User login
Guide to Recognizing and Treating Sleep Disturbances in the Nursing Home
From the School of Aging Studies, University of South Florida, Tampa, FL (Dr. AA Gamaldo) and the Department of Neurology, Johns Hopkins Medicine, Baltimore, MD (Drs. Sloane, CE Gamaldo and Salas).
Abstract
- Objective: To provide guidance on identifying and treating sleep disturbances commonly encountered in older nursing home residents.
- Methods: Review of the literature in the context of 5 clinical cases.
- Results: Sleep disturbances continue to be a growing global epidemic, and public health initiatives have been aimed at improving sleep health across all ages. In older adults, sleep disturbances are often associated with the development and/or worsening of health conditions. Common sleep disturbances observed in older nursing home residents include obstructive sleep apnea, restless legs syndrome/Willis-Ekbom disease, circadian rhythm sleep-wake disorders, insomnia, and parasomnias. The symptoms and recommended treatment plans vary across the sleep disturbances. For many sleep disturbances, modification of residents’ daily activities and/or nursing home environment can be helpful.
- Conclusion: As the number of people residing in nursing homes increases, it is important for health care providers to be knowledgable about sleep disturbances in this population.
By 2030, almost 20% of the US population (approximately 72.1 million people) will be age 65 and older [1]. As many as 63% of older adults in the general population report sleep disturbances [2]. Specifically, older adults demonstrate difficulty with decreased total sleep duration, an increase in sleep fragmentation (ie, interruptions in nighttime sleep), and reduced total sleep time spent in rapid eye movement (REM) and slow wave sleep [3–5]. Poor sleep, either because of not getting enough sleep or having an undiagnosed and thus untreated sleep disorder, is associated with physical illness, impaired cognition, poor physical function, and mortality risk [6,7]. In fact, over 50% of individuals older than 65 years meet the diagnostic criteria for a sleep disorder, many of which are undiagnosed [6,7].
It is forecasted that we will see substantial increases in the rate of nursing home residence among the elderly [8]. The prevalence and severity of disturbed sleep is reportedly higher in NH residents [6,7]. Generally, NH residents tend to be on several medications for various medical disorders that may negatively impact sleep [7]. Reciprocally, sleep disruption may put NH residents at an increased risk for behavioral issues (eg, agitation) [9,10] as well as developing and/or exacerbating health conditions (eg, mood disorders, dementia, cardiovascular disease) [8]. Furthermore, NH residents exhibiting disturbed sleep, behavioral issues, and/or mood disorders are at an increased risk for being prescribed antipsychotic drugs [11], which are associated with adverse side effects and poorer quality of life [12]. Thus, the identification and management of sleep disturbances in the NH setting has become progressively more vital in efforts to optimize medical management of this population. This review identifies common sleep disturbances frequently underdiagnosed and undertreated among residents of NH facilities.
Case 1
A 73-year-old woman with a history of type 2 diabetes mellitus reports poor sleep quality with frequent awakenings during the night and excessive daytime sleepiness. She states that she can fall asleep within 5 minutes, but often is awoken throughout the night with a sensation of breathlessness. She has snored for many years, but the nursing staff at her NH facility has recently commented that her snoring has gone from intermittent to constant. She cannot remember the last time she has had restful sleep. She consumes 3 to 4 cups of caffeinated beverages daily to counter her sleepiness. She denies smoking or illicit drug or alcohol use. Her review of systems was notable for a 30-lb weight gain over the last year, and she reports increasing fatigue, irritability, and memory and concentration issues. Her current medication list includes metformin and amlodipine. Her examination is remarkable for a BMI of 31, large neck circumference (> 16), tonsillar enlargement, a crowded oropharynx, micrognathia, lungs clear to auscultation bilaterally, heart sounds of normal S1 and S2, and legs with trace pitting edema.
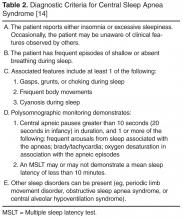
Case 1 Reflection: Sleep-Disordered Breathing
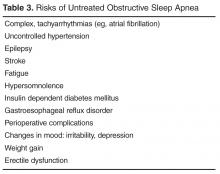
Although previous studies have observed high rates (60%–90%) of SDB in NH settings [16,17], one study observed that only 0.5% of nursing home residents carried a diagnosis with SDB, suggesting that SDB is being grossly underappreciated amongst NH residents over the age of 65 [18]. In order to evaluate for SBD, routine annual physical exams or medical chart reviews can elicit the risk factors for sleep apnea (eg, obesity [per BMI], male sex, postmenopausal women, family history of sleep apnea) as well as common comorbidities (eg, hypertension, coronary artery disease, and diabetes). Formal evaluation consists of a sleep evaluation with a sleep specialist and polysomnography (PSG; sleep study) that can be performed in the sleep center or at home depending on the patient’s history and other medical issues.
Case 1 Outcome
Case 2
An 85-year-old man with history of Alzheimer’s disease, major depression and arthritis, reports insomnia and “tingling in my legs” at bedtime. The patient cannot identify when the symptoms started but reports that his legs often jerk during sleep. He consumes a cup of coffee daily and has a previous 20 pack-year smoking history (he quit 40 years ago). On review of systems, he endorses fatigue. His current medication list includes fluoxetine, donepezil hydrochloride, ibuprofen as needed for arthritic pain, and a multivitamin. His examination was unremarkable, with a BMI of 26, neck circumference < 16, no tonsillar enlargement, normal (noncrowded) oropharynx, lungs clear to auscultation bilaterally, heart sounds demonstrating a normal S1 and S2, and legs without edema.
Case 2 Reflection: Restless Legs Syndrome/Willis-Ekbom Disease
Restless legs syndrome (RLS) also known as Willis-Ekbom disease, affects approximately 10 million adults in the United States alone [22]. RLS is a sensorimotor disorder that must satisfy the following 5 primary diagnostic criteria: (1) urge to move the legs with or without dysesthesias; (2) onset or exacerbation with rest or inactivity; (3) relief with movement; (4) symptoms are worse in the evening or at night (circadian component); (5) symptoms cannot be solely accounted for as consequence of another medical or behavioral condition. Other supporting clinical features can alert a clinician to the likelihood of a RLS diagnosis; these include positive family history, response to dopaminergic therapy, lack of profound daytime sleepiness, and presence of periodic limb movements during sleep (PLMS) [23–26]. In younger individuals, the symptoms present insidiously whereas older adults (> 50 years of age) will usually present with sudden onset [27].
Not only do patients lack the restorative sleep needed to ward off fatigue and restfulness, but patients also demonstrate higher rates of comorbidities (eg, anxiety, hypertension, depression) as well as large economic burden secondary to absenteeism and decreased on-the-job effectiveness [28,29]. As a results, patients with RLS experience significant reductions in quality of life related to this sensorimotor disorder [28].
No confirmatory laboratory test exists to diagnose RLS; however, patients suspected of having RLS should be evaluated with a basic metabolic panel, iron studies, and a thorough neurologic examination, as iron deficiency, kidney failure, uremia and peripheral neuropathy can lead to secondary RLS [30,31]. Evidence shows that RLS is common in NH residents [32] and may account for problematic behaviors, such as late night pacing [7]. Forty-five percent of community dwelling individuals over 65 years old exhibit a PLMS index (leg kicks per hour) of greater than 5 [33]. PLMS, while not a disorder in and of itself, can serve as a marker for potential disease. PLMS are characterized by intermittent episodes of stereotyped leg movements. PLMS typically do not awaken the patient from sleep and therefore do not contribute to insomnia or daytime sleepiness, representing a key clinical difference from RLS. It is important to note that PLMS are nonspecific and may be common in older adults that do not meet the diagnostic criteria for RLS.
Treatment of RLS is based on the frequency of symptoms and the level of functional impairment caused by the syndrome. RLS treatment recommendations should always espouse nonpharmacological interventions that include improving sleep practices, engagement in daily physical activity, targeted placement of sedentary activity in the morning when symptoms are less prominent, and concerted efforts to avoid the use of RLS-exacerbating medications (eg, selective serotonin reuptake inhibitor (SSRIs), neuroleptic agents, antihistamines) [28]. If there is an underlying condition contributing to RLS, such as metabolic disturbance or iron deficiency, then these conditions should be corrected before initiating RLS medications. Several medications are FDA-approved for treatment of RLS, including dopamine agonists (eg, ropinirole, rotigotine, pramipexole), dopamine precursor (eg, levodopa), glutamate-related (eg, gabapentin), benzodiazepines (eg, temazepam, clonazepam). Augmentation, the worsening of RLS symptoms, can occur in patients taking dopamine agonists. If this occurs, dopamine agents should be discontinued or switched to other agents (such as a long-acting dopamine agonist, gabapentin encarbil, as well as non-FDA approved therapies such as opioids). However, it is important to note that weaning off dopamine agents may result in mild but in most cases moderate and/or severe withdrawal from the medication, so counseling and close monitoring should be done.
Case 2 Outcome
Given the patient’s history of dementia, opioids, benzodiazepines and other delirium-inducing medications should be avoided. His antidepressive regimen, fluoxetine, should be re-evaluated as these medications have been associated with RLS exacerbation. In addition to SSRIs, medications associated with RLS are MAO inhibitors (selegeline, phenelzine), antipsychotics (risperdone, olanzapine), tricyclic antidepressants (mirtazapine), antihistamines (diphenhydramine, cimetidine), calcium channel blockers (verapamil, nifedipine, diltiazem), and phenytoin [34,35]. His treatment began with behavioral, nonpharmacological management, and blood testing for iron studies. His low iron level prompted initiation of oral supplementation, and he was asked to follow up in 3 months for reevaluation and possible initiation of low-dose dopamine agonists.
Case 3
A 73-year-old man with dementia is found to have very irregular sleep wake patterns with a variable bedtime and awakening time, often missing breakfast. He is found dozing off often during the day, particularly during times of inactivity. He has frequent awakenings during the night often calling for the staff to guide him back to bed. He has had some falls secondary to walking around his room. He has been prescribed various hypnotics without much benefit and instead, has suffered from some confusion while on these medications. His room is very dark and has no windows.
Case 3 Reflection: Circadian Rhythm Sleep-Wake Disorders
Circadian rhythm sleep-wake disorders (CRSWDs) are characterized by an individual’s natural propensity to want to go to sleep and be awake during a period that is undesirable personally and/or socially [36]. CRSWDs can be a result of the desynchronization of the 2 sleep processes: (1) homeostatic drive (regulates sleep intensity) and (2) circadian rhythm (maintains daytime alertness); [36]. CRSWDs can also be due to an individual’s naturally occurring sleep drives becoming misaligned with their social/personal sleep-wake demands (eg, employment schedule and socializing opportunities with family/friends). With increasing age, the circadian rhythm becomes less adept at functioning in a desynchronized pattern [7], which can result in daytime sleepiness and night time sleep fragmentation [7,37]. CRSWDs are highly prevalent in individuals with dementia [7,36]. As dementia progresses, the ability to maintain a balance of the 2 sleep process becomes more impaired [7]. As a result, individuals with dementia, particularly Alzheimer’s disease, are likely to experience agitation, irritability, and/or confusion during the evening and night, a behavioral problem referred to as “sundowning” [38].
There are several types of CRSWDs, including delayed sleep-phase syndrome, advanced sleep-phase syndrome, irregular sleep-wake disorder, non–24-hour sleep-wake disorder, shift work sleep disorder, and jet lag sleep disorder. However, the most common type of CRSWDs observed in older adults is advanced sleep-phase syndrome [39]. Due to excessive sleepiness in the early evening, affected individuals may report a need to shift to earlier and earlier bedtimes (~6 to 7 pm) and wake times (~3 to 4 am) [36]. For older affected adults, this can cause distress and frustration, particularly if their sleep phase prevents them from participating in evening activities (eg, socializing with family/friends) [36].
In the assessment of patients with suspected CRSWDs, sleep diaries (self-reported or caregiver) daily account of sleep and wake times over at least 1 week) and actigraphy (wrist-worn accelerometer designed to measure activity and inactivity at night) can be used, particularly in older adults with dementia [40,41].
CRSWD treatment may include behavioral modifications and/or pharmacological intervention. Behavioral modifications can consist of chronotherapy, relaxation training, and/or bright light therapy. Chronotherapy involves making gradual shifts in an individual’s sleep time to meet his/her desired sleep schedule. Relaxation training involves implementing behaviors/activities that reduce tension and enhance the smooth transition into sleep. Bright light therapy involves exposure to an appropriate intensity and duration of light, which is an important environmental cue to help the synchrony of the sleep-wake cycle [7]. Previous studies have observed that NH residents are exposed to a restricted amount of bright light during the daytime [42,43], but higher levels of artificial light at night (eg, hallway lighting) [7]. NH residents’ exposure to artificial bright light during the daytime has not only improved the residents’ sleep [44–46], but also has improved their cognitive functioning and reduced their depressive symptoms [47]. Thus, steps towards targeted light exposure in sync with the typical sleep-wake cycle (eg, mandated time in well-lit rooms during the day and during meals) for NH residents, particularly those with CRSWDs, could prove to be beneficial across several social, behavioral and neurocognitive domains. Lastly, NH residents exposed to at least 30 minutes of outdoor daylight and at least 3 occasions of low intensity physical activities for 10 to 15 minutes daily can potentially improve sleep-wake patterns [48]. Thus, it may be beneficial to have an intervention that couples bright light exposure and physical activity in the NH setting.
