User login
Top pregnancy apps for your patients
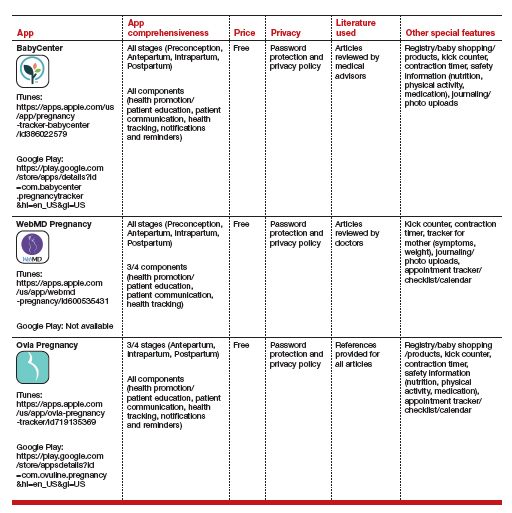
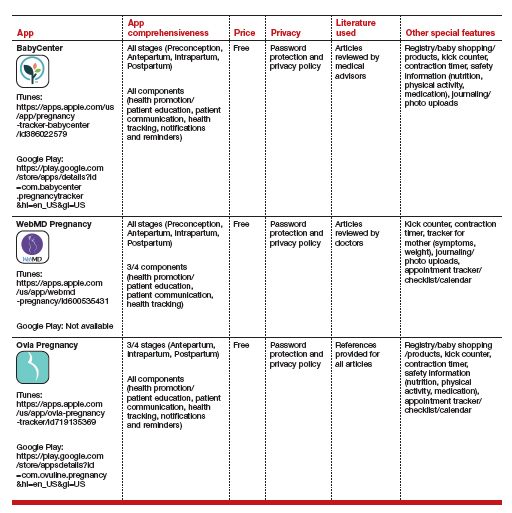
Pregnancy apps are more popular as patients use the internet to seek information about pregnancy and childbirth.1 Research has shown that over 50% of pregnant patients download apps focused on pregnancy, with an average of 3 being tried.2 This is especially true during the COVID-19 pandemic, when patients seek information but may want to minimize clinical exposures. Other research has shown that women primarily use apps to monitor fetal development and to obtain information on nutrition and antenatal care.3
We identified apps and rated their contents and features.4 To identify the apps, we performed a Google search to mimic what a patient may do. We scored the identified apps based on what has been shown to make apps successful, as well as desired functions of the most commonly used apps. The quality of the applications was relatively varied, with many of the apps (60%) not having comprehensive information for every stage of pregnancy and no app attaining a perfect score. However, the top 3 apps had near perfect scores of 15/16 and 14/16, missing points only for having advertisements and requiring an internet connection.
The table details these top 3 recommended pregnancy apps, along with a detailed shortened version of the APPLICATIONS scoring system, APPLI (App comprehensiveness, Price, Platform, Literature Used, Other special features). We hope this column will help you feel comfortable in helping patients use pregnancy apps, should they ask for recommendations.
1. Romano AM. A changing landscape: implications of pregnant women’s internet use for childbirth educators. J Perinat Educ. 2007;16:18-24. doi: 10.1624/105812407X244903.
2. Jayaseelan R, Pichandy C, Rushandramani D. Usage of smartphone apps by women on their maternal life. J Mass Communicat Journalism. 2015;29:05:158-164. doi: 10.4172/2165-7912.1000267.
3. Wang N, Deng Z, Wen LM, et al. Understanding the use of smartphone apps for health information among pregnant Chinese women: mixed methods study. JMIR mHealth uHealth. 2019;18:7:e12631. doi: 10.2196/12631.
4. Frid G, Bogaert K, Chen KT. Mobile health apps for pregnant women: systematic search, evaluation, and analysis of features. J Med Internet Res. 2021;18:23:e25667. doi: 10.2196/25667.
Pregnancy apps are more popular as patients use the internet to seek information about pregnancy and childbirth.1 Research has shown that over 50% of pregnant patients download apps focused on pregnancy, with an average of 3 being tried.2 This is especially true during the COVID-19 pandemic, when patients seek information but may want to minimize clinical exposures. Other research has shown that women primarily use apps to monitor fetal development and to obtain information on nutrition and antenatal care.3
We identified apps and rated their contents and features.4 To identify the apps, we performed a Google search to mimic what a patient may do. We scored the identified apps based on what has been shown to make apps successful, as well as desired functions of the most commonly used apps. The quality of the applications was relatively varied, with many of the apps (60%) not having comprehensive information for every stage of pregnancy and no app attaining a perfect score. However, the top 3 apps had near perfect scores of 15/16 and 14/16, missing points only for having advertisements and requiring an internet connection.
The table details these top 3 recommended pregnancy apps, along with a detailed shortened version of the APPLICATIONS scoring system, APPLI (App comprehensiveness, Price, Platform, Literature Used, Other special features). We hope this column will help you feel comfortable in helping patients use pregnancy apps, should they ask for recommendations.
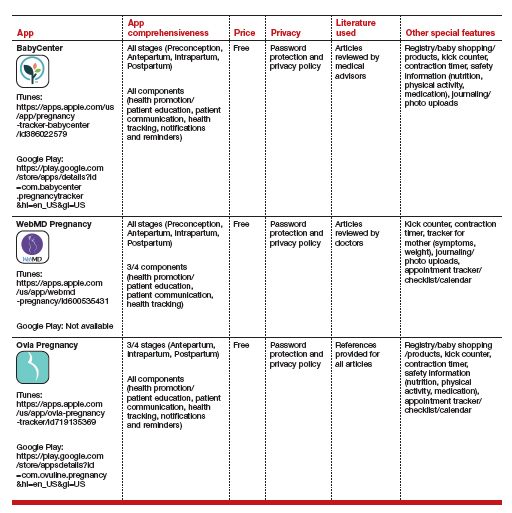
Pregnancy apps are more popular as patients use the internet to seek information about pregnancy and childbirth.1 Research has shown that over 50% of pregnant patients download apps focused on pregnancy, with an average of 3 being tried.2 This is especially true during the COVID-19 pandemic, when patients seek information but may want to minimize clinical exposures. Other research has shown that women primarily use apps to monitor fetal development and to obtain information on nutrition and antenatal care.3
We identified apps and rated their contents and features.4 To identify the apps, we performed a Google search to mimic what a patient may do. We scored the identified apps based on what has been shown to make apps successful, as well as desired functions of the most commonly used apps. The quality of the applications was relatively varied, with many of the apps (60%) not having comprehensive information for every stage of pregnancy and no app attaining a perfect score. However, the top 3 apps had near perfect scores of 15/16 and 14/16, missing points only for having advertisements and requiring an internet connection.
The table details these top 3 recommended pregnancy apps, along with a detailed shortened version of the APPLICATIONS scoring system, APPLI (App comprehensiveness, Price, Platform, Literature Used, Other special features). We hope this column will help you feel comfortable in helping patients use pregnancy apps, should they ask for recommendations.
1. Romano AM. A changing landscape: implications of pregnant women’s internet use for childbirth educators. J Perinat Educ. 2007;16:18-24. doi: 10.1624/105812407X244903.
2. Jayaseelan R, Pichandy C, Rushandramani D. Usage of smartphone apps by women on their maternal life. J Mass Communicat Journalism. 2015;29:05:158-164. doi: 10.4172/2165-7912.1000267.
3. Wang N, Deng Z, Wen LM, et al. Understanding the use of smartphone apps for health information among pregnant Chinese women: mixed methods study. JMIR mHealth uHealth. 2019;18:7:e12631. doi: 10.2196/12631.
4. Frid G, Bogaert K, Chen KT. Mobile health apps for pregnant women: systematic search, evaluation, and analysis of features. J Med Internet Res. 2021;18:23:e25667. doi: 10.2196/25667.
1. Romano AM. A changing landscape: implications of pregnant women’s internet use for childbirth educators. J Perinat Educ. 2007;16:18-24. doi: 10.1624/105812407X244903.
2. Jayaseelan R, Pichandy C, Rushandramani D. Usage of smartphone apps by women on their maternal life. J Mass Communicat Journalism. 2015;29:05:158-164. doi: 10.4172/2165-7912.1000267.
3. Wang N, Deng Z, Wen LM, et al. Understanding the use of smartphone apps for health information among pregnant Chinese women: mixed methods study. JMIR mHealth uHealth. 2019;18:7:e12631. doi: 10.2196/12631.
4. Frid G, Bogaert K, Chen KT. Mobile health apps for pregnant women: systematic search, evaluation, and analysis of features. J Med Internet Res. 2021;18:23:e25667. doi: 10.2196/25667.
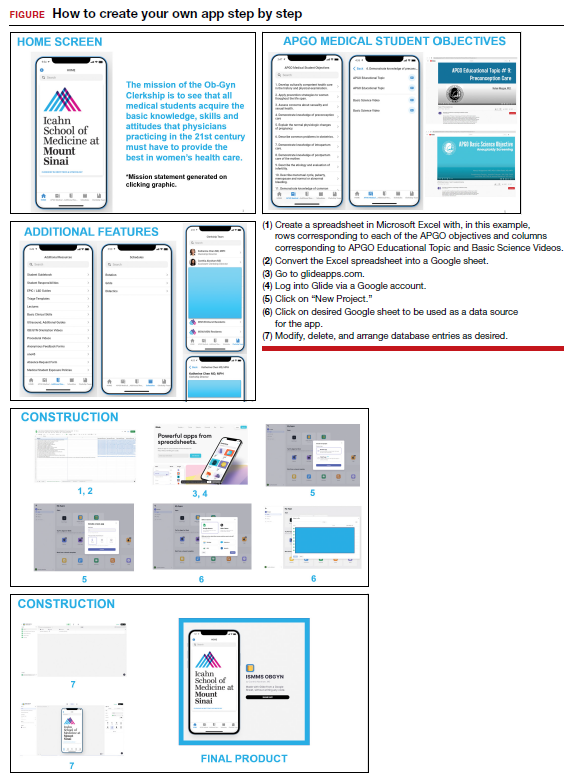
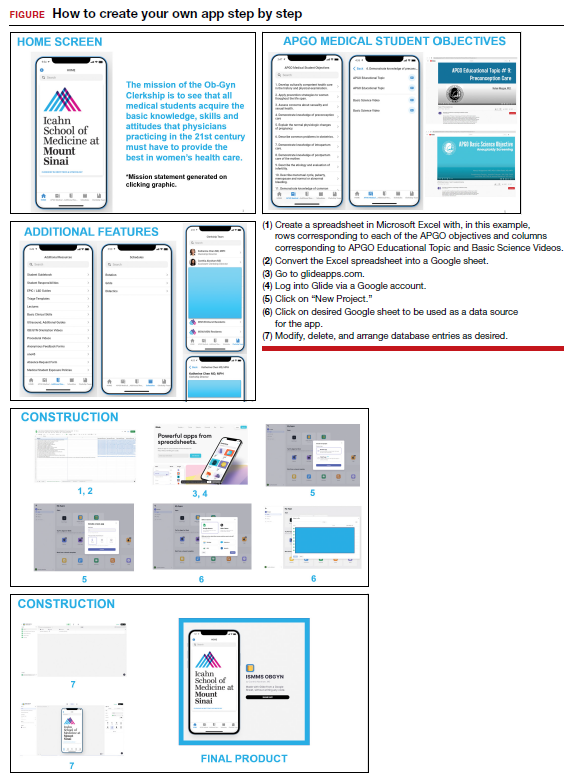
Home-grown apps for ObGyn clerkship students
Technology has revolutionized how we access information. One example is the increased use of mobile applications (apps). On the surface, building a new app may seem a daunting and intimidating task. However, new software—such as Glide (glideapps.com)—make it easy for anyone to design, build, and launch a custom web app within hours. This software is free for basic apps but does offer an upgrade for those wanting more professional services (glide-apps.com/pro). Here, by way of example, we identify an area of need and walk the reader
through the process of making an app.
Although there are many apps aimed at educating users on different aspects of obstetrics and gynecology, few are focused on undergraduate medical education (UME). With the assistance of Glide app building software, we created an app focused on providing rapid access to resources aimed at fulfilling medical student objectives from the Association of Professors of Gynecology and Obstetrics (APGO).1 We included 16 of the APGO objectives. On clicking an objective, the user is taken to a screen with links to associated APGO Educational Topic Video and Basic Science Videos. Basic Science Video links were included in order to provide longitudinal learning between the pre-clinical and clinical years of UME. We also created a tab for additional educational resources (including excerpts from the APGO Basic Clinical Skills Curriculum).2 We eventually added two other tabs: one for clerkship schedules that allows students to organize their daily schedule and another that facilitates quick contact with members of the clerkship team. As expected, the app was well-received by our students.
The steps needed for you to make your own app are listed in the FIGURE along with accompanying images for easy navigation. ●
- Association of Professors of Gynecology and Obstetrics (APGO) Medical Student Educational Objectives, 11th ed;2019.
- Association of Professors of Gynecology and Obstetrics (APGO) Basic Clinical Skills Curriculum. Updated 2017.
Technology has revolutionized how we access information. One example is the increased use of mobile applications (apps). On the surface, building a new app may seem a daunting and intimidating task. However, new software—such as Glide (glideapps.com)—make it easy for anyone to design, build, and launch a custom web app within hours. This software is free for basic apps but does offer an upgrade for those wanting more professional services (glide-apps.com/pro). Here, by way of example, we identify an area of need and walk the reader
through the process of making an app.
Although there are many apps aimed at educating users on different aspects of obstetrics and gynecology, few are focused on undergraduate medical education (UME). With the assistance of Glide app building software, we created an app focused on providing rapid access to resources aimed at fulfilling medical student objectives from the Association of Professors of Gynecology and Obstetrics (APGO).1 We included 16 of the APGO objectives. On clicking an objective, the user is taken to a screen with links to associated APGO Educational Topic Video and Basic Science Videos. Basic Science Video links were included in order to provide longitudinal learning between the pre-clinical and clinical years of UME. We also created a tab for additional educational resources (including excerpts from the APGO Basic Clinical Skills Curriculum).2 We eventually added two other tabs: one for clerkship schedules that allows students to organize their daily schedule and another that facilitates quick contact with members of the clerkship team. As expected, the app was well-received by our students.
The steps needed for you to make your own app are listed in the FIGURE along with accompanying images for easy navigation. ●
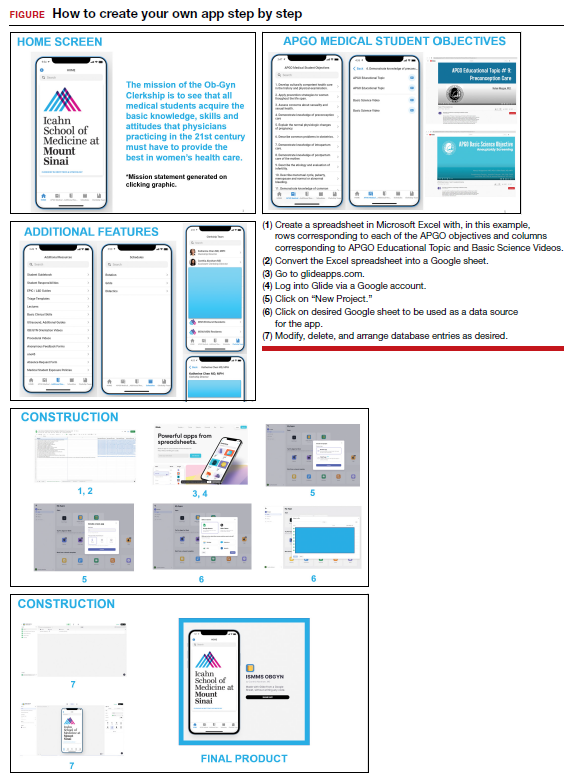
Technology has revolutionized how we access information. One example is the increased use of mobile applications (apps). On the surface, building a new app may seem a daunting and intimidating task. However, new software—such as Glide (glideapps.com)—make it easy for anyone to design, build, and launch a custom web app within hours. This software is free for basic apps but does offer an upgrade for those wanting more professional services (glide-apps.com/pro). Here, by way of example, we identify an area of need and walk the reader
through the process of making an app.
Although there are many apps aimed at educating users on different aspects of obstetrics and gynecology, few are focused on undergraduate medical education (UME). With the assistance of Glide app building software, we created an app focused on providing rapid access to resources aimed at fulfilling medical student objectives from the Association of Professors of Gynecology and Obstetrics (APGO).1 We included 16 of the APGO objectives. On clicking an objective, the user is taken to a screen with links to associated APGO Educational Topic Video and Basic Science Videos. Basic Science Video links were included in order to provide longitudinal learning between the pre-clinical and clinical years of UME. We also created a tab for additional educational resources (including excerpts from the APGO Basic Clinical Skills Curriculum).2 We eventually added two other tabs: one for clerkship schedules that allows students to organize their daily schedule and another that facilitates quick contact with members of the clerkship team. As expected, the app was well-received by our students.
The steps needed for you to make your own app are listed in the FIGURE along with accompanying images for easy navigation. ●
- Association of Professors of Gynecology and Obstetrics (APGO) Medical Student Educational Objectives, 11th ed;2019.
- Association of Professors of Gynecology and Obstetrics (APGO) Basic Clinical Skills Curriculum. Updated 2017.
- Association of Professors of Gynecology and Obstetrics (APGO) Medical Student Educational Objectives, 11th ed;2019.
- Association of Professors of Gynecology and Obstetrics (APGO) Basic Clinical Skills Curriculum. Updated 2017.
Telehealth apps in ObGyn practice
The COVID-19 pandemic has presented increasing demands on health care systems internationally. In addition to redistribution of inpatient health care resources, outpatient care practices evolved, with health care providers offering streamlined access to care to patients via telehealth.
Due to updated insurance practices, physicians now can receive reimbursement via private insurers, Medicare, and Medicaid (as determined by states) for telehealth visits both related and unrelated to COVID-19 care. Increased telehealth use has advantages, including increased health care access, reduced in-clinic wait times, and reduced patient and physician travel time. Within the field of obstetrics and gynecology, clinicians have used telehealth to maintain access to prenatal maternity care while redirecting resources and minimizing the risk of COVID-19 transmission. Additional advantages include provision of care during expanded hours, including evenings and weekends, to increase patient access without increasing the demand on office support staff and the ability to bill for 5- to 10-minute phone counseling encounters.1 Research shows that patients express satisfaction regarding the quality of telehealth care in the setting of prenatal care.2
In February 2020, the American College of Obstetricians and Gynecologists (ACOG) released a Committee Opinion regarding telehealth use in ObGyn, a sign of telehealth’s likely long-standing role within the field.3 Within the statement, ACOG commented on the increasing application of telemedicine in all aspects of obstetrics and gynecology and recommended that physicians become acquainted with new technologies and consider using them in their practice.
There is a large opportunity for development of mobile applications (apps) to further streamline telehealth-based medical care. During the pandemic, the Centers for Medicare and Medicaid Services instituted waivers for telemedicine use on non-HIPAA (Health Insurance Portability and Accountability Act) compliant video communications products, such as Google+ Hangout and Skype. However, HIPAA-compliant video services are preferred, and many virtual apps have released methods for patient communication that meet HIPAA guidelines.1,4 These apps offer services such as phone- and video-based patient visits, appointment scheduling, secure physician-patient messaging, and electronic health record (EHR) documentation.
App recommendations
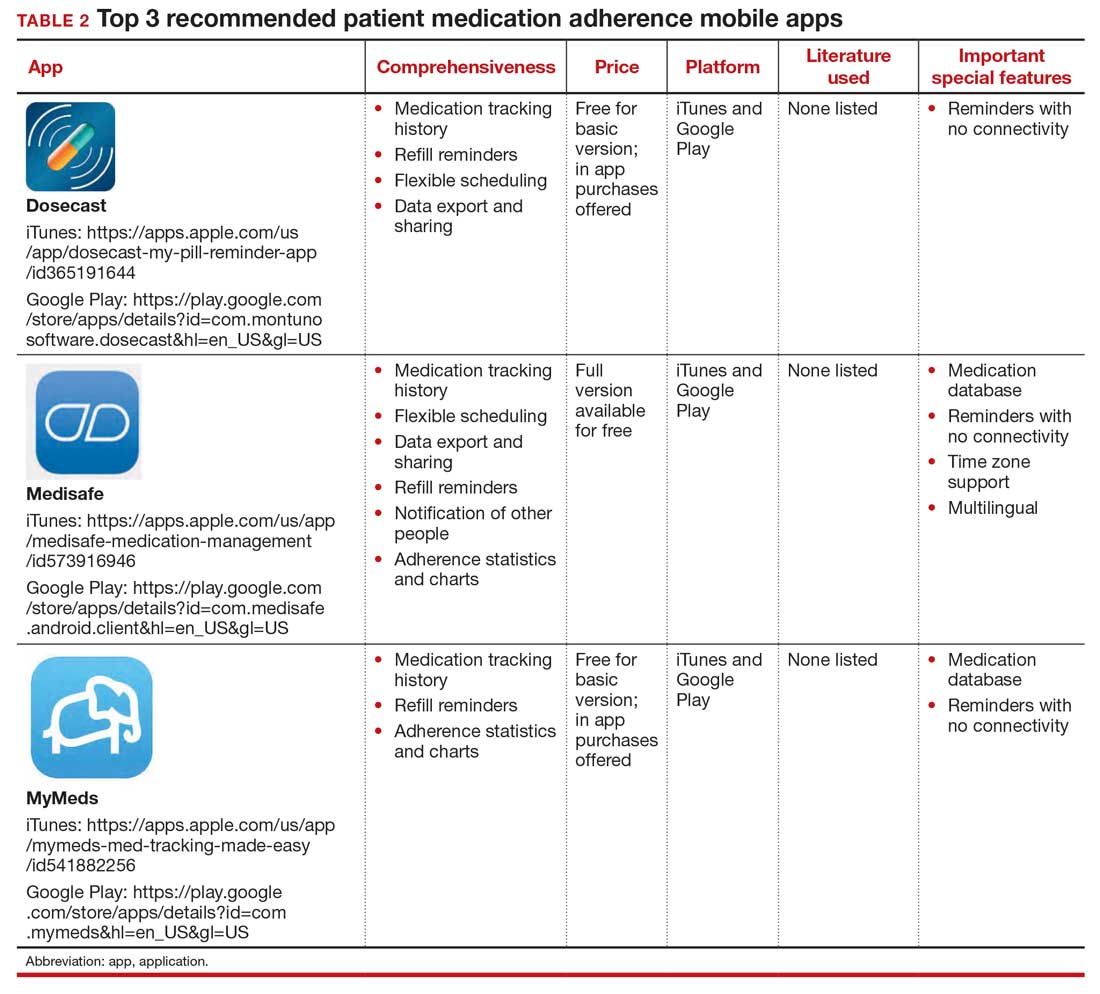
To identify current mobile apps with clinical use for the ObGyn, we conducted a search of the Apple App Store using the term “telehealth” between December 1, 2021 and January 1, 2022. We limited search results to apps that had at least 1,000 user ratings and to HIPAA-compliant user communication apps. Based on our review, we selected 4 apps to highlight here: Doximity, OhMD, Spruce, and Telehealth by SimplePractice (TABLE). We excluded apps that were advertised as having internal medical clinicians with first patient encounter on-demand through the app or that were associated with a singular insurance company or hospital system.
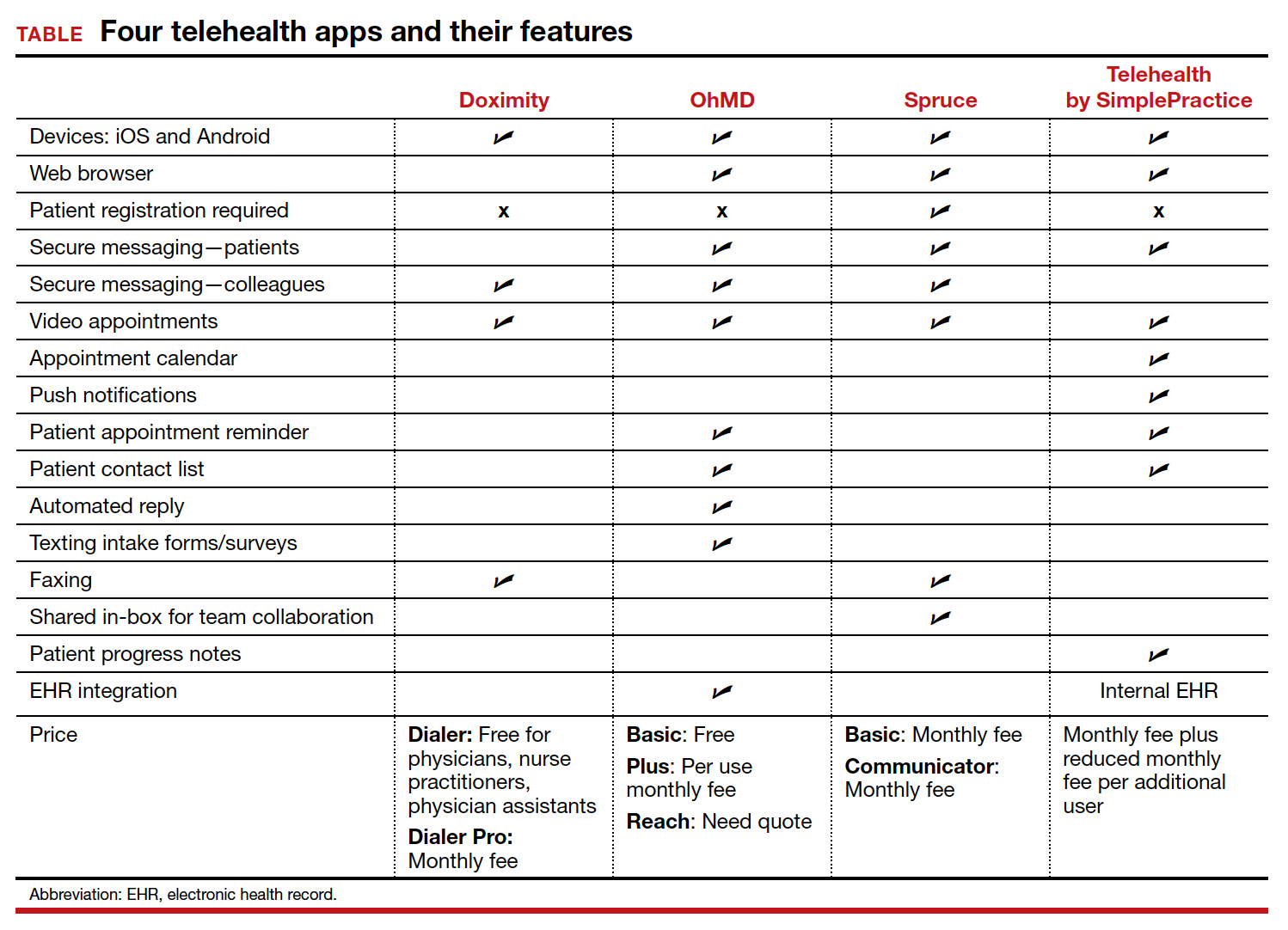
These apps are largely enabled for iOS and Android mobile devices and are offered at a range of price points for individual physician and practice-scale clinical implementation. Most apps offer secure messaging services between health care practitioners in addition to HIPAA-compliant patient messaging. Some apps offer additional features with the aim to increase patient attendance; these include push notifications, appointment reminders, and an option for automated replies with clinic information. For an additional fee, several apps offer integration to established EHR systems.
