User login
Reducing hospital readmissions through primary care practice transformation
ABSTRACT
Purpose To assess the impact of a multicomponent intervention on 30-day hospital readmissions in a group of primary care practices that undertook practice transformation, compared with rates in usual-care practices that admitted patients to the same hospital service.
Methods Four primary care clinics enhanced patient care coordination with care managers and inpatient care teams, and developed and used hospital readmission reports to monitor readmission rates. Patient readmissions to the hospital were analyzed over a 12-month period from May 2012 through April 2013, among patients who fell into 2 groups. Group 1 patients were those cared for by the primary care clinics that implemented transformation activities and who were admitted to the hospital associated with the practices. Group 2 patients were seen at clinics in the same catchment area that did not undertake any known practice redesign activities (usual care group).
Results A total of 961 patients were included in analyses; 685 (71.3%) were in Group 1, and 276 (28.7%) were in Group 2. Readmissions among Group 1 patients decreased from 27% to 7.1% (P=.02), and readmissions in Group 2 were variable with a nonsignificant trend (P=.53). The unadjusted regression model that compared the interaction between Group 1 and Group 2 patients found a significant difference in readmissions (P=.05).
Conclusion Developing a multicomponent intervention appears to have a significant impact on reducing hospital readmissions. Primary care groups seeking to reduce hospital readmissions should consider implementing similar processes.
An analysis of Medicare claims data between 2003 and 2004 found that nearly 20% of the >11 million Medicare patients who had been discharged from a hospital were readmitted within 30 days, at a cost of $17.4 billion.1 Certain patient subgroups were especially worrisome. Of those with congestive heart failure, for example, 50% were typically readmitted within 6 months of initial hospitalization.2
A longstanding issue comes to the fore. Concerns about hospital readmissions appeared in the literature nearly 40 years ago.3 In the 1990s, with the advent of managed care, organizations began “case management” to reduce preventable readmissions using several approaches, including enhanced primary care access.4 A meta-analysis at that time demonstrated some reduction in hospital readmissions associated with hospital-based case management interventions.5 Though quality improvement programs and case management have been assumed to reduce hospital readmissions, some studies have actually found the opposite,6,7 or have yielded conflicting evidence.8-13 Skyrocketing costs of health care have brought hospital readmissions to the forefront of health system redesign efforts.14-16
Section 3025 of the Affordable Care Act added section 1886(q) to the Social Security Act establishing the Hospital Readmissions Reduction Program, which requires Centers for Medicare & Medicaid Services to reduce payments to hospitals with excess readmissions.17 This change was introduced on October 1, 2012 and has precipitated discussion across the country about the prevention of unnecessary hospital readmissions.18,19
Patient factors contributing to hospital readmissions. Concerns patients cite most frequently as contributors to relapse and readmission are 1) feeling unprepared for discharge; 2) difficulty performing activities of daily living; 3) trouble adhering to discharge medications; 4) difficulty accessing discharge medications; and 5) lack of social support.20 While multiple tools have been developed to better assess unplanned readmissions—including the Identification of Seniors at Risk, the Flemish version of the Triage Risk Screening Tool, and Variable Indicative of Placement risk—none of these have accurately predicted unplanned readmission in older, hospitalized patients.21 Predicting which patients will require readmission remains elusive,22 though some new models show promise.23 z
Targeted interventions that show promise. Postdischarge telephone follow-up has been shown to reduce hospital readmissions,24,25 and a direct correlation has been observed between the timing of the intervention and readmission rates, with interventions implemented closer to the date of discharge being associated with greater reductions in the number of readmissions.26 Additionally, multicomponent interventions with both pre- and postdischarge elements that specifically target high-risk populations appear to be more effective in reducing readmissions than single-component interventions.27
Hansen et al28 identified a number of predischarge, postdischarge, and bridging interventions that could potentially reduce hospital readmissions (TABLE 1). No single intervention implemented alone consistently reduced the risk for 30-day rehospitalization.28 One multicomponent intervention that has reduced readmissions for patients with heart failure or acute myocardial infarction is a transition coach, who visits patients in the hospital and sees them again in clinic for follow-up appointments. The coach also calls patients between face-to-face visits to review treatment plans and answer questions.29
The impetus for our study. The patient-centered medical home (PCMH) has been gaining traction as a mechanism to improve patient care while reducing health care spending.30,31 An intensive multidimensional medical home model introduced into 11 primary care practices proved capable of significantly reducing admissions and readmissions for Medicare Advantage members.32 Additionally, intelligently leveraging clinical information technology is likely to be critical in reducing readmissions.33 The purpose of our observational study was to examine the impact of a multicomponent intervention on 30-day hospital readmissions over 12 months.
METHODS
Study setting and preintervention practice routines in 2 patient groups
The study setting for Group 1 involved patients with assigned primary care providers (PCPs) in a university-based practice group at 4 outpatient clinics. The study setting for Group 2 included patients with assigned PCPs from county and community health centers, involving 12 primary care clinics in total. While the groups’ patient populations were distinguished for descriptive purposes, in practice the patients were admitted to the same inpatient treatment teams and university-based hospital in a metropolitan setting. For both groups, the primary care practices admitted patients to the hospital directly from clinic or through the emergency department (ED).
An admitting team from one of the inpatient services completed the admission, initiated treatment, and discharged patients. Preintervention, limited discharge case management occurred at the hospital, driven primarily by the treating team’s requests. The admitting team also attempted to schedule outpatient follow-up appointments with an available PCP at the patient’s primary clinic after discharge. Obstacles to successful appointment scheduling prior to discharge included but were not limited to discharges over weekends or holidays or after clinic hours. Additionally, for both groups, discharge summaries were sent to the PCP either electronically via the electronic medical record (EMR) or via system-generated automated fax.
Creating a culture of continuity in Group 1
Transformation of outpatient activities. We developed several important processes to transform the patient experience through hospitalization and discharge. Together, these processes created a “culture of continuity” to prevent avoidable readmissions. We introduced an innovative, systematic approach to notifying the clinic and primary care clinician about initial admission. We also gave notification immediately upon discharge, rather than waiting until after discharge, as had been occurring. This patient-centered change engaged the primary care team in the care of the patient while hospitalized and during discharge planning; it actively ensured that follow-up appointments occurred within 1 week after discharge. Prior to this intervention, there was no system for ensuring timely follow-up after hospital discharge. The new expectation for the ambulatory clinics was that clinic staff could “reach in” to the patient during the hospital stay and actively contact the patient before discharge to schedule a postdischarge appointment at the patient’s convenience.
The 4 practices had embraced and implemented the PCMH model, a core component of which is care coordination.34,35 Each clinic appointed a registered nurse (RN) to serve as a team-based care manager (CM) for patients being discharged from the hospital. Responsibilities included fielding calls or electronic communications from the inpatient team, developing a hospital follow-up workflow, developing a standardized list of questions to ask each patient after discharge, and calling patients to ensure a follow-up appointment was scheduled, ideally within 2 to 3 days and at least within 7 days of discharge. The CM prioritized scheduling follow-up appointments with the patient’s PCP to ensure the highest level of continuity.
In addition to patient-specific documents, CMs received electronic reports from inpatient teams (including from the ED, medical and surgical intensive care units, and surgery) listing all Group 1 patients discharged from the hospital. Reports were run daily and allowed the outpatient clinic staff and CMs to verify patients against previous lists of anticipated discharges, and to generate their own lists. The CMs would then make follow-up phone calls and ensure that appointments were scheduled for these patients.
Medical directors at the 4 clinics received monthly summary reports profiling clinical activities related to hospitalizations. A data team (led by author SF) created the reports, which initially focused on care delivered in ambulatory settings (and included the development of a “balanced scorecard” to assess quality of care, financial productivity, and operational efficiency36). The data team developed new reports specifically for hospital admissions, discharges, and readmissions, identifying:
• all patients admitted by inpatient team
• the number and percentage of patients who were readmitted within 30 days
• the number and percentage of patients who had received a follow-up phone call or electronic communication from the outpatient team
• the number of patients who had follow-up visits after discharge within 7 and 30 days
• the number of patients who had clinic visits prior to readmission
• all patients discharged from any service within the prior 24 hours.
