User login
5 tips for talking to patients about postpartum sexuality
Related article How to prepare your patient for the many nuances of postpartum sexuality (January 2012)
Related article How to prepare your patient for the many nuances of postpartum sexuality (January 2012)
Related article How to prepare your patient for the many nuances of postpartum sexuality (January 2012)
How to prepare your patient for the many nuances of postpartum sexuality
CASE: Waiting for an OK to resume sex
L. L. is a 29-year-old woman, G1P1, who delivered a healthy infant 4 weeks ago by spontaneous vaginal birth. The delivery involved a 2-day induction of labor for preeclampsia and a second-degree tear that was repaired without complication. The patient also experienced postpartum hemorrhage that was managed with bimanual massage and uterotonics and for which she ultimately required transfusion of blood products. Her hospital course was otherwise unremarkable.
Before pregnancy, L. L. had a normal medical history and conceived spontaneously. Her antenatal course was uncomplicated.
Today, she returns for her postpartum visit. She reports being tired and says she still has some pain at the site of the tear, but reports no problems with urinary or fecal continence. She denies being depressed, and her Edinburgh Postnatal Depression Scale (EPDS) score is consistent with that report. She is breastfeeding and appears to be doing well on the progestin-only pill for contraception. She has not yet attempted intercourse because she is complying with instructions to wait until she sees you for her postpartum visit.
How should you counsel her about resuming sexual activity?

Childbirth is a central event in a woman’s life. Pregnancy and delivery are a time of psychological, biological, and physical transformation, and the postpartum period—the “fourth trimester”—is no exception. Sexual function may be affected. In fact, many women who seek assistance for sexual dissatisfaction note that their problem arose in the postpartum period.1
Postpartum sexuality involves considerably more than the physical act of genital stimulation—with or without intromission or penile penetration—and depends on more than the physical state of recovery of the vagina (after vaginal delivery). It also depends on:
- the woman’s sexual drive and motivation
- her general state of health and quality of life
- her emotional readiness to resume sexual intimacy with a partner
- her adaptation to the maternal role and ability to balance her identity as a mother with her identity as a sexual being
- her relationship with her partner.
Given all these contributing factors, many of which fall outside the scope of the clinical practice of obstetrics and gynecology, how do we go about counseling our patients about the resumption of sexual activity?
Other questions:
- How can we help patients manage expectations about the quality of their postpartum sexual function?
- What guidance can we provide regarding the interplay of psychosexual and physical aspects of the puerperium?
- Can we offer a method of screening for sexual dysfunction in the puerperium? If so, will it help prevent sexual problems or hasten their resolution?
This article addresses these issues. Ultimately, the answer to the question of when to resume sexual activity should reflect an awareness of cultural norms and taboos as well as familiarity with empirically based recommendations.
Traditional postpartum sexual education is not evidence-based and has limited effectiveness. More up-to-date strategies can be easily incorporated into even the busiest clinical practice. We offer the following counseling model for you to consider when addressing the sexual health of patients postpartum.
Educate, legitimize, and normalize
The first sexual encounter after childbirth can be an important step for couples to reclaim their intimate relationship.
Adaptation to the parental role, physical healing, hormonal changes, breastfeeding, and sleep deprivation contribute to a profound psychosocial challenge. The resumption of sexual activities and a satisfying postpartum sex life depend on many variables, many of which the patient may not even be aware.
First, do not assume that all patients are heterosexual and that intercourse is their only form of sexual activity.
Second, it is important to be proactive in antepartum and postpartum counseling and to offer anticipatory guidance. Counseling can take place any time during routine prenatal care, as well as at the time of hospital discharge and the postpartum visit.
Reassure the patient that, if sexual activity and frequency are lower during pregnancy and the postpartum period, it is likely a normal transition. Also give the patient time to talk about her expectations and perceptions. Explain to her the normal fluctuations and variability of sexual interest and enjoyment in pregnancy and the puerperium, and suggest that she consider alternative options for intimate expression, non-coital sexual activities, and mutual pleasure within her cultural context.
Be thorough
Take a comprehensive medical, obstetric, psychological, and social history as part of the sexual history. Also perform a physical intake and exam. Questions about urinary and fecal incontinence ought to be part of all postpartum assessment.
Other potential areas to address include the quality of the relationship, prepregnancy sexual function, the support network, planned or unplanned state of the pregnancy, previous pregnancy and delivery outcomes, the health status of current children, and present, previous, and future contraceptive use.29
Consider multiple visits
It is hard to know exactly when to evaluate a patient for postpartum sexual dysfunction, given the impact of pudendal nerve latency, fatigue, and breastfeeding. For this reason, assessment on multiple occasions may be appropriate. Numerous validated scales to assess sexual function can be easily incorporated into clinical practice.
Couples counseling and therapy may be needed in some cases; be aware of referral services in your area for sexual wellness specialists.
The bottom line: A “successful” sexual life does not necessarily mean adequate genital function (e.g., coital orgasm, improved clitoral blood flow, increased sexual frequency) but, rather, a sexual life that is intimate and satisfying to the individual patient.
A paucity of research
To date, research into sexuality during the postpartum period has focused primarily on the physical changes and constraints that affect the mechanics and frequency of intercourse and overall sexual satisfaction and desire.2 This perspective has begun to broaden to include the psychological aspects of sexuality.
TABLE 1
These validated tools can help you measure female sexual dysfunction
| Tool | Area assessed |
|---|---|
| Female Sexual Function Index (FSFI)30 | Desire, arousal, orgasm, and pain |
| Female Sexual Function Index 6-Item (FSFI-6)31 | Desire, arousal, orgasm, and pain |
| McCoy Female Sexual Function Questionnaire*32 | Presence of female sexual disorders |
| Brief Sexual Symptoms Checklist33 | Screener for sexual concerns |
| Female Sexual Distress Scale – Revised34 | Distress |
| Intimate Relationship Scale*35 | Changes in sexual relationship |
| Sexual Quality of Life – Female (SQol-F)36 | Quality of life in women with female sexual dysfunction |
| Golombok Rust Inventory of Sexual Satisfaction (GRISS)37 | Quality of sexual relationship |
| Decreased Sexual Desire Screener38 | Brief diagnostic tool for hypoactive sexual desire disorder |
| * Validated in pregnant and/or postpartum women | |
Women’s sexual health during the postpartum period has generally been under-researched. It wasn’t until the past decade that validated sexual function questionnaires were utilized. Although a number of these instruments are now available (TABLE 1, TABLE 2, FIGURE), it remains unclear whether they can accurately measure postpartum sexual function. Despite these limitations, significant information has been elicited that can be used to counsel patients struggling with postpartum sexual concerns.
TABLE 2
The 6-item Female Sexual Function Index*
| Question | Responses | |||||
|---|---|---|---|---|---|---|
| 0 points | 5 points | 4 points | 3 points | 2 points | 1 point | |
| How would you rate your level of sexual desire or interest? | No sexual activity | Very high | High | Moderate | Low | Very low or none at all |
| How would you rate your level of sexual arousal (“turn on”) during sexual activity or intercourse? | No sexual activity | Very high | High | Moderate | Low | Very low or none at all |
| How often did you become lubricated (“wet”) during sexual activity or intercourse? | No sexual activity | Almost always or always | Most times | Sometimes | A few times | Almost never or never |
| When you had sexual stimulation or intercourse, how often did you reach orgasm? | No sexual activity | Almost always or always | Most times | Sometimes | A few times | Almost never or never |
| How satisfied have you been overall with your sexual life? | No sexual activity | Very satisfied | Moderately satisfied | About equally satisfied and dissatisfied | Moderately dissatisfied | Very dissatisfied |
| How often did you experience discomfort or pain during vaginal penetration? | Did not attempt intercourse | Almost never or never | A few times | Sometimes | Most times | Almost always or always |
| *The components of this index are to be assessed over the past 4 weeks. The score is the sum of the ordinal responses to the 6 items and ranges from 2 to 30. A score of less than 19 indicates a need for further investigation, including the full-length Female Sexual Function Index. Source: Adapted from Isidori et al.31 | ||||||
Ideal period of abstinence is unknown
Although our knowledge of the female genital tract in the puerperium is based upon histologic evidence, there are no evidence-based policies to outline the ideal period of postpartum coital abstinence. It seems reasonable to assume that our traditional scientific recommendations developed in part to prevent uterine infection and disruption of sutured wounds. These concerns, combined with cultural and societal norms, have led to the routine discouragement of sexual activity until 4 to 6 weeks postpartum.
The possibility of shortening the period of postpartum abstinence was first suggested by the American College of Obstetricians and Gynecologists (ACOG) in 1984.1 In 1985, Pritchard and colleagues wrote about the individualization of postpartum prohibitions of sexual activity in Williams Obstetrics.1 The earliest time at which intercourse may be safely resumed is unknown, but the 23rd edition of Williams Obstetrics states that a woman can resume sexual intercourse as early as 2 weeks, based on her comfort and desire.3 The sixth edition of the American Academy of Pediatrics (AAP) and ACOG guidelines for perinatal care also states that the risks ought to be minimal at 2 weeks postpartum.4
BRIEF SEXUAL SYMPTOMS CHECKLIST FOR WOMEN (BSSC-W)
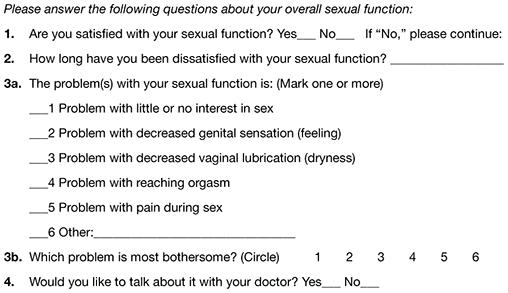
Reprinted from Hatzichristou et al. 33
Low desire is not unusual
Although a patient may be granted “permission” to engage in coital activity, other variables influence her decision. It is well known that sexual desire may fluctuate during pregnancy and typically decreases significantly during the third trimester.2 Many women enter the postpartum period with lower levels of sexual desire and satisfaction, and these depressed levels may continue for some time.2 Twenty-five percent of women report worsened sexual function, including diminished sexual satisfaction, during pregnancy that persists for 6 to 12 months postpartum.5 By 12 weeks postpartum, 80% to 93% of women have resumed intercourse, but as many as 83% report sexual problems during the first 3 months of the postpartum period. At 6 months, 18% to 30% of these women may still be experiencing sexual problems, including dyspareunia.5,6
In 1998, von Sydow performed a meta-content analysis of all existing studies on parental sexuality during pregnancy and the first 6 months postpartum.7 Using psychological and medical data banks, she brought together information from two branches of science and identified 59 relevant studies in English or German between 1950 and 1996. Although the majority of studies were retrospective and failed to utilize a validated instrument, von Sydow determined that, overall, sexual interest and activity were low or nonexistent during the first months after delivery. There was high variability between individuals, however, and levels of sexual interest and activity of individual women remained relatively constant from the time before pregnancy until 1 year postpartum.7 von Sydow determined that there is great variability in female sexuality during pregnancy and postpartum; this variability may represent fluctuations during this phase of life. She also determined that severe psychosexual and marital problems are much more prevalent in the postpartum period than during pregnancy and persist long after a physical cause can be used as an explanation.7
Fatigue and quality of the relationship have an impact on sexual function
De Judicibus and colleagues identified a broad range of variables that have a detrimental impact on sexuality at 12 weeks postpartum, most particularly:
- marital dissatisfaction
- dyspareunia
- fatigue
- depression
- breastfeeding.2
There is evidence to suggest that the addition of the first child reduces marital quality after the first month postpartum, and this decline in marital satisfaction continues for 6 to 18 months postpartum.2 Witting and coworkers suggested that this decline may represent a transitional phase of parenthood for some couples; data support the positive effects on overall marital satisfaction with the addition of children.8 Women who were more satisfied with their relationships reported higher sexual satisfaction and greater frequency of intercourse.2,8
Fatigue is one of the most common problems women experience during pregnancy and postpartum and is a common reason given for loss of sexual desire and interest, infrequent sexual activity, and lack of enjoyment.5 A high level of exhaustion is found during the first 8 weeks postpartum. Although it declines over the next 6 months, it does not appear to resolve completely in a good number of women.9
Don’t underestimate the impact of obstetric morbidity
Surprisingly, the long-term impact of severe obstetric events on postpartum maternal health is often overlooked. Waterstone and colleagues found that women who have severe obstetric morbidity, such as massive hemorrhage, preeclampsia, sepsis, and uterine rupture, experience significant changes in sexual health and well-being.10 They conducted a prospective cohort study of such women, measuring sexual activity, general health, and postpartum depression. They utilized two validated postnatal questionnaires—the Short Form 36 (SF-36) to measure general health and the EPDS. Women who had uncomplicated pregnancies and childbirth tended to perform well in most SF-36 categories, whereas women who had experienced severe morbidity scored worse in almost every category. These women also reported problems with intercourse. Thirteen percent of women had not resumed sexual relations by 6 to 12 months postpartum; of these women, more than half reported a fear of conceiving as a reason.
