User login
Evaluation of a Diabetes Care Coordination Program for African-American Women Living in Public Housing
From the University of Kansas Work Group for Community Health and Development, Lawrence, KS (Hassaballa, Schultz, Hunter-Skidmore, Fawcett, Watson-Thompson) and Whittier Street Health Center, Boston, MA (Ebekozien, Ogungbadero, Williams)
Abstract
- Objective: To examine the implementation of the Diabetes Care Coordination Program (DCCP) and its effects on diabetes-related clinical health outcomes.
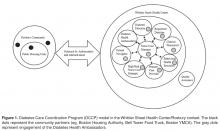
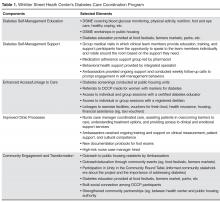
- Methods: Program participants were African American women (n = 148) with type 2 diabetes who lived in public housing in Boston’s Roxbury neighborhood. Through the DCCP, Whittier Street Health Center’s clinical team provided diabetes self-management education, support, and comprehensive diabetes care using the patient-centered medical home model and Diabetes Health Ambassadors as mediators for program delivery. Core intervention components of the DCCP included: 1) diabetes self-management education, 2) support for managing diabetes and distress, 3) enhancing access and linkage to care, 4) improving quality of care, 5) community organization, mobilization, and advocacy, and 6) health system and community transformation. A participatory monitoring and evaluation system was used to document and systematically reflect on program implementation.
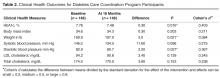
- Results: DCCP implementation was associated with modest improvements in diabetes-related clinical health outcomes for program participants. Results showed statistically significant improvements in HbA1c (P = 0.016), weight (P = 0.021) and diastolic blood pressure (P = 0.027).
- Conclusion: Using neighborhood Diabetes Health Ambassadors for program delivery has implications for assuring access to quality diabetes care for populations experiencing health disparities.
The growing prevalence of type 2 diabetes, with its high morbidity and excess mortality, is imposing a heavy burden on the U.S. health care system [1–3]. It has been recognized that adoption of self-management skills by the person with diabetes is necessary in order to manage their diabetes. Diabetes self-management education and support (DSME/S) provides the foundation to help people with diabetes to navigate these decisions and activities and has been shown to improve health outcomes.
Compared to the general population, African Americans are disproportionately affected by diabetes. African Americans are also less likely to seek diabetes care and have routine diabetes-related visits with a health care professional [4,5]. African Americans have higher HbA1c levels, which contribute to the increased mortality and morbidity rates among this population [6]. Furthermore, African-American women have the poorest HbA1c control as compared to other groups [4]. Concentrated poverty and lower socioeconomic status are social determinants associated with higher prevalence of diabetes [7]. Economic barriers, living conditions, and the built environment play a significant role in contributing to this health disparity [8].
In 2010, the Bristol-Myers Squibb (BMS) Foundation launched the Together on Diabetes initiative to improve the health outcomes of adult populations disproportionately affected by type 2 diabetes. In November 2010, Together on Diabetes issued a request for proposals to encourage, identify, and promote new and evidence-based approaches to empower African-American women to control their diabetes [9–11], taking into account the opportunity these women have to influence the health of their families and communities. Whittier Street Health Center in Boston received a grant to implement a program that would connect African-American women living in public housing in the Roxbury neighborhood with comprehensive diabetes management, including health education by a certified diabetes educator, nutritional counseling by a dietitian, and a tailored program of physical activity.
In this article, we describe the project and effects on diabetes-related clinical health outcomes.
Methods
Setting
Whittier Street Health Center (WSHC) is a federally qualified community health center that serves over 25,000 patients annually. The WSHC is situated in the heart of Boston’s Roxbury neighborhood, close to 5 public housing developments; 83% of WSHC patients live in public housing units. Roxbury is an underserved neighborhood with high rates of poverty, violence, and disease [12]. African Americans comprise the majority of residents living in Roxbury, making up 55.6% of the total population [13].
Diabetes Care Coordination Program
Ambassadors
Diabetes Health Ambassadors, a key component of the program, were hired to engage community members in managing their own health. Five Ambassadors were recruited and retained throughout the project period. Ambassadors were referred by their primary care provider at WSHC and interviewed for the job by the patient navigator. Ambassadors were required to be African-American women with type 2 diabetes living in a public housing unit within the Roxbury neighborhood. In addition, they were required to have their diabetes under control as defined by the WSHC clinical team (HbA1c of 8.0 or below). They also had to want to help other women control their diabetes and be able to deliver motivational presentations as well as have knowledge of available community resources.
Ambassadors received 30 hours of paid training from the certified diabetes educator. During training, they learned the definition, risk factors, and causes of diabetes, how it is controlled, and how to explain this information at a fifth-grade level. Modeling and feedback was used to assure that the information each Ambassador presented was accurate. Ambassadors were also trained on how to measure blood pressure and blood glucose levels and how to respectfully deliver the results. Additionally, Ambassadors received training on cultural competence. Ambassadors were engaged in community outreach and patient support for 20 hours per week and were compensated for their time with stipends.
Participant Recruitment and Outreach
A rolling enrollment for the DCCP began January 2012. The outreach team from the WSHC attended coffee hours at the public housing units and other community events where they conducted onsite blood pressure and glucose screenings as well as educated community members on healthy eating and active lifestyle to reduce the risks for diabetes. Mobile kits were used for testing, so participants received the test results immediately. Two Ambassadors, the outreach nurse, and the patient navigator conducted the outreach events. The set up included two tables, 6 chairs, education materials, and blood pressure and blood sugar screening materials.
Screenings were offered in the public housing units 3 times a week (twice during the week and once during the weekend). Posters in the neighborhood notifed women of the time and location of the screenings. Other settings for services such as screenings and referrals to primary care and health insurance applications included churches, mosques, community festivals, farmers markets, parks, and hair salons.
Women who had elevated glucose readings were invited to enroll in the DCCP program and an appointment at the WSHC was made for those who signed up.
During the period January 2012 to June 2013, 980 African-American women were screened for diabetes. Most screenings took place in the public housing units. Among those screened, 340 had an elevated blood glucose and were referred to WSHC for services. Of those, 175 women were recruited and enrolled into the DCCP. At the WSHC, a standardized protocol was used to measure HbA1c to confirm a diagnosis of diabetes once patients attended their first appointment. Age of participants ranged from 40 to 49. Most women were unemployed and had many competing responsibilities and stressors. Completed preassessment questionaires indicated that participants did not engage in healthy eating or physical activity as part of their daily routines prior to enrollment.
Program Components
At the Center, Ambassadors spoke with program participants and inquired about their barriers to diabetes care (eg, access to food [15], health insurance, etc.) using a standardized list. Ambassadors linked program participants to community support services as needed, including health insurance enrollment, financial support, and housing support. Services were also provided in collaboration with community organizations. For example, subsidized gym memberships were available at the local YMCA and a local fitness studio, and there was an instructor at the YMCA to guide the women through physical activity routines.
Participants could attend DSME group sessions provided by the certified diabetes educator. The course met twice a week for 2 hours for a period of 6 weeks. The course was interactive and included hands-on training in blood glucose measurement and food preparation. Healthy food was offered after each session, which provided a further opportunity for participants to engage in peer-to-peer support. After the completion of the DSME course, bi-weekly support group sessions were held until program completion (June 2013). All clinical team members were present at the support group sessions, with patients rotating to speak to them to ask questions or discuss concerns related to self-management.
