User login
Limited Use of Outpatient Stress Testing in Young Patients With Atypical Chest Pain (FULL)
Low prevalence of coronary artery disease within this population suggests that younger patients may not require stress testing for chest pain evaluations as long as pretest likelihood is low.
The decision to perform stress testing in the evaluation of chest pain is often based on the pretest likelihood of coronary artery disease (CAD).1-7 Cardiac risk scores, which incorporate smoking status, blood pressure, diabetes mellitus, and cholesterol levels, also may provide further risk stratification.8-11 Assuming that the prevalence of CAD increases with age, young adults could be deemed low risk, not warranting cardiac screening.12
Professional society guidelines from the American College of Cardiology/American Heart Association and American College of Physicians4,5 recommend stress testing as the initial diagnostic test for CAD in symptomatic patients; additionally, the guidelines also suggest that screening stress tests may confer primary prevention benefit in intermediate-risk asymptomatic patients.9,13 Exercise treadmill testing is considered the initial modality of choice, given its technical ease and lower cost, compared with stress echocardiography.14
Previously published reports have shown the limited use of stress testing to screen young asymptomatic adults.15-17 Because this patient demographic typically has a low pretest likelihood of CAD, positive stress tests are often false-positive results.7,18 The consequence of false-positive testing may be unnecessary additional cardiac testing, potentially leading to more patient harm than benefit.18,19 For active-duty service members, false-positive testing also has the potential to affect worldwide deployability and/or sea duty status while further risk stratification is performed; as a result, mission readiness may be impacted.Although the number of clinic visits for chest pain has declined, there has been a discordant increase in the rates of stress testing in the US.20-22 Additionally, the rate of stress testing among young adults, specifically in the 25- to 34-year age group, has increased in recent years. Given the rising use of stress tests in the young patient population, the clinical use of stress testing needs to be reassessed.
Although much of the literature has already demonstrated the low value of stress testing in young asymptomatic adults, no data currently exist regarding its outpatient use in evaluating young symptomatic patients. The military represents a predominantly young cross-section of the general population suitable for exploring this topic. Using a cohort of active-duty service members, we aimed to determine the use of outpatient stress testing in evaluating young patients with atypical chest pain.
Methods
The US Department of Defense (DoD) Military Health System Database Repository (MDR) and Comprehensive Ambulatory Professional Encounter Record (CAPER) were the data sources for this study. The MDR contains continually updated, longitudinal electronic medical records (EMRs) for nearly 1.4 million active-duty service members and is composed of administrative, medical, pharmacy, and clinical data. The Naval Medical Center Portsmouth (NMCP) Institutional Review Board approved this study.
Study Cohort
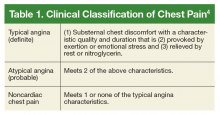
We performed chart reviews of service members aged 18 to 35 years who received cardiac stress testing at NMCP, an academic tertiary care center, within 30 days after an office visit for atypical chest pain between October 1, 2010, and September 30, 2015. Atypical chest pain was defined as any outpatient claim with ICD-9 code, 786.5x, in the primary diagnosis field (Table 1).4
Demographics and cardiac risk factors (ie, hypertension, hyperlipidemia, diabetes mellitus, and smoking status) were assessed prior to index chest pain evaluations and defined via ICD-9 codes within outpatient records.
Cardiac Testing Outcomes
Patients were initially categorized by the results of baseline electrocardiograms (ECG) and index stress tests (ie, exercise treadmill or stress echocardiography, exercise or Lexiscan myocardial perfusion imaging, dobutamine stress echocardiography). Positive tests were defined as those having electrical or structural ischemic changes. Chronotropic changes were infrequent and nonpathologic and were not counted. Patient endpoints were either additional cardiac testing or negative index stress test without additional testing.
Statistical Analysis
The agreement between both baseline ECG and index stress test as well as index stress test and additional cardiac testing were analyzed using McNemar test and matched-pair odds ratios (ORs) with corresponding 95% CIs. Analyses were stratified by demographics and cardiac risk factors to assess for potential confounding. Analyses were performed using SAS version 9.4 (Cary, NC).
Results
A total of 1,036 patients were evaluated for atypical chest pain and had index stress testing between October 1, 2010 and September 30, 2015. The study cohort was 69% male with a mean (SD) age of 27.3 (4.7) years. More than 60% of the cohort was older than aged > 25 years.
In the initial testing cohort, exercise treadmill test (59.3%) and exercise echocardiogram (37.1%) were the most common stress testing modalities. The mean (SD) metabolic equivalents (METS) achieved among individuals who performed exercise stress testing was 13.9 (2.8). There were 65 patients who had a positive baseline ECG/negative index stress test, 958 patients had a negative ECG/negative index test, and 8 patients had a negative ECG/positive index test.
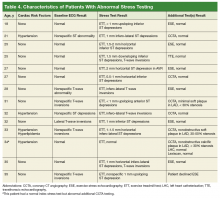
There were 102 patients (10%) who performed additional cardiac testing. Among this subgroup, 13 patients (1.3%) had additional testing for further evaluation of a positive index stress test (Table 4) and 89 patients (8.6%) had testing for continuing atypical chest pain despite a negative index stress test.
