User login
SGS 2023 Meeting: Daily Reporting from Tucson
Wednesday, March 22. Day 4 of SGS.
Day 4, and the final day of the 49th SGS conference started with a sunrise run up and down the hills surrounding the JW Marriott Starr Resort. After breakfast, I entered the Tucson Ballroom to attend the last 2 scientific sessions of the conference.

Highlights from the first session included a look at postoperative outcomes and complication rates between gynecologic surgeons and general surgeons using the National Surgical Quality Improvement Program (NSQIP) database by Dr. Douglas Luchristt, who showed no difference between the 2 surgical specialties (and even better outcomes by gynecologists in certain operative measures), as well as the work of Dr. Christopher Hong who used 2 separate surgical databases (NSQIP and Michigan Surgical Quality Collaborative) to show that rates of vaginal hysterectomy have been decreasing from 2017 to 2020, even amongst patients who are likely good candidates for a vaginal route of hysterectomy. Dr. Jocelyn Fitzgerald presented her unique mixed methods research on how to better design the gynecologic office to improve the patient experience, using 3,000 Twitter responses to a question on this topic. Lastly, Dr. Emily Aldrich shared her work on better understanding the patient perception of same day discharge after major vaginal reconstructive surgery. An interesting finding of Dr. Aldrich’s study was that the most common response to her question about the “worst part of the surgical experience” was going home with a postoperative catheter, which surgeons often consider a small and temporary discomfort. The first session ended with the passing of the gavel from current SGS president Dr. Cheryl Iglesia, to the incoming SGS president Dr. Rosanne Kho, with much applause and excitement for what Dr. Kho will bring to the table in her new role.
The research presented at the final scientific session of the conference did not disappoint. A retrospective study on the influence of body mass index (BMI) on the time to surgical diagnosis of endometriosis by Dr. Melissa Markowitz found that obesity was associated with a delay of over 1 year in surgical diagnosis of endometriosis compared with normal and underweight patients. Dr. David (Ike) Rahn presented additional findings on his randomized, double-blinded, multicenter trial on perioperative use of vaginal estrogen cream in postmenopausal patients with prolapse. He found that 5 weeks of estrogen cream use was not associated with any improvement in urinary incontinence or sexual function.
Dr. Stephanie Glass Clark used the Premier Healthcare Database to show that that there was no difference in postoperative mesh exposure in patients who underwent a total hysterectomy compared with supracervical hysterectomy at the time of sacrocolpopexy. Dr. Kavita Mishra presented results from the FLOWER trial, which found no difference in postoperative outcomes for transgender women undergoing vaginoplasty for gender affirmation who did and did not undergo preoperative pelvic floor physical therapy. Finally, Dr. Carly Crowder shared her video of anatomy for sacral neuromodulation with some excellent cadaveric dissections to exhibit the peri-sacral and gluteal anatomy.

As the conference ended, raindrops pounded the sandy grounds of the resort as I waited in the lobby for my Uber to the airport. Dr. Rosanne Kho happened to walk by and stopped to speak with me and one of my attendings. She smiled as she asked about our experience at the conference and to wish us safe travels. To me, this moment embodies the spirit of mentorship and connection that is so unique to the SGS conference. I feel incredibly lucky to have met some of the physician leaders of our field, who genuinely want to get to know and help the next generation. This year’s meeting was attended by ObGyn generalists and surgeons of all gynecologic subspecialties and certainly met its goal in addressing topics with an “Impact Factor.” I am inspired by all the work that is happening across the country to move the needle and better our field. This was my first SGS experience, but it certainly won’t be the last. I hope you too will consider attending in the future!
Tuesday, March 21. Day 3 of SGS.
It’s Day 3 of the SGS conference! In addition to the academic roundtables, conference attendees had the option of doing early-morning yoga with Dr. Mireille Truong. Yoga sounded nice, but I spent the morning in bed, catching up on sleep. (My own version of wellness!) The scientific sessions of the day started at 7:30 am, and I especially want to highlight the work of Dr. Amy Askew who performed a randomized controlled trial comparing patient removal of urinary catheters placed for postoperative urinary retention to office removal. She found that patient urinary catheter removal was a feasible and safe option with excellent patient satisfaction and a reduction of in-person postoperative office visits. At the end of the session, Dr. Cheryl Iglesia gave her presidential address, where she shared her journey to becoming the physician, educator, researcher, and leader she is today. She emphasized the importance of being a continual learner and to give back by mentoring and educating the next generation. “Learn it, earn it, and return it.”

This was followed by the Te Linde lecture, given by Dr. Pamela Moalli. An exceptional surgeon-scientist, Dr. Moalli shared about her work on the impact of mesh on tissue, as well as alternative biologic options being developed, such as 3D printed membranes, extracellular matrix scaffolds, and living tissue grafts to create new ligamentous supports for the vagina. She discussed novel research using stem cell transplantation to harness the power of regeneration in the urethra or vagina following injury. I think it is safe to say that the entire room was in awe of the work she has done, and what she continues to do to find better therapeutic options for girls and women with pelvic floor disorders. Her talk ended in a standing ovation. Afterwards, all the University of Pittsburgh Medical Center-Magee Womens Hospital trainees, faculty, and several alumni took a picture with Dr. Moalli (fifth from the right in the picture).
Lunch followed, which included a brief walk around the industry exhibition hall. I then returned back to the Tucson Ballroom to listen in on the next scientific session on surgical ergonomics. Organized by Dr. Amy Park who herself suffered from work-related musculoskeletal injuries, the session was composed of an excellent video by Dr. Abby Stork on stretches to prevent and reduce the risk of surgeon-associated musculoskeletal injuries, especially in vaginal surgeons. There was then a panel of 3 experts, Dr. Noor Abu-Alnadi, Dr. Ladin Yurteri-Kaplan, and Dr. Susan Hallbeck (PhD ergonomics expert), moderated by Dr. Amanda Fader and Dr. Kimberly Kho. In particular, Dr. Hallbeck developed a timer app as a reminder for surgeons to stop every 40 minutes to stretch for 1.5 minutes (orstretch.mayoclinic.org). This has been studied and found to reduce musculoskeletal pain after surgery and improve physical performance without increasing total operating time. If you would like to see some of these between- and in-OR stretches yourself, an informative handout can be accessed at mcforms.mayo.edu.
Tuesday afternoon was left open. I joined Dr. Veronica Lerner, Dr. Kelly Wright, and Dr. Louise Perkins King on a 7.5-mile hike into the surrounding desert hills. We marveled at the many Saguaro cacti, some over 100 years old and towering many feet high, as well as the beautiful yellow, purple, and magenta flowers that were scattered among the desert brush. Several rabbits and deer wandered by us during our hike. On one of the trails, the stone skeleton of an old house stood, once a home to the Bowen family who had moved to Arizona for health reasons. I could see why they would want to move here—I felt such a peace looking at the gorgeous view from what was once their doorway.

