American survey on clinical practices among trauma surgeons. J Trauma. 2005;59(2):375-382.
Palliative Medicine in the ED
Overview
Palliative medicine in the ED represents a paradigm shift for the emergency physician (EP)—from identifying and stabilizing acute medical and surgical conditions to providing symptomatic comfort care to a dying patient. When the ED became the “safety net” for patients who have serious, life-limiting illnesses,1-3 it also became the most frequent place where such care is initially sought4—although not considered an ideal place to begin such care.
In one study, approximately 40% of dying patients presented to the ED during their final 2 weeks of life.5 With the ED becoming more recognized as a location for palliative care, the EP plays a key role in the care of these patients. The 2013 Model of the Clinical Practice of Emergency Medicine explicitly lists palliative medicine within the EP’s scope of practice.6 Further support for providing palliative care in emergency medicine includes the cosponsorship of Hospice and Palliative Medicine subspecialty board certification by the American Board of Emergency Medicine in 2008. Finally, palliative care medicine principles have been endorsed in the “Choosing Wisely” initiative of the American College of Emergency Physicians.
Essential Palliative Care Skills
Quest et al7 have identified the following 12 primary palliative care skills in which every EP should be competent:
- Assessment of illness trajectory;
- Determination of prognosis;
- Communication of bad news;
- Interpretation and formation of an advance care plan;
- Allowance of family presence during resuscitation;
- Symptom management (both pain and nonpain);
- Withholding and withdrawal of life-sustaining treatments;
- Management of imminently dying patients;
- Identification and implementation of hospice and palliative care plans;
- Understanding of ethical and legal issues pertinent to end-of-life care;
- Display of spiritual and cultural competency; and
- Management of the dying child.
Although all of the above are important skills, this paper focuses on the symptom management of pain and nonpain (skill 6) in patients presenting to the ED with a life-limiting illness. The evidence base for these treatments is limited due to the many methodological challenges faced when studying symptoms in patients who are at end of life.
Pharmacologic Management of Symptoms
Recent research has found that symptom burden is high at end of life. Despite the increase in attention to these patients and their needs, symptoms including pain, depression, and delirium have repeatedly increased between 1998 and 2010.8 A 2013 study recommended that a minimum of four classes of medications be considered for patients who are at end of life: opioid (for pain); benzodiazepine (for anxiety); antipsychotic (for delirium and nausea); and antimuscarinic (for excessive secretions).9 The role and indications for each of these drug classes will be discussed.
Palliative Care Intervention
Though EPs frequently request specialty and subspecialty consultation for ED patients, they usually do not consider a palliative care medicine consult for the dying patient. Palliative care medicine utilizes an interdisciplinary, collaborative, team-based approach to decrease the pain and suffering of patients with advanced illness.10
Benefits from early palliative care intervention in the ED include improved symptom management, improved patient and family satisfaction, improved outcomes, decreased length of stay, less use of intensive care units, and less costs.4
Pain Management
Pain is one of the most devastating symptoms that a patient can experience, and its management is an integral component of palliative care medicine. Initial evaluation must include appropriate assessment of the pain and its impact on a patient’s function and quality of life.
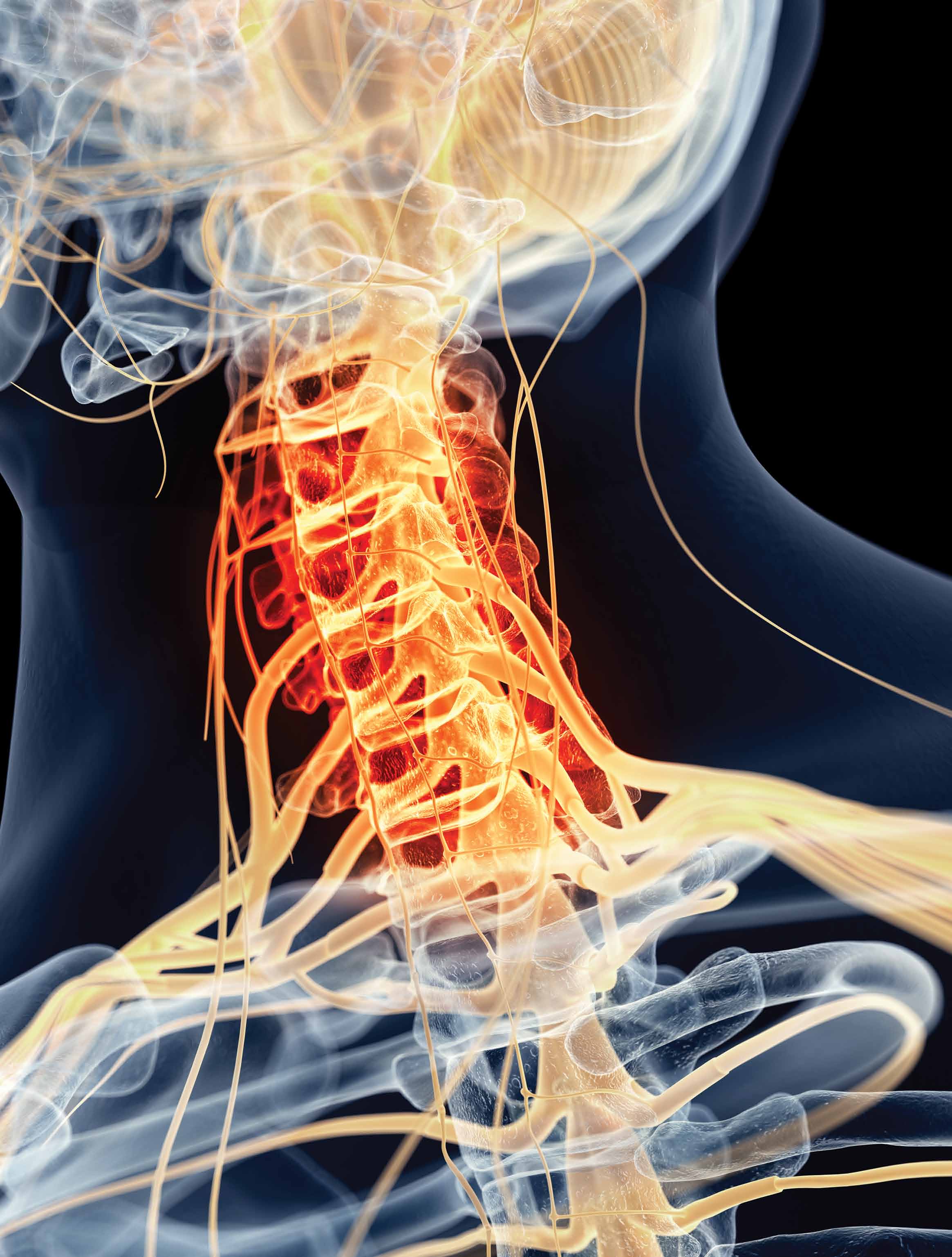
The general approach to pain management follows the World Health Organization pain ladder. For mild to moderate pain, step 1 begins with acetaminophen or a nonsteroidal anti-inflammatory drug (NSAID), with or without an adjuvant such as an antidepressant or anticonvulsant. If pain persists, step 2 involves the addition of an opioid. For moderate to severe pain, step 3 involves the addition of stronger opioids, such as hydromorphone, morphine, and oxycodone. Typically, a patient with a serious, life-limiting illness who presents to the ED for help will likely require treatment with strong opioids (step 3).
Opioids
In patients requiring step 3 management, opioids are the primary medication used to manage pain. An initial equivalent dose of morphine 5 mg intravenously (IV) is appropriate in an opioid-naïve patient. The adage of “starting low and going slow” is important to follow; however, an important corollary is “…and use enough.” If a patient’s pain is not controlled with initial dosages, additional bolus doses of 50% to 100% increments will be necessary. Because opioids do not have a ceiling effect, it is important to understand that dosages may seem very high for some patients compared to others. In this population, ensuring baseline pain control, with either an oral long-acting formulation or a continuous IV infusion, is important.11
Difficulties clinicians have in determining opioids for the management of pain are multifactorial. One consideration may be the growing public concern for prescription opioid abuse, potentially creating resistance to appropriate use of opioids by clinicians who fear legal or regulatory push back.
General principles in managing severe pain in the opioid-tolerant patient include the following: (1) calculating the morphine equivalent as a daily 24-hour dose; (2) determining the breakthrough dose, which is usually 10% to 15% of the calculated daily dose; (3) titrating doses upward if pain is not controlled, or if more than three breakthrough doses are being required daily; and (4) reducing the calculated conversion dose of a new opioid 25% to 50% when converting to a different opioid.12
The EP is frequently required to convert a patient’s oral opioid analgesic to an equivalent IV dose, and hydromorphone and morphine are the two most commonly used. The Table provides an approximation for this conversion.
Equianalgesic Dosing
Equianalgesic dosing is an important concept in pain management, especially for those patients already receiving opioids. There is great variation in the analgesic potency of the different opioids. The dose at which two opioids provide equivalent pain relief is the equianalgesic dose. Usually, this is standardized to 10 mg of parenteral morphine.13 Unfortunately, it is not uncommon for patients to be undertreated when switched to another opioid.
Nonpain Symptom Management
Nonpain symptoms that all EPs must know how to manage include constipation, dyspnea, nausea/vomiting, the so-called death rattle, and terminal delirium. In one study of reasons for ED visits by palliative care patients, the most common were dyspnea (26%), nausea/vomiting/constipation (17%), and uncontrolled pain (15%).14
Constipation
The most important adverse effect of opioids—one that does not improve or change during treatment—is constipation. Constipation in general—not just associated with opioids—has been ranked as one of the 10 most bothersome symptoms in the palliative care population, leading to discomfort, decreased quality of life, and potential small bowel obstruction or perforation.15 Unless contraindicated, a gastrointestinal stimulant such as senna, or an osmotic laxative such as lactulose, must be prescribed whenever an opioid is initiated. As the author (Galicia-Castillo) often notes, “The hand that writes the prescription for an opioid should be the hand that writes an Rx for a bowel regimen, or it becomes the hand that disimpacts the patient.”
The most recent Cochrane Review for the management of constipation in the palliative care population did not show any differences in the effectiveness among three commonly used laxatives: senna, docusate, and lactulose. This review did not evaluate polyethylene glycol, which is also commonly used.16 The addition of stool softeners, bisacodyl and nightly prune juice can also be helpful.10
Dyspnea
Dyspnea, the subjective feeling of breathing discomfort, is a common end-of-life complaint. Similar to pain, self-report is required for adequate assessment of dyspnea. Treatment recommendations include opioids, anxiolytics, and oxygen therapy.18 Opioids are the most widely studied treatment for dyspnea, demonstrating reduction in breathlessness in patients who have a variety of conditions, such as advanced chronic obstructive pulmonary disease, interstitial lung disease, cancer, and chronic heart failure.19
While many of the benefits of opioids are widely recognized and understood, the manner in which they improve symptoms of dyspnea is less well known. In addition, the evidence of effectiveness is limited to oral or parenteral morphine and fentanyl, and nebulized opioids have not been well studied. Oxygen treatments have been shown to reduce dyspnea in patients who suffer from hypoxemia; however, no benefit was found for patients who had only mild or no hypoxemia. A majority of dying patients did not experience a change in respiratory comfort after their supplemental oxygen was withdrawn. In these cases, when administration of oxygen is unnecessary, it may potentially introduce further discomfort to end-of-life patients by causing nasal dryness and impaired mobility.20
The use of benzodiazepines as the primary medication to manage dyspnea is unfounded, but may provide some benefit when used in conjunction with opioids.11 When indicated, a longer-acting agent (eg, clonazepam, with an initial starting does of 0.25 mg orally every 12 hours) may be used.4
Nausea and Vomiting
Nausea and vomiting have been reported by 16% to 68% of patients who had life-limiting illness, such as cancer, heart failure, renal failure, or acquired immunodeficiency syndrome.21 The etiology of nausea and vomiting is multifactorial in a dying patient. Assessment and treatment has been based on understanding how neurotransmitters are involved in the “emetic pathway,”22 but other pathways, such as a cytokine-mediated model of cancer symptoms, may also be important.23
Nonpharmacologic methods to utilize include avoidance of environmental stimuli, such as fatty, spicy, and salted foods; use of relaxation and distraction; and massage.22 Several medication classes have been utilized to treat nausea and vomiting: prokinetic agents (metoclopramide 10 mg three to four times a day, 30 minutes prior to meals and bedtime); dopamine receptor antagonists (haloperidol 1.5-5 mg two to three times a day); antihistaminic agents (promethazine 25 mg orally or IV every 4-6 hours, with a maximum dose of 100 mg/d); and selective 5 hydroxytryptamine-3 receptor antagonists (ondansetron 4-8 mg once or twice a day). Other agents that have been utilized include corticosteroids, benzodiazepines, octreotide, and cannabinoids.22
Procedures such as percutaneous endoscopic gastrostomy placement, nasogastric tube placement, and stenting may be necessary for patients who have advanced disease caused by a mechanical obstruction.22
Death Rattle
The death rattle occurs when secretions accumulate in the pharynx and/or airways when swallowing and cough mechanisms are no longer intact.24 This phenomenon occurs in 23% to 92% of dying patients.25 Generally, death occurs within 48 hours for about 75% of such patients.26 The noise that results from this process is usually more disturbing for those visiting the patients than to the patient themselves. Conservative measures to employ include placing patients on their sides to facilitate secretion drainage and to minimize upper airway sounds, gentle oral and pharyngeal suctioning, and limiting fluid input.11
One recent study reviewing the use of the anticholinergics atropine, scopolamine, and hyoscine demonstrated similar efficacy among the three drugs. Dosages used in this study included atropine 0.5 mg as a subcutaneous bolus, followed by 3 mg every 24 hours subcutaneously; scopolamine as a 0.25 mg subcutaneous bolus, followed by 1.5 mg every 24 hours IV or by subcutaneous infusion; and hyoscine 20 mg as a subcutaneous bolus followed by 60 mg every 24 hours IV or subcutaneous infusion. Glycopyrrolate is often used in the cognitively intact patient, as it does not cross the blood-brain barrier; however, supply concerns at the time of the study prevented a review of its efficiency.27 All of these medications are also available in oral and transdermal formulations.
Terminal Delirium
Delirium is a common complication for patients nearing the end of life, affecting as many as 88% of dying patients.28 It is characterized by an acute onset of cognitive impairment that may manifest as either a hyperactive or hypoactive state. Causes for terminal delirium are multifactorial. Initially, management should include prevention strategies, such as frequently orientating the patient, maintenance of day-night cycles, provision of adequate sleep, and minimization of sensory overload.11 When pharmacological therapy is required to improve quality of life, a neuroleptic medication, namely haloperidol, should be used initially. The addition of a benzodiazepine may help if the initial treatments are ineffective, or if sedation is desired.28
Summary
Emergency physicians have a unique opportunity to improve the quality of life for patients suffering serious illness, especially those who are actively dying. The management of pain and nonpain symptoms in patients who are at end of life, is a particularly important skill for every EP. If available, a consultation with a palliative care medicine consultant may improve both short- and long-term patient care.
Dr Galicia-Castillo is the Sue Faulkner Scribner professor of geriatrics at the Eastern Virginia Medical School Glennan Center for Geriatrics and Gerontology, and Medical Director for Palliative Care Medicine at Sentara Norfolk General Hospital. Dr Counselman is the distinguished professor and chairman of the department of emergency medicine at Eastern Virginia Medical School, Norfolk; and a physician at Emergency Physicians of Tidewater, Norfolk, Virginia. He is also the associate editor in chief of EMERGENCY MEDICINE editorial board.
- Alsirafy SA, Raheem AA, Al-Zahrani AS, et al. Emergency department visits at the end of life of patients with terminal cancer: pattern, causes, and avoidability. Am J Hosp Palliat Care. 2015:1049909115581819. [Epub ahead of print].
- Grudzen CR, Richardson LD, Morrison M, Cho E, Morrison RS. Palliative care needs of seriously ill, older adults presenting to the emergency department. Acad Emerg Med. 2010;17(11):1253-1257.
- Smith AK, Schonberg MA, Fisher J, et al. Emergency department experiences of acutely symptomatic patients with terminal illness and their family caregivers. J Pain Symptom Manage. 2010;39(6):972-981.
- Mierendorf S, Gidvani V. Palliative care in the emergency department. Perm J. 2014;18(2):77-85.
- Barbera L, Taylor C, Dudgeon D. Why do patients with cancer visit the emergency department near the end of life? CMAJ. 2010;182(6): 563-568.
- Counselman FL, Borenstein MA, Chisholm CD, et al; EM Model Review Task Force; American Board of Emergency Medicine. The 2013 Model of the Clinical Practice of Emergency Medicine. Acad Emerg Med. 2014;21(5):574-598.
- Quest TE, Marco CA, Derse AR. Hospice and palliative medicine: new subspecialty, new opportunities. Ann Emerg Med. 2009;54(1):94-102.
- Singer AE, Meeker D, Teno JM, Lynn J, Lunney JR, Lorenz KA. Symptom trends in the last year of life from 1998 to 2010: a cohort study. Ann Intern Med. 2015;162(3):175-183.
- Lindqvist O, Lundquist G, Dickman A, et al; OPCARE9. Four essential drugs needed for quality care of the dying: a Delphi-study based international expert consensus opinion. J Palliat Med. 2013;16(1):38-43.
- Kandarian B, Morrison RS, Richardson LD, Ortiz J, Grudzen CR. Emergency department-initiated palliative care for advanced cancer patients: protocol for a pilot randomized controlled trial. Trials. 2014;15:251.
- Campbell ML. Caring for dying patients in the intensive care unit: managing pain, dyspnea, anxiety, delirium, and death rattle. AACN Adv Crit Care. 2015;26(2):110-120.
- Lamba S, Quest TE. Hospice care and the emergency department: rules, regulations, and referrals. Ann Emerg Med. 2011;57(3):282-290.
- Shaheen PE, Walsh D, Lasheen W, Davis MP, Lagman RL. Opioid equianalgesic tables: are they all equally dangerous? J Pain Symptom Manage.2009;38(3):409-417.
- Wallace EM, Cooney MC, Walsh J, Conroy M, Twomey F. Why do palliative care patients present to the emergency department? Avoidable or unavoidable? Am J Hosp Palliat Care. 2013;30(3):253-253.
- Erichsén E, Milberg A, Jaarsma T, Friedrichsen MJ. Constipation in specialized palliative care: prevalence, definition, and patient-perceived symptom distress. J Palliat Med. 2015;18(7):585-592.
- Candy B, Jones L, Larkin PJ, Vickerstaff V, Tookman A, Stone P. Laxatives for the management of constipation in people receiving palliative care. Cochrane Database Syst Rev. 2015;5:CD003448.
- Parshall MB, Schwartzstein RM, Adams L, et al; American Thoracic Society Committee on Dyspnea. An official American Thoracic Society statement: update on the mechanisms, assessment, and management of dyspnea. Am J Respir Crit Care Med. 2012;185(4):435-452.
- LeGrand SB, Khawam EA, Walsh D, Rivera NI. Opioids, respiratory function, and dyspnea. Am J Hosp Palliat Care. 2003;20(1):57-61.
- Meek PM, Schwartzstein R, Adams L, el al. Dyspnea. Mechanisms, assessment, and management: a consensus statement. American Thoracic Society. Am J Respir Crit Care Med. 1999;159(1):321-340.
- Campbell ML, Yarandi H, Dove-Medows E. Oxygen is nonbeneficial for most patients who are near death. J Pain Symptom Manage. 2013;45(3):517-523.
- Solano JP, Gomes B, Higginson IJ. A comparison of symptom prevalence in far advanced cancer, AIDS, heart disease, chronic obstructive pulmonary disease and renal disease. J Pain Symptom Manage. 2006;31(1):58-69.
- Glare P, Miller J, Nikolova T, Tickoo R. Treating nausea and vomiting in palliative care: a review. Clin Interv Aging. 2011;6:243-259.
- Cleeland CS, Bennett GJ, Dantzer R, et al. Are the symptoms of cancer and cancer treatment due to a shared biologic mechanism? A cytokine-immunologic model of cancer symptoms. Cancer. 2003;97(11):2919-2925.
- Bennett M, Lucas V, Brennan M, Hughes A, O’Donnell V, Wee B; Association for Palliative Medicine’s Science Committee. Using anti-muscarinic drugs in the management of death rattle: evidence-based guidelines for palliative care. Palliat Med. 2002;16(5):369-374.
- Mercadamte S. Death rattle: critical review and research agenda. Support Care Cancer. 2014;22(2):
- 571-575.
- Wildiers H, Menten J. Death rattle: prevalence, prevention and treatment. J Pain Symptom Manage. 2002;23(4):310-317.
- Wildiers H, Dhaenekint C, Demeulenaere P, et al; Flemish Federation of Palliative Care. Atropine, hyoscine butylbromide, or scopolamine are equally effective for the treatment of death rattle in terminal care. J Pain Symptom Manage. 2009;38(1):124-133.
- Kehl KA. Treatment of terminal restlessness: a review of the evidence. J Pain Palliat Care Pharmacother. 2004;18(1):5-30.
Overview
Palliative medicine in the ED represents a paradigm shift for the emergency physician (EP)—from identifying and stabilizing acute medical and surgical conditions to providing symptomatic comfort care to a dying patient. When the ED became the “safety net” for patients who have serious, life-limiting illnesses,1-3 it also became the most frequent place where such care is initially sought4—although not considered an ideal place to begin such care.
In one study, approximately 40% of dying patients presented to the ED during their final 2 weeks of life.5 With the ED becoming more recognized as a location for palliative care, the EP plays a key role in the care of these patients. The 2013 Model of the Clinical Practice of Emergency Medicine explicitly lists palliative medicine within the EP’s scope of practice.6 Further support for providing palliative care in emergency medicine includes the cosponsorship of Hospice and Palliative Medicine subspecialty board certification by the American Board of Emergency Medicine in 2008. Finally, palliative care medicine principles have been endorsed in the “Choosing Wisely” initiative of the American College of Emergency Physicians.
Essential Palliative Care Skills
Quest et al7 have identified the following 12 primary palliative care skills in which every EP should be competent:
- Assessment of illness trajectory;
- Determination of prognosis;
- Communication of bad news;
- Interpretation and formation of an advance care plan;
- Allowance of family presence during resuscitation;
- Symptom management (both pain and nonpain);
- Withholding and withdrawal of life-sustaining treatments;
- Management of imminently dying patients;
- Identification and implementation of hospice and palliative care plans;
- Understanding of ethical and legal issues pertinent to end-of-life care;
- Display of spiritual and cultural competency; and
- Management of the dying child.
Although all of the above are important skills, this paper focuses on the symptom management of pain and nonpain (skill 6) in patients presenting to the ED with a life-limiting illness. The evidence base for these treatments is limited due to the many methodological challenges faced when studying symptoms in patients who are at end of life.
Pharmacologic Management of Symptoms
Recent research has found that symptom burden is high at end of life. Despite the increase in attention to these patients and their needs, symptoms including pain, depression, and delirium have repeatedly increased between 1998 and 2010.8 A 2013 study recommended that a minimum of four classes of medications be considered for patients who are at end of life: opioid (for pain); benzodiazepine (for anxiety); antipsychotic (for delirium and nausea); and antimuscarinic (for excessive secretions).9 The role and indications for each of these drug classes will be discussed.
Palliative Care Intervention
Though EPs frequently request specialty and subspecialty consultation for ED patients, they usually do not consider a palliative care medicine consult for the dying patient. Palliative care medicine utilizes an interdisciplinary, collaborative, team-based approach to decrease the pain and suffering of patients with advanced illness.10
Benefits from early palliative care intervention in the ED include improved symptom management, improved patient and family satisfaction, improved outcomes, decreased length of stay, less use of intensive care units, and less costs.4
Pain Management
Pain is one of the most devastating symptoms that a patient can experience, and its management is an integral component of palliative care medicine. Initial evaluation must include appropriate assessment of the pain and its impact on a patient’s function and quality of life.
The general approach to pain management follows the World Health Organization pain ladder. For mild to moderate pain, step 1 begins with acetaminophen or a nonsteroidal anti-inflammatory drug (NSAID), with or without an adjuvant such as an antidepressant or anticonvulsant. If pain persists, step 2 involves the addition of an opioid. For moderate to severe pain, step 3 involves the addition of stronger opioids, such as hydromorphone, morphine, and oxycodone. Typically, a patient with a serious, life-limiting illness who presents to the ED for help will likely require treatment with strong opioids (step 3).
Opioids
In patients requiring step 3 management, opioids are the primary medication used to manage pain. An initial equivalent dose of morphine 5 mg intravenously (IV) is appropriate in an opioid-naïve patient. The adage of “starting low and going slow” is important to follow; however, an important corollary is “…and use enough.” If a patient’s pain is not controlled with initial dosages, additional bolus doses of 50% to 100% increments will be necessary. Because opioids do not have a ceiling effect, it is important to understand that dosages may seem very high for some patients compared to others. In this population, ensuring baseline pain control, with either an oral long-acting formulation or a continuous IV infusion, is important.11
Difficulties clinicians have in determining opioids for the management of pain are multifactorial. One consideration may be the growing public concern for prescription opioid abuse, potentially creating resistance to appropriate use of opioids by clinicians who fear legal or regulatory push back.
General principles in managing severe pain in the opioid-tolerant patient include the following: (1) calculating the morphine equivalent as a daily 24-hour dose; (2) determining the breakthrough dose, which is usually 10% to 15% of the calculated daily dose; (3) titrating doses upward if pain is not controlled, or if more than three breakthrough doses are being required daily; and (4) reducing the calculated conversion dose of a new opioid 25% to 50% when converting to a different opioid.12
The EP is frequently required to convert a patient’s oral opioid analgesic to an equivalent IV dose, and hydromorphone and morphine are the two most commonly used. The Table provides an approximation for this conversion.
Equianalgesic Dosing
Equianalgesic dosing is an important concept in pain management, especially for those patients already receiving opioids. There is great variation in the analgesic potency of the different opioids. The dose at which two opioids provide equivalent pain relief is the equianalgesic dose. Usually, this is standardized to 10 mg of parenteral morphine.13 Unfortunately, it is not uncommon for patients to be undertreated when switched to another opioid.
Nonpain Symptom Management
Nonpain symptoms that all EPs must know how to manage include constipation, dyspnea, nausea/vomiting, the so-called death rattle, and terminal delirium. In one study of reasons for ED visits by palliative care patients, the most common were dyspnea (26%), nausea/vomiting/constipation (17%), and uncontrolled pain (15%).14
Constipation
The most important adverse effect of opioids—one that does not improve or change during treatment—is constipation. Constipation in general—not just associated with opioids—has been ranked as one of the 10 most bothersome symptoms in the palliative care population, leading to discomfort, decreased quality of life, and potential small bowel obstruction or perforation.15 Unless contraindicated, a gastrointestinal stimulant such as senna, or an osmotic laxative such as lactulose, must be prescribed whenever an opioid is initiated. As the author (Galicia-Castillo) often notes, “The hand that writes the prescription for an opioid should be the hand that writes an Rx for a bowel regimen, or it becomes the hand that disimpacts the patient.”
The most recent Cochrane Review for the management of constipation in the palliative care population did not show any differences in the effectiveness among three commonly used laxatives: senna, docusate, and lactulose. This review did not evaluate polyethylene glycol, which is also commonly used.16 The addition of stool softeners, bisacodyl and nightly prune juice can also be helpful.10
Dyspnea
Dyspnea, the subjective feeling of breathing discomfort, is a common end-of-life complaint. Similar to pain, self-report is required for adequate assessment of dyspnea. Treatment recommendations include opioids, anxiolytics, and oxygen therapy.18 Opioids are the most widely studied treatment for dyspnea, demonstrating reduction in breathlessness in patients who have a variety of conditions, such as advanced chronic obstructive pulmonary disease, interstitial lung disease, cancer, and chronic heart failure.19
While many of the benefits of opioids are widely recognized and understood, the manner in which they improve symptoms of dyspnea is less well known. In addition, the evidence of effectiveness is limited to oral or parenteral morphine and fentanyl, and nebulized opioids have not been well studied. Oxygen treatments have been shown to reduce dyspnea in patients who suffer from hypoxemia; however, no benefit was found for patients who had only mild or no hypoxemia. A majority of dying patients did not experience a change in respiratory comfort after their supplemental oxygen was withdrawn. In these cases, when administration of oxygen is unnecessary, it may potentially introduce further discomfort to end-of-life patients by causing nasal dryness and impaired mobility.20
The use of benzodiazepines as the primary medication to manage dyspnea is unfounded, but may provide some benefit when used in conjunction with opioids.11 When indicated, a longer-acting agent (eg, clonazepam, with an initial starting does of 0.25 mg orally every 12 hours) may be used.4
Nausea and Vomiting
Nausea and vomiting have been reported by 16% to 68% of patients who had life-limiting illness, such as cancer, heart failure, renal failure, or acquired immunodeficiency syndrome.21 The etiology of nausea and vomiting is multifactorial in a dying patient. Assessment and treatment has been based on understanding how neurotransmitters are involved in the “emetic pathway,”22 but other pathways, such as a cytokine-mediated model of cancer symptoms, may also be important.23
Nonpharmacologic methods to utilize include avoidance of environmental stimuli, such as fatty, spicy, and salted foods; use of relaxation and distraction; and massage.22 Several medication classes have been utilized to treat nausea and vomiting: prokinetic agents (metoclopramide 10 mg three to four times a day, 30 minutes prior to meals and bedtime); dopamine receptor antagonists (haloperidol 1.5-5 mg two to three times a day); antihistaminic agents (promethazine 25 mg orally or IV every 4-6 hours, with a maximum dose of 100 mg/d); and selective 5 hydroxytryptamine-3 receptor antagonists (ondansetron 4-8 mg once or twice a day). Other agents that have been utilized include corticosteroids, benzodiazepines, octreotide, and cannabinoids.22
Procedures such as percutaneous endoscopic gastrostomy placement, nasogastric tube placement, and stenting may be necessary for patients who have advanced disease caused by a mechanical obstruction.22
Death Rattle
The death rattle occurs when secretions accumulate in the pharynx and/or airways when swallowing and cough mechanisms are no longer intact.24 This phenomenon occurs in 23% to 92% of dying patients.25 Generally, death occurs within 48 hours for about 75% of such patients.26 The noise that results from this process is usually more disturbing for those visiting the patients than to the patient themselves. Conservative measures to employ include placing patients on their sides to facilitate secretion drainage and to minimize upper airway sounds, gentle oral and pharyngeal suctioning, and limiting fluid input.11
One recent study reviewing the use of the anticholinergics atropine, scopolamine, and hyoscine demonstrated similar efficacy among the three drugs. Dosages used in this study included atropine 0.5 mg as a subcutaneous bolus, followed by 3 mg every 24 hours subcutaneously; scopolamine as a 0.25 mg subcutaneous bolus, followed by 1.5 mg every 24 hours IV or by subcutaneous infusion; and hyoscine 20 mg as a subcutaneous bolus followed by 60 mg every 24 hours IV or subcutaneous infusion. Glycopyrrolate is often used in the cognitively intact patient, as it does not cross the blood-brain barrier; however, supply concerns at the time of the study prevented a review of its efficiency.27 All of these medications are also available in oral and transdermal formulations.