Coronary computed tomography angiography (CCTA) demonstrated nonobstructive CAD in 3 patients (0.3%) within the study cohort. There was no obstructive CAD identified in our cohort. Two patients had negative left heart catheterizations (LHC). One of these patients had a negative LHC and a negative Lexiscan after a CCTA showed CAD; all 3 of these additional tests were performed for evaluation of continued chest pain despite negative index stress testing. The positive predictive value of cardiac stress testing for nonobstructive CAD in this low-risk population was 15.4% (2 of 13). Stratification by demographics, CAD risk factors, and cardiac test results revealed no presence of confounding factors during analyses.
Discussion
In this retrospective, observational study of 1,036 young patients with atypical chest pain who had stress testing, there was relatively strong agreement between baseline ECG and index stress test results. Individuals also were 8 times more likely to have positive baseline ECGs and negative stress testing than having the opposite finding. Additional cardiac testing similarly demonstrated congruency with index stress testing and showed the propensity for false-positive stress tests. Further testing with CCTA demonstrated minimal nonobstructive CAD in < 1% of the study cohort and 2 LHC were negative. Despite the low prevalence of CAD and apparent low diagnostic use of stress testing in our young cohort, symptomatic service members still require stress testing to determine deployment suitability.
The low yield of outpatient stress testing in our young population is rooted in Bayes’ theorem, which highlights the importance of pretest likelihood in the diagnosis of CAD.7,23 Because our cohort had a low prevalence and low pretest likelihood of CAD, positive index stress tests were often false-positive results and consequently did not increase the posttest likelihood of CAD, resulting in low positive predictive value. Additional cardiac testing had limited clinical value in our cohort. The 3 cases of nonobstructive CAD were unlikely to be pathologic given the minimal degree of observed stenosis and the 2 LHC did not require revascularization. These results are similar to those shown by Christman and colleagues and Mudrick and colleagues, which highlighted the low yield of additional cardiac studies and low rate of revascularization among symptomatic patients without known cardiac disease, respectively.18,19
This is the first study, to our knowledge, to quantitatively demonstrate the low use of outpatient stress testing for young adults with atypical chest pain. Previous studies that assessed stress testing for young patients with chest pain in acute settings such as emergency departments and chest pain observation units, similarly demonstrated minimal yield of routine diagnostic testing.23,24 This further highlights the premise that outpatient and even emergent-setting stress testing in low cardiac risk individuals may be of limited value and not always necessary.
Limitations
There were several study limitations. As a single-center, cross-sectional review, we may not be able to extrapolate our findings to the general population. However, given the low prevalence of CAD in young adults, stress testing would likely have limited value regardless of the sample distribution; so it may be possible to extend our findings beyond our cohort. Also, neither baseline ECG nor index stress test (irrespective of modality) could be given a diagnostic value in predicting ischemia alone; doing so would require comparison with the gold standard—heart catheterization. Although referral bias has been associated with diagnostic performance of stress testing, we did not adjust for this phenomenon.25 Given the higher average metabolic equivalents achieved in our cohort, this potential bias likely did not affect diagnostic performance.
Conclusion
There was low diagnostic use of outpatient stress testing and additional cardiac testing for CAD among young patients with atypical chest pain. The limited value of cardiac stress testing is likely a function of the low CAD prevalence within this population, suggesting that younger patients may not necessarily require stress testing for chest pain evaluations as long as pretest likelihood is low. Despite our results, we maintain that the decision to perform stress testing should still be guided by clinical judgment, but perhaps our findings may alleviate physicians’ concerns over the urgency of when to refer low-risk patients for testing. Although we are cautious in inferring our findings to the general population, the similarity it shares with those from other published reports may suggest its applicability beyond our study cohort.
1. Fowler-Brown A, Pignone M, Pletcher M, et al. Exercise tolerance testing to screen for coronary heart disease: a systematic review for the technical support for the U.S. Preventive Services Task Force. Ann Intern Med. 2004;140(7):W9-W24.
2. Gibbons RJ, Balady GJ, Bricker JT, et al; American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Committee to Update the 1997 Exercise Testing Guidelines. ACC/AHA 2002 guideline update for exercise testing: summary article. A report of the American College of Cardiology/American Heart Association Task Force on practice guidelines (Committee to Update the 1997 Exercise Testing Guidelines). J Am Coll Cardiol. 2002;40(8):1531-1540.
3. Chou R, Arora B, Dana T, Fu R, Miranda Walker M, Humphrey L. Screening Asymptomatic Adults for Coronary Heart Disease With Resting or Exercise Electrocardiography: Systematic Review to Update the 2004 U.S. Preventive Services Task Force recommendation. Evidence Synthesis No. 88. AHRQ Publication No. 11-05158-EF-1. Rockville, MD: Agency for Healthcare Research and Quality; September 2011.
4. Fihn S, Gardin J, Abrams J, et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiology. 2012;60(24):e44-e164.
5. Gibbons RJ, Balady GJ, Beasley JW, et al. ACC/AHA guidelines for exercise testing: executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Exercise Testing). Circulation. 1997;96(1):345-354.
6. Greenland P, Alpert JS, Beller GA, et al. 2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults. A report of the American College of Cardiology Foundation/ American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2010;56(25):e50-e103.
7. Diamond G, Forrester J. Analysis of probability as an aid in the clinical diagnosis of coronary artery disease. N Engl J Med. 1979;300(24):1350-1358.
8. Goff D, Lloyd-Jones D, Bennett G, et al; American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25)(suppl 2):S49-S73.
