User login
Does a short course of nitrofurantoin cure acute uncomplicated cystitis?
In this randomized trial, 338 women 18 to 45 years old who had acute uncomplicated urinary tract infection (UTI) were randomized to open-label treatment with nitrofurantoin (Macrobid), 100 mg twice daily for 5 days, or trimethoprim-sulfamethoxazole, one double-strength tablet twice daily for 3 days. Clinical cure 30 days after therapy was achieved in 84% of the women taking nitrofurantoin and in 79% of women taking trimethoprim-sulfamethoxazole.
EXPERT COMMENTARY
This study is important because UTI is routinely treated empirically. The usual drugs prescribed for uncomplicated UTI are TMP-SMX, extended-release ciprofloxacin (Cipro), or a first- or second-generation cephalosporin. Empiric use of fluoroquinolones such as ciprofloxacin has replaced trimethoprim-sulfamethoxazole in the treatment of uncomplicated cystitis. Such replacements are inappropriate for empiric therapy, and indiscriminate use of fluoroquinolones has led to increased resistance among Staphylococcus aureus organisms.
Nor has there been proper concern about the way antibiotics alter the endogenous bacteria of the body. Overuse of antibiotics such as the β-lactams (cephalosporin and expanded-spectrum penicillins), fluoroquinolones, and macrolides has added not only to the emergence of resistant bacteria strains but also to an increase in adverse events.
Resistance to TMP-SMX ranged from 12% to 21%
In this study, the authors isolated and identified bacteria responsible for infection, and the outcome reflects the national bacterial etiology in this age group (18 to 45 years). The number one bacterium isolated in the study was Escherichia coli (82%) as the sole uropathogen (TABLE). These data confirm that E coli remains the bacterium most likely to cause acute uncomplicated UTI.
The problem is that E coli has developed resistance to the antibiotics most commonly prescribed to treat this condition. In this study, 12% of the E coli isolates were resistant to trimethoprim-sulfamethoxazole. Even more alarming, 21% of non-E coli strains were resistant to trimethoprim-sulfamethoxazole. In contrast, 99.6% of E coli isolates and 90% of non-E coli isolates were sensitive to nitrofurantoin.
TABLE
Bacteria isolated from the study population (n=338)
| BACTERIUM | NUMBER OF ISOLATES |
|---|---|
| Escherichia coli | 276 |
| Non-E coli | 61 |
| Staphylococcus aureus | 5 |
| Klebsiella species, Proteus mirabilis, Enterobacter species, and Streptococcus agalactiae made up the remainder of the isolates (1% to 3%). | |
Adverse effects did not deter use
In the trimethoprim-sulfamethoxazole group, 31% of women experienced adverse effects, as did 28% in the nitrofurantoin group. Side effects included those commonly seen with oral antibiotic therapy: nausea, diarrhea, headache, lightheadedness, and vaginal itching.
Adherence was good; only 1% of women taking trimethoprim-sulfamethoxazole and 2% of women taking nitrofurantoin discontinued the drug.
An advantage for women taking nitrofurantoin is that it is concentrated in the urine, with little uptake in tissue and other bodily fluids. Therefore, it has very little effect on the endogenous vaginal microflora and little chance of causing vaginitis.
Weaknesses of the study
This study was not blinded; therefore, clinical evaluation may have been biased.
The population involved in the study was rather homogenous—mostly white college students. A mix of races would have been more informative.
Another limitation is that the investigators chose cefotaxime (Claforan) as one of the comparative antibiotics in the microbiologic arm, but gave no reason for this choice. Cefotaxime is administered either intravenously or intramuscularly and therefore has questionable relevance to this study. The other antibiotics chosen in addition to the two study drugs were ciprofloxacin and amoxicillin-clavulanate—both commonly used to treat acute uncomplicated cystitis.
A 5-day course of nitrofurantoin is highly effective in treating uncomplicated UTI in women. It should be the initial empiric treatment of this infection because it is effective, safe, and well tolerated.
If a 3-day course of trimethoprim-sulfamethoxazole is used, the clinician should be aware that, as E coli resistance to this agent increases, its efficacy decreases.—Sebastian Faro, MD, PhD
In this randomized trial, 338 women 18 to 45 years old who had acute uncomplicated urinary tract infection (UTI) were randomized to open-label treatment with nitrofurantoin (Macrobid), 100 mg twice daily for 5 days, or trimethoprim-sulfamethoxazole, one double-strength tablet twice daily for 3 days. Clinical cure 30 days after therapy was achieved in 84% of the women taking nitrofurantoin and in 79% of women taking trimethoprim-sulfamethoxazole.
EXPERT COMMENTARY
This study is important because UTI is routinely treated empirically. The usual drugs prescribed for uncomplicated UTI are TMP-SMX, extended-release ciprofloxacin (Cipro), or a first- or second-generation cephalosporin. Empiric use of fluoroquinolones such as ciprofloxacin has replaced trimethoprim-sulfamethoxazole in the treatment of uncomplicated cystitis. Such replacements are inappropriate for empiric therapy, and indiscriminate use of fluoroquinolones has led to increased resistance among Staphylococcus aureus organisms.
Nor has there been proper concern about the way antibiotics alter the endogenous bacteria of the body. Overuse of antibiotics such as the β-lactams (cephalosporin and expanded-spectrum penicillins), fluoroquinolones, and macrolides has added not only to the emergence of resistant bacteria strains but also to an increase in adverse events.
Resistance to TMP-SMX ranged from 12% to 21%
In this study, the authors isolated and identified bacteria responsible for infection, and the outcome reflects the national bacterial etiology in this age group (18 to 45 years). The number one bacterium isolated in the study was Escherichia coli (82%) as the sole uropathogen (TABLE). These data confirm that E coli remains the bacterium most likely to cause acute uncomplicated UTI.
The problem is that E coli has developed resistance to the antibiotics most commonly prescribed to treat this condition. In this study, 12% of the E coli isolates were resistant to trimethoprim-sulfamethoxazole. Even more alarming, 21% of non-E coli strains were resistant to trimethoprim-sulfamethoxazole. In contrast, 99.6% of E coli isolates and 90% of non-E coli isolates were sensitive to nitrofurantoin.
TABLE
Bacteria isolated from the study population (n=338)
| BACTERIUM | NUMBER OF ISOLATES |
|---|---|
| Escherichia coli | 276 |
| Non-E coli | 61 |
| Staphylococcus aureus | 5 |
| Klebsiella species, Proteus mirabilis, Enterobacter species, and Streptococcus agalactiae made up the remainder of the isolates (1% to 3%). | |
Adverse effects did not deter use
In the trimethoprim-sulfamethoxazole group, 31% of women experienced adverse effects, as did 28% in the nitrofurantoin group. Side effects included those commonly seen with oral antibiotic therapy: nausea, diarrhea, headache, lightheadedness, and vaginal itching.
Adherence was good; only 1% of women taking trimethoprim-sulfamethoxazole and 2% of women taking nitrofurantoin discontinued the drug.
An advantage for women taking nitrofurantoin is that it is concentrated in the urine, with little uptake in tissue and other bodily fluids. Therefore, it has very little effect on the endogenous vaginal microflora and little chance of causing vaginitis.
Weaknesses of the study
This study was not blinded; therefore, clinical evaluation may have been biased.
The population involved in the study was rather homogenous—mostly white college students. A mix of races would have been more informative.
Another limitation is that the investigators chose cefotaxime (Claforan) as one of the comparative antibiotics in the microbiologic arm, but gave no reason for this choice. Cefotaxime is administered either intravenously or intramuscularly and therefore has questionable relevance to this study. The other antibiotics chosen in addition to the two study drugs were ciprofloxacin and amoxicillin-clavulanate—both commonly used to treat acute uncomplicated cystitis.
A 5-day course of nitrofurantoin is highly effective in treating uncomplicated UTI in women. It should be the initial empiric treatment of this infection because it is effective, safe, and well tolerated.
If a 3-day course of trimethoprim-sulfamethoxazole is used, the clinician should be aware that, as E coli resistance to this agent increases, its efficacy decreases.—Sebastian Faro, MD, PhD
In this randomized trial, 338 women 18 to 45 years old who had acute uncomplicated urinary tract infection (UTI) were randomized to open-label treatment with nitrofurantoin (Macrobid), 100 mg twice daily for 5 days, or trimethoprim-sulfamethoxazole, one double-strength tablet twice daily for 3 days. Clinical cure 30 days after therapy was achieved in 84% of the women taking nitrofurantoin and in 79% of women taking trimethoprim-sulfamethoxazole.
EXPERT COMMENTARY
This study is important because UTI is routinely treated empirically. The usual drugs prescribed for uncomplicated UTI are TMP-SMX, extended-release ciprofloxacin (Cipro), or a first- or second-generation cephalosporin. Empiric use of fluoroquinolones such as ciprofloxacin has replaced trimethoprim-sulfamethoxazole in the treatment of uncomplicated cystitis. Such replacements are inappropriate for empiric therapy, and indiscriminate use of fluoroquinolones has led to increased resistance among Staphylococcus aureus organisms.
Nor has there been proper concern about the way antibiotics alter the endogenous bacteria of the body. Overuse of antibiotics such as the β-lactams (cephalosporin and expanded-spectrum penicillins), fluoroquinolones, and macrolides has added not only to the emergence of resistant bacteria strains but also to an increase in adverse events.
Resistance to TMP-SMX ranged from 12% to 21%
In this study, the authors isolated and identified bacteria responsible for infection, and the outcome reflects the national bacterial etiology in this age group (18 to 45 years). The number one bacterium isolated in the study was Escherichia coli (82%) as the sole uropathogen (TABLE). These data confirm that E coli remains the bacterium most likely to cause acute uncomplicated UTI.
The problem is that E coli has developed resistance to the antibiotics most commonly prescribed to treat this condition. In this study, 12% of the E coli isolates were resistant to trimethoprim-sulfamethoxazole. Even more alarming, 21% of non-E coli strains were resistant to trimethoprim-sulfamethoxazole. In contrast, 99.6% of E coli isolates and 90% of non-E coli isolates were sensitive to nitrofurantoin.
TABLE
Bacteria isolated from the study population (n=338)
| BACTERIUM | NUMBER OF ISOLATES |
|---|---|
| Escherichia coli | 276 |
| Non-E coli | 61 |
| Staphylococcus aureus | 5 |
| Klebsiella species, Proteus mirabilis, Enterobacter species, and Streptococcus agalactiae made up the remainder of the isolates (1% to 3%). | |
Adverse effects did not deter use
In the trimethoprim-sulfamethoxazole group, 31% of women experienced adverse effects, as did 28% in the nitrofurantoin group. Side effects included those commonly seen with oral antibiotic therapy: nausea, diarrhea, headache, lightheadedness, and vaginal itching.
Adherence was good; only 1% of women taking trimethoprim-sulfamethoxazole and 2% of women taking nitrofurantoin discontinued the drug.
An advantage for women taking nitrofurantoin is that it is concentrated in the urine, with little uptake in tissue and other bodily fluids. Therefore, it has very little effect on the endogenous vaginal microflora and little chance of causing vaginitis.
Weaknesses of the study
This study was not blinded; therefore, clinical evaluation may have been biased.
The population involved in the study was rather homogenous—mostly white college students. A mix of races would have been more informative.
Another limitation is that the investigators chose cefotaxime (Claforan) as one of the comparative antibiotics in the microbiologic arm, but gave no reason for this choice. Cefotaxime is administered either intravenously or intramuscularly and therefore has questionable relevance to this study. The other antibiotics chosen in addition to the two study drugs were ciprofloxacin and amoxicillin-clavulanate—both commonly used to treat acute uncomplicated cystitis.
A 5-day course of nitrofurantoin is highly effective in treating uncomplicated UTI in women. It should be the initial empiric treatment of this infection because it is effective, safe, and well tolerated.
If a 3-day course of trimethoprim-sulfamethoxazole is used, the clinician should be aware that, as E coli resistance to this agent increases, its efficacy decreases.—Sebastian Faro, MD, PhD
Recent trials spotlight herpes, BV, and labor-related neutrophilia
Over the past few years, research in obstetric and gynecologic infectious diseases has led to improvements in diagnosis and management. Notable advances have been made in preventing group B streptococcus, sexually transmitted diseases, and postoperative pelvic infection.
Despite these successes and the development of broad-spectrum antibiotics, infection remains a serious cause of morbidity and mortality.
This update focuses on 3 studies from the past year:
- A randomized, controlled trial of famciclovir to suppress shedding of recurrent anogenital herpes simplex in women with and without symptoms,
- A randomized, controlled trial of metronidazole versus placebo in gravidas with asymptomatic bacterial vaginosis (BV), and
- The first non-observational investigation that explains the effects of labor on maternal neutrophil phenotype.
Using famciclovir to suppress shedding of recurrent anogenital herpes
Sacks SL. Famciclovir suppression of asymptomatic and symptomatic recurrent anogenital herpes simplex virus shedding in women: a randomized, double-blind, doubledummy, placebo-controlled, parallel-group, single-center trial. J Infect Dis. 2004;189:1341–1347.
- LEVEL I EVIDENCE: RANDOMIZED, CONTROLLED TRIAL
In this study, 169 women with frequently recurring, culture-proven, genital herpes simplex infection were randomized to famciclovir 125 mg, 250 mg, or placebo. Patients kept a daily diary of any symptoms, and each morning performed self-sampling from as high in the vagina as possible, with a second sample taken from external genitalia. This involved swabbing the mons pubis, clitoral hood, labia minora, labia majora, perineum, and the perianal area. Data were analyzed with appropriate statistical tests.
A significant reduction in asymptomatic viral shedding occurred with famciclovir treatment, compared with placebo (P<.0001 while reduction of viral shedding in symptomatic women was dose-dependent: for mg versus>P<.0001 versus for placebo>P<.0001>
This study is notable because viral shedding was reduced in both symptomatic and asymptomatic women. It also opens the door for studies in pregnant women known to have herpes, with the aim of reducing the risk of perinatal transmission.
Does metronidazole eliminate BV in asymptomatic gravidas?
Klebanoff MA, Hauth JC, MacPherson CA, et al. Time course of the regression of asymptomatic bacterial vaginosis in pregnancy with and without treatment. Am J Obstet Gynecol. 2004;190:363–370.
- LEVEL II-1 EVIDENCE: NONRANDOMIZED, CONTROLLED TRIAL
Resolution of BV was defined as a Nugent’s score of less than 7, and restoration of the normal vaginal microflora was defined as a score of less than 4. Overall, 72% and 55% of women in the metronidazole group had scores of less than 7 and less than 4, respectively, at follow-up. In the placebo group, these percentages were 21% and 11%, respectively.
Like most studies of BV, this one is flawed. The reason: Rather than conduct quantitative bacteriology, investigators used the Gram stain to interpret the microbiology of an ecosystem and then related it to a significant medical outcome: preterm birth. They attempted to define BV as an infectious disease and applied principles of infectious disease treatment to it. Most investigators define BV as an alteration in the endogenous microflora, specifically a flora dominated by obligate anaerobic bacteria. However, they treat it as an infection and administer an antibiotic to correct the alteration in the vaginal ecosystem.
Questions raised by this study include: How is asymptomatic BV defined? Is it truly asymptomatic, or have patients simply adapted to their condition? Do these patients have abnormal discharge in color, quantity, and odor?
In addition, the lack of definitive bacteriology in this study necessitates the following assumptions:
- All BV is similar; therefore, similar responses to antimicrobial therapy should be expected.
- A score below 7 but above 4 represents intermediate flora. This microflora is a precursor to BV or predisposes the patient to BV infection.
- A score below 4 represents Lactobacillus-dominant flora.
Lactobacillus. Moreover, it is necessary to determine the species of Lactobacillus present to confirm that it is the correct species to reestablish normal microflora.
Investigators did demonstrate a fact seen in most treatment studies: Metronidazole is not a particularly good agent for treating BV and restoring a patient’s vaginal ecology to Lactobacillus-dominant flora. However, they failed to demonstrate that treatment of asymptomatic BV reduces the risk of preterm delivery in a general obstetric population, or to establish a causal relationship between BV and preterm labor. This did not prevent them from asserting the idea that BV is a risk factor for preterm labor.
