User login
Raising the bar (and the OR table):Ergonomics in MIGS
Work-related musculoskeletal disorders (WMSDs) are “musculoskeletal disorders (injuries or disorders of the muscles, nerves, tendons, joints, cartilage, and spinal discs) in which the work environment and performance of work contribute significantly to the condition; and/or the condition is made worse or persists longer due to work conditions.”1 The health care industry has one of the highest rates of WMSDs, even when compared with traditional labor-intensive occupations, such as coal mining. In 2017, the health care industry reported more than a half million incidents of work-related injury and illness.2,3 In particular, surgeons are at increased risk for WMSDs, since they repetitively perform the classic tenets of poor ergonomics, including operating in static, extreme, and awkward positions and for prolonged periods of time.3
Gynecologic surgeons face unique ergonomic challenges. Operating in the pelvis requires an oblique approach that adds complexity and inhibits appropriate ergonomic positioning.4 All modalities of surgery incur their own challenges and risks to the surgeon, including minimally invasive gynecologic surgery (MIGS), which has become the standard of care for most conditions. Although MIGS has several benefits for the patient, a survey of gynecologic oncologists found that 88% of respondents reported discomfort related to MIGS.5 Several factors contribute to the development of WMSDs in surgery, including lack of ergonomic awareness, suboptimal ergonomic education and training,5,6 and ergonomically poor operating room (OR) equipment and instrument design.7 Furthermore, surgical culture does not generally prioritize ergonomics in the OR or requests for ergonomic accommodations.7,8
Within 5 years, a physician workforce shortage is projected for the United States.9 WMSDs contribute to workforce issues as they are associated with decreased productivity; time off needed for pain and treatment, including short-term disability; and possibly early retirement (as those who are older and have more work experience may be more likely to seek medical attention).10 In a 2013 study of vaginal surgeons, 14% missed work; 21% modified their work hours, work type, or amount of surgery; and 29% modified their surgical technique because of injury.10 Work-related pain also can negatively affect mental health, sleep, relationships, and quality of life.6
Recently, awareness has increased regarding WMSDs and their consequences, which has led to significant strides in the study of ergonomics among surgeons, a growing body of research on the topic, and guidance for optimizing ergonomics in the OR.
Risk factors for ergonomic strain
Several factors contribute to ergonomic strain and, subsequently, the development of WMSDs. Recognizing these factors can direct strategies for injury prevention.
Patient factors
The prevalence of obesity in the United States increased from 30.5% in 1999–2000 to 41.9% between 2017 and 2020.11 As the average patient’s body mass index (BMI) has increased, there is concern for a parallel increase in the ergonomic strain on laparoscopic surgeons.
A study of simulated laparoscopic tasks at varying model BMI levels demonstrated increased surgeon postural stress and workload at higher model BMIs (50 kg/m2) when compared with lower model BMIs (20 and 30 kg/m2).11 This result was supported in another study, which demonstrated both increased muscle activity and increased time needed to complete a surgical task with laparoscopic surgery; interestingly, when the same study measured these parameters for robotic surgery, this association was not seen.12 This suggests that a robotic rather than a laparoscopic approach may avoid some of the ergonomic strain associated with increased patient BMI.
Continue to: Surgeon factors...
Surgeon factors
Various surgeon characteristics have been shown to influence ergonomics in the OR. Surgeons with smaller hand sizes, for example, reported greater physical discomfort and demonstrated greater ergonomic workload when operating laparoscopically.13-15 In particular, those with a glove size of 6.5 or smaller have more difficulty using laparoscopic instruments, and those with a glove size smaller than 7 demonstrate a larger decline in grip strength when using laparoscopic instruments repeatedly.14,16
Surgeon height also can affect the amount of time spent in high-risk, nonergonomic positions. In a study that evaluated video recordings of surgeon posture during gynecologic laparoscopy, shorter surgeons were noted to use greater degrees of neck rotation to look at the monitor.17 Furthermore, surgeons with shorter arm lengths experienced more “extreme positions” of the nondominant shoulder and elbow.17 This trend also was seen in open and robotic surgery, where surgeons with a height of 66 cm or less reported increased pain scores after operating.18
Surgical instruments and OR setup
Surgical instrument characteristics can contribute to ergonomic strain, especially when the instruments have been designed with a one-size-fits-all mentality.8,19 In an examination of the anthropometric measurements of surgeon hand sizes and their correlation with difficulty when using a “standard” laparoscopic instrument, surgeons with smaller finger and hand spans had trouble using these instruments.19 Another study compared surgeon grip strength and ergonomic workloads after using 3 laparoscopic advanced bipolar instruments.16 Gender and hand size aside, the authors found that use of several of the laparoscopic devices led to greater decline in grip strength.16
The setup of the OR also can have a profound effect on the surgeon’s ergonomics. Monitor placement, for example, is crucial to ergonomic success. One study found that positioning the monitor directly in front of the surgeon at eye level was associated with the lowest neck muscle activity during a simulated task.20
Route of surgery
Each surgical approach has intrinsic ergonomic risks. With laparoscopy, surgeons often remain in straight head and back positions without much trunk motion, especially when compared with open surgery.21 In one study, laparoscopic surgeons spent more than 60% of a case in a static position and more than 80% of a case in a high-risk, “demanding” neck position.22
Robotic surgery, in contrast to laparoscopy, often has been cited as being more “ergonomic.” While robotic surgery has less of an effect on the neck, shoulders, arms, and legs than laparoscopy23 and often is associated with less physical discomfort than either open or laparoscopic surgery,23,24 robotic surgery still maintains its own innate ergonomic risks. Of robotic surgeons surveyed, 56.1% reported neck stiffness, finger fatigue, and eye symptoms in one study.25 In another survey study, more robotic surgeons (72%) reported physical symptoms than laparoscopic (57%) and open (49%) surgeons.26Vaginal surgery also puts surgeons at ergonomic risk. A majority of surgeons (87.2%) who completed more than 50% of their cases vaginally reported a history of WMSDs.10 Vaginal surgery places surgeons in awkward positions of the neck, shoulder, and trunk frequently and for longer durations.27
Continue to: Strategies for preventing WMSDs...
Strategies for preventing WMSDs
As factors that contribute to the development of WMSDs are identified, preventive strategies can be targeted to these individual factors. Research has focused on appropriate setup of the OR, surgeon posture, intraoperative microbreaks, and stretching both in and outside of the OR.
1. OR setup and positioning of the surgeon by MIGS route
The route of MIGS affects OR setup and surgeon posture. Ergonomic recommendations for laparoscopy, robotic surgery, and vaginal surgery are all unique to the risks posed by each particular approach.
Laparoscopic surgery. Laparoscopic monitors should face the surgeon directly, with the screen just below eye level to maintain the surgeon’s neck in a neutral position.28 The table height should be set for the tallest surgeon, and shorter surgeons should stand on steps as needed.28 The table height also should allow for the surgeon’s hands to be at elbow height, with the elbows bent at 90 degrees with the wrists straight.29 Foot pedals should be placed at the surgeons’ foot level and should be reached easily.28 Additionally, the patient’s arms should be tucked at their sides to allow surgeons a larger operative space.29 When using laparoscopic instruments, locking and ratcheting features should be used whenever possible to reduce prolonged grip or squeeze forces.28 The laparoscopic camera should be held in the palm with the wrist in a neutral position.29
Robotic surgery. Positioning and setup of the robotic console is a main focus of ergonomic recommendations. The surgeon’s chair should be brought as close to the console as possible, and the knees positioned in a 90-degree angle.30 The foot pedals should be brought toward the surgeon to maintain this angle of the knees.30 The console should be rotated toward the surgeon and then the height adjusted so that the surgeon can look through the eyepiece while sitting upright and can maintain the neck in a neutral position.28,30 The surgeon’s forehead should rest comfortably on the headrest.29 The forearms should rest on the armrest while the arms are maintained in a neutral position and the shoulders remain relaxed while the surgeon holds the robotic controls.30 It is important to utilize the armrest often to relieve stress on the arm while operating.28 Frequent use of the clutch function can keep the robotic controls in the center of the workspace.28
Vaginal surgery. Both seated and standing positions are associated with high-risk positioning of the trunk and bilateral shoulders, respectively, in vaginal surgery.31 However, surgeons who stand while operating vaginally reported more discomfort in the bilateral wrists, thighs, and lower legs than those who operated while seated.31 This suggests a potential ergonomic advantage to the seated position for vaginal surgery. Chair height should be adjusted so the surgeon can look straight ahead with the neck in a neutral position.32 Surgeons should consider using a headlamp, as this may prevent repetitive awkward movements to adjust overhead lights.32 For standing surgery, the table height should be adjusted for the tallest surgeon, and shorter surgeons or assistants should use steps as needed.3
Surgical assistants should switch sides during the course of the case to avoid excessive unilateral upper-extremity strain.32 The addition of a table-mounted vaginal retractor system may be useful in relieving physical strain for surgical assistants, but data currently are lacking to demonstrate this ergonomic benefit.33 Further studies are needed, especially since many surgeons take on the role of surgical assist in the teaching environment and subsequently report more WMSDs than their colleagues who do not work in teaching environments.10,34
2. Pain relief from individual ergonomic positioning devices
Apart from adjusting how the OR equipment is arranged or how the surgeons adjust their positioning, several devices that assist with surgeon positioning—including gel mats or insoles, exoskeletons, and “augmented reality” glasses—are being studied.
The use of gel mats or insoles in the OR has mixed evidence in the literature.35-37
Exoskeletons, external devices that support a surgeon’s posture and positioning, have been studied thus far in simulated nonsterile surgical environments. Preliminarily, it appears that use of an exoskeleton can decrease muscle activity and time spent in static positions, with a reported decrease in post-task user discomfort.38,39 More data are needed to determine if exoskeletons can be used in the sterile setting and for longer durations as may occur in actual OR cases.
Augmented reality glasses project the laparoscopic monitor image to the glasses, which frees the surgeon to place the “monitor” in a more neutral, ergonomic position. In one study, use of augmented reality glasses was associated with decreased muscle activity and a reduction in Rapid Entire Body Assessment (REBA) scores when compared with use of the conventional laparoscopic monitor.40More data are needed on these emerging technologies to determine whether adverse effects occur with prolonged use.
Continue to: 3. Implementing intraoperative microbreaks and stretching...
3. Implementing intraoperative microbreaks and stretching
The American College of Surgeons (ACS) recommends that surgeons avoid prolonged static postures during procedures.28 One strategy for preventing sustained positioning is to incorporate breaks with associated stretching routinely during surgery.28
Microbreaks. In a landmark study by Park and colleagues in 2017, 120-second long targeted stretching microbreaks (TSMBs) were completed every 20 to 40 minutes during a surgery, and results demonstrated improved postoperative surgeon pain scores without an associated increase in the length of the case.41 These surgeons reported improved pain in the neck, bilateral shoulders, bilateral hands, and lower back. Eighty-eight percent of surgeons reported either improvement or “no change” in their mental focus, and 100% reported improvement or “no change” in their physical performance after TSMBs were implemented.42 Of surveyed surgeons, 87% wanted TSMBs incorporated routinely.41,42
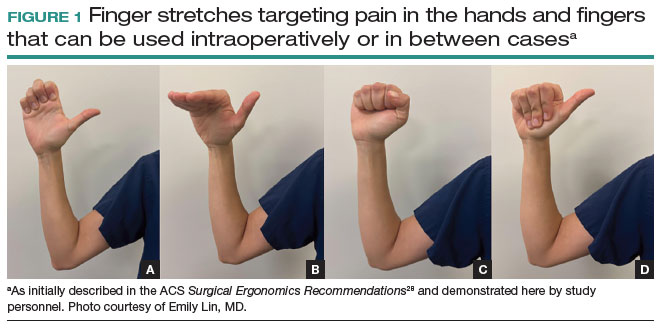
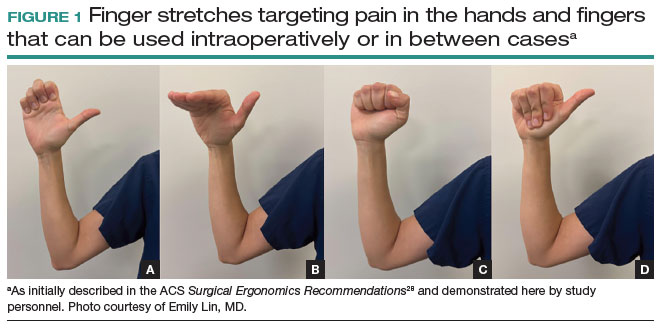
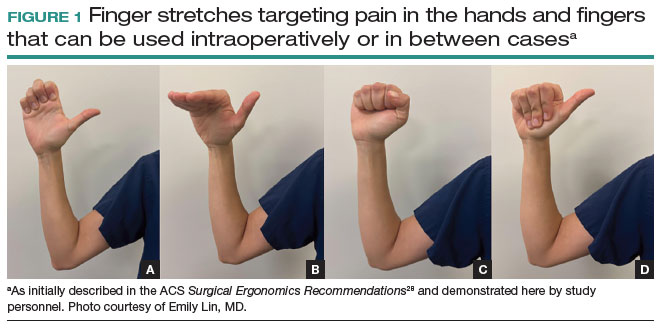
Stretches. Multiple resources, such as the ACS and the Mayo Clinic, for intraoperative stretches are available. The ACS recommends performing neck and shoulder stretches during intraoperative microbreaks, including a range-of-movement neck exercise, deep cervical flexor training, and standing scapular retraction.28 The ACS also demonstrates lumbrical stretches for the fingers and passive wrist extension exercises to be used intraoperatively (or between cases) (FIGURE 1).28 The Mayo Clinic Hallbeck Human Factors Engineering Laboratories has a publicly available “OR Stretch Instructional Video” in which the surgeon is guided through several different short stretches, including shoulder shrugging and side bends, that can be used during surgery.43
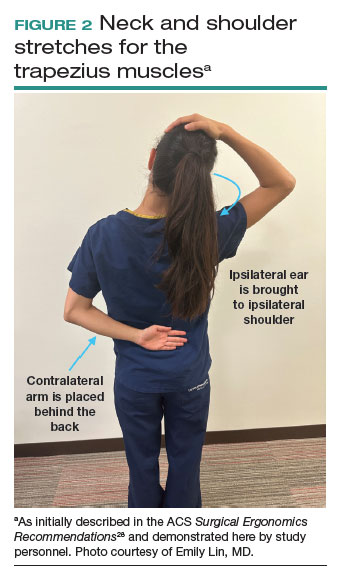
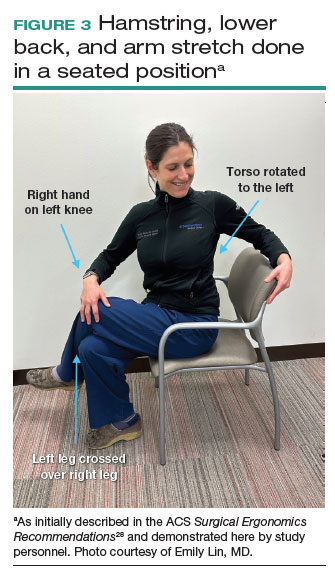
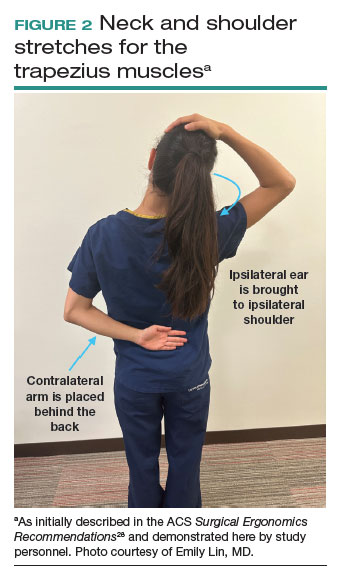
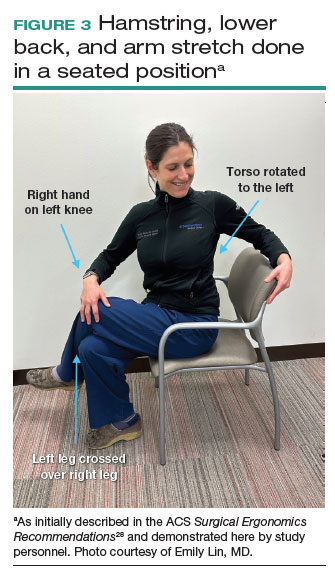
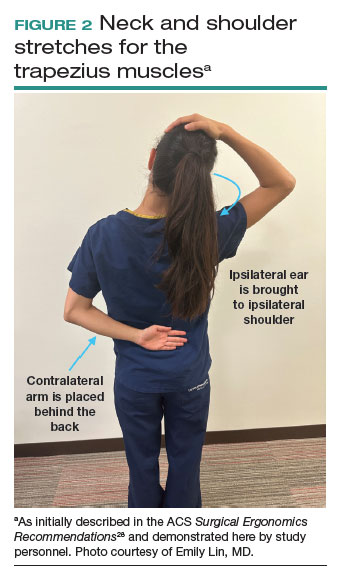
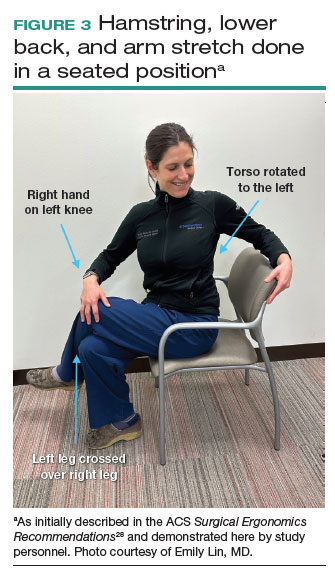
Both the ACS and the Mayo Clinic provide examples of pertinent stretch exercises for use when not in the sterile environment, between cases or after cases are complete. The ACS recommends several neck and shoulder stretches for the trapezius, levator scapulae, and pectoralis and recommends the use of a foam roller to improve thoracic mobility (FIGURE 2).28 As above, the Mayo Clinic Hallbeck Human Factors Engineering Laboratories has a publicly available “OR-Stretch Between Surgery Stretches Video” in which the surgeon is guided through several short stretches that are done in a seated position, including stretches for the hamstring, lower back, and arms (FIGURE 3).43
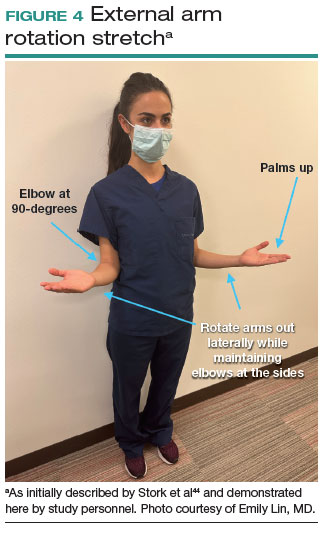
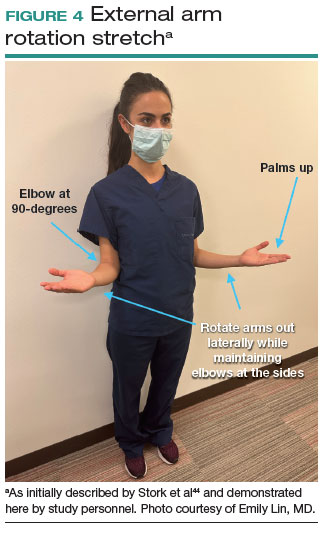
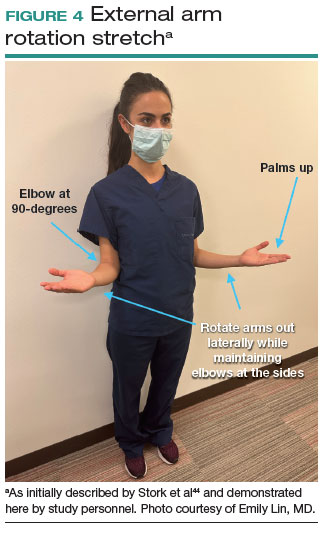
Many of the above-mentioned stretches were designed for use in the context of open, laparoscopic, or robotic surgery. For the vaginal surgeon, the intraoperative ergonomic stressors differ from those of other routes of surgery, and thus stretches tailored to the positioning during vaginal surgery are necessary. In a video recently published by the Society of Gynecologic Surgeons, several stretches are reviewed that target high-risk positions often held by the surgeon or assistant when operating vaginally.44 These stretches include cervical retraction, thoracic extension, external arm rotation, cervical side bending, and lumbar extension (FIGURE 4).44 The recommendation is to complete these exercises 2 times per day, with 8 to 10 repetitions per set.44
Prioritizing ergonomic awareness and training
As caregivers, it is not uncommon for us to prioritize the needs of others before those of ourselves. However, WMSDs are prevalent, and their downstream effects may cause catastrophic professional and personal losses. Cumulatively, the global impact of WMSDs is a significant issue for the health care workforce and its longevity.
