User login
A cheaper, faster way to resolve chronic cough
- When evaluating chronic cough, consider a trial of therapy aimed at the most likely presumptive diagnosis for your locality.
- In developing algorithms such as ours, take into account your experiences, patient characteristics, and the available medical equipment.
At the insistence of her family, a woman comes to you complaining of a cough that has lasted several weeks. Many experts would urge a thorough diagnostic investigation, justifying this action with a presumed shorter course of treatment. But is an involved work-up really necessary? Would a quicker, less expensive approach serve the patient just as well? We designed our study to answer these questions.
“Test all, then treat” is expensive
In the management of patients with chronic cough, most algorithms have advocated the approach of “test all, then treat.”1-6 This is an expensive approach and one that delays relief for the patient, though a confirmative diagnosis may decrease the overall duration of treatment. In most cases, however, this approach may be unnecessary. And because few of the underlying disorders are acutely debilitating or rapidly progressive, even misdiagnosis and resultant inappropriate treatment pose little risk to patients.
The less common approach is a sequence of trial-and-error treatments based on a presumptive hierarchy of possible diagnoses.6 The advantage with this strategy is a 3-to 5-fold cost savings.6 And we suspected that the associated length of treatment would be acceptable.
We proposed that the management of patients with chronic cough begin with a presumptive diagnosis, thus simplifying the initial evaluation, keeping costs low, and offering earlier treatment.
We developed an algorithm for the treatment of patients with chronic cough that relies on minimal diagnostic investigations, regardless of the confirmed diagnosis. We evaluated our approach from the perspectives of the presumptive diagnosis and the therapeutic response period.
Methods
Treatment algorithm reflects experience and local resources
Initially, we designed the algorithm to follow findings in the literature on the treatment of patients with chronic cough. We then simplified and modified the algorithm to reflect the experiences of doctors from the pulmonology clinic in our hospital, and to take into account local patient characteristics and available medical equipment and resources.
For this study, we defined chronic cough as a one that lasts more than 4 weeks. (This definition can vary, depending on the source you consult.1) the patients we enrolled had no abnormalities detected on auscultation, chest radiography, or CBC.
Chronic cough can be managed successfully by accurate treatment of the cause, and most specialists report high success rates in treating it.2-4 The 3 most common causes of chronic cough are 1) postnasal drip, 2) asthma, and 3) gastroesophageal reflux.5
Subjects were otherwise healthy
Between January 1 and December 31, 2005, at the internal medicine clinic of Cheju National University Hospital, we enrolled 378 patients whose chief complaint was cough persisting for more than 4 weeks and who had no abnormalities detected on auscultation by a physician, chest radiography (posterior–anterior view and left lateral view), or complete blood cell counts. Each patient had a complete blood count to detect anemia, hematologic disorders, or inflammatory conditions. Current users of angiotensin-converting enzyme (ACE) inhibitors were excluded.
All of the patients we enrolled were adults living in Jeju, Korea, and the mean age was 51 years. One hundred eighty-six (49%) were men. The median reported cough duration was 2 months (range, 1–36 months) (TABLE 1).
We instructed the patients on our algorithmic approach to treating chronic cough and encouraged them to follow the algorithm through to telephone notification of the next visit.
TABLE 1
Characteristics of the 378 enrolled patients
| Men/women | 186/192 (49/51%) |
| Age, years | 51.2±16.12 |
| Cough duration in months, median (range) | 2 (1–36) |
How we determined treatment outcomes
Patients graded their cough severity subjectively at each visit using a visual analogue scale (VAS) from 1 (no cough at all) to 10 (cough severity same as that remembered during first visit to the clinic). We recorded their reports on a questionnaire.
Successful responders were patients who reported a subjective grade of cough severity less than 3. Partial responders and nonresponders were defined, respectively, as those reporting VAS scores from 3 to 6 and more than 6.
We defined the response period as the number of days from enrollment until the next visit in which the patient first reported a VAS score of cough severity less than 3.
Algorithm: Addressing the 3 most common causes of chronic cough
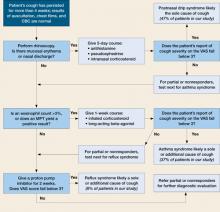
1. Postnasal drip syndrome. Patients first underwent a rhinoscopic examination (FIGURE). When clinicians detected redness or abnormal discharge on the nasal mucosa, they prescribed a 5-day course of antihistamine (10 mg/day ebastine [Ebastel] orally), pseudoephedrine (30 mg 3 times daily, orally), and intranasal corticosteroid (triamcinolone acetonide [Nasacort] 110 mcg twice daily intranasally). Patients without symptoms of rhinitis were referred to the next diagnostic phase.
With completion of the prescribed medication 5 days after the first visit, we graded the severity of cough by questionnaire. Patients in the successful and partial responder categories received a presumptive diagnosis of postnasal drip syndrome, and we asked them to continue using the medication for at least 2 weeks. We had each nonresponder stop the medication.
2. Asthma syndrome. Partial responder and nonresponder patients entered the next diagnostic phase: a methacholine bronchial provocation test (MPT)7 and eosinophil count with induced sputum by hypertonic saline (3% NaCl).8 We defined a positive MPT result as <10 mg/ mL of methacholine causing a 20% fall in FEV1 from baseline (PC20). Patients with more than 3% eosinophils in the induced sputum specimen or with a positive MPT received a 1-week prescription for inhaled budesonide 160 mcg twice daily and inhaled formoterol (Symbicort) 4.5 mcg twice daily. Patients who did not exhibit these asthma indicators were referred to the next step.
At the next visit, we again graded the severity of cough. Patients in the successful and partial responder categories received a presumptive diagnosis of asthma syndrome. We asked successful and partial responders to continue the medication for at least 2 weeks. Those classed as nonresponders were asked to stop their medication. We referred all patients with positive MPT test results to a special clinic for asthma, regardless of responses to this therapeutic trial or eosinophil count in the induced sputum.