Pharmacological interventions can also be implemented to improve older residents’ symptoms. However, the medications prescribed should be used with caution and should not be used as part of a long-term treatment plan. Melatonin is a commonly used herbal supplement that can assist advancing the timing of the circadian rhythms in the evening but can delay the circadian rhythms in the morning [49]. Several brands of this herbal supplement can be purchased over-the-counter and are not regulated by the FDA. Since the amount of melatonin used in the herbal supplement varies by brand, caution should be used when selecting a brand [50]. Two FDA-approved drugs (modafinil and armodafinil) are currently being used to reduce daytime sleepiness and improve vigilance amongst adults, but limited research has explored the effectiveness of these medication for older adults specifically suffering with CRSWDS [36,51,52]. Other stimulants (eg, caffeine, amphetamines, and nonamphetamine-derived medications) are also currently being used to reduce daytime sleepiness in patients with CRSWDS. Stimulant use, particularly caffeine consumption, has also been associated with better cognitive functioning in older adults [53]. However, stimulants should be taken with caution, particularly in older adults, because stimulant use has been associated with potentially serious and fatal health sequalae (eg, tachycardia, heart failure, irreversible heart damage and hypertension) [36,54].
Case 3 Outcome
The patient was moved to a room with a window. An alarm clock was set for 7:30 in the morning and he was taken to breakfast, where he sat at a table near a window. Any time he appeared to be sleepy, he was encouraged to go for a walk or engage in other activities so daytime napping opportunities were limited. His environment was assessed for safety and bedrails were utilized to prevent falls.
Case 4
A 75-year-old woman with a history of anxiety and depression moved into the NH 4 months ago after suffering a stroke. She now reports difficulty falling asleep for many years, which has significantly worsened since moving to the NH. Currently, she has been getting only 3 to 4 hour of sleep per night. She reports mild but increasing daytime sleepiness and does not fall asleep until 1:00 am despite getting into bed at 10:30 pm. She occasionally reports arthritic pain that interferes with her sleep. The NH staff has mentioned that she will occasionally cry for her family when she appears to be asleep.
Case 4 Reflection: Insomnia
According to the International Classification of Sleep Disorders (ICSD-3) [39], insomnia is characterized as “a repeated difficulty with sleep initiation, duration, consolidation, or quality that occurs despite adequate opportunity and circumstances for sleep, and results in some form of daytime impairment.” Among the sleep disorders, insomnia is one of the most common sleep issues observed in sleep clinics [34]. Older adults with insomnia often have comorbid physical (eg, pulmonary disease, arthritis, chronic pain, cancer diabetes, Parkinson’s disease) and mental illness (eg, depression, panic disorder) [55]. Medications (eg, stimulants, respiratory medications, chemotherapy, decongestants, hormones, or psychotropics) may cause and exacerbate insomnia symptoms [55].
Since insomnia is a clinical diagnosis, there is no specific diagnostic tool or gold standard test to identify individuals suffering with insomnia. Insomnia screening usually involves a clinical interview, in which a health provider, preferably trained in sleep, conducts a physical examination and collects an in-depth history of a patients’ sleep problems [56]. Insomnia screening tools may also include having a patient complete a sleep diary or questionnaire, such as the insomnia severity index (ISI) [57] or Pittsburgh Sleep Quality Index (PSQI) [58].
Cognitive behavioral therapy for insomnia (CBT-I) and/or pharmacological intervention are typically used to treat insomnia in older adults. CBT-I is a combination of cognitive (eg, changing dysfunctional sleep attitudes/beliefs) and behavioral treatment (eg, adhering to a regular sleep schedule) [59]. CBT-I or a combination of CBT-I and pharmacological intervention is recommended as more effective long-term approach to insomnia treatment compared to pharmacological intervention alone [55]. CBT-I involves altering older adults’ misconceptions of their sleep and implementing behavioral techniques to their everyday life (eg, routine sleep-wake schedule, relaxation therapy). Several FDA-approved medications are available to treat insomnia; however, many commonly used medications to treat insomnia in older adults (ie, antihistamines, antidepressants, anticonvulsants, and anti-psychotics) pose more risks than benefits to their health and well-being [35,60–62]. Some of the more recent hypnotics (egm zolpidem, exzopiclone, and ramelteon) on the market have been shown to be safer and more effective pharmacological options [55]. In 2014, the FDA approved the first in class orexin receptor antagonist medication (suvorexant) to treat insomnia [63]. Unlike other medications to treat insomnia, suvorexant, via the blockade of the orexin neurotransmitter, effectively inhibits orexin (one of neurotransmitters involved in the activation pathways of the arousal system), so sleep can easily be induced and maintained [64, 65]. Furthermore, preliminary studies suggest that this medication may be associated with less severe side effects (ie, habituation) than the other approved medications on the market [64, 65]. In fact, in a recent clinical series that included both young and older insomnia patients, the most common adverse reaction to suvorexant was drowsiness [66].
Case 4 Outcome
The patient was initiated on basic CBT-I therapy strategies which included stimulus control therapy [67]; implementation of a consistent bedtime and awakening routine; reducing the use of TV, smart phone, or other electronic leisure devices 1 hour before bedtime; refraining from caffeine after lunchtime; improving the sleep environment; and relaxation techniques.
Case 5
The patient is a 65-year-old man diagnosed with Parkinson’s disease several years ago. Recently, he has often has been experiencing what appears to be very violent and terrifying dreams. While asleep, he often screams and shouts for help. In addition, he occasionally will punch, kick, and/or thrash around in bed at night, which the NH staff has noted as a concern for his safety.
Case 5 Reflection: Parasomnias
Parasomnias represent frequent arousals during sleep or in the wake-to-sleep transition due to abnormal motor movements, behaviors (eg, shouting, flailing, and leaping from bed) and/or sensory experiences (eg, “dreamlike” hallucinations) [68]. Motor movements that occur for parasomnia can be disruptive for the individual and potentially dangerous for the individual and/or bed partner. There are 3 primary types of parasomnias based on the stage of sleep that the event occurs: non-REM (NREM), REM, and other parasomnias during transitions of sleep [68]. The most commonly observed parasomnia seen in older adults is the REM-associated parasomnia or REM sleep behavior disorder (RBD), which is characterized by experiencing vivid, sometimes violent, dreams typically involving fighting an intruder or an animal to protect a loved one [69]. For RBD, disruptive behaviors typically occur during REM sleep [69]. RBD has been associated with neurodegenerative disorders (Parkinson’s disease and Lewy body disease), neurologic disorders (eg, brain tumors and stroke), other primary disorders (narcolepsy and periodic limb movement disorder), and well as some medications (eg, antidepressants and β-blockers) [68]. There is limited knowledge on the prevalence of parasomnias in NH settings. One study, however, reported that 31% of older NH residents experience parasomnias [70]. Evaluation for parasomnias generally involve a clinical evaluation by a sleep specialist and overnight sleep study (ie, polysomnography at a sleep center if there is a concern for sleep apnea or RBD [71].
Medications are not typically first-line for parasomnia. Instead education about improving sleep practices, addressing other underlying sleep disorders, and securing a safe sleep environment are first recommended. Pharmacologic treatment, particularly the use of clonazepam, is commonly used to treat RBD [72]. However, this medication should be used with caution for older adults with a dementia diagnosis, gait disorders, and OSA because the common side effects include sedation, confusion, memory dysfunction, and early morning motor incoordination [68]. Several alternative medications have also been used to treat RBD. For example, medications commonly used to Parkinson disease symptoms, such Levodopa and dopamine agonists, have also been used to treat RBD [73]. Zopiclone, a nonbenzodiazepine hypnotic agent, has also been shown to be as effective as clonazepam, but with less potential side effects [74]. Melatonin, a nutritional supplement, has also been used as a treatment and appears to alleviate some of the RBD symptoms and has fewer side effects [68]. Since melatonin is not regulated by the FDA, it has been suggested that this treatment be used with caution in the older population [73].
Case 5 Outcome
The patient was evaluated with video synchronized in lab PSG. It confirmed REM sleep without evidence of the normal atonia that should be apparent during REM. These PSG findings in combination with repeated accounts of dream enactment established the diagnosis of RBD. Patient was treated with low-dose clonazepam and closely monitored for potential side effects of daytime sedation. Bedroom environment was also carefully reconfigured for safety to avoid potential risk of injury during a dream enactment episode.
Conclusion
Sleep disturbances remain an underappreciated and undertreated health issue in NH residents. Nursing homes can help facilitate optimal sleep health and day functioning by providing mandatory natural light outlets, physical exercise opportunities, and minimal allowable time residents can spend in their bed/bedroom outside of their routine sleep period. Educating NH providers and staff on sleep medicine may benefit residents, but workload and restricted resources may hinder this. Education via mobile and internet based educational platforms and resources (Mysleep101) may be helpful in addressing education barriers [75]. Convenient and cost-effective methods to deliver sleep medicine education to NH health care providers should be part of our ongoing efforts to improve the viability, vitality and quality of life of our aging citizens.
Corresponding author: Alyssa Gamaldo, PhD, Univ. of South Florida, 13301 Bruce B. Downs Blvd, MHC 1340, Tampa, FL 33612, agamaldo@usf.edu.
Financial disclosures: None.
1. Federal Interagency Forum on Aging-Related Statistics. Older Americans 2012: Key indicators of well-being. Washington, DC: U.S. Gov. Printing Office; 2012.
2. Almeida OP, Pfaff JJ. Sleep complaints among older general practice patients: association with depression. Br J Gen Pract 2005;55:864–866.
3. Wolkove N, Elkholy O, Baltzan M, et al. Sleep and aging: 1. Sleep disorders commonly found in older people. CMAJ 2007;176:1299–304.
4. Pace-Schott EF, Spencer RM. Age-related changes in the cognitive function of sleep. Prog Brain Res 2011;191:75–89.
5. Ohayon MM, Carskadon MA, Guilleminault C, et al. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep 2004;27:1255–73.
6. Jacobs D, Ancoli-Israel S, Parker L, et al. Twenty-four-hour sleep-wake patterns in a nursing home population. Psychol Aging 1989;4:352–6.
7. Neikrug AB, Ancoli-Israel S. Sleep disturbances in nursing homes. J Nutr Health Aging 2010;14:207–11.
8. Lakdawalla D, Goldman DP, Bhattacharya J, et al. Forecasting the nursing home population. Medical Care 2003;41:8-20.
9. Alessi CA, Yoon EJ, Schnelle JF, et al. A randomized trial of a combined physical activity and environmental intervention in nursing home residents: do sleep and agitation improve? J Am Geriatr Soc 1999;47:784–91.
10. Cohen-Mansfield J, Marx MS. The relationship between sleep disturbances and agitation in a nursing home. J Aging Health 1990;2:153–65.
11. Rolland Y, Andrieu S, Crochard A, et al. Psychotropic drug consumption at admission and discharge of nursing home residents. J Am Med Dir Assoc 2012;13:407 e407–412.
12. Salzman C. Antipsychotics in nursing homes. J Clin Psychopharmacol 2013;33:1–2.
13. Fleetham J, Ayas N, Bradley D, et al. Canadian Thoracic Society guidelines: diagnosis and treatment of sleep disordered breathing in adults. Can Respir J 2006;13:387–92.
14. International classification of sleep disorders: Chicago: American Academy of Sleep Medicine; 2005.
15. Gay PC. Complex sleep apnea: it really is a disease. J Clin Sleep Med 2008;4:403–5.
16. Ancoli-Israel S. Epidemiology of sleep disorders. In: Roth T, Roehrs TA, editors. Clinics in geriatric medicine. Philadelphia: WB Saunders; 1989:347–62.
17. Gehrman PR, Martin JL, Shochat T, et al. Sleep-disordered breathing and agitation in institutionalized adults with Alzheimer disease. Am J Geriatr Psychiatry 2003;11:426–33.
18. Resnick HE, Phillips B. Documentation of sleep apnea in nursing homes: United States 2004. J Am Med Dir Assoc 2008;9:260–4.
19. Park JG, Ramar K, Olson EJ. Updates on definition, consequences, and management of obstructive sleep apnea. Mayo Clin Proc 2011;86:549–54.
20. Yaggi HK, Concato J, Kernan WN, et al. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med 2005;353:2034–41.
21. McMillan A, Bratton DJ, Faria R, et al. Continuous positive airway pressure in older people with obstructive sleep apnoea syndrome (PREDICT): a 12-month, multicentre, randomised trial. Lancet Resp med 2014;2:804–12.
22. Allen RP, Walters AS, Montplaisir J, et al. Restless legs syndrome prevalence and impact: REST general population study. Arch Intern Med 2005;165:1286–92.
23. Allen RP, La Buda MC, Becker P, et al. Family history study of the restless legs syndrome. Sleep Med 2002;3 Suppl:S3–7.
