User login
10 ways in which ObGyn care can be more environmentally sustainable
Climate change has been called the biggest health threat of the 21st century.1 The health care sector is a huge contributor to global carbon emissions, accounting for almost double the emissions of global aviation. While other industries and countries are implementing mitigation measures to decrease their emissions, health care is currently on track to double its carbon emissions by 2050, even though it should be carbon neutral by that time to comply with the Paris Climate Agreement.2 There have been some national efforts to curb health care emissions, including the creation of the Office of Climate Change and Health Equity in 2021 and the passage of the Inflation Reduction Act in 2022.3 These are top-down, administrative approaches, and to be successful we will also need clinicians to understand and address this problem.
The negative impacts of heat, air pollution, and exposure to toxic substances on human health have been well documented in multiple regions across multiple specialties.4-7 The United States makes up 27% of the global health care carbon footprint—more emissions than the entire United Kingdom as a country—despite having only 4% of the world’s population.2 Culture and incentives for an overabundance of single-use supplies, not evidence for patient safety, have led to this uniquely American problem. It is evident that our health care industry is an excellent place to implement mitigation measures for carbon emissions that contribute to climate change and can improve health outcomes.
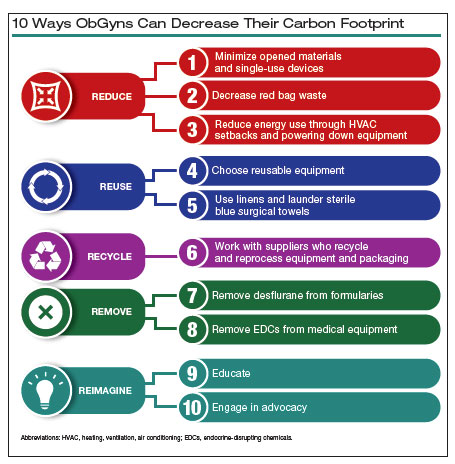
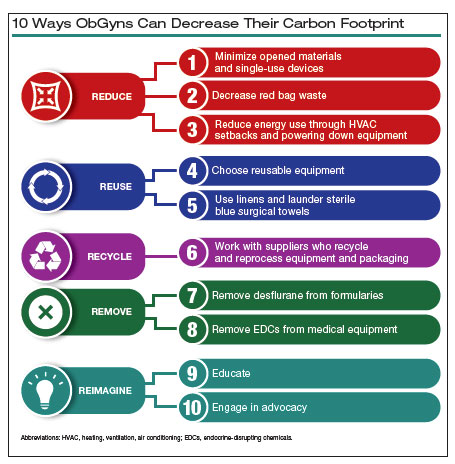
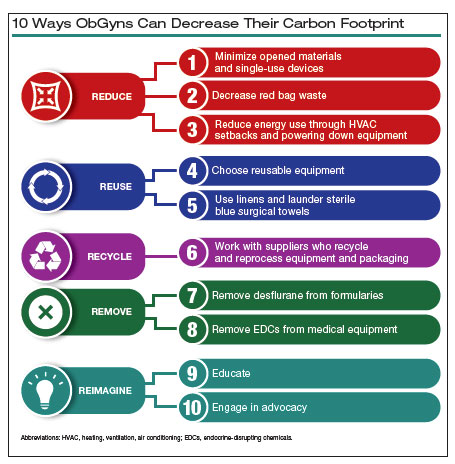
In this article, we recommend 10 practices that can decrease our carbon footprint in ObGyn. We focus on the classic motto of “Reduce, Reuse, Recycle,” while adding “Remove” and “Reimagine” to classify the ways in which we can reduce emissions while not compromising our care to patients.
Reduce
1. Minimize opened materials and single-use devices in the OR and labor and delivery
Health care is a unique setting where a culture of infection prevention and efficiency has led low-cost, single-use supplies to dominate over reusable items. While single-use items can have inexpensive purchasing costs compared to reusable items, the environmental costs required for the production and disposal of the former are often much greater. In operating rooms (ORs) and labor and delivery (LD) units, single-use items are omnipresent. Over the past decade, researchers and clinicians have started to take a closer look at these items and their carbon footprint. One group evaluated hysterectomy through a waste audit and found that the vast majority of waste from all of the cases was Spunbond Meltblown Spunbond, or SMS; plastic materialthat comprises gowns; blue wraps; and drapes; followed by hard plastic material that comprises trays and packaging.8 Moreover, production and manufacturing processes contributed to 95% of the environmental impacts of these items.8
In an effort to be time efficient, OR staff will open sterile surgical packs and individual peel-pack items prior to surgery to minimize having to find items during surgery. However, this creates an inordinate amount of waste. One group of neurosurgeons who evaluated their opened but unused supplies found that 85% of their unused items were individually opened items, leading to a waste of $2.9 million per year.9 Minor procedures like dilation and curettage, cystoscopy, and hysteroscopy do not need such a large sterile field, as these procedures are also safe to perform in the office. Hand surgeons have been quick to lead in this space, particularly with minor procedures such as carpal tunnel release. One division was able to eliminate 2.8 tons of waste and save $13,000 in a 2-year period by reducing the sterile field.10 ObGyns can work with OR and LD staff to create custom packs that minimize unused or underutilized items, helping to reduce both the carbon footprint and health care spending.
Bottom line: ObGyns can help foster a culture of having supplies available but not opened until needed during a case.
Continue to: 2. Decrease regulated medical waste...
2. Decrease regulated medical waste
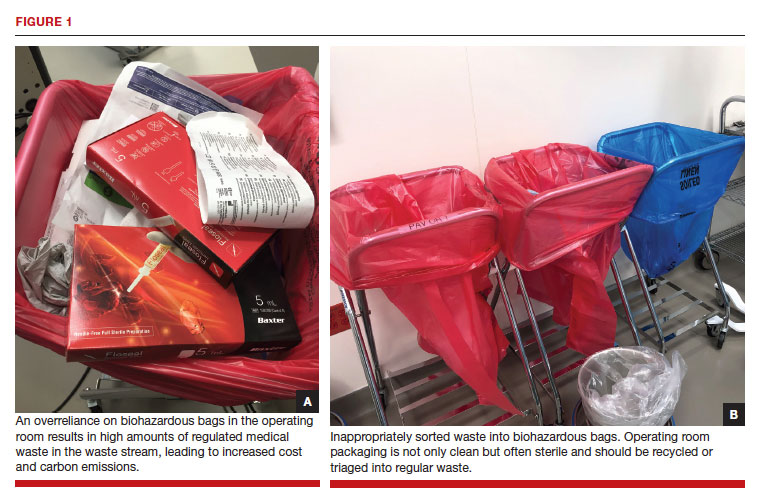
Health care is unique from other fields in that there are multiple waste streams to consider. Infectious waste and items saturated in blood or capable of causing infection must be placed into regulated medical waste (RMW), or more commonly, red biohazard bags. RMW is autoclaved or incinerated prior to disposal in a landfill. This process is more financially and environmentally costly than general municipal waste (GMW). This process also requires more transport—1 study revealed that GMW traveled 20 km to a landfill for disposal, compared with the 50 km that RMW traveled for sterilized-prior-to-landfill disposal.11
Unfortunately, the vast majority of items placed in RMW are incorrectly triaged and should instead be disposed in GMW.12,13 One study performed in an emergency department revealed that 85% of waste was incorrectly placed in the RMW.12
Bottom line: ObGyns can avoid placing items in RMW that may not qualify and advocate for institution policy changes to remove RMW from places such as waiting rooms, at the patient bedside, or next to scrub sinks.
3. Reduce energy use
ORs and LD units use a lot of energy, and numerous studies have demonstrated that the heating, ventilation, and air conditioning (HVAC) system plays a large role in emissions.8,11 This can easily be fixed by “HVAC setbacks” and powering down rooms when not in use. One institution powered down ORs when not in use and reduced 234 metric tons of CO2 emissions and saved $33,000 per year.14 Transitioning to light-emitting diode (LED) lights reduced energy usage at 1 institution by almost 50%.15 Finally, computers in clinical offices, examination rooms, and administrative offices can be powered down at the end of the day. One study found that in 1 radiology department, 29 computers left on overnight and on weekends emitted 17.7 tons of CO2 emissions in 1 year.16
Bottom line: We as ObGyns can advocate for how energy can be saved outside of surgical cases, including powering down ORs and LD units, transitioning to LED lighting, and powering down workstations.
Reuse
4. Choose reusable equipment
In ObGyn practice, the most commonly used tool is the speculum. Given its omnipresence, the speculum is a great place to start to decrease our carbon footprint. Two studies have evaluated the environmental impact of reusable versus single-use disposable specula, and both demonstrated that the stainless-steel versions have less global warming potential than the acrylic varieties.17,18 Donahue and colleagues17 demonstrated that it only took 2 to 3 pelvic examinations for the cost of stainless-steel specula to break even, even when sterilized in a half-filled autoclave tray. Rodriquez, et al18 revealed that, compared with an acrylic model, the stainless-steel specula had fewer negative impacts in terms of global warming, acidification, respiratory effects, smog, and fossil fuel depletion.18
Bottom line: Strongly consider using stainless-steel specula to reduce costs and carbon emissions.
In addition to specula, ObGyns can choose reusable equipment in the OR. For example, surgeons can use stainless-steel trocars instead of disposable trocars.19 In vaginal cases, Breisky-Navratil retractors can be used instead of disposable self-retaining retractors. Plastic basins that often are included in sterile supply packs can be replaced with stainless-steel basins, which could have profound positive effects on the carbon footprint of gynecologic surgery.8 One study of ObGyns demonstrated that 95% of physicians supported waste-reduction efforts, and 66% supported utilizing reusable surgical tools instead of disposable tools.20
Bottom line: As surgeons, ObGyns have influence over what they want to use in the OR, and they can petition for reusable options over disposable options.
5. Launder the sterile blue towels
Sterile blue towels, which are made of cotton, have the largest environmental footprint compared with other disposable materials, such as plastics, and contribute greatly to toxicity in human health.8,11 Although these towels cannot be laundered and sterilized again for use in a sterile surgical field, they can be laundered and repurposed, including by environmental services to clean hospital rooms. Blue towels should be able to be laundered no matter how saturated in body fluids they are.
Bottom line: ObGyns should strive to always launder the blue towels and educate trainees and other staff in the OR to do the same.
Recycle
6. Recycle and reprocess materials and devices
While recycling is immensely important, it requires a large amount of energy to break down a material to its raw components for manufacturing. It likely reduces our carbon footprint from OR procedures by only 5%.8 However, recycling is still a good way to divert appropriate materials from landfill, saving costs and emissions at the end of a material’s life. One example is sterile blue wrap, which is a petroleum product with a recycling number of 6 and a filtration rating of N99. Blue wrap can be recycled into plastic pellets, or it can be recreated into other hospital supplies, such as gowns.
Bottom line: ObGyns can petition their hospitals to work with suppliers and waste-processing companies who have recycling programs built into their supply chains.
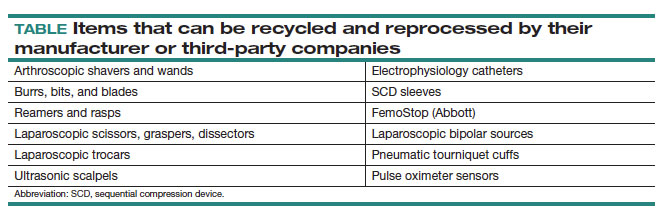
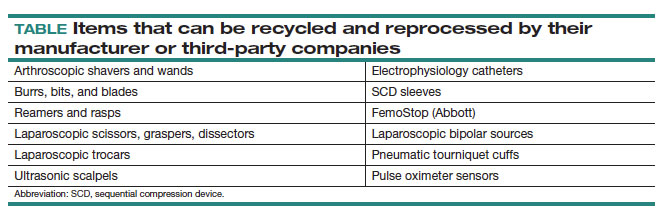
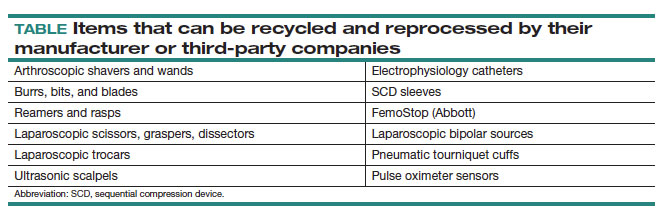
By contrast, reprocessing can have a much larger impact on carbon emissions. Complex items, such as advanced energy devices that can be reprocessed, result in a greater reduction in carbon emissions due to the reuse of their complex materials and manufacturing when compared with such devices that cannot be reprocessed. Recycling and reprocessing programs are already in place for several devices (TABLE). Authors of a systematic review showed that there is no evidence to support the use of single-use supplies and instruments over reprocessed items when considering instrument function, ease of use, patient safety, transmission of infection, or long-term patient outcomes.21
Bottom line: ObGyns can choose to use reprocessed items in ORs instead of single-use devices and educate staff on the safety of these items.
Continue to: Remove...
