User login
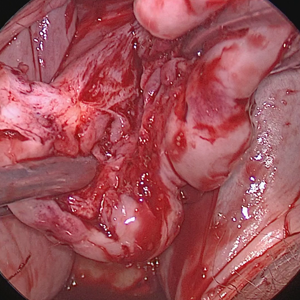
Retroperitoneal anatomy and parametrial dissection in robotic uterine artery-sparing radical trachelectomy
Morcellation at the time of vaginal hysterectomy

Visit the Society of Gynecologic Surgeons online: sgsonline.org
Additional videos from SGS are available here, including these recent offerings:

Visit the Society of Gynecologic Surgeons online: sgsonline.org
Additional videos from SGS are available here, including these recent offerings:

Visit the Society of Gynecologic Surgeons online: sgsonline.org
Additional videos from SGS are available here, including these recent offerings:
This video is brought to you by
When is the robot truly the best option for gynecologic surgery?
When laparoscopic hysterectomy was pioneered in the late 1980s, uptake among the gynecologic surgical community was slow—despite the fact that the benefits of laparoscopy soon were evident. Compared with abdominal hysterectomy, the laparoscopic approach offered less blood loss, shorter length of hospitalization, less pain, an earlier return to activity, and improved cosmesis.
Contrast this slow start with the rapid introduction of robotic assistance in gynecologic surgery. Soon after the robot was approved for gynecology in 2005, adoption of the new technology surged. In recent years, in fact, use of the robot has grown faster than use of laparoscopy for benign hysterectomy.
At the Pelvic Anatomy and Gynecologic Surgery (PAGS) Symposium in December 2014, Tommaso Falcone, MD, and Javier Magrina, MD, discussed the rapid adoption of the robot, its role in gynecologic surgery, and how it compares with traditional laparoscopy in a key domain—cost. When OBG Management asked these experts to defend their preferred route of hysterectomy, a lively discussion ensued.
Advantages of laparoscopy
OBG Management: What is your preferred approach for hysterectomy, and why do you consider it superior to other options?
Dr. Falcone: I’m a reproductive endocrinologist by training. In my practice at the Cleveland Clinic, I treat only benign disease—no cancer. For hysterectomy, I favor conventional laparoscopy for several reasons. First, it’s time-proven, with a long history of efficacy over the past 20 years. Second, apart from vaginal hysterectomy, it’s the most cost-effective approach to removal of the uterus in patients with benign disease.
Dr. Magrina: I have practiced as a gynecologic oncologist at the Mayo Clinic, Arizona, for the past 27 years, but I also do surgical procedures for benign disease. During my initial training, there were only two ways to perform a hysterectomy—either you made an incision in the abdomen, or you went through the vagina, which is a NOTES (natural orifice transluminal endoscopic surgery) procedure. Of the two, the vaginal approach is the most effective. It also is cheapest and offers the fastest recovery, but it never surpassed the abdominal approach in practice. The reason: The vaginal approach requires you to work through a small opening using specialized instruments, so it’s more difficult for the surgeon and has reduced visualization.
Laparoscopic hysterectomy—or, more specifically, laparoscopically assisted vaginal hysterectomy—arrived in 1989. This approach never gained popularity, but even pure laparoscopy, which came along shortly afterward, took a long time for surgeons to adopt. A main problem was that the technology made it counterintuitive for the surgeon. With the abdominal approach, the surgeon can work with his or her hands in the abdomen, with direct visualization and tactile feedback. In laparoscopy, however, the surgeon uses instruments inside of the abdomen with visualization via a camera. As a result, laparoscopy has a much steeperlearning curve, so it never replaced abdominal hysterectomy in the way that we expected.
When robotic surgery came along, in contrast, it quickly became an enabling technology for surgeons who could not perform conventional laparoscopy, and it has overtaken laparoscopy for that reason.
Today there are four options for hysterectomy: the abdominal approach, the vaginal approach, the laparoscopic approach, and robotic assistance. I prefer robotics for complicated surgeries—primarily gynecologic cancer and advanced endometriosis. I also prefer robotics when the patient is obese.