24. Allen RP. Restless legs syndrome/Willis Ekbom disease: evaluation and treatment. Int Rev Psychiatry 2014;26:248–62.
25. Hening WA, Allen RP, Earley CJ, et al. An update on the dopaminergic treatment of restless legs syndrome and periodic limb movement disorder. Sleep 2004;27:560–83.
26. Gamaldo C, Benbrook AR, Allen RP, et al. Evaluating daytime alertness in individuals with Restless Legs Syndrome (RLS) compared to sleep restricted controls. Sleep Med 2009;10:134–8.
27. Allen RP, Earley CJ. Defining the phenotype of the restless legs syndrome (RLS) using age-of-symptom-onset. Sleep Med 2000;1:11–9.
28. Salas RE, Kwan AB. The real burden of restless legs syndrome: clinical and economic outcomes. Am J Manag Care 2012;18(9 Suppl):S207–212.
29. Silber MH, Ehrenberg BL, Allen RP, et al. An algorithm for the management of restless legs syndrome. Mayo Clin Proc 2004;79:916–22.
30. Hattan E, Chalk C, Postuma RB. Is there a higher risk of restless legs syndrome in peripheral neuropathy? Neurology 2009;72:955–60.
31. Winkelman JW, Chertow GM, Lazarus JM. Restless legs syndrome in end-stage renal disease. Am J Kidney Dis 1996;28:372–8.
32. Hornyak M, Trenkwalder C. Restless legs syndrome and periodic limb movement disorder in the elderly. J Psychosom Res 2004;56:543–8.
33. Ancoli-Israel S, Kripke DF, Klauber MR, et al. Periodic limb movements in sleep in community-dwelling elderly. Sleep 1991;14:496–500.
34. Ahmed QA. Effects of common medications used for sleep disorders. Crit Care Clin 2008;24:493–515, vi.
35. Rye DB, Trotti LM. Restless legs syndrome and periodic leg movements of sleep. Neurol clin 2012;30:1137–66.
36. Gamaldo CE, Chung Y, Kang YM, et al. Tick-tock-tick-tock: the impact of circadian rhythm disorders on cardiovascular health and wellness. J Am Soc Hypertens 2014;8:921–9.
37. Myers BL, Badia P. Changes in circadian rhythms and sleep quality with aging: mechanisms and interventions. Neurosci Biobehav Rev 1995;19:553–71.
38. National Institute on Aging. Alzheimer’s caregiving tips: sundowning. June 2013.
39. International classification of sleep disorders. 3rd ed. Darien, IL: AASD; 2014.
40. Barion A, Zee PC. A clinical approach to circadian rhythm sleep disorders. Sleep Med 2007;8:566–77.
41. Morgenthaler TI, Lee-Chiong T, Alessi C, et al. Practice parameters for the clinical evaluation and treatment of circadian rhythm sleep disorders. An American Academy of Sleep Medicine report. Sleep 2007;30:1445–59.
42. Shochat T, Martin J, Marler M, et al. Illumination levels in nursing home patients: effects on sleep and activity rhythms. J Sleep Res 2000;9:373–9.
43. Ancoli-Israel S, Klauber MR, Jones DW, et al. Variations in circadian rhythms of activity, sleep, and light exposure related to dementia in nursing-home patients. Sleep 1997;20:18–23.
44. Satlin A, Volicer L, Ross V, et al. Bright light treatment of behavioral and sleep disturbances in patients with Alzheimer’s disease. Am J Psychiatry 1992;149:1028–32.
45. Koyama E, Matsubara H, Nakano T. Bright light treatment for sleep-wake disturbances in aged individuals with dementia. Psychiatry Clin Neurosci 1999;53:227–9.
46. Burns A, Allen H, Tomenson B, et al. Bright light therapy for agitation in dementia: a randomized controlled trial. Int Psychogeriatr 2009;21:711–21.
47. Riemersma-van der Lek RF, Swaab DF, Twisk J, et al. Effect of bright light and melatonin on cognitive and noncognitive function in elderly residents of group care facilities: a randomized controlled trial. JAMA 2008;299:2642–55.
48. Martin JL, Marler MR, Harker JO, et al. A multicomponent nonpharmacological intervention improves activity rhythms among nursing home residents with disrupted sleep/wake patterns. J Gerontol Series A Biol Sci Med Sci 2007;62:67–72.
49. Lewy AJ, Ahmed S, Jackson JM, et al. Melatonin shifts human circadian rhythms according to a phase-response curve. Chronobiol Int 1992;9:380–92.
50. Williamson BL, Tomlinson AJ, Mishra PK, et al. Structural characterization of contaminants found in commercial preparations of melatonin: similarities to case-related compounds from L-tryptophan associated with eosinophilia-myalgia syndrome. Chem Res Toxicol 1998;11:234-40.
51. Czeisler CA, Walsh JK, Roth T, et al. Modafinil for excessive sleepiness associated with shift-work sleep disorder. N Engl J Med 2005;353:476-86.
52. Howard R, Roth T, Drake CL. The effects of armodafinil on objective sleepiness and performance in a shift work disorder sample unselected for objective sleepiness. J Clin Psychopharmacol 2014;34:369–73.
53. Beydoun MA, Gamaldo AA, Beydoun HA, et al. Caffeine and alcohol intakes and overall nutrient adequacy are associated with longitudinal cognitive performance among U.S. adults. J Nutr 2014;144:890–901.
54. Pentel P. Toxicity of over-the-counter stimulants. JAMA 1984;252:1898–903.
55. Neikrug AB, Ancoli-Israel S. Sleep disorders in the older adult - a mini-review. Gerontology 2010;56:181–9.
56. Chesson A Jr, Hartse K, Anderson WM, et al. Practice parameters for the evaluation of chronic insomnia. An American Academy of Sleep Medicine report. Standards of Practice Committee of the American Academy of Sleep Medicine. Sleep 2000;23:237–41.
57. Bastien CH, Vallieres A, Morin CM. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med 2001;2:297–307.
58. Buysse DJ, Reynolds CF 3rd, Monk TH, et al. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 1989;28:193–213.
59. Trauer JM, Qian MY, Doyle JS, et al. Cognitive behavioral therapy for chronic insomnia: a systematic review and meta-analysis. Ann Intern Med 2015;163:191–204.
60. National Institutes of Health State of the Science Conference statement on manifestations and management of chronic insomnia in adults, June 13-15, 2005. Sleep 2005;28:1049–57.
61. Schutte-Rodin S, Broch L, Buysse D, et al. Clinical guideline for the evaluation and management of chronic insomnia in adults. J Clin Sleep Med 2008;4:487–504.
62. Bain KT. Management of chronic insomnia in elderly persons. Am J Geriatr Pharmacother 2006;4:168–92.
63. FDA approves new type of sleep drug, Belsomra. 13 Aug 2014. Available at fda.gov.
64. Dubey AK, Handu SS, Mediratta PK. Suvorexant: The first orexin receptor antagonist to treat insomnia. J Pharmacol Pharmacother 2015;6:118–21.
65. Patel KV, Aspesi AV, Evoy KE. Suvorexant: a dual orexin receptor antagonist for the treatment of sleep onset and sleep maintenance insomnia. Ann Pharmacother 2015;49:477–83.
66. Michelson D, Snyder E, Paradis E, et al. Safety and efficacy of suvorexant during 1-year treatment of insomnia with subsequent abrupt treatment discontinuation: a phase 3 randomised, double-blind, placebo-controlled trial. Lancet Neurol 2014;13:461–71.
67. Bootzin RR, Epstein D, Wood JM. Stimulus control instructions. Case studies in insomnia. New York: Springer; 1991:19–28.
68. Gulyani S, Salas RE, Gamaldo CE. Sleep medicine pharmacotherapeutics overview: today, tomorrow, and the future (part 2: hypersomnia, parasomnia, and movement disorders). Chest 2013;143:242–51.
69. Boeve BF, Silber MH, Saper CB, et al. Pathophysiology of REM sleep behaviour disorder and relevance to neurodegenerative disease. Brain 2007;130(Pt 11):2770–88.
70. Middelkoop HA, Kerkhof GA, Smilde-van den Doel DA, et al. Sleep and ageing: the effect of institutionalization on subjective and objective characteristics of sleep. Age Ageing 1994;23:411–7.
71. Tinuper P, Provini F, Bisulli F, et al. Movement disorders in sleep: guidelines for differentiating epileptic from non-epileptic motor phenomena arising from sleep. Sleep Med Rev 2007;11:255–67.
72. Aurora RN, Zak RS, Maganti RK, et al. Best practice guide for the treatment of REM sleep behavior disorder (RBD). J Clin Sleep Med 2010;6:85–95.
73. Bloom HG, Ahmed I, Alessi CA, et al. Evidence-based recommendations for the assessment and management of sleep disorders in older persons. J Am Geriatr Soc 2009;57:761–89.
74. Anderson KN, Shneerson JM. Drug treatment of REM sleep behavior disorder: the use of drug therapies other than clonazepam. J Clin Sleep Med 2009;5:235–9.
75. Doshi A, Gamaldo C, Kalloo A, et al. Implementing a clinical iPad application to detect sleep disorders is feasible across multiple non-sleep outpatient clinics (P7. 321). Neurology 2015;84(14 Suppl):P7.321.
From the School of Aging Studies, University of South Florida, Tampa, FL (Dr. AA Gamaldo) and the Department of Neurology, Johns Hopkins Medicine, Baltimore, MD (Drs. Sloane, CE Gamaldo and Salas).
Abstract
- Objective: To provide guidance on identifying and treating sleep disturbances commonly encountered in older nursing home residents.
- Methods: Review of the literature in the context of 5 clinical cases.
- Results: Sleep disturbances continue to be a growing global epidemic, and public health initiatives have been aimed at improving sleep health across all ages. In older adults, sleep disturbances are often associated with the development and/or worsening of health conditions. Common sleep disturbances observed in older nursing home residents include obstructive sleep apnea, restless legs syndrome/Willis-Ekbom disease, circadian rhythm sleep-wake disorders, insomnia, and parasomnias. The symptoms and recommended treatment plans vary across the sleep disturbances. For many sleep disturbances, modification of residents’ daily activities and/or nursing home environment can be helpful.
- Conclusion: As the number of people residing in nursing homes increases, it is important for health care providers to be knowledgable about sleep disturbances in this population.
By 2030, almost 20% of the US population (approximately 72.1 million people) will be age 65 and older [1]. As many as 63% of older adults in the general population report sleep disturbances [2]. Specifically, older adults demonstrate difficulty with decreased total sleep duration, an increase in sleep fragmentation (ie, interruptions in nighttime sleep), and reduced total sleep time spent in rapid eye movement (REM) and slow wave sleep [3–5]. Poor sleep, either because of not getting enough sleep or having an undiagnosed and thus untreated sleep disorder, is associated with physical illness, impaired cognition, poor physical function, and mortality risk [6,7]. In fact, over 50% of individuals older than 65 years meet the diagnostic criteria for a sleep disorder, many of which are undiagnosed [6,7].
It is forecasted that we will see substantial increases in the rate of nursing home residence among the elderly [8]. The prevalence and severity of disturbed sleep is reportedly higher in NH residents [6,7]. Generally, NH residents tend to be on several medications for various medical disorders that may negatively impact sleep [7]. Reciprocally, sleep disruption may put NH residents at an increased risk for behavioral issues (eg, agitation) [9,10] as well as developing and/or exacerbating health conditions (eg, mood disorders, dementia, cardiovascular disease) [8]. Furthermore, NH residents exhibiting disturbed sleep, behavioral issues, and/or mood disorders are at an increased risk for being prescribed antipsychotic drugs [11], which are associated with adverse side effects and poorer quality of life [12]. Thus, the identification and management of sleep disturbances in the NH setting has become progressively more vital in efforts to optimize medical management of this population. This review identifies common sleep disturbances frequently underdiagnosed and undertreated among residents of NH facilities.
Case 1
A 73-year-old woman with a history of type 2 diabetes mellitus reports poor sleep quality with frequent awakenings during the night and excessive daytime sleepiness. She states that she can fall asleep within 5 minutes, but often is awoken throughout the night with a sensation of breathlessness. She has snored for many years, but the nursing staff at her NH facility has recently commented that her snoring has gone from intermittent to constant. She cannot remember the last time she has had restful sleep. She consumes 3 to 4 cups of caffeinated beverages daily to counter her sleepiness. She denies smoking or illicit drug or alcohol use. Her review of systems was notable for a 30-lb weight gain over the last year, and she reports increasing fatigue, irritability, and memory and concentration issues. Her current medication list includes metformin and amlodipine. Her examination is remarkable for a BMI of 31, large neck circumference (> 16), tonsillar enlargement, a crowded oropharynx, micrognathia, lungs clear to auscultation bilaterally, heart sounds of normal S1 and S2, and legs with trace pitting edema.
Case 1 Reflection: Sleep-Disordered Breathing
Although previous studies have observed high rates (60%–90%) of SDB in NH settings [16,17], one study observed that only 0.5% of nursing home residents carried a diagnosis with SDB, suggesting that SDB is being grossly underappreciated amongst NH residents over the age of 65 [18]. In order to evaluate for SBD, routine annual physical exams or medical chart reviews can elicit the risk factors for sleep apnea (eg, obesity [per BMI], male sex, postmenopausal women, family history of sleep apnea) as well as common comorbidities (eg, hypertension, coronary artery disease, and diabetes). Formal evaluation consists of a sleep evaluation with a sleep specialist and polysomnography (PSG; sleep study) that can be performed in the sleep center or at home depending on the patient’s history and other medical issues.