After a shower and a lot of stretching, I got ready for the evening event, A Taste and Toast with SGS: Under the Arizona Skies. The food and drink were delicious, and I got to spend the evening catching up with a good friend. We watched as conference attendees assigned to different color teams (red, green, blue, and yellow), fought for the hallowed Golden Uterus Trophy in several competitive gynecology-themed games (eg, throwing sacral neuromodulation needle “darts” at balloons and removing small pom poms from a water bottle with a disposable operative hysteroscope). As the evening progressed, the DJ turned up the music and people made their way to the dance floor. The event served as a fundraiser for the SGS Pelvic Anatomy Group and successfully raised $35,000.
Monday, March 20. Day 2 of SGS.
Day 2 of the SGS meeting started off with a gentle sunrise over the cacti-covered hills surrounding the JW Marriot Starr Pass Hotel, the venue for the 49th SGS annual scientific meeting. The first official event of the day after some engaging academic round tables was the recognition of the new SGS members. Much celebration was had over the 18 gynecologic surgeons who were inducted.

The second day included the first 3 scientific sessions of the conference. Some highlights include the work of Dr. Shawn Menefee on a randomized trial of sacral colpopexy, transvaginal mesh, and native tissue apical repair for posthysterectomy vault prolapse; a video by Dr. Matthew Fallon on a robotic-assisted laparoscopic approach to repairing a chronic uterine inversion; and the impact of age on regret following hysterectomy by Dr. Nathan King. Dr. Candace Parker-Autry also presented her work on the impact of perineorrhaphy on both female and male sexual function, and Dr. Cassie (Clarissa) Niino spoke elegantly on the “red bag problem” that exists in all of our operating rooms, which increases pollution and cost unnecessarily.
There were also several excellent talks given. Dr. Jason Wright spoke about the importance of surgical volume on gynecologic surgery. In particular, he noted that surgical volume needs to be considered not only at the surgeon level but also at the hospital level. Higher-volume hospitals will provide better care, in the same way that general, high-volume surgeons have less complications and better long-term outcomes. Of note, volume is not the whole picture. We need to also consider measurements of surgery and hospital quality and surgeon skill in addition to volume, as Dr. Shawn Menefee insightfully commented.
Dr. Beri Ridgeway gave the Mark D. Walters Lecture about surgeons in the c-suite and the importance of having a seat at the leadership table as surgeons and medical providers. In her words: “If we aren’t at the table, then we are on the menu.” Overworked and underpaid, burned out doctors feel powerless because they are managed by leaders with a business and not a medical background, and we need to have physicians in leadership who understand how medicine is practiced and to ensure equitable care
Dr. Kelly Wright gave a talk on the environmental impact of gynecologic care—from OR to clinic. She gave examples of how metal, reusable speculums become more cost-effective and produce less waste after only 2-3 uses and how there is no evidence that bouffants reduce surgical site infections (and a reusable scrub cap could work just as well without creating waste). Finally, Dr. Ebony Carter gave an impassioned talk on the need for equity in publication and grant funding in our field. She shared about her initiative through the Green Journal (Obstetrics and Gynecology) to create an issue focused on furthering equity and dispelling racism in medical research.
Later in the afternoon, I attended the Fellows’ Pelvic Research Network (FPRN) meeting, which includes AUGS-SGS (urogynecology fellows) and FMIGS-SGS (fellows of all other gynecologic subspecialities, including minimally invasive gynecologic surgery, family planning, reproductive endocrinology and infertility, and pediatric and adolescent gynecology). Dr. John Gebhart gave an excellent lecture with some impressive photos and videos on how to manage mesh exposure and erosion.
Afterwards, updates were given on the current FPRN projects, and 4 new projects were proposed and underwent audience feedback for improvement. It was exciting to see the multicenter collaborations fostered through the FPRN, and I look forward to seeing which projects will get funded for this upcoming year!
The evening ended with the President's Award Ceremony led by Dr. Cheryl Iglesia, the 49th SGS President, as well as the President's Reception. I also wantd to highlight the winner of the Distinguished Surgeon Award: Dr. Dee Fenner. The remaining awardees are listed on the SGS website (https://sgsonline.org).
Sunday, March 19. Day 1 of SGS.
Last night around midnight, bleary-eyed from the long flight from Pittsburgh, I walked out into the dimly lit, mild air of Tucson, Arizona. The Saguaro cacti that lined the entrance to the airport stood tall and tree-like, with welcoming green arms. It was as if they too knew that the next 4 days would be filled with the building of new relationships and the strengthening of old ones, as well as with education, innovation, and the sharing of research. That spirit of collegiality, approachability, and connection in an intimate and vibrant meeting is what the Society of Gynecologic Surgeons (SGS) meeting has been known for and why it draws people to come back, year after year.
The first day of the conference was fantastic. As a first-time attendant at SGS, I was excited to have the opportunity to meet and rub elbows with mentors and role models from across the country. My day started off with the SGS Fellows and Young Attendings Course, moderated by 3 incredible faculty: Dr. Matthew Barker, Dr. Sadikah Behbehani, and Dr. Traci Ito. Some high-yield topics such as contract negotiation, developing a urogynecology- or MIGS-based practice, billing, academic promotion, and taking advantage of relationships with industry were discussed at length, and the session ended with a roundtable, where the experts had time to answer questions in smaller groups. One of the quotes that will ring true for many fellows about to embark on the job search was from Dr. Amanda Ecker: “Up until now, you were told where to go and what your schedule is. This is the first time you have flexibility and power to decide for yourself.” Therefore, it is important to reflect on what you really desire and/or prioritize in a job, whether it is location, compensation, protected time, or opportunities for advancement.

