User login
ObGyn’s steady progress toward going green in the OR—but gaps persist
Have you ever looked at the operating room (OR) trash bin at the end of a case and wondered if all that waste is necessary? Since I started my residency, not a day goes by that I have not asked myself this question.
In the mid-1990s, John Elkington introduced the concept of the triple bottom line—that is, people, planet, and profit—for implementation and measurement of sustainability in businesses.1 The health care sector is no exception when it comes to the bottom line! However, “people” remain the priority. What is our role, as ObGyns, in protecting the “planet” while keeping the “people” safe?
According to the World Health Organization (WHO), climate change remains the single biggest health threat to humanity.2 The health care system is both the victim and the culprit. Studies suggest that the health care system, second to the food industry, is the biggest contributor to waste production in the United States. This sector generates more than 6,000 metric tons of waste each day and nearly 4 million tons (3.6 million metric tons) of solid waste each year.3 The health care system is responsible for an estimated 8% to 10% of total greenhouse gas emissions in the United States; the US health care system alone contributes to more than one-fourth of the global health care carbon footprint. If it were a country, the US health care system would rank 13th among all countries in emissions.4In turn, pollution produced by the health sector negatively impacts population health, further burdening the health care system. According to 2013 study data, the annual health damage caused by health care pollution was comparable to that of the deaths caused by preventable medical error.4
Aside from the environmental aspects, hospital waste disposal is expensive; reducing this cost is a potential area of interest for institutions.
As ObGyns, what is our role in reducing our waste generation and carbon footprint while keeping patients safe?
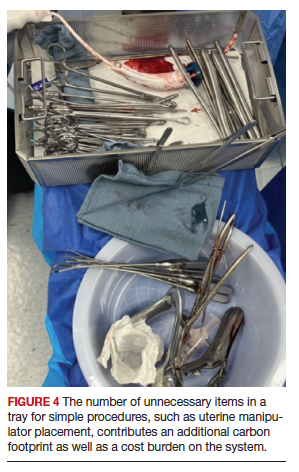
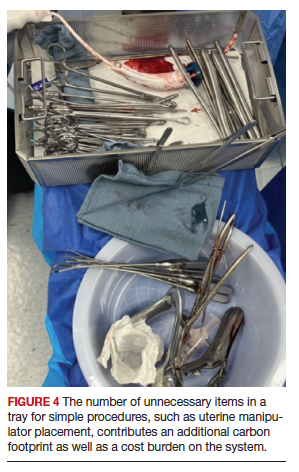
Defining health care waste, and disposal considerations
The WHO defines health care waste as including “the waste generated by health-care establishments, research facilities, and laboratories” as well as waste from scattered sources such as home dialysis and insulin injections.5 Despite representing a relatively small physical area of hospitals, labor and delivery units combined with ORs account for approximately 70% of all hospital waste.3 Operating room waste consists of disposable surgical supplies, personal protective equipment, drapes, plastic wrappers, sterile blue wraps, glass, cardboard, packaging material, medications, fluids, and other materials (FIGURE 1).
The WHO also notes that of all the waste generated by health care activities, about 85% is general, nonhazardous waste that is comparable to domestic waste.6 Hazardous waste is any material that poses a health risk, including potentially infectious materials, such as blood-soaked gauze, sharps, pharmaceuticals, or radioactive materials.6
Disposal of hazardous waste is expensiveand energy consuming as it is typically incinerated rather than disposed of in a landfill. This process produces substantial greenhouse gases, about 3 kg of carbon dioxide for every 1 kg of hazardous waste.7
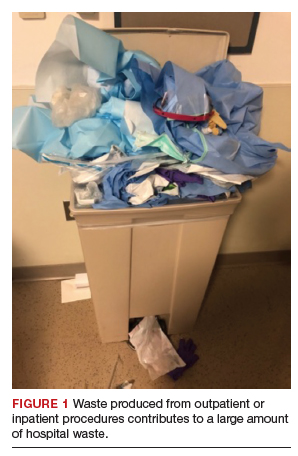
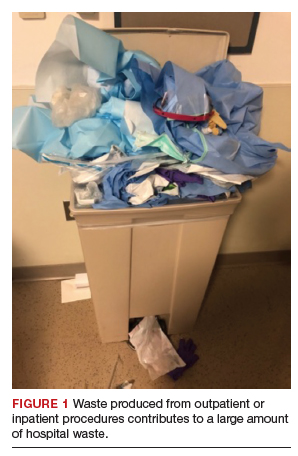
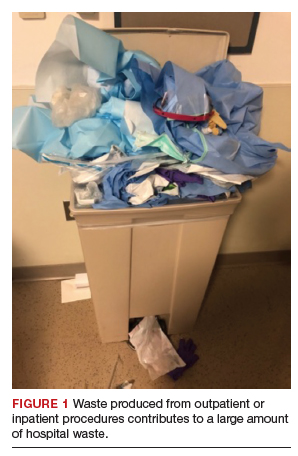
Red bags are used for hazardous waste disposal, while clear bags are used for general waste. Operating rooms produce about two-thirds of the hospital red-bag waste.8 Waste segregation unfortunately is not accurate, and as much as 90% of OR general waste is improperly designated as hazardous waste.3 Drapes and uncontaminated, needleless syringes, for example, should be disposed of in clear bags, but often they are instead directed to the red-bag and sharps container (FIGURE 2).
Obstetrics and gynecology has an important role to play in accurate waste segregation given the specialty’s frequent interaction with bodily fluids. Clinicians and other staff need to recognize and appropriately separate hazardous waste from general waste. For instance, not all fabrics involved in a case should be disposed of in the red bin, only those saturated with blood or body fluids. Educating health care staff and placing instruction posters on the red trash bins potentially could aid in accurate waste segregation and reduce regulated waste while decreasing disposal costs.