Case 1 Outcome
Case 2
An 85-year-old man with history of Alzheimer’s disease, major depression and arthritis, reports insomnia and “tingling in my legs” at bedtime. The patient cannot identify when the symptoms started but reports that his legs often jerk during sleep. He consumes a cup of coffee daily and has a previous 20 pack-year smoking history (he quit 40 years ago). On review of systems, he endorses fatigue. His current medication list includes fluoxetine, donepezil hydrochloride, ibuprofen as needed for arthritic pain, and a multivitamin. His examination was unremarkable, with a BMI of 26, neck circumference < 16, no tonsillar enlargement, normal (noncrowded) oropharynx, lungs clear to auscultation bilaterally, heart sounds demonstrating a normal S1 and S2, and legs without edema.
Case 2 Reflection: Restless Legs Syndrome/Willis-Ekbom Disease
Restless legs syndrome (RLS) also known as Willis-Ekbom disease, affects approximately 10 million adults in the United States alone [22]. RLS is a sensorimotor disorder that must satisfy the following 5 primary diagnostic criteria: (1) urge to move the legs with or without dysesthesias; (2) onset or exacerbation with rest or inactivity; (3) relief with movement; (4) symptoms are worse in the evening or at night (circadian component); (5) symptoms cannot be solely accounted for as consequence of another medical or behavioral condition. Other supporting clinical features can alert a clinician to the likelihood of a RLS diagnosis; these include positive family history, response to dopaminergic therapy, lack of profound daytime sleepiness, and presence of periodic limb movements during sleep (PLMS) [23–26]. In younger individuals, the symptoms present insidiously whereas older adults (> 50 years of age) will usually present with sudden onset [27].
Not only do patients lack the restorative sleep needed to ward off fatigue and restfulness, but patients also demonstrate higher rates of comorbidities (eg, anxiety, hypertension, depression) as well as large economic burden secondary to absenteeism and decreased on-the-job effectiveness [28,29]. As a results, patients with RLS experience significant reductions in quality of life related to this sensorimotor disorder [28].
No confirmatory laboratory test exists to diagnose RLS; however, patients suspected of having RLS should be evaluated with a basic metabolic panel, iron studies, and a thorough neurologic examination, as iron deficiency, kidney failure, uremia and peripheral neuropathy can lead to secondary RLS [30,31]. Evidence shows that RLS is common in NH residents [32] and may account for problematic behaviors, such as late night pacing [7]. Forty-five percent of community dwelling individuals over 65 years old exhibit a PLMS index (leg kicks per hour) of greater than 5 [33]. PLMS, while not a disorder in and of itself, can serve as a marker for potential disease. PLMS are characterized by intermittent episodes of stereotyped leg movements. PLMS typically do not awaken the patient from sleep and therefore do not contribute to insomnia or daytime sleepiness, representing a key clinical difference from RLS. It is important to note that PLMS are nonspecific and may be common in older adults that do not meet the diagnostic criteria for RLS.
Treatment of RLS is based on the frequency of symptoms and the level of functional impairment caused by the syndrome. RLS treatment recommendations should always espouse nonpharmacological interventions that include improving sleep practices, engagement in daily physical activity, targeted placement of sedentary activity in the morning when symptoms are less prominent, and concerted efforts to avoid the use of RLS-exacerbating medications (eg, selective serotonin reuptake inhibitor (SSRIs), neuroleptic agents, antihistamines) [28]. If there is an underlying condition contributing to RLS, such as metabolic disturbance or iron deficiency, then these conditions should be corrected before initiating RLS medications. Several medications are FDA-approved for treatment of RLS, including dopamine agonists (eg, ropinirole, rotigotine, pramipexole), dopamine precursor (eg, levodopa), glutamate-related (eg, gabapentin), benzodiazepines (eg, temazepam, clonazepam). Augmentation, the worsening of RLS symptoms, can occur in patients taking dopamine agonists. If this occurs, dopamine agents should be discontinued or switched to other agents (such as a long-acting dopamine agonist, gabapentin encarbil, as well as non-FDA approved therapies such as opioids). However, it is important to note that weaning off dopamine agents may result in mild but in most cases moderate and/or severe withdrawal from the medication, so counseling and close monitoring should be done.
Case 2 Outcome
Given the patient’s history of dementia, opioids, benzodiazepines and other delirium-inducing medications should be avoided. His antidepressive regimen, fluoxetine, should be re-evaluated as these medications have been associated with RLS exacerbation. In addition to SSRIs, medications associated with RLS are MAO inhibitors (selegeline, phenelzine), antipsychotics (risperdone, olanzapine), tricyclic antidepressants (mirtazapine), antihistamines (diphenhydramine, cimetidine), calcium channel blockers (verapamil, nifedipine, diltiazem), and phenytoin [34,35]. His treatment began with behavioral, nonpharmacological management, and blood testing for iron studies. His low iron level prompted initiation of oral supplementation, and he was asked to follow up in 3 months for reevaluation and possible initiation of low-dose dopamine agonists.
Case 3
A 73-year-old man with dementia is found to have very irregular sleep wake patterns with a variable bedtime and awakening time, often missing breakfast. He is found dozing off often during the day, particularly during times of inactivity. He has frequent awakenings during the night often calling for the staff to guide him back to bed. He has had some falls secondary to walking around his room. He has been prescribed various hypnotics without much benefit and instead, has suffered from some confusion while on these medications. His room is very dark and has no windows.
Case 3 Reflection: Circadian Rhythm Sleep-Wake Disorders
Circadian rhythm sleep-wake disorders (CRSWDs) are characterized by an individual’s natural propensity to want to go to sleep and be awake during a period that is undesirable personally and/or socially [36]. CRSWDs can be a result of the desynchronization of the 2 sleep processes: (1) homeostatic drive (regulates sleep intensity) and (2) circadian rhythm (maintains daytime alertness); [36]. CRSWDs can also be due to an individual’s naturally occurring sleep drives becoming misaligned with their social/personal sleep-wake demands (eg, employment schedule and socializing opportunities with family/friends). With increasing age, the circadian rhythm becomes less adept at functioning in a desynchronized pattern [7], which can result in daytime sleepiness and night time sleep fragmentation [7,37]. CRSWDs are highly prevalent in individuals with dementia [7,36]. As dementia progresses, the ability to maintain a balance of the 2 sleep process becomes more impaired [7]. As a result, individuals with dementia, particularly Alzheimer’s disease, are likely to experience agitation, irritability, and/or confusion during the evening and night, a behavioral problem referred to as “sundowning” [38].
There are several types of CRSWDs, including delayed sleep-phase syndrome, advanced sleep-phase syndrome, irregular sleep-wake disorder, non–24-hour sleep-wake disorder, shift work sleep disorder, and jet lag sleep disorder. However, the most common type of CRSWDs observed in older adults is advanced sleep-phase syndrome [39]. Due to excessive sleepiness in the early evening, affected individuals may report a need to shift to earlier and earlier bedtimes (~6 to 7 pm) and wake times (~3 to 4 am) [36]. For older affected adults, this can cause distress and frustration, particularly if their sleep phase prevents them from participating in evening activities (eg, socializing with family/friends) [36].
In the assessment of patients with suspected CRSWDs, sleep diaries (self-reported or caregiver) daily account of sleep and wake times over at least 1 week) and actigraphy (wrist-worn accelerometer designed to measure activity and inactivity at night) can be used, particularly in older adults with dementia [40,41].
CRSWD treatment may include behavioral modifications and/or pharmacological intervention. Behavioral modifications can consist of chronotherapy, relaxation training, and/or bright light therapy. Chronotherapy involves making gradual shifts in an individual’s sleep time to meet his/her desired sleep schedule. Relaxation training involves implementing behaviors/activities that reduce tension and enhance the smooth transition into sleep. Bright light therapy involves exposure to an appropriate intensity and duration of light, which is an important environmental cue to help the synchrony of the sleep-wake cycle [7]. Previous studies have observed that NH residents are exposed to a restricted amount of bright light during the daytime [42,43], but higher levels of artificial light at night (eg, hallway lighting) [7]. NH residents’ exposure to artificial bright light during the daytime has not only improved the residents’ sleep [44–46], but also has improved their cognitive functioning and reduced their depressive symptoms [47]. Thus, steps towards targeted light exposure in sync with the typical sleep-wake cycle (eg, mandated time in well-lit rooms during the day and during meals) for NH residents, particularly those with CRSWDs, could prove to be beneficial across several social, behavioral and neurocognitive domains. Lastly, NH residents exposed to at least 30 minutes of outdoor daylight and at least 3 occasions of low intensity physical activities for 10 to 15 minutes daily can potentially improve sleep-wake patterns [48]. Thus, it may be beneficial to have an intervention that couples bright light exposure and physical activity in the NH setting.
Pharmacological interventions can also be implemented to improve older residents’ symptoms. However, the medications prescribed should be used with caution and should not be used as part of a long-term treatment plan. Melatonin is a commonly used herbal supplement that can assist advancing the timing of the circadian rhythms in the evening but can delay the circadian rhythms in the morning [49]. Several brands of this herbal supplement can be purchased over-the-counter and are not regulated by the FDA. Since the amount of melatonin used in the herbal supplement varies by brand, caution should be used when selecting a brand [50]. Two FDA-approved drugs (modafinil and armodafinil) are currently being used to reduce daytime sleepiness and improve vigilance amongst adults, but limited research has explored the effectiveness of these medication for older adults specifically suffering with CRSWDS [36,51,52]. Other stimulants (eg, caffeine, amphetamines, and nonamphetamine-derived medications) are also currently being used to reduce daytime sleepiness in patients with CRSWDS. Stimulant use, particularly caffeine consumption, has also been associated with better cognitive functioning in older adults [53]. However, stimulants should be taken with caution, particularly in older adults, because stimulant use has been associated with potentially serious and fatal health sequalae (eg, tachycardia, heart failure, irreversible heart damage and hypertension) [36,54].
Case 3 Outcome
The patient was moved to a room with a window. An alarm clock was set for 7:30 in the morning and he was taken to breakfast, where he sat at a table near a window. Any time he appeared to be sleepy, he was encouraged to go for a walk or engage in other activities so daytime napping opportunities were limited. His environment was assessed for safety and bedrails were utilized to prevent falls.
Case 4
A 75-year-old woman with a history of anxiety and depression moved into the NH 4 months ago after suffering a stroke. She now reports difficulty falling asleep for many years, which has significantly worsened since moving to the NH. Currently, she has been getting only 3 to 4 hour of sleep per night. She reports mild but increasing daytime sleepiness and does not fall asleep until 1:00 am despite getting into bed at 10:30 pm. She occasionally reports arthritic pain that interferes with her sleep. The NH staff has mentioned that she will occasionally cry for her family when she appears to be asleep.
Case 4 Reflection: Insomnia
According to the International Classification of Sleep Disorders (ICSD-3) [39], insomnia is characterized as “a repeated difficulty with sleep initiation, duration, consolidation, or quality that occurs despite adequate opportunity and circumstances for sleep, and results in some form of daytime impairment.” Among the sleep disorders, insomnia is one of the most common sleep issues observed in sleep clinics [34]. Older adults with insomnia often have comorbid physical (eg, pulmonary disease, arthritis, chronic pain, cancer diabetes, Parkinson’s disease) and mental illness (eg, depression, panic disorder) [55]. Medications (eg, stimulants, respiratory medications, chemotherapy, decongestants, hormones, or psychotropics) may cause and exacerbate insomnia symptoms [55].
Since insomnia is a clinical diagnosis, there is no specific diagnostic tool or gold standard test to identify individuals suffering with insomnia. Insomnia screening usually involves a clinical interview, in which a health provider, preferably trained in sleep, conducts a physical examination and collects an in-depth history of a patients’ sleep problems [56]. Insomnia screening tools may also include having a patient complete a sleep diary or questionnaire, such as the insomnia severity index (ISI) [57] or Pittsburgh Sleep Quality Index (PSQI) [58].
Cognitive behavioral therapy for insomnia (CBT-I) and/or pharmacological intervention are typically used to treat insomnia in older adults. CBT-I is a combination of cognitive (eg, changing dysfunctional sleep attitudes/beliefs) and behavioral treatment (eg, adhering to a regular sleep schedule) [59]. CBT-I or a combination of CBT-I and pharmacological intervention is recommended as more effective long-term approach to insomnia treatment compared to pharmacological intervention alone [55]. CBT-I involves altering older adults’ misconceptions of their sleep and implementing behavioral techniques to their everyday life (eg, routine sleep-wake schedule, relaxation therapy). Several FDA-approved medications are available to treat insomnia; however, many commonly used medications to treat insomnia in older adults (ie, antihistamines, antidepressants, anticonvulsants, and anti-psychotics) pose more risks than benefits to their health and well-being [35,60–62]. Some of the more recent hypnotics (egm zolpidem, exzopiclone, and ramelteon) on the market have been shown to be safer and more effective pharmacological options [55]. In 2014, the FDA approved the first in class orexin receptor antagonist medication (suvorexant) to treat insomnia [63]. Unlike other medications to treat insomnia, suvorexant, via the blockade of the orexin neurotransmitter, effectively inhibits orexin (one of neurotransmitters involved in the activation pathways of the arousal system), so sleep can easily be induced and maintained [64, 65]. Furthermore, preliminary studies suggest that this medication may be associated with less severe side effects (ie, habituation) than the other approved medications on the market [64, 65]. In fact, in a recent clinical series that included both young and older insomnia patients, the most common adverse reaction to suvorexant was drowsiness [66].