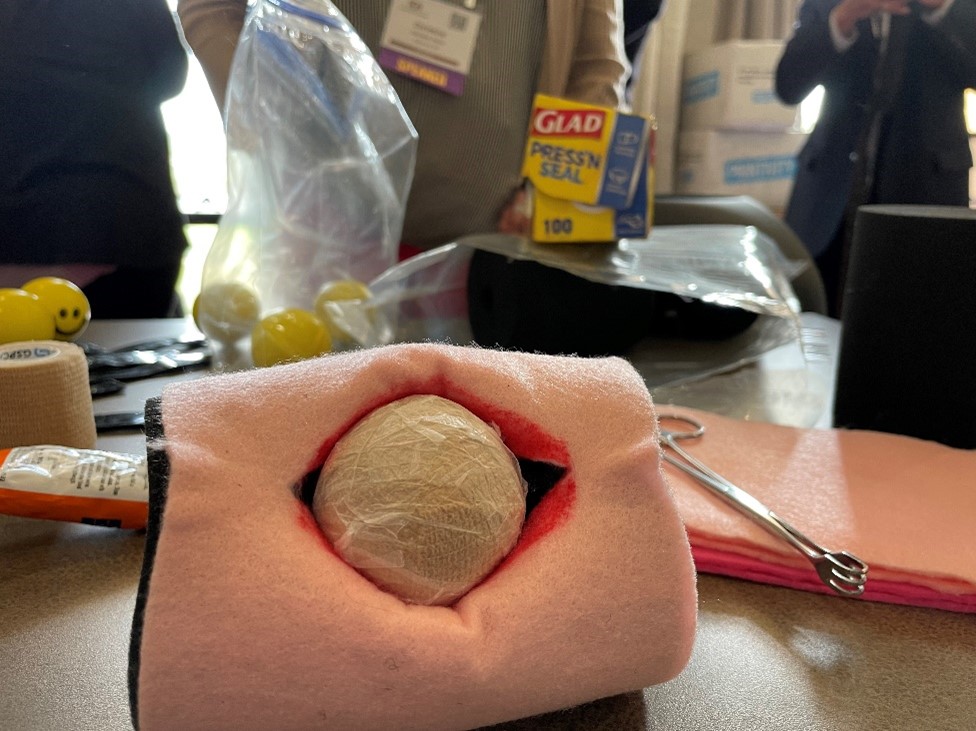
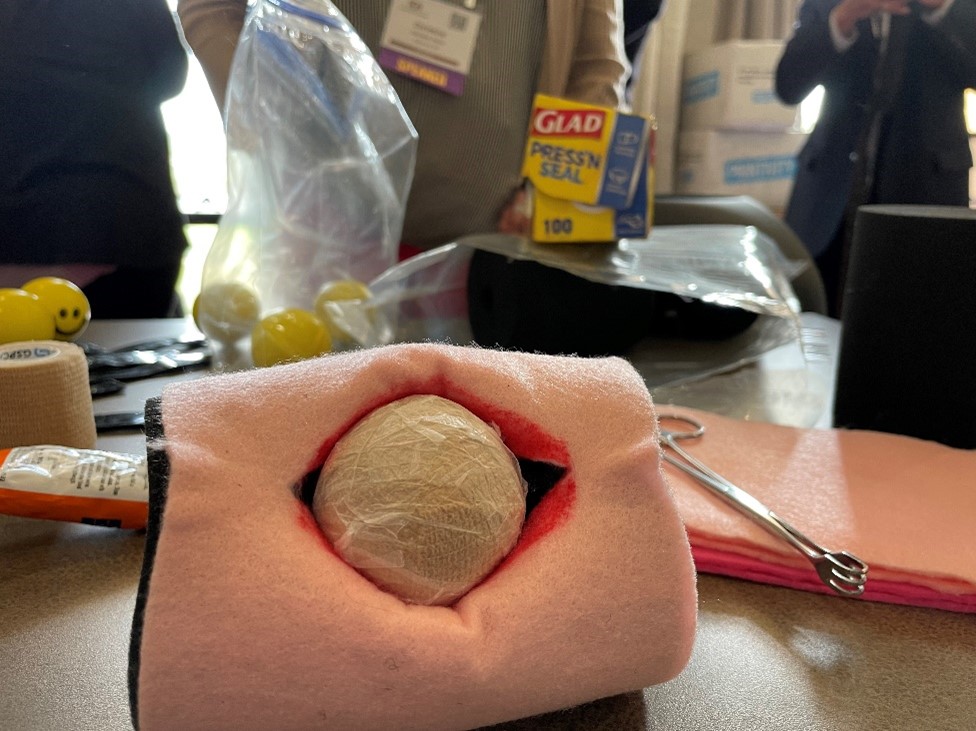
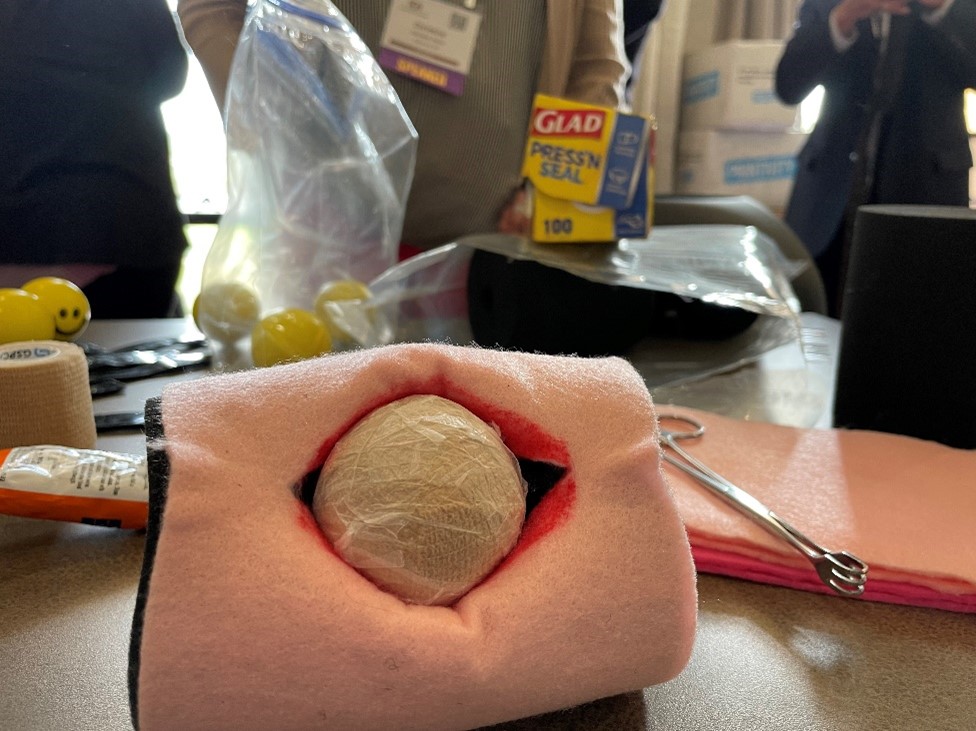
In the afternoon, I attended a postgraduate course led by Dr. Veronica Lerner and Dr. Mireille Truong called “The Sim Factor: Making an Impact in Surgical Education.” Several other excellent postgraduate courses were available, including “Advanced Endometriosis Surgery and Pelvic Pain Patient-Centered Approach,” “Social Media Workshop- #Gynfluencing: Using Social Media to Find Your Digital Voice,” and “Urologic Surgery for the Gynecologic Surgeon: GU Injury, Ureteral Stents, Complex Fistula and More.” I was grateful for the hands-on and tangible tools that Drs. Lerner and Truong left the group with—including ideas such as Zoom-based virtual coaching for trainees learning fundamentals of laparoscopic surgery types of tasks, table-top simulation for high-stakes scenarios (eg, operative vascular injury), and the importance of grounding educational activity in objectives and evaluation. I even got to make and take home my own myomectomy model. (Fun fact: The myoma is actually a stress ball wrapped in an Ace bandage and then Glad Press n’ Seal!
The late afternoon transitioned to an opportunity for trainees to interact with senior SGS members and a welcome reception. The indoor and outdoor spaces were filled with laughing and talking as people connected over drinks and snacks. Finally, the evening ended with a session presented by the SGS Equity Council, “What your Patients REALLY Want to Know.” Patty Brisben, of the Patty Brisben Foundation and founder of the company Pure Romance, was interviewed by Dr. Christine Vaccaro. It was heartwarming to hear how Patty took the stories of women suffering from sexual pain and dissatisfaction and chose to make it her life’s mission to improve women’s sexual health.
Wednesday, March 22. Day 4 of SGS.
Day 4, and the final day of the 49th SGS conference started with a sunrise run up and down the hills surrounding the JW Marriott Starr Resort. After breakfast, I entered the Tucson Ballroom to attend the last 2 scientific sessions of the conference.

