User login
Depressed and awkward: Is it more than that?
CASE Treatment-resistant MDD
Ms. P, age 21, presents to the outpatient clinic. She has diagnoses of treatment-resistant major depressive disorder (MDD) and schizoid personality disorder (SPD). Ms. P was diagnosed with MDD 3 years ago after reporting symptoms of prevailing sadness for approximately 8 years, described as feelings of worthlessness, anhedonia, social withdrawal, and decreased hygiene and self-care behaviors, as well as suicidal ideation and self-harm. SPD was diagnosed 1 year earlier based on her “odd” behaviors and disheveled appearance following observation and in collateral with her family. Her odd behaviors are described as spending most of her time alone, preferring solitary activities, and having little contact with people other than her parents.
Ms. P reports that she was previously treated with citalopram, 20 mg/d, bupropion, 150 mg/d, aripiprazole, 3.75 mg/d, topiramate, 100 mg twice daily, and melatonin, 9 mg/d at bedtime, but discontinued follow-up appointments and medications after no significant improvement in symptoms.
[polldaddy:11027942]
The authors’ observations
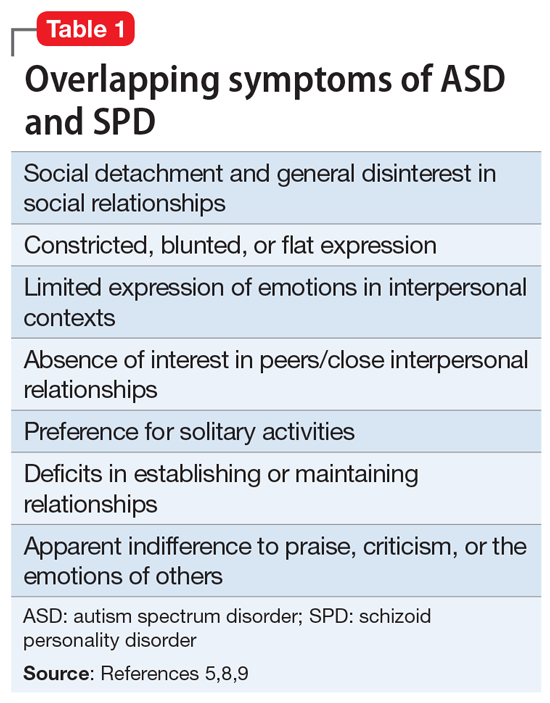
The term “schizoid” first made its debut in the medical community to describe the prodromal social withdrawal and isolation observed in schizophrenia.1 The use of schizoid to describe a personality type first occurred in DSM-III in 1980.2 SPD is a Cluster A personality disorder that groups personalities characterized by common traits that are “odd” or “eccentric” and may resemble the positive and/or negative symptoms of schizophrenia.3,4 Relatively uncommon in clinical settings, SPD includes individuals who do not desire or enjoy close relationships. Those afflicted with SPD will be described as isolated, aloof, and detached from social relationships with others, even immediate family members. Individuals with SPD may appear indifferent to criticism and praise, and may take pleasure in only a few activities. They may exhibit a general absence of affective range, which contributes to their characterization as flat, blunted, or emotionally vacant. SPD is more commonly diagnosed in males and may be present in childhood and adolescence. These children are typified by solitariness, poor peer relationships, and underachievement in school. SPD impacts 3.1% to 4.9% of the United States population and approximately 1% of community populations.5,6
EVALUATION Persistent depressive symptoms
Ms. P is accompanied by her parents for the examination. She reports a chronic, persistent sad mood, hopelessness, anergia, insomnia, anhedonia, and decreased concentration and appetite. She says she experiences episodes of intense worry, along with tension, restlessness, feelings of being on the edge, irritability, and difficulty relaxing. Socially, she is withdrawn, preferring to stay alone in her room most of the day watching YouTube or trying to write stories. She has 2 friends with whom she does not interact with in person, but rather through digital means. Ms. P has never enjoyed attending school and feels “nervous” when she is around people. She has difficulty expressing her thoughts and often looks to her parents for help. Her parents add that getting Ms. P to attend school was a struggle, which resulted in periods of home schooling throughout high school.
The treating team prescribes citalopram, 10 mg/d, and aripiprazole, 2 mg/d. On subsequent follow-up visits, Ms. P’s depression improves with an increase in citalopram to 40 mg/d. Psychotherapy is added to her treatment plan to help address the persistent social deficits, odd behavior, and anxieties.
Continue to: Evaluation Psychological assessment...
EVALUATION Psychological assessment
At her psychotherapy intake appointment with the clinical neuropsychologist, Ms. P is dressed in purple from head to toe and sits clutching her purse and looking at the ground. She is overweight with clean, fitting clothing. Ms. P takes a secondary role during most of the interview, allowing her parents to answer most questions. When asked why she is starting therapy, Ms. P replies, “Well, I’ve been using the bathroom a lot.” She describes a feeling of comfort and calmness while in the restroom. Suddenly, she asks her parents to exit the exam room for a moment. Once they leave, she leans in and whispers, “Have you ever heard of self-sabotage? I think that’s what I’m doing.”
Her mood is euthymic, with a blunted affect. She scores 2 on the Patient Health Questionnaire-9 (PHQ-9) and 10 on the Generalized Anxiety Disorder 7-item scale (GAD-7), which indicates the positive impact of medication on her depressive symptoms but continuing moderate anxious distress. She endorses fear of the night, insomnia, and suicidal ideation. She reports an unusual “constant itching sensation,” resulting in hours of repetitive excoriation. Physical examination reveals several significant scars and scabs covering her bilateral upper and lower extremities. Her vocational history is brief; she had held 2 entry-level customer service positions that lasted <1 year. She was fired due to excessive bathroom use.
As the interview progresses, the intake clinician’s background in neuropsychological assessment facilitates screening for possible developmental disorders. Given the nature of the referral and psychotherapy intake, a full neuropsychological assessment is not conducted. The clinician emphasizes verbal abstraction and theory of mind. Ms. P’s IQ was estimated to be average by Wide Range Achievement Test 4 word reading and interview questions about her academic history. Questions are abstracted from the Autism Diagnostic Observation Schedule, Module 4, to assess for conversation ability, emotional insight, awareness and expression, relationships, and areas of functioning in daily living. Developmental history questions, such as those found on the Adaptive Behavior Assessment System, 3rd edition, help guide developmental information provided by parents in the areas of communication, emotion and eye-gaze, gestures, sensory function, language, social functioning, hygiene behavior, and specific interests.