An additional tool
The COVID-19 pandemic caused health care systems and individual clinicians to rapidly evolve their practices to maintain patient access to essential health care. Notably, the pandemic led to accelerated implementation of virtual health care services. Telehealth apps likely will become another tool that ObGyns can use to improve the efficiency of their clinical practice and expand patient access to care. ●
- Karram M, Baum N. Telemedicine: a primer for today’s ObGyn. OBG Manag. 2020;32:28-32.
- Marko KI, Ganju N, Krapf JM, et al. A mobile prenatal care app to reduce in-person visits: prospective controlled trial. JMIR Mhealth Uhealth. 2019;7:e10520.
- American College of Obstetricians and Gynecologists. Implementing telehealth in practice: committee opinion no. 798. Obstet Gynecol. 2020;135:e73-e79.
- Karram M, Dooley A, de la Houssaye N, et al. Telemedicine: navigating legal issues. OBG Manag. 2020;32:18-24.
The COVID-19 pandemic has presented increasing demands on health care systems internationally. In addition to redistribution of inpatient health care resources, outpatient care practices evolved, with health care providers offering streamlined access to care to patients via telehealth.
Due to updated insurance practices, physicians now can receive reimbursement via private insurers, Medicare, and Medicaid (as determined by states) for telehealth visits both related and unrelated to COVID-19 care. Increased telehealth use has advantages, including increased health care access, reduced in-clinic wait times, and reduced patient and physician travel time. Within the field of obstetrics and gynecology, clinicians have used telehealth to maintain access to prenatal maternity care while redirecting resources and minimizing the risk of COVID-19 transmission. Additional advantages include provision of care during expanded hours, including evenings and weekends, to increase patient access without increasing the demand on office support staff and the ability to bill for 5- to 10-minute phone counseling encounters.1 Research shows that patients express satisfaction regarding the quality of telehealth care in the setting of prenatal care.2
In February 2020, the American College of Obstetricians and Gynecologists (ACOG) released a Committee Opinion regarding telehealth use in ObGyn, a sign of telehealth’s likely long-standing role within the field.3 Within the statement, ACOG commented on the increasing application of telemedicine in all aspects of obstetrics and gynecology and recommended that physicians become acquainted with new technologies and consider using them in their practice.
There is a large opportunity for development of mobile applications (apps) to further streamline telehealth-based medical care. During the pandemic, the Centers for Medicare and Medicaid Services instituted waivers for telemedicine use on non-HIPAA (Health Insurance Portability and Accountability Act) compliant video communications products, such as Google+ Hangout and Skype. However, HIPAA-compliant video services are preferred, and many virtual apps have released methods for patient communication that meet HIPAA guidelines.1,4 These apps offer services such as phone- and video-based patient visits, appointment scheduling, secure physician-patient messaging, and electronic health record (EHR) documentation.
App recommendations
To identify current mobile apps with clinical use for the ObGyn, we conducted a search of the Apple App Store using the term “telehealth” between December 1, 2021 and January 1, 2022. We limited search results to apps that had at least 1,000 user ratings and to HIPAA-compliant user communication apps. Based on our review, we selected 4 apps to highlight here: Doximity, OhMD, Spruce, and Telehealth by SimplePractice (TABLE). We excluded apps that were advertised as having internal medical clinicians with first patient encounter on-demand through the app or that were associated with a singular insurance company or hospital system.
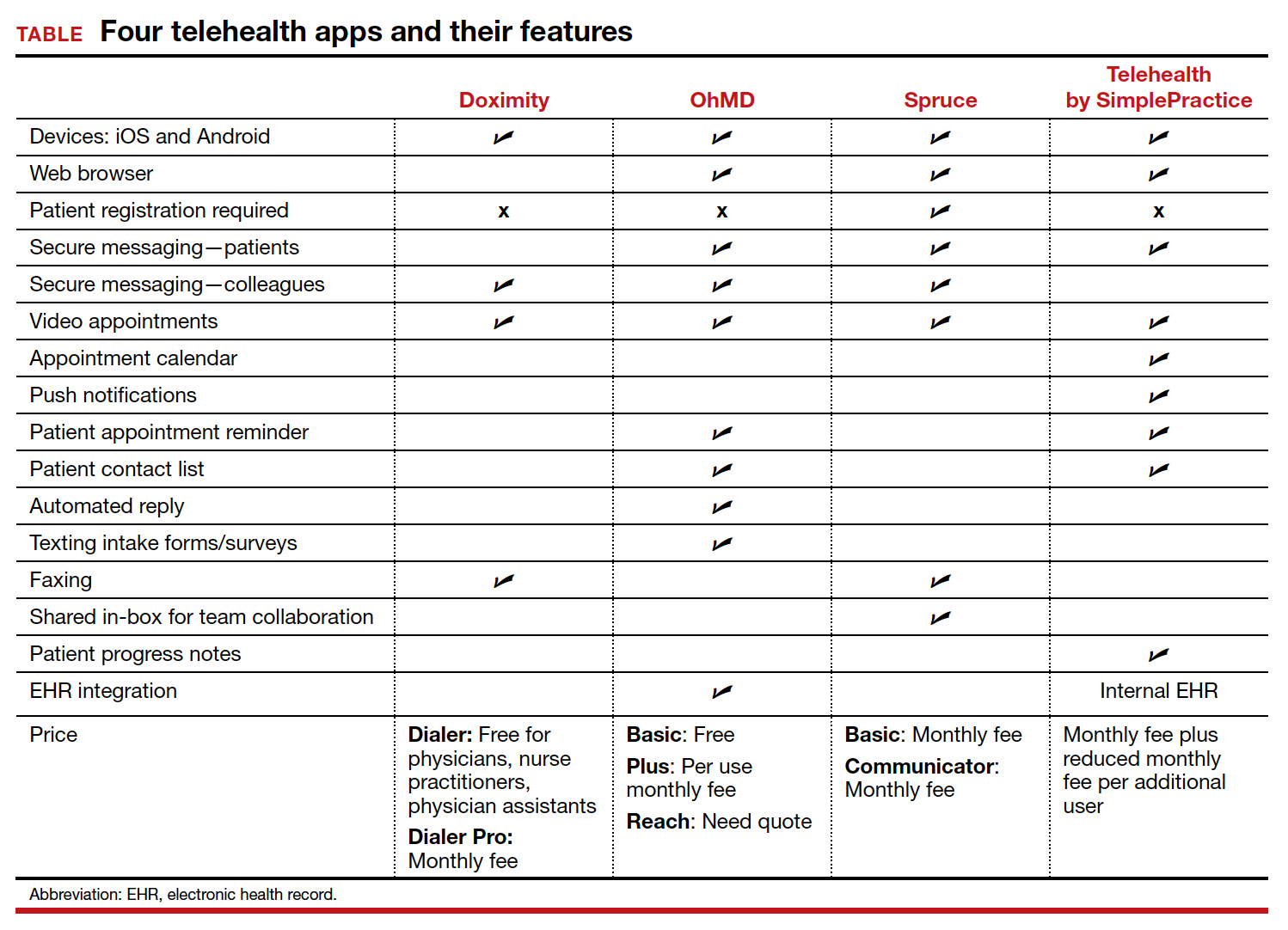
These apps are largely enabled for iOS and Android mobile devices and are offered at a range of price points for individual physician and practice-scale clinical implementation. Most apps offer secure messaging services between health care practitioners in addition to HIPAA-compliant patient messaging. Some apps offer additional features with the aim to increase patient attendance; these include push notifications, appointment reminders, and an option for automated replies with clinic information. For an additional fee, several apps offer integration to established EHR systems.
An additional tool
The COVID-19 pandemic caused health care systems and individual clinicians to rapidly evolve their practices to maintain patient access to essential health care. Notably, the pandemic led to accelerated implementation of virtual health care services. Telehealth apps likely will become another tool that ObGyns can use to improve the efficiency of their clinical practice and expand patient access to care. ●
The COVID-19 pandemic has presented increasing demands on health care systems internationally. In addition to redistribution of inpatient health care resources, outpatient care practices evolved, with health care providers offering streamlined access to care to patients via telehealth.
Due to updated insurance practices, physicians now can receive reimbursement via private insurers, Medicare, and Medicaid (as determined by states) for telehealth visits both related and unrelated to COVID-19 care. Increased telehealth use has advantages, including increased health care access, reduced in-clinic wait times, and reduced patient and physician travel time. Within the field of obstetrics and gynecology, clinicians have used telehealth to maintain access to prenatal maternity care while redirecting resources and minimizing the risk of COVID-19 transmission. Additional advantages include provision of care during expanded hours, including evenings and weekends, to increase patient access without increasing the demand on office support staff and the ability to bill for 5- to 10-minute phone counseling encounters.1 Research shows that patients express satisfaction regarding the quality of telehealth care in the setting of prenatal care.2
In February 2020, the American College of Obstetricians and Gynecologists (ACOG) released a Committee Opinion regarding telehealth use in ObGyn, a sign of telehealth’s likely long-standing role within the field.3 Within the statement, ACOG commented on the increasing application of telemedicine in all aspects of obstetrics and gynecology and recommended that physicians become acquainted with new technologies and consider using them in their practice.
There is a large opportunity for development of mobile applications (apps) to further streamline telehealth-based medical care. During the pandemic, the Centers for Medicare and Medicaid Services instituted waivers for telemedicine use on non-HIPAA (Health Insurance Portability and Accountability Act) compliant video communications products, such as Google+ Hangout and Skype. However, HIPAA-compliant video services are preferred, and many virtual apps have released methods for patient communication that meet HIPAA guidelines.1,4 These apps offer services such as phone- and video-based patient visits, appointment scheduling, secure physician-patient messaging, and electronic health record (EHR) documentation.
App recommendations
To identify current mobile apps with clinical use for the ObGyn, we conducted a search of the Apple App Store using the term “telehealth” between December 1, 2021 and January 1, 2022. We limited search results to apps that had at least 1,000 user ratings and to HIPAA-compliant user communication apps. Based on our review, we selected 4 apps to highlight here: Doximity, OhMD, Spruce, and Telehealth by SimplePractice (TABLE). We excluded apps that were advertised as having internal medical clinicians with first patient encounter on-demand through the app or that were associated with a singular insurance company or hospital system.
These apps are largely enabled for iOS and Android mobile devices and are offered at a range of price points for individual physician and practice-scale clinical implementation. Most apps offer secure messaging services between health care practitioners in addition to HIPAA-compliant patient messaging. Some apps offer additional features with the aim to increase patient attendance; these include push notifications, appointment reminders, and an option for automated replies with clinic information. For an additional fee, several apps offer integration to established EHR systems.
An additional tool
The COVID-19 pandemic caused health care systems and individual clinicians to rapidly evolve their practices to maintain patient access to essential health care. Notably, the pandemic led to accelerated implementation of virtual health care services. Telehealth apps likely will become another tool that ObGyns can use to improve the efficiency of their clinical practice and expand patient access to care. ●
- Karram M, Baum N. Telemedicine: a primer for today’s ObGyn. OBG Manag. 2020;32:28-32.
- Marko KI, Ganju N, Krapf JM, et al. A mobile prenatal care app to reduce in-person visits: prospective controlled trial. JMIR Mhealth Uhealth. 2019;7:e10520.
- American College of Obstetricians and Gynecologists. Implementing telehealth in practice: committee opinion no. 798. Obstet Gynecol. 2020;135:e73-e79.
- Karram M, Dooley A, de la Houssaye N, et al. Telemedicine: navigating legal issues. OBG Manag. 2020;32:18-24.
- Karram M, Baum N. Telemedicine: a primer for today’s ObGyn. OBG Manag. 2020;32:28-32.
- Marko KI, Ganju N, Krapf JM, et al. A mobile prenatal care app to reduce in-person visits: prospective controlled trial. JMIR Mhealth Uhealth. 2019;7:e10520.
- American College of Obstetricians and Gynecologists. Implementing telehealth in practice: committee opinion no. 798. Obstet Gynecol. 2020;135:e73-e79.
- Karram M, Dooley A, de la Houssaye N, et al. Telemedicine: navigating legal issues. OBG Manag. 2020;32:18-24.
Patient-facing mobile apps: Are ObGyns uniquely positioned to integrate them into practice?
Incorporating mobile apps into patient care programs can add immense value. Mobile apps enable data collection when a patient is beyond the walls of a doctor’s office and equip clinicians with new and relevant patient data. Patient engagement apps also provide a mechanism to “nudge” patients to encourage adherence to their care programs. These additional data and increased patient adherence can enable more personalized care,1 and ultimately can lead to improved outcomes. For example, a meta-analysis of 1,657 patients with diabetes showed a 5% reduction in hemoglobin A1c (HbA1c) values for those who used a diabetes-related app.2 The literature also shows positive results for heart failure, weight management, smoking reduction, and lifestyle improvement.3-5 Given their value, why aren’t patient engagement apps more routinely integrated into patient care programs?
From a software development perspective, mobile apps are fairly easy to create. However, from a user retention standpoint, creating an app with a large, sustainable userbase is challenging.5 User retention is measured in monthly active users. We are familiar with unused apps collecting digital dust on our smartphone home screens. A 2019 study showed that 25% of people typically use an application only once,6 and health care apps are not an exception. There are hundreds of thousands of mobile health apps on the market, but only 7% of these applications have more than 50,000 monthly active users. Further, 62% of digital health apps have less than 1,000 monthly active users.7
Using a new app daily or several times weekly requires new habit formation. Anyone who has tried to incorporate a new routine into their daily life knows how difficult habit formation can be. However, ObGyn patients may be particularly well suited to incorporate ObGyn-related apps into their care, given how many women already use mobile applications to track their menstrual cycles. A recent survey found that across all age groups, 47% of women use a mobile phone app to track their menstrual cycle,8 compared with 8% of US adults who regularly use an app to measure general health metrics.7 This removes one of the largest obstacles of market penetration since the habit of using an app for ObGyn purposes has already been established. As such, it presents an exciting opportunity to capitalize on the userbase already leveraging mobile apps to track their cycles and expand the patient engagement footprint into additional features that can broaden care to create a seamless, holistic patient application for ObGyn patient care.
One can envision a future in which a patient is “prescribed” an ObGyn app during their ObGyn appointment. Within the app, the patient can track their health data, engage with health providers, and gain access to educational materials. The clinician would be able to access data captured in the patient app at an aggregate level to analyze trends over time.
Current, patient-facing ObGyn mobile apps available for download on smartphones are for targeted aspects of ObGyn health. For example, there are separate apps for menstrual cycle tracking, contraception education, and medication adherence tracking. In the future, it would be ideal for clinicians and patients to have access to a single, holistic ObGyn mobile app that supports the end-to-end ObGyn patient journey, one in which clinicians could turn modules on or off given specific patient concerns. The technology for this type of holistic patient engagement platform exists, but unfortunately it is not as simple as downloading a mobile app. Standing up an end-to-end patient engagement platform requires enterprise-wide buy-in, tailoring user workflows, and building out integrations (eg, integrating provider dashboards into the existing electronic health record system). Full-scale solutions are powerful, but they can be expensive and time consuming to stand up. Until there is a more streamlined, outside-the-box ObGyn-tailored solution, there are patientfacing mobile apps available to support your patients for specific concerns.
Continue to: The top 3 recommended menstrual cycle tracking apps...
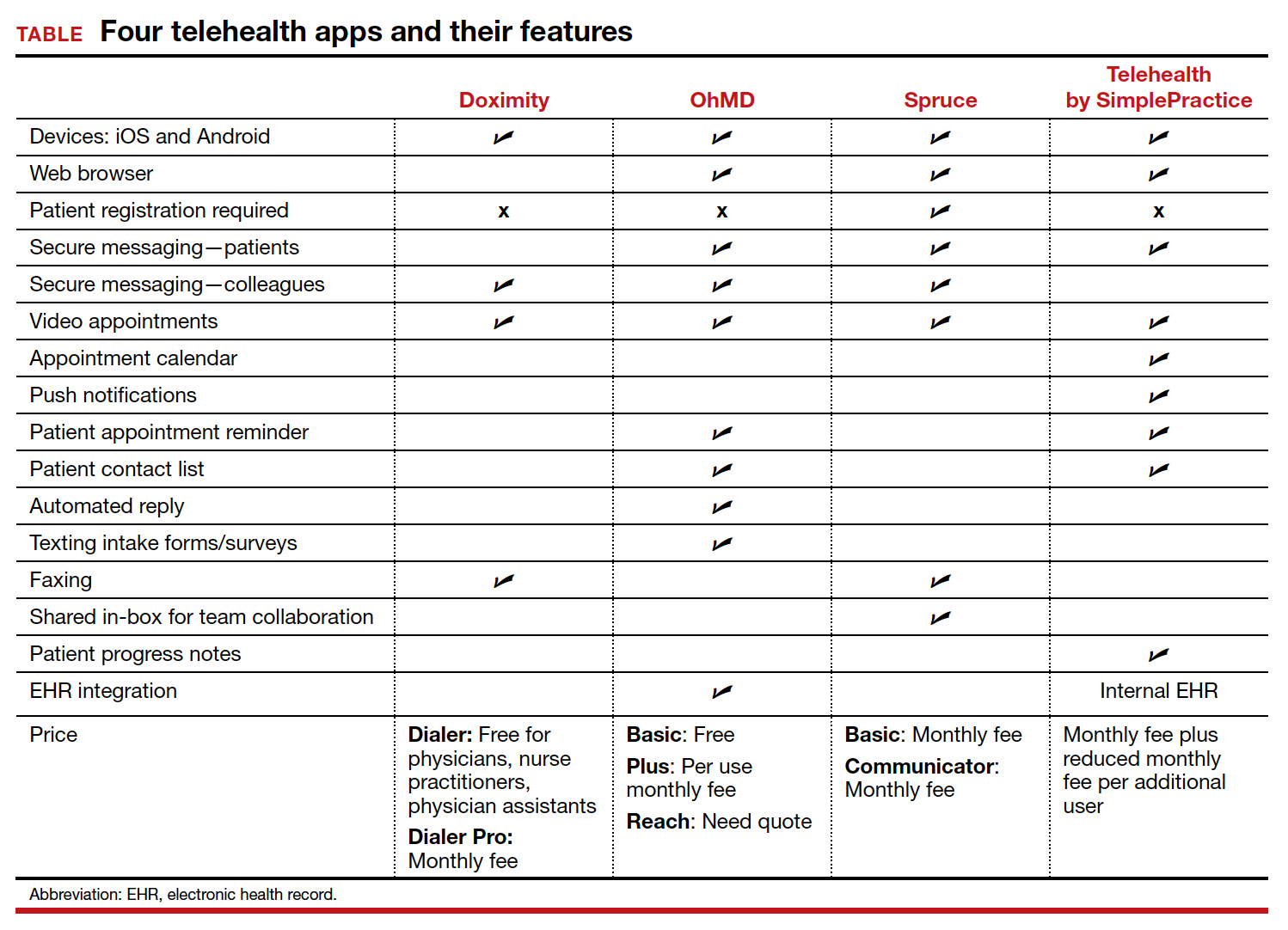
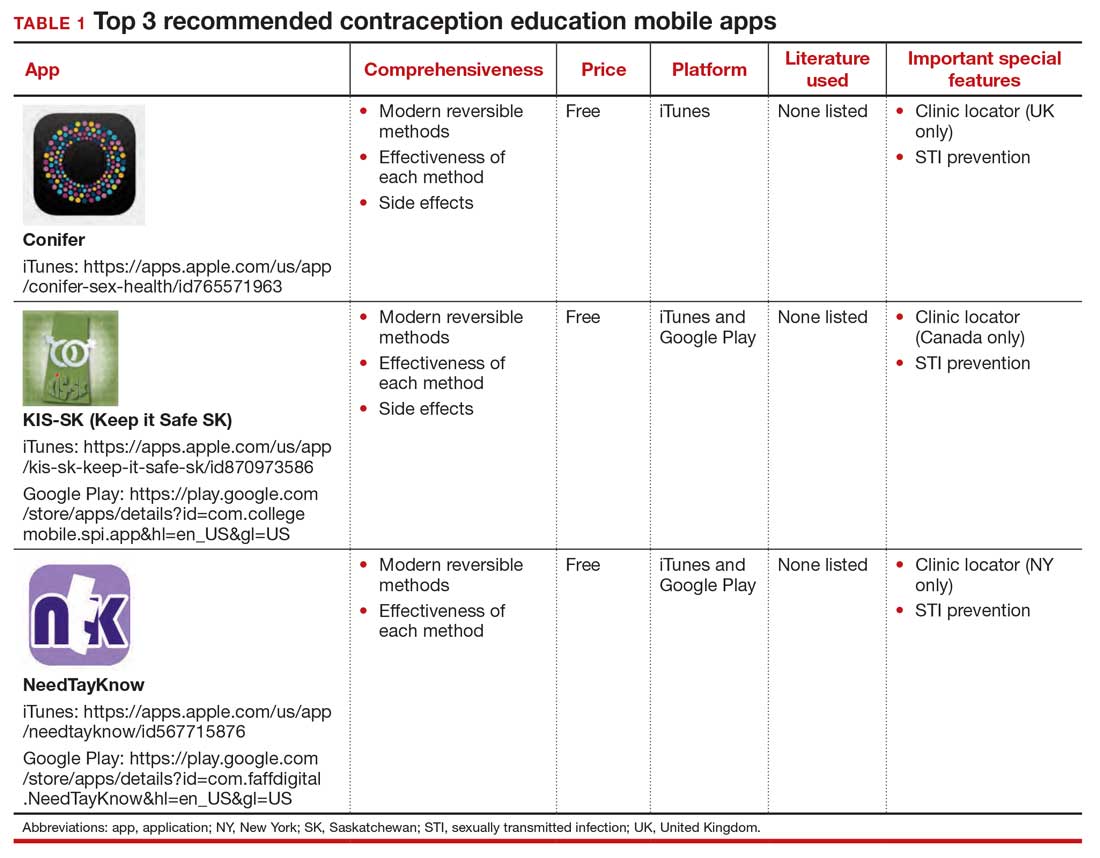
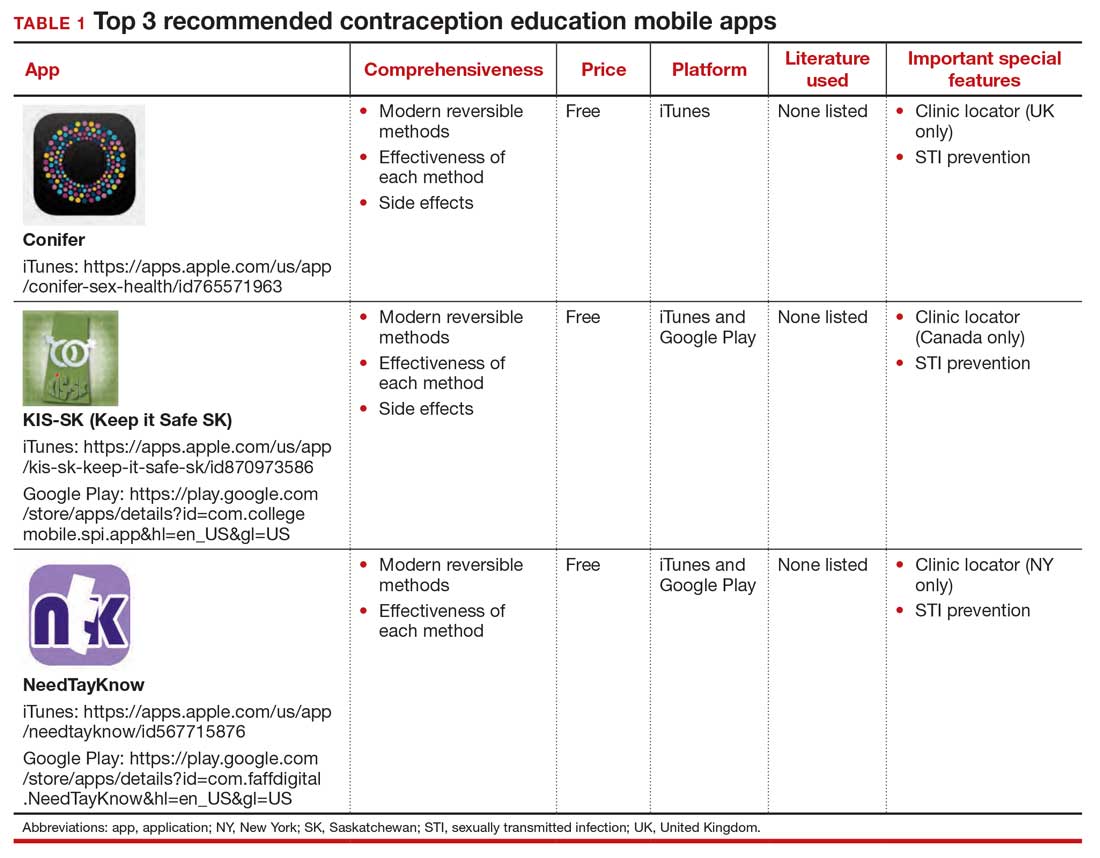
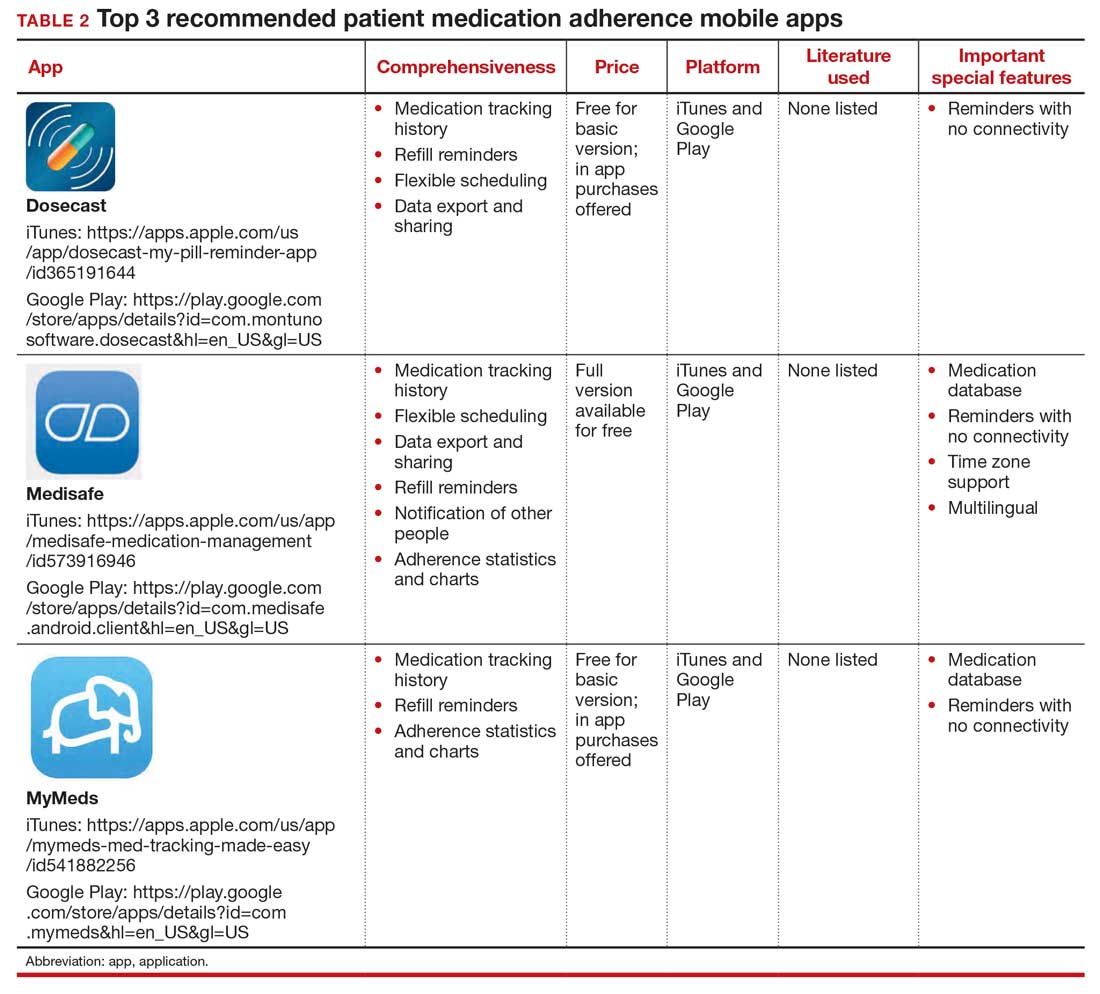
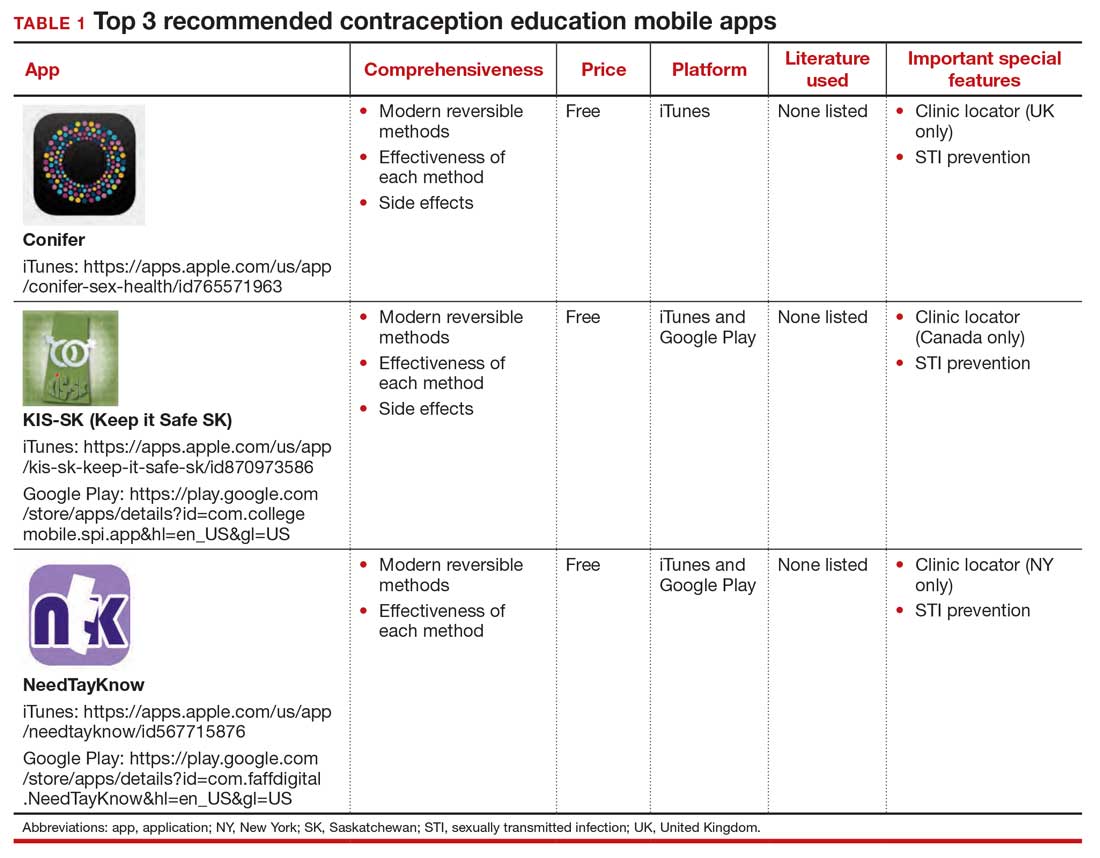
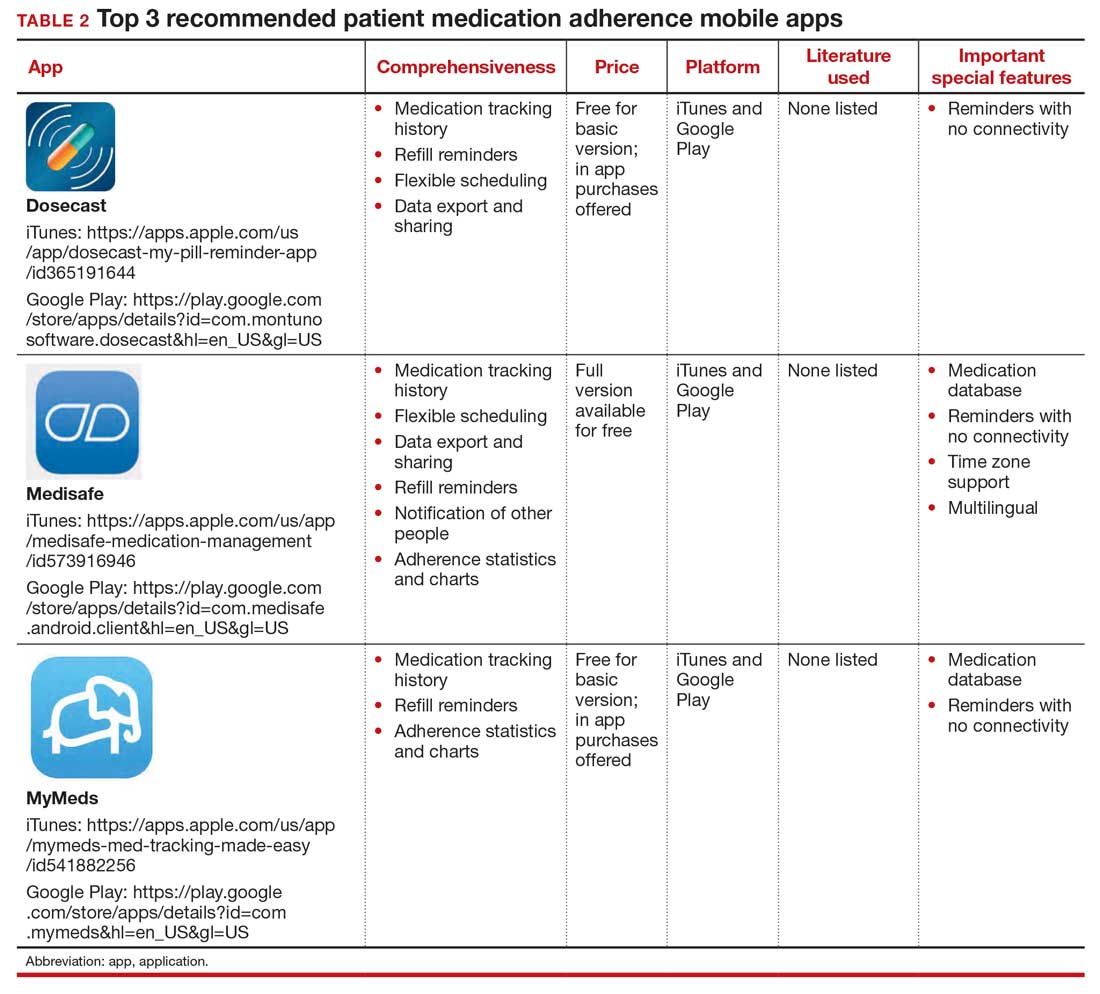
The top 3 recommended menstrual cycle tracking apps from Moglia and colleagues9 are listed in Dr. Chen’s article, “Top free menstrual cycle tracking apps for your patients.”10 The top 3 recommended contraception education mobile apps from Lunde and colleagues11 are listed in TABLE 1 and are detailed with a shortened version of the APPLICATIONS scoring system, APPLI (app comprehensiveness, price, platform, literature use, important special features).12 The top 3 recommended patient medication adherence mobile apps from the study by Santo and colleagues13 are listed in TABLE 2. The apps in the Stoyanov et al14 study were evaluated using the 23-item Mobile App Rating System scale. ●
- van Dijk MR, Koster MPH, et al. Healthy preconception nutrition and lifestyle using personalized mobile health coaching is associated with enhanced pregnancy chance. Reprod BioMed Online. 2017;35:453-460. doi:10.1016/j. rbmo.2017.06.014.
- Liang X, Wang Q, Yang X, et al. Effect of mobile phone intervention for diabetes on glycaemic control: a metaanalysis. Diabet Med. 2011;28:455-463. doi:10.1111/j.1464- 5491.2010.03180.x.
- Laing BY, Mangione CM, Tseng C-H, et al. Effectiveness of a smartphone application for weight loss compared with usual care in overweight primary care patients. Ann Intern Med. 2014;161(10 suppl):S5-S12. doi:10.7326/m13-3005.
- Dennison L, Morrison L, Conway G, et al. Opportunities and challenges for smartphone applications in supporting health behavior change: qualitative study. J Med Internet Res. 2013;15:E86. doi:10.2196/jmir.2583.
- Schoeppe S, Alley S, Van Lippevelde W, et al. Efficacy of interventions that use apps to improve diet, physical activity and sedentary behaviour: a systematic review. Int J Behav Nutr Phys Act. 2016;13:127. doi:10.1186/s12966- 016-0454-y.
- 25% of users abandon apps after one use. Upland Software website. Accessed May 6, 2021. https://uplandsoftware.com /localytics/resources/blog/25-of-users-abandon-apps-afterone-use/.
