User login
Part 2 of 2: Delivery and postpartum concerns in the obese gravida
The authors report no financial relationships relevant to this article.
Hear Dr Phillips discuss the key points of this series
With the ranks of the obese expanding, and the severity of obesity increasing as well, obstetricians see a greater percentage of obese and morbidly obese gravidas in their practice. At the end of pregnancy, when it is time to deliver the infant, a number of issues must be taken into account to ensure the safety and health of both mother and child. Part 2 of this two-part article discusses these issues, from intrapartum and intraoperative considerations to care during the postpartum period.
Intrapartum concerns
Induction of labor
Obese women are more likely to require induction of labor; they should be counseled accordingly. The rate of labor induction is as high as 35% in women who have a body mass index (BMI) above 35.1 Many of these inductions are indicated for maternal disease such as diabetes or preeclampsia. However, data suggest that obesity alone increases the induction rate, possibly through increased levels of leptin (an adipokine involved in obesity, appetite, and satiety), which may inhibit uterine contractions.2
Uterine and fetal monitoring
Monitoring of uterine contractions and fetal heart rate can be challenging in obese women. Early use of an intra uterine pressure catheter and fetal scalp electrode can help.
Shoulder dystocia
Obesity is a risk factor for macrosomia, which increases the likelihood of shoulder dystocia. In addition, at least one study supports maternal obesity as an independent risk factor for shoulder dystocia. Women who had a BMI above 30 were 2.7 times more likely to have a pregnancy complicated by shoulder dystocia, after adjustment for macrosomia, diabetes, parity, and induction of labor.3
Because of this risk, appropriate staff should be readily available for assistance, and operative vaginal delivery should be performed with caution, if at all.
Vaginal birth after cesarean delivery
Obese women who have a history of cesarean delivery need to be counseled about the higher risk of failed vaginal birth after cesarean (VBAC) and the likely need for repeat cesarean delivery. They also need to be told about the elevated risk of infection in the event that VBAC fails.
In women of normal weight, the likelihood of successful VBAC exceeds 80%, compared with a success rate of 68% for women who have a BMI above 29, and 60% for women who have a BMI above 40.4,5
Appropriate counseling and patient selection are critical components of the decision to proceed with a trial of labor in obese women who have a history of cesarean delivery. Twenty-four-hour anesthesia and NICU coverage are also necessary in case emergent cesarean delivery becomes necessary.
Cesarean delivery
Morbidly obese women (BMI >35) have approximately a 50% greater chance of requiring cesarean delivery than do women of normal weight.6 The need for cesarean delivery rises with increasing BMI, probably because of a greater degree of maternal pelvic soft tissue, which increases the risk of both dystocia and cephalopelvic disproportion.
Anesthesia
It may be advisable to place an early epidural in laboring obese patients because they are more likely to require multiple placement attempts and cesarean delivery.
Intraoperative considerations
Ensure availability of the proper equipment
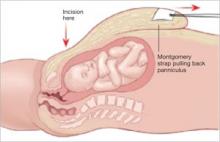
Table extenders, appropriate retractors, and long instruments should be readily available before surgery. For example, obstetricians often retract the panniculus to allow for a Pfannenstiel skin incision ( FIGURE 1 ), which works well to increase exposure. Moreover, the depth of the abdominal wall is much thinner beneath the panniculus.
However, be aware that, even in a supine patient with a leftward tilt, the weight of the panniculus can decrease vena caval return and cause uteroplacental insufficiency and compromised maternal respiration. Cesarean delivery should be performed expediently for these reasons.
A self-retaining elastic abdominal retractor may improve exposure at the same time that it minimizes the amount of retraction that must be exerted by the surgical assistant ( FIGURE 2 ).
FIGURE 1 Retract the panniculus
Retract the panniculus toward the patient’s head and use straps to secure it to facilitate a Pfannenstiel incision.
FIGURE 2 Elastic abdominal retractor improves visibility and access
Insert the inner ring of the adjustable elastic retractor into the abdominal cavity toward the patient’s head until it springs open against the parietal peritoneum. The outer ring is then rolled onto the plastic sleeve until it is snug against the skin.
Prophylaxis is warranted
Preoperative prophylactic antibiotics (weight-based) and prophylaxis for venous thromboembolism using sequential compression devices are recommended prior to surgery.
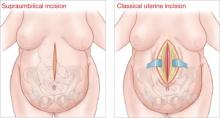
Data do not indicate whether vertical or transverse skin incisions for cesarean delivery are associated with higher infectious morbidity. In general, a Pfannenstiel incision is associated with less postoperative discomfort, allowing earlier mobilization and better respiratory function. A vertical incision allows optimal exposure, especially in the case of a macrosomic infant, and may thereby limit operating time and blood loss.7,8
A vertical supraumbilical incision is another option. If the lower uterine segment is not accessible, a fundal uterine incision can be made ( FIGURE 3 ). The advantage of this method is increased exposure as well as access to the incision for wound care. However, because this method may necessitate a classical uterine incision, counseling must be given regarding future pregnancy.
FIGURE 3 Pair incisions strategically to ease cesarean delivery
In an obese patient, a supraumbilical skin incision paired with a classical uterine incision may simplify the surgery.
Other intraoperative considerations
If the surgery is prolonged, consider administering another dose of antibiotics.
If the subcutaneous tissue is thicker than 2 cm, it should be reapproximated to minimize the risk of hematoma and seroma formation and wound infection.8,9
A subcutaneous drain should also be considered.