Case 4 Outcome
The patient was initiated on basic CBT-I therapy strategies which included stimulus control therapy [67]; implementation of a consistent bedtime and awakening routine; reducing the use of TV, smart phone, or other electronic leisure devices 1 hour before bedtime; refraining from caffeine after lunchtime; improving the sleep environment; and relaxation techniques.
Case 5
The patient is a 65-year-old man diagnosed with Parkinson’s disease several years ago. Recently, he has often has been experiencing what appears to be very violent and terrifying dreams. While asleep, he often screams and shouts for help. In addition, he occasionally will punch, kick, and/or thrash around in bed at night, which the NH staff has noted as a concern for his safety.
Case 5 Reflection: Parasomnias
Parasomnias represent frequent arousals during sleep or in the wake-to-sleep transition due to abnormal motor movements, behaviors (eg, shouting, flailing, and leaping from bed) and/or sensory experiences (eg, “dreamlike” hallucinations) [68]. Motor movements that occur for parasomnia can be disruptive for the individual and potentially dangerous for the individual and/or bed partner. There are 3 primary types of parasomnias based on the stage of sleep that the event occurs: non-REM (NREM), REM, and other parasomnias during transitions of sleep [68]. The most commonly observed parasomnia seen in older adults is the REM-associated parasomnia or REM sleep behavior disorder (RBD), which is characterized by experiencing vivid, sometimes violent, dreams typically involving fighting an intruder or an animal to protect a loved one [69]. For RBD, disruptive behaviors typically occur during REM sleep [69]. RBD has been associated with neurodegenerative disorders (Parkinson’s disease and Lewy body disease), neurologic disorders (eg, brain tumors and stroke), other primary disorders (narcolepsy and periodic limb movement disorder), and well as some medications (eg, antidepressants and β-blockers) [68]. There is limited knowledge on the prevalence of parasomnias in NH settings. One study, however, reported that 31% of older NH residents experience parasomnias [70]. Evaluation for parasomnias generally involve a clinical evaluation by a sleep specialist and overnight sleep study (ie, polysomnography at a sleep center if there is a concern for sleep apnea or RBD [71].
Medications are not typically first-line for parasomnia. Instead education about improving sleep practices, addressing other underlying sleep disorders, and securing a safe sleep environment are first recommended. Pharmacologic treatment, particularly the use of clonazepam, is commonly used to treat RBD [72]. However, this medication should be used with caution for older adults with a dementia diagnosis, gait disorders, and OSA because the common side effects include sedation, confusion, memory dysfunction, and early morning motor incoordination [68]. Several alternative medications have also been used to treat RBD. For example, medications commonly used to Parkinson disease symptoms, such Levodopa and dopamine agonists, have also been used to treat RBD [73]. Zopiclone, a nonbenzodiazepine hypnotic agent, has also been shown to be as effective as clonazepam, but with less potential side effects [74]. Melatonin, a nutritional supplement, has also been used as a treatment and appears to alleviate some of the RBD symptoms and has fewer side effects [68]. Since melatonin is not regulated by the FDA, it has been suggested that this treatment be used with caution in the older population [73].
Case 5 Outcome
The patient was evaluated with video synchronized in lab PSG. It confirmed REM sleep without evidence of the normal atonia that should be apparent during REM. These PSG findings in combination with repeated accounts of dream enactment established the diagnosis of RBD. Patient was treated with low-dose clonazepam and closely monitored for potential side effects of daytime sedation. Bedroom environment was also carefully reconfigured for safety to avoid potential risk of injury during a dream enactment episode.
Conclusion
Sleep disturbances remain an underappreciated and undertreated health issue in NH residents. Nursing homes can help facilitate optimal sleep health and day functioning by providing mandatory natural light outlets, physical exercise opportunities, and minimal allowable time residents can spend in their bed/bedroom outside of their routine sleep period. Educating NH providers and staff on sleep medicine may benefit residents, but workload and restricted resources may hinder this. Education via mobile and internet based educational platforms and resources (Mysleep101) may be helpful in addressing education barriers [75]. Convenient and cost-effective methods to deliver sleep medicine education to NH health care providers should be part of our ongoing efforts to improve the viability, vitality and quality of life of our aging citizens.
Corresponding author: Alyssa Gamaldo, PhD, Univ. of South Florida, 13301 Bruce B. Downs Blvd, MHC 1340, Tampa, FL 33612, agamaldo@usf.edu.
Financial disclosures: None.
From the School of Aging Studies, University of South Florida, Tampa, FL (Dr. AA Gamaldo) and the Department of Neurology, Johns Hopkins Medicine, Baltimore, MD (Drs. Sloane, CE Gamaldo and Salas).
Abstract
- Objective: To provide guidance on identifying and treating sleep disturbances commonly encountered in older nursing home residents.
- Methods: Review of the literature in the context of 5 clinical cases.
- Results: Sleep disturbances continue to be a growing global epidemic, and public health initiatives have been aimed at improving sleep health across all ages. In older adults, sleep disturbances are often associated with the development and/or worsening of health conditions. Common sleep disturbances observed in older nursing home residents include obstructive sleep apnea, restless legs syndrome/Willis-Ekbom disease, circadian rhythm sleep-wake disorders, insomnia, and parasomnias. The symptoms and recommended treatment plans vary across the sleep disturbances. For many sleep disturbances, modification of residents’ daily activities and/or nursing home environment can be helpful.
- Conclusion: As the number of people residing in nursing homes increases, it is important for health care providers to be knowledgable about sleep disturbances in this population.
By 2030, almost 20% of the US population (approximately 72.1 million people) will be age 65 and older [1]. As many as 63% of older adults in the general population report sleep disturbances [2]. Specifically, older adults demonstrate difficulty with decreased total sleep duration, an increase in sleep fragmentation (ie, interruptions in nighttime sleep), and reduced total sleep time spent in rapid eye movement (REM) and slow wave sleep [3–5]. Poor sleep, either because of not getting enough sleep or having an undiagnosed and thus untreated sleep disorder, is associated with physical illness, impaired cognition, poor physical function, and mortality risk [6,7]. In fact, over 50% of individuals older than 65 years meet the diagnostic criteria for a sleep disorder, many of which are undiagnosed [6,7].
It is forecasted that we will see substantial increases in the rate of nursing home residence among the elderly [8]. The prevalence and severity of disturbed sleep is reportedly higher in NH residents [6,7]. Generally, NH residents tend to be on several medications for various medical disorders that may negatively impact sleep [7]. Reciprocally, sleep disruption may put NH residents at an increased risk for behavioral issues (eg, agitation) [9,10] as well as developing and/or exacerbating health conditions (eg, mood disorders, dementia, cardiovascular disease) [8]. Furthermore, NH residents exhibiting disturbed sleep, behavioral issues, and/or mood disorders are at an increased risk for being prescribed antipsychotic drugs [11], which are associated with adverse side effects and poorer quality of life [12]. Thus, the identification and management of sleep disturbances in the NH setting has become progressively more vital in efforts to optimize medical management of this population. This review identifies common sleep disturbances frequently underdiagnosed and undertreated among residents of NH facilities.
Case 1
A 73-year-old woman with a history of type 2 diabetes mellitus reports poor sleep quality with frequent awakenings during the night and excessive daytime sleepiness. She states that she can fall asleep within 5 minutes, but often is awoken throughout the night with a sensation of breathlessness. She has snored for many years, but the nursing staff at her NH facility has recently commented that her snoring has gone from intermittent to constant. She cannot remember the last time she has had restful sleep. She consumes 3 to 4 cups of caffeinated beverages daily to counter her sleepiness. She denies smoking or illicit drug or alcohol use. Her review of systems was notable for a 30-lb weight gain over the last year, and she reports increasing fatigue, irritability, and memory and concentration issues. Her current medication list includes metformin and amlodipine. Her examination is remarkable for a BMI of 31, large neck circumference (> 16), tonsillar enlargement, a crowded oropharynx, micrognathia, lungs clear to auscultation bilaterally, heart sounds of normal S1 and S2, and legs with trace pitting edema.
Case 1 Reflection: Sleep-Disordered Breathing
Although previous studies have observed high rates (60%–90%) of SDB in NH settings [16,17], one study observed that only 0.5% of nursing home residents carried a diagnosis with SDB, suggesting that SDB is being grossly underappreciated amongst NH residents over the age of 65 [18]. In order to evaluate for SBD, routine annual physical exams or medical chart reviews can elicit the risk factors for sleep apnea (eg, obesity [per BMI], male sex, postmenopausal women, family history of sleep apnea) as well as common comorbidities (eg, hypertension, coronary artery disease, and diabetes). Formal evaluation consists of a sleep evaluation with a sleep specialist and polysomnography (PSG; sleep study) that can be performed in the sleep center or at home depending on the patient’s history and other medical issues.
Case 1 Outcome
Case 2
An 85-year-old man with history of Alzheimer’s disease, major depression and arthritis, reports insomnia and “tingling in my legs” at bedtime. The patient cannot identify when the symptoms started but reports that his legs often jerk during sleep. He consumes a cup of coffee daily and has a previous 20 pack-year smoking history (he quit 40 years ago). On review of systems, he endorses fatigue. His current medication list includes fluoxetine, donepezil hydrochloride, ibuprofen as needed for arthritic pain, and a multivitamin. His examination was unremarkable, with a BMI of 26, neck circumference < 16, no tonsillar enlargement, normal (noncrowded) oropharynx, lungs clear to auscultation bilaterally, heart sounds demonstrating a normal S1 and S2, and legs without edema.
Case 2 Reflection: Restless Legs Syndrome/Willis-Ekbom Disease
Restless legs syndrome (RLS) also known as Willis-Ekbom disease, affects approximately 10 million adults in the United States alone [22]. RLS is a sensorimotor disorder that must satisfy the following 5 primary diagnostic criteria: (1) urge to move the legs with or without dysesthesias; (2) onset or exacerbation with rest or inactivity; (3) relief with movement; (4) symptoms are worse in the evening or at night (circadian component); (5) symptoms cannot be solely accounted for as consequence of another medical or behavioral condition. Other supporting clinical features can alert a clinician to the likelihood of a RLS diagnosis; these include positive family history, response to dopaminergic therapy, lack of profound daytime sleepiness, and presence of periodic limb movements during sleep (PLMS) [23–26]. In younger individuals, the symptoms present insidiously whereas older adults (> 50 years of age) will usually present with sudden onset [27].
Not only do patients lack the restorative sleep needed to ward off fatigue and restfulness, but patients also demonstrate higher rates of comorbidities (eg, anxiety, hypertension, depression) as well as large economic burden secondary to absenteeism and decreased on-the-job effectiveness [28,29]. As a results, patients with RLS experience significant reductions in quality of life related to this sensorimotor disorder [28].
No confirmatory laboratory test exists to diagnose RLS; however, patients suspected of having RLS should be evaluated with a basic metabolic panel, iron studies, and a thorough neurologic examination, as iron deficiency, kidney failure, uremia and peripheral neuropathy can lead to secondary RLS [30,31]. Evidence shows that RLS is common in NH residents [32] and may account for problematic behaviors, such as late night pacing [7]. Forty-five percent of community dwelling individuals over 65 years old exhibit a PLMS index (leg kicks per hour) of greater than 5 [33]. PLMS, while not a disorder in and of itself, can serve as a marker for potential disease. PLMS are characterized by intermittent episodes of stereotyped leg movements. PLMS typically do not awaken the patient from sleep and therefore do not contribute to insomnia or daytime sleepiness, representing a key clinical difference from RLS. It is important to note that PLMS are nonspecific and may be common in older adults that do not meet the diagnostic criteria for RLS.
Treatment of RLS is based on the frequency of symptoms and the level of functional impairment caused by the syndrome. RLS treatment recommendations should always espouse nonpharmacological interventions that include improving sleep practices, engagement in daily physical activity, targeted placement of sedentary activity in the morning when symptoms are less prominent, and concerted efforts to avoid the use of RLS-exacerbating medications (eg, selective serotonin reuptake inhibitor (SSRIs), neuroleptic agents, antihistamines) [28]. If there is an underlying condition contributing to RLS, such as metabolic disturbance or iron deficiency, then these conditions should be corrected before initiating RLS medications. Several medications are FDA-approved for treatment of RLS, including dopamine agonists (eg, ropinirole, rotigotine, pramipexole), dopamine precursor (eg, levodopa), glutamate-related (eg, gabapentin), benzodiazepines (eg, temazepam, clonazepam). Augmentation, the worsening of RLS symptoms, can occur in patients taking dopamine agonists. If this occurs, dopamine agents should be discontinued or switched to other agents (such as a long-acting dopamine agonist, gabapentin encarbil, as well as non-FDA approved therapies such as opioids). However, it is important to note that weaning off dopamine agents may result in mild but in most cases moderate and/or severe withdrawal from the medication, so counseling and close monitoring should be done.