- mHealth economics 2017/2018 – connectivity in digital health. Published March 5, 2019. Accessed May 6, 2021. https:// research2guidance.com/product/connectivity-in-digitalhealth/.
- Epstein DA, Lee NB, Kang JH, et al. Examining menstrual tracking to inform the design of personal informatics tools. Proc SIGCHI Conf Hum Factor Comput Syst. 2017;2017:6876- 6888. doi:10.1145/3025453.3025635.
- Moglia M, Nguyen H, Chyjek K, et al. Evaluation of smartphone menstrual cycle tracking applications using an adapted APPLICATIONS scoring system. Obstet Gynecol. 2016;127:1153-1160. doi:10.1097/AOG.0000000000001444.
- Chen KT. Top free menstrual cycle tracking apps for your patients. OBG Manag. 2017;27:44-45.
- Lunde B, Perry R, Sridhar A, et al. An evaluation of contraception education and health promotion applications for patients. Womens Health Issues. 2017;27:29-35. doi:10.1016/j.whi.2016.09.012.
- Chyjek K, Farag S, Chen KT. Rating pregnancy wheel applications using the APPLICATIONS scoring system. Obstet Gynecol. 2015;125:1478-1483. doi:10.1097 /AOG.0000000000000842.
- Santo K, Richtering SS, Chalmers J, et al. Mobile phone apps to improve medication adherence: a systematic stepwise process to identify high-quality apps. JMIR Mhealth Uhealth. 2016;4:E132. doi:10.2196/mhealth.6742.
- Stoyanov SR, Hides L, Kavanagh DJ, et al. Mobile app rating scale: a new tool for assessing the quality of health mobile apps. JMIR Mhealth Uhealth. 2015;3:E27. doi:10.2196 /mhealth.3422.
Incorporating mobile apps into patient care programs can add immense value. Mobile apps enable data collection when a patient is beyond the walls of a doctor’s office and equip clinicians with new and relevant patient data. Patient engagement apps also provide a mechanism to “nudge” patients to encourage adherence to their care programs. These additional data and increased patient adherence can enable more personalized care,1 and ultimately can lead to improved outcomes. For example, a meta-analysis of 1,657 patients with diabetes showed a 5% reduction in hemoglobin A1c (HbA1c) values for those who used a diabetes-related app.2 The literature also shows positive results for heart failure, weight management, smoking reduction, and lifestyle improvement.3-5 Given their value, why aren’t patient engagement apps more routinely integrated into patient care programs?
From a software development perspective, mobile apps are fairly easy to create. However, from a user retention standpoint, creating an app with a large, sustainable userbase is challenging.5 User retention is measured in monthly active users. We are familiar with unused apps collecting digital dust on our smartphone home screens. A 2019 study showed that 25% of people typically use an application only once,6 and health care apps are not an exception. There are hundreds of thousands of mobile health apps on the market, but only 7% of these applications have more than 50,000 monthly active users. Further, 62% of digital health apps have less than 1,000 monthly active users.7
Using a new app daily or several times weekly requires new habit formation. Anyone who has tried to incorporate a new routine into their daily life knows how difficult habit formation can be. However, ObGyn patients may be particularly well suited to incorporate ObGyn-related apps into their care, given how many women already use mobile applications to track their menstrual cycles. A recent survey found that across all age groups, 47% of women use a mobile phone app to track their menstrual cycle,8 compared with 8% of US adults who regularly use an app to measure general health metrics.7 This removes one of the largest obstacles of market penetration since the habit of using an app for ObGyn purposes has already been established. As such, it presents an exciting opportunity to capitalize on the userbase already leveraging mobile apps to track their cycles and expand the patient engagement footprint into additional features that can broaden care to create a seamless, holistic patient application for ObGyn patient care.
One can envision a future in which a patient is “prescribed” an ObGyn app during their ObGyn appointment. Within the app, the patient can track their health data, engage with health providers, and gain access to educational materials. The clinician would be able to access data captured in the patient app at an aggregate level to analyze trends over time.
Current, patient-facing ObGyn mobile apps available for download on smartphones are for targeted aspects of ObGyn health. For example, there are separate apps for menstrual cycle tracking, contraception education, and medication adherence tracking. In the future, it would be ideal for clinicians and patients to have access to a single, holistic ObGyn mobile app that supports the end-to-end ObGyn patient journey, one in which clinicians could turn modules on or off given specific patient concerns. The technology for this type of holistic patient engagement platform exists, but unfortunately it is not as simple as downloading a mobile app. Standing up an end-to-end patient engagement platform requires enterprise-wide buy-in, tailoring user workflows, and building out integrations (eg, integrating provider dashboards into the existing electronic health record system). Full-scale solutions are powerful, but they can be expensive and time consuming to stand up. Until there is a more streamlined, outside-the-box ObGyn-tailored solution, there are patientfacing mobile apps available to support your patients for specific concerns.
Continue to: The top 3 recommended menstrual cycle tracking apps...
The top 3 recommended menstrual cycle tracking apps from Moglia and colleagues9 are listed in Dr. Chen’s article, “Top free menstrual cycle tracking apps for your patients.”10 The top 3 recommended contraception education mobile apps from Lunde and colleagues11 are listed in TABLE 1 and are detailed with a shortened version of the APPLICATIONS scoring system, APPLI (app comprehensiveness, price, platform, literature use, important special features).12 The top 3 recommended patient medication adherence mobile apps from the study by Santo and colleagues13 are listed in TABLE 2. The apps in the Stoyanov et al14 study were evaluated using the 23-item Mobile App Rating System scale. ●
Incorporating mobile apps into patient care programs can add immense value. Mobile apps enable data collection when a patient is beyond the walls of a doctor’s office and equip clinicians with new and relevant patient data. Patient engagement apps also provide a mechanism to “nudge” patients to encourage adherence to their care programs. These additional data and increased patient adherence can enable more personalized care,1 and ultimately can lead to improved outcomes. For example, a meta-analysis of 1,657 patients with diabetes showed a 5% reduction in hemoglobin A1c (HbA1c) values for those who used a diabetes-related app.2 The literature also shows positive results for heart failure, weight management, smoking reduction, and lifestyle improvement.3-5 Given their value, why aren’t patient engagement apps more routinely integrated into patient care programs?
From a software development perspective, mobile apps are fairly easy to create. However, from a user retention standpoint, creating an app with a large, sustainable userbase is challenging.5 User retention is measured in monthly active users. We are familiar with unused apps collecting digital dust on our smartphone home screens. A 2019 study showed that 25% of people typically use an application only once,6 and health care apps are not an exception. There are hundreds of thousands of mobile health apps on the market, but only 7% of these applications have more than 50,000 monthly active users. Further, 62% of digital health apps have less than 1,000 monthly active users.7
Using a new app daily or several times weekly requires new habit formation. Anyone who has tried to incorporate a new routine into their daily life knows how difficult habit formation can be. However, ObGyn patients may be particularly well suited to incorporate ObGyn-related apps into their care, given how many women already use mobile applications to track their menstrual cycles. A recent survey found that across all age groups, 47% of women use a mobile phone app to track their menstrual cycle,8 compared with 8% of US adults who regularly use an app to measure general health metrics.7 This removes one of the largest obstacles of market penetration since the habit of using an app for ObGyn purposes has already been established. As such, it presents an exciting opportunity to capitalize on the userbase already leveraging mobile apps to track their cycles and expand the patient engagement footprint into additional features that can broaden care to create a seamless, holistic patient application for ObGyn patient care.
One can envision a future in which a patient is “prescribed” an ObGyn app during their ObGyn appointment. Within the app, the patient can track their health data, engage with health providers, and gain access to educational materials. The clinician would be able to access data captured in the patient app at an aggregate level to analyze trends over time.
Current, patient-facing ObGyn mobile apps available for download on smartphones are for targeted aspects of ObGyn health. For example, there are separate apps for menstrual cycle tracking, contraception education, and medication adherence tracking. In the future, it would be ideal for clinicians and patients to have access to a single, holistic ObGyn mobile app that supports the end-to-end ObGyn patient journey, one in which clinicians could turn modules on or off given specific patient concerns. The technology for this type of holistic patient engagement platform exists, but unfortunately it is not as simple as downloading a mobile app. Standing up an end-to-end patient engagement platform requires enterprise-wide buy-in, tailoring user workflows, and building out integrations (eg, integrating provider dashboards into the existing electronic health record system). Full-scale solutions are powerful, but they can be expensive and time consuming to stand up. Until there is a more streamlined, outside-the-box ObGyn-tailored solution, there are patientfacing mobile apps available to support your patients for specific concerns.
Continue to: The top 3 recommended menstrual cycle tracking apps...
The top 3 recommended menstrual cycle tracking apps from Moglia and colleagues9 are listed in Dr. Chen’s article, “Top free menstrual cycle tracking apps for your patients.”10 The top 3 recommended contraception education mobile apps from Lunde and colleagues11 are listed in TABLE 1 and are detailed with a shortened version of the APPLICATIONS scoring system, APPLI (app comprehensiveness, price, platform, literature use, important special features).12 The top 3 recommended patient medication adherence mobile apps from the study by Santo and colleagues13 are listed in TABLE 2. The apps in the Stoyanov et al14 study were evaluated using the 23-item Mobile App Rating System scale. ●
- van Dijk MR, Koster MPH, et al. Healthy preconception nutrition and lifestyle using personalized mobile health coaching is associated with enhanced pregnancy chance. Reprod BioMed Online. 2017;35:453-460. doi:10.1016/j. rbmo.2017.06.014.
- Liang X, Wang Q, Yang X, et al. Effect of mobile phone intervention for diabetes on glycaemic control: a metaanalysis. Diabet Med. 2011;28:455-463. doi:10.1111/j.1464- 5491.2010.03180.x.
- Laing BY, Mangione CM, Tseng C-H, et al. Effectiveness of a smartphone application for weight loss compared with usual care in overweight primary care patients. Ann Intern Med. 2014;161(10 suppl):S5-S12. doi:10.7326/m13-3005.
- Dennison L, Morrison L, Conway G, et al. Opportunities and challenges for smartphone applications in supporting health behavior change: qualitative study. J Med Internet Res. 2013;15:E86. doi:10.2196/jmir.2583.
- Schoeppe S, Alley S, Van Lippevelde W, et al. Efficacy of interventions that use apps to improve diet, physical activity and sedentary behaviour: a systematic review. Int J Behav Nutr Phys Act. 2016;13:127. doi:10.1186/s12966- 016-0454-y.
- 25% of users abandon apps after one use. Upland Software website. Accessed May 6, 2021. https://uplandsoftware.com /localytics/resources/blog/25-of-users-abandon-apps-afterone-use/.
- mHealth economics 2017/2018 – connectivity in digital health. Published March 5, 2019. Accessed May 6, 2021. https:// research2guidance.com/product/connectivity-in-digitalhealth/.
- Epstein DA, Lee NB, Kang JH, et al. Examining menstrual tracking to inform the design of personal informatics tools. Proc SIGCHI Conf Hum Factor Comput Syst. 2017;2017:6876- 6888. doi:10.1145/3025453.3025635.
- Moglia M, Nguyen H, Chyjek K, et al. Evaluation of smartphone menstrual cycle tracking applications using an adapted APPLICATIONS scoring system. Obstet Gynecol. 2016;127:1153-1160. doi:10.1097/AOG.0000000000001444.
- Chen KT. Top free menstrual cycle tracking apps for your patients. OBG Manag. 2017;27:44-45.
- Lunde B, Perry R, Sridhar A, et al. An evaluation of contraception education and health promotion applications for patients. Womens Health Issues. 2017;27:29-35. doi:10.1016/j.whi.2016.09.012.
- Chyjek K, Farag S, Chen KT. Rating pregnancy wheel applications using the APPLICATIONS scoring system. Obstet Gynecol. 2015;125:1478-1483. doi:10.1097 /AOG.0000000000000842.
- Santo K, Richtering SS, Chalmers J, et al. Mobile phone apps to improve medication adherence: a systematic stepwise process to identify high-quality apps. JMIR Mhealth Uhealth. 2016;4:E132. doi:10.2196/mhealth.6742.
- Stoyanov SR, Hides L, Kavanagh DJ, et al. Mobile app rating scale: a new tool for assessing the quality of health mobile apps. JMIR Mhealth Uhealth. 2015;3:E27. doi:10.2196 /mhealth.3422.
- van Dijk MR, Koster MPH, et al. Healthy preconception nutrition and lifestyle using personalized mobile health coaching is associated with enhanced pregnancy chance. Reprod BioMed Online. 2017;35:453-460. doi:10.1016/j. rbmo.2017.06.014.
- Liang X, Wang Q, Yang X, et al. Effect of mobile phone intervention for diabetes on glycaemic control: a metaanalysis. Diabet Med. 2011;28:455-463. doi:10.1111/j.1464- 5491.2010.03180.x.
- Laing BY, Mangione CM, Tseng C-H, et al. Effectiveness of a smartphone application for weight loss compared with usual care in overweight primary care patients. Ann Intern Med. 2014;161(10 suppl):S5-S12. doi:10.7326/m13-3005.
- Dennison L, Morrison L, Conway G, et al. Opportunities and challenges for smartphone applications in supporting health behavior change: qualitative study. J Med Internet Res. 2013;15:E86. doi:10.2196/jmir.2583.
- Schoeppe S, Alley S, Van Lippevelde W, et al. Efficacy of interventions that use apps to improve diet, physical activity and sedentary behaviour: a systematic review. Int J Behav Nutr Phys Act. 2016;13:127. doi:10.1186/s12966- 016-0454-y.
- 25% of users abandon apps after one use. Upland Software website. Accessed May 6, 2021. https://uplandsoftware.com /localytics/resources/blog/25-of-users-abandon-apps-afterone-use/.
- mHealth economics 2017/2018 – connectivity in digital health. Published March 5, 2019. Accessed May 6, 2021. https:// research2guidance.com/product/connectivity-in-digitalhealth/.
- Epstein DA, Lee NB, Kang JH, et al. Examining menstrual tracking to inform the design of personal informatics tools. Proc SIGCHI Conf Hum Factor Comput Syst. 2017;2017:6876- 6888. doi:10.1145/3025453.3025635.
- Moglia M, Nguyen H, Chyjek K, et al. Evaluation of smartphone menstrual cycle tracking applications using an adapted APPLICATIONS scoring system. Obstet Gynecol. 2016;127:1153-1160. doi:10.1097/AOG.0000000000001444.
- Chen KT. Top free menstrual cycle tracking apps for your patients. OBG Manag. 2017;27:44-45.
- Lunde B, Perry R, Sridhar A, et al. An evaluation of contraception education and health promotion applications for patients. Womens Health Issues. 2017;27:29-35. doi:10.1016/j.whi.2016.09.012.
- Chyjek K, Farag S, Chen KT. Rating pregnancy wheel applications using the APPLICATIONS scoring system. Obstet Gynecol. 2015;125:1478-1483. doi:10.1097 /AOG.0000000000000842.
- Santo K, Richtering SS, Chalmers J, et al. Mobile phone apps to improve medication adherence: a systematic stepwise process to identify high-quality apps. JMIR Mhealth Uhealth. 2016;4:E132. doi:10.2196/mhealth.6742.
- Stoyanov SR, Hides L, Kavanagh DJ, et al. Mobile app rating scale: a new tool for assessing the quality of health mobile apps. JMIR Mhealth Uhealth. 2015;3:E27. doi:10.2196 /mhealth.3422.