Be aware of special risks
One retrospective study showed an increased risk of postpartum hemorrhage in women who had a BMI above 25, compared with women of normal weight. This risk increased as BMI increased. Knowledge of this complication and early use of uterotonic agents can minimize the morbidity associated with postpartum hemorrhage.
Postpartum infection is more likely in obese women, with three times the risk of endometritis of women of normal weight, and increased risks of wound infection, urinary tract infection, septic pelvic thrombophlebitis, and pneumonia.10 Early recognition of infection and administration of antibiotics can minimize morbidity.
Venous thromboembolism is more likely throughout pregnancy in obese women. Risk is heightened, however, during the postpartum period, when it is four times as high as the risk in women of normal weight.11 Early ambulation and use of venous compression devices are encouraged. Consider heparin in the immediate postpartum period, when mobility is compromised for a longer period, particularly for women undergoing cesarean delivery who have comorbidities.
Suggest breastfeeding, weight loss
Women who breastfeed longer than 1 month have a 22% reduction in the risk of developing metabolic syndrome later in life, compared with women who do not. It also appears that a longer duration of breastfeeding reduces the risk of diabetes.12
Weight loss should be strongly encouraged. Women who retained their pregnancy weight at 6 months were 18 lb heavier after 10 years than women who lost their pregnancy weight.
The risk of metabolic syndrome increases with parity, probably because of the tendency of many obese women to retain their pregnancy weight.12
1. Sukalich S, Mingione MJ, Glantz JC. Obstetric outcomes in overweight and obese adolescents. Am J Obstet Gynecol. 2006;195:851-855.
2. Vickers M. Developmental programming and adult obesity: the role of leptin. Curr Opin Endocrinol Diabetes Obes. 2007;14:17-22.
3. Mazouni C, Porcu G, Cohen-Solal E, et al. Maternal and anthropomorphic risk factors for shoulder dystocia. Acta Obstet Gynecol Scand. 2006;85:567-570.
4. Juhasz G, Gyamfi C, Gyamfi P, Tocce K, Stone JL. Effect of body mass index and excessive weight gain on success of vaginal birth after cesarean delivery. Obstet Gynecol. 2005;106:741-746.
5. Hibbard JU, Gilbert S, Landon MB, et al. National Institute of Child Health and Human Development Maternal–Fetal Medicine Units Network. Trial of labor or repeat cesarean delivery in women with morbid obesity and previous cesarean delivery. Obstet Gynecol. 2006;108:125-133.
6. Weiss JL, Malone FD, Emig D, et al:. FASTER Research Consortium. Obesity, obstetric complications and cesarean delivery rate—a population-based screening study. Am J Obstet Gynecol. 2004;190:1091-1097.
7. Wall PD, Deucy EE, Glantz JC, Pressman EK. Vertical skin incisions and wound complications in the obese parturient. Obstet Gynecol. 2003;102(5 Pt 1):952-956.
8. Alexander CI, Liston WA. Operating on the obese woman—a review. BJOG. 2006;113:1167-1172.
9. Ramsey PS, White AM, Guinn DA, et al. Subcutaneous tissue reapproximation, alone or in combination with drain, in obese women undergoing cesarean delivery. Obstet Gynecol. 2005;105(5 Pt 1):967-973.
10. Myles TD, Gooch J, Santolaya J. Obesity as an independent risk factor for infectious morbidity in patients who undergo cesarean delivery. Obstet Gynecol. 2002;100(5 Pt 1):959-964.
11. James AH, Jamison MG, Brancazio LR, Myers ER. Venous thromboembolism during pregnancy and the postpartum period: incidence, risk factors, and mortality. Am J Obstet Gynecol. 2006;194:1311-1315.
12. Bentley-Lewis R, Koruda K, Seely EW. The metabolic syndrome in women. Nat Clin Pract Endocrinol Metab. 2007;3:696-704.
The authors report no financial relationships relevant to this article.
Hear Dr Phillips discuss the key points of this series
With the ranks of the obese expanding, and the severity of obesity increasing as well, obstetricians see a greater percentage of obese and morbidly obese gravidas in their practice. At the end of pregnancy, when it is time to deliver the infant, a number of issues must be taken into account to ensure the safety and health of both mother and child. Part 2 of this two-part article discusses these issues, from intrapartum and intraoperative considerations to care during the postpartum period.
Intrapartum concerns
Induction of labor
Obese women are more likely to require induction of labor; they should be counseled accordingly. The rate of labor induction is as high as 35% in women who have a body mass index (BMI) above 35.1 Many of these inductions are indicated for maternal disease such as diabetes or preeclampsia. However, data suggest that obesity alone increases the induction rate, possibly through increased levels of leptin (an adipokine involved in obesity, appetite, and satiety), which may inhibit uterine contractions.2
Uterine and fetal monitoring
Monitoring of uterine contractions and fetal heart rate can be challenging in obese women. Early use of an intra uterine pressure catheter and fetal scalp electrode can help.
Shoulder dystocia
Obesity is a risk factor for macrosomia, which increases the likelihood of shoulder dystocia. In addition, at least one study supports maternal obesity as an independent risk factor for shoulder dystocia. Women who had a BMI above 30 were 2.7 times more likely to have a pregnancy complicated by shoulder dystocia, after adjustment for macrosomia, diabetes, parity, and induction of labor.3
Because of this risk, appropriate staff should be readily available for assistance, and operative vaginal delivery should be performed with caution, if at all.
Vaginal birth after cesarean delivery
Obese women who have a history of cesarean delivery need to be counseled about the higher risk of failed vaginal birth after cesarean (VBAC) and the likely need for repeat cesarean delivery. They also need to be told about the elevated risk of infection in the event that VBAC fails.
