User login
This is a drill
She had fallen on a garden implement, lacerating her superficial femoral artery. She used her cell phone to call 911. Thanks to an alert EMS crew and the Stop the Bleed training they recently received, a tourniquet was placed without delay. She got to our trauma bay in about 15 minutes after the tourniquet was applied. Although the patient made it abundantly clear that she was in pain, she was stable with moderate tachycardia and a good blood pressure.
Our trauma team leaped into action. The leader took report from the EMS while two nurses and a second surgeon assessed the patient, got her clothes cut off, and applied monitors. A third nurse got a second IV going. Primary survey was done in less than 90 seconds. The patient then underwent a focused exam including a log roll for back injuries.
The leg wound was still oozing a bit, so a second tourniquet was called for and pressure applied until it could be acquired. The patient was given 5 mg of morphine sulfate, which calmed her down a bit. Labs and x-rays were done quickly. The nursing staff suggested a tetanus booster, and the second surgeon who had gotten a basic past medical history suggested vancomycin since the patient said she was allergic to penicillin. Fifteen minutes after she hit the trauma bay, she was on her way to the OR for exploration, debridement, and vascular repair of her injury.
This was all done by four M2 medical students and five N4 nursing students, none of whom had had previous experience with this type of trauma patient
The students were managing this trauma situation in the simulation center of their medical school with four staff watching. This was their second run through for the afternoon. At debriefing, they compared their work on the first trauma of the day (a stab wound to the right chest) to their second attempt. They were satisfied with their efforts and so were we, the faculty who ran the simulation. Comparing their response to those I’ve seen in real life, I’d say these students understood their roles and responsibilities as well as the sort of thrown-together teams I’ve seen at places where trauma is not the main focus. While these young men and women are in the early stage of training and not ready for a real-world trauma emergency, they have gained knowledge about this kind of situation that I didn’t see until I was in residency and beyond. The times they are a-changing.
A couple of days later I was in Rochester, Minn., attending an American College of Surgeons Advanced Education Institute (ACS/AEI) course on simulations. At the end of that course, we participants were challenged by a manikin in extremis. Everyone there was an expert, had an advanced degree, had some experience in simulation, or were surgeons interested in simulation. I found that, even though this was a simulation and the patient was only a pretend human being, my adrenal cortex performed almost as if I were doing a real resuscitation. Previous training I’d had on teamwork, crew resource management, and ACLS all kicked in, and we got it done. But interestingly, we weren’t perfect. We debriefed and found that, even at our level of experience and training, a simple simulation could be very instructive. Seeing/doing is believing.
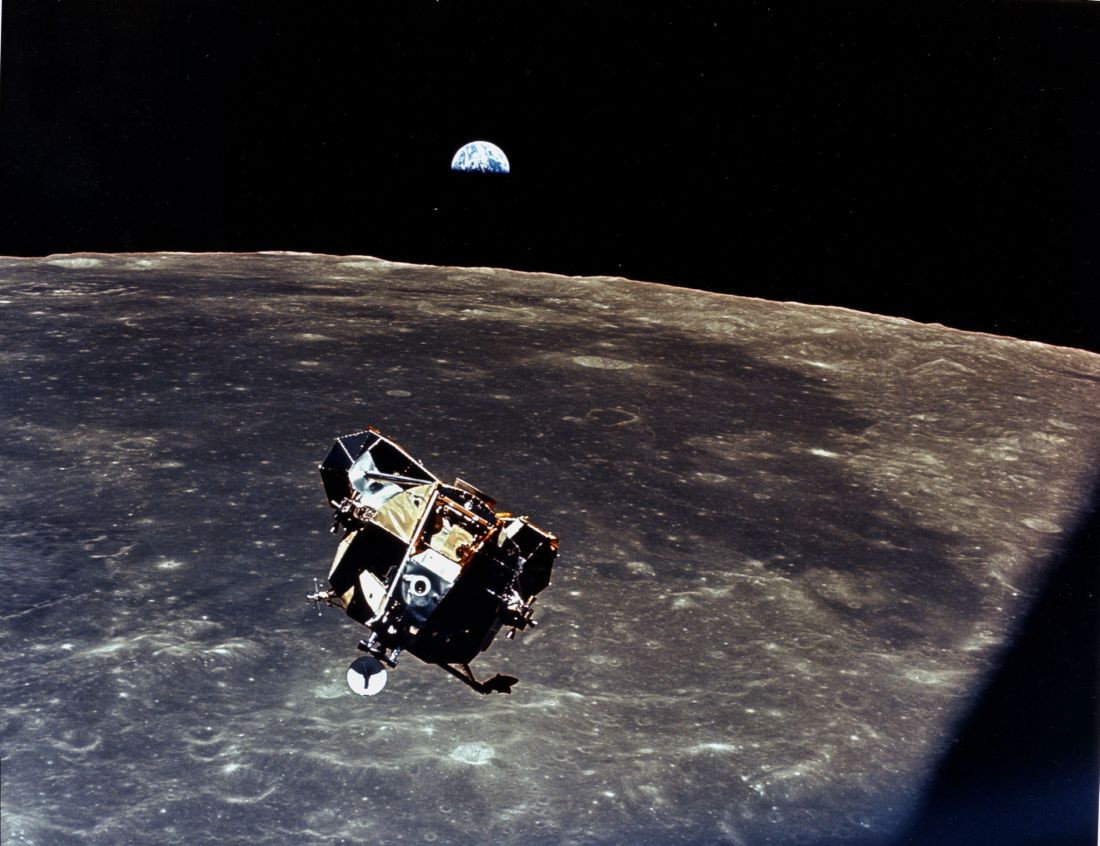
High-tech skills in high-risk occupations are well served by simulation training. Much of the airline piloting training is done by simulation. It works well for aviation, nuclear reactors, high voltage line work, and medicine. Most of these disciplines have embraced simulation as an essential part of training. Simulation is part of many surgical training programs, but it has other uses.
When was the last time you practiced a trauma resuscitation, an ultrasound fine-needle biopsy, laparoscopic maneuvers, or an unusual technique that you seldom perform, but when needed, must be pulled off very well? Most of us taking this simulation course agreed that time, money, and ego may get in the way of maintaining those skills for those rare instances when they are needed. Surgeons might want to consider simulation to keep some of our rarely used skills from getting rusty.
If you’re going to make a costly error, I would very much like you to do it on a piece of plastic, not on a patient. There are no consequences for messing up a procedure on a manikin and this kind of practice might teach you something critical. Practicing reduces stress and improves the performance of those placed on the spot by real-life events. Do you think Captain “Sully” Sullenberger could have landed that airliner in the Hudson River safely if he hadn’t practiced with countless mind-numbingly complex simulations? Sure, luck plays a part, and innate ability plays a part. But skill, knowledge, and practice are your best bet when all the eyes in the room swivel to you in a moment of crisis.
You may think that simulators have to cost $100,000 and be completely realistic to do the job. That’s not true. A banana, orange, or stick of butter can be fabulous sims for a med student. Felt and cardboard can make a realistic cricothyroidotomy model.
Surgeons all over the country are using simulation training to learn how to be better without getting real blood on their shoes. If you haven’t participated in a training simulation recently, I double-dog dare you to try it and tell me you found it without merit. The ACS Surgical Simulation Summit is being held in March 2019 in Chicago. You might want to check that out.
Dr. Hughes is clinical professor in the department of surgery and director of medical education at the University of Kansas School of Medicine, Salina, and Coeditor of ACS Surgery News.
She had fallen on a garden implement, lacerating her superficial femoral artery. She used her cell phone to call 911. Thanks to an alert EMS crew and the Stop the Bleed training they recently received, a tourniquet was placed without delay. She got to our trauma bay in about 15 minutes after the tourniquet was applied. Although the patient made it abundantly clear that she was in pain, she was stable with moderate tachycardia and a good blood pressure.
Our trauma team leaped into action. The leader took report from the EMS while two nurses and a second surgeon assessed the patient, got her clothes cut off, and applied monitors. A third nurse got a second IV going. Primary survey was done in less than 90 seconds. The patient then underwent a focused exam including a log roll for back injuries.
The leg wound was still oozing a bit, so a second tourniquet was called for and pressure applied until it could be acquired. The patient was given 5 mg of morphine sulfate, which calmed her down a bit. Labs and x-rays were done quickly. The nursing staff suggested a tetanus booster, and the second surgeon who had gotten a basic past medical history suggested vancomycin since the patient said she was allergic to penicillin. Fifteen minutes after she hit the trauma bay, she was on her way to the OR for exploration, debridement, and vascular repair of her injury.
This was all done by four M2 medical students and five N4 nursing students, none of whom had had previous experience with this type of trauma patient
The students were managing this trauma situation in the simulation center of their medical school with four staff watching. This was their second run through for the afternoon. At debriefing, they compared their work on the first trauma of the day (a stab wound to the right chest) to their second attempt. They were satisfied with their efforts and so were we, the faculty who ran the simulation. Comparing their response to those I’ve seen in real life, I’d say these students understood their roles and responsibilities as well as the sort of thrown-together teams I’ve seen at places where trauma is not the main focus. While these young men and women are in the early stage of training and not ready for a real-world trauma emergency, they have gained knowledge about this kind of situation that I didn’t see until I was in residency and beyond. The times they are a-changing.
A couple of days later I was in Rochester, Minn., attending an American College of Surgeons Advanced Education Institute (ACS/AEI) course on simulations. At the end of that course, we participants were challenged by a manikin in extremis. Everyone there was an expert, had an advanced degree, had some experience in simulation, or were surgeons interested in simulation. I found that, even though this was a simulation and the patient was only a pretend human being, my adrenal cortex performed almost as if I were doing a real resuscitation. Previous training I’d had on teamwork, crew resource management, and ACLS all kicked in, and we got it done. But interestingly, we weren’t perfect. We debriefed and found that, even at our level of experience and training, a simple simulation could be very instructive. Seeing/doing is believing.
High-tech skills in high-risk occupations are well served by simulation training. Much of the airline piloting training is done by simulation. It works well for aviation, nuclear reactors, high voltage line work, and medicine. Most of these disciplines have embraced simulation as an essential part of training. Simulation is part of many surgical training programs, but it has other uses.
When was the last time you practiced a trauma resuscitation, an ultrasound fine-needle biopsy, laparoscopic maneuvers, or an unusual technique that you seldom perform, but when needed, must be pulled off very well? Most of us taking this simulation course agreed that time, money, and ego may get in the way of maintaining those skills for those rare instances when they are needed. Surgeons might want to consider simulation to keep some of our rarely used skills from getting rusty.
If you’re going to make a costly error, I would very much like you to do it on a piece of plastic, not on a patient. There are no consequences for messing up a procedure on a manikin and this kind of practice might teach you something critical. Practicing reduces stress and improves the performance of those placed on the spot by real-life events. Do you think Captain “Sully” Sullenberger could have landed that airliner in the Hudson River safely if he hadn’t practiced with countless mind-numbingly complex simulations? Sure, luck plays a part, and innate ability plays a part. But skill, knowledge, and practice are your best bet when all the eyes in the room swivel to you in a moment of crisis.
You may think that simulators have to cost $100,000 and be completely realistic to do the job. That’s not true. A banana, orange, or stick of butter can be fabulous sims for a med student. Felt and cardboard can make a realistic cricothyroidotomy model.
Surgeons all over the country are using simulation training to learn how to be better without getting real blood on their shoes. If you haven’t participated in a training simulation recently, I double-dog dare you to try it and tell me you found it without merit. The ACS Surgical Simulation Summit is being held in March 2019 in Chicago. You might want to check that out.
Dr. Hughes is clinical professor in the department of surgery and director of medical education at the University of Kansas School of Medicine, Salina, and Coeditor of ACS Surgery News.
She had fallen on a garden implement, lacerating her superficial femoral artery. She used her cell phone to call 911. Thanks to an alert EMS crew and the Stop the Bleed training they recently received, a tourniquet was placed without delay. She got to our trauma bay in about 15 minutes after the tourniquet was applied. Although the patient made it abundantly clear that she was in pain, she was stable with moderate tachycardia and a good blood pressure.
Our trauma team leaped into action. The leader took report from the EMS while two nurses and a second surgeon assessed the patient, got her clothes cut off, and applied monitors. A third nurse got a second IV going. Primary survey was done in less than 90 seconds. The patient then underwent a focused exam including a log roll for back injuries.
The leg wound was still oozing a bit, so a second tourniquet was called for and pressure applied until it could be acquired. The patient was given 5 mg of morphine sulfate, which calmed her down a bit. Labs and x-rays were done quickly. The nursing staff suggested a tetanus booster, and the second surgeon who had gotten a basic past medical history suggested vancomycin since the patient said she was allergic to penicillin. Fifteen minutes after she hit the trauma bay, she was on her way to the OR for exploration, debridement, and vascular repair of her injury.