To prevent WMSDs, it is imperative that surgeons are aware of the factors that contribute to injury development and the appropriate, accessible modifications for these factors. While each surgical modality confers its own ergonomic challenges, these risks can be mitigated through increased awareness of OR setup, surgeon positioning, and incorporation of microbreaks and stretching exercises during and after surgical procedures.
Formal training in surgical ergonomics is lacking across specialties, including gynecology.45 Multiple educational interventions have been proposed and studied to help fill this training gap.30,46-49When used, these interventions have been associated with increased knowledge of surgical ergonomic principles or reduction in surgeon pain scores, including trainees.50 As we become more cognizant of WMSDs, standardized resident curricula should be developed in an effort to reduce the prevalence of these potentially career-ending injuries.
In addition to education, cultivating a culture in which ergonomics is prioritized is essential. Although most surgeons report work-related pain, very few report their injuries to occupational health. For example, while 29% of gynecologic oncologists reported seeking treatment for a WMSD, only 1% had reported their injury to their employer.5 In a study of ACS members, only 19% of injuries were reported, 30% of surgeons stated that they did not know how to report an injury, and 21% felt that the resources for surgeons during and after an injury were inadequate.6
As we prioritize the health and safety of our patients, we also need to promote ergonomic awareness in the OR, respect the need for accommodations, encourage injury reporting, support surgeons who need to take time away for medical treatment, and partner with industry to develop new instruments and technology with effective ergonomic features. ●
- Workplace health glossary. Reviewed February 12, 2020. Centers for Disease Control and Prevention. Accessed May 18, 2023. https://www.cdc.gov/workplacehealthpromotion/tools-resources /glossary/glossary.html#W
- Epstein S, Sparer EH, Tran BN, et al. Prevalence of work-related musculoskeletal disorders among surgeons and interventionalists: a systematic review and meta-analysis. JAMA Surg. 2018;153:e174947.
- Yurteri-Kaplan LA, Park AJ. Surgical ergonomics and preventing workrelated musculoskeletal disorders. Obstet Gynecol. 2023;141:455-462.
- Symer MM, Keller DS. Human factors in pelvic surgery. Eur J Surg Oncol. 2022;48:2346-2351.
- Franasiak J, Ko EM, Kidd J, et al. Physical strain and urgent need for ergonomic training among gynecologic oncologists who perform minimally invasive surgery. Gynecol Oncol. 2012;126:437-442.
- Davis WT, Fletcher SA, Guillamondegui OD. Musculoskeletal occupational injury among surgeons: effects for patients, providers, and institutions. J Surg Res. 2014;189:207-212.e6.
- Fox M. Surgeons face unique ergonomic challenges. American College of Surgeons. September 1, 2022. Accessed May 22, 2023. https://www.facs.org/for-medical-professionals/news-publications /news-and-articles/bulletin/september-2022-volume-107-issue-9 /surgeons-face-unique-ergonomic-challenges/
- Wong JMK, Carey ET, King C, et al. A call to action for ergonomic surgical devices designed for diverse surgeon end users. Obstet Gynecol. 2023;141:463-466.
- IHS Inc. The Complexities of Physician Supply and Demand: Projections from 2014 to 2025. Association of American Medical Colleges. April 5, 2016.
- Kim-Fine S, Woolley SM, Weaver AL, et al. Work-related musculoskeletal disorders among vaginal surgeons. Int Urogynecol J. 2013;24:1191-1200.
- Sers R, Forrester S, Zecca M, et al. The ergonomic impact of patient body mass index on surgeon posture during simulated laparoscopy. Appl Ergon. 2021;97:103501.
- Moss EL, Sarhanis P, Ind T, et al. Impact of obesity on surgeon ergonomics in robotic and straight-stick laparoscopic surgery. J Minim Invasive Gynecol. 2020;27:1063-1069.
- Sutton E, Irvin M, Zeigler C, et al. The ergonomics of women in surgery. Surg Endosc. 2014;28:1051-1055.
- Berguer R, Hreljac A. The relationship between hand size and difficulty using surgical instruments: a survey of 726 laparoscopic surgeons. Surg Endosc. 2004;18:508-512.
- Bellini MI, Amabile MI, Saullo P, et al. A woman’s place is in theatre, but are theatres designed with women in mind? A systematic review of ergonomics for women in surgery. J Clin Med. 2022;11:3496.
- Wong JMK, Moore KJ, Lewis P, et al. Ergonomic assessment of surgeon characteristics and laparoscopic device strain in gynecologic surgery. J Minim Invasive Gynecol. 2022;29:1357-1363.
- Aitchison LP, Cui CK, Arnold A, et al. The ergonomics of laparoscopic surgery: a quantitative study of the time and motion of laparoscopic surgeons in live surgical environments. Surg Endosc. 2016;30:5068-5076.
- Stewart C, Raoof M, Fong Y, et al. Who is hurting? A prospective study of surgeon ergonomics. Surg Endosc. 2022;36:292-299.
- Green SV, Morris DE, Naumann DN, et al. One size does not fit all: impact of hand size on ease of use of instruments for minimally invasive surgery. Surgeon. 2022;S1479-666X(22)00131-7.
- Matern U, Faist M, Kehl K, et al. Monitor position in laparoscopic surgery. Surg Endosc. 2005;19:436-440.
- Berguer R, Rab GT, Abu-Ghaida H, et al. A comparison of surgeons’ posture during laparoscopic and open surgical procedures. Surg Endosc. 1997;11:139-142.
- Athanasiadis DI, Monfared S, Asadi H, et al. An analysis of the ergonomic risk of surgical trainees and experienced surgeons during laparoscopic procedures. Surgery. 2021;169:496-501.
- Hotton J, Bogart E, Le Deley MC, et al. Ergonomic assessment of the surgeon’s physical workload during robot-assisted versus standard laparoscopy in a French multicenter randomized trial (ROBOGYN-1004 Trial). Ann Surg Oncol. 2023;30:916-923.
- Plerhoples TA, Hernandez-Boussard T, Wren SM. The aching surgeon: a survey of physical discomfort and symptoms following open, laparoscopic, and robotic surgery. J Robot Surg. 2012;6:65-72.
- Lee GI, Lee MR, Green I, et al. Surgeons’ physical discomfort and symptoms during robotic surgery: a comprehensive ergonomic survey study. Surg Endosc. 2017;31:1697-1706.
- McDonald ME, Ramirez PT, Munsell MF, et al. Physician pain and discomfort during minimally invasive gynecologic cancer surgery. Gynecol Oncol. 2014;134:243-247.
- Zhu X, Yurteri-Kaplan LA, Gutman RE, et al. Postural stress experienced by vaginal surgeons. Proc Hum Factors Ergonomics Soc Annu Meet. 2014;58:763-767.
- American College of Surgeons Division of Education and Surgical Ergonomics Committee. Surgical Ergonomics Recommendations. ACS Education. 2022.
- Cardenas-Trowers O, Kjellsson K, Hatch K. Ergonomics: making the OR a comfortable place. Int Urogynecol J. 2018;29:1065-1066.
- Hokenstad ED, Hallbeck MS, Lowndes BR, et al. Ergonomic robotic console configuration in gynecologic surgery: an interventional study. J Minim Invasive Gynecol. 2021;28:850-859.
- Singh R, Yurteri-Kaplan LA, Morrow MM, et al. Sitting versus standing makes a difference in musculoskeletal discomfort and postural load for surgeons performing vaginal surgery. Int Urogynecol J. 2019;30:231-237.
- Hullfish KL, Trowbridge ER, Bodine G. Ergonomics and gynecologic surgery: “surgeon protect thyself.” J Pelvic Med Surg. 2009;15:435-439.
- Woodburn KL, Kho RM. Vaginal surgery: don’t get bent out of shape. Am J Obstet Gynecol. 2020;223:762-763.
- Hobson DTG, Meriwether KV, Gaskins JT, et al. Learner satisfaction and experience with a high-definition telescopic camera during vaginal procedures: a randomized controlled trial. Female Pelvic Med Reconstr Surg. 2021;27:105-111.
- Speed G, Harris K, Keegel T. The effect of cushioning materials on musculoskeletal discomfort and fatigue during prolonged standing at work: a systematic review. Appl Ergon. 2018;70:300-334.
- Haramis G, Rosales JC, Palacios JM, et al. Prospective randomized evaluation of FOOT gel pads for operating room staff COMFORT during laparoscopic renal surgery. Urology. 2010;76:1405-1408.
- Voss RK, Chiang YJ, Cromwell KD, et al. Do no harm, except to ourselves? A survey of symptoms and injuries in oncologic surgeons and pilot study of an intraoperative ergonomic intervention. J Am Coll Surg. 2017;224:16-25.e1.
- Marquetand J, Gabriel J, Seibt R, et al. Ergonomics for surgeons—prototype of an external surgeon support system reduces muscular activity and fatigue. J Electromyogr Kinesiol. 2021;60:102586.
- Tetteh E, Hallbeck MS, Mirka GA. Effects of passive exoskeleton support on EMG measures of the neck, shoulder and trunk muscles while holding simulated surgical postures and performing a simulated surgical procedure. Appl Ergon. 2022;100:103646.
- Lim AK, Ryu J, Yoon HM, et al. Ergonomic effects of medical augmented reality glasses in video-assisted surgery. Surg Endosc. 2022;36:988-998.
- Park AE, Zahiri HR, Hallbeck MS, et al. Intraoperative “micro breaks” with targeted stretching enhance surgeon physical function and mental focus: a multicenter cohort study. Ann Surg. 2017;265:340-346.
- Hallbeck MS, Lowndes BR, Bingener J, et al. The impact of intraoperative microbreaks with exercises on surgeons: a multi-center cohort study. Appl Ergon. 2017;60:334-341.
- Hallbeck Human Factors Engineering Laboratories. OR Stretch Videos. Mayo Clinic, 2018. Accessed May 19, 2023. https://www.mayo .edu/research/labs/human-factors-engineering/or-stretch /or-stretch-videos
- Stork A, Bacon T, Corton M. Prevention of Work-Related Musculoskeletal Disorders in Vaginal Surgery. Video presentation at: Society of Gynecologic Surgeons’ Annual Scientific Meeting 2023, Tucson, AZ. Accessed April 3, 2023. https://sgs.eng.us/category.php?cat=2023 -video-presentations
- Aaron KA, Vaughan J, Gupta R, et al. The risk of ergonomic injury across surgical specialties. PLoS One. 2021;16:e0244868.
- Smith TG, Lowndes BR, Schmida E, et al. Course design and learning outcomes of a practical online ergonomics course for surgical residents. J Surg Educ. 2022;79:1489-1499.
- Franasiak J, Craven R, Mosaly P, et al. Feasibility and acceptance of a robotic surgery ergonomic training program. JSLS. 2014;18:e2014.00166.
- Cerier E, Hu A, Goldring A, et al. Ergonomics workshop improves musculoskeletal symptoms in general surgery residents. J Surg Res. 2022;280:567-574.
- Giagio S, Volpe G, Pillastrini P, et al. A preventive program for workrelated musculoskeletal disorders among surgeons: outcomes of a randomized controlled clinical trial. Ann Surg. 2019;270:969-975.
- Jensen MJ, Liao J, Van Gorp B, et al. Incorporating surgical ergonomics education into surgical residency curriculum. J Surg Educ. 2021;78:1209-1215.
Work-related musculoskeletal disorders (WMSDs) are “musculoskeletal disorders (injuries or disorders of the muscles, nerves, tendons, joints, cartilage, and spinal discs) in which the work environment and performance of work contribute significantly to the condition; and/or the condition is made worse or persists longer due to work conditions.”1 The health care industry has one of the highest rates of WMSDs, even when compared with traditional labor-intensive occupations, such as coal mining. In 2017, the health care industry reported more than a half million incidents of work-related injury and illness.2,3 In particular, surgeons are at increased risk for WMSDs, since they repetitively perform the classic tenets of poor ergonomics, including operating in static, extreme, and awkward positions and for prolonged periods of time.3
Gynecologic surgeons face unique ergonomic challenges. Operating in the pelvis requires an oblique approach that adds complexity and inhibits appropriate ergonomic positioning.4 All modalities of surgery incur their own challenges and risks to the surgeon, including minimally invasive gynecologic surgery (MIGS), which has become the standard of care for most conditions. Although MIGS has several benefits for the patient, a survey of gynecologic oncologists found that 88% of respondents reported discomfort related to MIGS.5 Several factors contribute to the development of WMSDs in surgery, including lack of ergonomic awareness, suboptimal ergonomic education and training,5,6 and ergonomically poor operating room (OR) equipment and instrument design.7 Furthermore, surgical culture does not generally prioritize ergonomics in the OR or requests for ergonomic accommodations.7,8
Within 5 years, a physician workforce shortage is projected for the United States.9 WMSDs contribute to workforce issues as they are associated with decreased productivity; time off needed for pain and treatment, including short-term disability; and possibly early retirement (as those who are older and have more work experience may be more likely to seek medical attention).10 In a 2013 study of vaginal surgeons, 14% missed work; 21% modified their work hours, work type, or amount of surgery; and 29% modified their surgical technique because of injury.10 Work-related pain also can negatively affect mental health, sleep, relationships, and quality of life.6
Recently, awareness has increased regarding WMSDs and their consequences, which has led to significant strides in the study of ergonomics among surgeons, a growing body of research on the topic, and guidance for optimizing ergonomics in the OR.