Case 2 Outcome
Given the patient’s history of dementia, opioids, benzodiazepines and other delirium-inducing medications should be avoided. His antidepressive regimen, fluoxetine, should be re-evaluated as these medications have been associated with RLS exacerbation. In addition to SSRIs, medications associated with RLS are MAO inhibitors (selegeline, phenelzine), antipsychotics (risperdone, olanzapine), tricyclic antidepressants (mirtazapine), antihistamines (diphenhydramine, cimetidine), calcium channel blockers (verapamil, nifedipine, diltiazem), and phenytoin [34,35]. His treatment began with behavioral, nonpharmacological management, and blood testing for iron studies. His low iron level prompted initiation of oral supplementation, and he was asked to follow up in 3 months for reevaluation and possible initiation of low-dose dopamine agonists.
Case 3
A 73-year-old man with dementia is found to have very irregular sleep wake patterns with a variable bedtime and awakening time, often missing breakfast. He is found dozing off often during the day, particularly during times of inactivity. He has frequent awakenings during the night often calling for the staff to guide him back to bed. He has had some falls secondary to walking around his room. He has been prescribed various hypnotics without much benefit and instead, has suffered from some confusion while on these medications. His room is very dark and has no windows.
Case 3 Reflection: Circadian Rhythm Sleep-Wake Disorders
Circadian rhythm sleep-wake disorders (CRSWDs) are characterized by an individual’s natural propensity to want to go to sleep and be awake during a period that is undesirable personally and/or socially [36]. CRSWDs can be a result of the desynchronization of the 2 sleep processes: (1) homeostatic drive (regulates sleep intensity) and (2) circadian rhythm (maintains daytime alertness); [36]. CRSWDs can also be due to an individual’s naturally occurring sleep drives becoming misaligned with their social/personal sleep-wake demands (eg, employment schedule and socializing opportunities with family/friends). With increasing age, the circadian rhythm becomes less adept at functioning in a desynchronized pattern [7], which can result in daytime sleepiness and night time sleep fragmentation [7,37]. CRSWDs are highly prevalent in individuals with dementia [7,36]. As dementia progresses, the ability to maintain a balance of the 2 sleep process becomes more impaired [7]. As a result, individuals with dementia, particularly Alzheimer’s disease, are likely to experience agitation, irritability, and/or confusion during the evening and night, a behavioral problem referred to as “sundowning” [38].
There are several types of CRSWDs, including delayed sleep-phase syndrome, advanced sleep-phase syndrome, irregular sleep-wake disorder, non–24-hour sleep-wake disorder, shift work sleep disorder, and jet lag sleep disorder. However, the most common type of CRSWDs observed in older adults is advanced sleep-phase syndrome [39]. Due to excessive sleepiness in the early evening, affected individuals may report a need to shift to earlier and earlier bedtimes (~6 to 7 pm) and wake times (~3 to 4 am) [36]. For older affected adults, this can cause distress and frustration, particularly if their sleep phase prevents them from participating in evening activities (eg, socializing with family/friends) [36].
In the assessment of patients with suspected CRSWDs, sleep diaries (self-reported or caregiver) daily account of sleep and wake times over at least 1 week) and actigraphy (wrist-worn accelerometer designed to measure activity and inactivity at night) can be used, particularly in older adults with dementia [40,41].
CRSWD treatment may include behavioral modifications and/or pharmacological intervention. Behavioral modifications can consist of chronotherapy, relaxation training, and/or bright light therapy. Chronotherapy involves making gradual shifts in an individual’s sleep time to meet his/her desired sleep schedule. Relaxation training involves implementing behaviors/activities that reduce tension and enhance the smooth transition into sleep. Bright light therapy involves exposure to an appropriate intensity and duration of light, which is an important environmental cue to help the synchrony of the sleep-wake cycle [7]. Previous studies have observed that NH residents are exposed to a restricted amount of bright light during the daytime [42,43], but higher levels of artificial light at night (eg, hallway lighting) [7]. NH residents’ exposure to artificial bright light during the daytime has not only improved the residents’ sleep [44–46], but also has improved their cognitive functioning and reduced their depressive symptoms [47]. Thus, steps towards targeted light exposure in sync with the typical sleep-wake cycle (eg, mandated time in well-lit rooms during the day and during meals) for NH residents, particularly those with CRSWDs, could prove to be beneficial across several social, behavioral and neurocognitive domains. Lastly, NH residents exposed to at least 30 minutes of outdoor daylight and at least 3 occasions of low intensity physical activities for 10 to 15 minutes daily can potentially improve sleep-wake patterns [48]. Thus, it may be beneficial to have an intervention that couples bright light exposure and physical activity in the NH setting.
Pharmacological interventions can also be implemented to improve older residents’ symptoms. However, the medications prescribed should be used with caution and should not be used as part of a long-term treatment plan. Melatonin is a commonly used herbal supplement that can assist advancing the timing of the circadian rhythms in the evening but can delay the circadian rhythms in the morning [49]. Several brands of this herbal supplement can be purchased over-the-counter and are not regulated by the FDA. Since the amount of melatonin used in the herbal supplement varies by brand, caution should be used when selecting a brand [50]. Two FDA-approved drugs (modafinil and armodafinil) are currently being used to reduce daytime sleepiness and improve vigilance amongst adults, but limited research has explored the effectiveness of these medication for older adults specifically suffering with CRSWDS [36,51,52]. Other stimulants (eg, caffeine, amphetamines, and nonamphetamine-derived medications) are also currently being used to reduce daytime sleepiness in patients with CRSWDS. Stimulant use, particularly caffeine consumption, has also been associated with better cognitive functioning in older adults [53]. However, stimulants should be taken with caution, particularly in older adults, because stimulant use has been associated with potentially serious and fatal health sequalae (eg, tachycardia, heart failure, irreversible heart damage and hypertension) [36,54].
Case 3 Outcome
The patient was moved to a room with a window. An alarm clock was set for 7:30 in the morning and he was taken to breakfast, where he sat at a table near a window. Any time he appeared to be sleepy, he was encouraged to go for a walk or engage in other activities so daytime napping opportunities were limited. His environment was assessed for safety and bedrails were utilized to prevent falls.
Case 4
A 75-year-old woman with a history of anxiety and depression moved into the NH 4 months ago after suffering a stroke. She now reports difficulty falling asleep for many years, which has significantly worsened since moving to the NH. Currently, she has been getting only 3 to 4 hour of sleep per night. She reports mild but increasing daytime sleepiness and does not fall asleep until 1:00 am despite getting into bed at 10:30 pm. She occasionally reports arthritic pain that interferes with her sleep. The NH staff has mentioned that she will occasionally cry for her family when she appears to be asleep.
Case 4 Reflection: Insomnia
According to the International Classification of Sleep Disorders (ICSD-3) [39], insomnia is characterized as “a repeated difficulty with sleep initiation, duration, consolidation, or quality that occurs despite adequate opportunity and circumstances for sleep, and results in some form of daytime impairment.” Among the sleep disorders, insomnia is one of the most common sleep issues observed in sleep clinics [34]. Older adults with insomnia often have comorbid physical (eg, pulmonary disease, arthritis, chronic pain, cancer diabetes, Parkinson’s disease) and mental illness (eg, depression, panic disorder) [55]. Medications (eg, stimulants, respiratory medications, chemotherapy, decongestants, hormones, or psychotropics) may cause and exacerbate insomnia symptoms [55].
Since insomnia is a clinical diagnosis, there is no specific diagnostic tool or gold standard test to identify individuals suffering with insomnia. Insomnia screening usually involves a clinical interview, in which a health provider, preferably trained in sleep, conducts a physical examination and collects an in-depth history of a patients’ sleep problems [56]. Insomnia screening tools may also include having a patient complete a sleep diary or questionnaire, such as the insomnia severity index (ISI) [57] or Pittsburgh Sleep Quality Index (PSQI) [58].
Cognitive behavioral therapy for insomnia (CBT-I) and/or pharmacological intervention are typically used to treat insomnia in older adults. CBT-I is a combination of cognitive (eg, changing dysfunctional sleep attitudes/beliefs) and behavioral treatment (eg, adhering to a regular sleep schedule) [59]. CBT-I or a combination of CBT-I and pharmacological intervention is recommended as more effective long-term approach to insomnia treatment compared to pharmacological intervention alone [55]. CBT-I involves altering older adults’ misconceptions of their sleep and implementing behavioral techniques to their everyday life (eg, routine sleep-wake schedule, relaxation therapy). Several FDA-approved medications are available to treat insomnia; however, many commonly used medications to treat insomnia in older adults (ie, antihistamines, antidepressants, anticonvulsants, and anti-psychotics) pose more risks than benefits to their health and well-being [35,60–62]. Some of the more recent hypnotics (egm zolpidem, exzopiclone, and ramelteon) on the market have been shown to be safer and more effective pharmacological options [55]. In 2014, the FDA approved the first in class orexin receptor antagonist medication (suvorexant) to treat insomnia [63]. Unlike other medications to treat insomnia, suvorexant, via the blockade of the orexin neurotransmitter, effectively inhibits orexin (one of neurotransmitters involved in the activation pathways of the arousal system), so sleep can easily be induced and maintained [64, 65]. Furthermore, preliminary studies suggest that this medication may be associated with less severe side effects (ie, habituation) than the other approved medications on the market [64, 65]. In fact, in a recent clinical series that included both young and older insomnia patients, the most common adverse reaction to suvorexant was drowsiness [66].
Case 4 Outcome
The patient was initiated on basic CBT-I therapy strategies which included stimulus control therapy [67]; implementation of a consistent bedtime and awakening routine; reducing the use of TV, smart phone, or other electronic leisure devices 1 hour before bedtime; refraining from caffeine after lunchtime; improving the sleep environment; and relaxation techniques.
Case 5
The patient is a 65-year-old man diagnosed with Parkinson’s disease several years ago. Recently, he has often has been experiencing what appears to be very violent and terrifying dreams. While asleep, he often screams and shouts for help. In addition, he occasionally will punch, kick, and/or thrash around in bed at night, which the NH staff has noted as a concern for his safety.
Case 5 Reflection: Parasomnias
Parasomnias represent frequent arousals during sleep or in the wake-to-sleep transition due to abnormal motor movements, behaviors (eg, shouting, flailing, and leaping from bed) and/or sensory experiences (eg, “dreamlike” hallucinations) [68]. Motor movements that occur for parasomnia can be disruptive for the individual and potentially dangerous for the individual and/or bed partner. There are 3 primary types of parasomnias based on the stage of sleep that the event occurs: non-REM (NREM), REM, and other parasomnias during transitions of sleep [68]. The most commonly observed parasomnia seen in older adults is the REM-associated parasomnia or REM sleep behavior disorder (RBD), which is characterized by experiencing vivid, sometimes violent, dreams typically involving fighting an intruder or an animal to protect a loved one [69]. For RBD, disruptive behaviors typically occur during REM sleep [69]. RBD has been associated with neurodegenerative disorders (Parkinson’s disease and Lewy body disease), neurologic disorders (eg, brain tumors and stroke), other primary disorders (narcolepsy and periodic limb movement disorder), and well as some medications (eg, antidepressants and β-blockers) [68]. There is limited knowledge on the prevalence of parasomnias in NH settings. One study, however, reported that 31% of older NH residents experience parasomnias [70]. Evaluation for parasomnias generally involve a clinical evaluation by a sleep specialist and overnight sleep study (ie, polysomnography at a sleep center if there is a concern for sleep apnea or RBD [71].
Medications are not typically first-line for parasomnia. Instead education about improving sleep practices, addressing other underlying sleep disorders, and securing a safe sleep environment are first recommended. Pharmacologic treatment, particularly the use of clonazepam, is commonly used to treat RBD [72]. However, this medication should be used with caution for older adults with a dementia diagnosis, gait disorders, and OSA because the common side effects include sedation, confusion, memory dysfunction, and early morning motor incoordination [68]. Several alternative medications have also been used to treat RBD. For example, medications commonly used to Parkinson disease symptoms, such Levodopa and dopamine agonists, have also been used to treat RBD [73]. Zopiclone, a nonbenzodiazepine hypnotic agent, has also been shown to be as effective as clonazepam, but with less potential side effects [74]. Melatonin, a nutritional supplement, has also been used as a treatment and appears to alleviate some of the RBD symptoms and has fewer side effects [68]. Since melatonin is not regulated by the FDA, it has been suggested that this treatment be used with caution in the older population [73].
Case 5 Outcome
The patient was evaluated with video synchronized in lab PSG. It confirmed REM sleep without evidence of the normal atonia that should be apparent during REM. These PSG findings in combination with repeated accounts of dream enactment established the diagnosis of RBD. Patient was treated with low-dose clonazepam and closely monitored for potential side effects of daytime sedation. Bedroom environment was also carefully reconfigured for safety to avoid potential risk of injury during a dream enactment episode.