9. Greenland P, Gaziano J. Selecting asymptomatic patients for coronary computed tomography or electrocardiographic exercise testing. N Engl J Med. 2003;349(5):465-473.
10. Shah N, Soon K, Wong C, Kellu AM. Screening for asymptomatic coronary heart disease in the young ‘at risk’ population: who and how? Int J Cardiol Heart Vasc. 2014;6:60-65.
11. Morise A, Evans M, Jalisi F, Shetty R, Stauffer M. A pretest prognostic score to assess patients undergoing exercise or pharmacological stress testing. Heart. 2007;93(2):200-204.
12. Amsterdam EA, Kirk JD, Bluemke DA, et al; American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee of the Council on Clinical Cardiology, Council on Cardiovascular Nursing, and Interdisciplinary Council on Quality of Care and Outcomes Research. Testing of low-risk patients presenting to the emergency department with chest pain: a scientific statement from the American Heart Association. Circulation. 2010;122(17):1756-1776.
13. Livschitz S, Sharabi Y, Yushin J, et al. Limited clinical value of exercise stress test for the screening of coronary artery disease in young, asymptomatic adult men. Am J Cardiol. 2000;86(4):462-464.
14. Miller T. Stress testing: the case for the standard treadmill test. Curr Opin Cardiol. 2011;26(5):363-369.
15. La Gerche A, Baggish A, Knuuti J, et al. Cardiac imaging and stress testing asymptomatic athletes to identify those at risk of sudden cardiac death. JACC Cardiovasc Imaging. 2013;6(9):993-1007.
16. Lauer M, Froelicher ES, Williams M, Kligfield P; American Heart Association Council on Clinical Cardiology, Subcommittee on Exercise, Cardiac Rehabilitation, and Prevention. Exercise testing in asymptomatic adults: a statement for professionals from the American Heart Association Council on Clinical Cardiology, Subcommittee on Exercise, Cardiac Rehabilitation, and Prevention. Circulation. 2005;112(5):771-776.
17. Sammito S, Gundlach N, Bockelmann I. Prevalence of cardiac arrhythmia under stress conditions in occupational health assessments of young military servicemen and servicewomen. Mil Med. 2016;181(4):369-372.
18. Mudrick DW, Cowper PA, Shah BR, et al. Downstream procedures and outcomes after stress testing for chest pain without known coronary artery disease in the United States. Am Heart J. 2012;163(3):454-461.
19. Christman MP, Bittencourt MS, Hulten E, et al. Yield of downstream tests after exercise treadmill testing. J Am Coll Cardiol. 2014;63(13):1264-1274.
20. Will J, Loustalot F, Hong Y. National trends in visits to physician offices and outpatient clinics for angina 1995 to 2010. Circ Cardiovasc Qual Outcomes. 2014;7(1):110-117.
21. Kini V, McCarthy F, Dayoub E, et al. Cardiac stress test trends among US patients younger than 65 years, 2005-2012. JAMA Cardiol. 2016;1(9):1038-1042.
22. Ladapo JA, Blecker S, Douglas PS. Physician decision making and trends in the use of cardiac stress testing in the United States: an analysis of repeated cross-sectional data. Ann Intern Med. 2014;161(7):482-490.
23. Winchester DE, Brandt J, Schmidt C, Schmidt C, Allen B, Payton T, Amsterdam EA. Diagnostic yield of routine noninvasive cardiovascular testing in low-risk acute chest pain patients. Am J Cardiol. 2015;116(2):204-207.
24. Hermann L, Weingart SD, Duvall W, Henzlova MJ. The limited utility of routine cardiac stress testing in emergency department chest pain patients younger than 40 years. Ann Emerg Med. 2009;54(1):12-16.
25. Ladapo JA, Blecker S, Elashoff MR, et al. Clinical implications of referral bias in the diagnostic performance of exercise testing for coronary artery disease. J Am Heart Assoc. 2013;2(6):e000505.
Low prevalence of coronary artery disease within this population suggests that younger patients may not require stress testing for chest pain evaluations as long as pretest likelihood is low.
Low prevalence of coronary artery disease within this population suggests that younger patients may not require stress testing for chest pain evaluations as long as pretest likelihood is low.
The decision to perform stress testing in the evaluation of chest pain is often based on the pretest likelihood of coronary artery disease (CAD).1-7 Cardiac risk scores, which incorporate smoking status, blood pressure, diabetes mellitus, and cholesterol levels, also may provide further risk stratification.8-11 Assuming that the prevalence of CAD increases with age, young adults could be deemed low risk, not warranting cardiac screening.12
Professional society guidelines from the American College of Cardiology/American Heart Association and American College of Physicians4,5 recommend stress testing as the initial diagnostic test for CAD in symptomatic patients; additionally, the guidelines also suggest that screening stress tests may confer primary prevention benefit in intermediate-risk asymptomatic patients.9,13 Exercise treadmill testing is considered the initial modality of choice, given its technical ease and lower cost, compared with stress echocardiography.14
Previously published reports have shown the limited use of stress testing to screen young asymptomatic adults.15-17 Because this patient demographic typically has a low pretest likelihood of CAD, positive stress tests are often false-positive results.7,18 The consequence of false-positive testing may be unnecessary additional cardiac testing, potentially leading to more patient harm than benefit.18,19 For active-duty service members, false-positive testing also has the potential to affect worldwide deployability and/or sea duty status while further risk stratification is performed; as a result, mission readiness may be impacted.Although the number of clinic visits for chest pain has declined, there has been a discordant increase in the rates of stress testing in the US.20-22 Additionally, the rate of stress testing among young adults, specifically in the 25- to 34-year age group, has increased in recent years. Given the rising use of stress tests in the young patient population, the clinical use of stress testing needs to be reassessed.