3. Reflux syndrome. Partial responders and nonresponders then received a 2-week prescription for a proton pump inhibitor, pantoprazole (Pantoloc), 40 mg orally once daily.9 At the next visit 2 weeks later, we graded the severity of cough. Successful and partial responders were given a presumptive diagnosis of reflux syndrome, but only successful responders were asked to continue the same medication for at least 6 weeks. At the discretion of their physicians, partial and nonresponders underwent other diagnostic investigations, including high-resolution computerized tomography (CT) of the lungs, bronchoscopic examination, sputum smear and culture for acid fast bacilli, sputum culture for ordinary bacteria and fungi, and a serological test for human immunodeficiency virus.
FIGURE
A presumptive-diagnosis algorithm
Chronic cough resolved for more than 90% of patients treated according to this algorithm.
MPT, methacholine bronchial provocation test; VAS, visual analog scale.
Results
Presumptive diagnoses
Among 378 patients, 346 (91%) showed erythematous mucosa or abnormal discharge in rhinoscopic examinations and received empiric medication for 5 days. The successful-responder category included 176 patients (47%); 79 (21%) were classed as partial responders, and 255 (67%) received the presumptive diagnosis of postnasal drip syndrome. Among the 346 treated patients, 91 (24% of those enrolled, or 26% of treated) showed no response.
Thirty-two patients with normal rhinoscopic findings and 170 categorized as partial or nonresponders in the first step underwent an MPT and eosinophil count of induced sputum. One hundred forty-four showed positive results and received empiric treatment for 1 week. Among these, 141 were deemed successful responders (37% of enrolled, or 98% of treated), 3 partial responders (1% of enrolled, or 2% of treated), and none were nonresponders.
In all, 61 patients had empiric treatment for reflux syndrome for 2 weeks; 58 had normal findings for both the MPT and sputum eosinophil count, and 3 were classified as partial responders in the previous therapeutic trial. Twenty-nine patients (8% of enrolled, or 47% of treated) were classified as successful responders after 2 weeks (TABLE 2).
TABLE 2
Presumptive diagnoses corresponded to expected frequency (and occasionally co-existed)
| DIAGNOSIS | NO. OF PATIENTS (%)* N=378 |
| Postnasal drip syndrome | 255 (67.5) |
| Asthma syndrome | 144 (38.1) |
| Reflux syndrome | 29 (7.7) |
| CO-EXISTING PATHOLOGIES | 82 (21.7) |
| Postnasal drip syndrome and asthma syndrome | 52 (13.8) |
| Postnasal drip syndrome and reflux syndrome | 7 (1.9) |
| Postnasal drip syndrome and other diagnosis | 20 (5.3) |
| Asthma syndrome and other diagnosis | 3 (0.8) |
| * The percentage of patients under "Diagnosis" does not add up to 100% because some patients had more than one condition, accounted for under "Co-existing pathologies." | |
Therapeutic response period for successful responders
Within 5 days of beginning the course determined by the algorithm (Figure), 176 patients (47%) who received treatment for presumed postnasal drip syndrome experienced resolution of their chronic cough.
Another 141 patients (37%) diagnosed with asthma syndrome (with or without postnasal drip syndrome) reported cough resolution following successful treatment between 7 and 12 days.
Another 29 patients (8%) with re-flux syndrome were successfully treated between 14 and 26 days.
Treatment of chronic cough by the algorithm
After application of the therapeutic algorithm, the chronic cough of 346 patients (92%) resolved. Thirty-two patients (8.5%) underwent other diagnostic investigations.
Final diagnoses after further diagnostic testing
Ten patients reported that they stopped coughing spontaneously while awaiting additional diagnostic investigations. Seven patients had mycobacterial infections confirmed by acid fast bacilli smears or culture of sputum or bronchoscopic washings. Six patients had localized or diffuse bronchiectasis confirmed by high-resolution CT, the results of which were used retrospectively to reassess normal or equivocal findings in the initial diagnostic investigations. Finally, the coughs of 12 patients were judged to be idiopathic or psychogenic.
Discussion
Cough is a symptom not easily assessed objectively. Previous studies measured severity of cough with daily diaries and visual analog scales, which are subjective measurement tools. We, too, used the visual analog scale to measure cough severity and treatment response. We did not pursue a definitive diagnosis of the cause of chronic cough. Rather, our algorithmic approach made presumptive diagnoses that were confirmed or refuted by patients’ successive reports of cough severity in response to treatment.
The logic behind our algorithm
Because studies in Korea have shown that postnasal drip is the most frequent cause of chronic cough, we chose rhinoscopy as the first diagnostic investigation. The second and third steps of our approach investigated asthma syndrome and reflux syndrome, respectively.
We did not take into account whether patients smoked cigarettes. Some investigators rightly point out that smoking might contribute to chronic cough. However, we have not met many smokers willing to quit because of a cough, and our algorithm is designed for practical clinical use. In contrast, patients with chronic cough secondary to ACE inhibitor therapy have readily accepted trials of different antihypertensive medications.
Our assumptions proved true
Patients with any abnormality of the nasal mucosa were treated for postnasal drip syndrome. Though the proportion of abnormal mucosal findings was greater than that reported in previous investigations of the same ethnic subjects, the eventual treatment response showed that the presumptive diagnosis of postnasal drip was equivalent to that in other studies.10,11
Postnasal drip syndrome did indeed turn out to be the most common presumptive cause of cough in our study. However, roughly one third of these patients proved to have an additional presumptive disorder. Previous investigations have also reported dual or multiple pathologies in patients with a chronic cough.11,12
If treatment succeeded at any step in our algorithm, we asked patients to stop taking medication—with the exception of those who had positive results on methacholine bronchial provocation test. Asthma is a chronic inflammatory disorder that needs persistent therapy to prevent exacerbations and declining lung function.13,14 Challenge studies with methacholine or histamine are sensitive tests and provide high negative predictive values for the diagnosis of asthma and cough variant asthma.15,16
What have other studies shown?
The natural course of chronic cough is still in question, primarily because of the heterogeneity of its etiology. The natural course of many common diseases has been investigated, of course, but few studies have focused on duration of symptoms such as cough. Park et al17 investigated the natural course of eosinophilic bronchitis, a common underlying disorder in chronic cough. In a 48-month follow-up of 36 patients diagnosed with eosinophilic bronchitis, 14% experienced recurrence after treatment. And patients with a higher percentage of eosinophils in the sputum had a risk for developing airway hyperresponsiveness.