COVID-19 apps for the ObGyn health care provider: An update
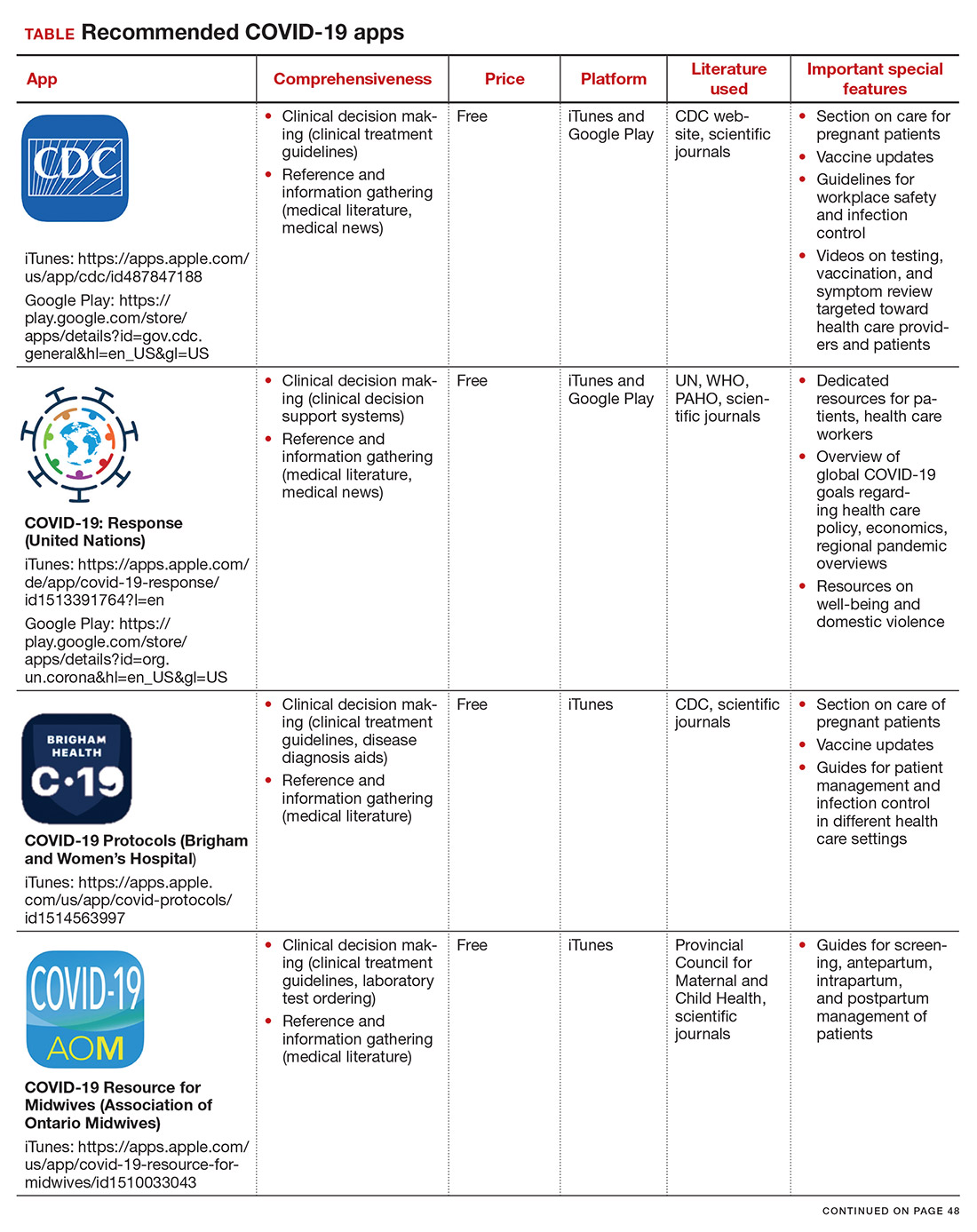
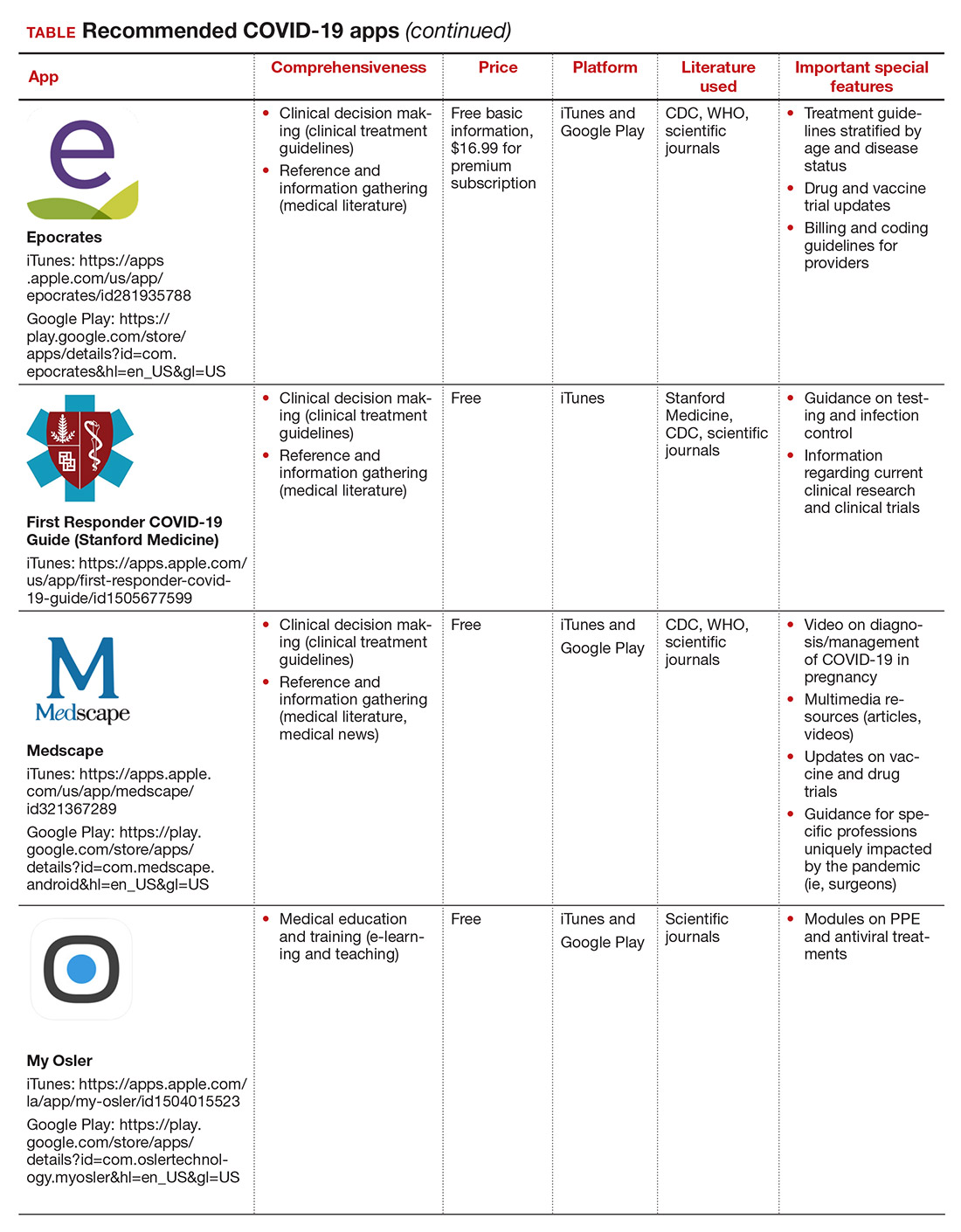
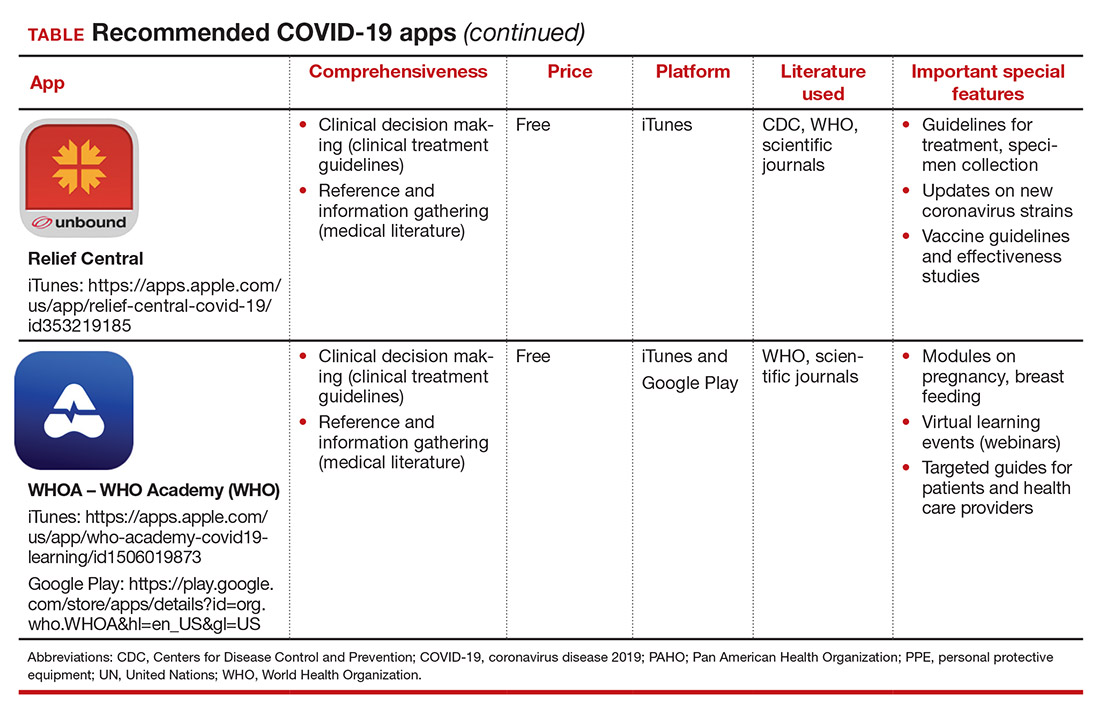
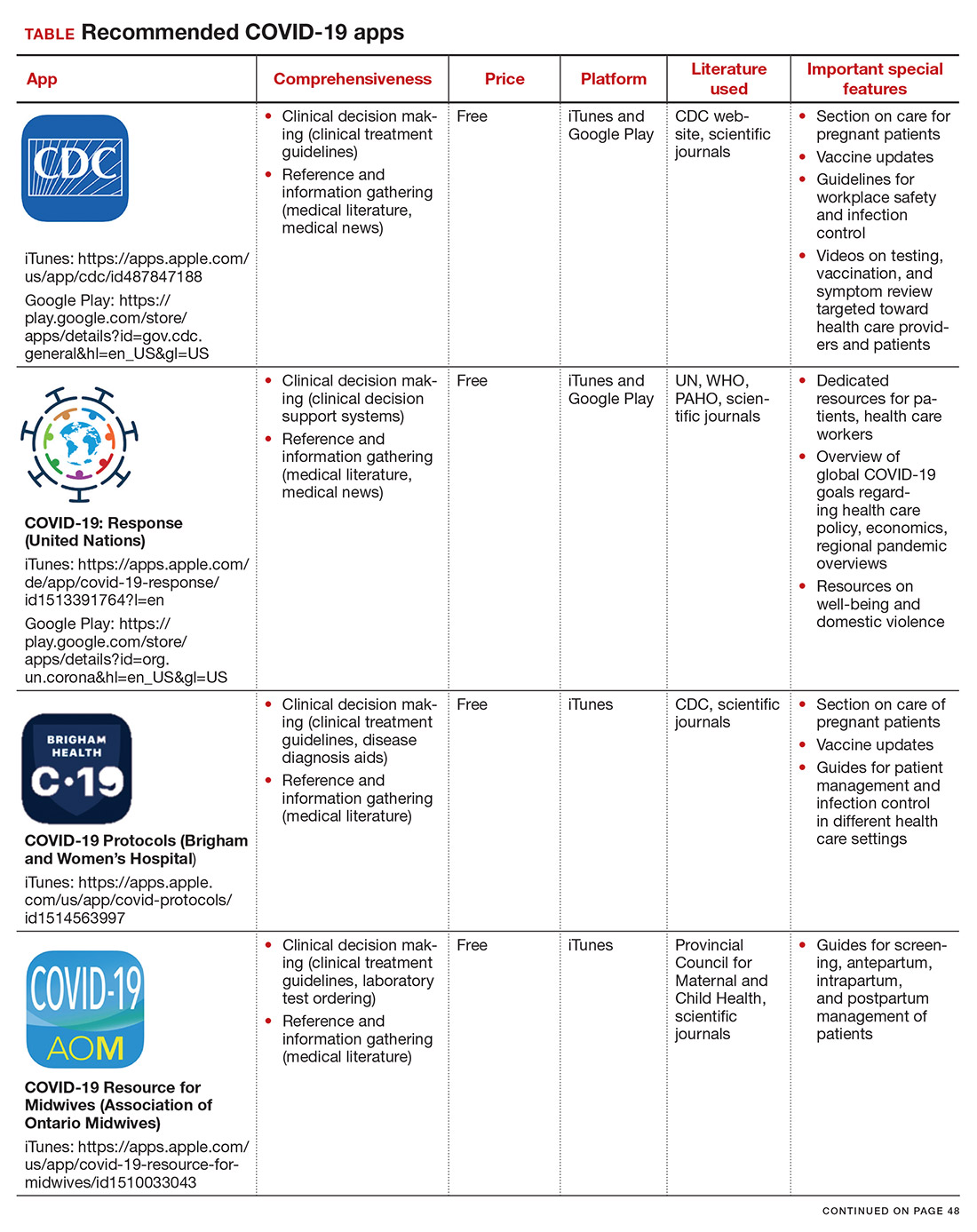
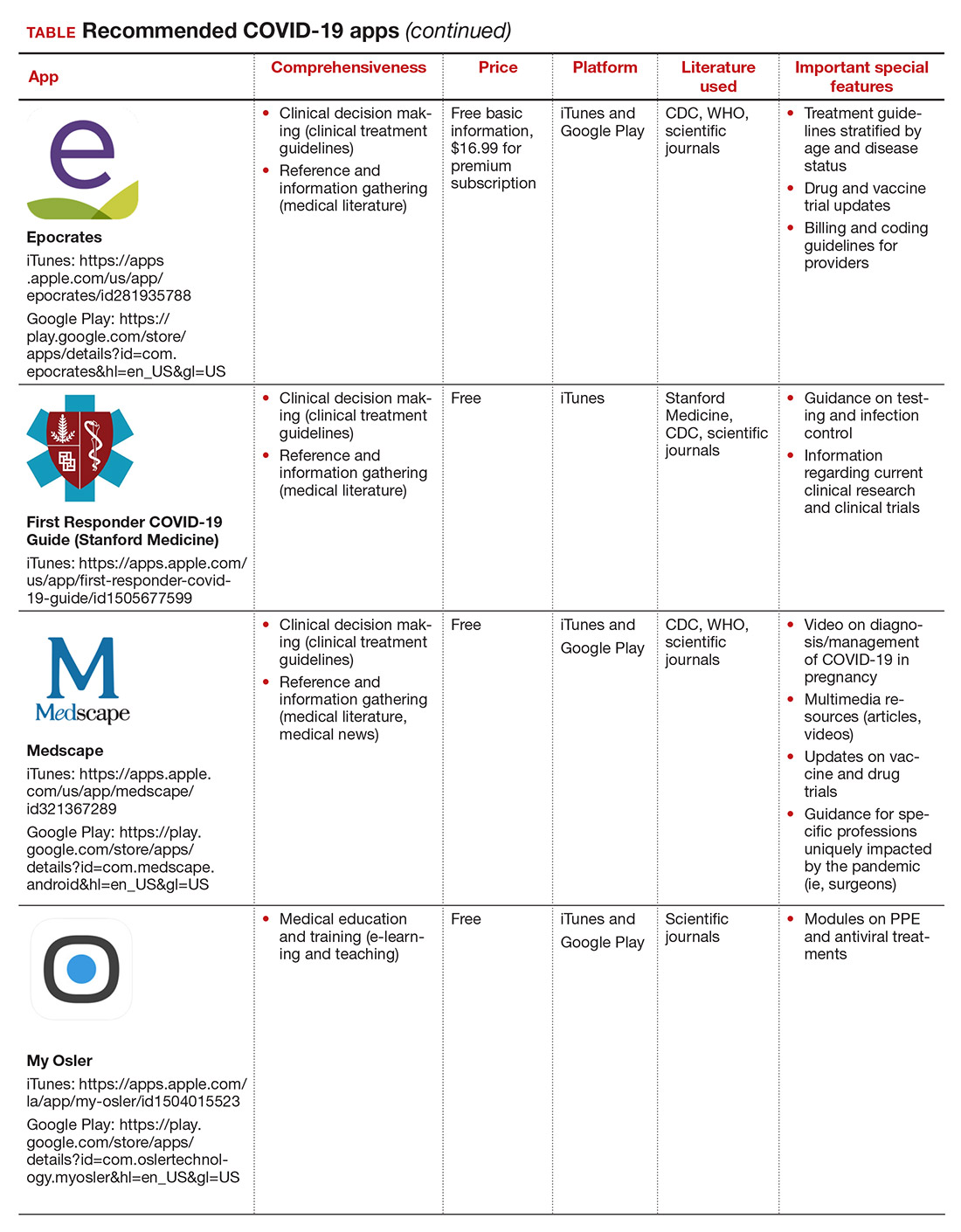
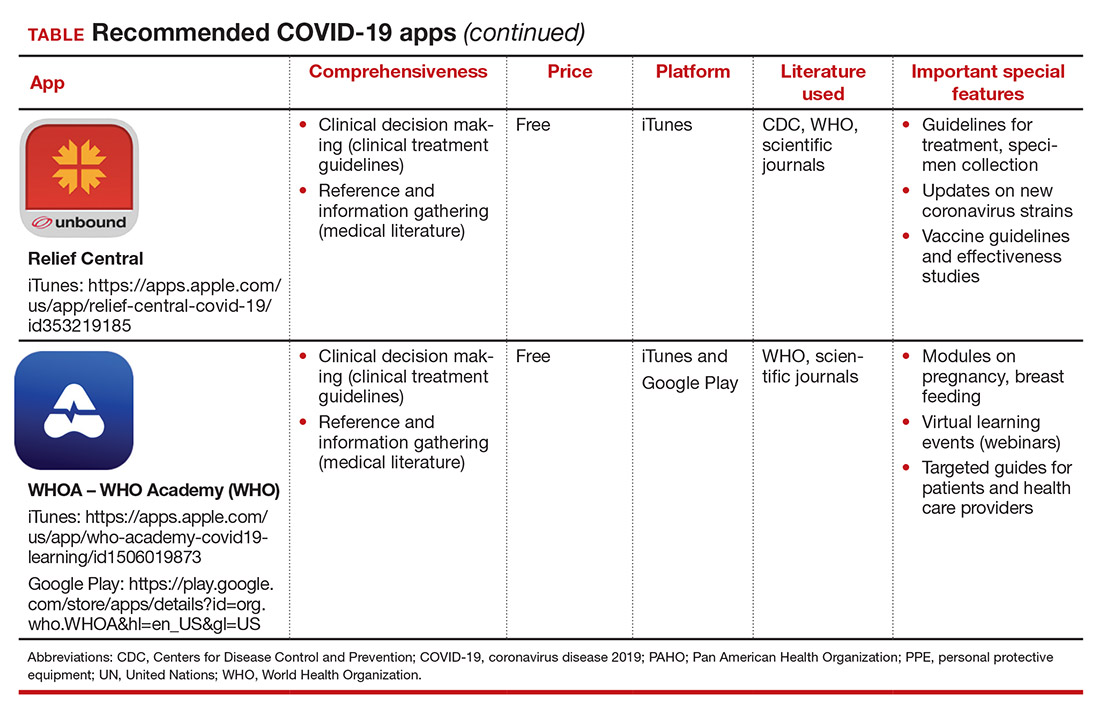
More than one year after COVID-19 was declared a worldwide pandemic by the World Health Organization on March 11, 2020, the disease continues to persist, infecting more than 110 million individuals to date globally.1 As new information emerges about the coronavirus, the literature on diagnosis and management also has grown exponentially over the last year, including specific guidance for obstetric populations. With abundant information available to health care providers, COVID-19 mobile apps have the advantage of summarizing and presenting information in an organized and easily accessible manner.2
This updated review expands on a previous article by Bogaert and Chen at the start of the COVID-19 pandemic.3 Using the same methodology, in March 2021 we searched the Apple iTunes and Google Play stores using the term “COVID.” The search yielded 230 unique applications available for download. We excluded apps that were primarily developed as geographic area-specific case trackers or personal symptom trackers (193), those that provide telemedicine services (7), and nonmedical apps or ones published in a language other than English (20).
Here, we focus on the 3 mobile apps previously discussed (CDC, My Osler, and Relief Central) and 7 additional apps (TABLE). Most summarize information on the prevention, diagnosis, and treatment of coronavirus, and several also provide information on the COVID-19 vaccine. One app (COVID-19 Resource for Midwives) is specifically designed for obstetric providers, and 4 others (CDC, COVID-19 Protocols, Medscape, and WHO Academy) contain information on specific guidance for obstetric and gynecologic patient populations.
Each app was evaluated based on a condensed version of the APPLICATIONS scoring system, APPLI (comprehensiveness, price, platform, literature used, and special features).4
We hope that these mobile apps will assist the ObGyn health care provider in continuing to care for patients during this pandemic.
- World Health Organization. WHO coronavirus (COVID-19) dashboard. https://covid19.who.int/. Accessed March 12, 2021.
2. Kondylakis H, Katehakis DG, Kouroubali A, et al. COVID-19 mobile apps: a systematic review of the literature. J Med Internet Res. 2020;22:e23170.
3. Bogaert K, Chen KT. COVID-19 apps for the ObGyn health care provider. OBG Manag. 2020; 32(5):44, 46.
4. Chyjek K, Farag S, Chen KT. Rating pregnancy wheel applications using the APPLICATIONS scoring system. Obstet Gynecol. 2015;125:1478-1483.
More than one year after COVID-19 was declared a worldwide pandemic by the World Health Organization on March 11, 2020, the disease continues to persist, infecting more than 110 million individuals to date globally.1 As new information emerges about the coronavirus, the literature on diagnosis and management also has grown exponentially over the last year, including specific guidance for obstetric populations. With abundant information available to health care providers, COVID-19 mobile apps have the advantage of summarizing and presenting information in an organized and easily accessible manner.2
This updated review expands on a previous article by Bogaert and Chen at the start of the COVID-19 pandemic.3 Using the same methodology, in March 2021 we searched the Apple iTunes and Google Play stores using the term “COVID.” The search yielded 230 unique applications available for download. We excluded apps that were primarily developed as geographic area-specific case trackers or personal symptom trackers (193), those that provide telemedicine services (7), and nonmedical apps or ones published in a language other than English (20).
Here, we focus on the 3 mobile apps previously discussed (CDC, My Osler, and Relief Central) and 7 additional apps (TABLE). Most summarize information on the prevention, diagnosis, and treatment of coronavirus, and several also provide information on the COVID-19 vaccine. One app (COVID-19 Resource for Midwives) is specifically designed for obstetric providers, and 4 others (CDC, COVID-19 Protocols, Medscape, and WHO Academy) contain information on specific guidance for obstetric and gynecologic patient populations.
Each app was evaluated based on a condensed version of the APPLICATIONS scoring system, APPLI (comprehensiveness, price, platform, literature used, and special features).4
We hope that these mobile apps will assist the ObGyn health care provider in continuing to care for patients during this pandemic.