Highlights from the first session included a look at postoperative outcomes and complication rates between gynecologic surgeons and general surgeons using the National Surgical Quality Improvement Program (NSQIP) database by Dr. Douglas Luchristt, who showed no difference between the 2 surgical specialties (and even better outcomes by gynecologists in certain operative measures), as well as the work of Dr. Christopher Hong who used 2 separate surgical databases (NSQIP and Michigan Surgical Quality Collaborative) to show that rates of vaginal hysterectomy have been decreasing from 2017 to 2020, even amongst patients who are likely good candidates for a vaginal route of hysterectomy. Dr. Jocelyn Fitzgerald presented her unique mixed methods research on how to better design the gynecologic office to improve the patient experience, using 3,000 Twitter responses to a question on this topic. Lastly, Dr. Emily Aldrich shared her work on better understanding the patient perception of same day discharge after major vaginal reconstructive surgery. An interesting finding of Dr. Aldrich’s study was that the most common response to her question about the “worst part of the surgical experience” was going home with a postoperative catheter, which surgeons often consider a small and temporary discomfort. The first session ended with the passing of the gavel from current SGS president Dr. Cheryl Iglesia, to the incoming SGS president Dr. Rosanne Kho, with much applause and excitement for what Dr. Kho will bring to the table in her new role.
The research presented at the final scientific session of the conference did not disappoint. A retrospective study on the influence of body mass index (BMI) on the time to surgical diagnosis of endometriosis by Dr. Melissa Markowitz found that obesity was associated with a delay of over 1 year in surgical diagnosis of endometriosis compared with normal and underweight patients. Dr. David (Ike) Rahn presented additional findings on his randomized, double-blinded, multicenter trial on perioperative use of vaginal estrogen cream in postmenopausal patients with prolapse. He found that 5 weeks of estrogen cream use was not associated with any improvement in urinary incontinence or sexual function.
Dr. Stephanie Glass Clark used the Premier Healthcare Database to show that that there was no difference in postoperative mesh exposure in patients who underwent a total hysterectomy compared with supracervical hysterectomy at the time of sacrocolpopexy. Dr. Kavita Mishra presented results from the FLOWER trial, which found no difference in postoperative outcomes for transgender women undergoing vaginoplasty for gender affirmation who did and did not undergo preoperative pelvic floor physical therapy. Finally, Dr. Carly Crowder shared her video of anatomy for sacral neuromodulation with some excellent cadaveric dissections to exhibit the peri-sacral and gluteal anatomy.

