User login
Evaluating Patient Barriers to Tobacco Cessation Treatment
Tobacco use continues to be the single most preventable cause of death and disease in the U.S., contributing to 480,000 deaths per year, 42,000 of these associated with second-hand tobacco exposure.1 Tobacco use costs Americans over $289 billion in lost productivity and health care costs every year.1
Within the VA, where prevalence exceeds that in the general population, tobacco use among patients is as follows: 19.7% of new enrollees (compared with 19.4% of the general population), 72% of those with a psychiatric disorder, 23% of Operation Enduring Freedom/Operation Iraqi Freedom veterans, and up to 98% of substance use disorder patients in treatment.2-4 In one report, veterans with posttraumatic stress disorder (PTSD) smoked at rates 2 to 3 times that of the general veteran population.5 In 2008, the VA spent over $5.2 billion on treatment of chronic obstructive pulmonary disease alone, a disease highly correlated with smoking tobacco.6 Within the VA, it is clear that tobacco abuse is a costly issue in both health matters as well as dollars spent.
To combat this preventable loss of human life, health, and financial capital, the VA offers high-quality, evidence-based tobacco cessation counseling programs with medical adjunct therapy. In 2010, the Center for Integrated Healthcare developed a training manual to assist tobacco cessation providers in conducting integrated smoking cessation treatment across the VA.7 The Atlanta VA Medical Center (VAMC) in Georgia has had an active and highly successful tobacco cessation treatment program for many years, and in 2004, participants who completed the 5-session treatment program self-reported an abstinence rate of 69.5%, reflecting both quit (28.9%) and smoking less (40.6%) rates for the sample.8
Since that time, tobacco cessation policy within VA has transitioned to offer pharmacotherapy upon veteran request and has eliminated copays for outpatient tobacco cessation visits. In addition, the electronic medical record used within the VA Health Care System includes clinical reminders for providers to assess tobacco use and offer treatment options at several visits per year. Despite these many improvements and enhancements for tobacco cessation care, reduced attendance, including last minute cancellations and “no-shows” for tobacco cessation appointments, remain an ongoing challenge at the Atlanta VAMC.
The purpose of this investigation was to examine through a telephone survey the reasons why identified veterans had not taken advantage of smoking cessation opportunities at the Atlanta VAMC. Specifically, the study evaluated the referral completion rate for veterans referred to the program, analyzed the potential barriers behind these utilization rates, and explored possible opportunities for overcoming them.
Study Design
The VA computerized patient record system (CPRS) provides a reliable means of identifying patients who use tobacco and is replete with clinical reminders for a variety of preventive health issues, including tobacco use cessation counseling. Tobacco use screening is considered a vital sign, and this information is solicited through automatic prompts for every visit. Patients who express an interest in receiving help for tobacco cessation are referred to in-house tobacco cessation counseling services, which consist of weekly, 1-hour sessions of psycho-educational counseling and medical adjunct therapy.
Methods
This project was conducted at the Atlanta VAMC, which was recognized in 2010 by The Joint Commission as a Top Performer on Key Quality Measures. The proposed plan was presented to the Research & Development (R&D) office (an International Review Board equivalent). After careful review and consideration, it was determined to be a quality improvement initiative and did not require full R&D approval.
The CPRS was used to generate a tally of all veterans referred to the tobacco cessation treatment program from January 2008 through November 2011. A total of 3,489 consults were referred by primary care and mental health providers, of which 2,358 patients (67.6%) cancelled or did not attend the program. Names and contact information for patients who did not attend the program for the more recent period of April 1, 2011, to September 8th, 2011 (n = 229) were then selected to participate in this survey study. For the purposes of this analysis, patients were considered a “non-attend” regardless of whether they called to cancel the appointment or simply did not show up for it.
For the survey portion of this study, each of these 229 individuals were contacted by telephone to inquire about potential barriers to participation, using a close-ended survey tool. The following 4 questions were asked: (1) Are you currently using tobacco in any form?; (2) Did you recently (in the past year) receive a referral for tobacco cessation counseling or classes?; (3) Did you attend the tobacco cessation program?; and (4) If you did not attend, what was/were the reason(s)?
These participants were called over several days between October 24, 2011, and November 28, 2011. The limits of confidentiality were explained to each veteran before they were asked to participate in this initiative as an effort to improve the Atlanta VAMC’s tobacco cessation program.
Of the 229 possible participants, only 115 were accessible by phone over the survey period. One declined to participate, leaving 114 potential respondents. Of the 114, 13 reported that they either did not receive a referral for tobacco cessation over the past year or did not recall receiving such a referral. These 13 were removed from the respondent pool, leaving 101. Of these individuals, 5 reported that they did attend the tobacco cessation counseling sessions. These individuals were also removed from the respondent pool, leaving a total of 96 respondents to answer the remaining multipart question regarding barriers to attendance.
Measures and Analysis
Simple descriptive statistics were used to characterize the data from the survey portion of this study, determining frequencies of responses to different barriers. Since respondents were allowed to select as many barriers as applied to their situation, totals did not add to 100%. In addition, a separate variable, consisting of positive responses to barriers that represent accessibility (eg, distance, time, transportation, parking, gas), was used to develop a composite accessibility score to further analyze the comprehensive impact of access.
Results
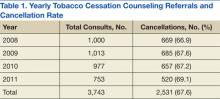
The rate of cancellations remained fairly stable between January 2008 and November 2011 (67%) (Table 1). The sample was representative of the male-dominated population at the VA with 84% of the respondents being male, aged 22 to 75 years. Of the 96 respondents who did not attend the cessation counseling, 85 reported they were still using tobacco products; 11 reported having quit. Of the 85 respondents who were still using tobacco products, the majority (97%) were smoking cigarettes, while 1% each reported using smokeless tobacco products such as chew, snuff, or a combination of these (Table 2).