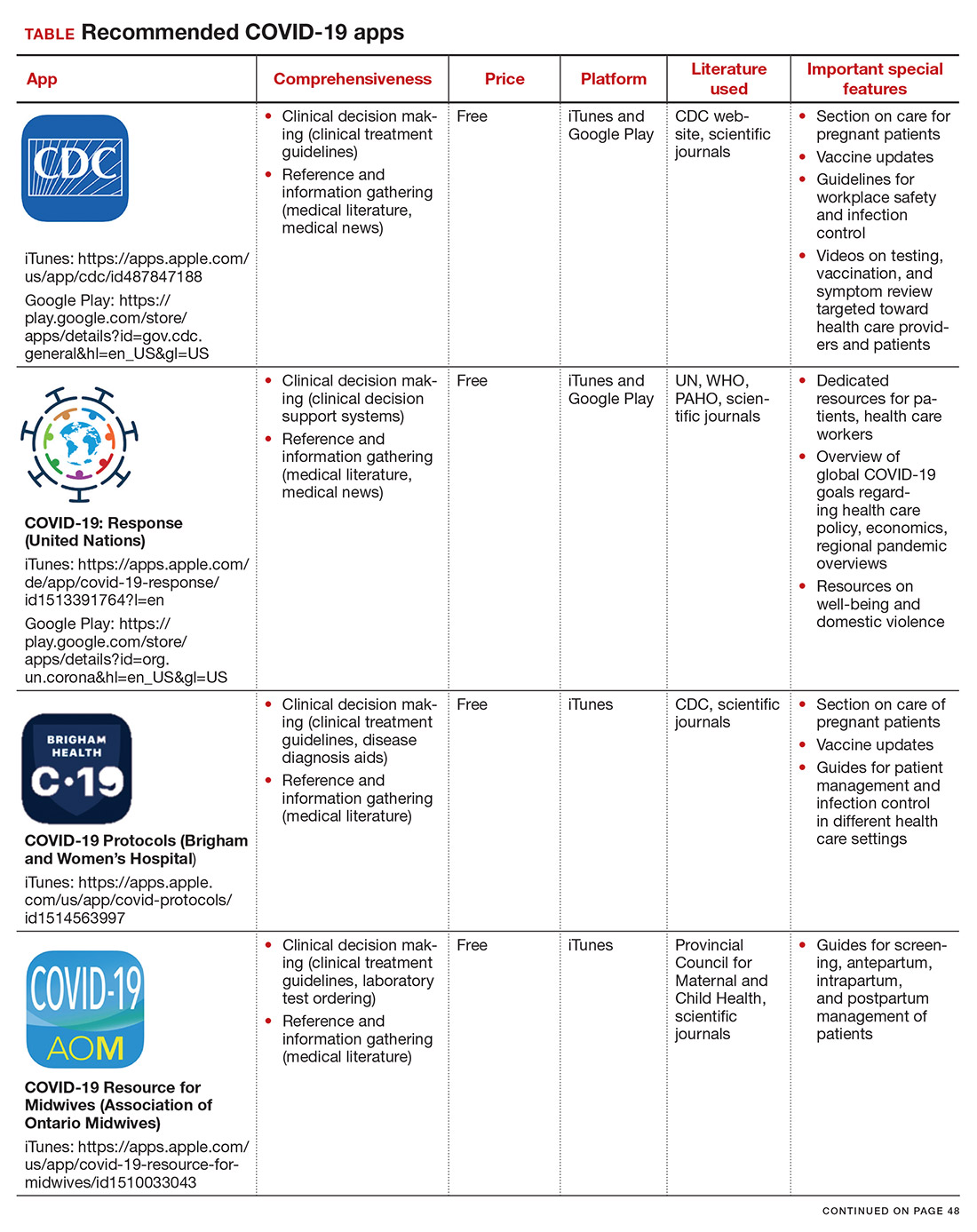
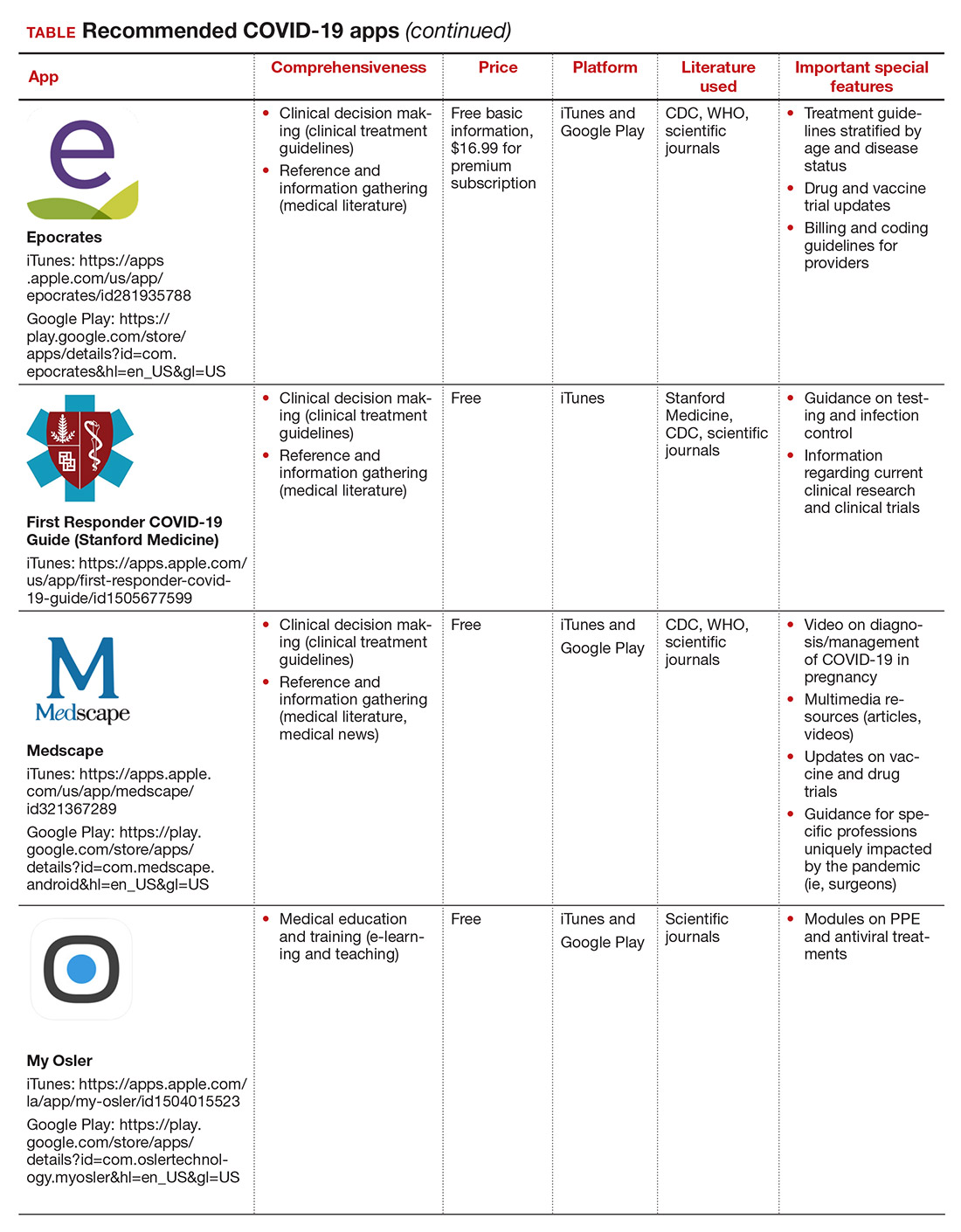
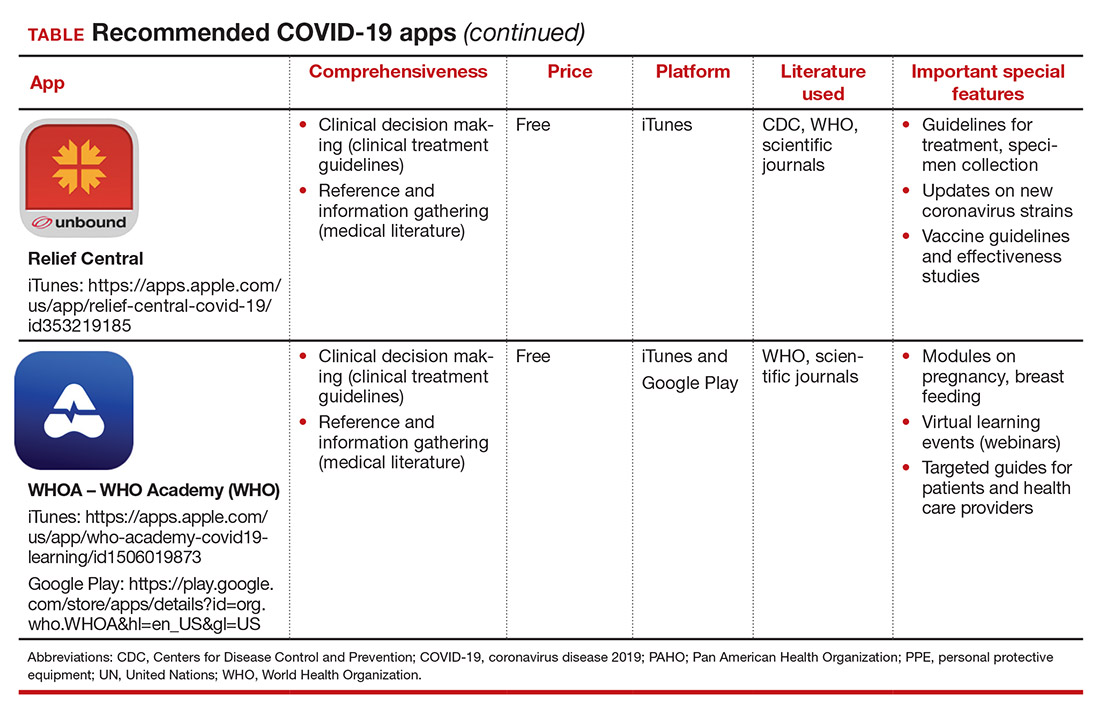
More than one year after COVID-19 was declared a worldwide pandemic by the World Health Organization on March 11, 2020, the disease continues to persist, infecting more than 110 million individuals to date globally.1 As new information emerges about the coronavirus, the literature on diagnosis and management also has grown exponentially over the last year, including specific guidance for obstetric populations. With abundant information available to health care providers, COVID-19 mobile apps have the advantage of summarizing and presenting information in an organized and easily accessible manner.2
This updated review expands on a previous article by Bogaert and Chen at the start of the COVID-19 pandemic.3 Using the same methodology, in March 2021 we searched the Apple iTunes and Google Play stores using the term “COVID.” The search yielded 230 unique applications available for download. We excluded apps that were primarily developed as geographic area-specific case trackers or personal symptom trackers (193), those that provide telemedicine services (7), and nonmedical apps or ones published in a language other than English (20).
Here, we focus on the 3 mobile apps previously discussed (CDC, My Osler, and Relief Central) and 7 additional apps (TABLE). Most summarize information on the prevention, diagnosis, and treatment of coronavirus, and several also provide information on the COVID-19 vaccine. One app (COVID-19 Resource for Midwives) is specifically designed for obstetric providers, and 4 others (CDC, COVID-19 Protocols, Medscape, and WHO Academy) contain information on specific guidance for obstetric and gynecologic patient populations.
Each app was evaluated based on a condensed version of the APPLICATIONS scoring system, APPLI (comprehensiveness, price, platform, literature used, and special features).4
We hope that these mobile apps will assist the ObGyn health care provider in continuing to care for patients during this pandemic.
- World Health Organization. WHO coronavirus (COVID-19) dashboard. https://covid19.who.int/. Accessed March 12, 2021.
2. Kondylakis H, Katehakis DG, Kouroubali A, et al. COVID-19 mobile apps: a systematic review of the literature. J Med Internet Res. 2020;22:e23170.
3. Bogaert K, Chen KT. COVID-19 apps for the ObGyn health care provider. OBG Manag. 2020; 32(5):44, 46.
4. Chyjek K, Farag S, Chen KT. Rating pregnancy wheel applications using the APPLICATIONS scoring system. Obstet Gynecol. 2015;125:1478-1483.
- World Health Organization. WHO coronavirus (COVID-19) dashboard. https://covid19.who.int/. Accessed March 12, 2021.
2. Kondylakis H, Katehakis DG, Kouroubali A, et al. COVID-19 mobile apps: a systematic review of the literature. J Med Internet Res. 2020;22:e23170.
3. Bogaert K, Chen KT. COVID-19 apps for the ObGyn health care provider. OBG Manag. 2020; 32(5):44, 46.
4. Chyjek K, Farag S, Chen KT. Rating pregnancy wheel applications using the APPLICATIONS scoring system. Obstet Gynecol. 2015;125:1478-1483.
Two at-home apps for patients with pelvic floor disorders
In the “You asked, Dr. Jen Gunter answered” series in The New York Times, Dr. Gunter writes that “pelvic floor exercises (also known as Kegel exercises) can be very helpful for urinary incontinence, pelvic organ prolapse, and fecal incontinence.” She continues to say that “pelvic floor exercises can be hard to master correctly, so it is important to make sure [one has] the correct technique. Many women can learn to do them after reading instructions like the ones found at the National Association for Continence, but some women may need their technique checked by their doctor, or help from a specialized pelvic floor physical therapist.”1
Similarly, Sudol and colleagues write that “guidelines from multiple medical societies emphasize the importance of patient education, behavioral therapy, and/or exercise regimens in the initial treatment and management of women with pelvic floor disorders. However, even with well-established recommendations, engaging patients and maintaining adherence to treatment plans and unmonitored programs at home are often difficult.”2 To help patients, those authors identified and evaluated patient-centered apps on topics in female pelvic medicine and reconstructive surgery.2
Two apps that assist patients in Kegel exercises are presented here. The Squeezy app includes guided pelvic floor muscle exercises with reminders, and the Kegel Nation app has a biofeedback feature.
The TABLE details the features of the 2 apps based on a shortened version of the APPLICATIONS scoring system, APPLI (app comprehensiveness, price, platform, literature used, and important special features).3
I hope clinicians find these apps helpful to their patients with pelvic floor disorders.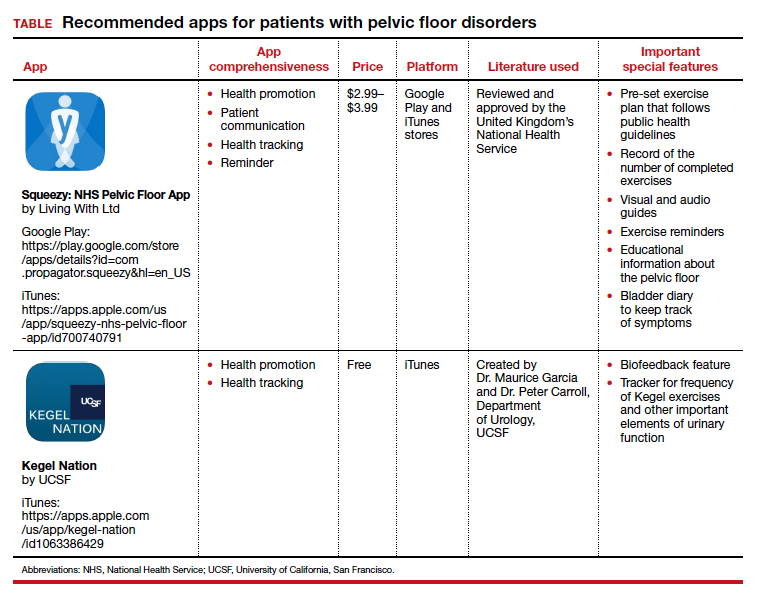
- Gunter J. You asked, Dr. Jen Gunter answered. New York Times. https://www.nytimes.com/ask/answers/kegels-pelvic-floor-exercises-yoni-eggs. Accessed December 22, 2020.
- Sudol NT, Adams-Piper E, Perry R, et al. In search of mobile applications for patients with pelvic floor disorders. Female Pelvic Med Reconstr Surg. 2019;25:252-256.
- Chyjek K, Farag S, Chen KT. Rating pregnancy wheel applications using the APPLICATIONS scoring system. Obstet Gynecol. 2015;125:1478-1483.
In the “You asked, Dr. Jen Gunter answered” series in The New York Times, Dr. Gunter writes that “pelvic floor exercises (also known as Kegel exercises) can be very helpful for urinary incontinence, pelvic organ prolapse, and fecal incontinence.” She continues to say that “pelvic floor exercises can be hard to master correctly, so it is important to make sure [one has] the correct technique. Many women can learn to do them after reading instructions like the ones found at the National Association for Continence, but some women may need their technique checked by their doctor, or help from a specialized pelvic floor physical therapist.”1
Similarly, Sudol and colleagues write that “guidelines from multiple medical societies emphasize the importance of patient education, behavioral therapy, and/or exercise regimens in the initial treatment and management of women with pelvic floor disorders. However, even with well-established recommendations, engaging patients and maintaining adherence to treatment plans and unmonitored programs at home are often difficult.”2 To help patients, those authors identified and evaluated patient-centered apps on topics in female pelvic medicine and reconstructive surgery.2
Two apps that assist patients in Kegel exercises are presented here. The Squeezy app includes guided pelvic floor muscle exercises with reminders, and the Kegel Nation app has a biofeedback feature.
The TABLE details the features of the 2 apps based on a shortened version of the APPLICATIONS scoring system, APPLI (app comprehensiveness, price, platform, literature used, and important special features).3
I hope clinicians find these apps helpful to their patients with pelvic floor disorders.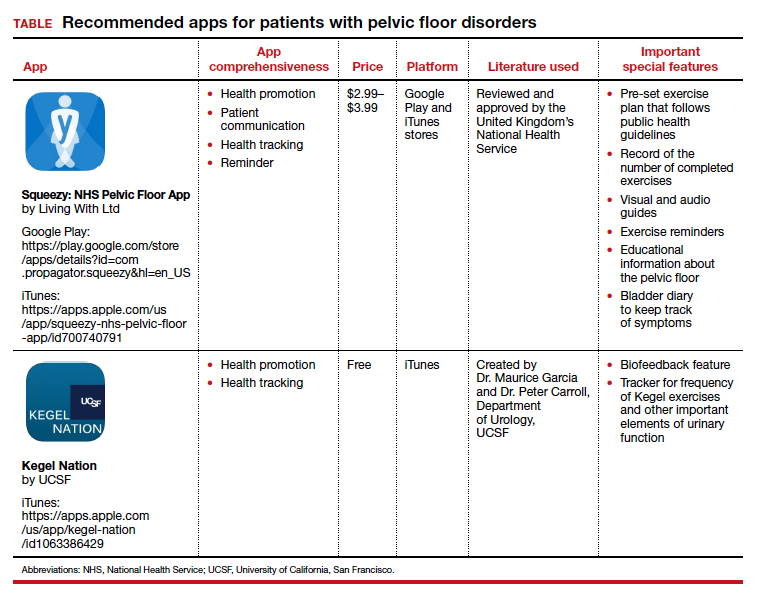
In the “You asked, Dr. Jen Gunter answered” series in The New York Times, Dr. Gunter writes that “pelvic floor exercises (also known as Kegel exercises) can be very helpful for urinary incontinence, pelvic organ prolapse, and fecal incontinence.” She continues to say that “pelvic floor exercises can be hard to master correctly, so it is important to make sure [one has] the correct technique. Many women can learn to do them after reading instructions like the ones found at the National Association for Continence, but some women may need their technique checked by their doctor, or help from a specialized pelvic floor physical therapist.”1
Similarly, Sudol and colleagues write that “guidelines from multiple medical societies emphasize the importance of patient education, behavioral therapy, and/or exercise regimens in the initial treatment and management of women with pelvic floor disorders. However, even with well-established recommendations, engaging patients and maintaining adherence to treatment plans and unmonitored programs at home are often difficult.”2 To help patients, those authors identified and evaluated patient-centered apps on topics in female pelvic medicine and reconstructive surgery.2
Two apps that assist patients in Kegel exercises are presented here. The Squeezy app includes guided pelvic floor muscle exercises with reminders, and the Kegel Nation app has a biofeedback feature.
The TABLE details the features of the 2 apps based on a shortened version of the APPLICATIONS scoring system, APPLI (app comprehensiveness, price, platform, literature used, and important special features).3
I hope clinicians find these apps helpful to their patients with pelvic floor disorders.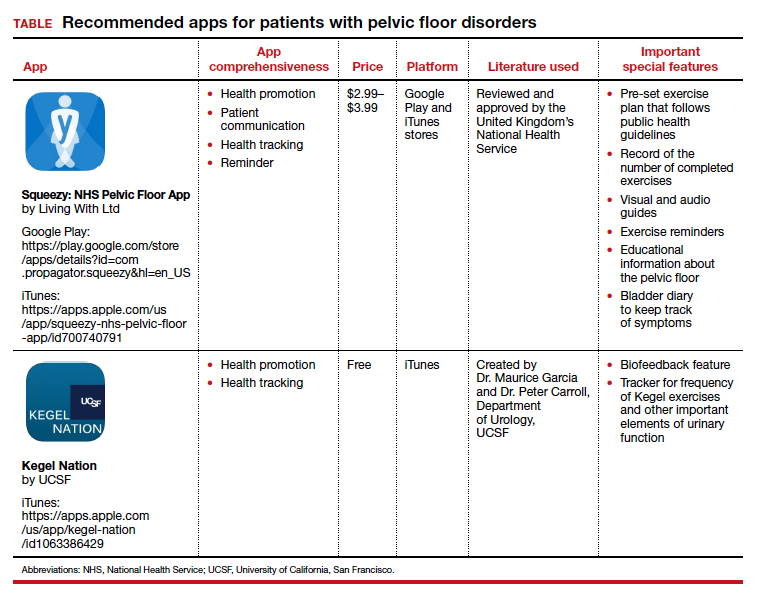
- Gunter J. You asked, Dr. Jen Gunter answered. New York Times. https://www.nytimes.com/ask/answers/kegels-pelvic-floor-exercises-yoni-eggs. Accessed December 22, 2020.
- Sudol NT, Adams-Piper E, Perry R, et al. In search of mobile applications for patients with pelvic floor disorders. Female Pelvic Med Reconstr Surg. 2019;25:252-256.
- Chyjek K, Farag S, Chen KT. Rating pregnancy wheel applications using the APPLICATIONS scoring system. Obstet Gynecol. 2015;125:1478-1483.
- Gunter J. You asked, Dr. Jen Gunter answered. New York Times. https://www.nytimes.com/ask/answers/kegels-pelvic-floor-exercises-yoni-eggs. Accessed December 22, 2020.
- Sudol NT, Adams-Piper E, Perry R, et al. In search of mobile applications for patients with pelvic floor disorders. Female Pelvic Med Reconstr Surg. 2019;25:252-256.
- Chyjek K, Farag S, Chen KT. Rating pregnancy wheel applications using the APPLICATIONS scoring system. Obstet Gynecol. 2015;125:1478-1483.
Apps for applying to ObGyn residency programs in the era of virtual interviews
The coronavirus disease 2019 (COVID-19) pandemic has upended the traditional 2020–2021 application season for ObGyn residency programs. In May 2020, the 2 national ObGyn education organizations, the Association of Professors of Gynecology and Obstetrics (APGO) and Council on Resident Education in ObGyn (CREOG), issued guidelines to ensure a fair and equitable application process.1 These guidelines are consistent with recommendations from the Association of American Medical Colleges (AAMC) and the Coalition for Physician Accountability. Important recommendations include:
- limiting away rotations
- being flexible in the number of specialty-specific letters of recommendation required
- encouraging residency programs to develop alternate means of conveying information about their curriculum.
In addition, these statements provide timing on when programs should release interview offers and when to begin interviews. Finally, programs are required to commit to online interviews and virtual visits for all applicants, including local students, rather than in-person interviews.
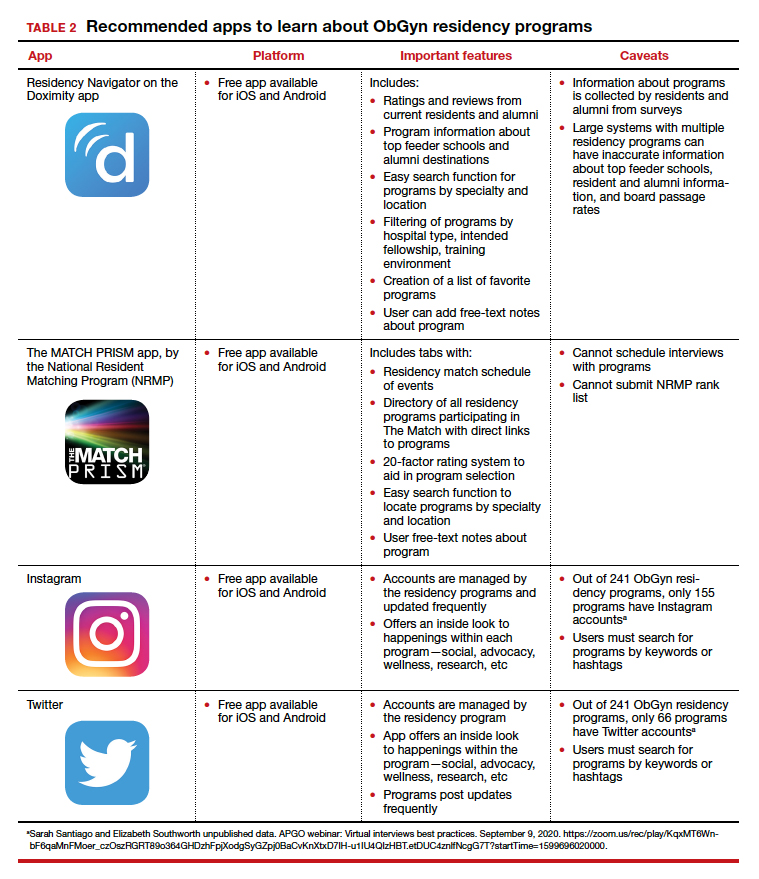
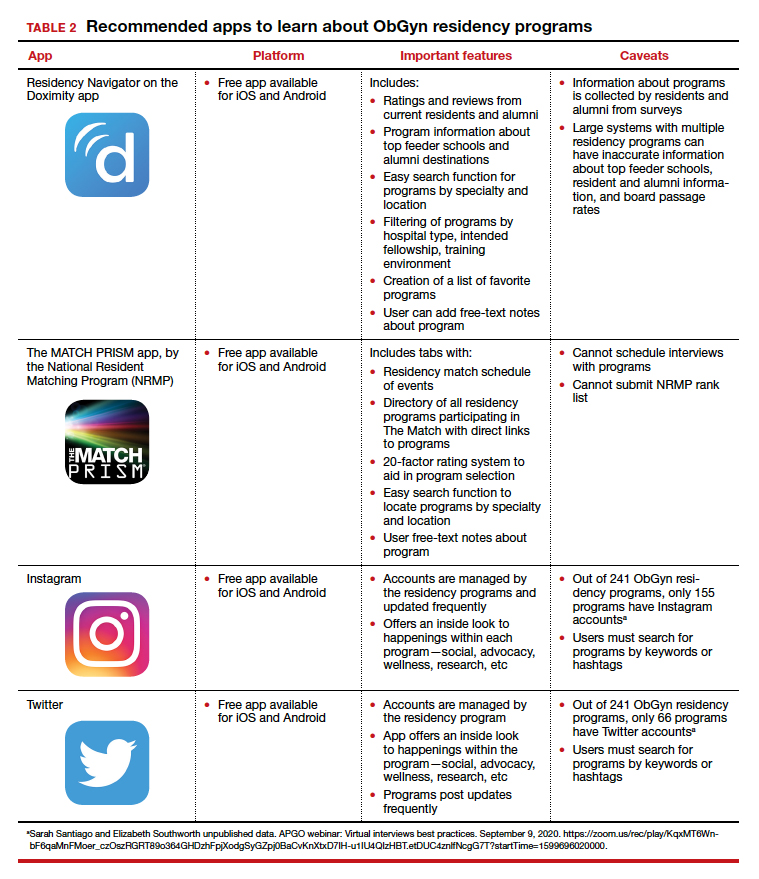
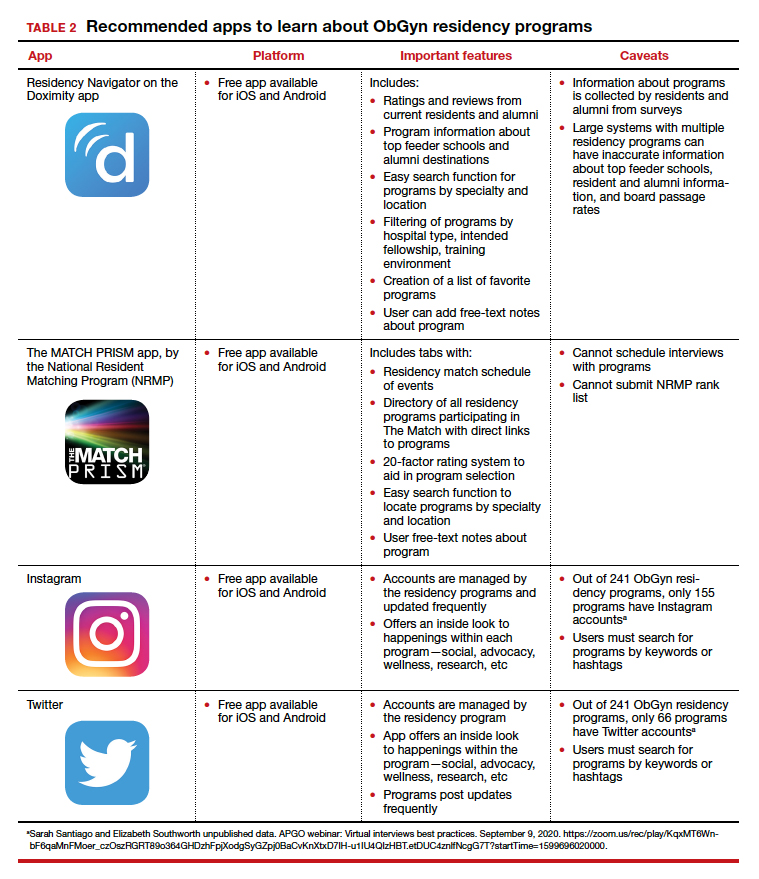
Here, we focus on identifying apps that students can use to help them with the application process—apps for the nuts and bolts of applying and interviewing and apps to learn more about individual programs.