The female body undergoes dramatic physiologic, anatomic, and psychological changes immediately following delivery and throughout the restoration of its pre-pregnant state. This fourth trimester usually lasts 6 to 12 weeks.39
Uterus. The uterus undergoes rapid involution after separation of the placenta. By 2 to 4 weeks postpartum, it may no longer be palpable abdominally, and by 6 weeks, it usually has returned to its nonpregnant state and size. Seven to 14 days after delivery, a woman often experiences an episode of heavier vaginal bleeding that corresponds with the sloughing of the placental bed eschar. During this time of involution, myometrial vessels may be 5 mm or larger in diameter.40
Lochia. The postpartum lochia begins to change within days of birth, transitioning through its stages of lochia rubra, serosa, and alba. It decreases by 3 weeks postpartum and is likely completely resolved by 6 weeks.
Prolactin is responsible for lactogenesis. When the prolactin level is maintained through breastfeeding, it depresses ovarian production of estrogen by suppressing pituitary gonadotropin secretion, triggering a period of “steroid starvation” after the loss of estrogen and progesterone production from the placenta.1
Vagina. Early in the postpartum period, the vagina is typically edematous and lax and, as a result of parturition, there may be not only a spontaneous tear or episiotomy that must heal, but superficial small tears that do not require suturing. Ruggae begin to reappear by 3 weeks, and the vaginal epithelium will begin to mature under the influence of estrogen production. Much of this tissue damage is healed by 6 weeks postpartum.
The perception of pregnant and postpartum women’s sexuality varies, based on religious and cultural norms. In some religions and cultures, sexual activity is forbidden for 2 to 3 months postpartum; in others, it is prohibited until the child is weaned from the breast. The postpartum woman and lochia have traditionally been perceived as unclean, and many religions have specific proscriptions regarding the management of this time in a woman’s life.1 Although early cultures did not study these issues specifically, their doctrines suggest that they had some awareness of the natural physiologic transition of a woman’s body after she has given birth.
Exploring the role of body image
Paul and coworkers prospectively assessed female sexual function, body image, and pelvic symptoms from the first trimester until 6 months postpartum.11 They utilized the validated questionnaire instruments of the Female Sexual Function Index (FSFI), the Body Exposure during Sexual Activities Questionnaire (BESAQ), the short forms of the Urogenital Distress Inventory (UDI-6), the Incontinence Impact Questionnaire (IIQ-7), and the Fecal Incontinence Quality of Life Scale (FIQOL). They found that sexual activity and sexual function scores were highest before pregnancy, declined between the first and third trimesters, and did not return to pre-pregnancy baselines even by 6 months postpartum.11
Differences in sexual practices contributed to these patterns. Kissing, fondling, and vaginal intercourse remained stable across pregnancy, whereas oral sex, breast stimulation, and masturbation declined in the third trimester.
The decline of these activities during pregnancy and postpartum has been seen in other studies as well.12
Obstacles to sexual activity also changed across pregnancy and the postpartum period. Vaginal pain was more problematic in the third trimester and postpartum, whereas feelings of unattractiveness and issues of body image were present throughout pregnancy and at their worst in the postpartum period. Sexual function scores based on the FSFI declined during pregnancy and did not return to pre-pregnancy or first-trimester levels by 6 months postpartum. Urinary symptoms, as measured by the UDI-6, were associated with lower sexual function scores during the postpartum period. The association between urinary incontinence and sexual dysfunction has been seen in other studies.13,14
The enduring effects of perineal trauma
Childbirth may physically affect a woman’s sexual function through perineal trauma, pudendal neuropathy, and vaginal dryness associated with breastfeeding. There is an obvious connection between perineal laceration and perineal pain and problems with intercourse.5 Overall, dyspareunia is reported by 41% to 67% of women 2 to 3 months after delivery.15 Women who have an episiotomy complain of increased perineal pain and delayed return of sexual activity, compared with women who deliver with an intact perineum.16
Persistent dyspareunia is strongly associated with the severity of perineal trauma and operative vaginal delivery.3,17 Multiple studies have investigated this association and found a positive correlation 3 to 6 months postpartum,6,9,17 but the long-term effects and association remain unclear.18
Findings from research. Rogers and colleagues prospectively studied the effect of perineal trauma on postpartum sexual function in a midwifery population of women who had a low rate of episiotomy and operative vaginal delivery.6 They utilized the Intimate Relationship Scale (IRS), a validated questionnaire to measure postpartum sexual function in couples. Most women in this study had resumed sexual activity by 3 months postpartum and did not have postpartum inactivity or dysfunction, based on their IRS scores. However, women who were identified as having experienced major trauma (second-, third-, or fourth-degree laceration or a repaired first-degree laceration) had significantly less desire to engage in activities such as touching and stroking with their partner.6
Present-day limits on the routine use of episiotomy and operative vaginal delivery have yielded a lower rate of third- and fourth-degree laceration.19 Second-degree lacerations are common and constitute the majority of perineal trauma in births without episiotomy.20 There is evidence that the use of synthetic absorbable suture, such as polyglactin, rather than chromic suture, results in less postpartum perineal pain, as does leaving the well-approximated perineal skin edges unsutured.20
Signorello and coworkers found that second-, third-, and fourth-degree lacerations increased the risk of postpartum dyspareunia; operative vaginal delivery (forceps or vacuum) was also an independent risk factor for dyspareunia.21
The impact of route of delivery
Some researchers have concluded that the route of delivery has an impact on the long-term pelvic floor health of women.18 In 1986, Snooks and colleagues analyzed possible obstetric risk factors for damage to the innervation of the pelvic floor, which can lead to both stress urinary and anorectal incontinence.22 They found that the process of vaginal delivery causes a compression and stretch type of injury to the pudendal nerve, as well as the possibility of severe perineal lacerations. This injury may be less likely to occur when cesarean delivery is performed before labor, avoiding direct perineal trauma and possible pudendal neuropathy.15 Because the pudendal nerve mediates some of the reflex pathways in the female sexual response, it is plausible that damage to it could result in sexual dysfunction.
Women who deliver vaginally have a higher rate of fecal and urinary incontinence than women who deliver by cesarean.16,23 The presence of incontinence, however, does not always have a significant long-term effect on one’s sexual life.6
In the Term Breech Trial, the route of delivery had no impact on the resumption of intercourse, dyspareunia, or sexual satisfaction.23 Although the trial was randomized and controlled, it had many limitations that call its generalizability into question in regard to postpartum sexual dysfunction.
The National Institutes of Health (NIH) State-of-the-Science Conference on Cesarean Delivery on Maternal Request indicated that, by 6 months postpartum, there is no difference in sexual function based on the route of delivery.24 However, Lydon-Rochelle and colleagues used the SF-36 to assess reported general health status and found that women who had cesarean delivery or assisted vaginal delivery exhibited significantly poorer postpartum functional status than women who had spontaneous vaginal delivery in five areas at 7 weeks postpartum: physical functioning, mental health, general health perception, bodily pain, social functioning, and ability to perform daily activities.25 Women were more likely to be readmitted to the hospital and more likely to report fatigue during the first 2 months after cesarean delivery.9 It appears that women who undergo cesarean delivery have an elevated risk of nondyspareunia-related causes of sexual dysfunction. Any protective effect of cesarean on sexual function is limited to the early postnatal period and is related to the absence of perineal injury.18
How breastfeeding can affect sexual desire
Evidence is strong that breastfeeding reduces a woman’s sexual desire and the frequency of intercourse.1,5 A high level of prolactin suppresses ovarian production of estrogen, thereby reducing vaginal lubrication. Some women and their partner may identify this loss of lubrication as a lack of arousal. This type of vaginal dryness should be explained, and the use of a lubricant should be encouraged in breastfeeding women.
Nipple sensitivity may develop, making touching and foreplay uncomfortable in some women. One third to one half of mothers find breastfeeding to be an erotic experience, and one fourth feel guilty about this sexual excitement; others stop nursing or wean early due to these feelings.1,7 Women are often not educated about the relationship between the release of oxytocin, uterine contractions, milk ejection, sexual arousal, and orgasm; raising the subject can help to diminish any potential distress over this response.
Sleep disturbances from feeding on demand contribute to fatigue and exhaustion.
Many women may not realize that their loss of interest in sex may be because they are receiving sufficient physical contact or touching through their nurturing interactions with the baby. This may leave the partner feeling isolated and envious of the mother-baby relationship.
Couples should be encouraged to discuss these feelings to avoid misperceptions and to maintain the relationship dyad as a priority to prevent the development of relationship problems.
The majority of women will discuss contraception with a health provider, but only 15% will voluntarily discuss their sexual needs or dysfunction.17 This finding is alarming given that, during the postpartum period, two of every three new mothers will experience at least one problem related to sexual function, including dyspareunia, decreased libido, difficulty achieving orgasm, and vaginal dryness.41 This lack of discussion with a health-care provider may be the result of several variables: incomplete knowledge on the part of the provider about what affects sexual function, poor training in the taking of an effective sexual history, and uneasiness on the part of the patient about discussing the issue.5,42
Postnatal depression takes a toll
Depressed mood and emotional lability in the postpartum period are negatively associated with sexual interest, enjoyment, coital activity, and perceived tenderness of the partner.7 Conversely, reduced sexual interest, desire and satisfaction; a lower frequency of intercourse; and later resumption of intercourse are associated with a higher number of psychiatric symptoms in the postpartum period.2 Between 10% and 15% of women experience postpartum depression (PPD).26 Depression has been associated with a decreased frequency and interest in sexual activity at 8 to 12 weeks postpartum.2,5
Chivers and colleagues assessed sexual functioning and sexual behavior in women with and without symptoms of PPD using the FSFI and EPDS. Although theirs was a small study, they found that women who had depressive symptoms also reported poorer functioning in regard to sexual arousal, orgasm, pain, lubrication, and sexual satisfaction.26 Morof and coworkers found that women who had PPD were less likely to have resumed intercourse by 6 months postpartum; they were also less likely to engage in other sexual activities.27
Role of pharmacotherapy
Many women are started on antidepressant medication near the time of delivery or during the immediate postpartum period. Often, serotonin reuptake inhibitors (SRIs) are used because there is minimal transmission of this class of medication through breast milk. However, the potential sexual side effects of these medications should be discussed because they are the agents most commonly associated with female sexual dysfunction.28
For clinicians
American Association of Sex Educators, Counselors, and Therapists – A not-for-profit, interdisciplinary professional organization comprising sexuality educators, sexuality counselors, sex therapists, physicians, social workers, and other clinicians. Its home page links to a referral page and other resources. http://www.aasect.org" target="_blank">http://www.aasect.org
Association of Reproductive Health Professionals offers a resource for clinicians on postpartum counseling about sexuality. http://www.arhp.org/publications-and-resources/quick-reference-guide-for-clinicians/postpartum-counseling/contraception" target="_blank">http://www.arhp.org/publications-and-resources/quick-reference-guide-for-clinicians/postpartum-counseling/contraception
For patients
Mayo Clinic provides a fact sheet entitled “Sex after pregnancy: Set your own timeline.” http://www.mayoclinic.com/health/sex-after-pregnancy/PR00146" target="_blank">http://www.mayoclinic.com/health/sex-after-pregnancy/PR00146
Sex and a Healthier You – This site offers information for patients on sexuality and relationships. http://www.sexandahealthieryou.org/sex-health/index.html" target="_blank">http://www.sexandahealthieryou.org/sex-health/index.html
We want to hear from you! Tell us what you think.