In women of normal weight, the likelihood of successful VBAC exceeds 80%, compared with a success rate of 68% for women who have a BMI above 29, and 60% for women who have a BMI above 40.4,5
Appropriate counseling and patient selection are critical components of the decision to proceed with a trial of labor in obese women who have a history of cesarean delivery. Twenty-four-hour anesthesia and NICU coverage are also necessary in case emergent cesarean delivery becomes necessary.
Cesarean delivery
Morbidly obese women (BMI >35) have approximately a 50% greater chance of requiring cesarean delivery than do women of normal weight.6 The need for cesarean delivery rises with increasing BMI, probably because of a greater degree of maternal pelvic soft tissue, which increases the risk of both dystocia and cephalopelvic disproportion.
Anesthesia
It may be advisable to place an early epidural in laboring obese patients because they are more likely to require multiple placement attempts and cesarean delivery.
Intraoperative considerations
Ensure availability of the proper equipment
Table extenders, appropriate retractors, and long instruments should be readily available before surgery. For example, obstetricians often retract the panniculus to allow for a Pfannenstiel skin incision ( FIGURE 1 ), which works well to increase exposure. Moreover, the depth of the abdominal wall is much thinner beneath the panniculus.
However, be aware that, even in a supine patient with a leftward tilt, the weight of the panniculus can decrease vena caval return and cause uteroplacental insufficiency and compromised maternal respiration. Cesarean delivery should be performed expediently for these reasons.
A self-retaining elastic abdominal retractor may improve exposure at the same time that it minimizes the amount of retraction that must be exerted by the surgical assistant ( FIGURE 2 ).
FIGURE 1 Retract the panniculus
Retract the panniculus toward the patient’s head and use straps to secure it to facilitate a Pfannenstiel incision.
FIGURE 2 Elastic abdominal retractor improves visibility and access
Insert the inner ring of the adjustable elastic retractor into the abdominal cavity toward the patient’s head until it springs open against the parietal peritoneum. The outer ring is then rolled onto the plastic sleeve until it is snug against the skin.
Prophylaxis is warranted
Preoperative prophylactic antibiotics (weight-based) and prophylaxis for venous thromboembolism using sequential compression devices are recommended prior to surgery.
Data do not indicate whether vertical or transverse skin incisions for cesarean delivery are associated with higher infectious morbidity. In general, a Pfannenstiel incision is associated with less postoperative discomfort, allowing earlier mobilization and better respiratory function. A vertical incision allows optimal exposure, especially in the case of a macrosomic infant, and may thereby limit operating time and blood loss.7,8
A vertical supraumbilical incision is another option. If the lower uterine segment is not accessible, a fundal uterine incision can be made ( FIGURE 3 ). The advantage of this method is increased exposure as well as access to the incision for wound care. However, because this method may necessitate a classical uterine incision, counseling must be given regarding future pregnancy.
FIGURE 3 Pair incisions strategically to ease cesarean delivery
In an obese patient, a supraumbilical skin incision paired with a classical uterine incision may simplify the surgery.
Other intraoperative considerations
If the surgery is prolonged, consider administering another dose of antibiotics.
If the subcutaneous tissue is thicker than 2 cm, it should be reapproximated to minimize the risk of hematoma and seroma formation and wound infection.8,9
A subcutaneous drain should also be considered.
Be aware of special risks
One retrospective study showed an increased risk of postpartum hemorrhage in women who had a BMI above 25, compared with women of normal weight. This risk increased as BMI increased. Knowledge of this complication and early use of uterotonic agents can minimize the morbidity associated with postpartum hemorrhage.
Postpartum infection is more likely in obese women, with three times the risk of endometritis of women of normal weight, and increased risks of wound infection, urinary tract infection, septic pelvic thrombophlebitis, and pneumonia.10 Early recognition of infection and administration of antibiotics can minimize morbidity.
Venous thromboembolism is more likely throughout pregnancy in obese women. Risk is heightened, however, during the postpartum period, when it is four times as high as the risk in women of normal weight.11 Early ambulation and use of venous compression devices are encouraged. Consider heparin in the immediate postpartum period, when mobility is compromised for a longer period, particularly for women undergoing cesarean delivery who have comorbidities.
Suggest breastfeeding, weight loss
Women who breastfeed longer than 1 month have a 22% reduction in the risk of developing metabolic syndrome later in life, compared with women who do not. It also appears that a longer duration of breastfeeding reduces the risk of diabetes.12
Weight loss should be strongly encouraged. Women who retained their pregnancy weight at 6 months were 18 lb heavier after 10 years than women who lost their pregnancy weight.
The risk of metabolic syndrome increases with parity, probably because of the tendency of many obese women to retain their pregnancy weight.12
The authors report no financial relationships relevant to this article.
Hear Dr Phillips discuss the key points of this series
With the ranks of the obese expanding, and the severity of obesity increasing as well, obstetricians see a greater percentage of obese and morbidly obese gravidas in their practice. At the end of pregnancy, when it is time to deliver the infant, a number of issues must be taken into account to ensure the safety and health of both mother and child. Part 2 of this two-part article discusses these issues, from intrapartum and intraoperative considerations to care during the postpartum period.