Recycling in the OR
Recycling has become an established practice in many health care facilities and ORs. Studies suggest that introducing recycling programs in ORs not only reduces carbon footprints but also reduces costs.3 One study reported that US academic medical centers consume 2 million lb ($15 million) each year of recoverable medical supplies.9
Single-stream recycling, a system in which all recyclable material—including plastics, paper, metal, and glass—are placed in a single bin without segregation at the collection site, has gained in popularity. Recycling can be implemented both in ORs and in other perioperative areas where regular trash bins are located.
In a study done at Oxford University Hospitals in the United Kingdom, introducing recycling bins in every OR, as well as in recovery and staff rest areas, helped improve waste segregation such that approximately 22% of OR waste was recycled.10 Studies show that recycling programs not only decrease the health care carbon footprint but also have a considerable financial impact. Albert and colleagues demonstrated that introducing a single-stream recycling program to a 9-OR day (or ambulatory) surgery center could redirect more than 4 tons of waste each month and saved thousands of dollars.11
Despite continued improvement in recycling programs, the segregation process is still far from optimal. In a survey done at the Mayo Clinic by Azouz and colleagues, more than half of the staff reported being unclear about which OR items are recyclable and nearly half reported that lack of knowledge was the barrier to proper recycling.12 That study also showed that after implementation of a recycling education program, costs decreased 10% relative to the same time period in prior years.12
Blue wraps. One example of recycling optimization is blue wraps, the polypropylene (No. 5 plastic) material used for wrapping surgical instruments. Blue wraps account for approximately 19% of OR waste and 5% of all hospital waste.11 Blue wraps are not biodegradable and also are not widely recycled. In recent years, a resale market has emerged for blue wraps, as they can be used for production of other No. 5 plastic items.9 By reselling blue wraps, revenue can be generated by recycling a necessary packing material that would otherwise require payment for disposal.
Sterility considerations. While recycling in ORs may raise concern due to the absolute sterility required in procedural settings, technologic developments have been promising in advancing safe recycling to reduce carbon footprints and health care costs without compromising patients’ safety. Segregation of waste from recyclable packaging material prior to the case, as well as directing trash to the correct bin (regular vs red bin), is one example. Moreover, because about 80% of all OR waste is generated during the set up before the patient arrives in the OR, it is not contaminated and can be safely recycled.13
Continue to: Packaging material...
Packaging material
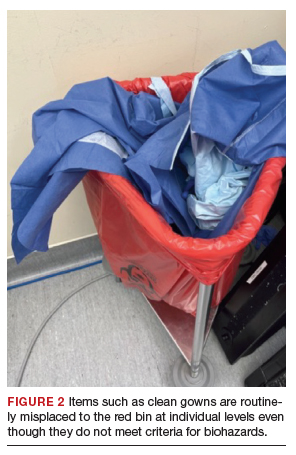
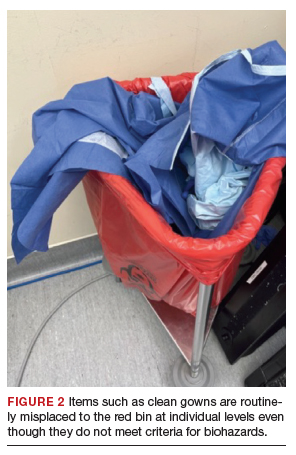
A substantial part of OR waste consists of packaging material; of all OR waste, 26% consists of plastics and 7%, paper and cartons.14 Increasing use of disposable or “single use” medical products in ORs, along with the intention to safeguard sterility, contributes significantly to the generation of medical waste in operating units. Containers, wraps and overwraps, cardboard, and plastic packaging are all composed of materials that when clean, can be recycled; however, these items often end up in the landfill (FIGURE 3).
Although the segregation of packaging material to recycling versus regular trash versus red bin is of paramount importance, packaging design plays a significant role as well. In 2018, Boston Scientific introduced a new packaging design for ureteral stents that reduced plastic use in packaging by 120,000 lb each year.15 Despite the advances in the medical packaging industry to increase sustainability while safeguarding sterility for medical devices, there is still room for innovation in this area.
Reducing overage by judicious selection of surgical devices, instruments, and supplies
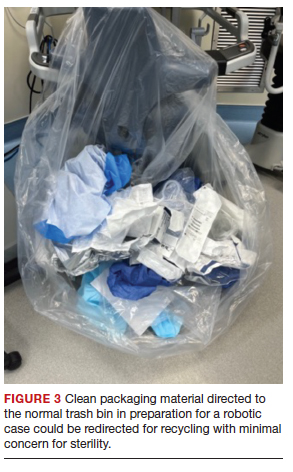
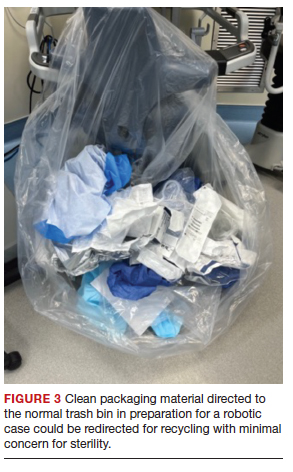
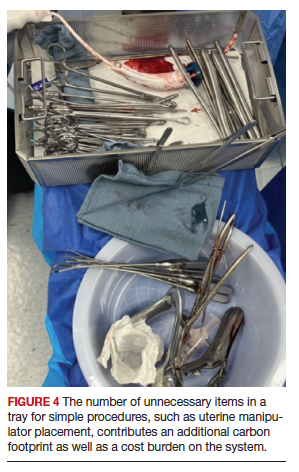
Overage is the term used to describe surgical inventory that is opened and prepared for surgery but ultimately not used and therefore discarded. Design of surgical carts and instrument and supply selection requires direct input from ObGyns. Opening only the needed instruments while ensuring ready availability of potentially needed supplies can significantly reduce OR waste generation as well as decrease chemical pollution generated by instrument sterilization. Decreasing OR overage reduces overall costs as well (FIGURE 4).