1. Reamy KJ, White SE. Sexuality in the puerperium: a review. Arch Sex Behav. 1987;16(2):165-186.
2. De Judicibus MA, McCabe MP. Psychological factors and the sexuality of pregnant and postpartum women. J Sex Res. 2002;39(2):94-103.
3. The puerperium. In: Cunningham FG Leveno KJ, Bloom SL, Hauth JC, Rouse DJ, Spong CY, eds. Williams Obstetrics. 23rd ed. New York, NY: McGraw-Hill Co.; 2010:646-660.
4. The American Academy of Pediatrics (AAP), American College of Obstetricians Gynecologists (ACOG) Guidelines for perinatal care. 6th ed. Washington DC: AAP, ACOG; 2008.
5. Glazener CM. Sexual function after childbirth: women’s experiences persistent morbidity and lack of professional recognition. Br J Obstet Gynaecol. 1997;104(3):330-335.
6. Rogers RG, Borders, N,, Leeman L, Albers L. Does spontaneous genital tract trauma impact postpartum sexual function? J Midwifery Womens Health. 2009;54(2):98-103.
7. von Sydow K. Sexuality during pregnancy and after childbirth: a metacontent analysis of 59 studies. J Psychosom Res. 1999;47(1):27-49.
8. Witting K, Santtila P, Alanko K, et al. Female sexual function and its associations with number of children, pregnancy, and relationship satisfaction. J Sex Marital Ther. 2008;34(2):89-106.
9. Thompson JF, Roberts CL, Currie M, Elwood DA. Prevalence and persistence of health problems after childbirth: associations with parity and method of birth. Birth. 2002;29(2):83-94.
10. Waterstone M, Wolfe C, Hooper R, Bewley S. Postnatal morbidity after childbirth and severe obstetric morbidity. BJOG. 2003;110(2):128-133.
11. Pauls RN, Occhino JA, Dryfhout VL. Effects of pregnancy on female sexual function and body image: A prospective study. J Sex Med. 2008;5(8):1915-1922.
12. von Sydow K, Ullmeyer M, Happ N. Sexual activity during pregnancy and after childbirth: Results from the Sexual P Questionnaire. J Psychosom Obstet Gynaecol. 2001;22(1):29-40.
13. Uebersax JS, Wyman JF, Shumaker SA, McClish DK, Fantl JA. Short forms to assess life quality and symptom distress for urinary incontinence in women: The Incontinence Impact Questionnaire and the Urogenital Distress Inventory. Continence Program for Women Rsearch Group. Neurourol Urodyn. 1995;14(2):131-139.
14. Barber MD, Visco AG, Wyman JF, Fantl JA, Bump RC; Continence Program for Women Research Group. Sexual function in women with urinary incontinence and pelvic organ prolapse. Obstet Gynecol. 2002;99(2):281-289.
15. Handa VL. Sexual function and childbirth. Semin Perinatol. 2006;30(5):253-256.
16. Klein MC, Gauthier RJ, Robbins JM, et al. Relationship of episiotomy to perineal trauma and morbidity, sexual dysfunction, and pelvic floor relaxation. Am J Obstet Gynecol. 1994;171(3):591-598.
17. Barrett G, Pendry E, Peacock J, Victor C, Thakar, Manyonda I. Women’s sexual health after childbirth. BJOG. 2000;107(2):186-195.
18. Barrett G, Peacock J, Victor CR, Manyonda I. Cesarean section and postnatal sexual health. Birth. 2005;32(4):306-311.
19. Eason E, Labrecque M, Wells G, Feldman P. Preventing perineal trauma during childbirth: a systematic review. Obstet Gynecol. 2000;95(3):464-471.
20. Leeman LM, Rogers RG, Greulich B, Albers LL. Do unsutured second-degree perineal lacerations affect postpartum functional outcomes? J Am Board Fam Med. 2007;20(5):451-457.
21. Signorello L, Harlow BL, Chekos AK, Repke JT. Postpartum sexual functioning and its relationship to perineal trauma: A retrospective cohort study of primiparous women. Am J Obstet Gynecol. 2001;184(5):881-890.
22. Snooks SJ, Swash M, Henry MW, Setchell M. Risk factors in childbirth causing damage to the pelvic floor innervation. In J Colorect Dis. 1986;1(1):20-24.
23. Hannah ME, Whyte H, Hannah WJ, et al. Term Breech Trial Collaborative Group. Maternal outcomes at 2 years after planned cesarean section versus planned vaginal birth for breech presentation at term: the international randomized Term Breech Trial. Am J Obstet Gynecol. 2004;191(3):917-927.
24. NIH State-of-the-Science Conference Statement on Cesarean Delivery on Maternal Request NIH Consens Sci Statements. 2006;23:1-29.http://consensus.nih.gov/2006/cesareanstatement.htm. Accessed December 6 2011.
25. Lydon-Rochelle MT, Holt VL, Martin DP. Delivery method and self-reported postpartum general health status among primiparous women. Paediatr Perinat Epidemiol. 2001;15(3):232-240.
26. Chivers ML, Pittini MD, Grigoriadis S, Villegas L, Ross LE. The relationship between sexual functioning and depressive symptomatology in postpartum women: a pilot study. J Sex Med. 2011;8(3):792-799.
27. Morof D, Barrett G, Peacock J, Victor CR, Manyonda I. Postnatal depression and sexual health after childbirth. Obstet Gynecol. 2003;102(6):1318-1325.
28. American College of Obstetricians and Gynecologists Committee on Practice Bulletins-Gynecology. ACOG Practice Bulletin No.119: Female sexual dysfunction. Obstet Gynecol. 2011;117(4):996-1007.
29. Read J. Sexual problems associated with infertility pregnancy and ageing. BMJ. 2004;329(7465):559-561.
30. Rosen R, Brown C, Heiman J, et al. The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000;26:191-208.
31. Isidori AM, Pozza C, Esposito K, et al. The Female Sexual Function Index (FSFI): Development and validation of a 6-item version of the female sexual function index (FSFI) as a diagnostic tool for female sexual dysfunction. J Sex Med. 2010;7(3):1139-11.
32. McCoy NL. The McCoy Female Sexuality Questionnaire. Quality Life Res. 2000;9(suppl 6):739-745.
33. Hatzichristou D, Rosen RC, Derogatis LR, et al. Recommendations for the clinical evaluation of men and women with sexual dysfunction. J Sex Med. 2010;7(1 Pt 1):337-348.
34. DeRogatis LR, Allgood A, Rosen RC, Leiblum S, Zipfel L, Guo CY. Development and evaluation of the Women’s Sexual Interest Diagnostic Interview (WSID): a structured interview to diagnose hypoactive sexual desire disorder (HSDD) in standardized patients. J Sex Med. 2008;5(12):2827-2841.
35. Fischman SH, Rankin EA, Soeken KL, Lenz ER. Changes in sexual relationships in postpartum couples. J Obstet Gynecol Neonatal Nurs. 1986;15(1):58-63.
36. Sillis T, Wunderlich G, Pyke R, et al. The Sexual Interest and Desire Inventory-Female (SIDI-F): item response analyses of data from women diagnosed with hypoactive sexual desire disorder. J Sex Med. 2005;2(6):801-818.
37. Rust J, Golombok S. The Golombok-Rust Inventory of Sexual Satisfaction (GRISS). Br J Clin Psych. 1985;24(Pt 1):63-64.
38. Clayton AH, Balon R. The impact of mental illness and psychotropic medications on sexual functioning: the evidence and management. J Sex Med. 2009;6(5):1200-1213.
39. Jennings B, Edmundson M. The postpartum period: after confinement: the fourth trimester. Clin Obstet Gynecol. 1980;23(4):1093-1103.
40. Oppenheimer LS, Sheriff EA, Goodman JDS, shah D, James CE. The duration of lochia. Br J Obstet Gynaecol. 1986;93(7):754-757.
41. Connolly A, Thorp J, Pahel L. Effects of pregnancy and childbirth on postpartum sexual function: a longitudinal prospective study. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16(4):263-267.
42. Pancholy AB, Goldenhar L, Fellner AN, Crisp C, Kleeman S, Pauls R. Resident education and training in female sexuality: results of a national survey. J Sex Med. 2011;8(2):361-366.
CASE: Waiting for an OK to resume sex
L. L. is a 29-year-old woman, G1P1, who delivered a healthy infant 4 weeks ago by spontaneous vaginal birth. The delivery involved a 2-day induction of labor for preeclampsia and a second-degree tear that was repaired without complication. The patient also experienced postpartum hemorrhage that was managed with bimanual massage and uterotonics and for which she ultimately required transfusion of blood products. Her hospital course was otherwise unremarkable.
Before pregnancy, L. L. had a normal medical history and conceived spontaneously. Her antenatal course was uncomplicated.
Today, she returns for her postpartum visit. She reports being tired and says she still has some pain at the site of the tear, but reports no problems with urinary or fecal continence. She denies being depressed, and her Edinburgh Postnatal Depression Scale (EPDS) score is consistent with that report. She is breastfeeding and appears to be doing well on the progestin-only pill for contraception. She has not yet attempted intercourse because she is complying with instructions to wait until she sees you for her postpartum visit.
How should you counsel her about resuming sexual activity?

Childbirth is a central event in a woman’s life. Pregnancy and delivery are a time of psychological, biological, and physical transformation, and the postpartum period—the “fourth trimester”—is no exception. Sexual function may be affected. In fact, many women who seek assistance for sexual dissatisfaction note that their problem arose in the postpartum period.1
Postpartum sexuality involves considerably more than the physical act of genital stimulation—with or without intromission or penile penetration—and depends on more than the physical state of recovery of the vagina (after vaginal delivery). It also depends on:
- the woman’s sexual drive and motivation
- her general state of health and quality of life
- her emotional readiness to resume sexual intimacy with a partner
- her adaptation to the maternal role and ability to balance her identity as a mother with her identity as a sexual being
- her relationship with her partner.
Given all these contributing factors, many of which fall outside the scope of the clinical practice of obstetrics and gynecology, how do we go about counseling our patients about the resumption of sexual activity?
Other questions:
- How can we help patients manage expectations about the quality of their postpartum sexual function?
- What guidance can we provide regarding the interplay of psychosexual and physical aspects of the puerperium?
- Can we offer a method of screening for sexual dysfunction in the puerperium? If so, will it help prevent sexual problems or hasten their resolution?
This article addresses these issues. Ultimately, the answer to the question of when to resume sexual activity should reflect an awareness of cultural norms and taboos as well as familiarity with empirically based recommendations.
Traditional postpartum sexual education is not evidence-based and has limited effectiveness. More up-to-date strategies can be easily incorporated into even the busiest clinical practice. We offer the following counseling model for you to consider when addressing the sexual health of patients postpartum.
Educate, legitimize, and normalize
The first sexual encounter after childbirth can be an important step for couples to reclaim their intimate relationship.
Adaptation to the parental role, physical healing, hormonal changes, breastfeeding, and sleep deprivation contribute to a profound psychosocial challenge. The resumption of sexual activities and a satisfying postpartum sex life depend on many variables, many of which the patient may not even be aware.
First, do not assume that all patients are heterosexual and that intercourse is their only form of sexual activity.
Second, it is important to be proactive in antepartum and postpartum counseling and to offer anticipatory guidance. Counseling can take place any time during routine prenatal care, as well as at the time of hospital discharge and the postpartum visit.
Reassure the patient that, if sexual activity and frequency are lower during pregnancy and the postpartum period, it is likely a normal transition. Also give the patient time to talk about her expectations and perceptions. Explain to her the normal fluctuations and variability of sexual interest and enjoyment in pregnancy and the puerperium, and suggest that she consider alternative options for intimate expression, non-coital sexual activities, and mutual pleasure within her cultural context.
Be thorough
Take a comprehensive medical, obstetric, psychological, and social history as part of the sexual history. Also perform a physical intake and exam. Questions about urinary and fecal incontinence ought to be part of all postpartum assessment.