This was all done by four M2 medical students and five N4 nursing students, none of whom had had previous experience with this type of trauma patient
The students were managing this trauma situation in the simulation center of their medical school with four staff watching. This was their second run through for the afternoon. At debriefing, they compared their work on the first trauma of the day (a stab wound to the right chest) to their second attempt. They were satisfied with their efforts and so were we, the faculty who ran the simulation. Comparing their response to those I’ve seen in real life, I’d say these students understood their roles and responsibilities as well as the sort of thrown-together teams I’ve seen at places where trauma is not the main focus. While these young men and women are in the early stage of training and not ready for a real-world trauma emergency, they have gained knowledge about this kind of situation that I didn’t see until I was in residency and beyond. The times they are a-changing.
A couple of days later I was in Rochester, Minn., attending an American College of Surgeons Advanced Education Institute (ACS/AEI) course on simulations. At the end of that course, we participants were challenged by a manikin in extremis. Everyone there was an expert, had an advanced degree, had some experience in simulation, or were surgeons interested in simulation. I found that, even though this was a simulation and the patient was only a pretend human being, my adrenal cortex performed almost as if I were doing a real resuscitation. Previous training I’d had on teamwork, crew resource management, and ACLS all kicked in, and we got it done. But interestingly, we weren’t perfect. We debriefed and found that, even at our level of experience and training, a simple simulation could be very instructive. Seeing/doing is believing.
High-tech skills in high-risk occupations are well served by simulation training. Much of the airline piloting training is done by simulation. It works well for aviation, nuclear reactors, high voltage line work, and medicine. Most of these disciplines have embraced simulation as an essential part of training. Simulation is part of many surgical training programs, but it has other uses.
When was the last time you practiced a trauma resuscitation, an ultrasound fine-needle biopsy, laparoscopic maneuvers, or an unusual technique that you seldom perform, but when needed, must be pulled off very well? Most of us taking this simulation course agreed that time, money, and ego may get in the way of maintaining those skills for those rare instances when they are needed. Surgeons might want to consider simulation to keep some of our rarely used skills from getting rusty.
If you’re going to make a costly error, I would very much like you to do it on a piece of plastic, not on a patient. There are no consequences for messing up a procedure on a manikin and this kind of practice might teach you something critical. Practicing reduces stress and improves the performance of those placed on the spot by real-life events. Do you think Captain “Sully” Sullenberger could have landed that airliner in the Hudson River safely if he hadn’t practiced with countless mind-numbingly complex simulations? Sure, luck plays a part, and innate ability plays a part. But skill, knowledge, and practice are your best bet when all the eyes in the room swivel to you in a moment of crisis.
You may think that simulators have to cost $100,000 and be completely realistic to do the job. That’s not true. A banana, orange, or stick of butter can be fabulous sims for a med student. Felt and cardboard can make a realistic cricothyroidotomy model.
Surgeons all over the country are using simulation training to learn how to be better without getting real blood on their shoes. If you haven’t participated in a training simulation recently, I double-dog dare you to try it and tell me you found it without merit. The ACS Surgical Simulation Summit is being held in March 2019 in Chicago. You might want to check that out.
Dr. Hughes is clinical professor in the department of surgery and director of medical education at the University of Kansas School of Medicine, Salina, and Coeditor of ACS Surgery News.
Fighting fires
When I grow up, I want to be a fireman. Not long ago, I had occasion to revisit why firefighters are such heroes to young and old. In the process, I learned quite a bit about how fires are managed and realized that a really good surgeon has much in common with a fire Incident Commander.
In late June 2018, a man started a fire in Southern Colorado. That small campfire became the Spring Fire, the third-largest forest fire in Colorado history, which is saying a lot. By the time the fire was mostly contained 2 weeks later, 175 square miles of land had been burned and 1,800 firefighters were involved in the disaster. More than 150 homes were destroyed. Not one person died in or as a result of this fire. Only the most grudging of critics would deny that, while the fire itself was a disaster, the response and outcome constituted a good definition of success.
This story was more than just 30 seconds on the nightly news to me because I was one of the people whose property and 32 years of precious family memories were in danger. I clung to any news of the fire. My own daughter had to evacuate our place there when smoke and flame were visible just a few miles away. I was helpless to do anything but hoped that somehow this conflagration could be stopped.
Within 48 hours, Rocky Mountain Black Team – headed by a man named Shane Greer – arrived in the area. Mr. Greer is the Incident Commander of the Black Team. Over the next 10 days he was the personification of the response to the Spring Fire. He was the main person carrying the overall responsibility for controlling the fire.
The fire is over now, but I reflect frequently on the parallels between surgery and firefighting. I identified with Mr. Greer as probably many did. He didn’t actually stop the fire, but he led the people who did. I was intrigued by this role and I did a little research in fire Incident Commanders. Here’s a list of their numerous roles and responsibilities that I gleaned from an article on the website Firehouse by editor Dennis Rubin from several years ago:
- The Incident Commander (IC) must be a qualified, single, central, and well-supported individual.
- The IC’s main concern is safety of lives and must be conversant in fire-safety procedures.
- The IC must have an understanding of his/her personal limitations. An IC must have firsthand experience at firefighting so that the IC is an individual well informed of the difficulties being experienced on the front line of the fire.
- The priorities of the IC are a) life safety; b) incident stabilization; and c) property conservation.
- The IC develops strategies (what to do) and tactics (how to do it) and follows action plans to achieve these goals.
- The IC develops a management structure that uses span of control (one supervisor per five subordinates) with each unit having a single boss.
- A good IC is a good delegator and calls for help early in the incident including placement of resources in staging areas.
- The IC is responsible for all communication among the team and to the media/public.
- The IC coordinates with outside agencies.
Does this sound familiar to you? Substitute surgeon for IC and you have today’s profile of a good surgeon. When executed well, everyone involved in an incident gets to be a hero and feels a part of something bigger than themselves. The IC (surgeon) gets a lot of credit, but that person also makes sure the whole team gets all the credit and thanks they deserve.
What I see happening in some situations is that we in medicine are putting the wrong ICs in charge or abdicating our positions as IC to others because being an IC is a hard, demanding, full-time job. I also see medicine violating the principles in the first bullet point above – a single, central, and well-supported individual. We get the job of IC and then payers, administrators, and outside agencies drop the support part of the ball. We also have a tendency to violate the “qualified” part of the job description. Someone who has put on the gown and gloves and borne the responsibility of operating should be the quarterback and not someone who has only observed that process.
I can’t thank enough the Black Team and all those who fought the Spring Fire. I hope we all aspire to be ICs in our surgical world. There is a great nobility in such professions as firefighting and surgery, where we jump in to help others who can’t help themselves. The Black Team showed that to me and my community in Colorado. It makes one proud of what we human beings can do when we decide to work together.
True leadership and teamwork do not fragment but instead pull resources together. Patients need that. They need to know that a qualified, single, central, and well-supported person is directing their incident. The existence of such a person fulfilling that role is key to keep the trust that the public places in us. May all our “fires” be led by a good surgeon, er, Incident Commander surgeon.
Dr. Hughes is clinical professor in the department of surgery and director of medical education at the Kansas University School of Medicine, Salina Campus, and Co-Editor of ACS Surgery News.
When I grow up, I want to be a fireman. Not long ago, I had occasion to revisit why firefighters are such heroes to young and old. In the process, I learned quite a bit about how fires are managed and realized that a really good surgeon has much in common with a fire Incident Commander.
In late June 2018, a man started a fire in Southern Colorado. That small campfire became the Spring Fire, the third-largest forest fire in Colorado history, which is saying a lot. By the time the fire was mostly contained 2 weeks later, 175 square miles of land had been burned and 1,800 firefighters were involved in the disaster. More than 150 homes were destroyed. Not one person died in or as a result of this fire. Only the most grudging of critics would deny that, while the fire itself was a disaster, the response and outcome constituted a good definition of success.
This story was more than just 30 seconds on the nightly news to me because I was one of the people whose property and 32 years of precious family memories were in danger. I clung to any news of the fire. My own daughter had to evacuate our place there when smoke and flame were visible just a few miles away. I was helpless to do anything but hoped that somehow this conflagration could be stopped.
Within 48 hours, Rocky Mountain Black Team – headed by a man named Shane Greer – arrived in the area. Mr. Greer is the Incident Commander of the Black Team. Over the next 10 days he was the personification of the response to the Spring Fire. He was the main person carrying the overall responsibility for controlling the fire.
The fire is over now, but I reflect frequently on the parallels between surgery and firefighting. I identified with Mr. Greer as probably many did. He didn’t actually stop the fire, but he led the people who did. I was intrigued by this role and I did a little research in fire Incident Commanders. Here’s a list of their numerous roles and responsibilities that I gleaned from an article on the website Firehouse by editor Dennis Rubin from several years ago:
- The Incident Commander (IC) must be a qualified, single, central, and well-supported individual.
- The IC’s main concern is safety of lives and must be conversant in fire-safety procedures.
- The IC must have an understanding of his/her personal limitations. An IC must have firsthand experience at firefighting so that the IC is an individual well informed of the difficulties being experienced on the front line of the fire.
- The priorities of the IC are a) life safety; b) incident stabilization; and c) property conservation.
- The IC develops strategies (what to do) and tactics (how to do it) and follows action plans to achieve these goals.
- The IC develops a management structure that uses span of control (one supervisor per five subordinates) with each unit having a single boss.
- A good IC is a good delegator and calls for help early in the incident including placement of resources in staging areas.
- The IC is responsible for all communication among the team and to the media/public.
- The IC coordinates with outside agencies.
Does this sound familiar to you? Substitute surgeon for IC and you have today’s profile of a good surgeon. When executed well, everyone involved in an incident gets to be a hero and feels a part of something bigger than themselves. The IC (surgeon) gets a lot of credit, but that person also makes sure the whole team gets all the credit and thanks they deserve.
What I see happening in some situations is that we in medicine are putting the wrong ICs in charge or abdicating our positions as IC to others because being an IC is a hard, demanding, full-time job. I also see medicine violating the principles in the first bullet point above – a single, central, and well-supported individual. We get the job of IC and then payers, administrators, and outside agencies drop the support part of the ball. We also have a tendency to violate the “qualified” part of the job description. Someone who has put on the gown and gloves and borne the responsibility of operating should be the quarterback and not someone who has only observed that process.
I can’t thank enough the Black Team and all those who fought the Spring Fire. I hope we all aspire to be ICs in our surgical world. There is a great nobility in such professions as firefighting and surgery, where we jump in to help others who can’t help themselves. The Black Team showed that to me and my community in Colorado. It makes one proud of what we human beings can do when we decide to work together.
True leadership and teamwork do not fragment but instead pull resources together. Patients need that. They need to know that a qualified, single, central, and well-supported person is directing their incident. The existence of such a person fulfilling that role is key to keep the trust that the public places in us. May all our “fires” be led by a good surgeon, er, Incident Commander surgeon.
Dr. Hughes is clinical professor in the department of surgery and director of medical education at the Kansas University School of Medicine, Salina Campus, and Co-Editor of ACS Surgery News.
When I grow up, I want to be a fireman. Not long ago, I had occasion to revisit why firefighters are such heroes to young and old. In the process, I learned quite a bit about how fires are managed and realized that a really good surgeon has much in common with a fire Incident Commander.
In late June 2018, a man started a fire in Southern Colorado. That small campfire became the Spring Fire, the third-largest forest fire in Colorado history, which is saying a lot. By the time the fire was mostly contained 2 weeks later, 175 square miles of land had been burned and 1,800 firefighters were involved in the disaster. More than 150 homes were destroyed. Not one person died in or as a result of this fire. Only the most grudging of critics would deny that, while the fire itself was a disaster, the response and outcome constituted a good definition of success.
This story was more than just 30 seconds on the nightly news to me because I was one of the people whose property and 32 years of precious family memories were in danger. I clung to any news of the fire. My own daughter had to evacuate our place there when smoke and flame were visible just a few miles away. I was helpless to do anything but hoped that somehow this conflagration could be stopped.
Within 48 hours, Rocky Mountain Black Team – headed by a man named Shane Greer – arrived in the area. Mr. Greer is the Incident Commander of the Black Team. Over the next 10 days he was the personification of the response to the Spring Fire. He was the main person carrying the overall responsibility for controlling the fire.