Risk factors for ergonomic strain
Several factors contribute to ergonomic strain and, subsequently, the development of WMSDs. Recognizing these factors can direct strategies for injury prevention.
Patient factors
The prevalence of obesity in the United States increased from 30.5% in 1999–2000 to 41.9% between 2017 and 2020.11 As the average patient’s body mass index (BMI) has increased, there is concern for a parallel increase in the ergonomic strain on laparoscopic surgeons.
A study of simulated laparoscopic tasks at varying model BMI levels demonstrated increased surgeon postural stress and workload at higher model BMIs (50 kg/m2) when compared with lower model BMIs (20 and 30 kg/m2).11 This result was supported in another study, which demonstrated both increased muscle activity and increased time needed to complete a surgical task with laparoscopic surgery; interestingly, when the same study measured these parameters for robotic surgery, this association was not seen.12 This suggests that a robotic rather than a laparoscopic approach may avoid some of the ergonomic strain associated with increased patient BMI.
Continue to: Surgeon factors...
Surgeon factors
Various surgeon characteristics have been shown to influence ergonomics in the OR. Surgeons with smaller hand sizes, for example, reported greater physical discomfort and demonstrated greater ergonomic workload when operating laparoscopically.13-15 In particular, those with a glove size of 6.5 or smaller have more difficulty using laparoscopic instruments, and those with a glove size smaller than 7 demonstrate a larger decline in grip strength when using laparoscopic instruments repeatedly.14,16
Surgeon height also can affect the amount of time spent in high-risk, nonergonomic positions. In a study that evaluated video recordings of surgeon posture during gynecologic laparoscopy, shorter surgeons were noted to use greater degrees of neck rotation to look at the monitor.17 Furthermore, surgeons with shorter arm lengths experienced more “extreme positions” of the nondominant shoulder and elbow.17 This trend also was seen in open and robotic surgery, where surgeons with a height of 66 cm or less reported increased pain scores after operating.18
Surgical instruments and OR setup
Surgical instrument characteristics can contribute to ergonomic strain, especially when the instruments have been designed with a one-size-fits-all mentality.8,19 In an examination of the anthropometric measurements of surgeon hand sizes and their correlation with difficulty when using a “standard” laparoscopic instrument, surgeons with smaller finger and hand spans had trouble using these instruments.19 Another study compared surgeon grip strength and ergonomic workloads after using 3 laparoscopic advanced bipolar instruments.16 Gender and hand size aside, the authors found that use of several of the laparoscopic devices led to greater decline in grip strength.16
The setup of the OR also can have a profound effect on the surgeon’s ergonomics. Monitor placement, for example, is crucial to ergonomic success. One study found that positioning the monitor directly in front of the surgeon at eye level was associated with the lowest neck muscle activity during a simulated task.20
Route of surgery
Each surgical approach has intrinsic ergonomic risks. With laparoscopy, surgeons often remain in straight head and back positions without much trunk motion, especially when compared with open surgery.21 In one study, laparoscopic surgeons spent more than 60% of a case in a static position and more than 80% of a case in a high-risk, “demanding” neck position.22
Robotic surgery, in contrast to laparoscopy, often has been cited as being more “ergonomic.” While robotic surgery has less of an effect on the neck, shoulders, arms, and legs than laparoscopy23 and often is associated with less physical discomfort than either open or laparoscopic surgery,23,24 robotic surgery still maintains its own innate ergonomic risks. Of robotic surgeons surveyed, 56.1% reported neck stiffness, finger fatigue, and eye symptoms in one study.25 In another survey study, more robotic surgeons (72%) reported physical symptoms than laparoscopic (57%) and open (49%) surgeons.26Vaginal surgery also puts surgeons at ergonomic risk. A majority of surgeons (87.2%) who completed more than 50% of their cases vaginally reported a history of WMSDs.10 Vaginal surgery places surgeons in awkward positions of the neck, shoulder, and trunk frequently and for longer durations.27
Continue to: Strategies for preventing WMSDs...
Strategies for preventing WMSDs
As factors that contribute to the development of WMSDs are identified, preventive strategies can be targeted to these individual factors. Research has focused on appropriate setup of the OR, surgeon posture, intraoperative microbreaks, and stretching both in and outside of the OR.
1. OR setup and positioning of the surgeon by MIGS route
The route of MIGS affects OR setup and surgeon posture. Ergonomic recommendations for laparoscopy, robotic surgery, and vaginal surgery are all unique to the risks posed by each particular approach.
Laparoscopic surgery. Laparoscopic monitors should face the surgeon directly, with the screen just below eye level to maintain the surgeon’s neck in a neutral position.28 The table height should be set for the tallest surgeon, and shorter surgeons should stand on steps as needed.28 The table height also should allow for the surgeon’s hands to be at elbow height, with the elbows bent at 90 degrees with the wrists straight.29 Foot pedals should be placed at the surgeons’ foot level and should be reached easily.28 Additionally, the patient’s arms should be tucked at their sides to allow surgeons a larger operative space.29 When using laparoscopic instruments, locking and ratcheting features should be used whenever possible to reduce prolonged grip or squeeze forces.28 The laparoscopic camera should be held in the palm with the wrist in a neutral position.29
Robotic surgery. Positioning and setup of the robotic console is a main focus of ergonomic recommendations. The surgeon’s chair should be brought as close to the console as possible, and the knees positioned in a 90-degree angle.30 The foot pedals should be brought toward the surgeon to maintain this angle of the knees.30 The console should be rotated toward the surgeon and then the height adjusted so that the surgeon can look through the eyepiece while sitting upright and can maintain the neck in a neutral position.28,30 The surgeon’s forehead should rest comfortably on the headrest.29 The forearms should rest on the armrest while the arms are maintained in a neutral position and the shoulders remain relaxed while the surgeon holds the robotic controls.30 It is important to utilize the armrest often to relieve stress on the arm while operating.28 Frequent use of the clutch function can keep the robotic controls in the center of the workspace.28
Vaginal surgery. Both seated and standing positions are associated with high-risk positioning of the trunk and bilateral shoulders, respectively, in vaginal surgery.31 However, surgeons who stand while operating vaginally reported more discomfort in the bilateral wrists, thighs, and lower legs than those who operated while seated.31 This suggests a potential ergonomic advantage to the seated position for vaginal surgery. Chair height should be adjusted so the surgeon can look straight ahead with the neck in a neutral position.32 Surgeons should consider using a headlamp, as this may prevent repetitive awkward movements to adjust overhead lights.32 For standing surgery, the table height should be adjusted for the tallest surgeon, and shorter surgeons or assistants should use steps as needed.3
Surgical assistants should switch sides during the course of the case to avoid excessive unilateral upper-extremity strain.32 The addition of a table-mounted vaginal retractor system may be useful in relieving physical strain for surgical assistants, but data currently are lacking to demonstrate this ergonomic benefit.33 Further studies are needed, especially since many surgeons take on the role of surgical assist in the teaching environment and subsequently report more WMSDs than their colleagues who do not work in teaching environments.10,34
2. Pain relief from individual ergonomic positioning devices
Apart from adjusting how the OR equipment is arranged or how the surgeons adjust their positioning, several devices that assist with surgeon positioning—including gel mats or insoles, exoskeletons, and “augmented reality” glasses—are being studied.
The use of gel mats or insoles in the OR has mixed evidence in the literature.35-37
Exoskeletons, external devices that support a surgeon’s posture and positioning, have been studied thus far in simulated nonsterile surgical environments. Preliminarily, it appears that use of an exoskeleton can decrease muscle activity and time spent in static positions, with a reported decrease in post-task user discomfort.38,39 More data are needed to determine if exoskeletons can be used in the sterile setting and for longer durations as may occur in actual OR cases.
Augmented reality glasses project the laparoscopic monitor image to the glasses, which frees the surgeon to place the “monitor” in a more neutral, ergonomic position. In one study, use of augmented reality glasses was associated with decreased muscle activity and a reduction in Rapid Entire Body Assessment (REBA) scores when compared with use of the conventional laparoscopic monitor.40More data are needed on these emerging technologies to determine whether adverse effects occur with prolonged use.
Continue to: 3. Implementing intraoperative microbreaks and stretching...
3. Implementing intraoperative microbreaks and stretching
The American College of Surgeons (ACS) recommends that surgeons avoid prolonged static postures during procedures.28 One strategy for preventing sustained positioning is to incorporate breaks with associated stretching routinely during surgery.28
Microbreaks. In a landmark study by Park and colleagues in 2017, 120-second long targeted stretching microbreaks (TSMBs) were completed every 20 to 40 minutes during a surgery, and results demonstrated improved postoperative surgeon pain scores without an associated increase in the length of the case.41 These surgeons reported improved pain in the neck, bilateral shoulders, bilateral hands, and lower back. Eighty-eight percent of surgeons reported either improvement or “no change” in their mental focus, and 100% reported improvement or “no change” in their physical performance after TSMBs were implemented.42 Of surveyed surgeons, 87% wanted TSMBs incorporated routinely.41,42
Stretches. Multiple resources, such as the ACS and the Mayo Clinic, for intraoperative stretches are available. The ACS recommends performing neck and shoulder stretches during intraoperative microbreaks, including a range-of-movement neck exercise, deep cervical flexor training, and standing scapular retraction.28 The ACS also demonstrates lumbrical stretches for the fingers and passive wrist extension exercises to be used intraoperatively (or between cases) (FIGURE 1).28 The Mayo Clinic Hallbeck Human Factors Engineering Laboratories has a publicly available “OR Stretch Instructional Video” in which the surgeon is guided through several different short stretches, including shoulder shrugging and side bends, that can be used during surgery.43
Both the ACS and the Mayo Clinic provide examples of pertinent stretch exercises for use when not in the sterile environment, between cases or after cases are complete. The ACS recommends several neck and shoulder stretches for the trapezius, levator scapulae, and pectoralis and recommends the use of a foam roller to improve thoracic mobility (FIGURE 2).28 As above, the Mayo Clinic Hallbeck Human Factors Engineering Laboratories has a publicly available “OR-Stretch Between Surgery Stretches Video” in which the surgeon is guided through several short stretches that are done in a seated position, including stretches for the hamstring, lower back, and arms (FIGURE 3).43
Many of the above-mentioned stretches were designed for use in the context of open, laparoscopic, or robotic surgery. For the vaginal surgeon, the intraoperative ergonomic stressors differ from those of other routes of surgery, and thus stretches tailored to the positioning during vaginal surgery are necessary. In a video recently published by the Society of Gynecologic Surgeons, several stretches are reviewed that target high-risk positions often held by the surgeon or assistant when operating vaginally.44 These stretches include cervical retraction, thoracic extension, external arm rotation, cervical side bending, and lumbar extension (FIGURE 4).44 The recommendation is to complete these exercises 2 times per day, with 8 to 10 repetitions per set.44
Prioritizing ergonomic awareness and training
As caregivers, it is not uncommon for us to prioritize the needs of others before those of ourselves. However, WMSDs are prevalent, and their downstream effects may cause catastrophic professional and personal losses. Cumulatively, the global impact of WMSDs is a significant issue for the health care workforce and its longevity.
To prevent WMSDs, it is imperative that surgeons are aware of the factors that contribute to injury development and the appropriate, accessible modifications for these factors. While each surgical modality confers its own ergonomic challenges, these risks can be mitigated through increased awareness of OR setup, surgeon positioning, and incorporation of microbreaks and stretching exercises during and after surgical procedures.
Formal training in surgical ergonomics is lacking across specialties, including gynecology.45 Multiple educational interventions have been proposed and studied to help fill this training gap.30,46-49When used, these interventions have been associated with increased knowledge of surgical ergonomic principles or reduction in surgeon pain scores, including trainees.50 As we become more cognizant of WMSDs, standardized resident curricula should be developed in an effort to reduce the prevalence of these potentially career-ending injuries.
In addition to education, cultivating a culture in which ergonomics is prioritized is essential. Although most surgeons report work-related pain, very few report their injuries to occupational health. For example, while 29% of gynecologic oncologists reported seeking treatment for a WMSD, only 1% had reported their injury to their employer.5 In a study of ACS members, only 19% of injuries were reported, 30% of surgeons stated that they did not know how to report an injury, and 21% felt that the resources for surgeons during and after an injury were inadequate.6
As we prioritize the health and safety of our patients, we also need to promote ergonomic awareness in the OR, respect the need for accommodations, encourage injury reporting, support surgeons who need to take time away for medical treatment, and partner with industry to develop new instruments and technology with effective ergonomic features. ●
Work-related musculoskeletal disorders (WMSDs) are “musculoskeletal disorders (injuries or disorders of the muscles, nerves, tendons, joints, cartilage, and spinal discs) in which the work environment and performance of work contribute significantly to the condition; and/or the condition is made worse or persists longer due to work conditions.”1 The health care industry has one of the highest rates of WMSDs, even when compared with traditional labor-intensive occupations, such as coal mining. In 2017, the health care industry reported more than a half million incidents of work-related injury and illness.2,3 In particular, surgeons are at increased risk for WMSDs, since they repetitively perform the classic tenets of poor ergonomics, including operating in static, extreme, and awkward positions and for prolonged periods of time.3
Gynecologic surgeons face unique ergonomic challenges. Operating in the pelvis requires an oblique approach that adds complexity and inhibits appropriate ergonomic positioning.4 All modalities of surgery incur their own challenges and risks to the surgeon, including minimally invasive gynecologic surgery (MIGS), which has become the standard of care for most conditions. Although MIGS has several benefits for the patient, a survey of gynecologic oncologists found that 88% of respondents reported discomfort related to MIGS.5 Several factors contribute to the development of WMSDs in surgery, including lack of ergonomic awareness, suboptimal ergonomic education and training,5,6 and ergonomically poor operating room (OR) equipment and instrument design.7 Furthermore, surgical culture does not generally prioritize ergonomics in the OR or requests for ergonomic accommodations.7,8
Within 5 years, a physician workforce shortage is projected for the United States.9 WMSDs contribute to workforce issues as they are associated with decreased productivity; time off needed for pain and treatment, including short-term disability; and possibly early retirement (as those who are older and have more work experience may be more likely to seek medical attention).10 In a 2013 study of vaginal surgeons, 14% missed work; 21% modified their work hours, work type, or amount of surgery; and 29% modified their surgical technique because of injury.10 Work-related pain also can negatively affect mental health, sleep, relationships, and quality of life.6
Recently, awareness has increased regarding WMSDs and their consequences, which has led to significant strides in the study of ergonomics among surgeons, a growing body of research on the topic, and guidance for optimizing ergonomics in the OR.
Risk factors for ergonomic strain
Several factors contribute to ergonomic strain and, subsequently, the development of WMSDs. Recognizing these factors can direct strategies for injury prevention.
Patient factors
The prevalence of obesity in the United States increased from 30.5% in 1999–2000 to 41.9% between 2017 and 2020.11 As the average patient’s body mass index (BMI) has increased, there is concern for a parallel increase in the ergonomic strain on laparoscopic surgeons.
A study of simulated laparoscopic tasks at varying model BMI levels demonstrated increased surgeon postural stress and workload at higher model BMIs (50 kg/m2) when compared with lower model BMIs (20 and 30 kg/m2).11 This result was supported in another study, which demonstrated both increased muscle activity and increased time needed to complete a surgical task with laparoscopic surgery; interestingly, when the same study measured these parameters for robotic surgery, this association was not seen.12 This suggests that a robotic rather than a laparoscopic approach may avoid some of the ergonomic strain associated with increased patient BMI.
Continue to: Surgeon factors...