Ours et al9 reported that, for patients without asthma or postnasal drip, an empiric 2-week trial of high-dose proton pump inhibitors was more reliable and cost effective for chronic cough than was treatment after esophageal manometry or 24 hours dual probe pH monitoring. Besides the expense of manometry and pH monitoring, both procedures are invasive and unavailable in many localities such as ours. Our algorithm supposes, for one thing, minimum availability of medical equipment in many locales.
The algorithm makes sense
Our approach decreased medical expenses and therapeutic response periods. Cough resolved for more than 90% of our patients. This success rate was equivalent to that reported by previous studies, most of which revealed no definitive diagnosis during the therapeutic response period.2-4,18 Half of all patients in our study experienced cough resolution within 5 days, and more than 80% did so within 12 days.
Development of algorithms similar to ours should take into account not just findings in the literature but the experiences of local doctors and available medical equipment and options.
1. Janson C, Chinn S, Jarvis D, Burney P. Determinants of cough in young adults participating in the European Community Respiratory Health Survey. Eur Resp J 2001;18:647-654.
2. Irwin RS, Carrao WM, Pratter MR. Chronic persistent cough in the adult: the spectrum and frequency of causes and successful outcome of specific therapy. Am Rev Respir Dis 1981;123:413-417.
3. Poe RH, Israel RH, Utell MJ, Hall WJ. Chronic cough: bronchoscopy or pulmonary function testing? Am Rev Respir Dis 1982;126:160-162.
4. Irwin RS, Curley FJ, French CL. Chronic cough. The spectrum and frequency of causes, key components of the diagnostic evaluation, and the outcome of specific therapy. Am Rev Respir Dis 1990;141:640-647.
5. Palombini BC, Villanova CA, Araujo E, et al. A pathogenic triad in chronic cough: asthma, postnasal drip syndrome and gastroesophageal reflux disease. Chest 1999;116:279-284.
6. Morice AH, Fontana GA, Sovijarvi ARA, et al. The diagnosis and management of chronic cough. Eur Respir J 2004;24:481-492.
7. Chatham M, Bleecker ER, Norman P, Smith PL, Mason P. A screening test for airways reactivity. An abbreviated methacholine inhalation challenge. Chest 1982;82:15-18.
8. Jang A, Lee J, Park S, et al. Factors influencing the responsiveness to inhaled glucocorticoids in patients with moderate to severe asthma. Korean J Asthma Allergy Clin Immunol 2005;25:175-180.
9. Ours TM, Kavuru MS, Schilz RJ, Richter JE. A prospective evaluation of esophageal testing and a double-blind randomized study of omeprazole in a diagnostic and therapeutic algorithm for chronic cough. Am J Gastroenterol 1999;94:3131-3138.
10. Cho JH, Ryu JS, Lee HL. Chronic cough: the spectrum and the frequency of etiologies. Tuberc Respir Dis 1999;46:555-563.
11. Jeon G, Jang SH, Song HG, et al. Diagnostic performance of routine objective tests and cost-effective approach for chronic cough. Tuberc Respir Dis 2004;57:535-542.
12. Smyrnios NA, Irwin RS, Curley FJ. Chronic cough with a history of excessive sputum production. The spectrum and frequency of causes, key components of the diagnostic evaluation, and outcome of specific therapy. Chest 1995;108:991-997.
13. Global Initiative for Asthma. Global strategy for asthma management and prevention. NHLBI/WHO workshop report. Bethesda, Md: National Heart, Lung and Blood Institute;2004.
14. James AL, Palmer LJ, Kicic E, et al. Decline in lung function in the Busselton Health Study: the effects of asthma and cigarette smoking. Am J Respir Crit Care Med 2005;171:109-114.
15. Fish JE, Peters SP. Bronchial challenge testing. Middleton’s Allergy Principles and Practice. 6th ed. St Louis, Mo: Mosby, Inc; 2003;657-670.
16. Dicpinigaitis PV. Chronic cough due to asthma: ACCP evidence-based clinical practice guidelines. Chest 2006;129:75S-79S
17. Park JK, Park SW, Lee JH, et al. Evaluation of clinical course in patients with eosinophilic bronchitis: A prospective follow up study. J Asthma Allergy Clin Immunol 2003;23:740-748.
18. Simpson G. Investigation and management of persistent dry cough. Thorax 1999;54:469-470.
- When evaluating chronic cough, consider a trial of therapy aimed at the most likely presumptive diagnosis for your locality.
- In developing algorithms such as ours, take into account your experiences, patient characteristics, and the available medical equipment.
At the insistence of her family, a woman comes to you complaining of a cough that has lasted several weeks. Many experts would urge a thorough diagnostic investigation, justifying this action with a presumed shorter course of treatment. But is an involved work-up really necessary? Would a quicker, less expensive approach serve the patient just as well? We designed our study to answer these questions.
“Test all, then treat” is expensive
In the management of patients with chronic cough, most algorithms have advocated the approach of “test all, then treat.”1-6 This is an expensive approach and one that delays relief for the patient, though a confirmative diagnosis may decrease the overall duration of treatment. In most cases, however, this approach may be unnecessary. And because few of the underlying disorders are acutely debilitating or rapidly progressive, even misdiagnosis and resultant inappropriate treatment pose little risk to patients.
The less common approach is a sequence of trial-and-error treatments based on a presumptive hierarchy of possible diagnoses.6 The advantage with this strategy is a 3-to 5-fold cost savings.6 And we suspected that the associated length of treatment would be acceptable.
We proposed that the management of patients with chronic cough begin with a presumptive diagnosis, thus simplifying the initial evaluation, keeping costs low, and offering earlier treatment.
We developed an algorithm for the treatment of patients with chronic cough that relies on minimal diagnostic investigations, regardless of the confirmed diagnosis. We evaluated our approach from the perspectives of the presumptive diagnosis and the therapeutic response period.
Methods
Treatment algorithm reflects experience and local resources
Initially, we designed the algorithm to follow findings in the literature on the treatment of patients with chronic cough. We then simplified and modified the algorithm to reflect the experiences of doctors from the pulmonology clinic in our hospital, and to take into account local patient characteristics and available medical equipment and resources.