Intrapartum concerns
Induction of labor
Obese women are more likely to require induction of labor; they should be counseled accordingly. The rate of labor induction is as high as 35% in women who have a body mass index (BMI) above 35.1 Many of these inductions are indicated for maternal disease such as diabetes or preeclampsia. However, data suggest that obesity alone increases the induction rate, possibly through increased levels of leptin (an adipokine involved in obesity, appetite, and satiety), which may inhibit uterine contractions.2
Uterine and fetal monitoring
Monitoring of uterine contractions and fetal heart rate can be challenging in obese women. Early use of an intra uterine pressure catheter and fetal scalp electrode can help.
Shoulder dystocia
Obesity is a risk factor for macrosomia, which increases the likelihood of shoulder dystocia. In addition, at least one study supports maternal obesity as an independent risk factor for shoulder dystocia. Women who had a BMI above 30 were 2.7 times more likely to have a pregnancy complicated by shoulder dystocia, after adjustment for macrosomia, diabetes, parity, and induction of labor.3
Because of this risk, appropriate staff should be readily available for assistance, and operative vaginal delivery should be performed with caution, if at all.
Vaginal birth after cesarean delivery
Obese women who have a history of cesarean delivery need to be counseled about the higher risk of failed vaginal birth after cesarean (VBAC) and the likely need for repeat cesarean delivery. They also need to be told about the elevated risk of infection in the event that VBAC fails.
In women of normal weight, the likelihood of successful VBAC exceeds 80%, compared with a success rate of 68% for women who have a BMI above 29, and 60% for women who have a BMI above 40.4,5
Appropriate counseling and patient selection are critical components of the decision to proceed with a trial of labor in obese women who have a history of cesarean delivery. Twenty-four-hour anesthesia and NICU coverage are also necessary in case emergent cesarean delivery becomes necessary.
Cesarean delivery
Morbidly obese women (BMI >35) have approximately a 50% greater chance of requiring cesarean delivery than do women of normal weight.6 The need for cesarean delivery rises with increasing BMI, probably because of a greater degree of maternal pelvic soft tissue, which increases the risk of both dystocia and cephalopelvic disproportion.
Anesthesia
It may be advisable to place an early epidural in laboring obese patients because they are more likely to require multiple placement attempts and cesarean delivery.
Intraoperative considerations
Ensure availability of the proper equipment
Table extenders, appropriate retractors, and long instruments should be readily available before surgery. For example, obstetricians often retract the panniculus to allow for a Pfannenstiel skin incision ( FIGURE 1 ), which works well to increase exposure. Moreover, the depth of the abdominal wall is much thinner beneath the panniculus.
However, be aware that, even in a supine patient with a leftward tilt, the weight of the panniculus can decrease vena caval return and cause uteroplacental insufficiency and compromised maternal respiration. Cesarean delivery should be performed expediently for these reasons.
A self-retaining elastic abdominal retractor may improve exposure at the same time that it minimizes the amount of retraction that must be exerted by the surgical assistant ( FIGURE 2 ).
FIGURE 1 Retract the panniculus
Retract the panniculus toward the patient’s head and use straps to secure it to facilitate a Pfannenstiel incision.
FIGURE 2 Elastic abdominal retractor improves visibility and access
Insert the inner ring of the adjustable elastic retractor into the abdominal cavity toward the patient’s head until it springs open against the parietal peritoneum. The outer ring is then rolled onto the plastic sleeve until it is snug against the skin.
Prophylaxis is warranted
Preoperative prophylactic antibiotics (weight-based) and prophylaxis for venous thromboembolism using sequential compression devices are recommended prior to surgery.
Data do not indicate whether vertical or transverse skin incisions for cesarean delivery are associated with higher infectious morbidity. In general, a Pfannenstiel incision is associated with less postoperative discomfort, allowing earlier mobilization and better respiratory function. A vertical incision allows optimal exposure, especially in the case of a macrosomic infant, and may thereby limit operating time and blood loss.7,8
A vertical supraumbilical incision is another option. If the lower uterine segment is not accessible, a fundal uterine incision can be made ( FIGURE 3 ). The advantage of this method is increased exposure as well as access to the incision for wound care. However, because this method may necessitate a classical uterine incision, counseling must be given regarding future pregnancy.
FIGURE 3 Pair incisions strategically to ease cesarean delivery
In an obese patient, a supraumbilical skin incision paired with a classical uterine incision may simplify the surgery.
Other intraoperative considerations
If the surgery is prolonged, consider administering another dose of antibiotics.
If the subcutaneous tissue is thicker than 2 cm, it should be reapproximated to minimize the risk of hematoma and seroma formation and wound infection.8,9
A subcutaneous drain should also be considered.
Be aware of special risks
One retrospective study showed an increased risk of postpartum hemorrhage in women who had a BMI above 25, compared with women of normal weight. This risk increased as BMI increased. Knowledge of this complication and early use of uterotonic agents can minimize the morbidity associated with postpartum hemorrhage.
Postpartum infection is more likely in obese women, with three times the risk of endometritis of women of normal weight, and increased risks of wound infection, urinary tract infection, septic pelvic thrombophlebitis, and pneumonia.10 Early recognition of infection and administration of antibiotics can minimize morbidity.
Venous thromboembolism is more likely throughout pregnancy in obese women. Risk is heightened, however, during the postpartum period, when it is four times as high as the risk in women of normal weight.11 Early ambulation and use of venous compression devices are encouraged. Consider heparin in the immediate postpartum period, when mobility is compromised for a longer period, particularly for women undergoing cesarean delivery who have comorbidities.
Suggest breastfeeding, weight loss
Women who breastfeed longer than 1 month have a 22% reduction in the risk of developing metabolic syndrome later in life, compared with women who do not. It also appears that a longer duration of breastfeeding reduces the risk of diabetes.12
Weight loss should be strongly encouraged. Women who retained their pregnancy weight at 6 months were 18 lb heavier after 10 years than women who lost their pregnancy weight.