Investigators clouded their findings further by concluding that two 2-g doses of metronidazole administered 48 hours apart were effective in 72% of cases (defined as the elimination of BV) and 55% effective in restoring Gram stain scores to the normal range, noting that this effect lasted 2 to 10 weeks or longer. In reality, this is neither elimination of BV nor restoration of a normal range of microflora, but simply an interpretation of the change in Gram stain characteristics. The results do not explain what is happening microbiologically; nor do they clarify the host response to these changing conditions. Intensive quantitative bacteriology is needed, along with research into the microbial ecopathophysiology and host response to specific bacteria, in patients with and without healthy vaginal flora.
It is important to understand vaginal microflora because, when it is altered, it can impact negatively on the patient’s health. Therefore, studies that elucidate the vaginal ecology and the relationships between various bacteria further our understanding of the microbial pathophysiology leading to infection. This, in turn, leads to development of preventive measures, thus reducing the risk for adverse outcomes in both the obstetric and gynecologic patient—especially those undergoing operative procedures.
Is labor inherently protective against infection?
Molloy EJ, O’Neill AJ, Grantham JJ, et al. Labor induces a maternal inflammatory response syndrome. Am J Obstet Gynecol. 2004;190:448–455.
- LEVEL II-3 EVIDENCE: MULTIPLE OBSERVATIONS WITH OR WITHOUT INTERVENTION; UNCONTROLLED STUDIES
Although the number of participants was relatively small, this study was well considered and constructed, investigating several immunologic responses in 5 groups of patients:
- 15 nonpregnant healthy women and 17 healthy men,
- 15 healthy women in labor at term before delivery,
- 9 women with normal term pregnancies before elective cesarean with no labor,
- 9 women before emergency cesarean section after partial labor, and
- 9 women at term before emergency cesarean section without labor.
Interestingly, researchers also observed an increase of CD11b, an adhesion molecule and marker for neutrophil activation. Increased CD11b results in greater neutrophil activity.
Investigators concluded that the rise in neutrophils and diminished apoptosis in laboring patients may be an immunologic response to potential infection associated with labor, and that this phenomenon appears to be an inherent host reaction to prevent infection. It is known that bacteria from the genital tract of laboring women ascend into the uterus and amniotic fluid and colonize the decidua, amniotic membranes, and amniotic fluid. Women subsequently delivered by cesarean section are at a greater risk of infection than women delivered vaginally.
This is an extremely important finding and the first non-observational study to explain the rise in white blood cell counts during labor. It begins to explain the differences in white blood cell counts between laboring and nonlaboring patients and should spawn further investigations of a significant problem: postpartum endometritis.
Dr. Faro reports no financial relationships relevant to this article.
Over the past few years, research in obstetric and gynecologic infectious diseases has led to improvements in diagnosis and management. Notable advances have been made in preventing group B streptococcus, sexually transmitted diseases, and postoperative pelvic infection.
Despite these successes and the development of broad-spectrum antibiotics, infection remains a serious cause of morbidity and mortality.
This update focuses on 3 studies from the past year:
- A randomized, controlled trial of famciclovir to suppress shedding of recurrent anogenital herpes simplex in women with and without symptoms,
- A randomized, controlled trial of metronidazole versus placebo in gravidas with asymptomatic bacterial vaginosis (BV), and
- The first non-observational investigation that explains the effects of labor on maternal neutrophil phenotype.
Using famciclovir to suppress shedding of recurrent anogenital herpes
Sacks SL. Famciclovir suppression of asymptomatic and symptomatic recurrent anogenital herpes simplex virus shedding in women: a randomized, double-blind, doubledummy, placebo-controlled, parallel-group, single-center trial. J Infect Dis. 2004;189:1341–1347.
- LEVEL I EVIDENCE: RANDOMIZED, CONTROLLED TRIAL
In this study, 169 women with frequently recurring, culture-proven, genital herpes simplex infection were randomized to famciclovir 125 mg, 250 mg, or placebo. Patients kept a daily diary of any symptoms, and each morning performed self-sampling from as high in the vagina as possible, with a second sample taken from external genitalia. This involved swabbing the mons pubis, clitoral hood, labia minora, labia majora, perineum, and the perianal area. Data were analyzed with appropriate statistical tests.
A significant reduction in asymptomatic viral shedding occurred with famciclovir treatment, compared with placebo (P<.0001 while reduction of viral shedding in symptomatic women was dose-dependent: for mg versus>P<.0001 versus for placebo>P<.0001>
This study is notable because viral shedding was reduced in both symptomatic and asymptomatic women. It also opens the door for studies in pregnant women known to have herpes, with the aim of reducing the risk of perinatal transmission.
Does metronidazole eliminate BV in asymptomatic gravidas?
Klebanoff MA, Hauth JC, MacPherson CA, et al. Time course of the regression of asymptomatic bacterial vaginosis in pregnancy with and without treatment. Am J Obstet Gynecol. 2004;190:363–370.
- LEVEL II-1 EVIDENCE: NONRANDOMIZED, CONTROLLED TRIAL
Resolution of BV was defined as a Nugent’s score of less than 7, and restoration of the normal vaginal microflora was defined as a score of less than 4. Overall, 72% and 55% of women in the metronidazole group had scores of less than 7 and less than 4, respectively, at follow-up. In the placebo group, these percentages were 21% and 11%, respectively.
Like most studies of BV, this one is flawed. The reason: Rather than conduct quantitative bacteriology, investigators used the Gram stain to interpret the microbiology of an ecosystem and then related it to a significant medical outcome: preterm birth. They attempted to define BV as an infectious disease and applied principles of infectious disease treatment to it. Most investigators define BV as an alteration in the endogenous microflora, specifically a flora dominated by obligate anaerobic bacteria. However, they treat it as an infection and administer an antibiotic to correct the alteration in the vaginal ecosystem.
Questions raised by this study include: How is asymptomatic BV defined? Is it truly asymptomatic, or have patients simply adapted to their condition? Do these patients have abnormal discharge in color, quantity, and odor?
In addition, the lack of definitive bacteriology in this study necessitates the following assumptions:
- All BV is similar; therefore, similar responses to antimicrobial therapy should be expected.
- A score below 7 but above 4 represents intermediate flora. This microflora is a precursor to BV or predisposes the patient to BV infection.
- A score below 4 represents Lactobacillus-dominant flora.
Lactobacillus. Moreover, it is necessary to determine the species of Lactobacillus present to confirm that it is the correct species to reestablish normal microflora.
Investigators did demonstrate a fact seen in most treatment studies: Metronidazole is not a particularly good agent for treating BV and restoring a patient’s vaginal ecology to Lactobacillus-dominant flora. However, they failed to demonstrate that treatment of asymptomatic BV reduces the risk of preterm delivery in a general obstetric population, or to establish a causal relationship between BV and preterm labor. This did not prevent them from asserting the idea that BV is a risk factor for preterm labor.
Investigators clouded their findings further by concluding that two 2-g doses of metronidazole administered 48 hours apart were effective in 72% of cases (defined as the elimination of BV) and 55% effective in restoring Gram stain scores to the normal range, noting that this effect lasted 2 to 10 weeks or longer. In reality, this is neither elimination of BV nor restoration of a normal range of microflora, but simply an interpretation of the change in Gram stain characteristics. The results do not explain what is happening microbiologically; nor do they clarify the host response to these changing conditions. Intensive quantitative bacteriology is needed, along with research into the microbial ecopathophysiology and host response to specific bacteria, in patients with and without healthy vaginal flora.
It is important to understand vaginal microflora because, when it is altered, it can impact negatively on the patient’s health. Therefore, studies that elucidate the vaginal ecology and the relationships between various bacteria further our understanding of the microbial pathophysiology leading to infection. This, in turn, leads to development of preventive measures, thus reducing the risk for adverse outcomes in both the obstetric and gynecologic patient—especially those undergoing operative procedures.
Is labor inherently protective against infection?
Molloy EJ, O’Neill AJ, Grantham JJ, et al. Labor induces a maternal inflammatory response syndrome. Am J Obstet Gynecol. 2004;190:448–455.
- LEVEL II-3 EVIDENCE: MULTIPLE OBSERVATIONS WITH OR WITHOUT INTERVENTION; UNCONTROLLED STUDIES
Although the number of participants was relatively small, this study was well considered and constructed, investigating several immunologic responses in 5 groups of patients:
- 15 nonpregnant healthy women and 17 healthy men,
- 15 healthy women in labor at term before delivery,
- 9 women with normal term pregnancies before elective cesarean with no labor,
- 9 women before emergency cesarean section after partial labor, and
- 9 women at term before emergency cesarean section without labor.
Interestingly, researchers also observed an increase of CD11b, an adhesion molecule and marker for neutrophil activation. Increased CD11b results in greater neutrophil activity.
Investigators concluded that the rise in neutrophils and diminished apoptosis in laboring patients may be an immunologic response to potential infection associated with labor, and that this phenomenon appears to be an inherent host reaction to prevent infection. It is known that bacteria from the genital tract of laboring women ascend into the uterus and amniotic fluid and colonize the decidua, amniotic membranes, and amniotic fluid. Women subsequently delivered by cesarean section are at a greater risk of infection than women delivered vaginally.
This is an extremely important finding and the first non-observational study to explain the rise in white blood cell counts during labor. It begins to explain the differences in white blood cell counts between laboring and nonlaboring patients and should spawn further investigations of a significant problem: postpartum endometritis.
Dr. Faro reports no financial relationships relevant to this article.
Over the past few years, research in obstetric and gynecologic infectious diseases has led to improvements in diagnosis and management. Notable advances have been made in preventing group B streptococcus, sexually transmitted diseases, and postoperative pelvic infection.
Despite these successes and the development of broad-spectrum antibiotics, infection remains a serious cause of morbidity and mortality.
This update focuses on 3 studies from the past year:
- A randomized, controlled trial of famciclovir to suppress shedding of recurrent anogenital herpes simplex in women with and without symptoms,
- A randomized, controlled trial of metronidazole versus placebo in gravidas with asymptomatic bacterial vaginosis (BV), and
- The first non-observational investigation that explains the effects of labor on maternal neutrophil phenotype.
Using famciclovir to suppress shedding of recurrent anogenital herpes
Sacks SL. Famciclovir suppression of asymptomatic and symptomatic recurrent anogenital herpes simplex virus shedding in women: a randomized, double-blind, doubledummy, placebo-controlled, parallel-group, single-center trial. J Infect Dis. 2004;189:1341–1347.
- LEVEL I EVIDENCE: RANDOMIZED, CONTROLLED TRIAL
In this study, 169 women with frequently recurring, culture-proven, genital herpes simplex infection were randomized to famciclovir 125 mg, 250 mg, or placebo. Patients kept a daily diary of any symptoms, and each morning performed self-sampling from as high in the vagina as possible, with a second sample taken from external genitalia. This involved swabbing the mons pubis, clitoral hood, labia minora, labia majora, perineum, and the perianal area. Data were analyzed with appropriate statistical tests.
A significant reduction in asymptomatic viral shedding occurred with famciclovir treatment, compared with placebo (P<.0001 while reduction of viral shedding in symptomatic women was dose-dependent: for mg versus>P<.0001 versus for placebo>P<.0001>
This study is notable because viral shedding was reduced in both symptomatic and asymptomatic women. It also opens the door for studies in pregnant women known to have herpes, with the aim of reducing the risk of perinatal transmission.
Does metronidazole eliminate BV in asymptomatic gravidas?
Klebanoff MA, Hauth JC, MacPherson CA, et al. Time course of the regression of asymptomatic bacterial vaginosis in pregnancy with and without treatment. Am J Obstet Gynecol. 2004;190:363–370.
- LEVEL II-1 EVIDENCE: NONRANDOMIZED, CONTROLLED TRIAL
Resolution of BV was defined as a Nugent’s score of less than 7, and restoration of the normal vaginal microflora was defined as a score of less than 4. Overall, 72% and 55% of women in the metronidazole group had scores of less than 7 and less than 4, respectively, at follow-up. In the placebo group, these percentages were 21% and 11%, respectively.
Like most studies of BV, this one is flawed. The reason: Rather than conduct quantitative bacteriology, investigators used the Gram stain to interpret the microbiology of an ecosystem and then related it to a significant medical outcome: preterm birth. They attempted to define BV as an infectious disease and applied principles of infectious disease treatment to it. Most investigators define BV as an alteration in the endogenous microflora, specifically a flora dominated by obligate anaerobic bacteria. However, they treat it as an infection and administer an antibiotic to correct the alteration in the vaginal ecosystem.
Questions raised by this study include: How is asymptomatic BV defined? Is it truly asymptomatic, or have patients simply adapted to their condition? Do these patients have abnormal discharge in color, quantity, and odor?
In addition, the lack of definitive bacteriology in this study necessitates the following assumptions:
- All BV is similar; therefore, similar responses to antimicrobial therapy should be expected.
- A score below 7 but above 4 represents intermediate flora. This microflora is a precursor to BV or predisposes the patient to BV infection.
- A score below 4 represents Lactobacillus-dominant flora.
Lactobacillus. Moreover, it is necessary to determine the species of Lactobacillus present to confirm that it is the correct species to reestablish normal microflora.
Investigators did demonstrate a fact seen in most treatment studies: Metronidazole is not a particularly good agent for treating BV and restoring a patient’s vaginal ecology to Lactobacillus-dominant flora. However, they failed to demonstrate that treatment of asymptomatic BV reduces the risk of preterm delivery in a general obstetric population, or to establish a causal relationship between BV and preterm labor. This did not prevent them from asserting the idea that BV is a risk factor for preterm labor.
Investigators clouded their findings further by concluding that two 2-g doses of metronidazole administered 48 hours apart were effective in 72% of cases (defined as the elimination of BV) and 55% effective in restoring Gram stain scores to the normal range, noting that this effect lasted 2 to 10 weeks or longer. In reality, this is neither elimination of BV nor restoration of a normal range of microflora, but simply an interpretation of the change in Gram stain characteristics. The results do not explain what is happening microbiologically; nor do they clarify the host response to these changing conditions. Intensive quantitative bacteriology is needed, along with research into the microbial ecopathophysiology and host response to specific bacteria, in patients with and without healthy vaginal flora.
It is important to understand vaginal microflora because, when it is altered, it can impact negatively on the patient’s health. Therefore, studies that elucidate the vaginal ecology and the relationships between various bacteria further our understanding of the microbial pathophysiology leading to infection. This, in turn, leads to development of preventive measures, thus reducing the risk for adverse outcomes in both the obstetric and gynecologic patient—especially those undergoing operative procedures.
Is labor inherently protective against infection?
Molloy EJ, O’Neill AJ, Grantham JJ, et al. Labor induces a maternal inflammatory response syndrome. Am J Obstet Gynecol. 2004;190:448–455.
- LEVEL II-3 EVIDENCE: MULTIPLE OBSERVATIONS WITH OR WITHOUT INTERVENTION; UNCONTROLLED STUDIES
Although the number of participants was relatively small, this study was well considered and constructed, investigating several immunologic responses in 5 groups of patients:
- 15 nonpregnant healthy women and 17 healthy men,
- 15 healthy women in labor at term before delivery,
- 9 women with normal term pregnancies before elective cesarean with no labor,
- 9 women before emergency cesarean section after partial labor, and
- 9 women at term before emergency cesarean section without labor.
Interestingly, researchers also observed an increase of CD11b, an adhesion molecule and marker for neutrophil activation. Increased CD11b results in greater neutrophil activity.
Investigators concluded that the rise in neutrophils and diminished apoptosis in laboring patients may be an immunologic response to potential infection associated with labor, and that this phenomenon appears to be an inherent host reaction to prevent infection. It is known that bacteria from the genital tract of laboring women ascend into the uterus and amniotic fluid and colonize the decidua, amniotic membranes, and amniotic fluid. Women subsequently delivered by cesarean section are at a greater risk of infection than women delivered vaginally.