A part of DSME, the registered dietitian provided nutrition information and healthy cooking demonstrations for program participants within group sessions. The primary care physician met the patient once a month and kept track of clinical changes over time. Patients with HbA1c ≥ 9% were referred to the high-risk nurse case manager who worked one-on-one with program participants to help them avoid serious diabetes complications.
Ambassadors were a part of all the course and support group sessions, and when needed they attended indivdual sessions, such as doctor visits and meetings with the high-risk nurse case manager. Ambassadors accompanied program participants during visits with clinical staff to provide additional support when requested.
The manager of quality assurance assured the safety of intervention procedures and employed performance improvement methods. Program participants provided informed consent, and had the right to withdraw at any time. The Quality Assurance Committee at WSHC protected the rights of participants, assured the safety of intervention procedures, and assured the quality of care received by each participant.
Evaluation
The Work Group for Community Health and Development at the University of Kansas was selected by the BMS Foundation to evaluate the implementation and related clinical outcomes of the program using a participatory evaluation framework [16–18]. A similarly funded study used the same study approach [19]. Clinical health outcomes were analyzed through a pre-post test comparison using STATA Version 12. Paired t tests were used to examine within-patient health outcome changes. The mean interval between the pre and post measurements was 16 months. A 0.05 level of significance was used. Using a one-sided t test, Cohen’s d was computed to measure effect size.
Results
Services
Clinical Outcomes
Discussion
This empirical case study examined the implementation of the Diabetes Care Coordination Program (DCCP) and its effects on diabetes-related clinical health outcomes for program participants. The program’ glucose screenings and educational workshops at public housing units provided enhanced access to diabetes care services for community members. Referrals to WSHC allowed for the provision of clinical health services through a comprehensive care model. Modest improvements in diabetes-related clinical health indicators were seen.
Some challenges were noted during implementation of the DCCP and addressed as part of a quality improvement process. First, Diabetes Health Ambassadors originally went door to door and had difficulty recruiting participants. Holding screening events in public spaces within housing units addressed this problem. Second, the WSHC team found that women needed more behavioral health support than was being provided, with some of the women reporting to their case managers that it was difficult for them to handle the stresses of life and at the same time manage their diabetes. In response, an integrated behavioral health specialist was hired to provide guidance on how to manage life stressors and how to increase health behaviors despite physical, social, and financial barriers.
Third, women reported a lack of access to fresh fruits and vegetables. In response, WSHC implemented a formal collaboration with a mobile food truck (June 2012) that sold subsidized fresh food 3 days a week to public housing residents. Fourth, participants reported some barriers related to transportation for scheduled appointments at the WSHC. The team addressed this issue by providing taxi vouchers for those who lacked adequate access to transportation. Finally, the coordinated team noticed that medication adherence was a barrier to care for many program participants. Consequently, they developed a medication management support group led by the clinical pharmacist to address barriers related to medication adherence.
There were several methodological challenges confronted in carrying out this study. First, the dose of services that were provided for each individual participant was difficult to ascertain. For example, some of those enrolled in the DCCP earlier may not have had the full set of services that were available towards the end of the program. Second, although group data were available, data on individual level outcomes were not; this made it difficult to assess whether there was change in behavior on the part of particular individuals. Third, a case study design, without a comparison group, does not control for threats to internal validity (eg, history, maturation, and attrition) that might have accounted for improvements in clinical outcomes. Finally, despite the comprehensive documentation, there could have been program elements that were implemented but not documented. Despite these methodological limitations, the case study design facilitated learning about associations between program implementation and changes in clinical health outcomes in a context of health disparities [20].
A particular strength of the program was use of Diabetes Health Ambassadors as mediators for DCCP service delivery. Ambassadors increased diabetes awareness within the community and also played a key role in building rapport and trust in the diabetes program among community members.
Lessons Learned
As part of a qualitative component, key informant interviews with WSHC staff were used to examine lessons learned during project implementation. First, an identified positive outcome was that the Ambassadors gained new insights into the management of their own diabetes and adopted additional lifestyle changes along with program participants. Second, the WSHC team affirmed that African-American women act as gatekeepers for their families, and that teaching and serving one woman allowed for teaching and serving the entire family. Program participants reported that their own lifestyle changes had an impact on other family members. For example, one participant reported she stopped purchasing soda beverages for her family. Another participant began using healthier cooking strategies, such as using olive oil instead of butter. Third, consistent with another study, the coordinated care model helped to assure comprehensive diabetes care [21]. Staff noted that “it takes a village” (a coordinated team) to address the diverse array of clinical issues needed for diabetes control. Fourth, self-management education was helpful, especially when coupled with social support from peers and family members. Fifth, working collaboratively with partners in non-health sectors was helpful in achieving the conditions needed for improved diabetes care [22].
Recommendations for Future Research and Practice
There are several recommendations for future research and practice. First, to achieve stronger clinical health outcomes, the DCCP would need to be enhanced by assuring lower caseloads for the WSHC clinical team. Second, to expand the evidence base, stronger experimental designs are needed to draw firmer conclusions about causal relationships. For instance, a multiple-baseline design across similar federally qualified heath centers could enable a better understanding of the effects of this community-based DCCP intervention in urban contexts. Third, research and practice would benefit from further testing of the model using community health workers for delivery of DSME and DSMS services. Fourth, implementation science can aid in enhancing the role of Ambassadors by providing tools/frameworks for improved delivery of services such as the core implementation components of selection and training [23]. Finally, the use of behavioral science methods can help extend the evidence base for the effects of the DCCP intervention on behavior change at the individual and the community levels [24,25].
Conclusion
This empirical case study adds to our understanding of delivering community-based diabetes care in a public housing context. This study examined the implementation and effects of a diabetes program for African-American women experiencing health disparities. The delivery of diabetes services by Diabetes Health Ambassadors was effective in engaging women with diabetes who lived in low-income housing. This study provided further evidence that coordinated diabetes care, with a focus on culturally and contextually appropriate service delivery, can have positive health outcomes. Further research is needed to examine effects of the DCCP intervention at the individual, clinic, family, and community levels.
Addressing the rapidly increasing prevalence of diabetes is a huge challenge, especially among vulnerable populations at disproportionate risk for adverse health outcomes. These patients face physical, emotional, and financial burdens. We need to assure that community health workers and coordinated clinical teams are prepared to support patients’ acquisition and maintenance of self-care behaviors. Eliminating diabetes-related disparities requires modifying the health system and the broader community environment [26]. Addressing the barriers to medical and self-care that vulnerable populations with type 2 diabetes face will provide them with greater opportunities for health and well-being.
Acknowledgments: The authors thank the many community partners throughout Boston that made this project possible.
Corresponding author: Ithar Hassaballa, KU Work Group for Community Health and Development, University of Kansas, 1000 Sunnyside Ave, 4082 Dole Center, Lawrence, KS 66045, ithar@ku.edu.
Funding/support: Funding for the Whittier Street Health Center’s Diabetes Care Coordination Program and for the evaluation of the Together on Diabetes initiative was provided by the Bristol-Myers Squibb Foundation.