In our practice at Mayo Clinic, Arizona, the abdominal open option essentially doesn’t exist for benign disease. If the patient has a simple problem, such as menorrhagia, which can be corrected by removing the uterus, I would choose a vaginal approach. However, if she has pain in addition to menorrhagia—particularly if it is not cyclic pain—I would prefer a laparoscopic approach.
 |  |
How cost comes into play
Dr. Falcone: I think that what has influenced this discussion in recent years is the cost of medicine. Both Dr. Magrina and I trained in an era when we taught ourselves laparoscopy—as no one else was using it—and then began to try to teach others. And Dr. Magrina is correct when he describes the very slow process of absorption of the new technology. Laparoscopic hysterectomy was performed at a low frequency for a long time, and then robotic technology came along—an enabling technology, to be sure—and minimally invasive surgery took off.
Now, however, cost pressures are increasing. Let’s say the robot is the “Lamborghini” of surgical technology, as it is the most expensive of all the approaches. Until a couple of years ago, we could say, “OK, you need a Lamborghini to cross the finish line, fine. We are so wealthy, you can buy that Lamborghini. I prefer the ‘Honda’ (laparoscopy) but as long as we both cross the finish line, there’s no problem.” Now we can no longer afford the Lamborghini.
The aim is not to eliminate the robot entirely. It definitely has a role in minimally invasive surgery. But doctors who need a sophisticated enabling device to perform minimally invasive surgery now may be discouraged from using the robot, owing to its higher cost. In the future, robotics cases are more likely to be performed by surgeons who can do complex procedures at a high volume. That’s already the model at the Mayo Clinic and Cleveland Clinic. More and more, we’re going to say, “You don’t do enough hysterectomies. Although you are performing the ones you do satisfactorily with the robot, you simply aren’t doing enough. So we’re going to move them into the hands of someone who can do them more cost-effectively.”
It’s the cost variable that has changed the game.
Dr. Magrina: I fully agree that we are in an era in which cost-effectiveness is imperative. At our institution, we have four gynecologic surgeons performing robotic, laparoscopic, and vaginal procedures. I happen to be in the low expensive end of the four, particularly in robotics, largely because I limit the number of robotic instruments—two or three, one assistant, and no manipulator. I utilize a reusable probe, and I look for ways to minimize costs. For example, instead of using an additional needle holder to suture the vaginal cuff, I use one of the robotic graspers already used in the hysterectomy part.
When surgeons begin performing robotic hysterectomy, they try multiple instruments, making the approach very expensive. As surgeons gain experience and begin to watch their costs, however, the expense comes down somewhat.
Why the robot should be reserved for high-volume surgeons
Dr. Magrina: In my opinion, if you have a basic “bread and butter” practice, I don’t think you need to have a robot. The robot should be reserved for advanced surgery. And because of fixed costs with the robot, such as maintenance, you need to perform a sufficient number of cases per year to cover those expenses. At my institution, the minimum number of robotic cases per year is about 200. Our cost for robotic surgery is 8% higher than it is for laparoscopy. If we perform fewer than 200 robotic surgeries, the difference is even greater.
Dr. Falcone: I agree with everything you’ve said, Dr. Magrina. But if you consider that about 120,000 of the 500,000 hysterectomies performed each year are done for abnormal uterine bleeding in women who have a normal uterus and no other complexity, there’s no need for the robot for these cases. A lot of places—certainly not the Cleveland Clinic or the Mayo Clinic, but other places—use the robot to remove that little uterus. That’s when conventional laparoscopy should be the preferred route.
When it comes to endometriosis, which accounts for another 20% of cases, the robot might break even because it’s the length of surgery that is important. Still, although the robot might allow most community surgeons to perform routine endometriosis cases, complex cases are another matter. The robot is an enabling device for simple cases for the average gynecologist but not for complex cases. For those cases, it requires a different skill set—sophisticated skills of retroperitoneal anatomy, which the robot doesn’t teach you. It requires experience working in a different space, which the robot doesn’t give you.
Dr. Magrina: That’s an important point. If a surgeon came to me and said, “Look, at my institution, if I don’t perform 35 robotic cases a year, they’ll take my privileges away,” that would indicate to me that the surgeon is performing some cases robotically that might be better done laparoscopically or vaginally. But he is doing them robotically just to maintain his privileges.
I would suggest to him that if his caseload is not that high, maybe he shouldn’t be doing any robotic cases. Another option is for him to propose to his institution that he perform the 20 well-indicated cases on the robot and the other 15 laparoscopically. Then, to maintain his robotic skills and privileges, he could log in the equivalent of 15 or more robotic cases by simulation.
Gynecologic surgeons have strong preferences when it comes to the route of hysterectomy for benign disease—at least among OBG Management’s Virtual Board of Editors (VBE). When they were asked to weigh in on laparoscopic hysterectomy versus robotic assistance, VBE members tended to come down firmly on one side or another, with very little “fence-sitting.”