For this study, we defined chronic cough as a one that lasts more than 4 weeks. (This definition can vary, depending on the source you consult.1) the patients we enrolled had no abnormalities detected on auscultation, chest radiography, or CBC.
Chronic cough can be managed successfully by accurate treatment of the cause, and most specialists report high success rates in treating it.2-4 The 3 most common causes of chronic cough are 1) postnasal drip, 2) asthma, and 3) gastroesophageal reflux.5
Subjects were otherwise healthy
Between January 1 and December 31, 2005, at the internal medicine clinic of Cheju National University Hospital, we enrolled 378 patients whose chief complaint was cough persisting for more than 4 weeks and who had no abnormalities detected on auscultation by a physician, chest radiography (posterior–anterior view and left lateral view), or complete blood cell counts. Each patient had a complete blood count to detect anemia, hematologic disorders, or inflammatory conditions. Current users of angiotensin-converting enzyme (ACE) inhibitors were excluded.
All of the patients we enrolled were adults living in Jeju, Korea, and the mean age was 51 years. One hundred eighty-six (49%) were men. The median reported cough duration was 2 months (range, 1–36 months) (TABLE 1).
We instructed the patients on our algorithmic approach to treating chronic cough and encouraged them to follow the algorithm through to telephone notification of the next visit.
TABLE 1
Characteristics of the 378 enrolled patients
| Men/women | 186/192 (49/51%) |
| Age, years | 51.2±16.12 |
| Cough duration in months, median (range) | 2 (1–36) |
How we determined treatment outcomes
Patients graded their cough severity subjectively at each visit using a visual analogue scale (VAS) from 1 (no cough at all) to 10 (cough severity same as that remembered during first visit to the clinic). We recorded their reports on a questionnaire.
Successful responders were patients who reported a subjective grade of cough severity less than 3. Partial responders and nonresponders were defined, respectively, as those reporting VAS scores from 3 to 6 and more than 6.
We defined the response period as the number of days from enrollment until the next visit in which the patient first reported a VAS score of cough severity less than 3.
Algorithm: Addressing the 3 most common causes of chronic cough
1. Postnasal drip syndrome. Patients first underwent a rhinoscopic examination (FIGURE). When clinicians detected redness or abnormal discharge on the nasal mucosa, they prescribed a 5-day course of antihistamine (10 mg/day ebastine [Ebastel] orally), pseudoephedrine (30 mg 3 times daily, orally), and intranasal corticosteroid (triamcinolone acetonide [Nasacort] 110 mcg twice daily intranasally). Patients without symptoms of rhinitis were referred to the next diagnostic phase.
With completion of the prescribed medication 5 days after the first visit, we graded the severity of cough by questionnaire. Patients in the successful and partial responder categories received a presumptive diagnosis of postnasal drip syndrome, and we asked them to continue using the medication for at least 2 weeks. We had each nonresponder stop the medication.
2. Asthma syndrome. Partial responder and nonresponder patients entered the next diagnostic phase: a methacholine bronchial provocation test (MPT)7 and eosinophil count with induced sputum by hypertonic saline (3% NaCl).8 We defined a positive MPT result as <10 mg/ mL of methacholine causing a 20% fall in FEV1 from baseline (PC20). Patients with more than 3% eosinophils in the induced sputum specimen or with a positive MPT received a 1-week prescription for inhaled budesonide 160 mcg twice daily and inhaled formoterol (Symbicort) 4.5 mcg twice daily. Patients who did not exhibit these asthma indicators were referred to the next step.
At the next visit, we again graded the severity of cough. Patients in the successful and partial responder categories received a presumptive diagnosis of asthma syndrome. We asked successful and partial responders to continue the medication for at least 2 weeks. Those classed as nonresponders were asked to stop their medication. We referred all patients with positive MPT test results to a special clinic for asthma, regardless of responses to this therapeutic trial or eosinophil count in the induced sputum.
3. Reflux syndrome. Partial responders and nonresponders then received a 2-week prescription for a proton pump inhibitor, pantoprazole (Pantoloc), 40 mg orally once daily.9 At the next visit 2 weeks later, we graded the severity of cough. Successful and partial responders were given a presumptive diagnosis of reflux syndrome, but only successful responders were asked to continue the same medication for at least 6 weeks. At the discretion of their physicians, partial and nonresponders underwent other diagnostic investigations, including high-resolution computerized tomography (CT) of the lungs, bronchoscopic examination, sputum smear and culture for acid fast bacilli, sputum culture for ordinary bacteria and fungi, and a serological test for human immunodeficiency virus.
FIGURE
A presumptive-diagnosis algorithm
Chronic cough resolved for more than 90% of patients treated according to this algorithm.
MPT, methacholine bronchial provocation test; VAS, visual analog scale.
Results
Presumptive diagnoses
Among 378 patients, 346 (91%) showed erythematous mucosa or abnormal discharge in rhinoscopic examinations and received empiric medication for 5 days. The successful-responder category included 176 patients (47%); 79 (21%) were classed as partial responders, and 255 (67%) received the presumptive diagnosis of postnasal drip syndrome. Among the 346 treated patients, 91 (24% of those enrolled, or 26% of treated) showed no response.
Thirty-two patients with normal rhinoscopic findings and 170 categorized as partial or nonresponders in the first step underwent an MPT and eosinophil count of induced sputum. One hundred forty-four showed positive results and received empiric treatment for 1 week. Among these, 141 were deemed successful responders (37% of enrolled, or 98% of treated), 3 partial responders (1% of enrolled, or 2% of treated), and none were nonresponders.
In all, 61 patients had empiric treatment for reflux syndrome for 2 weeks; 58 had normal findings for both the MPT and sputum eosinophil count, and 3 were classified as partial responders in the previous therapeutic trial. Twenty-nine patients (8% of enrolled, or 47% of treated) were classified as successful responders after 2 weeks (TABLE 2).