Other potential areas to address include the quality of the relationship, prepregnancy sexual function, the support network, planned or unplanned state of the pregnancy, previous pregnancy and delivery outcomes, the health status of current children, and present, previous, and future contraceptive use.29
Consider multiple visits
It is hard to know exactly when to evaluate a patient for postpartum sexual dysfunction, given the impact of pudendal nerve latency, fatigue, and breastfeeding. For this reason, assessment on multiple occasions may be appropriate. Numerous validated scales to assess sexual function can be easily incorporated into clinical practice.
Couples counseling and therapy may be needed in some cases; be aware of referral services in your area for sexual wellness specialists.
The bottom line: A “successful” sexual life does not necessarily mean adequate genital function (e.g., coital orgasm, improved clitoral blood flow, increased sexual frequency) but, rather, a sexual life that is intimate and satisfying to the individual patient.
A paucity of research
To date, research into sexuality during the postpartum period has focused primarily on the physical changes and constraints that affect the mechanics and frequency of intercourse and overall sexual satisfaction and desire.2 This perspective has begun to broaden to include the psychological aspects of sexuality.
TABLE 1
These validated tools can help you measure female sexual dysfunction
| Tool | Area assessed |
|---|---|
| Female Sexual Function Index (FSFI)30 | Desire, arousal, orgasm, and pain |
| Female Sexual Function Index 6-Item (FSFI-6)31 | Desire, arousal, orgasm, and pain |
| McCoy Female Sexual Function Questionnaire*32 | Presence of female sexual disorders |
| Brief Sexual Symptoms Checklist33 | Screener for sexual concerns |
| Female Sexual Distress Scale – Revised34 | Distress |
| Intimate Relationship Scale*35 | Changes in sexual relationship |
| Sexual Quality of Life – Female (SQol-F)36 | Quality of life in women with female sexual dysfunction |
| Golombok Rust Inventory of Sexual Satisfaction (GRISS)37 | Quality of sexual relationship |
| Decreased Sexual Desire Screener38 | Brief diagnostic tool for hypoactive sexual desire disorder |
| * Validated in pregnant and/or postpartum women | |
Women’s sexual health during the postpartum period has generally been under-researched. It wasn’t until the past decade that validated sexual function questionnaires were utilized. Although a number of these instruments are now available (TABLE 1, TABLE 2, FIGURE), it remains unclear whether they can accurately measure postpartum sexual function. Despite these limitations, significant information has been elicited that can be used to counsel patients struggling with postpartum sexual concerns.
TABLE 2
The 6-item Female Sexual Function Index*
| Question | Responses | |||||
|---|---|---|---|---|---|---|
| 0 points | 5 points | 4 points | 3 points | 2 points | 1 point | |
| How would you rate your level of sexual desire or interest? | No sexual activity | Very high | High | Moderate | Low | Very low or none at all |
| How would you rate your level of sexual arousal (“turn on”) during sexual activity or intercourse? | No sexual activity | Very high | High | Moderate | Low | Very low or none at all |
| How often did you become lubricated (“wet”) during sexual activity or intercourse? | No sexual activity | Almost always or always | Most times | Sometimes | A few times | Almost never or never |
| When you had sexual stimulation or intercourse, how often did you reach orgasm? | No sexual activity | Almost always or always | Most times | Sometimes | A few times | Almost never or never |
| How satisfied have you been overall with your sexual life? | No sexual activity | Very satisfied | Moderately satisfied | About equally satisfied and dissatisfied | Moderately dissatisfied | Very dissatisfied |
| How often did you experience discomfort or pain during vaginal penetration? | Did not attempt intercourse | Almost never or never | A few times | Sometimes | Most times | Almost always or always |
| *The components of this index are to be assessed over the past 4 weeks. The score is the sum of the ordinal responses to the 6 items and ranges from 2 to 30. A score of less than 19 indicates a need for further investigation, including the full-length Female Sexual Function Index. Source: Adapted from Isidori et al.31 | ||||||
Ideal period of abstinence is unknown
Although our knowledge of the female genital tract in the puerperium is based upon histologic evidence, there are no evidence-based policies to outline the ideal period of postpartum coital abstinence. It seems reasonable to assume that our traditional scientific recommendations developed in part to prevent uterine infection and disruption of sutured wounds. These concerns, combined with cultural and societal norms, have led to the routine discouragement of sexual activity until 4 to 6 weeks postpartum.
The possibility of shortening the period of postpartum abstinence was first suggested by the American College of Obstetricians and Gynecologists (ACOG) in 1984.1 In 1985, Pritchard and colleagues wrote about the individualization of postpartum prohibitions of sexual activity in Williams Obstetrics.1 The earliest time at which intercourse may be safely resumed is unknown, but the 23rd edition of Williams Obstetrics states that a woman can resume sexual intercourse as early as 2 weeks, based on her comfort and desire.3 The sixth edition of the American Academy of Pediatrics (AAP) and ACOG guidelines for perinatal care also states that the risks ought to be minimal at 2 weeks postpartum.4
BRIEF SEXUAL SYMPTOMS CHECKLIST FOR WOMEN (BSSC-W)
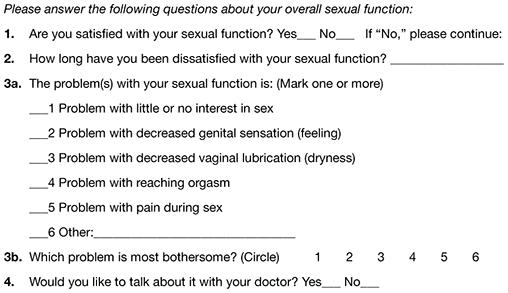
Reprinted from Hatzichristou et al. 33
Low desire is not unusual
Although a patient may be granted “permission” to engage in coital activity, other variables influence her decision. It is well known that sexual desire may fluctuate during pregnancy and typically decreases significantly during the third trimester.2 Many women enter the postpartum period with lower levels of sexual desire and satisfaction, and these depressed levels may continue for some time.2 Twenty-five percent of women report worsened sexual function, including diminished sexual satisfaction, during pregnancy that persists for 6 to 12 months postpartum.5 By 12 weeks postpartum, 80% to 93% of women have resumed intercourse, but as many as 83% report sexual problems during the first 3 months of the postpartum period. At 6 months, 18% to 30% of these women may still be experiencing sexual problems, including dyspareunia.5,6
In 1998, von Sydow performed a meta-content analysis of all existing studies on parental sexuality during pregnancy and the first 6 months postpartum.7 Using psychological and medical data banks, she brought together information from two branches of science and identified 59 relevant studies in English or German between 1950 and 1996. Although the majority of studies were retrospective and failed to utilize a validated instrument, von Sydow determined that, overall, sexual interest and activity were low or nonexistent during the first months after delivery. There was high variability between individuals, however, and levels of sexual interest and activity of individual women remained relatively constant from the time before pregnancy until 1 year postpartum.7 von Sydow determined that there is great variability in female sexuality during pregnancy and postpartum; this variability may represent fluctuations during this phase of life. She also determined that severe psychosexual and marital problems are much more prevalent in the postpartum period than during pregnancy and persist long after a physical cause can be used as an explanation.7
Fatigue and quality of the relationship have an impact on sexual function
De Judicibus and colleagues identified a broad range of variables that have a detrimental impact on sexuality at 12 weeks postpartum, most particularly:
- marital dissatisfaction
- dyspareunia
- fatigue
- depression
- breastfeeding.2
There is evidence to suggest that the addition of the first child reduces marital quality after the first month postpartum, and this decline in marital satisfaction continues for 6 to 18 months postpartum.2 Witting and coworkers suggested that this decline may represent a transitional phase of parenthood for some couples; data support the positive effects on overall marital satisfaction with the addition of children.8 Women who were more satisfied with their relationships reported higher sexual satisfaction and greater frequency of intercourse.2,8
Fatigue is one of the most common problems women experience during pregnancy and postpartum and is a common reason given for loss of sexual desire and interest, infrequent sexual activity, and lack of enjoyment.5 A high level of exhaustion is found during the first 8 weeks postpartum. Although it declines over the next 6 months, it does not appear to resolve completely in a good number of women.9
Don’t underestimate the impact of obstetric morbidity
Surprisingly, the long-term impact of severe obstetric events on postpartum maternal health is often overlooked. Waterstone and colleagues found that women who have severe obstetric morbidity, such as massive hemorrhage, preeclampsia, sepsis, and uterine rupture, experience significant changes in sexual health and well-being.10 They conducted a prospective cohort study of such women, measuring sexual activity, general health, and postpartum depression. They utilized two validated postnatal questionnaires—the Short Form 36 (SF-36) to measure general health and the EPDS. Women who had uncomplicated pregnancies and childbirth tended to perform well in most SF-36 categories, whereas women who had experienced severe morbidity scored worse in almost every category. These women also reported problems with intercourse. Thirteen percent of women had not resumed sexual relations by 6 to 12 months postpartum; of these women, more than half reported a fear of conceiving as a reason.
The female body undergoes dramatic physiologic, anatomic, and psychological changes immediately following delivery and throughout the restoration of its pre-pregnant state. This fourth trimester usually lasts 6 to 12 weeks.39
Uterus. The uterus undergoes rapid involution after separation of the placenta. By 2 to 4 weeks postpartum, it may no longer be palpable abdominally, and by 6 weeks, it usually has returned to its nonpregnant state and size. Seven to 14 days after delivery, a woman often experiences an episode of heavier vaginal bleeding that corresponds with the sloughing of the placental bed eschar. During this time of involution, myometrial vessels may be 5 mm or larger in diameter.40
Lochia. The postpartum lochia begins to change within days of birth, transitioning through its stages of lochia rubra, serosa, and alba. It decreases by 3 weeks postpartum and is likely completely resolved by 6 weeks.
Prolactin is responsible for lactogenesis. When the prolactin level is maintained through breastfeeding, it depresses ovarian production of estrogen by suppressing pituitary gonadotropin secretion, triggering a period of “steroid starvation” after the loss of estrogen and progesterone production from the placenta.1
Vagina. Early in the postpartum period, the vagina is typically edematous and lax and, as a result of parturition, there may be not only a spontaneous tear or episiotomy that must heal, but superficial small tears that do not require suturing. Ruggae begin to reappear by 3 weeks, and the vaginal epithelium will begin to mature under the influence of estrogen production. Much of this tissue damage is healed by 6 weeks postpartum.
The perception of pregnant and postpartum women’s sexuality varies, based on religious and cultural norms. In some religions and cultures, sexual activity is forbidden for 2 to 3 months postpartum; in others, it is prohibited until the child is weaned from the breast. The postpartum woman and lochia have traditionally been perceived as unclean, and many religions have specific proscriptions regarding the management of this time in a woman’s life.1 Although early cultures did not study these issues specifically, their doctrines suggest that they had some awareness of the natural physiologic transition of a woman’s body after she has given birth.
Exploring the role of body image
Paul and coworkers prospectively assessed female sexual function, body image, and pelvic symptoms from the first trimester until 6 months postpartum.11 They utilized the validated questionnaire instruments of the Female Sexual Function Index (FSFI), the Body Exposure during Sexual Activities Questionnaire (BESAQ), the short forms of the Urogenital Distress Inventory (UDI-6), the Incontinence Impact Questionnaire (IIQ-7), and the Fecal Incontinence Quality of Life Scale (FIQOL). They found that sexual activity and sexual function scores were highest before pregnancy, declined between the first and third trimesters, and did not return to pre-pregnancy baselines even by 6 months postpartum.11
Differences in sexual practices contributed to these patterns. Kissing, fondling, and vaginal intercourse remained stable across pregnancy, whereas oral sex, breast stimulation, and masturbation declined in the third trimester.