In a pilot study at the University of Massachusetts, Albert and colleagues examined the sets of disposable items and instruments designated for common plastic and hand surgery procedures.11 They identified the supplies and instruments that are routinely opened and wasted, based on surgeons’ interview responses, and redesigned the sets. Fifteen items were removed from disposable plastic surgery packs and 7 items from hand surgery packs. The authors reported saving thousands of dollars per year with these changes alone, as well as reducing waste.11 This same concept easily could be implemented in obstetrics and gynecology. We must ask ourselves: Do we always need, for example, a complete dilation and curettage kit to place the uterine manipulator prior to a minimally invasive hysterectomy?
In another pilot study, Greenberg and colleagues investigated whether cesarean deliveries consistently could be performed in a safe manner with only 20 instruments in the surgical kit.16 Obstetricians rated the 20-instrument kit an 8.7 out of 10 for performing cesarean deliveries safely.16
In addition to instrument selection, surgeons have a role in other supply use and waste generation: for instance, opening multiple pairs of surgical gloves and surgical gowns in advance when most of them will not be used during the case. Furthermore, many ObGyn surgeons routinely change gloves or even gowns during gynecologic procedures when they go back and forth between the vaginal and abdominal fields. Is the perineum “dirty” after application of a surgical prep solution?
In an observational study, Shockley and colleagues investigated the type and quantity of bacteria found intraoperatively on the abdomen, vagina, surgical gloves, instrument tips, and uterus at distinct time points during total laparoscopic hysterectomy.17 They showed that in 98.9% of cultures, the overall bacterial concentrations did not exceed the threshold for infection. There was no bacterial growth from vaginal cultures, and the only samples with some bacterial growth belonged to the surgeon’s gloves after specimen extraction; about one-third of samples showed growth after specimen extraction, but only 1 sample had a bacterial load above the infectious threshold of 5,000 colony-forming units per mL. The authors therefore suggested that if a surgeon changes gloves, doing so after specimen extraction and before turning attention back to the abdomen for vaginal cuff closure may be most effective in reducing bacterial load.17
Surgical site infection contributes to medical cost and likely medical waste as well. For example, surgical site infection may require prolonged treatments, tests, and medical instruments. In severe cases with abscesses, treatment entails hospitalization with prolonged antibiotic therapy with or without procedures to drain the collections. Further research therefore is warranted to investigate safe and environmentally friendly practices.
Myriad products are introduced to the medical system each day, some of which replace conventional tools. For instance, low-density polyethylene, or LDPE, transfer sheet is advertised for lateral patient transfer from the OR table to the bed or stretcher. This No. 4–coded plastic, while recyclable, is routinely discarded as trash in ORs. One ergonomic study found that reusable slide boards are as effective for reducing friction and staff muscle activities and are noninferior to the plastic sheets.18
Steps to making an impact
Operating rooms and labor and delivery units are responsible for a large proportion of hospital waste, and therefore they are of paramount importance in reducing waste and carbon footprint at the individual and institutional level. Reduction of OR waste not only is environmentally conscious but also decreases cost. Steps as small as individual practices to as big as changing infrastructures can make an impact. For instance:
- redesigning surgical carts
- reformulating surgeon-specific supply lists
- raising awareness about surgical overage
- encouraging recycling through education and audit
- optimizing surgical waste segregation through educational posters.
These are all simple steps that could significantly reduce waste and carbon footprint.
Bottom line
Although waste reduction is the responsibility of all health care providers, as leaders in their workplace physicians can serve as role models by implementing “green” practices in procedural units. Raising awareness and using a team approach is critical to succeed in our endeavors to move toward an environmentally friendly future. ●
- Elkington J. Towards the sustainable corporation: win-winwin business strategies for sustainable development. Calif Manage Rev. 1994;36:90-100.
- Climate change and health. October 30, 2021. World Health Organization. Accessed October 10, 2022. https://www.who .int/news-room/fact-sheets/detail/climate-change-and -health
- Kwakye G, Brat GA, Makary MA. Green surgical practices for health care. Arch Surg. 2011;146:131-136.
- Eckelman MJ, Sherman J. Environmental impacts of the US health care system and effects on public health. PloS One. 2016;11:e0157014.
- Pruss A, Giroult E, Rushbrook P. Safe management of wastes from health-care activities. World Health Organization; 1999.
- Health-care waste. February 8, 2018. World Health Organization. Accessed October 4, 2022. https://www.who. int/news-room/fact-sheets/detail/health-care-waste2
- Southorn T, Norrish AR, Gardner K, et al. Reducing the carbon footprint of the operating theatre: a multicentre quality improvement report. J Perioper Pract. 2013;23:144-146.
- Greening the OR. Practice Greenhealth. Accessed October 24, 2022. https://practicegreenhealth.org/topics/greening -operating-room/greening-or
- Babu MA, Dalenberg AK, Goodsell G, et al. Greening the operating room: results of a scalable initiative to reduce waste and recover supply costs. Neurosurgery. 2019;85:432-437.
- Oxford University Hospitals NHS Trust. Introducing recycling into the operating theatres. Mapping Greener Healthcare. Accessed October 14, 2022. https://map .sustainablehealthcare.org.uk/oxford-radcliffe-hospitals -nhs-trust/introducing-recycling-operating-theatres
- Albert MG, Rothkopf DM. Operating room waste reduction in plastic and hand surgery. Plast Surg. 2015;23:235-238.