These reports, which had patient drilldown capability, were forwarded to all providers and teams at each clinic by the medical director. Teams at each clinic were then charged with analyzing the readmissions, identifying high-risk patients, and improving the coordination of care for these patients, including the use of RN/clinician co-visits and proactive outreach from the team-based nurses and staff.
Transformation of inpatient activities. We reorganized inpatient teams to include clinician representatives from the clinics whose patients were being treated. This process ensured better continuity of experience and familiarity with the environment of care and discharge/follow-up processes for both patients and all providers.
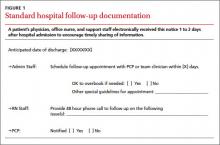
Additionally, inpatient teams developed new workflows to ensure that all involved members of the outpatient team were well informed of the hospitalization process. On the first or second day of admission, a hospital follow-up document was electronically routed to the administrative support staff, the PCP team nurse, and the PCP (FIGURE 1). An integrated EMR created a link between the hospital and all ambulatory practices that allowed for real-time transmission of patient information. The document identified the timing of a follow-up appointment and requested a 48-hour phone call from the team nurse after hospital discharge. The inpatient team also included a concise summary of the hospitalization for the PCP, to aid in anticipating patient discharge and any impending needs. The document was retrievable and traceable in the EMR.
Study groups and statistical analysis
The Oregon Health & Science University’s Institutional Review Board (IRB#9768) determined this study was not human subjects research because the proposed activity did not meet the definition of human subject per 45 CFR 46.102(f). The board made this determination because our analysis file included only hospital readmission rates and no patient-level data.
Adult patients admitted by the inpatient teams consisted of 2 distinct populations: patients whose PCP practiced at one of the 4 outpatient clinics (Group 1 patients); and patients admitted from other, unaffiliated clinics (Group 2 patients). In contrast to the transformations in patient care described in Group 1, care provided to Group 2 patients was considered usual care, as there was no interface between outpatient and inpatient teams to revise operations. Patients in either group were excluded from analyses if they died during the hospitalization. Maternity patients were also excluded.
We identified the percentage of patients readmitted within 30 days of a hospital admission using administrative data sources, which underwent careful data checking and validation, and were sub-grouped according to whether the patients were in Group 1 or Group 2. We used group-specific and overall linear regression to examine the changes in percentage of readmission within 30 days of discharge in the 2 study groups over 12 months, including a model that specifically assessed the interaction between Group 1 readmission percentages and those in Group 2. We considered a P-value ≤.05 to be significant in this exploratory study.
RESULTS
Patient readmissions decreased significantly
Our analysis included 961 patients; 685 patients (71.3%) were in Group 1, and 276 (28.7%) were in Group 2 (Table 2). The distribution of patient gender and mean age was similar within groups for patients readmitted and not readmitted during the study period. Among patients readmitted, the mean hospital length of stay was 5.8 days and 7.1 days for Group 1 and Group 2, respectively. Among those not readmitted, the mean hospital length of stay was 4.3 and 4.9 in Group 1 and 2, respectively.
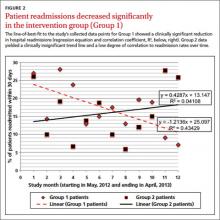
The percentage of patients readmitted per month ranged from 28.1% to 7.1% in Group 1 and 27.8% to 5.9% in Group 2 (Figure 2). Patient readmissions in Group 1 decreased significantly from 27% in May 2012 to 7.1% in April 2013 with an R2 of 0.43 (P=.02). Readmissions of patients in Group 2 were more variable; 26.1% in May 2012 and 25.9% in April 2013 with a non-significant R2 of 0.04 (P=.53). The regression model (unadjusted) that compared the interaction between Group 1 and Group 2 readmissions over the study period was significant, indicating a decrease in readmissions in Group 1 and no strong correlation between usual care and readmissions over time in Group 2 (P=.05).
DISCUSSION
Implementing intensive coordinated care management and transition processes in a group of primary care clinics appears to significantly decrease hospital readmissions for patients in Group 1, compared with those in Group 2 who received usual care. While it is possible that some of the ambulatory practices in Group 2 admitting patients to the inpatient services were using or developing care coordination programs including hospital follow-up, none of these providers or groups interfaced with the inpatient teams in this study. We are, therefore, confident that Group 2 providers were not undertaking any new or novel activities that reached in to hospital inpatient services to improve care coordination.
Our findings are consistent with the literature review conducted by Scott et al,27 which found that multicomponent interventions are more successful at reducing readmissions than single-component interventions. In our Group 1 clinics, we implemented 8 of the 12 predischarge, postdischarge, and bridging interventions identified by Hansen et al28 (medication reconciliation, discharge planning, scheduling of a follow-up appointment before discharge, follow-up telephone calls, timely communication with ambulatory providers, timely ambulatory provider follow-up, physician continuity across the inpatient and outpatient setting, and patient-centered discharge instructions).
Study strengths and weaknesses. The strengths of this study include means and quality of data capture for hospital readmission rates in the study setting. Limitations include the small sample sizes, which did not allow us to conduct a multivariable adjusted analysis that would have taken into account patient characteristics, seasons, and temporal correlations. These covariates might drive study findings in a way that results in us drawing inaccurate conclusions—the analysis we conducted (unadjusted) assumed that the events that occurred in each month were unrelated to what might have occurred in the prior month or subsequent month.
Patients in the 2 study groups did exhibit differences that could have contributed to our findings. For example, the average length of stay for Group 2 patients was longer by just over 1 day compared with that in Group 1. This may suggest Group 2 patients were sicker, and thus may have needed to be readmitted within 30 days of their discharge. We cannot know for certain that patients in Group 1 were less ill, as this would require a more discriminating study design. As with many studies, additional questions arise, but these serve to further a line of research that is vitally important.
Another factor that could have affected our findings is that Group 1 patient readmission rates started off higher than the Group 2 patients, so there is a chance that regression to the mean rather than changes in clinical care could have contributed to some of the decrease in Group 1 readmission rates. There are potential subject-level, provider-level, and clinic-level factors that could have been used to adjust for potential confounding. Future studies could address these factors. Longer study follow-up would provide an even better picture of the difference between the groups.
A multicomponent intervention works. Creating a culture of continuity is an important aspect of PCMH. Not all primary care clinics or PCMHs may have built-in relationships for inpatient care of their patients. We would argue that outpatient adoption of the enhanced “reaching in” and a multicomponent intervention would have a significant positive impact on patient care and improve the transition from in- to outpatient care, and likely reduce readmissions.
CORRESPONDENCE
Brett White, MD, 4411 SW Vermont St, Portland, OR 97219; brettwhitemd@gmail.com
The authors gratefully acknowledge the clinic and inpatient physicians and staffs as well as the Research Program in the Department of Family Medicine, Oregon Health & Science University.
1. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418-1428.
2. Zaya M, Phan A, Schwarz ER. The dilemma, causes and approaches to avoid recurrent hospital readmissions for patients with chronic heart failure. Heart Fail Rev. 2012;17:345-353.
3. Marriott PF, Grigor JM, Hiep A. Reducing hospital readmission rates among schizophrenics. Med J Aust. 1976;2:897-898.
4. Fitzgerald JF, Smith DM, Martin DK, et al. A case manager intervention to reduce readmissions. Arch Intern Med. 1994;154:1721-1729.
5. Kim YJ, Soeken KL. A meta-analysis of the effect of hospital-based case management on hospital length-of-stay and readmission. Nurs Res. 2005;54:255-264.