For example, Soheil Hanjani, MD, reported that he performs approximately 95% of benign hysterectomy cases using a minimally invasive approach, preferably robotic assistance.
“In the right hands, robotics is superior,” he said, adding that it gives him “better dissection control.”
Heather Hilkowitz, MD, agreed.
“I feel like the imaging is better with robotics, such that I can really see tissue and planes better than with 2D straight-stick laparoscopy. I also appreciate the wristed instrumentation of the robot, which allows me to do more difficult cases laparoscopically that I would have had to open in the past.”
Weighing in on the other side of the equation is Noor Ahmed-Ebbiary, MB, who practices in the United Kingdom. Dr. Ahmed-Ebbiary cites expense as a major disadvantage of the robot.
“If the surgeon is experienced in both vaginal and laparoscopic surgery, he or she should be able to manage the vast majority of hysterectomies without a robot. European countries are not as rich, and most of them cannot offer or justify the price of a robot,” he added.
Raksha Joshi, MD, uses a minimally invasive approach for about 50% of the benign hysterectomies she performs, favoring the vaginal route.
“Robotic surgery for hysterectomy for benign disease is ‘overkill,’” she says. “It’s expensive, takes much longer than laparoscopic surgery or a laparoscopically assisted vaginal approach, and does not give any outcomes advantage for the patient.”
Michael Kirwin, MD, prefers total laparoscopic hysterectomy, depending on the patient’s surgical history and anticipated abdominal conditions, because it allows him to “port-hop,” offers more options for energy instrumentation, is more economical than the robot, and yields smaller incisions.
John T. Armstrong Jr., MD, MS, prefers neither total laparoscopic hysterectomy nor robotic assistance. He opts instead for a straight vaginal approach or open hysterectomy through a minilaparotomy incision.
A look to the future
OBG Management: Now that cost pressures are beginning to discourage use of the robot for straightforward, low-complexity hysterectomy cases, do you anticipate that surgeons who lack laparoscopic skills will refer patients to minimally invasive surgical experts? Or are they likely to utilize abdominal hysterectomy more than in the past? In other words, what changes do you foresee as cost pressures increase?
Dr. Falcone: I think cost pressures will ensure that surgeons will think about their approach to a surgical procedure more critically. It will add the cost of the procedure to the conversation between doctor and patient of what is best for her.
Dr. Magrina: Cost pressures will force hospitals and gynecologists to change our present modus operandi. In general, high-volume surgeons have shorter operating times, fewer complications, and lower costs—a true fact among many different surgical specialties. Hospitals will start looking at the cost of specific procedures and compare costs among surgeons. Expensive surgeons may be asked to explore ways to reduce costs, and, if they don’t, may be denied privileges for specific procedures.
I envision ObGyn groups—so-called generalists—to be composed of physicians dedicated to obstetrics and gynecologists dedicated to office practice or surgery. The days when an ObGyn surgical practice offered care that encompassed both the delivery of babies and oncologic procedures, including urogynecologic, infertility, and complex operations, should be over. Our specialty is in need of a higher degree of focused practice.
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
____________________________________________________________________
Learn directly from experts Tommaso Falcone, MD, Javier Magrina, MD, and Mark Walters, MD
2015 PELVIC ANATOMY AND GYNECOLOGIC SURGERY (PAGS) SYMPOSIUM
Thursday, December 10 – Saturday December 12, 2015
At Paris in Las Vegas
Preconference hands-on workshops on laparoscopic suturing, hysteroscopy, and ultrasound on Wednesday, December 9.
Visit: www.PAGS-CME.org
When laparoscopic hysterectomy was pioneered in the late 1980s, uptake among the gynecologic surgical community was slow—despite the fact that the benefits of laparoscopy soon were evident. Compared with abdominal hysterectomy, the laparoscopic approach offered less blood loss, shorter length of hospitalization, less pain, an earlier return to activity, and improved cosmesis.
Contrast this slow start with the rapid introduction of robotic assistance in gynecologic surgery. Soon after the robot was approved for gynecology in 2005, adoption of the new technology surged. In recent years, in fact, use of the robot has grown faster than use of laparoscopy for benign hysterectomy.
At the Pelvic Anatomy and Gynecologic Surgery (PAGS) Symposium in December 2014, Tommaso Falcone, MD, and Javier Magrina, MD, discussed the rapid adoption of the robot, its role in gynecologic surgery, and how it compares with traditional laparoscopy in a key domain—cost. When OBG Management asked these experts to defend their preferred route of hysterectomy, a lively discussion ensued.