As the conference ended, raindrops pounded the sandy grounds of the resort as I waited in the lobby for my Uber to the airport. Dr. Rosanne Kho happened to walk by and stopped to speak with me and one of my attendings. She smiled as she asked about our experience at the conference and to wish us safe travels. To me, this moment embodies the spirit of mentorship and connection that is so unique to the SGS conference. I feel incredibly lucky to have met some of the physician leaders of our field, who genuinely want to get to know and help the next generation. This year’s meeting was attended by ObGyn generalists and surgeons of all gynecologic subspecialties and certainly met its goal in addressing topics with an “Impact Factor.” I am inspired by all the work that is happening across the country to move the needle and better our field. This was my first SGS experience, but it certainly won’t be the last. I hope you too will consider attending in the future!
Tuesday, March 21. Day 3 of SGS.
It’s Day 3 of the SGS conference! In addition to the academic roundtables, conference attendees had the option of doing early-morning yoga with Dr. Mireille Truong. Yoga sounded nice, but I spent the morning in bed, catching up on sleep. (My own version of wellness!) The scientific sessions of the day started at 7:30 am, and I especially want to highlight the work of Dr. Amy Askew who performed a randomized controlled trial comparing patient removal of urinary catheters placed for postoperative urinary retention to office removal. She found that patient urinary catheter removal was a feasible and safe option with excellent patient satisfaction and a reduction of in-person postoperative office visits. At the end of the session, Dr. Cheryl Iglesia gave her presidential address, where she shared her journey to becoming the physician, educator, researcher, and leader she is today. She emphasized the importance of being a continual learner and to give back by mentoring and educating the next generation. “Learn it, earn it, and return it.”

This was followed by the Te Linde lecture, given by Dr. Pamela Moalli. An exceptional surgeon-scientist, Dr. Moalli shared about her work on the impact of mesh on tissue, as well as alternative biologic options being developed, such as 3D printed membranes, extracellular matrix scaffolds, and living tissue grafts to create new ligamentous supports for the vagina. She discussed novel research using stem cell transplantation to harness the power of regeneration in the urethra or vagina following injury. I think it is safe to say that the entire room was in awe of the work she has done, and what she continues to do to find better therapeutic options for girls and women with pelvic floor disorders. Her talk ended in a standing ovation. Afterwards, all the University of Pittsburgh Medical Center-Magee Womens Hospital trainees, faculty, and several alumni took a picture with Dr. Moalli (fifth from the right in the picture).
Lunch followed, which included a brief walk around the industry exhibition hall. I then returned back to the Tucson Ballroom to listen in on the next scientific session on surgical ergonomics. Organized by Dr. Amy Park who herself suffered from work-related musculoskeletal injuries, the session was composed of an excellent video by Dr. Abby Stork on stretches to prevent and reduce the risk of surgeon-associated musculoskeletal injuries, especially in vaginal surgeons. There was then a panel of 3 experts, Dr. Noor Abu-Alnadi, Dr. Ladin Yurteri-Kaplan, and Dr. Susan Hallbeck (PhD ergonomics expert), moderated by Dr. Amanda Fader and Dr. Kimberly Kho. In particular, Dr. Hallbeck developed a timer app as a reminder for surgeons to stop every 40 minutes to stretch for 1.5 minutes (orstretch.mayoclinic.org). This has been studied and found to reduce musculoskeletal pain after surgery and improve physical performance without increasing total operating time. If you would like to see some of these between- and in-OR stretches yourself, an informative handout can be accessed at mcforms.mayo.edu.
Tuesday afternoon was left open. I joined Dr. Veronica Lerner, Dr. Kelly Wright, and Dr. Louise Perkins King on a 7.5-mile hike into the surrounding desert hills. We marveled at the many Saguaro cacti, some over 100 years old and towering many feet high, as well as the beautiful yellow, purple, and magenta flowers that were scattered among the desert brush. Several rabbits and deer wandered by us during our hike. On one of the trails, the stone skeleton of an old house stood, once a home to the Bowen family who had moved to Arizona for health reasons. I could see why they would want to move here—I felt such a peace looking at the gorgeous view from what was once their doorway.

After a shower and a lot of stretching, I got ready for the evening event, A Taste and Toast with SGS: Under the Arizona Skies. The food and drink were delicious, and I got to spend the evening catching up with a good friend. We watched as conference attendees assigned to different color teams (red, green, blue, and yellow), fought for the hallowed Golden Uterus Trophy in several competitive gynecology-themed games (eg, throwing sacral neuromodulation needle “darts” at balloons and removing small pom poms from a water bottle with a disposable operative hysteroscope). As the evening progressed, the DJ turned up the music and people made their way to the dance floor. The event served as a fundraiser for the SGS Pelvic Anatomy Group and successfully raised $35,000.
Monday, March 20. Day 2 of SGS.
Day 2 of the SGS meeting started off with a gentle sunrise over the cacti-covered hills surrounding the JW Marriot Starr Pass Hotel, the venue for the 49th SGS annual scientific meeting. The first official event of the day after some engaging academic round tables was the recognition of the new SGS members. Much celebration was had over the 18 gynecologic surgeons who were inducted.