6. Weinberger M, Oddone EZ, Henderson WG. Does increased access to primary care reduce hospital readmissions? Veterans Affairs Cooperative Study Group on Primary Care and Hospital Readmission. N Engl J Med. 1996;334:1441-1447.
7. Mudge A, Denaro C, Scott I, et al. The paradox of readmission: effect of a quality improvement program in hospitalized patients with heart failure. J Hosp Med. 2010;5:148-153.
8. Mistiaen P, Francke AL, Poot E. Interventions aimed at reducing problems in adult patients discharged from hospital to home: a systematic meta-review. BMC Health Serv Res. 2007;7:47.
9. Linertová R, García-Pérez L, Vázquez-Díaz JR, et al. Interventions to reduce hospital readmissions in the elderly: in-hospital or home care. A systematic review. J Eval Clin Pract. 2011;17:1167-1175.
10. Shepperd S, Parkes J, McClaren J, et al. Discharge planning from hospital to home. Cochrane Database Syst Rev. 2004;(1):CD000313. Review. Update in: Cochrane Database Syst Rev. 2010;(1):CD000313.
11. Huntley AL, Thomas R, Mann M, et al. Is case management effective in reducing the risk of unplanned hospital admissions for older people? A systematic review and meta-analysis. Fam Pract. 2013;30:266-275.
12. Crocker JB, Crocker JT, Greenwald JL. Telephone follow-up as a primary care intervention for postdischarge outcomes improvement: a systematic review. Am J Med. 2012;125:915-921.
13. Mistiaen P, Poot E. Telephone follow-up, initiated by a hospital-based health professional, for postdischarge problems in patients discharged from hospital to home. Cochrane Database Syst Rev. 2006;(4):CD004510.
14. Jack B, Paasche-Orlow M, Mitchell S, et al. An overview of the Re-Engineered Discharge (RED) toolkit. AHRQ Publication No.12(13)-0084. Rockville, MD: Agency for Healthcare Research and Quality; March 2013. 15. Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff (Millwood). 2008;27:759-769.
16. Greenwald J, Denham C, Jack B. The hospital discharge: A review of a high risk care transition with highlights of a reengineered discharge process. J Patient Saf. 2007;3:97-106.
17. Centers for Medicare & Medicaid Services. Readmissions Reduction Program. Available at: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html. Accessed June 18, 2013.
18. Joynt KE, Jha AK. A path forward on Medicare readmissions. N Engl J Med. 2013;368:1175-1177.
19. Joynt KE, Jha AK. Characteristics of hospitals receiving penalties under the Hospital Readmissions Reduction Program. JAMA. 2013;309:342-343.
20. Kangovi S, Grande D, Meehan P, et al. Perceptions of readmitted patients on the transition from hospital to home. J Hosp Med. 2012;7:709-712.
21. Braes T, Moons P, Lipkens P, et al. Screening for risk of unplanned readmission in older patients admitted to hospital: predictive accuracy of three instruments. Aging Clin Exp Res. 2010;22:345-351.
22. Allaudeen N, Schnipper JL, Orav EJ, et al. Inability of providers to predict unplanned readmissions. J Gen Intern Med. 2011;26:771-776.
23. Gruneir A, Dhalla IA, van Walraven C, et al. Unplanned readmissions after hospital discharge among patients identified as being at high risk for readmission using a validated predictive algorithm. Open Med. 2011;5:e104-e111.
24. Harrison PL, Hara PA, Pope JE, et al. The impact of postdischarge telephonic follow-up on hospital readmissions. Popul Health Manag. 2011;14:27-32.
25. Herrera-Espiñeira C, Rodríguez del Águila Mdel M, Navarro Espigares JL, et al. [Effect of a telephone care program after hospital discharge from a trauma surgery unit]. Gac Sanit. 2011;25:133-138.
26. Costantino ME, Frey B, Hall B, et al. The influence of a postdischarge intervention on reducing hospital readmissions in a Medicare population. Popul Health Manag. 2013;16:310-316.
27. Scott IA. Preventing the rebound: improving care transition in hospital discharge processes. Aust Health Rev. 2010;34:445-451.
28. Hansen LO, Young RS, Hinami K, et al. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med. 2011;155:520-528.
29. Coaching helps cut readmissions. Hosp Case Manag. 2011;19:155-156.
30. DeVries A, Li CH, Sridhar G, et al. Impact of medical homes on quality, healthcare utilization, and costs. Am J Manag Care. 2012;18:534-544.
31. Paustian ML, Alexander JA, El Reda DK, et al. Partial and incremental PCMH practice transformation: implications for quality and costs. Health Serv Res. 2013 Jul 5. [Epub ahead of print].
32. Gilfillan RJ, Tomcavage J, Rosenthal MB, et al. Value and the medical home: effects of transformed primary care. Am J Manag Care. 2010;16:607-614.
33. Haglund M. Mastering readmissions: laying the foundation for change. Post-healthcare reform, pioneers are laying the foundation for serious readmissions-reduction work. Healthc Inform. 2011;28:10-13,16.
34. Meyers D, Peikes D, Genevro J, et al. The roles of patient-centered medical homes and accountable care organizations in coordinating patient care. AHRQ Publication No. 11-M005-EF. Rockville, MD: Agency for Healthcare Research and Quality; December 2010.
35. Ferrante JM, Balasubramanian BA, Hudson SV, et al. Principles of the patient-centered medical home and preventive services delivery. Ann Fam Med. 2010;8:108-116.
36. Fields SA, Cohen D. Performance enhancement using a balanced scorecard in a patient-centered medical home. Fam Med. 2011;43:735-739.
ABSTRACT
Purpose To assess the impact of a multicomponent intervention on 30-day hospital readmissions in a group of primary care practices that undertook practice transformation, compared with rates in usual-care practices that admitted patients to the same hospital service.
Methods Four primary care clinics enhanced patient care coordination with care managers and inpatient care teams, and developed and used hospital readmission reports to monitor readmission rates. Patient readmissions to the hospital were analyzed over a 12-month period from May 2012 through April 2013, among patients who fell into 2 groups. Group 1 patients were those cared for by the primary care clinics that implemented transformation activities and who were admitted to the hospital associated with the practices. Group 2 patients were seen at clinics in the same catchment area that did not undertake any known practice redesign activities (usual care group).
Results A total of 961 patients were included in analyses; 685 (71.3%) were in Group 1, and 276 (28.7%) were in Group 2. Readmissions among Group 1 patients decreased from 27% to 7.1% (P=.02), and readmissions in Group 2 were variable with a nonsignificant trend (P=.53). The unadjusted regression model that compared the interaction between Group 1 and Group 2 patients found a significant difference in readmissions (P=.05).
Conclusion Developing a multicomponent intervention appears to have a significant impact on reducing hospital readmissions. Primary care groups seeking to reduce hospital readmissions should consider implementing similar processes.