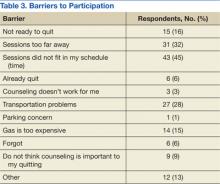
Of the 96 respondents who did not complete their tobacco cessation counseling referral, 45% reported that time or scheduling was a barrier to participation (Table 3). Thirty-two percent reported that distance to the counseling sessions was a barrier, and 28% reported transportation issues as a barrier. Also contributing to transportation issues, the cost of gasoline was given as a reason for not attending by 15% of the respondents. Sixteen percent reported that they were not yet ready to quit in spite of accepting a referral for cessation counseling. Smaller percentages reported that they had already quit (6%), believed that counseling did not work for them (3%), expressed that parking was a concern (1%), forgot (6%), or did not think that counseling was important to their quitting efforts (9%). Other reasons provided for nonattendance included concern that quitting is difficult, other medical and mental health priorities, discomfort in groups, and family illness.
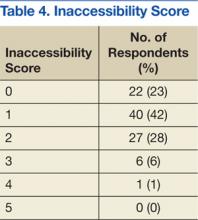
A final analysis was conducted, where an inaccessibility score was determined for each respondent based on barriers related to inaccessibility. A single point was given for each of the following answers reported as a barrier by the respondent: (1) too far away; (2) schedule/time; (3) transportation; (4) parking; or (5) gas. Twenty-three percent of the 96 respondents had no accessibility issues, reported as an inaccessibility score of 0. Most respondents had 1 inaccessibility issue (40%); while 28% reported 2, 6% reported 3, and only 1 individual reported having ≥ 4. Of note, a majority (77%) of the respondents reported 1 or more inaccessibility issues as a barrier to their attendance (Table 4).
Discussion
Studies abound regarding barriers to provider-offered smoking cessation counseling.9,10 Even oncologists report low levels of confidence in their ability to counsel patients to quit using tobacco.11 Physicians report lack of time, training, and patient willingness as barriers that prevent them from providing counseling on critical lifestyle issues. Few studies, however, have examined patient-reported barriers to tobacco counseling services. It bears examination, though, when 67% of the patients who accept a referral for tobacco cessation counseling, with no copay, fail to utilize the opportunity.
The results of this study suggest that accessibility issues played a major role in preventing participation, indicating that 77% of the respondents reported at least 1 accessibility issue (transportation, time, or cost) as a contributing factor that kept them from their appointment. The most common accessibility issues reported by this sample were timing and scheduling (45%), distance to the counseling sessions (32%), and transportation issues (28%). The VA is actively addressing these barriers through telehealth and computer-assisted options. In addition, a new telephone mobile application based on the integrated care model for smoking cessation is now available and provides tobacco quit tips for veterans with PTSD who smoke.12
Another noteworthy finding was that 16% reported they were not ready to quit in spite of accepting a referral for counseling. In addition, 13% offered “other” reasons as barriers to tobacco cessation, suggesting that these 2 groups may not have been properly assessed as to their “readiness-to-change” status at the time the referral was generated. Another possibility is the “demand characteristics” of the referral: For example, patients did not want to disappoint their provider, although they were not fully committed to treatment at the time of their visit.
Six percent of the respondents reported they did not attend the treatment program because they had already quit tobacco between the time of the original referral and the time of the survey. This time frame could have been from 6 weeks to 7 months for the respondents. However, these responses were not verified with biomarker testing but, rather, relied on self-reported status. For this reason, these responses could be suspect and may be the result of “demand characteristics” as well.
Another category of respondents of particular interest is the 9% who reported “counseling is not important to my quitting.” This group represents a segment of respondents who failed to appreciate the evidence that demonstrates the benefits of counseling and medical adjunct therapy. Further patient education is clearly needed to ensure patients understand how important smoking cessation is to their health and how important counseling is to their quitting efforts. To accomplish this goal, patient education concerning tobacco cessation in the form of televideo programming placed in the clinic wait areas is underway at the Atlanta VAMC.
Less frequently reported as barriers were “forgot” (6%), “counseling doesn’t work for me” (3%), and “parking concerns” (1%), suggesting that in this limited sample, these were not central reasons for not utilizing these services.
Limitations
The small sample size and that it was a convenience sample pose some concerns as to whether the results are truly representative of the population under study and whether the results can be extrapolated to similar populations. In addition, the results are from self-reported replies, relying on the integrity of the respondents to provide honest answers. Prefacing the study questions with an explanation that this was an opportunity to help the VA improve the quality of its programs was intended to ward off the desire to provide “acceptable” answers.
It is important to understand that patients within the VA system in certain categories of disability and financial means are reimbursed travel expenses for attending tobacco cessation treatment. It is possible that reimbursement factors might motivate patients to accept referrals for counseling that they may not be particularly committed to attend, contributing to a higher-than-expected number of referrals for patients who were not ready to quit.
Conclusion
The results of this study highlight several patient-reported barriers to tobacco cessation treatment, including scheduling conflicts, distance, and cost of travel. Only a small percentage (16%) actually reported they were not yet ready to quit or they did not feel counseling would work for them (3%). A slightly larger percentage reported they did not feel counseling is important (9%), and since it is well established that combining medication with behavioral counseling yields the greatest results for smoking cessation, it is clear that this segment of the patient population will require more education and attention.13
Accessibility issues were the biggest reason for nonattendance to the program (77%), and these issues highlight the need for continued work, at least at the Atlanta VAMC, on providing easier patient access to tobacco cessation treatment. Since the completion of this study, many updates have been implemented at the Atlanta VAMC to improve access, including the provision of telehealth education and the use of telephone quit lines.
Telehealth education, a technique that is highly compatible with lifestyle change counseling, has been shown to be cost-effective while providing intervention and education for patients who are too distant or unable to travel for other reasons.14
Tobacco quit lines are another option for patients with accessibility conflicts and are now operational in all 50 states. Most operate 24/7, manned by counselors trained in motivational interviewing and specifically tobacco cessation counseling. A meta-analysis of quit-line efficacy performed by Stead and colleagues demonstrated that quit lines improve long-term cessation for smokers who use them and even suggested a possible dose-response effect.15 Quit-line counseling, therefore, seems to offer a useful option for veterans who cannot easily access that counseling within the VA.