- Azouz S, Boyll P, Swanson M, et al. Managing barriers to recycling in the operating room. Am J Surg. 2019;217:634-638.
- Wyssusek KH, Keys MT, van Zundert AAJ. Operating room greening initiatives—the old, the new, and the way forward: a narrative review. Waste Manag Res. 2019;37:3-19.
- Tieszen ME, Gruenberg JC. A quantitative, qualitative, and critical assessment of surgical waste: surgeons venture through the trash can. JAMA. 1992;267:2765-2768.
- Boston Scientific 2018 Performance Report. Boston Scientific. Accessed November 19, 2022. https://www.bostonscientific. com/content/dam/bostonscientific/corporate/citizenship /sustainability/Boston_Scientific_Performance _Report_2018.pdf
- Greenberg JA, Wylie B, Robinson JN. A pilot study to assess the adequacy of the Brigham 20 Kit for cesarean delivery. Int J Gynaecol Obstet. 2012;117:157-159.
- Shockley ME, Beran B, Nutting H, et al. Sterility of selected operative sites during total laparoscopic hysterectomy. J Minim Invasive Gynecol. 2017;24:990-997.
- Al-Qaisi SK, El Tannir A, Younan LA, et al. An ergonomic assessment of using laterally-tilting operating room tables and friction reducing devices for patient lateral transfers. Appl Ergon. 2020;87:103122.
Have you ever looked at the operating room (OR) trash bin at the end of a case and wondered if all that waste is necessary? Since I started my residency, not a day goes by that I have not asked myself this question.
In the mid-1990s, John Elkington introduced the concept of the triple bottom line—that is, people, planet, and profit—for implementation and measurement of sustainability in businesses.1 The health care sector is no exception when it comes to the bottom line! However, “people” remain the priority. What is our role, as ObGyns, in protecting the “planet” while keeping the “people” safe?
According to the World Health Organization (WHO), climate change remains the single biggest health threat to humanity.2 The health care system is both the victim and the culprit. Studies suggest that the health care system, second to the food industry, is the biggest contributor to waste production in the United States. This sector generates more than 6,000 metric tons of waste each day and nearly 4 million tons (3.6 million metric tons) of solid waste each year.3 The health care system is responsible for an estimated 8% to 10% of total greenhouse gas emissions in the United States; the US health care system alone contributes to more than one-fourth of the global health care carbon footprint. If it were a country, the US health care system would rank 13th among all countries in emissions.4In turn, pollution produced by the health sector negatively impacts population health, further burdening the health care system. According to 2013 study data, the annual health damage caused by health care pollution was comparable to that of the deaths caused by preventable medical error.4
Aside from the environmental aspects, hospital waste disposal is expensive; reducing this cost is a potential area of interest for institutions.
As ObGyns, what is our role in reducing our waste generation and carbon footprint while keeping patients safe?
Defining health care waste, and disposal considerations
The WHO defines health care waste as including “the waste generated by health-care establishments, research facilities, and laboratories” as well as waste from scattered sources such as home dialysis and insulin injections.5 Despite representing a relatively small physical area of hospitals, labor and delivery units combined with ORs account for approximately 70% of all hospital waste.3 Operating room waste consists of disposable surgical supplies, personal protective equipment, drapes, plastic wrappers, sterile blue wraps, glass, cardboard, packaging material, medications, fluids, and other materials (FIGURE 1).
The WHO also notes that of all the waste generated by health care activities, about 85% is general, nonhazardous waste that is comparable to domestic waste.6 Hazardous waste is any material that poses a health risk, including potentially infectious materials, such as blood-soaked gauze, sharps, pharmaceuticals, or radioactive materials.6
Disposal of hazardous waste is expensiveand energy consuming as it is typically incinerated rather than disposed of in a landfill. This process produces substantial greenhouse gases, about 3 kg of carbon dioxide for every 1 kg of hazardous waste.7
Red bags are used for hazardous waste disposal, while clear bags are used for general waste. Operating rooms produce about two-thirds of the hospital red-bag waste.8 Waste segregation unfortunately is not accurate, and as much as 90% of OR general waste is improperly designated as hazardous waste.3 Drapes and uncontaminated, needleless syringes, for example, should be disposed of in clear bags, but often they are instead directed to the red-bag and sharps container (FIGURE 2).
Obstetrics and gynecology has an important role to play in accurate waste segregation given the specialty’s frequent interaction with bodily fluids. Clinicians and other staff need to recognize and appropriately separate hazardous waste from general waste. For instance, not all fabrics involved in a case should be disposed of in the red bin, only those saturated with blood or body fluids. Educating health care staff and placing instruction posters on the red trash bins potentially could aid in accurate waste segregation and reduce regulated waste while decreasing disposal costs.
Recycling in the OR
Recycling has become an established practice in many health care facilities and ORs. Studies suggest that introducing recycling programs in ORs not only reduces carbon footprints but also reduces costs.3 One study reported that US academic medical centers consume 2 million lb ($15 million) each year of recoverable medical supplies.9
Single-stream recycling, a system in which all recyclable material—including plastics, paper, metal, and glass—are placed in a single bin without segregation at the collection site, has gained in popularity. Recycling can be implemented both in ORs and in other perioperative areas where regular trash bins are located.