The fire is over now, but I reflect frequently on the parallels between surgery and firefighting. I identified with Mr. Greer as probably many did. He didn’t actually stop the fire, but he led the people who did. I was intrigued by this role and I did a little research in fire Incident Commanders. Here’s a list of their numerous roles and responsibilities that I gleaned from an article on the website Firehouse by editor Dennis Rubin from several years ago:
- The Incident Commander (IC) must be a qualified, single, central, and well-supported individual.
- The IC’s main concern is safety of lives and must be conversant in fire-safety procedures.
- The IC must have an understanding of his/her personal limitations. An IC must have firsthand experience at firefighting so that the IC is an individual well informed of the difficulties being experienced on the front line of the fire.
- The priorities of the IC are a) life safety; b) incident stabilization; and c) property conservation.
- The IC develops strategies (what to do) and tactics (how to do it) and follows action plans to achieve these goals.
- The IC develops a management structure that uses span of control (one supervisor per five subordinates) with each unit having a single boss.
- A good IC is a good delegator and calls for help early in the incident including placement of resources in staging areas.
- The IC is responsible for all communication among the team and to the media/public.
- The IC coordinates with outside agencies.
Does this sound familiar to you? Substitute surgeon for IC and you have today’s profile of a good surgeon. When executed well, everyone involved in an incident gets to be a hero and feels a part of something bigger than themselves. The IC (surgeon) gets a lot of credit, but that person also makes sure the whole team gets all the credit and thanks they deserve.
What I see happening in some situations is that we in medicine are putting the wrong ICs in charge or abdicating our positions as IC to others because being an IC is a hard, demanding, full-time job. I also see medicine violating the principles in the first bullet point above – a single, central, and well-supported individual. We get the job of IC and then payers, administrators, and outside agencies drop the support part of the ball. We also have a tendency to violate the “qualified” part of the job description. Someone who has put on the gown and gloves and borne the responsibility of operating should be the quarterback and not someone who has only observed that process.
I can’t thank enough the Black Team and all those who fought the Spring Fire. I hope we all aspire to be ICs in our surgical world. There is a great nobility in such professions as firefighting and surgery, where we jump in to help others who can’t help themselves. The Black Team showed that to me and my community in Colorado. It makes one proud of what we human beings can do when we decide to work together.
True leadership and teamwork do not fragment but instead pull resources together. Patients need that. They need to know that a qualified, single, central, and well-supported person is directing their incident. The existence of such a person fulfilling that role is key to keep the trust that the public places in us. May all our “fires” be led by a good surgeon, er, Incident Commander surgeon.
Dr. Hughes is clinical professor in the department of surgery and director of medical education at the Kansas University School of Medicine, Salina Campus, and Co-Editor of ACS Surgery News.
Eleven on a scale of 1 to 10
I literally rode into the sunset recently as I finished my tour of duty as one of the Director examiners for the American Board of Surgery. I was heading out of St. Louis westward toward my home in Kansas. It was a 9-hour drive, which gave me plenty of time to reflect on the 6 years I shared the responsibility of administering the certifying exam known by most surgeons as “the oral exam.”
Over the last dozen years, Directors V. Suzanne Klimberg and Karen J. Brasel, along with former Executive Director Frank Lewis, a team of psychometricians at the Board, and members of the certification committee of the Board, worked tirelessly to create a testing instrument as fair and statistically sound as possible given the inherently qualitative exam. I believe they did a magnificent job. Gone are the legends of yesteryear where candidates were subjected to the whims of whatever crossed the mind of the examiners, including their prejudices about the “right” answer. The oral exam now represents a well-constructed survey of surgical judgment issues that have been thoroughly vetted.
Being an examiner for the orals means you arrive Sunday afternoon before the exams that are given over the next two and a half days. Each examiner undergoes an overview briefing on Sunday afternoon and then studies “the book” for that test’s content usually until late into the night. This book is an impressive document.
We arise around 0530 to attend a breakfast meeting, which includes breaking into our six-person teams and going over each question that will be given that day. At 0800, the first candidates for the first session walk into a room and meet the two surgeons who will make some of the most important decisions affecting that candidate’s career. If you rate the intensity of this moment on a scale of 1 to 10, this is an 11 for both candidates and examiners. No one in the room knows how it will turn out because every session has its own twists and turns. Everyone there wants to see a passing score, but the two examiners know that they must make a decision that is safe for the public and fair for the candidate.
Twelve exams are given per team per day except for the final day which has only six. So, each team examines 30 candidates over 3 days. I’ve opened a door and shaken the moist hand of 438 candidates. I’ve seen every sort of emotion during those sessions. I’ve had moments of great joy and times of profound sadness as candidates respond to the questions. I’ve always tried to be friendly, but just like surgery, it is a serious business and decisions have to be made. That means ignoring one’s hopes and acting on the best facts available at the moment. Most surgeons remember their oral examiners and what they were asked for a lifetime. I know I do.
I could write a book on this experience (I won’t, though). But as I reflect on my time as a Director, what stands out in my mind are the associate examiners with whom I’ve worked. These surgeons are invited to participate and receive no compensation. It’s 3 days out of their lives, and because they don’t give the exam as frequently as the Directors do, the amount of study and effort is greater for them. Each is selected because he or she is considered to be a thoughtful surgeon with high standards. These surgeons do this job because they care about quality in our profession.
Most of the associates I have worked with are far more accomplished than I. I was once paired with a renowned breast surgeon (okay, it was Kelly K. Hunt). My ego was at great risk because I knew how accomplished she was. But like all the other associates, she was gracious and hard working. We rarely work with another Director, but Anne G. Rizzo, who later became a Director, and I did an exam together. She was a dazzling questioner with very high standards. In other words, she was typical of the people I met. My first associate (also later a Director) was Reid Adams. He was great; I was nervous. My last associate was Marc L. Melcher, a transplant surgeon who asked penetrating questions in a calm manner. I wish I could name each of my associates and thank them for making my work so much better, for teaching me things I didn’t know, for deepening my own knowledge, and serving in a hard job with grace. This column can’t be that long, but you all know who you are. Thank you.
At the end of the day, I believe the oral exam to be a great thing for our profession. When you think about the number of patients potentially affected throughout a surgeon’s career, the impact of decisions made on the day of the exam can be enormous. Given that, over a 20-year career, a surgeon may operate on 25,000 patients, a summative check on a surgeon’s judgment and knowledge is important. Each year, the ABS adjudicates on some 1,100 surgeons. A single year’s set of surgeons over the following 20-year period translates into 27.5 million patients. I hope we never stop doing the orals because of cost, time, or convenience. The exam is just too important to our profession to risk forgoing this last, big step before a surgeon is presented to the world as “certified.”
I literally rode into the sunset recently as I finished my tour of duty as one of the Director examiners for the American Board of Surgery. I was heading out of St. Louis westward toward my home in Kansas. It was a 9-hour drive, which gave me plenty of time to reflect on the 6 years I shared the responsibility of administering the certifying exam known by most surgeons as “the oral exam.”
Over the last dozen years, Directors V. Suzanne Klimberg and Karen J. Brasel, along with former Executive Director Frank Lewis, a team of psychometricians at the Board, and members of the certification committee of the Board, worked tirelessly to create a testing instrument as fair and statistically sound as possible given the inherently qualitative exam. I believe they did a magnificent job. Gone are the legends of yesteryear where candidates were subjected to the whims of whatever crossed the mind of the examiners, including their prejudices about the “right” answer. The oral exam now represents a well-constructed survey of surgical judgment issues that have been thoroughly vetted.
Being an examiner for the orals means you arrive Sunday afternoon before the exams that are given over the next two and a half days. Each examiner undergoes an overview briefing on Sunday afternoon and then studies “the book” for that test’s content usually until late into the night. This book is an impressive document.
We arise around 0530 to attend a breakfast meeting, which includes breaking into our six-person teams and going over each question that will be given that day. At 0800, the first candidates for the first session walk into a room and meet the two surgeons who will make some of the most important decisions affecting that candidate’s career. If you rate the intensity of this moment on a scale of 1 to 10, this is an 11 for both candidates and examiners. No one in the room knows how it will turn out because every session has its own twists and turns. Everyone there wants to see a passing score, but the two examiners know that they must make a decision that is safe for the public and fair for the candidate.
Twelve exams are given per team per day except for the final day which has only six. So, each team examines 30 candidates over 3 days. I’ve opened a door and shaken the moist hand of 438 candidates. I’ve seen every sort of emotion during those sessions. I’ve had moments of great joy and times of profound sadness as candidates respond to the questions. I’ve always tried to be friendly, but just like surgery, it is a serious business and decisions have to be made. That means ignoring one’s hopes and acting on the best facts available at the moment. Most surgeons remember their oral examiners and what they were asked for a lifetime. I know I do.
I could write a book on this experience (I won’t, though). But as I reflect on my time as a Director, what stands out in my mind are the associate examiners with whom I’ve worked. These surgeons are invited to participate and receive no compensation. It’s 3 days out of their lives, and because they don’t give the exam as frequently as the Directors do, the amount of study and effort is greater for them. Each is selected because he or she is considered to be a thoughtful surgeon with high standards. These surgeons do this job because they care about quality in our profession.
Most of the associates I have worked with are far more accomplished than I. I was once paired with a renowned breast surgeon (okay, it was Kelly K. Hunt). My ego was at great risk because I knew how accomplished she was. But like all the other associates, she was gracious and hard working. We rarely work with another Director, but Anne G. Rizzo, who later became a Director, and I did an exam together. She was a dazzling questioner with very high standards. In other words, she was typical of the people I met. My first associate (also later a Director) was Reid Adams. He was great; I was nervous. My last associate was Marc L. Melcher, a transplant surgeon who asked penetrating questions in a calm manner. I wish I could name each of my associates and thank them for making my work so much better, for teaching me things I didn’t know, for deepening my own knowledge, and serving in a hard job with grace. This column can’t be that long, but you all know who you are. Thank you.
At the end of the day, I believe the oral exam to be a great thing for our profession. When you think about the number of patients potentially affected throughout a surgeon’s career, the impact of decisions made on the day of the exam can be enormous. Given that, over a 20-year career, a surgeon may operate on 25,000 patients, a summative check on a surgeon’s judgment and knowledge is important. Each year, the ABS adjudicates on some 1,100 surgeons. A single year’s set of surgeons over the following 20-year period translates into 27.5 million patients. I hope we never stop doing the orals because of cost, time, or convenience. The exam is just too important to our profession to risk forgoing this last, big step before a surgeon is presented to the world as “certified.”
I literally rode into the sunset recently as I finished my tour of duty as one of the Director examiners for the American Board of Surgery. I was heading out of St. Louis westward toward my home in Kansas. It was a 9-hour drive, which gave me plenty of time to reflect on the 6 years I shared the responsibility of administering the certifying exam known by most surgeons as “the oral exam.”
Over the last dozen years, Directors V. Suzanne Klimberg and Karen J. Brasel, along with former Executive Director Frank Lewis, a team of psychometricians at the Board, and members of the certification committee of the Board, worked tirelessly to create a testing instrument as fair and statistically sound as possible given the inherently qualitative exam. I believe they did a magnificent job. Gone are the legends of yesteryear where candidates were subjected to the whims of whatever crossed the mind of the examiners, including their prejudices about the “right” answer. The oral exam now represents a well-constructed survey of surgical judgment issues that have been thoroughly vetted.
Being an examiner for the orals means you arrive Sunday afternoon before the exams that are given over the next two and a half days. Each examiner undergoes an overview briefing on Sunday afternoon and then studies “the book” for that test’s content usually until late into the night. This book is an impressive document.
We arise around 0530 to attend a breakfast meeting, which includes breaking into our six-person teams and going over each question that will be given that day. At 0800, the first candidates for the first session walk into a room and meet the two surgeons who will make some of the most important decisions affecting that candidate’s career. If you rate the intensity of this moment on a scale of 1 to 10, this is an 11 for both candidates and examiners. No one in the room knows how it will turn out because every session has its own twists and turns. Everyone there wants to see a passing score, but the two examiners know that they must make a decision that is safe for the public and fair for the candidate.
Twelve exams are given per team per day except for the final day which has only six. So, each team examines 30 candidates over 3 days. I’ve opened a door and shaken the moist hand of 438 candidates. I’ve seen every sort of emotion during those sessions. I’ve had moments of great joy and times of profound sadness as candidates respond to the questions. I’ve always tried to be friendly, but just like surgery, it is a serious business and decisions have to be made. That means ignoring one’s hopes and acting on the best facts available at the moment. Most surgeons remember their oral examiners and what they were asked for a lifetime. I know I do.
I could write a book on this experience (I won’t, though). But as I reflect on my time as a Director, what stands out in my mind are the associate examiners with whom I’ve worked. These surgeons are invited to participate and receive no compensation. It’s 3 days out of their lives, and because they don’t give the exam as frequently as the Directors do, the amount of study and effort is greater for them. Each is selected because he or she is considered to be a thoughtful surgeon with high standards. These surgeons do this job because they care about quality in our profession.