This is an extremely important finding and the first non-observational study to explain the rise in white blood cell counts during labor. It begins to explain the differences in white blood cell counts between laboring and nonlaboring patients and should spawn further investigations of a significant problem: postpartum endometritis.
Dr. Faro reports no financial relationships relevant to this article.
Does antibiotic prophylaxis with extended coverage limit postcesarean infection?
Objective
To determine whether extended-spectrum antibiotic prophylaxis that targets Ureaplasma urealyticum reduces postcesarean endometritis.
Results
Following cesarean, the frequency of endometritis, wound infections, and a combination of the 2 was significantly lower among treated women than women given placebo.
Methods
The 597 women enrolled in this randomized, double-blind trial all were given cefotetan prophylaxis after cord clamping at cesarean delivery. Subjects then were randomized to receive doxycycline plus azithromycin (n = 301) or placebo (n = 296). Both groups were monitored for endometritis, defined as a fever of 100.4° F or higher with 1 or more supporting clinical signs (maternal tachycardia, foul-smelling or purulent lochia, tender uterus, and maternal leukocytosis) or as a physician diagnosis of endometritis and no nonpelvic source of fever. Among study participants, 56% were black, with an age of 25.5±6.2 years, and 43% were nulliparous. Groups were similar for race, parity, maternal age, and most risk factors for postcesarean endometritis.
Outcome
Postcesarean endometritis occurred in 16.9% of treated women versus 24.7% of controls (P = .02), and wound infections affected 0.8% of treated women versus 3.6% of controls (P = .03).
Although the 2 groups were dissimilar for maternal leukocytosis (24.9% of treated women versus 12.5% of controls, P = .042) and classic uterine incision (7.6% versus 12.5%, P = .048), adjusting for these factors did not alter the risk ratio for postcesarean endometritis in the active versus placebotreated groups (relative risk 0.65, 95% confidence interval 0.43-0.98).
Length of stay was longer in the placebo group (104±56 versus 95±32 hours, P = .016) and among women with endometritis (146±52 versus 127±46 hours, P = .047).
Expert Commentary
This study tried to demonstrate that U. urealyticum is a significant pathogen and the etiologic agent for postpartum endometritis. However, the fact that U. urealyticum is found in the genital tract of approximately 70% to 90% of women does not support the thesis that it plays a major role in the microbial pathogenesis of postpartum endometritis.
Just because a microorganism is present in the lower genital tract does not mean that, in a state of infection, it is the etiologic agent. For example, many women harbor Enterococcus feacalis or Staphylococcus epidermidis in the genital tract; these often are isolated along with other bacteria from the site of infection. Yet the infection often is treated with antibiotics that offer no activity against these bacteria.
Lack of bacteriology limits relevance. Upon first analysis, this study appears to be sound, since it is both randomized and blinded. However, a major flaw weakens the conclusions significantly: lack of bacteriology.
The researchers neglected to obtain specimens for culture of bacteria from the uterus of each infected patient. Instead, they relied on statistical analysis, comparing the endpoint of infection versus no infection to extrapolate as to the cause. They failed to realize that the antibiotics used for prophylaxis—specifically doxycycline and azithromycin—also provide activity against Gram-positive and Gram-negative bacteria that make up the endogenous bacteriology of the vagina.
If endometrial specimens had been obtained from each infected patient, they would have provided a database on the frequency of involvement of the bacteria causing endometritis.
The authors do not state why they chose to use both doxycycline and azithromycin. In regard to the activity of these antibiotics against U. urealyticum there is probably not much difference as to efficacy.
Bottom Line
The use of combinations of antibiotics for surgical prophylaxis is not advisable because it can lead to the selection of resistant strains that will remain in the patient’s lower genital tract. Therefore, I would not use a cephalosporin plus doxycycline and/or azithromycin as a regimen for surgical prophylaxis. Before such a combination can be recommended, further study is necessary that includes microbiology to establish which bacteria are responsible for postpartum endometritis. The microbiological studies must be quantitative—not qualitative—before conclusions can be drawn and clinical recommendations made.
Objective
To determine whether extended-spectrum antibiotic prophylaxis that targets Ureaplasma urealyticum reduces postcesarean endometritis.
Results
Following cesarean, the frequency of endometritis, wound infections, and a combination of the 2 was significantly lower among treated women than women given placebo.
Methods
The 597 women enrolled in this randomized, double-blind trial all were given cefotetan prophylaxis after cord clamping at cesarean delivery. Subjects then were randomized to receive doxycycline plus azithromycin (n = 301) or placebo (n = 296). Both groups were monitored for endometritis, defined as a fever of 100.4° F or higher with 1 or more supporting clinical signs (maternal tachycardia, foul-smelling or purulent lochia, tender uterus, and maternal leukocytosis) or as a physician diagnosis of endometritis and no nonpelvic source of fever. Among study participants, 56% were black, with an age of 25.5±6.2 years, and 43% were nulliparous. Groups were similar for race, parity, maternal age, and most risk factors for postcesarean endometritis.
Outcome
Postcesarean endometritis occurred in 16.9% of treated women versus 24.7% of controls (P = .02), and wound infections affected 0.8% of treated women versus 3.6% of controls (P = .03).
Although the 2 groups were dissimilar for maternal leukocytosis (24.9% of treated women versus 12.5% of controls, P = .042) and classic uterine incision (7.6% versus 12.5%, P = .048), adjusting for these factors did not alter the risk ratio for postcesarean endometritis in the active versus placebotreated groups (relative risk 0.65, 95% confidence interval 0.43-0.98).
Length of stay was longer in the placebo group (104±56 versus 95±32 hours, P = .016) and among women with endometritis (146±52 versus 127±46 hours, P = .047).
Expert Commentary
This study tried to demonstrate that U. urealyticum is a significant pathogen and the etiologic agent for postpartum endometritis. However, the fact that U. urealyticum is found in the genital tract of approximately 70% to 90% of women does not support the thesis that it plays a major role in the microbial pathogenesis of postpartum endometritis.
Just because a microorganism is present in the lower genital tract does not mean that, in a state of infection, it is the etiologic agent. For example, many women harbor Enterococcus feacalis or Staphylococcus epidermidis in the genital tract; these often are isolated along with other bacteria from the site of infection. Yet the infection often is treated with antibiotics that offer no activity against these bacteria.
Lack of bacteriology limits relevance. Upon first analysis, this study appears to be sound, since it is both randomized and blinded. However, a major flaw weakens the conclusions significantly: lack of bacteriology.
The researchers neglected to obtain specimens for culture of bacteria from the uterus of each infected patient. Instead, they relied on statistical analysis, comparing the endpoint of infection versus no infection to extrapolate as to the cause. They failed to realize that the antibiotics used for prophylaxis—specifically doxycycline and azithromycin—also provide activity against Gram-positive and Gram-negative bacteria that make up the endogenous bacteriology of the vagina.
If endometrial specimens had been obtained from each infected patient, they would have provided a database on the frequency of involvement of the bacteria causing endometritis.
The authors do not state why they chose to use both doxycycline and azithromycin. In regard to the activity of these antibiotics against U. urealyticum there is probably not much difference as to efficacy.
Bottom Line
The use of combinations of antibiotics for surgical prophylaxis is not advisable because it can lead to the selection of resistant strains that will remain in the patient’s lower genital tract. Therefore, I would not use a cephalosporin plus doxycycline and/or azithromycin as a regimen for surgical prophylaxis. Before such a combination can be recommended, further study is necessary that includes microbiology to establish which bacteria are responsible for postpartum endometritis. The microbiological studies must be quantitative—not qualitative—before conclusions can be drawn and clinical recommendations made.
Objective
To determine whether extended-spectrum antibiotic prophylaxis that targets Ureaplasma urealyticum reduces postcesarean endometritis.
Results
Following cesarean, the frequency of endometritis, wound infections, and a combination of the 2 was significantly lower among treated women than women given placebo.
Methods
The 597 women enrolled in this randomized, double-blind trial all were given cefotetan prophylaxis after cord clamping at cesarean delivery. Subjects then were randomized to receive doxycycline plus azithromycin (n = 301) or placebo (n = 296). Both groups were monitored for endometritis, defined as a fever of 100.4° F or higher with 1 or more supporting clinical signs (maternal tachycardia, foul-smelling or purulent lochia, tender uterus, and maternal leukocytosis) or as a physician diagnosis of endometritis and no nonpelvic source of fever. Among study participants, 56% were black, with an age of 25.5±6.2 years, and 43% were nulliparous. Groups were similar for race, parity, maternal age, and most risk factors for postcesarean endometritis.
Outcome
Postcesarean endometritis occurred in 16.9% of treated women versus 24.7% of controls (P = .02), and wound infections affected 0.8% of treated women versus 3.6% of controls (P = .03).
Although the 2 groups were dissimilar for maternal leukocytosis (24.9% of treated women versus 12.5% of controls, P = .042) and classic uterine incision (7.6% versus 12.5%, P = .048), adjusting for these factors did not alter the risk ratio for postcesarean endometritis in the active versus placebotreated groups (relative risk 0.65, 95% confidence interval 0.43-0.98).
Length of stay was longer in the placebo group (104±56 versus 95±32 hours, P = .016) and among women with endometritis (146±52 versus 127±46 hours, P = .047).
Expert Commentary
This study tried to demonstrate that U. urealyticum is a significant pathogen and the etiologic agent for postpartum endometritis. However, the fact that U. urealyticum is found in the genital tract of approximately 70% to 90% of women does not support the thesis that it plays a major role in the microbial pathogenesis of postpartum endometritis.
Just because a microorganism is present in the lower genital tract does not mean that, in a state of infection, it is the etiologic agent. For example, many women harbor Enterococcus feacalis or Staphylococcus epidermidis in the genital tract; these often are isolated along with other bacteria from the site of infection. Yet the infection often is treated with antibiotics that offer no activity against these bacteria.
Lack of bacteriology limits relevance. Upon first analysis, this study appears to be sound, since it is both randomized and blinded. However, a major flaw weakens the conclusions significantly: lack of bacteriology.
The researchers neglected to obtain specimens for culture of bacteria from the uterus of each infected patient. Instead, they relied on statistical analysis, comparing the endpoint of infection versus no infection to extrapolate as to the cause. They failed to realize that the antibiotics used for prophylaxis—specifically doxycycline and azithromycin—also provide activity against Gram-positive and Gram-negative bacteria that make up the endogenous bacteriology of the vagina.
If endometrial specimens had been obtained from each infected patient, they would have provided a database on the frequency of involvement of the bacteria causing endometritis.
The authors do not state why they chose to use both doxycycline and azithromycin. In regard to the activity of these antibiotics against U. urealyticum there is probably not much difference as to efficacy.
Bottom Line
The use of combinations of antibiotics for surgical prophylaxis is not advisable because it can lead to the selection of resistant strains that will remain in the patient’s lower genital tract. Therefore, I would not use a cephalosporin plus doxycycline and/or azithromycin as a regimen for surgical prophylaxis. Before such a combination can be recommended, further study is necessary that includes microbiology to establish which bacteria are responsible for postpartum endometritis. The microbiological studies must be quantitative—not qualitative—before conclusions can be drawn and clinical recommendations made.
BV update: eliminating diagnostic confusion



- Physicians should not diagnose BV with a culture. A standard culture will not identify the number of anaerobic bacteria.
- In diagnosing BV, an Ob/Gyn must perform a microscopic exam, along with a whiff test and pH.
- Metronidazole and clindamycin are only 66% effective in treating BV.
- Topical clindamycin causes a temporary overgrowth of E. coli and Enterococcus in the vagina.
- Women whose vaginal microflora is colonized with hydrogen peroxide-producing Lactobacillus are less likely to acquire BV.
- All women should be screened for BV during an annual exam.
The number one reason women visit their gynecologists is for the treatment of vaginal infections. Yet a recent Gallup survey found that only 36% had ever heard of bacterial vaginosis (BV), the most common type of vaginal infection, affecting 1 in 4 American women. BV is a disease caused by an overgrowth of anaerobic bacteria and Gardnerella, all of which can be found in low numbers in the healthy vagina. In fact, women who have been diagnosed with BV have up to 1,000 times more anaerobic bacteria than normal women.
Studies have shown that many women confuse the symptoms of BV with a yeast infection and often self-medicate with over-the-counter preparations. Unlike Candida, however, BV has been associated with pelvic inflammatory disease (PID), as well as an increased risk of endometritis, cervicitis, and in pregnant women, premature delivery. Therefore, it is imperative that Ob/Gyns properly diagnose and treat BV while creating greater awareness of the signs and symptoms of this widespread disorder among their patients. Here, Sebastian Faro, MD, PhD, William Ledger, MD, and Sharon Hillier, PhD, respond to OBG Management editors’ questions on appropriate diagnosis, screening, and management modalities to combat this potentially dangerous yet treatable condition.
OBG Management: How does a woman contract BV? What are the predisposing factors?
Dr. Ledger: In many cases, it is related to sexual activity, though there are certainly women who are not sexually active who can get it. Basically, there’s a change in the bacterial flora of the vagina. Unfortunately, what triggers that change is unknown.
Dr. Faro: I think an alteration in pH levels stimulates a change in the vaginal microflora. We don’t know what causes that, but this alteration stimulates other bacteria such as Gardnerella to grow. Frequency of sexual intercourse does affect the pH and flora.
Dr. Hillier: In following a group of women without BV over time, we have found that women who use douching products and those with greater levels of sexual activity are more likely to acquire BV. However, there are many women who are monogamous and who do not douche who acquire BV. In our studies, it turned out that women who had H2O2-producing Lactobacillus vaginally were significantly less likely to acquire BV1 (Figure 1). There is no way presently for a woman or her physician to tell whether the Lactobacillus colonizing the vagina produces H2O2. Nevertheless, we think that many women who acquire BV simply lack the most protective kind of normal flora.
OBG Management: If there is a positive whiff test when examining the patient, is it necessary to do a wet mount or a pH test?
Dr. Hillier: A positive whiff test indicates that there are high levels of anaerobic bacteria producing trimethylamine in the vaginal flora. In our experience, nearly every woman who has a positive whiff test will also have an elevated pH. It is still advisable to do a wet mount on a woman with a positive whiff test in order to evaluate for mixed infections with other agents such as Trichomonas vaginalis.
Dr. Ledger: Unfortunately, many physicians are trying to cut corners on things that are very simple to do. An Ob/Gyn cannot diagnose any vaginitis unless he or she knows how to do a microscopic exam, along with a whiff test and pH (Figure 2). The whole process takes seconds. If they are not doing these tests, they ought to be sending patients to someone who is.
Dr. Faro: I think it is critical to perform a microscopic analysis, a whiff test, and a pH. If you only rely on the whiff test, you often will miss BV. Individuals can have an elevated pH of 5, 5.5, or 6, and not have BV. This could signify a dominant flora with E. coli or some other bacteria. Furthermore, the Trichomonas patient will have a positive whiff test, a pH that’s 5 or greater, and not have BV.
OBG Management: How important is it to submit a Gram stain to the lab? Should a physician wait for these results to begin treatment?
Dr. Faro: Often, we’ll get back a diagnosis of BV on a Gram stain. I’ll then go back and find that these patients had a normal pH and large bacillary forms, which is in contradistinction to what the cytopathologist is reading. What this means is that Gram stains can be misread.
Dr. Ledger: The Gram stain is done when physicians don’t have microscopes in their offices. But there is a two-fold problem: the results come back a few days after the patient is seen, and there is a danger of misdiagnosis. I get a diagnosis of BV from a Gram stain at least once a week on patients who had normal pHs and didn’t have a positive whiff test. I think it may be identifying patients who have changes in their flora, but who don’t clinically have BV. Unfortunately, there are very few physicians who have microscopes or pH paper in their offices. Often, women will be treated for a yeast infection. In that situation, a Gram stain would be more useful. The bottom line is that every Ob/Gyn should have a microscope and pH paper at his or her disposal.