The decline of these activities during pregnancy and postpartum has been seen in other studies as well.12
Obstacles to sexual activity also changed across pregnancy and the postpartum period. Vaginal pain was more problematic in the third trimester and postpartum, whereas feelings of unattractiveness and issues of body image were present throughout pregnancy and at their worst in the postpartum period. Sexual function scores based on the FSFI declined during pregnancy and did not return to pre-pregnancy or first-trimester levels by 6 months postpartum. Urinary symptoms, as measured by the UDI-6, were associated with lower sexual function scores during the postpartum period. The association between urinary incontinence and sexual dysfunction has been seen in other studies.13,14
The enduring effects of perineal trauma
Childbirth may physically affect a woman’s sexual function through perineal trauma, pudendal neuropathy, and vaginal dryness associated with breastfeeding. There is an obvious connection between perineal laceration and perineal pain and problems with intercourse.5 Overall, dyspareunia is reported by 41% to 67% of women 2 to 3 months after delivery.15 Women who have an episiotomy complain of increased perineal pain and delayed return of sexual activity, compared with women who deliver with an intact perineum.16
Persistent dyspareunia is strongly associated with the severity of perineal trauma and operative vaginal delivery.3,17 Multiple studies have investigated this association and found a positive correlation 3 to 6 months postpartum,6,9,17 but the long-term effects and association remain unclear.18
Findings from research. Rogers and colleagues prospectively studied the effect of perineal trauma on postpartum sexual function in a midwifery population of women who had a low rate of episiotomy and operative vaginal delivery.6 They utilized the Intimate Relationship Scale (IRS), a validated questionnaire to measure postpartum sexual function in couples. Most women in this study had resumed sexual activity by 3 months postpartum and did not have postpartum inactivity or dysfunction, based on their IRS scores. However, women who were identified as having experienced major trauma (second-, third-, or fourth-degree laceration or a repaired first-degree laceration) had significantly less desire to engage in activities such as touching and stroking with their partner.6
Present-day limits on the routine use of episiotomy and operative vaginal delivery have yielded a lower rate of third- and fourth-degree laceration.19 Second-degree lacerations are common and constitute the majority of perineal trauma in births without episiotomy.20 There is evidence that the use of synthetic absorbable suture, such as polyglactin, rather than chromic suture, results in less postpartum perineal pain, as does leaving the well-approximated perineal skin edges unsutured.20
Signorello and coworkers found that second-, third-, and fourth-degree lacerations increased the risk of postpartum dyspareunia; operative vaginal delivery (forceps or vacuum) was also an independent risk factor for dyspareunia.21
The impact of route of delivery
Some researchers have concluded that the route of delivery has an impact on the long-term pelvic floor health of women.18 In 1986, Snooks and colleagues analyzed possible obstetric risk factors for damage to the innervation of the pelvic floor, which can lead to both stress urinary and anorectal incontinence.22 They found that the process of vaginal delivery causes a compression and stretch type of injury to the pudendal nerve, as well as the possibility of severe perineal lacerations. This injury may be less likely to occur when cesarean delivery is performed before labor, avoiding direct perineal trauma and possible pudendal neuropathy.15 Because the pudendal nerve mediates some of the reflex pathways in the female sexual response, it is plausible that damage to it could result in sexual dysfunction.
Women who deliver vaginally have a higher rate of fecal and urinary incontinence than women who deliver by cesarean.16,23 The presence of incontinence, however, does not always have a significant long-term effect on one’s sexual life.6
In the Term Breech Trial, the route of delivery had no impact on the resumption of intercourse, dyspareunia, or sexual satisfaction.23 Although the trial was randomized and controlled, it had many limitations that call its generalizability into question in regard to postpartum sexual dysfunction.
The National Institutes of Health (NIH) State-of-the-Science Conference on Cesarean Delivery on Maternal Request indicated that, by 6 months postpartum, there is no difference in sexual function based on the route of delivery.24 However, Lydon-Rochelle and colleagues used the SF-36 to assess reported general health status and found that women who had cesarean delivery or assisted vaginal delivery exhibited significantly poorer postpartum functional status than women who had spontaneous vaginal delivery in five areas at 7 weeks postpartum: physical functioning, mental health, general health perception, bodily pain, social functioning, and ability to perform daily activities.25 Women were more likely to be readmitted to the hospital and more likely to report fatigue during the first 2 months after cesarean delivery.9 It appears that women who undergo cesarean delivery have an elevated risk of nondyspareunia-related causes of sexual dysfunction. Any protective effect of cesarean on sexual function is limited to the early postnatal period and is related to the absence of perineal injury.18
How breastfeeding can affect sexual desire
Evidence is strong that breastfeeding reduces a woman’s sexual desire and the frequency of intercourse.1,5 A high level of prolactin suppresses ovarian production of estrogen, thereby reducing vaginal lubrication. Some women and their partner may identify this loss of lubrication as a lack of arousal. This type of vaginal dryness should be explained, and the use of a lubricant should be encouraged in breastfeeding women.
Nipple sensitivity may develop, making touching and foreplay uncomfortable in some women. One third to one half of mothers find breastfeeding to be an erotic experience, and one fourth feel guilty about this sexual excitement; others stop nursing or wean early due to these feelings.1,7 Women are often not educated about the relationship between the release of oxytocin, uterine contractions, milk ejection, sexual arousal, and orgasm; raising the subject can help to diminish any potential distress over this response.
Sleep disturbances from feeding on demand contribute to fatigue and exhaustion.
Many women may not realize that their loss of interest in sex may be because they are receiving sufficient physical contact or touching through their nurturing interactions with the baby. This may leave the partner feeling isolated and envious of the mother-baby relationship.
Couples should be encouraged to discuss these feelings to avoid misperceptions and to maintain the relationship dyad as a priority to prevent the development of relationship problems.
The majority of women will discuss contraception with a health provider, but only 15% will voluntarily discuss their sexual needs or dysfunction.17 This finding is alarming given that, during the postpartum period, two of every three new mothers will experience at least one problem related to sexual function, including dyspareunia, decreased libido, difficulty achieving orgasm, and vaginal dryness.41 This lack of discussion with a health-care provider may be the result of several variables: incomplete knowledge on the part of the provider about what affects sexual function, poor training in the taking of an effective sexual history, and uneasiness on the part of the patient about discussing the issue.5,42
Postnatal depression takes a toll
Depressed mood and emotional lability in the postpartum period are negatively associated with sexual interest, enjoyment, coital activity, and perceived tenderness of the partner.7 Conversely, reduced sexual interest, desire and satisfaction; a lower frequency of intercourse; and later resumption of intercourse are associated with a higher number of psychiatric symptoms in the postpartum period.2 Between 10% and 15% of women experience postpartum depression (PPD).26 Depression has been associated with a decreased frequency and interest in sexual activity at 8 to 12 weeks postpartum.2,5
Chivers and colleagues assessed sexual functioning and sexual behavior in women with and without symptoms of PPD using the FSFI and EPDS. Although theirs was a small study, they found that women who had depressive symptoms also reported poorer functioning in regard to sexual arousal, orgasm, pain, lubrication, and sexual satisfaction.26 Morof and coworkers found that women who had PPD were less likely to have resumed intercourse by 6 months postpartum; they were also less likely to engage in other sexual activities.27
Role of pharmacotherapy
Many women are started on antidepressant medication near the time of delivery or during the immediate postpartum period. Often, serotonin reuptake inhibitors (SRIs) are used because there is minimal transmission of this class of medication through breast milk. However, the potential sexual side effects of these medications should be discussed because they are the agents most commonly associated with female sexual dysfunction.28
For clinicians
American Association of Sex Educators, Counselors, and Therapists – A not-for-profit, interdisciplinary professional organization comprising sexuality educators, sexuality counselors, sex therapists, physicians, social workers, and other clinicians. Its home page links to a referral page and other resources. http://www.aasect.org" target="_blank">http://www.aasect.org
Association of Reproductive Health Professionals offers a resource for clinicians on postpartum counseling about sexuality. http://www.arhp.org/publications-and-resources/quick-reference-guide-for-clinicians/postpartum-counseling/contraception" target="_blank">http://www.arhp.org/publications-and-resources/quick-reference-guide-for-clinicians/postpartum-counseling/contraception
For patients
Mayo Clinic provides a fact sheet entitled “Sex after pregnancy: Set your own timeline.” http://www.mayoclinic.com/health/sex-after-pregnancy/PR00146" target="_blank">http://www.mayoclinic.com/health/sex-after-pregnancy/PR00146
Sex and a Healthier You – This site offers information for patients on sexuality and relationships. http://www.sexandahealthieryou.org/sex-health/index.html" target="_blank">http://www.sexandahealthieryou.org/sex-health/index.html
We want to hear from you! Tell us what you think.
CASE: Waiting for an OK to resume sex
L. L. is a 29-year-old woman, G1P1, who delivered a healthy infant 4 weeks ago by spontaneous vaginal birth. The delivery involved a 2-day induction of labor for preeclampsia and a second-degree tear that was repaired without complication. The patient also experienced postpartum hemorrhage that was managed with bimanual massage and uterotonics and for which she ultimately required transfusion of blood products. Her hospital course was otherwise unremarkable.
Before pregnancy, L. L. had a normal medical history and conceived spontaneously. Her antenatal course was uncomplicated.
Today, she returns for her postpartum visit. She reports being tired and says she still has some pain at the site of the tear, but reports no problems with urinary or fecal continence. She denies being depressed, and her Edinburgh Postnatal Depression Scale (EPDS) score is consistent with that report. She is breastfeeding and appears to be doing well on the progestin-only pill for contraception. She has not yet attempted intercourse because she is complying with instructions to wait until she sees you for her postpartum visit.
How should you counsel her about resuming sexual activity?

Childbirth is a central event in a woman’s life. Pregnancy and delivery are a time of psychological, biological, and physical transformation, and the postpartum period—the “fourth trimester”—is no exception. Sexual function may be affected. In fact, many women who seek assistance for sexual dissatisfaction note that their problem arose in the postpartum period.1
Postpartum sexuality involves considerably more than the physical act of genital stimulation—with or without intromission or penile penetration—and depends on more than the physical state of recovery of the vagina (after vaginal delivery). It also depends on:
- the woman’s sexual drive and motivation
- her general state of health and quality of life
- her emotional readiness to resume sexual intimacy with a partner
- her adaptation to the maternal role and ability to balance her identity as a mother with her identity as a sexual being
- her relationship with her partner.
Given all these contributing factors, many of which fall outside the scope of the clinical practice of obstetrics and gynecology, how do we go about counseling our patients about the resumption of sexual activity?
Other questions:
- How can we help patients manage expectations about the quality of their postpartum sexual function?
- What guidance can we provide regarding the interplay of psychosexual and physical aspects of the puerperium?
- Can we offer a method of screening for sexual dysfunction in the puerperium? If so, will it help prevent sexual problems or hasten their resolution?
This article addresses these issues. Ultimately, the answer to the question of when to resume sexual activity should reflect an awareness of cultural norms and taboos as well as familiarity with empirically based recommendations.
Traditional postpartum sexual education is not evidence-based and has limited effectiveness. More up-to-date strategies can be easily incorporated into even the busiest clinical practice. We offer the following counseling model for you to consider when addressing the sexual health of patients postpartum.
Educate, legitimize, and normalize
The first sexual encounter after childbirth can be an important step for couples to reclaim their intimate relationship.
Adaptation to the parental role, physical healing, hormonal changes, breastfeeding, and sleep deprivation contribute to a profound psychosocial challenge. The resumption of sexual activities and a satisfying postpartum sex life depend on many variables, many of which the patient may not even be aware.
First, do not assume that all patients are heterosexual and that intercourse is their only form of sexual activity.
Second, it is important to be proactive in antepartum and postpartum counseling and to offer anticipatory guidance. Counseling can take place any time during routine prenatal care, as well as at the time of hospital discharge and the postpartum visit.
Reassure the patient that, if sexual activity and frequency are lower during pregnancy and the postpartum period, it is likely a normal transition. Also give the patient time to talk about her expectations and perceptions. Explain to her the normal fluctuations and variability of sexual interest and enjoyment in pregnancy and the puerperium, and suggest that she consider alternative options for intimate expression, non-coital sexual activities, and mutual pleasure within her cultural context.
Be thorough
Take a comprehensive medical, obstetric, psychological, and social history as part of the sexual history. Also perform a physical intake and exam. Questions about urinary and fecal incontinence ought to be part of all postpartum assessment.