TABLE 2
Presumptive diagnoses corresponded to expected frequency (and occasionally co-existed)
| DIAGNOSIS | NO. OF PATIENTS (%)* N=378 |
| Postnasal drip syndrome | 255 (67.5) |
| Asthma syndrome | 144 (38.1) |
| Reflux syndrome | 29 (7.7) |
| CO-EXISTING PATHOLOGIES | 82 (21.7) |
| Postnasal drip syndrome and asthma syndrome | 52 (13.8) |
| Postnasal drip syndrome and reflux syndrome | 7 (1.9) |
| Postnasal drip syndrome and other diagnosis | 20 (5.3) |
| Asthma syndrome and other diagnosis | 3 (0.8) |
| * The percentage of patients under "Diagnosis" does not add up to 100% because some patients had more than one condition, accounted for under "Co-existing pathologies." | |
Therapeutic response period for successful responders
Within 5 days of beginning the course determined by the algorithm (Figure), 176 patients (47%) who received treatment for presumed postnasal drip syndrome experienced resolution of their chronic cough.
Another 141 patients (37%) diagnosed with asthma syndrome (with or without postnasal drip syndrome) reported cough resolution following successful treatment between 7 and 12 days.
Another 29 patients (8%) with re-flux syndrome were successfully treated between 14 and 26 days.
Treatment of chronic cough by the algorithm
After application of the therapeutic algorithm, the chronic cough of 346 patients (92%) resolved. Thirty-two patients (8.5%) underwent other diagnostic investigations.
Final diagnoses after further diagnostic testing
Ten patients reported that they stopped coughing spontaneously while awaiting additional diagnostic investigations. Seven patients had mycobacterial infections confirmed by acid fast bacilli smears or culture of sputum or bronchoscopic washings. Six patients had localized or diffuse bronchiectasis confirmed by high-resolution CT, the results of which were used retrospectively to reassess normal or equivocal findings in the initial diagnostic investigations. Finally, the coughs of 12 patients were judged to be idiopathic or psychogenic.
Discussion
Cough is a symptom not easily assessed objectively. Previous studies measured severity of cough with daily diaries and visual analog scales, which are subjective measurement tools. We, too, used the visual analog scale to measure cough severity and treatment response. We did not pursue a definitive diagnosis of the cause of chronic cough. Rather, our algorithmic approach made presumptive diagnoses that were confirmed or refuted by patients’ successive reports of cough severity in response to treatment.
The logic behind our algorithm
Because studies in Korea have shown that postnasal drip is the most frequent cause of chronic cough, we chose rhinoscopy as the first diagnostic investigation. The second and third steps of our approach investigated asthma syndrome and reflux syndrome, respectively.
We did not take into account whether patients smoked cigarettes. Some investigators rightly point out that smoking might contribute to chronic cough. However, we have not met many smokers willing to quit because of a cough, and our algorithm is designed for practical clinical use. In contrast, patients with chronic cough secondary to ACE inhibitor therapy have readily accepted trials of different antihypertensive medications.
Our assumptions proved true
Patients with any abnormality of the nasal mucosa were treated for postnasal drip syndrome. Though the proportion of abnormal mucosal findings was greater than that reported in previous investigations of the same ethnic subjects, the eventual treatment response showed that the presumptive diagnosis of postnasal drip was equivalent to that in other studies.10,11
Postnasal drip syndrome did indeed turn out to be the most common presumptive cause of cough in our study. However, roughly one third of these patients proved to have an additional presumptive disorder. Previous investigations have also reported dual or multiple pathologies in patients with a chronic cough.11,12
If treatment succeeded at any step in our algorithm, we asked patients to stop taking medication—with the exception of those who had positive results on methacholine bronchial provocation test. Asthma is a chronic inflammatory disorder that needs persistent therapy to prevent exacerbations and declining lung function.13,14 Challenge studies with methacholine or histamine are sensitive tests and provide high negative predictive values for the diagnosis of asthma and cough variant asthma.15,16
What have other studies shown?
The natural course of chronic cough is still in question, primarily because of the heterogeneity of its etiology. The natural course of many common diseases has been investigated, of course, but few studies have focused on duration of symptoms such as cough. Park et al17 investigated the natural course of eosinophilic bronchitis, a common underlying disorder in chronic cough. In a 48-month follow-up of 36 patients diagnosed with eosinophilic bronchitis, 14% experienced recurrence after treatment. And patients with a higher percentage of eosinophils in the sputum had a risk for developing airway hyperresponsiveness.
Ours et al9 reported that, for patients without asthma or postnasal drip, an empiric 2-week trial of high-dose proton pump inhibitors was more reliable and cost effective for chronic cough than was treatment after esophageal manometry or 24 hours dual probe pH monitoring. Besides the expense of manometry and pH monitoring, both procedures are invasive and unavailable in many localities such as ours. Our algorithm supposes, for one thing, minimum availability of medical equipment in many locales.
The algorithm makes sense
Our approach decreased medical expenses and therapeutic response periods. Cough resolved for more than 90% of our patients. This success rate was equivalent to that reported by previous studies, most of which revealed no definitive diagnosis during the therapeutic response period.2-4,18 Half of all patients in our study experienced cough resolution within 5 days, and more than 80% did so within 12 days.
Development of algorithms similar to ours should take into account not just findings in the literature but the experiences of local doctors and available medical equipment and options.
- When evaluating chronic cough, consider a trial of therapy aimed at the most likely presumptive diagnosis for your locality.
- In developing algorithms such as ours, take into account your experiences, patient characteristics, and the available medical equipment.
At the insistence of her family, a woman comes to you complaining of a cough that has lasted several weeks. Many experts would urge a thorough diagnostic investigation, justifying this action with a presumed shorter course of treatment. But is an involved work-up really necessary? Would a quicker, less expensive approach serve the patient just as well? We designed our study to answer these questions.
“Test all, then treat” is expensive
In the management of patients with chronic cough, most algorithms have advocated the approach of “test all, then treat.”1-6 This is an expensive approach and one that delays relief for the patient, though a confirmative diagnosis may decrease the overall duration of treatment. In most cases, however, this approach may be unnecessary. And because few of the underlying disorders are acutely debilitating or rapidly progressive, even misdiagnosis and resultant inappropriate treatment pose little risk to patients.
The less common approach is a sequence of trial-and-error treatments based on a presumptive hierarchy of possible diagnoses.6 The advantage with this strategy is a 3-to 5-fold cost savings.6 And we suspected that the associated length of treatment would be acceptable.
We proposed that the management of patients with chronic cough begin with a presumptive diagnosis, thus simplifying the initial evaluation, keeping costs low, and offering earlier treatment.