Terminal Delirium
Delirium is a common complication for patients nearing the end of life, affecting as many as 88% of dying patients.28 It is characterized by an acute onset of cognitive impairment that may manifest as either a hyperactive or hypoactive state. Causes for terminal delirium are multifactorial. Initially, management should include prevention strategies, such as frequently orientating the patient, maintenance of day-night cycles, provision of adequate sleep, and minimization of sensory overload.11 When pharmacological therapy is required to improve quality of life, a neuroleptic medication, namely haloperidol, should be used initially. The addition of a benzodiazepine may help if the initial treatments are ineffective, or if sedation is desired.28
Summary
Emergency physicians have a unique opportunity to improve the quality of life for patients suffering serious illness, especially those who are actively dying. The management of pain and nonpain symptoms in patients who are at end of life, is a particularly important skill for every EP. If available, a consultation with a palliative care medicine consultant may improve both short- and long-term patient care.
Dr Galicia-Castillo is the Sue Faulkner Scribner professor of geriatrics at the Eastern Virginia Medical School Glennan Center for Geriatrics and Gerontology, and Medical Director for Palliative Care Medicine at Sentara Norfolk General Hospital. Dr Counselman is the distinguished professor and chairman of the department of emergency medicine at Eastern Virginia Medical School, Norfolk; and a physician at Emergency Physicians of Tidewater, Norfolk, Virginia. He is also the associate editor in chief of EMERGENCY MEDICINE editorial board.
Overview
Palliative medicine in the ED represents a paradigm shift for the emergency physician (EP)—from identifying and stabilizing acute medical and surgical conditions to providing symptomatic comfort care to a dying patient. When the ED became the “safety net” for patients who have serious, life-limiting illnesses,1-3 it also became the most frequent place where such care is initially sought4—although not considered an ideal place to begin such care.
In one study, approximately 40% of dying patients presented to the ED during their final 2 weeks of life.5 With the ED becoming more recognized as a location for palliative care, the EP plays a key role in the care of these patients. The 2013 Model of the Clinical Practice of Emergency Medicine explicitly lists palliative medicine within the EP’s scope of practice.6 Further support for providing palliative care in emergency medicine includes the cosponsorship of Hospice and Palliative Medicine subspecialty board certification by the American Board of Emergency Medicine in 2008. Finally, palliative care medicine principles have been endorsed in the “Choosing Wisely” initiative of the American College of Emergency Physicians.
Essential Palliative Care Skills
Quest et al7 have identified the following 12 primary palliative care skills in which every EP should be competent:
- Assessment of illness trajectory;
- Determination of prognosis;
- Communication of bad news;
- Interpretation and formation of an advance care plan;
- Allowance of family presence during resuscitation;
- Symptom management (both pain and nonpain);
- Withholding and withdrawal of life-sustaining treatments;
- Management of imminently dying patients;
- Identification and implementation of hospice and palliative care plans;
- Understanding of ethical and legal issues pertinent to end-of-life care;
- Display of spiritual and cultural competency; and
- Management of the dying child.
Although all of the above are important skills, this paper focuses on the symptom management of pain and nonpain (skill 6) in patients presenting to the ED with a life-limiting illness. The evidence base for these treatments is limited due to the many methodological challenges faced when studying symptoms in patients who are at end of life.
Pharmacologic Management of Symptoms
Recent research has found that symptom burden is high at end of life. Despite the increase in attention to these patients and their needs, symptoms including pain, depression, and delirium have repeatedly increased between 1998 and 2010.8 A 2013 study recommended that a minimum of four classes of medications be considered for patients who are at end of life: opioid (for pain); benzodiazepine (for anxiety); antipsychotic (for delirium and nausea); and antimuscarinic (for excessive secretions).9 The role and indications for each of these drug classes will be discussed.
Palliative Care Intervention
Though EPs frequently request specialty and subspecialty consultation for ED patients, they usually do not consider a palliative care medicine consult for the dying patient. Palliative care medicine utilizes an interdisciplinary, collaborative, team-based approach to decrease the pain and suffering of patients with advanced illness.10
Benefits from early palliative care intervention in the ED include improved symptom management, improved patient and family satisfaction, improved outcomes, decreased length of stay, less use of intensive care units, and less costs.4
Pain Management
Pain is one of the most devastating symptoms that a patient can experience, and its management is an integral component of palliative care medicine. Initial evaluation must include appropriate assessment of the pain and its impact on a patient’s function and quality of life.
The general approach to pain management follows the World Health Organization pain ladder. For mild to moderate pain, step 1 begins with acetaminophen or a nonsteroidal anti-inflammatory drug (NSAID), with or without an adjuvant such as an antidepressant or anticonvulsant. If pain persists, step 2 involves the addition of an opioid. For moderate to severe pain, step 3 involves the addition of stronger opioids, such as hydromorphone, morphine, and oxycodone. Typically, a patient with a serious, life-limiting illness who presents to the ED for help will likely require treatment with strong opioids (step 3).
Opioids
In patients requiring step 3 management, opioids are the primary medication used to manage pain. An initial equivalent dose of morphine 5 mg intravenously (IV) is appropriate in an opioid-naïve patient. The adage of “starting low and going slow” is important to follow; however, an important corollary is “…and use enough.” If a patient’s pain is not controlled with initial dosages, additional bolus doses of 50% to 100% increments will be necessary. Because opioids do not have a ceiling effect, it is important to understand that dosages may seem very high for some patients compared to others. In this population, ensuring baseline pain control, with either an oral long-acting formulation or a continuous IV infusion, is important.11
Difficulties clinicians have in determining opioids for the management of pain are multifactorial. One consideration may be the growing public concern for prescription opioid abuse, potentially creating resistance to appropriate use of opioids by clinicians who fear legal or regulatory push back.
General principles in managing severe pain in the opioid-tolerant patient include the following: (1) calculating the morphine equivalent as a daily 24-hour dose; (2) determining the breakthrough dose, which is usually 10% to 15% of the calculated daily dose; (3) titrating doses upward if pain is not controlled, or if more than three breakthrough doses are being required daily; and (4) reducing the calculated conversion dose of a new opioid 25% to 50% when converting to a different opioid.12
The EP is frequently required to convert a patient’s oral opioid analgesic to an equivalent IV dose, and hydromorphone and morphine are the two most commonly used. The Table provides an approximation for this conversion.
Equianalgesic Dosing
Equianalgesic dosing is an important concept in pain management, especially for those patients already receiving opioids. There is great variation in the analgesic potency of the different opioids. The dose at which two opioids provide equivalent pain relief is the equianalgesic dose. Usually, this is standardized to 10 mg of parenteral morphine.13 Unfortunately, it is not uncommon for patients to be undertreated when switched to another opioid.
Nonpain Symptom Management
Nonpain symptoms that all EPs must know how to manage include constipation, dyspnea, nausea/vomiting, the so-called death rattle, and terminal delirium. In one study of reasons for ED visits by palliative care patients, the most common were dyspnea (26%), nausea/vomiting/constipation (17%), and uncontrolled pain (15%).14
Constipation
The most important adverse effect of opioids—one that does not improve or change during treatment—is constipation. Constipation in general—not just associated with opioids—has been ranked as one of the 10 most bothersome symptoms in the palliative care population, leading to discomfort, decreased quality of life, and potential small bowel obstruction or perforation.15 Unless contraindicated, a gastrointestinal stimulant such as senna, or an osmotic laxative such as lactulose, must be prescribed whenever an opioid is initiated. As the author (Galicia-Castillo) often notes, “The hand that writes the prescription for an opioid should be the hand that writes an Rx for a bowel regimen, or it becomes the hand that disimpacts the patient.”
The most recent Cochrane Review for the management of constipation in the palliative care population did not show any differences in the effectiveness among three commonly used laxatives: senna, docusate, and lactulose. This review did not evaluate polyethylene glycol, which is also commonly used.16 The addition of stool softeners, bisacodyl and nightly prune juice can also be helpful.10
Dyspnea
Dyspnea, the subjective feeling of breathing discomfort, is a common end-of-life complaint. Similar to pain, self-report is required for adequate assessment of dyspnea. Treatment recommendations include opioids, anxiolytics, and oxygen therapy.18 Opioids are the most widely studied treatment for dyspnea, demonstrating reduction in breathlessness in patients who have a variety of conditions, such as advanced chronic obstructive pulmonary disease, interstitial lung disease, cancer, and chronic heart failure.19
While many of the benefits of opioids are widely recognized and understood, the manner in which they improve symptoms of dyspnea is less well known. In addition, the evidence of effectiveness is limited to oral or parenteral morphine and fentanyl, and nebulized opioids have not been well studied. Oxygen treatments have been shown to reduce dyspnea in patients who suffer from hypoxemia; however, no benefit was found for patients who had only mild or no hypoxemia. A majority of dying patients did not experience a change in respiratory comfort after their supplemental oxygen was withdrawn. In these cases, when administration of oxygen is unnecessary, it may potentially introduce further discomfort to end-of-life patients by causing nasal dryness and impaired mobility.20
The use of benzodiazepines as the primary medication to manage dyspnea is unfounded, but may provide some benefit when used in conjunction with opioids.11 When indicated, a longer-acting agent (eg, clonazepam, with an initial starting does of 0.25 mg orally every 12 hours) may be used.4
Nausea and Vomiting
Nausea and vomiting have been reported by 16% to 68% of patients who had life-limiting illness, such as cancer, heart failure, renal failure, or acquired immunodeficiency syndrome.21 The etiology of nausea and vomiting is multifactorial in a dying patient. Assessment and treatment has been based on understanding how neurotransmitters are involved in the “emetic pathway,”22 but other pathways, such as a cytokine-mediated model of cancer symptoms, may also be important.23
Nonpharmacologic methods to utilize include avoidance of environmental stimuli, such as fatty, spicy, and salted foods; use of relaxation and distraction; and massage.22 Several medication classes have been utilized to treat nausea and vomiting: prokinetic agents (metoclopramide 10 mg three to four times a day, 30 minutes prior to meals and bedtime); dopamine receptor antagonists (haloperidol 1.5-5 mg two to three times a day); antihistaminic agents (promethazine 25 mg orally or IV every 4-6 hours, with a maximum dose of 100 mg/d); and selective 5 hydroxytryptamine-3 receptor antagonists (ondansetron 4-8 mg once or twice a day). Other agents that have been utilized include corticosteroids, benzodiazepines, octreotide, and cannabinoids.22
Procedures such as percutaneous endoscopic gastrostomy placement, nasogastric tube placement, and stenting may be necessary for patients who have advanced disease caused by a mechanical obstruction.22
Death Rattle
The death rattle occurs when secretions accumulate in the pharynx and/or airways when swallowing and cough mechanisms are no longer intact.24 This phenomenon occurs in 23% to 92% of dying patients.25 Generally, death occurs within 48 hours for about 75% of such patients.26 The noise that results from this process is usually more disturbing for those visiting the patients than to the patient themselves. Conservative measures to employ include placing patients on their sides to facilitate secretion drainage and to minimize upper airway sounds, gentle oral and pharyngeal suctioning, and limiting fluid input.11
One recent study reviewing the use of the anticholinergics atropine, scopolamine, and hyoscine demonstrated similar efficacy among the three drugs. Dosages used in this study included atropine 0.5 mg as a subcutaneous bolus, followed by 3 mg every 24 hours subcutaneously; scopolamine as a 0.25 mg subcutaneous bolus, followed by 1.5 mg every 24 hours IV or by subcutaneous infusion; and hyoscine 20 mg as a subcutaneous bolus followed by 60 mg every 24 hours IV or subcutaneous infusion. Glycopyrrolate is often used in the cognitively intact patient, as it does not cross the blood-brain barrier; however, supply concerns at the time of the study prevented a review of its efficiency.27 All of these medications are also available in oral and transdermal formulations.
Terminal Delirium
Delirium is a common complication for patients nearing the end of life, affecting as many as 88% of dying patients.28 It is characterized by an acute onset of cognitive impairment that may manifest as either a hyperactive or hypoactive state. Causes for terminal delirium are multifactorial. Initially, management should include prevention strategies, such as frequently orientating the patient, maintenance of day-night cycles, provision of adequate sleep, and minimization of sensory overload.11 When pharmacological therapy is required to improve quality of life, a neuroleptic medication, namely haloperidol, should be used initially. The addition of a benzodiazepine may help if the initial treatments are ineffective, or if sedation is desired.28
Summary
Emergency physicians have a unique opportunity to improve the quality of life for patients suffering serious illness, especially those who are actively dying. The management of pain and nonpain symptoms in patients who are at end of life, is a particularly important skill for every EP. If available, a consultation with a palliative care medicine consultant may improve both short- and long-term patient care.
Dr Galicia-Castillo is the Sue Faulkner Scribner professor of geriatrics at the Eastern Virginia Medical School Glennan Center for Geriatrics and Gerontology, and Medical Director for Palliative Care Medicine at Sentara Norfolk General Hospital. Dr Counselman is the distinguished professor and chairman of the department of emergency medicine at Eastern Virginia Medical School, Norfolk; and a physician at Emergency Physicians of Tidewater, Norfolk, Virginia. He is also the associate editor in chief of EMERGENCY MEDICINE editorial board.
- Alsirafy SA, Raheem AA, Al-Zahrani AS, et al. Emergency department visits at the end of life of patients with terminal cancer: pattern, causes, and avoidability. Am J Hosp Palliat Care. 2015:1049909115581819. [Epub ahead of print].
- Grudzen CR, Richardson LD, Morrison M, Cho E, Morrison RS. Palliative care needs of seriously ill, older adults presenting to the emergency department. Acad Emerg Med. 2010;17(11):1253-1257.
- Smith AK, Schonberg MA, Fisher J, et al. Emergency department experiences of acutely symptomatic patients with terminal illness and their family caregivers. J Pain Symptom Manage. 2010;39(6):972-981.
- Mierendorf S, Gidvani V. Palliative care in the emergency department. Perm J. 2014;18(2):77-85.
- Barbera L, Taylor C, Dudgeon D. Why do patients with cancer visit the emergency department near the end of life? CMAJ. 2010;182(6): 563-568.
- Counselman FL, Borenstein MA, Chisholm CD, et al; EM Model Review Task Force; American Board of Emergency Medicine. The 2013 Model of the Clinical Practice of Emergency Medicine. Acad Emerg Med. 2014;21(5):574-598.
- Quest TE, Marco CA, Derse AR. Hospice and palliative medicine: new subspecialty, new opportunities. Ann Emerg Med. 2009;54(1):94-102.
- Singer AE, Meeker D, Teno JM, Lynn J, Lunney JR, Lorenz KA. Symptom trends in the last year of life from 1998 to 2010: a cohort study. Ann Intern Med. 2015;162(3):175-183.
- Lindqvist O, Lundquist G, Dickman A, et al; OPCARE9. Four essential drugs needed for quality care of the dying: a Delphi-study based international expert consensus opinion. J Palliat Med. 2013;16(1):38-43.
- Kandarian B, Morrison RS, Richardson LD, Ortiz J, Grudzen CR. Emergency department-initiated palliative care for advanced cancer patients: protocol for a pilot randomized controlled trial. Trials. 2014;15:251.
- Campbell ML. Caring for dying patients in the intensive care unit: managing pain, dyspnea, anxiety, delirium, and death rattle. AACN Adv Crit Care. 2015;26(2):110-120.
- Lamba S, Quest TE. Hospice care and the emergency department: rules, regulations, and referrals. Ann Emerg Med. 2011;57(3):282-290.
- Shaheen PE, Walsh D, Lasheen W, Davis MP, Lagman RL. Opioid equianalgesic tables: are they all equally dangerous? J Pain Symptom Manage.2009;38(3):409-417.
- Wallace EM, Cooney MC, Walsh J, Conroy M, Twomey F. Why do palliative care patients present to the emergency department? Avoidable or unavoidable? Am J Hosp Palliat Care. 2013;30(3):253-253.
- Erichsén E, Milberg A, Jaarsma T, Friedrichsen MJ. Constipation in specialized palliative care: prevalence, definition, and patient-perceived symptom distress. J Palliat Med. 2015;18(7):585-592.
- Candy B, Jones L, Larkin PJ, Vickerstaff V, Tookman A, Stone P. Laxatives for the management of constipation in people receiving palliative care. Cochrane Database Syst Rev. 2015;5:CD003448.
- Parshall MB, Schwartzstein RM, Adams L, et al; American Thoracic Society Committee on Dyspnea. An official American Thoracic Society statement: update on the mechanisms, assessment, and management of dyspnea. Am J Respir Crit Care Med. 2012;185(4):435-452.
- LeGrand SB, Khawam EA, Walsh D, Rivera NI. Opioids, respiratory function, and dyspnea. Am J Hosp Palliat Care. 2003;20(1):57-61.
- Meek PM, Schwartzstein R, Adams L, el al. Dyspnea. Mechanisms, assessment, and management: a consensus statement. American Thoracic Society. Am J Respir Crit Care Med. 1999;159(1):321-340.
- Campbell ML, Yarandi H, Dove-Medows E. Oxygen is nonbeneficial for most patients who are near death. J Pain Symptom Manage. 2013;45(3):517-523.
- Solano JP, Gomes B, Higginson IJ. A comparison of symptom prevalence in far advanced cancer, AIDS, heart disease, chronic obstructive pulmonary disease and renal disease. J Pain Symptom Manage. 2006;31(1):58-69.
- Glare P, Miller J, Nikolova T, Tickoo R. Treating nausea and vomiting in palliative care: a review. Clin Interv Aging. 2011;6:243-259.
- Cleeland CS, Bennett GJ, Dantzer R, et al. Are the symptoms of cancer and cancer treatment due to a shared biologic mechanism? A cytokine-immunologic model of cancer symptoms. Cancer. 2003;97(11):2919-2925.
- Bennett M, Lucas V, Brennan M, Hughes A, O’Donnell V, Wee B; Association for Palliative Medicine’s Science Committee. Using anti-muscarinic drugs in the management of death rattle: evidence-based guidelines for palliative care. Palliat Med. 2002;16(5):369-374.
- Mercadamte S. Death rattle: critical review and research agenda. Support Care Cancer. 2014;22(2):
- 571-575.
- Wildiers H, Menten J. Death rattle: prevalence, prevention and treatment. J Pain Symptom Manage. 2002;23(4):310-317.
- Wildiers H, Dhaenekint C, Demeulenaere P, et al; Flemish Federation of Palliative Care. Atropine, hyoscine butylbromide, or scopolamine are equally effective for the treatment of death rattle in terminal care. J Pain Symptom Manage. 2009;38(1):124-133.
- Kehl KA. Treatment of terminal restlessness: a review of the evidence. J Pain Palliat Care Pharmacother. 2004;18(1):5-30.
- Alsirafy SA, Raheem AA, Al-Zahrani AS, et al. Emergency department visits at the end of life of patients with terminal cancer: pattern, causes, and avoidability. Am J Hosp Palliat Care. 2015:1049909115581819. [Epub ahead of print].
- Grudzen CR, Richardson LD, Morrison M, Cho E, Morrison RS. Palliative care needs of seriously ill, older adults presenting to the emergency department. Acad Emerg Med. 2010;17(11):1253-1257.
- Smith AK, Schonberg MA, Fisher J, et al. Emergency department experiences of acutely symptomatic patients with terminal illness and their family caregivers. J Pain Symptom Manage. 2010;39(6):972-981.
- Mierendorf S, Gidvani V. Palliative care in the emergency department. Perm J. 2014;18(2):77-85.
- Barbera L, Taylor C, Dudgeon D. Why do patients with cancer visit the emergency department near the end of life? CMAJ. 2010;182(6): 563-568.
- Counselman FL, Borenstein MA, Chisholm CD, et al; EM Model Review Task Force; American Board of Emergency Medicine. The 2013 Model of the Clinical Practice of Emergency Medicine. Acad Emerg Med. 2014;21(5):574-598.
- Quest TE, Marco CA, Derse AR. Hospice and palliative medicine: new subspecialty, new opportunities. Ann Emerg Med. 2009;54(1):94-102.
- Singer AE, Meeker D, Teno JM, Lynn J, Lunney JR, Lorenz KA. Symptom trends in the last year of life from 1998 to 2010: a cohort study. Ann Intern Med. 2015;162(3):175-183.
- Lindqvist O, Lundquist G, Dickman A, et al; OPCARE9. Four essential drugs needed for quality care of the dying: a Delphi-study based international expert consensus opinion. J Palliat Med. 2013;16(1):38-43.
- Kandarian B, Morrison RS, Richardson LD, Ortiz J, Grudzen CR. Emergency department-initiated palliative care for advanced cancer patients: protocol for a pilot randomized controlled trial. Trials. 2014;15:251.
- Campbell ML. Caring for dying patients in the intensive care unit: managing pain, dyspnea, anxiety, delirium, and death rattle. AACN Adv Crit Care. 2015;26(2):110-120.
- Lamba S, Quest TE. Hospice care and the emergency department: rules, regulations, and referrals. Ann Emerg Med. 2011;57(3):282-290.
- Shaheen PE, Walsh D, Lasheen W, Davis MP, Lagman RL. Opioid equianalgesic tables: are they all equally dangerous? J Pain Symptom Manage.2009;38(3):409-417.
- Wallace EM, Cooney MC, Walsh J, Conroy M, Twomey F. Why do palliative care patients present to the emergency department? Avoidable or unavoidable? Am J Hosp Palliat Care. 2013;30(3):253-253.
- Erichsén E, Milberg A, Jaarsma T, Friedrichsen MJ. Constipation in specialized palliative care: prevalence, definition, and patient-perceived symptom distress. J Palliat Med. 2015;18(7):585-592.
- Candy B, Jones L, Larkin PJ, Vickerstaff V, Tookman A, Stone P. Laxatives for the management of constipation in people receiving palliative care. Cochrane Database Syst Rev. 2015;5:CD003448.
- Parshall MB, Schwartzstein RM, Adams L, et al; American Thoracic Society Committee on Dyspnea. An official American Thoracic Society statement: update on the mechanisms, assessment, and management of dyspnea. Am J Respir Crit Care Med. 2012;185(4):435-452.
- LeGrand SB, Khawam EA, Walsh D, Rivera NI. Opioids, respiratory function, and dyspnea. Am J Hosp Palliat Care. 2003;20(1):57-61.
- Meek PM, Schwartzstein R, Adams L, el al. Dyspnea. Mechanisms, assessment, and management: a consensus statement. American Thoracic Society. Am J Respir Crit Care Med. 1999;159(1):321-340.
- Campbell ML, Yarandi H, Dove-Medows E. Oxygen is nonbeneficial for most patients who are near death. J Pain Symptom Manage. 2013;45(3):517-523.
- Solano JP, Gomes B, Higginson IJ. A comparison of symptom prevalence in far advanced cancer, AIDS, heart disease, chronic obstructive pulmonary disease and renal disease. J Pain Symptom Manage. 2006;31(1):58-69.
- Glare P, Miller J, Nikolova T, Tickoo R. Treating nausea and vomiting in palliative care: a review. Clin Interv Aging. 2011;6:243-259.
- Cleeland CS, Bennett GJ, Dantzer R, et al. Are the symptoms of cancer and cancer treatment due to a shared biologic mechanism? A cytokine-immunologic model of cancer symptoms. Cancer. 2003;97(11):2919-2925.
- Bennett M, Lucas V, Brennan M, Hughes A, O’Donnell V, Wee B; Association for Palliative Medicine’s Science Committee. Using anti-muscarinic drugs in the management of death rattle: evidence-based guidelines for palliative care. Palliat Med. 2002;16(5):369-374.
- Mercadamte S. Death rattle: critical review and research agenda. Support Care Cancer. 2014;22(2):
- 571-575.
- Wildiers H, Menten J. Death rattle: prevalence, prevention and treatment. J Pain Symptom Manage. 2002;23(4):310-317.
- Wildiers H, Dhaenekint C, Demeulenaere P, et al; Flemish Federation of Palliative Care. Atropine, hyoscine butylbromide, or scopolamine are equally effective for the treatment of death rattle in terminal care. J Pain Symptom Manage. 2009;38(1):124-133.
- Kehl KA. Treatment of terminal restlessness: a review of the evidence. J Pain Palliat Care Pharmacother. 2004;18(1):5-30.
Malpractice Counsel
Acute Coronary Syndromes
A 53-year-old obese man presented to the ED complaining of pain in his chest, bilateral jaw, and back. He stated that his symptoms had started the previous evening and had increased in severity the morning of presentation. He denied any change in breathing, or any nausea or vomiting. The patient’s medical history was significant for hypertension and chronic back pain. Regarding his social history, the patient noted that he smoked one pack of cigarettes per day; he denied alcohol use.
On physical examination, the patient’s weight was 350 lb, and he was profusely diaphoretic. Vital signs were remarkable for an elevated blood pressure (BP) of 214/106 mm Hg; respiratory rate (RR), heart rate (HR), temperature (T), and oxygen saturation were normal. The head, eyes, ears, nose, and throat examination was normal, and there was no jugular venous distention. The lung and heart examinations were also normal, and the abdominal examination was unremarkable. The patient had 2+ pitting edema in his lower extremities, which he said had been present for the past few weeks. The back examination was unremarkable, and the neurological examination was completely normal, including deep tendon reflexes.
Because of the presence of chest and back pain and history of hypertension, the EP ordered a computed tomography (CT) scan of the chest with intravenous (IV) contrast to rule out aortic dissection. He also administered 0.2 mg of clonidine orally for the elevated BP. Approximately 20 minutes later, the patient was given 2 mg morphine IV for the back pain and another 0.2 mg of clonidine orally. The elevated BP responded to the clonidine, and the patient stated he was feeling better.
The CT scan of the chest was interpreted by radiology services as normal. The patient was then administered 325 mg of aspirin by mouth. Since the EP’s hospital did not have facilities for cardiac catheterization, the EP consulted with a physician at another facility regarding a possible transfer. The consulted physician did not accept the patient for transfer, but instead recommended keeping the patient at the EP’s institution for observation and continuing treatment for the elevated BP and pain. The EP agreed, and diagnosed the patient with a hypertensive emergency and a flare-up of his chronic back pain.
In the ED, the patient’s BP decreased to near normal levels, and he was feeling much improved. Approximately 5.5 hours after his arrival to the ED, he was admitted to a monitored bed under the care of a hospitalist.
A few hours later, the patient began to complain of burning in the epigastric area; analgesics and nitroglycerin were administered and a repeat ECG was ordered. A second troponin level, drawn approximately 6 hours after the original, was found to be significantly elevated. The repeat ECG demonstrated sinus tachycardia with ST-segment depression.
The hospitalist was concerned about an acute coronary syndrome (ACS) and attempted to make contact with the other facility to transfer the patient for an emergent cardiac catheterization. The consulted physician agreed to accept the patient and recommended starting an IV heparin drip and giving clopidogrel bisulfate (Plavix). While arranging for the transfer, the patient suffered a cardiac arrest; resuscitation attempts were unsuccessful.
The family of the patient sued the hospital, the EP, and the hospitalist, alleging the EP failed to recognize that the initial ECG and elevated troponin level were suggestive of an ACS. They also complained that the morphine, oxygen, nitroglycerin, and aspirin were not started in a timely manner. In addition, the family claimed the decedent should have been immediately transferred to another facility because the defendant’s hospital could not perform cardiac catheterization. They further alleged that the hospitalist failed to perform an independent evaluation of the patient and also failed to obtain a repeat 12-lead ECG sooner. Lastly, the plaintiffs claimed that the hospital’s nursing staff was negligent in failing to provide nursing care for 3 hours prior to the patient being found unresponsive.
The defendant EP asserted that the initial ECG was nondiagnostic and that the initial troponin level, while elevated, was nonspecific. He argued the ED evaluation and care provided was appropriate. Following trial, a defense verdict was returned.
Discussion
Fortunately, the jury ruled correctly in this case. Acute coronary sydromes can be some of the most challenging medical conditions to evaluate and manage in the ED. The EP’s initial cardiac workup and evaluation for a possible acute thoracic aortic dissection were appropriate—an acute thoracic aortic dissection is a true cardiovascular emergency. After interpreting the initial ECG as nondiagnostic (specifically, to rule out evidence of ST-segment elevation, myocardial infarction [MI], or STEMI), obtaining the contrast CT scan of the chest emergently was critically important. This patient had multiple risk factors for aortic dissection: he was a male between the ages of 50 and 55 years old (the mean age for proximal thoracic aortic dissection); he had a history of hypertension; and he was experiencing chest and back pain.1
Once an acute aortic dissection was excluded, focusing on a cardiac etiology, as the EP did, was appropriate. The only criticism is that this patient probably should have been managed with an IV antihypertensive agent to allow for a more controlled BP reduction; this, however, does not seem to have played any role in the patient’s ultimate outcome.
Acute coronary syndromes are a dynamic process and progress over time. The EP was clearly concerned about an ACS very early in the case, as evidenced by his attempt to transfer the patient to a facility with specialized cardiac capabilities. After not being able to do so, the most appropriate next step was his admission of the patient to a monitored bed with serial cardiac enzymes and ECGs. It is well known that initial evaluation of both ECG and cardiac enzymes can be normal early on in an ACS. Patients with a normal or nonspecific ECG have a 1% to 5% incidence of MI and a 4% to 23% incidence of unstable angina.2
This patient ultimately experienced a non-ST-segment elevation myocardial infarction (NSTEMI). However, this diagnosis did not become evident until several hours after the patient’s admission to the hospital. It is unfortunate the physician consulted by the EP at the onset did not agree to accept this patient. This patient’s best chance for survival was at a facility capable of percutaneous coronary intervention.