An analysis of Medicare claims data between 2003 and 2004 found that nearly 20% of the >11 million Medicare patients who had been discharged from a hospital were readmitted within 30 days, at a cost of $17.4 billion.1 Certain patient subgroups were especially worrisome. Of those with congestive heart failure, for example, 50% were typically readmitted within 6 months of initial hospitalization.2
A longstanding issue comes to the fore. Concerns about hospital readmissions appeared in the literature nearly 40 years ago.3 In the 1990s, with the advent of managed care, organizations began “case management” to reduce preventable readmissions using several approaches, including enhanced primary care access.4 A meta-analysis at that time demonstrated some reduction in hospital readmissions associated with hospital-based case management interventions.5 Though quality improvement programs and case management have been assumed to reduce hospital readmissions, some studies have actually found the opposite,6,7 or have yielded conflicting evidence.8-13 Skyrocketing costs of health care have brought hospital readmissions to the forefront of health system redesign efforts.14-16
Section 3025 of the Affordable Care Act added section 1886(q) to the Social Security Act establishing the Hospital Readmissions Reduction Program, which requires Centers for Medicare & Medicaid Services to reduce payments to hospitals with excess readmissions.17 This change was introduced on October 1, 2012 and has precipitated discussion across the country about the prevention of unnecessary hospital readmissions.18,19
Patient factors contributing to hospital readmissions. Concerns patients cite most frequently as contributors to relapse and readmission are 1) feeling unprepared for discharge; 2) difficulty performing activities of daily living; 3) trouble adhering to discharge medications; 4) difficulty accessing discharge medications; and 5) lack of social support.20 While multiple tools have been developed to better assess unplanned readmissions—including the Identification of Seniors at Risk, the Flemish version of the Triage Risk Screening Tool, and Variable Indicative of Placement risk—none of these have accurately predicted unplanned readmission in older, hospitalized patients.21 Predicting which patients will require readmission remains elusive,22 though some new models show promise.23 z
Targeted interventions that show promise. Postdischarge telephone follow-up has been shown to reduce hospital readmissions,24,25 and a direct correlation has been observed between the timing of the intervention and readmission rates, with interventions implemented closer to the date of discharge being associated with greater reductions in the number of readmissions.26 Additionally, multicomponent interventions with both pre- and postdischarge elements that specifically target high-risk populations appear to be more effective in reducing readmissions than single-component interventions.27
Hansen et al28 identified a number of predischarge, postdischarge, and bridging interventions that could potentially reduce hospital readmissions (TABLE 1). No single intervention implemented alone consistently reduced the risk for 30-day rehospitalization.28 One multicomponent intervention that has reduced readmissions for patients with heart failure or acute myocardial infarction is a transition coach, who visits patients in the hospital and sees them again in clinic for follow-up appointments. The coach also calls patients between face-to-face visits to review treatment plans and answer questions.29
The impetus for our study. The patient-centered medical home (PCMH) has been gaining traction as a mechanism to improve patient care while reducing health care spending.30,31 An intensive multidimensional medical home model introduced into 11 primary care practices proved capable of significantly reducing admissions and readmissions for Medicare Advantage members.32 Additionally, intelligently leveraging clinical information technology is likely to be critical in reducing readmissions.33 The purpose of our observational study was to examine the impact of a multicomponent intervention on 30-day hospital readmissions over 12 months.
METHODS
Study setting and preintervention practice routines in 2 patient groups
The study setting for Group 1 involved patients with assigned primary care providers (PCPs) in a university-based practice group at 4 outpatient clinics. The study setting for Group 2 included patients with assigned PCPs from county and community health centers, involving 12 primary care clinics in total. While the groups’ patient populations were distinguished for descriptive purposes, in practice the patients were admitted to the same inpatient treatment teams and university-based hospital in a metropolitan setting. For both groups, the primary care practices admitted patients to the hospital directly from clinic or through the emergency department (ED).
An admitting team from one of the inpatient services completed the admission, initiated treatment, and discharged patients. Preintervention, limited discharge case management occurred at the hospital, driven primarily by the treating team’s requests. The admitting team also attempted to schedule outpatient follow-up appointments with an available PCP at the patient’s primary clinic after discharge. Obstacles to successful appointment scheduling prior to discharge included but were not limited to discharges over weekends or holidays or after clinic hours. Additionally, for both groups, discharge summaries were sent to the PCP either electronically via the electronic medical record (EMR) or via system-generated automated fax.
Creating a culture of continuity in Group 1
Transformation of outpatient activities. We developed several important processes to transform the patient experience through hospitalization and discharge. Together, these processes created a “culture of continuity” to prevent avoidable readmissions. We introduced an innovative, systematic approach to notifying the clinic and primary care clinician about initial admission. We also gave notification immediately upon discharge, rather than waiting until after discharge, as had been occurring. This patient-centered change engaged the primary care team in the care of the patient while hospitalized and during discharge planning; it actively ensured that follow-up appointments occurred within 1 week after discharge. Prior to this intervention, there was no system for ensuring timely follow-up after hospital discharge. The new expectation for the ambulatory clinics was that clinic staff could “reach in” to the patient during the hospital stay and actively contact the patient before discharge to schedule a postdischarge appointment at the patient’s convenience.
The 4 practices had embraced and implemented the PCMH model, a core component of which is care coordination.34,35 Each clinic appointed a registered nurse (RN) to serve as a team-based care manager (CM) for patients being discharged from the hospital. Responsibilities included fielding calls or electronic communications from the inpatient team, developing a hospital follow-up workflow, developing a standardized list of questions to ask each patient after discharge, and calling patients to ensure a follow-up appointment was scheduled, ideally within 2 to 3 days and at least within 7 days of discharge. The CM prioritized scheduling follow-up appointments with the patient’s PCP to ensure the highest level of continuity.
In addition to patient-specific documents, CMs received electronic reports from inpatient teams (including from the ED, medical and surgical intensive care units, and surgery) listing all Group 1 patients discharged from the hospital. Reports were run daily and allowed the outpatient clinic staff and CMs to verify patients against previous lists of anticipated discharges, and to generate their own lists. The CMs would then make follow-up phone calls and ensure that appointments were scheduled for these patients.
Medical directors at the 4 clinics received monthly summary reports profiling clinical activities related to hospitalizations. A data team (led by author SF) created the reports, which initially focused on care delivered in ambulatory settings (and included the development of a “balanced scorecard” to assess quality of care, financial productivity, and operational efficiency36). The data team developed new reports specifically for hospital admissions, discharges, and readmissions, identifying:
• all patients admitted by inpatient team
• the number and percentage of patients who were readmitted within 30 days
• the number and percentage of patients who had received a follow-up phone call or electronic communication from the outpatient team
• the number of patients who had follow-up visits after discharge within 7 and 30 days
• the number of patients who had clinic visits prior to readmission
• all patients discharged from any service within the prior 24 hours.
These reports, which had patient drilldown capability, were forwarded to all providers and teams at each clinic by the medical director. Teams at each clinic were then charged with analyzing the readmissions, identifying high-risk patients, and improving the coordination of care for these patients, including the use of RN/clinician co-visits and proactive outreach from the team-based nurses and staff.
Transformation of inpatient activities. We reorganized inpatient teams to include clinician representatives from the clinics whose patients were being treated. This process ensured better continuity of experience and familiarity with the environment of care and discharge/follow-up processes for both patients and all providers.
Additionally, inpatient teams developed new workflows to ensure that all involved members of the outpatient team were well informed of the hospitalization process. On the first or second day of admission, a hospital follow-up document was electronically routed to the administrative support staff, the PCP team nurse, and the PCP (FIGURE 1). An integrated EMR created a link between the hospital and all ambulatory practices that allowed for real-time transmission of patient information. The document identified the timing of a follow-up appointment and requested a 48-hour phone call from the team nurse after hospital discharge. The inpatient team also included a concise summary of the hospitalization for the PCP, to aid in anticipating patient discharge and any impending needs. The document was retrievable and traceable in the EMR.
Study groups and statistical analysis
The Oregon Health & Science University’s Institutional Review Board (IRB#9768) determined this study was not human subjects research because the proposed activity did not meet the definition of human subject per 45 CFR 46.102(f). The board made this determination because our analysis file included only hospital readmission rates and no patient-level data.
Adult patients admitted by the inpatient teams consisted of 2 distinct populations: patients whose PCP practiced at one of the 4 outpatient clinics (Group 1 patients); and patients admitted from other, unaffiliated clinics (Group 2 patients). In contrast to the transformations in patient care described in Group 1, care provided to Group 2 patients was considered usual care, as there was no interface between outpatient and inpatient teams to revise operations. Patients in either group were excluded from analyses if they died during the hospitalization. Maternity patients were also excluded.
We identified the percentage of patients readmitted within 30 days of a hospital admission using administrative data sources, which underwent careful data checking and validation, and were sub-grouped according to whether the patients were in Group 1 or Group 2. We used group-specific and overall linear regression to examine the changes in percentage of readmission within 30 days of discharge in the 2 study groups over 12 months, including a model that specifically assessed the interaction between Group 1 readmission percentages and those in Group 2. We considered a P-value ≤.05 to be significant in this exploratory study.