Advantages of laparoscopy
OBG Management: What is your preferred approach for hysterectomy, and why do you consider it superior to other options?
Dr. Falcone: I’m a reproductive endocrinologist by training. In my practice at the Cleveland Clinic, I treat only benign disease—no cancer. For hysterectomy, I favor conventional laparoscopy for several reasons. First, it’s time-proven, with a long history of efficacy over the past 20 years. Second, apart from vaginal hysterectomy, it’s the most cost-effective approach to removal of the uterus in patients with benign disease.
Dr. Magrina: I have practiced as a gynecologic oncologist at the Mayo Clinic, Arizona, for the past 27 years, but I also do surgical procedures for benign disease. During my initial training, there were only two ways to perform a hysterectomy—either you made an incision in the abdomen, or you went through the vagina, which is a NOTES (natural orifice transluminal endoscopic surgery) procedure. Of the two, the vaginal approach is the most effective. It also is cheapest and offers the fastest recovery, but it never surpassed the abdominal approach in practice. The reason: The vaginal approach requires you to work through a small opening using specialized instruments, so it’s more difficult for the surgeon and has reduced visualization.
Laparoscopic hysterectomy—or, more specifically, laparoscopically assisted vaginal hysterectomy—arrived in 1989. This approach never gained popularity, but even pure laparoscopy, which came along shortly afterward, took a long time for surgeons to adopt. A main problem was that the technology made it counterintuitive for the surgeon. With the abdominal approach, the surgeon can work with his or her hands in the abdomen, with direct visualization and tactile feedback. In laparoscopy, however, the surgeon uses instruments inside of the abdomen with visualization via a camera. As a result, laparoscopy has a much steeperlearning curve, so it never replaced abdominal hysterectomy in the way that we expected.
When robotic surgery came along, in contrast, it quickly became an enabling technology for surgeons who could not perform conventional laparoscopy, and it has overtaken laparoscopy for that reason.
Today there are four options for hysterectomy: the abdominal approach, the vaginal approach, the laparoscopic approach, and robotic assistance. I prefer robotics for complicated surgeries—primarily gynecologic cancer and advanced endometriosis. I also prefer robotics when the patient is obese.
In our practice at Mayo Clinic, Arizona, the abdominal open option essentially doesn’t exist for benign disease. If the patient has a simple problem, such as menorrhagia, which can be corrected by removing the uterus, I would choose a vaginal approach. However, if she has pain in addition to menorrhagia—particularly if it is not cyclic pain—I would prefer a laparoscopic approach.
 |  |
How cost comes into play
Dr. Falcone: I think that what has influenced this discussion in recent years is the cost of medicine. Both Dr. Magrina and I trained in an era when we taught ourselves laparoscopy—as no one else was using it—and then began to try to teach others. And Dr. Magrina is correct when he describes the very slow process of absorption of the new technology. Laparoscopic hysterectomy was performed at a low frequency for a long time, and then robotic technology came along—an enabling technology, to be sure—and minimally invasive surgery took off.
Now, however, cost pressures are increasing. Let’s say the robot is the “Lamborghini” of surgical technology, as it is the most expensive of all the approaches. Until a couple of years ago, we could say, “OK, you need a Lamborghini to cross the finish line, fine. We are so wealthy, you can buy that Lamborghini. I prefer the ‘Honda’ (laparoscopy) but as long as we both cross the finish line, there’s no problem.” Now we can no longer afford the Lamborghini.
The aim is not to eliminate the robot entirely. It definitely has a role in minimally invasive surgery. But doctors who need a sophisticated enabling device to perform minimally invasive surgery now may be discouraged from using the robot, owing to its higher cost. In the future, robotics cases are more likely to be performed by surgeons who can do complex procedures at a high volume. That’s already the model at the Mayo Clinic and Cleveland Clinic. More and more, we’re going to say, “You don’t do enough hysterectomies. Although you are performing the ones you do satisfactorily with the robot, you simply aren’t doing enough. So we’re going to move them into the hands of someone who can do them more cost-effectively.”
It’s the cost variable that has changed the game.
Dr. Magrina: I fully agree that we are in an era in which cost-effectiveness is imperative. At our institution, we have four gynecologic surgeons performing robotic, laparoscopic, and vaginal procedures. I happen to be in the low expensive end of the four, particularly in robotics, largely because I limit the number of robotic instruments—two or three, one assistant, and no manipulator. I utilize a reusable probe, and I look for ways to minimize costs. For example, instead of using an additional needle holder to suture the vaginal cuff, I use one of the robotic graspers already used in the hysterectomy part.