Financial disclosures: None.
1. Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care 2004;27:1047–53.
2. Centers for Disease Control and Prevention. National diabetes statistics report: estimates of diabetes and its burden in the United States, 2014. Atlanta: U.S. Department of Health and Human Services; 2014.
3. Narayan KM, Boyle JP, Geiss LS, Saaddine JB, Thompson TJ. Impact of recent increase in incidence on future diabetes burden: U.S., 2005-2050. Diabetes Care 2006;29:2114–6.
4. Tang TS, Brown MB, Funnell MM, Anderson RM. Social support, quality of life, and self-care behaviors among African Americans with type 2 diabetes. Diabetes Educ 2008;34:266-76.
5. Crabtree K, Sherrer N, Rushton T, Willig A, Agne A, Shelton T, Cherrington A. Diabetes connect: African American men's preferences for a community-based diabetes management program. Diabetes Educ 2015;41:118-26.
6. Kirk JK, D'Agostino RB Jr, Bell RA, Passmore LV, Bonds DE, Karter AJ, Narayan KM. Disparities in HbA1c levels between African-American and non-Hispanic white adults with diabetes: a meta-analysis. Diabetes Care 2006;29:2130–6.
7. Batts ML, Gary TL, Huss K, Hill MN, Bone L, Brancati FL. Patient priorities and needs for diabetes care among urban African American adults. Diabetes Educ 2001;27:405–12.
8. Horowitz CR, Colson KA, Hebert PL, Lancaster K. Barriers to buying healthy foods for people with diabetes: evidence of environmental disparities. Am J Public Health 2004;94:1549–54.
9. Haas L, Maryniuk M, Beck J, et al; 2012 Standards Revision Task Force. National standards for diabetes self-management education and support. Diabetes Care 2013;36 Suppl 1:S100–8.
10. Cené CW, Haymore LB, Ellis D, Whitaker S, Henderson S, Lin FC, Corbie-Smith G. Implementation of the power to prevent diabetes prevention educational curriculum into rural African American communities: a feasibility study. Diabetes Educ 2013;39:776–85.
11. Feathers JT, Kieffer EC, Palmisano G, et al. The development, implementation, and process evaluation of the REACH Detroit Partnership's Diabetes Lifestyle Intervention. Diabetes Educ 2007;33:509–20.
12. Rahman S, Hu H, McNeely E, et al. Social and environmental risk factors for hypertension in African Americans. Fla Public Health Rev 2008;5:64–72.
13. US Bureau of the Census. Available at www.cityofboston.gov/dnd/PDR/Maps_and_Neighborhood_Profiles.asp.
14. Reid RJ, Coleman K, Johnson EA, Fishman PA, Hsu C, Soman MP, Trescott CE, Erikson M, Larson EB. The Group Health medical home at year two: cost savings, higher patient satisfaction, and less burnout for providers. Health Aff (Millwood) 2010;29:835–43.
15. Fulp RS, McManus KD, Johnson PA. Barriers to purchasing foods for a high-quality, healthy diet in a low-income African American community. Fam Community Health 2009;32:206–17.
16. Fawcett SB, Schultz JA. Supporting participatory evaluation using the Community Tool Box online documentation system. Community-Based Participatory Research for Health. San Francisco: Jossey-Bass; 2008: 419–23.
17. Collie-Akers V, Schultz JA, Carson V, Fawcett SB, Ronan M. REACH 2010: Kansas City, Missouri evaluating mobilization strategies with neighborhood and faith organizations to reduce risk for health disparities. Health Prom Pract 2009;10(Suppl 2):118S–127S.
18. Fawcett SB, Boothroyd R, Schultz JA, Francisco VT, Carson V, Bremby R. Building capacity for participatory evaluation within community initiatives. J Prev Interven Comm 2003;26:21–36.
19. Sepers CE Jr, Fawcett SB, Lipman R, Schultz J, Colie-Akers V, Perez A. Measuring the implementation and effects of a coordinated care model featuring diabetes self-management education within four patient-centered medical homes. Diabetes Educ 2015;41:328–42.
20. Yin RK. Case study research: Design and methods. Sage; 2013.
21. Mead H, Andres E, Regenstein M. Underserved patients' perspectives on patient-centered primary care: does the patient-centered medical home model meet their needs? Med Care Res Rev 2014;71:61–84.
22. Fawcett S, Schultz J, Watson-Thompson J, Fox M, Bremby R. Building multisectoral partnerships for population health and health equity. Prev Chronic Disease 2010;7:A118. Epub 2010 Oct 15.
23. Fixsen DL, Blase KA, Naoom SF, Wallace F. Core implementation components. Res Soc Work Prac 2009; 19:531–540.
24. Cooper JO, Heron TE, Heward WL. Applied behavior analysis. 2nd ed. Pearson; 2007.
25. Glanz K, Bishop DB. The role of behavioral science theory in development and implementation of public health interventions. Annu Rev Public Health 2010;31:399–418.
26. Jack L, Jack NH, Hayes SC. Social determinants of health in minority populations: a call for multidisciplinary approaches to eliminate diabetes-related health disparities. Diabetes Spectrum 2012;25:9–13.
From the University of Kansas Work Group for Community Health and Development, Lawrence, KS (Hassaballa, Schultz, Hunter-Skidmore, Fawcett, Watson-Thompson) and Whittier Street Health Center, Boston, MA (Ebekozien, Ogungbadero, Williams)
Abstract
- Objective: To examine the implementation of the Diabetes Care Coordination Program (DCCP) and its effects on diabetes-related clinical health outcomes.
- Methods: Program participants were African American women (n = 148) with type 2 diabetes who lived in public housing in Boston’s Roxbury neighborhood. Through the DCCP, Whittier Street Health Center’s clinical team provided diabetes self-management education, support, and comprehensive diabetes care using the patient-centered medical home model and Diabetes Health Ambassadors as mediators for program delivery. Core intervention components of the DCCP included: 1) diabetes self-management education, 2) support for managing diabetes and distress, 3) enhancing access and linkage to care, 4) improving quality of care, 5) community organization, mobilization, and advocacy, and 6) health system and community transformation. A participatory monitoring and evaluation system was used to document and systematically reflect on program implementation.
- Results: DCCP implementation was associated with modest improvements in diabetes-related clinical health outcomes for program participants. Results showed statistically significant improvements in HbA1c (P = 0.016), weight (P = 0.021) and diastolic blood pressure (P = 0.027).
- Conclusion: Using neighborhood Diabetes Health Ambassadors for program delivery has implications for assuring access to quality diabetes care for populations experiencing health disparities.
The growing prevalence of type 2 diabetes, with its high morbidity and excess mortality, is imposing a heavy burden on the U.S. health care system [1–3]. It has been recognized that adoption of self-management skills by the person with diabetes is necessary in order to manage their diabetes. Diabetes self-management education and support (DSME/S) provides the foundation to help people with diabetes to navigate these decisions and activities and has been shown to improve health outcomes.
Compared to the general population, African Americans are disproportionately affected by diabetes. African Americans are also less likely to seek diabetes care and have routine diabetes-related visits with a health care professional [4,5]. African Americans have higher HbA1c levels, which contribute to the increased mortality and morbidity rates among this population [6]. Furthermore, African-American women have the poorest HbA1c control as compared to other groups [4]. Concentrated poverty and lower socioeconomic status are social determinants associated with higher prevalence of diabetes [7]. Economic barriers, living conditions, and the built environment play a significant role in contributing to this health disparity [8].