Motivational interviewing principles have also been proposed by VA as a new approach with great promise for application with veterans who are unmotivated, resistant, or ambivalent about changing unhealthy habits.16 At the Atlanta VAMC, training in motivational interviewing for primary care clinicians is ongoing. It is the provider’s responsibility to strongly encourage patients who use tobacco to utilize alternative tobacco cessation resources when attending a VA treatment program is not a viable option.
This study was a first step in examining barriers to treatment. Although the sample size was small, it is representative and useful in providing a framework from which to improve access to tobacco cessation programs as well as encourage utilization of alternative resources.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. U.S. Department of Health and Human Services. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014.
2. 2011 Survey of Veteran Enrollees’ Health and Reliance Upon VA, With Selected Comparison to the 1999-2010 Surveys. Washington, DC: Department of Veterans Affairs, Veterans Health Administration, Office of the Assistant Deputy Under Secretary for Health For Policy and Planning, Healthcare Analysis and Information Group, Enrollment and Forecasting Services; 2012.
3. Landolt K, Ajdacic-Gross V, Angst J, et al. Smoking and psychiatric disorders: Have subthreshold disorders been overlooked? Nicotine Tob Res. 2010;12(5):516-520.
4. Baca CT, Yahne CE. Smoking cessation during substance abuse treatment: What you need to know. J Subst Abuse Treat. 2009;36(2):205-219.
5. Smoking and Tobacco Use Cessation Report. Washington, DC: Department of Veterans Affairs, Veterans Health Administration, Office of the Assistant Deputy Secretary for Health for Policy and Planning; 2010.
6. Committee on Smoking Cessation in Military and Veteran Populations, Board on Population Health and Public Health Practice, Institute of Medicine. Combating Tobacco Use in the Military and Veteran Populations. Washington, DC: The National Academies Press; 2009.
7. Dollar K, Dundon M, Kusche A. Tobacco Use Cessation: A Brief Primary Care Intervention, A Training Manual for Integrated Primary Care Behavioral Health Providers and Other Tobacco Cessation Providers. Washington, DC: Department of Veterans Affairs, Center for Integrated Healthcare; 2010.
8. Burchfield BE, Keller T, Avritt L, Wright M, Ackerman MD. A multi-disciplinary approach to smoking cessation within the Department of Veterans Affairs. Paper presented at: 2004 Georgia Psychological Association Annual Meeting; May 2004; Hilton Head, SC.
9. Raupach T, Merker J, Hasenfuss G, Andreas S, Pipe A. Knowledge gaps about smoking cessation in hospitalized patients and their doctors. Eur J Cardiovasc Prev Rehabil. 2011;18(2):334-341.
10. Huy C, Diehm C, Schneider S. Cardiovascular prevention at the general practitioner? First results of a study on attitudes, services, success and barriers in practice [in German]. Dtsch Med Wochenschr. 2012;137(1-2):17-22.
11. Weaver KE, Danhauer SC, Tooze JA, et al. Smoking cessation counseling beliefs and behaviors of outpatient oncology providers. Oncologist. 2012;17(3):455-462.
12. McFall M, Saxon AJ, Malte CA, et al; CSP 519 Study Team. Integrating tobacco cessation into mental health care for posttraumatic stress disorder: A randomized controlled trial. JAMA. 2010;304(22):2485-2493.
13. Fiore MC, Jaén CR, Baker TB, et al. Treating Tobacco Use and Dependence: 2008 Update. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service; 2008.
14. Saab PG, McCalla JR, Coons HL, et al. Technological and medical advances: Implications for health psychology. Health Psychol. 2004;23(2):142-146.
15. Stead LF, Perera R, Lancaster T. A systematic review of interventions for smokers who contact quitlines. Tob Control. 2007;16(suppl 1):i3-i8.
16. Rollnick S, Miller WR, Butler CC. Motivational Interviewing in Health Care: Helping Patients Change Behavior. New York, NY: The Guilford Press; 2008.
Tobacco use continues to be the single most preventable cause of death and disease in the U.S., contributing to 480,000 deaths per year, 42,000 of these associated with second-hand tobacco exposure.1 Tobacco use costs Americans over $289 billion in lost productivity and health care costs every year.1
Within the VA, where prevalence exceeds that in the general population, tobacco use among patients is as follows: 19.7% of new enrollees (compared with 19.4% of the general population), 72% of those with a psychiatric disorder, 23% of Operation Enduring Freedom/Operation Iraqi Freedom veterans, and up to 98% of substance use disorder patients in treatment.2-4 In one report, veterans with posttraumatic stress disorder (PTSD) smoked at rates 2 to 3 times that of the general veteran population.5 In 2008, the VA spent over $5.2 billion on treatment of chronic obstructive pulmonary disease alone, a disease highly correlated with smoking tobacco.6 Within the VA, it is clear that tobacco abuse is a costly issue in both health matters as well as dollars spent.
To combat this preventable loss of human life, health, and financial capital, the VA offers high-quality, evidence-based tobacco cessation counseling programs with medical adjunct therapy. In 2010, the Center for Integrated Healthcare developed a training manual to assist tobacco cessation providers in conducting integrated smoking cessation treatment across the VA.7 The Atlanta VA Medical Center (VAMC) in Georgia has had an active and highly successful tobacco cessation treatment program for many years, and in 2004, participants who completed the 5-session treatment program self-reported an abstinence rate of 69.5%, reflecting both quit (28.9%) and smoking less (40.6%) rates for the sample.8
Since that time, tobacco cessation policy within VA has transitioned to offer pharmacotherapy upon veteran request and has eliminated copays for outpatient tobacco cessation visits. In addition, the electronic medical record used within the VA Health Care System includes clinical reminders for providers to assess tobacco use and offer treatment options at several visits per year. Despite these many improvements and enhancements for tobacco cessation care, reduced attendance, including last minute cancellations and “no-shows” for tobacco cessation appointments, remain an ongoing challenge at the Atlanta VAMC.