Most of the associates I have worked with are far more accomplished than I. I was once paired with a renowned breast surgeon (okay, it was Kelly K. Hunt). My ego was at great risk because I knew how accomplished she was. But like all the other associates, she was gracious and hard working. We rarely work with another Director, but Anne G. Rizzo, who later became a Director, and I did an exam together. She was a dazzling questioner with very high standards. In other words, she was typical of the people I met. My first associate (also later a Director) was Reid Adams. He was great; I was nervous. My last associate was Marc L. Melcher, a transplant surgeon who asked penetrating questions in a calm manner. I wish I could name each of my associates and thank them for making my work so much better, for teaching me things I didn’t know, for deepening my own knowledge, and serving in a hard job with grace. This column can’t be that long, but you all know who you are. Thank you.
At the end of the day, I believe the oral exam to be a great thing for our profession. When you think about the number of patients potentially affected throughout a surgeon’s career, the impact of decisions made on the day of the exam can be enormous. Given that, over a 20-year career, a surgeon may operate on 25,000 patients, a summative check on a surgeon’s judgment and knowledge is important. Each year, the ABS adjudicates on some 1,100 surgeons. A single year’s set of surgeons over the following 20-year period translates into 27.5 million patients. I hope we never stop doing the orals because of cost, time, or convenience. The exam is just too important to our profession to risk forgoing this last, big step before a surgeon is presented to the world as “certified.”
From the Editors: Unexpected benefits
I am a member of several surgical societies, and more than once I’ve extolled the importance of going to meetings as part of my personal definition of a “good” surgeon.
While I mostly enjoy meetings nowadays, it hasn’t always been easy. My first experiences at surgical society meetings were painful. I was 32 years old, just out of training, and didn’t know anyone at the meetings. Receptions were the worst. My only friend sometimes was either my host or my wife. I was surrounded by these old guys, most of whom were famous.
Among the highlights of my life was being invited to join the Western Surgical Association. The year I was elected, J. David Richardson was the President. He gave such a rousing speech that at the President’s Dinner I rallied the courage to speak to the great man. When I called him “Dr. Richardson,” he waved that off and insisted I call him “Dave.” Little did I know that Dave would become one of my personal heroes and play an important part in the path that led to my being in a position to write a column such as this.
I never thought that being at a meeting might save my own life. As a devoted member of the Western Surgical Association, I breezed into Phoenix last year for the annual meeting. But I wasn’t feeling so well. Typical of a surgeon, I’d been denying that the symptoms in my abdomen and back were anything other than arthritis. Also, like most surgeons, I’d been pushing the accelerator pedal of life to the floorboard for some months. I arrived at the hotel at one in the morning with a stomach ache that clearly was becoming serious.
I lay in bed wondering what to do. Surgeons don’t get sick! Calling 911 seemed like an invitation to a 6-hour ED experience during which I would be demoted from surgeon to “the patient in Room 9” in a town where I didn’t know many people. As a surgeon, I knew that belly pain of this magnitude was not something I wanted to entrust to a nonsurgeon who was just trying to get through another long shift. This was personal.
Here’s where being a member of a surgical society became more than an academic exercise. I was in a hotel with many of the finest surgeons in the world – and I knew many of them! Among the attendees was my very good friend Margo Shoup, a first-rate cancer surgeon from Chicago. I knew she had come in that day because we were to have dinner together the next night. Rather than call her at 0300, I waited until 6. She came right over and examined me. We decided on a plan. As is always the case at a surgical meeting, one of the surgeon members is the local arrangement person. In this instance, it was none other than James Madura, MD, Chief of MIS GI surgery at Mayo Clinic, Scottsdale. We called James and when my abdomen decided to go nuclear with pain, he drove me to his hospital in his own car and got me in their ED.
The rest of the story is pretty mundane. My diagnosis turned out to be temporarily serious but benign. It was serious enough that without good people treating me, I could have done poorly. James and his fine team took superb care of me. Almost all of us go into surgery with the intent to help others. We take that extraseriously when it’s one of “us.” I can imagine the increased pressure on James when he was treating a colleague and the entire rest of the Western Surgical Association knew it. He never even broke a sweat. I am so glad he was my surgeon. His chief resident Ryan Day, MD, spent extra time with me. I saw a bunch of other residents as well. They reminded me of my fellow residents many years ago – eager, bright, and hyperdedicated. Several members of the Western came by the hospital to see me and even reviewed my images and diagnosis with me. I felt like I had a whole family of physicians who were both my friends and my support system a long way from home. I cannot thank James, Margo, and the rest enough for all they did. It’s great to feel back to normal again as well.
So, I would suggest you join and participate in the surgical societies that you think are a good fit for you. Develop those important professional relationships. Such activity will do your patients a world of good – and just might save your own life.
I am a member of several surgical societies, and more than once I’ve extolled the importance of going to meetings as part of my personal definition of a “good” surgeon.
While I mostly enjoy meetings nowadays, it hasn’t always been easy. My first experiences at surgical society meetings were painful. I was 32 years old, just out of training, and didn’t know anyone at the meetings. Receptions were the worst. My only friend sometimes was either my host or my wife. I was surrounded by these old guys, most of whom were famous.
Among the highlights of my life was being invited to join the Western Surgical Association. The year I was elected, J. David Richardson was the President. He gave such a rousing speech that at the President’s Dinner I rallied the courage to speak to the great man. When I called him “Dr. Richardson,” he waved that off and insisted I call him “Dave.” Little did I know that Dave would become one of my personal heroes and play an important part in the path that led to my being in a position to write a column such as this.
I never thought that being at a meeting might save my own life. As a devoted member of the Western Surgical Association, I breezed into Phoenix last year for the annual meeting. But I wasn’t feeling so well. Typical of a surgeon, I’d been denying that the symptoms in my abdomen and back were anything other than arthritis. Also, like most surgeons, I’d been pushing the accelerator pedal of life to the floorboard for some months. I arrived at the hotel at one in the morning with a stomach ache that clearly was becoming serious.
I lay in bed wondering what to do. Surgeons don’t get sick! Calling 911 seemed like an invitation to a 6-hour ED experience during which I would be demoted from surgeon to “the patient in Room 9” in a town where I didn’t know many people. As a surgeon, I knew that belly pain of this magnitude was not something I wanted to entrust to a nonsurgeon who was just trying to get through another long shift. This was personal.
Here’s where being a member of a surgical society became more than an academic exercise. I was in a hotel with many of the finest surgeons in the world – and I knew many of them! Among the attendees was my very good friend Margo Shoup, a first-rate cancer surgeon from Chicago. I knew she had come in that day because we were to have dinner together the next night. Rather than call her at 0300, I waited until 6. She came right over and examined me. We decided on a plan. As is always the case at a surgical meeting, one of the surgeon members is the local arrangement person. In this instance, it was none other than James Madura, MD, Chief of MIS GI surgery at Mayo Clinic, Scottsdale. We called James and when my abdomen decided to go nuclear with pain, he drove me to his hospital in his own car and got me in their ED.
The rest of the story is pretty mundane. My diagnosis turned out to be temporarily serious but benign. It was serious enough that without good people treating me, I could have done poorly. James and his fine team took superb care of me. Almost all of us go into surgery with the intent to help others. We take that extraseriously when it’s one of “us.” I can imagine the increased pressure on James when he was treating a colleague and the entire rest of the Western Surgical Association knew it. He never even broke a sweat. I am so glad he was my surgeon. His chief resident Ryan Day, MD, spent extra time with me. I saw a bunch of other residents as well. They reminded me of my fellow residents many years ago – eager, bright, and hyperdedicated. Several members of the Western came by the hospital to see me and even reviewed my images and diagnosis with me. I felt like I had a whole family of physicians who were both my friends and my support system a long way from home. I cannot thank James, Margo, and the rest enough for all they did. It’s great to feel back to normal again as well.
So, I would suggest you join and participate in the surgical societies that you think are a good fit for you. Develop those important professional relationships. Such activity will do your patients a world of good – and just might save your own life.
I am a member of several surgical societies, and more than once I’ve extolled the importance of going to meetings as part of my personal definition of a “good” surgeon.
While I mostly enjoy meetings nowadays, it hasn’t always been easy. My first experiences at surgical society meetings were painful. I was 32 years old, just out of training, and didn’t know anyone at the meetings. Receptions were the worst. My only friend sometimes was either my host or my wife. I was surrounded by these old guys, most of whom were famous.
Among the highlights of my life was being invited to join the Western Surgical Association. The year I was elected, J. David Richardson was the President. He gave such a rousing speech that at the President’s Dinner I rallied the courage to speak to the great man. When I called him “Dr. Richardson,” he waved that off and insisted I call him “Dave.” Little did I know that Dave would become one of my personal heroes and play an important part in the path that led to my being in a position to write a column such as this.
I never thought that being at a meeting might save my own life. As a devoted member of the Western Surgical Association, I breezed into Phoenix last year for the annual meeting. But I wasn’t feeling so well. Typical of a surgeon, I’d been denying that the symptoms in my abdomen and back were anything other than arthritis. Also, like most surgeons, I’d been pushing the accelerator pedal of life to the floorboard for some months. I arrived at the hotel at one in the morning with a stomach ache that clearly was becoming serious.
I lay in bed wondering what to do. Surgeons don’t get sick! Calling 911 seemed like an invitation to a 6-hour ED experience during which I would be demoted from surgeon to “the patient in Room 9” in a town where I didn’t know many people. As a surgeon, I knew that belly pain of this magnitude was not something I wanted to entrust to a nonsurgeon who was just trying to get through another long shift. This was personal.
Here’s where being a member of a surgical society became more than an academic exercise. I was in a hotel with many of the finest surgeons in the world – and I knew many of them! Among the attendees was my very good friend Margo Shoup, a first-rate cancer surgeon from Chicago. I knew she had come in that day because we were to have dinner together the next night. Rather than call her at 0300, I waited until 6. She came right over and examined me. We decided on a plan. As is always the case at a surgical meeting, one of the surgeon members is the local arrangement person. In this instance, it was none other than James Madura, MD, Chief of MIS GI surgery at Mayo Clinic, Scottsdale. We called James and when my abdomen decided to go nuclear with pain, he drove me to his hospital in his own car and got me in their ED.
The rest of the story is pretty mundane. My diagnosis turned out to be temporarily serious but benign. It was serious enough that without good people treating me, I could have done poorly. James and his fine team took superb care of me. Almost all of us go into surgery with the intent to help others. We take that extraseriously when it’s one of “us.” I can imagine the increased pressure on James when he was treating a colleague and the entire rest of the Western Surgical Association knew it. He never even broke a sweat. I am so glad he was my surgeon. His chief resident Ryan Day, MD, spent extra time with me. I saw a bunch of other residents as well. They reminded me of my fellow residents many years ago – eager, bright, and hyperdedicated. Several members of the Western came by the hospital to see me and even reviewed my images and diagnosis with me. I felt like I had a whole family of physicians who were both my friends and my support system a long way from home. I cannot thank James, Margo, and the rest enough for all they did. It’s great to feel back to normal again as well.
So, I would suggest you join and participate in the surgical societies that you think are a good fit for you. Develop those important professional relationships. Such activity will do your patients a world of good – and just might save your own life.
From the Editors: How about that!
For all those who say that the surgeon in the trenches doesn’t have a voice in the world of organized surgery, I have a story or two for you.
About 10 or more years ago, I was at a lovely old hotel in Cooperstown, N.Y., listening to a group of elder rural surgery colleagues hold forth about feeling ignored by the American College of Surgeons and how we should all band together to form a new society of rural surgeons. Like most crowds, they were getting pretty worked up. They were pretty sure such a revolution would solve our problems and we would quit being the Rodney Dangerfields of surgery (not getting any respect, as the great comic used to say).
It took a while – a few years – for the rural surgeons and ACS leadership to get to know each other better. We did, however, get there. An Advisory Council was created with the help of some very heavy hitters not often regarded as rural champions, most of whom had roots in the rural world that helped them understand what this group of surgeons wanted and needed.
Not too much removed from this event, many surgeons were feeling isolated in general due to the many challenges of rural practice familiar to so many of us. ACS leadership sensed that surgeons needed to be connected and with considerable effort they formed listservs and found that they were successful to some degree. So, under Dr. David Hoyt’s guidance a better technology was found, resources were committed, and the ACS Communities was launched. A new era in surgeon-to-surgeon and surgeon-to-leadership communication was born. It was as if we had developed talk radio for surgeons. Some stations were loud, others came in rather softly, but all were on the air. The pulse of the Fellows became audible.