Remove
7. Remove desflurane and other volatile gases from formularies
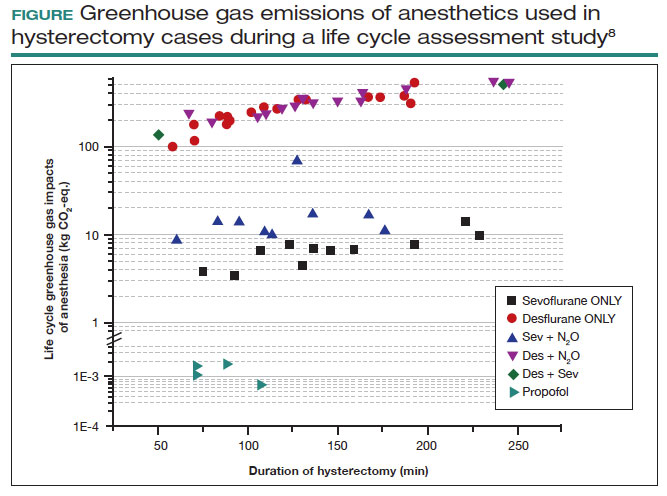
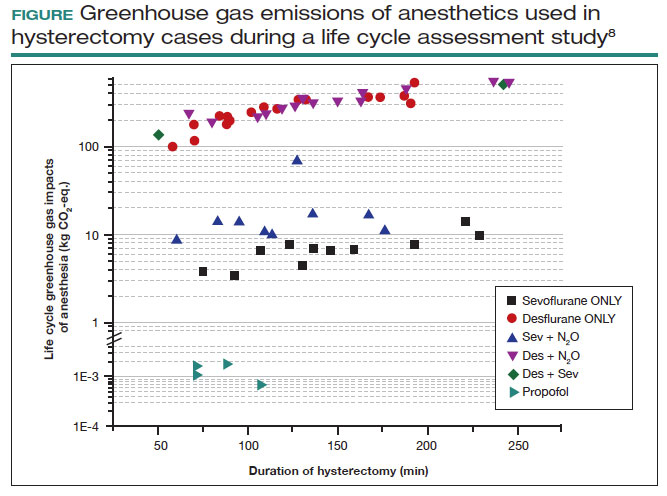
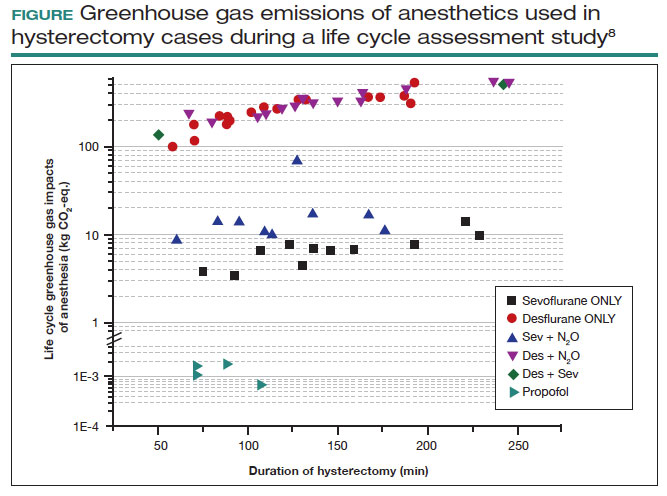
Volatile anesthetic gases, such as desflurane, isoflurane, and nitrous oxide, are themselves potent greenhouse gases, comprising a large portion of the carbon emissions that come from the OR.22 Desflurane was developed to have a rapid onset for induction and quick recovery; however, studies have shown no clinical benefit over other gases.23 Furthermore, the costs and greenhouse gas potential are substantial. Desflurane costs 2 to 3 times more and has more than 20 times the global warming potential of the other volatile gases (FIGURE).8 Using 1 hour of desflurane is equivalent to driving 378 miles in a gas-powered vehicle, while the use of isoflurane and sevoflurane create equivalents of only 15 and 8 miles, respectively.23
Nitrous oxide is another powerful greenhouse gas that is a direct ozone depletor and can stay in the atmosphere for 114 years.22 Nitrous oxide has limited clinical use in hospitals, but it is often stored in central hospital piping. Most of the impact of nitrous oxide comes through leaks in a poor system design rather than patient delivery. One estimate reveals that more than 13 million liters of nitrous oxide are lost annually from leaks in European hospitals.22 The American Society of Anesthesiologists recommends decommissioning central piping of nitrous oxide in favor of cylinders at the point of care.24
Literature on enhanced recovery after surgery in gynecology promotes the use of propofol over volatile gases for our patients because of the high rate of postoperative nausea and vomiting seen with gases.25 Volatile gases should be a last-choice anesthetic for our patients.
Bottom line: It is critical that ObGyns work with colleagues in anesthesia to develop climate- and patient-friendly protocols for procedures.
8. Remove endocrine-disrupting chemicals from clinical supplies
Endocrine-disrupting chemicals (EDCs) are a type of chemical that alter the hormonal systems of humans, which can result in adverse health effects. Multiple studies and reviews have tied EDCs to reproductive abnormalities, such as the effects of bisphenol A (BPA) on estradiol levels, antral follicle counts, oocyte quality, and implantation rates; phthalates on fibroid burden; triclosan on embryo quality; parabens on live birth rates; and perfluoroalkylsubstances (PFAS or “forever substances”) on hypertensive disorders of pregnancy.5,26,27
What might be most shocking is that these EDCs are incorporated into medical supplies and pharmaceuticals. For example, BPA is known to line dialysis and ointment tubes, parabens are used for their antimicrobial properties in ultrasound gel and hep-locks, and phthalates are found in up to 40% of medical-use plastics and controlled-release medications. Authors of an observational study found that 74% of patients admitted to an LD unit were exposed to EDCs. In a neonatal intensive care unit (NICU), most of the supplies contained an EDC, and urinary BPA levels were elevated in neonates admitted to a NICU, raising concerns about long-term health risks.5
Bottom line: Physicians and health care institutions have an obligation to petition industry partners and suppliers to remove EDCs from their supply chains.
Reimagine
9. Educate
The field of health care sustainability remains in its infancy, but from 2007 to 2019, publications on climate change and health in academia increased by a factor of 8.29 Additionally, through waste audits, quality-improvement projects, and life cycle analyses (analytical tools to evaluate product or process emissions from materials extraction to disposal), we have gained insight into the scope of the problem, with evidence showing that our practices are largely derived from culture. It is time to provide formal education on health care sustainability to medical trainees, staff, and clinicians alike, who desire to see this topic reflected in their formal curricula.30 Start talking about it!
Bottom line: Commentaries, webinars, formal didactics sessions, in-services, and hospital workgroups to introduce this topic are a good way to teach others about the carbon footprint of our care and solutions to minimize it.
10. Engage in advocacy
Physicians have an ethical duty to advocate for change at the local, regional, and national levels if we want to see a better future for our patients, their children, and even ourselves. We should reimagine this work as an important public health initiative.31 Surveys of physicians, including ObGyns, reveal a concern about the sustainability of health care and a commitment to addressing this issue.20 ObGyns are on the frontlines of delivering care every day, so we are poised to implement changes that can impact our patients, especially when we can lead and petition hospital or local committees.20,28,32 There is much to be done, but every voice counts and can make impactful changes at every level. ●
- Costello A, Abbas M, Allen et al. Managing the health effects of climate change: Lancet and University College London Institute for Global Health Commission. Lancet. 2009;373:1693-1733.
- Health care climate footprint report. Health Care Without Harm website. https://www.noharm.org/ClimateFootprintReport. Accessed May 12, 2023.
- Balbus JM, McCannon CJ, Mataka A, et al. After COP26—putting health and equity at the center of the climate movement. N Engl J Med. 2022;386:1295-1297.
- Bekkar B, Pacheco S, Basu R, et al. Association of air pollution and heat exposure with preterm birth, low birth weight, and stillbirth in the US: a systematic review. JAMA Netw Open. 2020;3:e208243.
- Genco M, Anderson-Shaw L, Sargis RM. Unwitting accomplices: endocrine disruptors confounding clinical care. J Clin Endocrinol Metab. 2020;105:e3822-e3827.
- Al-Kindi SG, Sarode A, Zullo M, et al. Ambient air pollution and mortality after cardiac transplantation. J Am Coll Cardiol. 2019;74:30263035.
- Ghosh R, Gauderman WJ, Minor H, et al. Air pollution, weight loss and metabolic benefits of bariatric surgery: a potential model for study of metabolic effects of environmental exposures. Pediatr Obes. 2018;13:312-320.
- Thiel CL, Eckelman M, Guido R, et al. Environmental impacts of surgical procedures: life cycle assessment of hysterectomy in the United States. Environ Sci Technol. 2015;49:1779-1786.
- Zygourakis CC, Yoon S, Valencia V, et al. Operating room waste: disposable supply utilization in neurosurgical procedures. J Neurosurg. 2017;126:620-625.
- van Demark RE, Smith VJS, Fiegen A. Lean and green hand surgery. J Hand Surg. 2018;43:179-181.
- Campion N, Thiel CL, DeBlois J, et al. Life cycle assessment perspectives on delivering an infant in the US. Sci Total Environ. 2012;425:191198.
- Hsu S, Thiel CL, Mello MJ, Slutzman JE. Dumpster diving in the emergency department. West J Emerg Med. 2020;21:1211-1217.
- Mcgain F, Story D, Hendel S. An audit of intensive care unit recyclable waste. Anaesthesia. 2009;64:1299-1302.
- Wormer BA, Augenstein VA, Carpenter CL, et al. The green operating room: simple changes to reduce cost and our carbon footprint. Am Surg. 2013;79:666-671.
- Kagoma Y, Stall N, Rubinstein E, et al. People, planet and profits: the case for greening operating rooms. Can Med Assoc J. 2012;184:19051911.
- McCarthy CJ, Gerstenmaier JF, O’ Neill AC, et al. “EcoRadiology”— pulling the plug on wasted energy in the radiology department. Acad Radiol. 2014;21:1563-1566.
- Donahue LM, Hilton S, Bell SG, et al. A comparative carbon footprint analysis of disposable and reusable vaginal specula. Am J Obstet Gynecol. 2020;223:225.e1-225.e7.
- Rodriguez Morris MI, Hicks A. Life cycle assessment of stainless-steel reusable speculums versus disposable acrylic speculums in a university clinic setting: a case study. Environ Res Commun. 2022;4:025002.
- MacNeill AJ, Lillywhite R, Brown CJ. The impact of surgery on global climate: a carbon footprinting study of operating theatres in three health systems. Lancet Planet Health. 2017;1:e381-e388.
- Thiel C, Duncan P, Woods N. Attitude of US obstetricians and gynaecologists to global warming and medical waste. J Health Serv Res Policy. 2017;22:162-167.
- Siu J, Hill AG, MacCormick AD. Systematic review of reusable versus disposable laparoscopic instruments: costs and safety. ANZ J Surg. 2017;87:28-33.
- Ryan SM, Nielsen CJ. Global warming potential of inhaled anesthetics: application to clinical use. Anesth Analg. 2010;111:92-98.
- Meyer MJ. Desflurane should des-appear: global and financial rationale. Anesth Analg. 2020;131:1317-1322.
- Rollins MD, Arendt KW, Carvalho B, et al. ASA Committee on Obstetric Anesthesia Working Group. Nitrous oxide. American Society of Anesthesiologists website. Accessed May 12, 2023. https://www .asahq.org/about-asa/governance-and-committees/asa-committees /committee-on-obstetric-anesthesia/nitrous-oxide.
- Kalogera E, Dowdy SC. Enhanced recovery pathway in gynecologic surgery: improving outcomes through evidence-based medicine. Obstet Gynecol Clin North Am. 2016;43:551-573.
- Zota AR, Geller RJ, Calafat AM, et al. Phthalates exposure and uterine fibroid burden among women undergoing surgical treatment for fibroids: a preliminary study. Fertil Steril. 2019;111:112-121.
- Bommartio PA, Ferguson KK, Meeker JD, et al. Maternal levels of perfluoroalkyl substances (PFAS) during early pregnancy in relation to preeclampsia subtypes and biomarkers of preeclampsia risk. Environ Health Perspect. 2021;129:107004.
- Azouz S, Boyll P, Swanson M, et al. Managing barriers to recycling in the operating room. Am J Surg. 2019;217:634-638.
- Watts N, Amann M, Arnell N, et al. The 2020 report of The Lancet Countdown on health and climate change: responding to converging crises. Lancet. 2021;397:129-170.
- Ryan EC, Dubrow R, Sherman JD. Medical, nursing, and physician assistant student knowledge and attitudes toward climate change, pollution, and resource conservation in health care. BMC Med Educ. 2020;20:200.
- Giudice LC, Llamas-Clark EF, DeNicola Net al; FIGO Committee on Climate Change and Toxic Environmental Exposures. Climate change, women’s health, and the role of obstetricians and gynecologists in leadership. Int J Gynaecol Obstet. 2021;155:345-356.
- Yates EF, Bowder AN, Roa L, et al. Empowering surgeons, anesthesiologists, and obstetricians to incorporate environmental sustainability in the operating room. Ann Surg. 2021;273:1108-1114.
Climate change has been called the biggest health threat of the 21st century.1 The health care sector is a huge contributor to global carbon emissions, accounting for almost double the emissions of global aviation. While other industries and countries are implementing mitigation measures to decrease their emissions, health care is currently on track to double its carbon emissions by 2050, even though it should be carbon neutral by that time to comply with the Paris Climate Agreement.2 There have been some national efforts to curb health care emissions, including the creation of the Office of Climate Change and Health Equity in 2021 and the passage of the Inflation Reduction Act in 2022.3 These are top-down, administrative approaches, and to be successful we will also need clinicians to understand and address this problem.
The negative impacts of heat, air pollution, and exposure to toxic substances on human health have been well documented in multiple regions across multiple specialties.4-7 The United States makes up 27% of the global health care carbon footprint—more emissions than the entire United Kingdom as a country—despite having only 4% of the world’s population.2 Culture and incentives for an overabundance of single-use supplies, not evidence for patient safety, have led to this uniquely American problem. It is evident that our health care industry is an excellent place to implement mitigation measures for carbon emissions that contribute to climate change and can improve health outcomes.
In this article, we recommend 10 practices that can decrease our carbon footprint in ObGyn. We focus on the classic motto of “Reduce, Reuse, Recycle,” while adding “Remove” and “Reimagine” to classify the ways in which we can reduce emissions while not compromising our care to patients.
Reduce
1. Minimize opened materials and single-use devices in the OR and labor and delivery
Health care is a unique setting where a culture of infection prevention and efficiency has led low-cost, single-use supplies to dominate over reusable items. While single-use items can have inexpensive purchasing costs compared to reusable items, the environmental costs required for the production and disposal of the former are often much greater. In operating rooms (ORs) and labor and delivery (LD) units, single-use items are omnipresent. Over the past decade, researchers and clinicians have started to take a closer look at these items and their carbon footprint. One group evaluated hysterectomy through a waste audit and found that the vast majority of waste from all of the cases was Spunbond Meltblown Spunbond, or SMS; plastic materialthat comprises gowns; blue wraps; and drapes; followed by hard plastic material that comprises trays and packaging.8 Moreover, production and manufacturing processes contributed to 95% of the environmental impacts of these items.8
In an effort to be time efficient, OR staff will open sterile surgical packs and individual peel-pack items prior to surgery to minimize having to find items during surgery. However, this creates an inordinate amount of waste. One group of neurosurgeons who evaluated their opened but unused supplies found that 85% of their unused items were individually opened items, leading to a waste of $2.9 million per year.9 Minor procedures like dilation and curettage, cystoscopy, and hysteroscopy do not need such a large sterile field, as these procedures are also safe to perform in the office. Hand surgeons have been quick to lead in this space, particularly with minor procedures such as carpal tunnel release. One division was able to eliminate 2.8 tons of waste and save $13,000 in a 2-year period by reducing the sterile field.10 ObGyns can work with OR and LD staff to create custom packs that minimize unused or underutilized items, helping to reduce both the carbon footprint and health care spending.