The purpose of this investigation was to examine through a telephone survey the reasons why identified veterans had not taken advantage of smoking cessation opportunities at the Atlanta VAMC. Specifically, the study evaluated the referral completion rate for veterans referred to the program, analyzed the potential barriers behind these utilization rates, and explored possible opportunities for overcoming them.
Study Design
The VA computerized patient record system (CPRS) provides a reliable means of identifying patients who use tobacco and is replete with clinical reminders for a variety of preventive health issues, including tobacco use cessation counseling. Tobacco use screening is considered a vital sign, and this information is solicited through automatic prompts for every visit. Patients who express an interest in receiving help for tobacco cessation are referred to in-house tobacco cessation counseling services, which consist of weekly, 1-hour sessions of psycho-educational counseling and medical adjunct therapy.
Methods
This project was conducted at the Atlanta VAMC, which was recognized in 2010 by The Joint Commission as a Top Performer on Key Quality Measures. The proposed plan was presented to the Research & Development (R&D) office (an International Review Board equivalent). After careful review and consideration, it was determined to be a quality improvement initiative and did not require full R&D approval.
The CPRS was used to generate a tally of all veterans referred to the tobacco cessation treatment program from January 2008 through November 2011. A total of 3,489 consults were referred by primary care and mental health providers, of which 2,358 patients (67.6%) cancelled or did not attend the program. Names and contact information for patients who did not attend the program for the more recent period of April 1, 2011, to September 8th, 2011 (n = 229) were then selected to participate in this survey study. For the purposes of this analysis, patients were considered a “non-attend” regardless of whether they called to cancel the appointment or simply did not show up for it.
For the survey portion of this study, each of these 229 individuals were contacted by telephone to inquire about potential barriers to participation, using a close-ended survey tool. The following 4 questions were asked: (1) Are you currently using tobacco in any form?; (2) Did you recently (in the past year) receive a referral for tobacco cessation counseling or classes?; (3) Did you attend the tobacco cessation program?; and (4) If you did not attend, what was/were the reason(s)?
These participants were called over several days between October 24, 2011, and November 28, 2011. The limits of confidentiality were explained to each veteran before they were asked to participate in this initiative as an effort to improve the Atlanta VAMC’s tobacco cessation program.
Of the 229 possible participants, only 115 were accessible by phone over the survey period. One declined to participate, leaving 114 potential respondents. Of the 114, 13 reported that they either did not receive a referral for tobacco cessation over the past year or did not recall receiving such a referral. These 13 were removed from the respondent pool, leaving 101. Of these individuals, 5 reported that they did attend the tobacco cessation counseling sessions. These individuals were also removed from the respondent pool, leaving a total of 96 respondents to answer the remaining multipart question regarding barriers to attendance.
Measures and Analysis
Simple descriptive statistics were used to characterize the data from the survey portion of this study, determining frequencies of responses to different barriers. Since respondents were allowed to select as many barriers as applied to their situation, totals did not add to 100%. In addition, a separate variable, consisting of positive responses to barriers that represent accessibility (eg, distance, time, transportation, parking, gas), was used to develop a composite accessibility score to further analyze the comprehensive impact of access.
Results
The rate of cancellations remained fairly stable between January 2008 and November 2011 (67%) (Table 1). The sample was representative of the male-dominated population at the VA with 84% of the respondents being male, aged 22 to 75 years. Of the 96 respondents who did not attend the cessation counseling, 85 reported they were still using tobacco products; 11 reported having quit. Of the 85 respondents who were still using tobacco products, the majority (97%) were smoking cigarettes, while 1% each reported using smokeless tobacco products such as chew, snuff, or a combination of these (Table 2).
Of the 96 respondents who did not complete their tobacco cessation counseling referral, 45% reported that time or scheduling was a barrier to participation (Table 3). Thirty-two percent reported that distance to the counseling sessions was a barrier, and 28% reported transportation issues as a barrier. Also contributing to transportation issues, the cost of gasoline was given as a reason for not attending by 15% of the respondents. Sixteen percent reported that they were not yet ready to quit in spite of accepting a referral for cessation counseling. Smaller percentages reported that they had already quit (6%), believed that counseling did not work for them (3%), expressed that parking was a concern (1%), forgot (6%), or did not think that counseling was important to their quitting efforts (9%). Other reasons provided for nonattendance included concern that quitting is difficult, other medical and mental health priorities, discomfort in groups, and family illness.
A final analysis was conducted, where an inaccessibility score was determined for each respondent based on barriers related to inaccessibility. A single point was given for each of the following answers reported as a barrier by the respondent: (1) too far away; (2) schedule/time; (3) transportation; (4) parking; or (5) gas. Twenty-three percent of the 96 respondents had no accessibility issues, reported as an inaccessibility score of 0. Most respondents had 1 inaccessibility issue (40%); while 28% reported 2, 6% reported 3, and only 1 individual reported having ≥ 4. Of note, a majority (77%) of the respondents reported 1 or more inaccessibility issues as a barrier to their attendance (Table 4).
Discussion
Studies abound regarding barriers to provider-offered smoking cessation counseling.9,10 Even oncologists report low levels of confidence in their ability to counsel patients to quit using tobacco.11 Physicians report lack of time, training, and patient willingness as barriers that prevent them from providing counseling on critical lifestyle issues. Few studies, however, have examined patient-reported barriers to tobacco counseling services. It bears examination, though, when 67% of the patients who accept a referral for tobacco cessation counseling, with no copay, fail to utilize the opportunity.