The risk of metabolic syndrome increases with parity, probably because of the tendency of many obese women to retain their pregnancy weight.12
1. Sukalich S, Mingione MJ, Glantz JC. Obstetric outcomes in overweight and obese adolescents. Am J Obstet Gynecol. 2006;195:851-855.
2. Vickers M. Developmental programming and adult obesity: the role of leptin. Curr Opin Endocrinol Diabetes Obes. 2007;14:17-22.
3. Mazouni C, Porcu G, Cohen-Solal E, et al. Maternal and anthropomorphic risk factors for shoulder dystocia. Acta Obstet Gynecol Scand. 2006;85:567-570.
4. Juhasz G, Gyamfi C, Gyamfi P, Tocce K, Stone JL. Effect of body mass index and excessive weight gain on success of vaginal birth after cesarean delivery. Obstet Gynecol. 2005;106:741-746.
5. Hibbard JU, Gilbert S, Landon MB, et al. National Institute of Child Health and Human Development Maternal–Fetal Medicine Units Network. Trial of labor or repeat cesarean delivery in women with morbid obesity and previous cesarean delivery. Obstet Gynecol. 2006;108:125-133.
6. Weiss JL, Malone FD, Emig D, et al:. FASTER Research Consortium. Obesity, obstetric complications and cesarean delivery rate—a population-based screening study. Am J Obstet Gynecol. 2004;190:1091-1097.
7. Wall PD, Deucy EE, Glantz JC, Pressman EK. Vertical skin incisions and wound complications in the obese parturient. Obstet Gynecol. 2003;102(5 Pt 1):952-956.
8. Alexander CI, Liston WA. Operating on the obese woman—a review. BJOG. 2006;113:1167-1172.
9. Ramsey PS, White AM, Guinn DA, et al. Subcutaneous tissue reapproximation, alone or in combination with drain, in obese women undergoing cesarean delivery. Obstet Gynecol. 2005;105(5 Pt 1):967-973.
10. Myles TD, Gooch J, Santolaya J. Obesity as an independent risk factor for infectious morbidity in patients who undergo cesarean delivery. Obstet Gynecol. 2002;100(5 Pt 1):959-964.
11. James AH, Jamison MG, Brancazio LR, Myers ER. Venous thromboembolism during pregnancy and the postpartum period: incidence, risk factors, and mortality. Am J Obstet Gynecol. 2006;194:1311-1315.
12. Bentley-Lewis R, Koruda K, Seely EW. The metabolic syndrome in women. Nat Clin Pract Endocrinol Metab. 2007;3:696-704.
1. Sukalich S, Mingione MJ, Glantz JC. Obstetric outcomes in overweight and obese adolescents. Am J Obstet Gynecol. 2006;195:851-855.
2. Vickers M. Developmental programming and adult obesity: the role of leptin. Curr Opin Endocrinol Diabetes Obes. 2007;14:17-22.
3. Mazouni C, Porcu G, Cohen-Solal E, et al. Maternal and anthropomorphic risk factors for shoulder dystocia. Acta Obstet Gynecol Scand. 2006;85:567-570.
4. Juhasz G, Gyamfi C, Gyamfi P, Tocce K, Stone JL. Effect of body mass index and excessive weight gain on success of vaginal birth after cesarean delivery. Obstet Gynecol. 2005;106:741-746.
5. Hibbard JU, Gilbert S, Landon MB, et al. National Institute of Child Health and Human Development Maternal–Fetal Medicine Units Network. Trial of labor or repeat cesarean delivery in women with morbid obesity and previous cesarean delivery. Obstet Gynecol. 2006;108:125-133.
6. Weiss JL, Malone FD, Emig D, et al:. FASTER Research Consortium. Obesity, obstetric complications and cesarean delivery rate—a population-based screening study. Am J Obstet Gynecol. 2004;190:1091-1097.
7. Wall PD, Deucy EE, Glantz JC, Pressman EK. Vertical skin incisions and wound complications in the obese parturient. Obstet Gynecol. 2003;102(5 Pt 1):952-956.
8. Alexander CI, Liston WA. Operating on the obese woman—a review. BJOG. 2006;113:1167-1172.
9. Ramsey PS, White AM, Guinn DA, et al. Subcutaneous tissue reapproximation, alone or in combination with drain, in obese women undergoing cesarean delivery. Obstet Gynecol. 2005;105(5 Pt 1):967-973.
10. Myles TD, Gooch J, Santolaya J. Obesity as an independent risk factor for infectious morbidity in patients who undergo cesarean delivery. Obstet Gynecol. 2002;100(5 Pt 1):959-964.
11. James AH, Jamison MG, Brancazio LR, Myers ER. Venous thromboembolism during pregnancy and the postpartum period: incidence, risk factors, and mortality. Am J Obstet Gynecol. 2006;194:1311-1315.
12. Bentley-Lewis R, Koruda K, Seely EW. The metabolic syndrome in women. Nat Clin Pract Endocrinol Metab. 2007;3:696-704.
PART 1 OF 2: For the obese gravida, try strong counseling and close follow-up
Hear Dr Phillips discuss the key points of this series
CASE: Obesity + coexisting conditions = complicated pregnancy and delivery
A 30-year-old gravida 8 para 5026 is referred from the clinic for evaluation of elevated blood pressure at 36 4/7 weeks’ gestation. She is morbidly obese, with a weight of 440 lb and a body mass index (BMI) of 67. She also has a history of chronic hypertension and was recently given a diagnosis of gestational diabetes, which has been controlled through diet.