Bottom line: ObGyns can help foster a culture of having supplies available but not opened until needed during a case.
Continue to: 2. Decrease regulated medical waste...
2. Decrease regulated medical waste
Health care is unique from other fields in that there are multiple waste streams to consider. Infectious waste and items saturated in blood or capable of causing infection must be placed into regulated medical waste (RMW), or more commonly, red biohazard bags. RMW is autoclaved or incinerated prior to disposal in a landfill. This process is more financially and environmentally costly than general municipal waste (GMW). This process also requires more transport—1 study revealed that GMW traveled 20 km to a landfill for disposal, compared with the 50 km that RMW traveled for sterilized-prior-to-landfill disposal.11
Unfortunately, the vast majority of items placed in RMW are incorrectly triaged and should instead be disposed in GMW.12,13 One study performed in an emergency department revealed that 85% of waste was incorrectly placed in the RMW.12
Bottom line: ObGyns can avoid placing items in RMW that may not qualify and advocate for institution policy changes to remove RMW from places such as waiting rooms, at the patient bedside, or next to scrub sinks.
3. Reduce energy use
ORs and LD units use a lot of energy, and numerous studies have demonstrated that the heating, ventilation, and air conditioning (HVAC) system plays a large role in emissions.8,11 This can easily be fixed by “HVAC setbacks” and powering down rooms when not in use. One institution powered down ORs when not in use and reduced 234 metric tons of CO2 emissions and saved $33,000 per year.14 Transitioning to light-emitting diode (LED) lights reduced energy usage at 1 institution by almost 50%.15 Finally, computers in clinical offices, examination rooms, and administrative offices can be powered down at the end of the day. One study found that in 1 radiology department, 29 computers left on overnight and on weekends emitted 17.7 tons of CO2 emissions in 1 year.16
Bottom line: We as ObGyns can advocate for how energy can be saved outside of surgical cases, including powering down ORs and LD units, transitioning to LED lighting, and powering down workstations.
Reuse
4. Choose reusable equipment
In ObGyn practice, the most commonly used tool is the speculum. Given its omnipresence, the speculum is a great place to start to decrease our carbon footprint. Two studies have evaluated the environmental impact of reusable versus single-use disposable specula, and both demonstrated that the stainless-steel versions have less global warming potential than the acrylic varieties.17,18 Donahue and colleagues17 demonstrated that it only took 2 to 3 pelvic examinations for the cost of stainless-steel specula to break even, even when sterilized in a half-filled autoclave tray. Rodriquez, et al18 revealed that, compared with an acrylic model, the stainless-steel specula had fewer negative impacts in terms of global warming, acidification, respiratory effects, smog, and fossil fuel depletion.18
Bottom line: Strongly consider using stainless-steel specula to reduce costs and carbon emissions.
In addition to specula, ObGyns can choose reusable equipment in the OR. For example, surgeons can use stainless-steel trocars instead of disposable trocars.19 In vaginal cases, Breisky-Navratil retractors can be used instead of disposable self-retaining retractors. Plastic basins that often are included in sterile supply packs can be replaced with stainless-steel basins, which could have profound positive effects on the carbon footprint of gynecologic surgery.8 One study of ObGyns demonstrated that 95% of physicians supported waste-reduction efforts, and 66% supported utilizing reusable surgical tools instead of disposable tools.20
Bottom line: As surgeons, ObGyns have influence over what they want to use in the OR, and they can petition for reusable options over disposable options.
5. Launder the sterile blue towels
Sterile blue towels, which are made of cotton, have the largest environmental footprint compared with other disposable materials, such as plastics, and contribute greatly to toxicity in human health.8,11 Although these towels cannot be laundered and sterilized again for use in a sterile surgical field, they can be laundered and repurposed, including by environmental services to clean hospital rooms. Blue towels should be able to be laundered no matter how saturated in body fluids they are.
Bottom line: ObGyns should strive to always launder the blue towels and educate trainees and other staff in the OR to do the same.
Recycle
6. Recycle and reprocess materials and devices
While recycling is immensely important, it requires a large amount of energy to break down a material to its raw components for manufacturing. It likely reduces our carbon footprint from OR procedures by only 5%.8 However, recycling is still a good way to divert appropriate materials from landfill, saving costs and emissions at the end of a material’s life. One example is sterile blue wrap, which is a petroleum product with a recycling number of 6 and a filtration rating of N99. Blue wrap can be recycled into plastic pellets, or it can be recreated into other hospital supplies, such as gowns.
Bottom line: ObGyns can petition their hospitals to work with suppliers and waste-processing companies who have recycling programs built into their supply chains.
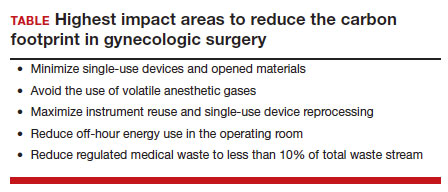
By contrast, reprocessing can have a much larger impact on carbon emissions. Complex items, such as advanced energy devices that can be reprocessed, result in a greater reduction in carbon emissions due to the reuse of their complex materials and manufacturing when compared with such devices that cannot be reprocessed. Recycling and reprocessing programs are already in place for several devices (TABLE). Authors of a systematic review showed that there is no evidence to support the use of single-use supplies and instruments over reprocessed items when considering instrument function, ease of use, patient safety, transmission of infection, or long-term patient outcomes.21
Bottom line: ObGyns can choose to use reprocessed items in ORs instead of single-use devices and educate staff on the safety of these items.
Continue to: Remove...
Remove
7. Remove desflurane and other volatile gases from formularies
Volatile anesthetic gases, such as desflurane, isoflurane, and nitrous oxide, are themselves potent greenhouse gases, comprising a large portion of the carbon emissions that come from the OR.22 Desflurane was developed to have a rapid onset for induction and quick recovery; however, studies have shown no clinical benefit over other gases.23 Furthermore, the costs and greenhouse gas potential are substantial. Desflurane costs 2 to 3 times more and has more than 20 times the global warming potential of the other volatile gases (FIGURE).8 Using 1 hour of desflurane is equivalent to driving 378 miles in a gas-powered vehicle, while the use of isoflurane and sevoflurane create equivalents of only 15 and 8 miles, respectively.23
Nitrous oxide is another powerful greenhouse gas that is a direct ozone depletor and can stay in the atmosphere for 114 years.22 Nitrous oxide has limited clinical use in hospitals, but it is often stored in central hospital piping. Most of the impact of nitrous oxide comes through leaks in a poor system design rather than patient delivery. One estimate reveals that more than 13 million liters of nitrous oxide are lost annually from leaks in European hospitals.22 The American Society of Anesthesiologists recommends decommissioning central piping of nitrous oxide in favor of cylinders at the point of care.24
Literature on enhanced recovery after surgery in gynecology promotes the use of propofol over volatile gases for our patients because of the high rate of postoperative nausea and vomiting seen with gases.25 Volatile gases should be a last-choice anesthetic for our patients.
Bottom line: It is critical that ObGyns work with colleagues in anesthesia to develop climate- and patient-friendly protocols for procedures.
8. Remove endocrine-disrupting chemicals from clinical supplies
Endocrine-disrupting chemicals (EDCs) are a type of chemical that alter the hormonal systems of humans, which can result in adverse health effects. Multiple studies and reviews have tied EDCs to reproductive abnormalities, such as the effects of bisphenol A (BPA) on estradiol levels, antral follicle counts, oocyte quality, and implantation rates; phthalates on fibroid burden; triclosan on embryo quality; parabens on live birth rates; and perfluoroalkylsubstances (PFAS or “forever substances”) on hypertensive disorders of pregnancy.5,26,27
What might be most shocking is that these EDCs are incorporated into medical supplies and pharmaceuticals. For example, BPA is known to line dialysis and ointment tubes, parabens are used for their antimicrobial properties in ultrasound gel and hep-locks, and phthalates are found in up to 40% of medical-use plastics and controlled-release medications. Authors of an observational study found that 74% of patients admitted to an LD unit were exposed to EDCs. In a neonatal intensive care unit (NICU), most of the supplies contained an EDC, and urinary BPA levels were elevated in neonates admitted to a NICU, raising concerns about long-term health risks.5
Bottom line: Physicians and health care institutions have an obligation to petition industry partners and suppliers to remove EDCs from their supply chains.
Reimagine
9. Educate
The field of health care sustainability remains in its infancy, but from 2007 to 2019, publications on climate change and health in academia increased by a factor of 8.29 Additionally, through waste audits, quality-improvement projects, and life cycle analyses (analytical tools to evaluate product or process emissions from materials extraction to disposal), we have gained insight into the scope of the problem, with evidence showing that our practices are largely derived from culture. It is time to provide formal education on health care sustainability to medical trainees, staff, and clinicians alike, who desire to see this topic reflected in their formal curricula.30 Start talking about it!
Bottom line: Commentaries, webinars, formal didactics sessions, in-services, and hospital workgroups to introduce this topic are a good way to teach others about the carbon footprint of our care and solutions to minimize it.
10. Engage in advocacy
Physicians have an ethical duty to advocate for change at the local, regional, and national levels if we want to see a better future for our patients, their children, and even ourselves. We should reimagine this work as an important public health initiative.31 Surveys of physicians, including ObGyns, reveal a concern about the sustainability of health care and a commitment to addressing this issue.20 ObGyns are on the frontlines of delivering care every day, so we are poised to implement changes that can impact our patients, especially when we can lead and petition hospital or local committees.20,28,32 There is much to be done, but every voice counts and can make impactful changes at every level. ●
Climate change has been called the biggest health threat of the 21st century.1 The health care sector is a huge contributor to global carbon emissions, accounting for almost double the emissions of global aviation. While other industries and countries are implementing mitigation measures to decrease their emissions, health care is currently on track to double its carbon emissions by 2050, even though it should be carbon neutral by that time to comply with the Paris Climate Agreement.2 There have been some national efforts to curb health care emissions, including the creation of the Office of Climate Change and Health Equity in 2021 and the passage of the Inflation Reduction Act in 2022.3 These are top-down, administrative approaches, and to be successful we will also need clinicians to understand and address this problem.
The negative impacts of heat, air pollution, and exposure to toxic substances on human health have been well documented in multiple regions across multiple specialties.4-7 The United States makes up 27% of the global health care carbon footprint—more emissions than the entire United Kingdom as a country—despite having only 4% of the world’s population.2 Culture and incentives for an overabundance of single-use supplies, not evidence for patient safety, have led to this uniquely American problem. It is evident that our health care industry is an excellent place to implement mitigation measures for carbon emissions that contribute to climate change and can improve health outcomes.
In this article, we recommend 10 practices that can decrease our carbon footprint in ObGyn. We focus on the classic motto of “Reduce, Reuse, Recycle,” while adding “Remove” and “Reimagine” to classify the ways in which we can reduce emissions while not compromising our care to patients.
Reduce
1. Minimize opened materials and single-use devices in the OR and labor and delivery
Health care is a unique setting where a culture of infection prevention and efficiency has led low-cost, single-use supplies to dominate over reusable items. While single-use items can have inexpensive purchasing costs compared to reusable items, the environmental costs required for the production and disposal of the former are often much greater. In operating rooms (ORs) and labor and delivery (LD) units, single-use items are omnipresent. Over the past decade, researchers and clinicians have started to take a closer look at these items and their carbon footprint. One group evaluated hysterectomy through a waste audit and found that the vast majority of waste from all of the cases was Spunbond Meltblown Spunbond, or SMS; plastic materialthat comprises gowns; blue wraps; and drapes; followed by hard plastic material that comprises trays and packaging.8 Moreover, production and manufacturing processes contributed to 95% of the environmental impacts of these items.8
In an effort to be time efficient, OR staff will open sterile surgical packs and individual peel-pack items prior to surgery to minimize having to find items during surgery. However, this creates an inordinate amount of waste. One group of neurosurgeons who evaluated their opened but unused supplies found that 85% of their unused items were individually opened items, leading to a waste of $2.9 million per year.9 Minor procedures like dilation and curettage, cystoscopy, and hysteroscopy do not need such a large sterile field, as these procedures are also safe to perform in the office. Hand surgeons have been quick to lead in this space, particularly with minor procedures such as carpal tunnel release. One division was able to eliminate 2.8 tons of waste and save $13,000 in a 2-year period by reducing the sterile field.10 ObGyns can work with OR and LD staff to create custom packs that minimize unused or underutilized items, helping to reduce both the carbon footprint and health care spending.
Bottom line: ObGyns can help foster a culture of having supplies available but not opened until needed during a case.
Continue to: 2. Decrease regulated medical waste...
2. Decrease regulated medical waste
Health care is unique from other fields in that there are multiple waste streams to consider. Infectious waste and items saturated in blood or capable of causing infection must be placed into regulated medical waste (RMW), or more commonly, red biohazard bags. RMW is autoclaved or incinerated prior to disposal in a landfill. This process is more financially and environmentally costly than general municipal waste (GMW). This process also requires more transport—1 study revealed that GMW traveled 20 km to a landfill for disposal, compared with the 50 km that RMW traveled for sterilized-prior-to-landfill disposal.11
Unfortunately, the vast majority of items placed in RMW are incorrectly triaged and should instead be disposed in GMW.12,13 One study performed in an emergency department revealed that 85% of waste was incorrectly placed in the RMW.12
Bottom line: ObGyns can avoid placing items in RMW that may not qualify and advocate for institution policy changes to remove RMW from places such as waiting rooms, at the patient bedside, or next to scrub sinks.
3. Reduce energy use
ORs and LD units use a lot of energy, and numerous studies have demonstrated that the heating, ventilation, and air conditioning (HVAC) system plays a large role in emissions.8,11 This can easily be fixed by “HVAC setbacks” and powering down rooms when not in use. One institution powered down ORs when not in use and reduced 234 metric tons of CO2 emissions and saved $33,000 per year.14 Transitioning to light-emitting diode (LED) lights reduced energy usage at 1 institution by almost 50%.15 Finally, computers in clinical offices, examination rooms, and administrative offices can be powered down at the end of the day. One study found that in 1 radiology department, 29 computers left on overnight and on weekends emitted 17.7 tons of CO2 emissions in 1 year.16
Bottom line: We as ObGyns can advocate for how energy can be saved outside of surgical cases, including powering down ORs and LD units, transitioning to LED lighting, and powering down workstations.