Dr. Hillier: I agree. The diagnosis of BV is best made using a microscopic exam of vaginal fluid, evaluation of pH, and the whiff test. However, if a microscope is unavailable or microscopy is not interpretable, a Gram stain of vaginal fluid can be a useful test for BV. Because the test needs to be sent to a central laboratory, it is not as practical as the wet mount, pH, and whiff test, but it does have good correlation with a well-performed clinical examination. If the results are in question following the clinical evaluation, it may be prudent to delay treatment until Gram stain diagnosis is available, which should take no more than 1 working day.
OBG Management: Who should be screened and when?
Dr. Faro: I think anyone who has any type of abnormality in the lower genital tract, including complaints of discomfort, burning, itching, and odor should be screened. In addition, a patient who is going to have gynecologic surgery or vaginal surgery should be screened. Also, I screen all gravidas, but not to prevent preterm labor. A gravida who has an abnormal flora and has a cesarean is at a greater risk of developing postpartum endometritis than a gravida who has a normal flora.2
Dr. Ledger: We screen almost everyone. Screening definitely should be done if the patient is complaining of abnormal discharge or has abnormal vulvar or vaginal findings.
Dr. Hillier: Women with symptoms of vaginal discharge or odor should always be evaluated for the presence of BV and other causes of vaginitis. Screening of asymptomatic women should be undertaken for those who are planning termination of pregnancy. Randomized, placebo-controlled trials have demonstrated that treatment of asymptomatic women with BV can reduce the incidence of post-abortal PID.3 There is a consistent relationship between BV and post-hysterectomy infections, which has lead some authorities to recommend routine screening of women before planned hysterectomy.4
OBG Management: Do you recommend BV screening during an annual exam? A recent study noted that approximately 50% of women with BV are asymptomatic.
Dr. Faro: Yes. I normally perform a pH test then. If the pH is 4 and she has no symptoms, I stop right there. If the pH is more than 4, I will progress to a whiff test and a microscopic examination of the discharge just to be certain. The dilemma is when you have a lady who may be totally asymptomatic with no complaints, and you find this abnormality in her vaginal flora. Should you treat or not treat? I tend to err on the side of not treating because an altered flora does not necessarily mean BV. One of the things we’re seeing a lot of lately is group B vaginitis, if such a thing exists.
Since there is a consistent relationship between BV and post-hysterectomy infections, some authorities recommend routine pre-hysterectomy screening.
Dr. Ledger: I agree. I also see something called desquamative vaginitis. In 40% of these women, the predominant organism is a group B streptococcus. So I’m not sure whether it’s desquamative vaginitis or group B strep. One of the realities is that we see all the patients who are not getting better with their first round of treatment.
OBG Management: Gravidas at 23 to 26 weeks’ gestation with BV are 40% more likely to deliver a low-birth-weight baby. If you find that gravidas have BV early in their pregnancy, how often do you screen them thereafter?
Dr. Ledger: I screen these patients every time I do a vaginal exam. But the problem is I’m not going to diagnose any patients who have asymptomatic BV because I don’t do a vaginal exam at every prenatal visit. Hoyme recommends that patients examine themselves twice a week. If they have an alkaline pH, they are to see the doctor right away. If the doctor confirms BV, they are treated.5 However, I think more studies are needed to determine whether twice-weekly screening is appropriate in the United States. Guidelines should not be established until we have some good data.
Dr. Faro: I also screen my patients every time I do a vaginal exam. As for twice-weekly screening, there has not been any research that has statistically shown a cause and effect between BV and preterm delivery (PTD). To come up with screening guidelines for something we aren’t sure is really causing a problem is not in our best interest. Furthermore, we really don’t have good treatments for these women. Metronidazole and clindamycin are only 66% effective, and they are a short-term treatment.6
OBG Management: Can you describe how BV causes preterm delivery?
Dr. Hillier: Although we understand that BV leads to an increased incidence of chorioamnion infection, placental inflammation, and amniotic fluid infection, the mechanisms by which BV causes preterm delivery are not completely understood. Failure to understand the pathophysiology of infection-related PTD has complicated these issues. Most women with BV deliver at term without complication. However, a really important question is why some women with BV deliver preterm. When we are better able to target the subset of women at increased risk—and offer them preventive treatment—I believe we will begin to see successes with clinical trials.
To normalize pH levels, prescribe Aci-jel and/or boric acid vaginal capsules or suppositories.
OBG Management: The current treatment for BV in gravidas and nonpregnant women is metronidazole and clindamycin. Because clinical studies have shown that these medications are not 100% effective, should physicians consider other agents? If so, what would these be?
Dr. Ledger: Certainly. The Europeans have come up with a number of alternate treatments that have lactobacilli in them. These are used to encourage the flora to get back to normal. I know there are researchers in the United States working on this, too. And Secundo Guaschino of Italy recently presented a paper at the seventh annual meeting of the International Infectious Disease Society of Obstetrics and Gynecology in which estrogen therapy for menopausal women resulted in a more normal flora dominated by lactobacilli. Of note, pretreated women with an absence of lactobacilli did not have BV.
Dr. Faro: Yes, researchers are working in this area. It is important to note that if Lactobacillus is the key organism needed to normalize the vaginal flora, the only way you will be able to correct an altered flora is by creating an environment in the vagina that is conducive to the growth of Lactobacillus. But the problem is these patients have such an altered pH that even Lactobacillus cannot compete well with other bacteria. To normalize pH levels, I prescribe either 1 applicator of Aci-jel (Ortho Pharmaceutical Corp, Raritan, NJ) twice a day for 2 to 3 weeks, and/or 600 mg of boric acid vaginal capsules or suppositories twice a day for 14 days.
Dr. Ledger: I think you will find that these agents will not be effective in the long term. But these are things that need to be confirmed by testing.
Dr. Hillier: Current treatment guidelines for BV are based on a substantial body of literature generated over the past 20 years. Both metronidazole and clindamycin have excellent activity against anaerobic bacteria, which are thought to be the primary pathogens among women with BV. Clinical trials have taught us that agents such as sulfa cream or quinolones, which do not have anaerobic activity, yield lower cure rates overall than either metronidazole or clindamycin.7 It is important to note that topical clindamycin, because of its broad-spectrum activity against Lactobacillus and other organisms, causes a temporary overgrowth of E. coli and Enterococcus in the vagina.8 This overgrowth is thought to lead to an increased incidence of early PTD and, perhaps, neonatal infections in women given intravaginal clindamycin treatment during pregnancy. Therefore, it is important for clinicians to remember that intravaginal clindamycin cream is not a recommended treatment by the Centers for Disease Control and Prevention (CDC) for BV during pregnancy.9
OBG Management: Does it follow then that metronidazole and clindamycin do not help reestablish normal vaginal flora?
Dr. Hillier: In our experience, women who are treated with oral or intravaginal metronidazole have a much more rapid return of normal vaginal flora than women treated with clindamycin. Clindamycin has activity against Lactobacillus, so that in the week or two following therapy, women have very low levels of lactobacilli in the vagina.10
Dr. Ledger: I think these agents help cut down on the numbers of bacteria, which is certainly a better environment for reestablishing normal flora.
Dr. Faro: The problem with antibiotics is that they are broad-spectrum agents. They aren’t guns with a bullet directed at a certain bacterium or even a certain group of bacteria. They affect all bacteria. This is why we have such poor results.
Dr. Ledger: I think we need something more specific, but to get it we’re going to have to acquire more information on lactobacilli. On the other hand, postmenopausal patients with absent lactobacilli and no BV cast doubt in my mind that the lack of lactobacilli is the sole cause of BV.
Studies have shown that vaginal antifungal cream may markedly reduce the number of good lactobacilli in women who use them.
Dr. Faro: I’ve seen patients whose counts run around 10 to 4 or 10 to 5, yet they have healthy floras. I think the reason is that the Lactobacillus species they have are very potent producers of bacteriocin and hydrogen peroxide. In addition, we have found some ladies with strains or biotypes of Gardnerella who get recurrent BV and some who never have had the infection. So we end up dealing with a dual problem. We have a shift in the environment and we’re nurturing an organism that’s unaffected by the biodefense mechanisms that Lactobacillus produces. It’s very complex because we’re trying to change the environment of an ecological system to make it more conducive to the growth of Lactobacillus.
OBG Management: Since we know that lactobacilli excrete the natural disinfectant hydrogen peroxide to help maintain a healthy and normal balance of microorganisms in the vagina, is there an agent or a way to recolonize the vagina with it?
Dr. Hillier: In order for Lactobacillus to colonize the vagina it is necessary for the organism to attach to the vaginal epithelial cells. We are currently conducting trials to evaluate the value of recolonization therapy using a human-derived strain of a peroxide-producing Lactobacillus. In our study, women with BV were treated with metronidazole and randomized to receive capsules containing either 108Lactobacillus crispatus or placebo. The results are promising.
Dr. Ledger: There are other factors to consider since some women do not have a vaginal environment conducive to the health of lactobacilli. In fact, Guaschino showed that postmenopausal women not receiving HRT achieved a lactobacilli-dominated vaginal flora with exogenous estrogen therapy.
OBG Management: A recent survey noted that 30% of women thought it was acceptable to self-medicate symptoms of vaginal infections with home remedies. What are your thoughts?
Dr. Faro: Patients who self-diagnose and self-medicate often misdiagnose and medicate with the wrong agent.
Dr. Ledger: That’s right. In fact, Onderdonk, a premier clinical microbiologist at Harvard Medical School, looked at the impact of 1 vaginal antifungal cream and demonstrated that it markedly reduced the number of good lactobacilli in women who used it.11 It could be that some of these women who are self-medicating with over-the-counter antifungals may be altering their vaginal flora and doing more harm than good by creating an abnormal bacterial environment.
The male ejaculate may alter the vaginal microflora because it is usually very alkaline and has some immunologic-suppressing activities.
Dr. Faro: Absolutely. There are agents such as clotrimazole and tioconazole that have antibacterial activity that may alter their flora.12,13
OBG Management: How do you manage a patient with recurrent BV?
Dr. Hillier: There are no clear guidelines at present based on large, randomized, placebo-controlled trials showing that any specific regimen is effective for management of women with recurrent BV. Based on a small, randomized treatment trial presented by Sobel at the second international BV meeting, it was suggested that use of intravaginal metronidazole therapy for 10 days followed by twice-weekly intravaginal metronidazole for 3 months effectively suppressed the recurrence of BV in most women.14 Since this is a well-tolerated regimen that presents a practical approach, we currently employ this strategy. Larger randomized trials evaluating this strategy are ongoing.
Dr. Ledger: I have never been a big fan of giving antibiotics to the male partner in women with recurrent BV. One of the things that I do with recurrent BV patients is have the male use a condom. While there is no scientific evidence, I find that these women do not experience as many recurrences. The male ejaculate can alter the vaginal microflora because it is usually very alkaline. Also, the male ejaculate does have some immunological-suppressing activities. Sperm are foreign antigens that may inhibit the mechanisms that help control the growth of bacteria in the vagina. This may be what is affecting the overgrowth in some women
Dr. Faro: When we see a woman with recurrent BV, we base our treatment on the premise that this is an ecological situation and not an infection. We then try to change the pH using Aci-jel and boric acid suppositories. Currently, we’re looking at some buffering agents in clinical studies. In addition, we also ask the patient not to have sexual intercourse because, as Dr. Ledger suggested, the male ejaculate can have a tremendous impact on the vaginal ecosystem. If we’re fortunate to get the pH down below 4.5, we usually see a correction. In instances where we’re having difficulty getting the pH down, we will go to an antibiotic, such as oral metronidazole.
When examined microscopically, normal discharge contains only 1 dominant form of bacteria—Lactobacillus.
OBG Management: Once a patient has been treated, what is the best way to determine normal vaginal microflora? When is she in the clear, so to speak?
Dr. Faro: We go back and do a pH and microscopic analysis. If a physician relies solely on a whiff test, he or she is going to be in error because many ladies will have a pH that is 5 or greater and not have BV. This is because the flora has shifted and is now dominated by other bacteria. The pH is key for us because if it has not gone below 4.5, we know there’s still a problem.
Dr. Hillier: The most underutilized test in women’s health today is the vaginal pH. The easiest way to determine whether there has been reestablishment of Lactobacillus-pre-dominant flora is to measure vaginal pH. A vaginal pH of less than 4.7 indicates a predominance of vaginal lactobacilli.
Dr. Ledger: I’d like to stress here that, despite dozens of articles and hundreds of chapters in medical textbooks, physicians should not diagnose BV with a culture. They often will get a report showing the presence of Gardnerella. The problem is that Gardnerella can be present in the vagina of normal people and in women who have been successfully treated. A standard culture will not identify the number of anaerobic bacteria.
OBG Management: Women often experience a certain amount of discharge. What would you consider normal?
Dr. Faro: Normal discharge is white to slightly gray in color, odorless, and has a pH of 3.8 to 4.2. When you look at it microscopically, the squamous cells are well-estrogenized and white blood cells are rare. Also, you see only 1 dominant form of bacteria: large rods. When you culture this, it will be Lactobacillus. If you do the microbiology, you’ll find other bacteria, but their counts are 10 to 3 or lower per milliliter of fluid. Lastly, the amount of discharge a woman has is also related to her hormonal status.
OBG Management: A recent study conducted by the CDC found that many women still douche despite the fact that clinicians do not support the practice. In fact, douching has been linked to the development of BV. What should physicians recommend to their patients?
Dr. Ledger: I would not advise a patient to douche. However, I don’t believe that douching is a risk factor for BV. Rather, sexual intercourse and exposure to the male ejaculate are such culprits. Retrospective epidemiological studies have linked douching to BV. But these same analyses overstated the risk of infection with regard to intrauterine devices, as indicated in a recent study from Mexico City.15 While it is said that douching lowers the number of good lactobacilli in the vagina, over-the-counter antifungal agents have the same impact on vaginal lactobacilli. Further, the absence of lactobacilli in postmenopausal women is not uniformly associated with BV. The danger of douching is when women who have been exposed to bacterial agents delay medical care because of this primary intervention method.
Dr. Hillier: There is definitely a link between douching and acquiring BV. We think that douching can deplete the beneficial Lactobacillus from the vagina, especially those with unstable flora. We routinely counsel the women who come to our clinic to avoid douching.
Dr.Faro: Many of my patients have been douching for years—more than 10 to 20 years—and have experienced problems with vaginitis. This practice has been going on for several generations. Patients who have never douched are discouraged from beginning such a practice because it presents no benefits and there is the possibility of an adverse reaction. However, it would be difficult to get women who have not had an adverse effect to douching to discontinue a practice that has been an integral part of their hygienic practices.
OBG Management: Many women mistake BV for a yeast infection and seek over-the-counter medication. How can physicians manage and educate this population?
Dr. Hillier: Most women who mistake BV for a yeast infection have never heard of BV. In fact, most women have been “educated” by reading articles in women’s magazines and watching television ads. Although it is important for physicians to review the symptoms of BV and other common infections with their patients, they also should advise them that symptoms are not necessarily predictive of specific diagnoses. Among women seeking care at our hospital, we find that only 1 in 4 who think they have yeast infections actually do have yeast vaginitis. When we followed women who had absolutely no evidence of yeast by culture, assessing them at 4-month intervals over a year, 25% of them reported using vaginal yeast medication. The overuse of topical medications and the inaccuracy of self-diagnosis is a huge problem in women’s health today. Personally, I would like to see much less diagnosis over the telephone and better testing for vaginal infections so that women are given the correct diagnosis.
Dr. Faro: Unfortunately, even we clinicians can look at a wet mount and miss a field that has yeast in it. We’ll look at 10 fields on each patient. Yet, when we culture that patient, it comes back positive. That raises an interesting question. Is it the yeast that’s causing their symptoms or not?
The overuse of topical medications and the inaccuracy of self-diagnosis is a huge problem.
Dr. Ledger: Most studies suggest that only 30% to 40% of women who think they have yeast, actually do. If there were a good over-the-counter test that was sensitive and specific, that would be terrific. But I don’t see that on the horizon quite yet.