In 2010, the Bristol-Myers Squibb (BMS) Foundation launched the Together on Diabetes initiative to improve the health outcomes of adult populations disproportionately affected by type 2 diabetes. In November 2010, Together on Diabetes issued a request for proposals to encourage, identify, and promote new and evidence-based approaches to empower African-American women to control their diabetes [9–11], taking into account the opportunity these women have to influence the health of their families and communities. Whittier Street Health Center in Boston received a grant to implement a program that would connect African-American women living in public housing in the Roxbury neighborhood with comprehensive diabetes management, including health education by a certified diabetes educator, nutritional counseling by a dietitian, and a tailored program of physical activity.
In this article, we describe the project and effects on diabetes-related clinical health outcomes.
Methods
Setting
Whittier Street Health Center (WSHC) is a federally qualified community health center that serves over 25,000 patients annually. The WSHC is situated in the heart of Boston’s Roxbury neighborhood, close to 5 public housing developments; 83% of WSHC patients live in public housing units. Roxbury is an underserved neighborhood with high rates of poverty, violence, and disease [12]. African Americans comprise the majority of residents living in Roxbury, making up 55.6% of the total population [13].
Diabetes Care Coordination Program
Ambassadors
Diabetes Health Ambassadors, a key component of the program, were hired to engage community members in managing their own health. Five Ambassadors were recruited and retained throughout the project period. Ambassadors were referred by their primary care provider at WSHC and interviewed for the job by the patient navigator. Ambassadors were required to be African-American women with type 2 diabetes living in a public housing unit within the Roxbury neighborhood. In addition, they were required to have their diabetes under control as defined by the WSHC clinical team (HbA1c of 8.0 or below). They also had to want to help other women control their diabetes and be able to deliver motivational presentations as well as have knowledge of available community resources.
Ambassadors received 30 hours of paid training from the certified diabetes educator. During training, they learned the definition, risk factors, and causes of diabetes, how it is controlled, and how to explain this information at a fifth-grade level. Modeling and feedback was used to assure that the information each Ambassador presented was accurate. Ambassadors were also trained on how to measure blood pressure and blood glucose levels and how to respectfully deliver the results. Additionally, Ambassadors received training on cultural competence. Ambassadors were engaged in community outreach and patient support for 20 hours per week and were compensated for their time with stipends.
Participant Recruitment and Outreach
A rolling enrollment for the DCCP began January 2012. The outreach team from the WSHC attended coffee hours at the public housing units and other community events where they conducted onsite blood pressure and glucose screenings as well as educated community members on healthy eating and active lifestyle to reduce the risks for diabetes. Mobile kits were used for testing, so participants received the test results immediately. Two Ambassadors, the outreach nurse, and the patient navigator conducted the outreach events. The set up included two tables, 6 chairs, education materials, and blood pressure and blood sugar screening materials.
Screenings were offered in the public housing units 3 times a week (twice during the week and once during the weekend). Posters in the neighborhood notifed women of the time and location of the screenings. Other settings for services such as screenings and referrals to primary care and health insurance applications included churches, mosques, community festivals, farmers markets, parks, and hair salons.
Women who had elevated glucose readings were invited to enroll in the DCCP program and an appointment at the WSHC was made for those who signed up.
During the period January 2012 to June 2013, 980 African-American women were screened for diabetes. Most screenings took place in the public housing units. Among those screened, 340 had an elevated blood glucose and were referred to WSHC for services. Of those, 175 women were recruited and enrolled into the DCCP. At the WSHC, a standardized protocol was used to measure HbA1c to confirm a diagnosis of diabetes once patients attended their first appointment. Age of participants ranged from 40 to 49. Most women were unemployed and had many competing responsibilities and stressors. Completed preassessment questionaires indicated that participants did not engage in healthy eating or physical activity as part of their daily routines prior to enrollment.
Program Components
At the Center, Ambassadors spoke with program participants and inquired about their barriers to diabetes care (eg, access to food [15], health insurance, etc.) using a standardized list. Ambassadors linked program participants to community support services as needed, including health insurance enrollment, financial support, and housing support. Services were also provided in collaboration with community organizations. For example, subsidized gym memberships were available at the local YMCA and a local fitness studio, and there was an instructor at the YMCA to guide the women through physical activity routines.
Participants could attend DSME group sessions provided by the certified diabetes educator. The course met twice a week for 2 hours for a period of 6 weeks. The course was interactive and included hands-on training in blood glucose measurement and food preparation. Healthy food was offered after each session, which provided a further opportunity for participants to engage in peer-to-peer support. After the completion of the DSME course, bi-weekly support group sessions were held until program completion (June 2013). All clinical team members were present at the support group sessions, with patients rotating to speak to them to ask questions or discuss concerns related to self-management.
A part of DSME, the registered dietitian provided nutrition information and healthy cooking demonstrations for program participants within group sessions. The primary care physician met the patient once a month and kept track of clinical changes over time. Patients with HbA1c ≥ 9% were referred to the high-risk nurse case manager who worked one-on-one with program participants to help them avoid serious diabetes complications.
Ambassadors were a part of all the course and support group sessions, and when needed they attended indivdual sessions, such as doctor visits and meetings with the high-risk nurse case manager. Ambassadors accompanied program participants during visits with clinical staff to provide additional support when requested.
The manager of quality assurance assured the safety of intervention procedures and employed performance improvement methods. Program participants provided informed consent, and had the right to withdraw at any time. The Quality Assurance Committee at WSHC protected the rights of participants, assured the safety of intervention procedures, and assured the quality of care received by each participant.
Evaluation
The Work Group for Community Health and Development at the University of Kansas was selected by the BMS Foundation to evaluate the implementation and related clinical outcomes of the program using a participatory evaluation framework [16–18]. A similarly funded study used the same study approach [19]. Clinical health outcomes were analyzed through a pre-post test comparison using STATA Version 12. Paired t tests were used to examine within-patient health outcome changes. The mean interval between the pre and post measurements was 16 months. A 0.05 level of significance was used. Using a one-sided t test, Cohen’s d was computed to measure effect size.
Results
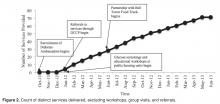
Services
Clinical Outcomes
Discussion
This empirical case study examined the implementation of the Diabetes Care Coordination Program (DCCP) and its effects on diabetes-related clinical health outcomes for program participants. The program’ glucose screenings and educational workshops at public housing units provided enhanced access to diabetes care services for community members. Referrals to WSHC allowed for the provision of clinical health services through a comprehensive care model. Modest improvements in diabetes-related clinical health indicators were seen.
Some challenges were noted during implementation of the DCCP and addressed as part of a quality improvement process. First, Diabetes Health Ambassadors originally went door to door and had difficulty recruiting participants. Holding screening events in public spaces within housing units addressed this problem. Second, the WSHC team found that women needed more behavioral health support than was being provided, with some of the women reporting to their case managers that it was difficult for them to handle the stresses of life and at the same time manage their diabetes. In response, an integrated behavioral health specialist was hired to provide guidance on how to manage life stressors and how to increase health behaviors despite physical, social, and financial barriers.