Other potential areas to address include the quality of the relationship, prepregnancy sexual function, the support network, planned or unplanned state of the pregnancy, previous pregnancy and delivery outcomes, the health status of current children, and present, previous, and future contraceptive use.29
Consider multiple visits
It is hard to know exactly when to evaluate a patient for postpartum sexual dysfunction, given the impact of pudendal nerve latency, fatigue, and breastfeeding. For this reason, assessment on multiple occasions may be appropriate. Numerous validated scales to assess sexual function can be easily incorporated into clinical practice.
Couples counseling and therapy may be needed in some cases; be aware of referral services in your area for sexual wellness specialists.
The bottom line: A “successful” sexual life does not necessarily mean adequate genital function (e.g., coital orgasm, improved clitoral blood flow, increased sexual frequency) but, rather, a sexual life that is intimate and satisfying to the individual patient.
A paucity of research
To date, research into sexuality during the postpartum period has focused primarily on the physical changes and constraints that affect the mechanics and frequency of intercourse and overall sexual satisfaction and desire.2 This perspective has begun to broaden to include the psychological aspects of sexuality.
TABLE 1
These validated tools can help you measure female sexual dysfunction
| Tool | Area assessed |
|---|---|
| Female Sexual Function Index (FSFI)30 | Desire, arousal, orgasm, and pain |
| Female Sexual Function Index 6-Item (FSFI-6)31 | Desire, arousal, orgasm, and pain |
| McCoy Female Sexual Function Questionnaire*32 | Presence of female sexual disorders |
| Brief Sexual Symptoms Checklist33 | Screener for sexual concerns |
| Female Sexual Distress Scale – Revised34 | Distress |
| Intimate Relationship Scale*35 | Changes in sexual relationship |
| Sexual Quality of Life – Female (SQol-F)36 | Quality of life in women with female sexual dysfunction |
| Golombok Rust Inventory of Sexual Satisfaction (GRISS)37 | Quality of sexual relationship |
| Decreased Sexual Desire Screener38 | Brief diagnostic tool for hypoactive sexual desire disorder |
| * Validated in pregnant and/or postpartum women | |
Women’s sexual health during the postpartum period has generally been under-researched. It wasn’t until the past decade that validated sexual function questionnaires were utilized. Although a number of these instruments are now available (TABLE 1, TABLE 2, FIGURE), it remains unclear whether they can accurately measure postpartum sexual function. Despite these limitations, significant information has been elicited that can be used to counsel patients struggling with postpartum sexual concerns.
TABLE 2
The 6-item Female Sexual Function Index*
| Question | Responses | |||||
|---|---|---|---|---|---|---|
| 0 points | 5 points | 4 points | 3 points | 2 points | 1 point | |
| How would you rate your level of sexual desire or interest? | No sexual activity | Very high | High | Moderate | Low | Very low or none at all |
| How would you rate your level of sexual arousal (“turn on”) during sexual activity or intercourse? | No sexual activity | Very high | High | Moderate | Low | Very low or none at all |
| How often did you become lubricated (“wet”) during sexual activity or intercourse? | No sexual activity | Almost always or always | Most times | Sometimes | A few times | Almost never or never |
| When you had sexual stimulation or intercourse, how often did you reach orgasm? | No sexual activity | Almost always or always | Most times | Sometimes | A few times | Almost never or never |
| How satisfied have you been overall with your sexual life? | No sexual activity | Very satisfied | Moderately satisfied | About equally satisfied and dissatisfied | Moderately dissatisfied | Very dissatisfied |
| How often did you experience discomfort or pain during vaginal penetration? | Did not attempt intercourse | Almost never or never | A few times | Sometimes | Most times | Almost always or always |
| *The components of this index are to be assessed over the past 4 weeks. The score is the sum of the ordinal responses to the 6 items and ranges from 2 to 30. A score of less than 19 indicates a need for further investigation, including the full-length Female Sexual Function Index. Source: Adapted from Isidori et al.31 | ||||||
Ideal period of abstinence is unknown
Although our knowledge of the female genital tract in the puerperium is based upon histologic evidence, there are no evidence-based policies to outline the ideal period of postpartum coital abstinence. It seems reasonable to assume that our traditional scientific recommendations developed in part to prevent uterine infection and disruption of sutured wounds. These concerns, combined with cultural and societal norms, have led to the routine discouragement of sexual activity until 4 to 6 weeks postpartum.
The possibility of shortening the period of postpartum abstinence was first suggested by the American College of Obstetricians and Gynecologists (ACOG) in 1984.1 In 1985, Pritchard and colleagues wrote about the individualization of postpartum prohibitions of sexual activity in Williams Obstetrics.1 The earliest time at which intercourse may be safely resumed is unknown, but the 23rd edition of Williams Obstetrics states that a woman can resume sexual intercourse as early as 2 weeks, based on her comfort and desire.3 The sixth edition of the American Academy of Pediatrics (AAP) and ACOG guidelines for perinatal care also states that the risks ought to be minimal at 2 weeks postpartum.4
BRIEF SEXUAL SYMPTOMS CHECKLIST FOR WOMEN (BSSC-W)
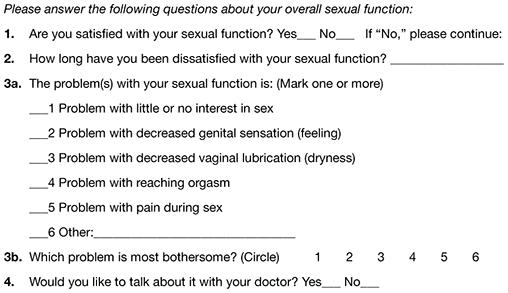
Reprinted from Hatzichristou et al. 33
Low desire is not unusual
Although a patient may be granted “permission” to engage in coital activity, other variables influence her decision. It is well known that sexual desire may fluctuate during pregnancy and typically decreases significantly during the third trimester.2 Many women enter the postpartum period with lower levels of sexual desire and satisfaction, and these depressed levels may continue for some time.2 Twenty-five percent of women report worsened sexual function, including diminished sexual satisfaction, during pregnancy that persists for 6 to 12 months postpartum.5 By 12 weeks postpartum, 80% to 93% of women have resumed intercourse, but as many as 83% report sexual problems during the first 3 months of the postpartum period. At 6 months, 18% to 30% of these women may still be experiencing sexual problems, including dyspareunia.5,6
In 1998, von Sydow performed a meta-content analysis of all existing studies on parental sexuality during pregnancy and the first 6 months postpartum.7 Using psychological and medical data banks, she brought together information from two branches of science and identified 59 relevant studies in English or German between 1950 and 1996. Although the majority of studies were retrospective and failed to utilize a validated instrument, von Sydow determined that, overall, sexual interest and activity were low or nonexistent during the first months after delivery. There was high variability between individuals, however, and levels of sexual interest and activity of individual women remained relatively constant from the time before pregnancy until 1 year postpartum.7 von Sydow determined that there is great variability in female sexuality during pregnancy and postpartum; this variability may represent fluctuations during this phase of life. She also determined that severe psychosexual and marital problems are much more prevalent in the postpartum period than during pregnancy and persist long after a physical cause can be used as an explanation.7
Fatigue and quality of the relationship have an impact on sexual function
De Judicibus and colleagues identified a broad range of variables that have a detrimental impact on sexuality at 12 weeks postpartum, most particularly:
- marital dissatisfaction
- dyspareunia
- fatigue
- depression
- breastfeeding.2
There is evidence to suggest that the addition of the first child reduces marital quality after the first month postpartum, and this decline in marital satisfaction continues for 6 to 18 months postpartum.2 Witting and coworkers suggested that this decline may represent a transitional phase of parenthood for some couples; data support the positive effects on overall marital satisfaction with the addition of children.8 Women who were more satisfied with their relationships reported higher sexual satisfaction and greater frequency of intercourse.2,8
Fatigue is one of the most common problems women experience during pregnancy and postpartum and is a common reason given for loss of sexual desire and interest, infrequent sexual activity, and lack of enjoyment.5 A high level of exhaustion is found during the first 8 weeks postpartum. Although it declines over the next 6 months, it does not appear to resolve completely in a good number of women.9
Don’t underestimate the impact of obstetric morbidity
Surprisingly, the long-term impact of severe obstetric events on postpartum maternal health is often overlooked. Waterstone and colleagues found that women who have severe obstetric morbidity, such as massive hemorrhage, preeclampsia, sepsis, and uterine rupture, experience significant changes in sexual health and well-being.10 They conducted a prospective cohort study of such women, measuring sexual activity, general health, and postpartum depression. They utilized two validated postnatal questionnaires—the Short Form 36 (SF-36) to measure general health and the EPDS. Women who had uncomplicated pregnancies and childbirth tended to perform well in most SF-36 categories, whereas women who had experienced severe morbidity scored worse in almost every category. These women also reported problems with intercourse. Thirteen percent of women had not resumed sexual relations by 6 to 12 months postpartum; of these women, more than half reported a fear of conceiving as a reason.
The female body undergoes dramatic physiologic, anatomic, and psychological changes immediately following delivery and throughout the restoration of its pre-pregnant state. This fourth trimester usually lasts 6 to 12 weeks.39
Uterus. The uterus undergoes rapid involution after separation of the placenta. By 2 to 4 weeks postpartum, it may no longer be palpable abdominally, and by 6 weeks, it usually has returned to its nonpregnant state and size. Seven to 14 days after delivery, a woman often experiences an episode of heavier vaginal bleeding that corresponds with the sloughing of the placental bed eschar. During this time of involution, myometrial vessels may be 5 mm or larger in diameter.40
Lochia. The postpartum lochia begins to change within days of birth, transitioning through its stages of lochia rubra, serosa, and alba. It decreases by 3 weeks postpartum and is likely completely resolved by 6 weeks.
Prolactin is responsible for lactogenesis. When the prolactin level is maintained through breastfeeding, it depresses ovarian production of estrogen by suppressing pituitary gonadotropin secretion, triggering a period of “steroid starvation” after the loss of estrogen and progesterone production from the placenta.1
Vagina. Early in the postpartum period, the vagina is typically edematous and lax and, as a result of parturition, there may be not only a spontaneous tear or episiotomy that must heal, but superficial small tears that do not require suturing. Ruggae begin to reappear by 3 weeks, and the vaginal epithelium will begin to mature under the influence of estrogen production. Much of this tissue damage is healed by 6 weeks postpartum.
The perception of pregnant and postpartum women’s sexuality varies, based on religious and cultural norms. In some religions and cultures, sexual activity is forbidden for 2 to 3 months postpartum; in others, it is prohibited until the child is weaned from the breast. The postpartum woman and lochia have traditionally been perceived as unclean, and many religions have specific proscriptions regarding the management of this time in a woman’s life.1 Although early cultures did not study these issues specifically, their doctrines suggest that they had some awareness of the natural physiologic transition of a woman’s body after she has given birth.
Exploring the role of body image
Paul and coworkers prospectively assessed female sexual function, body image, and pelvic symptoms from the first trimester until 6 months postpartum.11 They utilized the validated questionnaire instruments of the Female Sexual Function Index (FSFI), the Body Exposure during Sexual Activities Questionnaire (BESAQ), the short forms of the Urogenital Distress Inventory (UDI-6), the Incontinence Impact Questionnaire (IIQ-7), and the Fecal Incontinence Quality of Life Scale (FIQOL). They found that sexual activity and sexual function scores were highest before pregnancy, declined between the first and third trimesters, and did not return to pre-pregnancy baselines even by 6 months postpartum.11
Differences in sexual practices contributed to these patterns. Kissing, fondling, and vaginal intercourse remained stable across pregnancy, whereas oral sex, breast stimulation, and masturbation declined in the third trimester.