RESULTS
Patient readmissions decreased significantly
Our analysis included 961 patients; 685 patients (71.3%) were in Group 1, and 276 (28.7%) were in Group 2 (Table 2). The distribution of patient gender and mean age was similar within groups for patients readmitted and not readmitted during the study period. Among patients readmitted, the mean hospital length of stay was 5.8 days and 7.1 days for Group 1 and Group 2, respectively. Among those not readmitted, the mean hospital length of stay was 4.3 and 4.9 in Group 1 and 2, respectively.
The percentage of patients readmitted per month ranged from 28.1% to 7.1% in Group 1 and 27.8% to 5.9% in Group 2 (Figure 2). Patient readmissions in Group 1 decreased significantly from 27% in May 2012 to 7.1% in April 2013 with an R2 of 0.43 (P=.02). Readmissions of patients in Group 2 were more variable; 26.1% in May 2012 and 25.9% in April 2013 with a non-significant R2 of 0.04 (P=.53). The regression model (unadjusted) that compared the interaction between Group 1 and Group 2 readmissions over the study period was significant, indicating a decrease in readmissions in Group 1 and no strong correlation between usual care and readmissions over time in Group 2 (P=.05).
DISCUSSION
Implementing intensive coordinated care management and transition processes in a group of primary care clinics appears to significantly decrease hospital readmissions for patients in Group 1, compared with those in Group 2 who received usual care. While it is possible that some of the ambulatory practices in Group 2 admitting patients to the inpatient services were using or developing care coordination programs including hospital follow-up, none of these providers or groups interfaced with the inpatient teams in this study. We are, therefore, confident that Group 2 providers were not undertaking any new or novel activities that reached in to hospital inpatient services to improve care coordination.
Our findings are consistent with the literature review conducted by Scott et al,27 which found that multicomponent interventions are more successful at reducing readmissions than single-component interventions. In our Group 1 clinics, we implemented 8 of the 12 predischarge, postdischarge, and bridging interventions identified by Hansen et al28 (medication reconciliation, discharge planning, scheduling of a follow-up appointment before discharge, follow-up telephone calls, timely communication with ambulatory providers, timely ambulatory provider follow-up, physician continuity across the inpatient and outpatient setting, and patient-centered discharge instructions).
Study strengths and weaknesses. The strengths of this study include means and quality of data capture for hospital readmission rates in the study setting. Limitations include the small sample sizes, which did not allow us to conduct a multivariable adjusted analysis that would have taken into account patient characteristics, seasons, and temporal correlations. These covariates might drive study findings in a way that results in us drawing inaccurate conclusions—the analysis we conducted (unadjusted) assumed that the events that occurred in each month were unrelated to what might have occurred in the prior month or subsequent month.
Patients in the 2 study groups did exhibit differences that could have contributed to our findings. For example, the average length of stay for Group 2 patients was longer by just over 1 day compared with that in Group 1. This may suggest Group 2 patients were sicker, and thus may have needed to be readmitted within 30 days of their discharge. We cannot know for certain that patients in Group 1 were less ill, as this would require a more discriminating study design. As with many studies, additional questions arise, but these serve to further a line of research that is vitally important.
Another factor that could have affected our findings is that Group 1 patient readmission rates started off higher than the Group 2 patients, so there is a chance that regression to the mean rather than changes in clinical care could have contributed to some of the decrease in Group 1 readmission rates. There are potential subject-level, provider-level, and clinic-level factors that could have been used to adjust for potential confounding. Future studies could address these factors. Longer study follow-up would provide an even better picture of the difference between the groups.
A multicomponent intervention works. Creating a culture of continuity is an important aspect of PCMH. Not all primary care clinics or PCMHs may have built-in relationships for inpatient care of their patients. We would argue that outpatient adoption of the enhanced “reaching in” and a multicomponent intervention would have a significant positive impact on patient care and improve the transition from in- to outpatient care, and likely reduce readmissions.
CORRESPONDENCE
Brett White, MD, 4411 SW Vermont St, Portland, OR 97219; brettwhitemd@gmail.com
The authors gratefully acknowledge the clinic and inpatient physicians and staffs as well as the Research Program in the Department of Family Medicine, Oregon Health & Science University.
ABSTRACT
Purpose To assess the impact of a multicomponent intervention on 30-day hospital readmissions in a group of primary care practices that undertook practice transformation, compared with rates in usual-care practices that admitted patients to the same hospital service.
Methods Four primary care clinics enhanced patient care coordination with care managers and inpatient care teams, and developed and used hospital readmission reports to monitor readmission rates. Patient readmissions to the hospital were analyzed over a 12-month period from May 2012 through April 2013, among patients who fell into 2 groups. Group 1 patients were those cared for by the primary care clinics that implemented transformation activities and who were admitted to the hospital associated with the practices. Group 2 patients were seen at clinics in the same catchment area that did not undertake any known practice redesign activities (usual care group).
Results A total of 961 patients were included in analyses; 685 (71.3%) were in Group 1, and 276 (28.7%) were in Group 2. Readmissions among Group 1 patients decreased from 27% to 7.1% (P=.02), and readmissions in Group 2 were variable with a nonsignificant trend (P=.53). The unadjusted regression model that compared the interaction between Group 1 and Group 2 patients found a significant difference in readmissions (P=.05).
Conclusion Developing a multicomponent intervention appears to have a significant impact on reducing hospital readmissions. Primary care groups seeking to reduce hospital readmissions should consider implementing similar processes.
An analysis of Medicare claims data between 2003 and 2004 found that nearly 20% of the >11 million Medicare patients who had been discharged from a hospital were readmitted within 30 days, at a cost of $17.4 billion.1 Certain patient subgroups were especially worrisome. Of those with congestive heart failure, for example, 50% were typically readmitted within 6 months of initial hospitalization.2
A longstanding issue comes to the fore. Concerns about hospital readmissions appeared in the literature nearly 40 years ago.3 In the 1990s, with the advent of managed care, organizations began “case management” to reduce preventable readmissions using several approaches, including enhanced primary care access.4 A meta-analysis at that time demonstrated some reduction in hospital readmissions associated with hospital-based case management interventions.5 Though quality improvement programs and case management have been assumed to reduce hospital readmissions, some studies have actually found the opposite,6,7 or have yielded conflicting evidence.8-13 Skyrocketing costs of health care have brought hospital readmissions to the forefront of health system redesign efforts.14-16
Section 3025 of the Affordable Care Act added section 1886(q) to the Social Security Act establishing the Hospital Readmissions Reduction Program, which requires Centers for Medicare & Medicaid Services to reduce payments to hospitals with excess readmissions.17 This change was introduced on October 1, 2012 and has precipitated discussion across the country about the prevention of unnecessary hospital readmissions.18,19
Patient factors contributing to hospital readmissions. Concerns patients cite most frequently as contributors to relapse and readmission are 1) feeling unprepared for discharge; 2) difficulty performing activities of daily living; 3) trouble adhering to discharge medications; 4) difficulty accessing discharge medications; and 5) lack of social support.20 While multiple tools have been developed to better assess unplanned readmissions—including the Identification of Seniors at Risk, the Flemish version of the Triage Risk Screening Tool, and Variable Indicative of Placement risk—none of these have accurately predicted unplanned readmission in older, hospitalized patients.21 Predicting which patients will require readmission remains elusive,22 though some new models show promise.23 z
Targeted interventions that show promise. Postdischarge telephone follow-up has been shown to reduce hospital readmissions,24,25 and a direct correlation has been observed between the timing of the intervention and readmission rates, with interventions implemented closer to the date of discharge being associated with greater reductions in the number of readmissions.26 Additionally, multicomponent interventions with both pre- and postdischarge elements that specifically target high-risk populations appear to be more effective in reducing readmissions than single-component interventions.27
Hansen et al28 identified a number of predischarge, postdischarge, and bridging interventions that could potentially reduce hospital readmissions (TABLE 1). No single intervention implemented alone consistently reduced the risk for 30-day rehospitalization.28 One multicomponent intervention that has reduced readmissions for patients with heart failure or acute myocardial infarction is a transition coach, who visits patients in the hospital and sees them again in clinic for follow-up appointments. The coach also calls patients between face-to-face visits to review treatment plans and answer questions.29
The impetus for our study. The patient-centered medical home (PCMH) has been gaining traction as a mechanism to improve patient care while reducing health care spending.30,31 An intensive multidimensional medical home model introduced into 11 primary care practices proved capable of significantly reducing admissions and readmissions for Medicare Advantage members.32 Additionally, intelligently leveraging clinical information technology is likely to be critical in reducing readmissions.33 The purpose of our observational study was to examine the impact of a multicomponent intervention on 30-day hospital readmissions over 12 months.