Almost simultaneously, dissatisfaction with Maintenance of Certification grew as surgeons in practice began reaching their second and third recertification and the practice of surgery became ever more specialized. Many surgeons believed that nothing would ever change, that the front-line surgeon didn’t have a chance to affect change, and that the big dogs wouldn’t listen. But the College leadership heard the voices of concern and took steps to support a new approach to certification.
So here we are in 2017, coming off a very successful Clinical Congress. The formerly obscure rural surgeon contingent had several panels on the program. Surgeons practicing in towns as small as 3,000 moderated sessions. Some of those sessions were standing room only. The College assisted (and had for a few years) those rural surgeons in organizing a Rural Surgery Dinner, which filled a restaurant full of surgeons delighted to meet in person surgeons from small communities all over the country. They shared their common experiences and planned for a better tomorrow. Later in the week, the 2nd Vice President-Elect was announced. He is a surgeon from Keokuk, IA, and one of the leaders of the rural surgeon movement within the College, Philip Caropreso, MD, FACS. A new Regent was announced: Gary Timmerman, MD, FACS. Dr. Timmerman started his career in Watertown, S.D., and now runs a rural-based surgery training program.
The Clinical Congress program included many topics and issues that Fellows from every branch of surgery had posted about on the ACS Communities. The American Board of Surgery announced sweeping coming changes to help surgeons move on from an MOC system no one was really happy with to one that has great hope of making ongoing certification more than a hoop to jump through, but instead, a real value to the Diplomate. Sitting on the main committee for the American Board of Surgery’s sprint team on certification is a surgeon from Crockett, Texas, Pat Walker, MD, FACS, who practiced surgery “on the ground” in a small community setting for three decades.
Most of us would agree that rural surgeons are facing truly daunting professional headwinds, despite their critical work in serving rural patients. Yet I have been gladdened at the response and respect that the College leadership has given to rural surgeons in recent years. The outreach by the College to support rural surgeons is part of a broader effort to hear every Fellow and make the College more relevant in the life of hard-working surgeons of every type. Changes in how we retain and improve our certification process in some significant ways came out of College efforts to listen and respond to the concerns of Fellows in the College. These and other initiatives by the College leadership show a degree of farsightedness and caring that should be gratifying to all Fellows.
When Lindsay Fox, MD, FACS, a young rural surgeon in private practice with an 8-week-old baby, receives an award for excellence, moderates her panel at the Clinical Congress to a standing-room-only crowd, and then shares her experience through the Communities, I’d say the American College of Surgeons has done an amazing job in a short period of time to make our organization reflect all of us. As Mel Allen, the voice of the Yankees in their heyday, would say, “How about that!”
Dr. Hughes is clinical professor in the department of surgery and director of medical education at the Kansas University School of Medicine, Salina Campus, and Co-Editor of ACS Surgery News.
For all those who say that the surgeon in the trenches doesn’t have a voice in the world of organized surgery, I have a story or two for you.
About 10 or more years ago, I was at a lovely old hotel in Cooperstown, N.Y., listening to a group of elder rural surgery colleagues hold forth about feeling ignored by the American College of Surgeons and how we should all band together to form a new society of rural surgeons. Like most crowds, they were getting pretty worked up. They were pretty sure such a revolution would solve our problems and we would quit being the Rodney Dangerfields of surgery (not getting any respect, as the great comic used to say).
It took a while – a few years – for the rural surgeons and ACS leadership to get to know each other better. We did, however, get there. An Advisory Council was created with the help of some very heavy hitters not often regarded as rural champions, most of whom had roots in the rural world that helped them understand what this group of surgeons wanted and needed.
Not too much removed from this event, many surgeons were feeling isolated in general due to the many challenges of rural practice familiar to so many of us. ACS leadership sensed that surgeons needed to be connected and with considerable effort they formed listservs and found that they were successful to some degree. So, under Dr. David Hoyt’s guidance a better technology was found, resources were committed, and the ACS Communities was launched. A new era in surgeon-to-surgeon and surgeon-to-leadership communication was born. It was as if we had developed talk radio for surgeons. Some stations were loud, others came in rather softly, but all were on the air. The pulse of the Fellows became audible.
Almost simultaneously, dissatisfaction with Maintenance of Certification grew as surgeons in practice began reaching their second and third recertification and the practice of surgery became ever more specialized. Many surgeons believed that nothing would ever change, that the front-line surgeon didn’t have a chance to affect change, and that the big dogs wouldn’t listen. But the College leadership heard the voices of concern and took steps to support a new approach to certification.
So here we are in 2017, coming off a very successful Clinical Congress. The formerly obscure rural surgeon contingent had several panels on the program. Surgeons practicing in towns as small as 3,000 moderated sessions. Some of those sessions were standing room only. The College assisted (and had for a few years) those rural surgeons in organizing a Rural Surgery Dinner, which filled a restaurant full of surgeons delighted to meet in person surgeons from small communities all over the country. They shared their common experiences and planned for a better tomorrow. Later in the week, the 2nd Vice President-Elect was announced. He is a surgeon from Keokuk, IA, and one of the leaders of the rural surgeon movement within the College, Philip Caropreso, MD, FACS. A new Regent was announced: Gary Timmerman, MD, FACS. Dr. Timmerman started his career in Watertown, S.D., and now runs a rural-based surgery training program.
The Clinical Congress program included many topics and issues that Fellows from every branch of surgery had posted about on the ACS Communities. The American Board of Surgery announced sweeping coming changes to help surgeons move on from an MOC system no one was really happy with to one that has great hope of making ongoing certification more than a hoop to jump through, but instead, a real value to the Diplomate. Sitting on the main committee for the American Board of Surgery’s sprint team on certification is a surgeon from Crockett, Texas, Pat Walker, MD, FACS, who practiced surgery “on the ground” in a small community setting for three decades.
Most of us would agree that rural surgeons are facing truly daunting professional headwinds, despite their critical work in serving rural patients. Yet I have been gladdened at the response and respect that the College leadership has given to rural surgeons in recent years. The outreach by the College to support rural surgeons is part of a broader effort to hear every Fellow and make the College more relevant in the life of hard-working surgeons of every type. Changes in how we retain and improve our certification process in some significant ways came out of College efforts to listen and respond to the concerns of Fellows in the College. These and other initiatives by the College leadership show a degree of farsightedness and caring that should be gratifying to all Fellows.
When Lindsay Fox, MD, FACS, a young rural surgeon in private practice with an 8-week-old baby, receives an award for excellence, moderates her panel at the Clinical Congress to a standing-room-only crowd, and then shares her experience through the Communities, I’d say the American College of Surgeons has done an amazing job in a short period of time to make our organization reflect all of us. As Mel Allen, the voice of the Yankees in their heyday, would say, “How about that!”
Dr. Hughes is clinical professor in the department of surgery and director of medical education at the Kansas University School of Medicine, Salina Campus, and Co-Editor of ACS Surgery News.
For all those who say that the surgeon in the trenches doesn’t have a voice in the world of organized surgery, I have a story or two for you.
About 10 or more years ago, I was at a lovely old hotel in Cooperstown, N.Y., listening to a group of elder rural surgery colleagues hold forth about feeling ignored by the American College of Surgeons and how we should all band together to form a new society of rural surgeons. Like most crowds, they were getting pretty worked up. They were pretty sure such a revolution would solve our problems and we would quit being the Rodney Dangerfields of surgery (not getting any respect, as the great comic used to say).
It took a while – a few years – for the rural surgeons and ACS leadership to get to know each other better. We did, however, get there. An Advisory Council was created with the help of some very heavy hitters not often regarded as rural champions, most of whom had roots in the rural world that helped them understand what this group of surgeons wanted and needed.
Not too much removed from this event, many surgeons were feeling isolated in general due to the many challenges of rural practice familiar to so many of us. ACS leadership sensed that surgeons needed to be connected and with considerable effort they formed listservs and found that they were successful to some degree. So, under Dr. David Hoyt’s guidance a better technology was found, resources were committed, and the ACS Communities was launched. A new era in surgeon-to-surgeon and surgeon-to-leadership communication was born. It was as if we had developed talk radio for surgeons. Some stations were loud, others came in rather softly, but all were on the air. The pulse of the Fellows became audible.
Almost simultaneously, dissatisfaction with Maintenance of Certification grew as surgeons in practice began reaching their second and third recertification and the practice of surgery became ever more specialized. Many surgeons believed that nothing would ever change, that the front-line surgeon didn’t have a chance to affect change, and that the big dogs wouldn’t listen. But the College leadership heard the voices of concern and took steps to support a new approach to certification.
So here we are in 2017, coming off a very successful Clinical Congress. The formerly obscure rural surgeon contingent had several panels on the program. Surgeons practicing in towns as small as 3,000 moderated sessions. Some of those sessions were standing room only. The College assisted (and had for a few years) those rural surgeons in organizing a Rural Surgery Dinner, which filled a restaurant full of surgeons delighted to meet in person surgeons from small communities all over the country. They shared their common experiences and planned for a better tomorrow. Later in the week, the 2nd Vice President-Elect was announced. He is a surgeon from Keokuk, IA, and one of the leaders of the rural surgeon movement within the College, Philip Caropreso, MD, FACS. A new Regent was announced: Gary Timmerman, MD, FACS. Dr. Timmerman started his career in Watertown, S.D., and now runs a rural-based surgery training program.
The Clinical Congress program included many topics and issues that Fellows from every branch of surgery had posted about on the ACS Communities. The American Board of Surgery announced sweeping coming changes to help surgeons move on from an MOC system no one was really happy with to one that has great hope of making ongoing certification more than a hoop to jump through, but instead, a real value to the Diplomate. Sitting on the main committee for the American Board of Surgery’s sprint team on certification is a surgeon from Crockett, Texas, Pat Walker, MD, FACS, who practiced surgery “on the ground” in a small community setting for three decades.
Most of us would agree that rural surgeons are facing truly daunting professional headwinds, despite their critical work in serving rural patients. Yet I have been gladdened at the response and respect that the College leadership has given to rural surgeons in recent years. The outreach by the College to support rural surgeons is part of a broader effort to hear every Fellow and make the College more relevant in the life of hard-working surgeons of every type. Changes in how we retain and improve our certification process in some significant ways came out of College efforts to listen and respond to the concerns of Fellows in the College. These and other initiatives by the College leadership show a degree of farsightedness and caring that should be gratifying to all Fellows.
When Lindsay Fox, MD, FACS, a young rural surgeon in private practice with an 8-week-old baby, receives an award for excellence, moderates her panel at the Clinical Congress to a standing-room-only crowd, and then shares her experience through the Communities, I’d say the American College of Surgeons has done an amazing job in a short period of time to make our organization reflect all of us. As Mel Allen, the voice of the Yankees in their heyday, would say, “How about that!”
Dr. Hughes is clinical professor in the department of surgery and director of medical education at the Kansas University School of Medicine, Salina Campus, and Co-Editor of ACS Surgery News.
From the Editors: Halsted, Holmes, and penguins
Is it not ironic that in a profession that is always seeking answers – What does this patient have? Is that mass malignant? What’s the best way to make a diagnosis? – too much information has become a major problem?
Unlike William Stewart Halsted or Theodor Billroth, who blazed surgical trails in an age when much was unknown, today’s surgeons face a jungle of information obscuring the trail ahead. Every morning we wake up to another 30 or 40 unread emails. Journals multiply on our desks. The books we need to read pile up and spill over onto our desks, bookshelves, and side tables. Sometimes, it makes one long for the old days when definitive answers might not be found in the literature. These days, we know it is likely that someone has published exactly what we need at any particular moment, and yet finding it in the jungle of information can be a great challenge.
Another outcome of too much information is the accumulation in our brains of unsorted bits of medical/surgical knowledge. Some of those bits are pearls, and others are just gum wrappers that take up space. It becomes an overwhelming task of ranking, sorting, prioritizing, and discarding.
A friend of mine years of ago called his brain an iceberg on which thousands of penguins stand. The penguins just kept coming and, finally, in order to learn anything new, he had to push some penguins off the iceberg. We have a lot of penguins on our icebergs these days.
This brings to mind many doctors’ favorite fictional character, Sherlock Holmes. That denizen of 221B Baker Street was a master at data management. He always had the right information available in his head relevant for the mystery at hand. How did he do it? Recall that Dr. Watson (a surgeon, I might add) was intermittently shocked by what Holmes didn’t know, to which the tobacco- and opiate-addicted hero would reply that he purposely forgot things that did not help him solve his cases.