Third, women reported a lack of access to fresh fruits and vegetables. In response, WSHC implemented a formal collaboration with a mobile food truck (June 2012) that sold subsidized fresh food 3 days a week to public housing residents. Fourth, participants reported some barriers related to transportation for scheduled appointments at the WSHC. The team addressed this issue by providing taxi vouchers for those who lacked adequate access to transportation. Finally, the coordinated team noticed that medication adherence was a barrier to care for many program participants. Consequently, they developed a medication management support group led by the clinical pharmacist to address barriers related to medication adherence.
There were several methodological challenges confronted in carrying out this study. First, the dose of services that were provided for each individual participant was difficult to ascertain. For example, some of those enrolled in the DCCP earlier may not have had the full set of services that were available towards the end of the program. Second, although group data were available, data on individual level outcomes were not; this made it difficult to assess whether there was change in behavior on the part of particular individuals. Third, a case study design, without a comparison group, does not control for threats to internal validity (eg, history, maturation, and attrition) that might have accounted for improvements in clinical outcomes. Finally, despite the comprehensive documentation, there could have been program elements that were implemented but not documented. Despite these methodological limitations, the case study design facilitated learning about associations between program implementation and changes in clinical health outcomes in a context of health disparities [20].
A particular strength of the program was use of Diabetes Health Ambassadors as mediators for DCCP service delivery. Ambassadors increased diabetes awareness within the community and also played a key role in building rapport and trust in the diabetes program among community members.
Lessons Learned
As part of a qualitative component, key informant interviews with WSHC staff were used to examine lessons learned during project implementation. First, an identified positive outcome was that the Ambassadors gained new insights into the management of their own diabetes and adopted additional lifestyle changes along with program participants. Second, the WSHC team affirmed that African-American women act as gatekeepers for their families, and that teaching and serving one woman allowed for teaching and serving the entire family. Program participants reported that their own lifestyle changes had an impact on other family members. For example, one participant reported she stopped purchasing soda beverages for her family. Another participant began using healthier cooking strategies, such as using olive oil instead of butter. Third, consistent with another study, the coordinated care model helped to assure comprehensive diabetes care [21]. Staff noted that “it takes a village” (a coordinated team) to address the diverse array of clinical issues needed for diabetes control. Fourth, self-management education was helpful, especially when coupled with social support from peers and family members. Fifth, working collaboratively with partners in non-health sectors was helpful in achieving the conditions needed for improved diabetes care [22].
Recommendations for Future Research and Practice
There are several recommendations for future research and practice. First, to achieve stronger clinical health outcomes, the DCCP would need to be enhanced by assuring lower caseloads for the WSHC clinical team. Second, to expand the evidence base, stronger experimental designs are needed to draw firmer conclusions about causal relationships. For instance, a multiple-baseline design across similar federally qualified heath centers could enable a better understanding of the effects of this community-based DCCP intervention in urban contexts. Third, research and practice would benefit from further testing of the model using community health workers for delivery of DSME and DSMS services. Fourth, implementation science can aid in enhancing the role of Ambassadors by providing tools/frameworks for improved delivery of services such as the core implementation components of selection and training [23]. Finally, the use of behavioral science methods can help extend the evidence base for the effects of the DCCP intervention on behavior change at the individual and the community levels [24,25].
Conclusion
This empirical case study adds to our understanding of delivering community-based diabetes care in a public housing context. This study examined the implementation and effects of a diabetes program for African-American women experiencing health disparities. The delivery of diabetes services by Diabetes Health Ambassadors was effective in engaging women with diabetes who lived in low-income housing. This study provided further evidence that coordinated diabetes care, with a focus on culturally and contextually appropriate service delivery, can have positive health outcomes. Further research is needed to examine effects of the DCCP intervention at the individual, clinic, family, and community levels.
Addressing the rapidly increasing prevalence of diabetes is a huge challenge, especially among vulnerable populations at disproportionate risk for adverse health outcomes. These patients face physical, emotional, and financial burdens. We need to assure that community health workers and coordinated clinical teams are prepared to support patients’ acquisition and maintenance of self-care behaviors. Eliminating diabetes-related disparities requires modifying the health system and the broader community environment [26]. Addressing the barriers to medical and self-care that vulnerable populations with type 2 diabetes face will provide them with greater opportunities for health and well-being.
Acknowledgments: The authors thank the many community partners throughout Boston that made this project possible.
Corresponding author: Ithar Hassaballa, KU Work Group for Community Health and Development, University of Kansas, 1000 Sunnyside Ave, 4082 Dole Center, Lawrence, KS 66045, ithar@ku.edu.
Funding/support: Funding for the Whittier Street Health Center’s Diabetes Care Coordination Program and for the evaluation of the Together on Diabetes initiative was provided by the Bristol-Myers Squibb Foundation.
Financial disclosures: None.
From the University of Kansas Work Group for Community Health and Development, Lawrence, KS (Hassaballa, Schultz, Hunter-Skidmore, Fawcett, Watson-Thompson) and Whittier Street Health Center, Boston, MA (Ebekozien, Ogungbadero, Williams)
Abstract
- Objective: To examine the implementation of the Diabetes Care Coordination Program (DCCP) and its effects on diabetes-related clinical health outcomes.
- Methods: Program participants were African American women (n = 148) with type 2 diabetes who lived in public housing in Boston’s Roxbury neighborhood. Through the DCCP, Whittier Street Health Center’s clinical team provided diabetes self-management education, support, and comprehensive diabetes care using the patient-centered medical home model and Diabetes Health Ambassadors as mediators for program delivery. Core intervention components of the DCCP included: 1) diabetes self-management education, 2) support for managing diabetes and distress, 3) enhancing access and linkage to care, 4) improving quality of care, 5) community organization, mobilization, and advocacy, and 6) health system and community transformation. A participatory monitoring and evaluation system was used to document and systematically reflect on program implementation.
- Results: DCCP implementation was associated with modest improvements in diabetes-related clinical health outcomes for program participants. Results showed statistically significant improvements in HbA1c (P = 0.016), weight (P = 0.021) and diastolic blood pressure (P = 0.027).
- Conclusion: Using neighborhood Diabetes Health Ambassadors for program delivery has implications for assuring access to quality diabetes care for populations experiencing health disparities.
The growing prevalence of type 2 diabetes, with its high morbidity and excess mortality, is imposing a heavy burden on the U.S. health care system [1–3]. It has been recognized that adoption of self-management skills by the person with diabetes is necessary in order to manage their diabetes. Diabetes self-management education and support (DSME/S) provides the foundation to help people with diabetes to navigate these decisions and activities and has been shown to improve health outcomes.
Compared to the general population, African Americans are disproportionately affected by diabetes. African Americans are also less likely to seek diabetes care and have routine diabetes-related visits with a health care professional [4,5]. African Americans have higher HbA1c levels, which contribute to the increased mortality and morbidity rates among this population [6]. Furthermore, African-American women have the poorest HbA1c control as compared to other groups [4]. Concentrated poverty and lower socioeconomic status are social determinants associated with higher prevalence of diabetes [7]. Economic barriers, living conditions, and the built environment play a significant role in contributing to this health disparity [8].