Her reproductive history includes four full-term vaginal deliveries followed by cesarean delivery for malpresentation of twins. Her blood pressure is 180/100 mm Hg, and she has new-onset proteinuria (3+) and a headache. The diagnosis? Preeclampsia superimposed on chronic hypertension.
Induction of labor is initiated using a Foley bulb and oxytocin, and magnesium sulfate is given to prevent seizures. Over the next 48 hours there is minimal cervical change, and the patient develops chorioamnionitis, for which she is given intravenous antibiotics. A repeat cesarean delivery is performed via a Pfannenstiel skin incision. The surgery is uneventful, and the infant is healthy.
Are further complications likely?
Yes—additional complications are considerably more likely in this scenario than in one involving a patient of normal weight, especially given the patient’s chronic hypertension and gestational diabetes. Obesity can affect all aspects of pregnancy, from conception through the postpartum period, with the potential for significant adverse maternal and fetal outcomes, including maternal mortality.
As the number of obese women of reproductive age increases, obstetricians face new challenges in the management of complications during pregnancy, labor, delivery, and beyond. In Part 1 of this two-part article, we offer advice on how to counsel the obese patient about the very real risks she faces in pregnancy, and detail trimester-specific recommendations. In Part 2, which follows on page 51, we offer practical management strategies during intrapartum, intraoperative, and postpartum periods.
CASE CONTINUED
The patient becomes febrile and hypoxic on postoperative day 1. When a computed tomography scan fails to rule out pulmonary embolism, she is started on heparin.
On postoperative day 7, omentum is detected at the incision, and the patient is taken to the operating room, where fascial dehiscence is identified and necrotic tissue is debrided. Two days later, a wound vac and inferior vena cava filter are placed.
The patient is discharged to a rehabilitation center on postoperative day 22.
Management starts before conception
The most important strategy to prevent complications associated with obesity and pregnancy is prepregnancy weight loss. Ideally, all obese patients should have a prepregnancy consultation that includes the recommendation to lose weight before conception. At this consultation, the ObGyn should determine the patient’s BMI and risk category and advise her of the relevant maternal and fetal risks (page 51, we take up intrapartum and postpartum concerns.
1. Gray AD, Power ML, Zinberg S, Schulkin J. Assessment and management of obesity. Obstet Gynecol Surv. 2006;61:742-748.
2. Centers for Disease Control and Prevention. Physical activity for everyone. Atlanta: CDC. Available at www.cdc.gov/nccdphp/dnpa/physical/everyone/recommendations/index.htm. Accessed December 30, 2008.
3. Lashen H, Fear K, Sturdee DW. Obesity is associated with increased risk of first trimester and recurrent miscarriage: matched case-control study. Hum Reprod. 2004;19:1644-1646.
4. Institute of Medicine, Committee on Nutritional Status During Pregnancy. Nutrition during pregnancy. Washington, DC: National Academy Press; 1990.
5. Doherty DA, Magann EF, Francis J, Morrison JC, Newnham JP. Pre-pregnancy body mass index and pregnancy outcomes. Int J Gynaecol Obstet. 2006;95:242-247.
6. Waller DK, Shaw GM, Rasmussen SA, et al. National Birth Defects Prevention Study. Prepregnancy obesity as a risk factor for structural birth defects. Arch Pediatr Adolesc Med. 2007;161:745-750.
7. O’Brien TE, Ray JG, Chan WS. Maternal body mass index and the risk of preeclampsia: a systematic overview. Epidemiology. 2003;14:368-374.
8. Heiskanen N, Raatikainen K, Heinonen S. Fetal macrosomia—a continuing obstetric challenge. Biol Neonate. 2006;90:98-103.
9. Endler GC, Mariona FG, Sokol RJ, Stevenson LB. Anesthesia-related maternal mortality in Michigan, 1972 to 1984. Am J Obstet Gynecol. 1988;159:187-193.
10. Saravanakumar K, Rao SG, Cooper GM. Obesity and obstetric anaesthesia. Anaesthesia. 2006;61:36-48.
11. Salihu HM, Dunlop AL, Hedayatzadeh M, Alio AP, Kirby RS, Alexander GR. Extreme obesity and risk of stillbirth among black and white gravidas. Obstet Gynecol. 2007;110:552-557.
12. World Health Organization. Obesity and overweight. Fact sheet No. 311. Geneva, Switzerland: WHO; 2006. Available at: www.who.int/mediacentre/factsheets/fs311/en/index.html. Accessed December 30, 2008.
13. Centers for Disease Control and Prevention. Overweight and obesity. Atlanta: CDC. Available at: www.cdc.gov/nccdphp/dnpa/obesity/index.htm. Accessed December 30, 2008.
14. Bentley-Lewis R, Koruda K, Seely EW. The metabolic syndrome in women. Nat Clin Pract Endocrinol Metab. 2007;3:696-704.
15. Dixon JB, Dixon ME, O’Brien PE. Birth outcomes in obese women after laparoscopic adjustable gastric banding. Obstet Gynecol. 2005;106(5 Pt 1):966-972.
16. American College of Obstetricians and Gynecologists. Committee Opinion No. 315. Obesity in pregnancy. Washington, DC: ACOG; 2005.