The results of this study suggest that accessibility issues played a major role in preventing participation, indicating that 77% of the respondents reported at least 1 accessibility issue (transportation, time, or cost) as a contributing factor that kept them from their appointment. The most common accessibility issues reported by this sample were timing and scheduling (45%), distance to the counseling sessions (32%), and transportation issues (28%). The VA is actively addressing these barriers through telehealth and computer-assisted options. In addition, a new telephone mobile application based on the integrated care model for smoking cessation is now available and provides tobacco quit tips for veterans with PTSD who smoke.12
Another noteworthy finding was that 16% reported they were not ready to quit in spite of accepting a referral for counseling. In addition, 13% offered “other” reasons as barriers to tobacco cessation, suggesting that these 2 groups may not have been properly assessed as to their “readiness-to-change” status at the time the referral was generated. Another possibility is the “demand characteristics” of the referral: For example, patients did not want to disappoint their provider, although they were not fully committed to treatment at the time of their visit.
Six percent of the respondents reported they did not attend the treatment program because they had already quit tobacco between the time of the original referral and the time of the survey. This time frame could have been from 6 weeks to 7 months for the respondents. However, these responses were not verified with biomarker testing but, rather, relied on self-reported status. For this reason, these responses could be suspect and may be the result of “demand characteristics” as well.
Another category of respondents of particular interest is the 9% who reported “counseling is not important to my quitting.” This group represents a segment of respondents who failed to appreciate the evidence that demonstrates the benefits of counseling and medical adjunct therapy. Further patient education is clearly needed to ensure patients understand how important smoking cessation is to their health and how important counseling is to their quitting efforts. To accomplish this goal, patient education concerning tobacco cessation in the form of televideo programming placed in the clinic wait areas is underway at the Atlanta VAMC.
Less frequently reported as barriers were “forgot” (6%), “counseling doesn’t work for me” (3%), and “parking concerns” (1%), suggesting that in this limited sample, these were not central reasons for not utilizing these services.
Limitations
The small sample size and that it was a convenience sample pose some concerns as to whether the results are truly representative of the population under study and whether the results can be extrapolated to similar populations. In addition, the results are from self-reported replies, relying on the integrity of the respondents to provide honest answers. Prefacing the study questions with an explanation that this was an opportunity to help the VA improve the quality of its programs was intended to ward off the desire to provide “acceptable” answers.
It is important to understand that patients within the VA system in certain categories of disability and financial means are reimbursed travel expenses for attending tobacco cessation treatment. It is possible that reimbursement factors might motivate patients to accept referrals for counseling that they may not be particularly committed to attend, contributing to a higher-than-expected number of referrals for patients who were not ready to quit.
Conclusion
The results of this study highlight several patient-reported barriers to tobacco cessation treatment, including scheduling conflicts, distance, and cost of travel. Only a small percentage (16%) actually reported they were not yet ready to quit or they did not feel counseling would work for them (3%). A slightly larger percentage reported they did not feel counseling is important (9%), and since it is well established that combining medication with behavioral counseling yields the greatest results for smoking cessation, it is clear that this segment of the patient population will require more education and attention.13
Accessibility issues were the biggest reason for nonattendance to the program (77%), and these issues highlight the need for continued work, at least at the Atlanta VAMC, on providing easier patient access to tobacco cessation treatment. Since the completion of this study, many updates have been implemented at the Atlanta VAMC to improve access, including the provision of telehealth education and the use of telephone quit lines.
Telehealth education, a technique that is highly compatible with lifestyle change counseling, has been shown to be cost-effective while providing intervention and education for patients who are too distant or unable to travel for other reasons.14
Tobacco quit lines are another option for patients with accessibility conflicts and are now operational in all 50 states. Most operate 24/7, manned by counselors trained in motivational interviewing and specifically tobacco cessation counseling. A meta-analysis of quit-line efficacy performed by Stead and colleagues demonstrated that quit lines improve long-term cessation for smokers who use them and even suggested a possible dose-response effect.15 Quit-line counseling, therefore, seems to offer a useful option for veterans who cannot easily access that counseling within the VA.
Motivational interviewing principles have also been proposed by VA as a new approach with great promise for application with veterans who are unmotivated, resistant, or ambivalent about changing unhealthy habits.16 At the Atlanta VAMC, training in motivational interviewing for primary care clinicians is ongoing. It is the provider’s responsibility to strongly encourage patients who use tobacco to utilize alternative tobacco cessation resources when attending a VA treatment program is not a viable option.
This study was a first step in examining barriers to treatment. Although the sample size was small, it is representative and useful in providing a framework from which to improve access to tobacco cessation programs as well as encourage utilization of alternative resources.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
Tobacco use continues to be the single most preventable cause of death and disease in the U.S., contributing to 480,000 deaths per year, 42,000 of these associated with second-hand tobacco exposure.1 Tobacco use costs Americans over $289 billion in lost productivity and health care costs every year.1
Within the VA, where prevalence exceeds that in the general population, tobacco use among patients is as follows: 19.7% of new enrollees (compared with 19.4% of the general population), 72% of those with a psychiatric disorder, 23% of Operation Enduring Freedom/Operation Iraqi Freedom veterans, and up to 98% of substance use disorder patients in treatment.2-4 In one report, veterans with posttraumatic stress disorder (PTSD) smoked at rates 2 to 3 times that of the general veteran population.5 In 2008, the VA spent over $5.2 billion on treatment of chronic obstructive pulmonary disease alone, a disease highly correlated with smoking tobacco.6 Within the VA, it is clear that tobacco abuse is a costly issue in both health matters as well as dollars spent.