And so, what is the modern surgeon – who must keep in the forefront of his or her mind every best practice, algorithm, and guideline – to do in this age of too much information? Like Holmes, we need to sort what is critical from what is not and let go of those items that no longer are germane. We then need to triage the vast amount of information delivered to us yearly, weekly, monthly, daily, hourly. The stream of little notes flashing at you from your black mirror (the screen of your mobile device) needs to be controlled lest it control you.
So, might I suggest a few strategies I have used to triage the flow of information? For hourly and daily information, I tend to ignore everything except ACS NewsScope and the ACS Communities items I find most interesting. For monthly information, I tend to use ACS Surgery News (plug intended) because it is “news” – the stuff that just happened in the meeting sphere or has not yet hit print (sorry, e-publication). The Journal of the American College of Surgeons is another monthly source that is reliable.
You may see a theme here. I’ve used the American College of Surgeons as my main filter. What gets through the editors of these outlets generally is viable and useful information. That’s what I need to know for right now. Such knowledge allows me to push those penguins no longer needed off my iceberg and greet the new ones with joy. We often wonder what the benefit of membership in the College may be. For me, these filters are worth the price of admission.
Dr. Hughes is clinical professor in the department of surgery and director of medical education at the Kansas University School of Medicine, Salina Campus, and Co-Editor of ACS Surgery News.
Is it not ironic that in a profession that is always seeking answers – What does this patient have? Is that mass malignant? What’s the best way to make a diagnosis? – too much information has become a major problem?
Unlike William Stewart Halsted or Theodor Billroth, who blazed surgical trails in an age when much was unknown, today’s surgeons face a jungle of information obscuring the trail ahead. Every morning we wake up to another 30 or 40 unread emails. Journals multiply on our desks. The books we need to read pile up and spill over onto our desks, bookshelves, and side tables. Sometimes, it makes one long for the old days when definitive answers might not be found in the literature. These days, we know it is likely that someone has published exactly what we need at any particular moment, and yet finding it in the jungle of information can be a great challenge.
Another outcome of too much information is the accumulation in our brains of unsorted bits of medical/surgical knowledge. Some of those bits are pearls, and others are just gum wrappers that take up space. It becomes an overwhelming task of ranking, sorting, prioritizing, and discarding.
A friend of mine years of ago called his brain an iceberg on which thousands of penguins stand. The penguins just kept coming and, finally, in order to learn anything new, he had to push some penguins off the iceberg. We have a lot of penguins on our icebergs these days.
This brings to mind many doctors’ favorite fictional character, Sherlock Holmes. That denizen of 221B Baker Street was a master at data management. He always had the right information available in his head relevant for the mystery at hand. How did he do it? Recall that Dr. Watson (a surgeon, I might add) was intermittently shocked by what Holmes didn’t know, to which the tobacco- and opiate-addicted hero would reply that he purposely forgot things that did not help him solve his cases.
And so, what is the modern surgeon – who must keep in the forefront of his or her mind every best practice, algorithm, and guideline – to do in this age of too much information? Like Holmes, we need to sort what is critical from what is not and let go of those items that no longer are germane. We then need to triage the vast amount of information delivered to us yearly, weekly, monthly, daily, hourly. The stream of little notes flashing at you from your black mirror (the screen of your mobile device) needs to be controlled lest it control you.
So, might I suggest a few strategies I have used to triage the flow of information? For hourly and daily information, I tend to ignore everything except ACS NewsScope and the ACS Communities items I find most interesting. For monthly information, I tend to use ACS Surgery News (plug intended) because it is “news” – the stuff that just happened in the meeting sphere or has not yet hit print (sorry, e-publication). The Journal of the American College of Surgeons is another monthly source that is reliable.
You may see a theme here. I’ve used the American College of Surgeons as my main filter. What gets through the editors of these outlets generally is viable and useful information. That’s what I need to know for right now. Such knowledge allows me to push those penguins no longer needed off my iceberg and greet the new ones with joy. We often wonder what the benefit of membership in the College may be. For me, these filters are worth the price of admission.
Dr. Hughes is clinical professor in the department of surgery and director of medical education at the Kansas University School of Medicine, Salina Campus, and Co-Editor of ACS Surgery News.
Is it not ironic that in a profession that is always seeking answers – What does this patient have? Is that mass malignant? What’s the best way to make a diagnosis? – too much information has become a major problem?
Unlike William Stewart Halsted or Theodor Billroth, who blazed surgical trails in an age when much was unknown, today’s surgeons face a jungle of information obscuring the trail ahead. Every morning we wake up to another 30 or 40 unread emails. Journals multiply on our desks. The books we need to read pile up and spill over onto our desks, bookshelves, and side tables. Sometimes, it makes one long for the old days when definitive answers might not be found in the literature. These days, we know it is likely that someone has published exactly what we need at any particular moment, and yet finding it in the jungle of information can be a great challenge.
Another outcome of too much information is the accumulation in our brains of unsorted bits of medical/surgical knowledge. Some of those bits are pearls, and others are just gum wrappers that take up space. It becomes an overwhelming task of ranking, sorting, prioritizing, and discarding.
A friend of mine years of ago called his brain an iceberg on which thousands of penguins stand. The penguins just kept coming and, finally, in order to learn anything new, he had to push some penguins off the iceberg. We have a lot of penguins on our icebergs these days.
This brings to mind many doctors’ favorite fictional character, Sherlock Holmes. That denizen of 221B Baker Street was a master at data management. He always had the right information available in his head relevant for the mystery at hand. How did he do it? Recall that Dr. Watson (a surgeon, I might add) was intermittently shocked by what Holmes didn’t know, to which the tobacco- and opiate-addicted hero would reply that he purposely forgot things that did not help him solve his cases.
And so, what is the modern surgeon – who must keep in the forefront of his or her mind every best practice, algorithm, and guideline – to do in this age of too much information? Like Holmes, we need to sort what is critical from what is not and let go of those items that no longer are germane. We then need to triage the vast amount of information delivered to us yearly, weekly, monthly, daily, hourly. The stream of little notes flashing at you from your black mirror (the screen of your mobile device) needs to be controlled lest it control you.
So, might I suggest a few strategies I have used to triage the flow of information? For hourly and daily information, I tend to ignore everything except ACS NewsScope and the ACS Communities items I find most interesting. For monthly information, I tend to use ACS Surgery News (plug intended) because it is “news” – the stuff that just happened in the meeting sphere or has not yet hit print (sorry, e-publication). The Journal of the American College of Surgeons is another monthly source that is reliable.
You may see a theme here. I’ve used the American College of Surgeons as my main filter. What gets through the editors of these outlets generally is viable and useful information. That’s what I need to know for right now. Such knowledge allows me to push those penguins no longer needed off my iceberg and greet the new ones with joy. We often wonder what the benefit of membership in the College may be. For me, these filters are worth the price of admission.
Dr. Hughes is clinical professor in the department of surgery and director of medical education at the Kansas University School of Medicine, Salina Campus, and Co-Editor of ACS Surgery News.
From the Editors: Your call is important to us
There they were – dropping like a stone toward the lunar surface some 48 years ago. Buzz Aldrin looked at his onboard computer and it reported Error 1202, and alarms started going off in the Lunar Module. Fortunately for Neil Armstrong and Buzz Aldrin, they had a healthy relationship with their computer systems and IT support. Mission control was only 1.5 seconds away and had a huge team of experts that told them they could ignore the error message. The rest is, of course, history. Human beings, not computer software, landed the Eagle. They used their own judgment and experience and data provided by the computer to make their landing decisions.
At 25,000 feet Mission Control answers. Buzz describes the error code. Mission Control reports that his computer is made by Grumman and that Mission Control uses Lockheed-based software. He is advised to call the Grumman help line. At 15,000 feet Grumman responds. They report that Buzz’s password expired about the time the lunar descent burn occurred. He needs to put in a new password and confirm it. He will receive a confirmation email within the next 24 hours. Neil is getting increasingly restive despite his famously bland emotional responses in crises.
At 10,000 feet Buzz gets a new password confirmation, but Error 1202 remains on the display. The moon is enormous in the windshield. Grumman support responds that the error is likely because Buzz put in the wrong weight for the Lunar Module. Buzz begins again feeding in the data to the onboard computer. Grumman suggests that had Buzz simply created the right template, this problem would not have occurred. Buzz, through gritted teeth, asks how he was supposed to create a template for a problem that no one seemed to expect.
They are down to 150 feet now. Neil tells Buzz what he thinks of the computer systems and is told by Mission Control his microphone is hot and that such comments are not appropriate. At Mission Control, a notation is made on their system that Neil will need to discuss this pilot error with the astronaut office upon his return. Neil simply turns off the onboard computer and lands the Lunar Module with seconds of fuel left as he avoids a large boulder field and finds just the right spot. Tranquility Base reports in to Mission Control. Mankind has landed on the Moon.
The alternative history is what surgeons are experiencing every day because of the unhealthy relationship existing between American health care today and our institutional computer systems. Like Neil and Buzz, these surgeons are heroes who avoid boulder fields despite so many obstacles unrelated to their missions. No wonder burnout (a missile term) is so prevalent. We’ve gone from inconvenient to intolerable. Our health care computer systems must be interoperable to have any meaningful use. Our formats need to be understandable. Surgeons need computers to help them make judgments based on easily accessible data in real time. Surgeons need to “fly” the missions and computer systems need to be our servants, not our masters.
Dr. Hughes is clinical professor in the department of surgery and director of medical education at the Kansas University School of Medicine, Salina Campus, and Co-Editor of ACS Surgery News.
There they were – dropping like a stone toward the lunar surface some 48 years ago. Buzz Aldrin looked at his onboard computer and it reported Error 1202, and alarms started going off in the Lunar Module. Fortunately for Neil Armstrong and Buzz Aldrin, they had a healthy relationship with their computer systems and IT support. Mission control was only 1.5 seconds away and had a huge team of experts that told them they could ignore the error message. The rest is, of course, history. Human beings, not computer software, landed the Eagle. They used their own judgment and experience and data provided by the computer to make their landing decisions.
At 25,000 feet Mission Control answers. Buzz describes the error code. Mission Control reports that his computer is made by Grumman and that Mission Control uses Lockheed-based software. He is advised to call the Grumman help line. At 15,000 feet Grumman responds. They report that Buzz’s password expired about the time the lunar descent burn occurred. He needs to put in a new password and confirm it. He will receive a confirmation email within the next 24 hours. Neil is getting increasingly restive despite his famously bland emotional responses in crises.
At 10,000 feet Buzz gets a new password confirmation, but Error 1202 remains on the display. The moon is enormous in the windshield. Grumman support responds that the error is likely because Buzz put in the wrong weight for the Lunar Module. Buzz begins again feeding in the data to the onboard computer. Grumman suggests that had Buzz simply created the right template, this problem would not have occurred. Buzz, through gritted teeth, asks how he was supposed to create a template for a problem that no one seemed to expect.
They are down to 150 feet now. Neil tells Buzz what he thinks of the computer systems and is told by Mission Control his microphone is hot and that such comments are not appropriate. At Mission Control, a notation is made on their system that Neil will need to discuss this pilot error with the astronaut office upon his return. Neil simply turns off the onboard computer and lands the Lunar Module with seconds of fuel left as he avoids a large boulder field and finds just the right spot. Tranquility Base reports in to Mission Control. Mankind has landed on the Moon.
The alternative history is what surgeons are experiencing every day because of the unhealthy relationship existing between American health care today and our institutional computer systems. Like Neil and Buzz, these surgeons are heroes who avoid boulder fields despite so many obstacles unrelated to their missions. No wonder burnout (a missile term) is so prevalent. We’ve gone from inconvenient to intolerable. Our health care computer systems must be interoperable to have any meaningful use. Our formats need to be understandable. Surgeons need computers to help them make judgments based on easily accessible data in real time. Surgeons need to “fly” the missions and computer systems need to be our servants, not our masters.
Dr. Hughes is clinical professor in the department of surgery and director of medical education at the Kansas University School of Medicine, Salina Campus, and Co-Editor of ACS Surgery News.
There they were – dropping like a stone toward the lunar surface some 48 years ago. Buzz Aldrin looked at his onboard computer and it reported Error 1202, and alarms started going off in the Lunar Module. Fortunately for Neil Armstrong and Buzz Aldrin, they had a healthy relationship with their computer systems and IT support. Mission control was only 1.5 seconds away and had a huge team of experts that told them they could ignore the error message. The rest is, of course, history. Human beings, not computer software, landed the Eagle. They used their own judgment and experience and data provided by the computer to make their landing decisions.