The second day included the first 3 scientific sessions of the conference. Some highlights include the work of Dr. Shawn Menefee on a randomized trial of sacral colpopexy, transvaginal mesh, and native tissue apical repair for posthysterectomy vault prolapse; a video by Dr. Matthew Fallon on a robotic-assisted laparoscopic approach to repairing a chronic uterine inversion; and the impact of age on regret following hysterectomy by Dr. Nathan King. Dr. Candace Parker-Autry also presented her work on the impact of perineorrhaphy on both female and male sexual function, and Dr. Cassie (Clarissa) Niino spoke elegantly on the “red bag problem” that exists in all of our operating rooms, which increases pollution and cost unnecessarily.
There were also several excellent talks given. Dr. Jason Wright spoke about the importance of surgical volume on gynecologic surgery. In particular, he noted that surgical volume needs to be considered not only at the surgeon level but also at the hospital level. Higher-volume hospitals will provide better care, in the same way that general, high-volume surgeons have less complications and better long-term outcomes. Of note, volume is not the whole picture. We need to also consider measurements of surgery and hospital quality and surgeon skill in addition to volume, as Dr. Shawn Menefee insightfully commented.
Dr. Beri Ridgeway gave the Mark D. Walters Lecture about surgeons in the c-suite and the importance of having a seat at the leadership table as surgeons and medical providers. In her words: “If we aren’t at the table, then we are on the menu.” Overworked and underpaid, burned out doctors feel powerless because they are managed by leaders with a business and not a medical background, and we need to have physicians in leadership who understand how medicine is practiced and to ensure equitable care
Dr. Kelly Wright gave a talk on the environmental impact of gynecologic care—from OR to clinic. She gave examples of how metal, reusable speculums become more cost-effective and produce less waste after only 2-3 uses and how there is no evidence that bouffants reduce surgical site infections (and a reusable scrub cap could work just as well without creating waste). Finally, Dr. Ebony Carter gave an impassioned talk on the need for equity in publication and grant funding in our field. She shared about her initiative through the Green Journal (Obstetrics and Gynecology) to create an issue focused on furthering equity and dispelling racism in medical research.
Later in the afternoon, I attended the Fellows’ Pelvic Research Network (FPRN) meeting, which includes AUGS-SGS (urogynecology fellows) and FMIGS-SGS (fellows of all other gynecologic subspecialities, including minimally invasive gynecologic surgery, family planning, reproductive endocrinology and infertility, and pediatric and adolescent gynecology). Dr. John Gebhart gave an excellent lecture with some impressive photos and videos on how to manage mesh exposure and erosion.
Afterwards, updates were given on the current FPRN projects, and 4 new projects were proposed and underwent audience feedback for improvement. It was exciting to see the multicenter collaborations fostered through the FPRN, and I look forward to seeing which projects will get funded for this upcoming year!
The evening ended with the President's Award Ceremony led by Dr. Cheryl Iglesia, the 49th SGS President, as well as the President's Reception. I also wantd to highlight the winner of the Distinguished Surgeon Award: Dr. Dee Fenner. The remaining awardees are listed on the SGS website (https://sgsonline.org).
Sunday, March 19. Day 1 of SGS.
Last night around midnight, bleary-eyed from the long flight from Pittsburgh, I walked out into the dimly lit, mild air of Tucson, Arizona. The Saguaro cacti that lined the entrance to the airport stood tall and tree-like, with welcoming green arms. It was as if they too knew that the next 4 days would be filled with the building of new relationships and the strengthening of old ones, as well as with education, innovation, and the sharing of research. That spirit of collegiality, approachability, and connection in an intimate and vibrant meeting is what the Society of Gynecologic Surgeons (SGS) meeting has been known for and why it draws people to come back, year after year.
The first day of the conference was fantastic. As a first-time attendant at SGS, I was excited to have the opportunity to meet and rub elbows with mentors and role models from across the country. My day started off with the SGS Fellows and Young Attendings Course, moderated by 3 incredible faculty: Dr. Matthew Barker, Dr. Sadikah Behbehani, and Dr. Traci Ito. Some high-yield topics such as contract negotiation, developing a urogynecology- or MIGS-based practice, billing, academic promotion, and taking advantage of relationships with industry were discussed at length, and the session ended with a roundtable, where the experts had time to answer questions in smaller groups. One of the quotes that will ring true for many fellows about to embark on the job search was from Dr. Amanda Ecker: “Up until now, you were told where to go and what your schedule is. This is the first time you have flexibility and power to decide for yourself.” Therefore, it is important to reflect on what you really desire and/or prioritize in a job, whether it is location, compensation, protected time, or opportunities for advancement.

In the afternoon, I attended a postgraduate course led by Dr. Veronica Lerner and Dr. Mireille Truong called “The Sim Factor: Making an Impact in Surgical Education.” Several other excellent postgraduate courses were available, including “Advanced Endometriosis Surgery and Pelvic Pain Patient-Centered Approach,” “Social Media Workshop- #Gynfluencing: Using Social Media to Find Your Digital Voice,” and “Urologic Surgery for the Gynecologic Surgeon: GU Injury, Ureteral Stents, Complex Fistula and More.” I was grateful for the hands-on and tangible tools that Drs. Lerner and Truong left the group with—including ideas such as Zoom-based virtual coaching for trainees learning fundamentals of laparoscopic surgery types of tasks, table-top simulation for high-stakes scenarios (eg, operative vascular injury), and the importance of grounding educational activity in objectives and evaluation. I even got to make and take home my own myomectomy model. (Fun fact: The myoma is actually a stress ball wrapped in an Ace bandage and then Glad Press n’ Seal!
The late afternoon transitioned to an opportunity for trainees to interact with senior SGS members and a welcome reception. The indoor and outdoor spaces were filled with laughing and talking as people connected over drinks and snacks. Finally, the evening ended with a session presented by the SGS Equity Council, “What your Patients REALLY Want to Know.” Patty Brisben, of the Patty Brisben Foundation and founder of the company Pure Romance, was interviewed by Dr. Christine Vaccaro. It was heartwarming to hear how Patty took the stories of women suffering from sexual pain and dissatisfaction and chose to make it her life’s mission to improve women’s sexual health.
Wednesday, March 22. Day 4 of SGS.
Day 4, and the final day of the 49th SGS conference started with a sunrise run up and down the hills surrounding the JW Marriott Starr Resort. After breakfast, I entered the Tucson Ballroom to attend the last 2 scientific sessions of the conference.

Highlights from the first session included a look at postoperative outcomes and complication rates between gynecologic surgeons and general surgeons using the National Surgical Quality Improvement Program (NSQIP) database by Dr. Douglas Luchristt, who showed no difference between the 2 surgical specialties (and even better outcomes by gynecologists in certain operative measures), as well as the work of Dr. Christopher Hong who used 2 separate surgical databases (NSQIP and Michigan Surgical Quality Collaborative) to show that rates of vaginal hysterectomy have been decreasing from 2017 to 2020, even amongst patients who are likely good candidates for a vaginal route of hysterectomy. Dr. Jocelyn Fitzgerald presented her unique mixed methods research on how to better design the gynecologic office to improve the patient experience, using 3,000 Twitter responses to a question on this topic. Lastly, Dr. Emily Aldrich shared her work on better understanding the patient perception of same day discharge after major vaginal reconstructive surgery. An interesting finding of Dr. Aldrich’s study was that the most common response to her question about the “worst part of the surgical experience” was going home with a postoperative catheter, which surgeons often consider a small and temporary discomfort. The first session ended with the passing of the gavel from current SGS president Dr. Cheryl Iglesia, to the incoming SGS president Dr. Rosanne Kho, with much applause and excitement for what Dr. Kho will bring to the table in her new role.
The research presented at the final scientific session of the conference did not disappoint. A retrospective study on the influence of body mass index (BMI) on the time to surgical diagnosis of endometriosis by Dr. Melissa Markowitz found that obesity was associated with a delay of over 1 year in surgical diagnosis of endometriosis compared with normal and underweight patients. Dr. David (Ike) Rahn presented additional findings on his randomized, double-blinded, multicenter trial on perioperative use of vaginal estrogen cream in postmenopausal patients with prolapse. He found that 5 weeks of estrogen cream use was not associated with any improvement in urinary incontinence or sexual function.
Dr. Stephanie Glass Clark used the Premier Healthcare Database to show that that there was no difference in postoperative mesh exposure in patients who underwent a total hysterectomy compared with supracervical hysterectomy at the time of sacrocolpopexy. Dr. Kavita Mishra presented results from the FLOWER trial, which found no difference in postoperative outcomes for transgender women undergoing vaginoplasty for gender affirmation who did and did not undergo preoperative pelvic floor physical therapy. Finally, Dr. Carly Crowder shared her video of anatomy for sacral neuromodulation with some excellent cadaveric dissections to exhibit the peri-sacral and gluteal anatomy.