Students must use the Electronic Residency Application Service (ERAS) platform from AAMC to enter their information and register with the National Resident Matching Program (NRMP). Students also must use the ERAS to submit their applications to their selected residency programs. The ERAS platform does not include an app to aid in the completion or submission of an application. The NRMP has developed the MATCH PRISM app, but this does not allow students to register for the match or submit their rank list. To learn about how to schedule interviews, residency programs may use one of the following sources: ERAS, Interview Broker, or Thalamus. Moreover, APGO/CREOG has partnered with Thalamus for the upcoming application cycle, which provides residency programs and applicants tools for application management, interview scheduling, and itinerary building. Thalamus offers a free app.
This year offers some unique challenges. The application process for ObGyn residencies is likely to be more competitive, and students face the added stress of having to navigate the interview season:
- without away rotations (audition interviews)
- without in-person visits of the city/hospital/program or social events before or after interview day
- with an all-virtual interview day.
Continue to: To find information on individual residency programs...
To find information on individual residency programs, the APGO website lists the FREIDA and APGO Residency Directories, which are not apps. Students are also aware of the Doximity Residency Navigator, which does include an app. The NRMP MATCH PRISM app is another resource, as it provides students with a directory of residency programs and information about each program.
The American College of Obstetricians and Gynecologists (ACOG) recognizes that residency program websites and social media will be crucial in helping applicants learn about individual programs, faculty, and residents. As such, ACOG hosted a Virtual Residency Showcase in September 2020 in which programs posted content on Instagram and Twitter using the hashtag #ACOG-ResWeek20.2 Similarly, APGO and CREOG produced a report containing a social media directory, which lists individual residency programs and whether or not they have a social media handle/account.3 In a recent webinar,4 Drs. Sarah Santiago and Elizabeth Southworth noted that the number of residency programs that have an Instagram account more than doubled (from 60 to 128) between May and September 2020.
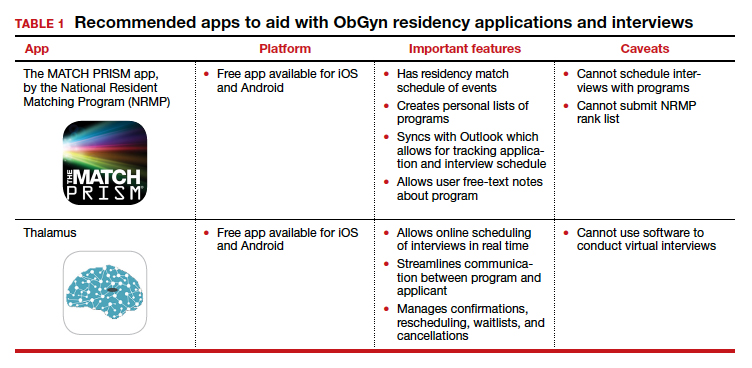
We present 2 tables describing the important features and caveats of apps available to students to assist them with residency applications this year—TABLE 1 summarizes apps to aid with applications and interviews; TABLE 2 lists apps designed for students to learn more about individual residency programs. We wish all of this year’s students every success in their search for the right program. ●
- Association of Professors of Gynecology and Obstetrics, Council on Resident Education in ObGyn. Updated APGO and CREOG Residency Application Response to COVID-19. https://www.apgo.org/wp-content/uploads/2020/05 /Updated-APGO-CREOG-Residency-Response-to -COVID-19-.pdf. Accessed October 27, 2020.
- https://www.acog.org/education-and-events/webinars /virtual-residency-showcase. Accessed October 4, 2020.
- Social media directory-ObGyn. https://docs.google.com /spreadsheets/d/e/2PACX-1vQ6boyn7FWV9tEhfQp1o3 XJgNIPNBQ3qCYf4IpV-rOPcd212J-HNR84p0r85nXrAz MvOmcNlgjywDP/pubhtml?gid=1472916499&single =true. Accessed October 27, 2020.
- APGO webinar: Virtual interviews best practices. September 9, 2020. https://zoom.us/rec/play/KqxMT6Wnb F6qaMnFMoer_czOszRGRT89o364GHDzhFpjXodgSyGZpj 0BaCvKnXtxD7IH-u1IU4QIzHBT.etDUC4znlfNcgG7T?start Time=1599696020000. Accessed October 4, 2020.
The coronavirus disease 2019 (COVID-19) pandemic has upended the traditional 2020–2021 application season for ObGyn residency programs. In May 2020, the 2 national ObGyn education organizations, the Association of Professors of Gynecology and Obstetrics (APGO) and Council on Resident Education in ObGyn (CREOG), issued guidelines to ensure a fair and equitable application process.1 These guidelines are consistent with recommendations from the Association of American Medical Colleges (AAMC) and the Coalition for Physician Accountability. Important recommendations include:
- limiting away rotations
- being flexible in the number of specialty-specific letters of recommendation required
- encouraging residency programs to develop alternate means of conveying information about their curriculum.
In addition, these statements provide timing on when programs should release interview offers and when to begin interviews. Finally, programs are required to commit to online interviews and virtual visits for all applicants, including local students, rather than in-person interviews.
Here, we focus on identifying apps that students can use to help them with the application process—apps for the nuts and bolts of applying and interviewing and apps to learn more about individual programs.
Students must use the Electronic Residency Application Service (ERAS) platform from AAMC to enter their information and register with the National Resident Matching Program (NRMP). Students also must use the ERAS to submit their applications to their selected residency programs. The ERAS platform does not include an app to aid in the completion or submission of an application. The NRMP has developed the MATCH PRISM app, but this does not allow students to register for the match or submit their rank list. To learn about how to schedule interviews, residency programs may use one of the following sources: ERAS, Interview Broker, or Thalamus. Moreover, APGO/CREOG has partnered with Thalamus for the upcoming application cycle, which provides residency programs and applicants tools for application management, interview scheduling, and itinerary building. Thalamus offers a free app.
This year offers some unique challenges. The application process for ObGyn residencies is likely to be more competitive, and students face the added stress of having to navigate the interview season:
- without away rotations (audition interviews)
- without in-person visits of the city/hospital/program or social events before or after interview day
- with an all-virtual interview day.
Continue to: To find information on individual residency programs...
To find information on individual residency programs, the APGO website lists the FREIDA and APGO Residency Directories, which are not apps. Students are also aware of the Doximity Residency Navigator, which does include an app. The NRMP MATCH PRISM app is another resource, as it provides students with a directory of residency programs and information about each program.
The American College of Obstetricians and Gynecologists (ACOG) recognizes that residency program websites and social media will be crucial in helping applicants learn about individual programs, faculty, and residents. As such, ACOG hosted a Virtual Residency Showcase in September 2020 in which programs posted content on Instagram and Twitter using the hashtag #ACOG-ResWeek20.2 Similarly, APGO and CREOG produced a report containing a social media directory, which lists individual residency programs and whether or not they have a social media handle/account.3 In a recent webinar,4 Drs. Sarah Santiago and Elizabeth Southworth noted that the number of residency programs that have an Instagram account more than doubled (from 60 to 128) between May and September 2020.
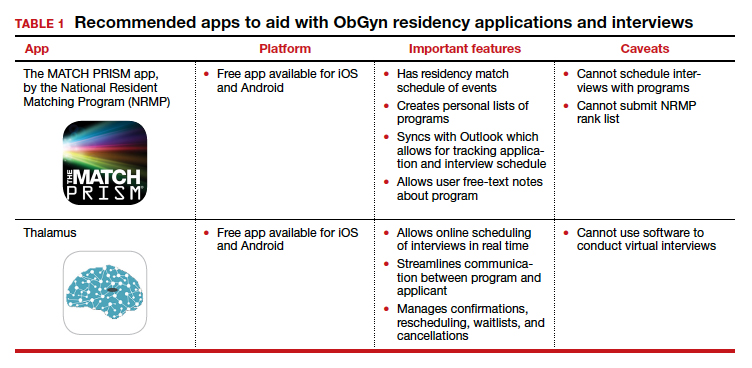
We present 2 tables describing the important features and caveats of apps available to students to assist them with residency applications this year—TABLE 1 summarizes apps to aid with applications and interviews; TABLE 2 lists apps designed for students to learn more about individual residency programs. We wish all of this year’s students every success in their search for the right program. ●
The coronavirus disease 2019 (COVID-19) pandemic has upended the traditional 2020–2021 application season for ObGyn residency programs. In May 2020, the 2 national ObGyn education organizations, the Association of Professors of Gynecology and Obstetrics (APGO) and Council on Resident Education in ObGyn (CREOG), issued guidelines to ensure a fair and equitable application process.1 These guidelines are consistent with recommendations from the Association of American Medical Colleges (AAMC) and the Coalition for Physician Accountability. Important recommendations include:
- limiting away rotations
- being flexible in the number of specialty-specific letters of recommendation required
- encouraging residency programs to develop alternate means of conveying information about their curriculum.
In addition, these statements provide timing on when programs should release interview offers and when to begin interviews. Finally, programs are required to commit to online interviews and virtual visits for all applicants, including local students, rather than in-person interviews.
Here, we focus on identifying apps that students can use to help them with the application process—apps for the nuts and bolts of applying and interviewing and apps to learn more about individual programs.
Students must use the Electronic Residency Application Service (ERAS) platform from AAMC to enter their information and register with the National Resident Matching Program (NRMP). Students also must use the ERAS to submit their applications to their selected residency programs. The ERAS platform does not include an app to aid in the completion or submission of an application. The NRMP has developed the MATCH PRISM app, but this does not allow students to register for the match or submit their rank list. To learn about how to schedule interviews, residency programs may use one of the following sources: ERAS, Interview Broker, or Thalamus. Moreover, APGO/CREOG has partnered with Thalamus for the upcoming application cycle, which provides residency programs and applicants tools for application management, interview scheduling, and itinerary building. Thalamus offers a free app.
This year offers some unique challenges. The application process for ObGyn residencies is likely to be more competitive, and students face the added stress of having to navigate the interview season:
- without away rotations (audition interviews)
- without in-person visits of the city/hospital/program or social events before or after interview day
- with an all-virtual interview day.
Continue to: To find information on individual residency programs...
To find information on individual residency programs, the APGO website lists the FREIDA and APGO Residency Directories, which are not apps. Students are also aware of the Doximity Residency Navigator, which does include an app. The NRMP MATCH PRISM app is another resource, as it provides students with a directory of residency programs and information about each program.
The American College of Obstetricians and Gynecologists (ACOG) recognizes that residency program websites and social media will be crucial in helping applicants learn about individual programs, faculty, and residents. As such, ACOG hosted a Virtual Residency Showcase in September 2020 in which programs posted content on Instagram and Twitter using the hashtag #ACOG-ResWeek20.2 Similarly, APGO and CREOG produced a report containing a social media directory, which lists individual residency programs and whether or not they have a social media handle/account.3 In a recent webinar,4 Drs. Sarah Santiago and Elizabeth Southworth noted that the number of residency programs that have an Instagram account more than doubled (from 60 to 128) between May and September 2020.
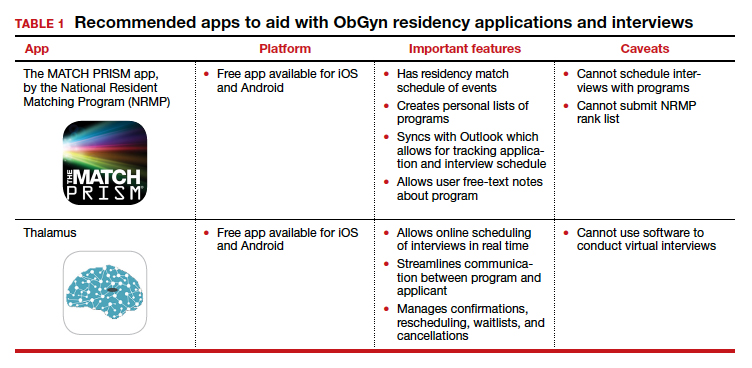
We present 2 tables describing the important features and caveats of apps available to students to assist them with residency applications this year—TABLE 1 summarizes apps to aid with applications and interviews; TABLE 2 lists apps designed for students to learn more about individual residency programs. We wish all of this year’s students every success in their search for the right program. ●
- Association of Professors of Gynecology and Obstetrics, Council on Resident Education in ObGyn. Updated APGO and CREOG Residency Application Response to COVID-19. https://www.apgo.org/wp-content/uploads/2020/05 /Updated-APGO-CREOG-Residency-Response-to -COVID-19-.pdf. Accessed October 27, 2020.
- https://www.acog.org/education-and-events/webinars /virtual-residency-showcase. Accessed October 4, 2020.
- Social media directory-ObGyn. https://docs.google.com /spreadsheets/d/e/2PACX-1vQ6boyn7FWV9tEhfQp1o3 XJgNIPNBQ3qCYf4IpV-rOPcd212J-HNR84p0r85nXrAz MvOmcNlgjywDP/pubhtml?gid=1472916499&single =true. Accessed October 27, 2020.
- APGO webinar: Virtual interviews best practices. September 9, 2020. https://zoom.us/rec/play/KqxMT6Wnb F6qaMnFMoer_czOszRGRT89o364GHDzhFpjXodgSyGZpj 0BaCvKnXtxD7IH-u1IU4QIzHBT.etDUC4znlfNcgG7T?start Time=1599696020000. Accessed October 4, 2020.
- Association of Professors of Gynecology and Obstetrics, Council on Resident Education in ObGyn. Updated APGO and CREOG Residency Application Response to COVID-19. https://www.apgo.org/wp-content/uploads/2020/05 /Updated-APGO-CREOG-Residency-Response-to -COVID-19-.pdf. Accessed October 27, 2020.
- https://www.acog.org/education-and-events/webinars /virtual-residency-showcase. Accessed October 4, 2020.
- Social media directory-ObGyn. https://docs.google.com /spreadsheets/d/e/2PACX-1vQ6boyn7FWV9tEhfQp1o3 XJgNIPNBQ3qCYf4IpV-rOPcd212J-HNR84p0r85nXrAz MvOmcNlgjywDP/pubhtml?gid=1472916499&single =true. Accessed October 27, 2020.
- APGO webinar: Virtual interviews best practices. September 9, 2020. https://zoom.us/rec/play/KqxMT6Wnb F6qaMnFMoer_czOszRGRT89o364GHDzhFpjXodgSyGZpj 0BaCvKnXtxD7IH-u1IU4QIzHBT.etDUC4znlfNcgG7T?start Time=1599696020000. Accessed October 4, 2020.
A pandemic playbook for residency programs in the COVID-19 era: Lessons learned from ObGyn programs at the epicenter
The 2020 pandemic of coronavirus disease 2019 (COVID-19) has presented significant challenges to the health care workforce.1,2 As New York City and its environs became the epicenter of the pandemic in the United States, we continued to care for our patients while simultaneously maintaining the education and well-being of our residents.3 Keeping this balance significantly strained resources and presented new challenges for education and service in residency education. What first emerged as an acute emergency has become a chronic disruption in the clinical learning environment. Programs are working to respond to the critical patient needs while ensuring continued progress toward training goals.
Since pregnancy is one condition for which healthy patients continued to require both outpatient visits and inpatient hospitalization, volume was not anticipated to be significantly decreased on our units. Thus, our ObGyn residency programs sought to expeditiously restructure our workforce and educational methods to address the demands of the pandemic. We were aided in our efforts by the Accreditation Council for Graduate Medical Education (ACGME) Extraordinary Circumstances policy. Our institutions were deemed to be functioning at Stage 3 Pandemic Emergency Status, a state in which “the increase in volume and/or severity of illness creates an extraordinary circumstance where routine care, education, and delivery must be reconfigured to focus only on patient care.”4
As of May 18, 2020, 26% of residency and fellowship programs in the United States were under Stage 3 COVID-19 Pandemic Emergency Status.5 Accordingly, our patient care delivery and educational processes were reconfigured within the context of Stage 3 Status, governed by the overriding principles of ensuring appropriate resources and training, adhering to work hour limits, providing adequate supervision, and credentialing fellows to function in our core specialty.
As ObGyn education leaders from 5 academic medical centers within the COVID-19 epicenter, we present a summary of best practices, based on our experiences, for each of the 4 categories of Stage 3 Status outlined by the ACGME. In an era of globalization, we must learn from pandemics, a call made after the Ebola outbreak in 2015.6 We recognize that this type of disruption could happen again with a possible second wave of COVID-19 or another emerging disease.7 Thus, we emphasize “lessons learned” that are applicable to a wide range of residency training programs facing various clinical crises.
Ensuring adequate resources and training
Within the context of Stage 3 Status, residency programs have the flexibility to increase residents’ availability in the clinical care setting. However, programs must ensure the safety of both patients and residents.
Continue to: Measures to decrease risk of infection...
Measures to decrease risk of infection
One critical resource needed to protect patients and residents is personal protective equipment (PPE). Online instruction and in-person training were used to educate residents and staff on appropriate techniques for donning, doffing, and conserving PPE. Surgical teams were limited to 1 surgeon and 1 resident in each case. In an effort to limit direct contact with COVID-19 infected patients, the number of health care providers rounding on inpatients was restricted, and phone or video conversations were used for communication.
The workforce was modified to decrease exposure to infection and maintain a reserve of healthy residents who were working from home—anticipating that some residents would become ill and this reserve would be called for duty. Similar to other specialties, our programs organized the workforce by arranging residents into teams in which residents worked a number of shifts in a row.8-12 Regular block schedules were disrupted and non-core rotations were deferred.
As surgeries were canceled and outpatient visits curtailed, many rotations required less resident coverage. Residents were reassigned from rotations where clinical work was suspended to accommodate increased staffing needs in other areas, while accounting for residents who were ill or on leave for postexposure quarantine. Typically, residents worked 12-hour shifts for 3 to 6 days followed by several days off or days working remotely. This team-based strategy decreased the number of residents exposed to COVID-19 at one time, provided time for recuperation, encouraged camaraderie, and enabled residents working remotely to coordinate care and participate in telehealth without direct patient contact.
To minimize high-risk exposure of pregnant residents or residents with underlying health conditions, these residents also worked remotely. Similar to other specialties, it was important to determine essential resident duties and enlist assistance from other clinicians, such as fellows, nurse practitioners, physician assistants, and midwives.
To protect residents and patients, maximizing testing of patients for COVID-19 was an important strategy. Based on early experience at 1 center with patients who were initially asymptomatic but later developed symptoms and tested positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), universal testing was implemented and endorsed by the New York State COVID-19 Maternity Task Force.13 Notably, 87.9% of patients who were positive for SARS-CoV-2 at the time of admission had no symptoms of COVID-19 at presentation. Because the asymptomatic carrier rate appears to be high in obstetric patients, testing of patients is paramount.3,14 Finally, suspending visitation (except for 1 support person) also was instrumental in decreasing the risk of infection to residents.13
Resources for residents with COVID-19
This pandemic placed residency program directors in an unusual situation as frontline caregivers for their own residents. It was imperative to track residents with physical symptoms, conduct testing when possible, and follow the course of residents with confirmed or suspected COVID-19. As serious illness and death have been reported among otherwise healthy young people, we ensured that our homebound residents were frequently monitored.15 At several of our centers, residents with COVID-19 from any program who chose to separate from their families were provided with alternative housing accommodations. In addition, some of our graduate medical education offices identified specific physicians to care for residents with COVID-19 who did not require hospitalization.
Continue to: Deployment to other specialties...
Deployment to other specialties
Several hospitals in the United States redeployed residents because of staffing shortages in high-impact settings.12 It was important for ObGyns to emphasize that the labor and delivery unit functions as the emergency ward for pregnant women, and that ObGyn residents possess skills specific to the care of these patients.
For our departments, we highlighted that external redeployment could adversely affect our workforce restructuring and, ultimately, patient care. We focused efforts on internal deployment or reassignment as much as possible. Some faculty and fellows in nonobstetric subspecialty areas were redirected to provide care on our inpatient obstetric services.
Educating residents
To maintain educational efforts with social distancing, we used videoconferencing to preserve the protected didactic education time that existed for our residents before the pandemic. This regularly scheduled, nonclinical time also was utilized to instruct residents on the rapidly changing clinical guidelines and to disseminate information about new institutional policies and procedures, ensuring that residents were adequately prepared for their new clinical work.
Work hour requirements
The ACGME requires that work hour limitations remain unchanged during Stage 3 Pandemic Emergency Status. As the pandemic presented new challenges and stressors for residents inside and outside the workplace, ensuring adequate time off to rest and recover was critical for maintaining the resident workforce’s health and wellness.
Thus, our workforce restructuring plans accounted for work hour limitations. As detailed above, the restructuring was accomplished by cohorting residents into small teams that remained unchanged for several weeks. Most shifts were limited to 12 hours, residents continued to be assigned at least 1 day off each week, and daily schedules were structured to ensure at least 10 hours off between shifts. Time spent working remotely was included in work hour calculations.
In addition, residents on “jeopardy” who were available for those who needed to be removed from direct patient care were given at least 1 day off per week in which they could not be pulled for clinical duty. Finally, prolonged inpatient assignments were limited; after these assignments, residents were given increased time for rest and recuperation.
Ensuring adequate supervision
The expectation during Stage 3 Pandemic Emergency Status is that residents, with adequate supervision, provide care that is appropriate for their level of training. To adequately and safely supervise residents, faculty needed training to remain well informed about the clinical care of COVID-19 patients. This was accomplished through frequent communication and consultation with colleagues in infectious disease, occupational health, and guidance from national organizations, such as the American College of Obstetricians and Gynecologists and the Centers for Disease Control and Prevention, and information from our state health departments.
Faculty members were trained in safe donning and doffing of PPE and infection control strategies to ensure they could safely oversee and train residents in these practices. Faculty schedules were significantly altered to ensure an adequate workforce and adequate resident supervision. Faculty efforts were focused on areas of critical need—in our case inpatient obstetrics—with a smaller workforce assigned to outpatient services and inpatient gynecology and gynecologic oncology. Many ObGyn subspecialist faculty were redeployed to general ObGyn inpatient units, thus permitting appropriate resident supervision at all times. In the outpatient setting, faculty adjusted to the changing demands and learned to conduct and supervise telehealth visits.
Finally, for those whose residents were deployed to other services (for example, internal medicine, emergency medicine, or critical care), supervision became paramount. We checked in with our deployed residents daily to be sure that their supervision on those services was adequate. Considering the extreme complexity, rapidly changing understanding of the disease, and often tragic patient outcomes, it was essential to ensure appropriate support and supervision on “off service” deployment.
Continue to: Fellows functioning in core specialty...
Fellows functioning in core specialty
Anticipating the increased need for clinicians on the obstetric services, fellows in subspecialty areas were granted emergency privileges to act as attending faculty in the core specialty, supervising residents and providing patient care. On the other hand, some of those fellows, primarily in gynecologic oncology, were externally redeployed out of core specialty to internal medicine and critical care units. Careful consideration of the fellows’ needs for supervision and support in these roles was essential, and similar support measures that were put in place for our residents were offered to fellows.
In conclusion
The COVID-19 pandemic has presented diverse and complex challenges to the entire health care workforce. Because this crisis is widespread and likely will be lengthy, a sustained and organized response is required.16 We have highlighted unique challenges specific to residency programs and presented collective best practices from our experiences in ObGyn navigating these obstacles, which are applicable to many other programs.
The flexibility and relief afforded by the ACGME Stage 3 Pandemic Emergency Status designation allowed us to meet the needs of the surge of patients that required care while we maintained our educational framework and tenets of providing adequate resources and training, working within the confines of safe work hours, ensuring proper supervision, and granting attending privileges to fellows in their core specialty. ●
- Panahi L, Amiri M, Pouy S. Risks of novel coronavirus disease (COVID-19) in pregnancy; a narrative review. Arch Acad Emerg Med. 2020;8e34.
- Rasmussen SA, Smulian JC, Lednicky JA, et al. Coronavirus disease 2019 (COVID-19) and pregnancy: what obstetricians need to know. Am J Obstet Gynecol. 2020;222:415-426.
- Sutton D, Fuchs K, D'Alton M, et al. Universal screening for SARS-CoV-2 in women admitted for delivery. N Engl J Med. 2020;382:2163-2164.
- Accreditation Council for Graduate Medical Education. Three stages of GME during the COVID-19 pandemic. https://www.acgme.org/COVID-19/Three-Stages-of-GME-During-the-COVID-19-Pandemic. Accessed May 28, 2020.
- Accreditation Council for Graduate Medical Education. Emergency category maps/5-18-20: percentage of residents in each state/territory under pandemic emergency status. Percentage of residency and fellowship programs under ACGME COVID-19 pandemic emergency status (stage 3). https://dl.acgme.org/learn/course/sponsoring-institution-idea-exchange/emergency-category-maps/5-18-20-percentage-of-residents-in-each-state-territory-under-pandemic-emergency-status. Accessed May 28, 2020.
- Gates B. The next epidemic--lessons from Ebola. N Engl J Med. 2015;372:1381-1384.
- Pepe D, Martinello RA, Juthani-Mehta M. Involving physicians-in-training in the care of patients during epidemics. J Grad Med Educ. 2019;11:632-634.
- Crosby DL, Sharma A. Insights on otolaryngology residency training during the COVID-19 pandemic. Otolaryngol Head Neck Surg. 2020;163:38-41.
- Kim CS, Lynch JB, Seth C, et al. One academic health system's early (and ongoing) experience responding to COVID-19: recommendations from the initial epicenter of the pandemic in the United States. Acad Med. 2020;95:1146-1148.
- Kogan M, Klein SE, Hannon CP, et al. Orthopaedic education during the COVID-19 pandemic. J Am Acad Orthop Surg. 2020; 28:e456-e464.
- Vargo E, Ali M, Henry F, et al. Cleveland Clinic Akron general urology residency program's COVID-19 experience. Urology. 2020;140:1-3.