When surgeons begin performing robotic hysterectomy, they try multiple instruments, making the approach very expensive. As surgeons gain experience and begin to watch their costs, however, the expense comes down somewhat.
Why the robot should be reserved for high-volume surgeons
Dr. Magrina: In my opinion, if you have a basic “bread and butter” practice, I don’t think you need to have a robot. The robot should be reserved for advanced surgery. And because of fixed costs with the robot, such as maintenance, you need to perform a sufficient number of cases per year to cover those expenses. At my institution, the minimum number of robotic cases per year is about 200. Our cost for robotic surgery is 8% higher than it is for laparoscopy. If we perform fewer than 200 robotic surgeries, the difference is even greater.
Dr. Falcone: I agree with everything you’ve said, Dr. Magrina. But if you consider that about 120,000 of the 500,000 hysterectomies performed each year are done for abnormal uterine bleeding in women who have a normal uterus and no other complexity, there’s no need for the robot for these cases. A lot of places—certainly not the Cleveland Clinic or the Mayo Clinic, but other places—use the robot to remove that little uterus. That’s when conventional laparoscopy should be the preferred route.
When it comes to endometriosis, which accounts for another 20% of cases, the robot might break even because it’s the length of surgery that is important. Still, although the robot might allow most community surgeons to perform routine endometriosis cases, complex cases are another matter. The robot is an enabling device for simple cases for the average gynecologist but not for complex cases. For those cases, it requires a different skill set—sophisticated skills of retroperitoneal anatomy, which the robot doesn’t teach you. It requires experience working in a different space, which the robot doesn’t give you.
Dr. Magrina: That’s an important point. If a surgeon came to me and said, “Look, at my institution, if I don’t perform 35 robotic cases a year, they’ll take my privileges away,” that would indicate to me that the surgeon is performing some cases robotically that might be better done laparoscopically or vaginally. But he is doing them robotically just to maintain his privileges.
I would suggest to him that if his caseload is not that high, maybe he shouldn’t be doing any robotic cases. Another option is for him to propose to his institution that he perform the 20 well-indicated cases on the robot and the other 15 laparoscopically. Then, to maintain his robotic skills and privileges, he could log in the equivalent of 15 or more robotic cases by simulation.
Gynecologic surgeons have strong preferences when it comes to the route of hysterectomy for benign disease—at least among OBG Management’s Virtual Board of Editors (VBE). When they were asked to weigh in on laparoscopic hysterectomy versus robotic assistance, VBE members tended to come down firmly on one side or another, with very little “fence-sitting.”
For example, Soheil Hanjani, MD, reported that he performs approximately 95% of benign hysterectomy cases using a minimally invasive approach, preferably robotic assistance.
“In the right hands, robotics is superior,” he said, adding that it gives him “better dissection control.”
Heather Hilkowitz, MD, agreed.
“I feel like the imaging is better with robotics, such that I can really see tissue and planes better than with 2D straight-stick laparoscopy. I also appreciate the wristed instrumentation of the robot, which allows me to do more difficult cases laparoscopically that I would have had to open in the past.”
Weighing in on the other side of the equation is Noor Ahmed-Ebbiary, MB, who practices in the United Kingdom. Dr. Ahmed-Ebbiary cites expense as a major disadvantage of the robot.
“If the surgeon is experienced in both vaginal and laparoscopic surgery, he or she should be able to manage the vast majority of hysterectomies without a robot. European countries are not as rich, and most of them cannot offer or justify the price of a robot,” he added.
Raksha Joshi, MD, uses a minimally invasive approach for about 50% of the benign hysterectomies she performs, favoring the vaginal route.
“Robotic surgery for hysterectomy for benign disease is ‘overkill,’” she says. “It’s expensive, takes much longer than laparoscopic surgery or a laparoscopically assisted vaginal approach, and does not give any outcomes advantage for the patient.”
Michael Kirwin, MD, prefers total laparoscopic hysterectomy, depending on the patient’s surgical history and anticipated abdominal conditions, because it allows him to “port-hop,” offers more options for energy instrumentation, is more economical than the robot, and yields smaller incisions.
John T. Armstrong Jr., MD, MS, prefers neither total laparoscopic hysterectomy nor robotic assistance. He opts instead for a straight vaginal approach or open hysterectomy through a minilaparotomy incision.