Although much of the literature has already demonstrated the low value of stress testing in young asymptomatic adults, no data currently exist regarding its outpatient use in evaluating young symptomatic patients. The military represents a predominantly young cross-section of the general population suitable for exploring this topic. Using a cohort of active-duty service members, we aimed to determine the use of outpatient stress testing in evaluating young patients with atypical chest pain.
Methods
The US Department of Defense (DoD) Military Health System Database Repository (MDR) and Comprehensive Ambulatory Professional Encounter Record (CAPER) were the data sources for this study. The MDR contains continually updated, longitudinal electronic medical records (EMRs) for nearly 1.4 million active-duty service members and is composed of administrative, medical, pharmacy, and clinical data. The Naval Medical Center Portsmouth (NMCP) Institutional Review Board approved this study.
Study Cohort
We performed chart reviews of service members aged 18 to 35 years who received cardiac stress testing at NMCP, an academic tertiary care center, within 30 days after an office visit for atypical chest pain between October 1, 2010, and September 30, 2015. Atypical chest pain was defined as any outpatient claim with ICD-9 code, 786.5x, in the primary diagnosis field (Table 1).4
Demographics and cardiac risk factors (ie, hypertension, hyperlipidemia, diabetes mellitus, and smoking status) were assessed prior to index chest pain evaluations and defined via ICD-9 codes within outpatient records.
Cardiac Testing Outcomes
Patients were initially categorized by the results of baseline electrocardiograms (ECG) and index stress tests (ie, exercise treadmill or stress echocardiography, exercise or Lexiscan myocardial perfusion imaging, dobutamine stress echocardiography). Positive tests were defined as those having electrical or structural ischemic changes. Chronotropic changes were infrequent and nonpathologic and were not counted. Patient endpoints were either additional cardiac testing or negative index stress test without additional testing.
Statistical Analysis
The agreement between both baseline ECG and index stress test as well as index stress test and additional cardiac testing were analyzed using McNemar test and matched-pair odds ratios (ORs) with corresponding 95% CIs. Analyses were stratified by demographics and cardiac risk factors to assess for potential confounding. Analyses were performed using SAS version 9.4 (Cary, NC).
Results
A total of 1,036 patients were evaluated for atypical chest pain and had index stress testing between October 1, 2010 and September 30, 2015. The study cohort was 69% male with a mean (SD) age of 27.3 (4.7) years. More than 60% of the cohort was older than aged > 25 years.
In the initial testing cohort, exercise treadmill test (59.3%) and exercise echocardiogram (37.1%) were the most common stress testing modalities. The mean (SD) metabolic equivalents (METS) achieved among individuals who performed exercise stress testing was 13.9 (2.8). There were 65 patients who had a positive baseline ECG/negative index stress test, 958 patients had a negative ECG/negative index test, and 8 patients had a negative ECG/positive index test.
There were 102 patients (10%) who performed additional cardiac testing. Among this subgroup, 13 patients (1.3%) had additional testing for further evaluation of a positive index stress test (Table 4) and 89 patients (8.6%) had testing for continuing atypical chest pain despite a negative index stress test.
Coronary computed tomography angiography (CCTA) demonstrated nonobstructive CAD in 3 patients (0.3%) within the study cohort. There was no obstructive CAD identified in our cohort. Two patients had negative left heart catheterizations (LHC). One of these patients had a negative LHC and a negative Lexiscan after a CCTA showed CAD; all 3 of these additional tests were performed for evaluation of continued chest pain despite negative index stress testing. The positive predictive value of cardiac stress testing for nonobstructive CAD in this low-risk population was 15.4% (2 of 13). Stratification by demographics, CAD risk factors, and cardiac test results revealed no presence of confounding factors during analyses.
Discussion
In this retrospective, observational study of 1,036 young patients with atypical chest pain who had stress testing, there was relatively strong agreement between baseline ECG and index stress test results. Individuals also were 8 times more likely to have positive baseline ECGs and negative stress testing than having the opposite finding. Additional cardiac testing similarly demonstrated congruency with index stress testing and showed the propensity for false-positive stress tests. Further testing with CCTA demonstrated minimal nonobstructive CAD in < 1% of the study cohort and 2 LHC were negative. Despite the low prevalence of CAD and apparent low diagnostic use of stress testing in our young cohort, symptomatic service members still require stress testing to determine deployment suitability.
The low yield of outpatient stress testing in our young population is rooted in Bayes’ theorem, which highlights the importance of pretest likelihood in the diagnosis of CAD.7,23 Because our cohort had a low prevalence and low pretest likelihood of CAD, positive index stress tests were often false-positive results and consequently did not increase the posttest likelihood of CAD, resulting in low positive predictive value. Additional cardiac testing had limited clinical value in our cohort. The 3 cases of nonobstructive CAD were unlikely to be pathologic given the minimal degree of observed stenosis and the 2 LHC did not require revascularization. These results are similar to those shown by Christman and colleagues and Mudrick and colleagues, which highlighted the low yield of additional cardiac studies and low rate of revascularization among symptomatic patients without known cardiac disease, respectively.18,19
This is the first study, to our knowledge, to quantitatively demonstrate the low use of outpatient stress testing for young adults with atypical chest pain. Previous studies that assessed stress testing for young patients with chest pain in acute settings such as emergency departments and chest pain observation units, similarly demonstrated minimal yield of routine diagnostic testing.23,24 This further highlights the premise that outpatient and even emergent-setting stress testing in low cardiac risk individuals may be of limited value and not always necessary.