As the conference ended, raindrops pounded the sandy grounds of the resort as I waited in the lobby for my Uber to the airport. Dr. Rosanne Kho happened to walk by and stopped to speak with me and one of my attendings. She smiled as she asked about our experience at the conference and to wish us safe travels. To me, this moment embodies the spirit of mentorship and connection that is so unique to the SGS conference. I feel incredibly lucky to have met some of the physician leaders of our field, who genuinely want to get to know and help the next generation. This year’s meeting was attended by ObGyn generalists and surgeons of all gynecologic subspecialties and certainly met its goal in addressing topics with an “Impact Factor.” I am inspired by all the work that is happening across the country to move the needle and better our field. This was my first SGS experience, but it certainly won’t be the last. I hope you too will consider attending in the future!
Tuesday, March 21. Day 3 of SGS.
It’s Day 3 of the SGS conference! In addition to the academic roundtables, conference attendees had the option of doing early-morning yoga with Dr. Mireille Truong. Yoga sounded nice, but I spent the morning in bed, catching up on sleep. (My own version of wellness!) The scientific sessions of the day started at 7:30 am, and I especially want to highlight the work of Dr. Amy Askew who performed a randomized controlled trial comparing patient removal of urinary catheters placed for postoperative urinary retention to office removal. She found that patient urinary catheter removal was a feasible and safe option with excellent patient satisfaction and a reduction of in-person postoperative office visits. At the end of the session, Dr. Cheryl Iglesia gave her presidential address, where she shared her journey to becoming the physician, educator, researcher, and leader she is today. She emphasized the importance of being a continual learner and to give back by mentoring and educating the next generation. “Learn it, earn it, and return it.”

This was followed by the Te Linde lecture, given by Dr. Pamela Moalli. An exceptional surgeon-scientist, Dr. Moalli shared about her work on the impact of mesh on tissue, as well as alternative biologic options being developed, such as 3D printed membranes, extracellular matrix scaffolds, and living tissue grafts to create new ligamentous supports for the vagina. She discussed novel research using stem cell transplantation to harness the power of regeneration in the urethra or vagina following injury. I think it is safe to say that the entire room was in awe of the work she has done, and what she continues to do to find better therapeutic options for girls and women with pelvic floor disorders. Her talk ended in a standing ovation. Afterwards, all the University of Pittsburgh Medical Center-Magee Womens Hospital trainees, faculty, and several alumni took a picture with Dr. Moalli (fifth from the right in the picture).
Lunch followed, which included a brief walk around the industry exhibition hall. I then returned back to the Tucson Ballroom to listen in on the next scientific session on surgical ergonomics. Organized by Dr. Amy Park who herself suffered from work-related musculoskeletal injuries, the session was composed of an excellent video by Dr. Abby Stork on stretches to prevent and reduce the risk of surgeon-associated musculoskeletal injuries, especially in vaginal surgeons. There was then a panel of 3 experts, Dr. Noor Abu-Alnadi, Dr. Ladin Yurteri-Kaplan, and Dr. Susan Hallbeck (PhD ergonomics expert), moderated by Dr. Amanda Fader and Dr. Kimberly Kho. In particular, Dr. Hallbeck developed a timer app as a reminder for surgeons to stop every 40 minutes to stretch for 1.5 minutes (orstretch.mayoclinic.org). This has been studied and found to reduce musculoskeletal pain after surgery and improve physical performance without increasing total operating time. If you would like to see some of these between- and in-OR stretches yourself, an informative handout can be accessed at mcforms.mayo.edu.
Tuesday afternoon was left open. I joined Dr. Veronica Lerner, Dr. Kelly Wright, and Dr. Louise Perkins King on a 7.5-mile hike into the surrounding desert hills. We marveled at the many Saguaro cacti, some over 100 years old and towering many feet high, as well as the beautiful yellow, purple, and magenta flowers that were scattered among the desert brush. Several rabbits and deer wandered by us during our hike. On one of the trails, the stone skeleton of an old house stood, once a home to the Bowen family who had moved to Arizona for health reasons. I could see why they would want to move here—I felt such a peace looking at the gorgeous view from what was once their doorway.

After a shower and a lot of stretching, I got ready for the evening event, A Taste and Toast with SGS: Under the Arizona Skies. The food and drink were delicious, and I got to spend the evening catching up with a good friend. We watched as conference attendees assigned to different color teams (red, green, blue, and yellow), fought for the hallowed Golden Uterus Trophy in several competitive gynecology-themed games (eg, throwing sacral neuromodulation needle “darts” at balloons and removing small pom poms from a water bottle with a disposable operative hysteroscope). As the evening progressed, the DJ turned up the music and people made their way to the dance floor. The event served as a fundraiser for the SGS Pelvic Anatomy Group and successfully raised $35,000.
Monday, March 20. Day 2 of SGS.
Day 2 of the SGS meeting started off with a gentle sunrise over the cacti-covered hills surrounding the JW Marriot Starr Pass Hotel, the venue for the 49th SGS annual scientific meeting. The first official event of the day after some engaging academic round tables was the recognition of the new SGS members. Much celebration was had over the 18 gynecologic surgeons who were inducted.