Conclusion
Sleep disturbances remain an underappreciated and undertreated health issue in NH residents. Nursing homes can help facilitate optimal sleep health and day functioning by providing mandatory natural light outlets, physical exercise opportunities, and minimal allowable time residents can spend in their bed/bedroom outside of their routine sleep period. Educating NH providers and staff on sleep medicine may benefit residents, but workload and restricted resources may hinder this. Education via mobile and internet based educational platforms and resources (Mysleep101) may be helpful in addressing education barriers [75]. Convenient and cost-effective methods to deliver sleep medicine education to NH health care providers should be part of our ongoing efforts to improve the viability, vitality and quality of life of our aging citizens.
Corresponding author: Alyssa Gamaldo, PhD, Univ. of South Florida, 13301 Bruce B. Downs Blvd, MHC 1340, Tampa, FL 33612, agamaldo@usf.edu.
Financial disclosures: None.
1. Federal Interagency Forum on Aging-Related Statistics. Older Americans 2012: Key indicators of well-being. Washington, DC: U.S. Gov. Printing Office; 2012.
2. Almeida OP, Pfaff JJ. Sleep complaints among older general practice patients: association with depression. Br J Gen Pract 2005;55:864–866.
3. Wolkove N, Elkholy O, Baltzan M, et al. Sleep and aging: 1. Sleep disorders commonly found in older people. CMAJ 2007;176:1299–304.
4. Pace-Schott EF, Spencer RM. Age-related changes in the cognitive function of sleep. Prog Brain Res 2011;191:75–89.
5. Ohayon MM, Carskadon MA, Guilleminault C, et al. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep 2004;27:1255–73.
6. Jacobs D, Ancoli-Israel S, Parker L, et al. Twenty-four-hour sleep-wake patterns in a nursing home population. Psychol Aging 1989;4:352–6.
7. Neikrug AB, Ancoli-Israel S. Sleep disturbances in nursing homes. J Nutr Health Aging 2010;14:207–11.
8. Lakdawalla D, Goldman DP, Bhattacharya J, et al. Forecasting the nursing home population. Medical Care 2003;41:8-20.
9. Alessi CA, Yoon EJ, Schnelle JF, et al. A randomized trial of a combined physical activity and environmental intervention in nursing home residents: do sleep and agitation improve? J Am Geriatr Soc 1999;47:784–91.
10. Cohen-Mansfield J, Marx MS. The relationship between sleep disturbances and agitation in a nursing home. J Aging Health 1990;2:153–65.
11. Rolland Y, Andrieu S, Crochard A, et al. Psychotropic drug consumption at admission and discharge of nursing home residents. J Am Med Dir Assoc 2012;13:407 e407–412.
12. Salzman C. Antipsychotics in nursing homes. J Clin Psychopharmacol 2013;33:1–2.
13. Fleetham J, Ayas N, Bradley D, et al. Canadian Thoracic Society guidelines: diagnosis and treatment of sleep disordered breathing in adults. Can Respir J 2006;13:387–92.
14. International classification of sleep disorders: Chicago: American Academy of Sleep Medicine; 2005.
15. Gay PC. Complex sleep apnea: it really is a disease. J Clin Sleep Med 2008;4:403–5.
16. Ancoli-Israel S. Epidemiology of sleep disorders. In: Roth T, Roehrs TA, editors. Clinics in geriatric medicine. Philadelphia: WB Saunders; 1989:347–62.
17. Gehrman PR, Martin JL, Shochat T, et al. Sleep-disordered breathing and agitation in institutionalized adults with Alzheimer disease. Am J Geriatr Psychiatry 2003;11:426–33.
18. Resnick HE, Phillips B. Documentation of sleep apnea in nursing homes: United States 2004. J Am Med Dir Assoc 2008;9:260–4.
19. Park JG, Ramar K, Olson EJ. Updates on definition, consequences, and management of obstructive sleep apnea. Mayo Clin Proc 2011;86:549–54.
20. Yaggi HK, Concato J, Kernan WN, et al. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med 2005;353:2034–41.
21. McMillan A, Bratton DJ, Faria R, et al. Continuous positive airway pressure in older people with obstructive sleep apnoea syndrome (PREDICT): a 12-month, multicentre, randomised trial. Lancet Resp med 2014;2:804–12.
22. Allen RP, Walters AS, Montplaisir J, et al. Restless legs syndrome prevalence and impact: REST general population study. Arch Intern Med 2005;165:1286–92.
23. Allen RP, La Buda MC, Becker P, et al. Family history study of the restless legs syndrome. Sleep Med 2002;3 Suppl:S3–7.
24. Allen RP. Restless legs syndrome/Willis Ekbom disease: evaluation and treatment. Int Rev Psychiatry 2014;26:248–62.
25. Hening WA, Allen RP, Earley CJ, et al. An update on the dopaminergic treatment of restless legs syndrome and periodic limb movement disorder. Sleep 2004;27:560–83.
26. Gamaldo C, Benbrook AR, Allen RP, et al. Evaluating daytime alertness in individuals with Restless Legs Syndrome (RLS) compared to sleep restricted controls. Sleep Med 2009;10:134–8.
27. Allen RP, Earley CJ. Defining the phenotype of the restless legs syndrome (RLS) using age-of-symptom-onset. Sleep Med 2000;1:11–9.
28. Salas RE, Kwan AB. The real burden of restless legs syndrome: clinical and economic outcomes. Am J Manag Care 2012;18(9 Suppl):S207–212.
29. Silber MH, Ehrenberg BL, Allen RP, et al. An algorithm for the management of restless legs syndrome. Mayo Clin Proc 2004;79:916–22.
30. Hattan E, Chalk C, Postuma RB. Is there a higher risk of restless legs syndrome in peripheral neuropathy? Neurology 2009;72:955–60.
31. Winkelman JW, Chertow GM, Lazarus JM. Restless legs syndrome in end-stage renal disease. Am J Kidney Dis 1996;28:372–8.
32. Hornyak M, Trenkwalder C. Restless legs syndrome and periodic limb movement disorder in the elderly. J Psychosom Res 2004;56:543–8.
33. Ancoli-Israel S, Kripke DF, Klauber MR, et al. Periodic limb movements in sleep in community-dwelling elderly. Sleep 1991;14:496–500.
34. Ahmed QA. Effects of common medications used for sleep disorders. Crit Care Clin 2008;24:493–515, vi.
35. Rye DB, Trotti LM. Restless legs syndrome and periodic leg movements of sleep. Neurol clin 2012;30:1137–66.
36. Gamaldo CE, Chung Y, Kang YM, et al. Tick-tock-tick-tock: the impact of circadian rhythm disorders on cardiovascular health and wellness. J Am Soc Hypertens 2014;8:921–9.
37. Myers BL, Badia P. Changes in circadian rhythms and sleep quality with aging: mechanisms and interventions. Neurosci Biobehav Rev 1995;19:553–71.
38. National Institute on Aging. Alzheimer’s caregiving tips: sundowning. June 2013.
39. International classification of sleep disorders. 3rd ed. Darien, IL: AASD; 2014.
40. Barion A, Zee PC. A clinical approach to circadian rhythm sleep disorders. Sleep Med 2007;8:566–77.
41. Morgenthaler TI, Lee-Chiong T, Alessi C, et al. Practice parameters for the clinical evaluation and treatment of circadian rhythm sleep disorders. An American Academy of Sleep Medicine report. Sleep 2007;30:1445–59.
42. Shochat T, Martin J, Marler M, et al. Illumination levels in nursing home patients: effects on sleep and activity rhythms. J Sleep Res 2000;9:373–9.
43. Ancoli-Israel S, Klauber MR, Jones DW, et al. Variations in circadian rhythms of activity, sleep, and light exposure related to dementia in nursing-home patients. Sleep 1997;20:18–23.
44. Satlin A, Volicer L, Ross V, et al. Bright light treatment of behavioral and sleep disturbances in patients with Alzheimer’s disease. Am J Psychiatry 1992;149:1028–32.
45. Koyama E, Matsubara H, Nakano T. Bright light treatment for sleep-wake disturbances in aged individuals with dementia. Psychiatry Clin Neurosci 1999;53:227–9.
46. Burns A, Allen H, Tomenson B, et al. Bright light therapy for agitation in dementia: a randomized controlled trial. Int Psychogeriatr 2009;21:711–21.
47. Riemersma-van der Lek RF, Swaab DF, Twisk J, et al. Effect of bright light and melatonin on cognitive and noncognitive function in elderly residents of group care facilities: a randomized controlled trial. JAMA 2008;299:2642–55.
48. Martin JL, Marler MR, Harker JO, et al. A multicomponent nonpharmacological intervention improves activity rhythms among nursing home residents with disrupted sleep/wake patterns. J Gerontol Series A Biol Sci Med Sci 2007;62:67–72.
49. Lewy AJ, Ahmed S, Jackson JM, et al. Melatonin shifts human circadian rhythms according to a phase-response curve. Chronobiol Int 1992;9:380–92.
50. Williamson BL, Tomlinson AJ, Mishra PK, et al. Structural characterization of contaminants found in commercial preparations of melatonin: similarities to case-related compounds from L-tryptophan associated with eosinophilia-myalgia syndrome. Chem Res Toxicol 1998;11:234-40.
51. Czeisler CA, Walsh JK, Roth T, et al. Modafinil for excessive sleepiness associated with shift-work sleep disorder. N Engl J Med 2005;353:476-86.
52. Howard R, Roth T, Drake CL. The effects of armodafinil on objective sleepiness and performance in a shift work disorder sample unselected for objective sleepiness. J Clin Psychopharmacol 2014;34:369–73.
53. Beydoun MA, Gamaldo AA, Beydoun HA, et al. Caffeine and alcohol intakes and overall nutrient adequacy are associated with longitudinal cognitive performance among U.S. adults. J Nutr 2014;144:890–901.
54. Pentel P. Toxicity of over-the-counter stimulants. JAMA 1984;252:1898–903.
55. Neikrug AB, Ancoli-Israel S. Sleep disorders in the older adult - a mini-review. Gerontology 2010;56:181–9.
56. Chesson A Jr, Hartse K, Anderson WM, et al. Practice parameters for the evaluation of chronic insomnia. An American Academy of Sleep Medicine report. Standards of Practice Committee of the American Academy of Sleep Medicine. Sleep 2000;23:237–41.
57. Bastien CH, Vallieres A, Morin CM. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med 2001;2:297–307.
58. Buysse DJ, Reynolds CF 3rd, Monk TH, et al. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 1989;28:193–213.
59. Trauer JM, Qian MY, Doyle JS, et al. Cognitive behavioral therapy for chronic insomnia: a systematic review and meta-analysis. Ann Intern Med 2015;163:191–204.
60. National Institutes of Health State of the Science Conference statement on manifestations and management of chronic insomnia in adults, June 13-15, 2005. Sleep 2005;28:1049–57.
61. Schutte-Rodin S, Broch L, Buysse D, et al. Clinical guideline for the evaluation and management of chronic insomnia in adults. J Clin Sleep Med 2008;4:487–504.
62. Bain KT. Management of chronic insomnia in elderly persons. Am J Geriatr Pharmacother 2006;4:168–92.
63. FDA approves new type of sleep drug, Belsomra. 13 Aug 2014. Available at fda.gov.
64. Dubey AK, Handu SS, Mediratta PK. Suvorexant: The first orexin receptor antagonist to treat insomnia. J Pharmacol Pharmacother 2015;6:118–21.
65. Patel KV, Aspesi AV, Evoy KE. Suvorexant: a dual orexin receptor antagonist for the treatment of sleep onset and sleep maintenance insomnia. Ann Pharmacother 2015;49:477–83.
66. Michelson D, Snyder E, Paradis E, et al. Safety and efficacy of suvorexant during 1-year treatment of insomnia with subsequent abrupt treatment discontinuation: a phase 3 randomised, double-blind, placebo-controlled trial. Lancet Neurol 2014;13:461–71.
67. Bootzin RR, Epstein D, Wood JM. Stimulus control instructions. Case studies in insomnia. New York: Springer; 1991:19–28.
68. Gulyani S, Salas RE, Gamaldo CE. Sleep medicine pharmacotherapeutics overview: today, tomorrow, and the future (part 2: hypersomnia, parasomnia, and movement disorders). Chest 2013;143:242–51.
69. Boeve BF, Silber MH, Saper CB, et al. Pathophysiology of REM sleep behaviour disorder and relevance to neurodegenerative disease. Brain 2007;130(Pt 11):2770–88.
70. Middelkoop HA, Kerkhof GA, Smilde-van den Doel DA, et al. Sleep and ageing: the effect of institutionalization on subjective and objective characteristics of sleep. Age Ageing 1994;23:411–7.
71. Tinuper P, Provini F, Bisulli F, et al. Movement disorders in sleep: guidelines for differentiating epileptic from non-epileptic motor phenomena arising from sleep. Sleep Med Rev 2007;11:255–67.
72. Aurora RN, Zak RS, Maganti RK, et al. Best practice guide for the treatment of REM sleep behavior disorder (RBD). J Clin Sleep Med 2010;6:85–95.
73. Bloom HG, Ahmed I, Alessi CA, et al. Evidence-based recommendations for the assessment and management of sleep disorders in older persons. J Am Geriatr Soc 2009;57:761–89.