Serotonin Syndrome
| A 20-year-old man was brought to the ED by his friends for concerns of an overdose. Just prior to arrival, the patient reportedly drank the entire contents of a bottle of cough medicine containing dextromethorphan. His friends reported the patient had been depressed lately, but was otherwise in good health. The patient was not known to abuse alcohol or use illicit drugs. The EP was unable to obtain any history from the patient, who was extremely agitated and yelling frequently. A review of the hospital records revealed the patient had been admitted a few months prior for a suicide attempt. On physical examination, the patient’s vital signs were: pulse, 126 beats/minute; BP, 144/92 mm Hg, RR 22 breaths/minute; and T, 100.6˚F. Oxygen saturation was 99% on room air. The patient was diaphoretic, agitated, and only able to provide one-word answers between screaming episodes. His pupils were mildly dilated but reactive. The cardiac examination revealed a tachycardic rate with a normal rhythm, and no murmurs, rubs, or gallops. The lungs were clear to auscultation bilaterally. The abdomen was soft and nontender, without guarding or rebound. The patient would not cooperate for a neurological examination, but was found to be moving all four extremities with good strength. He was noted to have myoclonus. The EP immediately called the Poison Control Center for advice about treatment. In the meantime, laboratory studies were drawn, including an alcohol level, acetaminophen level, salicylate level, and a urine drug screen. A 12-lead ECG demonstrated a sinus tachycardia with a normal axis. The patient was given IV lorazepam to treat the agitation. The patient’s alcohol, acetaminophen, and salicylate levels were all negative. The EP attempted to transfer the patient to another facility with a higher level of care, but unfortunately, the patient went into cardiac arrest and died in the ED. An autopsy showed that the patient died from serotonin syndrome as a result of acute dextromethorphan and selegiline toxicity. It was later discovered that the patient had been prescribed selegiline as an antidepressant following his recent hospitalization for the suicide attempt. Unfortunately, this information was not available in the records from his previous presentation or from the patient or his friends during the history taking. The patient’s family sued the EP for failing to diagnose serotonin syndrome. They argued the patient did not die from a suicide, but rather from serotonin syndrome. The EP contended the patient had deliberately combined the two drugs to commit suicide. Both parties argued application of the state’s “dead man’s statute” (also known as a “dead man’s act” or “dead man’s rule”). Following trial, a defense verdict was returned. Discussion Serotonin syndrome (or serotonin toxicity) is a drug-induced syndrome characterized by a cluster of dose-related adverse effects due to increased serotonin concentrations in the central nervous system.1 Severe toxicity, as seen in this case, usually occurs only when two or more serotonergic drugs (even when each is at therapeutic dose) are combined. One of the drugs is usually a monoamine oxidase inhibitor (MAOI).1 While selegiline is used primarily as an adjunct treatment for Parkinson disease, it is also used to treat depression, attention deficit and hyperactivity disorder, and Alzheimer disease. Its primary mechanism of action is as an irreversible inhibitor of MAO. Dextromethorphan is used primarily as an antitussive (cough suppressant). It is also used recreationally for its reported effects as a hallucinogen. Its mechanism of action occurs through several effects, one of which is as a nonselective serotonin reuptake inhibitor (NSRI). Although the label on all NSRIs clearly states this medication should not be taken with MAOIs (ie, selegiline), few lay people know the mechanism of action of their medications. The patient in this case took a combination of medications that are known to cause severe serotonin toxicity. It is unclear whether or not he was aware of the dangers associated with combining these two medications. The classic triad of clinical features of serotonin syndrome are neuromuscular excitation (eg, clonus, hyperreflexia, myoclonus, rigidity); autonomic nervous system excitation (eg, hyperthermia, tachycardia); and altered mental status (eg, agitation, confusion).1 The onset of symptoms typically occurs within a few hours of ingestion. Serotonin syndrome can be confused with neuroleptic malignant syndrome (NMS), but there are three key differentiating features: (1) In NMS, symptom onset is slow, usually over days, not hours; (2) extrapyramidal features and rigidity are much more prominent in NMS; and (3) clonus is usually pronounced and easily elicited (especially with ankle dorsiflexion) in serotonin syndrome, but minimal to absent in NMS.1 The initial treatment of serotonin syndrome involves symptomatic care and discontinuation of all serotonergic drugs.2 Benzodiazepines can be used for muscle relaxation and treatment of agitation. All patients with serotonin syndrome require hospital admission, and those with severe toxicity should be admitted to an intensive care unit. Cyproheptadine is the most effective antiserotonergic agent, but it is only available in oral formulation. Chlorpromazine IV has also been used to treat serotonin syndrome, but resulting hypotension is a drawback.1 Approximately 25% of patients with severe serotonin toxicity require intubation and mechanical ventilation. Most patients show dramatic improvement within 24 hours of symptom onset.2 Regarding the dead man statute, according to Cornell University Law School, this statute states that in a civil action, a party with an interest in the litigation may not testify against a dead party about communications with the dead party. This is a state statute and therefore the exact wording varies from state to state. The Federal Rules of Evidence does not contain a dead man’s statute. |
Reference - Acute Coronary Syndromes
- Pacini D, Di Marco L, Fortuna D, et al. Acute aortic dissection: epidemiology and outcomes. Int J Cardiol. 2013;167(6):2806-2812.
- Hollander JE, Diercks DB. Acute coronary syndromes: acute myocardial infarction and unstable angina. In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD, eds. Tintinalli’s Emergency Medicine—A Comprehensive Study Guide. 7th ed. New York; McGraw Hill Medical; 2011:367.
Reference - Serotonin Syndrome
- Buckley NA, Dawson AH, Isbister GK. Serotonin Syndrome. BMJ. 2014;348:g1626.
- Mills KC, Bora KM. Atypical antidepressants, serotonin reuptake inhibitors, and serotonin syndrome. In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD, eds. Tintinalli’s Emergency Medicine—A Comprehensive Study Guide. 7th ed. New York; McGraw Hill Medical; 2011:1202.
Acute Coronary Syndromes
A 53-year-old obese man presented to the ED complaining of pain in his chest, bilateral jaw, and back. He stated that his symptoms had started the previous evening and had increased in severity the morning of presentation. He denied any change in breathing, or any nausea or vomiting. The patient’s medical history was significant for hypertension and chronic back pain. Regarding his social history, the patient noted that he smoked one pack of cigarettes per day; he denied alcohol use.
On physical examination, the patient’s weight was 350 lb, and he was profusely diaphoretic. Vital signs were remarkable for an elevated blood pressure (BP) of 214/106 mm Hg; respiratory rate (RR), heart rate (HR), temperature (T), and oxygen saturation were normal. The head, eyes, ears, nose, and throat examination was normal, and there was no jugular venous distention. The lung and heart examinations were also normal, and the abdominal examination was unremarkable. The patient had 2+ pitting edema in his lower extremities, which he said had been present for the past few weeks. The back examination was unremarkable, and the neurological examination was completely normal, including deep tendon reflexes.
Because of the presence of chest and back pain and history of hypertension, the EP ordered a computed tomography (CT) scan of the chest with intravenous (IV) contrast to rule out aortic dissection. He also administered 0.2 mg of clonidine orally for the elevated BP. Approximately 20 minutes later, the patient was given 2 mg morphine IV for the back pain and another 0.2 mg of clonidine orally. The elevated BP responded to the clonidine, and the patient stated he was feeling better.
The CT scan of the chest was interpreted by radiology services as normal. The patient was then administered 325 mg of aspirin by mouth. Since the EP’s hospital did not have facilities for cardiac catheterization, the EP consulted with a physician at another facility regarding a possible transfer. The consulted physician did not accept the patient for transfer, but instead recommended keeping the patient at the EP’s institution for observation and continuing treatment for the elevated BP and pain. The EP agreed, and diagnosed the patient with a hypertensive emergency and a flare-up of his chronic back pain.
In the ED, the patient’s BP decreased to near normal levels, and he was feeling much improved. Approximately 5.5 hours after his arrival to the ED, he was admitted to a monitored bed under the care of a hospitalist.
A few hours later, the patient began to complain of burning in the epigastric area; analgesics and nitroglycerin were administered and a repeat ECG was ordered. A second troponin level, drawn approximately 6 hours after the original, was found to be significantly elevated. The repeat ECG demonstrated sinus tachycardia with ST-segment depression.
The hospitalist was concerned about an acute coronary syndrome (ACS) and attempted to make contact with the other facility to transfer the patient for an emergent cardiac catheterization. The consulted physician agreed to accept the patient and recommended starting an IV heparin drip and giving clopidogrel bisulfate (Plavix). While arranging for the transfer, the patient suffered a cardiac arrest; resuscitation attempts were unsuccessful.
The family of the patient sued the hospital, the EP, and the hospitalist, alleging the EP failed to recognize that the initial ECG and elevated troponin level were suggestive of an ACS. They also complained that the morphine, oxygen, nitroglycerin, and aspirin were not started in a timely manner. In addition, the family claimed the decedent should have been immediately transferred to another facility because the defendant’s hospital could not perform cardiac catheterization. They further alleged that the hospitalist failed to perform an independent evaluation of the patient and also failed to obtain a repeat 12-lead ECG sooner. Lastly, the plaintiffs claimed that the hospital’s nursing staff was negligent in failing to provide nursing care for 3 hours prior to the patient being found unresponsive.
The defendant EP asserted that the initial ECG was nondiagnostic and that the initial troponin level, while elevated, was nonspecific. He argued the ED evaluation and care provided was appropriate. Following trial, a defense verdict was returned.
Discussion
Fortunately, the jury ruled correctly in this case. Acute coronary sydromes can be some of the most challenging medical conditions to evaluate and manage in the ED. The EP’s initial cardiac workup and evaluation for a possible acute thoracic aortic dissection were appropriate—an acute thoracic aortic dissection is a true cardiovascular emergency. After interpreting the initial ECG as nondiagnostic (specifically, to rule out evidence of ST-segment elevation, myocardial infarction [MI], or STEMI), obtaining the contrast CT scan of the chest emergently was critically important. This patient had multiple risk factors for aortic dissection: he was a male between the ages of 50 and 55 years old (the mean age for proximal thoracic aortic dissection); he had a history of hypertension; and he was experiencing chest and back pain.1
Once an acute aortic dissection was excluded, focusing on a cardiac etiology, as the EP did, was appropriate. The only criticism is that this patient probably should have been managed with an IV antihypertensive agent to allow for a more controlled BP reduction; this, however, does not seem to have played any role in the patient’s ultimate outcome.
Acute coronary syndromes are a dynamic process and progress over time. The EP was clearly concerned about an ACS very early in the case, as evidenced by his attempt to transfer the patient to a facility with specialized cardiac capabilities. After not being able to do so, the most appropriate next step was his admission of the patient to a monitored bed with serial cardiac enzymes and ECGs. It is well known that initial evaluation of both ECG and cardiac enzymes can be normal early on in an ACS. Patients with a normal or nonspecific ECG have a 1% to 5% incidence of MI and a 4% to 23% incidence of unstable angina.2
This patient ultimately experienced a non-ST-segment elevation myocardial infarction (NSTEMI). However, this diagnosis did not become evident until several hours after the patient’s admission to the hospital. It is unfortunate the physician consulted by the EP at the onset did not agree to accept this patient. This patient’s best chance for survival was at a facility capable of percutaneous coronary intervention.
Serotonin Syndrome
| A 20-year-old man was brought to the ED by his friends for concerns of an overdose. Just prior to arrival, the patient reportedly drank the entire contents of a bottle of cough medicine containing dextromethorphan. His friends reported the patient had been depressed lately, but was otherwise in good health. The patient was not known to abuse alcohol or use illicit drugs. The EP was unable to obtain any history from the patient, who was extremely agitated and yelling frequently. A review of the hospital records revealed the patient had been admitted a few months prior for a suicide attempt. On physical examination, the patient’s vital signs were: pulse, 126 beats/minute; BP, 144/92 mm Hg, RR 22 breaths/minute; and T, 100.6˚F. Oxygen saturation was 99% on room air. The patient was diaphoretic, agitated, and only able to provide one-word answers between screaming episodes. His pupils were mildly dilated but reactive. The cardiac examination revealed a tachycardic rate with a normal rhythm, and no murmurs, rubs, or gallops. The lungs were clear to auscultation bilaterally. The abdomen was soft and nontender, without guarding or rebound. The patient would not cooperate for a neurological examination, but was found to be moving all four extremities with good strength. He was noted to have myoclonus. The EP immediately called the Poison Control Center for advice about treatment. In the meantime, laboratory studies were drawn, including an alcohol level, acetaminophen level, salicylate level, and a urine drug screen. A 12-lead ECG demonstrated a sinus tachycardia with a normal axis. The patient was given IV lorazepam to treat the agitation. The patient’s alcohol, acetaminophen, and salicylate levels were all negative. The EP attempted to transfer the patient to another facility with a higher level of care, but unfortunately, the patient went into cardiac arrest and died in the ED. An autopsy showed that the patient died from serotonin syndrome as a result of acute dextromethorphan and selegiline toxicity. It was later discovered that the patient had been prescribed selegiline as an antidepressant following his recent hospitalization for the suicide attempt. Unfortunately, this information was not available in the records from his previous presentation or from the patient or his friends during the history taking. The patient’s family sued the EP for failing to diagnose serotonin syndrome. They argued the patient did not die from a suicide, but rather from serotonin syndrome. The EP contended the patient had deliberately combined the two drugs to commit suicide. Both parties argued application of the state’s “dead man’s statute” (also known as a “dead man’s act” or “dead man’s rule”). Following trial, a defense verdict was returned. Discussion Serotonin syndrome (or serotonin toxicity) is a drug-induced syndrome characterized by a cluster of dose-related adverse effects due to increased serotonin concentrations in the central nervous system.1 Severe toxicity, as seen in this case, usually occurs only when two or more serotonergic drugs (even when each is at therapeutic dose) are combined. One of the drugs is usually a monoamine oxidase inhibitor (MAOI).1 While selegiline is used primarily as an adjunct treatment for Parkinson disease, it is also used to treat depression, attention deficit and hyperactivity disorder, and Alzheimer disease. Its primary mechanism of action is as an irreversible inhibitor of MAO. Dextromethorphan is used primarily as an antitussive (cough suppressant). It is also used recreationally for its reported effects as a hallucinogen. Its mechanism of action occurs through several effects, one of which is as a nonselective serotonin reuptake inhibitor (NSRI). Although the label on all NSRIs clearly states this medication should not be taken with MAOIs (ie, selegiline), few lay people know the mechanism of action of their medications. The patient in this case took a combination of medications that are known to cause severe serotonin toxicity. It is unclear whether or not he was aware of the dangers associated with combining these two medications. The classic triad of clinical features of serotonin syndrome are neuromuscular excitation (eg, clonus, hyperreflexia, myoclonus, rigidity); autonomic nervous system excitation (eg, hyperthermia, tachycardia); and altered mental status (eg, agitation, confusion).1 The onset of symptoms typically occurs within a few hours of ingestion. Serotonin syndrome can be confused with neuroleptic malignant syndrome (NMS), but there are three key differentiating features: (1) In NMS, symptom onset is slow, usually over days, not hours; (2) extrapyramidal features and rigidity are much more prominent in NMS; and (3) clonus is usually pronounced and easily elicited (especially with ankle dorsiflexion) in serotonin syndrome, but minimal to absent in NMS.1 The initial treatment of serotonin syndrome involves symptomatic care and discontinuation of all serotonergic drugs.2 Benzodiazepines can be used for muscle relaxation and treatment of agitation. All patients with serotonin syndrome require hospital admission, and those with severe toxicity should be admitted to an intensive care unit. Cyproheptadine is the most effective antiserotonergic agent, but it is only available in oral formulation. Chlorpromazine IV has also been used to treat serotonin syndrome, but resulting hypotension is a drawback.1 Approximately 25% of patients with severe serotonin toxicity require intubation and mechanical ventilation. Most patients show dramatic improvement within 24 hours of symptom onset.2 Regarding the dead man statute, according to Cornell University Law School, this statute states that in a civil action, a party with an interest in the litigation may not testify against a dead party about communications with the dead party. This is a state statute and therefore the exact wording varies from state to state. The Federal Rules of Evidence does not contain a dead man’s statute. |
Acute Coronary Syndromes
A 53-year-old obese man presented to the ED complaining of pain in his chest, bilateral jaw, and back. He stated that his symptoms had started the previous evening and had increased in severity the morning of presentation. He denied any change in breathing, or any nausea or vomiting. The patient’s medical history was significant for hypertension and chronic back pain. Regarding his social history, the patient noted that he smoked one pack of cigarettes per day; he denied alcohol use.
On physical examination, the patient’s weight was 350 lb, and he was profusely diaphoretic. Vital signs were remarkable for an elevated blood pressure (BP) of 214/106 mm Hg; respiratory rate (RR), heart rate (HR), temperature (T), and oxygen saturation were normal. The head, eyes, ears, nose, and throat examination was normal, and there was no jugular venous distention. The lung and heart examinations were also normal, and the abdominal examination was unremarkable. The patient had 2+ pitting edema in his lower extremities, which he said had been present for the past few weeks. The back examination was unremarkable, and the neurological examination was completely normal, including deep tendon reflexes.
Because of the presence of chest and back pain and history of hypertension, the EP ordered a computed tomography (CT) scan of the chest with intravenous (IV) contrast to rule out aortic dissection. He also administered 0.2 mg of clonidine orally for the elevated BP. Approximately 20 minutes later, the patient was given 2 mg morphine IV for the back pain and another 0.2 mg of clonidine orally. The elevated BP responded to the clonidine, and the patient stated he was feeling better.
The CT scan of the chest was interpreted by radiology services as normal. The patient was then administered 325 mg of aspirin by mouth. Since the EP’s hospital did not have facilities for cardiac catheterization, the EP consulted with a physician at another facility regarding a possible transfer. The consulted physician did not accept the patient for transfer, but instead recommended keeping the patient at the EP’s institution for observation and continuing treatment for the elevated BP and pain. The EP agreed, and diagnosed the patient with a hypertensive emergency and a flare-up of his chronic back pain.
In the ED, the patient’s BP decreased to near normal levels, and he was feeling much improved. Approximately 5.5 hours after his arrival to the ED, he was admitted to a monitored bed under the care of a hospitalist.
A few hours later, the patient began to complain of burning in the epigastric area; analgesics and nitroglycerin were administered and a repeat ECG was ordered. A second troponin level, drawn approximately 6 hours after the original, was found to be significantly elevated. The repeat ECG demonstrated sinus tachycardia with ST-segment depression.
The hospitalist was concerned about an acute coronary syndrome (ACS) and attempted to make contact with the other facility to transfer the patient for an emergent cardiac catheterization. The consulted physician agreed to accept the patient and recommended starting an IV heparin drip and giving clopidogrel bisulfate (Plavix). While arranging for the transfer, the patient suffered a cardiac arrest; resuscitation attempts were unsuccessful.
The family of the patient sued the hospital, the EP, and the hospitalist, alleging the EP failed to recognize that the initial ECG and elevated troponin level were suggestive of an ACS. They also complained that the morphine, oxygen, nitroglycerin, and aspirin were not started in a timely manner. In addition, the family claimed the decedent should have been immediately transferred to another facility because the defendant’s hospital could not perform cardiac catheterization. They further alleged that the hospitalist failed to perform an independent evaluation of the patient and also failed to obtain a repeat 12-lead ECG sooner. Lastly, the plaintiffs claimed that the hospital’s nursing staff was negligent in failing to provide nursing care for 3 hours prior to the patient being found unresponsive.
The defendant EP asserted that the initial ECG was nondiagnostic and that the initial troponin level, while elevated, was nonspecific. He argued the ED evaluation and care provided was appropriate. Following trial, a defense verdict was returned.
Discussion
Fortunately, the jury ruled correctly in this case. Acute coronary sydromes can be some of the most challenging medical conditions to evaluate and manage in the ED. The EP’s initial cardiac workup and evaluation for a possible acute thoracic aortic dissection were appropriate—an acute thoracic aortic dissection is a true cardiovascular emergency. After interpreting the initial ECG as nondiagnostic (specifically, to rule out evidence of ST-segment elevation, myocardial infarction [MI], or STEMI), obtaining the contrast CT scan of the chest emergently was critically important. This patient had multiple risk factors for aortic dissection: he was a male between the ages of 50 and 55 years old (the mean age for proximal thoracic aortic dissection); he had a history of hypertension; and he was experiencing chest and back pain.1
Once an acute aortic dissection was excluded, focusing on a cardiac etiology, as the EP did, was appropriate. The only criticism is that this patient probably should have been managed with an IV antihypertensive agent to allow for a more controlled BP reduction; this, however, does not seem to have played any role in the patient’s ultimate outcome.
Acute coronary syndromes are a dynamic process and progress over time. The EP was clearly concerned about an ACS very early in the case, as evidenced by his attempt to transfer the patient to a facility with specialized cardiac capabilities. After not being able to do so, the most appropriate next step was his admission of the patient to a monitored bed with serial cardiac enzymes and ECGs. It is well known that initial evaluation of both ECG and cardiac enzymes can be normal early on in an ACS. Patients with a normal or nonspecific ECG have a 1% to 5% incidence of MI and a 4% to 23% incidence of unstable angina.2
This patient ultimately experienced a non-ST-segment elevation myocardial infarction (NSTEMI). However, this diagnosis did not become evident until several hours after the patient’s admission to the hospital. It is unfortunate the physician consulted by the EP at the onset did not agree to accept this patient. This patient’s best chance for survival was at a facility capable of percutaneous coronary intervention.
Serotonin Syndrome
| A 20-year-old man was brought to the ED by his friends for concerns of an overdose. Just prior to arrival, the patient reportedly drank the entire contents of a bottle of cough medicine containing dextromethorphan. His friends reported the patient had been depressed lately, but was otherwise in good health. The patient was not known to abuse alcohol or use illicit drugs. The EP was unable to obtain any history from the patient, who was extremely agitated and yelling frequently. A review of the hospital records revealed the patient had been admitted a few months prior for a suicide attempt. On physical examination, the patient’s vital signs were: pulse, 126 beats/minute; BP, 144/92 mm Hg, RR 22 breaths/minute; and T, 100.6˚F. Oxygen saturation was 99% on room air. The patient was diaphoretic, agitated, and only able to provide one-word answers between screaming episodes. His pupils were mildly dilated but reactive. The cardiac examination revealed a tachycardic rate with a normal rhythm, and no murmurs, rubs, or gallops. The lungs were clear to auscultation bilaterally. The abdomen was soft and nontender, without guarding or rebound. The patient would not cooperate for a neurological examination, but was found to be moving all four extremities with good strength. He was noted to have myoclonus. The EP immediately called the Poison Control Center for advice about treatment. In the meantime, laboratory studies were drawn, including an alcohol level, acetaminophen level, salicylate level, and a urine drug screen. A 12-lead ECG demonstrated a sinus tachycardia with a normal axis. The patient was given IV lorazepam to treat the agitation. The patient’s alcohol, acetaminophen, and salicylate levels were all negative. The EP attempted to transfer the patient to another facility with a higher level of care, but unfortunately, the patient went into cardiac arrest and died in the ED. An autopsy showed that the patient died from serotonin syndrome as a result of acute dextromethorphan and selegiline toxicity. It was later discovered that the patient had been prescribed selegiline as an antidepressant following his recent hospitalization for the suicide attempt. Unfortunately, this information was not available in the records from his previous presentation or from the patient or his friends during the history taking. The patient’s family sued the EP for failing to diagnose serotonin syndrome. They argued the patient did not die from a suicide, but rather from serotonin syndrome. The EP contended the patient had deliberately combined the two drugs to commit suicide. Both parties argued application of the state’s “dead man’s statute” (also known as a “dead man’s act” or “dead man’s rule”). Following trial, a defense verdict was returned. Discussion Serotonin syndrome (or serotonin toxicity) is a drug-induced syndrome characterized by a cluster of dose-related adverse effects due to increased serotonin concentrations in the central nervous system.1 Severe toxicity, as seen in this case, usually occurs only when two or more serotonergic drugs (even when each is at therapeutic dose) are combined. One of the drugs is usually a monoamine oxidase inhibitor (MAOI).1 While selegiline is used primarily as an adjunct treatment for Parkinson disease, it is also used to treat depression, attention deficit and hyperactivity disorder, and Alzheimer disease. Its primary mechanism of action is as an irreversible inhibitor of MAO. Dextromethorphan is used primarily as an antitussive (cough suppressant). It is also used recreationally for its reported effects as a hallucinogen. Its mechanism of action occurs through several effects, one of which is as a nonselective serotonin reuptake inhibitor (NSRI). Although the label on all NSRIs clearly states this medication should not be taken with MAOIs (ie, selegiline), few lay people know the mechanism of action of their medications. The patient in this case took a combination of medications that are known to cause severe serotonin toxicity. It is unclear whether or not he was aware of the dangers associated with combining these two medications. The classic triad of clinical features of serotonin syndrome are neuromuscular excitation (eg, clonus, hyperreflexia, myoclonus, rigidity); autonomic nervous system excitation (eg, hyperthermia, tachycardia); and altered mental status (eg, agitation, confusion).1 The onset of symptoms typically occurs within a few hours of ingestion. Serotonin syndrome can be confused with neuroleptic malignant syndrome (NMS), but there are three key differentiating features: (1) In NMS, symptom onset is slow, usually over days, not hours; (2) extrapyramidal features and rigidity are much more prominent in NMS; and (3) clonus is usually pronounced and easily elicited (especially with ankle dorsiflexion) in serotonin syndrome, but minimal to absent in NMS.1 The initial treatment of serotonin syndrome involves symptomatic care and discontinuation of all serotonergic drugs.2 Benzodiazepines can be used for muscle relaxation and treatment of agitation. All patients with serotonin syndrome require hospital admission, and those with severe toxicity should be admitted to an intensive care unit. Cyproheptadine is the most effective antiserotonergic agent, but it is only available in oral formulation. Chlorpromazine IV has also been used to treat serotonin syndrome, but resulting hypotension is a drawback.1 Approximately 25% of patients with severe serotonin toxicity require intubation and mechanical ventilation. Most patients show dramatic improvement within 24 hours of symptom onset.2 Regarding the dead man statute, according to Cornell University Law School, this statute states that in a civil action, a party with an interest in the litigation may not testify against a dead party about communications with the dead party. This is a state statute and therefore the exact wording varies from state to state. The Federal Rules of Evidence does not contain a dead man’s statute. |
Reference - Acute Coronary Syndromes
- Pacini D, Di Marco L, Fortuna D, et al. Acute aortic dissection: epidemiology and outcomes. Int J Cardiol. 2013;167(6):2806-2812.
- Hollander JE, Diercks DB. Acute coronary syndromes: acute myocardial infarction and unstable angina. In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD, eds. Tintinalli’s Emergency Medicine—A Comprehensive Study Guide. 7th ed. New York; McGraw Hill Medical; 2011:367.
Reference - Serotonin Syndrome
- Buckley NA, Dawson AH, Isbister GK. Serotonin Syndrome. BMJ. 2014;348:g1626.
- Mills KC, Bora KM. Atypical antidepressants, serotonin reuptake inhibitors, and serotonin syndrome. In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD, eds. Tintinalli’s Emergency Medicine—A Comprehensive Study Guide. 7th ed. New York; McGraw Hill Medical; 2011:1202.
Reference - Acute Coronary Syndromes
- Pacini D, Di Marco L, Fortuna D, et al. Acute aortic dissection: epidemiology and outcomes. Int J Cardiol. 2013;167(6):2806-2812.
- Hollander JE, Diercks DB. Acute coronary syndromes: acute myocardial infarction and unstable angina. In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD, eds. Tintinalli’s Emergency Medicine—A Comprehensive Study Guide. 7th ed. New York; McGraw Hill Medical; 2011:367.
Reference - Serotonin Syndrome
- Buckley NA, Dawson AH, Isbister GK. Serotonin Syndrome. BMJ. 2014;348:g1626.
- Mills KC, Bora KM. Atypical antidepressants, serotonin reuptake inhibitors, and serotonin syndrome. In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD, eds. Tintinalli’s Emergency Medicine—A Comprehensive Study Guide. 7th ed. New York; McGraw Hill Medical; 2011:1202.
Malpractice Counsel
Hypoglycemia
A 44-year-old-man with type 1 diabetes mellitus (DM) was transported to the ED via emergency medical services (EMS) with a chief complaint of hypoglycemia. His wife stated the patient had been acting strangely prior to presentation. She further noted that after checking his blood sugar, which was 19 mg/dL, she gave her husband an oral glucose tablet with some water before calling EMS.
Upon arrival to the ED, the patient was triaged and designated as an urgent level III. At that time, he was alert and oriented, with a blood glucose level of 66 mg/dL. The patient was examined by a physician assistant (PA) within 15 minutes of his arrival. When interviewed by the PA, the patient described feelings of weakness, dizziness, and lightheadedness. The PA attributed these symptoms to the patient’s hypoglycemic state and ordered him a food tray. The patient was then observed for approximately 2 hours, during which time repeat blood-glucose testing revealed a level of 438 mg/dL. Approximately 20 minutes later, another blood-glucose test showed a level of 400 mg/dL. The patient felt well, appeared back to baseline, and expressed the desire to go home. At discharge, the PA instructed the patient to reduce his insulin by 20% and to follow up with his primary care physician (PCP) that same week.
Approximately 3 hours after discharge, the patient was found unresponsive by his wife, and EMS was again called. When EMS arrived at the patient’s house, his blood glucose level was 85 mg/dL. At presentation to the ED, the patient was unresponsive and without a pulse. Despite approximately 30 minutes of intensive resuscitative efforts, the code was called and the patient was pronounced dead.
The family sued the hospital, the emergency physician (EP), and the PA. They claimed the triage nurse failed to obtain an adequate history of the patient’s recent glucometer checks, previous hypoglycemic episodes, the amount and time of his last dose of insulin, and when and how much food he had recently ingested. The plaintiff further argued that that PA failed to obtain an electrocardiogram (ECG) to determine if the patient’s heart rhythm had been affected by his hypoglycemic state. The plaintiff also claimed the PA should have notified the patient’s PCP that the patient was in the ED, so that he could be admitted.
The defendants denied any negligence and argued the patient’s death was due to a sudden cardiac event, which was unrelated to the low-blood sugar levels. The defense contended that the patient’s enlarged heart and preexisting cardiovascular disease, hypertension, hypercholesterolemia, poorly controlled type 1 DM, history of alcohol abuse, and documented evidence of medication noncompliance were the cause of death. According to published accounts, a defense verdict was returned.
Discussion
It seems that rarely a shift goes by without a patient presenting with diabetes-associated complications such as hyperglycemia or hypoglycemia. While the jury reached the correct conclusion in this case, it does serve as a reminder that cases of hypoglycemia should not be treated lightly, and the EP must attempt to determine its cause.
The most commonly accepted definition of hypoglycemia is a blood-glucose level <50 mg/dL with associated symptoms. The causes of hypoglycemia in patients treated with insulin typically involves inadequate or no food intake, or accidental administration of too much insulin or the wrong type of insulin.1
The differential diagnosis, however, needs to be more than just these two conditions. Since insulin is cleared by the kidneys, and patients with DM are at increased risk for kidney disease, acute renal failure should be considered in the differential. Other conditions to consider include infection, acute coronary syndromes, or unusual physical or mental stress.2
As with every patient presenting to the ED, patients with DM require a good history taking and physical examination. Additional testing, such as an ECG, troponin level, and kidney function test, should be performed based on the history and physical examination. Once the cause is determined, the majority of these patients can be treated with either intravenous (IV) or oral medications, observed, and discharged home with follow-up instructions.
Diabetic patients presenting with hypoglycemia due to a sulfonylurea agent or a long-acting insulin are in a completely different category. Because of the longer half-life of these agents, such patients will usually require admission to the hospital for serial glucose monitoring and treatment.2 On occasion, patients with diabetic hypoglycemia and who are on a regular form of insulin will also require hospital admission. Those at highest risk are patients with DM aged 80 years and older.1
Hyperkalemia
A 59-year-old man presented to the ED complaining of generalized weakness, the onset of which he stated had developed gradually over the previous 3 days. He denied chest pain, shortness of breath, or nausea and vomiting. His medical history was significant only for renal insufficiency. The patient was on no medications and denied alcohol or tobacco use.