Hear Dr Phillips discuss the key points of this series
CASE: Obesity + coexisting conditions = complicated pregnancy and delivery
A 30-year-old gravida 8 para 5026 is referred from the clinic for evaluation of elevated blood pressure at 36 4/7 weeks’ gestation. She is morbidly obese, with a weight of 440 lb and a body mass index (BMI) of 67. She also has a history of chronic hypertension and was recently given a diagnosis of gestational diabetes, which has been controlled through diet.
Her reproductive history includes four full-term vaginal deliveries followed by cesarean delivery for malpresentation of twins. Her blood pressure is 180/100 mm Hg, and she has new-onset proteinuria (3+) and a headache. The diagnosis? Preeclampsia superimposed on chronic hypertension.
Induction of labor is initiated using a Foley bulb and oxytocin, and magnesium sulfate is given to prevent seizures. Over the next 48 hours there is minimal cervical change, and the patient develops chorioamnionitis, for which she is given intravenous antibiotics. A repeat cesarean delivery is performed via a Pfannenstiel skin incision. The surgery is uneventful, and the infant is healthy.
Are further complications likely?
Yes—additional complications are considerably more likely in this scenario than in one involving a patient of normal weight, especially given the patient’s chronic hypertension and gestational diabetes. Obesity can affect all aspects of pregnancy, from conception through the postpartum period, with the potential for significant adverse maternal and fetal outcomes, including maternal mortality.
As the number of obese women of reproductive age increases, obstetricians face new challenges in the management of complications during pregnancy, labor, delivery, and beyond. In Part 1 of this two-part article, we offer advice on how to counsel the obese patient about the very real risks she faces in pregnancy, and detail trimester-specific recommendations. In Part 2, which follows on page 51, we offer practical management strategies during intrapartum, intraoperative, and postpartum periods.
CASE CONTINUED
The patient becomes febrile and hypoxic on postoperative day 1. When a computed tomography scan fails to rule out pulmonary embolism, she is started on heparin.
On postoperative day 7, omentum is detected at the incision, and the patient is taken to the operating room, where fascial dehiscence is identified and necrotic tissue is debrided. Two days later, a wound vac and inferior vena cava filter are placed.
The patient is discharged to a rehabilitation center on postoperative day 22.
Management starts before conception
The most important strategy to prevent complications associated with obesity and pregnancy is prepregnancy weight loss. Ideally, all obese patients should have a prepregnancy consultation that includes the recommendation to lose weight before conception. At this consultation, the ObGyn should determine the patient’s BMI and risk category and advise her of the relevant maternal and fetal risks (page 51, we take up intrapartum and postpartum concerns.
Hear Dr Phillips discuss the key points of this series
CASE: Obesity + coexisting conditions = complicated pregnancy and delivery
A 30-year-old gravida 8 para 5026 is referred from the clinic for evaluation of elevated blood pressure at 36 4/7 weeks’ gestation. She is morbidly obese, with a weight of 440 lb and a body mass index (BMI) of 67. She also has a history of chronic hypertension and was recently given a diagnosis of gestational diabetes, which has been controlled through diet.
Her reproductive history includes four full-term vaginal deliveries followed by cesarean delivery for malpresentation of twins. Her blood pressure is 180/100 mm Hg, and she has new-onset proteinuria (3+) and a headache. The diagnosis? Preeclampsia superimposed on chronic hypertension.
Induction of labor is initiated using a Foley bulb and oxytocin, and magnesium sulfate is given to prevent seizures. Over the next 48 hours there is minimal cervical change, and the patient develops chorioamnionitis, for which she is given intravenous antibiotics. A repeat cesarean delivery is performed via a Pfannenstiel skin incision. The surgery is uneventful, and the infant is healthy.
Are further complications likely?
Yes—additional complications are considerably more likely in this scenario than in one involving a patient of normal weight, especially given the patient’s chronic hypertension and gestational diabetes. Obesity can affect all aspects of pregnancy, from conception through the postpartum period, with the potential for significant adverse maternal and fetal outcomes, including maternal mortality.
As the number of obese women of reproductive age increases, obstetricians face new challenges in the management of complications during pregnancy, labor, delivery, and beyond. In Part 1 of this two-part article, we offer advice on how to counsel the obese patient about the very real risks she faces in pregnancy, and detail trimester-specific recommendations. In Part 2, which follows on page 51, we offer practical management strategies during intrapartum, intraoperative, and postpartum periods.
CASE CONTINUED
The patient becomes febrile and hypoxic on postoperative day 1. When a computed tomography scan fails to rule out pulmonary embolism, she is started on heparin.
On postoperative day 7, omentum is detected at the incision, and the patient is taken to the operating room, where fascial dehiscence is identified and necrotic tissue is debrided. Two days later, a wound vac and inferior vena cava filter are placed.
The patient is discharged to a rehabilitation center on postoperative day 22.
Management starts before conception
The most important strategy to prevent complications associated with obesity and pregnancy is prepregnancy weight loss. Ideally, all obese patients should have a prepregnancy consultation that includes the recommendation to lose weight before conception. At this consultation, the ObGyn should determine the patient’s BMI and risk category and advise her of the relevant maternal and fetal risks (page 51, we take up intrapartum and postpartum concerns.
1. Gray AD, Power ML, Zinberg S, Schulkin J. Assessment and management of obesity. Obstet Gynecol Surv. 2006;61:742-748.
2. Centers for Disease Control and Prevention. Physical activity for everyone. Atlanta: CDC. Available at www.cdc.gov/nccdphp/dnpa/physical/everyone/recommendations/index.htm. Accessed December 30, 2008.
3. Lashen H, Fear K, Sturdee DW. Obesity is associated with increased risk of first trimester and recurrent miscarriage: matched case-control study. Hum Reprod. 2004;19:1644-1646.