Surgeon factors
Various surgeon characteristics have been shown to influence ergonomics in the OR. Surgeons with smaller hand sizes, for example, reported greater physical discomfort and demonstrated greater ergonomic workload when operating laparoscopically.13-15 In particular, those with a glove size of 6.5 or smaller have more difficulty using laparoscopic instruments, and those with a glove size smaller than 7 demonstrate a larger decline in grip strength when using laparoscopic instruments repeatedly.14,16
Surgeon height also can affect the amount of time spent in high-risk, nonergonomic positions. In a study that evaluated video recordings of surgeon posture during gynecologic laparoscopy, shorter surgeons were noted to use greater degrees of neck rotation to look at the monitor.17 Furthermore, surgeons with shorter arm lengths experienced more “extreme positions” of the nondominant shoulder and elbow.17 This trend also was seen in open and robotic surgery, where surgeons with a height of 66 cm or less reported increased pain scores after operating.18
Surgical instruments and OR setup
Surgical instrument characteristics can contribute to ergonomic strain, especially when the instruments have been designed with a one-size-fits-all mentality.8,19 In an examination of the anthropometric measurements of surgeon hand sizes and their correlation with difficulty when using a “standard” laparoscopic instrument, surgeons with smaller finger and hand spans had trouble using these instruments.19 Another study compared surgeon grip strength and ergonomic workloads after using 3 laparoscopic advanced bipolar instruments.16 Gender and hand size aside, the authors found that use of several of the laparoscopic devices led to greater decline in grip strength.16
The setup of the OR also can have a profound effect on the surgeon’s ergonomics. Monitor placement, for example, is crucial to ergonomic success. One study found that positioning the monitor directly in front of the surgeon at eye level was associated with the lowest neck muscle activity during a simulated task.20
Route of surgery
Each surgical approach has intrinsic ergonomic risks. With laparoscopy, surgeons often remain in straight head and back positions without much trunk motion, especially when compared with open surgery.21 In one study, laparoscopic surgeons spent more than 60% of a case in a static position and more than 80% of a case in a high-risk, “demanding” neck position.22
Robotic surgery, in contrast to laparoscopy, often has been cited as being more “ergonomic.” While robotic surgery has less of an effect on the neck, shoulders, arms, and legs than laparoscopy23 and often is associated with less physical discomfort than either open or laparoscopic surgery,23,24 robotic surgery still maintains its own innate ergonomic risks. Of robotic surgeons surveyed, 56.1% reported neck stiffness, finger fatigue, and eye symptoms in one study.25 In another survey study, more robotic surgeons (72%) reported physical symptoms than laparoscopic (57%) and open (49%) surgeons.26Vaginal surgery also puts surgeons at ergonomic risk. A majority of surgeons (87.2%) who completed more than 50% of their cases vaginally reported a history of WMSDs.10 Vaginal surgery places surgeons in awkward positions of the neck, shoulder, and trunk frequently and for longer durations.27
Continue to: Strategies for preventing WMSDs...
Strategies for preventing WMSDs
As factors that contribute to the development of WMSDs are identified, preventive strategies can be targeted to these individual factors. Research has focused on appropriate setup of the OR, surgeon posture, intraoperative microbreaks, and stretching both in and outside of the OR.
1. OR setup and positioning of the surgeon by MIGS route
The route of MIGS affects OR setup and surgeon posture. Ergonomic recommendations for laparoscopy, robotic surgery, and vaginal surgery are all unique to the risks posed by each particular approach.
Laparoscopic surgery. Laparoscopic monitors should face the surgeon directly, with the screen just below eye level to maintain the surgeon’s neck in a neutral position.28 The table height should be set for the tallest surgeon, and shorter surgeons should stand on steps as needed.28 The table height also should allow for the surgeon’s hands to be at elbow height, with the elbows bent at 90 degrees with the wrists straight.29 Foot pedals should be placed at the surgeons’ foot level and should be reached easily.28 Additionally, the patient’s arms should be tucked at their sides to allow surgeons a larger operative space.29 When using laparoscopic instruments, locking and ratcheting features should be used whenever possible to reduce prolonged grip or squeeze forces.28 The laparoscopic camera should be held in the palm with the wrist in a neutral position.29
Robotic surgery. Positioning and setup of the robotic console is a main focus of ergonomic recommendations. The surgeon’s chair should be brought as close to the console as possible, and the knees positioned in a 90-degree angle.30 The foot pedals should be brought toward the surgeon to maintain this angle of the knees.30 The console should be rotated toward the surgeon and then the height adjusted so that the surgeon can look through the eyepiece while sitting upright and can maintain the neck in a neutral position.28,30 The surgeon’s forehead should rest comfortably on the headrest.29 The forearms should rest on the armrest while the arms are maintained in a neutral position and the shoulders remain relaxed while the surgeon holds the robotic controls.30 It is important to utilize the armrest often to relieve stress on the arm while operating.28 Frequent use of the clutch function can keep the robotic controls in the center of the workspace.28
Vaginal surgery. Both seated and standing positions are associated with high-risk positioning of the trunk and bilateral shoulders, respectively, in vaginal surgery.31 However, surgeons who stand while operating vaginally reported more discomfort in the bilateral wrists, thighs, and lower legs than those who operated while seated.31 This suggests a potential ergonomic advantage to the seated position for vaginal surgery. Chair height should be adjusted so the surgeon can look straight ahead with the neck in a neutral position.32 Surgeons should consider using a headlamp, as this may prevent repetitive awkward movements to adjust overhead lights.32 For standing surgery, the table height should be adjusted for the tallest surgeon, and shorter surgeons or assistants should use steps as needed.3
Surgical assistants should switch sides during the course of the case to avoid excessive unilateral upper-extremity strain.32 The addition of a table-mounted vaginal retractor system may be useful in relieving physical strain for surgical assistants, but data currently are lacking to demonstrate this ergonomic benefit.33 Further studies are needed, especially since many surgeons take on the role of surgical assist in the teaching environment and subsequently report more WMSDs than their colleagues who do not work in teaching environments.10,34
2. Pain relief from individual ergonomic positioning devices
Apart from adjusting how the OR equipment is arranged or how the surgeons adjust their positioning, several devices that assist with surgeon positioning—including gel mats or insoles, exoskeletons, and “augmented reality” glasses—are being studied.
The use of gel mats or insoles in the OR has mixed evidence in the literature.35-37
Exoskeletons, external devices that support a surgeon’s posture and positioning, have been studied thus far in simulated nonsterile surgical environments. Preliminarily, it appears that use of an exoskeleton can decrease muscle activity and time spent in static positions, with a reported decrease in post-task user discomfort.38,39 More data are needed to determine if exoskeletons can be used in the sterile setting and for longer durations as may occur in actual OR cases.
Augmented reality glasses project the laparoscopic monitor image to the glasses, which frees the surgeon to place the “monitor” in a more neutral, ergonomic position. In one study, use of augmented reality glasses was associated with decreased muscle activity and a reduction in Rapid Entire Body Assessment (REBA) scores when compared with use of the conventional laparoscopic monitor.40More data are needed on these emerging technologies to determine whether adverse effects occur with prolonged use.
Continue to: 3. Implementing intraoperative microbreaks and stretching...
3. Implementing intraoperative microbreaks and stretching
The American College of Surgeons (ACS) recommends that surgeons avoid prolonged static postures during procedures.28 One strategy for preventing sustained positioning is to incorporate breaks with associated stretching routinely during surgery.28
Microbreaks. In a landmark study by Park and colleagues in 2017, 120-second long targeted stretching microbreaks (TSMBs) were completed every 20 to 40 minutes during a surgery, and results demonstrated improved postoperative surgeon pain scores without an associated increase in the length of the case.41 These surgeons reported improved pain in the neck, bilateral shoulders, bilateral hands, and lower back. Eighty-eight percent of surgeons reported either improvement or “no change” in their mental focus, and 100% reported improvement or “no change” in their physical performance after TSMBs were implemented.42 Of surveyed surgeons, 87% wanted TSMBs incorporated routinely.41,42
Stretches. Multiple resources, such as the ACS and the Mayo Clinic, for intraoperative stretches are available. The ACS recommends performing neck and shoulder stretches during intraoperative microbreaks, including a range-of-movement neck exercise, deep cervical flexor training, and standing scapular retraction.28 The ACS also demonstrates lumbrical stretches for the fingers and passive wrist extension exercises to be used intraoperatively (or between cases) (FIGURE 1).28 The Mayo Clinic Hallbeck Human Factors Engineering Laboratories has a publicly available “OR Stretch Instructional Video” in which the surgeon is guided through several different short stretches, including shoulder shrugging and side bends, that can be used during surgery.43
Both the ACS and the Mayo Clinic provide examples of pertinent stretch exercises for use when not in the sterile environment, between cases or after cases are complete. The ACS recommends several neck and shoulder stretches for the trapezius, levator scapulae, and pectoralis and recommends the use of a foam roller to improve thoracic mobility (FIGURE 2).28 As above, the Mayo Clinic Hallbeck Human Factors Engineering Laboratories has a publicly available “OR-Stretch Between Surgery Stretches Video” in which the surgeon is guided through several short stretches that are done in a seated position, including stretches for the hamstring, lower back, and arms (FIGURE 3).43
Many of the above-mentioned stretches were designed for use in the context of open, laparoscopic, or robotic surgery. For the vaginal surgeon, the intraoperative ergonomic stressors differ from those of other routes of surgery, and thus stretches tailored to the positioning during vaginal surgery are necessary. In a video recently published by the Society of Gynecologic Surgeons, several stretches are reviewed that target high-risk positions often held by the surgeon or assistant when operating vaginally.44 These stretches include cervical retraction, thoracic extension, external arm rotation, cervical side bending, and lumbar extension (FIGURE 4).44 The recommendation is to complete these exercises 2 times per day, with 8 to 10 repetitions per set.44
Prioritizing ergonomic awareness and training
As caregivers, it is not uncommon for us to prioritize the needs of others before those of ourselves. However, WMSDs are prevalent, and their downstream effects may cause catastrophic professional and personal losses. Cumulatively, the global impact of WMSDs is a significant issue for the health care workforce and its longevity.
To prevent WMSDs, it is imperative that surgeons are aware of the factors that contribute to injury development and the appropriate, accessible modifications for these factors. While each surgical modality confers its own ergonomic challenges, these risks can be mitigated through increased awareness of OR setup, surgeon positioning, and incorporation of microbreaks and stretching exercises during and after surgical procedures.
Formal training in surgical ergonomics is lacking across specialties, including gynecology.45 Multiple educational interventions have been proposed and studied to help fill this training gap.30,46-49When used, these interventions have been associated with increased knowledge of surgical ergonomic principles or reduction in surgeon pain scores, including trainees.50 As we become more cognizant of WMSDs, standardized resident curricula should be developed in an effort to reduce the prevalence of these potentially career-ending injuries.
In addition to education, cultivating a culture in which ergonomics is prioritized is essential. Although most surgeons report work-related pain, very few report their injuries to occupational health. For example, while 29% of gynecologic oncologists reported seeking treatment for a WMSD, only 1% had reported their injury to their employer.5 In a study of ACS members, only 19% of injuries were reported, 30% of surgeons stated that they did not know how to report an injury, and 21% felt that the resources for surgeons during and after an injury were inadequate.6
As we prioritize the health and safety of our patients, we also need to promote ergonomic awareness in the OR, respect the need for accommodations, encourage injury reporting, support surgeons who need to take time away for medical treatment, and partner with industry to develop new instruments and technology with effective ergonomic features. ●
- Workplace health glossary. Reviewed February 12, 2020. Centers for Disease Control and Prevention. Accessed May 18, 2023. https://www.cdc.gov/workplacehealthpromotion/tools-resources /glossary/glossary.html#W
- Epstein S, Sparer EH, Tran BN, et al. Prevalence of work-related musculoskeletal disorders among surgeons and interventionalists: a systematic review and meta-analysis. JAMA Surg. 2018;153:e174947.
- Yurteri-Kaplan LA, Park AJ. Surgical ergonomics and preventing workrelated musculoskeletal disorders. Obstet Gynecol. 2023;141:455-462.
- Symer MM, Keller DS. Human factors in pelvic surgery. Eur J Surg Oncol. 2022;48:2346-2351.
- Franasiak J, Ko EM, Kidd J, et al. Physical strain and urgent need for ergonomic training among gynecologic oncologists who perform minimally invasive surgery. Gynecol Oncol. 2012;126:437-442.
- Davis WT, Fletcher SA, Guillamondegui OD. Musculoskeletal occupational injury among surgeons: effects for patients, providers, and institutions. J Surg Res. 2014;189:207-212.e6.
- Fox M. Surgeons face unique ergonomic challenges. American College of Surgeons. September 1, 2022. Accessed May 22, 2023. https://www.facs.org/for-medical-professionals/news-publications /news-and-articles/bulletin/september-2022-volume-107-issue-9 /surgeons-face-unique-ergonomic-challenges/
- Wong JMK, Carey ET, King C, et al. A call to action for ergonomic surgical devices designed for diverse surgeon end users. Obstet Gynecol. 2023;141:463-466.
- IHS Inc. The Complexities of Physician Supply and Demand: Projections from 2014 to 2025. Association of American Medical Colleges. April 5, 2016.
- Kim-Fine S, Woolley SM, Weaver AL, et al. Work-related musculoskeletal disorders among vaginal surgeons. Int Urogynecol J. 2013;24:1191-1200.
- Sers R, Forrester S, Zecca M, et al. The ergonomic impact of patient body mass index on surgeon posture during simulated laparoscopy. Appl Ergon. 2021;97:103501.
- Moss EL, Sarhanis P, Ind T, et al. Impact of obesity on surgeon ergonomics in robotic and straight-stick laparoscopic surgery. J Minim Invasive Gynecol. 2020;27:1063-1069.
- Sutton E, Irvin M, Zeigler C, et al. The ergonomics of women in surgery. Surg Endosc. 2014;28:1051-1055.
- Berguer R, Hreljac A. The relationship between hand size and difficulty using surgical instruments: a survey of 726 laparoscopic surgeons. Surg Endosc. 2004;18:508-512.
- Bellini MI, Amabile MI, Saullo P, et al. A woman’s place is in theatre, but are theatres designed with women in mind? A systematic review of ergonomics for women in surgery. J Clin Med. 2022;11:3496.
- Wong JMK, Moore KJ, Lewis P, et al. Ergonomic assessment of surgeon characteristics and laparoscopic device strain in gynecologic surgery. J Minim Invasive Gynecol. 2022;29:1357-1363.
- Aitchison LP, Cui CK, Arnold A, et al. The ergonomics of laparoscopic surgery: a quantitative study of the time and motion of laparoscopic surgeons in live surgical environments. Surg Endosc. 2016;30:5068-5076.
- Stewart C, Raoof M, Fong Y, et al. Who is hurting? A prospective study of surgeon ergonomics. Surg Endosc. 2022;36:292-299.
- Green SV, Morris DE, Naumann DN, et al. One size does not fit all: impact of hand size on ease of use of instruments for minimally invasive surgery. Surgeon. 2022;S1479-666X(22)00131-7.
- Matern U, Faist M, Kehl K, et al. Monitor position in laparoscopic surgery. Surg Endosc. 2005;19:436-440.
- Berguer R, Rab GT, Abu-Ghaida H, et al. A comparison of surgeons’ posture during laparoscopic and open surgical procedures. Surg Endosc. 1997;11:139-142.
- Athanasiadis DI, Monfared S, Asadi H, et al. An analysis of the ergonomic risk of surgical trainees and experienced surgeons during laparoscopic procedures. Surgery. 2021;169:496-501.
- Hotton J, Bogart E, Le Deley MC, et al. Ergonomic assessment of the surgeon’s physical workload during robot-assisted versus standard laparoscopy in a French multicenter randomized trial (ROBOGYN-1004 Trial). Ann Surg Oncol. 2023;30:916-923.
- Plerhoples TA, Hernandez-Boussard T, Wren SM. The aching surgeon: a survey of physical discomfort and symptoms following open, laparoscopic, and robotic surgery. J Robot Surg. 2012;6:65-72.
- Lee GI, Lee MR, Green I, et al. Surgeons’ physical discomfort and symptoms during robotic surgery: a comprehensive ergonomic survey study. Surg Endosc. 2017;31:1697-1706.
- McDonald ME, Ramirez PT, Munsell MF, et al. Physician pain and discomfort during minimally invasive gynecologic cancer surgery. Gynecol Oncol. 2014;134:243-247.
- Zhu X, Yurteri-Kaplan LA, Gutman RE, et al. Postural stress experienced by vaginal surgeons. Proc Hum Factors Ergonomics Soc Annu Meet. 2014;58:763-767.
- American College of Surgeons Division of Education and Surgical Ergonomics Committee. Surgical Ergonomics Recommendations. ACS Education. 2022.