In 2010, the Bristol-Myers Squibb (BMS) Foundation launched the Together on Diabetes initiative to improve the health outcomes of adult populations disproportionately affected by type 2 diabetes. In November 2010, Together on Diabetes issued a request for proposals to encourage, identify, and promote new and evidence-based approaches to empower African-American women to control their diabetes [9–11], taking into account the opportunity these women have to influence the health of their families and communities. Whittier Street Health Center in Boston received a grant to implement a program that would connect African-American women living in public housing in the Roxbury neighborhood with comprehensive diabetes management, including health education by a certified diabetes educator, nutritional counseling by a dietitian, and a tailored program of physical activity.
In this article, we describe the project and effects on diabetes-related clinical health outcomes.
Methods
Setting
Whittier Street Health Center (WSHC) is a federally qualified community health center that serves over 25,000 patients annually. The WSHC is situated in the heart of Boston’s Roxbury neighborhood, close to 5 public housing developments; 83% of WSHC patients live in public housing units. Roxbury is an underserved neighborhood with high rates of poverty, violence, and disease [12]. African Americans comprise the majority of residents living in Roxbury, making up 55.6% of the total population [13].
Diabetes Care Coordination Program
Ambassadors
Diabetes Health Ambassadors, a key component of the program, were hired to engage community members in managing their own health. Five Ambassadors were recruited and retained throughout the project period. Ambassadors were referred by their primary care provider at WSHC and interviewed for the job by the patient navigator. Ambassadors were required to be African-American women with type 2 diabetes living in a public housing unit within the Roxbury neighborhood. In addition, they were required to have their diabetes under control as defined by the WSHC clinical team (HbA1c of 8.0 or below). They also had to want to help other women control their diabetes and be able to deliver motivational presentations as well as have knowledge of available community resources.
Ambassadors received 30 hours of paid training from the certified diabetes educator. During training, they learned the definition, risk factors, and causes of diabetes, how it is controlled, and how to explain this information at a fifth-grade level. Modeling and feedback was used to assure that the information each Ambassador presented was accurate. Ambassadors were also trained on how to measure blood pressure and blood glucose levels and how to respectfully deliver the results. Additionally, Ambassadors received training on cultural competence. Ambassadors were engaged in community outreach and patient support for 20 hours per week and were compensated for their time with stipends.
Participant Recruitment and Outreach
A rolling enrollment for the DCCP began January 2012. The outreach team from the WSHC attended coffee hours at the public housing units and other community events where they conducted onsite blood pressure and glucose screenings as well as educated community members on healthy eating and active lifestyle to reduce the risks for diabetes. Mobile kits were used for testing, so participants received the test results immediately. Two Ambassadors, the outreach nurse, and the patient navigator conducted the outreach events. The set up included two tables, 6 chairs, education materials, and blood pressure and blood sugar screening materials.
Screenings were offered in the public housing units 3 times a week (twice during the week and once during the weekend). Posters in the neighborhood notifed women of the time and location of the screenings. Other settings for services such as screenings and referrals to primary care and health insurance applications included churches, mosques, community festivals, farmers markets, parks, and hair salons.
Women who had elevated glucose readings were invited to enroll in the DCCP program and an appointment at the WSHC was made for those who signed up.
During the period January 2012 to June 2013, 980 African-American women were screened for diabetes. Most screenings took place in the public housing units. Among those screened, 340 had an elevated blood glucose and were referred to WSHC for services. Of those, 175 women were recruited and enrolled into the DCCP. At the WSHC, a standardized protocol was used to measure HbA1c to confirm a diagnosis of diabetes once patients attended their first appointment. Age of participants ranged from 40 to 49. Most women were unemployed and had many competing responsibilities and stressors. Completed preassessment questionaires indicated that participants did not engage in healthy eating or physical activity as part of their daily routines prior to enrollment.
Program Components
At the Center, Ambassadors spoke with program participants and inquired about their barriers to diabetes care (eg, access to food [15], health insurance, etc.) using a standardized list. Ambassadors linked program participants to community support services as needed, including health insurance enrollment, financial support, and housing support. Services were also provided in collaboration with community organizations. For example, subsidized gym memberships were available at the local YMCA and a local fitness studio, and there was an instructor at the YMCA to guide the women through physical activity routines.
Participants could attend DSME group sessions provided by the certified diabetes educator. The course met twice a week for 2 hours for a period of 6 weeks. The course was interactive and included hands-on training in blood glucose measurement and food preparation. Healthy food was offered after each session, which provided a further opportunity for participants to engage in peer-to-peer support. After the completion of the DSME course, bi-weekly support group sessions were held until program completion (June 2013). All clinical team members were present at the support group sessions, with patients rotating to speak to them to ask questions or discuss concerns related to self-management.
A part of DSME, the registered dietitian provided nutrition information and healthy cooking demonstrations for program participants within group sessions. The primary care physician met the patient once a month and kept track of clinical changes over time. Patients with HbA1c ≥ 9% were referred to the high-risk nurse case manager who worked one-on-one with program participants to help them avoid serious diabetes complications.
Ambassadors were a part of all the course and support group sessions, and when needed they attended indivdual sessions, such as doctor visits and meetings with the high-risk nurse case manager. Ambassadors accompanied program participants during visits with clinical staff to provide additional support when requested.
The manager of quality assurance assured the safety of intervention procedures and employed performance improvement methods. Program participants provided informed consent, and had the right to withdraw at any time. The Quality Assurance Committee at WSHC protected the rights of participants, assured the safety of intervention procedures, and assured the quality of care received by each participant.
Evaluation
The Work Group for Community Health and Development at the University of Kansas was selected by the BMS Foundation to evaluate the implementation and related clinical outcomes of the program using a participatory evaluation framework [16–18]. A similarly funded study used the same study approach [19]. Clinical health outcomes were analyzed through a pre-post test comparison using STATA Version 12. Paired t tests were used to examine within-patient health outcome changes. The mean interval between the pre and post measurements was 16 months. A 0.05 level of significance was used. Using a one-sided t test, Cohen’s d was computed to measure effect size.
Results
Services
Clinical Outcomes
Discussion
This empirical case study examined the implementation of the Diabetes Care Coordination Program (DCCP) and its effects on diabetes-related clinical health outcomes for program participants. The program’ glucose screenings and educational workshops at public housing units provided enhanced access to diabetes care services for community members. Referrals to WSHC allowed for the provision of clinical health services through a comprehensive care model. Modest improvements in diabetes-related clinical health indicators were seen.
Some challenges were noted during implementation of the DCCP and addressed as part of a quality improvement process. First, Diabetes Health Ambassadors originally went door to door and had difficulty recruiting participants. Holding screening events in public spaces within housing units addressed this problem. Second, the WSHC team found that women needed more behavioral health support than was being provided, with some of the women reporting to their case managers that it was difficult for them to handle the stresses of life and at the same time manage their diabetes. In response, an integrated behavioral health specialist was hired to provide guidance on how to manage life stressors and how to increase health behaviors despite physical, social, and financial barriers.
Third, women reported a lack of access to fresh fruits and vegetables. In response, WSHC implemented a formal collaboration with a mobile food truck (June 2012) that sold subsidized fresh food 3 days a week to public housing residents. Fourth, participants reported some barriers related to transportation for scheduled appointments at the WSHC. The team addressed this issue by providing taxi vouchers for those who lacked adequate access to transportation. Finally, the coordinated team noticed that medication adherence was a barrier to care for many program participants. Consequently, they developed a medication management support group led by the clinical pharmacist to address barriers related to medication adherence.