We developed an algorithm for the treatment of patients with chronic cough that relies on minimal diagnostic investigations, regardless of the confirmed diagnosis. We evaluated our approach from the perspectives of the presumptive diagnosis and the therapeutic response period.
Methods
Treatment algorithm reflects experience and local resources
Initially, we designed the algorithm to follow findings in the literature on the treatment of patients with chronic cough. We then simplified and modified the algorithm to reflect the experiences of doctors from the pulmonology clinic in our hospital, and to take into account local patient characteristics and available medical equipment and resources.
For this study, we defined chronic cough as a one that lasts more than 4 weeks. (This definition can vary, depending on the source you consult.1) the patients we enrolled had no abnormalities detected on auscultation, chest radiography, or CBC.
Chronic cough can be managed successfully by accurate treatment of the cause, and most specialists report high success rates in treating it.2-4 The 3 most common causes of chronic cough are 1) postnasal drip, 2) asthma, and 3) gastroesophageal reflux.5
Subjects were otherwise healthy
Between January 1 and December 31, 2005, at the internal medicine clinic of Cheju National University Hospital, we enrolled 378 patients whose chief complaint was cough persisting for more than 4 weeks and who had no abnormalities detected on auscultation by a physician, chest radiography (posterior–anterior view and left lateral view), or complete blood cell counts. Each patient had a complete blood count to detect anemia, hematologic disorders, or inflammatory conditions. Current users of angiotensin-converting enzyme (ACE) inhibitors were excluded.
All of the patients we enrolled were adults living in Jeju, Korea, and the mean age was 51 years. One hundred eighty-six (49%) were men. The median reported cough duration was 2 months (range, 1–36 months) (TABLE 1).
We instructed the patients on our algorithmic approach to treating chronic cough and encouraged them to follow the algorithm through to telephone notification of the next visit.
TABLE 1
Characteristics of the 378 enrolled patients
| Men/women | 186/192 (49/51%) |
| Age, years | 51.2±16.12 |
| Cough duration in months, median (range) | 2 (1–36) |
How we determined treatment outcomes
Patients graded their cough severity subjectively at each visit using a visual analogue scale (VAS) from 1 (no cough at all) to 10 (cough severity same as that remembered during first visit to the clinic). We recorded their reports on a questionnaire.
Successful responders were patients who reported a subjective grade of cough severity less than 3. Partial responders and nonresponders were defined, respectively, as those reporting VAS scores from 3 to 6 and more than 6.
We defined the response period as the number of days from enrollment until the next visit in which the patient first reported a VAS score of cough severity less than 3.
Algorithm: Addressing the 3 most common causes of chronic cough
1. Postnasal drip syndrome. Patients first underwent a rhinoscopic examination (FIGURE). When clinicians detected redness or abnormal discharge on the nasal mucosa, they prescribed a 5-day course of antihistamine (10 mg/day ebastine [Ebastel] orally), pseudoephedrine (30 mg 3 times daily, orally), and intranasal corticosteroid (triamcinolone acetonide [Nasacort] 110 mcg twice daily intranasally). Patients without symptoms of rhinitis were referred to the next diagnostic phase.
With completion of the prescribed medication 5 days after the first visit, we graded the severity of cough by questionnaire. Patients in the successful and partial responder categories received a presumptive diagnosis of postnasal drip syndrome, and we asked them to continue using the medication for at least 2 weeks. We had each nonresponder stop the medication.
2. Asthma syndrome. Partial responder and nonresponder patients entered the next diagnostic phase: a methacholine bronchial provocation test (MPT)7 and eosinophil count with induced sputum by hypertonic saline (3% NaCl).8 We defined a positive MPT result as <10 mg/ mL of methacholine causing a 20% fall in FEV1 from baseline (PC20). Patients with more than 3% eosinophils in the induced sputum specimen or with a positive MPT received a 1-week prescription for inhaled budesonide 160 mcg twice daily and inhaled formoterol (Symbicort) 4.5 mcg twice daily. Patients who did not exhibit these asthma indicators were referred to the next step.
At the next visit, we again graded the severity of cough. Patients in the successful and partial responder categories received a presumptive diagnosis of asthma syndrome. We asked successful and partial responders to continue the medication for at least 2 weeks. Those classed as nonresponders were asked to stop their medication. We referred all patients with positive MPT test results to a special clinic for asthma, regardless of responses to this therapeutic trial or eosinophil count in the induced sputum.
3. Reflux syndrome. Partial responders and nonresponders then received a 2-week prescription for a proton pump inhibitor, pantoprazole (Pantoloc), 40 mg orally once daily.9 At the next visit 2 weeks later, we graded the severity of cough. Successful and partial responders were given a presumptive diagnosis of reflux syndrome, but only successful responders were asked to continue the same medication for at least 6 weeks. At the discretion of their physicians, partial and nonresponders underwent other diagnostic investigations, including high-resolution computerized tomography (CT) of the lungs, bronchoscopic examination, sputum smear and culture for acid fast bacilli, sputum culture for ordinary bacteria and fungi, and a serological test for human immunodeficiency virus.
FIGURE
A presumptive-diagnosis algorithm
Chronic cough resolved for more than 90% of patients treated according to this algorithm.
MPT, methacholine bronchial provocation test; VAS, visual analog scale.
Results
Presumptive diagnoses
Among 378 patients, 346 (91%) showed erythematous mucosa or abnormal discharge in rhinoscopic examinations and received empiric medication for 5 days. The successful-responder category included 176 patients (47%); 79 (21%) were classed as partial responders, and 255 (67%) received the presumptive diagnosis of postnasal drip syndrome. Among the 346 treated patients, 91 (24% of those enrolled, or 26% of treated) showed no response.
Thirty-two patients with normal rhinoscopic findings and 170 categorized as partial or nonresponders in the first step underwent an MPT and eosinophil count of induced sputum. One hundred forty-four showed positive results and received empiric treatment for 1 week. Among these, 141 were deemed successful responders (37% of enrolled, or 98% of treated), 3 partial responders (1% of enrolled, or 2% of treated), and none were nonresponders.