To combat this preventable loss of human life, health, and financial capital, the VA offers high-quality, evidence-based tobacco cessation counseling programs with medical adjunct therapy. In 2010, the Center for Integrated Healthcare developed a training manual to assist tobacco cessation providers in conducting integrated smoking cessation treatment across the VA.7 The Atlanta VA Medical Center (VAMC) in Georgia has had an active and highly successful tobacco cessation treatment program for many years, and in 2004, participants who completed the 5-session treatment program self-reported an abstinence rate of 69.5%, reflecting both quit (28.9%) and smoking less (40.6%) rates for the sample.8
Since that time, tobacco cessation policy within VA has transitioned to offer pharmacotherapy upon veteran request and has eliminated copays for outpatient tobacco cessation visits. In addition, the electronic medical record used within the VA Health Care System includes clinical reminders for providers to assess tobacco use and offer treatment options at several visits per year. Despite these many improvements and enhancements for tobacco cessation care, reduced attendance, including last minute cancellations and “no-shows” for tobacco cessation appointments, remain an ongoing challenge at the Atlanta VAMC.
The purpose of this investigation was to examine through a telephone survey the reasons why identified veterans had not taken advantage of smoking cessation opportunities at the Atlanta VAMC. Specifically, the study evaluated the referral completion rate for veterans referred to the program, analyzed the potential barriers behind these utilization rates, and explored possible opportunities for overcoming them.
Study Design
The VA computerized patient record system (CPRS) provides a reliable means of identifying patients who use tobacco and is replete with clinical reminders for a variety of preventive health issues, including tobacco use cessation counseling. Tobacco use screening is considered a vital sign, and this information is solicited through automatic prompts for every visit. Patients who express an interest in receiving help for tobacco cessation are referred to in-house tobacco cessation counseling services, which consist of weekly, 1-hour sessions of psycho-educational counseling and medical adjunct therapy.
Methods
This project was conducted at the Atlanta VAMC, which was recognized in 2010 by The Joint Commission as a Top Performer on Key Quality Measures. The proposed plan was presented to the Research & Development (R&D) office (an International Review Board equivalent). After careful review and consideration, it was determined to be a quality improvement initiative and did not require full R&D approval.
The CPRS was used to generate a tally of all veterans referred to the tobacco cessation treatment program from January 2008 through November 2011. A total of 3,489 consults were referred by primary care and mental health providers, of which 2,358 patients (67.6%) cancelled or did not attend the program. Names and contact information for patients who did not attend the program for the more recent period of April 1, 2011, to September 8th, 2011 (n = 229) were then selected to participate in this survey study. For the purposes of this analysis, patients were considered a “non-attend” regardless of whether they called to cancel the appointment or simply did not show up for it.
For the survey portion of this study, each of these 229 individuals were contacted by telephone to inquire about potential barriers to participation, using a close-ended survey tool. The following 4 questions were asked: (1) Are you currently using tobacco in any form?; (2) Did you recently (in the past year) receive a referral for tobacco cessation counseling or classes?; (3) Did you attend the tobacco cessation program?; and (4) If you did not attend, what was/were the reason(s)?
These participants were called over several days between October 24, 2011, and November 28, 2011. The limits of confidentiality were explained to each veteran before they were asked to participate in this initiative as an effort to improve the Atlanta VAMC’s tobacco cessation program.
Of the 229 possible participants, only 115 were accessible by phone over the survey period. One declined to participate, leaving 114 potential respondents. Of the 114, 13 reported that they either did not receive a referral for tobacco cessation over the past year or did not recall receiving such a referral. These 13 were removed from the respondent pool, leaving 101. Of these individuals, 5 reported that they did attend the tobacco cessation counseling sessions. These individuals were also removed from the respondent pool, leaving a total of 96 respondents to answer the remaining multipart question regarding barriers to attendance.
Measures and Analysis
Simple descriptive statistics were used to characterize the data from the survey portion of this study, determining frequencies of responses to different barriers. Since respondents were allowed to select as many barriers as applied to their situation, totals did not add to 100%. In addition, a separate variable, consisting of positive responses to barriers that represent accessibility (eg, distance, time, transportation, parking, gas), was used to develop a composite accessibility score to further analyze the comprehensive impact of access.
Results
The rate of cancellations remained fairly stable between January 2008 and November 2011 (67%) (Table 1). The sample was representative of the male-dominated population at the VA with 84% of the respondents being male, aged 22 to 75 years. Of the 96 respondents who did not attend the cessation counseling, 85 reported they were still using tobacco products; 11 reported having quit. Of the 85 respondents who were still using tobacco products, the majority (97%) were smoking cigarettes, while 1% each reported using smokeless tobacco products such as chew, snuff, or a combination of these (Table 2).
Of the 96 respondents who did not complete their tobacco cessation counseling referral, 45% reported that time or scheduling was a barrier to participation (Table 3). Thirty-two percent reported that distance to the counseling sessions was a barrier, and 28% reported transportation issues as a barrier. Also contributing to transportation issues, the cost of gasoline was given as a reason for not attending by 15% of the respondents. Sixteen percent reported that they were not yet ready to quit in spite of accepting a referral for cessation counseling. Smaller percentages reported that they had already quit (6%), believed that counseling did not work for them (3%), expressed that parking was a concern (1%), forgot (6%), or did not think that counseling was important to their quitting efforts (9%). Other reasons provided for nonattendance included concern that quitting is difficult, other medical and mental health priorities, discomfort in groups, and family illness.
A final analysis was conducted, where an inaccessibility score was determined for each respondent based on barriers related to inaccessibility. A single point was given for each of the following answers reported as a barrier by the respondent: (1) too far away; (2) schedule/time; (3) transportation; (4) parking; or (5) gas. Twenty-three percent of the 96 respondents had no accessibility issues, reported as an inaccessibility score of 0. Most respondents had 1 inaccessibility issue (40%); while 28% reported 2, 6% reported 3, and only 1 individual reported having ≥ 4. Of note, a majority (77%) of the respondents reported 1 or more inaccessibility issues as a barrier to their attendance (Table 4).