Limitations
There were several study limitations. As a single-center, cross-sectional review, we may not be able to extrapolate our findings to the general population. However, given the low prevalence of CAD in young adults, stress testing would likely have limited value regardless of the sample distribution; so it may be possible to extend our findings beyond our cohort. Also, neither baseline ECG nor index stress test (irrespective of modality) could be given a diagnostic value in predicting ischemia alone; doing so would require comparison with the gold standard—heart catheterization. Although referral bias has been associated with diagnostic performance of stress testing, we did not adjust for this phenomenon.25 Given the higher average metabolic equivalents achieved in our cohort, this potential bias likely did not affect diagnostic performance.
Conclusion
There was low diagnostic use of outpatient stress testing and additional cardiac testing for CAD among young patients with atypical chest pain. The limited value of cardiac stress testing is likely a function of the low CAD prevalence within this population, suggesting that younger patients may not necessarily require stress testing for chest pain evaluations as long as pretest likelihood is low. Despite our results, we maintain that the decision to perform stress testing should still be guided by clinical judgment, but perhaps our findings may alleviate physicians’ concerns over the urgency of when to refer low-risk patients for testing. Although we are cautious in inferring our findings to the general population, the similarity it shares with those from other published reports may suggest its applicability beyond our study cohort.
The decision to perform stress testing in the evaluation of chest pain is often based on the pretest likelihood of coronary artery disease (CAD).1-7 Cardiac risk scores, which incorporate smoking status, blood pressure, diabetes mellitus, and cholesterol levels, also may provide further risk stratification.8-11 Assuming that the prevalence of CAD increases with age, young adults could be deemed low risk, not warranting cardiac screening.12
Professional society guidelines from the American College of Cardiology/American Heart Association and American College of Physicians4,5 recommend stress testing as the initial diagnostic test for CAD in symptomatic patients; additionally, the guidelines also suggest that screening stress tests may confer primary prevention benefit in intermediate-risk asymptomatic patients.9,13 Exercise treadmill testing is considered the initial modality of choice, given its technical ease and lower cost, compared with stress echocardiography.14
Previously published reports have shown the limited use of stress testing to screen young asymptomatic adults.15-17 Because this patient demographic typically has a low pretest likelihood of CAD, positive stress tests are often false-positive results.7,18 The consequence of false-positive testing may be unnecessary additional cardiac testing, potentially leading to more patient harm than benefit.18,19 For active-duty service members, false-positive testing also has the potential to affect worldwide deployability and/or sea duty status while further risk stratification is performed; as a result, mission readiness may be impacted.Although the number of clinic visits for chest pain has declined, there has been a discordant increase in the rates of stress testing in the US.20-22 Additionally, the rate of stress testing among young adults, specifically in the 25- to 34-year age group, has increased in recent years. Given the rising use of stress tests in the young patient population, the clinical use of stress testing needs to be reassessed.
Although much of the literature has already demonstrated the low value of stress testing in young asymptomatic adults, no data currently exist regarding its outpatient use in evaluating young symptomatic patients. The military represents a predominantly young cross-section of the general population suitable for exploring this topic. Using a cohort of active-duty service members, we aimed to determine the use of outpatient stress testing in evaluating young patients with atypical chest pain.
Methods
The US Department of Defense (DoD) Military Health System Database Repository (MDR) and Comprehensive Ambulatory Professional Encounter Record (CAPER) were the data sources for this study. The MDR contains continually updated, longitudinal electronic medical records (EMRs) for nearly 1.4 million active-duty service members and is composed of administrative, medical, pharmacy, and clinical data. The Naval Medical Center Portsmouth (NMCP) Institutional Review Board approved this study.
Study Cohort
We performed chart reviews of service members aged 18 to 35 years who received cardiac stress testing at NMCP, an academic tertiary care center, within 30 days after an office visit for atypical chest pain between October 1, 2010, and September 30, 2015. Atypical chest pain was defined as any outpatient claim with ICD-9 code, 786.5x, in the primary diagnosis field (Table 1).4
Demographics and cardiac risk factors (ie, hypertension, hyperlipidemia, diabetes mellitus, and smoking status) were assessed prior to index chest pain evaluations and defined via ICD-9 codes within outpatient records.
Cardiac Testing Outcomes
Patients were initially categorized by the results of baseline electrocardiograms (ECG) and index stress tests (ie, exercise treadmill or stress echocardiography, exercise or Lexiscan myocardial perfusion imaging, dobutamine stress echocardiography). Positive tests were defined as those having electrical or structural ischemic changes. Chronotropic changes were infrequent and nonpathologic and were not counted. Patient endpoints were either additional cardiac testing or negative index stress test without additional testing.
Statistical Analysis
The agreement between both baseline ECG and index stress test as well as index stress test and additional cardiac testing were analyzed using McNemar test and matched-pair odds ratios (ORs) with corresponding 95% CIs. Analyses were stratified by demographics and cardiac risk factors to assess for potential confounding. Analyses were performed using SAS version 9.4 (Cary, NC).