In all, 61 patients had empiric treatment for reflux syndrome for 2 weeks; 58 had normal findings for both the MPT and sputum eosinophil count, and 3 were classified as partial responders in the previous therapeutic trial. Twenty-nine patients (8% of enrolled, or 47% of treated) were classified as successful responders after 2 weeks (TABLE 2).
TABLE 2
Presumptive diagnoses corresponded to expected frequency (and occasionally co-existed)
| DIAGNOSIS | NO. OF PATIENTS (%)* N=378 |
| Postnasal drip syndrome | 255 (67.5) |
| Asthma syndrome | 144 (38.1) |
| Reflux syndrome | 29 (7.7) |
| CO-EXISTING PATHOLOGIES | 82 (21.7) |
| Postnasal drip syndrome and asthma syndrome | 52 (13.8) |
| Postnasal drip syndrome and reflux syndrome | 7 (1.9) |
| Postnasal drip syndrome and other diagnosis | 20 (5.3) |
| Asthma syndrome and other diagnosis | 3 (0.8) |
| * The percentage of patients under "Diagnosis" does not add up to 100% because some patients had more than one condition, accounted for under "Co-existing pathologies." | |
Therapeutic response period for successful responders
Within 5 days of beginning the course determined by the algorithm (Figure), 176 patients (47%) who received treatment for presumed postnasal drip syndrome experienced resolution of their chronic cough.
Another 141 patients (37%) diagnosed with asthma syndrome (with or without postnasal drip syndrome) reported cough resolution following successful treatment between 7 and 12 days.
Another 29 patients (8%) with re-flux syndrome were successfully treated between 14 and 26 days.
Treatment of chronic cough by the algorithm
After application of the therapeutic algorithm, the chronic cough of 346 patients (92%) resolved. Thirty-two patients (8.5%) underwent other diagnostic investigations.
Final diagnoses after further diagnostic testing
Ten patients reported that they stopped coughing spontaneously while awaiting additional diagnostic investigations. Seven patients had mycobacterial infections confirmed by acid fast bacilli smears or culture of sputum or bronchoscopic washings. Six patients had localized or diffuse bronchiectasis confirmed by high-resolution CT, the results of which were used retrospectively to reassess normal or equivocal findings in the initial diagnostic investigations. Finally, the coughs of 12 patients were judged to be idiopathic or psychogenic.
Discussion
Cough is a symptom not easily assessed objectively. Previous studies measured severity of cough with daily diaries and visual analog scales, which are subjective measurement tools. We, too, used the visual analog scale to measure cough severity and treatment response. We did not pursue a definitive diagnosis of the cause of chronic cough. Rather, our algorithmic approach made presumptive diagnoses that were confirmed or refuted by patients’ successive reports of cough severity in response to treatment.
The logic behind our algorithm
Because studies in Korea have shown that postnasal drip is the most frequent cause of chronic cough, we chose rhinoscopy as the first diagnostic investigation. The second and third steps of our approach investigated asthma syndrome and reflux syndrome, respectively.
We did not take into account whether patients smoked cigarettes. Some investigators rightly point out that smoking might contribute to chronic cough. However, we have not met many smokers willing to quit because of a cough, and our algorithm is designed for practical clinical use. In contrast, patients with chronic cough secondary to ACE inhibitor therapy have readily accepted trials of different antihypertensive medications.
Our assumptions proved true
Patients with any abnormality of the nasal mucosa were treated for postnasal drip syndrome. Though the proportion of abnormal mucosal findings was greater than that reported in previous investigations of the same ethnic subjects, the eventual treatment response showed that the presumptive diagnosis of postnasal drip was equivalent to that in other studies.10,11
Postnasal drip syndrome did indeed turn out to be the most common presumptive cause of cough in our study. However, roughly one third of these patients proved to have an additional presumptive disorder. Previous investigations have also reported dual or multiple pathologies in patients with a chronic cough.11,12
If treatment succeeded at any step in our algorithm, we asked patients to stop taking medication—with the exception of those who had positive results on methacholine bronchial provocation test. Asthma is a chronic inflammatory disorder that needs persistent therapy to prevent exacerbations and declining lung function.13,14 Challenge studies with methacholine or histamine are sensitive tests and provide high negative predictive values for the diagnosis of asthma and cough variant asthma.15,16
What have other studies shown?
The natural course of chronic cough is still in question, primarily because of the heterogeneity of its etiology. The natural course of many common diseases has been investigated, of course, but few studies have focused on duration of symptoms such as cough. Park et al17 investigated the natural course of eosinophilic bronchitis, a common underlying disorder in chronic cough. In a 48-month follow-up of 36 patients diagnosed with eosinophilic bronchitis, 14% experienced recurrence after treatment. And patients with a higher percentage of eosinophils in the sputum had a risk for developing airway hyperresponsiveness.
Ours et al9 reported that, for patients without asthma or postnasal drip, an empiric 2-week trial of high-dose proton pump inhibitors was more reliable and cost effective for chronic cough than was treatment after esophageal manometry or 24 hours dual probe pH monitoring. Besides the expense of manometry and pH monitoring, both procedures are invasive and unavailable in many localities such as ours. Our algorithm supposes, for one thing, minimum availability of medical equipment in many locales.
The algorithm makes sense
Our approach decreased medical expenses and therapeutic response periods. Cough resolved for more than 90% of our patients. This success rate was equivalent to that reported by previous studies, most of which revealed no definitive diagnosis during the therapeutic response period.2-4,18 Half of all patients in our study experienced cough resolution within 5 days, and more than 80% did so within 12 days.
Development of algorithms similar to ours should take into account not just findings in the literature but the experiences of local doctors and available medical equipment and options.
1. Janson C, Chinn S, Jarvis D, Burney P. Determinants of cough in young adults participating in the European Community Respiratory Health Survey. Eur Resp J 2001;18:647-654.
2. Irwin RS, Carrao WM, Pratter MR. Chronic persistent cough in the adult: the spectrum and frequency of causes and successful outcome of specific therapy. Am Rev Respir Dis 1981;123:413-417.
3. Poe RH, Israel RH, Utell MJ, Hall WJ. Chronic cough: bronchoscopy or pulmonary function testing? Am Rev Respir Dis 1982;126:160-162.