METHODS
Study setting and preintervention practice routines in 2 patient groups
The study setting for Group 1 involved patients with assigned primary care providers (PCPs) in a university-based practice group at 4 outpatient clinics. The study setting for Group 2 included patients with assigned PCPs from county and community health centers, involving 12 primary care clinics in total. While the groups’ patient populations were distinguished for descriptive purposes, in practice the patients were admitted to the same inpatient treatment teams and university-based hospital in a metropolitan setting. For both groups, the primary care practices admitted patients to the hospital directly from clinic or through the emergency department (ED).
An admitting team from one of the inpatient services completed the admission, initiated treatment, and discharged patients. Preintervention, limited discharge case management occurred at the hospital, driven primarily by the treating team’s requests. The admitting team also attempted to schedule outpatient follow-up appointments with an available PCP at the patient’s primary clinic after discharge. Obstacles to successful appointment scheduling prior to discharge included but were not limited to discharges over weekends or holidays or after clinic hours. Additionally, for both groups, discharge summaries were sent to the PCP either electronically via the electronic medical record (EMR) or via system-generated automated fax.
Creating a culture of continuity in Group 1
Transformation of outpatient activities. We developed several important processes to transform the patient experience through hospitalization and discharge. Together, these processes created a “culture of continuity” to prevent avoidable readmissions. We introduced an innovative, systematic approach to notifying the clinic and primary care clinician about initial admission. We also gave notification immediately upon discharge, rather than waiting until after discharge, as had been occurring. This patient-centered change engaged the primary care team in the care of the patient while hospitalized and during discharge planning; it actively ensured that follow-up appointments occurred within 1 week after discharge. Prior to this intervention, there was no system for ensuring timely follow-up after hospital discharge. The new expectation for the ambulatory clinics was that clinic staff could “reach in” to the patient during the hospital stay and actively contact the patient before discharge to schedule a postdischarge appointment at the patient’s convenience.
The 4 practices had embraced and implemented the PCMH model, a core component of which is care coordination.34,35 Each clinic appointed a registered nurse (RN) to serve as a team-based care manager (CM) for patients being discharged from the hospital. Responsibilities included fielding calls or electronic communications from the inpatient team, developing a hospital follow-up workflow, developing a standardized list of questions to ask each patient after discharge, and calling patients to ensure a follow-up appointment was scheduled, ideally within 2 to 3 days and at least within 7 days of discharge. The CM prioritized scheduling follow-up appointments with the patient’s PCP to ensure the highest level of continuity.
In addition to patient-specific documents, CMs received electronic reports from inpatient teams (including from the ED, medical and surgical intensive care units, and surgery) listing all Group 1 patients discharged from the hospital. Reports were run daily and allowed the outpatient clinic staff and CMs to verify patients against previous lists of anticipated discharges, and to generate their own lists. The CMs would then make follow-up phone calls and ensure that appointments were scheduled for these patients.
Medical directors at the 4 clinics received monthly summary reports profiling clinical activities related to hospitalizations. A data team (led by author SF) created the reports, which initially focused on care delivered in ambulatory settings (and included the development of a “balanced scorecard” to assess quality of care, financial productivity, and operational efficiency36). The data team developed new reports specifically for hospital admissions, discharges, and readmissions, identifying:
• all patients admitted by inpatient team
• the number and percentage of patients who were readmitted within 30 days
• the number and percentage of patients who had received a follow-up phone call or electronic communication from the outpatient team
• the number of patients who had follow-up visits after discharge within 7 and 30 days
• the number of patients who had clinic visits prior to readmission
• all patients discharged from any service within the prior 24 hours.
These reports, which had patient drilldown capability, were forwarded to all providers and teams at each clinic by the medical director. Teams at each clinic were then charged with analyzing the readmissions, identifying high-risk patients, and improving the coordination of care for these patients, including the use of RN/clinician co-visits and proactive outreach from the team-based nurses and staff.
Transformation of inpatient activities. We reorganized inpatient teams to include clinician representatives from the clinics whose patients were being treated. This process ensured better continuity of experience and familiarity with the environment of care and discharge/follow-up processes for both patients and all providers.
Additionally, inpatient teams developed new workflows to ensure that all involved members of the outpatient team were well informed of the hospitalization process. On the first or second day of admission, a hospital follow-up document was electronically routed to the administrative support staff, the PCP team nurse, and the PCP (FIGURE 1). An integrated EMR created a link between the hospital and all ambulatory practices that allowed for real-time transmission of patient information. The document identified the timing of a follow-up appointment and requested a 48-hour phone call from the team nurse after hospital discharge. The inpatient team also included a concise summary of the hospitalization for the PCP, to aid in anticipating patient discharge and any impending needs. The document was retrievable and traceable in the EMR.
Study groups and statistical analysis
The Oregon Health & Science University’s Institutional Review Board (IRB#9768) determined this study was not human subjects research because the proposed activity did not meet the definition of human subject per 45 CFR 46.102(f). The board made this determination because our analysis file included only hospital readmission rates and no patient-level data.
Adult patients admitted by the inpatient teams consisted of 2 distinct populations: patients whose PCP practiced at one of the 4 outpatient clinics (Group 1 patients); and patients admitted from other, unaffiliated clinics (Group 2 patients). In contrast to the transformations in patient care described in Group 1, care provided to Group 2 patients was considered usual care, as there was no interface between outpatient and inpatient teams to revise operations. Patients in either group were excluded from analyses if they died during the hospitalization. Maternity patients were also excluded.
We identified the percentage of patients readmitted within 30 days of a hospital admission using administrative data sources, which underwent careful data checking and validation, and were sub-grouped according to whether the patients were in Group 1 or Group 2. We used group-specific and overall linear regression to examine the changes in percentage of readmission within 30 days of discharge in the 2 study groups over 12 months, including a model that specifically assessed the interaction between Group 1 readmission percentages and those in Group 2. We considered a P-value ≤.05 to be significant in this exploratory study.
RESULTS
Patient readmissions decreased significantly
Our analysis included 961 patients; 685 patients (71.3%) were in Group 1, and 276 (28.7%) were in Group 2 (Table 2). The distribution of patient gender and mean age was similar within groups for patients readmitted and not readmitted during the study period. Among patients readmitted, the mean hospital length of stay was 5.8 days and 7.1 days for Group 1 and Group 2, respectively. Among those not readmitted, the mean hospital length of stay was 4.3 and 4.9 in Group 1 and 2, respectively.
The percentage of patients readmitted per month ranged from 28.1% to 7.1% in Group 1 and 27.8% to 5.9% in Group 2 (Figure 2). Patient readmissions in Group 1 decreased significantly from 27% in May 2012 to 7.1% in April 2013 with an R2 of 0.43 (P=.02). Readmissions of patients in Group 2 were more variable; 26.1% in May 2012 and 25.9% in April 2013 with a non-significant R2 of 0.04 (P=.53). The regression model (unadjusted) that compared the interaction between Group 1 and Group 2 readmissions over the study period was significant, indicating a decrease in readmissions in Group 1 and no strong correlation between usual care and readmissions over time in Group 2 (P=.05).