On physical examination, the patient had normal vital signs, including normal pulse oximetry. Similarly, the heart, lung, and abdominal examinations were all normal. On neurological examination, the patient had 5/5 motor strength in all four extremities and exhibited a normal gait.
The EP ordered an ECG, complete blood count (CBC), basic metabolic panel, urinalysis, and a chest X-ray (CXR). Laboratory evaluation showed an elevated potassium level of 6 mEq/L. The results of the CBC, urinalysis, and CXR were all reported as normal. (Unfortunately, there was no published information on the results of the BUN, creatinine, serum bicarbonate, or ECG findings.)
Based on the patient’s elevated potassium level, the EP ordered sodium polystyrene (Kayexalate) orally and arranged for admission to the hospital. The sodium polystyrene was administered to the patient approximately 1 hour after it was ordered. While waiting for an inpatient bed, the patient experienced a cardiac arrest and died in the ED.
The family sued the EP and hospital for failure to properly respond to the patient’s elevated potassium level. The hospital denied any negligence, and the defense argued that the death was not related to any electrolyte abnormality, but was due to a respiratory arrest that led to the cardiac arrest. The defendants also maintained the sodium polystyrene had been administered in a timely manner. At trial, a defense verdict was returned.
Discussion
Hyperkalemia has been variably defined as serum potassium concentrations >5 mEq/L, >5.5 mEq/L, or >6 mEq/L.1 Symptoms of hyperkalemia include generalized muscle weakness (as seen in this patient), muscle cramps, paresthesias, nausea, vomiting, and/or diarrhea. However, it is the cardiac manifestations (eg, ventricular arrhythmias, complete heart block, asystole) associated with hyperkalemia that are most concerning.
There are numerous causes of hyperkalemia, including medications, renal failure, digitalis toxicity, and metabolic acidosis. Therefore, it is important for the EP to identify the etiology in order to definitively treat the hyperkalemia.
Traditionally, it has been taught that hyperkalemia only requires treatment if abnormalities on the ECG are noted. Classic findings seen on ECG include prolonged PR interval, peaked T waves,2 shortened QT interval, QRS widening, and a sinusoidal wave pattern. Once fictitious or hemolysis has been ruled out as the etiology, most EPs will initiate treatment above a specific threshold value (frequently 6 mEq/L),
Since it is the cardiac effects of hyperkalemia that can result in death, the initial treatment must be directed toward cardiac membrane stabilization. This is best accomplished by the administration of calcium gluconate 10% IV. This medication has a rapid onset of action (typically 1-3 minutes) and helps prevent the development of cardiac arrhythmias. Additional measures, which involve moving potassium intracellullarly, include sodium bicarbonate IV and insulin with glucose IV.
Actual removal of potassium from the body involves either the administration sodium polystyrene sulfonate or hemodialysis. Sodium polystyrene sulfonate, which is an ion-exchange resin designed to exchange sodium for potassium in the colon, can be given either orally or as an enema. Even though sodium polystyrene sulfonate has been approved for the treatment of hyperkalemia since 1958, it does not take effect for 1 to 2 hours after administration; there is also growing evidence questioning its efficacy and safety.3 In addition, sodium polystyrene sulfonate can exacerbate volume overload due to the associated increase in serum sodium. Therefore, hemodialysis is the most effective treatment for hyperkalemia, and is the treatment of choice for unstable patients with hyperkalemia and acute or chronic renal failure.
Reference - Hypoglycemia
- Geller AI, Shehab N, Lovegrove MC, et al. National estimates of insulin-related hypoglycemia and errors leading to emergency department visits and hospitalizations. JAMA Intern Med. 2014;174(5): 678-686.
- Jalili M: Type 2 Diabetes Mellitus. In: Tintinalli JE, et al, eds. Tintinalli’s Emergency Medicine – A Comprehensive Study Guide, 7th ed. New York; McGraw Hill Medical; 2011:1419.
Reference - Hyperkalemia
- Jain N, Kotla S, Little BB, et al. Predictors of hyperkalemia and death in patients with cardiac and renal disease. Am J Cardiol. 2012;109(10):1510-1513.
- Welch A, Maroz N, Wingo CS. Hyperkalemia: getting to the heart of the matter. Nephrol Dial Transplant. 2013;28(1):15-16.
- Sterns RH, Rojas M, Bernstein P, Chennupati S. Ion-exchange resins for the treatment of hyperkalemia: are they safe and effective? J Am Soc Nephrol. 2010; 21(5):73-735.
Hypoglycemia
A 44-year-old-man with type 1 diabetes mellitus (DM) was transported to the ED via emergency medical services (EMS) with a chief complaint of hypoglycemia. His wife stated the patient had been acting strangely prior to presentation. She further noted that after checking his blood sugar, which was 19 mg/dL, she gave her husband an oral glucose tablet with some water before calling EMS.
Upon arrival to the ED, the patient was triaged and designated as an urgent level III. At that time, he was alert and oriented, with a blood glucose level of 66 mg/dL. The patient was examined by a physician assistant (PA) within 15 minutes of his arrival. When interviewed by the PA, the patient described feelings of weakness, dizziness, and lightheadedness. The PA attributed these symptoms to the patient’s hypoglycemic state and ordered him a food tray. The patient was then observed for approximately 2 hours, during which time repeat blood-glucose testing revealed a level of 438 mg/dL. Approximately 20 minutes later, another blood-glucose test showed a level of 400 mg/dL. The patient felt well, appeared back to baseline, and expressed the desire to go home. At discharge, the PA instructed the patient to reduce his insulin by 20% and to follow up with his primary care physician (PCP) that same week.
Approximately 3 hours after discharge, the patient was found unresponsive by his wife, and EMS was again called. When EMS arrived at the patient’s house, his blood glucose level was 85 mg/dL. At presentation to the ED, the patient was unresponsive and without a pulse. Despite approximately 30 minutes of intensive resuscitative efforts, the code was called and the patient was pronounced dead.
The family sued the hospital, the emergency physician (EP), and the PA. They claimed the triage nurse failed to obtain an adequate history of the patient’s recent glucometer checks, previous hypoglycemic episodes, the amount and time of his last dose of insulin, and when and how much food he had recently ingested. The plaintiff further argued that that PA failed to obtain an electrocardiogram (ECG) to determine if the patient’s heart rhythm had been affected by his hypoglycemic state. The plaintiff also claimed the PA should have notified the patient’s PCP that the patient was in the ED, so that he could be admitted.
The defendants denied any negligence and argued the patient’s death was due to a sudden cardiac event, which was unrelated to the low-blood sugar levels. The defense contended that the patient’s enlarged heart and preexisting cardiovascular disease, hypertension, hypercholesterolemia, poorly controlled type 1 DM, history of alcohol abuse, and documented evidence of medication noncompliance were the cause of death. According to published accounts, a defense verdict was returned.
Discussion
It seems that rarely a shift goes by without a patient presenting with diabetes-associated complications such as hyperglycemia or hypoglycemia. While the jury reached the correct conclusion in this case, it does serve as a reminder that cases of hypoglycemia should not be treated lightly, and the EP must attempt to determine its cause.
The most commonly accepted definition of hypoglycemia is a blood-glucose level <50 mg/dL with associated symptoms. The causes of hypoglycemia in patients treated with insulin typically involves inadequate or no food intake, or accidental administration of too much insulin or the wrong type of insulin.1
The differential diagnosis, however, needs to be more than just these two conditions. Since insulin is cleared by the kidneys, and patients with DM are at increased risk for kidney disease, acute renal failure should be considered in the differential. Other conditions to consider include infection, acute coronary syndromes, or unusual physical or mental stress.2
As with every patient presenting to the ED, patients with DM require a good history taking and physical examination. Additional testing, such as an ECG, troponin level, and kidney function test, should be performed based on the history and physical examination. Once the cause is determined, the majority of these patients can be treated with either intravenous (IV) or oral medications, observed, and discharged home with follow-up instructions.
Diabetic patients presenting with hypoglycemia due to a sulfonylurea agent or a long-acting insulin are in a completely different category. Because of the longer half-life of these agents, such patients will usually require admission to the hospital for serial glucose monitoring and treatment.2 On occasion, patients with diabetic hypoglycemia and who are on a regular form of insulin will also require hospital admission. Those at highest risk are patients with DM aged 80 years and older.1
Hyperkalemia
A 59-year-old man presented to the ED complaining of generalized weakness, the onset of which he stated had developed gradually over the previous 3 days. He denied chest pain, shortness of breath, or nausea and vomiting. His medical history was significant only for renal insufficiency. The patient was on no medications and denied alcohol or tobacco use.
On physical examination, the patient had normal vital signs, including normal pulse oximetry. Similarly, the heart, lung, and abdominal examinations were all normal. On neurological examination, the patient had 5/5 motor strength in all four extremities and exhibited a normal gait.
The EP ordered an ECG, complete blood count (CBC), basic metabolic panel, urinalysis, and a chest X-ray (CXR). Laboratory evaluation showed an elevated potassium level of 6 mEq/L. The results of the CBC, urinalysis, and CXR were all reported as normal. (Unfortunately, there was no published information on the results of the BUN, creatinine, serum bicarbonate, or ECG findings.)
Based on the patient’s elevated potassium level, the EP ordered sodium polystyrene (Kayexalate) orally and arranged for admission to the hospital. The sodium polystyrene was administered to the patient approximately 1 hour after it was ordered. While waiting for an inpatient bed, the patient experienced a cardiac arrest and died in the ED.
The family sued the EP and hospital for failure to properly respond to the patient’s elevated potassium level. The hospital denied any negligence, and the defense argued that the death was not related to any electrolyte abnormality, but was due to a respiratory arrest that led to the cardiac arrest. The defendants also maintained the sodium polystyrene had been administered in a timely manner. At trial, a defense verdict was returned.
Discussion
Hyperkalemia has been variably defined as serum potassium concentrations >5 mEq/L, >5.5 mEq/L, or >6 mEq/L.1 Symptoms of hyperkalemia include generalized muscle weakness (as seen in this patient), muscle cramps, paresthesias, nausea, vomiting, and/or diarrhea. However, it is the cardiac manifestations (eg, ventricular arrhythmias, complete heart block, asystole) associated with hyperkalemia that are most concerning.
There are numerous causes of hyperkalemia, including medications, renal failure, digitalis toxicity, and metabolic acidosis. Therefore, it is important for the EP to identify the etiology in order to definitively treat the hyperkalemia.
Traditionally, it has been taught that hyperkalemia only requires treatment if abnormalities on the ECG are noted. Classic findings seen on ECG include prolonged PR interval, peaked T waves,2 shortened QT interval, QRS widening, and a sinusoidal wave pattern. Once fictitious or hemolysis has been ruled out as the etiology, most EPs will initiate treatment above a specific threshold value (frequently 6 mEq/L),
Since it is the cardiac effects of hyperkalemia that can result in death, the initial treatment must be directed toward cardiac membrane stabilization. This is best accomplished by the administration of calcium gluconate 10% IV. This medication has a rapid onset of action (typically 1-3 minutes) and helps prevent the development of cardiac arrhythmias. Additional measures, which involve moving potassium intracellullarly, include sodium bicarbonate IV and insulin with glucose IV.
Actual removal of potassium from the body involves either the administration sodium polystyrene sulfonate or hemodialysis. Sodium polystyrene sulfonate, which is an ion-exchange resin designed to exchange sodium for potassium in the colon, can be given either orally or as an enema. Even though sodium polystyrene sulfonate has been approved for the treatment of hyperkalemia since 1958, it does not take effect for 1 to 2 hours after administration; there is also growing evidence questioning its efficacy and safety.3 In addition, sodium polystyrene sulfonate can exacerbate volume overload due to the associated increase in serum sodium. Therefore, hemodialysis is the most effective treatment for hyperkalemia, and is the treatment of choice for unstable patients with hyperkalemia and acute or chronic renal failure.
Hypoglycemia
A 44-year-old-man with type 1 diabetes mellitus (DM) was transported to the ED via emergency medical services (EMS) with a chief complaint of hypoglycemia. His wife stated the patient had been acting strangely prior to presentation. She further noted that after checking his blood sugar, which was 19 mg/dL, she gave her husband an oral glucose tablet with some water before calling EMS.
Upon arrival to the ED, the patient was triaged and designated as an urgent level III. At that time, he was alert and oriented, with a blood glucose level of 66 mg/dL. The patient was examined by a physician assistant (PA) within 15 minutes of his arrival. When interviewed by the PA, the patient described feelings of weakness, dizziness, and lightheadedness. The PA attributed these symptoms to the patient’s hypoglycemic state and ordered him a food tray. The patient was then observed for approximately 2 hours, during which time repeat blood-glucose testing revealed a level of 438 mg/dL. Approximately 20 minutes later, another blood-glucose test showed a level of 400 mg/dL. The patient felt well, appeared back to baseline, and expressed the desire to go home. At discharge, the PA instructed the patient to reduce his insulin by 20% and to follow up with his primary care physician (PCP) that same week.
Approximately 3 hours after discharge, the patient was found unresponsive by his wife, and EMS was again called. When EMS arrived at the patient’s house, his blood glucose level was 85 mg/dL. At presentation to the ED, the patient was unresponsive and without a pulse. Despite approximately 30 minutes of intensive resuscitative efforts, the code was called and the patient was pronounced dead.
The family sued the hospital, the emergency physician (EP), and the PA. They claimed the triage nurse failed to obtain an adequate history of the patient’s recent glucometer checks, previous hypoglycemic episodes, the amount and time of his last dose of insulin, and when and how much food he had recently ingested. The plaintiff further argued that that PA failed to obtain an electrocardiogram (ECG) to determine if the patient’s heart rhythm had been affected by his hypoglycemic state. The plaintiff also claimed the PA should have notified the patient’s PCP that the patient was in the ED, so that he could be admitted.
The defendants denied any negligence and argued the patient’s death was due to a sudden cardiac event, which was unrelated to the low-blood sugar levels. The defense contended that the patient’s enlarged heart and preexisting cardiovascular disease, hypertension, hypercholesterolemia, poorly controlled type 1 DM, history of alcohol abuse, and documented evidence of medication noncompliance were the cause of death. According to published accounts, a defense verdict was returned.
Discussion
It seems that rarely a shift goes by without a patient presenting with diabetes-associated complications such as hyperglycemia or hypoglycemia. While the jury reached the correct conclusion in this case, it does serve as a reminder that cases of hypoglycemia should not be treated lightly, and the EP must attempt to determine its cause.
The most commonly accepted definition of hypoglycemia is a blood-glucose level <50 mg/dL with associated symptoms. The causes of hypoglycemia in patients treated with insulin typically involves inadequate or no food intake, or accidental administration of too much insulin or the wrong type of insulin.1
The differential diagnosis, however, needs to be more than just these two conditions. Since insulin is cleared by the kidneys, and patients with DM are at increased risk for kidney disease, acute renal failure should be considered in the differential. Other conditions to consider include infection, acute coronary syndromes, or unusual physical or mental stress.2
As with every patient presenting to the ED, patients with DM require a good history taking and physical examination. Additional testing, such as an ECG, troponin level, and kidney function test, should be performed based on the history and physical examination. Once the cause is determined, the majority of these patients can be treated with either intravenous (IV) or oral medications, observed, and discharged home with follow-up instructions.
Diabetic patients presenting with hypoglycemia due to a sulfonylurea agent or a long-acting insulin are in a completely different category. Because of the longer half-life of these agents, such patients will usually require admission to the hospital for serial glucose monitoring and treatment.2 On occasion, patients with diabetic hypoglycemia and who are on a regular form of insulin will also require hospital admission. Those at highest risk are patients with DM aged 80 years and older.1
Hyperkalemia
A 59-year-old man presented to the ED complaining of generalized weakness, the onset of which he stated had developed gradually over the previous 3 days. He denied chest pain, shortness of breath, or nausea and vomiting. His medical history was significant only for renal insufficiency. The patient was on no medications and denied alcohol or tobacco use.
On physical examination, the patient had normal vital signs, including normal pulse oximetry. Similarly, the heart, lung, and abdominal examinations were all normal. On neurological examination, the patient had 5/5 motor strength in all four extremities and exhibited a normal gait.
The EP ordered an ECG, complete blood count (CBC), basic metabolic panel, urinalysis, and a chest X-ray (CXR). Laboratory evaluation showed an elevated potassium level of 6 mEq/L. The results of the CBC, urinalysis, and CXR were all reported as normal. (Unfortunately, there was no published information on the results of the BUN, creatinine, serum bicarbonate, or ECG findings.)
Based on the patient’s elevated potassium level, the EP ordered sodium polystyrene (Kayexalate) orally and arranged for admission to the hospital. The sodium polystyrene was administered to the patient approximately 1 hour after it was ordered. While waiting for an inpatient bed, the patient experienced a cardiac arrest and died in the ED.
The family sued the EP and hospital for failure to properly respond to the patient’s elevated potassium level. The hospital denied any negligence, and the defense argued that the death was not related to any electrolyte abnormality, but was due to a respiratory arrest that led to the cardiac arrest. The defendants also maintained the sodium polystyrene had been administered in a timely manner. At trial, a defense verdict was returned.
Discussion
Hyperkalemia has been variably defined as serum potassium concentrations >5 mEq/L, >5.5 mEq/L, or >6 mEq/L.1 Symptoms of hyperkalemia include generalized muscle weakness (as seen in this patient), muscle cramps, paresthesias, nausea, vomiting, and/or diarrhea. However, it is the cardiac manifestations (eg, ventricular arrhythmias, complete heart block, asystole) associated with hyperkalemia that are most concerning.
There are numerous causes of hyperkalemia, including medications, renal failure, digitalis toxicity, and metabolic acidosis. Therefore, it is important for the EP to identify the etiology in order to definitively treat the hyperkalemia.
Traditionally, it has been taught that hyperkalemia only requires treatment if abnormalities on the ECG are noted. Classic findings seen on ECG include prolonged PR interval, peaked T waves,2 shortened QT interval, QRS widening, and a sinusoidal wave pattern. Once fictitious or hemolysis has been ruled out as the etiology, most EPs will initiate treatment above a specific threshold value (frequently 6 mEq/L),
Since it is the cardiac effects of hyperkalemia that can result in death, the initial treatment must be directed toward cardiac membrane stabilization. This is best accomplished by the administration of calcium gluconate 10% IV. This medication has a rapid onset of action (typically 1-3 minutes) and helps prevent the development of cardiac arrhythmias. Additional measures, which involve moving potassium intracellullarly, include sodium bicarbonate IV and insulin with glucose IV.
Actual removal of potassium from the body involves either the administration sodium polystyrene sulfonate or hemodialysis. Sodium polystyrene sulfonate, which is an ion-exchange resin designed to exchange sodium for potassium in the colon, can be given either orally or as an enema. Even though sodium polystyrene sulfonate has been approved for the treatment of hyperkalemia since 1958, it does not take effect for 1 to 2 hours after administration; there is also growing evidence questioning its efficacy and safety.3 In addition, sodium polystyrene sulfonate can exacerbate volume overload due to the associated increase in serum sodium. Therefore, hemodialysis is the most effective treatment for hyperkalemia, and is the treatment of choice for unstable patients with hyperkalemia and acute or chronic renal failure.
Reference - Hypoglycemia
- Geller AI, Shehab N, Lovegrove MC, et al. National estimates of insulin-related hypoglycemia and errors leading to emergency department visits and hospitalizations. JAMA Intern Med. 2014;174(5): 678-686.
- Jalili M: Type 2 Diabetes Mellitus. In: Tintinalli JE, et al, eds. Tintinalli’s Emergency Medicine – A Comprehensive Study Guide, 7th ed. New York; McGraw Hill Medical; 2011:1419.
Reference - Hyperkalemia
- Jain N, Kotla S, Little BB, et al. Predictors of hyperkalemia and death in patients with cardiac and renal disease. Am J Cardiol. 2012;109(10):1510-1513.
- Welch A, Maroz N, Wingo CS. Hyperkalemia: getting to the heart of the matter. Nephrol Dial Transplant. 2013;28(1):15-16.
- Sterns RH, Rojas M, Bernstein P, Chennupati S. Ion-exchange resins for the treatment of hyperkalemia: are they safe and effective? J Am Soc Nephrol. 2010; 21(5):73-735.
Reference - Hypoglycemia
- Geller AI, Shehab N, Lovegrove MC, et al. National estimates of insulin-related hypoglycemia and errors leading to emergency department visits and hospitalizations. JAMA Intern Med. 2014;174(5): 678-686.
- Jalili M: Type 2 Diabetes Mellitus. In: Tintinalli JE, et al, eds. Tintinalli’s Emergency Medicine – A Comprehensive Study Guide, 7th ed. New York; McGraw Hill Medical; 2011:1419.
Reference - Hyperkalemia
- Jain N, Kotla S, Little BB, et al. Predictors of hyperkalemia and death in patients with cardiac and renal disease. Am J Cardiol. 2012;109(10):1510-1513.
- Welch A, Maroz N, Wingo CS. Hyperkalemia: getting to the heart of the matter. Nephrol Dial Transplant. 2013;28(1):15-16.
- Sterns RH, Rojas M, Bernstein P, Chennupati S. Ion-exchange resins for the treatment of hyperkalemia: are they safe and effective? J Am Soc Nephrol. 2010; 21(5):73-735.
Malpractice Counsel
Sepsis Following Vaginal Hysterectomy
| A 45-year-old woman presented to the ED complaining of lower abdominal pain, which she described as gradual, aching, and intermittent. The patient stated that she had undergone a vaginal hysterectomy a few days prior and that the pain started less than 24 hours after discharge from the hospital. She denied fever or chills, nausea, or vomiting, and said that she had a bowel movement earlier that day. She also denied any urinary symptoms. Her medical history was significant only for hypothyroidism, for which she was taking levothyroxine. The patient denied cigarette smoking or alcohol consumption. She said she had been taking acetaminophen-hydrocodone for postoperative pain, but that it did not provide any relief. |
The patient’s vital signs were: temperature, 98.6˚F; blood pressure, 112/65 mm Hg; heart rate, 98 beats/minute; and respiratory rate, 20 breaths/minute. The head, eyes, ears, nose, and throat examination was normal, as were the heart and lung examinations. The patient’s abdomen was soft, with mild diffuse lower abdominal tenderness. There was no guarding, rebound, or mass present. A gross nonspeculum examination of the vaginal area did not reveal any discharge or erythema; a rectal examination was not performed.
The EP ordered a complete blood count (CBC), lipase evaluation, and urinalysis. All test results were normal. The emergency physician (EP) then contacted the obstetrician-gynecologist (OB/GYN) who had performed the hysterectomy. The OB/GYN recommended the EP change the analgesic agent to acetaminophen-oxycodone and to encourage the patient to keep her follow-up postoperative appointment in 1 week. The EP followed these instructions and discharged the patient home with a prescription for the new analgesic.
Three days later, however, the patient presented back to the same ED complaining of increased and now generalized abdominal pain, nausea, and vomiting. She was noted to be febrile, tachycardic, and hypotensive. On physical examination, her abdomen was diffusely tender with guarding and rebound. She was given a 2-L bolus of intravenous (IV) normal saline and started on broad spectrum IV antibiotics. After another consultation with the patient’s OB/GYN surgeon, the patient was taken immediately to the operating room. On exploration, she was found to have a segment of perforated bowel and peritonitis. A portion of the bowel was resected, but her postoperative course was complicated by sepsis. After a 1-month stay in the hospital, she was discharged home.
The patient sued the EP—but not her OB/GYN—for failure to obtain a CT scan of the abdomen/pelvis on her initial ED visit, or at least to admit her to the hospital for observation. The EP argued that even if a computed tomography (CT) scan had been performed on the initial visit, it probably would have been normal, since the bowel had not yet perforated. After trial, a defense verdict was returned.
Discussion
This case illustrates two important points. First, not every patient with abdominal pain requires a CT scan of the abdomen/pelvis. So many malpractice cases against EPs involve the failure to perform advanced imaging. Unfortunately, that is usually only through the benefit of hindsight. For a patient with mild abdominal pain, only minimal tenderness on examination, and a negative laboratory workup, it can be perfectly appropriate to treat him or her symptomatically with close follow-up and specific instructions to return to the ED if his or her condition worsens (as was the case with this patient).
The second important point is to not over-rely on a consultant(s), especially if she or he has not independently examined the patient. When calling a consultant, it is best to have a specific question (ie, “Can you see the patient in the morning?”) or action (ie, “I would like to admit the patient to your service”). In general, the EP should not rely on the consultant to give “permission” to discharge the patient. As the physician seeing the patient, the EP is the most well-equipped to work up the patient and determine the needed disposition. Rare is the consultant that can arrive at a better disposition than the EP who performed the history and physical examination on the patient.
Regarding the patient’s GYN surgery, vaginal hysterectomy (VH) is preferred over abdominal hysterectomy (AH) for benign disease as it is associated with reduced infective morbidity and earlier return to normal activities.1 With respect to postoperative events, clinicians typically employ the Clavien-Dindo grading system for the classification of surgical complications.2 The system consists of five grades, ranging from Grade I (any deviation from normal postoperative course, without the need for pharmacological intervention) to Grade V (death).
Following hysterectomy, postoperative urinary or pelvic infections are not uncommon, with an incidence of 15% to 20%.1 In the Clavien-Dindo system, these complications would typically be considered Grade II (pharmacological treatment other than what is considered an acceptable therapeutic regimen), requiring antibiotics and no surgical intervention. Grade III complications, however, usually involve postoperative issues that require surgical, endoscopic, or radiological intervention, which in VH would include ureteral, bladder, or bowel injury.1 In a study by Gendy et al,1 the incidence of such complications posthysterectomy, ranged from 1.7% to 5.7%. So while not extremely common, serious complications can occur postoperatively.
The last point is a minor one, but a truth every EP needs to remember: While it may be difficult for a patient to sue her or his own physician, especially one with whom she or he has a longstanding patient-physician relationship, it is much easier for her or him to place blame upon and sue another physician—for example, the EP.
Missed Testicular Torsion?
| A 14-year-old boy presented to the ED with a several day history of abdominal pain with radiation to the right testicle. The patient denied any nausea, vomiting, or changes in bowel habits. He also denied any genitourinary symptoms, including dysuria or urinary frequency. The boy was otherwise in good health, on no medications, and up to date on his immunizations. |
The patient was a well appearing teenager in no acute distress. All vital signs were normal, as were the heart and lung examinations. The abdominal examination revealed mild, generalized tenderness without guarding or rebound. The genitalia examination was normal.
The EP ordered a CBC, urinalysis, and a testicular ultrasound, the results of which were all normal. The patient was discharged home with instructions to follow up with his pediatrician in 2 days and to return to the ED if his symptoms worsened.
The patient was seen by his pediatrician approximately 1 month later for his scheduled annual physical examination. The pediatrician, who was aware of the boy’s prior ED visit, found the patient in good health, and performed no additional testing.
Approximately 9 months after the initial ED visit, the patient was accidently kicked in the groin while jumping on a trampoline. He experienced immediate onset of severe, excruciating right testicular pain and presented to the ED approximately 24 hours later with continued pain and swelling. A testicular ultrasound was immediately ordered and demonstrated an enlarged right testicle due to torsion.
The patient underwent surgery to remove the right testicle. His family sued the EP and hospital from the initial visit (9 months earlier) for missed intermittent testicular torsion. They argued that the patient should have been referred to a urologist for further evaluation. In addition, the plaintiff claimed he could no longer participate in sports and suffered disfigurement as a result of the surgery. The EP asserted that the patient’s pain during that initial visit was primarily abdominal in nature and that an ultrasound of the testicles was normal, and did not reveal any evidence of testicular torsion. The EP further argued that the testicular torsion was due to the trauma incurred on the trampoline. According to published accounts, a defense verdict was returned.
Discussion
Testicular torsion occurs in a bimodal age distribution—during the first year of life (perinatal) and between ages 13 and 16 years (as was the case with this patient).1 In approximately 4% to 8% of patients, there is a history of an athletic event, strenuous physical activity, or trauma just prior to the onset of scrotal pain.2
Patients typically present with sudden onset of testicular pain that is frequently associated with nausea and vomiting. However, this condition can present with only lower abdominal pain—in part be due to the fact that adolescents and children may be reluctant to complain of testicular or scrotal pain out of fear or embarrassment.1 In all cases, a genital examination should be performed on every adolescent male with a chief complaint of lower abdominal pain.3
On physical examination, the patient will usually have a swollen tender testicle. In comparison to the opposite side, the affected testicle is frequently raised and rests on a horizontal axis. The cremasteric reflex (ie, scratching the proximal inner thigh causes the ipsilateral testicle to rise) is frequently absent.4
Because of the time sensitive nature of the disease process, in classic presentations, a urologist should be immediately consulted. Ischemic changes to the testicle can begin within hours, and complete testicular atrophy occurs after 24 hours in most cases.4 Detorsion within 6 hours of onset of symptoms has a salvage rate of 90% to 100%, which drops to 25% to 50% after 12 hours and to less than 10% after 24 hours.4
For less obvious cases, color duplex testicular ultrasonography can be very helpful. Demonstration of decreased or absent blood flow is diagnostic and requires operative intervention. If untwisting the testis restores blood flow, then the condition is resolved; if this procedure fails, the testis is removed. Regardless of the outcome, the contralateral testis is fixed to prevent future torsion.
Intermittent testicular torsion is a difficult diagnosis to make. A history of recurrent unilateral scrotal pain is highly suspicious and warrants referral to a urologist. This patient had only one previous episode, which was primarily abdominal pain—not scrotal or testicular pain.
In this case, it appears the jury came to the correct decision. Given the patient had only one previous episode of abdominal pain, and an inciting event (trauma to the testicle) on the second presentation, this does not appear to be a case of missed intermittent testicular torsion. Rather, this was a correctly diagnosed testicular torsion with a delayed presentation, resulting in an unsalvageable testicle.
Reference - Sepsis Following Vaginal Hysterectomy
- Gendy R, Walsh CA, Walsh SR, Karantanis E. Vaginal hysterectomy versus total laparoscopic hysterectomy for benign disease: a metaanalysis of randomized controlled trials. Am J Obstet Gynecol. 2011;204(5):388.e1-8.
- Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009:250(2):187-196.
Reference - Missed Testicular Torsion?
- Pogorelić Z, Mrklić I, Jurić I. Do not forget to include testicular torsion in differential diagnosis of lower acute abdominal pain in young males. J Pediatr Urol. 2013;9(6 Pt B):1161-1165.
- Nicks BA, Manthey DE. Male genital problems. In: Tintinalli JE, Stapczynski JS, Ma OJ, Cine DM, Cydulka RK, Meckler GD, eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 7th ed. New York: McGraw-Hill Medical; 2011:649.