- Cardenas-Trowers O, Kjellsson K, Hatch K. Ergonomics: making the OR a comfortable place. Int Urogynecol J. 2018;29:1065-1066.
- Hokenstad ED, Hallbeck MS, Lowndes BR, et al. Ergonomic robotic console configuration in gynecologic surgery: an interventional study. J Minim Invasive Gynecol. 2021;28:850-859.
- Singh R, Yurteri-Kaplan LA, Morrow MM, et al. Sitting versus standing makes a difference in musculoskeletal discomfort and postural load for surgeons performing vaginal surgery. Int Urogynecol J. 2019;30:231-237.
- Hullfish KL, Trowbridge ER, Bodine G. Ergonomics and gynecologic surgery: “surgeon protect thyself.” J Pelvic Med Surg. 2009;15:435-439.
- Woodburn KL, Kho RM. Vaginal surgery: don’t get bent out of shape. Am J Obstet Gynecol. 2020;223:762-763.
- Hobson DTG, Meriwether KV, Gaskins JT, et al. Learner satisfaction and experience with a high-definition telescopic camera during vaginal procedures: a randomized controlled trial. Female Pelvic Med Reconstr Surg. 2021;27:105-111.
- Speed G, Harris K, Keegel T. The effect of cushioning materials on musculoskeletal discomfort and fatigue during prolonged standing at work: a systematic review. Appl Ergon. 2018;70:300-334.
- Haramis G, Rosales JC, Palacios JM, et al. Prospective randomized evaluation of FOOT gel pads for operating room staff COMFORT during laparoscopic renal surgery. Urology. 2010;76:1405-1408.
- Voss RK, Chiang YJ, Cromwell KD, et al. Do no harm, except to ourselves? A survey of symptoms and injuries in oncologic surgeons and pilot study of an intraoperative ergonomic intervention. J Am Coll Surg. 2017;224:16-25.e1.
- Marquetand J, Gabriel J, Seibt R, et al. Ergonomics for surgeons—prototype of an external surgeon support system reduces muscular activity and fatigue. J Electromyogr Kinesiol. 2021;60:102586.
- Tetteh E, Hallbeck MS, Mirka GA. Effects of passive exoskeleton support on EMG measures of the neck, shoulder and trunk muscles while holding simulated surgical postures and performing a simulated surgical procedure. Appl Ergon. 2022;100:103646.
- Lim AK, Ryu J, Yoon HM, et al. Ergonomic effects of medical augmented reality glasses in video-assisted surgery. Surg Endosc. 2022;36:988-998.
- Park AE, Zahiri HR, Hallbeck MS, et al. Intraoperative “micro breaks” with targeted stretching enhance surgeon physical function and mental focus: a multicenter cohort study. Ann Surg. 2017;265:340-346.
- Hallbeck MS, Lowndes BR, Bingener J, et al. The impact of intraoperative microbreaks with exercises on surgeons: a multi-center cohort study. Appl Ergon. 2017;60:334-341.
- Hallbeck Human Factors Engineering Laboratories. OR Stretch Videos. Mayo Clinic, 2018. Accessed May 19, 2023. https://www.mayo .edu/research/labs/human-factors-engineering/or-stretch /or-stretch-videos
- Stork A, Bacon T, Corton M. Prevention of Work-Related Musculoskeletal Disorders in Vaginal Surgery. Video presentation at: Society of Gynecologic Surgeons’ Annual Scientific Meeting 2023, Tucson, AZ. Accessed April 3, 2023. https://sgs.eng.us/category.php?cat=2023 -video-presentations
- Aaron KA, Vaughan J, Gupta R, et al. The risk of ergonomic injury across surgical specialties. PLoS One. 2021;16:e0244868.
- Smith TG, Lowndes BR, Schmida E, et al. Course design and learning outcomes of a practical online ergonomics course for surgical residents. J Surg Educ. 2022;79:1489-1499.
- Franasiak J, Craven R, Mosaly P, et al. Feasibility and acceptance of a robotic surgery ergonomic training program. JSLS. 2014;18:e2014.00166.
- Cerier E, Hu A, Goldring A, et al. Ergonomics workshop improves musculoskeletal symptoms in general surgery residents. J Surg Res. 2022;280:567-574.
- Giagio S, Volpe G, Pillastrini P, et al. A preventive program for workrelated musculoskeletal disorders among surgeons: outcomes of a randomized controlled clinical trial. Ann Surg. 2019;270:969-975.
- Jensen MJ, Liao J, Van Gorp B, et al. Incorporating surgical ergonomics education into surgical residency curriculum. J Surg Educ. 2021;78:1209-1215.
- Workplace health glossary. Reviewed February 12, 2020. Centers for Disease Control and Prevention. Accessed May 18, 2023. https://www.cdc.gov/workplacehealthpromotion/tools-resources /glossary/glossary.html#W
- Epstein S, Sparer EH, Tran BN, et al. Prevalence of work-related musculoskeletal disorders among surgeons and interventionalists: a systematic review and meta-analysis. JAMA Surg. 2018;153:e174947.
- Yurteri-Kaplan LA, Park AJ. Surgical ergonomics and preventing workrelated musculoskeletal disorders. Obstet Gynecol. 2023;141:455-462.
- Symer MM, Keller DS. Human factors in pelvic surgery. Eur J Surg Oncol. 2022;48:2346-2351.
- Franasiak J, Ko EM, Kidd J, et al. Physical strain and urgent need for ergonomic training among gynecologic oncologists who perform minimally invasive surgery. Gynecol Oncol. 2012;126:437-442.
- Davis WT, Fletcher SA, Guillamondegui OD. Musculoskeletal occupational injury among surgeons: effects for patients, providers, and institutions. J Surg Res. 2014;189:207-212.e6.
- Fox M. Surgeons face unique ergonomic challenges. American College of Surgeons. September 1, 2022. Accessed May 22, 2023. https://www.facs.org/for-medical-professionals/news-publications /news-and-articles/bulletin/september-2022-volume-107-issue-9 /surgeons-face-unique-ergonomic-challenges/
- Wong JMK, Carey ET, King C, et al. A call to action for ergonomic surgical devices designed for diverse surgeon end users. Obstet Gynecol. 2023;141:463-466.
- IHS Inc. The Complexities of Physician Supply and Demand: Projections from 2014 to 2025. Association of American Medical Colleges. April 5, 2016.
- Kim-Fine S, Woolley SM, Weaver AL, et al. Work-related musculoskeletal disorders among vaginal surgeons. Int Urogynecol J. 2013;24:1191-1200.
- Sers R, Forrester S, Zecca M, et al. The ergonomic impact of patient body mass index on surgeon posture during simulated laparoscopy. Appl Ergon. 2021;97:103501.
- Moss EL, Sarhanis P, Ind T, et al. Impact of obesity on surgeon ergonomics in robotic and straight-stick laparoscopic surgery. J Minim Invasive Gynecol. 2020;27:1063-1069.
- Sutton E, Irvin M, Zeigler C, et al. The ergonomics of women in surgery. Surg Endosc. 2014;28:1051-1055.
- Berguer R, Hreljac A. The relationship between hand size and difficulty using surgical instruments: a survey of 726 laparoscopic surgeons. Surg Endosc. 2004;18:508-512.
- Bellini MI, Amabile MI, Saullo P, et al. A woman’s place is in theatre, but are theatres designed with women in mind? A systematic review of ergonomics for women in surgery. J Clin Med. 2022;11:3496.
- Wong JMK, Moore KJ, Lewis P, et al. Ergonomic assessment of surgeon characteristics and laparoscopic device strain in gynecologic surgery. J Minim Invasive Gynecol. 2022;29:1357-1363.
- Aitchison LP, Cui CK, Arnold A, et al. The ergonomics of laparoscopic surgery: a quantitative study of the time and motion of laparoscopic surgeons in live surgical environments. Surg Endosc. 2016;30:5068-5076.
- Stewart C, Raoof M, Fong Y, et al. Who is hurting? A prospective study of surgeon ergonomics. Surg Endosc. 2022;36:292-299.
- Green SV, Morris DE, Naumann DN, et al. One size does not fit all: impact of hand size on ease of use of instruments for minimally invasive surgery. Surgeon. 2022;S1479-666X(22)00131-7.
- Matern U, Faist M, Kehl K, et al. Monitor position in laparoscopic surgery. Surg Endosc. 2005;19:436-440.
- Berguer R, Rab GT, Abu-Ghaida H, et al. A comparison of surgeons’ posture during laparoscopic and open surgical procedures. Surg Endosc. 1997;11:139-142.
- Athanasiadis DI, Monfared S, Asadi H, et al. An analysis of the ergonomic risk of surgical trainees and experienced surgeons during laparoscopic procedures. Surgery. 2021;169:496-501.
- Hotton J, Bogart E, Le Deley MC, et al. Ergonomic assessment of the surgeon’s physical workload during robot-assisted versus standard laparoscopy in a French multicenter randomized trial (ROBOGYN-1004 Trial). Ann Surg Oncol. 2023;30:916-923.
- Plerhoples TA, Hernandez-Boussard T, Wren SM. The aching surgeon: a survey of physical discomfort and symptoms following open, laparoscopic, and robotic surgery. J Robot Surg. 2012;6:65-72.
- Lee GI, Lee MR, Green I, et al. Surgeons’ physical discomfort and symptoms during robotic surgery: a comprehensive ergonomic survey study. Surg Endosc. 2017;31:1697-1706.
- McDonald ME, Ramirez PT, Munsell MF, et al. Physician pain and discomfort during minimally invasive gynecologic cancer surgery. Gynecol Oncol. 2014;134:243-247.
- Zhu X, Yurteri-Kaplan LA, Gutman RE, et al. Postural stress experienced by vaginal surgeons. Proc Hum Factors Ergonomics Soc Annu Meet. 2014;58:763-767.
- American College of Surgeons Division of Education and Surgical Ergonomics Committee. Surgical Ergonomics Recommendations. ACS Education. 2022.
- Cardenas-Trowers O, Kjellsson K, Hatch K. Ergonomics: making the OR a comfortable place. Int Urogynecol J. 2018;29:1065-1066.
- Hokenstad ED, Hallbeck MS, Lowndes BR, et al. Ergonomic robotic console configuration in gynecologic surgery: an interventional study. J Minim Invasive Gynecol. 2021;28:850-859.
- Singh R, Yurteri-Kaplan LA, Morrow MM, et al. Sitting versus standing makes a difference in musculoskeletal discomfort and postural load for surgeons performing vaginal surgery. Int Urogynecol J. 2019;30:231-237.
- Hullfish KL, Trowbridge ER, Bodine G. Ergonomics and gynecologic surgery: “surgeon protect thyself.” J Pelvic Med Surg. 2009;15:435-439.
- Woodburn KL, Kho RM. Vaginal surgery: don’t get bent out of shape. Am J Obstet Gynecol. 2020;223:762-763.
- Hobson DTG, Meriwether KV, Gaskins JT, et al. Learner satisfaction and experience with a high-definition telescopic camera during vaginal procedures: a randomized controlled trial. Female Pelvic Med Reconstr Surg. 2021;27:105-111.
- Speed G, Harris K, Keegel T. The effect of cushioning materials on musculoskeletal discomfort and fatigue during prolonged standing at work: a systematic review. Appl Ergon. 2018;70:300-334.
- Haramis G, Rosales JC, Palacios JM, et al. Prospective randomized evaluation of FOOT gel pads for operating room staff COMFORT during laparoscopic renal surgery. Urology. 2010;76:1405-1408.
- Voss RK, Chiang YJ, Cromwell KD, et al. Do no harm, except to ourselves? A survey of symptoms and injuries in oncologic surgeons and pilot study of an intraoperative ergonomic intervention. J Am Coll Surg. 2017;224:16-25.e1.
- Marquetand J, Gabriel J, Seibt R, et al. Ergonomics for surgeons—prototype of an external surgeon support system reduces muscular activity and fatigue. J Electromyogr Kinesiol. 2021;60:102586.
- Tetteh E, Hallbeck MS, Mirka GA. Effects of passive exoskeleton support on EMG measures of the neck, shoulder and trunk muscles while holding simulated surgical postures and performing a simulated surgical procedure. Appl Ergon. 2022;100:103646.
- Lim AK, Ryu J, Yoon HM, et al. Ergonomic effects of medical augmented reality glasses in video-assisted surgery. Surg Endosc. 2022;36:988-998.
- Park AE, Zahiri HR, Hallbeck MS, et al. Intraoperative “micro breaks” with targeted stretching enhance surgeon physical function and mental focus: a multicenter cohort study. Ann Surg. 2017;265:340-346.
- Hallbeck MS, Lowndes BR, Bingener J, et al. The impact of intraoperative microbreaks with exercises on surgeons: a multi-center cohort study. Appl Ergon. 2017;60:334-341.
- Hallbeck Human Factors Engineering Laboratories. OR Stretch Videos. Mayo Clinic, 2018. Accessed May 19, 2023. https://www.mayo .edu/research/labs/human-factors-engineering/or-stretch /or-stretch-videos
- Stork A, Bacon T, Corton M. Prevention of Work-Related Musculoskeletal Disorders in Vaginal Surgery. Video presentation at: Society of Gynecologic Surgeons’ Annual Scientific Meeting 2023, Tucson, AZ. Accessed April 3, 2023. https://sgs.eng.us/category.php?cat=2023 -video-presentations
- Aaron KA, Vaughan J, Gupta R, et al. The risk of ergonomic injury across surgical specialties. PLoS One. 2021;16:e0244868.
- Smith TG, Lowndes BR, Schmida E, et al. Course design and learning outcomes of a practical online ergonomics course for surgical residents. J Surg Educ. 2022;79:1489-1499.
- Franasiak J, Craven R, Mosaly P, et al. Feasibility and acceptance of a robotic surgery ergonomic training program. JSLS. 2014;18:e2014.00166.
- Cerier E, Hu A, Goldring A, et al. Ergonomics workshop improves musculoskeletal symptoms in general surgery residents. J Surg Res. 2022;280:567-574.
- Giagio S, Volpe G, Pillastrini P, et al. A preventive program for workrelated musculoskeletal disorders among surgeons: outcomes of a randomized controlled clinical trial. Ann Surg. 2019;270:969-975.
- Jensen MJ, Liao J, Van Gorp B, et al. Incorporating surgical ergonomics education into surgical residency curriculum. J Surg Educ. 2021;78:1209-1215.
Replace routine preoperative testing with individualized risk assessment and indicated testing
CASE Patient questions need for preoperative tests
A healthy 42-year-old woman (G2P2) with abnormal uterine bleeding and a 2-cm endometrial polyp is scheduled for hysteroscopic polypectomy. After your preoperative clinic visit, the patient receives her paperwork containing information about preoperative lab work and diagnostic studies. You are asked to come into the room because she has further questions. When you arrive, the patient holds the papers out and asks, “Is all this blood work and a chest x-ray necessary? I thought I was healthy and this was a fairly simple surgery. Is there more I should be worried about?”
How would you respond?
The goal of preoperative testing is to determine which patients may be at an increased risk for experiencing an adverse perioperative event, taking into account both the inherent risks of the surgical procedure and the health of the individual patient. In the literature, the general consensus is that physicians rely too heavily on unnecessary laboratory and diagnostic testing during their preoperative assessment.1 More than 50% of patients who underwent preoperative evaluation had at least 1 unindicated test.2 These tests may result in a high frequency of abnormal findings, with less than 3% of abnormalities having clinical value or leading to a change in management.3
With health care costs accounting for almost 20% of the gross domestic product in the United States (totaling about $3.5 billion in 2017), performing unindicated preoperative testing contributes to the economic burden on health care systems, with an estimated cost of $3 to $18 million annually.4,5 In addition, unindicated tests can increase patient anxiety and necessitate follow-up testing, possibly exposing physicians to increased liability if abnormal results are not adequately investigated.6
It is time to rethink our use of routine preoperative testing.