DISCUSSION
Implementing intensive coordinated care management and transition processes in a group of primary care clinics appears to significantly decrease hospital readmissions for patients in Group 1, compared with those in Group 2 who received usual care. While it is possible that some of the ambulatory practices in Group 2 admitting patients to the inpatient services were using or developing care coordination programs including hospital follow-up, none of these providers or groups interfaced with the inpatient teams in this study. We are, therefore, confident that Group 2 providers were not undertaking any new or novel activities that reached in to hospital inpatient services to improve care coordination.
Our findings are consistent with the literature review conducted by Scott et al,27 which found that multicomponent interventions are more successful at reducing readmissions than single-component interventions. In our Group 1 clinics, we implemented 8 of the 12 predischarge, postdischarge, and bridging interventions identified by Hansen et al28 (medication reconciliation, discharge planning, scheduling of a follow-up appointment before discharge, follow-up telephone calls, timely communication with ambulatory providers, timely ambulatory provider follow-up, physician continuity across the inpatient and outpatient setting, and patient-centered discharge instructions).
Study strengths and weaknesses. The strengths of this study include means and quality of data capture for hospital readmission rates in the study setting. Limitations include the small sample sizes, which did not allow us to conduct a multivariable adjusted analysis that would have taken into account patient characteristics, seasons, and temporal correlations. These covariates might drive study findings in a way that results in us drawing inaccurate conclusions—the analysis we conducted (unadjusted) assumed that the events that occurred in each month were unrelated to what might have occurred in the prior month or subsequent month.
Patients in the 2 study groups did exhibit differences that could have contributed to our findings. For example, the average length of stay for Group 2 patients was longer by just over 1 day compared with that in Group 1. This may suggest Group 2 patients were sicker, and thus may have needed to be readmitted within 30 days of their discharge. We cannot know for certain that patients in Group 1 were less ill, as this would require a more discriminating study design. As with many studies, additional questions arise, but these serve to further a line of research that is vitally important.
Another factor that could have affected our findings is that Group 1 patient readmission rates started off higher than the Group 2 patients, so there is a chance that regression to the mean rather than changes in clinical care could have contributed to some of the decrease in Group 1 readmission rates. There are potential subject-level, provider-level, and clinic-level factors that could have been used to adjust for potential confounding. Future studies could address these factors. Longer study follow-up would provide an even better picture of the difference between the groups.
A multicomponent intervention works. Creating a culture of continuity is an important aspect of PCMH. Not all primary care clinics or PCMHs may have built-in relationships for inpatient care of their patients. We would argue that outpatient adoption of the enhanced “reaching in” and a multicomponent intervention would have a significant positive impact on patient care and improve the transition from in- to outpatient care, and likely reduce readmissions.
CORRESPONDENCE
Brett White, MD, 4411 SW Vermont St, Portland, OR 97219; brettwhitemd@gmail.com
The authors gratefully acknowledge the clinic and inpatient physicians and staffs as well as the Research Program in the Department of Family Medicine, Oregon Health & Science University.
1. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418-1428.
2. Zaya M, Phan A, Schwarz ER. The dilemma, causes and approaches to avoid recurrent hospital readmissions for patients with chronic heart failure. Heart Fail Rev. 2012;17:345-353.
3. Marriott PF, Grigor JM, Hiep A. Reducing hospital readmission rates among schizophrenics. Med J Aust. 1976;2:897-898.
4. Fitzgerald JF, Smith DM, Martin DK, et al. A case manager intervention to reduce readmissions. Arch Intern Med. 1994;154:1721-1729.
5. Kim YJ, Soeken KL. A meta-analysis of the effect of hospital-based case management on hospital length-of-stay and readmission. Nurs Res. 2005;54:255-264.
6. Weinberger M, Oddone EZ, Henderson WG. Does increased access to primary care reduce hospital readmissions? Veterans Affairs Cooperative Study Group on Primary Care and Hospital Readmission. N Engl J Med. 1996;334:1441-1447.
7. Mudge A, Denaro C, Scott I, et al. The paradox of readmission: effect of a quality improvement program in hospitalized patients with heart failure. J Hosp Med. 2010;5:148-153.
8. Mistiaen P, Francke AL, Poot E. Interventions aimed at reducing problems in adult patients discharged from hospital to home: a systematic meta-review. BMC Health Serv Res. 2007;7:47.
9. Linertová R, García-Pérez L, Vázquez-Díaz JR, et al. Interventions to reduce hospital readmissions in the elderly: in-hospital or home care. A systematic review. J Eval Clin Pract. 2011;17:1167-1175.
10. Shepperd S, Parkes J, McClaren J, et al. Discharge planning from hospital to home. Cochrane Database Syst Rev. 2004;(1):CD000313. Review. Update in: Cochrane Database Syst Rev. 2010;(1):CD000313.
11. Huntley AL, Thomas R, Mann M, et al. Is case management effective in reducing the risk of unplanned hospital admissions for older people? A systematic review and meta-analysis. Fam Pract. 2013;30:266-275.
12. Crocker JB, Crocker JT, Greenwald JL. Telephone follow-up as a primary care intervention for postdischarge outcomes improvement: a systematic review. Am J Med. 2012;125:915-921.
13. Mistiaen P, Poot E. Telephone follow-up, initiated by a hospital-based health professional, for postdischarge problems in patients discharged from hospital to home. Cochrane Database Syst Rev. 2006;(4):CD004510.
14. Jack B, Paasche-Orlow M, Mitchell S, et al. An overview of the Re-Engineered Discharge (RED) toolkit. AHRQ Publication No.12(13)-0084. Rockville, MD: Agency for Healthcare Research and Quality; March 2013. 15. Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff (Millwood). 2008;27:759-769.
16. Greenwald J, Denham C, Jack B. The hospital discharge: A review of a high risk care transition with highlights of a reengineered discharge process. J Patient Saf. 2007;3:97-106.
17. Centers for Medicare & Medicaid Services. Readmissions Reduction Program. Available at: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html. Accessed June 18, 2013.
18. Joynt KE, Jha AK. A path forward on Medicare readmissions. N Engl J Med. 2013;368:1175-1177.
19. Joynt KE, Jha AK. Characteristics of hospitals receiving penalties under the Hospital Readmissions Reduction Program. JAMA. 2013;309:342-343.
20. Kangovi S, Grande D, Meehan P, et al. Perceptions of readmitted patients on the transition from hospital to home. J Hosp Med. 2012;7:709-712.
21. Braes T, Moons P, Lipkens P, et al. Screening for risk of unplanned readmission in older patients admitted to hospital: predictive accuracy of three instruments. Aging Clin Exp Res. 2010;22:345-351.
22. Allaudeen N, Schnipper JL, Orav EJ, et al. Inability of providers to predict unplanned readmissions. J Gen Intern Med. 2011;26:771-776.
23. Gruneir A, Dhalla IA, van Walraven C, et al. Unplanned readmissions after hospital discharge among patients identified as being at high risk for readmission using a validated predictive algorithm. Open Med. 2011;5:e104-e111.
24. Harrison PL, Hara PA, Pope JE, et al. The impact of postdischarge telephonic follow-up on hospital readmissions. Popul Health Manag. 2011;14:27-32.
25. Herrera-Espiñeira C, Rodríguez del Águila Mdel M, Navarro Espigares JL, et al. [Effect of a telephone care program after hospital discharge from a trauma surgery unit]. Gac Sanit. 2011;25:133-138.
26. Costantino ME, Frey B, Hall B, et al. The influence of a postdischarge intervention on reducing hospital readmissions in a Medicare population. Popul Health Manag. 2013;16:310-316.