At 25,000 feet Mission Control answers. Buzz describes the error code. Mission Control reports that his computer is made by Grumman and that Mission Control uses Lockheed-based software. He is advised to call the Grumman help line. At 15,000 feet Grumman responds. They report that Buzz’s password expired about the time the lunar descent burn occurred. He needs to put in a new password and confirm it. He will receive a confirmation email within the next 24 hours. Neil is getting increasingly restive despite his famously bland emotional responses in crises.
At 10,000 feet Buzz gets a new password confirmation, but Error 1202 remains on the display. The moon is enormous in the windshield. Grumman support responds that the error is likely because Buzz put in the wrong weight for the Lunar Module. Buzz begins again feeding in the data to the onboard computer. Grumman suggests that had Buzz simply created the right template, this problem would not have occurred. Buzz, through gritted teeth, asks how he was supposed to create a template for a problem that no one seemed to expect.
They are down to 150 feet now. Neil tells Buzz what he thinks of the computer systems and is told by Mission Control his microphone is hot and that such comments are not appropriate. At Mission Control, a notation is made on their system that Neil will need to discuss this pilot error with the astronaut office upon his return. Neil simply turns off the onboard computer and lands the Lunar Module with seconds of fuel left as he avoids a large boulder field and finds just the right spot. Tranquility Base reports in to Mission Control. Mankind has landed on the Moon.
The alternative history is what surgeons are experiencing every day because of the unhealthy relationship existing between American health care today and our institutional computer systems. Like Neil and Buzz, these surgeons are heroes who avoid boulder fields despite so many obstacles unrelated to their missions. No wonder burnout (a missile term) is so prevalent. We’ve gone from inconvenient to intolerable. Our health care computer systems must be interoperable to have any meaningful use. Our formats need to be understandable. Surgeons need computers to help them make judgments based on easily accessible data in real time. Surgeons need to “fly” the missions and computer systems need to be our servants, not our masters.
Dr. Hughes is clinical professor in the department of surgery and director of medical education at the Kansas University School of Medicine, Salina Campus, and Co-Editor of ACS Surgery News.
Three days in the life of a surgeon
By sheer happenstance, I was visiting a surgery program on the day after “the Match.” As all of you know, four days before the official release of the placement of every new surgical trainee, both the medical students involved and the programs affected are informed as to whether they have been matched. Students don’t know where they are going, just that the last rung of training is now in place. They have a job and a relatively secure future. Those who have not been matched and those programs that did not fill all their slots now enter into a scramble (officially called SOAP) to find students for the remaining slots. This year, the scramble occurred on a Wednesday and was orchestrated by a set of rules I’d never been privy to before.
On Tuesday night, all the programs in need of students for their open slots, whether categorical or preliminary, looked over the list of candidates remaining and made their choices. So did the students now hoping to find a place. At 10 a.m., the offers went out to students in the first round. Next, in precisely timed order, the programs found out who had accepted the offers. And, if slots were left over, the programs had a short time to put up another set of offers – and so on throughout the day until all the slots were gone. Like a game of musical chairs, the music finally stopped and the Match was over for the entering class of residents for 2017.
Dr. Hughes is clinical professor in the department of surgery and director of medical education at the Kansas University School of Medicine, Salina Campus, and coeditor of ACS Surgery News.
By sheer happenstance, I was visiting a surgery program on the day after “the Match.” As all of you know, four days before the official release of the placement of every new surgical trainee, both the medical students involved and the programs affected are informed as to whether they have been matched. Students don’t know where they are going, just that the last rung of training is now in place. They have a job and a relatively secure future. Those who have not been matched and those programs that did not fill all their slots now enter into a scramble (officially called SOAP) to find students for the remaining slots. This year, the scramble occurred on a Wednesday and was orchestrated by a set of rules I’d never been privy to before.
On Tuesday night, all the programs in need of students for their open slots, whether categorical or preliminary, looked over the list of candidates remaining and made their choices. So did the students now hoping to find a place. At 10 a.m., the offers went out to students in the first round. Next, in precisely timed order, the programs found out who had accepted the offers. And, if slots were left over, the programs had a short time to put up another set of offers – and so on throughout the day until all the slots were gone. Like a game of musical chairs, the music finally stopped and the Match was over for the entering class of residents for 2017.
Dr. Hughes is clinical professor in the department of surgery and director of medical education at the Kansas University School of Medicine, Salina Campus, and coeditor of ACS Surgery News.
By sheer happenstance, I was visiting a surgery program on the day after “the Match.” As all of you know, four days before the official release of the placement of every new surgical trainee, both the medical students involved and the programs affected are informed as to whether they have been matched. Students don’t know where they are going, just that the last rung of training is now in place. They have a job and a relatively secure future. Those who have not been matched and those programs that did not fill all their slots now enter into a scramble (officially called SOAP) to find students for the remaining slots. This year, the scramble occurred on a Wednesday and was orchestrated by a set of rules I’d never been privy to before.
On Tuesday night, all the programs in need of students for their open slots, whether categorical or preliminary, looked over the list of candidates remaining and made their choices. So did the students now hoping to find a place. At 10 a.m., the offers went out to students in the first round. Next, in precisely timed order, the programs found out who had accepted the offers. And, if slots were left over, the programs had a short time to put up another set of offers – and so on throughout the day until all the slots were gone. Like a game of musical chairs, the music finally stopped and the Match was over for the entering class of residents for 2017.
Dr. Hughes is clinical professor in the department of surgery and director of medical education at the Kansas University School of Medicine, Salina Campus, and coeditor of ACS Surgery News.
Music in the OR
I am sure that even though Theodor Billroth and Johannes Brahms were close friends, Billroth never listened to music in his operating room. I’m pretty sure because the Victrola was invented around 1906 and the first commercial radio broadcast was in 1920. So unless Billroth hired a Viennese string quartet to play in his amphitheater, it is likely the operating room was a pretty quiet place.
Radios were the size of a small refrigerator into the 1940s when Bell Laboratories’ invention of the transistor technology permitted small units to play tinny music through speakers about 2 inches across. So, I would guess that Alfred Blalock didn’t listen to Elvis Presley or Buddy Holly during his pioneering days at Hopkins.
By the late 1960s high-quality, recorded music was available on 8-track tapes invented by the Lear Jet Corporation. Music at that point was literally available everywhere and the OR became a theater once more for some surgeons. Cassette tapes followed, and Johnny Paycheck echoed in the heart room where I trained in Dallas – usually at high volume. When Apple changed the world with the iPod in 2001 and then the Internet streaming services emerged, it became possible to take out a gall bladder accompanied by Vladimir Horowitz or Madonna. And it happens routinely.
As I write this, I am listening to a jazz streaming station. Music is one of the most important elements of my life. Yet, my operating room has had music on only one occasion since I became an attending surgeon. I love music too much for it to be in my OR. It not only relaxes me, which may not be entirely a good thing in surgery, but it engages my intellect, taking up needed CPU time which might be useful in avoiding catastrophe for the patient before me.
Not long ago this subject was the focus of a discussion thread on the ACS Communities. Many reported that they never listen to music in the OR, others said it was essential to their performance, and still others took a middle ground. Everyone said the music shouldn’t be loud; however, I can recall visiting a number of operating rooms in which loud was the standard volume setting. Most respondents spoke in terms of what they needed and like. Several felt that as captain of the SS Operating Room they had the final say of whether, what, and when music would be played.
I noted in the conversation justification, defensiveness, authoritarianism mixed with personal insight that is so characteristic of many surgeons. Of course, there isn’t a “right” answer here any more than there is in a number of OR traditions. The evidence is all over the place except when it comes to volume. There, it is clear that loud music causes or exacerbates communications errors due to inability of the OR team to hear one another or distraction of the team from their primary task.
Music affects everyone in the OR. It represents one of many operating room components that hold the potential of both betterment of care or endangerment of the patient. To say that music in the OR is wrong is like saying propellers on aircraft are somehow wrong. Among the most serious injuries at general aviation airports is individuals walking into a spinning propeller; however, without the propeller the plane can’t fly and deliver its benefits enjoyed at large. The problem isn’t that propellers are evil. It is that they are invisible to the victim who ignores their dangers.
My point is that music is an example of the need for us to be aware of the primary and secondary effects of even the small things we do in the OR because innocuous as they seem, they have potential dangers. The Council on Surgical and Perioperative Care of which the ACS is a member, has more data and resources on their homepage (cspsteam.org) for those interested in the subject on distractions in the OR.
So, what I’ve learned through listening to the music of my colleagues opinions is that when it comes to music, we need to be aware of the spinning propeller of noise pollution in the OR. Many invisible dangers inhabit the OR. Take a moment and listen for them.
Dr. Hughes is clinical professor in the department of surgery and director of medical education at the Kansas University School of Medicine, Salina Campus, and Co-Editor of ACS Surgery News.
I am sure that even though Theodor Billroth and Johannes Brahms were close friends, Billroth never listened to music in his operating room. I’m pretty sure because the Victrola was invented around 1906 and the first commercial radio broadcast was in 1920. So unless Billroth hired a Viennese string quartet to play in his amphitheater, it is likely the operating room was a pretty quiet place.
Radios were the size of a small refrigerator into the 1940s when Bell Laboratories’ invention of the transistor technology permitted small units to play tinny music through speakers about 2 inches across. So, I would guess that Alfred Blalock didn’t listen to Elvis Presley or Buddy Holly during his pioneering days at Hopkins.
By the late 1960s high-quality, recorded music was available on 8-track tapes invented by the Lear Jet Corporation. Music at that point was literally available everywhere and the OR became a theater once more for some surgeons. Cassette tapes followed, and Johnny Paycheck echoed in the heart room where I trained in Dallas – usually at high volume. When Apple changed the world with the iPod in 2001 and then the Internet streaming services emerged, it became possible to take out a gall bladder accompanied by Vladimir Horowitz or Madonna. And it happens routinely.
As I write this, I am listening to a jazz streaming station. Music is one of the most important elements of my life. Yet, my operating room has had music on only one occasion since I became an attending surgeon. I love music too much for it to be in my OR. It not only relaxes me, which may not be entirely a good thing in surgery, but it engages my intellect, taking up needed CPU time which might be useful in avoiding catastrophe for the patient before me.
Not long ago this subject was the focus of a discussion thread on the ACS Communities. Many reported that they never listen to music in the OR, others said it was essential to their performance, and still others took a middle ground. Everyone said the music shouldn’t be loud; however, I can recall visiting a number of operating rooms in which loud was the standard volume setting. Most respondents spoke in terms of what they needed and like. Several felt that as captain of the SS Operating Room they had the final say of whether, what, and when music would be played.
I noted in the conversation justification, defensiveness, authoritarianism mixed with personal insight that is so characteristic of many surgeons. Of course, there isn’t a “right” answer here any more than there is in a number of OR traditions. The evidence is all over the place except when it comes to volume. There, it is clear that loud music causes or exacerbates communications errors due to inability of the OR team to hear one another or distraction of the team from their primary task.
Music affects everyone in the OR. It represents one of many operating room components that hold the potential of both betterment of care or endangerment of the patient. To say that music in the OR is wrong is like saying propellers on aircraft are somehow wrong. Among the most serious injuries at general aviation airports is individuals walking into a spinning propeller; however, without the propeller the plane can’t fly and deliver its benefits enjoyed at large. The problem isn’t that propellers are evil. It is that they are invisible to the victim who ignores their dangers.
My point is that music is an example of the need for us to be aware of the primary and secondary effects of even the small things we do in the OR because innocuous as they seem, they have potential dangers. The Council on Surgical and Perioperative Care of which the ACS is a member, has more data and resources on their homepage (cspsteam.org) for those interested in the subject on distractions in the OR.
So, what I’ve learned through listening to the music of my colleagues opinions is that when it comes to music, we need to be aware of the spinning propeller of noise pollution in the OR. Many invisible dangers inhabit the OR. Take a moment and listen for them.
Dr. Hughes is clinical professor in the department of surgery and director of medical education at the Kansas University School of Medicine, Salina Campus, and Co-Editor of ACS Surgery News.
I am sure that even though Theodor Billroth and Johannes Brahms were close friends, Billroth never listened to music in his operating room. I’m pretty sure because the Victrola was invented around 1906 and the first commercial radio broadcast was in 1920. So unless Billroth hired a Viennese string quartet to play in his amphitheater, it is likely the operating room was a pretty quiet place.
Radios were the size of a small refrigerator into the 1940s when Bell Laboratories’ invention of the transistor technology permitted small units to play tinny music through speakers about 2 inches across. So, I would guess that Alfred Blalock didn’t listen to Elvis Presley or Buddy Holly during his pioneering days at Hopkins.