Ms. P’s mother describes a normal pregnancy and delivery; however, she states that Ms. P was “born with problems,” including difficulty with rooting and sucking, and required gastrointestinal intubation until age 3. Cyclical vomiting followed normal food consumption. Ambulation, language acquisition, toilet training, and hygiene behavior were delayed. Ms. P experienced improvements with early intervention in intensive physical and occupational therapy.
Ms. P’s hygiene is well below average, and she requires cueing from her parents. She attended general education until she reached high school, when she began special education. She was sensitive to sensory stimulation from infancy, with sensory sensitivity to textures. Ms. P continues to report sensory sensitivity and lapses in hygiene.
She has difficulty establishing and maintaining relationships with her peers, and prefers solitary activities. Ms. P has no history of romantic relationships, although she does desire one. When asked about her understanding of various relationships, Ms. P’s responses are stereotyped, such as “I know someone is my friend because they are nice to me” and “People get married because they love each other.” She struggles to offer greater insight into the nuances that form lasting relationships and bonds. Ms. P struggles to imitate and describe the physical and internal cues of several basic emotions (eg, fear, joy, anger).
Her conversational and social skills are assessed by asking her to engage in a conversation with the examiner as if meeting for the first time. Her speech is reciprocal, aprosodic, and delayed. The conversation is one-sided, and the examiner fills in several awkward pauses. Ms. P’s gaze at times is intense and prolonged, especially when responding to questions. She tends to use descriptive statements (eg, “I like your purple pen, I like your shirt”) to engage in conversation, rather than gathering more information through reflective statements, questions, or expressing a shared interest.
Ms. P’s verbal abstraction is screened using questions from the Wechsler Adult Intelligence Scale, 4th edition Similarities subtest, to which she provides several responses within normal limits. Her understanding of colloquial speech is assessed by asking her the meaning of common phrases (eg, “Get knocked down 9 times, get up 10,” “Jack and Jill are 2 peas in a pod”). On many occasions, she is able to limit her response to 1 word, (eg, “resiliency”), demonstrating intact ability to decipher idioms.
[polldaddy:11027971]
The authors’ observations
Upon reflection of Ms. P’s clinical presentation and history of developmental delays, social deficits, sensory sensitivity since infancy, and repetitive behaviors (all which continue to impact her), the clinical team concluded that the diagnosis of autism spectrum disorder (ASD) helps explain the patient’s “odd” behaviors, more so than SPD.
ASD is a heterogenous, complex neuropsychiatric disorder characterized by a persistent deficit in social reciprocity, verbal, and nonverbal communication, and includes a pattern of restricted, repetitive and/or stereotyped behaviors and/or interests.5 The term “autismus” is Greek meaning “self,” and was first used to classify the qualities of “morbid self-admiration” observed in prodromal schizophrenia.7
To properly distinguish these disorders, keep in mind that patients with ASD have repetitive and restricted patterns of behaviors or interests that are not found in SPD, and experience deficits in forming, maintaining, and understanding relationships since they lack those skills, while patients with SPD are more prone to desire solitary activities and limited relationships.5,9
There has been an increased interest in determining why for some patients the diagnosis of ASD is delayed until they reach adulthood. Limited or no access to the patient’s childhood caregiver to obtain a developmental history, as well as generational differences on what constitutes typical childhood behavior, could contribute to a delayed diagnosis of ASD until adulthood. Some patients develop camouflaging strategies that allow them to navigate social expectations to a limited degree, such as learning stock phrases, imitating gestures, and telling anecdotes. Another factor to consider is that co-occurring psychiatric disorders may take center stage when patients present for mental health services.10 Fusar-Poli et al11 investigated the characteristics of patients who received a diagnosis of ASD in adulthood. They found that the median time from the initial clinical evaluation to diagnosis of ASD in adulthood was 11 years. In adults identified with ASD, their cognitive abilities ranged from average to above average, and they required less support. Additionally, they also had higher rates of being previously diagnosed with psychotic disorders and personality disorders.11
It is important to keep in mind that the wide spectrum of autism as currently defined by DSM-5 and its overlap of symptoms with other psychiatric disorders can make the diagnosis challenging for both child and adolescent psychiatrists and adult psychiatrists and might help explain why severe cases of ASD are more readily identified earlier than milder cases of ASD.10
Ms. P’s case is also an example of how women are more likely than men to be overlooked when evaluated for ASD. According to DSM-5, the estimated gender ratio for ASD is believed to be 4:1 (male:female).5 However, upon systematic review and meta-analysis, Loomes et al12 found that the gender ratio may be closer to 3:1 (male:female). These authors suggested that diagnostic bias and a failure of passive case ascertainment to estimate gender ratios as stated by DSM-5 in identifying ASD might explain the lower gender ratio.12 A growing body of evidence suggests that ASD is different in males and females. A 2019 qualitative study by Milner et al13 found that female participants reported using masking and camouflaging strategies to appear neurotypical. Compensatory behaviors were found to be linked to a delay in diagnosis and support for ASD.13
Cognitive ability as measured by IQ has also been found to be a factor in receiving a diagnosis of ASD. In a 2010 secondary analysis of a population-based study of the prevalence of ASD, Giarelli et al14found that girls with cognitive impairments as measured by IQ were less likely to be diagnosed with ASD than boys with cognitive impairment, despite meeting the criteria for ASD. Females tend to exhibit fewer repetitive behaviors than males, and tend to be more likely to show accompanying intellectual disability, which suggests that females with ASD may go unrecognized when they exhibit average intelligence with less impairment of behavior and subtler manifestation of social and communication deficits.15 Consequently, females tend to receive this diagnosis later than males.
Continue to: Treatment...