Reuse
4. Choose reusable equipment
In ObGyn practice, the most commonly used tool is the speculum. Given its omnipresence, the speculum is a great place to start to decrease our carbon footprint. Two studies have evaluated the environmental impact of reusable versus single-use disposable specula, and both demonstrated that the stainless-steel versions have less global warming potential than the acrylic varieties.17,18 Donahue and colleagues17 demonstrated that it only took 2 to 3 pelvic examinations for the cost of stainless-steel specula to break even, even when sterilized in a half-filled autoclave tray. Rodriquez, et al18 revealed that, compared with an acrylic model, the stainless-steel specula had fewer negative impacts in terms of global warming, acidification, respiratory effects, smog, and fossil fuel depletion.18
Bottom line: Strongly consider using stainless-steel specula to reduce costs and carbon emissions.
In addition to specula, ObGyns can choose reusable equipment in the OR. For example, surgeons can use stainless-steel trocars instead of disposable trocars.19 In vaginal cases, Breisky-Navratil retractors can be used instead of disposable self-retaining retractors. Plastic basins that often are included in sterile supply packs can be replaced with stainless-steel basins, which could have profound positive effects on the carbon footprint of gynecologic surgery.8 One study of ObGyns demonstrated that 95% of physicians supported waste-reduction efforts, and 66% supported utilizing reusable surgical tools instead of disposable tools.20
Bottom line: As surgeons, ObGyns have influence over what they want to use in the OR, and they can petition for reusable options over disposable options.
5. Launder the sterile blue towels
Sterile blue towels, which are made of cotton, have the largest environmental footprint compared with other disposable materials, such as plastics, and contribute greatly to toxicity in human health.8,11 Although these towels cannot be laundered and sterilized again for use in a sterile surgical field, they can be laundered and repurposed, including by environmental services to clean hospital rooms. Blue towels should be able to be laundered no matter how saturated in body fluids they are.
Bottom line: ObGyns should strive to always launder the blue towels and educate trainees and other staff in the OR to do the same.
Recycle
6. Recycle and reprocess materials and devices
While recycling is immensely important, it requires a large amount of energy to break down a material to its raw components for manufacturing. It likely reduces our carbon footprint from OR procedures by only 5%.8 However, recycling is still a good way to divert appropriate materials from landfill, saving costs and emissions at the end of a material’s life. One example is sterile blue wrap, which is a petroleum product with a recycling number of 6 and a filtration rating of N99. Blue wrap can be recycled into plastic pellets, or it can be recreated into other hospital supplies, such as gowns.
Bottom line: ObGyns can petition their hospitals to work with suppliers and waste-processing companies who have recycling programs built into their supply chains.
By contrast, reprocessing can have a much larger impact on carbon emissions. Complex items, such as advanced energy devices that can be reprocessed, result in a greater reduction in carbon emissions due to the reuse of their complex materials and manufacturing when compared with such devices that cannot be reprocessed. Recycling and reprocessing programs are already in place for several devices (TABLE). Authors of a systematic review showed that there is no evidence to support the use of single-use supplies and instruments over reprocessed items when considering instrument function, ease of use, patient safety, transmission of infection, or long-term patient outcomes.21
Bottom line: ObGyns can choose to use reprocessed items in ORs instead of single-use devices and educate staff on the safety of these items.
Continue to: Remove...
Remove
7. Remove desflurane and other volatile gases from formularies
Volatile anesthetic gases, such as desflurane, isoflurane, and nitrous oxide, are themselves potent greenhouse gases, comprising a large portion of the carbon emissions that come from the OR.22 Desflurane was developed to have a rapid onset for induction and quick recovery; however, studies have shown no clinical benefit over other gases.23 Furthermore, the costs and greenhouse gas potential are substantial. Desflurane costs 2 to 3 times more and has more than 20 times the global warming potential of the other volatile gases (FIGURE).8 Using 1 hour of desflurane is equivalent to driving 378 miles in a gas-powered vehicle, while the use of isoflurane and sevoflurane create equivalents of only 15 and 8 miles, respectively.23
Nitrous oxide is another powerful greenhouse gas that is a direct ozone depletor and can stay in the atmosphere for 114 years.22 Nitrous oxide has limited clinical use in hospitals, but it is often stored in central hospital piping. Most of the impact of nitrous oxide comes through leaks in a poor system design rather than patient delivery. One estimate reveals that more than 13 million liters of nitrous oxide are lost annually from leaks in European hospitals.22 The American Society of Anesthesiologists recommends decommissioning central piping of nitrous oxide in favor of cylinders at the point of care.24
Literature on enhanced recovery after surgery in gynecology promotes the use of propofol over volatile gases for our patients because of the high rate of postoperative nausea and vomiting seen with gases.25 Volatile gases should be a last-choice anesthetic for our patients.
Bottom line: It is critical that ObGyns work with colleagues in anesthesia to develop climate- and patient-friendly protocols for procedures.
8. Remove endocrine-disrupting chemicals from clinical supplies
Endocrine-disrupting chemicals (EDCs) are a type of chemical that alter the hormonal systems of humans, which can result in adverse health effects. Multiple studies and reviews have tied EDCs to reproductive abnormalities, such as the effects of bisphenol A (BPA) on estradiol levels, antral follicle counts, oocyte quality, and implantation rates; phthalates on fibroid burden; triclosan on embryo quality; parabens on live birth rates; and perfluoroalkylsubstances (PFAS or “forever substances”) on hypertensive disorders of pregnancy.5,26,27
What might be most shocking is that these EDCs are incorporated into medical supplies and pharmaceuticals. For example, BPA is known to line dialysis and ointment tubes, parabens are used for their antimicrobial properties in ultrasound gel and hep-locks, and phthalates are found in up to 40% of medical-use plastics and controlled-release medications. Authors of an observational study found that 74% of patients admitted to an LD unit were exposed to EDCs. In a neonatal intensive care unit (NICU), most of the supplies contained an EDC, and urinary BPA levels were elevated in neonates admitted to a NICU, raising concerns about long-term health risks.5
Bottom line: Physicians and health care institutions have an obligation to petition industry partners and suppliers to remove EDCs from their supply chains.
Reimagine
9. Educate
The field of health care sustainability remains in its infancy, but from 2007 to 2019, publications on climate change and health in academia increased by a factor of 8.29 Additionally, through waste audits, quality-improvement projects, and life cycle analyses (analytical tools to evaluate product or process emissions from materials extraction to disposal), we have gained insight into the scope of the problem, with evidence showing that our practices are largely derived from culture. It is time to provide formal education on health care sustainability to medical trainees, staff, and clinicians alike, who desire to see this topic reflected in their formal curricula.30 Start talking about it!
Bottom line: Commentaries, webinars, formal didactics sessions, in-services, and hospital workgroups to introduce this topic are a good way to teach others about the carbon footprint of our care and solutions to minimize it.
10. Engage in advocacy
Physicians have an ethical duty to advocate for change at the local, regional, and national levels if we want to see a better future for our patients, their children, and even ourselves. We should reimagine this work as an important public health initiative.31 Surveys of physicians, including ObGyns, reveal a concern about the sustainability of health care and a commitment to addressing this issue.20 ObGyns are on the frontlines of delivering care every day, so we are poised to implement changes that can impact our patients, especially when we can lead and petition hospital or local committees.20,28,32 There is much to be done, but every voice counts and can make impactful changes at every level. ●
- Costello A, Abbas M, Allen et al. Managing the health effects of climate change: Lancet and University College London Institute for Global Health Commission. Lancet. 2009;373:1693-1733.
- Health care climate footprint report. Health Care Without Harm website. https://www.noharm.org/ClimateFootprintReport. Accessed May 12, 2023.
- Balbus JM, McCannon CJ, Mataka A, et al. After COP26—putting health and equity at the center of the climate movement. N Engl J Med. 2022;386:1295-1297.
- Bekkar B, Pacheco S, Basu R, et al. Association of air pollution and heat exposure with preterm birth, low birth weight, and stillbirth in the US: a systematic review. JAMA Netw Open. 2020;3:e208243.
- Genco M, Anderson-Shaw L, Sargis RM. Unwitting accomplices: endocrine disruptors confounding clinical care. J Clin Endocrinol Metab. 2020;105:e3822-e3827.
- Al-Kindi SG, Sarode A, Zullo M, et al. Ambient air pollution and mortality after cardiac transplantation. J Am Coll Cardiol. 2019;74:30263035.
- Ghosh R, Gauderman WJ, Minor H, et al. Air pollution, weight loss and metabolic benefits of bariatric surgery: a potential model for study of metabolic effects of environmental exposures. Pediatr Obes. 2018;13:312-320.
- Thiel CL, Eckelman M, Guido R, et al. Environmental impacts of surgical procedures: life cycle assessment of hysterectomy in the United States. Environ Sci Technol. 2015;49:1779-1786.
- Zygourakis CC, Yoon S, Valencia V, et al. Operating room waste: disposable supply utilization in neurosurgical procedures. J Neurosurg. 2017;126:620-625.
- van Demark RE, Smith VJS, Fiegen A. Lean and green hand surgery. J Hand Surg. 2018;43:179-181.
- Campion N, Thiel CL, DeBlois J, et al. Life cycle assessment perspectives on delivering an infant in the US. Sci Total Environ. 2012;425:191198.
- Hsu S, Thiel CL, Mello MJ, Slutzman JE. Dumpster diving in the emergency department. West J Emerg Med. 2020;21:1211-1217.
- Mcgain F, Story D, Hendel S. An audit of intensive care unit recyclable waste. Anaesthesia. 2009;64:1299-1302.
- Wormer BA, Augenstein VA, Carpenter CL, et al. The green operating room: simple changes to reduce cost and our carbon footprint. Am Surg. 2013;79:666-671.
- Kagoma Y, Stall N, Rubinstein E, et al. People, planet and profits: the case for greening operating rooms. Can Med Assoc J. 2012;184:19051911.
- McCarthy CJ, Gerstenmaier JF, O’ Neill AC, et al. “EcoRadiology”— pulling the plug on wasted energy in the radiology department. Acad Radiol. 2014;21:1563-1566.
- Donahue LM, Hilton S, Bell SG, et al. A comparative carbon footprint analysis of disposable and reusable vaginal specula. Am J Obstet Gynecol. 2020;223:225.e1-225.e7.
- Rodriguez Morris MI, Hicks A. Life cycle assessment of stainless-steel reusable speculums versus disposable acrylic speculums in a university clinic setting: a case study. Environ Res Commun. 2022;4:025002.
- MacNeill AJ, Lillywhite R, Brown CJ. The impact of surgery on global climate: a carbon footprinting study of operating theatres in three health systems. Lancet Planet Health. 2017;1:e381-e388.
- Thiel C, Duncan P, Woods N. Attitude of US obstetricians and gynaecologists to global warming and medical waste. J Health Serv Res Policy. 2017;22:162-167.
- Siu J, Hill AG, MacCormick AD. Systematic review of reusable versus disposable laparoscopic instruments: costs and safety. ANZ J Surg. 2017;87:28-33.
- Ryan SM, Nielsen CJ. Global warming potential of inhaled anesthetics: application to clinical use. Anesth Analg. 2010;111:92-98.
- Meyer MJ. Desflurane should des-appear: global and financial rationale. Anesth Analg. 2020;131:1317-1322.
- Rollins MD, Arendt KW, Carvalho B, et al. ASA Committee on Obstetric Anesthesia Working Group. Nitrous oxide. American Society of Anesthesiologists website. Accessed May 12, 2023. https://www .asahq.org/about-asa/governance-and-committees/asa-committees /committee-on-obstetric-anesthesia/nitrous-oxide.
- Kalogera E, Dowdy SC. Enhanced recovery pathway in gynecologic surgery: improving outcomes through evidence-based medicine. Obstet Gynecol Clin North Am. 2016;43:551-573.
- Zota AR, Geller RJ, Calafat AM, et al. Phthalates exposure and uterine fibroid burden among women undergoing surgical treatment for fibroids: a preliminary study. Fertil Steril. 2019;111:112-121.
- Bommartio PA, Ferguson KK, Meeker JD, et al. Maternal levels of perfluoroalkyl substances (PFAS) during early pregnancy in relation to preeclampsia subtypes and biomarkers of preeclampsia risk. Environ Health Perspect. 2021;129:107004.
- Azouz S, Boyll P, Swanson M, et al. Managing barriers to recycling in the operating room. Am J Surg. 2019;217:634-638.
- Watts N, Amann M, Arnell N, et al. The 2020 report of The Lancet Countdown on health and climate change: responding to converging crises. Lancet. 2021;397:129-170.
- Ryan EC, Dubrow R, Sherman JD. Medical, nursing, and physician assistant student knowledge and attitudes toward climate change, pollution, and resource conservation in health care. BMC Med Educ. 2020;20:200.
- Giudice LC, Llamas-Clark EF, DeNicola Net al; FIGO Committee on Climate Change and Toxic Environmental Exposures. Climate change, women’s health, and the role of obstetricians and gynecologists in leadership. Int J Gynaecol Obstet. 2021;155:345-356.
- Yates EF, Bowder AN, Roa L, et al. Empowering surgeons, anesthesiologists, and obstetricians to incorporate environmental sustainability in the operating room. Ann Surg. 2021;273:1108-1114.
- Costello A, Abbas M, Allen et al. Managing the health effects of climate change: Lancet and University College London Institute for Global Health Commission. Lancet. 2009;373:1693-1733.
- Health care climate footprint report. Health Care Without Harm website. https://www.noharm.org/ClimateFootprintReport. Accessed May 12, 2023.
- Balbus JM, McCannon CJ, Mataka A, et al. After COP26—putting health and equity at the center of the climate movement. N Engl J Med. 2022;386:1295-1297.
- Bekkar B, Pacheco S, Basu R, et al. Association of air pollution and heat exposure with preterm birth, low birth weight, and stillbirth in the US: a systematic review. JAMA Netw Open. 2020;3:e208243.
- Genco M, Anderson-Shaw L, Sargis RM. Unwitting accomplices: endocrine disruptors confounding clinical care. J Clin Endocrinol Metab. 2020;105:e3822-e3827.
- Al-Kindi SG, Sarode A, Zullo M, et al. Ambient air pollution and mortality after cardiac transplantation. J Am Coll Cardiol. 2019;74:30263035.
- Ghosh R, Gauderman WJ, Minor H, et al. Air pollution, weight loss and metabolic benefits of bariatric surgery: a potential model for study of metabolic effects of environmental exposures. Pediatr Obes. 2018;13:312-320.