There were several methodological challenges confronted in carrying out this study. First, the dose of services that were provided for each individual participant was difficult to ascertain. For example, some of those enrolled in the DCCP earlier may not have had the full set of services that were available towards the end of the program. Second, although group data were available, data on individual level outcomes were not; this made it difficult to assess whether there was change in behavior on the part of particular individuals. Third, a case study design, without a comparison group, does not control for threats to internal validity (eg, history, maturation, and attrition) that might have accounted for improvements in clinical outcomes. Finally, despite the comprehensive documentation, there could have been program elements that were implemented but not documented. Despite these methodological limitations, the case study design facilitated learning about associations between program implementation and changes in clinical health outcomes in a context of health disparities [20].
A particular strength of the program was use of Diabetes Health Ambassadors as mediators for DCCP service delivery. Ambassadors increased diabetes awareness within the community and also played a key role in building rapport and trust in the diabetes program among community members.
Lessons Learned
As part of a qualitative component, key informant interviews with WSHC staff were used to examine lessons learned during project implementation. First, an identified positive outcome was that the Ambassadors gained new insights into the management of their own diabetes and adopted additional lifestyle changes along with program participants. Second, the WSHC team affirmed that African-American women act as gatekeepers for their families, and that teaching and serving one woman allowed for teaching and serving the entire family. Program participants reported that their own lifestyle changes had an impact on other family members. For example, one participant reported she stopped purchasing soda beverages for her family. Another participant began using healthier cooking strategies, such as using olive oil instead of butter. Third, consistent with another study, the coordinated care model helped to assure comprehensive diabetes care [21]. Staff noted that “it takes a village” (a coordinated team) to address the diverse array of clinical issues needed for diabetes control. Fourth, self-management education was helpful, especially when coupled with social support from peers and family members. Fifth, working collaboratively with partners in non-health sectors was helpful in achieving the conditions needed for improved diabetes care [22].
Recommendations for Future Research and Practice
There are several recommendations for future research and practice. First, to achieve stronger clinical health outcomes, the DCCP would need to be enhanced by assuring lower caseloads for the WSHC clinical team. Second, to expand the evidence base, stronger experimental designs are needed to draw firmer conclusions about causal relationships. For instance, a multiple-baseline design across similar federally qualified heath centers could enable a better understanding of the effects of this community-based DCCP intervention in urban contexts. Third, research and practice would benefit from further testing of the model using community health workers for delivery of DSME and DSMS services. Fourth, implementation science can aid in enhancing the role of Ambassadors by providing tools/frameworks for improved delivery of services such as the core implementation components of selection and training [23]. Finally, the use of behavioral science methods can help extend the evidence base for the effects of the DCCP intervention on behavior change at the individual and the community levels [24,25].
Conclusion
This empirical case study adds to our understanding of delivering community-based diabetes care in a public housing context. This study examined the implementation and effects of a diabetes program for African-American women experiencing health disparities. The delivery of diabetes services by Diabetes Health Ambassadors was effective in engaging women with diabetes who lived in low-income housing. This study provided further evidence that coordinated diabetes care, with a focus on culturally and contextually appropriate service delivery, can have positive health outcomes. Further research is needed to examine effects of the DCCP intervention at the individual, clinic, family, and community levels.
Addressing the rapidly increasing prevalence of diabetes is a huge challenge, especially among vulnerable populations at disproportionate risk for adverse health outcomes. These patients face physical, emotional, and financial burdens. We need to assure that community health workers and coordinated clinical teams are prepared to support patients’ acquisition and maintenance of self-care behaviors. Eliminating diabetes-related disparities requires modifying the health system and the broader community environment [26]. Addressing the barriers to medical and self-care that vulnerable populations with type 2 diabetes face will provide them with greater opportunities for health and well-being.
Acknowledgments: The authors thank the many community partners throughout Boston that made this project possible.
Corresponding author: Ithar Hassaballa, KU Work Group for Community Health and Development, University of Kansas, 1000 Sunnyside Ave, 4082 Dole Center, Lawrence, KS 66045, ithar@ku.edu.
Funding/support: Funding for the Whittier Street Health Center’s Diabetes Care Coordination Program and for the evaluation of the Together on Diabetes initiative was provided by the Bristol-Myers Squibb Foundation.
Financial disclosures: None.
1. Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care 2004;27:1047–53.
2. Centers for Disease Control and Prevention. National diabetes statistics report: estimates of diabetes and its burden in the United States, 2014. Atlanta: U.S. Department of Health and Human Services; 2014.
3. Narayan KM, Boyle JP, Geiss LS, Saaddine JB, Thompson TJ. Impact of recent increase in incidence on future diabetes burden: U.S., 2005-2050. Diabetes Care 2006;29:2114–6.
4. Tang TS, Brown MB, Funnell MM, Anderson RM. Social support, quality of life, and self-care behaviors among African Americans with type 2 diabetes. Diabetes Educ 2008;34:266-76.
5. Crabtree K, Sherrer N, Rushton T, Willig A, Agne A, Shelton T, Cherrington A. Diabetes connect: African American men's preferences for a community-based diabetes management program. Diabetes Educ 2015;41:118-26.
6. Kirk JK, D'Agostino RB Jr, Bell RA, Passmore LV, Bonds DE, Karter AJ, Narayan KM. Disparities in HbA1c levels between African-American and non-Hispanic white adults with diabetes: a meta-analysis. Diabetes Care 2006;29:2130–6.
7. Batts ML, Gary TL, Huss K, Hill MN, Bone L, Brancati FL. Patient priorities and needs for diabetes care among urban African American adults. Diabetes Educ 2001;27:405–12.
8. Horowitz CR, Colson KA, Hebert PL, Lancaster K. Barriers to buying healthy foods for people with diabetes: evidence of environmental disparities. Am J Public Health 2004;94:1549–54.
9. Haas L, Maryniuk M, Beck J, et al; 2012 Standards Revision Task Force. National standards for diabetes self-management education and support. Diabetes Care 2013;36 Suppl 1:S100–8.
10. Cené CW, Haymore LB, Ellis D, Whitaker S, Henderson S, Lin FC, Corbie-Smith G. Implementation of the power to prevent diabetes prevention educational curriculum into rural African American communities: a feasibility study. Diabetes Educ 2013;39:776–85.
11. Feathers JT, Kieffer EC, Palmisano G, et al. The development, implementation, and process evaluation of the REACH Detroit Partnership's Diabetes Lifestyle Intervention. Diabetes Educ 2007;33:509–20.
12. Rahman S, Hu H, McNeely E, et al. Social and environmental risk factors for hypertension in African Americans. Fla Public Health Rev 2008;5:64–72.
13. US Bureau of the Census. Available at www.cityofboston.gov/dnd/PDR/Maps_and_Neighborhood_Profiles.asp.
14. Reid RJ, Coleman K, Johnson EA, Fishman PA, Hsu C, Soman MP, Trescott CE, Erikson M, Larson EB. The Group Health medical home at year two: cost savings, higher patient satisfaction, and less burnout for providers. Health Aff (Millwood) 2010;29:835–43.