74. Anderson KN, Shneerson JM. Drug treatment of REM sleep behavior disorder: the use of drug therapies other than clonazepam. J Clin Sleep Med 2009;5:235–9.
75. Doshi A, Gamaldo C, Kalloo A, et al. Implementing a clinical iPad application to detect sleep disorders is feasible across multiple non-sleep outpatient clinics (P7. 321). Neurology 2015;84(14 Suppl):P7.321.
1. Federal Interagency Forum on Aging-Related Statistics. Older Americans 2012: Key indicators of well-being. Washington, DC: U.S. Gov. Printing Office; 2012.
2. Almeida OP, Pfaff JJ. Sleep complaints among older general practice patients: association with depression. Br J Gen Pract 2005;55:864–866.
3. Wolkove N, Elkholy O, Baltzan M, et al. Sleep and aging: 1. Sleep disorders commonly found in older people. CMAJ 2007;176:1299–304.
4. Pace-Schott EF, Spencer RM. Age-related changes in the cognitive function of sleep. Prog Brain Res 2011;191:75–89.
5. Ohayon MM, Carskadon MA, Guilleminault C, et al. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep 2004;27:1255–73.
6. Jacobs D, Ancoli-Israel S, Parker L, et al. Twenty-four-hour sleep-wake patterns in a nursing home population. Psychol Aging 1989;4:352–6.
7. Neikrug AB, Ancoli-Israel S. Sleep disturbances in nursing homes. J Nutr Health Aging 2010;14:207–11.
8. Lakdawalla D, Goldman DP, Bhattacharya J, et al. Forecasting the nursing home population. Medical Care 2003;41:8-20.
9. Alessi CA, Yoon EJ, Schnelle JF, et al. A randomized trial of a combined physical activity and environmental intervention in nursing home residents: do sleep and agitation improve? J Am Geriatr Soc 1999;47:784–91.
10. Cohen-Mansfield J, Marx MS. The relationship between sleep disturbances and agitation in a nursing home. J Aging Health 1990;2:153–65.
11. Rolland Y, Andrieu S, Crochard A, et al. Psychotropic drug consumption at admission and discharge of nursing home residents. J Am Med Dir Assoc 2012;13:407 e407–412.
12. Salzman C. Antipsychotics in nursing homes. J Clin Psychopharmacol 2013;33:1–2.
13. Fleetham J, Ayas N, Bradley D, et al. Canadian Thoracic Society guidelines: diagnosis and treatment of sleep disordered breathing in adults. Can Respir J 2006;13:387–92.
14. International classification of sleep disorders: Chicago: American Academy of Sleep Medicine; 2005.
15. Gay PC. Complex sleep apnea: it really is a disease. J Clin Sleep Med 2008;4:403–5.
16. Ancoli-Israel S. Epidemiology of sleep disorders. In: Roth T, Roehrs TA, editors. Clinics in geriatric medicine. Philadelphia: WB Saunders; 1989:347–62.
17. Gehrman PR, Martin JL, Shochat T, et al. Sleep-disordered breathing and agitation in institutionalized adults with Alzheimer disease. Am J Geriatr Psychiatry 2003;11:426–33.
18. Resnick HE, Phillips B. Documentation of sleep apnea in nursing homes: United States 2004. J Am Med Dir Assoc 2008;9:260–4.
19. Park JG, Ramar K, Olson EJ. Updates on definition, consequences, and management of obstructive sleep apnea. Mayo Clin Proc 2011;86:549–54.
20. Yaggi HK, Concato J, Kernan WN, et al. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med 2005;353:2034–41.
21. McMillan A, Bratton DJ, Faria R, et al. Continuous positive airway pressure in older people with obstructive sleep apnoea syndrome (PREDICT): a 12-month, multicentre, randomised trial. Lancet Resp med 2014;2:804–12.
22. Allen RP, Walters AS, Montplaisir J, et al. Restless legs syndrome prevalence and impact: REST general population study. Arch Intern Med 2005;165:1286–92.
23. Allen RP, La Buda MC, Becker P, et al. Family history study of the restless legs syndrome. Sleep Med 2002;3 Suppl:S3–7.
24. Allen RP. Restless legs syndrome/Willis Ekbom disease: evaluation and treatment. Int Rev Psychiatry 2014;26:248–62.
25. Hening WA, Allen RP, Earley CJ, et al. An update on the dopaminergic treatment of restless legs syndrome and periodic limb movement disorder. Sleep 2004;27:560–83.
26. Gamaldo C, Benbrook AR, Allen RP, et al. Evaluating daytime alertness in individuals with Restless Legs Syndrome (RLS) compared to sleep restricted controls. Sleep Med 2009;10:134–8.
27. Allen RP, Earley CJ. Defining the phenotype of the restless legs syndrome (RLS) using age-of-symptom-onset. Sleep Med 2000;1:11–9.
28. Salas RE, Kwan AB. The real burden of restless legs syndrome: clinical and economic outcomes. Am J Manag Care 2012;18(9 Suppl):S207–212.
29. Silber MH, Ehrenberg BL, Allen RP, et al. An algorithm for the management of restless legs syndrome. Mayo Clin Proc 2004;79:916–22.
30. Hattan E, Chalk C, Postuma RB. Is there a higher risk of restless legs syndrome in peripheral neuropathy? Neurology 2009;72:955–60.
31. Winkelman JW, Chertow GM, Lazarus JM. Restless legs syndrome in end-stage renal disease. Am J Kidney Dis 1996;28:372–8.
32. Hornyak M, Trenkwalder C. Restless legs syndrome and periodic limb movement disorder in the elderly. J Psychosom Res 2004;56:543–8.
33. Ancoli-Israel S, Kripke DF, Klauber MR, et al. Periodic limb movements in sleep in community-dwelling elderly. Sleep 1991;14:496–500.
34. Ahmed QA. Effects of common medications used for sleep disorders. Crit Care Clin 2008;24:493–515, vi.
35. Rye DB, Trotti LM. Restless legs syndrome and periodic leg movements of sleep. Neurol clin 2012;30:1137–66.
36. Gamaldo CE, Chung Y, Kang YM, et al. Tick-tock-tick-tock: the impact of circadian rhythm disorders on cardiovascular health and wellness. J Am Soc Hypertens 2014;8:921–9.
37. Myers BL, Badia P. Changes in circadian rhythms and sleep quality with aging: mechanisms and interventions. Neurosci Biobehav Rev 1995;19:553–71.
38. National Institute on Aging. Alzheimer’s caregiving tips: sundowning. June 2013.
39. International classification of sleep disorders. 3rd ed. Darien, IL: AASD; 2014.
40. Barion A, Zee PC. A clinical approach to circadian rhythm sleep disorders. Sleep Med 2007;8:566–77.
41. Morgenthaler TI, Lee-Chiong T, Alessi C, et al. Practice parameters for the clinical evaluation and treatment of circadian rhythm sleep disorders. An American Academy of Sleep Medicine report. Sleep 2007;30:1445–59.
42. Shochat T, Martin J, Marler M, et al. Illumination levels in nursing home patients: effects on sleep and activity rhythms. J Sleep Res 2000;9:373–9.
43. Ancoli-Israel S, Klauber MR, Jones DW, et al. Variations in circadian rhythms of activity, sleep, and light exposure related to dementia in nursing-home patients. Sleep 1997;20:18–23.
44. Satlin A, Volicer L, Ross V, et al. Bright light treatment of behavioral and sleep disturbances in patients with Alzheimer’s disease. Am J Psychiatry 1992;149:1028–32.
45. Koyama E, Matsubara H, Nakano T. Bright light treatment for sleep-wake disturbances in aged individuals with dementia. Psychiatry Clin Neurosci 1999;53:227–9.
46. Burns A, Allen H, Tomenson B, et al. Bright light therapy for agitation in dementia: a randomized controlled trial. Int Psychogeriatr 2009;21:711–21.
47. Riemersma-van der Lek RF, Swaab DF, Twisk J, et al. Effect of bright light and melatonin on cognitive and noncognitive function in elderly residents of group care facilities: a randomized controlled trial. JAMA 2008;299:2642–55.
48. Martin JL, Marler MR, Harker JO, et al. A multicomponent nonpharmacological intervention improves activity rhythms among nursing home residents with disrupted sleep/wake patterns. J Gerontol Series A Biol Sci Med Sci 2007;62:67–72.
49. Lewy AJ, Ahmed S, Jackson JM, et al. Melatonin shifts human circadian rhythms according to a phase-response curve. Chronobiol Int 1992;9:380–92.
50. Williamson BL, Tomlinson AJ, Mishra PK, et al. Structural characterization of contaminants found in commercial preparations of melatonin: similarities to case-related compounds from L-tryptophan associated with eosinophilia-myalgia syndrome. Chem Res Toxicol 1998;11:234-40.
51. Czeisler CA, Walsh JK, Roth T, et al. Modafinil for excessive sleepiness associated with shift-work sleep disorder. N Engl J Med 2005;353:476-86.
52. Howard R, Roth T, Drake CL. The effects of armodafinil on objective sleepiness and performance in a shift work disorder sample unselected for objective sleepiness. J Clin Psychopharmacol 2014;34:369–73.
53. Beydoun MA, Gamaldo AA, Beydoun HA, et al. Caffeine and alcohol intakes and overall nutrient adequacy are associated with longitudinal cognitive performance among U.S. adults. J Nutr 2014;144:890–901.
54. Pentel P. Toxicity of over-the-counter stimulants. JAMA 1984;252:1898–903.
55. Neikrug AB, Ancoli-Israel S. Sleep disorders in the older adult - a mini-review. Gerontology 2010;56:181–9.
56. Chesson A Jr, Hartse K, Anderson WM, et al. Practice parameters for the evaluation of chronic insomnia. An American Academy of Sleep Medicine report. Standards of Practice Committee of the American Academy of Sleep Medicine. Sleep 2000;23:237–41.
57. Bastien CH, Vallieres A, Morin CM. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med 2001;2:297–307.
58. Buysse DJ, Reynolds CF 3rd, Monk TH, et al. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 1989;28:193–213.
59. Trauer JM, Qian MY, Doyle JS, et al. Cognitive behavioral therapy for chronic insomnia: a systematic review and meta-analysis. Ann Intern Med 2015;163:191–204.
60. National Institutes of Health State of the Science Conference statement on manifestations and management of chronic insomnia in adults, June 13-15, 2005. Sleep 2005;28:1049–57.
61. Schutte-Rodin S, Broch L, Buysse D, et al. Clinical guideline for the evaluation and management of chronic insomnia in adults. J Clin Sleep Med 2008;4:487–504.
62. Bain KT. Management of chronic insomnia in elderly persons. Am J Geriatr Pharmacother 2006;4:168–92.
63. FDA approves new type of sleep drug, Belsomra. 13 Aug 2014. Available at fda.gov.
64. Dubey AK, Handu SS, Mediratta PK. Suvorexant: The first orexin receptor antagonist to treat insomnia. J Pharmacol Pharmacother 2015;6:118–21.
65. Patel KV, Aspesi AV, Evoy KE. Suvorexant: a dual orexin receptor antagonist for the treatment of sleep onset and sleep maintenance insomnia. Ann Pharmacother 2015;49:477–83.
66. Michelson D, Snyder E, Paradis E, et al. Safety and efficacy of suvorexant during 1-year treatment of insomnia with subsequent abrupt treatment discontinuation: a phase 3 randomised, double-blind, placebo-controlled trial. Lancet Neurol 2014;13:461–71.
67. Bootzin RR, Epstein D, Wood JM. Stimulus control instructions. Case studies in insomnia. New York: Springer; 1991:19–28.
68. Gulyani S, Salas RE, Gamaldo CE. Sleep medicine pharmacotherapeutics overview: today, tomorrow, and the future (part 2: hypersomnia, parasomnia, and movement disorders). Chest 2013;143:242–51.
69. Boeve BF, Silber MH, Saper CB, et al. Pathophysiology of REM sleep behaviour disorder and relevance to neurodegenerative disease. Brain 2007;130(Pt 11):2770–88.
70. Middelkoop HA, Kerkhof GA, Smilde-van den Doel DA, et al. Sleep and ageing: the effect of institutionalization on subjective and objective characteristics of sleep. Age Ageing 1994;23:411–7.
71. Tinuper P, Provini F, Bisulli F, et al. Movement disorders in sleep: guidelines for differentiating epileptic from non-epileptic motor phenomena arising from sleep. Sleep Med Rev 2007;11:255–67.
72. Aurora RN, Zak RS, Maganti RK, et al. Best practice guide for the treatment of REM sleep behavior disorder (RBD). J Clin Sleep Med 2010;6:85–95.
73. Bloom HG, Ahmed I, Alessi CA, et al. Evidence-based recommendations for the assessment and management of sleep disorders in older persons. J Am Geriatr Soc 2009;57:761–89.
74. Anderson KN, Shneerson JM. Drug treatment of REM sleep behavior disorder: the use of drug therapies other than clonazepam. J Clin Sleep Med 2009;5:235–9.
75. Doshi A, Gamaldo C, Kalloo A, et al. Implementing a clinical iPad application to detect sleep disorders is feasible across multiple non-sleep outpatient clinics (P7. 321). Neurology 2015;84(14 Suppl):P7.321.