- Thiel CL, Eckelman M, Guido R, et al. Environmental impacts of surgical procedures: life cycle assessment of hysterectomy in the United States. Environ Sci Technol. 2015;49:1779-1786.
- Zygourakis CC, Yoon S, Valencia V, et al. Operating room waste: disposable supply utilization in neurosurgical procedures. J Neurosurg. 2017;126:620-625.
- van Demark RE, Smith VJS, Fiegen A. Lean and green hand surgery. J Hand Surg. 2018;43:179-181.
- Campion N, Thiel CL, DeBlois J, et al. Life cycle assessment perspectives on delivering an infant in the US. Sci Total Environ. 2012;425:191198.
- Hsu S, Thiel CL, Mello MJ, Slutzman JE. Dumpster diving in the emergency department. West J Emerg Med. 2020;21:1211-1217.
- Mcgain F, Story D, Hendel S. An audit of intensive care unit recyclable waste. Anaesthesia. 2009;64:1299-1302.
- Wormer BA, Augenstein VA, Carpenter CL, et al. The green operating room: simple changes to reduce cost and our carbon footprint. Am Surg. 2013;79:666-671.
- Kagoma Y, Stall N, Rubinstein E, et al. People, planet and profits: the case for greening operating rooms. Can Med Assoc J. 2012;184:19051911.
- McCarthy CJ, Gerstenmaier JF, O’ Neill AC, et al. “EcoRadiology”— pulling the plug on wasted energy in the radiology department. Acad Radiol. 2014;21:1563-1566.
- Donahue LM, Hilton S, Bell SG, et al. A comparative carbon footprint analysis of disposable and reusable vaginal specula. Am J Obstet Gynecol. 2020;223:225.e1-225.e7.
- Rodriguez Morris MI, Hicks A. Life cycle assessment of stainless-steel reusable speculums versus disposable acrylic speculums in a university clinic setting: a case study. Environ Res Commun. 2022;4:025002.
- MacNeill AJ, Lillywhite R, Brown CJ. The impact of surgery on global climate: a carbon footprinting study of operating theatres in three health systems. Lancet Planet Health. 2017;1:e381-e388.
- Thiel C, Duncan P, Woods N. Attitude of US obstetricians and gynaecologists to global warming and medical waste. J Health Serv Res Policy. 2017;22:162-167.
- Siu J, Hill AG, MacCormick AD. Systematic review of reusable versus disposable laparoscopic instruments: costs and safety. ANZ J Surg. 2017;87:28-33.
- Ryan SM, Nielsen CJ. Global warming potential of inhaled anesthetics: application to clinical use. Anesth Analg. 2010;111:92-98.
- Meyer MJ. Desflurane should des-appear: global and financial rationale. Anesth Analg. 2020;131:1317-1322.
- Rollins MD, Arendt KW, Carvalho B, et al. ASA Committee on Obstetric Anesthesia Working Group. Nitrous oxide. American Society of Anesthesiologists website. Accessed May 12, 2023. https://www .asahq.org/about-asa/governance-and-committees/asa-committees /committee-on-obstetric-anesthesia/nitrous-oxide.
- Kalogera E, Dowdy SC. Enhanced recovery pathway in gynecologic surgery: improving outcomes through evidence-based medicine. Obstet Gynecol Clin North Am. 2016;43:551-573.
- Zota AR, Geller RJ, Calafat AM, et al. Phthalates exposure and uterine fibroid burden among women undergoing surgical treatment for fibroids: a preliminary study. Fertil Steril. 2019;111:112-121.
- Bommartio PA, Ferguson KK, Meeker JD, et al. Maternal levels of perfluoroalkyl substances (PFAS) during early pregnancy in relation to preeclampsia subtypes and biomarkers of preeclampsia risk. Environ Health Perspect. 2021;129:107004.
- Azouz S, Boyll P, Swanson M, et al. Managing barriers to recycling in the operating room. Am J Surg. 2019;217:634-638.
- Watts N, Amann M, Arnell N, et al. The 2020 report of The Lancet Countdown on health and climate change: responding to converging crises. Lancet. 2021;397:129-170.
- Ryan EC, Dubrow R, Sherman JD. Medical, nursing, and physician assistant student knowledge and attitudes toward climate change, pollution, and resource conservation in health care. BMC Med Educ. 2020;20:200.
- Giudice LC, Llamas-Clark EF, DeNicola Net al; FIGO Committee on Climate Change and Toxic Environmental Exposures. Climate change, women’s health, and the role of obstetricians and gynecologists in leadership. Int J Gynaecol Obstet. 2021;155:345-356.
- Yates EF, Bowder AN, Roa L, et al. Empowering surgeons, anesthesiologists, and obstetricians to incorporate environmental sustainability in the operating room. Ann Surg. 2021;273:1108-1114.
Addressing OR sustainability: How we can decrease waste and emissions
In 2009, the Lancet called climate change the biggest global health threat of the 21st century, the effects of which will be experienced in our lifetimes.1 Significant amounts of data have demonstrated the negative health effects of heat, air pollution, and exposure to toxic substances.2,3 These effects have been seen in every geographic region of the United States, and in multiple organ systems and specialties, including obstetrics, pediatrics, and even cardiopulmonary and bariatric surgery.2-5
Although it does not receive the scrutiny of other industries, the global health care industry accounts for almost double the amount of carbon emissions as global aviation, and the United States accounts for 27% of this footprint despite only having 4% of the world’s population.6 It therefore serves that our own industry is an excellent target for reducing the carbon emissions that contribute to climate change. Consider the climate impact of hysterectomy, the second-most common surgery that women undergo. In this article, we will use the example of a 50-year-old woman with fibroids who plans to undergo definitive treatment via total laparoscopic hysterectomy (TLH).
Climate impact of US health care
Hospital buildings in the United States are energy intensive, consuming 10% of the energy used in commercial buildings every year, accounting for over $8 billion. Operating rooms (ORs) account for a third of this usage.7 Hospitals also use more water than any other type of commercial building, for necessary actions like cooling, sterilization, and laundry.8 Further, US hospitals generate 14,000 tons of waste per day, with a third of this coming from the ORs. Sadly, up to 15% is food waste, as we are not very good about selecting and proportioning healthy food for our staff and inpatients.6
While health care is utility intensive, the majority of emissions are created through the production, transport, and disposal of goods coming through our supply chain.6 Hospitals are significant consumers of single-use objects, the majority of which are petroleum-derived plastics—accounting for an estimated 71% of emissions coming from the health care sector. Supply chain is the second largest expense in health care, but with current shortages, it is estimated to overtake labor costs by this year. The United States is also the largest consumer of pharmaceuticals worldwide, supporting a $20 billion packaging industry,9 which creates a significant amount of waste.
Climate impact of the OR
Although ORs only account for a small portion of hospital square footage, they account for a significant amount of health care’s carbon footprint through high waste production and excessive consumption of single-use items. Just one surgical procedure in a hospital is estimated to produce about the same amount of waste as a typical family of 4 would in an entire week.10 Furthermore, the majority of these single-use items, including sterile packaging, are sorted inappropriately as regulated medical waste (RMW, “biohazardous” or “red bag” waste) (FIGURE 1a). RMW has significant effects on the environment since it must be incinerated or steam autoclaved prior to transport to the landfill, leading to high amounts of air pollution and energy usage.
We all notice the visible impacts of waste in the OR, but other contributors to carbon emissions are invisible. Energy consumption is a huge contributor to the overall carbon footprint of surgery. Heating, ventilation, and air conditioning [HVAC] is responsible for 52% of hospital energy needs but accounts for 99% of OR energy consumption.11 Despite the large energy requirements of the ORs, they are largely unoccupied in the evenings and on weekends, and thermostats are not adjusted accordingly.
Anesthetic gases are another powerful contributor to greenhouse gas emissions from the OR. Anesthetic gases alone contribute about 25% of the overall carbon footprint of the OR, and US health care emits 660,000 tons of carbon equivalents from anesthetic gas use per year.12 Desflurane is 1,600 times more potent than carbon dioxide (CO2) in its global warming potential followed by isoflurane and sevoflurane;13 this underscores the importance of working with our anesthesia colleagues on the differences between the anesthetic gases they use. Enhanced recovery after surgery recommendations in gynecology already recommend avoiding the use of volatile anesthetic gases in favor of propofol to reduce postoperative nausea and vomiting.14
In the context of a patient undergoing a TLH, the estimated carbon footprint in the United States is about 560 kg of CO2 equivalents—roughly the same as driving 1,563 miles in a gas-powered car.
Continue to: Climate impact on our patients...
Climate impact on our patients
The data in obstetrics and gynecology is clear that climate change is affecting patient outcomes, both globally and in our own country. A systematic review of 32 million births found that air pollution and heat exposure were associated with preterm birth and low birth weight, and these effects were seen in all geographic regions across the United States.1 A study of 5.9 million births in California found that patients who lived near coal- and oil-power plants had up to a 27% reduction in preterm births when those power plants closed and air pollution decreased.15 A study in Nature Sustainability on 250,000 pregnancies that ended in missed abortions at 14 weeks or less found the odds ratio of missed abortion increased with the cumulative exposure to air pollution.16 When air pollution was examined in comparison to other factors, neighborhood air pollution better predicted preterm birth, very preterm birth, and small for gestational age more than race, ethnicity, or any other socio-economic factor.17 The effects of air pollution have been demonstrated in other fields as well, including increased mortality after cardiac transplantation with exposure to air pollution,4 and for patients undergoing bariatric surgery who live near major roadways, decreased weight loss, less improvement in hemoglobin A1c, and less change in lipids compared with those with less exposure to roadway pollution.5
Air pollution and heat are not the only factors that influence health. Endocrine disrupting chemicals (EDCs) and single-use plastic polymers, which are used in significant supply in US health care, have been found in human blood,18 intestine, and all portions of the placenta.19 Phthalates, an EDC found in medical use plastics and medications to control delivery, have been associated with increasing fibroid burden in patients undergoing hysterectomy and myomectomy.20 The example case patient with fibroids undergoing TLH may have had her condition worsened by exposure to phthalates.
Specific areas for improvement
There is a huge opportunity for improvement to reduce the total carbon footprint of a TLH.
A lifecycle assessment of hysterectomy in the United States concluded that an 80% reduction in carbon emissions could be achieved by minimizing opened materials, using reusable and reprocessed instruments, reducing off-hour energy use in the OR (HVAC setbacks), and avoiding the use of volatile anesthetic gases.21 The sterilization and re-processing of reusable instruments represented the smallest proportion of carbon emissions from a TLH. Data on patient safety supports these interventions, as current practices have more to do with hospital culture and processes than evidence.
Despite a push to use single-use objects by industry and regulatory agencies in the name of patient safety, data demonstrate that single-use objects are in actuality not safer for patients and may be associated with increased surgical site infections (SSIs). A study from a cancer center in California found that when single-use head covers, shoe covers, and facemasks were eliminated due to supply shortages during the pandemic, SSIs went down by half, despite an increase in surgical volume and an increase in the number of contaminated cases.22 The authors reported an increase in hand hygiene throughout the hospital, which likely contributed to the success of reducing SSIs.
Similarly, a systematic review found no evidence to support single-use instruments over reusable or reprocessed instruments when considering instrument function, ease of use, patient safety, SSIs, or long-term patient outcomes.23 While it may be easy for regulatory agencies to focus on disposing objects as paramount to reducing infections, the Centers for Disease Control and Prevention states that the biggest factors affecting SSIs are appropriate use of prophylactic antibiotics, skin antisepsis, and patient metabolic control.24 Disposing of single-use objects in the name of patient safety will worsen patient health outcomes when considering patient proximity to waste, pollution, and EDCs.
The sterilization process for reusable items is often called out by the medical supply industry as wasteful and energy intensive; however, data refute these claims. A Swedish study researching reusable versus single-use trocars found that a reusable trocar system offers a robust opportunity to reduce both the environmental and financial costs for laparoscopic surgery.25 We can further decrease the environmental impact of reusable instruments by using sets instead of individually packed instruments and packing autoclaves more efficiently. By using rigid sterilization containers, there was an 85% reduction in carbon footprint as compared with the blue wrap system.
Electricity use can be easily reduced across all surgical spaces by performing HVAC setbacks during low occupancy times of day. On nights and weekends, when there are very few surgical cases occurring, one study found that by decreasing the ventilation rate, turning off lights, and performing the minimum temperature control in unused ORs, electricity use was cut in half.11
Waste triage and recycling
Reducing regulated medical waste is another area where hospitals can make a huge impact on carbon emissions and costs with little more than education and process change. Guidelines for regulated medical waste sorting developed out of the HIV epidemic due to the fear of blood products. Although studies show that regulated medical waste is not more infectious than household waste, state departments of public health have kept these guidelines in place for sorting fluid blood and tissue into RMW containers and bags.26 The best hospital performers keep RMW below 10% of the total waste stream, while many ORs send close to 100% of their waste as RMW (FIGURE 1b). ORs can work with nursing and environmental services staff to assess processes and divert waste into recycling and regular waste. Many OR staff are acutely aware of the huge amount of waste produced and want to make a positive impact. Success in this small area often builds momentum to tackle harder sustainability practices throughout the hospital.
Continue to: Removal of EDCs from medical products...
Removal of EDCs from medical products
Single-use medical supplies are not only wasteful but also contain harmful EDCs, such as phthalates, bisphenol A (BPA), parabens, perfluoroalkyl substances, and triclosan. Phthalates, for example, account for 30% to 40% of the weight of medical-use plastics, and parabens are ubiquitously found in ultrasound gel.3 Studies looking at exposure to EDCs within the neonatal intensive care unit reveal substantial BPA, phthalate, and paraben levels within biologic samples from premature infants, thought to be above toxicity limits. While we do not know the full extent to which EDCs can affect neonatal development, there is already mounting evidence that EDCs are associated with endocrine, metabolic, and neurodevelopmental disorders throughout our lifespan.3
30-day climate challenge
Although the example case patient undergoing TLH for fibroids will never need care for her fibroids again, the climate impact of her time in the OR represents the most carbon-intensive care she will ever need. Surgery as practiced in the United States today is unsustainable.