Which tests to consider—or not: Evidence-based guidance
Professional societies, including the American Board of Internal Medicine’s Choosing Wisely campaign, promote a move away from routine testing to avoid unnecessary visits and studies. In addition, the American Society of Anesthesiologists (ASA) has published recommendations to guide preoperative testing.7 To stratify patients’ surgical risk according to their pre-existing health conditions, the ASA created a physical status classification system (TABLE 1).8
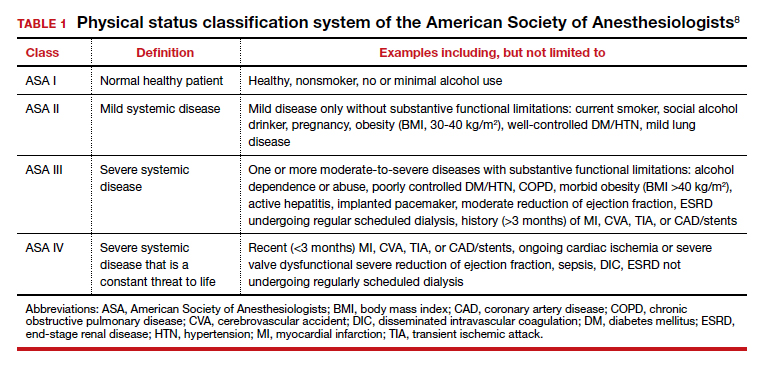
In addition to individual patient characteristics, some guidelines similarly stratify surgical procedures into minor, intermediate, and major risk. The modified Johns Hopkins surgical criteria allocates surgical risk based on expected blood loss, insensible loss, and the inherent risk of a procedure separate from anesthesia (TABLE 2).9 Despite these guidelines, physicians responsible for preoperative evaluations continue to order laboratory and diagnostic tests that are not indicated, often over concerns of case delays or cancellations.10,11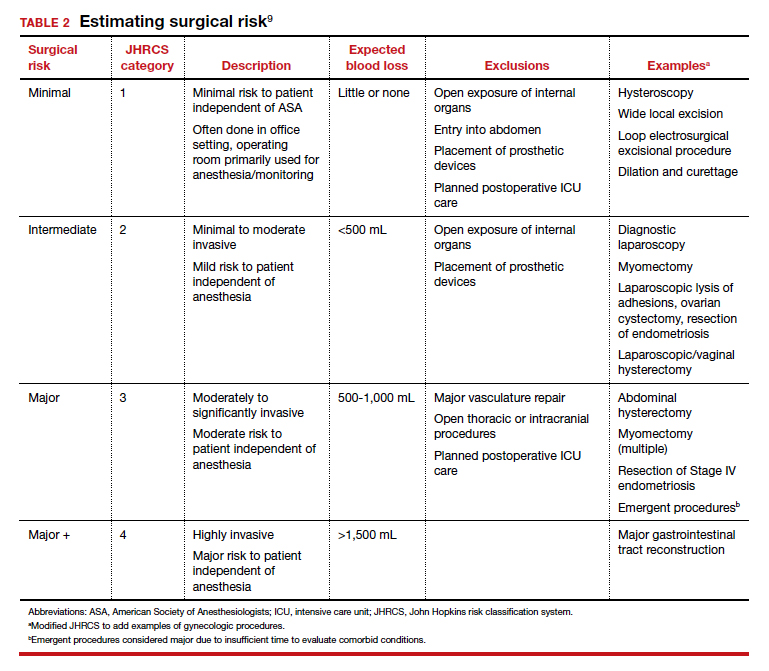
The following evidence-based recommendations provide guidance to gynecologists performing surgery for benign indications to determine which preoperative studies should be performed.
Serum chemistries
Basic metabolic panel (BMP). In both contemporary studies and earlier prospective studies, a preoperative BMP has a low likelihood of changing the surgical procedure or the patient’s management, especially in patients who are classified as ASA I and are undergoing minor- and intermediate-risk procedures.12,13 Therefore, we recommend a BMP for patients in class ASA II or higher who are undergoing intermediate-risk or major surgery.14
Thyroid function. A basic tenet of preoperative evaluation is that asymptomatic patients should not be diagnosed according to lab values prior to surgical intervention. Therefore, we do not recommend routine preoperative thyroid function testing in patients without a history of thyroid disease.10 For patients with known thyroid disease, a thyroid stimulating hormone (TSH) level should be evaluated prior to major surgery, or with any changes in medication dose or symptoms, within the past year.15
Liver function tests (LFTs). Routine screening of asymptomatic individuals without risk factors for liver disease is not recommended because there is a significantly lower incidence of abnormal lab values for LFTs than for other lab tests.16 We recommend LFTs only in symptomatic patients or patients diagnosed with severe liver disease undergoing intermediate-risk or major procedures.14
Hemoglobin A1c (HbA1c). Poorly controlled diabetes is a risk factor for poor wound healing, hospital readmission, prolonged hospitalization, and adverse events following surgery.17 We recommend that HbA1c levels be drawn only for patients with known diabetes undergoing intermediate-risk or major surgery who do not have an available lab value within the past 3 months.14
Continue to: Hematologic studies...
Hematologic studies
Complete blood count (CBC). Many patients undergoing gynecologic procedures may have unreported or undiagnosed anemia secondary to abnormal uterine bleeding, which also may encompass heavy menstrual bleeding. With an abnormal CBC likely to affect preoperative management, assessment of preoperative hemoglobin levels is critical so that hemoglobin levels can be appropriately corrected before surgery. We therefore recommend obtaining a CBC for patients in class ASA II or higher who are undergoing intermediate-risk or major surgery.10,14
Coagulation studies. Preoperative coagulation studies are unlikely to uncover previously undiagnosed inherited coagulopathies, which are generally uncommon in the general population, and they do not predict operative bleeding when ordered unnecessarily.18,19 Therefore, we recommend preoperative coagulation studies only in patients 1) currently on anticoagulation therapy undergoing intermediate-risk or major surgery or 2) in class ASA III or higher with bleeding disorders or cirrhosis undergoing intermediate-risk or major surgery.14
Type and screen (T&S). Complicated algorithms have been proposed to determine when a preoperative T&S is necessary, but these may be impractical for busy gynecologists.20 We recommend a T&S within 72 hours, or on the day, of surgery for all patients undergoing major surgery, including hysterectomy, or with an anticipated blood loss of more than 500 mL; routine crossmatching of blood is not recommended.10,14
Urologic studies
Urine pregnancy test. Although the probability of a positive pregnancy test is likely very low, its occurrence frequently leads to the cancellation of surgery. We therefore recommend a preoperative urine pregnancy test, particularly in reproductive-aged patients with unknown pregnancy status or unreliable contraceptive habits.14 Preoperative urine pregnancy testing, even in patients who report sexual inactivity, ideally should be individualized and based on risk of fetal harm during or subsequent to surgery. Surgeries involving the uterus, or those involving possible teratogens like radiation, also should be considered when making recommendations for testing.
Urinalysis and urine culture. In asymptomatic patients undergoing general gynecologic procedures, a routine preoperative urinalysis and urine culture are of little value.18 However, among patients undergoing a urogynecologic surgical procedure, the risk of a postoperative urinary tract infection is higher than among patients undergoing a nonurogynecologic procedure.21,22 Therefore, we typically do not recommend routine preoperative urinalysis or urine culture, but a preoperative urine culture may be beneficial in patients undergoing urogynecologic surgery.14
Continue to: Diagnostic studies...
Diagnostic studies
Electrocardiography (ECG). The absolute difference in cardiovascular death is less than 1% among patients with and without ECG abnormalities undergoing a noncardiac procedure with minimal to moderate risk; therefore, routine ECG for low-risk patients should not be performed.23 Instead, ECG should be performed in patients with known coronary artery disease or structural heart disease and in patients aged 65 years and older, since age older than 65 years is an independent predictor of significant ECG abnormalities.24,25 We therefore recommend that the following individuals have an ECG within the last 12 months: patients aged 65 years and older, patients in class ASA II or higher with cardiovascular disease, and patients in class ASA III or higher undergoing general anesthesia. If there is a change in cardiovascular health since the most recent ECG—even if it was performed within 12 months—a repeat ECG is warranted.10,14
Chest x-ray. Despite a high rate of abnormalities seen on routine and indicated chest x-rays, there is no significant difference in perioperative pulmonary complications among patients with a normal or abnormal chest x-ray.16 Rather than changing surgical management, these abnormal results are more likely to lead to the cancellation or postponement of a surgical procedure.7 We therefore recommend against routine preoperative chest x-ray.14
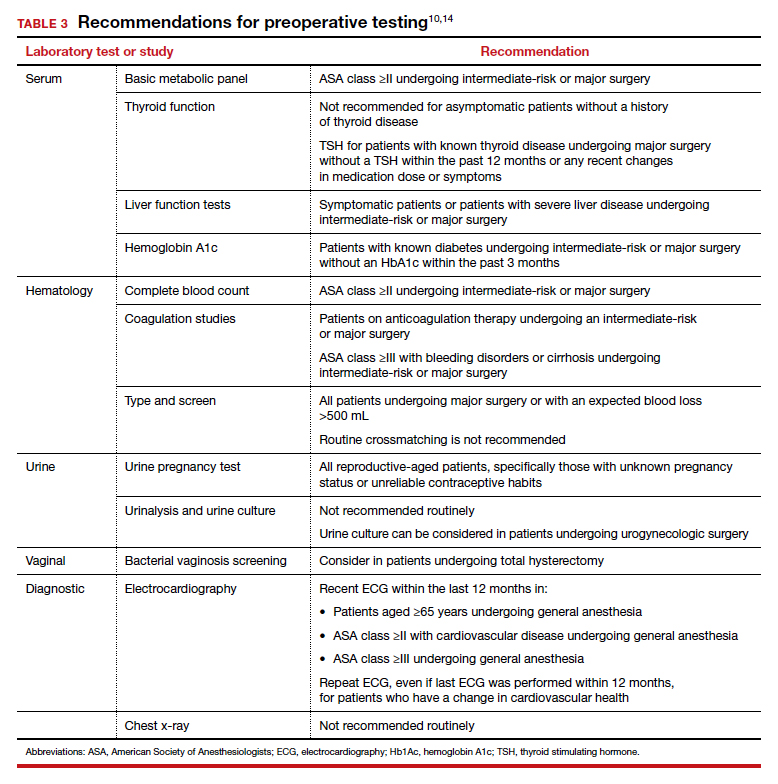
The bottom line
Preoperative testing serves as an additional component of surgical planning. The fact is, however, that abnormal test results are common and frequently do not correlate with surgical outcomes.26 Instead, they can lead to unnecessary surgical procedure cancellations or postponements, undue anxiety in patients, increased liability among physicians, and rising health care costs.5-7
Rather than overly relying on routine laboratory or diagnostic studies, the history and physical examination should continue to be the cornerstone for surgeons responsible for assessing surgical risk. With individualized risk assessment, specific, indicated testing rather than routine nonspecific testing can be obtained.10,14 In short, low-risk patients undergoing noncardiac surgery are unlikely to benefit from preoperative ECG, chest x-ray, or routine laboratory testing without clinical indication. ●
- Kachalia A, Berg A, Fagerlin A, et al. Overuse of testing in preoperative evaluation and syncope: a survey of hospitalists. Ann Intern Med. 2015;162:100-108.
- Onuoha OC, Hatch M, Miano TA, et al. The incidence of un-indicated preoperative testing in a tertiary academic ambulatory center: a retrospective cohort study. Perioper Med. 2015; 4:14.
- Kaplan EB, Sheiner LB, Boeckmann AJ, et al. The usefulness of preoperative laboratory screening. JAMA. 1985;253:3576-3581.
- Centers for Disease Control and Prevention National Center for Health Statistics. Table 42: Gross domestic product, national health expenditures, per capita amounts, percent distribution, and average annual percent change: United States, selected years 1960-2017. https://www.cdc.gov/nchs/ data/hus/2018/042.pdf. Accessed July 2020.
- Benarroch-Gampel J, Sheffield KM, Duncan CB, et al. Preoperative laboratory testing in patients undergoing elective, low-risk ambulatory surgery. Ann Surg. 2012;256:518-528.
- O’Neill F, Carter E, Pink N, et al. Routine preoperative tests for elective surgery: summary of updated NICE guidance. BMJ. 2016;354: i3292.
- Committee on Standards and Practice Parameters; Apfelbaum JL, Connis RT, Nickinovich DG, et al. Practice advisory for preanesthesia evaluation: an updated report by the American Society of Anesthesiologists Task Force on Preanesthesia Evaluation. Anesthesiology. 2012;116:522-538.
- American Society of Anesthesiologists. ASA physical status classification system. https://www.asahq.org/standardsand-guidelines/asa-physical-status-classification-system. Accessed July 2020.
- Pasternak LR, Johns A. Ambulatory gynaecological surgery: risk and assessment. Best Pract Res Clin Obstet Gynaecol. 2005;19:663-679.
- Shields J, Lupo A, Walsh T, et al. Preoperative evaluation for gynecologic surgery: a guide to judicious, evidence-based testing. Curr Opin Obstet Gynecol. 2018;30:252-259.
- Sigmund AE, Stevens ER, Blitz JD, et al. Use of preoperative testing and physicians’ response to professional society guidance. JAMA Intern Med. 2015;175:1352-1359.
- St Clair CM, Shah M, Diver EJ, et al. Adherence to evidence-based guidelines for preoperative testing in women undergoing gynecologic surgery. Obstet Gynecol. 2010;116:694-700.
- De Sousa Soares D, Brandao RR, Mourao MR, et al. Relevance of routine testing in low-risk patients undergoing minor and medium surgical procedures. Braz J Anesthesiol. 2013;63:197-201.
- Shields J, Kho KA. Preoperative evaluation for minimally invasive gynecologic surgery: what is the best evidence and recommendations for clinical practice. J Minim Invasive Gynecol. 2019;26:312-320.
- Palace MR. Perioperative management of thyroid dysfunction. Health Serv Insights. 2017;10:1178632916689677.
- Smetana GW, Macpherson DS. The case against routine preoperative laboratory testing. Med Clin North Am. 2003;87:7-40.
- Jehan F, Khan M, Sakran JV, et al. Perioperative glycemic control and postoperative complications in patients undergoing emergency general surgery: what is the role of plasma hemoglobin A1c? J Trauma Acute Care Surg. 2018;84:112-117.
- Feely MA, Collins CS, Daniels PR, et al. Preoperative testing before noncardiac surgery: guidelines and recommendations. Am Fam Physician. 2013;87:414-418.
- Rusk MH. Avoiding unnecessary preoperative testing. Med Clin North Am. 2016;100:1003-1008.
- Dexter F, Ledolter J, Davis E, et al. Systematic criteria for type and screen based on procedure’s probability of erythrocyte transfusion. Anesthesiology. 2012;116:768-778.
- Gehrich AP, Lustik MB, Mehr AA, et al. Risk of postoperative urinary tract infections following midurethral sling operations in women undergoing hysterectomy. Int Urogynecol J. 2016;27:483-490.
- American College of Obstetricians and Gynecologists. ACOG practice bulletin No. 195 summary: prevention of infection after gynecologic procedures. Obstet Gynecol. 2018;131:1177- 1179.
- Noordzij PG, Boersma E, Bax JJ, et al. Prognostic value of routine preoperative electrocardiography in patients undergoing noncardiac surgery. Am J Cardiol, 2006;97: 1103-1106.
- Fleisher LA, Fleischmann KE, Auerbach AD, et al. 2014 ACC/ AHA guideline on perioperative cardiovascular examination and management of patients undergoing noncardiac surgery: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;130:2215-2245.
- Correll DJ, Hepner DL, Chang C, et al. Preoperative electrocardiograms: patient factors predictive of abnormalities. Anesthesiology. 2009;110:1217-1122.
- Fritsch G, Flamm M, Hepner DL, et al. Abnormal preoperative tests, pathologic findings of medical history, and their predictive value for perioperative complications. Acta Anaesthesiol Scand. 2012;56:339-350.
CASE Patient questions need for preoperative tests
A healthy 42-year-old woman (G2P2) with abnormal uterine bleeding and a 2-cm endometrial polyp is scheduled for hysteroscopic polypectomy. After your preoperative clinic visit, the patient receives her paperwork containing information about preoperative lab work and diagnostic studies. You are asked to come into the room because she has further questions. When you arrive, the patient holds the papers out and asks, “Is all this blood work and a chest x-ray necessary? I thought I was healthy and this was a fairly simple surgery. Is there more I should be worried about?”
How would you respond?
The goal of preoperative testing is to determine which patients may be at an increased risk for experiencing an adverse perioperative event, taking into account both the inherent risks of the surgical procedure and the health of the individual patient. In the literature, the general consensus is that physicians rely too heavily on unnecessary laboratory and diagnostic testing during their preoperative assessment.1 More than 50% of patients who underwent preoperative evaluation had at least 1 unindicated test.2 These tests may result in a high frequency of abnormal findings, with less than 3% of abnormalities having clinical value or leading to a change in management.3
With health care costs accounting for almost 20% of the gross domestic product in the United States (totaling about $3.5 billion in 2017), performing unindicated preoperative testing contributes to the economic burden on health care systems, with an estimated cost of $3 to $18 million annually.4,5 In addition, unindicated tests can increase patient anxiety and necessitate follow-up testing, possibly exposing physicians to increased liability if abnormal results are not adequately investigated.6
It is time to rethink our use of routine preoperative testing.