15. Fulp RS, McManus KD, Johnson PA. Barriers to purchasing foods for a high-quality, healthy diet in a low-income African American community. Fam Community Health 2009;32:206–17.
16. Fawcett SB, Schultz JA. Supporting participatory evaluation using the Community Tool Box online documentation system. Community-Based Participatory Research for Health. San Francisco: Jossey-Bass; 2008: 419–23.
17. Collie-Akers V, Schultz JA, Carson V, Fawcett SB, Ronan M. REACH 2010: Kansas City, Missouri evaluating mobilization strategies with neighborhood and faith organizations to reduce risk for health disparities. Health Prom Pract 2009;10(Suppl 2):118S–127S.
18. Fawcett SB, Boothroyd R, Schultz JA, Francisco VT, Carson V, Bremby R. Building capacity for participatory evaluation within community initiatives. J Prev Interven Comm 2003;26:21–36.
19. Sepers CE Jr, Fawcett SB, Lipman R, Schultz J, Colie-Akers V, Perez A. Measuring the implementation and effects of a coordinated care model featuring diabetes self-management education within four patient-centered medical homes. Diabetes Educ 2015;41:328–42.
20. Yin RK. Case study research: Design and methods. Sage; 2013.
21. Mead H, Andres E, Regenstein M. Underserved patients' perspectives on patient-centered primary care: does the patient-centered medical home model meet their needs? Med Care Res Rev 2014;71:61–84.
22. Fawcett S, Schultz J, Watson-Thompson J, Fox M, Bremby R. Building multisectoral partnerships for population health and health equity. Prev Chronic Disease 2010;7:A118. Epub 2010 Oct 15.
23. Fixsen DL, Blase KA, Naoom SF, Wallace F. Core implementation components. Res Soc Work Prac 2009; 19:531–540.
24. Cooper JO, Heron TE, Heward WL. Applied behavior analysis. 2nd ed. Pearson; 2007.
25. Glanz K, Bishop DB. The role of behavioral science theory in development and implementation of public health interventions. Annu Rev Public Health 2010;31:399–418.
26. Jack L, Jack NH, Hayes SC. Social determinants of health in minority populations: a call for multidisciplinary approaches to eliminate diabetes-related health disparities. Diabetes Spectrum 2012;25:9–13.
1. Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care 2004;27:1047–53.
2. Centers for Disease Control and Prevention. National diabetes statistics report: estimates of diabetes and its burden in the United States, 2014. Atlanta: U.S. Department of Health and Human Services; 2014.
3. Narayan KM, Boyle JP, Geiss LS, Saaddine JB, Thompson TJ. Impact of recent increase in incidence on future diabetes burden: U.S., 2005-2050. Diabetes Care 2006;29:2114–6.
4. Tang TS, Brown MB, Funnell MM, Anderson RM. Social support, quality of life, and self-care behaviors among African Americans with type 2 diabetes. Diabetes Educ 2008;34:266-76.
5. Crabtree K, Sherrer N, Rushton T, Willig A, Agne A, Shelton T, Cherrington A. Diabetes connect: African American men's preferences for a community-based diabetes management program. Diabetes Educ 2015;41:118-26.
6. Kirk JK, D'Agostino RB Jr, Bell RA, Passmore LV, Bonds DE, Karter AJ, Narayan KM. Disparities in HbA1c levels between African-American and non-Hispanic white adults with diabetes: a meta-analysis. Diabetes Care 2006;29:2130–6.
7. Batts ML, Gary TL, Huss K, Hill MN, Bone L, Brancati FL. Patient priorities and needs for diabetes care among urban African American adults. Diabetes Educ 2001;27:405–12.
8. Horowitz CR, Colson KA, Hebert PL, Lancaster K. Barriers to buying healthy foods for people with diabetes: evidence of environmental disparities. Am J Public Health 2004;94:1549–54.
9. Haas L, Maryniuk M, Beck J, et al; 2012 Standards Revision Task Force. National standards for diabetes self-management education and support. Diabetes Care 2013;36 Suppl 1:S100–8.
10. Cené CW, Haymore LB, Ellis D, Whitaker S, Henderson S, Lin FC, Corbie-Smith G. Implementation of the power to prevent diabetes prevention educational curriculum into rural African American communities: a feasibility study. Diabetes Educ 2013;39:776–85.
11. Feathers JT, Kieffer EC, Palmisano G, et al. The development, implementation, and process evaluation of the REACH Detroit Partnership's Diabetes Lifestyle Intervention. Diabetes Educ 2007;33:509–20.
12. Rahman S, Hu H, McNeely E, et al. Social and environmental risk factors for hypertension in African Americans. Fla Public Health Rev 2008;5:64–72.
13. US Bureau of the Census. Available at www.cityofboston.gov/dnd/PDR/Maps_and_Neighborhood_Profiles.asp.
14. Reid RJ, Coleman K, Johnson EA, Fishman PA, Hsu C, Soman MP, Trescott CE, Erikson M, Larson EB. The Group Health medical home at year two: cost savings, higher patient satisfaction, and less burnout for providers. Health Aff (Millwood) 2010;29:835–43.
15. Fulp RS, McManus KD, Johnson PA. Barriers to purchasing foods for a high-quality, healthy diet in a low-income African American community. Fam Community Health 2009;32:206–17.
16. Fawcett SB, Schultz JA. Supporting participatory evaluation using the Community Tool Box online documentation system. Community-Based Participatory Research for Health. San Francisco: Jossey-Bass; 2008: 419–23.
17. Collie-Akers V, Schultz JA, Carson V, Fawcett SB, Ronan M. REACH 2010: Kansas City, Missouri evaluating mobilization strategies with neighborhood and faith organizations to reduce risk for health disparities. Health Prom Pract 2009;10(Suppl 2):118S–127S.
18. Fawcett SB, Boothroyd R, Schultz JA, Francisco VT, Carson V, Bremby R. Building capacity for participatory evaluation within community initiatives. J Prev Interven Comm 2003;26:21–36.
19. Sepers CE Jr, Fawcett SB, Lipman R, Schultz J, Colie-Akers V, Perez A. Measuring the implementation and effects of a coordinated care model featuring diabetes self-management education within four patient-centered medical homes. Diabetes Educ 2015;41:328–42.
20. Yin RK. Case study research: Design and methods. Sage; 2013.
21. Mead H, Andres E, Regenstein M. Underserved patients' perspectives on patient-centered primary care: does the patient-centered medical home model meet their needs? Med Care Res Rev 2014;71:61–84.
22. Fawcett S, Schultz J, Watson-Thompson J, Fox M, Bremby R. Building multisectoral partnerships for population health and health equity. Prev Chronic Disease 2010;7:A118. Epub 2010 Oct 15.
23. Fixsen DL, Blase KA, Naoom SF, Wallace F. Core implementation components. Res Soc Work Prac 2009; 19:531–540.
24. Cooper JO, Heron TE, Heward WL. Applied behavior analysis. 2nd ed. Pearson; 2007.
25. Glanz K, Bishop DB. The role of behavioral science theory in development and implementation of public health interventions. Annu Rev Public Health 2010;31:399–418.
26. Jack L, Jack NH, Hayes SC. Social determinants of health in minority populations: a call for multidisciplinary approaches to eliminate diabetes-related health disparities. Diabetes Spectrum 2012;25:9–13.