- Zarzaur BL, Stahl CC, Greenberg JA, et al. Blueprint for restructuring a department of surgery in concert with the health care system during a pandemic: the University of Wisconsin experience. JAMA Surg. 2020. doi: 10.1001/jamasurg.2020.1386.
- New York State COVID-19 Maternity Task Force. Recommendations to the governor to promote increased choice and access to safe maternity care during the COVID-19 pandemic. https://www.governor.ny.gov/sites/governor.ny.gov/files/atoms/files/042920_CMTF_Recommendations.pdf. Accessed May 28, 2020.
- Campbell KH, Tornatore JM, Lawrence KE, et al. Prevalence of SARS-CoV-2 among patients admitted for childbirth in southern Connecticut. JAMA. 2020;323:2520-2522.
- CDC COVID-19 Response Team. Severe outcomes among patients with coronavirus disease 2019 (COVID-19)--United States, February 12-March 16, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:343-346.
- Kissler SM, Tedijanto C, Goldstein E, et al. Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period. Science. 2020;368:860-868.
The 2020 pandemic of coronavirus disease 2019 (COVID-19) has presented significant challenges to the health care workforce.1,2 As New York City and its environs became the epicenter of the pandemic in the United States, we continued to care for our patients while simultaneously maintaining the education and well-being of our residents.3 Keeping this balance significantly strained resources and presented new challenges for education and service in residency education. What first emerged as an acute emergency has become a chronic disruption in the clinical learning environment. Programs are working to respond to the critical patient needs while ensuring continued progress toward training goals.
Since pregnancy is one condition for which healthy patients continued to require both outpatient visits and inpatient hospitalization, volume was not anticipated to be significantly decreased on our units. Thus, our ObGyn residency programs sought to expeditiously restructure our workforce and educational methods to address the demands of the pandemic. We were aided in our efforts by the Accreditation Council for Graduate Medical Education (ACGME) Extraordinary Circumstances policy. Our institutions were deemed to be functioning at Stage 3 Pandemic Emergency Status, a state in which “the increase in volume and/or severity of illness creates an extraordinary circumstance where routine care, education, and delivery must be reconfigured to focus only on patient care.”4
As of May 18, 2020, 26% of residency and fellowship programs in the United States were under Stage 3 COVID-19 Pandemic Emergency Status.5 Accordingly, our patient care delivery and educational processes were reconfigured within the context of Stage 3 Status, governed by the overriding principles of ensuring appropriate resources and training, adhering to work hour limits, providing adequate supervision, and credentialing fellows to function in our core specialty.
As ObGyn education leaders from 5 academic medical centers within the COVID-19 epicenter, we present a summary of best practices, based on our experiences, for each of the 4 categories of Stage 3 Status outlined by the ACGME. In an era of globalization, we must learn from pandemics, a call made after the Ebola outbreak in 2015.6 We recognize that this type of disruption could happen again with a possible second wave of COVID-19 or another emerging disease.7 Thus, we emphasize “lessons learned” that are applicable to a wide range of residency training programs facing various clinical crises.
Ensuring adequate resources and training
Within the context of Stage 3 Status, residency programs have the flexibility to increase residents’ availability in the clinical care setting. However, programs must ensure the safety of both patients and residents.
Continue to: Measures to decrease risk of infection...
Measures to decrease risk of infection
One critical resource needed to protect patients and residents is personal protective equipment (PPE). Online instruction and in-person training were used to educate residents and staff on appropriate techniques for donning, doffing, and conserving PPE. Surgical teams were limited to 1 surgeon and 1 resident in each case. In an effort to limit direct contact with COVID-19 infected patients, the number of health care providers rounding on inpatients was restricted, and phone or video conversations were used for communication.
The workforce was modified to decrease exposure to infection and maintain a reserve of healthy residents who were working from home—anticipating that some residents would become ill and this reserve would be called for duty. Similar to other specialties, our programs organized the workforce by arranging residents into teams in which residents worked a number of shifts in a row.8-12 Regular block schedules were disrupted and non-core rotations were deferred.
As surgeries were canceled and outpatient visits curtailed, many rotations required less resident coverage. Residents were reassigned from rotations where clinical work was suspended to accommodate increased staffing needs in other areas, while accounting for residents who were ill or on leave for postexposure quarantine. Typically, residents worked 12-hour shifts for 3 to 6 days followed by several days off or days working remotely. This team-based strategy decreased the number of residents exposed to COVID-19 at one time, provided time for recuperation, encouraged camaraderie, and enabled residents working remotely to coordinate care and participate in telehealth without direct patient contact.
To minimize high-risk exposure of pregnant residents or residents with underlying health conditions, these residents also worked remotely. Similar to other specialties, it was important to determine essential resident duties and enlist assistance from other clinicians, such as fellows, nurse practitioners, physician assistants, and midwives.
To protect residents and patients, maximizing testing of patients for COVID-19 was an important strategy. Based on early experience at 1 center with patients who were initially asymptomatic but later developed symptoms and tested positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), universal testing was implemented and endorsed by the New York State COVID-19 Maternity Task Force.13 Notably, 87.9% of patients who were positive for SARS-CoV-2 at the time of admission had no symptoms of COVID-19 at presentation. Because the asymptomatic carrier rate appears to be high in obstetric patients, testing of patients is paramount.3,14 Finally, suspending visitation (except for 1 support person) also was instrumental in decreasing the risk of infection to residents.13
Resources for residents with COVID-19
This pandemic placed residency program directors in an unusual situation as frontline caregivers for their own residents. It was imperative to track residents with physical symptoms, conduct testing when possible, and follow the course of residents with confirmed or suspected COVID-19. As serious illness and death have been reported among otherwise healthy young people, we ensured that our homebound residents were frequently monitored.15 At several of our centers, residents with COVID-19 from any program who chose to separate from their families were provided with alternative housing accommodations. In addition, some of our graduate medical education offices identified specific physicians to care for residents with COVID-19 who did not require hospitalization.
Continue to: Deployment to other specialties...
Deployment to other specialties
Several hospitals in the United States redeployed residents because of staffing shortages in high-impact settings.12 It was important for ObGyns to emphasize that the labor and delivery unit functions as the emergency ward for pregnant women, and that ObGyn residents possess skills specific to the care of these patients.
For our departments, we highlighted that external redeployment could adversely affect our workforce restructuring and, ultimately, patient care. We focused efforts on internal deployment or reassignment as much as possible. Some faculty and fellows in nonobstetric subspecialty areas were redirected to provide care on our inpatient obstetric services.
Educating residents
To maintain educational efforts with social distancing, we used videoconferencing to preserve the protected didactic education time that existed for our residents before the pandemic. This regularly scheduled, nonclinical time also was utilized to instruct residents on the rapidly changing clinical guidelines and to disseminate information about new institutional policies and procedures, ensuring that residents were adequately prepared for their new clinical work.
Work hour requirements
The ACGME requires that work hour limitations remain unchanged during Stage 3 Pandemic Emergency Status. As the pandemic presented new challenges and stressors for residents inside and outside the workplace, ensuring adequate time off to rest and recover was critical for maintaining the resident workforce’s health and wellness.
Thus, our workforce restructuring plans accounted for work hour limitations. As detailed above, the restructuring was accomplished by cohorting residents into small teams that remained unchanged for several weeks. Most shifts were limited to 12 hours, residents continued to be assigned at least 1 day off each week, and daily schedules were structured to ensure at least 10 hours off between shifts. Time spent working remotely was included in work hour calculations.
In addition, residents on “jeopardy” who were available for those who needed to be removed from direct patient care were given at least 1 day off per week in which they could not be pulled for clinical duty. Finally, prolonged inpatient assignments were limited; after these assignments, residents were given increased time for rest and recuperation.
Ensuring adequate supervision
The expectation during Stage 3 Pandemic Emergency Status is that residents, with adequate supervision, provide care that is appropriate for their level of training. To adequately and safely supervise residents, faculty needed training to remain well informed about the clinical care of COVID-19 patients. This was accomplished through frequent communication and consultation with colleagues in infectious disease, occupational health, and guidance from national organizations, such as the American College of Obstetricians and Gynecologists and the Centers for Disease Control and Prevention, and information from our state health departments.
Faculty members were trained in safe donning and doffing of PPE and infection control strategies to ensure they could safely oversee and train residents in these practices. Faculty schedules were significantly altered to ensure an adequate workforce and adequate resident supervision. Faculty efforts were focused on areas of critical need—in our case inpatient obstetrics—with a smaller workforce assigned to outpatient services and inpatient gynecology and gynecologic oncology. Many ObGyn subspecialist faculty were redeployed to general ObGyn inpatient units, thus permitting appropriate resident supervision at all times. In the outpatient setting, faculty adjusted to the changing demands and learned to conduct and supervise telehealth visits.
Finally, for those whose residents were deployed to other services (for example, internal medicine, emergency medicine, or critical care), supervision became paramount. We checked in with our deployed residents daily to be sure that their supervision on those services was adequate. Considering the extreme complexity, rapidly changing understanding of the disease, and often tragic patient outcomes, it was essential to ensure appropriate support and supervision on “off service” deployment.
Continue to: Fellows functioning in core specialty...
Fellows functioning in core specialty
Anticipating the increased need for clinicians on the obstetric services, fellows in subspecialty areas were granted emergency privileges to act as attending faculty in the core specialty, supervising residents and providing patient care. On the other hand, some of those fellows, primarily in gynecologic oncology, were externally redeployed out of core specialty to internal medicine and critical care units. Careful consideration of the fellows’ needs for supervision and support in these roles was essential, and similar support measures that were put in place for our residents were offered to fellows.
In conclusion
The COVID-19 pandemic has presented diverse and complex challenges to the entire health care workforce. Because this crisis is widespread and likely will be lengthy, a sustained and organized response is required.16 We have highlighted unique challenges specific to residency programs and presented collective best practices from our experiences in ObGyn navigating these obstacles, which are applicable to many other programs.
The flexibility and relief afforded by the ACGME Stage 3 Pandemic Emergency Status designation allowed us to meet the needs of the surge of patients that required care while we maintained our educational framework and tenets of providing adequate resources and training, working within the confines of safe work hours, ensuring proper supervision, and granting attending privileges to fellows in their core specialty. ●
The 2020 pandemic of coronavirus disease 2019 (COVID-19) has presented significant challenges to the health care workforce.1,2 As New York City and its environs became the epicenter of the pandemic in the United States, we continued to care for our patients while simultaneously maintaining the education and well-being of our residents.3 Keeping this balance significantly strained resources and presented new challenges for education and service in residency education. What first emerged as an acute emergency has become a chronic disruption in the clinical learning environment. Programs are working to respond to the critical patient needs while ensuring continued progress toward training goals.
Since pregnancy is one condition for which healthy patients continued to require both outpatient visits and inpatient hospitalization, volume was not anticipated to be significantly decreased on our units. Thus, our ObGyn residency programs sought to expeditiously restructure our workforce and educational methods to address the demands of the pandemic. We were aided in our efforts by the Accreditation Council for Graduate Medical Education (ACGME) Extraordinary Circumstances policy. Our institutions were deemed to be functioning at Stage 3 Pandemic Emergency Status, a state in which “the increase in volume and/or severity of illness creates an extraordinary circumstance where routine care, education, and delivery must be reconfigured to focus only on patient care.”4
As of May 18, 2020, 26% of residency and fellowship programs in the United States were under Stage 3 COVID-19 Pandemic Emergency Status.5 Accordingly, our patient care delivery and educational processes were reconfigured within the context of Stage 3 Status, governed by the overriding principles of ensuring appropriate resources and training, adhering to work hour limits, providing adequate supervision, and credentialing fellows to function in our core specialty.
As ObGyn education leaders from 5 academic medical centers within the COVID-19 epicenter, we present a summary of best practices, based on our experiences, for each of the 4 categories of Stage 3 Status outlined by the ACGME. In an era of globalization, we must learn from pandemics, a call made after the Ebola outbreak in 2015.6 We recognize that this type of disruption could happen again with a possible second wave of COVID-19 or another emerging disease.7 Thus, we emphasize “lessons learned” that are applicable to a wide range of residency training programs facing various clinical crises.
Ensuring adequate resources and training
Within the context of Stage 3 Status, residency programs have the flexibility to increase residents’ availability in the clinical care setting. However, programs must ensure the safety of both patients and residents.
Continue to: Measures to decrease risk of infection...
Measures to decrease risk of infection
One critical resource needed to protect patients and residents is personal protective equipment (PPE). Online instruction and in-person training were used to educate residents and staff on appropriate techniques for donning, doffing, and conserving PPE. Surgical teams were limited to 1 surgeon and 1 resident in each case. In an effort to limit direct contact with COVID-19 infected patients, the number of health care providers rounding on inpatients was restricted, and phone or video conversations were used for communication.
The workforce was modified to decrease exposure to infection and maintain a reserve of healthy residents who were working from home—anticipating that some residents would become ill and this reserve would be called for duty. Similar to other specialties, our programs organized the workforce by arranging residents into teams in which residents worked a number of shifts in a row.8-12 Regular block schedules were disrupted and non-core rotations were deferred.
As surgeries were canceled and outpatient visits curtailed, many rotations required less resident coverage. Residents were reassigned from rotations where clinical work was suspended to accommodate increased staffing needs in other areas, while accounting for residents who were ill or on leave for postexposure quarantine. Typically, residents worked 12-hour shifts for 3 to 6 days followed by several days off or days working remotely. This team-based strategy decreased the number of residents exposed to COVID-19 at one time, provided time for recuperation, encouraged camaraderie, and enabled residents working remotely to coordinate care and participate in telehealth without direct patient contact.
To minimize high-risk exposure of pregnant residents or residents with underlying health conditions, these residents also worked remotely. Similar to other specialties, it was important to determine essential resident duties and enlist assistance from other clinicians, such as fellows, nurse practitioners, physician assistants, and midwives.
To protect residents and patients, maximizing testing of patients for COVID-19 was an important strategy. Based on early experience at 1 center with patients who were initially asymptomatic but later developed symptoms and tested positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), universal testing was implemented and endorsed by the New York State COVID-19 Maternity Task Force.13 Notably, 87.9% of patients who were positive for SARS-CoV-2 at the time of admission had no symptoms of COVID-19 at presentation. Because the asymptomatic carrier rate appears to be high in obstetric patients, testing of patients is paramount.3,14 Finally, suspending visitation (except for 1 support person) also was instrumental in decreasing the risk of infection to residents.13
Resources for residents with COVID-19
This pandemic placed residency program directors in an unusual situation as frontline caregivers for their own residents. It was imperative to track residents with physical symptoms, conduct testing when possible, and follow the course of residents with confirmed or suspected COVID-19. As serious illness and death have been reported among otherwise healthy young people, we ensured that our homebound residents were frequently monitored.15 At several of our centers, residents with COVID-19 from any program who chose to separate from their families were provided with alternative housing accommodations. In addition, some of our graduate medical education offices identified specific physicians to care for residents with COVID-19 who did not require hospitalization.
Continue to: Deployment to other specialties...
Deployment to other specialties
Several hospitals in the United States redeployed residents because of staffing shortages in high-impact settings.12 It was important for ObGyns to emphasize that the labor and delivery unit functions as the emergency ward for pregnant women, and that ObGyn residents possess skills specific to the care of these patients.
For our departments, we highlighted that external redeployment could adversely affect our workforce restructuring and, ultimately, patient care. We focused efforts on internal deployment or reassignment as much as possible. Some faculty and fellows in nonobstetric subspecialty areas were redirected to provide care on our inpatient obstetric services.
Educating residents
To maintain educational efforts with social distancing, we used videoconferencing to preserve the protected didactic education time that existed for our residents before the pandemic. This regularly scheduled, nonclinical time also was utilized to instruct residents on the rapidly changing clinical guidelines and to disseminate information about new institutional policies and procedures, ensuring that residents were adequately prepared for their new clinical work.
Work hour requirements
The ACGME requires that work hour limitations remain unchanged during Stage 3 Pandemic Emergency Status. As the pandemic presented new challenges and stressors for residents inside and outside the workplace, ensuring adequate time off to rest and recover was critical for maintaining the resident workforce’s health and wellness.
Thus, our workforce restructuring plans accounted for work hour limitations. As detailed above, the restructuring was accomplished by cohorting residents into small teams that remained unchanged for several weeks. Most shifts were limited to 12 hours, residents continued to be assigned at least 1 day off each week, and daily schedules were structured to ensure at least 10 hours off between shifts. Time spent working remotely was included in work hour calculations.
In addition, residents on “jeopardy” who were available for those who needed to be removed from direct patient care were given at least 1 day off per week in which they could not be pulled for clinical duty. Finally, prolonged inpatient assignments were limited; after these assignments, residents were given increased time for rest and recuperation.
Ensuring adequate supervision
The expectation during Stage 3 Pandemic Emergency Status is that residents, with adequate supervision, provide care that is appropriate for their level of training. To adequately and safely supervise residents, faculty needed training to remain well informed about the clinical care of COVID-19 patients. This was accomplished through frequent communication and consultation with colleagues in infectious disease, occupational health, and guidance from national organizations, such as the American College of Obstetricians and Gynecologists and the Centers for Disease Control and Prevention, and information from our state health departments.
Faculty members were trained in safe donning and doffing of PPE and infection control strategies to ensure they could safely oversee and train residents in these practices. Faculty schedules were significantly altered to ensure an adequate workforce and adequate resident supervision. Faculty efforts were focused on areas of critical need—in our case inpatient obstetrics—with a smaller workforce assigned to outpatient services and inpatient gynecology and gynecologic oncology. Many ObGyn subspecialist faculty were redeployed to general ObGyn inpatient units, thus permitting appropriate resident supervision at all times. In the outpatient setting, faculty adjusted to the changing demands and learned to conduct and supervise telehealth visits.
Finally, for those whose residents were deployed to other services (for example, internal medicine, emergency medicine, or critical care), supervision became paramount. We checked in with our deployed residents daily to be sure that their supervision on those services was adequate. Considering the extreme complexity, rapidly changing understanding of the disease, and often tragic patient outcomes, it was essential to ensure appropriate support and supervision on “off service” deployment.
Continue to: Fellows functioning in core specialty...
Fellows functioning in core specialty
Anticipating the increased need for clinicians on the obstetric services, fellows in subspecialty areas were granted emergency privileges to act as attending faculty in the core specialty, supervising residents and providing patient care. On the other hand, some of those fellows, primarily in gynecologic oncology, were externally redeployed out of core specialty to internal medicine and critical care units. Careful consideration of the fellows’ needs for supervision and support in these roles was essential, and similar support measures that were put in place for our residents were offered to fellows.
In conclusion
The COVID-19 pandemic has presented diverse and complex challenges to the entire health care workforce. Because this crisis is widespread and likely will be lengthy, a sustained and organized response is required.16 We have highlighted unique challenges specific to residency programs and presented collective best practices from our experiences in ObGyn navigating these obstacles, which are applicable to many other programs.
The flexibility and relief afforded by the ACGME Stage 3 Pandemic Emergency Status designation allowed us to meet the needs of the surge of patients that required care while we maintained our educational framework and tenets of providing adequate resources and training, working within the confines of safe work hours, ensuring proper supervision, and granting attending privileges to fellows in their core specialty. ●
- Panahi L, Amiri M, Pouy S. Risks of novel coronavirus disease (COVID-19) in pregnancy; a narrative review. Arch Acad Emerg Med. 2020;8e34.
- Rasmussen SA, Smulian JC, Lednicky JA, et al. Coronavirus disease 2019 (COVID-19) and pregnancy: what obstetricians need to know. Am J Obstet Gynecol. 2020;222:415-426.
- Sutton D, Fuchs K, D'Alton M, et al. Universal screening for SARS-CoV-2 in women admitted for delivery. N Engl J Med. 2020;382:2163-2164.
- Accreditation Council for Graduate Medical Education. Three stages of GME during the COVID-19 pandemic. https://www.acgme.org/COVID-19/Three-Stages-of-GME-During-the-COVID-19-Pandemic. Accessed May 28, 2020.
- Accreditation Council for Graduate Medical Education. Emergency category maps/5-18-20: percentage of residents in each state/territory under pandemic emergency status. Percentage of residency and fellowship programs under ACGME COVID-19 pandemic emergency status (stage 3). https://dl.acgme.org/learn/course/sponsoring-institution-idea-exchange/emergency-category-maps/5-18-20-percentage-of-residents-in-each-state-territory-under-pandemic-emergency-status. Accessed May 28, 2020.
- Gates B. The next epidemic--lessons from Ebola. N Engl J Med. 2015;372:1381-1384.
- Pepe D, Martinello RA, Juthani-Mehta M. Involving physicians-in-training in the care of patients during epidemics. J Grad Med Educ. 2019;11:632-634.
- Crosby DL, Sharma A. Insights on otolaryngology residency training during the COVID-19 pandemic. Otolaryngol Head Neck Surg. 2020;163:38-41.
- Kim CS, Lynch JB, Seth C, et al. One academic health system's early (and ongoing) experience responding to COVID-19: recommendations from the initial epicenter of the pandemic in the United States. Acad Med. 2020;95:1146-1148.
- Kogan M, Klein SE, Hannon CP, et al. Orthopaedic education during the COVID-19 pandemic. J Am Acad Orthop Surg. 2020; 28:e456-e464.
- Vargo E, Ali M, Henry F, et al. Cleveland Clinic Akron general urology residency program's COVID-19 experience. Urology. 2020;140:1-3.
- Zarzaur BL, Stahl CC, Greenberg JA, et al. Blueprint for restructuring a department of surgery in concert with the health care system during a pandemic: the University of Wisconsin experience. JAMA Surg. 2020. doi: 10.1001/jamasurg.2020.1386.
- New York State COVID-19 Maternity Task Force. Recommendations to the governor to promote increased choice and access to safe maternity care during the COVID-19 pandemic. https://www.governor.ny.gov/sites/governor.ny.gov/files/atoms/files/042920_CMTF_Recommendations.pdf. Accessed May 28, 2020.
- Campbell KH, Tornatore JM, Lawrence KE, et al. Prevalence of SARS-CoV-2 among patients admitted for childbirth in southern Connecticut. JAMA. 2020;323:2520-2522.
- CDC COVID-19 Response Team. Severe outcomes among patients with coronavirus disease 2019 (COVID-19)--United States, February 12-March 16, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:343-346.
- Kissler SM, Tedijanto C, Goldstein E, et al. Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period. Science. 2020;368:860-868.
- Panahi L, Amiri M, Pouy S. Risks of novel coronavirus disease (COVID-19) in pregnancy; a narrative review. Arch Acad Emerg Med. 2020;8e34.
- Rasmussen SA, Smulian JC, Lednicky JA, et al. Coronavirus disease 2019 (COVID-19) and pregnancy: what obstetricians need to know. Am J Obstet Gynecol. 2020;222:415-426.
- Sutton D, Fuchs K, D'Alton M, et al. Universal screening for SARS-CoV-2 in women admitted for delivery. N Engl J Med. 2020;382:2163-2164.
- Accreditation Council for Graduate Medical Education. Three stages of GME during the COVID-19 pandemic. https://www.acgme.org/COVID-19/Three-Stages-of-GME-During-the-COVID-19-Pandemic. Accessed May 28, 2020.
- Accreditation Council for Graduate Medical Education. Emergency category maps/5-18-20: percentage of residents in each state/territory under pandemic emergency status. Percentage of residency and fellowship programs under ACGME COVID-19 pandemic emergency status (stage 3). https://dl.acgme.org/learn/course/sponsoring-institution-idea-exchange/emergency-category-maps/5-18-20-percentage-of-residents-in-each-state-territory-under-pandemic-emergency-status. Accessed May 28, 2020.
- Gates B. The next epidemic--lessons from Ebola. N Engl J Med. 2015;372:1381-1384.
- Pepe D, Martinello RA, Juthani-Mehta M. Involving physicians-in-training in the care of patients during epidemics. J Grad Med Educ. 2019;11:632-634.
- Crosby DL, Sharma A. Insights on otolaryngology residency training during the COVID-19 pandemic. Otolaryngol Head Neck Surg. 2020;163:38-41.
- Kim CS, Lynch JB, Seth C, et al. One academic health system's early (and ongoing) experience responding to COVID-19: recommendations from the initial epicenter of the pandemic in the United States. Acad Med. 2020;95:1146-1148.
- Kogan M, Klein SE, Hannon CP, et al. Orthopaedic education during the COVID-19 pandemic. J Am Acad Orthop Surg. 2020; 28:e456-e464.
- Vargo E, Ali M, Henry F, et al. Cleveland Clinic Akron general urology residency program's COVID-19 experience. Urology. 2020;140:1-3.
- Zarzaur BL, Stahl CC, Greenberg JA, et al. Blueprint for restructuring a department of surgery in concert with the health care system during a pandemic: the University of Wisconsin experience. JAMA Surg. 2020. doi: 10.1001/jamasurg.2020.1386.
- New York State COVID-19 Maternity Task Force. Recommendations to the governor to promote increased choice and access to safe maternity care during the COVID-19 pandemic. https://www.governor.ny.gov/sites/governor.ny.gov/files/atoms/files/042920_CMTF_Recommendations.pdf. Accessed May 28, 2020.
- Campbell KH, Tornatore JM, Lawrence KE, et al. Prevalence of SARS-CoV-2 among patients admitted for childbirth in southern Connecticut. JAMA. 2020;323:2520-2522.
- CDC COVID-19 Response Team. Severe outcomes among patients with coronavirus disease 2019 (COVID-19)--United States, February 12-March 16, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:343-346.
- Kissler SM, Tedijanto C, Goldstein E, et al. Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period. Science. 2020;368:860-868.
Free videoconferencing apps for the ObGyn

The COVID-19 pandemic has created a metamorphosis in human interactions. One way we have adapted is our increased use of virtual platforms for tasks such as lectures, meetings, interviews, conferences, and patient care via telemedicine.1 Virtual platforms have allowed for the continuation of existing programs and facilitated new collaborations ranging from international webinars on patient care to national lectures for residents and fellows in ObGyn. New virtual platforms continue to emerge. We present here a review of free virtual communication apps available to the ObGyn care provider.
We used the term “videoconference” to search the Apple and Google Play app stores between May 29, 2020, and June 1, 2020. A total of 25 apps that offered both audio and videoconferencing were identified. All were free for download, but the majority required an ongoing paid subscription fee for the service. Thirteen programs were either completely free or offered a free version of their services. Based on our review and a systematic analysis, we selected 5 apps to feature here: Cisco Webex Meetings, Free Conference Call, Jitsi Meet, Microsoft Teams, and Zoom.