In a study done at Oxford University Hospitals in the United Kingdom, introducing recycling bins in every OR, as well as in recovery and staff rest areas, helped improve waste segregation such that approximately 22% of OR waste was recycled.10 Studies show that recycling programs not only decrease the health care carbon footprint but also have a considerable financial impact. Albert and colleagues demonstrated that introducing a single-stream recycling program to a 9-OR day (or ambulatory) surgery center could redirect more than 4 tons of waste each month and saved thousands of dollars.11
Despite continued improvement in recycling programs, the segregation process is still far from optimal. In a survey done at the Mayo Clinic by Azouz and colleagues, more than half of the staff reported being unclear about which OR items are recyclable and nearly half reported that lack of knowledge was the barrier to proper recycling.12 That study also showed that after implementation of a recycling education program, costs decreased 10% relative to the same time period in prior years.12
Blue wraps. One example of recycling optimization is blue wraps, the polypropylene (No. 5 plastic) material used for wrapping surgical instruments. Blue wraps account for approximately 19% of OR waste and 5% of all hospital waste.11 Blue wraps are not biodegradable and also are not widely recycled. In recent years, a resale market has emerged for blue wraps, as they can be used for production of other No. 5 plastic items.9 By reselling blue wraps, revenue can be generated by recycling a necessary packing material that would otherwise require payment for disposal.
Sterility considerations. While recycling in ORs may raise concern due to the absolute sterility required in procedural settings, technologic developments have been promising in advancing safe recycling to reduce carbon footprints and health care costs without compromising patients’ safety. Segregation of waste from recyclable packaging material prior to the case, as well as directing trash to the correct bin (regular vs red bin), is one example. Moreover, because about 80% of all OR waste is generated during the set up before the patient arrives in the OR, it is not contaminated and can be safely recycled.13
Continue to: Packaging material...
Packaging material
A substantial part of OR waste consists of packaging material; of all OR waste, 26% consists of plastics and 7%, paper and cartons.14 Increasing use of disposable or “single use” medical products in ORs, along with the intention to safeguard sterility, contributes significantly to the generation of medical waste in operating units. Containers, wraps and overwraps, cardboard, and plastic packaging are all composed of materials that when clean, can be recycled; however, these items often end up in the landfill (FIGURE 3).
Although the segregation of packaging material to recycling versus regular trash versus red bin is of paramount importance, packaging design plays a significant role as well. In 2018, Boston Scientific introduced a new packaging design for ureteral stents that reduced plastic use in packaging by 120,000 lb each year.15 Despite the advances in the medical packaging industry to increase sustainability while safeguarding sterility for medical devices, there is still room for innovation in this area.
Reducing overage by judicious selection of surgical devices, instruments, and supplies
Overage is the term used to describe surgical inventory that is opened and prepared for surgery but ultimately not used and therefore discarded. Design of surgical carts and instrument and supply selection requires direct input from ObGyns. Opening only the needed instruments while ensuring ready availability of potentially needed supplies can significantly reduce OR waste generation as well as decrease chemical pollution generated by instrument sterilization. Decreasing OR overage reduces overall costs as well (FIGURE 4).
In a pilot study at the University of Massachusetts, Albert and colleagues examined the sets of disposable items and instruments designated for common plastic and hand surgery procedures.11 They identified the supplies and instruments that are routinely opened and wasted, based on surgeons’ interview responses, and redesigned the sets. Fifteen items were removed from disposable plastic surgery packs and 7 items from hand surgery packs. The authors reported saving thousands of dollars per year with these changes alone, as well as reducing waste.11 This same concept easily could be implemented in obstetrics and gynecology. We must ask ourselves: Do we always need, for example, a complete dilation and curettage kit to place the uterine manipulator prior to a minimally invasive hysterectomy?
In another pilot study, Greenberg and colleagues investigated whether cesarean deliveries consistently could be performed in a safe manner with only 20 instruments in the surgical kit.16 Obstetricians rated the 20-instrument kit an 8.7 out of 10 for performing cesarean deliveries safely.16
In addition to instrument selection, surgeons have a role in other supply use and waste generation: for instance, opening multiple pairs of surgical gloves and surgical gowns in advance when most of them will not be used during the case. Furthermore, many ObGyn surgeons routinely change gloves or even gowns during gynecologic procedures when they go back and forth between the vaginal and abdominal fields. Is the perineum “dirty” after application of a surgical prep solution?
In an observational study, Shockley and colleagues investigated the type and quantity of bacteria found intraoperatively on the abdomen, vagina, surgical gloves, instrument tips, and uterus at distinct time points during total laparoscopic hysterectomy.17 They showed that in 98.9% of cultures, the overall bacterial concentrations did not exceed the threshold for infection. There was no bacterial growth from vaginal cultures, and the only samples with some bacterial growth belonged to the surgeon’s gloves after specimen extraction; about one-third of samples showed growth after specimen extraction, but only 1 sample had a bacterial load above the infectious threshold of 5,000 colony-forming units per mL. The authors therefore suggested that if a surgeon changes gloves, doing so after specimen extraction and before turning attention back to the abdomen for vaginal cuff closure may be most effective in reducing bacterial load.17
Surgical site infection contributes to medical cost and likely medical waste as well. For example, surgical site infection may require prolonged treatments, tests, and medical instruments. In severe cases with abscesses, treatment entails hospitalization with prolonged antibiotic therapy with or without procedures to drain the collections. Further research therefore is warranted to investigate safe and environmentally friendly practices.
Myriad products are introduced to the medical system each day, some of which replace conventional tools. For instance, low-density polyethylene, or LDPE, transfer sheet is advertised for lateral patient transfer from the OR table to the bed or stretcher. This No. 4–coded plastic, while recyclable, is routinely discarded as trash in ORs. One ergonomic study found that reusable slide boards are as effective for reducing friction and staff muscle activities and are noninferior to the plastic sheets.18
Steps to making an impact
Operating rooms and labor and delivery units are responsible for a large proportion of hospital waste, and therefore they are of paramount importance in reducing waste and carbon footprint at the individual and institutional level. Reduction of OR waste not only is environmentally conscious but also decreases cost. Steps as small as individual practices to as big as changing infrastructures can make an impact. For instance:
- redesigning surgical carts
- reformulating surgeon-specific supply lists
- raising awareness about surgical overage
- encouraging recycling through education and audit
- optimizing surgical waste segregation through educational posters.