A look to the future
OBG Management: Now that cost pressures are beginning to discourage use of the robot for straightforward, low-complexity hysterectomy cases, do you anticipate that surgeons who lack laparoscopic skills will refer patients to minimally invasive surgical experts? Or are they likely to utilize abdominal hysterectomy more than in the past? In other words, what changes do you foresee as cost pressures increase?
Dr. Falcone: I think cost pressures will ensure that surgeons will think about their approach to a surgical procedure more critically. It will add the cost of the procedure to the conversation between doctor and patient of what is best for her.
Dr. Magrina: Cost pressures will force hospitals and gynecologists to change our present modus operandi. In general, high-volume surgeons have shorter operating times, fewer complications, and lower costs—a true fact among many different surgical specialties. Hospitals will start looking at the cost of specific procedures and compare costs among surgeons. Expensive surgeons may be asked to explore ways to reduce costs, and, if they don’t, may be denied privileges for specific procedures.
I envision ObGyn groups—so-called generalists—to be composed of physicians dedicated to obstetrics and gynecologists dedicated to office practice or surgery. The days when an ObGyn surgical practice offered care that encompassed both the delivery of babies and oncologic procedures, including urogynecologic, infertility, and complex operations, should be over. Our specialty is in need of a higher degree of focused practice.
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
____________________________________________________________________
Learn directly from experts Tommaso Falcone, MD, Javier Magrina, MD, and Mark Walters, MD
2015 PELVIC ANATOMY AND GYNECOLOGIC SURGERY (PAGS) SYMPOSIUM
Thursday, December 10 – Saturday December 12, 2015
At Paris in Las Vegas
Preconference hands-on workshops on laparoscopic suturing, hysteroscopy, and ultrasound on Wednesday, December 9.
Visit: www.PAGS-CME.org
When laparoscopic hysterectomy was pioneered in the late 1980s, uptake among the gynecologic surgical community was slow—despite the fact that the benefits of laparoscopy soon were evident. Compared with abdominal hysterectomy, the laparoscopic approach offered less blood loss, shorter length of hospitalization, less pain, an earlier return to activity, and improved cosmesis.
Contrast this slow start with the rapid introduction of robotic assistance in gynecologic surgery. Soon after the robot was approved for gynecology in 2005, adoption of the new technology surged. In recent years, in fact, use of the robot has grown faster than use of laparoscopy for benign hysterectomy.
At the Pelvic Anatomy and Gynecologic Surgery (PAGS) Symposium in December 2014, Tommaso Falcone, MD, and Javier Magrina, MD, discussed the rapid adoption of the robot, its role in gynecologic surgery, and how it compares with traditional laparoscopy in a key domain—cost. When OBG Management asked these experts to defend their preferred route of hysterectomy, a lively discussion ensued.
Advantages of laparoscopy
OBG Management: What is your preferred approach for hysterectomy, and why do you consider it superior to other options?
Dr. Falcone: I’m a reproductive endocrinologist by training. In my practice at the Cleveland Clinic, I treat only benign disease—no cancer. For hysterectomy, I favor conventional laparoscopy for several reasons. First, it’s time-proven, with a long history of efficacy over the past 20 years. Second, apart from vaginal hysterectomy, it’s the most cost-effective approach to removal of the uterus in patients with benign disease.
Dr. Magrina: I have practiced as a gynecologic oncologist at the Mayo Clinic, Arizona, for the past 27 years, but I also do surgical procedures for benign disease. During my initial training, there were only two ways to perform a hysterectomy—either you made an incision in the abdomen, or you went through the vagina, which is a NOTES (natural orifice transluminal endoscopic surgery) procedure. Of the two, the vaginal approach is the most effective. It also is cheapest and offers the fastest recovery, but it never surpassed the abdominal approach in practice. The reason: The vaginal approach requires you to work through a small opening using specialized instruments, so it’s more difficult for the surgeon and has reduced visualization.
Laparoscopic hysterectomy—or, more specifically, laparoscopically assisted vaginal hysterectomy—arrived in 1989. This approach never gained popularity, but even pure laparoscopy, which came along shortly afterward, took a long time for surgeons to adopt. A main problem was that the technology made it counterintuitive for the surgeon. With the abdominal approach, the surgeon can work with his or her hands in the abdomen, with direct visualization and tactile feedback. In laparoscopy, however, the surgeon uses instruments inside of the abdomen with visualization via a camera. As a result, laparoscopy has a much steeperlearning curve, so it never replaced abdominal hysterectomy in the way that we expected.