Which tests to consider—or not: Evidence-based guidance
Professional societies, including the American Board of Internal Medicine’s Choosing Wisely campaign, promote a move away from routine testing to avoid unnecessary visits and studies. In addition, the American Society of Anesthesiologists (ASA) has published recommendations to guide preoperative testing.7 To stratify patients’ surgical risk according to their pre-existing health conditions, the ASA created a physical status classification system (TABLE 1).8
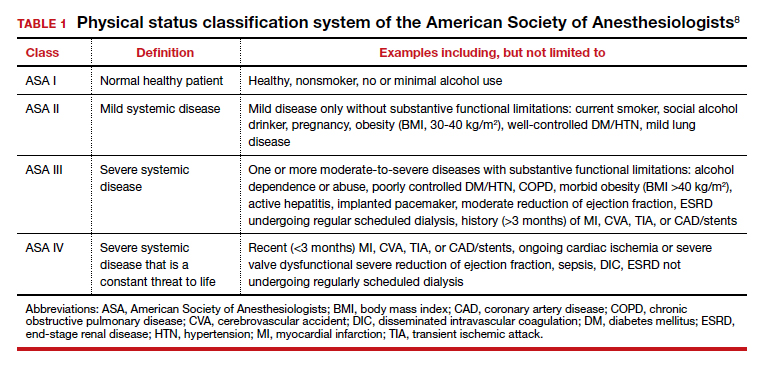
In addition to individual patient characteristics, some guidelines similarly stratify surgical procedures into minor, intermediate, and major risk. The modified Johns Hopkins surgical criteria allocates surgical risk based on expected blood loss, insensible loss, and the inherent risk of a procedure separate from anesthesia (TABLE 2).9 Despite these guidelines, physicians responsible for preoperative evaluations continue to order laboratory and diagnostic tests that are not indicated, often over concerns of case delays or cancellations.10,11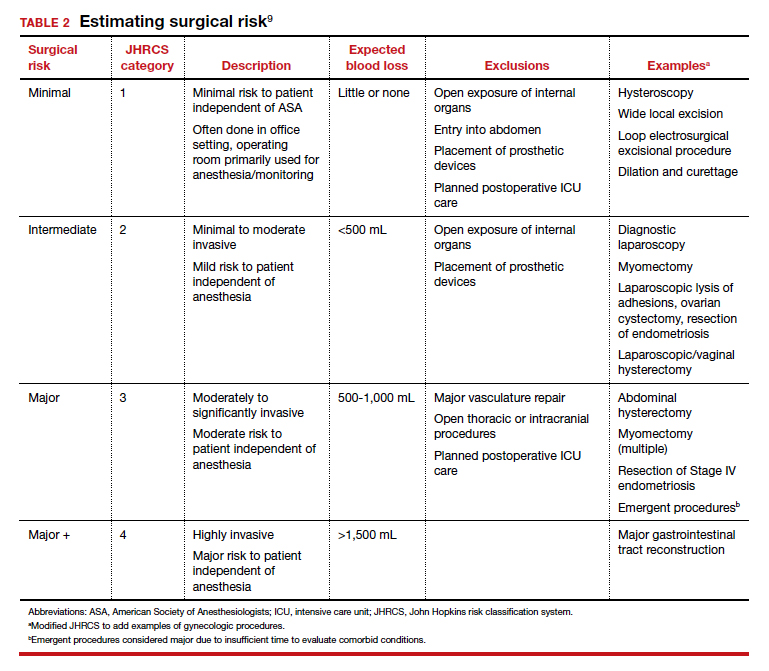
The following evidence-based recommendations provide guidance to gynecologists performing surgery for benign indications to determine which preoperative studies should be performed.
Serum chemistries
Basic metabolic panel (BMP). In both contemporary studies and earlier prospective studies, a preoperative BMP has a low likelihood of changing the surgical procedure or the patient’s management, especially in patients who are classified as ASA I and are undergoing minor- and intermediate-risk procedures.12,13 Therefore, we recommend a BMP for patients in class ASA II or higher who are undergoing intermediate-risk or major surgery.14
Thyroid function. A basic tenet of preoperative evaluation is that asymptomatic patients should not be diagnosed according to lab values prior to surgical intervention. Therefore, we do not recommend routine preoperative thyroid function testing in patients without a history of thyroid disease.10 For patients with known thyroid disease, a thyroid stimulating hormone (TSH) level should be evaluated prior to major surgery, or with any changes in medication dose or symptoms, within the past year.15
Liver function tests (LFTs). Routine screening of asymptomatic individuals without risk factors for liver disease is not recommended because there is a significantly lower incidence of abnormal lab values for LFTs than for other lab tests.16 We recommend LFTs only in symptomatic patients or patients diagnosed with severe liver disease undergoing intermediate-risk or major procedures.14
Hemoglobin A1c (HbA1c). Poorly controlled diabetes is a risk factor for poor wound healing, hospital readmission, prolonged hospitalization, and adverse events following surgery.17 We recommend that HbA1c levels be drawn only for patients with known diabetes undergoing intermediate-risk or major surgery who do not have an available lab value within the past 3 months.14
Continue to: Hematologic studies...
Hematologic studies
Complete blood count (CBC). Many patients undergoing gynecologic procedures may have unreported or undiagnosed anemia secondary to abnormal uterine bleeding, which also may encompass heavy menstrual bleeding. With an abnormal CBC likely to affect preoperative management, assessment of preoperative hemoglobin levels is critical so that hemoglobin levels can be appropriately corrected before surgery. We therefore recommend obtaining a CBC for patients in class ASA II or higher who are undergoing intermediate-risk or major surgery.10,14
Coagulation studies. Preoperative coagulation studies are unlikely to uncover previously undiagnosed inherited coagulopathies, which are generally uncommon in the general population, and they do not predict operative bleeding when ordered unnecessarily.18,19 Therefore, we recommend preoperative coagulation studies only in patients 1) currently on anticoagulation therapy undergoing intermediate-risk or major surgery or 2) in class ASA III or higher with bleeding disorders or cirrhosis undergoing intermediate-risk or major surgery.14
Type and screen (T&S). Complicated algorithms have been proposed to determine when a preoperative T&S is necessary, but these may be impractical for busy gynecologists.20 We recommend a T&S within 72 hours, or on the day, of surgery for all patients undergoing major surgery, including hysterectomy, or with an anticipated blood loss of more than 500 mL; routine crossmatching of blood is not recommended.10,14
Urologic studies
Urine pregnancy test. Although the probability of a positive pregnancy test is likely very low, its occurrence frequently leads to the cancellation of surgery. We therefore recommend a preoperative urine pregnancy test, particularly in reproductive-aged patients with unknown pregnancy status or unreliable contraceptive habits.14 Preoperative urine pregnancy testing, even in patients who report sexual inactivity, ideally should be individualized and based on risk of fetal harm during or subsequent to surgery. Surgeries involving the uterus, or those involving possible teratogens like radiation, also should be considered when making recommendations for testing.
Urinalysis and urine culture. In asymptomatic patients undergoing general gynecologic procedures, a routine preoperative urinalysis and urine culture are of little value.18 However, among patients undergoing a urogynecologic surgical procedure, the risk of a postoperative urinary tract infection is higher than among patients undergoing a nonurogynecologic procedure.21,22 Therefore, we typically do not recommend routine preoperative urinalysis or urine culture, but a preoperative urine culture may be beneficial in patients undergoing urogynecologic surgery.14
Continue to: Diagnostic studies...
Diagnostic studies
Electrocardiography (ECG). The absolute difference in cardiovascular death is less than 1% among patients with and without ECG abnormalities undergoing a noncardiac procedure with minimal to moderate risk; therefore, routine ECG for low-risk patients should not be performed.23 Instead, ECG should be performed in patients with known coronary artery disease or structural heart disease and in patients aged 65 years and older, since age older than 65 years is an independent predictor of significant ECG abnormalities.24,25 We therefore recommend that the following individuals have an ECG within the last 12 months: patients aged 65 years and older, patients in class ASA II or higher with cardiovascular disease, and patients in class ASA III or higher undergoing general anesthesia. If there is a change in cardiovascular health since the most recent ECG—even if it was performed within 12 months—a repeat ECG is warranted.10,14
Chest x-ray. Despite a high rate of abnormalities seen on routine and indicated chest x-rays, there is no significant difference in perioperative pulmonary complications among patients with a normal or abnormal chest x-ray.16 Rather than changing surgical management, these abnormal results are more likely to lead to the cancellation or postponement of a surgical procedure.7 We therefore recommend against routine preoperative chest x-ray.14
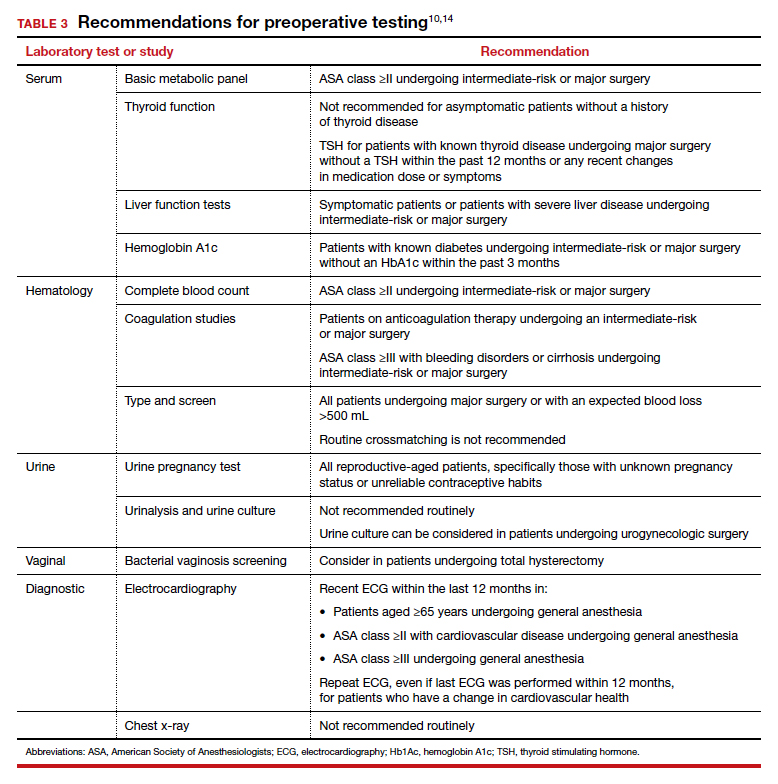
The bottom line
Preoperative testing serves as an additional component of surgical planning. The fact is, however, that abnormal test results are common and frequently do not correlate with surgical outcomes.26 Instead, they can lead to unnecessary surgical procedure cancellations or postponements, undue anxiety in patients, increased liability among physicians, and rising health care costs.5-7
Rather than overly relying on routine laboratory or diagnostic studies, the history and physical examination should continue to be the cornerstone for surgeons responsible for assessing surgical risk. With individualized risk assessment, specific, indicated testing rather than routine nonspecific testing can be obtained.10,14 In short, low-risk patients undergoing noncardiac surgery are unlikely to benefit from preoperative ECG, chest x-ray, or routine laboratory testing without clinical indication. ●
CASE Patient questions need for preoperative tests
A healthy 42-year-old woman (G2P2) with abnormal uterine bleeding and a 2-cm endometrial polyp is scheduled for hysteroscopic polypectomy. After your preoperative clinic visit, the patient receives her paperwork containing information about preoperative lab work and diagnostic studies. You are asked to come into the room because she has further questions. When you arrive, the patient holds the papers out and asks, “Is all this blood work and a chest x-ray necessary? I thought I was healthy and this was a fairly simple surgery. Is there more I should be worried about?”
How would you respond?
The goal of preoperative testing is to determine which patients may be at an increased risk for experiencing an adverse perioperative event, taking into account both the inherent risks of the surgical procedure and the health of the individual patient. In the literature, the general consensus is that physicians rely too heavily on unnecessary laboratory and diagnostic testing during their preoperative assessment.1 More than 50% of patients who underwent preoperative evaluation had at least 1 unindicated test.2 These tests may result in a high frequency of abnormal findings, with less than 3% of abnormalities having clinical value or leading to a change in management.3
With health care costs accounting for almost 20% of the gross domestic product in the United States (totaling about $3.5 billion in 2017), performing unindicated preoperative testing contributes to the economic burden on health care systems, with an estimated cost of $3 to $18 million annually.4,5 In addition, unindicated tests can increase patient anxiety and necessitate follow-up testing, possibly exposing physicians to increased liability if abnormal results are not adequately investigated.6
It is time to rethink our use of routine preoperative testing.
Which tests to consider—or not: Evidence-based guidance
Professional societies, including the American Board of Internal Medicine’s Choosing Wisely campaign, promote a move away from routine testing to avoid unnecessary visits and studies. In addition, the American Society of Anesthesiologists (ASA) has published recommendations to guide preoperative testing.7 To stratify patients’ surgical risk according to their pre-existing health conditions, the ASA created a physical status classification system (TABLE 1).8
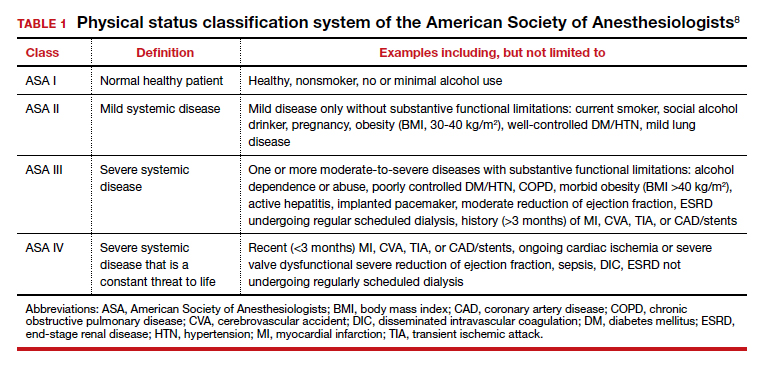
In addition to individual patient characteristics, some guidelines similarly stratify surgical procedures into minor, intermediate, and major risk. The modified Johns Hopkins surgical criteria allocates surgical risk based on expected blood loss, insensible loss, and the inherent risk of a procedure separate from anesthesia (TABLE 2).9 Despite these guidelines, physicians responsible for preoperative evaluations continue to order laboratory and diagnostic tests that are not indicated, often over concerns of case delays or cancellations.10,11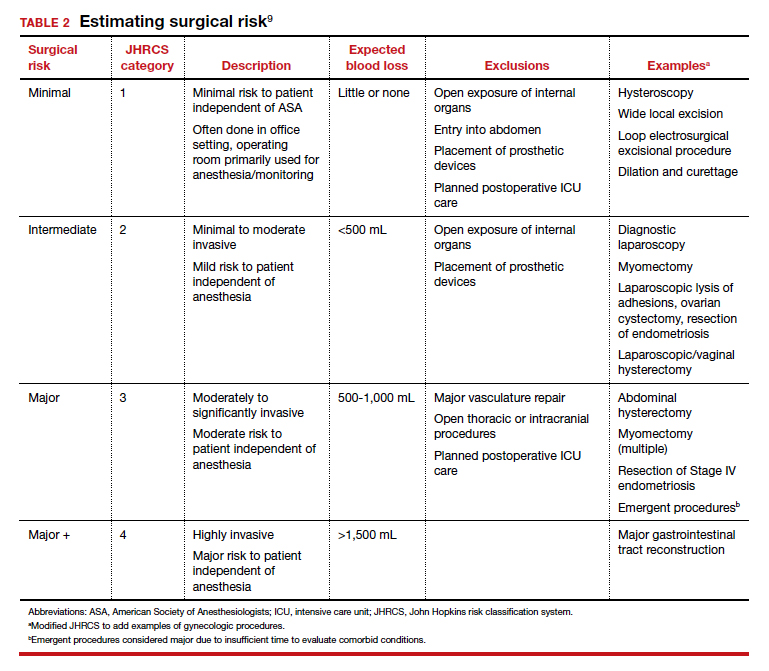
The following evidence-based recommendations provide guidance to gynecologists performing surgery for benign indications to determine which preoperative studies should be performed.