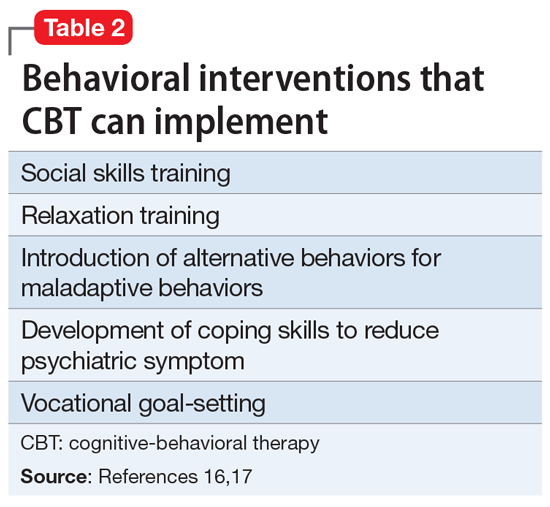
TREATMENT Adding CBT
At an interdisciplinary session several weeks later that includes Ms. P and her parents, the treatment team discusses the revised diagnoses of ASD and MDD, a treatment recommendation for cognitive-behavioral therapy (CBT), and continued use of medication. At this session, Ms. P discloses that she has not been consistent with her medication regimen since her last appointment, which helps explain the increase in her PHQ-9 score from 2 to 14 and GAD-7 score
[polldaddy:11027990]
The authors’ observations
CBT can be helpful in improving medication adherence, developing coping skills, and modifying maladaptive behaviors.
OUTCOME Improvement with psychotherapy
Ms. P and family agree with the team’s recommendations. The aims of Ms. P’s psychotherapy are to maintain medication compliance; implement behavioral modification, vocational rehabilitation, and community engagement; develop social skills; increase functional independence; and develop coping skills for depression and anxiety.
Bottom Line
The prevalence of schizoid personality disorder (SPD) is low, and its symptoms overlap with those of autism spectrum disorder. Therefore, before diagnosing SPD in an adult patient, it is important to obtain a detailed developmental history and include an interdisciplinary team to assess for autism spectrum disorder.
1. Fariba K, Gupta V. Schizoid personality disorder. StatPearls Publishing. Updated June 9, 2021. Accessed January 6, 2021. https://www.ncbi.nlm.nih.gov/books/NBK559234/
2. Diagnostic and Statistical Manual of Mental Disorders: DSM-III. 3rd ed rev. American Psychiatric Association; 1987.
3. Esterberg ML, Goulding SM, Walker EF. Cluster A personality disorders: schizotypal, schizoid and paranoid personality disorders in childhood and adolescence. J Psychopathol Behav Assess. 2010;32(4):515-528. doi:10.1007/s10862-010-9183-8
4. Kalus O, Bernstein DP, Siever LJ. Schizoid personality disorder: a review of current status and implications for DSM-IV. Journal of Personality Disorders. 1993;7(1), 43-52.
5. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. American Psychiatric Association; 2013.
6. Eaton NR, Greene AL. Personality disorders: community prevalence and socio-demographic correlates. Curr Opin Psychol. 2018;21:28-32. doi:10.1016/j.copsyc.2017.09.001
7. Vatano
8. Ritsner MS. Handbook of Schizophrenia Spectrum Disorders, Volume I: Conceptual Issues and Neurobiological Advances. Springer; 2011.
9. Cook ML, Zhang Y, Constantino JN. On the continuity between autistic and schizoid personality disorder trait burden: a prospective study in adolescence. J Nerv Ment Dis. 2020;208(2):94-100. doi:10.1097/NMD.0000000000001105
10. Lai MC, Baron-Cohen S. Identifying the lost generation of adults with autism spectrum conditions. Lancet Psychiatry. 2015;2(11):1013-1027. doi:10.1016/S2215-0366(15)00277-1
11. Fusar-Poli L, Brondino N, Politi P, et al. Missed diagnoses and misdiagnoses of adults with autism spectrum disorder. Eur Arch Psychiatry Clin Neurosci. 2020;10.1007/s00406-020-01189-2. doi:10.1007/s00406-020-01189-w
12. Loomes R, Hull L, Mandy WPL. What is the male-to-female ratio in autism spectrum disorder? A systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry. 2017;56(6):466-474. doi:10.1016/j.jaac.2017.03.013
13. Milner V, McIntosh H, Colvert E, et al. A qualitative exploration of the female experience of autism spectrum disorder (ASD). J Autism Dev Disord. 2019;49(6):2389-2402. doi:10.1007/s10803-019-03906-4
14. Giarelli E, Wiggins LD, Rice CE, et al. Sex differences in the evaluation and diagnosis of autism spectrum disorders among children. Disabil Health J. 2010;3(2):107-116. doi:10.1016/j.dhjo.2009.07.001
15. Frazier TW, Georgiades S, Bishop SL, et al. Behavioral and cognitive characteristics of females and males with autism in the Simons Simplex Collection. J Am Acad Child Adolesc Psychiatry. 2014;53(3):329-40.e403. doi:10.1016/j.jaac.2013.12.004
16. Julius RJ, Novitsky MA Jr, et al. Medication adherence: a review of the literature and implications for clinical practice. J Psychiatr Pract. 2009;15(1):34-44. doi:10.1097/01.pra.0000344917.43780.77
17. Spain D, Sin J, Chalder T, et al. Cognitive behaviour therapy for adults with autism spectrum disorders and psychiatric co-morbidity: a review. Research in Autism Spectrum Disorders. 2015;9, 151-162. https://doi.org/10.1016/j.rasd.2014.10.019
18. Bishop-Fitzpatrick L, Minshew NJ, Eack SM. A systematic review of psychosocial interventions for adults with autism spectrum disorders. J Autism Dev Disord. 2013;43(3):687-694. doi:10.1007/s10803-012-1615-8
CASE Treatment-resistant MDD
Ms. P, age 21, presents to the outpatient clinic. She has diagnoses of treatment-resistant major depressive disorder (MDD) and schizoid personality disorder (SPD). Ms. P was diagnosed with MDD 3 years ago after reporting symptoms of prevailing sadness for approximately 8 years, described as feelings of worthlessness, anhedonia, social withdrawal, and decreased hygiene and self-care behaviors, as well as suicidal ideation and self-harm. SPD was diagnosed 1 year earlier based on her “odd” behaviors and disheveled appearance following observation and in collateral with her family. Her odd behaviors are described as spending most of her time alone, preferring solitary activities, and having little contact with people other than her parents.