27. Scott IA. Preventing the rebound: improving care transition in hospital discharge processes. Aust Health Rev. 2010;34:445-451.
28. Hansen LO, Young RS, Hinami K, et al. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med. 2011;155:520-528.
29. Coaching helps cut readmissions. Hosp Case Manag. 2011;19:155-156.
30. DeVries A, Li CH, Sridhar G, et al. Impact of medical homes on quality, healthcare utilization, and costs. Am J Manag Care. 2012;18:534-544.
31. Paustian ML, Alexander JA, El Reda DK, et al. Partial and incremental PCMH practice transformation: implications for quality and costs. Health Serv Res. 2013 Jul 5. [Epub ahead of print].
32. Gilfillan RJ, Tomcavage J, Rosenthal MB, et al. Value and the medical home: effects of transformed primary care. Am J Manag Care. 2010;16:607-614.
33. Haglund M. Mastering readmissions: laying the foundation for change. Post-healthcare reform, pioneers are laying the foundation for serious readmissions-reduction work. Healthc Inform. 2011;28:10-13,16.
34. Meyers D, Peikes D, Genevro J, et al. The roles of patient-centered medical homes and accountable care organizations in coordinating patient care. AHRQ Publication No. 11-M005-EF. Rockville, MD: Agency for Healthcare Research and Quality; December 2010.
35. Ferrante JM, Balasubramanian BA, Hudson SV, et al. Principles of the patient-centered medical home and preventive services delivery. Ann Fam Med. 2010;8:108-116.
36. Fields SA, Cohen D. Performance enhancement using a balanced scorecard in a patient-centered medical home. Fam Med. 2011;43:735-739.
1. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418-1428.
2. Zaya M, Phan A, Schwarz ER. The dilemma, causes and approaches to avoid recurrent hospital readmissions for patients with chronic heart failure. Heart Fail Rev. 2012;17:345-353.
3. Marriott PF, Grigor JM, Hiep A. Reducing hospital readmission rates among schizophrenics. Med J Aust. 1976;2:897-898.
4. Fitzgerald JF, Smith DM, Martin DK, et al. A case manager intervention to reduce readmissions. Arch Intern Med. 1994;154:1721-1729.
5. Kim YJ, Soeken KL. A meta-analysis of the effect of hospital-based case management on hospital length-of-stay and readmission. Nurs Res. 2005;54:255-264.
6. Weinberger M, Oddone EZ, Henderson WG. Does increased access to primary care reduce hospital readmissions? Veterans Affairs Cooperative Study Group on Primary Care and Hospital Readmission. N Engl J Med. 1996;334:1441-1447.
7. Mudge A, Denaro C, Scott I, et al. The paradox of readmission: effect of a quality improvement program in hospitalized patients with heart failure. J Hosp Med. 2010;5:148-153.
8. Mistiaen P, Francke AL, Poot E. Interventions aimed at reducing problems in adult patients discharged from hospital to home: a systematic meta-review. BMC Health Serv Res. 2007;7:47.
9. Linertová R, García-Pérez L, Vázquez-Díaz JR, et al. Interventions to reduce hospital readmissions in the elderly: in-hospital or home care. A systematic review. J Eval Clin Pract. 2011;17:1167-1175.
10. Shepperd S, Parkes J, McClaren J, et al. Discharge planning from hospital to home. Cochrane Database Syst Rev. 2004;(1):CD000313. Review. Update in: Cochrane Database Syst Rev. 2010;(1):CD000313.
11. Huntley AL, Thomas R, Mann M, et al. Is case management effective in reducing the risk of unplanned hospital admissions for older people? A systematic review and meta-analysis. Fam Pract. 2013;30:266-275.
12. Crocker JB, Crocker JT, Greenwald JL. Telephone follow-up as a primary care intervention for postdischarge outcomes improvement: a systematic review. Am J Med. 2012;125:915-921.
13. Mistiaen P, Poot E. Telephone follow-up, initiated by a hospital-based health professional, for postdischarge problems in patients discharged from hospital to home. Cochrane Database Syst Rev. 2006;(4):CD004510.
14. Jack B, Paasche-Orlow M, Mitchell S, et al. An overview of the Re-Engineered Discharge (RED) toolkit. AHRQ Publication No.12(13)-0084. Rockville, MD: Agency for Healthcare Research and Quality; March 2013. 15. Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff (Millwood). 2008;27:759-769.
16. Greenwald J, Denham C, Jack B. The hospital discharge: A review of a high risk care transition with highlights of a reengineered discharge process. J Patient Saf. 2007;3:97-106.
17. Centers for Medicare & Medicaid Services. Readmissions Reduction Program. Available at: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html. Accessed June 18, 2013.
18. Joynt KE, Jha AK. A path forward on Medicare readmissions. N Engl J Med. 2013;368:1175-1177.
19. Joynt KE, Jha AK. Characteristics of hospitals receiving penalties under the Hospital Readmissions Reduction Program. JAMA. 2013;309:342-343.
20. Kangovi S, Grande D, Meehan P, et al. Perceptions of readmitted patients on the transition from hospital to home. J Hosp Med. 2012;7:709-712.
21. Braes T, Moons P, Lipkens P, et al. Screening for risk of unplanned readmission in older patients admitted to hospital: predictive accuracy of three instruments. Aging Clin Exp Res. 2010;22:345-351.
22. Allaudeen N, Schnipper JL, Orav EJ, et al. Inability of providers to predict unplanned readmissions. J Gen Intern Med. 2011;26:771-776.
23. Gruneir A, Dhalla IA, van Walraven C, et al. Unplanned readmissions after hospital discharge among patients identified as being at high risk for readmission using a validated predictive algorithm. Open Med. 2011;5:e104-e111.
24. Harrison PL, Hara PA, Pope JE, et al. The impact of postdischarge telephonic follow-up on hospital readmissions. Popul Health Manag. 2011;14:27-32.
25. Herrera-Espiñeira C, Rodríguez del Águila Mdel M, Navarro Espigares JL, et al. [Effect of a telephone care program after hospital discharge from a trauma surgery unit]. Gac Sanit. 2011;25:133-138.
26. Costantino ME, Frey B, Hall B, et al. The influence of a postdischarge intervention on reducing hospital readmissions in a Medicare population. Popul Health Manag. 2013;16:310-316.
27. Scott IA. Preventing the rebound: improving care transition in hospital discharge processes. Aust Health Rev. 2010;34:445-451.
28. Hansen LO, Young RS, Hinami K, et al. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med. 2011;155:520-528.
29. Coaching helps cut readmissions. Hosp Case Manag. 2011;19:155-156.
30. DeVries A, Li CH, Sridhar G, et al. Impact of medical homes on quality, healthcare utilization, and costs. Am J Manag Care. 2012;18:534-544.
31. Paustian ML, Alexander JA, El Reda DK, et al. Partial and incremental PCMH practice transformation: implications for quality and costs. Health Serv Res. 2013 Jul 5. [Epub ahead of print].
32. Gilfillan RJ, Tomcavage J, Rosenthal MB, et al. Value and the medical home: effects of transformed primary care. Am J Manag Care. 2010;16:607-614.
33. Haglund M. Mastering readmissions: laying the foundation for change. Post-healthcare reform, pioneers are laying the foundation for serious readmissions-reduction work. Healthc Inform. 2011;28:10-13,16.
34. Meyers D, Peikes D, Genevro J, et al. The roles of patient-centered medical homes and accountable care organizations in coordinating patient care. AHRQ Publication No. 11-M005-EF. Rockville, MD: Agency for Healthcare Research and Quality; December 2010.
35. Ferrante JM, Balasubramanian BA, Hudson SV, et al. Principles of the patient-centered medical home and preventive services delivery. Ann Fam Med. 2010;8:108-116.
36. Fields SA, Cohen D. Performance enhancement using a balanced scorecard in a patient-centered medical home. Fam Med. 2011;43:735-739.