Results
A total of 1,036 patients were evaluated for atypical chest pain and had index stress testing between October 1, 2010 and September 30, 2015. The study cohort was 69% male with a mean (SD) age of 27.3 (4.7) years. More than 60% of the cohort was older than aged > 25 years.
In the initial testing cohort, exercise treadmill test (59.3%) and exercise echocardiogram (37.1%) were the most common stress testing modalities. The mean (SD) metabolic equivalents (METS) achieved among individuals who performed exercise stress testing was 13.9 (2.8). There were 65 patients who had a positive baseline ECG/negative index stress test, 958 patients had a negative ECG/negative index test, and 8 patients had a negative ECG/positive index test.
There were 102 patients (10%) who performed additional cardiac testing. Among this subgroup, 13 patients (1.3%) had additional testing for further evaluation of a positive index stress test (Table 4) and 89 patients (8.6%) had testing for continuing atypical chest pain despite a negative index stress test.
Coronary computed tomography angiography (CCTA) demonstrated nonobstructive CAD in 3 patients (0.3%) within the study cohort. There was no obstructive CAD identified in our cohort. Two patients had negative left heart catheterizations (LHC). One of these patients had a negative LHC and a negative Lexiscan after a CCTA showed CAD; all 3 of these additional tests were performed for evaluation of continued chest pain despite negative index stress testing. The positive predictive value of cardiac stress testing for nonobstructive CAD in this low-risk population was 15.4% (2 of 13). Stratification by demographics, CAD risk factors, and cardiac test results revealed no presence of confounding factors during analyses.
Discussion
In this retrospective, observational study of 1,036 young patients with atypical chest pain who had stress testing, there was relatively strong agreement between baseline ECG and index stress test results. Individuals also were 8 times more likely to have positive baseline ECGs and negative stress testing than having the opposite finding. Additional cardiac testing similarly demonstrated congruency with index stress testing and showed the propensity for false-positive stress tests. Further testing with CCTA demonstrated minimal nonobstructive CAD in < 1% of the study cohort and 2 LHC were negative. Despite the low prevalence of CAD and apparent low diagnostic use of stress testing in our young cohort, symptomatic service members still require stress testing to determine deployment suitability.
The low yield of outpatient stress testing in our young population is rooted in Bayes’ theorem, which highlights the importance of pretest likelihood in the diagnosis of CAD.7,23 Because our cohort had a low prevalence and low pretest likelihood of CAD, positive index stress tests were often false-positive results and consequently did not increase the posttest likelihood of CAD, resulting in low positive predictive value. Additional cardiac testing had limited clinical value in our cohort. The 3 cases of nonobstructive CAD were unlikely to be pathologic given the minimal degree of observed stenosis and the 2 LHC did not require revascularization. These results are similar to those shown by Christman and colleagues and Mudrick and colleagues, which highlighted the low yield of additional cardiac studies and low rate of revascularization among symptomatic patients without known cardiac disease, respectively.18,19
This is the first study, to our knowledge, to quantitatively demonstrate the low use of outpatient stress testing for young adults with atypical chest pain. Previous studies that assessed stress testing for young patients with chest pain in acute settings such as emergency departments and chest pain observation units, similarly demonstrated minimal yield of routine diagnostic testing.23,24 This further highlights the premise that outpatient and even emergent-setting stress testing in low cardiac risk individuals may be of limited value and not always necessary.
Limitations
There were several study limitations. As a single-center, cross-sectional review, we may not be able to extrapolate our findings to the general population. However, given the low prevalence of CAD in young adults, stress testing would likely have limited value regardless of the sample distribution; so it may be possible to extend our findings beyond our cohort. Also, neither baseline ECG nor index stress test (irrespective of modality) could be given a diagnostic value in predicting ischemia alone; doing so would require comparison with the gold standard—heart catheterization. Although referral bias has been associated with diagnostic performance of stress testing, we did not adjust for this phenomenon.25 Given the higher average metabolic equivalents achieved in our cohort, this potential bias likely did not affect diagnostic performance.
Conclusion
There was low diagnostic use of outpatient stress testing and additional cardiac testing for CAD among young patients with atypical chest pain. The limited value of cardiac stress testing is likely a function of the low CAD prevalence within this population, suggesting that younger patients may not necessarily require stress testing for chest pain evaluations as long as pretest likelihood is low. Despite our results, we maintain that the decision to perform stress testing should still be guided by clinical judgment, but perhaps our findings may alleviate physicians’ concerns over the urgency of when to refer low-risk patients for testing. Although we are cautious in inferring our findings to the general population, the similarity it shares with those from other published reports may suggest its applicability beyond our study cohort.
1. Fowler-Brown A, Pignone M, Pletcher M, et al. Exercise tolerance testing to screen for coronary heart disease: a systematic review for the technical support for the U.S. Preventive Services Task Force. Ann Intern Med. 2004;140(7):W9-W24.
2. Gibbons RJ, Balady GJ, Bricker JT, et al; American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Committee to Update the 1997 Exercise Testing Guidelines. ACC/AHA 2002 guideline update for exercise testing: summary article. A report of the American College of Cardiology/American Heart Association Task Force on practice guidelines (Committee to Update the 1997 Exercise Testing Guidelines). J Am Coll Cardiol. 2002;40(8):1531-1540.