These are all simple steps that could significantly reduce waste and carbon footprint.
Bottom line
Although waste reduction is the responsibility of all health care providers, as leaders in their workplace physicians can serve as role models by implementing “green” practices in procedural units. Raising awareness and using a team approach is critical to succeed in our endeavors to move toward an environmentally friendly future. ●
Have you ever looked at the operating room (OR) trash bin at the end of a case and wondered if all that waste is necessary? Since I started my residency, not a day goes by that I have not asked myself this question.
In the mid-1990s, John Elkington introduced the concept of the triple bottom line—that is, people, planet, and profit—for implementation and measurement of sustainability in businesses.1 The health care sector is no exception when it comes to the bottom line! However, “people” remain the priority. What is our role, as ObGyns, in protecting the “planet” while keeping the “people” safe?
According to the World Health Organization (WHO), climate change remains the single biggest health threat to humanity.2 The health care system is both the victim and the culprit. Studies suggest that the health care system, second to the food industry, is the biggest contributor to waste production in the United States. This sector generates more than 6,000 metric tons of waste each day and nearly 4 million tons (3.6 million metric tons) of solid waste each year.3 The health care system is responsible for an estimated 8% to 10% of total greenhouse gas emissions in the United States; the US health care system alone contributes to more than one-fourth of the global health care carbon footprint. If it were a country, the US health care system would rank 13th among all countries in emissions.4In turn, pollution produced by the health sector negatively impacts population health, further burdening the health care system. According to 2013 study data, the annual health damage caused by health care pollution was comparable to that of the deaths caused by preventable medical error.4
Aside from the environmental aspects, hospital waste disposal is expensive; reducing this cost is a potential area of interest for institutions.
As ObGyns, what is our role in reducing our waste generation and carbon footprint while keeping patients safe?
Defining health care waste, and disposal considerations
The WHO defines health care waste as including “the waste generated by health-care establishments, research facilities, and laboratories” as well as waste from scattered sources such as home dialysis and insulin injections.5 Despite representing a relatively small physical area of hospitals, labor and delivery units combined with ORs account for approximately 70% of all hospital waste.3 Operating room waste consists of disposable surgical supplies, personal protective equipment, drapes, plastic wrappers, sterile blue wraps, glass, cardboard, packaging material, medications, fluids, and other materials (FIGURE 1).
The WHO also notes that of all the waste generated by health care activities, about 85% is general, nonhazardous waste that is comparable to domestic waste.6 Hazardous waste is any material that poses a health risk, including potentially infectious materials, such as blood-soaked gauze, sharps, pharmaceuticals, or radioactive materials.6
Disposal of hazardous waste is expensiveand energy consuming as it is typically incinerated rather than disposed of in a landfill. This process produces substantial greenhouse gases, about 3 kg of carbon dioxide for every 1 kg of hazardous waste.7
Red bags are used for hazardous waste disposal, while clear bags are used for general waste. Operating rooms produce about two-thirds of the hospital red-bag waste.8 Waste segregation unfortunately is not accurate, and as much as 90% of OR general waste is improperly designated as hazardous waste.3 Drapes and uncontaminated, needleless syringes, for example, should be disposed of in clear bags, but often they are instead directed to the red-bag and sharps container (FIGURE 2).
Obstetrics and gynecology has an important role to play in accurate waste segregation given the specialty’s frequent interaction with bodily fluids. Clinicians and other staff need to recognize and appropriately separate hazardous waste from general waste. For instance, not all fabrics involved in a case should be disposed of in the red bin, only those saturated with blood or body fluids. Educating health care staff and placing instruction posters on the red trash bins potentially could aid in accurate waste segregation and reduce regulated waste while decreasing disposal costs.
Recycling in the OR
Recycling has become an established practice in many health care facilities and ORs. Studies suggest that introducing recycling programs in ORs not only reduces carbon footprints but also reduces costs.3 One study reported that US academic medical centers consume 2 million lb ($15 million) each year of recoverable medical supplies.9
Single-stream recycling, a system in which all recyclable material—including plastics, paper, metal, and glass—are placed in a single bin without segregation at the collection site, has gained in popularity. Recycling can be implemented both in ORs and in other perioperative areas where regular trash bins are located.
In a study done at Oxford University Hospitals in the United Kingdom, introducing recycling bins in every OR, as well as in recovery and staff rest areas, helped improve waste segregation such that approximately 22% of OR waste was recycled.10 Studies show that recycling programs not only decrease the health care carbon footprint but also have a considerable financial impact. Albert and colleagues demonstrated that introducing a single-stream recycling program to a 9-OR day (or ambulatory) surgery center could redirect more than 4 tons of waste each month and saved thousands of dollars.11
Despite continued improvement in recycling programs, the segregation process is still far from optimal. In a survey done at the Mayo Clinic by Azouz and colleagues, more than half of the staff reported being unclear about which OR items are recyclable and nearly half reported that lack of knowledge was the barrier to proper recycling.12 That study also showed that after implementation of a recycling education program, costs decreased 10% relative to the same time period in prior years.12
Blue wraps. One example of recycling optimization is blue wraps, the polypropylene (No. 5 plastic) material used for wrapping surgical instruments. Blue wraps account for approximately 19% of OR waste and 5% of all hospital waste.11 Blue wraps are not biodegradable and also are not widely recycled. In recent years, a resale market has emerged for blue wraps, as they can be used for production of other No. 5 plastic items.9 By reselling blue wraps, revenue can be generated by recycling a necessary packing material that would otherwise require payment for disposal.