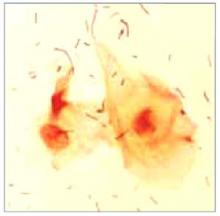
FIGURE 1 Bacterial vaginosis
Normal vaginal microflora as seen under a microscope. The flat segments depict the helpful bacteria, lactobacilli
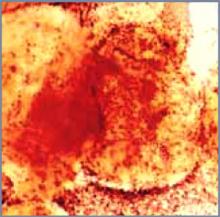
FIGURE 2 Bacterial vaginosis
An overgrowth of harmful bacteria called clue cells detected under the microscope confirms a diagnosis of BV.
Vaginal infections: detecting the difference
| BV | Yeast | Trichomoniasis | |
|---|---|---|---|
| Odor | Foul, fishy | None | Foul or fishy |
| Discharge | Thin, milky-white or gray | Thick, curdy, white | Yellow-green-gray, frothy or sticky |
| Discomfort | Itching, burning | Itching, burning | Painful urination, itch |
| Cause | Bacteria | Yeast | Parasite |
| Health risks | PID, cervicitis, cervical abnormality, endometritis, obstetric complications | None | Obstetric problems |
Dr. Faro reports no financial relationship with any companies whose products are mentioned in this article. Dr. Ledger reports receiving research grants from 3M. Dr. Hilllier reports that she has received research grants on vaginitis treatments from 3M and Pfizer, and is a consultant for Johnson & Johnson.
1. Hawes SE, Hillier SL, Benedetti J, et al. Hydrogen peroxide-producing lactobacilli and acquisition of vaginal infections. JID. 1996;174:1058-1063.
2. Watts DH, Krohn MA, Hillier SL, et al. Bacterial vaginosis as a risk factor for post-cesarean endometritis. Obstet Gynecol. 1990;75:52-58.
3. Larsson PG, Bergman B, Forsum U, et al. Mobiluncus and clue cells as predictors of PID after first-trimester abortion. Acta Obstet Gynecol Scand. 1989;68:217-220.
4. Larsson PG, Platz-Christensen J, Thejls H, et al. Incidence of pelvic inflammatory disease after first-trimester legal abortion in women with bacterial vaginosis after treatment with metronidazole: a double-blind, randomized study. Am J Obstet Gynecol. 1992;166:100-103.
5. Hoyme U, et al. Results and potential consequences of the Thuringa prematurity preventional campaign 2000. Geburtsch Frauenheilk. 2002;62:257-263.
6. Paavonen J, Mangioni C, Martin MA, et al. Vaginal clindamycin and oral metronidazole for bacterial vaginosis: a randomized trial. Obstet Gynecol. 2000;96:256-260.
7. Sobel JD, Chaim W, Thomason J, Livengood C, et al. Comparative study of intravaginal metronidazole and triple-sulfa therapy for bacterial vaginosis. Infect Dis Obstet Gynecol. 1996;4:66-70.
8. Hill GB, Livengood CH. Bacterial vaginosis-associated microflora and effects of topical intravaginal clindamycin. Am J Obstet Gynecol. 1994;171:1198-1204.
9. Centers for Disease Control and Prevention. 1998 guidelines for treatment of sexually transmitted diseases. MMWR. 1998;47(No. RR-1).:
10. Hillier SL, Krohn MA, Watts DH, et al. Microbiologic efficacy of intravaginal clindamycin cream for the treatment of bacterial vaginosis. Obstet Gynecol. 1990;76:407.-
11. Ross RA, et al. Effect of Candida albicans infection and clotrimazole treatment on vaginal microflora in vitro. Obstet Gynecol. 1995;86:925-930.
12. Clissold SP, Heel RC. Tioconazole: a review of its antimicrobial and ther-apeutic use in superficial mycoses. Drugs. 1986;31:29-51.
13. Jones RN, Cali MJ, Hoban D, et al. In vitro antimicrobial activity of tioconazole and its concentration in vaginal fluids following topical (vagistat-1 6.5%) application. Diag Microbiol Infect Dis. 1993;17:45-51.
14. Sobel JD, Leaman D. Suppressive maintenance therapy of recurrent bac-terial vaginosis utilizing 0.75% metronidazole vaginal gel. Int J Gynecol Obstet. 1999;67:S41, abstract #010115
15. Hubacher D, et al. Use of copper intrauterine devices and the risk of tubal infertility among nulligravid women. N Engl J Med. 2001;345:561-567.



- Physicians should not diagnose BV with a culture. A standard culture will not identify the number of anaerobic bacteria.
- In diagnosing BV, an Ob/Gyn must perform a microscopic exam, along with a whiff test and pH.
- Metronidazole and clindamycin are only 66% effective in treating BV.
- Topical clindamycin causes a temporary overgrowth of E. coli and Enterococcus in the vagina.
- Women whose vaginal microflora is colonized with hydrogen peroxide-producing Lactobacillus are less likely to acquire BV.
- All women should be screened for BV during an annual exam.
The number one reason women visit their gynecologists is for the treatment of vaginal infections. Yet a recent Gallup survey found that only 36% had ever heard of bacterial vaginosis (BV), the most common type of vaginal infection, affecting 1 in 4 American women. BV is a disease caused by an overgrowth of anaerobic bacteria and Gardnerella, all of which can be found in low numbers in the healthy vagina. In fact, women who have been diagnosed with BV have up to 1,000 times more anaerobic bacteria than normal women.
Studies have shown that many women confuse the symptoms of BV with a yeast infection and often self-medicate with over-the-counter preparations. Unlike Candida, however, BV has been associated with pelvic inflammatory disease (PID), as well as an increased risk of endometritis, cervicitis, and in pregnant women, premature delivery. Therefore, it is imperative that Ob/Gyns properly diagnose and treat BV while creating greater awareness of the signs and symptoms of this widespread disorder among their patients. Here, Sebastian Faro, MD, PhD, William Ledger, MD, and Sharon Hillier, PhD, respond to OBG Management editors’ questions on appropriate diagnosis, screening, and management modalities to combat this potentially dangerous yet treatable condition.
OBG Management: How does a woman contract BV? What are the predisposing factors?
Dr. Ledger: In many cases, it is related to sexual activity, though there are certainly women who are not sexually active who can get it. Basically, there’s a change in the bacterial flora of the vagina. Unfortunately, what triggers that change is unknown.
Dr. Faro: I think an alteration in pH levels stimulates a change in the vaginal microflora. We don’t know what causes that, but this alteration stimulates other bacteria such as Gardnerella to grow. Frequency of sexual intercourse does affect the pH and flora.
Dr. Hillier: In following a group of women without BV over time, we have found that women who use douching products and those with greater levels of sexual activity are more likely to acquire BV. However, there are many women who are monogamous and who do not douche who acquire BV. In our studies, it turned out that women who had H2O2-producing Lactobacillus vaginally were significantly less likely to acquire BV1 (Figure 1). There is no way presently for a woman or her physician to tell whether the Lactobacillus colonizing the vagina produces H2O2. Nevertheless, we think that many women who acquire BV simply lack the most protective kind of normal flora.
OBG Management: If there is a positive whiff test when examining the patient, is it necessary to do a wet mount or a pH test?
Dr. Hillier: A positive whiff test indicates that there are high levels of anaerobic bacteria producing trimethylamine in the vaginal flora. In our experience, nearly every woman who has a positive whiff test will also have an elevated pH. It is still advisable to do a wet mount on a woman with a positive whiff test in order to evaluate for mixed infections with other agents such as Trichomonas vaginalis.
Dr. Ledger: Unfortunately, many physicians are trying to cut corners on things that are very simple to do. An Ob/Gyn cannot diagnose any vaginitis unless he or she knows how to do a microscopic exam, along with a whiff test and pH (Figure 2). The whole process takes seconds. If they are not doing these tests, they ought to be sending patients to someone who is.
Dr. Faro: I think it is critical to perform a microscopic analysis, a whiff test, and a pH. If you only rely on the whiff test, you often will miss BV. Individuals can have an elevated pH of 5, 5.5, or 6, and not have BV. This could signify a dominant flora with E. coli or some other bacteria. Furthermore, the Trichomonas patient will have a positive whiff test, a pH that’s 5 or greater, and not have BV.
OBG Management: How important is it to submit a Gram stain to the lab? Should a physician wait for these results to begin treatment?
Dr. Faro: Often, we’ll get back a diagnosis of BV on a Gram stain. I’ll then go back and find that these patients had a normal pH and large bacillary forms, which is in contradistinction to what the cytopathologist is reading. What this means is that Gram stains can be misread.
Dr. Ledger: The Gram stain is done when physicians don’t have microscopes in their offices. But there is a two-fold problem: the results come back a few days after the patient is seen, and there is a danger of misdiagnosis. I get a diagnosis of BV from a Gram stain at least once a week on patients who had normal pHs and didn’t have a positive whiff test. I think it may be identifying patients who have changes in their flora, but who don’t clinically have BV. Unfortunately, there are very few physicians who have microscopes or pH paper in their offices. Often, women will be treated for a yeast infection. In that situation, a Gram stain would be more useful. The bottom line is that every Ob/Gyn should have a microscope and pH paper at his or her disposal.
Dr. Hillier: I agree. The diagnosis of BV is best made using a microscopic exam of vaginal fluid, evaluation of pH, and the whiff test. However, if a microscope is unavailable or microscopy is not interpretable, a Gram stain of vaginal fluid can be a useful test for BV. Because the test needs to be sent to a central laboratory, it is not as practical as the wet mount, pH, and whiff test, but it does have good correlation with a well-performed clinical examination. If the results are in question following the clinical evaluation, it may be prudent to delay treatment until Gram stain diagnosis is available, which should take no more than 1 working day.
OBG Management: Who should be screened and when?
Dr. Faro: I think anyone who has any type of abnormality in the lower genital tract, including complaints of discomfort, burning, itching, and odor should be screened. In addition, a patient who is going to have gynecologic surgery or vaginal surgery should be screened. Also, I screen all gravidas, but not to prevent preterm labor. A gravida who has an abnormal flora and has a cesarean is at a greater risk of developing postpartum endometritis than a gravida who has a normal flora.2
Dr. Ledger: We screen almost everyone. Screening definitely should be done if the patient is complaining of abnormal discharge or has abnormal vulvar or vaginal findings.
Dr. Hillier: Women with symptoms of vaginal discharge or odor should always be evaluated for the presence of BV and other causes of vaginitis. Screening of asymptomatic women should be undertaken for those who are planning termination of pregnancy. Randomized, placebo-controlled trials have demonstrated that treatment of asymptomatic women with BV can reduce the incidence of post-abortal PID.3 There is a consistent relationship between BV and post-hysterectomy infections, which has lead some authorities to recommend routine screening of women before planned hysterectomy.4
OBG Management: Do you recommend BV screening during an annual exam? A recent study noted that approximately 50% of women with BV are asymptomatic.
Dr. Faro: Yes. I normally perform a pH test then. If the pH is 4 and she has no symptoms, I stop right there. If the pH is more than 4, I will progress to a whiff test and a microscopic examination of the discharge just to be certain. The dilemma is when you have a lady who may be totally asymptomatic with no complaints, and you find this abnormality in her vaginal flora. Should you treat or not treat? I tend to err on the side of not treating because an altered flora does not necessarily mean BV. One of the things we’re seeing a lot of lately is group B vaginitis, if such a thing exists.
Since there is a consistent relationship between BV and post-hysterectomy infections, some authorities recommend routine pre-hysterectomy screening.
Dr. Ledger: I agree. I also see something called desquamative vaginitis. In 40% of these women, the predominant organism is a group B streptococcus. So I’m not sure whether it’s desquamative vaginitis or group B strep. One of the realities is that we see all the patients who are not getting better with their first round of treatment.
OBG Management: Gravidas at 23 to 26 weeks’ gestation with BV are 40% more likely to deliver a low-birth-weight baby. If you find that gravidas have BV early in their pregnancy, how often do you screen them thereafter?
Dr. Ledger: I screen these patients every time I do a vaginal exam. But the problem is I’m not going to diagnose any patients who have asymptomatic BV because I don’t do a vaginal exam at every prenatal visit. Hoyme recommends that patients examine themselves twice a week. If they have an alkaline pH, they are to see the doctor right away. If the doctor confirms BV, they are treated.5 However, I think more studies are needed to determine whether twice-weekly screening is appropriate in the United States. Guidelines should not be established until we have some good data.
Dr. Faro: I also screen my patients every time I do a vaginal exam. As for twice-weekly screening, there has not been any research that has statistically shown a cause and effect between BV and preterm delivery (PTD). To come up with screening guidelines for something we aren’t sure is really causing a problem is not in our best interest. Furthermore, we really don’t have good treatments for these women. Metronidazole and clindamycin are only 66% effective, and they are a short-term treatment.6
OBG Management: Can you describe how BV causes preterm delivery?
Dr. Hillier: Although we understand that BV leads to an increased incidence of chorioamnion infection, placental inflammation, and amniotic fluid infection, the mechanisms by which BV causes preterm delivery are not completely understood. Failure to understand the pathophysiology of infection-related PTD has complicated these issues. Most women with BV deliver at term without complication. However, a really important question is why some women with BV deliver preterm. When we are better able to target the subset of women at increased risk—and offer them preventive treatment—I believe we will begin to see successes with clinical trials.
To normalize pH levels, prescribe Aci-jel and/or boric acid vaginal capsules or suppositories.
OBG Management: The current treatment for BV in gravidas and nonpregnant women is metronidazole and clindamycin. Because clinical studies have shown that these medications are not 100% effective, should physicians consider other agents? If so, what would these be?
Dr. Ledger: Certainly. The Europeans have come up with a number of alternate treatments that have lactobacilli in them. These are used to encourage the flora to get back to normal. I know there are researchers in the United States working on this, too. And Secundo Guaschino of Italy recently presented a paper at the seventh annual meeting of the International Infectious Disease Society of Obstetrics and Gynecology in which estrogen therapy for menopausal women resulted in a more normal flora dominated by lactobacilli. Of note, pretreated women with an absence of lactobacilli did not have BV.
Dr. Faro: Yes, researchers are working in this area. It is important to note that if Lactobacillus is the key organism needed to normalize the vaginal flora, the only way you will be able to correct an altered flora is by creating an environment in the vagina that is conducive to the growth of Lactobacillus. But the problem is these patients have such an altered pH that even Lactobacillus cannot compete well with other bacteria. To normalize pH levels, I prescribe either 1 applicator of Aci-jel (Ortho Pharmaceutical Corp, Raritan, NJ) twice a day for 2 to 3 weeks, and/or 600 mg of boric acid vaginal capsules or suppositories twice a day for 14 days.
Dr. Ledger: I think you will find that these agents will not be effective in the long term. But these are things that need to be confirmed by testing.
Dr. Hillier: Current treatment guidelines for BV are based on a substantial body of literature generated over the past 20 years. Both metronidazole and clindamycin have excellent activity against anaerobic bacteria, which are thought to be the primary pathogens among women with BV. Clinical trials have taught us that agents such as sulfa cream or quinolones, which do not have anaerobic activity, yield lower cure rates overall than either metronidazole or clindamycin.7 It is important to note that topical clindamycin, because of its broad-spectrum activity against Lactobacillus and other organisms, causes a temporary overgrowth of E. coli and Enterococcus in the vagina.8 This overgrowth is thought to lead to an increased incidence of early PTD and, perhaps, neonatal infections in women given intravaginal clindamycin treatment during pregnancy. Therefore, it is important for clinicians to remember that intravaginal clindamycin cream is not a recommended treatment by the Centers for Disease Control and Prevention (CDC) for BV during pregnancy.9
OBG Management: Does it follow then that metronidazole and clindamycin do not help reestablish normal vaginal flora?
Dr. Hillier: In our experience, women who are treated with oral or intravaginal metronidazole have a much more rapid return of normal vaginal flora than women treated with clindamycin. Clindamycin has activity against Lactobacillus, so that in the week or two following therapy, women have very low levels of lactobacilli in the vagina.10
Dr. Ledger: I think these agents help cut down on the numbers of bacteria, which is certainly a better environment for reestablishing normal flora.