Ms. P reports that she was previously treated with citalopram, 20 mg/d, bupropion, 150 mg/d, aripiprazole, 3.75 mg/d, topiramate, 100 mg twice daily, and melatonin, 9 mg/d at bedtime, but discontinued follow-up appointments and medications after no significant improvement in symptoms.
[polldaddy:11027942]
The authors’ observations
The term “schizoid” first made its debut in the medical community to describe the prodromal social withdrawal and isolation observed in schizophrenia.1 The use of schizoid to describe a personality type first occurred in DSM-III in 1980.2 SPD is a Cluster A personality disorder that groups personalities characterized by common traits that are “odd” or “eccentric” and may resemble the positive and/or negative symptoms of schizophrenia.3,4 Relatively uncommon in clinical settings, SPD includes individuals who do not desire or enjoy close relationships. Those afflicted with SPD will be described as isolated, aloof, and detached from social relationships with others, even immediate family members. Individuals with SPD may appear indifferent to criticism and praise, and may take pleasure in only a few activities. They may exhibit a general absence of affective range, which contributes to their characterization as flat, blunted, or emotionally vacant. SPD is more commonly diagnosed in males and may be present in childhood and adolescence. These children are typified by solitariness, poor peer relationships, and underachievement in school. SPD impacts 3.1% to 4.9% of the United States population and approximately 1% of community populations.5,6
EVALUATION Persistent depressive symptoms
Ms. P is accompanied by her parents for the examination. She reports a chronic, persistent sad mood, hopelessness, anergia, insomnia, anhedonia, and decreased concentration and appetite. She says she experiences episodes of intense worry, along with tension, restlessness, feelings of being on the edge, irritability, and difficulty relaxing. Socially, she is withdrawn, preferring to stay alone in her room most of the day watching YouTube or trying to write stories. She has 2 friends with whom she does not interact with in person, but rather through digital means. Ms. P has never enjoyed attending school and feels “nervous” when she is around people. She has difficulty expressing her thoughts and often looks to her parents for help. Her parents add that getting Ms. P to attend school was a struggle, which resulted in periods of home schooling throughout high school.
The treating team prescribes citalopram, 10 mg/d, and aripiprazole, 2 mg/d. On subsequent follow-up visits, Ms. P’s depression improves with an increase in citalopram to 40 mg/d. Psychotherapy is added to her treatment plan to help address the persistent social deficits, odd behavior, and anxieties.
Continue to: Evaluation Psychological assessment...
EVALUATION Psychological assessment
At her psychotherapy intake appointment with the clinical neuropsychologist, Ms. P is dressed in purple from head to toe and sits clutching her purse and looking at the ground. She is overweight with clean, fitting clothing. Ms. P takes a secondary role during most of the interview, allowing her parents to answer most questions. When asked why she is starting therapy, Ms. P replies, “Well, I’ve been using the bathroom a lot.” She describes a feeling of comfort and calmness while in the restroom. Suddenly, she asks her parents to exit the exam room for a moment. Once they leave, she leans in and whispers, “Have you ever heard of self-sabotage? I think that’s what I’m doing.”
Her mood is euthymic, with a blunted affect. She scores 2 on the Patient Health Questionnaire-9 (PHQ-9) and 10 on the Generalized Anxiety Disorder 7-item scale (GAD-7), which indicates the positive impact of medication on her depressive symptoms but continuing moderate anxious distress. She endorses fear of the night, insomnia, and suicidal ideation. She reports an unusual “constant itching sensation,” resulting in hours of repetitive excoriation. Physical examination reveals several significant scars and scabs covering her bilateral upper and lower extremities. Her vocational history is brief; she had held 2 entry-level customer service positions that lasted <1 year. She was fired due to excessive bathroom use.
As the interview progresses, the intake clinician’s background in neuropsychological assessment facilitates screening for possible developmental disorders. Given the nature of the referral and psychotherapy intake, a full neuropsychological assessment is not conducted. The clinician emphasizes verbal abstraction and theory of mind. Ms. P’s IQ was estimated to be average by Wide Range Achievement Test 4 word reading and interview questions about her academic history. Questions are abstracted from the Autism Diagnostic Observation Schedule, Module 4, to assess for conversation ability, emotional insight, awareness and expression, relationships, and areas of functioning in daily living. Developmental history questions, such as those found on the Adaptive Behavior Assessment System, 3rd edition, help guide developmental information provided by parents in the areas of communication, emotion and eye-gaze, gestures, sensory function, language, social functioning, hygiene behavior, and specific interests.
Ms. P’s mother describes a normal pregnancy and delivery; however, she states that Ms. P was “born with problems,” including difficulty with rooting and sucking, and required gastrointestinal intubation until age 3. Cyclical vomiting followed normal food consumption. Ambulation, language acquisition, toilet training, and hygiene behavior were delayed. Ms. P experienced improvements with early intervention in intensive physical and occupational therapy.
Ms. P’s hygiene is well below average, and she requires cueing from her parents. She attended general education until she reached high school, when she began special education. She was sensitive to sensory stimulation from infancy, with sensory sensitivity to textures. Ms. P continues to report sensory sensitivity and lapses in hygiene.
She has difficulty establishing and maintaining relationships with her peers, and prefers solitary activities. Ms. P has no history of romantic relationships, although she does desire one. When asked about her understanding of various relationships, Ms. P’s responses are stereotyped, such as “I know someone is my friend because they are nice to me” and “People get married because they love each other.” She struggles to offer greater insight into the nuances that form lasting relationships and bonds. Ms. P struggles to imitate and describe the physical and internal cues of several basic emotions (eg, fear, joy, anger).
Her conversational and social skills are assessed by asking her to engage in a conversation with the examiner as if meeting for the first time. Her speech is reciprocal, aprosodic, and delayed. The conversation is one-sided, and the examiner fills in several awkward pauses. Ms. P’s gaze at times is intense and prolonged, especially when responding to questions. She tends to use descriptive statements (eg, “I like your purple pen, I like your shirt”) to engage in conversation, rather than gathering more information through reflective statements, questions, or expressing a shared interest.