3. Chou R, Arora B, Dana T, Fu R, Miranda Walker M, Humphrey L. Screening Asymptomatic Adults for Coronary Heart Disease With Resting or Exercise Electrocardiography: Systematic Review to Update the 2004 U.S. Preventive Services Task Force recommendation. Evidence Synthesis No. 88. AHRQ Publication No. 11-05158-EF-1. Rockville, MD: Agency for Healthcare Research and Quality; September 2011.
4. Fihn S, Gardin J, Abrams J, et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiology. 2012;60(24):e44-e164.
5. Gibbons RJ, Balady GJ, Beasley JW, et al. ACC/AHA guidelines for exercise testing: executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Exercise Testing). Circulation. 1997;96(1):345-354.
6. Greenland P, Alpert JS, Beller GA, et al. 2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults. A report of the American College of Cardiology Foundation/ American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2010;56(25):e50-e103.
7. Diamond G, Forrester J. Analysis of probability as an aid in the clinical diagnosis of coronary artery disease. N Engl J Med. 1979;300(24):1350-1358.
8. Goff D, Lloyd-Jones D, Bennett G, et al; American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25)(suppl 2):S49-S73.
9. Greenland P, Gaziano J. Selecting asymptomatic patients for coronary computed tomography or electrocardiographic exercise testing. N Engl J Med. 2003;349(5):465-473.
10. Shah N, Soon K, Wong C, Kellu AM. Screening for asymptomatic coronary heart disease in the young ‘at risk’ population: who and how? Int J Cardiol Heart Vasc. 2014;6:60-65.
11. Morise A, Evans M, Jalisi F, Shetty R, Stauffer M. A pretest prognostic score to assess patients undergoing exercise or pharmacological stress testing. Heart. 2007;93(2):200-204.
12. Amsterdam EA, Kirk JD, Bluemke DA, et al; American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee of the Council on Clinical Cardiology, Council on Cardiovascular Nursing, and Interdisciplinary Council on Quality of Care and Outcomes Research. Testing of low-risk patients presenting to the emergency department with chest pain: a scientific statement from the American Heart Association. Circulation. 2010;122(17):1756-1776.
13. Livschitz S, Sharabi Y, Yushin J, et al. Limited clinical value of exercise stress test for the screening of coronary artery disease in young, asymptomatic adult men. Am J Cardiol. 2000;86(4):462-464.
14. Miller T. Stress testing: the case for the standard treadmill test. Curr Opin Cardiol. 2011;26(5):363-369.
15. La Gerche A, Baggish A, Knuuti J, et al. Cardiac imaging and stress testing asymptomatic athletes to identify those at risk of sudden cardiac death. JACC Cardiovasc Imaging. 2013;6(9):993-1007.
16. Lauer M, Froelicher ES, Williams M, Kligfield P; American Heart Association Council on Clinical Cardiology, Subcommittee on Exercise, Cardiac Rehabilitation, and Prevention. Exercise testing in asymptomatic adults: a statement for professionals from the American Heart Association Council on Clinical Cardiology, Subcommittee on Exercise, Cardiac Rehabilitation, and Prevention. Circulation. 2005;112(5):771-776.
17. Sammito S, Gundlach N, Bockelmann I. Prevalence of cardiac arrhythmia under stress conditions in occupational health assessments of young military servicemen and servicewomen. Mil Med. 2016;181(4):369-372.
18. Mudrick DW, Cowper PA, Shah BR, et al. Downstream procedures and outcomes after stress testing for chest pain without known coronary artery disease in the United States. Am Heart J. 2012;163(3):454-461.
19. Christman MP, Bittencourt MS, Hulten E, et al. Yield of downstream tests after exercise treadmill testing. J Am Coll Cardiol. 2014;63(13):1264-1274.
20. Will J, Loustalot F, Hong Y. National trends in visits to physician offices and outpatient clinics for angina 1995 to 2010. Circ Cardiovasc Qual Outcomes. 2014;7(1):110-117.
21. Kini V, McCarthy F, Dayoub E, et al. Cardiac stress test trends among US patients younger than 65 years, 2005-2012. JAMA Cardiol. 2016;1(9):1038-1042.
22. Ladapo JA, Blecker S, Douglas PS. Physician decision making and trends in the use of cardiac stress testing in the United States: an analysis of repeated cross-sectional data. Ann Intern Med. 2014;161(7):482-490.
23. Winchester DE, Brandt J, Schmidt C, Schmidt C, Allen B, Payton T, Amsterdam EA. Diagnostic yield of routine noninvasive cardiovascular testing in low-risk acute chest pain patients. Am J Cardiol. 2015;116(2):204-207.
24. Hermann L, Weingart SD, Duvall W, Henzlova MJ. The limited utility of routine cardiac stress testing in emergency department chest pain patients younger than 40 years. Ann Emerg Med. 2009;54(1):12-16.
25. Ladapo JA, Blecker S, Elashoff MR, et al. Clinical implications of referral bias in the diagnostic performance of exercise testing for coronary artery disease. J Am Heart Assoc. 2013;2(6):e000505.
1. Fowler-Brown A, Pignone M, Pletcher M, et al. Exercise tolerance testing to screen for coronary heart disease: a systematic review for the technical support for the U.S. Preventive Services Task Force. Ann Intern Med. 2004;140(7):W9-W24.