Dr. Faro: The problem with antibiotics is that they are broad-spectrum agents. They aren’t guns with a bullet directed at a certain bacterium or even a certain group of bacteria. They affect all bacteria. This is why we have such poor results.
Dr. Ledger: I think we need something more specific, but to get it we’re going to have to acquire more information on lactobacilli. On the other hand, postmenopausal patients with absent lactobacilli and no BV cast doubt in my mind that the lack of lactobacilli is the sole cause of BV.
Studies have shown that vaginal antifungal cream may markedly reduce the number of good lactobacilli in women who use them.
Dr. Faro: I’ve seen patients whose counts run around 10 to 4 or 10 to 5, yet they have healthy floras. I think the reason is that the Lactobacillus species they have are very potent producers of bacteriocin and hydrogen peroxide. In addition, we have found some ladies with strains or biotypes of Gardnerella who get recurrent BV and some who never have had the infection. So we end up dealing with a dual problem. We have a shift in the environment and we’re nurturing an organism that’s unaffected by the biodefense mechanisms that Lactobacillus produces. It’s very complex because we’re trying to change the environment of an ecological system to make it more conducive to the growth of Lactobacillus.
OBG Management: Since we know that lactobacilli excrete the natural disinfectant hydrogen peroxide to help maintain a healthy and normal balance of microorganisms in the vagina, is there an agent or a way to recolonize the vagina with it?
Dr. Hillier: In order for Lactobacillus to colonize the vagina it is necessary for the organism to attach to the vaginal epithelial cells. We are currently conducting trials to evaluate the value of recolonization therapy using a human-derived strain of a peroxide-producing Lactobacillus. In our study, women with BV were treated with metronidazole and randomized to receive capsules containing either 108Lactobacillus crispatus or placebo. The results are promising.
Dr. Ledger: There are other factors to consider since some women do not have a vaginal environment conducive to the health of lactobacilli. In fact, Guaschino showed that postmenopausal women not receiving HRT achieved a lactobacilli-dominated vaginal flora with exogenous estrogen therapy.
OBG Management: A recent survey noted that 30% of women thought it was acceptable to self-medicate symptoms of vaginal infections with home remedies. What are your thoughts?
Dr. Faro: Patients who self-diagnose and self-medicate often misdiagnose and medicate with the wrong agent.
Dr. Ledger: That’s right. In fact, Onderdonk, a premier clinical microbiologist at Harvard Medical School, looked at the impact of 1 vaginal antifungal cream and demonstrated that it markedly reduced the number of good lactobacilli in women who used it.11 It could be that some of these women who are self-medicating with over-the-counter antifungals may be altering their vaginal flora and doing more harm than good by creating an abnormal bacterial environment.
The male ejaculate may alter the vaginal microflora because it is usually very alkaline and has some immunologic-suppressing activities.
Dr. Faro: Absolutely. There are agents such as clotrimazole and tioconazole that have antibacterial activity that may alter their flora.12,13
OBG Management: How do you manage a patient with recurrent BV?
Dr. Hillier: There are no clear guidelines at present based on large, randomized, placebo-controlled trials showing that any specific regimen is effective for management of women with recurrent BV. Based on a small, randomized treatment trial presented by Sobel at the second international BV meeting, it was suggested that use of intravaginal metronidazole therapy for 10 days followed by twice-weekly intravaginal metronidazole for 3 months effectively suppressed the recurrence of BV in most women.14 Since this is a well-tolerated regimen that presents a practical approach, we currently employ this strategy. Larger randomized trials evaluating this strategy are ongoing.
Dr. Ledger: I have never been a big fan of giving antibiotics to the male partner in women with recurrent BV. One of the things that I do with recurrent BV patients is have the male use a condom. While there is no scientific evidence, I find that these women do not experience as many recurrences. The male ejaculate can alter the vaginal microflora because it is usually very alkaline. Also, the male ejaculate does have some immunological-suppressing activities. Sperm are foreign antigens that may inhibit the mechanisms that help control the growth of bacteria in the vagina. This may be what is affecting the overgrowth in some women
Dr. Faro: When we see a woman with recurrent BV, we base our treatment on the premise that this is an ecological situation and not an infection. We then try to change the pH using Aci-jel and boric acid suppositories. Currently, we’re looking at some buffering agents in clinical studies. In addition, we also ask the patient not to have sexual intercourse because, as Dr. Ledger suggested, the male ejaculate can have a tremendous impact on the vaginal ecosystem. If we’re fortunate to get the pH down below 4.5, we usually see a correction. In instances where we’re having difficulty getting the pH down, we will go to an antibiotic, such as oral metronidazole.
When examined microscopically, normal discharge contains only 1 dominant form of bacteria—Lactobacillus.
OBG Management: Once a patient has been treated, what is the best way to determine normal vaginal microflora? When is she in the clear, so to speak?
Dr. Faro: We go back and do a pH and microscopic analysis. If a physician relies solely on a whiff test, he or she is going to be in error because many ladies will have a pH that is 5 or greater and not have BV. This is because the flora has shifted and is now dominated by other bacteria. The pH is key for us because if it has not gone below 4.5, we know there’s still a problem.
Dr. Hillier: The most underutilized test in women’s health today is the vaginal pH. The easiest way to determine whether there has been reestablishment of Lactobacillus-pre-dominant flora is to measure vaginal pH. A vaginal pH of less than 4.7 indicates a predominance of vaginal lactobacilli.
Dr. Ledger: I’d like to stress here that, despite dozens of articles and hundreds of chapters in medical textbooks, physicians should not diagnose BV with a culture. They often will get a report showing the presence of Gardnerella. The problem is that Gardnerella can be present in the vagina of normal people and in women who have been successfully treated. A standard culture will not identify the number of anaerobic bacteria.
OBG Management: Women often experience a certain amount of discharge. What would you consider normal?
Dr. Faro: Normal discharge is white to slightly gray in color, odorless, and has a pH of 3.8 to 4.2. When you look at it microscopically, the squamous cells are well-estrogenized and white blood cells are rare. Also, you see only 1 dominant form of bacteria: large rods. When you culture this, it will be Lactobacillus. If you do the microbiology, you’ll find other bacteria, but their counts are 10 to 3 or lower per milliliter of fluid. Lastly, the amount of discharge a woman has is also related to her hormonal status.
OBG Management: A recent study conducted by the CDC found that many women still douche despite the fact that clinicians do not support the practice. In fact, douching has been linked to the development of BV. What should physicians recommend to their patients?
Dr. Ledger: I would not advise a patient to douche. However, I don’t believe that douching is a risk factor for BV. Rather, sexual intercourse and exposure to the male ejaculate are such culprits. Retrospective epidemiological studies have linked douching to BV. But these same analyses overstated the risk of infection with regard to intrauterine devices, as indicated in a recent study from Mexico City.15 While it is said that douching lowers the number of good lactobacilli in the vagina, over-the-counter antifungal agents have the same impact on vaginal lactobacilli. Further, the absence of lactobacilli in postmenopausal women is not uniformly associated with BV. The danger of douching is when women who have been exposed to bacterial agents delay medical care because of this primary intervention method.
Dr. Hillier: There is definitely a link between douching and acquiring BV. We think that douching can deplete the beneficial Lactobacillus from the vagina, especially those with unstable flora. We routinely counsel the women who come to our clinic to avoid douching.
Dr.Faro: Many of my patients have been douching for years—more than 10 to 20 years—and have experienced problems with vaginitis. This practice has been going on for several generations. Patients who have never douched are discouraged from beginning such a practice because it presents no benefits and there is the possibility of an adverse reaction. However, it would be difficult to get women who have not had an adverse effect to douching to discontinue a practice that has been an integral part of their hygienic practices.
OBG Management: Many women mistake BV for a yeast infection and seek over-the-counter medication. How can physicians manage and educate this population?
Dr. Hillier: Most women who mistake BV for a yeast infection have never heard of BV. In fact, most women have been “educated” by reading articles in women’s magazines and watching television ads. Although it is important for physicians to review the symptoms of BV and other common infections with their patients, they also should advise them that symptoms are not necessarily predictive of specific diagnoses. Among women seeking care at our hospital, we find that only 1 in 4 who think they have yeast infections actually do have yeast vaginitis. When we followed women who had absolutely no evidence of yeast by culture, assessing them at 4-month intervals over a year, 25% of them reported using vaginal yeast medication. The overuse of topical medications and the inaccuracy of self-diagnosis is a huge problem in women’s health today. Personally, I would like to see much less diagnosis over the telephone and better testing for vaginal infections so that women are given the correct diagnosis.
Dr. Faro: Unfortunately, even we clinicians can look at a wet mount and miss a field that has yeast in it. We’ll look at 10 fields on each patient. Yet, when we culture that patient, it comes back positive. That raises an interesting question. Is it the yeast that’s causing their symptoms or not?
The overuse of topical medications and the inaccuracy of self-diagnosis is a huge problem.
Dr. Ledger: Most studies suggest that only 30% to 40% of women who think they have yeast, actually do. If there were a good over-the-counter test that was sensitive and specific, that would be terrific. But I don’t see that on the horizon quite yet.
FIGURE 1 Bacterial vaginosis
Normal vaginal microflora as seen under a microscope. The flat segments depict the helpful bacteria, lactobacilli
FIGURE 2 Bacterial vaginosis
An overgrowth of harmful bacteria called clue cells detected under the microscope confirms a diagnosis of BV.
Vaginal infections: detecting the difference
| BV | Yeast | Trichomoniasis | |
|---|---|---|---|
| Odor | Foul, fishy | None | Foul or fishy |
| Discharge | Thin, milky-white or gray | Thick, curdy, white | Yellow-green-gray, frothy or sticky |
| Discomfort | Itching, burning | Itching, burning | Painful urination, itch |
| Cause | Bacteria | Yeast | Parasite |
| Health risks | PID, cervicitis, cervical abnormality, endometritis, obstetric complications | None | Obstetric problems |
Dr. Faro reports no financial relationship with any companies whose products are mentioned in this article. Dr. Ledger reports receiving research grants from 3M. Dr. Hilllier reports that she has received research grants on vaginitis treatments from 3M and Pfizer, and is a consultant for Johnson & Johnson.



- Physicians should not diagnose BV with a culture. A standard culture will not identify the number of anaerobic bacteria.
- In diagnosing BV, an Ob/Gyn must perform a microscopic exam, along with a whiff test and pH.
- Metronidazole and clindamycin are only 66% effective in treating BV.
- Topical clindamycin causes a temporary overgrowth of E. coli and Enterococcus in the vagina.
- Women whose vaginal microflora is colonized with hydrogen peroxide-producing Lactobacillus are less likely to acquire BV.
- All women should be screened for BV during an annual exam.
The number one reason women visit their gynecologists is for the treatment of vaginal infections. Yet a recent Gallup survey found that only 36% had ever heard of bacterial vaginosis (BV), the most common type of vaginal infection, affecting 1 in 4 American women. BV is a disease caused by an overgrowth of anaerobic bacteria and Gardnerella, all of which can be found in low numbers in the healthy vagina. In fact, women who have been diagnosed with BV have up to 1,000 times more anaerobic bacteria than normal women.
Studies have shown that many women confuse the symptoms of BV with a yeast infection and often self-medicate with over-the-counter preparations. Unlike Candida, however, BV has been associated with pelvic inflammatory disease (PID), as well as an increased risk of endometritis, cervicitis, and in pregnant women, premature delivery. Therefore, it is imperative that Ob/Gyns properly diagnose and treat BV while creating greater awareness of the signs and symptoms of this widespread disorder among their patients. Here, Sebastian Faro, MD, PhD, William Ledger, MD, and Sharon Hillier, PhD, respond to OBG Management editors’ questions on appropriate diagnosis, screening, and management modalities to combat this potentially dangerous yet treatable condition.
OBG Management: How does a woman contract BV? What are the predisposing factors?
Dr. Ledger: In many cases, it is related to sexual activity, though there are certainly women who are not sexually active who can get it. Basically, there’s a change in the bacterial flora of the vagina. Unfortunately, what triggers that change is unknown.
Dr. Faro: I think an alteration in pH levels stimulates a change in the vaginal microflora. We don’t know what causes that, but this alteration stimulates other bacteria such as Gardnerella to grow. Frequency of sexual intercourse does affect the pH and flora.
Dr. Hillier: In following a group of women without BV over time, we have found that women who use douching products and those with greater levels of sexual activity are more likely to acquire BV. However, there are many women who are monogamous and who do not douche who acquire BV. In our studies, it turned out that women who had H2O2-producing Lactobacillus vaginally were significantly less likely to acquire BV1 (Figure 1). There is no way presently for a woman or her physician to tell whether the Lactobacillus colonizing the vagina produces H2O2. Nevertheless, we think that many women who acquire BV simply lack the most protective kind of normal flora.
OBG Management: If there is a positive whiff test when examining the patient, is it necessary to do a wet mount or a pH test?
Dr. Hillier: A positive whiff test indicates that there are high levels of anaerobic bacteria producing trimethylamine in the vaginal flora. In our experience, nearly every woman who has a positive whiff test will also have an elevated pH. It is still advisable to do a wet mount on a woman with a positive whiff test in order to evaluate for mixed infections with other agents such as Trichomonas vaginalis.
Dr. Ledger: Unfortunately, many physicians are trying to cut corners on things that are very simple to do. An Ob/Gyn cannot diagnose any vaginitis unless he or she knows how to do a microscopic exam, along with a whiff test and pH (Figure 2). The whole process takes seconds. If they are not doing these tests, they ought to be sending patients to someone who is.
Dr. Faro: I think it is critical to perform a microscopic analysis, a whiff test, and a pH. If you only rely on the whiff test, you often will miss BV. Individuals can have an elevated pH of 5, 5.5, or 6, and not have BV. This could signify a dominant flora with E. coli or some other bacteria. Furthermore, the Trichomonas patient will have a positive whiff test, a pH that’s 5 or greater, and not have BV.
OBG Management: How important is it to submit a Gram stain to the lab? Should a physician wait for these results to begin treatment?
Dr. Faro: Often, we’ll get back a diagnosis of BV on a Gram stain. I’ll then go back and find that these patients had a normal pH and large bacillary forms, which is in contradistinction to what the cytopathologist is reading. What this means is that Gram stains can be misread.
Dr. Ledger: The Gram stain is done when physicians don’t have microscopes in their offices. But there is a two-fold problem: the results come back a few days after the patient is seen, and there is a danger of misdiagnosis. I get a diagnosis of BV from a Gram stain at least once a week on patients who had normal pHs and didn’t have a positive whiff test. I think it may be identifying patients who have changes in their flora, but who don’t clinically have BV. Unfortunately, there are very few physicians who have microscopes or pH paper in their offices. Often, women will be treated for a yeast infection. In that situation, a Gram stain would be more useful. The bottom line is that every Ob/Gyn should have a microscope and pH paper at his or her disposal.
Dr. Hillier: I agree. The diagnosis of BV is best made using a microscopic exam of vaginal fluid, evaluation of pH, and the whiff test. However, if a microscope is unavailable or microscopy is not interpretable, a Gram stain of vaginal fluid can be a useful test for BV. Because the test needs to be sent to a central laboratory, it is not as practical as the wet mount, pH, and whiff test, but it does have good correlation with a well-performed clinical examination. If the results are in question following the clinical evaluation, it may be prudent to delay treatment until Gram stain diagnosis is available, which should take no more than 1 working day.
OBG Management: Who should be screened and when?
Dr. Faro: I think anyone who has any type of abnormality in the lower genital tract, including complaints of discomfort, burning, itching, and odor should be screened. In addition, a patient who is going to have gynecologic surgery or vaginal surgery should be screened. Also, I screen all gravidas, but not to prevent preterm labor. A gravida who has an abnormal flora and has a cesarean is at a greater risk of developing postpartum endometritis than a gravida who has a normal flora.2
Dr. Ledger: We screen almost everyone. Screening definitely should be done if the patient is complaining of abnormal discharge or has abnormal vulvar or vaginal findings.