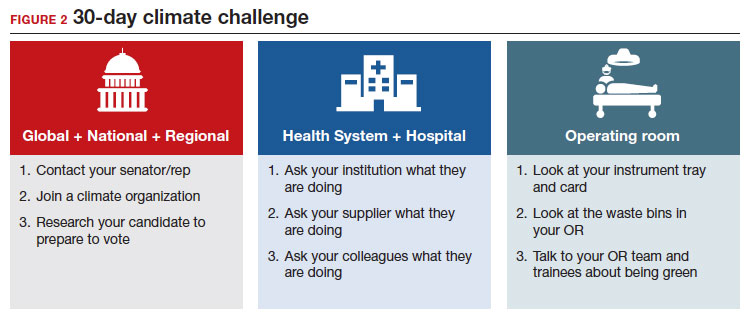
In 2021, the Biden administration issued an executive order requiring all federal facilities, including health care facilities and hospitals, to be carbon neutral by 2035. In order to make meaningful changes industry-wide, we should be petitioning lawmakers for stricter environmental regulations in health care, similar to regulations in the manufacturing and airline industries. We recommend a 30-day climate challenge (FIGURE 2) for bringing awareness to your circles of influence. Physicians have an ethical duty to advocate for change at the local, regional, and national level if we want to see a better future for our patients, their children, and even ourselves. Organizations such as Practice Greenhealth, Health Care without Harm, and Citizens’ Climate Lobby can help amplify our voices to reach the right people to implement sweeping policy changes. ●
- Costello A, Abbas M, Allen et al. Managing the health effects of climate change: Lancet and University College London Institute for Global Health Commission. Lancet. 2009;373:1693-1733. doi: 10.1016/S0140-6736(09)60935-1.
- Bekkar B, Pacheco S, Basu R, et al. Association of air pollution and heat exposure with preterm birth, low birth weight, and stillbirth in the US: a systematic review. JAMA Netw Open. 2020;3. doi:10.1001/JAMANETWORKOPEN.2020.8243.
- Genco M, Anderson-Shaw L, Sargis RM. Unwitting accomplices: endocrine disruptors confounding clinical care. J Clin Endocrinol Metab. 2020;105:e3822–7. doi: 10.1210/cline2. m/dgaa358.
- Al-Kindi SG, Sarode A, Zullo M, et al. Ambient air pollution and mortality after cardiac transplantation. J Am Coll Cardiol. 2019;74:3026-3035. doi: 10.1016/j.jacc.2019.09.066.
- Ghosh R, Gauderman WJ, Minor H, et al. Air pollution, weight loss and metabolic benefits of bariatric surgery: a potential model for study of metabolic effects of environmental exposures. Pediatr Obes. 2018;13:312-320. doi: 10.1111/ijpo.12210.
- Health Care’s Climate Footprint. Health care without harm climate-smart health care series, Green Paper Number one. September 2019. https://www.noharm.org/
ClimateFootprintReport. Accessed December 11, 2022. - Healthcare Energy End-Use Monitoring. US Department of Energy. https://www.energy.gov/eere/
buildings/downloads/ healthcare-energy-end-use- monitoring. Accessed December 11, 2022. - 2012 Commercial Buildings Energy Consumption Survey: Water Consumption in Large Buildings Summary. U.S Energy Information Administration. https://www.eia.gov/
consumption/commercial/ reports/2012/water. Accessed December 11, 2022. - Belkhir L, Elmeligi A. Carbon footprint of the global pharmaceutical industry and relative implact of its major players. J Cleaner Production. 2019;214:185-194. doi: 10.1016 /j.jclearpro.2019.11.204.
- Esaki RK, Macario A. Wastage of Supplies and Drugs in the Operating Room. 2015:8-13.
- MacNeill AJ, et al. The Impact of Surgery on Global Climate: A Carbon Footprinting Study of Operating Theatres in Three Health Systems. Lancet Planet Health.2017;1:e360–367. doi:10.1016/S2542-5196(17)30162-6.
- Shoham MA, Baker NM, Peterson ME, et al. The environmental impact of surgery: a systematic review. 2022;172:897-905. doi:10.1016/j.surg.2022.04.010.
- Ryan SM, Nielsen CJ. Global warming potential of inhaled anesthetics: application to clinical use. Anesth Analg. 2010;111:92-98. doi:10.1213/ANE.0B013E3181E058D7.
- Kalogera E, Dowdy SC. Enhanced recovery pathway in gynecologic surgery: improving outcomes through evidence-based medicine. Obstet Gynecol Clin North Am. 2016;43:551-573. doi: 10.1016/j.ogc.2016.04.006.
- Casey JA, Karasek D, Ogburn EL, et al. Retirements of coal and oil power plants in California: association with reduced preterm birth among populations nearby. Am J Epidemiol. 2018;187:1586-1594. doi: 10.1093/aje/kwy110.
- Zhang L, Liu W, Hou K, et al. Air pollution-induced missed abortion risk for pregnancies. Nat Sustain. 2019:1011–1017.
- Benmarhnia T, Huang J, Basu R, et al. Decomposition analysis of Black-White disparities in birth outcomes: the relative contribution of air pollution and social factors in California. Environ Health Perspect. 2017;125:107003. doi: 10.1289/EHP490.
- Leslie HA, van Velzen MJM, Brandsma SH, et al. Discovery and quantification of plastic particle pollution in human blood. Environ Int. 2022;163:107199. doi: 10.1016/j.envint.2022.107199.
- Ragusa A, Svelato A, Santacroce C, et al. Plasticenta: first evidence of microplastics in human placenta. Environ Int. 2021;146:106274. doi: 10.1016/j.envint.2020.106274.
- Zota AR, Geller RJ, Calafat AM, et al. Phthalates exposure and uterine fibroid burden among women undergoing surgical treatment for fibroids: a preliminary study. Fertil Steril. 2019;111:112-121. doi: 10.1016/j.fertnstert.2018.09.009.
- Thiel CL, Eckelman M, Guido R, et al. Environmental impacts of surgical procedures: life cycle assessment of hysterectomy in the United States. Environ Sci Technol. 2015;49:1779-1786. doi: 10.1021/es504719g.
- Malhotra GK, Tran T, Stewart C, et al. Pandemic operating room supply shortage and surgical site infection: considerations as we emerge from the Coronavirus Disease 2019 Pandemic. J Am Coll Surg. 2022;234:571-578. doi: 10.1097/XCS.0000000000000087.
- Siu J, Hill AG, MacCormick AD. Systematic review of reusable versus disposable laparoscopic instruments: costs and safety. ANZ J Surg. 2017;87:28-33. doi:10.1111/ANS.13856.
- Berríos-Torres SI, Umscheid CA, Bratzler DW, et al; Healthcare Infection Control Practices Advisory Committee. Centers for Disease Control and Prevention Guideline for the Prevention of Surgical Site Infection, 2017 [published correction appears in: JAMA Surg. 2017;152:803]. JAMA Surg. 2017;152:784-791. doi: 10.1001/jamasurg.2017.0904.
- Rizan, Chantelle, Lillywhite, et al. Minimising carbon and financial costs of steam sterilisation and packaging of reusable surgical instruments. Br J Surg. 2022;109:200-210. doi:10.1093/BJS/ZNAB406.
- Sustainability Benchmarking Report, 2010. Practice Greenhealth. https://www.practicegreenhealth.org. Accessed December 11, 2022.
In 2009, the Lancet called climate change the biggest global health threat of the 21st century, the effects of which will be experienced in our lifetimes.1 Significant amounts of data have demonstrated the negative health effects of heat, air pollution, and exposure to toxic substances.2,3 These effects have been seen in every geographic region of the United States, and in multiple organ systems and specialties, including obstetrics, pediatrics, and even cardiopulmonary and bariatric surgery.2-5
Although it does not receive the scrutiny of other industries, the global health care industry accounts for almost double the amount of carbon emissions as global aviation, and the United States accounts for 27% of this footprint despite only having 4% of the world’s population.6 It therefore serves that our own industry is an excellent target for reducing the carbon emissions that contribute to climate change. Consider the climate impact of hysterectomy, the second-most common surgery that women undergo. In this article, we will use the example of a 50-year-old woman with fibroids who plans to undergo definitive treatment via total laparoscopic hysterectomy (TLH).
Climate impact of US health care
Hospital buildings in the United States are energy intensive, consuming 10% of the energy used in commercial buildings every year, accounting for over $8 billion. Operating rooms (ORs) account for a third of this usage.7 Hospitals also use more water than any other type of commercial building, for necessary actions like cooling, sterilization, and laundry.8 Further, US hospitals generate 14,000 tons of waste per day, with a third of this coming from the ORs. Sadly, up to 15% is food waste, as we are not very good about selecting and proportioning healthy food for our staff and inpatients.6
While health care is utility intensive, the majority of emissions are created through the production, transport, and disposal of goods coming through our supply chain.6 Hospitals are significant consumers of single-use objects, the majority of which are petroleum-derived plastics—accounting for an estimated 71% of emissions coming from the health care sector. Supply chain is the second largest expense in health care, but with current shortages, it is estimated to overtake labor costs by this year. The United States is also the largest consumer of pharmaceuticals worldwide, supporting a $20 billion packaging industry,9 which creates a significant amount of waste.
Climate impact of the OR
Although ORs only account for a small portion of hospital square footage, they account for a significant amount of health care’s carbon footprint through high waste production and excessive consumption of single-use items. Just one surgical procedure in a hospital is estimated to produce about the same amount of waste as a typical family of 4 would in an entire week.10 Furthermore, the majority of these single-use items, including sterile packaging, are sorted inappropriately as regulated medical waste (RMW, “biohazardous” or “red bag” waste) (FIGURE 1a). RMW has significant effects on the environment since it must be incinerated or steam autoclaved prior to transport to the landfill, leading to high amounts of air pollution and energy usage.
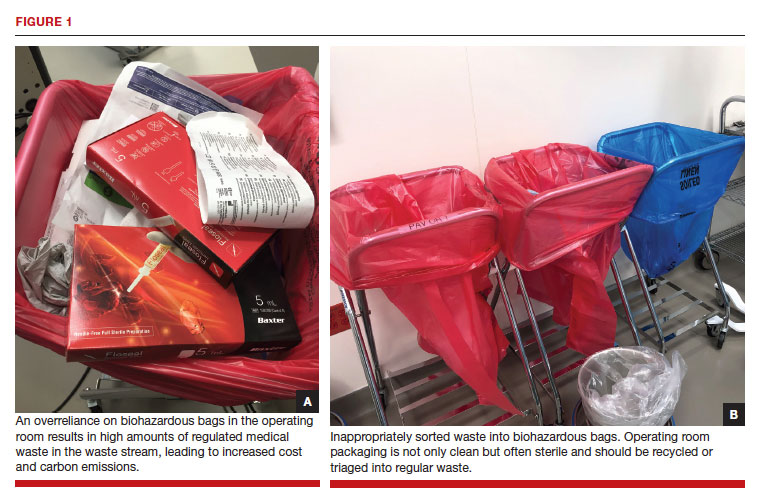
We all notice the visible impacts of waste in the OR, but other contributors to carbon emissions are invisible. Energy consumption is a huge contributor to the overall carbon footprint of surgery. Heating, ventilation, and air conditioning [HVAC] is responsible for 52% of hospital energy needs but accounts for 99% of OR energy consumption.11 Despite the large energy requirements of the ORs, they are largely unoccupied in the evenings and on weekends, and thermostats are not adjusted accordingly.
Anesthetic gases are another powerful contributor to greenhouse gas emissions from the OR. Anesthetic gases alone contribute about 25% of the overall carbon footprint of the OR, and US health care emits 660,000 tons of carbon equivalents from anesthetic gas use per year.12 Desflurane is 1,600 times more potent than carbon dioxide (CO2) in its global warming potential followed by isoflurane and sevoflurane;13 this underscores the importance of working with our anesthesia colleagues on the differences between the anesthetic gases they use. Enhanced recovery after surgery recommendations in gynecology already recommend avoiding the use of volatile anesthetic gases in favor of propofol to reduce postoperative nausea and vomiting.14
In the context of a patient undergoing a TLH, the estimated carbon footprint in the United States is about 560 kg of CO2 equivalents—roughly the same as driving 1,563 miles in a gas-powered car.
Continue to: Climate impact on our patients...
Climate impact on our patients
The data in obstetrics and gynecology is clear that climate change is affecting patient outcomes, both globally and in our own country. A systematic review of 32 million births found that air pollution and heat exposure were associated with preterm birth and low birth weight, and these effects were seen in all geographic regions across the United States.1 A study of 5.9 million births in California found that patients who lived near coal- and oil-power plants had up to a 27% reduction in preterm births when those power plants closed and air pollution decreased.15 A study in Nature Sustainability on 250,000 pregnancies that ended in missed abortions at 14 weeks or less found the odds ratio of missed abortion increased with the cumulative exposure to air pollution.16 When air pollution was examined in comparison to other factors, neighborhood air pollution better predicted preterm birth, very preterm birth, and small for gestational age more than race, ethnicity, or any other socio-economic factor.17 The effects of air pollution have been demonstrated in other fields as well, including increased mortality after cardiac transplantation with exposure to air pollution,4 and for patients undergoing bariatric surgery who live near major roadways, decreased weight loss, less improvement in hemoglobin A1c, and less change in lipids compared with those with less exposure to roadway pollution.5
Air pollution and heat are not the only factors that influence health. Endocrine disrupting chemicals (EDCs) and single-use plastic polymers, which are used in significant supply in US health care, have been found in human blood,18 intestine, and all portions of the placenta.19 Phthalates, an EDC found in medical use plastics and medications to control delivery, have been associated with increasing fibroid burden in patients undergoing hysterectomy and myomectomy.20 The example case patient with fibroids undergoing TLH may have had her condition worsened by exposure to phthalates.
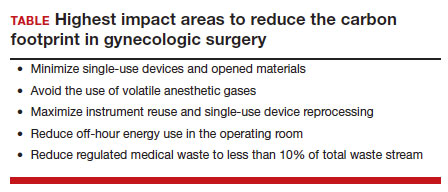
Specific areas for improvement
There is a huge opportunity for improvement to reduce the total carbon footprint of a TLH.
A lifecycle assessment of hysterectomy in the United States concluded that an 80% reduction in carbon emissions could be achieved by minimizing opened materials, using reusable and reprocessed instruments, reducing off-hour energy use in the OR (HVAC setbacks), and avoiding the use of volatile anesthetic gases.21 The sterilization and re-processing of reusable instruments represented the smallest proportion of carbon emissions from a TLH. Data on patient safety supports these interventions, as current practices have more to do with hospital culture and processes than evidence.