Ms. P’s verbal abstraction is screened using questions from the Wechsler Adult Intelligence Scale, 4th edition Similarities subtest, to which she provides several responses within normal limits. Her understanding of colloquial speech is assessed by asking her the meaning of common phrases (eg, “Get knocked down 9 times, get up 10,” “Jack and Jill are 2 peas in a pod”). On many occasions, she is able to limit her response to 1 word, (eg, “resiliency”), demonstrating intact ability to decipher idioms.
[polldaddy:11027971]
The authors’ observations
Upon reflection of Ms. P’s clinical presentation and history of developmental delays, social deficits, sensory sensitivity since infancy, and repetitive behaviors (all which continue to impact her), the clinical team concluded that the diagnosis of autism spectrum disorder (ASD) helps explain the patient’s “odd” behaviors, more so than SPD.
ASD is a heterogenous, complex neuropsychiatric disorder characterized by a persistent deficit in social reciprocity, verbal, and nonverbal communication, and includes a pattern of restricted, repetitive and/or stereotyped behaviors and/or interests.5 The term “autismus” is Greek meaning “self,” and was first used to classify the qualities of “morbid self-admiration” observed in prodromal schizophrenia.7
To properly distinguish these disorders, keep in mind that patients with ASD have repetitive and restricted patterns of behaviors or interests that are not found in SPD, and experience deficits in forming, maintaining, and understanding relationships since they lack those skills, while patients with SPD are more prone to desire solitary activities and limited relationships.5,9
There has been an increased interest in determining why for some patients the diagnosis of ASD is delayed until they reach adulthood. Limited or no access to the patient’s childhood caregiver to obtain a developmental history, as well as generational differences on what constitutes typical childhood behavior, could contribute to a delayed diagnosis of ASD until adulthood. Some patients develop camouflaging strategies that allow them to navigate social expectations to a limited degree, such as learning stock phrases, imitating gestures, and telling anecdotes. Another factor to consider is that co-occurring psychiatric disorders may take center stage when patients present for mental health services.10 Fusar-Poli et al11 investigated the characteristics of patients who received a diagnosis of ASD in adulthood. They found that the median time from the initial clinical evaluation to diagnosis of ASD in adulthood was 11 years. In adults identified with ASD, their cognitive abilities ranged from average to above average, and they required less support. Additionally, they also had higher rates of being previously diagnosed with psychotic disorders and personality disorders.11
It is important to keep in mind that the wide spectrum of autism as currently defined by DSM-5 and its overlap of symptoms with other psychiatric disorders can make the diagnosis challenging for both child and adolescent psychiatrists and adult psychiatrists and might help explain why severe cases of ASD are more readily identified earlier than milder cases of ASD.10
Ms. P’s case is also an example of how women are more likely than men to be overlooked when evaluated for ASD. According to DSM-5, the estimated gender ratio for ASD is believed to be 4:1 (male:female).5 However, upon systematic review and meta-analysis, Loomes et al12 found that the gender ratio may be closer to 3:1 (male:female). These authors suggested that diagnostic bias and a failure of passive case ascertainment to estimate gender ratios as stated by DSM-5 in identifying ASD might explain the lower gender ratio.12 A growing body of evidence suggests that ASD is different in males and females. A 2019 qualitative study by Milner et al13 found that female participants reported using masking and camouflaging strategies to appear neurotypical. Compensatory behaviors were found to be linked to a delay in diagnosis and support for ASD.13
Cognitive ability as measured by IQ has also been found to be a factor in receiving a diagnosis of ASD. In a 2010 secondary analysis of a population-based study of the prevalence of ASD, Giarelli et al14found that girls with cognitive impairments as measured by IQ were less likely to be diagnosed with ASD than boys with cognitive impairment, despite meeting the criteria for ASD. Females tend to exhibit fewer repetitive behaviors than males, and tend to be more likely to show accompanying intellectual disability, which suggests that females with ASD may go unrecognized when they exhibit average intelligence with less impairment of behavior and subtler manifestation of social and communication deficits.15 Consequently, females tend to receive this diagnosis later than males.
Continue to: Treatment...
TREATMENT Adding CBT
At an interdisciplinary session several weeks later that includes Ms. P and her parents, the treatment team discusses the revised diagnoses of ASD and MDD, a treatment recommendation for cognitive-behavioral therapy (CBT), and continued use of medication. At this session, Ms. P discloses that she has not been consistent with her medication regimen since her last appointment, which helps explain the increase in her PHQ-9 score from 2 to 14 and GAD-7 score
[polldaddy:11027990]
The authors’ observations
CBT can be helpful in improving medication adherence, developing coping skills, and modifying maladaptive behaviors.
OUTCOME Improvement with psychotherapy
Ms. P and family agree with the team’s recommendations. The aims of Ms. P’s psychotherapy are to maintain medication compliance; implement behavioral modification, vocational rehabilitation, and community engagement; develop social skills; increase functional independence; and develop coping skills for depression and anxiety.
Bottom Line
The prevalence of schizoid personality disorder (SPD) is low, and its symptoms overlap with those of autism spectrum disorder. Therefore, before diagnosing SPD in an adult patient, it is important to obtain a detailed developmental history and include an interdisciplinary team to assess for autism spectrum disorder.
CASE Treatment-resistant MDD
Ms. P, age 21, presents to the outpatient clinic. She has diagnoses of treatment-resistant major depressive disorder (MDD) and schizoid personality disorder (SPD). Ms. P was diagnosed with MDD 3 years ago after reporting symptoms of prevailing sadness for approximately 8 years, described as feelings of worthlessness, anhedonia, social withdrawal, and decreased hygiene and self-care behaviors, as well as suicidal ideation and self-harm. SPD was diagnosed 1 year earlier based on her “odd” behaviors and disheveled appearance following observation and in collateral with her family. Her odd behaviors are described as spending most of her time alone, preferring solitary activities, and having little contact with people other than her parents.
Ms. P reports that she was previously treated with citalopram, 20 mg/d, bupropion, 150 mg/d, aripiprazole, 3.75 mg/d, topiramate, 100 mg twice daily, and melatonin, 9 mg/d at bedtime, but discontinued follow-up appointments and medications after no significant improvement in symptoms.