Featured videoconferencing apps
Cisco Webex Meetings and Free Conference Call offer an easy video meeting setup from both a smartphone and a desktop app. They provide seamless access to functions on the virtual main page, including chat with other participants in the meeting and screen sharing. These apps both require screen recording in order to share screens.
Jitsi Meet is a web app usable on an iPhone or Android as well as on a desktop through the meet.jit.si website. No account is required. On the app or website, the user creates a meeting name and shares the unique URL or meeting name with invitees to join the videoconference. The mobile app and website both offer a “raise your hand” feature, full screen and/or gallery (tile) view, group chat, and live streaming. In both settings, users may lock the meeting and require a password. Additional features through the website include screen sharing, recording the meeting, blurred background, muting all participants, and sharing YouTube videos.
The Microsoft Teams app asks you the purpose of signing up on the website—“use for school,” “with friends and family,” or “for work.” If you choose “with friends and family,” the app directs you to Skype. Choosing the “for work” function directs you to complete your free registration. Microsoft Teams requires participants to create teams; thus, others participating in the videoconference need to have their own account. However, “guest access” also is available.
On the Zoom platform, immediate and scheduled meetings can be set up on the app as well as on the website, or directly on Microsoft Outlook and Google Calendar if the plug-in has been established. The desktop and smartphone apps are similar in function and provide access to personalized settings.
For patient care, since HIPAA (Health Insurance Portability and Accountability Act) protection is a concern, we recommend following guidelines at the user’s institution regarding use of apps such as Epic Haiku for telehealth visits. For teaching and interacting with colleagues, we recommend Cisco Webex, Free Conference Call, Microsoft Teams, and Zoom, keeping in mind the time limitations of each app for the free account.
Overall, these 5 apps are easy to set up and user-friendly. Deciding which program to choose will depend on the number of participants allowed for a meeting and the duration of the meeting, as these two factors seem to be the most constraining among the free videoconferencing apps. ●
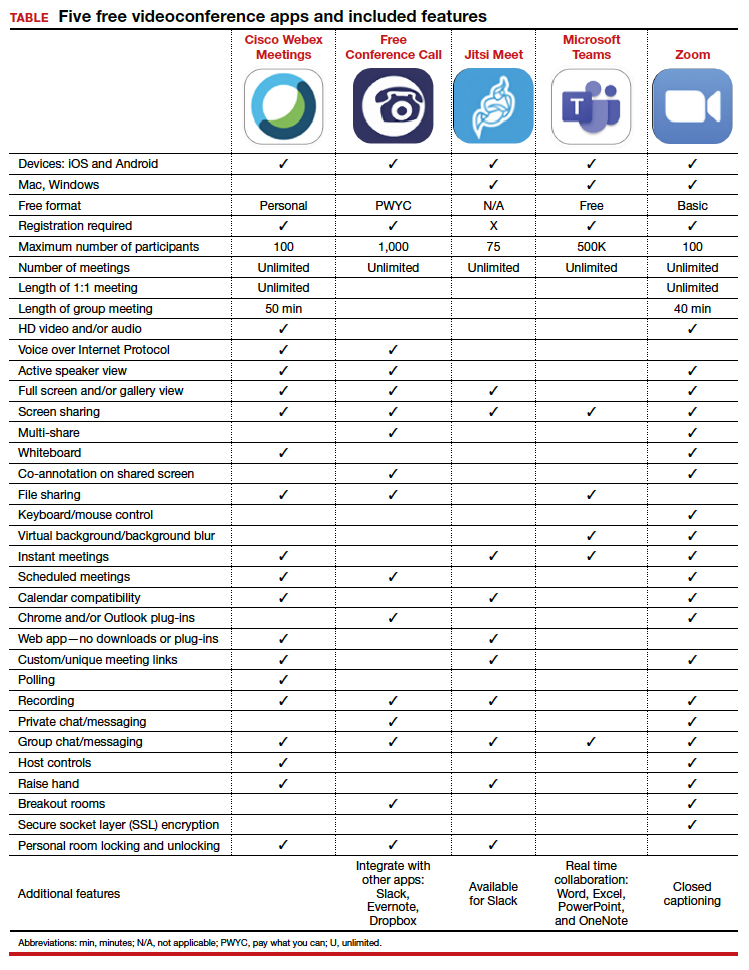
- Karram M, Baum N. Telemedicine: a primer for today’s ObGyn. OBG Manag. 2020;32(5):28-32.

The COVID-19 pandemic has created a metamorphosis in human interactions. One way we have adapted is our increased use of virtual platforms for tasks such as lectures, meetings, interviews, conferences, and patient care via telemedicine.1 Virtual platforms have allowed for the continuation of existing programs and facilitated new collaborations ranging from international webinars on patient care to national lectures for residents and fellows in ObGyn. New virtual platforms continue to emerge. We present here a review of free virtual communication apps available to the ObGyn care provider.
We used the term “videoconference” to search the Apple and Google Play app stores between May 29, 2020, and June 1, 2020. A total of 25 apps that offered both audio and videoconferencing were identified. All were free for download, but the majority required an ongoing paid subscription fee for the service. Thirteen programs were either completely free or offered a free version of their services. Based on our review and a systematic analysis, we selected 5 apps to feature here: Cisco Webex Meetings, Free Conference Call, Jitsi Meet, Microsoft Teams, and Zoom.
Featured videoconferencing apps
Cisco Webex Meetings and Free Conference Call offer an easy video meeting setup from both a smartphone and a desktop app. They provide seamless access to functions on the virtual main page, including chat with other participants in the meeting and screen sharing. These apps both require screen recording in order to share screens.
Jitsi Meet is a web app usable on an iPhone or Android as well as on a desktop through the meet.jit.si website. No account is required. On the app or website, the user creates a meeting name and shares the unique URL or meeting name with invitees to join the videoconference. The mobile app and website both offer a “raise your hand” feature, full screen and/or gallery (tile) view, group chat, and live streaming. In both settings, users may lock the meeting and require a password. Additional features through the website include screen sharing, recording the meeting, blurred background, muting all participants, and sharing YouTube videos.
The Microsoft Teams app asks you the purpose of signing up on the website—“use for school,” “with friends and family,” or “for work.” If you choose “with friends and family,” the app directs you to Skype. Choosing the “for work” function directs you to complete your free registration. Microsoft Teams requires participants to create teams; thus, others participating in the videoconference need to have their own account. However, “guest access” also is available.
On the Zoom platform, immediate and scheduled meetings can be set up on the app as well as on the website, or directly on Microsoft Outlook and Google Calendar if the plug-in has been established. The desktop and smartphone apps are similar in function and provide access to personalized settings.
For patient care, since HIPAA (Health Insurance Portability and Accountability Act) protection is a concern, we recommend following guidelines at the user’s institution regarding use of apps such as Epic Haiku for telehealth visits. For teaching and interacting with colleagues, we recommend Cisco Webex, Free Conference Call, Microsoft Teams, and Zoom, keeping in mind the time limitations of each app for the free account.
Overall, these 5 apps are easy to set up and user-friendly. Deciding which program to choose will depend on the number of participants allowed for a meeting and the duration of the meeting, as these two factors seem to be the most constraining among the free videoconferencing apps. ●
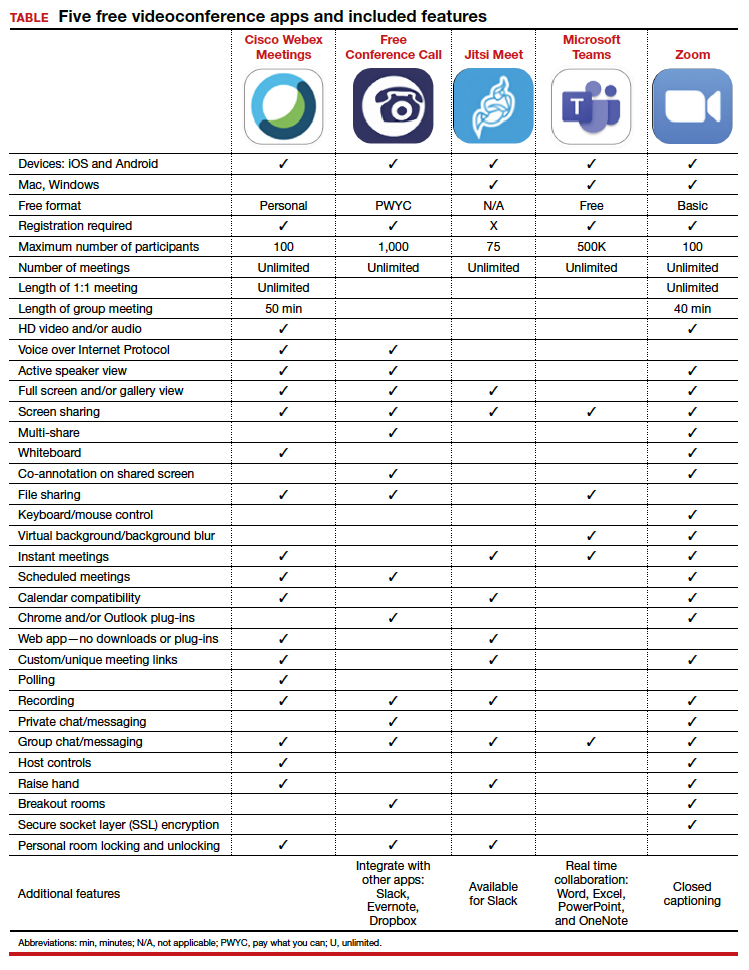

The COVID-19 pandemic has created a metamorphosis in human interactions. One way we have adapted is our increased use of virtual platforms for tasks such as lectures, meetings, interviews, conferences, and patient care via telemedicine.1 Virtual platforms have allowed for the continuation of existing programs and facilitated new collaborations ranging from international webinars on patient care to national lectures for residents and fellows in ObGyn. New virtual platforms continue to emerge. We present here a review of free virtual communication apps available to the ObGyn care provider.
We used the term “videoconference” to search the Apple and Google Play app stores between May 29, 2020, and June 1, 2020. A total of 25 apps that offered both audio and videoconferencing were identified. All were free for download, but the majority required an ongoing paid subscription fee for the service. Thirteen programs were either completely free or offered a free version of their services. Based on our review and a systematic analysis, we selected 5 apps to feature here: Cisco Webex Meetings, Free Conference Call, Jitsi Meet, Microsoft Teams, and Zoom.
Featured videoconferencing apps
Cisco Webex Meetings and Free Conference Call offer an easy video meeting setup from both a smartphone and a desktop app. They provide seamless access to functions on the virtual main page, including chat with other participants in the meeting and screen sharing. These apps both require screen recording in order to share screens.
Jitsi Meet is a web app usable on an iPhone or Android as well as on a desktop through the meet.jit.si website. No account is required. On the app or website, the user creates a meeting name and shares the unique URL or meeting name with invitees to join the videoconference. The mobile app and website both offer a “raise your hand” feature, full screen and/or gallery (tile) view, group chat, and live streaming. In both settings, users may lock the meeting and require a password. Additional features through the website include screen sharing, recording the meeting, blurred background, muting all participants, and sharing YouTube videos.
The Microsoft Teams app asks you the purpose of signing up on the website—“use for school,” “with friends and family,” or “for work.” If you choose “with friends and family,” the app directs you to Skype. Choosing the “for work” function directs you to complete your free registration. Microsoft Teams requires participants to create teams; thus, others participating in the videoconference need to have their own account. However, “guest access” also is available.
On the Zoom platform, immediate and scheduled meetings can be set up on the app as well as on the website, or directly on Microsoft Outlook and Google Calendar if the plug-in has been established. The desktop and smartphone apps are similar in function and provide access to personalized settings.
For patient care, since HIPAA (Health Insurance Portability and Accountability Act) protection is a concern, we recommend following guidelines at the user’s institution regarding use of apps such as Epic Haiku for telehealth visits. For teaching and interacting with colleagues, we recommend Cisco Webex, Free Conference Call, Microsoft Teams, and Zoom, keeping in mind the time limitations of each app for the free account.
Overall, these 5 apps are easy to set up and user-friendly. Deciding which program to choose will depend on the number of participants allowed for a meeting and the duration of the meeting, as these two factors seem to be the most constraining among the free videoconferencing apps. ●
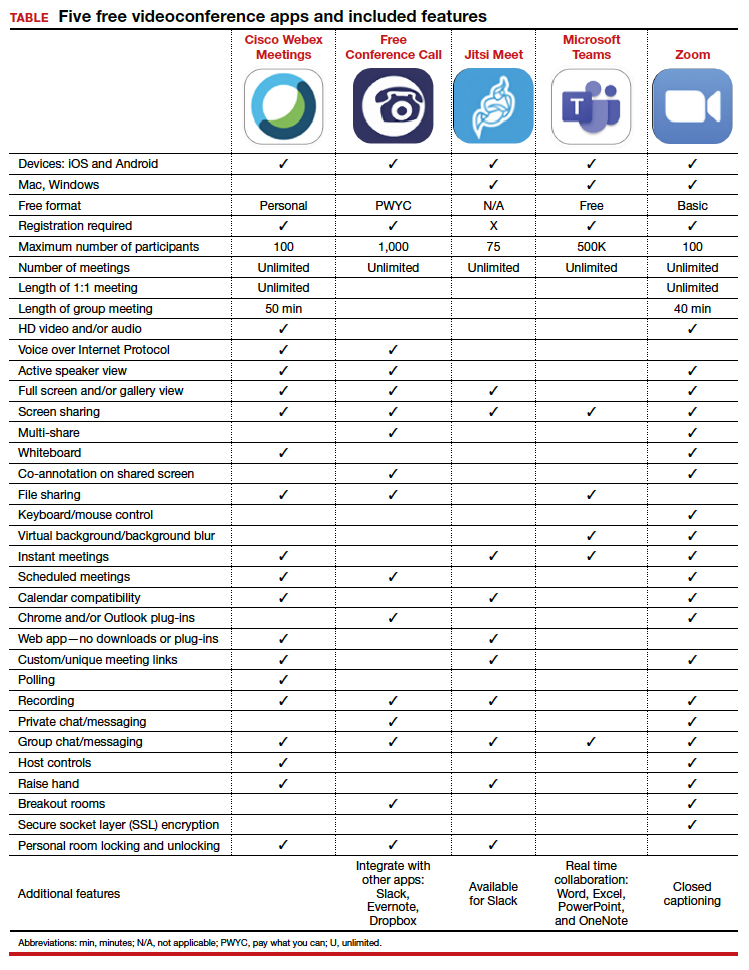
- Karram M, Baum N. Telemedicine: a primer for today’s ObGyn. OBG Manag. 2020;32(5):28-32.
- Karram M, Baum N. Telemedicine: a primer for today’s ObGyn. OBG Manag. 2020;32(5):28-32.
COVID-19 apps for the ObGyn health care provider

In the midst of the coronavirus disease 2019 (COVID-19) pandemic, health care providers, including ObGyns, need up-to-date information to keep pace with the ever-changing health care crisis. Literature regarding obstetric populations is emerging in journals.1,2 General guidance in the management of COVID-19–positive patients may also be helpful to the ObGyn provider. Although scientific journals are now publishing COVID-19 research at warp speed, those same journals tend to be too specialized for general readers.3 Mobile apps may make the information more accessible.
This app review focuses on 3 apps that provide information about the ongoing COVID-19 pandemic and detail general guidance for treatment of COVID-19–positive patients. An initial search in early April 2020 of major national health care organizations and ObGyn-specific organizational apps yielded the Centers for Disease Control and Prevention (CDC) app. A subsequent search in the app stores using the term “COVID” yielded 2 additional apps: the Osler COVID Learning Centre app and the Relief Central app.
The CDC app contains a COVID-19-specific section that highlights pertinent information for health care providers as well as a section on caring for the obstetric patient. The Osler app includes podcasts and videos on critical care for noncritical care providers. Finally, the Relief Central app contains updated information on screening and treatment for COVID-19. The TABLE features details of the 3 apps.
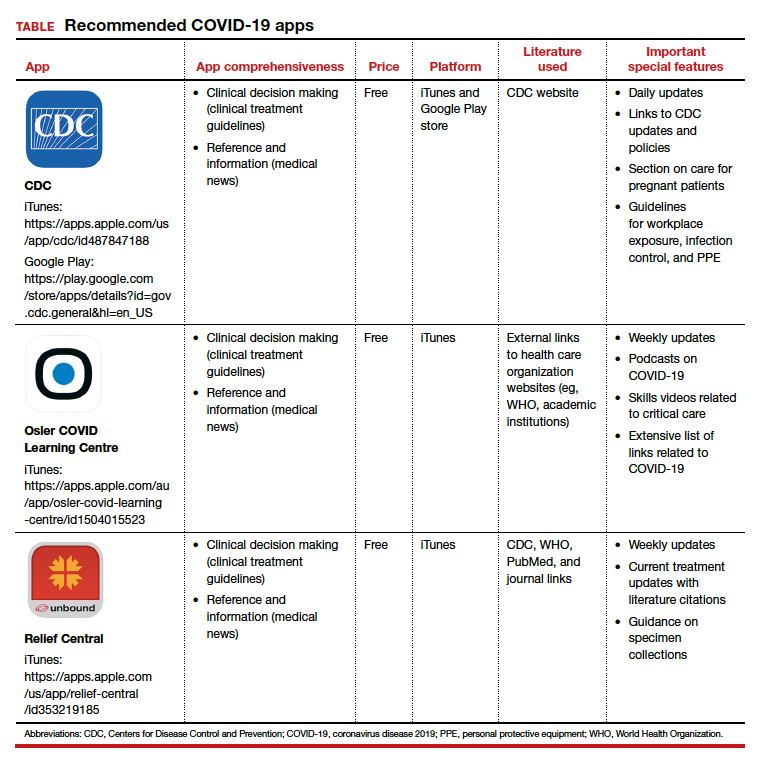
Each app is evaluated based on a shortened version of the APPLICATIONS scoring system, APPLI (app comprehensiveness, price, platform, literature use, and important special features).4 ●
- Rasmussen SA, Smulian JC, Lednicky JA, et al. Coronavirus disease 2019 (COVID-19) and pregnancy: what obstetricians need to know. Am J Obstet Gynecol. February 24, 2020. doi:10.1016/j.ajog.2020.02.017.
- Dashraath P, Jing Lin Jeslyn W, Mei Xian Karen L, et al. Coronavirus disease 2019 (COVID-19) pandemic and pregnancy. Am J Obstet Gynecol. March 23, 2020. doi:10.1016/j.ajog.2020.03.021.
- Tingley K. Coronavirus is forcing medical research to speed up. New York Times Magazine. April 26, 2020:16-18.
- Chyjek K, Farag S, Chen KT. Rating pregnancy wheel applications using the APPLICATIONS scoring system. Obstet Gynecol. 2015;125:1478-1483.

In the midst of the coronavirus disease 2019 (COVID-19) pandemic, health care providers, including ObGyns, need up-to-date information to keep pace with the ever-changing health care crisis. Literature regarding obstetric populations is emerging in journals.1,2 General guidance in the management of COVID-19–positive patients may also be helpful to the ObGyn provider. Although scientific journals are now publishing COVID-19 research at warp speed, those same journals tend to be too specialized for general readers.3 Mobile apps may make the information more accessible.
This app review focuses on 3 apps that provide information about the ongoing COVID-19 pandemic and detail general guidance for treatment of COVID-19–positive patients. An initial search in early April 2020 of major national health care organizations and ObGyn-specific organizational apps yielded the Centers for Disease Control and Prevention (CDC) app. A subsequent search in the app stores using the term “COVID” yielded 2 additional apps: the Osler COVID Learning Centre app and the Relief Central app.
The CDC app contains a COVID-19-specific section that highlights pertinent information for health care providers as well as a section on caring for the obstetric patient. The Osler app includes podcasts and videos on critical care for noncritical care providers. Finally, the Relief Central app contains updated information on screening and treatment for COVID-19. The TABLE features details of the 3 apps.
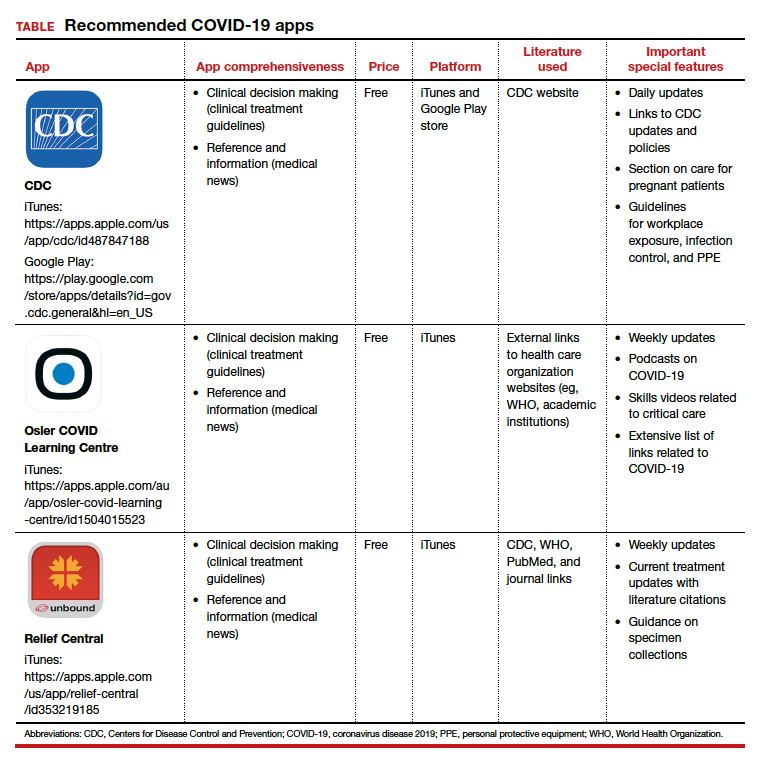
Each app is evaluated based on a shortened version of the APPLICATIONS scoring system, APPLI (app comprehensiveness, price, platform, literature use, and important special features).4 ●

In the midst of the coronavirus disease 2019 (COVID-19) pandemic, health care providers, including ObGyns, need up-to-date information to keep pace with the ever-changing health care crisis. Literature regarding obstetric populations is emerging in journals.1,2 General guidance in the management of COVID-19–positive patients may also be helpful to the ObGyn provider. Although scientific journals are now publishing COVID-19 research at warp speed, those same journals tend to be too specialized for general readers.3 Mobile apps may make the information more accessible.
This app review focuses on 3 apps that provide information about the ongoing COVID-19 pandemic and detail general guidance for treatment of COVID-19–positive patients. An initial search in early April 2020 of major national health care organizations and ObGyn-specific organizational apps yielded the Centers for Disease Control and Prevention (CDC) app. A subsequent search in the app stores using the term “COVID” yielded 2 additional apps: the Osler COVID Learning Centre app and the Relief Central app.
The CDC app contains a COVID-19-specific section that highlights pertinent information for health care providers as well as a section on caring for the obstetric patient. The Osler app includes podcasts and videos on critical care for noncritical care providers. Finally, the Relief Central app contains updated information on screening and treatment for COVID-19. The TABLE features details of the 3 apps.
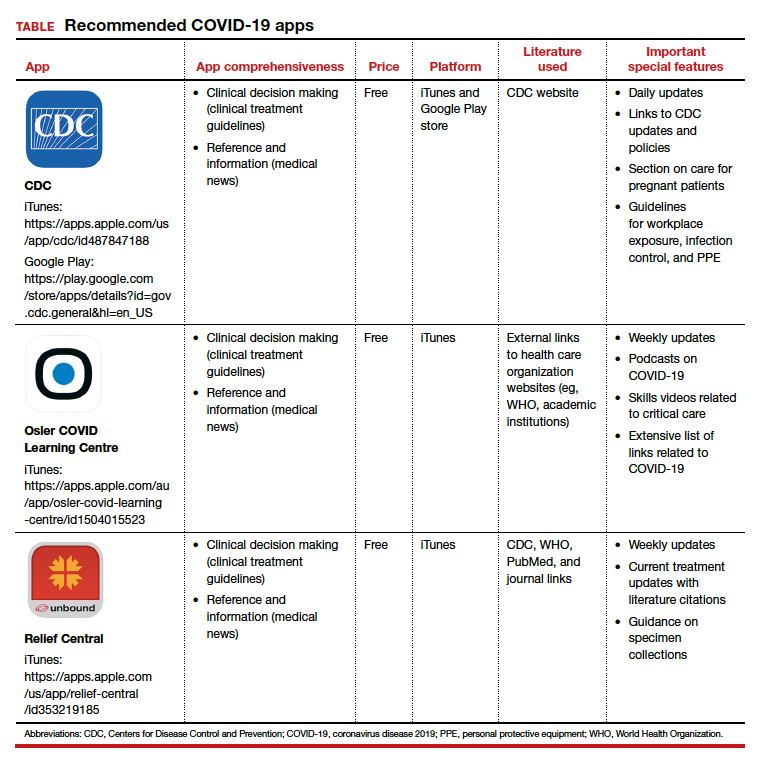
Each app is evaluated based on a shortened version of the APPLICATIONS scoring system, APPLI (app comprehensiveness, price, platform, literature use, and important special features).4 ●
- Rasmussen SA, Smulian JC, Lednicky JA, et al. Coronavirus disease 2019 (COVID-19) and pregnancy: what obstetricians need to know. Am J Obstet Gynecol. February 24, 2020. doi:10.1016/j.ajog.2020.02.017.
- Dashraath P, Jing Lin Jeslyn W, Mei Xian Karen L, et al. Coronavirus disease 2019 (COVID-19) pandemic and pregnancy. Am J Obstet Gynecol. March 23, 2020. doi:10.1016/j.ajog.2020.03.021.
- Tingley K. Coronavirus is forcing medical research to speed up. New York Times Magazine. April 26, 2020:16-18.
- Chyjek K, Farag S, Chen KT. Rating pregnancy wheel applications using the APPLICATIONS scoring system. Obstet Gynecol. 2015;125:1478-1483.
- Rasmussen SA, Smulian JC, Lednicky JA, et al. Coronavirus disease 2019 (COVID-19) and pregnancy: what obstetricians need to know. Am J Obstet Gynecol. February 24, 2020. doi:10.1016/j.ajog.2020.02.017.
- Dashraath P, Jing Lin Jeslyn W, Mei Xian Karen L, et al. Coronavirus disease 2019 (COVID-19) pandemic and pregnancy. Am J Obstet Gynecol. March 23, 2020. doi:10.1016/j.ajog.2020.03.021.
- Tingley K. Coronavirus is forcing medical research to speed up. New York Times Magazine. April 26, 2020:16-18.
- Chyjek K, Farag S, Chen KT. Rating pregnancy wheel applications using the APPLICATIONS scoring system. Obstet Gynecol. 2015;125:1478-1483.