Discussion
Studies abound regarding barriers to provider-offered smoking cessation counseling.9,10 Even oncologists report low levels of confidence in their ability to counsel patients to quit using tobacco.11 Physicians report lack of time, training, and patient willingness as barriers that prevent them from providing counseling on critical lifestyle issues. Few studies, however, have examined patient-reported barriers to tobacco counseling services. It bears examination, though, when 67% of the patients who accept a referral for tobacco cessation counseling, with no copay, fail to utilize the opportunity.
The results of this study suggest that accessibility issues played a major role in preventing participation, indicating that 77% of the respondents reported at least 1 accessibility issue (transportation, time, or cost) as a contributing factor that kept them from their appointment. The most common accessibility issues reported by this sample were timing and scheduling (45%), distance to the counseling sessions (32%), and transportation issues (28%). The VA is actively addressing these barriers through telehealth and computer-assisted options. In addition, a new telephone mobile application based on the integrated care model for smoking cessation is now available and provides tobacco quit tips for veterans with PTSD who smoke.12
Another noteworthy finding was that 16% reported they were not ready to quit in spite of accepting a referral for counseling. In addition, 13% offered “other” reasons as barriers to tobacco cessation, suggesting that these 2 groups may not have been properly assessed as to their “readiness-to-change” status at the time the referral was generated. Another possibility is the “demand characteristics” of the referral: For example, patients did not want to disappoint their provider, although they were not fully committed to treatment at the time of their visit.
Six percent of the respondents reported they did not attend the treatment program because they had already quit tobacco between the time of the original referral and the time of the survey. This time frame could have been from 6 weeks to 7 months for the respondents. However, these responses were not verified with biomarker testing but, rather, relied on self-reported status. For this reason, these responses could be suspect and may be the result of “demand characteristics” as well.
Another category of respondents of particular interest is the 9% who reported “counseling is not important to my quitting.” This group represents a segment of respondents who failed to appreciate the evidence that demonstrates the benefits of counseling and medical adjunct therapy. Further patient education is clearly needed to ensure patients understand how important smoking cessation is to their health and how important counseling is to their quitting efforts. To accomplish this goal, patient education concerning tobacco cessation in the form of televideo programming placed in the clinic wait areas is underway at the Atlanta VAMC.
Less frequently reported as barriers were “forgot” (6%), “counseling doesn’t work for me” (3%), and “parking concerns” (1%), suggesting that in this limited sample, these were not central reasons for not utilizing these services.
Limitations
The small sample size and that it was a convenience sample pose some concerns as to whether the results are truly representative of the population under study and whether the results can be extrapolated to similar populations. In addition, the results are from self-reported replies, relying on the integrity of the respondents to provide honest answers. Prefacing the study questions with an explanation that this was an opportunity to help the VA improve the quality of its programs was intended to ward off the desire to provide “acceptable” answers.
It is important to understand that patients within the VA system in certain categories of disability and financial means are reimbursed travel expenses for attending tobacco cessation treatment. It is possible that reimbursement factors might motivate patients to accept referrals for counseling that they may not be particularly committed to attend, contributing to a higher-than-expected number of referrals for patients who were not ready to quit.
Conclusion
The results of this study highlight several patient-reported barriers to tobacco cessation treatment, including scheduling conflicts, distance, and cost of travel. Only a small percentage (16%) actually reported they were not yet ready to quit or they did not feel counseling would work for them (3%). A slightly larger percentage reported they did not feel counseling is important (9%), and since it is well established that combining medication with behavioral counseling yields the greatest results for smoking cessation, it is clear that this segment of the patient population will require more education and attention.13
Accessibility issues were the biggest reason for nonattendance to the program (77%), and these issues highlight the need for continued work, at least at the Atlanta VAMC, on providing easier patient access to tobacco cessation treatment. Since the completion of this study, many updates have been implemented at the Atlanta VAMC to improve access, including the provision of telehealth education and the use of telephone quit lines.
Telehealth education, a technique that is highly compatible with lifestyle change counseling, has been shown to be cost-effective while providing intervention and education for patients who are too distant or unable to travel for other reasons.14
Tobacco quit lines are another option for patients with accessibility conflicts and are now operational in all 50 states. Most operate 24/7, manned by counselors trained in motivational interviewing and specifically tobacco cessation counseling. A meta-analysis of quit-line efficacy performed by Stead and colleagues demonstrated that quit lines improve long-term cessation for smokers who use them and even suggested a possible dose-response effect.15 Quit-line counseling, therefore, seems to offer a useful option for veterans who cannot easily access that counseling within the VA.
Motivational interviewing principles have also been proposed by VA as a new approach with great promise for application with veterans who are unmotivated, resistant, or ambivalent about changing unhealthy habits.16 At the Atlanta VAMC, training in motivational interviewing for primary care clinicians is ongoing. It is the provider’s responsibility to strongly encourage patients who use tobacco to utilize alternative tobacco cessation resources when attending a VA treatment program is not a viable option.
This study was a first step in examining barriers to treatment. Although the sample size was small, it is representative and useful in providing a framework from which to improve access to tobacco cessation programs as well as encourage utilization of alternative resources.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. U.S. Department of Health and Human Services. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014.
2. 2011 Survey of Veteran Enrollees’ Health and Reliance Upon VA, With Selected Comparison to the 1999-2010 Surveys. Washington, DC: Department of Veterans Affairs, Veterans Health Administration, Office of the Assistant Deputy Under Secretary for Health For Policy and Planning, Healthcare Analysis and Information Group, Enrollment and Forecasting Services; 2012.
3. Landolt K, Ajdacic-Gross V, Angst J, et al. Smoking and psychiatric disorders: Have subthreshold disorders been overlooked? Nicotine Tob Res. 2010;12(5):516-520.
4. Baca CT, Yahne CE. Smoking cessation during substance abuse treatment: What you need to know. J Subst Abuse Treat. 2009;36(2):205-219.