The second day included the first 3 scientific sessions of the conference. Some highlights include the work of Dr. Shawn Menefee on a randomized trial of sacral colpopexy, transvaginal mesh, and native tissue apical repair for posthysterectomy vault prolapse; a video by Dr. Matthew Fallon on a robotic-assisted laparoscopic approach to repairing a chronic uterine inversion; and the impact of age on regret following hysterectomy by Dr. Nathan King. Dr. Candace Parker-Autry also presented her work on the impact of perineorrhaphy on both female and male sexual function, and Dr. Cassie (Clarissa) Niino spoke elegantly on the “red bag problem” that exists in all of our operating rooms, which increases pollution and cost unnecessarily.
There were also several excellent talks given. Dr. Jason Wright spoke about the importance of surgical volume on gynecologic surgery. In particular, he noted that surgical volume needs to be considered not only at the surgeon level but also at the hospital level. Higher-volume hospitals will provide better care, in the same way that general, high-volume surgeons have less complications and better long-term outcomes. Of note, volume is not the whole picture. We need to also consider measurements of surgery and hospital quality and surgeon skill in addition to volume, as Dr. Shawn Menefee insightfully commented.
Dr. Beri Ridgeway gave the Mark D. Walters Lecture about surgeons in the c-suite and the importance of having a seat at the leadership table as surgeons and medical providers. In her words: “If we aren’t at the table, then we are on the menu.” Overworked and underpaid, burned out doctors feel powerless because they are managed by leaders with a business and not a medical background, and we need to have physicians in leadership who understand how medicine is practiced and to ensure equitable care
Dr. Kelly Wright gave a talk on the environmental impact of gynecologic care—from OR to clinic. She gave examples of how metal, reusable speculums become more cost-effective and produce less waste after only 2-3 uses and how there is no evidence that bouffants reduce surgical site infections (and a reusable scrub cap could work just as well without creating waste). Finally, Dr. Ebony Carter gave an impassioned talk on the need for equity in publication and grant funding in our field. She shared about her initiative through the Green Journal (Obstetrics and Gynecology) to create an issue focused on furthering equity and dispelling racism in medical research.
Later in the afternoon, I attended the Fellows’ Pelvic Research Network (FPRN) meeting, which includes AUGS-SGS (urogynecology fellows) and FMIGS-SGS (fellows of all other gynecologic subspecialities, including minimally invasive gynecologic surgery, family planning, reproductive endocrinology and infertility, and pediatric and adolescent gynecology). Dr. John Gebhart gave an excellent lecture with some impressive photos and videos on how to manage mesh exposure and erosion.
Afterwards, updates were given on the current FPRN projects, and 4 new projects were proposed and underwent audience feedback for improvement. It was exciting to see the multicenter collaborations fostered through the FPRN, and I look forward to seeing which projects will get funded for this upcoming year!
The evening ended with the President's Award Ceremony led by Dr. Cheryl Iglesia, the 49th SGS President, as well as the President's Reception. I also wantd to highlight the winner of the Distinguished Surgeon Award: Dr. Dee Fenner. The remaining awardees are listed on the SGS website (https://sgsonline.org).
Sunday, March 19. Day 1 of SGS.
Last night around midnight, bleary-eyed from the long flight from Pittsburgh, I walked out into the dimly lit, mild air of Tucson, Arizona. The Saguaro cacti that lined the entrance to the airport stood tall and tree-like, with welcoming green arms. It was as if they too knew that the next 4 days would be filled with the building of new relationships and the strengthening of old ones, as well as with education, innovation, and the sharing of research. That spirit of collegiality, approachability, and connection in an intimate and vibrant meeting is what the Society of Gynecologic Surgeons (SGS) meeting has been known for and why it draws people to come back, year after year.
The first day of the conference was fantastic. As a first-time attendant at SGS, I was excited to have the opportunity to meet and rub elbows with mentors and role models from across the country. My day started off with the SGS Fellows and Young Attendings Course, moderated by 3 incredible faculty: Dr. Matthew Barker, Dr. Sadikah Behbehani, and Dr. Traci Ito. Some high-yield topics such as contract negotiation, developing a urogynecology- or MIGS-based practice, billing, academic promotion, and taking advantage of relationships with industry were discussed at length, and the session ended with a roundtable, where the experts had time to answer questions in smaller groups. One of the quotes that will ring true for many fellows about to embark on the job search was from Dr. Amanda Ecker: “Up until now, you were told where to go and what your schedule is. This is the first time you have flexibility and power to decide for yourself.” Therefore, it is important to reflect on what you really desire and/or prioritize in a job, whether it is location, compensation, protected time, or opportunities for advancement.

In the afternoon, I attended a postgraduate course led by Dr. Veronica Lerner and Dr. Mireille Truong called “The Sim Factor: Making an Impact in Surgical Education.” Several other excellent postgraduate courses were available, including “Advanced Endometriosis Surgery and Pelvic Pain Patient-Centered Approach,” “Social Media Workshop- #Gynfluencing: Using Social Media to Find Your Digital Voice,” and “Urologic Surgery for the Gynecologic Surgeon: GU Injury, Ureteral Stents, Complex Fistula and More.” I was grateful for the hands-on and tangible tools that Drs. Lerner and Truong left the group with—including ideas such as Zoom-based virtual coaching for trainees learning fundamentals of laparoscopic surgery types of tasks, table-top simulation for high-stakes scenarios (eg, operative vascular injury), and the importance of grounding educational activity in objectives and evaluation. I even got to make and take home my own myomectomy model. (Fun fact: The myoma is actually a stress ball wrapped in an Ace bandage and then Glad Press n’ Seal!
The late afternoon transitioned to an opportunity for trainees to interact with senior SGS members and a welcome reception. The indoor and outdoor spaces were filled with laughing and talking as people connected over drinks and snacks. Finally, the evening ended with a session presented by the SGS Equity Council, “What your Patients REALLY Want to Know.” Patty Brisben, of the Patty Brisben Foundation and founder of the company Pure Romance, was interviewed by Dr. Christine Vaccaro. It was heartwarming to hear how Patty took the stories of women suffering from sexual pain and dissatisfaction and chose to make it her life’s mission to improve women’s sexual health.