[polldaddy:11027942]
The authors’ observations
The term “schizoid” first made its debut in the medical community to describe the prodromal social withdrawal and isolation observed in schizophrenia.1 The use of schizoid to describe a personality type first occurred in DSM-III in 1980.2 SPD is a Cluster A personality disorder that groups personalities characterized by common traits that are “odd” or “eccentric” and may resemble the positive and/or negative symptoms of schizophrenia.3,4 Relatively uncommon in clinical settings, SPD includes individuals who do not desire or enjoy close relationships. Those afflicted with SPD will be described as isolated, aloof, and detached from social relationships with others, even immediate family members. Individuals with SPD may appear indifferent to criticism and praise, and may take pleasure in only a few activities. They may exhibit a general absence of affective range, which contributes to their characterization as flat, blunted, or emotionally vacant. SPD is more commonly diagnosed in males and may be present in childhood and adolescence. These children are typified by solitariness, poor peer relationships, and underachievement in school. SPD impacts 3.1% to 4.9% of the United States population and approximately 1% of community populations.5,6
EVALUATION Persistent depressive symptoms
Ms. P is accompanied by her parents for the examination. She reports a chronic, persistent sad mood, hopelessness, anergia, insomnia, anhedonia, and decreased concentration and appetite. She says she experiences episodes of intense worry, along with tension, restlessness, feelings of being on the edge, irritability, and difficulty relaxing. Socially, she is withdrawn, preferring to stay alone in her room most of the day watching YouTube or trying to write stories. She has 2 friends with whom she does not interact with in person, but rather through digital means. Ms. P has never enjoyed attending school and feels “nervous” when she is around people. She has difficulty expressing her thoughts and often looks to her parents for help. Her parents add that getting Ms. P to attend school was a struggle, which resulted in periods of home schooling throughout high school.
The treating team prescribes citalopram, 10 mg/d, and aripiprazole, 2 mg/d. On subsequent follow-up visits, Ms. P’s depression improves with an increase in citalopram to 40 mg/d. Psychotherapy is added to her treatment plan to help address the persistent social deficits, odd behavior, and anxieties.
Continue to: Evaluation Psychological assessment...
EVALUATION Psychological assessment
At her psychotherapy intake appointment with the clinical neuropsychologist, Ms. P is dressed in purple from head to toe and sits clutching her purse and looking at the ground. She is overweight with clean, fitting clothing. Ms. P takes a secondary role during most of the interview, allowing her parents to answer most questions. When asked why she is starting therapy, Ms. P replies, “Well, I’ve been using the bathroom a lot.” She describes a feeling of comfort and calmness while in the restroom. Suddenly, she asks her parents to exit the exam room for a moment. Once they leave, she leans in and whispers, “Have you ever heard of self-sabotage? I think that’s what I’m doing.”
Her mood is euthymic, with a blunted affect. She scores 2 on the Patient Health Questionnaire-9 (PHQ-9) and 10 on the Generalized Anxiety Disorder 7-item scale (GAD-7), which indicates the positive impact of medication on her depressive symptoms but continuing moderate anxious distress. She endorses fear of the night, insomnia, and suicidal ideation. She reports an unusual “constant itching sensation,” resulting in hours of repetitive excoriation. Physical examination reveals several significant scars and scabs covering her bilateral upper and lower extremities. Her vocational history is brief; she had held 2 entry-level customer service positions that lasted <1 year. She was fired due to excessive bathroom use.
As the interview progresses, the intake clinician’s background in neuropsychological assessment facilitates screening for possible developmental disorders. Given the nature of the referral and psychotherapy intake, a full neuropsychological assessment is not conducted. The clinician emphasizes verbal abstraction and theory of mind. Ms. P’s IQ was estimated to be average by Wide Range Achievement Test 4 word reading and interview questions about her academic history. Questions are abstracted from the Autism Diagnostic Observation Schedule, Module 4, to assess for conversation ability, emotional insight, awareness and expression, relationships, and areas of functioning in daily living. Developmental history questions, such as those found on the Adaptive Behavior Assessment System, 3rd edition, help guide developmental information provided by parents in the areas of communication, emotion and eye-gaze, gestures, sensory function, language, social functioning, hygiene behavior, and specific interests.
Ms. P’s mother describes a normal pregnancy and delivery; however, she states that Ms. P was “born with problems,” including difficulty with rooting and sucking, and required gastrointestinal intubation until age 3. Cyclical vomiting followed normal food consumption. Ambulation, language acquisition, toilet training, and hygiene behavior were delayed. Ms. P experienced improvements with early intervention in intensive physical and occupational therapy.
Ms. P’s hygiene is well below average, and she requires cueing from her parents. She attended general education until she reached high school, when she began special education. She was sensitive to sensory stimulation from infancy, with sensory sensitivity to textures. Ms. P continues to report sensory sensitivity and lapses in hygiene.
She has difficulty establishing and maintaining relationships with her peers, and prefers solitary activities. Ms. P has no history of romantic relationships, although she does desire one. When asked about her understanding of various relationships, Ms. P’s responses are stereotyped, such as “I know someone is my friend because they are nice to me” and “People get married because they love each other.” She struggles to offer greater insight into the nuances that form lasting relationships and bonds. Ms. P struggles to imitate and describe the physical and internal cues of several basic emotions (eg, fear, joy, anger).
Her conversational and social skills are assessed by asking her to engage in a conversation with the examiner as if meeting for the first time. Her speech is reciprocal, aprosodic, and delayed. The conversation is one-sided, and the examiner fills in several awkward pauses. Ms. P’s gaze at times is intense and prolonged, especially when responding to questions. She tends to use descriptive statements (eg, “I like your purple pen, I like your shirt”) to engage in conversation, rather than gathering more information through reflective statements, questions, or expressing a shared interest.
Ms. P’s verbal abstraction is screened using questions from the Wechsler Adult Intelligence Scale, 4th edition Similarities subtest, to which she provides several responses within normal limits. Her understanding of colloquial speech is assessed by asking her the meaning of common phrases (eg, “Get knocked down 9 times, get up 10,” “Jack and Jill are 2 peas in a pod”). On many occasions, she is able to limit her response to 1 word, (eg, “resiliency”), demonstrating intact ability to decipher idioms.