- Lopez RN, Beasley SW. Testicular torsion: potential pitfalls in its diagnosis and management. J Paediatr Child Health. 2012;48(2):E30-E32.
- Somani BK, Watson G, Townell N. Testicular torsion. BMJ. 2010;341:c3213.
Sepsis Following Vaginal Hysterectomy
| A 45-year-old woman presented to the ED complaining of lower abdominal pain, which she described as gradual, aching, and intermittent. The patient stated that she had undergone a vaginal hysterectomy a few days prior and that the pain started less than 24 hours after discharge from the hospital. She denied fever or chills, nausea, or vomiting, and said that she had a bowel movement earlier that day. She also denied any urinary symptoms. Her medical history was significant only for hypothyroidism, for which she was taking levothyroxine. The patient denied cigarette smoking or alcohol consumption. She said she had been taking acetaminophen-hydrocodone for postoperative pain, but that it did not provide any relief. |
The patient’s vital signs were: temperature, 98.6˚F; blood pressure, 112/65 mm Hg; heart rate, 98 beats/minute; and respiratory rate, 20 breaths/minute. The head, eyes, ears, nose, and throat examination was normal, as were the heart and lung examinations. The patient’s abdomen was soft, with mild diffuse lower abdominal tenderness. There was no guarding, rebound, or mass present. A gross nonspeculum examination of the vaginal area did not reveal any discharge or erythema; a rectal examination was not performed.
The EP ordered a complete blood count (CBC), lipase evaluation, and urinalysis. All test results were normal. The emergency physician (EP) then contacted the obstetrician-gynecologist (OB/GYN) who had performed the hysterectomy. The OB/GYN recommended the EP change the analgesic agent to acetaminophen-oxycodone and to encourage the patient to keep her follow-up postoperative appointment in 1 week. The EP followed these instructions and discharged the patient home with a prescription for the new analgesic.
Three days later, however, the patient presented back to the same ED complaining of increased and now generalized abdominal pain, nausea, and vomiting. She was noted to be febrile, tachycardic, and hypotensive. On physical examination, her abdomen was diffusely tender with guarding and rebound. She was given a 2-L bolus of intravenous (IV) normal saline and started on broad spectrum IV antibiotics. After another consultation with the patient’s OB/GYN surgeon, the patient was taken immediately to the operating room. On exploration, she was found to have a segment of perforated bowel and peritonitis. A portion of the bowel was resected, but her postoperative course was complicated by sepsis. After a 1-month stay in the hospital, she was discharged home.
The patient sued the EP—but not her OB/GYN—for failure to obtain a CT scan of the abdomen/pelvis on her initial ED visit, or at least to admit her to the hospital for observation. The EP argued that even if a computed tomography (CT) scan had been performed on the initial visit, it probably would have been normal, since the bowel had not yet perforated. After trial, a defense verdict was returned.
Discussion
This case illustrates two important points. First, not every patient with abdominal pain requires a CT scan of the abdomen/pelvis. So many malpractice cases against EPs involve the failure to perform advanced imaging. Unfortunately, that is usually only through the benefit of hindsight. For a patient with mild abdominal pain, only minimal tenderness on examination, and a negative laboratory workup, it can be perfectly appropriate to treat him or her symptomatically with close follow-up and specific instructions to return to the ED if his or her condition worsens (as was the case with this patient).
The second important point is to not over-rely on a consultant(s), especially if she or he has not independently examined the patient. When calling a consultant, it is best to have a specific question (ie, “Can you see the patient in the morning?”) or action (ie, “I would like to admit the patient to your service”). In general, the EP should not rely on the consultant to give “permission” to discharge the patient. As the physician seeing the patient, the EP is the most well-equipped to work up the patient and determine the needed disposition. Rare is the consultant that can arrive at a better disposition than the EP who performed the history and physical examination on the patient.
Regarding the patient’s GYN surgery, vaginal hysterectomy (VH) is preferred over abdominal hysterectomy (AH) for benign disease as it is associated with reduced infective morbidity and earlier return to normal activities.1 With respect to postoperative events, clinicians typically employ the Clavien-Dindo grading system for the classification of surgical complications.2 The system consists of five grades, ranging from Grade I (any deviation from normal postoperative course, without the need for pharmacological intervention) to Grade V (death).
Following hysterectomy, postoperative urinary or pelvic infections are not uncommon, with an incidence of 15% to 20%.1 In the Clavien-Dindo system, these complications would typically be considered Grade II (pharmacological treatment other than what is considered an acceptable therapeutic regimen), requiring antibiotics and no surgical intervention. Grade III complications, however, usually involve postoperative issues that require surgical, endoscopic, or radiological intervention, which in VH would include ureteral, bladder, or bowel injury.1 In a study by Gendy et al,1 the incidence of such complications posthysterectomy, ranged from 1.7% to 5.7%. So while not extremely common, serious complications can occur postoperatively.
The last point is a minor one, but a truth every EP needs to remember: While it may be difficult for a patient to sue her or his own physician, especially one with whom she or he has a longstanding patient-physician relationship, it is much easier for her or him to place blame upon and sue another physician—for example, the EP.
Missed Testicular Torsion?
| A 14-year-old boy presented to the ED with a several day history of abdominal pain with radiation to the right testicle. The patient denied any nausea, vomiting, or changes in bowel habits. He also denied any genitourinary symptoms, including dysuria or urinary frequency. The boy was otherwise in good health, on no medications, and up to date on his immunizations. |
The patient was a well appearing teenager in no acute distress. All vital signs were normal, as were the heart and lung examinations. The abdominal examination revealed mild, generalized tenderness without guarding or rebound. The genitalia examination was normal.
The EP ordered a CBC, urinalysis, and a testicular ultrasound, the results of which were all normal. The patient was discharged home with instructions to follow up with his pediatrician in 2 days and to return to the ED if his symptoms worsened.
The patient was seen by his pediatrician approximately 1 month later for his scheduled annual physical examination. The pediatrician, who was aware of the boy’s prior ED visit, found the patient in good health, and performed no additional testing.
Approximately 9 months after the initial ED visit, the patient was accidently kicked in the groin while jumping on a trampoline. He experienced immediate onset of severe, excruciating right testicular pain and presented to the ED approximately 24 hours later with continued pain and swelling. A testicular ultrasound was immediately ordered and demonstrated an enlarged right testicle due to torsion.
The patient underwent surgery to remove the right testicle. His family sued the EP and hospital from the initial visit (9 months earlier) for missed intermittent testicular torsion. They argued that the patient should have been referred to a urologist for further evaluation. In addition, the plaintiff claimed he could no longer participate in sports and suffered disfigurement as a result of the surgery. The EP asserted that the patient’s pain during that initial visit was primarily abdominal in nature and that an ultrasound of the testicles was normal, and did not reveal any evidence of testicular torsion. The EP further argued that the testicular torsion was due to the trauma incurred on the trampoline. According to published accounts, a defense verdict was returned.
Discussion
Testicular torsion occurs in a bimodal age distribution—during the first year of life (perinatal) and between ages 13 and 16 years (as was the case with this patient).1 In approximately 4% to 8% of patients, there is a history of an athletic event, strenuous physical activity, or trauma just prior to the onset of scrotal pain.2
Patients typically present with sudden onset of testicular pain that is frequently associated with nausea and vomiting. However, this condition can present with only lower abdominal pain—in part be due to the fact that adolescents and children may be reluctant to complain of testicular or scrotal pain out of fear or embarrassment.1 In all cases, a genital examination should be performed on every adolescent male with a chief complaint of lower abdominal pain.3
On physical examination, the patient will usually have a swollen tender testicle. In comparison to the opposite side, the affected testicle is frequently raised and rests on a horizontal axis. The cremasteric reflex (ie, scratching the proximal inner thigh causes the ipsilateral testicle to rise) is frequently absent.4
Because of the time sensitive nature of the disease process, in classic presentations, a urologist should be immediately consulted. Ischemic changes to the testicle can begin within hours, and complete testicular atrophy occurs after 24 hours in most cases.4 Detorsion within 6 hours of onset of symptoms has a salvage rate of 90% to 100%, which drops to 25% to 50% after 12 hours and to less than 10% after 24 hours.4
For less obvious cases, color duplex testicular ultrasonography can be very helpful. Demonstration of decreased or absent blood flow is diagnostic and requires operative intervention. If untwisting the testis restores blood flow, then the condition is resolved; if this procedure fails, the testis is removed. Regardless of the outcome, the contralateral testis is fixed to prevent future torsion.
Intermittent testicular torsion is a difficult diagnosis to make. A history of recurrent unilateral scrotal pain is highly suspicious and warrants referral to a urologist. This patient had only one previous episode, which was primarily abdominal pain—not scrotal or testicular pain.
In this case, it appears the jury came to the correct decision. Given the patient had only one previous episode of abdominal pain, and an inciting event (trauma to the testicle) on the second presentation, this does not appear to be a case of missed intermittent testicular torsion. Rather, this was a correctly diagnosed testicular torsion with a delayed presentation, resulting in an unsalvageable testicle.
Sepsis Following Vaginal Hysterectomy
| A 45-year-old woman presented to the ED complaining of lower abdominal pain, which she described as gradual, aching, and intermittent. The patient stated that she had undergone a vaginal hysterectomy a few days prior and that the pain started less than 24 hours after discharge from the hospital. She denied fever or chills, nausea, or vomiting, and said that she had a bowel movement earlier that day. She also denied any urinary symptoms. Her medical history was significant only for hypothyroidism, for which she was taking levothyroxine. The patient denied cigarette smoking or alcohol consumption. She said she had been taking acetaminophen-hydrocodone for postoperative pain, but that it did not provide any relief. |
The patient’s vital signs were: temperature, 98.6˚F; blood pressure, 112/65 mm Hg; heart rate, 98 beats/minute; and respiratory rate, 20 breaths/minute. The head, eyes, ears, nose, and throat examination was normal, as were the heart and lung examinations. The patient’s abdomen was soft, with mild diffuse lower abdominal tenderness. There was no guarding, rebound, or mass present. A gross nonspeculum examination of the vaginal area did not reveal any discharge or erythema; a rectal examination was not performed.
The EP ordered a complete blood count (CBC), lipase evaluation, and urinalysis. All test results were normal. The emergency physician (EP) then contacted the obstetrician-gynecologist (OB/GYN) who had performed the hysterectomy. The OB/GYN recommended the EP change the analgesic agent to acetaminophen-oxycodone and to encourage the patient to keep her follow-up postoperative appointment in 1 week. The EP followed these instructions and discharged the patient home with a prescription for the new analgesic.
Three days later, however, the patient presented back to the same ED complaining of increased and now generalized abdominal pain, nausea, and vomiting. She was noted to be febrile, tachycardic, and hypotensive. On physical examination, her abdomen was diffusely tender with guarding and rebound. She was given a 2-L bolus of intravenous (IV) normal saline and started on broad spectrum IV antibiotics. After another consultation with the patient’s OB/GYN surgeon, the patient was taken immediately to the operating room. On exploration, she was found to have a segment of perforated bowel and peritonitis. A portion of the bowel was resected, but her postoperative course was complicated by sepsis. After a 1-month stay in the hospital, she was discharged home.
The patient sued the EP—but not her OB/GYN—for failure to obtain a CT scan of the abdomen/pelvis on her initial ED visit, or at least to admit her to the hospital for observation. The EP argued that even if a computed tomography (CT) scan had been performed on the initial visit, it probably would have been normal, since the bowel had not yet perforated. After trial, a defense verdict was returned.
Discussion
This case illustrates two important points. First, not every patient with abdominal pain requires a CT scan of the abdomen/pelvis. So many malpractice cases against EPs involve the failure to perform advanced imaging. Unfortunately, that is usually only through the benefit of hindsight. For a patient with mild abdominal pain, only minimal tenderness on examination, and a negative laboratory workup, it can be perfectly appropriate to treat him or her symptomatically with close follow-up and specific instructions to return to the ED if his or her condition worsens (as was the case with this patient).
The second important point is to not over-rely on a consultant(s), especially if she or he has not independently examined the patient. When calling a consultant, it is best to have a specific question (ie, “Can you see the patient in the morning?”) or action (ie, “I would like to admit the patient to your service”). In general, the EP should not rely on the consultant to give “permission” to discharge the patient. As the physician seeing the patient, the EP is the most well-equipped to work up the patient and determine the needed disposition. Rare is the consultant that can arrive at a better disposition than the EP who performed the history and physical examination on the patient.
Regarding the patient’s GYN surgery, vaginal hysterectomy (VH) is preferred over abdominal hysterectomy (AH) for benign disease as it is associated with reduced infective morbidity and earlier return to normal activities.1 With respect to postoperative events, clinicians typically employ the Clavien-Dindo grading system for the classification of surgical complications.2 The system consists of five grades, ranging from Grade I (any deviation from normal postoperative course, without the need for pharmacological intervention) to Grade V (death).
Following hysterectomy, postoperative urinary or pelvic infections are not uncommon, with an incidence of 15% to 20%.1 In the Clavien-Dindo system, these complications would typically be considered Grade II (pharmacological treatment other than what is considered an acceptable therapeutic regimen), requiring antibiotics and no surgical intervention. Grade III complications, however, usually involve postoperative issues that require surgical, endoscopic, or radiological intervention, which in VH would include ureteral, bladder, or bowel injury.1 In a study by Gendy et al,1 the incidence of such complications posthysterectomy, ranged from 1.7% to 5.7%. So while not extremely common, serious complications can occur postoperatively.
The last point is a minor one, but a truth every EP needs to remember: While it may be difficult for a patient to sue her or his own physician, especially one with whom she or he has a longstanding patient-physician relationship, it is much easier for her or him to place blame upon and sue another physician—for example, the EP.
Missed Testicular Torsion?
| A 14-year-old boy presented to the ED with a several day history of abdominal pain with radiation to the right testicle. The patient denied any nausea, vomiting, or changes in bowel habits. He also denied any genitourinary symptoms, including dysuria or urinary frequency. The boy was otherwise in good health, on no medications, and up to date on his immunizations. |
The patient was a well appearing teenager in no acute distress. All vital signs were normal, as were the heart and lung examinations. The abdominal examination revealed mild, generalized tenderness without guarding or rebound. The genitalia examination was normal.
The EP ordered a CBC, urinalysis, and a testicular ultrasound, the results of which were all normal. The patient was discharged home with instructions to follow up with his pediatrician in 2 days and to return to the ED if his symptoms worsened.
The patient was seen by his pediatrician approximately 1 month later for his scheduled annual physical examination. The pediatrician, who was aware of the boy’s prior ED visit, found the patient in good health, and performed no additional testing.
Approximately 9 months after the initial ED visit, the patient was accidently kicked in the groin while jumping on a trampoline. He experienced immediate onset of severe, excruciating right testicular pain and presented to the ED approximately 24 hours later with continued pain and swelling. A testicular ultrasound was immediately ordered and demonstrated an enlarged right testicle due to torsion.
The patient underwent surgery to remove the right testicle. His family sued the EP and hospital from the initial visit (9 months earlier) for missed intermittent testicular torsion. They argued that the patient should have been referred to a urologist for further evaluation. In addition, the plaintiff claimed he could no longer participate in sports and suffered disfigurement as a result of the surgery. The EP asserted that the patient’s pain during that initial visit was primarily abdominal in nature and that an ultrasound of the testicles was normal, and did not reveal any evidence of testicular torsion. The EP further argued that the testicular torsion was due to the trauma incurred on the trampoline. According to published accounts, a defense verdict was returned.
Discussion
Testicular torsion occurs in a bimodal age distribution—during the first year of life (perinatal) and between ages 13 and 16 years (as was the case with this patient).1 In approximately 4% to 8% of patients, there is a history of an athletic event, strenuous physical activity, or trauma just prior to the onset of scrotal pain.2
Patients typically present with sudden onset of testicular pain that is frequently associated with nausea and vomiting. However, this condition can present with only lower abdominal pain—in part be due to the fact that adolescents and children may be reluctant to complain of testicular or scrotal pain out of fear or embarrassment.1 In all cases, a genital examination should be performed on every adolescent male with a chief complaint of lower abdominal pain.3
On physical examination, the patient will usually have a swollen tender testicle. In comparison to the opposite side, the affected testicle is frequently raised and rests on a horizontal axis. The cremasteric reflex (ie, scratching the proximal inner thigh causes the ipsilateral testicle to rise) is frequently absent.4
Because of the time sensitive nature of the disease process, in classic presentations, a urologist should be immediately consulted. Ischemic changes to the testicle can begin within hours, and complete testicular atrophy occurs after 24 hours in most cases.4 Detorsion within 6 hours of onset of symptoms has a salvage rate of 90% to 100%, which drops to 25% to 50% after 12 hours and to less than 10% after 24 hours.4
For less obvious cases, color duplex testicular ultrasonography can be very helpful. Demonstration of decreased or absent blood flow is diagnostic and requires operative intervention. If untwisting the testis restores blood flow, then the condition is resolved; if this procedure fails, the testis is removed. Regardless of the outcome, the contralateral testis is fixed to prevent future torsion.
Intermittent testicular torsion is a difficult diagnosis to make. A history of recurrent unilateral scrotal pain is highly suspicious and warrants referral to a urologist. This patient had only one previous episode, which was primarily abdominal pain—not scrotal or testicular pain.
In this case, it appears the jury came to the correct decision. Given the patient had only one previous episode of abdominal pain, and an inciting event (trauma to the testicle) on the second presentation, this does not appear to be a case of missed intermittent testicular torsion. Rather, this was a correctly diagnosed testicular torsion with a delayed presentation, resulting in an unsalvageable testicle.
Reference - Sepsis Following Vaginal Hysterectomy
- Gendy R, Walsh CA, Walsh SR, Karantanis E. Vaginal hysterectomy versus total laparoscopic hysterectomy for benign disease: a metaanalysis of randomized controlled trials. Am J Obstet Gynecol. 2011;204(5):388.e1-8.
- Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009:250(2):187-196.
Reference - Missed Testicular Torsion?
- Pogorelić Z, Mrklić I, Jurić I. Do not forget to include testicular torsion in differential diagnosis of lower acute abdominal pain in young males. J Pediatr Urol. 2013;9(6 Pt B):1161-1165.
- Nicks BA, Manthey DE. Male genital problems. In: Tintinalli JE, Stapczynski JS, Ma OJ, Cine DM, Cydulka RK, Meckler GD, eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 7th ed. New York: McGraw-Hill Medical; 2011:649.
- Lopez RN, Beasley SW. Testicular torsion: potential pitfalls in its diagnosis and management. J Paediatr Child Health. 2012;48(2):E30-E32.
- Somani BK, Watson G, Townell N. Testicular torsion. BMJ. 2010;341:c3213.
Reference - Sepsis Following Vaginal Hysterectomy
- Gendy R, Walsh CA, Walsh SR, Karantanis E. Vaginal hysterectomy versus total laparoscopic hysterectomy for benign disease: a metaanalysis of randomized controlled trials. Am J Obstet Gynecol. 2011;204(5):388.e1-8.
- Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009:250(2):187-196.
Reference - Missed Testicular Torsion?
- Pogorelić Z, Mrklić I, Jurić I. Do not forget to include testicular torsion in differential diagnosis of lower acute abdominal pain in young males. J Pediatr Urol. 2013;9(6 Pt B):1161-1165.
- Nicks BA, Manthey DE. Male genital problems. In: Tintinalli JE, Stapczynski JS, Ma OJ, Cine DM, Cydulka RK, Meckler GD, eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 7th ed. New York: McGraw-Hill Medical; 2011:649.
- Lopez RN, Beasley SW. Testicular torsion: potential pitfalls in its diagnosis and management. J Paediatr Child Health. 2012;48(2):E30-E32.
- Somani BK, Watson G, Townell N. Testicular torsion. BMJ. 2010;341:c3213.
Malpractice Counsel
Carbon Monoxide Poisoning
A 72-year-old man was brought to the ED by paramedics with inability to move his left leg and difficulty speaking. The patient had been heating his home with a generator placed inside the house during an ice storm, and paramedics reported a strong smell of gas inside the house.
The patient was unable to describe the time of onset of his symptoms. He complained of headache, slurred speech, and inability to move his left leg. He also said he felt the urge to urinate, but was unable to do so. He denied chest pain or shortness of breath. His medical history was significant only for hypertension, which was controlled with hydrochlorothiazide and lisinopril. He admitted to smoking a few cigarettes daily, but denied any alcohol use.
On physical examination, the patient’s vital signs were: blood pressure (BP) 162/98 mm Hg; heart rate (HR), 110 beats/minute; respiratory rate (RR), 20 breaths/minute; and temperature (T), 98.6˚F. The patient had 100% oxygen (O2) saturation on 4L O2 via nasal cannula. The head, eyes, ears, nose, and throat examination was normal. There was no facial droop; his speech was slurred, but he was easily understandable. The cardiopulmonary examination revealed tachycardia without murmurs, rubs, or gallop; the lungs were clear to auscultation bilaterally. The neurological examination revealed 5/5 motor strength in the upper extremities and symmetrical; there was no pronator drift. The left leg had 2/5 motor strength compared to 5/5 in the right lower extremity. There was also fullness and tenderness over his suprapubic region.
The emergency physician (EP) ordered a complete blood count, basic metabolic profile, carboxyhemoglobin (COHb) test, electrocardiogram (ECG), portable chest X-ray (CXR), and a noncontrast computed tomography (CT) scan of the head. Since the history and physical examination suggested urinary retention, a Foley catheter was placed; a total of 1,200 cc of clear urine was obtained, after which the patient expressed a feeling of relief.
The patient’s COHb level was 8.5%. The portable CXR and CT scan of the head were both reported as normal by the radiologist. Likewise, the results of the rest of the laboratory evaluation were normal. The ECG revealed sinus tachycardia without evidence of strain or injury.
The EP diagnosed an acute cerebrovascular accident (CVA) and admitted the patient to the hospital. He did not feel that carbon monoxide (CO) contributed to the event given the low level in a cigarette smoker. After an uneventful hospital stay, the patient was transferred to a physical rehabilitation unit. He was ultimately discharged with a neurogenic bladder and weak left leg.
The patient sued the EP for negligence in the failure to diagnose CO poisoning and prompt initiation of 100% O2 therapy. The EP argued that CO poisoning had been properly ruled out and that the diagnosis of CVA was correct. The defense also claimed that even if the patient had suffered CO poisoning, the length of the exposure would have led to the same outcome. A defense verdict was returned.
Discussion
Carbon monoxide poisoning is one of the leading causes of poisoning morbidity and mortality in the United States. This is in part due to the fact that CO is a colorless, odorless, and tasteless gas. The peak incidence for CO poisoning is in the fall and winter, when people are more likely to use space heaters, wood burning stoves, or portable generators inside without adequate ventilation.
The clinical presentation of CO poisoning can range from mild (eg, headache, flu-like symptoms) to devastating (eg, coma, death). The central nervous system is the organ system that is most sensitive to CO poisoning. Symptoms can range from a dull frontal headache, dizziness, and ataxia, to syncope, seizures, focal neurological deficit, and coma. In fact, the most serious complication of CO poisoning may be persistent or delayed neurological or neurocognitive sequelae, which can occur in up to 50% of patients with symptomatic acute poisoning.1 Unfortunately, COHb levels and symptoms do not always correlate well. In fact, particular COHb levels are not predictive of symptoms or outcome.1
The treatment for CO poisoning consists of administering 100% O2 as soon as the diagnosis is considered. If 100% O2 is administered, the half-life of COHb can be reduced from 5 hours (room air) to approximately 1 hour.1 While some argue that treatment with hyperbaric O2 (HBO) therapy should be considered standard of care, it has not yet been determined which patient population benefits from HBO therapy; moreover, there is currently no established optimum timing of therapy. Regardless, the jury came to the correct decision in this case as it is impossible to determine, with any degree of medical certainty, if the patient’s neurological deficits were due to the natural course of an ischemic stroke, or if CO contributed to or was the sole cause of the CVA.
Death in the Emergency Department
A 43-year-old man presented to the ED with the chief complaint of a lower lip laceration. The patient stated he had gotten into an altercation with his girlfriend just prior to arrival. She had punched the patient in the face with her fist, resulting in the lip laceration. The patient denied any loss of consciousness or other pain. He did, however, smell of alcohol and was emotionally labile, crying one moment and yelling the next.
The patient was instructed to remove all of his clothes, change into a hospital gown and give all of his belongings to hospital security. He removed his clothes, but refused to turn them over to security. This prompted a physical altercation between the patient and hospital security. Three hospital security guards wrestled the patient to the ground and placed him face down; one guard placed the patient in a choke hold while the other two guards sat on top of him. Within a few moments, the patient became unresponsive. He was placed immediately on a stretcher and intubated by the EP. After successful intubation and bagging with 100% O2, the patient regained a palpable pulse, but remained unresponsive.
The patient was admitted to the intensive care unit, but never regained consciousness and died 5 days later. The cause of death was thought to be anoxic brain injury due to asphyxiation. The family of the patient sued the hospital and the EP for causing asphyxiation and death in this patient seeking medical care. The hospital denied responsibility for the death because the patient both instigated the altercation and had a preexisting heart condition. According to published reports, a $2.5 million settlement was reached.
Discussion
This unfortunate case did not involve the EP; all of the important events transpired prior to the EP’s initial interaction with the patient. There are not enough details to explain how this situation escalated so rapidly, or why hospital security felt this was the best way to subdue the patient.
Unfortunately, EPs are no strangers to agitated patients. Behavioral emergencies account for approximately 5% of all ED visits, and these usually involve some form of violence or agitation.1 Every physician and nurse working in the ED must be prepared to deal with patients who have the potential to become violent. Clearly, training of all patient-care personnel to handle such patients in the ED is important to ensuring both staff and patient safety. Having the patient undress and change into a hospital gown is the correct first step. This allows for removal of real or potential weapons, and makes it much less likely for the patient to leave before his or her evaluation and management is complete. Doing this properly, however, is key. Providing the patient with a warm blanket or food, or just talking to him or her in a calm and reassuring voice, can often prevent escalation. Simply arguing with the patient rarely works, and often has the opposite desired effect.
If the situation continues to escalate, and it appears either physical or chemical restraint will be necessary, a “show of force” should be made. A restraint team consisting of at least five trained members should be assembled, with the EP acting as the team leader. The team should all enter the room at the same time, explain what will happen, and then move quickly.1 The leader should move to the head of the bed and direct the team, while the remaining four members each take a limb. To preserve the physician-patient relationship, it is best if the EP is not actively involved in placing the physical restraints.
The choke hold should only be considered as a method of last resort. Many police departments in the country prohibit use of the choke hold because of complications such as those observed in this case. The use of choke holds became a topic of intense debate this summer with the death of Eric Garner in Staten Island, New York; it was thought that his pre-existing conditions of obesity, asthma, and heart disease were all aggravated by the choke hold. Although obese patients are often at a higher risk for complications due to pre-existing issues with adequate oxygenation, it is unclear whether the patient in this case was obese.
An alternative strategy in handling an agitated patient would be the use of a taser by trained security personnel. In one study, 99.75% of tasered patients had no significant injury as a result of the device.2 In 2009, the American Medical Association found that tasers, “when used appropriately, can save lives during interventions that would have otherwise involved the use of deadly force.” While the safety of patients and the ED staff (nurses, physicians, and technicians) is paramount, the clinician should always adhere to the principle of “primum non nocere”—“first, do no harm.”
Reference - Carbon Monoxide Poisoning
- Tomaszewski C: Carbon monoxide. In: Nelson LS, Lewin NA, Howland MA, Hoffman RS, Goldfrank LR, Flomenbaum NE, eds. Goldfrank’s Toxicologic Emergencies. 9th ed. New York, NY: McGraw Hill; 2011:1658.
Reference - Death in the Emergency Department
- Rossi J, Swan MC, Issacs ED. The violent or agitated patient. Emerg Med Clin North Am. 2010;28(1):235-256.
- Bozeman WP, Hauda WE 2nd, Heck JJ, Graham DD Jr, Martin BP, Winslow JE. Safety and injury profile of conducted electrical weapons used by law enforcement officers against criminal suspects. Ann Emerg Med. 2009;53(4):480-489.
Carbon Monoxide Poisoning
A 72-year-old man was brought to the ED by paramedics with inability to move his left leg and difficulty speaking. The patient had been heating his home with a generator placed inside the house during an ice storm, and paramedics reported a strong smell of gas inside the house.
The patient was unable to describe the time of onset of his symptoms. He complained of headache, slurred speech, and inability to move his left leg. He also said he felt the urge to urinate, but was unable to do so. He denied chest pain or shortness of breath. His medical history was significant only for hypertension, which was controlled with hydrochlorothiazide and lisinopril. He admitted to smoking a few cigarettes daily, but denied any alcohol use.
On physical examination, the patient’s vital signs were: blood pressure (BP) 162/98 mm Hg; heart rate (HR), 110 beats/minute; respiratory rate (RR), 20 breaths/minute; and temperature (T), 98.6˚F. The patient had 100% oxygen (O2) saturation on 4L O2 via nasal cannula. The head, eyes, ears, nose, and throat examination was normal. There was no facial droop; his speech was slurred, but he was easily understandable. The cardiopulmonary examination revealed tachycardia without murmurs, rubs, or gallop; the lungs were clear to auscultation bilaterally. The neurological examination revealed 5/5 motor strength in the upper extremities and symmetrical; there was no pronator drift. The left leg had 2/5 motor strength compared to 5/5 in the right lower extremity. There was also fullness and tenderness over his suprapubic region.
The emergency physician (EP) ordered a complete blood count, basic metabolic profile, carboxyhemoglobin (COHb) test, electrocardiogram (ECG), portable chest X-ray (CXR), and a noncontrast computed tomography (CT) scan of the head. Since the history and physical examination suggested urinary retention, a Foley catheter was placed; a total of 1,200 cc of clear urine was obtained, after which the patient expressed a feeling of relief.
The patient’s COHb level was 8.5%. The portable CXR and CT scan of the head were both reported as normal by the radiologist. Likewise, the results of the rest of the laboratory evaluation were normal. The ECG revealed sinus tachycardia without evidence of strain or injury.
The EP diagnosed an acute cerebrovascular accident (CVA) and admitted the patient to the hospital. He did not feel that carbon monoxide (CO) contributed to the event given the low level in a cigarette smoker. After an uneventful hospital stay, the patient was transferred to a physical rehabilitation unit. He was ultimately discharged with a neurogenic bladder and weak left leg.
The patient sued the EP for negligence in the failure to diagnose CO poisoning and prompt initiation of 100% O2 therapy. The EP argued that CO poisoning had been properly ruled out and that the diagnosis of CVA was correct. The defense also claimed that even if the patient had suffered CO poisoning, the length of the exposure would have led to the same outcome. A defense verdict was returned.
Discussion
Carbon monoxide poisoning is one of the leading causes of poisoning morbidity and mortality in the United States. This is in part due to the fact that CO is a colorless, odorless, and tasteless gas. The peak incidence for CO poisoning is in the fall and winter, when people are more likely to use space heaters, wood burning stoves, or portable generators inside without adequate ventilation.