2. Gibbons RJ, Balady GJ, Bricker JT, et al; American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Committee to Update the 1997 Exercise Testing Guidelines. ACC/AHA 2002 guideline update for exercise testing: summary article. A report of the American College of Cardiology/American Heart Association Task Force on practice guidelines (Committee to Update the 1997 Exercise Testing Guidelines). J Am Coll Cardiol. 2002;40(8):1531-1540.
3. Chou R, Arora B, Dana T, Fu R, Miranda Walker M, Humphrey L. Screening Asymptomatic Adults for Coronary Heart Disease With Resting or Exercise Electrocardiography: Systematic Review to Update the 2004 U.S. Preventive Services Task Force recommendation. Evidence Synthesis No. 88. AHRQ Publication No. 11-05158-EF-1. Rockville, MD: Agency for Healthcare Research and Quality; September 2011.
4. Fihn S, Gardin J, Abrams J, et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiology. 2012;60(24):e44-e164.
5. Gibbons RJ, Balady GJ, Beasley JW, et al. ACC/AHA guidelines for exercise testing: executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Exercise Testing). Circulation. 1997;96(1):345-354.
6. Greenland P, Alpert JS, Beller GA, et al. 2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults. A report of the American College of Cardiology Foundation/ American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2010;56(25):e50-e103.
7. Diamond G, Forrester J. Analysis of probability as an aid in the clinical diagnosis of coronary artery disease. N Engl J Med. 1979;300(24):1350-1358.
8. Goff D, Lloyd-Jones D, Bennett G, et al; American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25)(suppl 2):S49-S73.
9. Greenland P, Gaziano J. Selecting asymptomatic patients for coronary computed tomography or electrocardiographic exercise testing. N Engl J Med. 2003;349(5):465-473.
10. Shah N, Soon K, Wong C, Kellu AM. Screening for asymptomatic coronary heart disease in the young ‘at risk’ population: who and how? Int J Cardiol Heart Vasc. 2014;6:60-65.
11. Morise A, Evans M, Jalisi F, Shetty R, Stauffer M. A pretest prognostic score to assess patients undergoing exercise or pharmacological stress testing. Heart. 2007;93(2):200-204.
12. Amsterdam EA, Kirk JD, Bluemke DA, et al; American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee of the Council on Clinical Cardiology, Council on Cardiovascular Nursing, and Interdisciplinary Council on Quality of Care and Outcomes Research. Testing of low-risk patients presenting to the emergency department with chest pain: a scientific statement from the American Heart Association. Circulation. 2010;122(17):1756-1776.
13. Livschitz S, Sharabi Y, Yushin J, et al. Limited clinical value of exercise stress test for the screening of coronary artery disease in young, asymptomatic adult men. Am J Cardiol. 2000;86(4):462-464.
14. Miller T. Stress testing: the case for the standard treadmill test. Curr Opin Cardiol. 2011;26(5):363-369.
15. La Gerche A, Baggish A, Knuuti J, et al. Cardiac imaging and stress testing asymptomatic athletes to identify those at risk of sudden cardiac death. JACC Cardiovasc Imaging. 2013;6(9):993-1007.
16. Lauer M, Froelicher ES, Williams M, Kligfield P; American Heart Association Council on Clinical Cardiology, Subcommittee on Exercise, Cardiac Rehabilitation, and Prevention. Exercise testing in asymptomatic adults: a statement for professionals from the American Heart Association Council on Clinical Cardiology, Subcommittee on Exercise, Cardiac Rehabilitation, and Prevention. Circulation. 2005;112(5):771-776.
17. Sammito S, Gundlach N, Bockelmann I. Prevalence of cardiac arrhythmia under stress conditions in occupational health assessments of young military servicemen and servicewomen. Mil Med. 2016;181(4):369-372.
18. Mudrick DW, Cowper PA, Shah BR, et al. Downstream procedures and outcomes after stress testing for chest pain without known coronary artery disease in the United States. Am Heart J. 2012;163(3):454-461.
19. Christman MP, Bittencourt MS, Hulten E, et al. Yield of downstream tests after exercise treadmill testing. J Am Coll Cardiol. 2014;63(13):1264-1274.
20. Will J, Loustalot F, Hong Y. National trends in visits to physician offices and outpatient clinics for angina 1995 to 2010. Circ Cardiovasc Qual Outcomes. 2014;7(1):110-117.
21. Kini V, McCarthy F, Dayoub E, et al. Cardiac stress test trends among US patients younger than 65 years, 2005-2012. JAMA Cardiol. 2016;1(9):1038-1042.
22. Ladapo JA, Blecker S, Douglas PS. Physician decision making and trends in the use of cardiac stress testing in the United States: an analysis of repeated cross-sectional data. Ann Intern Med. 2014;161(7):482-490.
23. Winchester DE, Brandt J, Schmidt C, Schmidt C, Allen B, Payton T, Amsterdam EA. Diagnostic yield of routine noninvasive cardiovascular testing in low-risk acute chest pain patients. Am J Cardiol. 2015;116(2):204-207.
24. Hermann L, Weingart SD, Duvall W, Henzlova MJ. The limited utility of routine cardiac stress testing in emergency department chest pain patients younger than 40 years. Ann Emerg Med. 2009;54(1):12-16.
25. Ladapo JA, Blecker S, Elashoff MR, et al. Clinical implications of referral bias in the diagnostic performance of exercise testing for coronary artery disease. J Am Heart Assoc. 2013;2(6):e000505.