By the late 1960s high-quality, recorded music was available on 8-track tapes invented by the Lear Jet Corporation. Music at that point was literally available everywhere and the OR became a theater once more for some surgeons. Cassette tapes followed, and Johnny Paycheck echoed in the heart room where I trained in Dallas – usually at high volume. When Apple changed the world with the iPod in 2001 and then the Internet streaming services emerged, it became possible to take out a gall bladder accompanied by Vladimir Horowitz or Madonna. And it happens routinely.
As I write this, I am listening to a jazz streaming station. Music is one of the most important elements of my life. Yet, my operating room has had music on only one occasion since I became an attending surgeon. I love music too much for it to be in my OR. It not only relaxes me, which may not be entirely a good thing in surgery, but it engages my intellect, taking up needed CPU time which might be useful in avoiding catastrophe for the patient before me.
Not long ago this subject was the focus of a discussion thread on the ACS Communities. Many reported that they never listen to music in the OR, others said it was essential to their performance, and still others took a middle ground. Everyone said the music shouldn’t be loud; however, I can recall visiting a number of operating rooms in which loud was the standard volume setting. Most respondents spoke in terms of what they needed and like. Several felt that as captain of the SS Operating Room they had the final say of whether, what, and when music would be played.
I noted in the conversation justification, defensiveness, authoritarianism mixed with personal insight that is so characteristic of many surgeons. Of course, there isn’t a “right” answer here any more than there is in a number of OR traditions. The evidence is all over the place except when it comes to volume. There, it is clear that loud music causes or exacerbates communications errors due to inability of the OR team to hear one another or distraction of the team from their primary task.
Music affects everyone in the OR. It represents one of many operating room components that hold the potential of both betterment of care or endangerment of the patient. To say that music in the OR is wrong is like saying propellers on aircraft are somehow wrong. Among the most serious injuries at general aviation airports is individuals walking into a spinning propeller; however, without the propeller the plane can’t fly and deliver its benefits enjoyed at large. The problem isn’t that propellers are evil. It is that they are invisible to the victim who ignores their dangers.
My point is that music is an example of the need for us to be aware of the primary and secondary effects of even the small things we do in the OR because innocuous as they seem, they have potential dangers. The Council on Surgical and Perioperative Care of which the ACS is a member, has more data and resources on their homepage (cspsteam.org) for those interested in the subject on distractions in the OR.
So, what I’ve learned through listening to the music of my colleagues opinions is that when it comes to music, we need to be aware of the spinning propeller of noise pollution in the OR. Many invisible dangers inhabit the OR. Take a moment and listen for them.
Dr. Hughes is clinical professor in the department of surgery and director of medical education at the Kansas University School of Medicine, Salina Campus, and Co-Editor of ACS Surgery News.
From the Editors: One pebble at a time
This is a story about Sarah Prince, FRCS, and thousands of others here and abroad who are surgeons. Only a few of you may have heard of Miss Prince, consultant surgeon from Fort William, Scotland; but she represents to me one of thousands of stories that make surgery such a rich subject that spans more than pure science. Sarah achieved immortality in what she accomplished in 43 short years.
Sarah was trained in the United Kingdom system, attaining specialty training in hepatobiliary disease. While she loved that sort of work she decided, with her internist husband Patrick Byrne, to work in a rural town in northern Scotland. In nine years she built up the hospital there and its training paradigm. She went on to work toward creating a better rural surgical system in Scotland, eventually becoming an expert who spoke all over the world about rural surgery and allocating resources to build surgical capacity in rural areas. She understood the volume debate and the need for rural surgeons to have a connection that was substantive with a larger center in a collaborative way benefiting both locales.
I bring her up because she represents something we all can do. A few surgeons become academic giants known far and wide, but all surgeons have the ability to be local giants, unknown but immortal and essential in their own way. Sarah’s accomplishments confirm that.
Unlike surgery in the United States, the U.K. system is more regimented in many ways and even more political than what the average U.S. surgeon experiences. It is a single-payer system that was there long before Sarah became a surgeon and will be there long after. The fact that the system into which she was born was not of her making did not deter Sarah from taking on that very system to make her corner of the world a better place. I was always surprised when speaking with her that the problems she faced in Scotland were much the same as what I’ve seen in rural surgery in the United States and in other countries. She didn’t bend the whole system but she made a significant dent in how things were done. Isn’t that the challenge for us all?
Recently on the ACS Communities and elsewhere, the debate on single-payer, multitier, and market-driven health care is being argued. In light of the current political environment, the path forward seems bewilderingly tangled. Most surgeons just want to operate. The OR may be the last bastion of control we surgeons have in our professional lives. There may be a barrage of obstacles getting to the OR and hordes of explanations and details postoperatively, but in the OR we still get to do what we think is best at the moment using all those skills we so painfully acquired during a career of learning and practice. To despair is easy until one takes a look at what so many surgeons achieve in their lives.
Like Sarah, most of us try to make the profession a little better. In small town Iowa, that may be getting sonography privileges for FAST exams that improves the lot of trauma patients in that town. In an exburbia hospital, the surgeon may bring new expertise not previously available. It goes on and on with each of us contributing one pebble at a time to a mountain of effort. Any one pebble seems so insignificant in itself and sometimes just placing it on the mountain takes enormous effort, but each is worth the toil to put it there.
Which brings us back to Miss Prince (it is a faux pas to call a consultant surgeon in the U.K. by the honorific doctor). Sarah faced just as many challenges and perhaps more than surgeons elsewhere. Yet she brought her best every day to her hospital until cruel fate delivered her a fatal blow at a young age. Even then facing her imminent death, Sarah made sure that her patients and trainees would be well cared for after her passing. Her indomitable approach to surgical life shows that no matter what the opposition, a surgeon can with grit and wit make life better in his or her town, region, and maybe even the world.
As we face 2017 with all its potential for defeat or victory for our patients, let us remember surgeons like Sarah Prince who made a difference and commit ourselves to the same goal. We can do it one pebble at a time until we’ve created a mountain of accomplishment.
Dr. Hughes is clinical professor in the department of surgery and director of medical education at the Kansas University School of Medicine, Salina Campus, and Co-Editor of ACS Surgery News.
This is a story about Sarah Prince, FRCS, and thousands of others here and abroad who are surgeons. Only a few of you may have heard of Miss Prince, consultant surgeon from Fort William, Scotland; but she represents to me one of thousands of stories that make surgery such a rich subject that spans more than pure science. Sarah achieved immortality in what she accomplished in 43 short years.
Sarah was trained in the United Kingdom system, attaining specialty training in hepatobiliary disease. While she loved that sort of work she decided, with her internist husband Patrick Byrne, to work in a rural town in northern Scotland. In nine years she built up the hospital there and its training paradigm. She went on to work toward creating a better rural surgical system in Scotland, eventually becoming an expert who spoke all over the world about rural surgery and allocating resources to build surgical capacity in rural areas. She understood the volume debate and the need for rural surgeons to have a connection that was substantive with a larger center in a collaborative way benefiting both locales.
I bring her up because she represents something we all can do. A few surgeons become academic giants known far and wide, but all surgeons have the ability to be local giants, unknown but immortal and essential in their own way. Sarah’s accomplishments confirm that.
Unlike surgery in the United States, the U.K. system is more regimented in many ways and even more political than what the average U.S. surgeon experiences. It is a single-payer system that was there long before Sarah became a surgeon and will be there long after. The fact that the system into which she was born was not of her making did not deter Sarah from taking on that very system to make her corner of the world a better place. I was always surprised when speaking with her that the problems she faced in Scotland were much the same as what I’ve seen in rural surgery in the United States and in other countries. She didn’t bend the whole system but she made a significant dent in how things were done. Isn’t that the challenge for us all?
Recently on the ACS Communities and elsewhere, the debate on single-payer, multitier, and market-driven health care is being argued. In light of the current political environment, the path forward seems bewilderingly tangled. Most surgeons just want to operate. The OR may be the last bastion of control we surgeons have in our professional lives. There may be a barrage of obstacles getting to the OR and hordes of explanations and details postoperatively, but in the OR we still get to do what we think is best at the moment using all those skills we so painfully acquired during a career of learning and practice. To despair is easy until one takes a look at what so many surgeons achieve in their lives.
Like Sarah, most of us try to make the profession a little better. In small town Iowa, that may be getting sonography privileges for FAST exams that improves the lot of trauma patients in that town. In an exburbia hospital, the surgeon may bring new expertise not previously available. It goes on and on with each of us contributing one pebble at a time to a mountain of effort. Any one pebble seems so insignificant in itself and sometimes just placing it on the mountain takes enormous effort, but each is worth the toil to put it there.
Which brings us back to Miss Prince (it is a faux pas to call a consultant surgeon in the U.K. by the honorific doctor). Sarah faced just as many challenges and perhaps more than surgeons elsewhere. Yet she brought her best every day to her hospital until cruel fate delivered her a fatal blow at a young age. Even then facing her imminent death, Sarah made sure that her patients and trainees would be well cared for after her passing. Her indomitable approach to surgical life shows that no matter what the opposition, a surgeon can with grit and wit make life better in his or her town, region, and maybe even the world.
As we face 2017 with all its potential for defeat or victory for our patients, let us remember surgeons like Sarah Prince who made a difference and commit ourselves to the same goal. We can do it one pebble at a time until we’ve created a mountain of accomplishment.
Dr. Hughes is clinical professor in the department of surgery and director of medical education at the Kansas University School of Medicine, Salina Campus, and Co-Editor of ACS Surgery News.
This is a story about Sarah Prince, FRCS, and thousands of others here and abroad who are surgeons. Only a few of you may have heard of Miss Prince, consultant surgeon from Fort William, Scotland; but she represents to me one of thousands of stories that make surgery such a rich subject that spans more than pure science. Sarah achieved immortality in what she accomplished in 43 short years.
Sarah was trained in the United Kingdom system, attaining specialty training in hepatobiliary disease. While she loved that sort of work she decided, with her internist husband Patrick Byrne, to work in a rural town in northern Scotland. In nine years she built up the hospital there and its training paradigm. She went on to work toward creating a better rural surgical system in Scotland, eventually becoming an expert who spoke all over the world about rural surgery and allocating resources to build surgical capacity in rural areas. She understood the volume debate and the need for rural surgeons to have a connection that was substantive with a larger center in a collaborative way benefiting both locales.
I bring her up because she represents something we all can do. A few surgeons become academic giants known far and wide, but all surgeons have the ability to be local giants, unknown but immortal and essential in their own way. Sarah’s accomplishments confirm that.
Unlike surgery in the United States, the U.K. system is more regimented in many ways and even more political than what the average U.S. surgeon experiences. It is a single-payer system that was there long before Sarah became a surgeon and will be there long after. The fact that the system into which she was born was not of her making did not deter Sarah from taking on that very system to make her corner of the world a better place. I was always surprised when speaking with her that the problems she faced in Scotland were much the same as what I’ve seen in rural surgery in the United States and in other countries. She didn’t bend the whole system but she made a significant dent in how things were done. Isn’t that the challenge for us all?
Recently on the ACS Communities and elsewhere, the debate on single-payer, multitier, and market-driven health care is being argued. In light of the current political environment, the path forward seems bewilderingly tangled. Most surgeons just want to operate. The OR may be the last bastion of control we surgeons have in our professional lives. There may be a barrage of obstacles getting to the OR and hordes of explanations and details postoperatively, but in the OR we still get to do what we think is best at the moment using all those skills we so painfully acquired during a career of learning and practice. To despair is easy until one takes a look at what so many surgeons achieve in their lives.
Like Sarah, most of us try to make the profession a little better. In small town Iowa, that may be getting sonography privileges for FAST exams that improves the lot of trauma patients in that town. In an exburbia hospital, the surgeon may bring new expertise not previously available. It goes on and on with each of us contributing one pebble at a time to a mountain of effort. Any one pebble seems so insignificant in itself and sometimes just placing it on the mountain takes enormous effort, but each is worth the toil to put it there.
Which brings us back to Miss Prince (it is a faux pas to call a consultant surgeon in the U.K. by the honorific doctor). Sarah faced just as many challenges and perhaps more than surgeons elsewhere. Yet she brought her best every day to her hospital until cruel fate delivered her a fatal blow at a young age. Even then facing her imminent death, Sarah made sure that her patients and trainees would be well cared for after her passing. Her indomitable approach to surgical life shows that no matter what the opposition, a surgeon can with grit and wit make life better in his or her town, region, and maybe even the world.
As we face 2017 with all its potential for defeat or victory for our patients, let us remember surgeons like Sarah Prince who made a difference and commit ourselves to the same goal. We can do it one pebble at a time until we’ve created a mountain of accomplishment.
Dr. Hughes is clinical professor in the department of surgery and director of medical education at the Kansas University School of Medicine, Salina Campus, and Co-Editor of ACS Surgery News.