The clinical presentation of CO poisoning can range from mild (eg, headache, flu-like symptoms) to devastating (eg, coma, death). The central nervous system is the organ system that is most sensitive to CO poisoning. Symptoms can range from a dull frontal headache, dizziness, and ataxia, to syncope, seizures, focal neurological deficit, and coma. In fact, the most serious complication of CO poisoning may be persistent or delayed neurological or neurocognitive sequelae, which can occur in up to 50% of patients with symptomatic acute poisoning.1 Unfortunately, COHb levels and symptoms do not always correlate well. In fact, particular COHb levels are not predictive of symptoms or outcome.1
The treatment for CO poisoning consists of administering 100% O2 as soon as the diagnosis is considered. If 100% O2 is administered, the half-life of COHb can be reduced from 5 hours (room air) to approximately 1 hour.1 While some argue that treatment with hyperbaric O2 (HBO) therapy should be considered standard of care, it has not yet been determined which patient population benefits from HBO therapy; moreover, there is currently no established optimum timing of therapy. Regardless, the jury came to the correct decision in this case as it is impossible to determine, with any degree of medical certainty, if the patient’s neurological deficits were due to the natural course of an ischemic stroke, or if CO contributed to or was the sole cause of the CVA.
Death in the Emergency Department
A 43-year-old man presented to the ED with the chief complaint of a lower lip laceration. The patient stated he had gotten into an altercation with his girlfriend just prior to arrival. She had punched the patient in the face with her fist, resulting in the lip laceration. The patient denied any loss of consciousness or other pain. He did, however, smell of alcohol and was emotionally labile, crying one moment and yelling the next.
The patient was instructed to remove all of his clothes, change into a hospital gown and give all of his belongings to hospital security. He removed his clothes, but refused to turn them over to security. This prompted a physical altercation between the patient and hospital security. Three hospital security guards wrestled the patient to the ground and placed him face down; one guard placed the patient in a choke hold while the other two guards sat on top of him. Within a few moments, the patient became unresponsive. He was placed immediately on a stretcher and intubated by the EP. After successful intubation and bagging with 100% O2, the patient regained a palpable pulse, but remained unresponsive.
The patient was admitted to the intensive care unit, but never regained consciousness and died 5 days later. The cause of death was thought to be anoxic brain injury due to asphyxiation. The family of the patient sued the hospital and the EP for causing asphyxiation and death in this patient seeking medical care. The hospital denied responsibility for the death because the patient both instigated the altercation and had a preexisting heart condition. According to published reports, a $2.5 million settlement was reached.
Discussion
This unfortunate case did not involve the EP; all of the important events transpired prior to the EP’s initial interaction with the patient. There are not enough details to explain how this situation escalated so rapidly, or why hospital security felt this was the best way to subdue the patient.
Unfortunately, EPs are no strangers to agitated patients. Behavioral emergencies account for approximately 5% of all ED visits, and these usually involve some form of violence or agitation.1 Every physician and nurse working in the ED must be prepared to deal with patients who have the potential to become violent. Clearly, training of all patient-care personnel to handle such patients in the ED is important to ensuring both staff and patient safety. Having the patient undress and change into a hospital gown is the correct first step. This allows for removal of real or potential weapons, and makes it much less likely for the patient to leave before his or her evaluation and management is complete. Doing this properly, however, is key. Providing the patient with a warm blanket or food, or just talking to him or her in a calm and reassuring voice, can often prevent escalation. Simply arguing with the patient rarely works, and often has the opposite desired effect.
If the situation continues to escalate, and it appears either physical or chemical restraint will be necessary, a “show of force” should be made. A restraint team consisting of at least five trained members should be assembled, with the EP acting as the team leader. The team should all enter the room at the same time, explain what will happen, and then move quickly.1 The leader should move to the head of the bed and direct the team, while the remaining four members each take a limb. To preserve the physician-patient relationship, it is best if the EP is not actively involved in placing the physical restraints.
The choke hold should only be considered as a method of last resort. Many police departments in the country prohibit use of the choke hold because of complications such as those observed in this case. The use of choke holds became a topic of intense debate this summer with the death of Eric Garner in Staten Island, New York; it was thought that his pre-existing conditions of obesity, asthma, and heart disease were all aggravated by the choke hold. Although obese patients are often at a higher risk for complications due to pre-existing issues with adequate oxygenation, it is unclear whether the patient in this case was obese.
An alternative strategy in handling an agitated patient would be the use of a taser by trained security personnel. In one study, 99.75% of tasered patients had no significant injury as a result of the device.2 In 2009, the American Medical Association found that tasers, “when used appropriately, can save lives during interventions that would have otherwise involved the use of deadly force.” While the safety of patients and the ED staff (nurses, physicians, and technicians) is paramount, the clinician should always adhere to the principle of “primum non nocere”—“first, do no harm.”
Carbon Monoxide Poisoning
A 72-year-old man was brought to the ED by paramedics with inability to move his left leg and difficulty speaking. The patient had been heating his home with a generator placed inside the house during an ice storm, and paramedics reported a strong smell of gas inside the house.
The patient was unable to describe the time of onset of his symptoms. He complained of headache, slurred speech, and inability to move his left leg. He also said he felt the urge to urinate, but was unable to do so. He denied chest pain or shortness of breath. His medical history was significant only for hypertension, which was controlled with hydrochlorothiazide and lisinopril. He admitted to smoking a few cigarettes daily, but denied any alcohol use.
On physical examination, the patient’s vital signs were: blood pressure (BP) 162/98 mm Hg; heart rate (HR), 110 beats/minute; respiratory rate (RR), 20 breaths/minute; and temperature (T), 98.6˚F. The patient had 100% oxygen (O2) saturation on 4L O2 via nasal cannula. The head, eyes, ears, nose, and throat examination was normal. There was no facial droop; his speech was slurred, but he was easily understandable. The cardiopulmonary examination revealed tachycardia without murmurs, rubs, or gallop; the lungs were clear to auscultation bilaterally. The neurological examination revealed 5/5 motor strength in the upper extremities and symmetrical; there was no pronator drift. The left leg had 2/5 motor strength compared to 5/5 in the right lower extremity. There was also fullness and tenderness over his suprapubic region.
The emergency physician (EP) ordered a complete blood count, basic metabolic profile, carboxyhemoglobin (COHb) test, electrocardiogram (ECG), portable chest X-ray (CXR), and a noncontrast computed tomography (CT) scan of the head. Since the history and physical examination suggested urinary retention, a Foley catheter was placed; a total of 1,200 cc of clear urine was obtained, after which the patient expressed a feeling of relief.
The patient’s COHb level was 8.5%. The portable CXR and CT scan of the head were both reported as normal by the radiologist. Likewise, the results of the rest of the laboratory evaluation were normal. The ECG revealed sinus tachycardia without evidence of strain or injury.
The EP diagnosed an acute cerebrovascular accident (CVA) and admitted the patient to the hospital. He did not feel that carbon monoxide (CO) contributed to the event given the low level in a cigarette smoker. After an uneventful hospital stay, the patient was transferred to a physical rehabilitation unit. He was ultimately discharged with a neurogenic bladder and weak left leg.
The patient sued the EP for negligence in the failure to diagnose CO poisoning and prompt initiation of 100% O2 therapy. The EP argued that CO poisoning had been properly ruled out and that the diagnosis of CVA was correct. The defense also claimed that even if the patient had suffered CO poisoning, the length of the exposure would have led to the same outcome. A defense verdict was returned.
Discussion
Carbon monoxide poisoning is one of the leading causes of poisoning morbidity and mortality in the United States. This is in part due to the fact that CO is a colorless, odorless, and tasteless gas. The peak incidence for CO poisoning is in the fall and winter, when people are more likely to use space heaters, wood burning stoves, or portable generators inside without adequate ventilation.
The clinical presentation of CO poisoning can range from mild (eg, headache, flu-like symptoms) to devastating (eg, coma, death). The central nervous system is the organ system that is most sensitive to CO poisoning. Symptoms can range from a dull frontal headache, dizziness, and ataxia, to syncope, seizures, focal neurological deficit, and coma. In fact, the most serious complication of CO poisoning may be persistent or delayed neurological or neurocognitive sequelae, which can occur in up to 50% of patients with symptomatic acute poisoning.1 Unfortunately, COHb levels and symptoms do not always correlate well. In fact, particular COHb levels are not predictive of symptoms or outcome.1
The treatment for CO poisoning consists of administering 100% O2 as soon as the diagnosis is considered. If 100% O2 is administered, the half-life of COHb can be reduced from 5 hours (room air) to approximately 1 hour.1 While some argue that treatment with hyperbaric O2 (HBO) therapy should be considered standard of care, it has not yet been determined which patient population benefits from HBO therapy; moreover, there is currently no established optimum timing of therapy. Regardless, the jury came to the correct decision in this case as it is impossible to determine, with any degree of medical certainty, if the patient’s neurological deficits were due to the natural course of an ischemic stroke, or if CO contributed to or was the sole cause of the CVA.
Death in the Emergency Department
A 43-year-old man presented to the ED with the chief complaint of a lower lip laceration. The patient stated he had gotten into an altercation with his girlfriend just prior to arrival. She had punched the patient in the face with her fist, resulting in the lip laceration. The patient denied any loss of consciousness or other pain. He did, however, smell of alcohol and was emotionally labile, crying one moment and yelling the next.
The patient was instructed to remove all of his clothes, change into a hospital gown and give all of his belongings to hospital security. He removed his clothes, but refused to turn them over to security. This prompted a physical altercation between the patient and hospital security. Three hospital security guards wrestled the patient to the ground and placed him face down; one guard placed the patient in a choke hold while the other two guards sat on top of him. Within a few moments, the patient became unresponsive. He was placed immediately on a stretcher and intubated by the EP. After successful intubation and bagging with 100% O2, the patient regained a palpable pulse, but remained unresponsive.
The patient was admitted to the intensive care unit, but never regained consciousness and died 5 days later. The cause of death was thought to be anoxic brain injury due to asphyxiation. The family of the patient sued the hospital and the EP for causing asphyxiation and death in this patient seeking medical care. The hospital denied responsibility for the death because the patient both instigated the altercation and had a preexisting heart condition. According to published reports, a $2.5 million settlement was reached.
Discussion
This unfortunate case did not involve the EP; all of the important events transpired prior to the EP’s initial interaction with the patient. There are not enough details to explain how this situation escalated so rapidly, or why hospital security felt this was the best way to subdue the patient.
Unfortunately, EPs are no strangers to agitated patients. Behavioral emergencies account for approximately 5% of all ED visits, and these usually involve some form of violence or agitation.1 Every physician and nurse working in the ED must be prepared to deal with patients who have the potential to become violent. Clearly, training of all patient-care personnel to handle such patients in the ED is important to ensuring both staff and patient safety. Having the patient undress and change into a hospital gown is the correct first step. This allows for removal of real or potential weapons, and makes it much less likely for the patient to leave before his or her evaluation and management is complete. Doing this properly, however, is key. Providing the patient with a warm blanket or food, or just talking to him or her in a calm and reassuring voice, can often prevent escalation. Simply arguing with the patient rarely works, and often has the opposite desired effect.
If the situation continues to escalate, and it appears either physical or chemical restraint will be necessary, a “show of force” should be made. A restraint team consisting of at least five trained members should be assembled, with the EP acting as the team leader. The team should all enter the room at the same time, explain what will happen, and then move quickly.1 The leader should move to the head of the bed and direct the team, while the remaining four members each take a limb. To preserve the physician-patient relationship, it is best if the EP is not actively involved in placing the physical restraints.
The choke hold should only be considered as a method of last resort. Many police departments in the country prohibit use of the choke hold because of complications such as those observed in this case. The use of choke holds became a topic of intense debate this summer with the death of Eric Garner in Staten Island, New York; it was thought that his pre-existing conditions of obesity, asthma, and heart disease were all aggravated by the choke hold. Although obese patients are often at a higher risk for complications due to pre-existing issues with adequate oxygenation, it is unclear whether the patient in this case was obese.
An alternative strategy in handling an agitated patient would be the use of a taser by trained security personnel. In one study, 99.75% of tasered patients had no significant injury as a result of the device.2 In 2009, the American Medical Association found that tasers, “when used appropriately, can save lives during interventions that would have otherwise involved the use of deadly force.” While the safety of patients and the ED staff (nurses, physicians, and technicians) is paramount, the clinician should always adhere to the principle of “primum non nocere”—“first, do no harm.”
Reference - Carbon Monoxide Poisoning
- Tomaszewski C: Carbon monoxide. In: Nelson LS, Lewin NA, Howland MA, Hoffman RS, Goldfrank LR, Flomenbaum NE, eds. Goldfrank’s Toxicologic Emergencies. 9th ed. New York, NY: McGraw Hill; 2011:1658.
Reference - Death in the Emergency Department
- Rossi J, Swan MC, Issacs ED. The violent or agitated patient. Emerg Med Clin North Am. 2010;28(1):235-256.
- Bozeman WP, Hauda WE 2nd, Heck JJ, Graham DD Jr, Martin BP, Winslow JE. Safety and injury profile of conducted electrical weapons used by law enforcement officers against criminal suspects. Ann Emerg Med. 2009;53(4):480-489.
Reference - Carbon Monoxide Poisoning
- Tomaszewski C: Carbon monoxide. In: Nelson LS, Lewin NA, Howland MA, Hoffman RS, Goldfrank LR, Flomenbaum NE, eds. Goldfrank’s Toxicologic Emergencies. 9th ed. New York, NY: McGraw Hill; 2011:1658.
Reference - Death in the Emergency Department
- Rossi J, Swan MC, Issacs ED. The violent or agitated patient. Emerg Med Clin North Am. 2010;28(1):235-256.
- Bozeman WP, Hauda WE 2nd, Heck JJ, Graham DD Jr, Martin BP, Winslow JE. Safety and injury profile of conducted electrical weapons used by law enforcement officers against criminal suspects. Ann Emerg Med. 2009;53(4):480-489.
Malpractice Counsel
Traumatic Back Pain
An 84-year-old man with low-back pain following a motor vehicle crash was brought to the ED by emergency medical services (EMS). He had been the restrained driver, stopped at a traffic light, when he was struck from behind by a second vehicle.
In the ED, the patient only complained of low-back pain. He denied any radiation of pain or lower-extremity numbness or weakness. He also denied any head injury, loss of consciousness, neck pain, or abdominal pain. His past medical history was significant for hypertension, arthritis, and coronary artery disease.
On physical examination, the patient’s vital signs were normal. The head, eyes, ears, nose, and throat (HEENT) examination was also normal; specifically, there was no tenderness to palpation of the cervical spine in the posterior midline. Regarding the cardiopulmonary examination, auscultation of the lungs revealed clear, bilateral breath sounds; the heart examination was normal. The patient had a soft abdomen, without tenderness, guarding, or rebound. His pelvis was stable, but he did exhibit some tenderness on palpation of the lower-thoracic and upper-lumbar spine. The neurological examination revealed normal motor strength and sensation in the lower extremities.
The emergency physician (EP) ordered X-rays of the thoracic and lumbar spine and a urinalysis. The films were interpreted by both the EP and radiologist as normal; the results of the urinalysis were also normal. The patient was diagnosed with a lower back strain secondary to the motor vehicle crash and was discharged home with an analgesic.
The next day, however, the patient began to complain of increased back pain and lower-extremity numbness and weakness. He was brought back to the same hospital ED where he was noted to have severe weakness of both lower extremities and decreased sensation to touch. Additional imaging was performed, which demonstrated a fracture of T11 with spinal cord impingement. He was taken to surgery, but unfortunately the injury was permanent, and the patient was left with lower-extremity paralysis and bowel and bladder incontinence.
The plaintiff sued the EP and the radiologist for not properly interpreting the initial X-rays. The defendants denied liability, asserting the patient’s injury was a result of the collision and that nothing could have prevented it. According to a published account, the jury returned a verdict finding the EP to be 40% at fault and the radiologist 60% at fault.
Discussion
Emergency physicians frequently manage patients experiencing pain or injury following a motor vehicle crash. If the patient is complaining of neck or back pain, the prehospital providers will immobilize the patient with a rigid cervical collar (ie, if neck pain is present) and a long backboard if pain anywhere along the spine is present (ie, cervical, thoracic, or lumbar).
When the initial airway, breathing, circulation, and disability assessment for the trauma patient is performed and found to be normal, a secondary examination should be performed. Trauma patients with back pain should be log-rolled onto their side, with spinal immobilization followed by visual inspection and palpation/percussion of the midline of the thoracic and lumbar spine. The presence of midline tenderness suggests an acute injury and the need to keep the patient immobilized. Patients should be removed off the backboard and onto the gurney mattress while immobilizing the spine. The standard hospital mattress provides acceptable spinal support.1
Historically, plain radiographs of the thoracic and lumbar spine have been the imaging test of choice in the initial evaluation of suspected traumatic spinal column injury. However, similar to cervical spine trauma, computed tomography (CT) is assuming a larger role in the evaluation of patients with suspected thoracic or lumbar spine injury. When thoracic and abdominal CT scans are performed to evaluate for possible chest or abdominal trauma, those images can be reformatted and used to reconstruct images of the thoracic and lumbar spine, significantly reducing radiation exposure.1 While CT is the gold standard imaging study for evaluation of bony or ligamentous injury of the spine, magnetic resonance imaging (MRI) is the study of choice for patients with neurological deficits or suspected spinal cord injury.
This patient had a completely normal neurological examination at initial presentation, so there was no indication for an MRI. The bony injury to T11 must have been very subtle for both the EP and the radiologist to have missed it. Unfortunately, the jury appears to have used the standard of “perfection,” rather than the “reasonable and prudent physician” in judging that the injury should have been detected. This case serves as a reminder that EPs cannot rely on consulting specialists to consistently and reliably provide accurate information. Moreover, this case emphasizes the need to consider CT imaging of the spine in the evaluation of patients with severe back pain of traumatic origin when plain radiographs appear normal.
Hip-Reduction Problem
A 79-year-old man with left hip pain presented to the ED via EMS. The patient stated that when he had bent over to retrieve his dropped glasses, he experienced the immediate onset of left hip pain and fell to the floor. He was unable to get up on his own and called EMS. The patient had undergone total left hip replacement 1 month prior. At presentation, he complained only of severe pain in his left hip; he denied head injury, neck pain or stiffness, chest pain, or abdominal pain. His past medical history was significant for hypertension and type 2 diabetes mellitus. The patient had no known drug allergies.
On physical examination, he was mildly tachycardic. His vital signs were: heart rate, 102 beats/minute; blood pressure, 156/88 mm Hg; respiratory rate, 20 breaths/minutes; and temperature, afebrile. His pulse oximetry was 98% on room air. The HEENT, lung, heart, and abdominal examinations were all normal. Standing at the foot of the bed, the patient had obvious shortening, internal rotation, and adduction of the left leg. The left knee was without tenderness or swelling. The neurovascular examination of the left lower extremity was completely normal.
Plain radiographs of the pelvis and left hip ordered by the EP demonstrated a posterior hip dislocation with intact hardware. The EP consulted the patient’s orthopedic physician, and both agreed the EP should attempt to reduce the dislocation in the ED. Using conscious sedation, the EP was able to reduce the dislocation, but postreduction films demonstrated a new fracture requiring orthopedic surgery. Unfortunately, the patient had a very difficult recovery, ultimately resulting in death.
The patient’s estate sued the EP, stating he should have had the orthopedic physician reduce the dislocation. The defense argued that fracture is a known complication of reduction of a dislocated hip. A defense verdict was returned.
Discussion
Approximately 85% to 90% of hip dislocations are posterior; the remaining 10% are anterior. Posterior hip dislocations are a common complication following total hip-replacement surgery.1 Hip dislocation is a true orthopedic and time-dependent emergency. The longer the hip remains dislocated, the more likely complications are to occur, including osteonecrosis of the femoral head, arthritic degeneration of the hip joint, and long-term neurological sequelae.2 The treatment of posterior hip dislocation (without fracture) is closed reduction as quickly as possible, and preferably within 6 hours.3 As this case demonstrates, minimal forces can result in a hip dislocation following a total hip replacement. In healthy patients, however, significant forces (eg, high-speed motor vehicle crashes) are required to cause posterior hip dislocation.
Patients with a posterior hip dislocation will present in severe pain and an inability to ambulate. In most cases of posterior hip dislocation, the affected lower extremity will be visibly shortened, internally rotated, and adducted. The knee should always be examined for injury, as well as performance of a thorough neurovascular examination of the affected extremity.
Plain X-ray films will usually identify a posterior hip dislocation. On an anteroposterior pelvis X-ray, the femoral head will be seen outside and just superior to the acetabulum. Special attention should be made to the acetabulum to ensure a concomitant acetabular fracture is not missed.
Indications for closed reduction of a posterior hip dislocation include dislocation with or without neurological deficit and no associated fracture, or dislocation with an associated fracture if no neurological deficits are present.2 An open traumatic hip dislocation should only be reduced in the operating room.
It is certainly within the purview of the EP to attempt a closed reduction for a posterior hip dislocation if no contraindications exist. The patient will need to be sedated (ie, procedural sedation, conscious sedation, or moderate sedation) for any chance of success at reduction. While it is beyond the scope of this article to review the various techniques used to reduce a posterior hip dislocation, one of the guiding principles is that after two or three unsuccessful attempts by the EP to reduce the dislocation, no further attempts should be made and orthopedic surgery services should be consulted. This is because the risk of complications increases as the number of failed attempts increase.
It is unclear how many attempts the EP made in this case. Fracture is a known complication when attempting reduction for a hip dislocation, be it an orthopedic surgeon or an EP. It was certainly appropriate for the EP in this case to attempt closed reduction, given the importance of timely reduction.
Reference (Traumatic Back Pain)
- Baron BJ, McSherry KJ, Larson JL, Scalea TM. Spinal and spinal cord trauma In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD, eds. Tintinalli’s Emergency Medicine—A Comprehensive Study Guide. 7th ed. New York: NY: McGraw Hill Medical; 2011:1709-1730.
(Hip-Reduction Problem)
- Dela Cruz JE, Sullivan DN, Varboncouer E, et al. Comparison of proceduralsedation for the reduction of dislocated total hip arthroplasty.West J Emerg Med. 2014:15(1):76-80.
- Davenport M. Joint reduction, hip dislocation, posterior. Medscape Web site. eMedicine.medscape.com/article/109225. Updated February 11, 2014. Accessed January 27, 2015.
- Steele MT, Stubbs AM. Hip and femur injuries. In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD, eds. Tintinalli’s Emergency Medicine—A Comprehensive Study Guide. 7th ed. New York: NY: McGraw Hill Medical; 2011:1848-1856.
Traumatic Back Pain
An 84-year-old man with low-back pain following a motor vehicle crash was brought to the ED by emergency medical services (EMS). He had been the restrained driver, stopped at a traffic light, when he was struck from behind by a second vehicle.
In the ED, the patient only complained of low-back pain. He denied any radiation of pain or lower-extremity numbness or weakness. He also denied any head injury, loss of consciousness, neck pain, or abdominal pain. His past medical history was significant for hypertension, arthritis, and coronary artery disease.
On physical examination, the patient’s vital signs were normal. The head, eyes, ears, nose, and throat (HEENT) examination was also normal; specifically, there was no tenderness to palpation of the cervical spine in the posterior midline. Regarding the cardiopulmonary examination, auscultation of the lungs revealed clear, bilateral breath sounds; the heart examination was normal. The patient had a soft abdomen, without tenderness, guarding, or rebound. His pelvis was stable, but he did exhibit some tenderness on palpation of the lower-thoracic and upper-lumbar spine. The neurological examination revealed normal motor strength and sensation in the lower extremities.
The emergency physician (EP) ordered X-rays of the thoracic and lumbar spine and a urinalysis. The films were interpreted by both the EP and radiologist as normal; the results of the urinalysis were also normal. The patient was diagnosed with a lower back strain secondary to the motor vehicle crash and was discharged home with an analgesic.
The next day, however, the patient began to complain of increased back pain and lower-extremity numbness and weakness. He was brought back to the same hospital ED where he was noted to have severe weakness of both lower extremities and decreased sensation to touch. Additional imaging was performed, which demonstrated a fracture of T11 with spinal cord impingement. He was taken to surgery, but unfortunately the injury was permanent, and the patient was left with lower-extremity paralysis and bowel and bladder incontinence.
The plaintiff sued the EP and the radiologist for not properly interpreting the initial X-rays. The defendants denied liability, asserting the patient’s injury was a result of the collision and that nothing could have prevented it. According to a published account, the jury returned a verdict finding the EP to be 40% at fault and the radiologist 60% at fault.
Discussion
Emergency physicians frequently manage patients experiencing pain or injury following a motor vehicle crash. If the patient is complaining of neck or back pain, the prehospital providers will immobilize the patient with a rigid cervical collar (ie, if neck pain is present) and a long backboard if pain anywhere along the spine is present (ie, cervical, thoracic, or lumbar).
When the initial airway, breathing, circulation, and disability assessment for the trauma patient is performed and found to be normal, a secondary examination should be performed. Trauma patients with back pain should be log-rolled onto their side, with spinal immobilization followed by visual inspection and palpation/percussion of the midline of the thoracic and lumbar spine. The presence of midline tenderness suggests an acute injury and the need to keep the patient immobilized. Patients should be removed off the backboard and onto the gurney mattress while immobilizing the spine. The standard hospital mattress provides acceptable spinal support.1
Historically, plain radiographs of the thoracic and lumbar spine have been the imaging test of choice in the initial evaluation of suspected traumatic spinal column injury. However, similar to cervical spine trauma, computed tomography (CT) is assuming a larger role in the evaluation of patients with suspected thoracic or lumbar spine injury. When thoracic and abdominal CT scans are performed to evaluate for possible chest or abdominal trauma, those images can be reformatted and used to reconstruct images of the thoracic and lumbar spine, significantly reducing radiation exposure.1 While CT is the gold standard imaging study for evaluation of bony or ligamentous injury of the spine, magnetic resonance imaging (MRI) is the study of choice for patients with neurological deficits or suspected spinal cord injury.
This patient had a completely normal neurological examination at initial presentation, so there was no indication for an MRI. The bony injury to T11 must have been very subtle for both the EP and the radiologist to have missed it. Unfortunately, the jury appears to have used the standard of “perfection,” rather than the “reasonable and prudent physician” in judging that the injury should have been detected. This case serves as a reminder that EPs cannot rely on consulting specialists to consistently and reliably provide accurate information. Moreover, this case emphasizes the need to consider CT imaging of the spine in the evaluation of patients with severe back pain of traumatic origin when plain radiographs appear normal.
Hip-Reduction Problem
A 79-year-old man with left hip pain presented to the ED via EMS. The patient stated that when he had bent over to retrieve his dropped glasses, he experienced the immediate onset of left hip pain and fell to the floor. He was unable to get up on his own and called EMS. The patient had undergone total left hip replacement 1 month prior. At presentation, he complained only of severe pain in his left hip; he denied head injury, neck pain or stiffness, chest pain, or abdominal pain. His past medical history was significant for hypertension and type 2 diabetes mellitus. The patient had no known drug allergies.
On physical examination, he was mildly tachycardic. His vital signs were: heart rate, 102 beats/minute; blood pressure, 156/88 mm Hg; respiratory rate, 20 breaths/minutes; and temperature, afebrile. His pulse oximetry was 98% on room air. The HEENT, lung, heart, and abdominal examinations were all normal. Standing at the foot of the bed, the patient had obvious shortening, internal rotation, and adduction of the left leg. The left knee was without tenderness or swelling. The neurovascular examination of the left lower extremity was completely normal.
Plain radiographs of the pelvis and left hip ordered by the EP demonstrated a posterior hip dislocation with intact hardware. The EP consulted the patient’s orthopedic physician, and both agreed the EP should attempt to reduce the dislocation in the ED. Using conscious sedation, the EP was able to reduce the dislocation, but postreduction films demonstrated a new fracture requiring orthopedic surgery. Unfortunately, the patient had a very difficult recovery, ultimately resulting in death.
The patient’s estate sued the EP, stating he should have had the orthopedic physician reduce the dislocation. The defense argued that fracture is a known complication of reduction of a dislocated hip. A defense verdict was returned.
Discussion
Approximately 85% to 90% of hip dislocations are posterior; the remaining 10% are anterior. Posterior hip dislocations are a common complication following total hip-replacement surgery.1 Hip dislocation is a true orthopedic and time-dependent emergency. The longer the hip remains dislocated, the more likely complications are to occur, including osteonecrosis of the femoral head, arthritic degeneration of the hip joint, and long-term neurological sequelae.2 The treatment of posterior hip dislocation (without fracture) is closed reduction as quickly as possible, and preferably within 6 hours.3 As this case demonstrates, minimal forces can result in a hip dislocation following a total hip replacement. In healthy patients, however, significant forces (eg, high-speed motor vehicle crashes) are required to cause posterior hip dislocation.
Patients with a posterior hip dislocation will present in severe pain and an inability to ambulate. In most cases of posterior hip dislocation, the affected lower extremity will be visibly shortened, internally rotated, and adducted. The knee should always be examined for injury, as well as performance of a thorough neurovascular examination of the affected extremity.
Plain X-ray films will usually identify a posterior hip dislocation. On an anteroposterior pelvis X-ray, the femoral head will be seen outside and just superior to the acetabulum. Special attention should be made to the acetabulum to ensure a concomitant acetabular fracture is not missed.
Indications for closed reduction of a posterior hip dislocation include dislocation with or without neurological deficit and no associated fracture, or dislocation with an associated fracture if no neurological deficits are present.2 An open traumatic hip dislocation should only be reduced in the operating room.
It is certainly within the purview of the EP to attempt a closed reduction for a posterior hip dislocation if no contraindications exist. The patient will need to be sedated (ie, procedural sedation, conscious sedation, or moderate sedation) for any chance of success at reduction. While it is beyond the scope of this article to review the various techniques used to reduce a posterior hip dislocation, one of the guiding principles is that after two or three unsuccessful attempts by the EP to reduce the dislocation, no further attempts should be made and orthopedic surgery services should be consulted. This is because the risk of complications increases as the number of failed attempts increase.
It is unclear how many attempts the EP made in this case. Fracture is a known complication when attempting reduction for a hip dislocation, be it an orthopedic surgeon or an EP. It was certainly appropriate for the EP in this case to attempt closed reduction, given the importance of timely reduction.
Traumatic Back Pain
An 84-year-old man with low-back pain following a motor vehicle crash was brought to the ED by emergency medical services (EMS). He had been the restrained driver, stopped at a traffic light, when he was struck from behind by a second vehicle.
In the ED, the patient only complained of low-back pain. He denied any radiation of pain or lower-extremity numbness or weakness. He also denied any head injury, loss of consciousness, neck pain, or abdominal pain. His past medical history was significant for hypertension, arthritis, and coronary artery disease.