Despite a push to use single-use objects by industry and regulatory agencies in the name of patient safety, data demonstrate that single-use objects are in actuality not safer for patients and may be associated with increased surgical site infections (SSIs). A study from a cancer center in California found that when single-use head covers, shoe covers, and facemasks were eliminated due to supply shortages during the pandemic, SSIs went down by half, despite an increase in surgical volume and an increase in the number of contaminated cases.22 The authors reported an increase in hand hygiene throughout the hospital, which likely contributed to the success of reducing SSIs.
Similarly, a systematic review found no evidence to support single-use instruments over reusable or reprocessed instruments when considering instrument function, ease of use, patient safety, SSIs, or long-term patient outcomes.23 While it may be easy for regulatory agencies to focus on disposing objects as paramount to reducing infections, the Centers for Disease Control and Prevention states that the biggest factors affecting SSIs are appropriate use of prophylactic antibiotics, skin antisepsis, and patient metabolic control.24 Disposing of single-use objects in the name of patient safety will worsen patient health outcomes when considering patient proximity to waste, pollution, and EDCs.
The sterilization process for reusable items is often called out by the medical supply industry as wasteful and energy intensive; however, data refute these claims. A Swedish study researching reusable versus single-use trocars found that a reusable trocar system offers a robust opportunity to reduce both the environmental and financial costs for laparoscopic surgery.25 We can further decrease the environmental impact of reusable instruments by using sets instead of individually packed instruments and packing autoclaves more efficiently. By using rigid sterilization containers, there was an 85% reduction in carbon footprint as compared with the blue wrap system.
Electricity use can be easily reduced across all surgical spaces by performing HVAC setbacks during low occupancy times of day. On nights and weekends, when there are very few surgical cases occurring, one study found that by decreasing the ventilation rate, turning off lights, and performing the minimum temperature control in unused ORs, electricity use was cut in half.11
Waste triage and recycling
Reducing regulated medical waste is another area where hospitals can make a huge impact on carbon emissions and costs with little more than education and process change. Guidelines for regulated medical waste sorting developed out of the HIV epidemic due to the fear of blood products. Although studies show that regulated medical waste is not more infectious than household waste, state departments of public health have kept these guidelines in place for sorting fluid blood and tissue into RMW containers and bags.26 The best hospital performers keep RMW below 10% of the total waste stream, while many ORs send close to 100% of their waste as RMW (FIGURE 1b). ORs can work with nursing and environmental services staff to assess processes and divert waste into recycling and regular waste. Many OR staff are acutely aware of the huge amount of waste produced and want to make a positive impact. Success in this small area often builds momentum to tackle harder sustainability practices throughout the hospital.
Continue to: Removal of EDCs from medical products...
Removal of EDCs from medical products
Single-use medical supplies are not only wasteful but also contain harmful EDCs, such as phthalates, bisphenol A (BPA), parabens, perfluoroalkyl substances, and triclosan. Phthalates, for example, account for 30% to 40% of the weight of medical-use plastics, and parabens are ubiquitously found in ultrasound gel.3 Studies looking at exposure to EDCs within the neonatal intensive care unit reveal substantial BPA, phthalate, and paraben levels within biologic samples from premature infants, thought to be above toxicity limits. While we do not know the full extent to which EDCs can affect neonatal development, there is already mounting evidence that EDCs are associated with endocrine, metabolic, and neurodevelopmental disorders throughout our lifespan.3
30-day climate challenge
Although the example case patient undergoing TLH for fibroids will never need care for her fibroids again, the climate impact of her time in the OR represents the most carbon-intensive care she will ever need. Surgery as practiced in the United States today is unsustainable.
In 2021, the Biden administration issued an executive order requiring all federal facilities, including health care facilities and hospitals, to be carbon neutral by 2035. In order to make meaningful changes industry-wide, we should be petitioning lawmakers for stricter environmental regulations in health care, similar to regulations in the manufacturing and airline industries. We recommend a 30-day climate challenge (FIGURE 2) for bringing awareness to your circles of influence. Physicians have an ethical duty to advocate for change at the local, regional, and national level if we want to see a better future for our patients, their children, and even ourselves. Organizations such as Practice Greenhealth, Health Care without Harm, and Citizens’ Climate Lobby can help amplify our voices to reach the right people to implement sweeping policy changes. ●
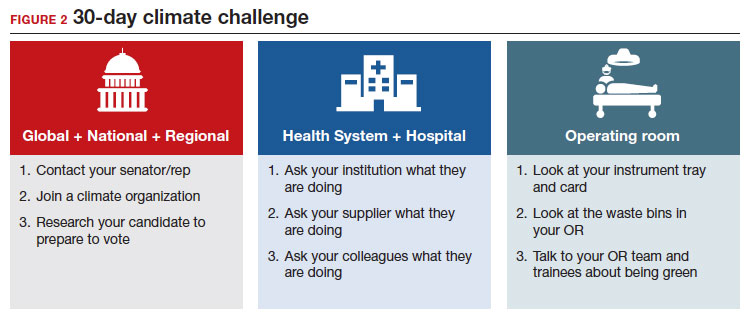
In 2009, the Lancet called climate change the biggest global health threat of the 21st century, the effects of which will be experienced in our lifetimes.1 Significant amounts of data have demonstrated the negative health effects of heat, air pollution, and exposure to toxic substances.2,3 These effects have been seen in every geographic region of the United States, and in multiple organ systems and specialties, including obstetrics, pediatrics, and even cardiopulmonary and bariatric surgery.2-5
Although it does not receive the scrutiny of other industries, the global health care industry accounts for almost double the amount of carbon emissions as global aviation, and the United States accounts for 27% of this footprint despite only having 4% of the world’s population.6 It therefore serves that our own industry is an excellent target for reducing the carbon emissions that contribute to climate change. Consider the climate impact of hysterectomy, the second-most common surgery that women undergo. In this article, we will use the example of a 50-year-old woman with fibroids who plans to undergo definitive treatment via total laparoscopic hysterectomy (TLH).
Climate impact of US health care
Hospital buildings in the United States are energy intensive, consuming 10% of the energy used in commercial buildings every year, accounting for over $8 billion. Operating rooms (ORs) account for a third of this usage.7 Hospitals also use more water than any other type of commercial building, for necessary actions like cooling, sterilization, and laundry.8 Further, US hospitals generate 14,000 tons of waste per day, with a third of this coming from the ORs. Sadly, up to 15% is food waste, as we are not very good about selecting and proportioning healthy food for our staff and inpatients.6
While health care is utility intensive, the majority of emissions are created through the production, transport, and disposal of goods coming through our supply chain.6 Hospitals are significant consumers of single-use objects, the majority of which are petroleum-derived plastics—accounting for an estimated 71% of emissions coming from the health care sector. Supply chain is the second largest expense in health care, but with current shortages, it is estimated to overtake labor costs by this year. The United States is also the largest consumer of pharmaceuticals worldwide, supporting a $20 billion packaging industry,9 which creates a significant amount of waste.
Climate impact of the OR
Although ORs only account for a small portion of hospital square footage, they account for a significant amount of health care’s carbon footprint through high waste production and excessive consumption of single-use items. Just one surgical procedure in a hospital is estimated to produce about the same amount of waste as a typical family of 4 would in an entire week.10 Furthermore, the majority of these single-use items, including sterile packaging, are sorted inappropriately as regulated medical waste (RMW, “biohazardous” or “red bag” waste) (FIGURE 1a). RMW has significant effects on the environment since it must be incinerated or steam autoclaved prior to transport to the landfill, leading to high amounts of air pollution and energy usage.
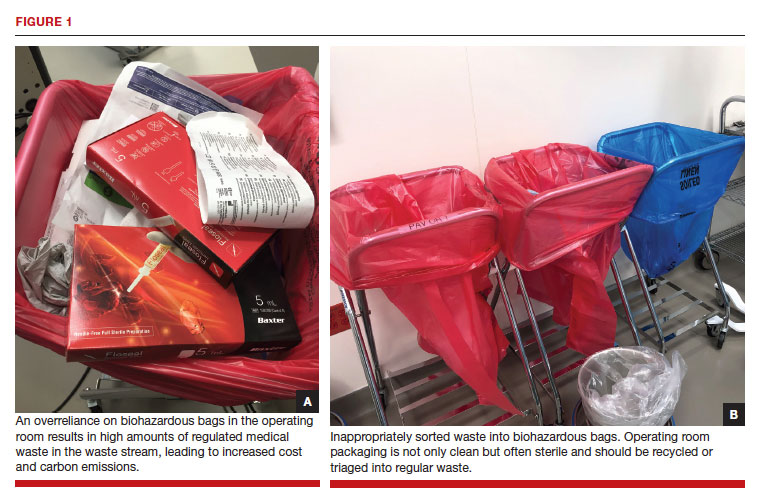
We all notice the visible impacts of waste in the OR, but other contributors to carbon emissions are invisible. Energy consumption is a huge contributor to the overall carbon footprint of surgery. Heating, ventilation, and air conditioning [HVAC] is responsible for 52% of hospital energy needs but accounts for 99% of OR energy consumption.11 Despite the large energy requirements of the ORs, they are largely unoccupied in the evenings and on weekends, and thermostats are not adjusted accordingly.
Anesthetic gases are another powerful contributor to greenhouse gas emissions from the OR. Anesthetic gases alone contribute about 25% of the overall carbon footprint of the OR, and US health care emits 660,000 tons of carbon equivalents from anesthetic gas use per year.12 Desflurane is 1,600 times more potent than carbon dioxide (CO2) in its global warming potential followed by isoflurane and sevoflurane;13 this underscores the importance of working with our anesthesia colleagues on the differences between the anesthetic gases they use. Enhanced recovery after surgery recommendations in gynecology already recommend avoiding the use of volatile anesthetic gases in favor of propofol to reduce postoperative nausea and vomiting.14
In the context of a patient undergoing a TLH, the estimated carbon footprint in the United States is about 560 kg of CO2 equivalents—roughly the same as driving 1,563 miles in a gas-powered car.
Continue to: Climate impact on our patients...
Climate impact on our patients
The data in obstetrics and gynecology is clear that climate change is affecting patient outcomes, both globally and in our own country. A systematic review of 32 million births found that air pollution and heat exposure were associated with preterm birth and low birth weight, and these effects were seen in all geographic regions across the United States.1 A study of 5.9 million births in California found that patients who lived near coal- and oil-power plants had up to a 27% reduction in preterm births when those power plants closed and air pollution decreased.15 A study in Nature Sustainability on 250,000 pregnancies that ended in missed abortions at 14 weeks or less found the odds ratio of missed abortion increased with the cumulative exposure to air pollution.16 When air pollution was examined in comparison to other factors, neighborhood air pollution better predicted preterm birth, very preterm birth, and small for gestational age more than race, ethnicity, or any other socio-economic factor.17 The effects of air pollution have been demonstrated in other fields as well, including increased mortality after cardiac transplantation with exposure to air pollution,4 and for patients undergoing bariatric surgery who live near major roadways, decreased weight loss, less improvement in hemoglobin A1c, and less change in lipids compared with those with less exposure to roadway pollution.5
Air pollution and heat are not the only factors that influence health. Endocrine disrupting chemicals (EDCs) and single-use plastic polymers, which are used in significant supply in US health care, have been found in human blood,18 intestine, and all portions of the placenta.19 Phthalates, an EDC found in medical use plastics and medications to control delivery, have been associated with increasing fibroid burden in patients undergoing hysterectomy and myomectomy.20 The example case patient with fibroids undergoing TLH may have had her condition worsened by exposure to phthalates.
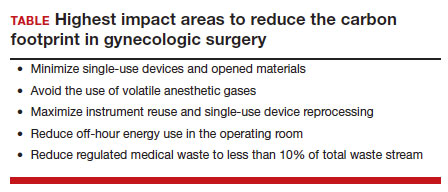
Specific areas for improvement
There is a huge opportunity for improvement to reduce the total carbon footprint of a TLH.
A lifecycle assessment of hysterectomy in the United States concluded that an 80% reduction in carbon emissions could be achieved by minimizing opened materials, using reusable and reprocessed instruments, reducing off-hour energy use in the OR (HVAC setbacks), and avoiding the use of volatile anesthetic gases.21 The sterilization and re-processing of reusable instruments represented the smallest proportion of carbon emissions from a TLH. Data on patient safety supports these interventions, as current practices have more to do with hospital culture and processes than evidence.
Despite a push to use single-use objects by industry and regulatory agencies in the name of patient safety, data demonstrate that single-use objects are in actuality not safer for patients and may be associated with increased surgical site infections (SSIs). A study from a cancer center in California found that when single-use head covers, shoe covers, and facemasks were eliminated due to supply shortages during the pandemic, SSIs went down by half, despite an increase in surgical volume and an increase in the number of contaminated cases.22 The authors reported an increase in hand hygiene throughout the hospital, which likely contributed to the success of reducing SSIs.
Similarly, a systematic review found no evidence to support single-use instruments over reusable or reprocessed instruments when considering instrument function, ease of use, patient safety, SSIs, or long-term patient outcomes.23 While it may be easy for regulatory agencies to focus on disposing objects as paramount to reducing infections, the Centers for Disease Control and Prevention states that the biggest factors affecting SSIs are appropriate use of prophylactic antibiotics, skin antisepsis, and patient metabolic control.24 Disposing of single-use objects in the name of patient safety will worsen patient health outcomes when considering patient proximity to waste, pollution, and EDCs.
The sterilization process for reusable items is often called out by the medical supply industry as wasteful and energy intensive; however, data refute these claims. A Swedish study researching reusable versus single-use trocars found that a reusable trocar system offers a robust opportunity to reduce both the environmental and financial costs for laparoscopic surgery.25 We can further decrease the environmental impact of reusable instruments by using sets instead of individually packed instruments and packing autoclaves more efficiently. By using rigid sterilization containers, there was an 85% reduction in carbon footprint as compared with the blue wrap system.
Electricity use can be easily reduced across all surgical spaces by performing HVAC setbacks during low occupancy times of day. On nights and weekends, when there are very few surgical cases occurring, one study found that by decreasing the ventilation rate, turning off lights, and performing the minimum temperature control in unused ORs, electricity use was cut in half.11
Waste triage and recycling
Reducing regulated medical waste is another area where hospitals can make a huge impact on carbon emissions and costs with little more than education and process change. Guidelines for regulated medical waste sorting developed out of the HIV epidemic due to the fear of blood products. Although studies show that regulated medical waste is not more infectious than household waste, state departments of public health have kept these guidelines in place for sorting fluid blood and tissue into RMW containers and bags.26 The best hospital performers keep RMW below 10% of the total waste stream, while many ORs send close to 100% of their waste as RMW (FIGURE 1b). ORs can work with nursing and environmental services staff to assess processes and divert waste into recycling and regular waste. Many OR staff are acutely aware of the huge amount of waste produced and want to make a positive impact. Success in this small area often builds momentum to tackle harder sustainability practices throughout the hospital.