Sterility considerations. While recycling in ORs may raise concern due to the absolute sterility required in procedural settings, technologic developments have been promising in advancing safe recycling to reduce carbon footprints and health care costs without compromising patients’ safety. Segregation of waste from recyclable packaging material prior to the case, as well as directing trash to the correct bin (regular vs red bin), is one example. Moreover, because about 80% of all OR waste is generated during the set up before the patient arrives in the OR, it is not contaminated and can be safely recycled.13
Continue to: Packaging material...
Packaging material
A substantial part of OR waste consists of packaging material; of all OR waste, 26% consists of plastics and 7%, paper and cartons.14 Increasing use of disposable or “single use” medical products in ORs, along with the intention to safeguard sterility, contributes significantly to the generation of medical waste in operating units. Containers, wraps and overwraps, cardboard, and plastic packaging are all composed of materials that when clean, can be recycled; however, these items often end up in the landfill (FIGURE 3).
Although the segregation of packaging material to recycling versus regular trash versus red bin is of paramount importance, packaging design plays a significant role as well. In 2018, Boston Scientific introduced a new packaging design for ureteral stents that reduced plastic use in packaging by 120,000 lb each year.15 Despite the advances in the medical packaging industry to increase sustainability while safeguarding sterility for medical devices, there is still room for innovation in this area.
Reducing overage by judicious selection of surgical devices, instruments, and supplies
Overage is the term used to describe surgical inventory that is opened and prepared for surgery but ultimately not used and therefore discarded. Design of surgical carts and instrument and supply selection requires direct input from ObGyns. Opening only the needed instruments while ensuring ready availability of potentially needed supplies can significantly reduce OR waste generation as well as decrease chemical pollution generated by instrument sterilization. Decreasing OR overage reduces overall costs as well (FIGURE 4).
In a pilot study at the University of Massachusetts, Albert and colleagues examined the sets of disposable items and instruments designated for common plastic and hand surgery procedures.11 They identified the supplies and instruments that are routinely opened and wasted, based on surgeons’ interview responses, and redesigned the sets. Fifteen items were removed from disposable plastic surgery packs and 7 items from hand surgery packs. The authors reported saving thousands of dollars per year with these changes alone, as well as reducing waste.11 This same concept easily could be implemented in obstetrics and gynecology. We must ask ourselves: Do we always need, for example, a complete dilation and curettage kit to place the uterine manipulator prior to a minimally invasive hysterectomy?
In another pilot study, Greenberg and colleagues investigated whether cesarean deliveries consistently could be performed in a safe manner with only 20 instruments in the surgical kit.16 Obstetricians rated the 20-instrument kit an 8.7 out of 10 for performing cesarean deliveries safely.16
In addition to instrument selection, surgeons have a role in other supply use and waste generation: for instance, opening multiple pairs of surgical gloves and surgical gowns in advance when most of them will not be used during the case. Furthermore, many ObGyn surgeons routinely change gloves or even gowns during gynecologic procedures when they go back and forth between the vaginal and abdominal fields. Is the perineum “dirty” after application of a surgical prep solution?
In an observational study, Shockley and colleagues investigated the type and quantity of bacteria found intraoperatively on the abdomen, vagina, surgical gloves, instrument tips, and uterus at distinct time points during total laparoscopic hysterectomy.17 They showed that in 98.9% of cultures, the overall bacterial concentrations did not exceed the threshold for infection. There was no bacterial growth from vaginal cultures, and the only samples with some bacterial growth belonged to the surgeon’s gloves after specimen extraction; about one-third of samples showed growth after specimen extraction, but only 1 sample had a bacterial load above the infectious threshold of 5,000 colony-forming units per mL. The authors therefore suggested that if a surgeon changes gloves, doing so after specimen extraction and before turning attention back to the abdomen for vaginal cuff closure may be most effective in reducing bacterial load.17
Surgical site infection contributes to medical cost and likely medical waste as well. For example, surgical site infection may require prolonged treatments, tests, and medical instruments. In severe cases with abscesses, treatment entails hospitalization with prolonged antibiotic therapy with or without procedures to drain the collections. Further research therefore is warranted to investigate safe and environmentally friendly practices.
Myriad products are introduced to the medical system each day, some of which replace conventional tools. For instance, low-density polyethylene, or LDPE, transfer sheet is advertised for lateral patient transfer from the OR table to the bed or stretcher. This No. 4–coded plastic, while recyclable, is routinely discarded as trash in ORs. One ergonomic study found that reusable slide boards are as effective for reducing friction and staff muscle activities and are noninferior to the plastic sheets.18
Steps to making an impact
Operating rooms and labor and delivery units are responsible for a large proportion of hospital waste, and therefore they are of paramount importance in reducing waste and carbon footprint at the individual and institutional level. Reduction of OR waste not only is environmentally conscious but also decreases cost. Steps as small as individual practices to as big as changing infrastructures can make an impact. For instance:
- redesigning surgical carts
- reformulating surgeon-specific supply lists
- raising awareness about surgical overage
- encouraging recycling through education and audit
- optimizing surgical waste segregation through educational posters.
These are all simple steps that could significantly reduce waste and carbon footprint.
Bottom line
Although waste reduction is the responsibility of all health care providers, as leaders in their workplace physicians can serve as role models by implementing “green” practices in procedural units. Raising awareness and using a team approach is critical to succeed in our endeavors to move toward an environmentally friendly future. ●
- Elkington J. Towards the sustainable corporation: win-winwin business strategies for sustainable development. Calif Manage Rev. 1994;36:90-100.
- Climate change and health. October 30, 2021. World Health Organization. Accessed October 10, 2022. https://www.who .int/news-room/fact-sheets/detail/climate-change-and -health
- Kwakye G, Brat GA, Makary MA. Green surgical practices for health care. Arch Surg. 2011;146:131-136.
- Eckelman MJ, Sherman J. Environmental impacts of the US health care system and effects on public health. PloS One. 2016;11:e0157014.