On physical examination, the patient’s vital signs were normal. The head, eyes, ears, nose, and throat (HEENT) examination was also normal; specifically, there was no tenderness to palpation of the cervical spine in the posterior midline. Regarding the cardiopulmonary examination, auscultation of the lungs revealed clear, bilateral breath sounds; the heart examination was normal. The patient had a soft abdomen, without tenderness, guarding, or rebound. His pelvis was stable, but he did exhibit some tenderness on palpation of the lower-thoracic and upper-lumbar spine. The neurological examination revealed normal motor strength and sensation in the lower extremities.
The emergency physician (EP) ordered X-rays of the thoracic and lumbar spine and a urinalysis. The films were interpreted by both the EP and radiologist as normal; the results of the urinalysis were also normal. The patient was diagnosed with a lower back strain secondary to the motor vehicle crash and was discharged home with an analgesic.
The next day, however, the patient began to complain of increased back pain and lower-extremity numbness and weakness. He was brought back to the same hospital ED where he was noted to have severe weakness of both lower extremities and decreased sensation to touch. Additional imaging was performed, which demonstrated a fracture of T11 with spinal cord impingement. He was taken to surgery, but unfortunately the injury was permanent, and the patient was left with lower-extremity paralysis and bowel and bladder incontinence.
The plaintiff sued the EP and the radiologist for not properly interpreting the initial X-rays. The defendants denied liability, asserting the patient’s injury was a result of the collision and that nothing could have prevented it. According to a published account, the jury returned a verdict finding the EP to be 40% at fault and the radiologist 60% at fault.
Discussion
Emergency physicians frequently manage patients experiencing pain or injury following a motor vehicle crash. If the patient is complaining of neck or back pain, the prehospital providers will immobilize the patient with a rigid cervical collar (ie, if neck pain is present) and a long backboard if pain anywhere along the spine is present (ie, cervical, thoracic, or lumbar).
When the initial airway, breathing, circulation, and disability assessment for the trauma patient is performed and found to be normal, a secondary examination should be performed. Trauma patients with back pain should be log-rolled onto their side, with spinal immobilization followed by visual inspection and palpation/percussion of the midline of the thoracic and lumbar spine. The presence of midline tenderness suggests an acute injury and the need to keep the patient immobilized. Patients should be removed off the backboard and onto the gurney mattress while immobilizing the spine. The standard hospital mattress provides acceptable spinal support.1
Historically, plain radiographs of the thoracic and lumbar spine have been the imaging test of choice in the initial evaluation of suspected traumatic spinal column injury. However, similar to cervical spine trauma, computed tomography (CT) is assuming a larger role in the evaluation of patients with suspected thoracic or lumbar spine injury. When thoracic and abdominal CT scans are performed to evaluate for possible chest or abdominal trauma, those images can be reformatted and used to reconstruct images of the thoracic and lumbar spine, significantly reducing radiation exposure.1 While CT is the gold standard imaging study for evaluation of bony or ligamentous injury of the spine, magnetic resonance imaging (MRI) is the study of choice for patients with neurological deficits or suspected spinal cord injury.
This patient had a completely normal neurological examination at initial presentation, so there was no indication for an MRI. The bony injury to T11 must have been very subtle for both the EP and the radiologist to have missed it. Unfortunately, the jury appears to have used the standard of “perfection,” rather than the “reasonable and prudent physician” in judging that the injury should have been detected. This case serves as a reminder that EPs cannot rely on consulting specialists to consistently and reliably provide accurate information. Moreover, this case emphasizes the need to consider CT imaging of the spine in the evaluation of patients with severe back pain of traumatic origin when plain radiographs appear normal.
Hip-Reduction Problem
A 79-year-old man with left hip pain presented to the ED via EMS. The patient stated that when he had bent over to retrieve his dropped glasses, he experienced the immediate onset of left hip pain and fell to the floor. He was unable to get up on his own and called EMS. The patient had undergone total left hip replacement 1 month prior. At presentation, he complained only of severe pain in his left hip; he denied head injury, neck pain or stiffness, chest pain, or abdominal pain. His past medical history was significant for hypertension and type 2 diabetes mellitus. The patient had no known drug allergies.
On physical examination, he was mildly tachycardic. His vital signs were: heart rate, 102 beats/minute; blood pressure, 156/88 mm Hg; respiratory rate, 20 breaths/minutes; and temperature, afebrile. His pulse oximetry was 98% on room air. The HEENT, lung, heart, and abdominal examinations were all normal. Standing at the foot of the bed, the patient had obvious shortening, internal rotation, and adduction of the left leg. The left knee was without tenderness or swelling. The neurovascular examination of the left lower extremity was completely normal.
Plain radiographs of the pelvis and left hip ordered by the EP demonstrated a posterior hip dislocation with intact hardware. The EP consulted the patient’s orthopedic physician, and both agreed the EP should attempt to reduce the dislocation in the ED. Using conscious sedation, the EP was able to reduce the dislocation, but postreduction films demonstrated a new fracture requiring orthopedic surgery. Unfortunately, the patient had a very difficult recovery, ultimately resulting in death.
The patient’s estate sued the EP, stating he should have had the orthopedic physician reduce the dislocation. The defense argued that fracture is a known complication of reduction of a dislocated hip. A defense verdict was returned.
Discussion
Approximately 85% to 90% of hip dislocations are posterior; the remaining 10% are anterior. Posterior hip dislocations are a common complication following total hip-replacement surgery.1 Hip dislocation is a true orthopedic and time-dependent emergency. The longer the hip remains dislocated, the more likely complications are to occur, including osteonecrosis of the femoral head, arthritic degeneration of the hip joint, and long-term neurological sequelae.2 The treatment of posterior hip dislocation (without fracture) is closed reduction as quickly as possible, and preferably within 6 hours.3 As this case demonstrates, minimal forces can result in a hip dislocation following a total hip replacement. In healthy patients, however, significant forces (eg, high-speed motor vehicle crashes) are required to cause posterior hip dislocation.
Patients with a posterior hip dislocation will present in severe pain and an inability to ambulate. In most cases of posterior hip dislocation, the affected lower extremity will be visibly shortened, internally rotated, and adducted. The knee should always be examined for injury, as well as performance of a thorough neurovascular examination of the affected extremity.
Plain X-ray films will usually identify a posterior hip dislocation. On an anteroposterior pelvis X-ray, the femoral head will be seen outside and just superior to the acetabulum. Special attention should be made to the acetabulum to ensure a concomitant acetabular fracture is not missed.
Indications for closed reduction of a posterior hip dislocation include dislocation with or without neurological deficit and no associated fracture, or dislocation with an associated fracture if no neurological deficits are present.2 An open traumatic hip dislocation should only be reduced in the operating room.
It is certainly within the purview of the EP to attempt a closed reduction for a posterior hip dislocation if no contraindications exist. The patient will need to be sedated (ie, procedural sedation, conscious sedation, or moderate sedation) for any chance of success at reduction. While it is beyond the scope of this article to review the various techniques used to reduce a posterior hip dislocation, one of the guiding principles is that after two or three unsuccessful attempts by the EP to reduce the dislocation, no further attempts should be made and orthopedic surgery services should be consulted. This is because the risk of complications increases as the number of failed attempts increase.
It is unclear how many attempts the EP made in this case. Fracture is a known complication when attempting reduction for a hip dislocation, be it an orthopedic surgeon or an EP. It was certainly appropriate for the EP in this case to attempt closed reduction, given the importance of timely reduction.
Reference (Traumatic Back Pain)
- Baron BJ, McSherry KJ, Larson JL, Scalea TM. Spinal and spinal cord trauma In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD, eds. Tintinalli’s Emergency Medicine—A Comprehensive Study Guide. 7th ed. New York: NY: McGraw Hill Medical; 2011:1709-1730.
(Hip-Reduction Problem)
- Dela Cruz JE, Sullivan DN, Varboncouer E, et al. Comparison of proceduralsedation for the reduction of dislocated total hip arthroplasty.West J Emerg Med. 2014:15(1):76-80.
- Davenport M. Joint reduction, hip dislocation, posterior. Medscape Web site. eMedicine.medscape.com/article/109225. Updated February 11, 2014. Accessed January 27, 2015.
- Steele MT, Stubbs AM. Hip and femur injuries. In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD, eds. Tintinalli’s Emergency Medicine—A Comprehensive Study Guide. 7th ed. New York: NY: McGraw Hill Medical; 2011:1848-1856.
Reference (Traumatic Back Pain)
- Baron BJ, McSherry KJ, Larson JL, Scalea TM. Spinal and spinal cord trauma In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD, eds. Tintinalli’s Emergency Medicine—A Comprehensive Study Guide. 7th ed. New York: NY: McGraw Hill Medical; 2011:1709-1730.
(Hip-Reduction Problem)
- Dela Cruz JE, Sullivan DN, Varboncouer E, et al. Comparison of proceduralsedation for the reduction of dislocated total hip arthroplasty.West J Emerg Med. 2014:15(1):76-80.
- Davenport M. Joint reduction, hip dislocation, posterior. Medscape Web site. eMedicine.medscape.com/article/109225. Updated February 11, 2014. Accessed January 27, 2015.
- Steele MT, Stubbs AM. Hip and femur injuries. In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD, eds. Tintinalli’s Emergency Medicine—A Comprehensive Study Guide. 7th ed. New York: NY: McGraw Hill Medical; 2011:1848-1856.
Malpractice Counsel
Stroke in a Young Man
A 26-year-old man presented to the ED with the chief complaint of mild right-sided weakness, paresthesias, and slurred speech. He stated the onset was sudden—approximately 30 minutes prior to arrival to the ED. The patient denied any previous similar symptoms and was otherwise in good health; he denied taking any medications. He drank alcohol socially, but denied smoking or illicit drug use.
On physical examination, his vital signs and oxygen saturation were normal. Pulmonary, cardiovascular, and abdominal examinations were also normal. The patient thought his speech was somewhat slurred, but the triage nurse and treating emergency physician (EP) had difficulty detecting any altered speech. He was noted to have mild (4+/5) right upper and lower extremity weakness; no facial droop was detected. The patient did have a mild pronator drift of the right upper extremity. Gait testing revealed a mild limp of the right lower extremity.
The EP consulted the hospitalist, and the patient was admitted to a monitored bed. The following morning, a brain magnetic resonance image revealed an ischemic stroke in the distribution of the left middle cerebral artery. The patient’s hospital course was uncomplicated, but at the time of discharge, he continued to have mild right-sided weakness and required the use of a cane.
The patient sued the hospital and the EP for negligence in failing to treat his condition in a timely manner and for not consulting a neurologist. The plaintiff’s attorneys argued the patient should have been given tissue plasminogen activator (tPA), which would have avoided the residual right-sided weakness. The defense denied negligence and argued the patient’s symptoms could have been due to several things for which tPA would have been an inappropriate treatment. A defense verdict was returned.
Discussion
Stroke in young patients is relatively rare. With “young” defined as aged 18 to 45 years, this population accounts for approximately 2% to 12% of cerebral infarcts.1 In one nationwide US study of stroke in young adults, Ellis2 found that 4.9% of individuals experiencing a stroke in 2007 were between ages 18 and 44 years. Among this group, 78% experienced an ischemic stroke; 11.2% experienced a subarachnoid hemorrhage (SAH); and 10.8% had an intracerebral hemorrhage.2
While the clinical presentation of stroke in young adults is similar to that of older patients, the etiologies and risk factors are very different. In older patients, atherosclerosis is the major cause of ischemic stroke. In studies of young adults with ischemic stroke, cardioembolism was found to be the leading cause. Under this category, a patent foramen ovale (PFO) was considered a common cause, followed by atrial fibrillation, bacterial endocarditis, rheumatic heart disease, and atrial myxoma. There is, however, increasing controversy over the role of PFO as an etiology of stroke. Many investigators think its role has been overstated and is probably more of an incidental finding than a causal relationship.3 Patients with a suspected cardioembolic etiology will usually require an echocardiogram (with saline contrast or a “bubble study” for suspected PFO), cardiac monitoring, and a possible Holter monitor at the time of discharge (to detect paroxysmal arrhythmias).
Following cardioembolic etiologies, arterial dissection is the next most common category.4 In one study of patients aged 31 to 45 years old, arterial dissection was the most common cause of ischemic stroke.4 Clinical features suggesting dissection include a history of head or neck trauma (even minor trauma), headache or neck pain, and local neurological findings (eg, cranial nerve palsy or Horner syndrome).3 Unfortunately, only about 25% of patients volunteer a history of recent neck trauma. If a cervical or vertebral artery dissection is suspected, contrast enhanced magnetic resonance angiography (MRA) is the most sensitive and specific test, followed by carotid ultrasound and CT angiography.3
Traditional risk factors for stroke include hypertension and diabetes mellitus (DM). This is not true for younger adults that experience an ischemic stroke. Cigarette smoking is a very important risk factor for cerebrovascular accident in young adults; in addition, the more one smokes, the greater the risk. Other risk factors in young adults include history of migraine headaches (especially migraine with aura), pregnancy and the postpartum period, and illicit drug use.3
The defense’s argument that there are many causes of stroke in young adults that would be inappropriate for treatment with tPA, such as a PFO, carotid dissection or bacterial endocarditis, is absolutely true. Young patients need to be aggressively worked up for the etiology of their stroke, and may require additional testing, such as an MRA, echocardiogram, or Holter monitoring to determine the underlying cause of their stroke.
Obstruction Following Gastric Bypass Surgery
A 47-year-old woman presented to the ED complaining of severe back and abdominal pain. Onset had been gradual and began approximately 4 hours prior to arrival. She described the pain as crampy and constant. The patient had vomited twice; she denied diarrhea and had a normal bowel movement the previous day. She denied any vaginal or urinary complaints. Her past medical history was significant for hypertension and status post gastric bypass surgery 6 months prior. She had lost 42 pounds to date. She denied smoking or alcohol use.
The patient’s vital signs on physical examination were: blood pressure, 154/92 mm Hg; pulse, 106 beats/minute; respiratory rate, 18 breaths/minute; and temperature, 99˚F. Oxygen saturation was 96% on room air. The patient’s lungs were clear to auscultation bilaterally. The heart was mildly tachycardic, with a regular rhythm and without murmurs, rubs, or gallops. The abdominal examination revealed diffuse tenderness and involuntary guarding. There was no distention or rebound. Bowel sounds were present but hypoactive. Examination of the back revealed bilateral paraspinal muscle tenderness without costovertebral angle tenderness.
The EP ordered a CBC, BMP, serum lipase, and a urinalysis. The patient was given an intravenous (IV) bolus of 250 cc normal saline in addition to IV morphine 4 mg and IV ondansetron 4 mg. Her white blood cell (WBC) count was slightly elevated at 12.2 g/dL, with a normal differential. The remainder of the laboratory studies were normal, except for a serum bicarbonate of 22 mmol/L.
The patient stated she felt somewhat improved, but continued to have abdominal and back pain. The EP admitted her to the hospital for observation and pain control. She died the following day from a bowel obstruction. The family sued the EP for negligence in failing to order appropriate testing and for not consulting with specialists to diagnose the bowel obstruction, which is a known complication of gastric bypass surgery. The jury returned a verdict of $2.4 million against the EP.
Discussion
The frequency of bariatric surgery in the United States continues to increase, primarily due to its success with regard to weight loss, but also because of its demonstrated improvement in hypertension, obstructive sleep apnea, hyperlipidemia, and type 2 DM.1
Frequently, the term “gastric bypass surgery” is used interchangeably with bariatric surgery. However, the EP must realize these terms encompass multiple different operations. The four most common types of bariatric surgery in the United Stated are (1) adjustable gastric banding (AGB); (2) the Roux-en-Y gastric bypass (RYGB); (3) biliopancreatic diversion with duodenal switch (BPD-DS); and (4) vertical sleeve gastrectomy (VSG).2 (See the Table for a brief explanation of each type of procedure.)
Since each procedure has its own respective associated complications, it is important for the EP to know which the type of gastric bypass surgery the patient had. For example, leakage is much more frequent following RYGB than in gastric banding, while slippage and obstruction are the most common complications of gastric banding.3,4 It is also very helpful to know the specific type of procedure when discussing the case with the surgical consultant.
Based on a recent review of over 800,000 bariatric surgery patients, seven serious common complications following the surgery were identified.3 These included bleeding, leakage, obstruction, stomal ulceration, pulmonary embolism and respiratory complications, blood sugar disturbances (usually hypoglycemia and/or metabolic acidosis), and nutritional disturbances. While not all-inclusive, this list represents the most common serious complications of gastric bypass surgery.
The complaint of abdominal pain in a patient that has undergone bariatric surgery should be taken very seriously. In addition to determining the specific procedure performed and date, the patient should be questioned about vomiting, bowel movements, and the presence of blood in stool or vomit. Depending upon the degree of pain present, the patient may need to be given IV opioid analgesia to facilitate a thorough abdominal examination. A rectal examination should be performed to identify occult gastrointestinal bleeding.
These patients require laboratory testing, including CBC, BMP, and other laboratory evaluation as indicated by the history and physical examination. Early consultation with the bariatric surgeon is recommended. Many, if not most, patients with abdominal pain and vomiting will require imaging, usually a CT scan with contrast of the abdomen and pelvis. Because of the difficulty in interpreting the CT scan results in these patients, the bariatric surgeon will often want to personally review the films rather than rely solely on the interpretation by radiology services.
Unfortunately, the EP in this case did not appreciate the seriousness of the situation. The presence of severe abdominal pain, tenderness, guarding, mild tachycardia with leukocytosis, and metabolic acidosis all pointed to a more serious etiology than muscle spasm. This patient required IV fluids, analgesia, and imaging, as well as consultation with the bariatric surgeon.
- Chatzikonstantinou A, Wolf ME, Hennerici MG. Ischemic stroke in young adults: classification and risk factors. J Neurol. 2012;259(4):653-659.
- Ellis C. Stroke in young adults. Disabil Health J. 2010;3(3):222-224.
- Ferro JM, Massaro AR, Mas JL. Aetiological diagnosis of ischemic stroke in young adults. Lancet Neurol. 2010;9(11):1085-1096.
- Chan MT, Nadareishvili ZG, Norris JW; Canadian Stroke Consortium. Diagnostic strategies in young patients with ischemic stroke in Canada. Can J Neurol Sci. 2000;27(2):120-124.
- Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292(14):1724-1737.
- Livingston EH. Patient guide: Endocrine and nutritional management after bariatric surgery: A patient’s guide. Hormone Health Network Web site. http://www.hormone.org/~/media/Hormone/Files/Patient%20Guides/Mens%20Health/PGBariatricSurgery_2014.pdf. Accessed December 17, 2014.
- Hussain A, El-Hasani S. Bariatric emergencies: current evidence and strategies of management. World J Emerg Surg. 2013;8(1):58.
- Campanille FC, Boru C, Rizzello M, et al. Acute complications after laparoscopic bariatric procedures: update for the general surgeon. Langenbecks Arch Surg. 2013;398(5):669-686
Stroke in a Young Man
A 26-year-old man presented to the ED with the chief complaint of mild right-sided weakness, paresthesias, and slurred speech. He stated the onset was sudden—approximately 30 minutes prior to arrival to the ED. The patient denied any previous similar symptoms and was otherwise in good health; he denied taking any medications. He drank alcohol socially, but denied smoking or illicit drug use.
On physical examination, his vital signs and oxygen saturation were normal. Pulmonary, cardiovascular, and abdominal examinations were also normal. The patient thought his speech was somewhat slurred, but the triage nurse and treating emergency physician (EP) had difficulty detecting any altered speech. He was noted to have mild (4+/5) right upper and lower extremity weakness; no facial droop was detected. The patient did have a mild pronator drift of the right upper extremity. Gait testing revealed a mild limp of the right lower extremity.
The EP consulted the hospitalist, and the patient was admitted to a monitored bed. The following morning, a brain magnetic resonance image revealed an ischemic stroke in the distribution of the left middle cerebral artery. The patient’s hospital course was uncomplicated, but at the time of discharge, he continued to have mild right-sided weakness and required the use of a cane.
The patient sued the hospital and the EP for negligence in failing to treat his condition in a timely manner and for not consulting a neurologist. The plaintiff’s attorneys argued the patient should have been given tissue plasminogen activator (tPA), which would have avoided the residual right-sided weakness. The defense denied negligence and argued the patient’s symptoms could have been due to several things for which tPA would have been an inappropriate treatment. A defense verdict was returned.
Discussion
Stroke in young patients is relatively rare. With “young” defined as aged 18 to 45 years, this population accounts for approximately 2% to 12% of cerebral infarcts.1 In one nationwide US study of stroke in young adults, Ellis2 found that 4.9% of individuals experiencing a stroke in 2007 were between ages 18 and 44 years. Among this group, 78% experienced an ischemic stroke; 11.2% experienced a subarachnoid hemorrhage (SAH); and 10.8% had an intracerebral hemorrhage.2
While the clinical presentation of stroke in young adults is similar to that of older patients, the etiologies and risk factors are very different. In older patients, atherosclerosis is the major cause of ischemic stroke. In studies of young adults with ischemic stroke, cardioembolism was found to be the leading cause. Under this category, a patent foramen ovale (PFO) was considered a common cause, followed by atrial fibrillation, bacterial endocarditis, rheumatic heart disease, and atrial myxoma. There is, however, increasing controversy over the role of PFO as an etiology of stroke. Many investigators think its role has been overstated and is probably more of an incidental finding than a causal relationship.3 Patients with a suspected cardioembolic etiology will usually require an echocardiogram (with saline contrast or a “bubble study” for suspected PFO), cardiac monitoring, and a possible Holter monitor at the time of discharge (to detect paroxysmal arrhythmias).
Following cardioembolic etiologies, arterial dissection is the next most common category.4 In one study of patients aged 31 to 45 years old, arterial dissection was the most common cause of ischemic stroke.4 Clinical features suggesting dissection include a history of head or neck trauma (even minor trauma), headache or neck pain, and local neurological findings (eg, cranial nerve palsy or Horner syndrome).3 Unfortunately, only about 25% of patients volunteer a history of recent neck trauma. If a cervical or vertebral artery dissection is suspected, contrast enhanced magnetic resonance angiography (MRA) is the most sensitive and specific test, followed by carotid ultrasound and CT angiography.3
Traditional risk factors for stroke include hypertension and diabetes mellitus (DM). This is not true for younger adults that experience an ischemic stroke. Cigarette smoking is a very important risk factor for cerebrovascular accident in young adults; in addition, the more one smokes, the greater the risk. Other risk factors in young adults include history of migraine headaches (especially migraine with aura), pregnancy and the postpartum period, and illicit drug use.3
The defense’s argument that there are many causes of stroke in young adults that would be inappropriate for treatment with tPA, such as a PFO, carotid dissection or bacterial endocarditis, is absolutely true. Young patients need to be aggressively worked up for the etiology of their stroke, and may require additional testing, such as an MRA, echocardiogram, or Holter monitoring to determine the underlying cause of their stroke.
Obstruction Following Gastric Bypass Surgery
A 47-year-old woman presented to the ED complaining of severe back and abdominal pain. Onset had been gradual and began approximately 4 hours prior to arrival. She described the pain as crampy and constant. The patient had vomited twice; she denied diarrhea and had a normal bowel movement the previous day. She denied any vaginal or urinary complaints. Her past medical history was significant for hypertension and status post gastric bypass surgery 6 months prior. She had lost 42 pounds to date. She denied smoking or alcohol use.
The patient’s vital signs on physical examination were: blood pressure, 154/92 mm Hg; pulse, 106 beats/minute; respiratory rate, 18 breaths/minute; and temperature, 99˚F. Oxygen saturation was 96% on room air. The patient’s lungs were clear to auscultation bilaterally. The heart was mildly tachycardic, with a regular rhythm and without murmurs, rubs, or gallops. The abdominal examination revealed diffuse tenderness and involuntary guarding. There was no distention or rebound. Bowel sounds were present but hypoactive. Examination of the back revealed bilateral paraspinal muscle tenderness without costovertebral angle tenderness.
The EP ordered a CBC, BMP, serum lipase, and a urinalysis. The patient was given an intravenous (IV) bolus of 250 cc normal saline in addition to IV morphine 4 mg and IV ondansetron 4 mg. Her white blood cell (WBC) count was slightly elevated at 12.2 g/dL, with a normal differential. The remainder of the laboratory studies were normal, except for a serum bicarbonate of 22 mmol/L.
The patient stated she felt somewhat improved, but continued to have abdominal and back pain. The EP admitted her to the hospital for observation and pain control. She died the following day from a bowel obstruction. The family sued the EP for negligence in failing to order appropriate testing and for not consulting with specialists to diagnose the bowel obstruction, which is a known complication of gastric bypass surgery. The jury returned a verdict of $2.4 million against the EP.
Discussion
The frequency of bariatric surgery in the United States continues to increase, primarily due to its success with regard to weight loss, but also because of its demonstrated improvement in hypertension, obstructive sleep apnea, hyperlipidemia, and type 2 DM.1
Frequently, the term “gastric bypass surgery” is used interchangeably with bariatric surgery. However, the EP must realize these terms encompass multiple different operations. The four most common types of bariatric surgery in the United Stated are (1) adjustable gastric banding (AGB); (2) the Roux-en-Y gastric bypass (RYGB); (3) biliopancreatic diversion with duodenal switch (BPD-DS); and (4) vertical sleeve gastrectomy (VSG).2 (See the Table for a brief explanation of each type of procedure.)
Since each procedure has its own respective associated complications, it is important for the EP to know which the type of gastric bypass surgery the patient had. For example, leakage is much more frequent following RYGB than in gastric banding, while slippage and obstruction are the most common complications of gastric banding.3,4 It is also very helpful to know the specific type of procedure when discussing the case with the surgical consultant.
Based on a recent review of over 800,000 bariatric surgery patients, seven serious common complications following the surgery were identified.3 These included bleeding, leakage, obstruction, stomal ulceration, pulmonary embolism and respiratory complications, blood sugar disturbances (usually hypoglycemia and/or metabolic acidosis), and nutritional disturbances. While not all-inclusive, this list represents the most common serious complications of gastric bypass surgery.
The complaint of abdominal pain in a patient that has undergone bariatric surgery should be taken very seriously. In addition to determining the specific procedure performed and date, the patient should be questioned about vomiting, bowel movements, and the presence of blood in stool or vomit. Depending upon the degree of pain present, the patient may need to be given IV opioid analgesia to facilitate a thorough abdominal examination. A rectal examination should be performed to identify occult gastrointestinal bleeding.
These patients require laboratory testing, including CBC, BMP, and other laboratory evaluation as indicated by the history and physical examination. Early consultation with the bariatric surgeon is recommended. Many, if not most, patients with abdominal pain and vomiting will require imaging, usually a CT scan with contrast of the abdomen and pelvis. Because of the difficulty in interpreting the CT scan results in these patients, the bariatric surgeon will often want to personally review the films rather than rely solely on the interpretation by radiology services.
Unfortunately, the EP in this case did not appreciate the seriousness of the situation. The presence of severe abdominal pain, tenderness, guarding, mild tachycardia with leukocytosis, and metabolic acidosis all pointed to a more serious etiology than muscle spasm. This patient required IV fluids, analgesia, and imaging, as well as consultation with the bariatric surgeon.
Stroke in a Young Man
A 26-year-old man presented to the ED with the chief complaint of mild right-sided weakness, paresthesias, and slurred speech. He stated the onset was sudden—approximately 30 minutes prior to arrival to the ED. The patient denied any previous similar symptoms and was otherwise in good health; he denied taking any medications. He drank alcohol socially, but denied smoking or illicit drug use.
On physical examination, his vital signs and oxygen saturation were normal. Pulmonary, cardiovascular, and abdominal examinations were also normal. The patient thought his speech was somewhat slurred, but the triage nurse and treating emergency physician (EP) had difficulty detecting any altered speech. He was noted to have mild (4+/5) right upper and lower extremity weakness; no facial droop was detected. The patient did have a mild pronator drift of the right upper extremity. Gait testing revealed a mild limp of the right lower extremity.
The EP consulted the hospitalist, and the patient was admitted to a monitored bed. The following morning, a brain magnetic resonance image revealed an ischemic stroke in the distribution of the left middle cerebral artery. The patient’s hospital course was uncomplicated, but at the time of discharge, he continued to have mild right-sided weakness and required the use of a cane.
The patient sued the hospital and the EP for negligence in failing to treat his condition in a timely manner and for not consulting a neurologist. The plaintiff’s attorneys argued the patient should have been given tissue plasminogen activator (tPA), which would have avoided the residual right-sided weakness. The defense denied negligence and argued the patient’s symptoms could have been due to several things for which tPA would have been an inappropriate treatment. A defense verdict was returned.
Discussion
Stroke in young patients is relatively rare. With “young” defined as aged 18 to 45 years, this population accounts for approximately 2% to 12% of cerebral infarcts.1 In one nationwide US study of stroke in young adults, Ellis2 found that 4.9% of individuals experiencing a stroke in 2007 were between ages 18 and 44 years. Among this group, 78% experienced an ischemic stroke; 11.2% experienced a subarachnoid hemorrhage (SAH); and 10.8% had an intracerebral hemorrhage.2
While the clinical presentation of stroke in young adults is similar to that of older patients, the etiologies and risk factors are very different. In older patients, atherosclerosis is the major cause of ischemic stroke. In studies of young adults with ischemic stroke, cardioembolism was found to be the leading cause. Under this category, a patent foramen ovale (PFO) was considered a common cause, followed by atrial fibrillation, bacterial endocarditis, rheumatic heart disease, and atrial myxoma. There is, however, increasing controversy over the role of PFO as an etiology of stroke. Many investigators think its role has been overstated and is probably more of an incidental finding than a causal relationship.3 Patients with a suspected cardioembolic etiology will usually require an echocardiogram (with saline contrast or a “bubble study” for suspected PFO), cardiac monitoring, and a possible Holter monitor at the time of discharge (to detect paroxysmal arrhythmias).
Following cardioembolic etiologies, arterial dissection is the next most common category.4 In one study of patients aged 31 to 45 years old, arterial dissection was the most common cause of ischemic stroke.4 Clinical features suggesting dissection include a history of head or neck trauma (even minor trauma), headache or neck pain, and local neurological findings (eg, cranial nerve palsy or Horner syndrome).3 Unfortunately, only about 25% of patients volunteer a history of recent neck trauma. If a cervical or vertebral artery dissection is suspected, contrast enhanced magnetic resonance angiography (MRA) is the most sensitive and specific test, followed by carotid ultrasound and CT angiography.3
Traditional risk factors for stroke include hypertension and diabetes mellitus (DM). This is not true for younger adults that experience an ischemic stroke. Cigarette smoking is a very important risk factor for cerebrovascular accident in young adults; in addition, the more one smokes, the greater the risk. Other risk factors in young adults include history of migraine headaches (especially migraine with aura), pregnancy and the postpartum period, and illicit drug use.3
The defense’s argument that there are many causes of stroke in young adults that would be inappropriate for treatment with tPA, such as a PFO, carotid dissection or bacterial endocarditis, is absolutely true. Young patients need to be aggressively worked up for the etiology of their stroke, and may require additional testing, such as an MRA, echocardiogram, or Holter monitoring to determine the underlying cause of their stroke.