The decline of these activities during pregnancy and postpartum has been seen in other studies as well.12
Obstacles to sexual activity also changed across pregnancy and the postpartum period. Vaginal pain was more problematic in the third trimester and postpartum, whereas feelings of unattractiveness and issues of body image were present throughout pregnancy and at their worst in the postpartum period. Sexual function scores based on the FSFI declined during pregnancy and did not return to pre-pregnancy or first-trimester levels by 6 months postpartum. Urinary symptoms, as measured by the UDI-6, were associated with lower sexual function scores during the postpartum period. The association between urinary incontinence and sexual dysfunction has been seen in other studies.13,14
The enduring effects of perineal trauma
Childbirth may physically affect a woman’s sexual function through perineal trauma, pudendal neuropathy, and vaginal dryness associated with breastfeeding. There is an obvious connection between perineal laceration and perineal pain and problems with intercourse.5 Overall, dyspareunia is reported by 41% to 67% of women 2 to 3 months after delivery.15 Women who have an episiotomy complain of increased perineal pain and delayed return of sexual activity, compared with women who deliver with an intact perineum.16
Persistent dyspareunia is strongly associated with the severity of perineal trauma and operative vaginal delivery.3,17 Multiple studies have investigated this association and found a positive correlation 3 to 6 months postpartum,6,9,17 but the long-term effects and association remain unclear.18
Findings from research. Rogers and colleagues prospectively studied the effect of perineal trauma on postpartum sexual function in a midwifery population of women who had a low rate of episiotomy and operative vaginal delivery.6 They utilized the Intimate Relationship Scale (IRS), a validated questionnaire to measure postpartum sexual function in couples. Most women in this study had resumed sexual activity by 3 months postpartum and did not have postpartum inactivity or dysfunction, based on their IRS scores. However, women who were identified as having experienced major trauma (second-, third-, or fourth-degree laceration or a repaired first-degree laceration) had significantly less desire to engage in activities such as touching and stroking with their partner.6
Present-day limits on the routine use of episiotomy and operative vaginal delivery have yielded a lower rate of third- and fourth-degree laceration.19 Second-degree lacerations are common and constitute the majority of perineal trauma in births without episiotomy.20 There is evidence that the use of synthetic absorbable suture, such as polyglactin, rather than chromic suture, results in less postpartum perineal pain, as does leaving the well-approximated perineal skin edges unsutured.20
Signorello and coworkers found that second-, third-, and fourth-degree lacerations increased the risk of postpartum dyspareunia; operative vaginal delivery (forceps or vacuum) was also an independent risk factor for dyspareunia.21
The impact of route of delivery
Some researchers have concluded that the route of delivery has an impact on the long-term pelvic floor health of women.18 In 1986, Snooks and colleagues analyzed possible obstetric risk factors for damage to the innervation of the pelvic floor, which can lead to both stress urinary and anorectal incontinence.22 They found that the process of vaginal delivery causes a compression and stretch type of injury to the pudendal nerve, as well as the possibility of severe perineal lacerations. This injury may be less likely to occur when cesarean delivery is performed before labor, avoiding direct perineal trauma and possible pudendal neuropathy.15 Because the pudendal nerve mediates some of the reflex pathways in the female sexual response, it is plausible that damage to it could result in sexual dysfunction.
Women who deliver vaginally have a higher rate of fecal and urinary incontinence than women who deliver by cesarean.16,23 The presence of incontinence, however, does not always have a significant long-term effect on one’s sexual life.6
In the Term Breech Trial, the route of delivery had no impact on the resumption of intercourse, dyspareunia, or sexual satisfaction.23 Although the trial was randomized and controlled, it had many limitations that call its generalizability into question in regard to postpartum sexual dysfunction.
The National Institutes of Health (NIH) State-of-the-Science Conference on Cesarean Delivery on Maternal Request indicated that, by 6 months postpartum, there is no difference in sexual function based on the route of delivery.24 However, Lydon-Rochelle and colleagues used the SF-36 to assess reported general health status and found that women who had cesarean delivery or assisted vaginal delivery exhibited significantly poorer postpartum functional status than women who had spontaneous vaginal delivery in five areas at 7 weeks postpartum: physical functioning, mental health, general health perception, bodily pain, social functioning, and ability to perform daily activities.25 Women were more likely to be readmitted to the hospital and more likely to report fatigue during the first 2 months after cesarean delivery.9 It appears that women who undergo cesarean delivery have an elevated risk of nondyspareunia-related causes of sexual dysfunction. Any protective effect of cesarean on sexual function is limited to the early postnatal period and is related to the absence of perineal injury.18
How breastfeeding can affect sexual desire
Evidence is strong that breastfeeding reduces a woman’s sexual desire and the frequency of intercourse.1,5 A high level of prolactin suppresses ovarian production of estrogen, thereby reducing vaginal lubrication. Some women and their partner may identify this loss of lubrication as a lack of arousal. This type of vaginal dryness should be explained, and the use of a lubricant should be encouraged in breastfeeding women.
Nipple sensitivity may develop, making touching and foreplay uncomfortable in some women. One third to one half of mothers find breastfeeding to be an erotic experience, and one fourth feel guilty about this sexual excitement; others stop nursing or wean early due to these feelings.1,7 Women are often not educated about the relationship between the release of oxytocin, uterine contractions, milk ejection, sexual arousal, and orgasm; raising the subject can help to diminish any potential distress over this response.
Sleep disturbances from feeding on demand contribute to fatigue and exhaustion.
Many women may not realize that their loss of interest in sex may be because they are receiving sufficient physical contact or touching through their nurturing interactions with the baby. This may leave the partner feeling isolated and envious of the mother-baby relationship.
Couples should be encouraged to discuss these feelings to avoid misperceptions and to maintain the relationship dyad as a priority to prevent the development of relationship problems.
The majority of women will discuss contraception with a health provider, but only 15% will voluntarily discuss their sexual needs or dysfunction.17 This finding is alarming given that, during the postpartum period, two of every three new mothers will experience at least one problem related to sexual function, including dyspareunia, decreased libido, difficulty achieving orgasm, and vaginal dryness.41 This lack of discussion with a health-care provider may be the result of several variables: incomplete knowledge on the part of the provider about what affects sexual function, poor training in the taking of an effective sexual history, and uneasiness on the part of the patient about discussing the issue.5,42
Postnatal depression takes a toll
Depressed mood and emotional lability in the postpartum period are negatively associated with sexual interest, enjoyment, coital activity, and perceived tenderness of the partner.7 Conversely, reduced sexual interest, desire and satisfaction; a lower frequency of intercourse; and later resumption of intercourse are associated with a higher number of psychiatric symptoms in the postpartum period.2 Between 10% and 15% of women experience postpartum depression (PPD).26 Depression has been associated with a decreased frequency and interest in sexual activity at 8 to 12 weeks postpartum.2,5
Chivers and colleagues assessed sexual functioning and sexual behavior in women with and without symptoms of PPD using the FSFI and EPDS. Although theirs was a small study, they found that women who had depressive symptoms also reported poorer functioning in regard to sexual arousal, orgasm, pain, lubrication, and sexual satisfaction.26 Morof and coworkers found that women who had PPD were less likely to have resumed intercourse by 6 months postpartum; they were also less likely to engage in other sexual activities.27
Role of pharmacotherapy
Many women are started on antidepressant medication near the time of delivery or during the immediate postpartum period. Often, serotonin reuptake inhibitors (SRIs) are used because there is minimal transmission of this class of medication through breast milk. However, the potential sexual side effects of these medications should be discussed because they are the agents most commonly associated with female sexual dysfunction.28
For clinicians
American Association of Sex Educators, Counselors, and Therapists – A not-for-profit, interdisciplinary professional organization comprising sexuality educators, sexuality counselors, sex therapists, physicians, social workers, and other clinicians. Its home page links to a referral page and other resources. http://www.aasect.org" target="_blank">http://www.aasect.org
Association of Reproductive Health Professionals offers a resource for clinicians on postpartum counseling about sexuality. http://www.arhp.org/publications-and-resources/quick-reference-guide-for-clinicians/postpartum-counseling/contraception" target="_blank">http://www.arhp.org/publications-and-resources/quick-reference-guide-for-clinicians/postpartum-counseling/contraception
For patients
Mayo Clinic provides a fact sheet entitled “Sex after pregnancy: Set your own timeline.” http://www.mayoclinic.com/health/sex-after-pregnancy/PR00146" target="_blank">http://www.mayoclinic.com/health/sex-after-pregnancy/PR00146
Sex and a Healthier You – This site offers information for patients on sexuality and relationships. http://www.sexandahealthieryou.org/sex-health/index.html" target="_blank">http://www.sexandahealthieryou.org/sex-health/index.html
We want to hear from you! Tell us what you think.
1. Reamy KJ, White SE. Sexuality in the puerperium: a review. Arch Sex Behav. 1987;16(2):165-186.
2. De Judicibus MA, McCabe MP. Psychological factors and the sexuality of pregnant and postpartum women. J Sex Res. 2002;39(2):94-103.
3. The puerperium. In: Cunningham FG Leveno KJ, Bloom SL, Hauth JC, Rouse DJ, Spong CY, eds. Williams Obstetrics. 23rd ed. New York, NY: McGraw-Hill Co.; 2010:646-660.
4. The American Academy of Pediatrics (AAP), American College of Obstetricians Gynecologists (ACOG) Guidelines for perinatal care. 6th ed. Washington DC: AAP, ACOG; 2008.
5. Glazener CM. Sexual function after childbirth: women’s experiences persistent morbidity and lack of professional recognition. Br J Obstet Gynaecol. 1997;104(3):330-335.
6. Rogers RG, Borders, N,, Leeman L, Albers L. Does spontaneous genital tract trauma impact postpartum sexual function? J Midwifery Womens Health. 2009;54(2):98-103.
7. von Sydow K. Sexuality during pregnancy and after childbirth: a metacontent analysis of 59 studies. J Psychosom Res. 1999;47(1):27-49.
8. Witting K, Santtila P, Alanko K, et al. Female sexual function and its associations with number of children, pregnancy, and relationship satisfaction. J Sex Marital Ther. 2008;34(2):89-106.
9. Thompson JF, Roberts CL, Currie M, Elwood DA. Prevalence and persistence of health problems after childbirth: associations with parity and method of birth. Birth. 2002;29(2):83-94.
10. Waterstone M, Wolfe C, Hooper R, Bewley S. Postnatal morbidity after childbirth and severe obstetric morbidity. BJOG. 2003;110(2):128-133.
11. Pauls RN, Occhino JA, Dryfhout VL. Effects of pregnancy on female sexual function and body image: A prospective study. J Sex Med. 2008;5(8):1915-1922.
12. von Sydow K, Ullmeyer M, Happ N. Sexual activity during pregnancy and after childbirth: Results from the Sexual P Questionnaire. J Psychosom Obstet Gynaecol. 2001;22(1):29-40.
13. Uebersax JS, Wyman JF, Shumaker SA, McClish DK, Fantl JA. Short forms to assess life quality and symptom distress for urinary incontinence in women: The Incontinence Impact Questionnaire and the Urogenital Distress Inventory. Continence Program for Women Rsearch Group. Neurourol Urodyn. 1995;14(2):131-139.
14. Barber MD, Visco AG, Wyman JF, Fantl JA, Bump RC; Continence Program for Women Research Group. Sexual function in women with urinary incontinence and pelvic organ prolapse. Obstet Gynecol. 2002;99(2):281-289.
15. Handa VL. Sexual function and childbirth. Semin Perinatol. 2006;30(5):253-256.
16. Klein MC, Gauthier RJ, Robbins JM, et al. Relationship of episiotomy to perineal trauma and morbidity, sexual dysfunction, and pelvic floor relaxation. Am J Obstet Gynecol. 1994;171(3):591-598.
17. Barrett G, Pendry E, Peacock J, Victor C, Thakar, Manyonda I. Women’s sexual health after childbirth. BJOG. 2000;107(2):186-195.
18. Barrett G, Peacock J, Victor CR, Manyonda I. Cesarean section and postnatal sexual health. Birth. 2005;32(4):306-311.
19. Eason E, Labrecque M, Wells G, Feldman P. Preventing perineal trauma during childbirth: a systematic review. Obstet Gynecol. 2000;95(3):464-471.
20. Leeman LM, Rogers RG, Greulich B, Albers LL. Do unsutured second-degree perineal lacerations affect postpartum functional outcomes? J Am Board Fam Med. 2007;20(5):451-457.
21. Signorello L, Harlow BL, Chekos AK, Repke JT. Postpartum sexual functioning and its relationship to perineal trauma: A retrospective cohort study of primiparous women. Am J Obstet Gynecol. 2001;184(5):881-890.
22. Snooks SJ, Swash M, Henry MW, Setchell M. Risk factors in childbirth causing damage to the pelvic floor innervation. In J Colorect Dis. 1986;1(1):20-24.