Dr. Hillier: Women with symptoms of vaginal discharge or odor should always be evaluated for the presence of BV and other causes of vaginitis. Screening of asymptomatic women should be undertaken for those who are planning termination of pregnancy. Randomized, placebo-controlled trials have demonstrated that treatment of asymptomatic women with BV can reduce the incidence of post-abortal PID.3 There is a consistent relationship between BV and post-hysterectomy infections, which has lead some authorities to recommend routine screening of women before planned hysterectomy.4
OBG Management: Do you recommend BV screening during an annual exam? A recent study noted that approximately 50% of women with BV are asymptomatic.
Dr. Faro: Yes. I normally perform a pH test then. If the pH is 4 and she has no symptoms, I stop right there. If the pH is more than 4, I will progress to a whiff test and a microscopic examination of the discharge just to be certain. The dilemma is when you have a lady who may be totally asymptomatic with no complaints, and you find this abnormality in her vaginal flora. Should you treat or not treat? I tend to err on the side of not treating because an altered flora does not necessarily mean BV. One of the things we’re seeing a lot of lately is group B vaginitis, if such a thing exists.
Since there is a consistent relationship between BV and post-hysterectomy infections, some authorities recommend routine pre-hysterectomy screening.
Dr. Ledger: I agree. I also see something called desquamative vaginitis. In 40% of these women, the predominant organism is a group B streptococcus. So I’m not sure whether it’s desquamative vaginitis or group B strep. One of the realities is that we see all the patients who are not getting better with their first round of treatment.
OBG Management: Gravidas at 23 to 26 weeks’ gestation with BV are 40% more likely to deliver a low-birth-weight baby. If you find that gravidas have BV early in their pregnancy, how often do you screen them thereafter?
Dr. Ledger: I screen these patients every time I do a vaginal exam. But the problem is I’m not going to diagnose any patients who have asymptomatic BV because I don’t do a vaginal exam at every prenatal visit. Hoyme recommends that patients examine themselves twice a week. If they have an alkaline pH, they are to see the doctor right away. If the doctor confirms BV, they are treated.5 However, I think more studies are needed to determine whether twice-weekly screening is appropriate in the United States. Guidelines should not be established until we have some good data.
Dr. Faro: I also screen my patients every time I do a vaginal exam. As for twice-weekly screening, there has not been any research that has statistically shown a cause and effect between BV and preterm delivery (PTD). To come up with screening guidelines for something we aren’t sure is really causing a problem is not in our best interest. Furthermore, we really don’t have good treatments for these women. Metronidazole and clindamycin are only 66% effective, and they are a short-term treatment.6
OBG Management: Can you describe how BV causes preterm delivery?
Dr. Hillier: Although we understand that BV leads to an increased incidence of chorioamnion infection, placental inflammation, and amniotic fluid infection, the mechanisms by which BV causes preterm delivery are not completely understood. Failure to understand the pathophysiology of infection-related PTD has complicated these issues. Most women with BV deliver at term without complication. However, a really important question is why some women with BV deliver preterm. When we are better able to target the subset of women at increased risk—and offer them preventive treatment—I believe we will begin to see successes with clinical trials.
To normalize pH levels, prescribe Aci-jel and/or boric acid vaginal capsules or suppositories.
OBG Management: The current treatment for BV in gravidas and nonpregnant women is metronidazole and clindamycin. Because clinical studies have shown that these medications are not 100% effective, should physicians consider other agents? If so, what would these be?
Dr. Ledger: Certainly. The Europeans have come up with a number of alternate treatments that have lactobacilli in them. These are used to encourage the flora to get back to normal. I know there are researchers in the United States working on this, too. And Secundo Guaschino of Italy recently presented a paper at the seventh annual meeting of the International Infectious Disease Society of Obstetrics and Gynecology in which estrogen therapy for menopausal women resulted in a more normal flora dominated by lactobacilli. Of note, pretreated women with an absence of lactobacilli did not have BV.
Dr. Faro: Yes, researchers are working in this area. It is important to note that if Lactobacillus is the key organism needed to normalize the vaginal flora, the only way you will be able to correct an altered flora is by creating an environment in the vagina that is conducive to the growth of Lactobacillus. But the problem is these patients have such an altered pH that even Lactobacillus cannot compete well with other bacteria. To normalize pH levels, I prescribe either 1 applicator of Aci-jel (Ortho Pharmaceutical Corp, Raritan, NJ) twice a day for 2 to 3 weeks, and/or 600 mg of boric acid vaginal capsules or suppositories twice a day for 14 days.
Dr. Ledger: I think you will find that these agents will not be effective in the long term. But these are things that need to be confirmed by testing.
Dr. Hillier: Current treatment guidelines for BV are based on a substantial body of literature generated over the past 20 years. Both metronidazole and clindamycin have excellent activity against anaerobic bacteria, which are thought to be the primary pathogens among women with BV. Clinical trials have taught us that agents such as sulfa cream or quinolones, which do not have anaerobic activity, yield lower cure rates overall than either metronidazole or clindamycin.7 It is important to note that topical clindamycin, because of its broad-spectrum activity against Lactobacillus and other organisms, causes a temporary overgrowth of E. coli and Enterococcus in the vagina.8 This overgrowth is thought to lead to an increased incidence of early PTD and, perhaps, neonatal infections in women given intravaginal clindamycin treatment during pregnancy. Therefore, it is important for clinicians to remember that intravaginal clindamycin cream is not a recommended treatment by the Centers for Disease Control and Prevention (CDC) for BV during pregnancy.9
OBG Management: Does it follow then that metronidazole and clindamycin do not help reestablish normal vaginal flora?
Dr. Hillier: In our experience, women who are treated with oral or intravaginal metronidazole have a much more rapid return of normal vaginal flora than women treated with clindamycin. Clindamycin has activity against Lactobacillus, so that in the week or two following therapy, women have very low levels of lactobacilli in the vagina.10
Dr. Ledger: I think these agents help cut down on the numbers of bacteria, which is certainly a better environment for reestablishing normal flora.
Dr. Faro: The problem with antibiotics is that they are broad-spectrum agents. They aren’t guns with a bullet directed at a certain bacterium or even a certain group of bacteria. They affect all bacteria. This is why we have such poor results.
Dr. Ledger: I think we need something more specific, but to get it we’re going to have to acquire more information on lactobacilli. On the other hand, postmenopausal patients with absent lactobacilli and no BV cast doubt in my mind that the lack of lactobacilli is the sole cause of BV.
Studies have shown that vaginal antifungal cream may markedly reduce the number of good lactobacilli in women who use them.
Dr. Faro: I’ve seen patients whose counts run around 10 to 4 or 10 to 5, yet they have healthy floras. I think the reason is that the Lactobacillus species they have are very potent producers of bacteriocin and hydrogen peroxide. In addition, we have found some ladies with strains or biotypes of Gardnerella who get recurrent BV and some who never have had the infection. So we end up dealing with a dual problem. We have a shift in the environment and we’re nurturing an organism that’s unaffected by the biodefense mechanisms that Lactobacillus produces. It’s very complex because we’re trying to change the environment of an ecological system to make it more conducive to the growth of Lactobacillus.
OBG Management: Since we know that lactobacilli excrete the natural disinfectant hydrogen peroxide to help maintain a healthy and normal balance of microorganisms in the vagina, is there an agent or a way to recolonize the vagina with it?
Dr. Hillier: In order for Lactobacillus to colonize the vagina it is necessary for the organism to attach to the vaginal epithelial cells. We are currently conducting trials to evaluate the value of recolonization therapy using a human-derived strain of a peroxide-producing Lactobacillus. In our study, women with BV were treated with metronidazole and randomized to receive capsules containing either 108Lactobacillus crispatus or placebo. The results are promising.
Dr. Ledger: There are other factors to consider since some women do not have a vaginal environment conducive to the health of lactobacilli. In fact, Guaschino showed that postmenopausal women not receiving HRT achieved a lactobacilli-dominated vaginal flora with exogenous estrogen therapy.
OBG Management: A recent survey noted that 30% of women thought it was acceptable to self-medicate symptoms of vaginal infections with home remedies. What are your thoughts?
Dr. Faro: Patients who self-diagnose and self-medicate often misdiagnose and medicate with the wrong agent.
Dr. Ledger: That’s right. In fact, Onderdonk, a premier clinical microbiologist at Harvard Medical School, looked at the impact of 1 vaginal antifungal cream and demonstrated that it markedly reduced the number of good lactobacilli in women who used it.11 It could be that some of these women who are self-medicating with over-the-counter antifungals may be altering their vaginal flora and doing more harm than good by creating an abnormal bacterial environment.
The male ejaculate may alter the vaginal microflora because it is usually very alkaline and has some immunologic-suppressing activities.
Dr. Faro: Absolutely. There are agents such as clotrimazole and tioconazole that have antibacterial activity that may alter their flora.12,13
OBG Management: How do you manage a patient with recurrent BV?
Dr. Hillier: There are no clear guidelines at present based on large, randomized, placebo-controlled trials showing that any specific regimen is effective for management of women with recurrent BV. Based on a small, randomized treatment trial presented by Sobel at the second international BV meeting, it was suggested that use of intravaginal metronidazole therapy for 10 days followed by twice-weekly intravaginal metronidazole for 3 months effectively suppressed the recurrence of BV in most women.14 Since this is a well-tolerated regimen that presents a practical approach, we currently employ this strategy. Larger randomized trials evaluating this strategy are ongoing.
Dr. Ledger: I have never been a big fan of giving antibiotics to the male partner in women with recurrent BV. One of the things that I do with recurrent BV patients is have the male use a condom. While there is no scientific evidence, I find that these women do not experience as many recurrences. The male ejaculate can alter the vaginal microflora because it is usually very alkaline. Also, the male ejaculate does have some immunological-suppressing activities. Sperm are foreign antigens that may inhibit the mechanisms that help control the growth of bacteria in the vagina. This may be what is affecting the overgrowth in some women
Dr. Faro: When we see a woman with recurrent BV, we base our treatment on the premise that this is an ecological situation and not an infection. We then try to change the pH using Aci-jel and boric acid suppositories. Currently, we’re looking at some buffering agents in clinical studies. In addition, we also ask the patient not to have sexual intercourse because, as Dr. Ledger suggested, the male ejaculate can have a tremendous impact on the vaginal ecosystem. If we’re fortunate to get the pH down below 4.5, we usually see a correction. In instances where we’re having difficulty getting the pH down, we will go to an antibiotic, such as oral metronidazole.
When examined microscopically, normal discharge contains only 1 dominant form of bacteria—Lactobacillus.
OBG Management: Once a patient has been treated, what is the best way to determine normal vaginal microflora? When is she in the clear, so to speak?
Dr. Faro: We go back and do a pH and microscopic analysis. If a physician relies solely on a whiff test, he or she is going to be in error because many ladies will have a pH that is 5 or greater and not have BV. This is because the flora has shifted and is now dominated by other bacteria. The pH is key for us because if it has not gone below 4.5, we know there’s still a problem.
Dr. Hillier: The most underutilized test in women’s health today is the vaginal pH. The easiest way to determine whether there has been reestablishment of Lactobacillus-pre-dominant flora is to measure vaginal pH. A vaginal pH of less than 4.7 indicates a predominance of vaginal lactobacilli.
Dr. Ledger: I’d like to stress here that, despite dozens of articles and hundreds of chapters in medical textbooks, physicians should not diagnose BV with a culture. They often will get a report showing the presence of Gardnerella. The problem is that Gardnerella can be present in the vagina of normal people and in women who have been successfully treated. A standard culture will not identify the number of anaerobic bacteria.
OBG Management: Women often experience a certain amount of discharge. What would you consider normal?
Dr. Faro: Normal discharge is white to slightly gray in color, odorless, and has a pH of 3.8 to 4.2. When you look at it microscopically, the squamous cells are well-estrogenized and white blood cells are rare. Also, you see only 1 dominant form of bacteria: large rods. When you culture this, it will be Lactobacillus. If you do the microbiology, you’ll find other bacteria, but their counts are 10 to 3 or lower per milliliter of fluid. Lastly, the amount of discharge a woman has is also related to her hormonal status.
OBG Management: A recent study conducted by the CDC found that many women still douche despite the fact that clinicians do not support the practice. In fact, douching has been linked to the development of BV. What should physicians recommend to their patients?
Dr. Ledger: I would not advise a patient to douche. However, I don’t believe that douching is a risk factor for BV. Rather, sexual intercourse and exposure to the male ejaculate are such culprits. Retrospective epidemiological studies have linked douching to BV. But these same analyses overstated the risk of infection with regard to intrauterine devices, as indicated in a recent study from Mexico City.15 While it is said that douching lowers the number of good lactobacilli in the vagina, over-the-counter antifungal agents have the same impact on vaginal lactobacilli. Further, the absence of lactobacilli in postmenopausal women is not uniformly associated with BV. The danger of douching is when women who have been exposed to bacterial agents delay medical care because of this primary intervention method.
Dr. Hillier: There is definitely a link between douching and acquiring BV. We think that douching can deplete the beneficial Lactobacillus from the vagina, especially those with unstable flora. We routinely counsel the women who come to our clinic to avoid douching.
Dr.Faro: Many of my patients have been douching for years—more than 10 to 20 years—and have experienced problems with vaginitis. This practice has been going on for several generations. Patients who have never douched are discouraged from beginning such a practice because it presents no benefits and there is the possibility of an adverse reaction. However, it would be difficult to get women who have not had an adverse effect to douching to discontinue a practice that has been an integral part of their hygienic practices.
OBG Management: Many women mistake BV for a yeast infection and seek over-the-counter medication. How can physicians manage and educate this population?
Dr. Hillier: Most women who mistake BV for a yeast infection have never heard of BV. In fact, most women have been “educated” by reading articles in women’s magazines and watching television ads. Although it is important for physicians to review the symptoms of BV and other common infections with their patients, they also should advise them that symptoms are not necessarily predictive of specific diagnoses. Among women seeking care at our hospital, we find that only 1 in 4 who think they have yeast infections actually do have yeast vaginitis. When we followed women who had absolutely no evidence of yeast by culture, assessing them at 4-month intervals over a year, 25% of them reported using vaginal yeast medication. The overuse of topical medications and the inaccuracy of self-diagnosis is a huge problem in women’s health today. Personally, I would like to see much less diagnosis over the telephone and better testing for vaginal infections so that women are given the correct diagnosis.
Dr. Faro: Unfortunately, even we clinicians can look at a wet mount and miss a field that has yeast in it. We’ll look at 10 fields on each patient. Yet, when we culture that patient, it comes back positive. That raises an interesting question. Is it the yeast that’s causing their symptoms or not?
The overuse of topical medications and the inaccuracy of self-diagnosis is a huge problem.
Dr. Ledger: Most studies suggest that only 30% to 40% of women who think they have yeast, actually do. If there were a good over-the-counter test that was sensitive and specific, that would be terrific. But I don’t see that on the horizon quite yet.
FIGURE 1 Bacterial vaginosis
Normal vaginal microflora as seen under a microscope. The flat segments depict the helpful bacteria, lactobacilli
FIGURE 2 Bacterial vaginosis
An overgrowth of harmful bacteria called clue cells detected under the microscope confirms a diagnosis of BV.
Vaginal infections: detecting the difference
| BV | Yeast | Trichomoniasis | |
|---|---|---|---|
| Odor | Foul, fishy | None | Foul or fishy |
| Discharge | Thin, milky-white or gray | Thick, curdy, white | Yellow-green-gray, frothy or sticky |
| Discomfort | Itching, burning | Itching, burning | Painful urination, itch |
| Cause | Bacteria | Yeast | Parasite |
| Health risks | PID, cervicitis, cervical abnormality, endometritis, obstetric complications | None | Obstetric problems |
Dr. Faro reports no financial relationship with any companies whose products are mentioned in this article. Dr. Ledger reports receiving research grants from 3M. Dr. Hilllier reports that she has received research grants on vaginitis treatments from 3M and Pfizer, and is a consultant for Johnson & Johnson.