Obstruction Following Gastric Bypass Surgery
A 47-year-old woman presented to the ED complaining of severe back and abdominal pain. Onset had been gradual and began approximately 4 hours prior to arrival. She described the pain as crampy and constant. The patient had vomited twice; she denied diarrhea and had a normal bowel movement the previous day. She denied any vaginal or urinary complaints. Her past medical history was significant for hypertension and status post gastric bypass surgery 6 months prior. She had lost 42 pounds to date. She denied smoking or alcohol use.
The patient’s vital signs on physical examination were: blood pressure, 154/92 mm Hg; pulse, 106 beats/minute; respiratory rate, 18 breaths/minute; and temperature, 99˚F. Oxygen saturation was 96% on room air. The patient’s lungs were clear to auscultation bilaterally. The heart was mildly tachycardic, with a regular rhythm and without murmurs, rubs, or gallops. The abdominal examination revealed diffuse tenderness and involuntary guarding. There was no distention or rebound. Bowel sounds were present but hypoactive. Examination of the back revealed bilateral paraspinal muscle tenderness without costovertebral angle tenderness.
The EP ordered a CBC, BMP, serum lipase, and a urinalysis. The patient was given an intravenous (IV) bolus of 250 cc normal saline in addition to IV morphine 4 mg and IV ondansetron 4 mg. Her white blood cell (WBC) count was slightly elevated at 12.2 g/dL, with a normal differential. The remainder of the laboratory studies were normal, except for a serum bicarbonate of 22 mmol/L.
The patient stated she felt somewhat improved, but continued to have abdominal and back pain. The EP admitted her to the hospital for observation and pain control. She died the following day from a bowel obstruction. The family sued the EP for negligence in failing to order appropriate testing and for not consulting with specialists to diagnose the bowel obstruction, which is a known complication of gastric bypass surgery. The jury returned a verdict of $2.4 million against the EP.
Discussion
The frequency of bariatric surgery in the United States continues to increase, primarily due to its success with regard to weight loss, but also because of its demonstrated improvement in hypertension, obstructive sleep apnea, hyperlipidemia, and type 2 DM.1
Frequently, the term “gastric bypass surgery” is used interchangeably with bariatric surgery. However, the EP must realize these terms encompass multiple different operations. The four most common types of bariatric surgery in the United Stated are (1) adjustable gastric banding (AGB); (2) the Roux-en-Y gastric bypass (RYGB); (3) biliopancreatic diversion with duodenal switch (BPD-DS); and (4) vertical sleeve gastrectomy (VSG).2 (See the Table for a brief explanation of each type of procedure.)
Since each procedure has its own respective associated complications, it is important for the EP to know which the type of gastric bypass surgery the patient had. For example, leakage is much more frequent following RYGB than in gastric banding, while slippage and obstruction are the most common complications of gastric banding.3,4 It is also very helpful to know the specific type of procedure when discussing the case with the surgical consultant.
Based on a recent review of over 800,000 bariatric surgery patients, seven serious common complications following the surgery were identified.3 These included bleeding, leakage, obstruction, stomal ulceration, pulmonary embolism and respiratory complications, blood sugar disturbances (usually hypoglycemia and/or metabolic acidosis), and nutritional disturbances. While not all-inclusive, this list represents the most common serious complications of gastric bypass surgery.
The complaint of abdominal pain in a patient that has undergone bariatric surgery should be taken very seriously. In addition to determining the specific procedure performed and date, the patient should be questioned about vomiting, bowel movements, and the presence of blood in stool or vomit. Depending upon the degree of pain present, the patient may need to be given IV opioid analgesia to facilitate a thorough abdominal examination. A rectal examination should be performed to identify occult gastrointestinal bleeding.
These patients require laboratory testing, including CBC, BMP, and other laboratory evaluation as indicated by the history and physical examination. Early consultation with the bariatric surgeon is recommended. Many, if not most, patients with abdominal pain and vomiting will require imaging, usually a CT scan with contrast of the abdomen and pelvis. Because of the difficulty in interpreting the CT scan results in these patients, the bariatric surgeon will often want to personally review the films rather than rely solely on the interpretation by radiology services.
Unfortunately, the EP in this case did not appreciate the seriousness of the situation. The presence of severe abdominal pain, tenderness, guarding, mild tachycardia with leukocytosis, and metabolic acidosis all pointed to a more serious etiology than muscle spasm. This patient required IV fluids, analgesia, and imaging, as well as consultation with the bariatric surgeon.
- Chatzikonstantinou A, Wolf ME, Hennerici MG. Ischemic stroke in young adults: classification and risk factors. J Neurol. 2012;259(4):653-659.
- Ellis C. Stroke in young adults. Disabil Health J. 2010;3(3):222-224.
- Ferro JM, Massaro AR, Mas JL. Aetiological diagnosis of ischemic stroke in young adults. Lancet Neurol. 2010;9(11):1085-1096.
- Chan MT, Nadareishvili ZG, Norris JW; Canadian Stroke Consortium. Diagnostic strategies in young patients with ischemic stroke in Canada. Can J Neurol Sci. 2000;27(2):120-124.
- Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292(14):1724-1737.
- Livingston EH. Patient guide: Endocrine and nutritional management after bariatric surgery: A patient’s guide. Hormone Health Network Web site. http://www.hormone.org/~/media/Hormone/Files/Patient%20Guides/Mens%20Health/PGBariatricSurgery_2014.pdf. Accessed December 17, 2014.
- Hussain A, El-Hasani S. Bariatric emergencies: current evidence and strategies of management. World J Emerg Surg. 2013;8(1):58.
- Campanille FC, Boru C, Rizzello M, et al. Acute complications after laparoscopic bariatric procedures: update for the general surgeon. Langenbecks Arch Surg. 2013;398(5):669-686
- Chatzikonstantinou A, Wolf ME, Hennerici MG. Ischemic stroke in young adults: classification and risk factors. J Neurol. 2012;259(4):653-659.
- Ellis C. Stroke in young adults. Disabil Health J. 2010;3(3):222-224.
- Ferro JM, Massaro AR, Mas JL. Aetiological diagnosis of ischemic stroke in young adults. Lancet Neurol. 2010;9(11):1085-1096.
- Chan MT, Nadareishvili ZG, Norris JW; Canadian Stroke Consortium. Diagnostic strategies in young patients with ischemic stroke in Canada. Can J Neurol Sci. 2000;27(2):120-124.
- Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292(14):1724-1737.
- Livingston EH. Patient guide: Endocrine and nutritional management after bariatric surgery: A patient’s guide. Hormone Health Network Web site. http://www.hormone.org/~/media/Hormone/Files/Patient%20Guides/Mens%20Health/PGBariatricSurgery_2014.pdf. Accessed December 17, 2014.
- Hussain A, El-Hasani S. Bariatric emergencies: current evidence and strategies of management. World J Emerg Surg. 2013;8(1):58.
- Campanille FC, Boru C, Rizzello M, et al. Acute complications after laparoscopic bariatric procedures: update for the general surgeon. Langenbecks Arch Surg. 2013;398(5):669-686
Malpractice Counsel: Child abuse, methadone overdose
Missed Child Abuse
A 7-year-old girl was brought to the ED by her mother for discomfort with urination. The patient was otherwise healthy, up-to-date on all of her immunizations, and without any other complaints. Her vital signs were normal, and the physical examination was unremarkable. Although the chart did not reflect that a genitourinary examination was performed, the emergency physician (EP) stated that he had performed one.
A urinalysis was obtained, which was consistent with a bacterial infection. The patient was diagnosed with a urinary tract infection (UTI), prescribed an antibiotic, and discharged home with appropriate instructions.
Approximately 11 months later, it was discovered that the patient and her older sister were victims of sexual abuse by their 17-year-old stepbrother. Apparently, the abuse had started several months prior to the patient’s ED visit. The mother sued the EP and hospital for failure to recognize the signs and symptoms of sexual abuse. The plaintiff argued the child and mother should have been questioned about the possibility of sexual abuse, and that a more detailed physical examination would have shown evidence of abuse. The defense argued that the child’s presentation did not suggest sexual abuse; a defense verdict was returned.
Discussion
There are no reliable estimates of the incidence of pediatric sexual abuse in the United States. According to the most recent US Department of Health and Human Services Child Maltreatment Report, approximately 62,936 cases of child sexual abuse were reported in the United States in 2012, representing 9.3% of the total number of reported maltreatment cases that year.1 A meta-analysis of 22 US-based studies using national, local, and regional sampling found a much higher rate. This data suggest that 30% to 40% of girls and 13% of boys experienced sexual abuse during childhood.2
For EPs, sexually abused pediatric patients usually present in one of two ways: they are presented by a caregiver based on a suspicion or a disclosure of sexual abuse; or, in the more difficult presentation, they are brought in for evaluation of symptoms related to the genitourinary system or rectum. Such symptoms include vaginal discharge or anal or vaginal bleeding, and the presence of a sexually transmitted infection or UTI. While UTI is frequently listed as a potential sign of sexual abuse in children, there are no good data to demonstrate its frequency. Compounding this problem is that approximately 3% of girls and 1% of boys in the general population are diagnosed with a UTI prior to the onset of puberty.3 Interestingly, though most texts and articles discussing pediatric sexual abuse usually include UTI as a potential sign of abuse, reviews of UTIs in pediatric patients seldom include a discussion of sexual abuse as a potential etiology.
Emergency physicians must therefore maintain a high index of suspicion when evaluating a pediatric patient with a genitourinary or rectal complaint. If the child is old enough to give a history, the caregiver(s) should be asked to leave the room and the patient questioned directly about improper touching, physical activity, etc. The genital and perianal areas should be visually inspected. In general, a speculum examination is not necessary unless vaginal penetration is suspected or the patient is an older adolescent. The majority of pediatric patients can simply be examined in the supine, frog-leg position.
Physical signs of penetration include the presence of concavities (hymen notches), especially at the 6 o’clock position. In addition, irregularities in the hymen contour may be associated with prior injury. More obvious signs of sexual abuse include the presence of warts (condyloma acuminata or lata), vesicles, ulcers, bruising, or vaginal discharge.4 It is important to remember that the absence of physical findings does not exclude sexual abuse.
Laboratory testing of suspected victims of sexual abuse should include cultures of the vagina and rectum for gonorrhea and chlamydia, and throat cultures for gonorrhea.4 Additional testing should be based on the history and physical examination.
When an EP suspects child abuse, he or she must contact child protective services and/or law enforcement agencies, as required by law. It is imperative that the child be placed in a protected environment immediately; on occasion, this may require hospital admission.
This case emphasizes the need for EPs to at least consider sexual abuse in the pediatric patient with a genitourinary or rectal complaint.
Methadone Overdose: Intentional or Not
A 19-year-old woman presented to the ED via emergency medical services (EMS) unresponsive with shallow respirations. She had been found in her home by her grandmother. The paramedics brought the patient’s prescription medications to the ED, which included methadone, morphine, and naproxen. Reportedly, these medications had been prescribed by the patient’s family practitioner for chronic neck pain.
The patient was given intravenous naloxone (Narcan) and rapidly returned to her usual baseline. Her vital signs were normal and the physical examination was unremarkable. She told the EP that she had mistakenly taken the wrong dose of methadone, and vehemently denied any suicidal ideations or past attempts; she did not want to be admitted to the hospital. After several hours of observation, the patient remained in stable condition and without complaint. She was discharged home in the company of her grandmother, with instructions to continue her methadone, morphine, and naproxen, but to pay special attention to the dosage and frequency of use for each drug.
Four days later, the patient was found dead at home by her grandmother; the death was attributed to an overdose of methadone. The EP and hospital were sued by the plaintiff because of the discharge instructions to continue the same medication which had resulted in her first ED visit. The family practitioner was also sued for prescribing these medications to a patient with a history of drug abuse. At trial, it came to light that the patient had also probably ingested some illegally obtained hydrocodone/acetaminophen tablets (Vicodin). A defense verdict was returned.
Discussion
Deaths due to methadone overdose are becoming an increasing problem in the United States. In 2009 alone, more than 4 million prescriptions for methadone were written for pain patients.1 To place this figure in perspective, between 1997 and 2007 the number of grams of methadone prescribed in the United States increased more than 1,200%.2 According to US Centers for Disease Control and Prevention data from 2009, although methadone comprises approximately 2% of all analgesic prescription medications, it has been linked to more than 30% of overdose-related deaths due to prescription analgesics.1
Two factors contribute to this problem. Since methadone is so inexpensive, many states and insurance companies list it as the preferred opioid medication on their formularies. In addition, there is also the increased emphasis on physicians to adequately control pain. This helps explain, in part, for the dramatic increase in its use.
The second factor involves the toxicokinetics of methadone. This drug has a long and often unpredictable half-life, which can lead to toxic levels resulting in respiratory depression and death.1 Thus, methadone should only be prescribed by physicians well versed in its pharmacotherapy. Combined with the fact that there is very limited evidence supporting the use of methadone to treat acute or chronic pain unrelated to cancer, most experts agree there are better and safer alternatives.
This patient was treated appropriately in the ED regarding her resuscitation and observation. The real problem lies with the two narcotic medications she was prescribed for chronic pain. The combination of methadone and morphine in an otherwise healthy young woman probably should have raised a red flag. A conversation with the prescribing physician might have been helpful and resulted in a decrease in the dosage of one or both medications. Abrupt discontinuation, however, would not have been appropriate, since this would have resulted in opiate withdrawal and the associated effects of attending nausea, vomiting, diarrhea, diaphoresis, and abdominal cramping.
This patient was not a missed opportunity for psychiatric intervention and prevention of a suicide as there was no evidence she was ever depressed or suicidal. Rather, this was the case of a drug abuser accidently overdosing from multiple prescribed narcotic medications. It is going to take a multipronged effort to reverse this trend, including improved physician education regarding narcotic prescribing, additional resources to treat narcotic addiction, and improved identification of those at risk.
(Missed Child Abuse)
- U.S. Department of Health & Human Services. Administration on Children, Youth and Families, Administration for Children and Families Web site. Child maltreatment 2012. http://www.acf.hhs.gov/sites/default/files/cb/cm2012.pdf. Accessed October 23, 2014.
- Bolen RM, Scannapieco M. Presentation of child sexual abuse: a corrective meta-analysis. Social Serv Rev. 1999; 73(3): 281-313.
- Byerley JS, Steiner MJ: Urinary tract infection in infants and children. In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 7th ed. New York, NY: McGraw Hill Medical; 2011:854-860.
- Berkowitz CD, Claudius I, Tieder JS. Child abuse and neglect. In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 7th ed. New York, NY: McGraw Hill Medical; 2011:1976-1978.
(Methadone Overdose: Intentional or Not)
- Kuehn BM. Methadone overdose deaths rise with increased prescribing for pain. JAMA. 2012; 308(8):749-750.
- U.S. Department of Justice. Drug Enforcement Administration Office of Diversion Control Web site. Automation of reports and consolidation order system (ARCOS). http://www.deadiversion.usdoj.gov/arcos/index.html. Accessed October 23, 2014.
Missed Child Abuse
A 7-year-old girl was brought to the ED by her mother for discomfort with urination. The patient was otherwise healthy, up-to-date on all of her immunizations, and without any other complaints. Her vital signs were normal, and the physical examination was unremarkable. Although the chart did not reflect that a genitourinary examination was performed, the emergency physician (EP) stated that he had performed one.
A urinalysis was obtained, which was consistent with a bacterial infection. The patient was diagnosed with a urinary tract infection (UTI), prescribed an antibiotic, and discharged home with appropriate instructions.
Approximately 11 months later, it was discovered that the patient and her older sister were victims of sexual abuse by their 17-year-old stepbrother. Apparently, the abuse had started several months prior to the patient’s ED visit. The mother sued the EP and hospital for failure to recognize the signs and symptoms of sexual abuse. The plaintiff argued the child and mother should have been questioned about the possibility of sexual abuse, and that a more detailed physical examination would have shown evidence of abuse. The defense argued that the child’s presentation did not suggest sexual abuse; a defense verdict was returned.
Discussion
There are no reliable estimates of the incidence of pediatric sexual abuse in the United States. According to the most recent US Department of Health and Human Services Child Maltreatment Report, approximately 62,936 cases of child sexual abuse were reported in the United States in 2012, representing 9.3% of the total number of reported maltreatment cases that year.1 A meta-analysis of 22 US-based studies using national, local, and regional sampling found a much higher rate. This data suggest that 30% to 40% of girls and 13% of boys experienced sexual abuse during childhood.2
For EPs, sexually abused pediatric patients usually present in one of two ways: they are presented by a caregiver based on a suspicion or a disclosure of sexual abuse; or, in the more difficult presentation, they are brought in for evaluation of symptoms related to the genitourinary system or rectum. Such symptoms include vaginal discharge or anal or vaginal bleeding, and the presence of a sexually transmitted infection or UTI. While UTI is frequently listed as a potential sign of sexual abuse in children, there are no good data to demonstrate its frequency. Compounding this problem is that approximately 3% of girls and 1% of boys in the general population are diagnosed with a UTI prior to the onset of puberty.3 Interestingly, though most texts and articles discussing pediatric sexual abuse usually include UTI as a potential sign of abuse, reviews of UTIs in pediatric patients seldom include a discussion of sexual abuse as a potential etiology.
Emergency physicians must therefore maintain a high index of suspicion when evaluating a pediatric patient with a genitourinary or rectal complaint. If the child is old enough to give a history, the caregiver(s) should be asked to leave the room and the patient questioned directly about improper touching, physical activity, etc. The genital and perianal areas should be visually inspected. In general, a speculum examination is not necessary unless vaginal penetration is suspected or the patient is an older adolescent. The majority of pediatric patients can simply be examined in the supine, frog-leg position.
Physical signs of penetration include the presence of concavities (hymen notches), especially at the 6 o’clock position. In addition, irregularities in the hymen contour may be associated with prior injury. More obvious signs of sexual abuse include the presence of warts (condyloma acuminata or lata), vesicles, ulcers, bruising, or vaginal discharge.4 It is important to remember that the absence of physical findings does not exclude sexual abuse.
Laboratory testing of suspected victims of sexual abuse should include cultures of the vagina and rectum for gonorrhea and chlamydia, and throat cultures for gonorrhea.4 Additional testing should be based on the history and physical examination.
When an EP suspects child abuse, he or she must contact child protective services and/or law enforcement agencies, as required by law. It is imperative that the child be placed in a protected environment immediately; on occasion, this may require hospital admission.
This case emphasizes the need for EPs to at least consider sexual abuse in the pediatric patient with a genitourinary or rectal complaint.
Methadone Overdose: Intentional or Not
A 19-year-old woman presented to the ED via emergency medical services (EMS) unresponsive with shallow respirations. She had been found in her home by her grandmother. The paramedics brought the patient’s prescription medications to the ED, which included methadone, morphine, and naproxen. Reportedly, these medications had been prescribed by the patient’s family practitioner for chronic neck pain.
The patient was given intravenous naloxone (Narcan) and rapidly returned to her usual baseline. Her vital signs were normal and the physical examination was unremarkable. She told the EP that she had mistakenly taken the wrong dose of methadone, and vehemently denied any suicidal ideations or past attempts; she did not want to be admitted to the hospital. After several hours of observation, the patient remained in stable condition and without complaint. She was discharged home in the company of her grandmother, with instructions to continue her methadone, morphine, and naproxen, but to pay special attention to the dosage and frequency of use for each drug.
Four days later, the patient was found dead at home by her grandmother; the death was attributed to an overdose of methadone. The EP and hospital were sued by the plaintiff because of the discharge instructions to continue the same medication which had resulted in her first ED visit. The family practitioner was also sued for prescribing these medications to a patient with a history of drug abuse. At trial, it came to light that the patient had also probably ingested some illegally obtained hydrocodone/acetaminophen tablets (Vicodin). A defense verdict was returned.
Discussion
Deaths due to methadone overdose are becoming an increasing problem in the United States. In 2009 alone, more than 4 million prescriptions for methadone were written for pain patients.1 To place this figure in perspective, between 1997 and 2007 the number of grams of methadone prescribed in the United States increased more than 1,200%.2 According to US Centers for Disease Control and Prevention data from 2009, although methadone comprises approximately 2% of all analgesic prescription medications, it has been linked to more than 30% of overdose-related deaths due to prescription analgesics.1
Two factors contribute to this problem. Since methadone is so inexpensive, many states and insurance companies list it as the preferred opioid medication on their formularies. In addition, there is also the increased emphasis on physicians to adequately control pain. This helps explain, in part, for the dramatic increase in its use.
The second factor involves the toxicokinetics of methadone. This drug has a long and often unpredictable half-life, which can lead to toxic levels resulting in respiratory depression and death.1 Thus, methadone should only be prescribed by physicians well versed in its pharmacotherapy. Combined with the fact that there is very limited evidence supporting the use of methadone to treat acute or chronic pain unrelated to cancer, most experts agree there are better and safer alternatives.
This patient was treated appropriately in the ED regarding her resuscitation and observation. The real problem lies with the two narcotic medications she was prescribed for chronic pain. The combination of methadone and morphine in an otherwise healthy young woman probably should have raised a red flag. A conversation with the prescribing physician might have been helpful and resulted in a decrease in the dosage of one or both medications. Abrupt discontinuation, however, would not have been appropriate, since this would have resulted in opiate withdrawal and the associated effects of attending nausea, vomiting, diarrhea, diaphoresis, and abdominal cramping.
This patient was not a missed opportunity for psychiatric intervention and prevention of a suicide as there was no evidence she was ever depressed or suicidal. Rather, this was the case of a drug abuser accidently overdosing from multiple prescribed narcotic medications. It is going to take a multipronged effort to reverse this trend, including improved physician education regarding narcotic prescribing, additional resources to treat narcotic addiction, and improved identification of those at risk.
Missed Child Abuse
A 7-year-old girl was brought to the ED by her mother for discomfort with urination. The patient was otherwise healthy, up-to-date on all of her immunizations, and without any other complaints. Her vital signs were normal, and the physical examination was unremarkable. Although the chart did not reflect that a genitourinary examination was performed, the emergency physician (EP) stated that he had performed one.
A urinalysis was obtained, which was consistent with a bacterial infection. The patient was diagnosed with a urinary tract infection (UTI), prescribed an antibiotic, and discharged home with appropriate instructions.
Approximately 11 months later, it was discovered that the patient and her older sister were victims of sexual abuse by their 17-year-old stepbrother. Apparently, the abuse had started several months prior to the patient’s ED visit. The mother sued the EP and hospital for failure to recognize the signs and symptoms of sexual abuse. The plaintiff argued the child and mother should have been questioned about the possibility of sexual abuse, and that a more detailed physical examination would have shown evidence of abuse. The defense argued that the child’s presentation did not suggest sexual abuse; a defense verdict was returned.
Discussion
There are no reliable estimates of the incidence of pediatric sexual abuse in the United States. According to the most recent US Department of Health and Human Services Child Maltreatment Report, approximately 62,936 cases of child sexual abuse were reported in the United States in 2012, representing 9.3% of the total number of reported maltreatment cases that year.1 A meta-analysis of 22 US-based studies using national, local, and regional sampling found a much higher rate. This data suggest that 30% to 40% of girls and 13% of boys experienced sexual abuse during childhood.2
For EPs, sexually abused pediatric patients usually present in one of two ways: they are presented by a caregiver based on a suspicion or a disclosure of sexual abuse; or, in the more difficult presentation, they are brought in for evaluation of symptoms related to the genitourinary system or rectum. Such symptoms include vaginal discharge or anal or vaginal bleeding, and the presence of a sexually transmitted infection or UTI. While UTI is frequently listed as a potential sign of sexual abuse in children, there are no good data to demonstrate its frequency. Compounding this problem is that approximately 3% of girls and 1% of boys in the general population are diagnosed with a UTI prior to the onset of puberty.3 Interestingly, though most texts and articles discussing pediatric sexual abuse usually include UTI as a potential sign of abuse, reviews of UTIs in pediatric patients seldom include a discussion of sexual abuse as a potential etiology.
Emergency physicians must therefore maintain a high index of suspicion when evaluating a pediatric patient with a genitourinary or rectal complaint. If the child is old enough to give a history, the caregiver(s) should be asked to leave the room and the patient questioned directly about improper touching, physical activity, etc. The genital and perianal areas should be visually inspected. In general, a speculum examination is not necessary unless vaginal penetration is suspected or the patient is an older adolescent. The majority of pediatric patients can simply be examined in the supine, frog-leg position.
Physical signs of penetration include the presence of concavities (hymen notches), especially at the 6 o’clock position. In addition, irregularities in the hymen contour may be associated with prior injury. More obvious signs of sexual abuse include the presence of warts (condyloma acuminata or lata), vesicles, ulcers, bruising, or vaginal discharge.4 It is important to remember that the absence of physical findings does not exclude sexual abuse.
Laboratory testing of suspected victims of sexual abuse should include cultures of the vagina and rectum for gonorrhea and chlamydia, and throat cultures for gonorrhea.4 Additional testing should be based on the history and physical examination.
When an EP suspects child abuse, he or she must contact child protective services and/or law enforcement agencies, as required by law. It is imperative that the child be placed in a protected environment immediately; on occasion, this may require hospital admission.
This case emphasizes the need for EPs to at least consider sexual abuse in the pediatric patient with a genitourinary or rectal complaint.
Methadone Overdose: Intentional or Not
A 19-year-old woman presented to the ED via emergency medical services (EMS) unresponsive with shallow respirations. She had been found in her home by her grandmother. The paramedics brought the patient’s prescription medications to the ED, which included methadone, morphine, and naproxen. Reportedly, these medications had been prescribed by the patient’s family practitioner for chronic neck pain.
The patient was given intravenous naloxone (Narcan) and rapidly returned to her usual baseline. Her vital signs were normal and the physical examination was unremarkable. She told the EP that she had mistakenly taken the wrong dose of methadone, and vehemently denied any suicidal ideations or past attempts; she did not want to be admitted to the hospital. After several hours of observation, the patient remained in stable condition and without complaint. She was discharged home in the company of her grandmother, with instructions to continue her methadone, morphine, and naproxen, but to pay special attention to the dosage and frequency of use for each drug.
Four days later, the patient was found dead at home by her grandmother; the death was attributed to an overdose of methadone. The EP and hospital were sued by the plaintiff because of the discharge instructions to continue the same medication which had resulted in her first ED visit. The family practitioner was also sued for prescribing these medications to a patient with a history of drug abuse. At trial, it came to light that the patient had also probably ingested some illegally obtained hydrocodone/acetaminophen tablets (Vicodin). A defense verdict was returned.
Discussion
Deaths due to methadone overdose are becoming an increasing problem in the United States. In 2009 alone, more than 4 million prescriptions for methadone were written for pain patients.1 To place this figure in perspective, between 1997 and 2007 the number of grams of methadone prescribed in the United States increased more than 1,200%.2 According to US Centers for Disease Control and Prevention data from 2009, although methadone comprises approximately 2% of all analgesic prescription medications, it has been linked to more than 30% of overdose-related deaths due to prescription analgesics.1
Two factors contribute to this problem. Since methadone is so inexpensive, many states and insurance companies list it as the preferred opioid medication on their formularies. In addition, there is also the increased emphasis on physicians to adequately control pain. This helps explain, in part, for the dramatic increase in its use.
The second factor involves the toxicokinetics of methadone. This drug has a long and often unpredictable half-life, which can lead to toxic levels resulting in respiratory depression and death.1 Thus, methadone should only be prescribed by physicians well versed in its pharmacotherapy. Combined with the fact that there is very limited evidence supporting the use of methadone to treat acute or chronic pain unrelated to cancer, most experts agree there are better and safer alternatives.
This patient was treated appropriately in the ED regarding her resuscitation and observation. The real problem lies with the two narcotic medications she was prescribed for chronic pain. The combination of methadone and morphine in an otherwise healthy young woman probably should have raised a red flag. A conversation with the prescribing physician might have been helpful and resulted in a decrease in the dosage of one or both medications. Abrupt discontinuation, however, would not have been appropriate, since this would have resulted in opiate withdrawal and the associated effects of attending nausea, vomiting, diarrhea, diaphoresis, and abdominal cramping.
This patient was not a missed opportunity for psychiatric intervention and prevention of a suicide as there was no evidence she was ever depressed or suicidal. Rather, this was the case of a drug abuser accidently overdosing from multiple prescribed narcotic medications. It is going to take a multipronged effort to reverse this trend, including improved physician education regarding narcotic prescribing, additional resources to treat narcotic addiction, and improved identification of those at risk.
(Missed Child Abuse)
- U.S. Department of Health & Human Services. Administration on Children, Youth and Families, Administration for Children and Families Web site. Child maltreatment 2012. http://www.acf.hhs.gov/sites/default/files/cb/cm2012.pdf. Accessed October 23, 2014.
- Bolen RM, Scannapieco M. Presentation of child sexual abuse: a corrective meta-analysis. Social Serv Rev. 1999; 73(3): 281-313.
- Byerley JS, Steiner MJ: Urinary tract infection in infants and children. In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 7th ed. New York, NY: McGraw Hill Medical; 2011:854-860.
- Berkowitz CD, Claudius I, Tieder JS. Child abuse and neglect. In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 7th ed. New York, NY: McGraw Hill Medical; 2011:1976-1978.
(Methadone Overdose: Intentional or Not)
- Kuehn BM. Methadone overdose deaths rise with increased prescribing for pain. JAMA. 2012; 308(8):749-750.
- U.S. Department of Justice. Drug Enforcement Administration Office of Diversion Control Web site. Automation of reports and consolidation order system (ARCOS). http://www.deadiversion.usdoj.gov/arcos/index.html. Accessed October 23, 2014.
(Missed Child Abuse)
- U.S. Department of Health & Human Services. Administration on Children, Youth and Families, Administration for Children and Families Web site. Child maltreatment 2012. http://www.acf.hhs.gov/sites/default/files/cb/cm2012.pdf. Accessed October 23, 2014.
- Bolen RM, Scannapieco M. Presentation of child sexual abuse: a corrective meta-analysis. Social Serv Rev. 1999; 73(3): 281-313.
- Byerley JS, Steiner MJ: Urinary tract infection in infants and children. In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 7th ed. New York, NY: McGraw Hill Medical; 2011:854-860.
- Berkowitz CD, Claudius I, Tieder JS. Child abuse and neglect. In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 7th ed. New York, NY: McGraw Hill Medical; 2011:1976-1978.
(Methadone Overdose: Intentional or Not)
- Kuehn BM. Methadone overdose deaths rise with increased prescribing for pain. JAMA. 2012; 308(8):749-750.
- U.S. Department of Justice. Drug Enforcement Administration Office of Diversion Control Web site. Automation of reports and consolidation order system (ARCOS). http://www.deadiversion.usdoj.gov/arcos/index.html. Accessed October 23, 2014.