Continue to: Removal of EDCs from medical products...
Removal of EDCs from medical products
Single-use medical supplies are not only wasteful but also contain harmful EDCs, such as phthalates, bisphenol A (BPA), parabens, perfluoroalkyl substances, and triclosan. Phthalates, for example, account for 30% to 40% of the weight of medical-use plastics, and parabens are ubiquitously found in ultrasound gel.3 Studies looking at exposure to EDCs within the neonatal intensive care unit reveal substantial BPA, phthalate, and paraben levels within biologic samples from premature infants, thought to be above toxicity limits. While we do not know the full extent to which EDCs can affect neonatal development, there is already mounting evidence that EDCs are associated with endocrine, metabolic, and neurodevelopmental disorders throughout our lifespan.3
30-day climate challenge
Although the example case patient undergoing TLH for fibroids will never need care for her fibroids again, the climate impact of her time in the OR represents the most carbon-intensive care she will ever need. Surgery as practiced in the United States today is unsustainable.
In 2021, the Biden administration issued an executive order requiring all federal facilities, including health care facilities and hospitals, to be carbon neutral by 2035. In order to make meaningful changes industry-wide, we should be petitioning lawmakers for stricter environmental regulations in health care, similar to regulations in the manufacturing and airline industries. We recommend a 30-day climate challenge (FIGURE 2) for bringing awareness to your circles of influence. Physicians have an ethical duty to advocate for change at the local, regional, and national level if we want to see a better future for our patients, their children, and even ourselves. Organizations such as Practice Greenhealth, Health Care without Harm, and Citizens’ Climate Lobby can help amplify our voices to reach the right people to implement sweeping policy changes. ●
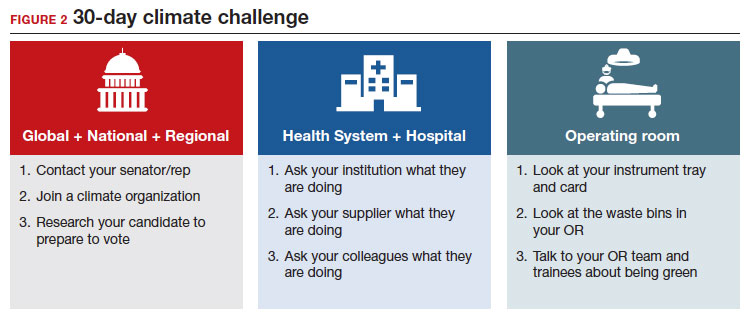
- Costello A, Abbas M, Allen et al. Managing the health effects of climate change: Lancet and University College London Institute for Global Health Commission. Lancet. 2009;373:1693-1733. doi: 10.1016/S0140-6736(09)60935-1.
- Bekkar B, Pacheco S, Basu R, et al. Association of air pollution and heat exposure with preterm birth, low birth weight, and stillbirth in the US: a systematic review. JAMA Netw Open. 2020;3. doi:10.1001/JAMANETWORKOPEN.2020.8243.
- Genco M, Anderson-Shaw L, Sargis RM. Unwitting accomplices: endocrine disruptors confounding clinical care. J Clin Endocrinol Metab. 2020;105:e3822–7. doi: 10.1210/cline2. m/dgaa358.
- Al-Kindi SG, Sarode A, Zullo M, et al. Ambient air pollution and mortality after cardiac transplantation. J Am Coll Cardiol. 2019;74:3026-3035. doi: 10.1016/j.jacc.2019.09.066.
- Ghosh R, Gauderman WJ, Minor H, et al. Air pollution, weight loss and metabolic benefits of bariatric surgery: a potential model for study of metabolic effects of environmental exposures. Pediatr Obes. 2018;13:312-320. doi: 10.1111/ijpo.12210.
- Health Care’s Climate Footprint. Health care without harm climate-smart health care series, Green Paper Number one. September 2019. https://www.noharm.org/
ClimateFootprintReport. Accessed December 11, 2022. - Healthcare Energy End-Use Monitoring. US Department of Energy. https://www.energy.gov/eere/
buildings/downloads/ healthcare-energy-end-use- monitoring. Accessed December 11, 2022. - 2012 Commercial Buildings Energy Consumption Survey: Water Consumption in Large Buildings Summary. U.S Energy Information Administration. https://www.eia.gov/
consumption/commercial/ reports/2012/water. Accessed December 11, 2022. - Belkhir L, Elmeligi A. Carbon footprint of the global pharmaceutical industry and relative implact of its major players. J Cleaner Production. 2019;214:185-194. doi: 10.1016 /j.jclearpro.2019.11.204.
- Esaki RK, Macario A. Wastage of Supplies and Drugs in the Operating Room. 2015:8-13.
- MacNeill AJ, et al. The Impact of Surgery on Global Climate: A Carbon Footprinting Study of Operating Theatres in Three Health Systems. Lancet Planet Health.2017;1:e360–367. doi:10.1016/S2542-5196(17)30162-6.
- Shoham MA, Baker NM, Peterson ME, et al. The environmental impact of surgery: a systematic review. 2022;172:897-905. doi:10.1016/j.surg.2022.04.010.
- Ryan SM, Nielsen CJ. Global warming potential of inhaled anesthetics: application to clinical use. Anesth Analg. 2010;111:92-98. doi:10.1213/ANE.0B013E3181E058D7.
- Kalogera E, Dowdy SC. Enhanced recovery pathway in gynecologic surgery: improving outcomes through evidence-based medicine. Obstet Gynecol Clin North Am. 2016;43:551-573. doi: 10.1016/j.ogc.2016.04.006.
- Casey JA, Karasek D, Ogburn EL, et al. Retirements of coal and oil power plants in California: association with reduced preterm birth among populations nearby. Am J Epidemiol. 2018;187:1586-1594. doi: 10.1093/aje/kwy110.
- Zhang L, Liu W, Hou K, et al. Air pollution-induced missed abortion risk for pregnancies. Nat Sustain. 2019:1011–1017.
- Benmarhnia T, Huang J, Basu R, et al. Decomposition analysis of Black-White disparities in birth outcomes: the relative contribution of air pollution and social factors in California. Environ Health Perspect. 2017;125:107003. doi: 10.1289/EHP490.
- Leslie HA, van Velzen MJM, Brandsma SH, et al. Discovery and quantification of plastic particle pollution in human blood. Environ Int. 2022;163:107199. doi: 10.1016/j.envint.2022.107199.
- Ragusa A, Svelato A, Santacroce C, et al. Plasticenta: first evidence of microplastics in human placenta. Environ Int. 2021;146:106274. doi: 10.1016/j.envint.2020.106274.
- Zota AR, Geller RJ, Calafat AM, et al. Phthalates exposure and uterine fibroid burden among women undergoing surgical treatment for fibroids: a preliminary study. Fertil Steril. 2019;111:112-121. doi: 10.1016/j.fertnstert.2018.09.009.
- Thiel CL, Eckelman M, Guido R, et al. Environmental impacts of surgical procedures: life cycle assessment of hysterectomy in the United States. Environ Sci Technol. 2015;49:1779-1786. doi: 10.1021/es504719g.
- Malhotra GK, Tran T, Stewart C, et al. Pandemic operating room supply shortage and surgical site infection: considerations as we emerge from the Coronavirus Disease 2019 Pandemic. J Am Coll Surg. 2022;234:571-578. doi: 10.1097/XCS.0000000000000087.
- Siu J, Hill AG, MacCormick AD. Systematic review of reusable versus disposable laparoscopic instruments: costs and safety. ANZ J Surg. 2017;87:28-33. doi:10.1111/ANS.13856.
- Berríos-Torres SI, Umscheid CA, Bratzler DW, et al; Healthcare Infection Control Practices Advisory Committee. Centers for Disease Control and Prevention Guideline for the Prevention of Surgical Site Infection, 2017 [published correction appears in: JAMA Surg. 2017;152:803]. JAMA Surg. 2017;152:784-791. doi: 10.1001/jamasurg.2017.0904.
- Rizan, Chantelle, Lillywhite, et al. Minimising carbon and financial costs of steam sterilisation and packaging of reusable surgical instruments. Br J Surg. 2022;109:200-210. doi:10.1093/BJS/ZNAB406.
- Sustainability Benchmarking Report, 2010. Practice Greenhealth. https://www.practicegreenhealth.org. Accessed December 11, 2022.
- Costello A, Abbas M, Allen et al. Managing the health effects of climate change: Lancet and University College London Institute for Global Health Commission. Lancet. 2009;373:1693-1733. doi: 10.1016/S0140-6736(09)60935-1.
- Bekkar B, Pacheco S, Basu R, et al. Association of air pollution and heat exposure with preterm birth, low birth weight, and stillbirth in the US: a systematic review. JAMA Netw Open. 2020;3. doi:10.1001/JAMANETWORKOPEN.2020.8243.
- Genco M, Anderson-Shaw L, Sargis RM. Unwitting accomplices: endocrine disruptors confounding clinical care. J Clin Endocrinol Metab. 2020;105:e3822–7. doi: 10.1210/cline2. m/dgaa358.
- Al-Kindi SG, Sarode A, Zullo M, et al. Ambient air pollution and mortality after cardiac transplantation. J Am Coll Cardiol. 2019;74:3026-3035. doi: 10.1016/j.jacc.2019.09.066.
- Ghosh R, Gauderman WJ, Minor H, et al. Air pollution, weight loss and metabolic benefits of bariatric surgery: a potential model for study of metabolic effects of environmental exposures. Pediatr Obes. 2018;13:312-320. doi: 10.1111/ijpo.12210.
- Health Care’s Climate Footprint. Health care without harm climate-smart health care series, Green Paper Number one. September 2019. https://www.noharm.org/
ClimateFootprintReport. Accessed December 11, 2022. - Healthcare Energy End-Use Monitoring. US Department of Energy. https://www.energy.gov/eere/
buildings/downloads/ healthcare-energy-end-use- monitoring. Accessed December 11, 2022. - 2012 Commercial Buildings Energy Consumption Survey: Water Consumption in Large Buildings Summary. U.S Energy Information Administration. https://www.eia.gov/
consumption/commercial/ reports/2012/water. Accessed December 11, 2022. - Belkhir L, Elmeligi A. Carbon footprint of the global pharmaceutical industry and relative implact of its major players. J Cleaner Production. 2019;214:185-194. doi: 10.1016 /j.jclearpro.2019.11.204.
- Esaki RK, Macario A. Wastage of Supplies and Drugs in the Operating Room. 2015:8-13.
- MacNeill AJ, et al. The Impact of Surgery on Global Climate: A Carbon Footprinting Study of Operating Theatres in Three Health Systems. Lancet Planet Health.2017;1:e360–367. doi:10.1016/S2542-5196(17)30162-6.
- Shoham MA, Baker NM, Peterson ME, et al. The environmental impact of surgery: a systematic review. 2022;172:897-905. doi:10.1016/j.surg.2022.04.010.
- Ryan SM, Nielsen CJ. Global warming potential of inhaled anesthetics: application to clinical use. Anesth Analg. 2010;111:92-98. doi:10.1213/ANE.0B013E3181E058D7.
- Kalogera E, Dowdy SC. Enhanced recovery pathway in gynecologic surgery: improving outcomes through evidence-based medicine. Obstet Gynecol Clin North Am. 2016;43:551-573. doi: 10.1016/j.ogc.2016.04.006.
- Casey JA, Karasek D, Ogburn EL, et al. Retirements of coal and oil power plants in California: association with reduced preterm birth among populations nearby. Am J Epidemiol. 2018;187:1586-1594. doi: 10.1093/aje/kwy110.
- Zhang L, Liu W, Hou K, et al. Air pollution-induced missed abortion risk for pregnancies. Nat Sustain. 2019:1011–1017.
- Benmarhnia T, Huang J, Basu R, et al. Decomposition analysis of Black-White disparities in birth outcomes: the relative contribution of air pollution and social factors in California. Environ Health Perspect. 2017;125:107003. doi: 10.1289/EHP490.
- Leslie HA, van Velzen MJM, Brandsma SH, et al. Discovery and quantification of plastic particle pollution in human blood. Environ Int. 2022;163:107199. doi: 10.1016/j.envint.2022.107199.
- Ragusa A, Svelato A, Santacroce C, et al. Plasticenta: first evidence of microplastics in human placenta. Environ Int. 2021;146:106274. doi: 10.1016/j.envint.2020.106274.
- Zota AR, Geller RJ, Calafat AM, et al. Phthalates exposure and uterine fibroid burden among women undergoing surgical treatment for fibroids: a preliminary study. Fertil Steril. 2019;111:112-121. doi: 10.1016/j.fertnstert.2018.09.009.
- Thiel CL, Eckelman M, Guido R, et al. Environmental impacts of surgical procedures: life cycle assessment of hysterectomy in the United States. Environ Sci Technol. 2015;49:1779-1786. doi: 10.1021/es504719g.
- Malhotra GK, Tran T, Stewart C, et al. Pandemic operating room supply shortage and surgical site infection: considerations as we emerge from the Coronavirus Disease 2019 Pandemic. J Am Coll Surg. 2022;234:571-578. doi: 10.1097/XCS.0000000000000087.
- Siu J, Hill AG, MacCormick AD. Systematic review of reusable versus disposable laparoscopic instruments: costs and safety. ANZ J Surg. 2017;87:28-33. doi:10.1111/ANS.13856.
- Berríos-Torres SI, Umscheid CA, Bratzler DW, et al; Healthcare Infection Control Practices Advisory Committee. Centers for Disease Control and Prevention Guideline for the Prevention of Surgical Site Infection, 2017 [published correction appears in: JAMA Surg. 2017;152:803]. JAMA Surg. 2017;152:784-791. doi: 10.1001/jamasurg.2017.0904.
- Rizan, Chantelle, Lillywhite, et al. Minimising carbon and financial costs of steam sterilisation and packaging of reusable surgical instruments. Br J Surg. 2022;109:200-210. doi:10.1093/BJS/ZNAB406.
- Sustainability Benchmarking Report, 2010. Practice Greenhealth. https://www.practicegreenhealth.org. Accessed December 11, 2022.