Serum chemistries
Basic metabolic panel (BMP). In both contemporary studies and earlier prospective studies, a preoperative BMP has a low likelihood of changing the surgical procedure or the patient’s management, especially in patients who are classified as ASA I and are undergoing minor- and intermediate-risk procedures.12,13 Therefore, we recommend a BMP for patients in class ASA II or higher who are undergoing intermediate-risk or major surgery.14
Thyroid function. A basic tenet of preoperative evaluation is that asymptomatic patients should not be diagnosed according to lab values prior to surgical intervention. Therefore, we do not recommend routine preoperative thyroid function testing in patients without a history of thyroid disease.10 For patients with known thyroid disease, a thyroid stimulating hormone (TSH) level should be evaluated prior to major surgery, or with any changes in medication dose or symptoms, within the past year.15
Liver function tests (LFTs). Routine screening of asymptomatic individuals without risk factors for liver disease is not recommended because there is a significantly lower incidence of abnormal lab values for LFTs than for other lab tests.16 We recommend LFTs only in symptomatic patients or patients diagnosed with severe liver disease undergoing intermediate-risk or major procedures.14
Hemoglobin A1c (HbA1c). Poorly controlled diabetes is a risk factor for poor wound healing, hospital readmission, prolonged hospitalization, and adverse events following surgery.17 We recommend that HbA1c levels be drawn only for patients with known diabetes undergoing intermediate-risk or major surgery who do not have an available lab value within the past 3 months.14
Continue to: Hematologic studies...
Hematologic studies
Complete blood count (CBC). Many patients undergoing gynecologic procedures may have unreported or undiagnosed anemia secondary to abnormal uterine bleeding, which also may encompass heavy menstrual bleeding. With an abnormal CBC likely to affect preoperative management, assessment of preoperative hemoglobin levels is critical so that hemoglobin levels can be appropriately corrected before surgery. We therefore recommend obtaining a CBC for patients in class ASA II or higher who are undergoing intermediate-risk or major surgery.10,14
Coagulation studies. Preoperative coagulation studies are unlikely to uncover previously undiagnosed inherited coagulopathies, which are generally uncommon in the general population, and they do not predict operative bleeding when ordered unnecessarily.18,19 Therefore, we recommend preoperative coagulation studies only in patients 1) currently on anticoagulation therapy undergoing intermediate-risk or major surgery or 2) in class ASA III or higher with bleeding disorders or cirrhosis undergoing intermediate-risk or major surgery.14
Type and screen (T&S). Complicated algorithms have been proposed to determine when a preoperative T&S is necessary, but these may be impractical for busy gynecologists.20 We recommend a T&S within 72 hours, or on the day, of surgery for all patients undergoing major surgery, including hysterectomy, or with an anticipated blood loss of more than 500 mL; routine crossmatching of blood is not recommended.10,14
Urologic studies
Urine pregnancy test. Although the probability of a positive pregnancy test is likely very low, its occurrence frequently leads to the cancellation of surgery. We therefore recommend a preoperative urine pregnancy test, particularly in reproductive-aged patients with unknown pregnancy status or unreliable contraceptive habits.14 Preoperative urine pregnancy testing, even in patients who report sexual inactivity, ideally should be individualized and based on risk of fetal harm during or subsequent to surgery. Surgeries involving the uterus, or those involving possible teratogens like radiation, also should be considered when making recommendations for testing.
Urinalysis and urine culture. In asymptomatic patients undergoing general gynecologic procedures, a routine preoperative urinalysis and urine culture are of little value.18 However, among patients undergoing a urogynecologic surgical procedure, the risk of a postoperative urinary tract infection is higher than among patients undergoing a nonurogynecologic procedure.21,22 Therefore, we typically do not recommend routine preoperative urinalysis or urine culture, but a preoperative urine culture may be beneficial in patients undergoing urogynecologic surgery.14
Continue to: Diagnostic studies...
Diagnostic studies
Electrocardiography (ECG). The absolute difference in cardiovascular death is less than 1% among patients with and without ECG abnormalities undergoing a noncardiac procedure with minimal to moderate risk; therefore, routine ECG for low-risk patients should not be performed.23 Instead, ECG should be performed in patients with known coronary artery disease or structural heart disease and in patients aged 65 years and older, since age older than 65 years is an independent predictor of significant ECG abnormalities.24,25 We therefore recommend that the following individuals have an ECG within the last 12 months: patients aged 65 years and older, patients in class ASA II or higher with cardiovascular disease, and patients in class ASA III or higher undergoing general anesthesia. If there is a change in cardiovascular health since the most recent ECG—even if it was performed within 12 months—a repeat ECG is warranted.10,14
Chest x-ray. Despite a high rate of abnormalities seen on routine and indicated chest x-rays, there is no significant difference in perioperative pulmonary complications among patients with a normal or abnormal chest x-ray.16 Rather than changing surgical management, these abnormal results are more likely to lead to the cancellation or postponement of a surgical procedure.7 We therefore recommend against routine preoperative chest x-ray.14
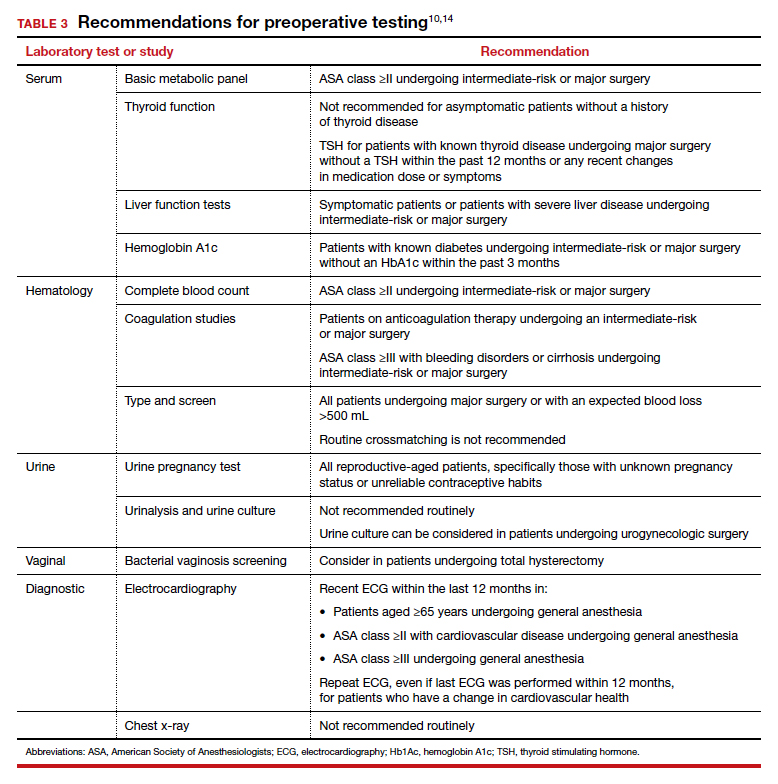
The bottom line
Preoperative testing serves as an additional component of surgical planning. The fact is, however, that abnormal test results are common and frequently do not correlate with surgical outcomes.26 Instead, they can lead to unnecessary surgical procedure cancellations or postponements, undue anxiety in patients, increased liability among physicians, and rising health care costs.5-7
Rather than overly relying on routine laboratory or diagnostic studies, the history and physical examination should continue to be the cornerstone for surgeons responsible for assessing surgical risk. With individualized risk assessment, specific, indicated testing rather than routine nonspecific testing can be obtained.10,14 In short, low-risk patients undergoing noncardiac surgery are unlikely to benefit from preoperative ECG, chest x-ray, or routine laboratory testing without clinical indication. ●
- Kachalia A, Berg A, Fagerlin A, et al. Overuse of testing in preoperative evaluation and syncope: a survey of hospitalists. Ann Intern Med. 2015;162:100-108.
- Onuoha OC, Hatch M, Miano TA, et al. The incidence of un-indicated preoperative testing in a tertiary academic ambulatory center: a retrospective cohort study. Perioper Med. 2015; 4:14.
- Kaplan EB, Sheiner LB, Boeckmann AJ, et al. The usefulness of preoperative laboratory screening. JAMA. 1985;253:3576-3581.
- Centers for Disease Control and Prevention National Center for Health Statistics. Table 42: Gross domestic product, national health expenditures, per capita amounts, percent distribution, and average annual percent change: United States, selected years 1960-2017. https://www.cdc.gov/nchs/ data/hus/2018/042.pdf. Accessed July 2020.
- Benarroch-Gampel J, Sheffield KM, Duncan CB, et al. Preoperative laboratory testing in patients undergoing elective, low-risk ambulatory surgery. Ann Surg. 2012;256:518-528.
- O’Neill F, Carter E, Pink N, et al. Routine preoperative tests for elective surgery: summary of updated NICE guidance. BMJ. 2016;354: i3292.
- Committee on Standards and Practice Parameters; Apfelbaum JL, Connis RT, Nickinovich DG, et al. Practice advisory for preanesthesia evaluation: an updated report by the American Society of Anesthesiologists Task Force on Preanesthesia Evaluation. Anesthesiology. 2012;116:522-538.
- American Society of Anesthesiologists. ASA physical status classification system. https://www.asahq.org/standardsand-guidelines/asa-physical-status-classification-system. Accessed July 2020.
- Pasternak LR, Johns A. Ambulatory gynaecological surgery: risk and assessment. Best Pract Res Clin Obstet Gynaecol. 2005;19:663-679.
- Shields J, Lupo A, Walsh T, et al. Preoperative evaluation for gynecologic surgery: a guide to judicious, evidence-based testing. Curr Opin Obstet Gynecol. 2018;30:252-259.
- Sigmund AE, Stevens ER, Blitz JD, et al. Use of preoperative testing and physicians’ response to professional society guidance. JAMA Intern Med. 2015;175:1352-1359.
- St Clair CM, Shah M, Diver EJ, et al. Adherence to evidence-based guidelines for preoperative testing in women undergoing gynecologic surgery. Obstet Gynecol. 2010;116:694-700.
- De Sousa Soares D, Brandao RR, Mourao MR, et al. Relevance of routine testing in low-risk patients undergoing minor and medium surgical procedures. Braz J Anesthesiol. 2013;63:197-201.
- Shields J, Kho KA. Preoperative evaluation for minimally invasive gynecologic surgery: what is the best evidence and recommendations for clinical practice. J Minim Invasive Gynecol. 2019;26:312-320.
- Palace MR. Perioperative management of thyroid dysfunction. Health Serv Insights. 2017;10:1178632916689677.
- Smetana GW, Macpherson DS. The case against routine preoperative laboratory testing. Med Clin North Am. 2003;87:7-40.
- Jehan F, Khan M, Sakran JV, et al. Perioperative glycemic control and postoperative complications in patients undergoing emergency general surgery: what is the role of plasma hemoglobin A1c? J Trauma Acute Care Surg. 2018;84:112-117.
- Feely MA, Collins CS, Daniels PR, et al. Preoperative testing before noncardiac surgery: guidelines and recommendations. Am Fam Physician. 2013;87:414-418.
- Rusk MH. Avoiding unnecessary preoperative testing. Med Clin North Am. 2016;100:1003-1008.
- Dexter F, Ledolter J, Davis E, et al. Systematic criteria for type and screen based on procedure’s probability of erythrocyte transfusion. Anesthesiology. 2012;116:768-778.
- Gehrich AP, Lustik MB, Mehr AA, et al. Risk of postoperative urinary tract infections following midurethral sling operations in women undergoing hysterectomy. Int Urogynecol J. 2016;27:483-490.
- American College of Obstetricians and Gynecologists. ACOG practice bulletin No. 195 summary: prevention of infection after gynecologic procedures. Obstet Gynecol. 2018;131:1177- 1179.
- Noordzij PG, Boersma E, Bax JJ, et al. Prognostic value of routine preoperative electrocardiography in patients undergoing noncardiac surgery. Am J Cardiol, 2006;97: 1103-1106.
- Fleisher LA, Fleischmann KE, Auerbach AD, et al. 2014 ACC/ AHA guideline on perioperative cardiovascular examination and management of patients undergoing noncardiac surgery: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;130:2215-2245.
- Correll DJ, Hepner DL, Chang C, et al. Preoperative electrocardiograms: patient factors predictive of abnormalities. Anesthesiology. 2009;110:1217-1122.
- Fritsch G, Flamm M, Hepner DL, et al. Abnormal preoperative tests, pathologic findings of medical history, and their predictive value for perioperative complications. Acta Anaesthesiol Scand. 2012;56:339-350.
- Kachalia A, Berg A, Fagerlin A, et al. Overuse of testing in preoperative evaluation and syncope: a survey of hospitalists. Ann Intern Med. 2015;162:100-108.
- Onuoha OC, Hatch M, Miano TA, et al. The incidence of un-indicated preoperative testing in a tertiary academic ambulatory center: a retrospective cohort study. Perioper Med. 2015; 4:14.
- Kaplan EB, Sheiner LB, Boeckmann AJ, et al. The usefulness of preoperative laboratory screening. JAMA. 1985;253:3576-3581.
- Centers for Disease Control and Prevention National Center for Health Statistics. Table 42: Gross domestic product, national health expenditures, per capita amounts, percent distribution, and average annual percent change: United States, selected years 1960-2017. https://www.cdc.gov/nchs/ data/hus/2018/042.pdf. Accessed July 2020.
- Benarroch-Gampel J, Sheffield KM, Duncan CB, et al. Preoperative laboratory testing in patients undergoing elective, low-risk ambulatory surgery. Ann Surg. 2012;256:518-528.
- O’Neill F, Carter E, Pink N, et al. Routine preoperative tests for elective surgery: summary of updated NICE guidance. BMJ. 2016;354: i3292.
- Committee on Standards and Practice Parameters; Apfelbaum JL, Connis RT, Nickinovich DG, et al. Practice advisory for preanesthesia evaluation: an updated report by the American Society of Anesthesiologists Task Force on Preanesthesia Evaluation. Anesthesiology. 2012;116:522-538.
- American Society of Anesthesiologists. ASA physical status classification system. https://www.asahq.org/standardsand-guidelines/asa-physical-status-classification-system. Accessed July 2020.
- Pasternak LR, Johns A. Ambulatory gynaecological surgery: risk and assessment. Best Pract Res Clin Obstet Gynaecol. 2005;19:663-679.
- Shields J, Lupo A, Walsh T, et al. Preoperative evaluation for gynecologic surgery: a guide to judicious, evidence-based testing. Curr Opin Obstet Gynecol. 2018;30:252-259.
- Sigmund AE, Stevens ER, Blitz JD, et al. Use of preoperative testing and physicians’ response to professional society guidance. JAMA Intern Med. 2015;175:1352-1359.
- St Clair CM, Shah M, Diver EJ, et al. Adherence to evidence-based guidelines for preoperative testing in women undergoing gynecologic surgery. Obstet Gynecol. 2010;116:694-700.
- De Sousa Soares D, Brandao RR, Mourao MR, et al. Relevance of routine testing in low-risk patients undergoing minor and medium surgical procedures. Braz J Anesthesiol. 2013;63:197-201.
- Shields J, Kho KA. Preoperative evaluation for minimally invasive gynecologic surgery: what is the best evidence and recommendations for clinical practice. J Minim Invasive Gynecol. 2019;26:312-320.
- Palace MR. Perioperative management of thyroid dysfunction. Health Serv Insights. 2017;10:1178632916689677.
- Smetana GW, Macpherson DS. The case against routine preoperative laboratory testing. Med Clin North Am. 2003;87:7-40.
- Jehan F, Khan M, Sakran JV, et al. Perioperative glycemic control and postoperative complications in patients undergoing emergency general surgery: what is the role of plasma hemoglobin A1c? J Trauma Acute Care Surg. 2018;84:112-117.
- Feely MA, Collins CS, Daniels PR, et al. Preoperative testing before noncardiac surgery: guidelines and recommendations. Am Fam Physician. 2013;87:414-418.
- Rusk MH. Avoiding unnecessary preoperative testing. Med Clin North Am. 2016;100:1003-1008.
- Dexter F, Ledolter J, Davis E, et al. Systematic criteria for type and screen based on procedure’s probability of erythrocyte transfusion. Anesthesiology. 2012;116:768-778.
- Gehrich AP, Lustik MB, Mehr AA, et al. Risk of postoperative urinary tract infections following midurethral sling operations in women undergoing hysterectomy. Int Urogynecol J. 2016;27:483-490.
- American College of Obstetricians and Gynecologists. ACOG practice bulletin No. 195 summary: prevention of infection after gynecologic procedures. Obstet Gynecol. 2018;131:1177- 1179.
- Noordzij PG, Boersma E, Bax JJ, et al. Prognostic value of routine preoperative electrocardiography in patients undergoing noncardiac surgery. Am J Cardiol, 2006;97: 1103-1106.
- Fleisher LA, Fleischmann KE, Auerbach AD, et al. 2014 ACC/ AHA guideline on perioperative cardiovascular examination and management of patients undergoing noncardiac surgery: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;130:2215-2245.
- Correll DJ, Hepner DL, Chang C, et al. Preoperative electrocardiograms: patient factors predictive of abnormalities. Anesthesiology. 2009;110:1217-1122.
- Fritsch G, Flamm M, Hepner DL, et al. Abnormal preoperative tests, pathologic findings of medical history, and their predictive value for perioperative complications. Acta Anaesthesiol Scand. 2012;56:339-350.