When robotic surgery came along, in contrast, it quickly became an enabling technology for surgeons who could not perform conventional laparoscopy, and it has overtaken laparoscopy for that reason.
Today there are four options for hysterectomy: the abdominal approach, the vaginal approach, the laparoscopic approach, and robotic assistance. I prefer robotics for complicated surgeries—primarily gynecologic cancer and advanced endometriosis. I also prefer robotics when the patient is obese.
In our practice at Mayo Clinic, Arizona, the abdominal open option essentially doesn’t exist for benign disease. If the patient has a simple problem, such as menorrhagia, which can be corrected by removing the uterus, I would choose a vaginal approach. However, if she has pain in addition to menorrhagia—particularly if it is not cyclic pain—I would prefer a laparoscopic approach.
 |  |
How cost comes into play
Dr. Falcone: I think that what has influenced this discussion in recent years is the cost of medicine. Both Dr. Magrina and I trained in an era when we taught ourselves laparoscopy—as no one else was using it—and then began to try to teach others. And Dr. Magrina is correct when he describes the very slow process of absorption of the new technology. Laparoscopic hysterectomy was performed at a low frequency for a long time, and then robotic technology came along—an enabling technology, to be sure—and minimally invasive surgery took off.
Now, however, cost pressures are increasing. Let’s say the robot is the “Lamborghini” of surgical technology, as it is the most expensive of all the approaches. Until a couple of years ago, we could say, “OK, you need a Lamborghini to cross the finish line, fine. We are so wealthy, you can buy that Lamborghini. I prefer the ‘Honda’ (laparoscopy) but as long as we both cross the finish line, there’s no problem.” Now we can no longer afford the Lamborghini.
The aim is not to eliminate the robot entirely. It definitely has a role in minimally invasive surgery. But doctors who need a sophisticated enabling device to perform minimally invasive surgery now may be discouraged from using the robot, owing to its higher cost. In the future, robotics cases are more likely to be performed by surgeons who can do complex procedures at a high volume. That’s already the model at the Mayo Clinic and Cleveland Clinic. More and more, we’re going to say, “You don’t do enough hysterectomies. Although you are performing the ones you do satisfactorily with the robot, you simply aren’t doing enough. So we’re going to move them into the hands of someone who can do them more cost-effectively.”
It’s the cost variable that has changed the game.
Dr. Magrina: I fully agree that we are in an era in which cost-effectiveness is imperative. At our institution, we have four gynecologic surgeons performing robotic, laparoscopic, and vaginal procedures. I happen to be in the low expensive end of the four, particularly in robotics, largely because I limit the number of robotic instruments—two or three, one assistant, and no manipulator. I utilize a reusable probe, and I look for ways to minimize costs. For example, instead of using an additional needle holder to suture the vaginal cuff, I use one of the robotic graspers already used in the hysterectomy part.
When surgeons begin performing robotic hysterectomy, they try multiple instruments, making the approach very expensive. As surgeons gain experience and begin to watch their costs, however, the expense comes down somewhat.
Why the robot should be reserved for high-volume surgeons
Dr. Magrina: In my opinion, if you have a basic “bread and butter” practice, I don’t think you need to have a robot. The robot should be reserved for advanced surgery. And because of fixed costs with the robot, such as maintenance, you need to perform a sufficient number of cases per year to cover those expenses. At my institution, the minimum number of robotic cases per year is about 200. Our cost for robotic surgery is 8% higher than it is for laparoscopy. If we perform fewer than 200 robotic surgeries, the difference is even greater.
Dr. Falcone: I agree with everything you’ve said, Dr. Magrina. But if you consider that about 120,000 of the 500,000 hysterectomies performed each year are done for abnormal uterine bleeding in women who have a normal uterus and no other complexity, there’s no need for the robot for these cases. A lot of places—certainly not the Cleveland Clinic or the Mayo Clinic, but other places—use the robot to remove that little uterus. That’s when conventional laparoscopy should be the preferred route.
When it comes to endometriosis, which accounts for another 20% of cases, the robot might break even because it’s the length of surgery that is important. Still, although the robot might allow most community surgeons to perform routine endometriosis cases, complex cases are another matter. The robot is an enabling device for simple cases for the average gynecologist but not for complex cases. For those cases, it requires a different skill set—sophisticated skills of retroperitoneal anatomy, which the robot doesn’t teach you. It requires experience working in a different space, which the robot doesn’t give you.