4. Irwin RS, Curley FJ, French CL. Chronic cough. The spectrum and frequency of causes, key components of the diagnostic evaluation, and the outcome of specific therapy. Am Rev Respir Dis 1990;141:640-647.
5. Palombini BC, Villanova CA, Araujo E, et al. A pathogenic triad in chronic cough: asthma, postnasal drip syndrome and gastroesophageal reflux disease. Chest 1999;116:279-284.
6. Morice AH, Fontana GA, Sovijarvi ARA, et al. The diagnosis and management of chronic cough. Eur Respir J 2004;24:481-492.
7. Chatham M, Bleecker ER, Norman P, Smith PL, Mason P. A screening test for airways reactivity. An abbreviated methacholine inhalation challenge. Chest 1982;82:15-18.
8. Jang A, Lee J, Park S, et al. Factors influencing the responsiveness to inhaled glucocorticoids in patients with moderate to severe asthma. Korean J Asthma Allergy Clin Immunol 2005;25:175-180.
9. Ours TM, Kavuru MS, Schilz RJ, Richter JE. A prospective evaluation of esophageal testing and a double-blind randomized study of omeprazole in a diagnostic and therapeutic algorithm for chronic cough. Am J Gastroenterol 1999;94:3131-3138.
10. Cho JH, Ryu JS, Lee HL. Chronic cough: the spectrum and the frequency of etiologies. Tuberc Respir Dis 1999;46:555-563.
11. Jeon G, Jang SH, Song HG, et al. Diagnostic performance of routine objective tests and cost-effective approach for chronic cough. Tuberc Respir Dis 2004;57:535-542.
12. Smyrnios NA, Irwin RS, Curley FJ. Chronic cough with a history of excessive sputum production. The spectrum and frequency of causes, key components of the diagnostic evaluation, and outcome of specific therapy. Chest 1995;108:991-997.
13. Global Initiative for Asthma. Global strategy for asthma management and prevention. NHLBI/WHO workshop report. Bethesda, Md: National Heart, Lung and Blood Institute;2004.
14. James AL, Palmer LJ, Kicic E, et al. Decline in lung function in the Busselton Health Study: the effects of asthma and cigarette smoking. Am J Respir Crit Care Med 2005;171:109-114.
15. Fish JE, Peters SP. Bronchial challenge testing. Middleton’s Allergy Principles and Practice. 6th ed. St Louis, Mo: Mosby, Inc; 2003;657-670.
16. Dicpinigaitis PV. Chronic cough due to asthma: ACCP evidence-based clinical practice guidelines. Chest 2006;129:75S-79S
17. Park JK, Park SW, Lee JH, et al. Evaluation of clinical course in patients with eosinophilic bronchitis: A prospective follow up study. J Asthma Allergy Clin Immunol 2003;23:740-748.
18. Simpson G. Investigation and management of persistent dry cough. Thorax 1999;54:469-470.
1. Janson C, Chinn S, Jarvis D, Burney P. Determinants of cough in young adults participating in the European Community Respiratory Health Survey. Eur Resp J 2001;18:647-654.
2. Irwin RS, Carrao WM, Pratter MR. Chronic persistent cough in the adult: the spectrum and frequency of causes and successful outcome of specific therapy. Am Rev Respir Dis 1981;123:413-417.
3. Poe RH, Israel RH, Utell MJ, Hall WJ. Chronic cough: bronchoscopy or pulmonary function testing? Am Rev Respir Dis 1982;126:160-162.
4. Irwin RS, Curley FJ, French CL. Chronic cough. The spectrum and frequency of causes, key components of the diagnostic evaluation, and the outcome of specific therapy. Am Rev Respir Dis 1990;141:640-647.
5. Palombini BC, Villanova CA, Araujo E, et al. A pathogenic triad in chronic cough: asthma, postnasal drip syndrome and gastroesophageal reflux disease. Chest 1999;116:279-284.
6. Morice AH, Fontana GA, Sovijarvi ARA, et al. The diagnosis and management of chronic cough. Eur Respir J 2004;24:481-492.
7. Chatham M, Bleecker ER, Norman P, Smith PL, Mason P. A screening test for airways reactivity. An abbreviated methacholine inhalation challenge. Chest 1982;82:15-18.
8. Jang A, Lee J, Park S, et al. Factors influencing the responsiveness to inhaled glucocorticoids in patients with moderate to severe asthma. Korean J Asthma Allergy Clin Immunol 2005;25:175-180.
9. Ours TM, Kavuru MS, Schilz RJ, Richter JE. A prospective evaluation of esophageal testing and a double-blind randomized study of omeprazole in a diagnostic and therapeutic algorithm for chronic cough. Am J Gastroenterol 1999;94:3131-3138.
10. Cho JH, Ryu JS, Lee HL. Chronic cough: the spectrum and the frequency of etiologies. Tuberc Respir Dis 1999;46:555-563.
11. Jeon G, Jang SH, Song HG, et al. Diagnostic performance of routine objective tests and cost-effective approach for chronic cough. Tuberc Respir Dis 2004;57:535-542.
12. Smyrnios NA, Irwin RS, Curley FJ. Chronic cough with a history of excessive sputum production. The spectrum and frequency of causes, key components of the diagnostic evaluation, and outcome of specific therapy. Chest 1995;108:991-997.
13. Global Initiative for Asthma. Global strategy for asthma management and prevention. NHLBI/WHO workshop report. Bethesda, Md: National Heart, Lung and Blood Institute;2004.
14. James AL, Palmer LJ, Kicic E, et al. Decline in lung function in the Busselton Health Study: the effects of asthma and cigarette smoking. Am J Respir Crit Care Med 2005;171:109-114.
15. Fish JE, Peters SP. Bronchial challenge testing. Middleton’s Allergy Principles and Practice. 6th ed. St Louis, Mo: Mosby, Inc; 2003;657-670.
16. Dicpinigaitis PV. Chronic cough due to asthma: ACCP evidence-based clinical practice guidelines. Chest 2006;129:75S-79S
17. Park JK, Park SW, Lee JH, et al. Evaluation of clinical course in patients with eosinophilic bronchitis: A prospective follow up study. J Asthma Allergy Clin Immunol 2003;23:740-748.
18. Simpson G. Investigation and management of persistent dry cough. Thorax 1999;54:469-470.