1. Hawes SE, Hillier SL, Benedetti J, et al. Hydrogen peroxide-producing lactobacilli and acquisition of vaginal infections. JID. 1996;174:1058-1063.
2. Watts DH, Krohn MA, Hillier SL, et al. Bacterial vaginosis as a risk factor for post-cesarean endometritis. Obstet Gynecol. 1990;75:52-58.
3. Larsson PG, Bergman B, Forsum U, et al. Mobiluncus and clue cells as predictors of PID after first-trimester abortion. Acta Obstet Gynecol Scand. 1989;68:217-220.
4. Larsson PG, Platz-Christensen J, Thejls H, et al. Incidence of pelvic inflammatory disease after first-trimester legal abortion in women with bacterial vaginosis after treatment with metronidazole: a double-blind, randomized study. Am J Obstet Gynecol. 1992;166:100-103.
5. Hoyme U, et al. Results and potential consequences of the Thuringa prematurity preventional campaign 2000. Geburtsch Frauenheilk. 2002;62:257-263.
6. Paavonen J, Mangioni C, Martin MA, et al. Vaginal clindamycin and oral metronidazole for bacterial vaginosis: a randomized trial. Obstet Gynecol. 2000;96:256-260.
7. Sobel JD, Chaim W, Thomason J, Livengood C, et al. Comparative study of intravaginal metronidazole and triple-sulfa therapy for bacterial vaginosis. Infect Dis Obstet Gynecol. 1996;4:66-70.
8. Hill GB, Livengood CH. Bacterial vaginosis-associated microflora and effects of topical intravaginal clindamycin. Am J Obstet Gynecol. 1994;171:1198-1204.
9. Centers for Disease Control and Prevention. 1998 guidelines for treatment of sexually transmitted diseases. MMWR. 1998;47(No. RR-1).:
10. Hillier SL, Krohn MA, Watts DH, et al. Microbiologic efficacy of intravaginal clindamycin cream for the treatment of bacterial vaginosis. Obstet Gynecol. 1990;76:407.-
11. Ross RA, et al. Effect of Candida albicans infection and clotrimazole treatment on vaginal microflora in vitro. Obstet Gynecol. 1995;86:925-930.
12. Clissold SP, Heel RC. Tioconazole: a review of its antimicrobial and ther-apeutic use in superficial mycoses. Drugs. 1986;31:29-51.
13. Jones RN, Cali MJ, Hoban D, et al. In vitro antimicrobial activity of tioconazole and its concentration in vaginal fluids following topical (vagistat-1 6.5%) application. Diag Microbiol Infect Dis. 1993;17:45-51.
14. Sobel JD, Leaman D. Suppressive maintenance therapy of recurrent bac-terial vaginosis utilizing 0.75% metronidazole vaginal gel. Int J Gynecol Obstet. 1999;67:S41, abstract #010115
15. Hubacher D, et al. Use of copper intrauterine devices and the risk of tubal infertility among nulligravid women. N Engl J Med. 2001;345:561-567.
1. Hawes SE, Hillier SL, Benedetti J, et al. Hydrogen peroxide-producing lactobacilli and acquisition of vaginal infections. JID. 1996;174:1058-1063.
2. Watts DH, Krohn MA, Hillier SL, et al. Bacterial vaginosis as a risk factor for post-cesarean endometritis. Obstet Gynecol. 1990;75:52-58.
3. Larsson PG, Bergman B, Forsum U, et al. Mobiluncus and clue cells as predictors of PID after first-trimester abortion. Acta Obstet Gynecol Scand. 1989;68:217-220.
4. Larsson PG, Platz-Christensen J, Thejls H, et al. Incidence of pelvic inflammatory disease after first-trimester legal abortion in women with bacterial vaginosis after treatment with metronidazole: a double-blind, randomized study. Am J Obstet Gynecol. 1992;166:100-103.
5. Hoyme U, et al. Results and potential consequences of the Thuringa prematurity preventional campaign 2000. Geburtsch Frauenheilk. 2002;62:257-263.
6. Paavonen J, Mangioni C, Martin MA, et al. Vaginal clindamycin and oral metronidazole for bacterial vaginosis: a randomized trial. Obstet Gynecol. 2000;96:256-260.
7. Sobel JD, Chaim W, Thomason J, Livengood C, et al. Comparative study of intravaginal metronidazole and triple-sulfa therapy for bacterial vaginosis. Infect Dis Obstet Gynecol. 1996;4:66-70.
8. Hill GB, Livengood CH. Bacterial vaginosis-associated microflora and effects of topical intravaginal clindamycin. Am J Obstet Gynecol. 1994;171:1198-1204.
9. Centers for Disease Control and Prevention. 1998 guidelines for treatment of sexually transmitted diseases. MMWR. 1998;47(No. RR-1).:
10. Hillier SL, Krohn MA, Watts DH, et al. Microbiologic efficacy of intravaginal clindamycin cream for the treatment of bacterial vaginosis. Obstet Gynecol. 1990;76:407.-
11. Ross RA, et al. Effect of Candida albicans infection and clotrimazole treatment on vaginal microflora in vitro. Obstet Gynecol. 1995;86:925-930.
12. Clissold SP, Heel RC. Tioconazole: a review of its antimicrobial and ther-apeutic use in superficial mycoses. Drugs. 1986;31:29-51.
13. Jones RN, Cali MJ, Hoban D, et al. In vitro antimicrobial activity of tioconazole and its concentration in vaginal fluids following topical (vagistat-1 6.5%) application. Diag Microbiol Infect Dis. 1993;17:45-51.
14. Sobel JD, Leaman D. Suppressive maintenance therapy of recurrent bac-terial vaginosis utilizing 0.75% metronidazole vaginal gel. Int J Gynecol Obstet. 1999;67:S41, abstract #010115
15. Hubacher D, et al. Use of copper intrauterine devices and the risk of tubal infertility among nulligravid women. N Engl J Med. 2001;345:561-567.
Optimal treatment for BV
THE QUESTION:
Is intravaginal clindamycin more effective than oral metronidazole for the treatment of bacterial vaginosis (BV)?
Past Studies
Metronidazole is the standard treatment for BV. However, other trials have shown that regimens of intravaginal clindamycin were as effective as oral metronidazole for treating BV.
This Study
Women with BV received either 100 mg of intravaginal clindamycin for 3 consecutive days plus placebo capsules orally for 7 days or 500 mg of metronidazole twice daily orally for 7 days along with intravaginal placebo ovules for 3 days. Subjects were excluded if they were pregnant or breastfeeding, had received systemic or vaginal antimicrobial therapy 2 weeks prior to the study, or if they were taking antibiotics. Also, women who had gonorrhea, candidiasis, chlamydia, or genital herpes could not participate in the trial.
Of the 399 women enrolled, 233 were evaluated for treatment efficacy. Of those, 77 of 113 patients were cured of BV with clindamycin and 80 of 120 women were cured with metronidazole. Side effects of nausea and unpleasant taste were reported more frequently in the metronidazole treatment group. Clinical outcome was determined by vaginal fluid amine odor and clue cells.
While there was no significant difference in the effectiveness of both regimens, the researchers observed that clindamycin had fewer systemic effects because of its shorter dosage regimen (3 days as opposed to 7 days of metronidazole). Therefore, clindamycin was better tolerated among participants.
Find this Study
August 2000 issue of Obstetrics and Gynecology; abstract online at www.acog.com.
Who May be Affected by These Findings?
Women who have BV.
Expert Commentary
BV is present in 10% to 30% of pregnant women and 12% to 61% of women with sexually transmitted diseases. While BV is perceived as a mild medical problem, often without symptoms or signs of vaginal inflammation, it could lead to postoperative infection after hysterectomy, postpartum endometritis, and preterm labor if left untreated. Therefore, fast and effective treatment is imperative.
Unfortunately, the researchers’ findings that the clindamycin was as effective as and better tolerated than the metronidazole are marred by several methodological errors. First, the resolution of the amine odor and clue cells is a poor outcome measure. While the patients may no longer have a malodorous vaginal discharge, this does not mean that a healthy, Lactobacillus-dominant, vaginal microflora has been established. In fact, if the pH level has not been restored to less than 4.5, there is a possibility that the vaginal microflora will be plagued by a gram-positive bacterium, including Streptococcus agalactia or Enterococcus faecalis, or a gram-negative bacterium such as Escherichia coli. Neither agent was particularly satisfactory in restoring a Lactobacillus-dominant microflora. Furthermore, the cure rates were not impressive, as they did not reach 70%.
Moreover, comparing the systemic absorption of clindamycin administered vaginally to metronidazole taken orally is like comparing apples to oranges. Legitimate results will not come from measuring the adverse effects of 2 different antimicrobial agents administered by different routes. In fact, it is well known that many antibiotics taken orally cause the patient to experience nausea, often resulting in discontinuation of the medication.
The Bottom Line
BV continues to be a poorly understood condition. Knowledge of microbial interactions will make it easier to restore an altered vaginal microflora to a healthy one. In the meantime, administer 500 mg of metronidazole orally 3 times a day for 7 days.
At present, women treated for BV should be checked for the following: whether the pH level has returned to a normal range of 3.8 to 4.2 and if Lactobacillus has regained dominance. Failure to achieve these 2 goals means that the treatment was not successful.
THE QUESTION:
Is intravaginal clindamycin more effective than oral metronidazole for the treatment of bacterial vaginosis (BV)?
Past Studies
Metronidazole is the standard treatment for BV. However, other trials have shown that regimens of intravaginal clindamycin were as effective as oral metronidazole for treating BV.
This Study
Women with BV received either 100 mg of intravaginal clindamycin for 3 consecutive days plus placebo capsules orally for 7 days or 500 mg of metronidazole twice daily orally for 7 days along with intravaginal placebo ovules for 3 days. Subjects were excluded if they were pregnant or breastfeeding, had received systemic or vaginal antimicrobial therapy 2 weeks prior to the study, or if they were taking antibiotics. Also, women who had gonorrhea, candidiasis, chlamydia, or genital herpes could not participate in the trial.
Of the 399 women enrolled, 233 were evaluated for treatment efficacy. Of those, 77 of 113 patients were cured of BV with clindamycin and 80 of 120 women were cured with metronidazole. Side effects of nausea and unpleasant taste were reported more frequently in the metronidazole treatment group. Clinical outcome was determined by vaginal fluid amine odor and clue cells.
While there was no significant difference in the effectiveness of both regimens, the researchers observed that clindamycin had fewer systemic effects because of its shorter dosage regimen (3 days as opposed to 7 days of metronidazole). Therefore, clindamycin was better tolerated among participants.
Find this Study
August 2000 issue of Obstetrics and Gynecology; abstract online at www.acog.com.
Who May be Affected by These Findings?
Women who have BV.
Expert Commentary
BV is present in 10% to 30% of pregnant women and 12% to 61% of women with sexually transmitted diseases. While BV is perceived as a mild medical problem, often without symptoms or signs of vaginal inflammation, it could lead to postoperative infection after hysterectomy, postpartum endometritis, and preterm labor if left untreated. Therefore, fast and effective treatment is imperative.
Unfortunately, the researchers’ findings that the clindamycin was as effective as and better tolerated than the metronidazole are marred by several methodological errors. First, the resolution of the amine odor and clue cells is a poor outcome measure. While the patients may no longer have a malodorous vaginal discharge, this does not mean that a healthy, Lactobacillus-dominant, vaginal microflora has been established. In fact, if the pH level has not been restored to less than 4.5, there is a possibility that the vaginal microflora will be plagued by a gram-positive bacterium, including Streptococcus agalactia or Enterococcus faecalis, or a gram-negative bacterium such as Escherichia coli. Neither agent was particularly satisfactory in restoring a Lactobacillus-dominant microflora. Furthermore, the cure rates were not impressive, as they did not reach 70%.
Moreover, comparing the systemic absorption of clindamycin administered vaginally to metronidazole taken orally is like comparing apples to oranges. Legitimate results will not come from measuring the adverse effects of 2 different antimicrobial agents administered by different routes. In fact, it is well known that many antibiotics taken orally cause the patient to experience nausea, often resulting in discontinuation of the medication.
The Bottom Line
BV continues to be a poorly understood condition. Knowledge of microbial interactions will make it easier to restore an altered vaginal microflora to a healthy one. In the meantime, administer 500 mg of metronidazole orally 3 times a day for 7 days.
At present, women treated for BV should be checked for the following: whether the pH level has returned to a normal range of 3.8 to 4.2 and if Lactobacillus has regained dominance. Failure to achieve these 2 goals means that the treatment was not successful.
THE QUESTION:
Is intravaginal clindamycin more effective than oral metronidazole for the treatment of bacterial vaginosis (BV)?
Past Studies
Metronidazole is the standard treatment for BV. However, other trials have shown that regimens of intravaginal clindamycin were as effective as oral metronidazole for treating BV.
This Study
Women with BV received either 100 mg of intravaginal clindamycin for 3 consecutive days plus placebo capsules orally for 7 days or 500 mg of metronidazole twice daily orally for 7 days along with intravaginal placebo ovules for 3 days. Subjects were excluded if they were pregnant or breastfeeding, had received systemic or vaginal antimicrobial therapy 2 weeks prior to the study, or if they were taking antibiotics. Also, women who had gonorrhea, candidiasis, chlamydia, or genital herpes could not participate in the trial.
Of the 399 women enrolled, 233 were evaluated for treatment efficacy. Of those, 77 of 113 patients were cured of BV with clindamycin and 80 of 120 women were cured with metronidazole. Side effects of nausea and unpleasant taste were reported more frequently in the metronidazole treatment group. Clinical outcome was determined by vaginal fluid amine odor and clue cells.
While there was no significant difference in the effectiveness of both regimens, the researchers observed that clindamycin had fewer systemic effects because of its shorter dosage regimen (3 days as opposed to 7 days of metronidazole). Therefore, clindamycin was better tolerated among participants.
Find this Study
August 2000 issue of Obstetrics and Gynecology; abstract online at www.acog.com.
Who May be Affected by These Findings?
Women who have BV.
Expert Commentary
BV is present in 10% to 30% of pregnant women and 12% to 61% of women with sexually transmitted diseases. While BV is perceived as a mild medical problem, often without symptoms or signs of vaginal inflammation, it could lead to postoperative infection after hysterectomy, postpartum endometritis, and preterm labor if left untreated. Therefore, fast and effective treatment is imperative.
Unfortunately, the researchers’ findings that the clindamycin was as effective as and better tolerated than the metronidazole are marred by several methodological errors. First, the resolution of the amine odor and clue cells is a poor outcome measure. While the patients may no longer have a malodorous vaginal discharge, this does not mean that a healthy, Lactobacillus-dominant, vaginal microflora has been established. In fact, if the pH level has not been restored to less than 4.5, there is a possibility that the vaginal microflora will be plagued by a gram-positive bacterium, including Streptococcus agalactia or Enterococcus faecalis, or a gram-negative bacterium such as Escherichia coli. Neither agent was particularly satisfactory in restoring a Lactobacillus-dominant microflora. Furthermore, the cure rates were not impressive, as they did not reach 70%.
Moreover, comparing the systemic absorption of clindamycin administered vaginally to metronidazole taken orally is like comparing apples to oranges. Legitimate results will not come from measuring the adverse effects of 2 different antimicrobial agents administered by different routes. In fact, it is well known that many antibiotics taken orally cause the patient to experience nausea, often resulting in discontinuation of the medication.
The Bottom Line
BV continues to be a poorly understood condition. Knowledge of microbial interactions will make it easier to restore an altered vaginal microflora to a healthy one. In the meantime, administer 500 mg of metronidazole orally 3 times a day for 7 days.
At present, women treated for BV should be checked for the following: whether the pH level has returned to a normal range of 3.8 to 4.2 and if Lactobacillus has regained dominance. Failure to achieve these 2 goals means that the treatment was not successful.