[polldaddy:11027971]
The authors’ observations
Upon reflection of Ms. P’s clinical presentation and history of developmental delays, social deficits, sensory sensitivity since infancy, and repetitive behaviors (all which continue to impact her), the clinical team concluded that the diagnosis of autism spectrum disorder (ASD) helps explain the patient’s “odd” behaviors, more so than SPD.
ASD is a heterogenous, complex neuropsychiatric disorder characterized by a persistent deficit in social reciprocity, verbal, and nonverbal communication, and includes a pattern of restricted, repetitive and/or stereotyped behaviors and/or interests.5 The term “autismus” is Greek meaning “self,” and was first used to classify the qualities of “morbid self-admiration” observed in prodromal schizophrenia.7
To properly distinguish these disorders, keep in mind that patients with ASD have repetitive and restricted patterns of behaviors or interests that are not found in SPD, and experience deficits in forming, maintaining, and understanding relationships since they lack those skills, while patients with SPD are more prone to desire solitary activities and limited relationships.5,9
There has been an increased interest in determining why for some patients the diagnosis of ASD is delayed until they reach adulthood. Limited or no access to the patient’s childhood caregiver to obtain a developmental history, as well as generational differences on what constitutes typical childhood behavior, could contribute to a delayed diagnosis of ASD until adulthood. Some patients develop camouflaging strategies that allow them to navigate social expectations to a limited degree, such as learning stock phrases, imitating gestures, and telling anecdotes. Another factor to consider is that co-occurring psychiatric disorders may take center stage when patients present for mental health services.10 Fusar-Poli et al11 investigated the characteristics of patients who received a diagnosis of ASD in adulthood. They found that the median time from the initial clinical evaluation to diagnosis of ASD in adulthood was 11 years. In adults identified with ASD, their cognitive abilities ranged from average to above average, and they required less support. Additionally, they also had higher rates of being previously diagnosed with psychotic disorders and personality disorders.11
It is important to keep in mind that the wide spectrum of autism as currently defined by DSM-5 and its overlap of symptoms with other psychiatric disorders can make the diagnosis challenging for both child and adolescent psychiatrists and adult psychiatrists and might help explain why severe cases of ASD are more readily identified earlier than milder cases of ASD.10
Ms. P’s case is also an example of how women are more likely than men to be overlooked when evaluated for ASD. According to DSM-5, the estimated gender ratio for ASD is believed to be 4:1 (male:female).5 However, upon systematic review and meta-analysis, Loomes et al12 found that the gender ratio may be closer to 3:1 (male:female). These authors suggested that diagnostic bias and a failure of passive case ascertainment to estimate gender ratios as stated by DSM-5 in identifying ASD might explain the lower gender ratio.12 A growing body of evidence suggests that ASD is different in males and females. A 2019 qualitative study by Milner et al13 found that female participants reported using masking and camouflaging strategies to appear neurotypical. Compensatory behaviors were found to be linked to a delay in diagnosis and support for ASD.13
Cognitive ability as measured by IQ has also been found to be a factor in receiving a diagnosis of ASD. In a 2010 secondary analysis of a population-based study of the prevalence of ASD, Giarelli et al14found that girls with cognitive impairments as measured by IQ were less likely to be diagnosed with ASD than boys with cognitive impairment, despite meeting the criteria for ASD. Females tend to exhibit fewer repetitive behaviors than males, and tend to be more likely to show accompanying intellectual disability, which suggests that females with ASD may go unrecognized when they exhibit average intelligence with less impairment of behavior and subtler manifestation of social and communication deficits.15 Consequently, females tend to receive this diagnosis later than males.
Continue to: Treatment...
TREATMENT Adding CBT
At an interdisciplinary session several weeks later that includes Ms. P and her parents, the treatment team discusses the revised diagnoses of ASD and MDD, a treatment recommendation for cognitive-behavioral therapy (CBT), and continued use of medication. At this session, Ms. P discloses that she has not been consistent with her medication regimen since her last appointment, which helps explain the increase in her PHQ-9 score from 2 to 14 and GAD-7 score
[polldaddy:11027990]
The authors’ observations
CBT can be helpful in improving medication adherence, developing coping skills, and modifying maladaptive behaviors.
OUTCOME Improvement with psychotherapy
Ms. P and family agree with the team’s recommendations. The aims of Ms. P’s psychotherapy are to maintain medication compliance; implement behavioral modification, vocational rehabilitation, and community engagement; develop social skills; increase functional independence; and develop coping skills for depression and anxiety.
Bottom Line
The prevalence of schizoid personality disorder (SPD) is low, and its symptoms overlap with those of autism spectrum disorder. Therefore, before diagnosing SPD in an adult patient, it is important to obtain a detailed developmental history and include an interdisciplinary team to assess for autism spectrum disorder.
1. Fariba K, Gupta V. Schizoid personality disorder. StatPearls Publishing. Updated June 9, 2021. Accessed January 6, 2021. https://www.ncbi.nlm.nih.gov/books/NBK559234/
2. Diagnostic and Statistical Manual of Mental Disorders: DSM-III. 3rd ed rev. American Psychiatric Association; 1987.
3. Esterberg ML, Goulding SM, Walker EF. Cluster A personality disorders: schizotypal, schizoid and paranoid personality disorders in childhood and adolescence. J Psychopathol Behav Assess. 2010;32(4):515-528. doi:10.1007/s10862-010-9183-8
4. Kalus O, Bernstein DP, Siever LJ. Schizoid personality disorder: a review of current status and implications for DSM-IV. Journal of Personality Disorders. 1993;7(1), 43-52.
5. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. American Psychiatric Association; 2013.
6. Eaton NR, Greene AL. Personality disorders: community prevalence and socio-demographic correlates. Curr Opin Psychol. 2018;21:28-32. doi:10.1016/j.copsyc.2017.09.001
7. Vatano
8. Ritsner MS. Handbook of Schizophrenia Spectrum Disorders, Volume I: Conceptual Issues and Neurobiological Advances. Springer; 2011.