5. Smoking and Tobacco Use Cessation Report. Washington, DC: Department of Veterans Affairs, Veterans Health Administration, Office of the Assistant Deputy Secretary for Health for Policy and Planning; 2010.
6. Committee on Smoking Cessation in Military and Veteran Populations, Board on Population Health and Public Health Practice, Institute of Medicine. Combating Tobacco Use in the Military and Veteran Populations. Washington, DC: The National Academies Press; 2009.
7. Dollar K, Dundon M, Kusche A. Tobacco Use Cessation: A Brief Primary Care Intervention, A Training Manual for Integrated Primary Care Behavioral Health Providers and Other Tobacco Cessation Providers. Washington, DC: Department of Veterans Affairs, Center for Integrated Healthcare; 2010.
8. Burchfield BE, Keller T, Avritt L, Wright M, Ackerman MD. A multi-disciplinary approach to smoking cessation within the Department of Veterans Affairs. Paper presented at: 2004 Georgia Psychological Association Annual Meeting; May 2004; Hilton Head, SC.
9. Raupach T, Merker J, Hasenfuss G, Andreas S, Pipe A. Knowledge gaps about smoking cessation in hospitalized patients and their doctors. Eur J Cardiovasc Prev Rehabil. 2011;18(2):334-341.
10. Huy C, Diehm C, Schneider S. Cardiovascular prevention at the general practitioner? First results of a study on attitudes, services, success and barriers in practice [in German]. Dtsch Med Wochenschr. 2012;137(1-2):17-22.
11. Weaver KE, Danhauer SC, Tooze JA, et al. Smoking cessation counseling beliefs and behaviors of outpatient oncology providers. Oncologist. 2012;17(3):455-462.
12. McFall M, Saxon AJ, Malte CA, et al; CSP 519 Study Team. Integrating tobacco cessation into mental health care for posttraumatic stress disorder: A randomized controlled trial. JAMA. 2010;304(22):2485-2493.
13. Fiore MC, Jaén CR, Baker TB, et al. Treating Tobacco Use and Dependence: 2008 Update. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service; 2008.
14. Saab PG, McCalla JR, Coons HL, et al. Technological and medical advances: Implications for health psychology. Health Psychol. 2004;23(2):142-146.
15. Stead LF, Perera R, Lancaster T. A systematic review of interventions for smokers who contact quitlines. Tob Control. 2007;16(suppl 1):i3-i8.
16. Rollnick S, Miller WR, Butler CC. Motivational Interviewing in Health Care: Helping Patients Change Behavior. New York, NY: The Guilford Press; 2008.
1. U.S. Department of Health and Human Services. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014.
2. 2011 Survey of Veteran Enrollees’ Health and Reliance Upon VA, With Selected Comparison to the 1999-2010 Surveys. Washington, DC: Department of Veterans Affairs, Veterans Health Administration, Office of the Assistant Deputy Under Secretary for Health For Policy and Planning, Healthcare Analysis and Information Group, Enrollment and Forecasting Services; 2012.
3. Landolt K, Ajdacic-Gross V, Angst J, et al. Smoking and psychiatric disorders: Have subthreshold disorders been overlooked? Nicotine Tob Res. 2010;12(5):516-520.
4. Baca CT, Yahne CE. Smoking cessation during substance abuse treatment: What you need to know. J Subst Abuse Treat. 2009;36(2):205-219.
5. Smoking and Tobacco Use Cessation Report. Washington, DC: Department of Veterans Affairs, Veterans Health Administration, Office of the Assistant Deputy Secretary for Health for Policy and Planning; 2010.
6. Committee on Smoking Cessation in Military and Veteran Populations, Board on Population Health and Public Health Practice, Institute of Medicine. Combating Tobacco Use in the Military and Veteran Populations. Washington, DC: The National Academies Press; 2009.
7. Dollar K, Dundon M, Kusche A. Tobacco Use Cessation: A Brief Primary Care Intervention, A Training Manual for Integrated Primary Care Behavioral Health Providers and Other Tobacco Cessation Providers. Washington, DC: Department of Veterans Affairs, Center for Integrated Healthcare; 2010.
8. Burchfield BE, Keller T, Avritt L, Wright M, Ackerman MD. A multi-disciplinary approach to smoking cessation within the Department of Veterans Affairs. Paper presented at: 2004 Georgia Psychological Association Annual Meeting; May 2004; Hilton Head, SC.
9. Raupach T, Merker J, Hasenfuss G, Andreas S, Pipe A. Knowledge gaps about smoking cessation in hospitalized patients and their doctors. Eur J Cardiovasc Prev Rehabil. 2011;18(2):334-341.
10. Huy C, Diehm C, Schneider S. Cardiovascular prevention at the general practitioner? First results of a study on attitudes, services, success and barriers in practice [in German]. Dtsch Med Wochenschr. 2012;137(1-2):17-22.
11. Weaver KE, Danhauer SC, Tooze JA, et al. Smoking cessation counseling beliefs and behaviors of outpatient oncology providers. Oncologist. 2012;17(3):455-462.
12. McFall M, Saxon AJ, Malte CA, et al; CSP 519 Study Team. Integrating tobacco cessation into mental health care for posttraumatic stress disorder: A randomized controlled trial. JAMA. 2010;304(22):2485-2493.
13. Fiore MC, Jaén CR, Baker TB, et al. Treating Tobacco Use and Dependence: 2008 Update. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service; 2008.
14. Saab PG, McCalla JR, Coons HL, et al. Technological and medical advances: Implications for health psychology. Health Psychol. 2004;23(2):142-146.
15. Stead LF, Perera R, Lancaster T. A systematic review of interventions for smokers who contact quitlines. Tob Control. 2007;16(suppl 1):i3-i8.
16. Rollnick S, Miller WR, Butler CC. Motivational Interviewing in Health Care: Helping Patients Change Behavior. New York, NY: The Guilford Press; 2008.