Dr. Magrina: That’s an important point. If a surgeon came to me and said, “Look, at my institution, if I don’t perform 35 robotic cases a year, they’ll take my privileges away,” that would indicate to me that the surgeon is performing some cases robotically that might be better done laparoscopically or vaginally. But he is doing them robotically just to maintain his privileges.
I would suggest to him that if his caseload is not that high, maybe he shouldn’t be doing any robotic cases. Another option is for him to propose to his institution that he perform the 20 well-indicated cases on the robot and the other 15 laparoscopically. Then, to maintain his robotic skills and privileges, he could log in the equivalent of 15 or more robotic cases by simulation.
Gynecologic surgeons have strong preferences when it comes to the route of hysterectomy for benign disease—at least among OBG Management’s Virtual Board of Editors (VBE). When they were asked to weigh in on laparoscopic hysterectomy versus robotic assistance, VBE members tended to come down firmly on one side or another, with very little “fence-sitting.”
For example, Soheil Hanjani, MD, reported that he performs approximately 95% of benign hysterectomy cases using a minimally invasive approach, preferably robotic assistance.
“In the right hands, robotics is superior,” he said, adding that it gives him “better dissection control.”
Heather Hilkowitz, MD, agreed.
“I feel like the imaging is better with robotics, such that I can really see tissue and planes better than with 2D straight-stick laparoscopy. I also appreciate the wristed instrumentation of the robot, which allows me to do more difficult cases laparoscopically that I would have had to open in the past.”
Weighing in on the other side of the equation is Noor Ahmed-Ebbiary, MB, who practices in the United Kingdom. Dr. Ahmed-Ebbiary cites expense as a major disadvantage of the robot.
“If the surgeon is experienced in both vaginal and laparoscopic surgery, he or she should be able to manage the vast majority of hysterectomies without a robot. European countries are not as rich, and most of them cannot offer or justify the price of a robot,” he added.
Raksha Joshi, MD, uses a minimally invasive approach for about 50% of the benign hysterectomies she performs, favoring the vaginal route.
“Robotic surgery for hysterectomy for benign disease is ‘overkill,’” she says. “It’s expensive, takes much longer than laparoscopic surgery or a laparoscopically assisted vaginal approach, and does not give any outcomes advantage for the patient.”
Michael Kirwin, MD, prefers total laparoscopic hysterectomy, depending on the patient’s surgical history and anticipated abdominal conditions, because it allows him to “port-hop,” offers more options for energy instrumentation, is more economical than the robot, and yields smaller incisions.
John T. Armstrong Jr., MD, MS, prefers neither total laparoscopic hysterectomy nor robotic assistance. He opts instead for a straight vaginal approach or open hysterectomy through a minilaparotomy incision.
A look to the future
OBG Management: Now that cost pressures are beginning to discourage use of the robot for straightforward, low-complexity hysterectomy cases, do you anticipate that surgeons who lack laparoscopic skills will refer patients to minimally invasive surgical experts? Or are they likely to utilize abdominal hysterectomy more than in the past? In other words, what changes do you foresee as cost pressures increase?
Dr. Falcone: I think cost pressures will ensure that surgeons will think about their approach to a surgical procedure more critically. It will add the cost of the procedure to the conversation between doctor and patient of what is best for her.
Dr. Magrina: Cost pressures will force hospitals and gynecologists to change our present modus operandi. In general, high-volume surgeons have shorter operating times, fewer complications, and lower costs—a true fact among many different surgical specialties. Hospitals will start looking at the cost of specific procedures and compare costs among surgeons. Expensive surgeons may be asked to explore ways to reduce costs, and, if they don’t, may be denied privileges for specific procedures.
I envision ObGyn groups—so-called generalists—to be composed of physicians dedicated to obstetrics and gynecologists dedicated to office practice or surgery. The days when an ObGyn surgical practice offered care that encompassed both the delivery of babies and oncologic procedures, including urogynecologic, infertility, and complex operations, should be over. Our specialty is in need of a higher degree of focused practice.
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
____________________________________________________________________
Learn directly from experts Tommaso Falcone, MD, Javier Magrina, MD, and Mark Walters, MD
2015 PELVIC ANATOMY AND GYNECOLOGIC SURGERY (PAGS) SYMPOSIUM
Thursday, December 10 – Saturday December 12, 2015
At Paris in Las Vegas
Preconference hands-on workshops on laparoscopic suturing, hysteroscopy, and ultrasound on Wednesday, December 9.
Visit: www.PAGS-CME.org