4. Institute of Medicine, Committee on Nutritional Status During Pregnancy. Nutrition during pregnancy. Washington, DC: National Academy Press; 1990.
5. Doherty DA, Magann EF, Francis J, Morrison JC, Newnham JP. Pre-pregnancy body mass index and pregnancy outcomes. Int J Gynaecol Obstet. 2006;95:242-247.
6. Waller DK, Shaw GM, Rasmussen SA, et al. National Birth Defects Prevention Study. Prepregnancy obesity as a risk factor for structural birth defects. Arch Pediatr Adolesc Med. 2007;161:745-750.
7. O’Brien TE, Ray JG, Chan WS. Maternal body mass index and the risk of preeclampsia: a systematic overview. Epidemiology. 2003;14:368-374.
8. Heiskanen N, Raatikainen K, Heinonen S. Fetal macrosomia—a continuing obstetric challenge. Biol Neonate. 2006;90:98-103.
9. Endler GC, Mariona FG, Sokol RJ, Stevenson LB. Anesthesia-related maternal mortality in Michigan, 1972 to 1984. Am J Obstet Gynecol. 1988;159:187-193.
10. Saravanakumar K, Rao SG, Cooper GM. Obesity and obstetric anaesthesia. Anaesthesia. 2006;61:36-48.
11. Salihu HM, Dunlop AL, Hedayatzadeh M, Alio AP, Kirby RS, Alexander GR. Extreme obesity and risk of stillbirth among black and white gravidas. Obstet Gynecol. 2007;110:552-557.
12. World Health Organization. Obesity and overweight. Fact sheet No. 311. Geneva, Switzerland: WHO; 2006. Available at: www.who.int/mediacentre/factsheets/fs311/en/index.html. Accessed December 30, 2008.
13. Centers for Disease Control and Prevention. Overweight and obesity. Atlanta: CDC. Available at: www.cdc.gov/nccdphp/dnpa/obesity/index.htm. Accessed December 30, 2008.
14. Bentley-Lewis R, Koruda K, Seely EW. The metabolic syndrome in women. Nat Clin Pract Endocrinol Metab. 2007;3:696-704.
15. Dixon JB, Dixon ME, O’Brien PE. Birth outcomes in obese women after laparoscopic adjustable gastric banding. Obstet Gynecol. 2005;106(5 Pt 1):966-972.
16. American College of Obstetricians and Gynecologists. Committee Opinion No. 315. Obesity in pregnancy. Washington, DC: ACOG; 2005.
1. Gray AD, Power ML, Zinberg S, Schulkin J. Assessment and management of obesity. Obstet Gynecol Surv. 2006;61:742-748.
2. Centers for Disease Control and Prevention. Physical activity for everyone. Atlanta: CDC. Available at www.cdc.gov/nccdphp/dnpa/physical/everyone/recommendations/index.htm. Accessed December 30, 2008.
3. Lashen H, Fear K, Sturdee DW. Obesity is associated with increased risk of first trimester and recurrent miscarriage: matched case-control study. Hum Reprod. 2004;19:1644-1646.
4. Institute of Medicine, Committee on Nutritional Status During Pregnancy. Nutrition during pregnancy. Washington, DC: National Academy Press; 1990.
5. Doherty DA, Magann EF, Francis J, Morrison JC, Newnham JP. Pre-pregnancy body mass index and pregnancy outcomes. Int J Gynaecol Obstet. 2006;95:242-247.
6. Waller DK, Shaw GM, Rasmussen SA, et al. National Birth Defects Prevention Study. Prepregnancy obesity as a risk factor for structural birth defects. Arch Pediatr Adolesc Med. 2007;161:745-750.
7. O’Brien TE, Ray JG, Chan WS. Maternal body mass index and the risk of preeclampsia: a systematic overview. Epidemiology. 2003;14:368-374.
8. Heiskanen N, Raatikainen K, Heinonen S. Fetal macrosomia—a continuing obstetric challenge. Biol Neonate. 2006;90:98-103.
9. Endler GC, Mariona FG, Sokol RJ, Stevenson LB. Anesthesia-related maternal mortality in Michigan, 1972 to 1984. Am J Obstet Gynecol. 1988;159:187-193.
10. Saravanakumar K, Rao SG, Cooper GM. Obesity and obstetric anaesthesia. Anaesthesia. 2006;61:36-48.
11. Salihu HM, Dunlop AL, Hedayatzadeh M, Alio AP, Kirby RS, Alexander GR. Extreme obesity and risk of stillbirth among black and white gravidas. Obstet Gynecol. 2007;110:552-557.
12. World Health Organization. Obesity and overweight. Fact sheet No. 311. Geneva, Switzerland: WHO; 2006. Available at: www.who.int/mediacentre/factsheets/fs311/en/index.html. Accessed December 30, 2008.
13. Centers for Disease Control and Prevention. Overweight and obesity. Atlanta: CDC. Available at: www.cdc.gov/nccdphp/dnpa/obesity/index.htm. Accessed December 30, 2008.
14. Bentley-Lewis R, Koruda K, Seely EW. The metabolic syndrome in women. Nat Clin Pract Endocrinol Metab. 2007;3:696-704.
15. Dixon JB, Dixon ME, O’Brien PE. Birth outcomes in obese women after laparoscopic adjustable gastric banding. Obstet Gynecol. 2005;106(5 Pt 1):966-972.
16. American College of Obstetricians and Gynecologists. Committee Opinion No. 315. Obesity in pregnancy. Washington, DC: ACOG; 2005.