- Pruss A, Giroult E, Rushbrook P. Safe management of wastes from health-care activities. World Health Organization; 1999.
- Health-care waste. February 8, 2018. World Health Organization. Accessed October 4, 2022. https://www.who. int/news-room/fact-sheets/detail/health-care-waste2
- Southorn T, Norrish AR, Gardner K, et al. Reducing the carbon footprint of the operating theatre: a multicentre quality improvement report. J Perioper Pract. 2013;23:144-146.
- Greening the OR. Practice Greenhealth. Accessed October 24, 2022. https://practicegreenhealth.org/topics/greening -operating-room/greening-or
- Babu MA, Dalenberg AK, Goodsell G, et al. Greening the operating room: results of a scalable initiative to reduce waste and recover supply costs. Neurosurgery. 2019;85:432-437.
- Oxford University Hospitals NHS Trust. Introducing recycling into the operating theatres. Mapping Greener Healthcare. Accessed October 14, 2022. https://map .sustainablehealthcare.org.uk/oxford-radcliffe-hospitals -nhs-trust/introducing-recycling-operating-theatres
- Albert MG, Rothkopf DM. Operating room waste reduction in plastic and hand surgery. Plast Surg. 2015;23:235-238.
- Azouz S, Boyll P, Swanson M, et al. Managing barriers to recycling in the operating room. Am J Surg. 2019;217:634-638.
- Wyssusek KH, Keys MT, van Zundert AAJ. Operating room greening initiatives—the old, the new, and the way forward: a narrative review. Waste Manag Res. 2019;37:3-19.
- Tieszen ME, Gruenberg JC. A quantitative, qualitative, and critical assessment of surgical waste: surgeons venture through the trash can. JAMA. 1992;267:2765-2768.
- Boston Scientific 2018 Performance Report. Boston Scientific. Accessed November 19, 2022. https://www.bostonscientific. com/content/dam/bostonscientific/corporate/citizenship /sustainability/Boston_Scientific_Performance _Report_2018.pdf
- Greenberg JA, Wylie B, Robinson JN. A pilot study to assess the adequacy of the Brigham 20 Kit for cesarean delivery. Int J Gynaecol Obstet. 2012;117:157-159.
- Shockley ME, Beran B, Nutting H, et al. Sterility of selected operative sites during total laparoscopic hysterectomy. J Minim Invasive Gynecol. 2017;24:990-997.
- Al-Qaisi SK, El Tannir A, Younan LA, et al. An ergonomic assessment of using laterally-tilting operating room tables and friction reducing devices for patient lateral transfers. Appl Ergon. 2020;87:103122.
- Elkington J. Towards the sustainable corporation: win-winwin business strategies for sustainable development. Calif Manage Rev. 1994;36:90-100.
- Climate change and health. October 30, 2021. World Health Organization. Accessed October 10, 2022. https://www.who .int/news-room/fact-sheets/detail/climate-change-and -health
- Kwakye G, Brat GA, Makary MA. Green surgical practices for health care. Arch Surg. 2011;146:131-136.
- Eckelman MJ, Sherman J. Environmental impacts of the US health care system and effects on public health. PloS One. 2016;11:e0157014.
- Pruss A, Giroult E, Rushbrook P. Safe management of wastes from health-care activities. World Health Organization; 1999.
- Health-care waste. February 8, 2018. World Health Organization. Accessed October 4, 2022. https://www.who. int/news-room/fact-sheets/detail/health-care-waste2
- Southorn T, Norrish AR, Gardner K, et al. Reducing the carbon footprint of the operating theatre: a multicentre quality improvement report. J Perioper Pract. 2013;23:144-146.
- Greening the OR. Practice Greenhealth. Accessed October 24, 2022. https://practicegreenhealth.org/topics/greening -operating-room/greening-or
- Babu MA, Dalenberg AK, Goodsell G, et al. Greening the operating room: results of a scalable initiative to reduce waste and recover supply costs. Neurosurgery. 2019;85:432-437.
- Oxford University Hospitals NHS Trust. Introducing recycling into the operating theatres. Mapping Greener Healthcare. Accessed October 14, 2022. https://map .sustainablehealthcare.org.uk/oxford-radcliffe-hospitals -nhs-trust/introducing-recycling-operating-theatres
- Albert MG, Rothkopf DM. Operating room waste reduction in plastic and hand surgery. Plast Surg. 2015;23:235-238.
- Azouz S, Boyll P, Swanson M, et al. Managing barriers to recycling in the operating room. Am J Surg. 2019;217:634-638.
- Wyssusek KH, Keys MT, van Zundert AAJ. Operating room greening initiatives—the old, the new, and the way forward: a narrative review. Waste Manag Res. 2019;37:3-19.
- Tieszen ME, Gruenberg JC. A quantitative, qualitative, and critical assessment of surgical waste: surgeons venture through the trash can. JAMA. 1992;267:2765-2768.
- Boston Scientific 2018 Performance Report. Boston Scientific. Accessed November 19, 2022. https://www.bostonscientific. com/content/dam/bostonscientific/corporate/citizenship /sustainability/Boston_Scientific_Performance _Report_2018.pdf
- Greenberg JA, Wylie B, Robinson JN. A pilot study to assess the adequacy of the Brigham 20 Kit for cesarean delivery. Int J Gynaecol Obstet. 2012;117:157-159.
- Shockley ME, Beran B, Nutting H, et al. Sterility of selected operative sites during total laparoscopic hysterectomy. J Minim Invasive Gynecol. 2017;24:990-997.
- Al-Qaisi SK, El Tannir A, Younan LA, et al. An ergonomic assessment of using laterally-tilting operating room tables and friction reducing devices for patient lateral transfers. Appl Ergon. 2020;87:103122.