23. Hannah ME, Whyte H, Hannah WJ, et al. Term Breech Trial Collaborative Group. Maternal outcomes at 2 years after planned cesarean section versus planned vaginal birth for breech presentation at term: the international randomized Term Breech Trial. Am J Obstet Gynecol. 2004;191(3):917-927.
24. NIH State-of-the-Science Conference Statement on Cesarean Delivery on Maternal Request NIH Consens Sci Statements. 2006;23:1-29.http://consensus.nih.gov/2006/cesareanstatement.htm. Accessed December 6 2011.
25. Lydon-Rochelle MT, Holt VL, Martin DP. Delivery method and self-reported postpartum general health status among primiparous women. Paediatr Perinat Epidemiol. 2001;15(3):232-240.
26. Chivers ML, Pittini MD, Grigoriadis S, Villegas L, Ross LE. The relationship between sexual functioning and depressive symptomatology in postpartum women: a pilot study. J Sex Med. 2011;8(3):792-799.
27. Morof D, Barrett G, Peacock J, Victor CR, Manyonda I. Postnatal depression and sexual health after childbirth. Obstet Gynecol. 2003;102(6):1318-1325.
28. American College of Obstetricians and Gynecologists Committee on Practice Bulletins-Gynecology. ACOG Practice Bulletin No.119: Female sexual dysfunction. Obstet Gynecol. 2011;117(4):996-1007.
29. Read J. Sexual problems associated with infertility pregnancy and ageing. BMJ. 2004;329(7465):559-561.
30. Rosen R, Brown C, Heiman J, et al. The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000;26:191-208.
31. Isidori AM, Pozza C, Esposito K, et al. The Female Sexual Function Index (FSFI): Development and validation of a 6-item version of the female sexual function index (FSFI) as a diagnostic tool for female sexual dysfunction. J Sex Med. 2010;7(3):1139-11.
32. McCoy NL. The McCoy Female Sexuality Questionnaire. Quality Life Res. 2000;9(suppl 6):739-745.
33. Hatzichristou D, Rosen RC, Derogatis LR, et al. Recommendations for the clinical evaluation of men and women with sexual dysfunction. J Sex Med. 2010;7(1 Pt 1):337-348.
34. DeRogatis LR, Allgood A, Rosen RC, Leiblum S, Zipfel L, Guo CY. Development and evaluation of the Women’s Sexual Interest Diagnostic Interview (WSID): a structured interview to diagnose hypoactive sexual desire disorder (HSDD) in standardized patients. J Sex Med. 2008;5(12):2827-2841.
35. Fischman SH, Rankin EA, Soeken KL, Lenz ER. Changes in sexual relationships in postpartum couples. J Obstet Gynecol Neonatal Nurs. 1986;15(1):58-63.
36. Sillis T, Wunderlich G, Pyke R, et al. The Sexual Interest and Desire Inventory-Female (SIDI-F): item response analyses of data from women diagnosed with hypoactive sexual desire disorder. J Sex Med. 2005;2(6):801-818.
37. Rust J, Golombok S. The Golombok-Rust Inventory of Sexual Satisfaction (GRISS). Br J Clin Psych. 1985;24(Pt 1):63-64.
38. Clayton AH, Balon R. The impact of mental illness and psychotropic medications on sexual functioning: the evidence and management. J Sex Med. 2009;6(5):1200-1213.
39. Jennings B, Edmundson M. The postpartum period: after confinement: the fourth trimester. Clin Obstet Gynecol. 1980;23(4):1093-1103.
40. Oppenheimer LS, Sheriff EA, Goodman JDS, shah D, James CE. The duration of lochia. Br J Obstet Gynaecol. 1986;93(7):754-757.
41. Connolly A, Thorp J, Pahel L. Effects of pregnancy and childbirth on postpartum sexual function: a longitudinal prospective study. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16(4):263-267.
42. Pancholy AB, Goldenhar L, Fellner AN, Crisp C, Kleeman S, Pauls R. Resident education and training in female sexuality: results of a national survey. J Sex Med. 2011;8(2):361-366.
1. Reamy KJ, White SE. Sexuality in the puerperium: a review. Arch Sex Behav. 1987;16(2):165-186.
2. De Judicibus MA, McCabe MP. Psychological factors and the sexuality of pregnant and postpartum women. J Sex Res. 2002;39(2):94-103.
3. The puerperium. In: Cunningham FG Leveno KJ, Bloom SL, Hauth JC, Rouse DJ, Spong CY, eds. Williams Obstetrics. 23rd ed. New York, NY: McGraw-Hill Co.; 2010:646-660.
4. The American Academy of Pediatrics (AAP), American College of Obstetricians Gynecologists (ACOG) Guidelines for perinatal care. 6th ed. Washington DC: AAP, ACOG; 2008.
5. Glazener CM. Sexual function after childbirth: women’s experiences persistent morbidity and lack of professional recognition. Br J Obstet Gynaecol. 1997;104(3):330-335.
6. Rogers RG, Borders, N,, Leeman L, Albers L. Does spontaneous genital tract trauma impact postpartum sexual function? J Midwifery Womens Health. 2009;54(2):98-103.
7. von Sydow K. Sexuality during pregnancy and after childbirth: a metacontent analysis of 59 studies. J Psychosom Res. 1999;47(1):27-49.
8. Witting K, Santtila P, Alanko K, et al. Female sexual function and its associations with number of children, pregnancy, and relationship satisfaction. J Sex Marital Ther. 2008;34(2):89-106.
9. Thompson JF, Roberts CL, Currie M, Elwood DA. Prevalence and persistence of health problems after childbirth: associations with parity and method of birth. Birth. 2002;29(2):83-94.
10. Waterstone M, Wolfe C, Hooper R, Bewley S. Postnatal morbidity after childbirth and severe obstetric morbidity. BJOG. 2003;110(2):128-133.
11. Pauls RN, Occhino JA, Dryfhout VL. Effects of pregnancy on female sexual function and body image: A prospective study. J Sex Med. 2008;5(8):1915-1922.
12. von Sydow K, Ullmeyer M, Happ N. Sexual activity during pregnancy and after childbirth: Results from the Sexual P Questionnaire. J Psychosom Obstet Gynaecol. 2001;22(1):29-40.
13. Uebersax JS, Wyman JF, Shumaker SA, McClish DK, Fantl JA. Short forms to assess life quality and symptom distress for urinary incontinence in women: The Incontinence Impact Questionnaire and the Urogenital Distress Inventory. Continence Program for Women Rsearch Group. Neurourol Urodyn. 1995;14(2):131-139.
14. Barber MD, Visco AG, Wyman JF, Fantl JA, Bump RC; Continence Program for Women Research Group. Sexual function in women with urinary incontinence and pelvic organ prolapse. Obstet Gynecol. 2002;99(2):281-289.
15. Handa VL. Sexual function and childbirth. Semin Perinatol. 2006;30(5):253-256.
16. Klein MC, Gauthier RJ, Robbins JM, et al. Relationship of episiotomy to perineal trauma and morbidity, sexual dysfunction, and pelvic floor relaxation. Am J Obstet Gynecol. 1994;171(3):591-598.
17. Barrett G, Pendry E, Peacock J, Victor C, Thakar, Manyonda I. Women’s sexual health after childbirth. BJOG. 2000;107(2):186-195.
18. Barrett G, Peacock J, Victor CR, Manyonda I. Cesarean section and postnatal sexual health. Birth. 2005;32(4):306-311.
19. Eason E, Labrecque M, Wells G, Feldman P. Preventing perineal trauma during childbirth: a systematic review. Obstet Gynecol. 2000;95(3):464-471.
20. Leeman LM, Rogers RG, Greulich B, Albers LL. Do unsutured second-degree perineal lacerations affect postpartum functional outcomes? J Am Board Fam Med. 2007;20(5):451-457.
21. Signorello L, Harlow BL, Chekos AK, Repke JT. Postpartum sexual functioning and its relationship to perineal trauma: A retrospective cohort study of primiparous women. Am J Obstet Gynecol. 2001;184(5):881-890.
22. Snooks SJ, Swash M, Henry MW, Setchell M. Risk factors in childbirth causing damage to the pelvic floor innervation. In J Colorect Dis. 1986;1(1):20-24.
23. Hannah ME, Whyte H, Hannah WJ, et al. Term Breech Trial Collaborative Group. Maternal outcomes at 2 years after planned cesarean section versus planned vaginal birth for breech presentation at term: the international randomized Term Breech Trial. Am J Obstet Gynecol. 2004;191(3):917-927.
24. NIH State-of-the-Science Conference Statement on Cesarean Delivery on Maternal Request NIH Consens Sci Statements. 2006;23:1-29.http://consensus.nih.gov/2006/cesareanstatement.htm. Accessed December 6 2011.
25. Lydon-Rochelle MT, Holt VL, Martin DP. Delivery method and self-reported postpartum general health status among primiparous women. Paediatr Perinat Epidemiol. 2001;15(3):232-240.
26. Chivers ML, Pittini MD, Grigoriadis S, Villegas L, Ross LE. The relationship between sexual functioning and depressive symptomatology in postpartum women: a pilot study. J Sex Med. 2011;8(3):792-799.
27. Morof D, Barrett G, Peacock J, Victor CR, Manyonda I. Postnatal depression and sexual health after childbirth. Obstet Gynecol. 2003;102(6):1318-1325.
28. American College of Obstetricians and Gynecologists Committee on Practice Bulletins-Gynecology. ACOG Practice Bulletin No.119: Female sexual dysfunction. Obstet Gynecol. 2011;117(4):996-1007.
29. Read J. Sexual problems associated with infertility pregnancy and ageing. BMJ. 2004;329(7465):559-561.
30. Rosen R, Brown C, Heiman J, et al. The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000;26:191-208.
31. Isidori AM, Pozza C, Esposito K, et al. The Female Sexual Function Index (FSFI): Development and validation of a 6-item version of the female sexual function index (FSFI) as a diagnostic tool for female sexual dysfunction. J Sex Med. 2010;7(3):1139-11.
32. McCoy NL. The McCoy Female Sexuality Questionnaire. Quality Life Res. 2000;9(suppl 6):739-745.
33. Hatzichristou D, Rosen RC, Derogatis LR, et al. Recommendations for the clinical evaluation of men and women with sexual dysfunction. J Sex Med. 2010;7(1 Pt 1):337-348.
34. DeRogatis LR, Allgood A, Rosen RC, Leiblum S, Zipfel L, Guo CY. Development and evaluation of the Women’s Sexual Interest Diagnostic Interview (WSID): a structured interview to diagnose hypoactive sexual desire disorder (HSDD) in standardized patients. J Sex Med. 2008;5(12):2827-2841.
35. Fischman SH, Rankin EA, Soeken KL, Lenz ER. Changes in sexual relationships in postpartum couples. J Obstet Gynecol Neonatal Nurs. 1986;15(1):58-63.
36. Sillis T, Wunderlich G, Pyke R, et al. The Sexual Interest and Desire Inventory-Female (SIDI-F): item response analyses of data from women diagnosed with hypoactive sexual desire disorder. J Sex Med. 2005;2(6):801-818.
37. Rust J, Golombok S. The Golombok-Rust Inventory of Sexual Satisfaction (GRISS). Br J Clin Psych. 1985;24(Pt 1):63-64.
38. Clayton AH, Balon R. The impact of mental illness and psychotropic medications on sexual functioning: the evidence and management. J Sex Med. 2009;6(5):1200-1213.
39. Jennings B, Edmundson M. The postpartum period: after confinement: the fourth trimester. Clin Obstet Gynecol. 1980;23(4):1093-1103.
40. Oppenheimer LS, Sheriff EA, Goodman JDS, shah D, James CE. The duration of lochia. Br J Obstet Gynaecol. 1986;93(7):754-757.
41. Connolly A, Thorp J, Pahel L. Effects of pregnancy and childbirth on postpartum sexual function: a longitudinal prospective study. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16(4):263-267.
42. Pancholy AB, Goldenhar L, Fellner AN, Crisp C, Kleeman S, Pauls R. Resident education and training in female sexuality: results of a national survey. J Sex Med. 2011;8(2):361-366.