9. Cook ML, Zhang Y, Constantino JN. On the continuity between autistic and schizoid personality disorder trait burden: a prospective study in adolescence. J Nerv Ment Dis. 2020;208(2):94-100. doi:10.1097/NMD.0000000000001105
10. Lai MC, Baron-Cohen S. Identifying the lost generation of adults with autism spectrum conditions. Lancet Psychiatry. 2015;2(11):1013-1027. doi:10.1016/S2215-0366(15)00277-1
11. Fusar-Poli L, Brondino N, Politi P, et al. Missed diagnoses and misdiagnoses of adults with autism spectrum disorder. Eur Arch Psychiatry Clin Neurosci. 2020;10.1007/s00406-020-01189-2. doi:10.1007/s00406-020-01189-w
12. Loomes R, Hull L, Mandy WPL. What is the male-to-female ratio in autism spectrum disorder? A systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry. 2017;56(6):466-474. doi:10.1016/j.jaac.2017.03.013
13. Milner V, McIntosh H, Colvert E, et al. A qualitative exploration of the female experience of autism spectrum disorder (ASD). J Autism Dev Disord. 2019;49(6):2389-2402. doi:10.1007/s10803-019-03906-4
14. Giarelli E, Wiggins LD, Rice CE, et al. Sex differences in the evaluation and diagnosis of autism spectrum disorders among children. Disabil Health J. 2010;3(2):107-116. doi:10.1016/j.dhjo.2009.07.001
15. Frazier TW, Georgiades S, Bishop SL, et al. Behavioral and cognitive characteristics of females and males with autism in the Simons Simplex Collection. J Am Acad Child Adolesc Psychiatry. 2014;53(3):329-40.e403. doi:10.1016/j.jaac.2013.12.004
16. Julius RJ, Novitsky MA Jr, et al. Medication adherence: a review of the literature and implications for clinical practice. J Psychiatr Pract. 2009;15(1):34-44. doi:10.1097/01.pra.0000344917.43780.77
17. Spain D, Sin J, Chalder T, et al. Cognitive behaviour therapy for adults with autism spectrum disorders and psychiatric co-morbidity: a review. Research in Autism Spectrum Disorders. 2015;9, 151-162. https://doi.org/10.1016/j.rasd.2014.10.019
18. Bishop-Fitzpatrick L, Minshew NJ, Eack SM. A systematic review of psychosocial interventions for adults with autism spectrum disorders. J Autism Dev Disord. 2013;43(3):687-694. doi:10.1007/s10803-012-1615-8
1. Fariba K, Gupta V. Schizoid personality disorder. StatPearls Publishing. Updated June 9, 2021. Accessed January 6, 2021. https://www.ncbi.nlm.nih.gov/books/NBK559234/
2. Diagnostic and Statistical Manual of Mental Disorders: DSM-III. 3rd ed rev. American Psychiatric Association; 1987.
3. Esterberg ML, Goulding SM, Walker EF. Cluster A personality disorders: schizotypal, schizoid and paranoid personality disorders in childhood and adolescence. J Psychopathol Behav Assess. 2010;32(4):515-528. doi:10.1007/s10862-010-9183-8
4. Kalus O, Bernstein DP, Siever LJ. Schizoid personality disorder: a review of current status and implications for DSM-IV. Journal of Personality Disorders. 1993;7(1), 43-52.
5. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. American Psychiatric Association; 2013.
6. Eaton NR, Greene AL. Personality disorders: community prevalence and socio-demographic correlates. Curr Opin Psychol. 2018;21:28-32. doi:10.1016/j.copsyc.2017.09.001
7. Vatano
8. Ritsner MS. Handbook of Schizophrenia Spectrum Disorders, Volume I: Conceptual Issues and Neurobiological Advances. Springer; 2011.
9. Cook ML, Zhang Y, Constantino JN. On the continuity between autistic and schizoid personality disorder trait burden: a prospective study in adolescence. J Nerv Ment Dis. 2020;208(2):94-100. doi:10.1097/NMD.0000000000001105
10. Lai MC, Baron-Cohen S. Identifying the lost generation of adults with autism spectrum conditions. Lancet Psychiatry. 2015;2(11):1013-1027. doi:10.1016/S2215-0366(15)00277-1
11. Fusar-Poli L, Brondino N, Politi P, et al. Missed diagnoses and misdiagnoses of adults with autism spectrum disorder. Eur Arch Psychiatry Clin Neurosci. 2020;10.1007/s00406-020-01189-2. doi:10.1007/s00406-020-01189-w
12. Loomes R, Hull L, Mandy WPL. What is the male-to-female ratio in autism spectrum disorder? A systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry. 2017;56(6):466-474. doi:10.1016/j.jaac.2017.03.013
13. Milner V, McIntosh H, Colvert E, et al. A qualitative exploration of the female experience of autism spectrum disorder (ASD). J Autism Dev Disord. 2019;49(6):2389-2402. doi:10.1007/s10803-019-03906-4
14. Giarelli E, Wiggins LD, Rice CE, et al. Sex differences in the evaluation and diagnosis of autism spectrum disorders among children. Disabil Health J. 2010;3(2):107-116. doi:10.1016/j.dhjo.2009.07.001
15. Frazier TW, Georgiades S, Bishop SL, et al. Behavioral and cognitive characteristics of females and males with autism in the Simons Simplex Collection. J Am Acad Child Adolesc Psychiatry. 2014;53(3):329-40.e403. doi:10.1016/j.jaac.2013.12.004
16. Julius RJ, Novitsky MA Jr, et al. Medication adherence: a review of the literature and implications for clinical practice. J Psychiatr Pract. 2009;15(1):34-44. doi:10.1097/01.pra.0000344917.43780.77
17. Spain D, Sin J, Chalder T, et al. Cognitive behaviour therapy for adults with autism spectrum disorders and psychiatric co-morbidity: a review. Research in Autism Spectrum Disorders. 2015;9, 151-162. https://doi.org/10.1016/j.rasd.2014.10.019
18. Bishop-Fitzpatrick L, Minshew NJ, Eack SM. A systematic review of psychosocial interventions for adults with autism spectrum disorders. J Autism Dev Disord. 2013;43(3):687-694. doi:10.1007/s10803-012-1615-8