User login
Cultivating competencies for value-based care
It is my privilege this month to assume responsibility for the “Practice Management: The Road Ahead” section of Clinical Gastroenterology and Hepatology. I am honored to join an impressive board of editors led by Dr Fasiha Kanwal, and anchored by global leaders in the field of gastroenterology and hepatology. This board of editors promises to continue the high level of excellence that has propelled the journal to its preeminent position among clinical journals. I am confident that the practice management section will uphold that tradition and continue to meet the expectation of our readers. I would like to mark this transition by acknowledging the history of the practice management section of Clinical Gastroenterology and Hepatology and outlining a vision for the future.
The section was introduced in 2010 under the leadership of Dr. Joel V. Brill. The section, titled “Practice Management: Opportunities and Challenges,” aimed to help practices navigate the disparate issues facing the field. Some of these issues included use of capnography in endoscopy, the importance of registries for quality reporting, and the burdens of meaningful use on physician practices. Dr Brill introduced this section in a video in May 2010 (https://www.youtube.com/watch?v=8FMsc2Wl5E8). Dr. Brill’s reference to these “interesting and challenging times” in gastroenterology resonates even more loudly today.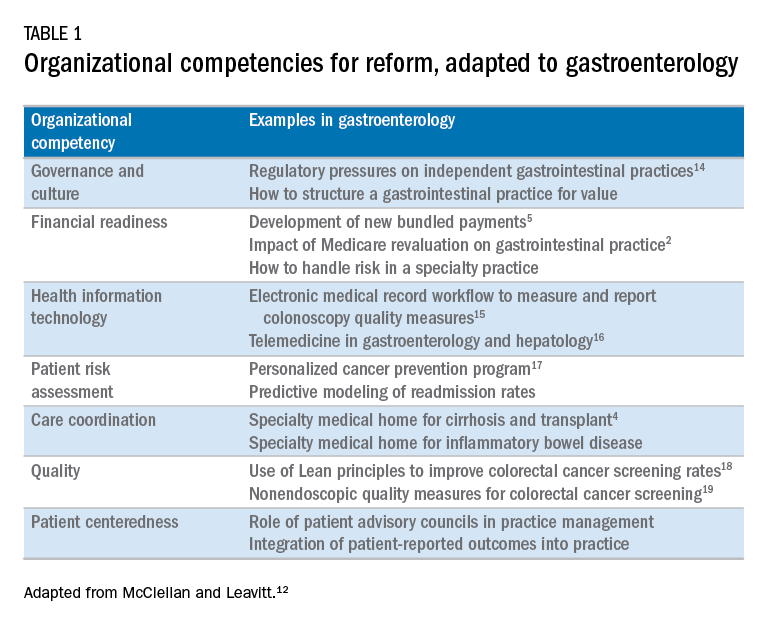
Over the next 5 years, the Road Ahead section will continue and strengthen its focus on the current and emerging issues facing gastroenterology and hepatology practices. I believe that high-value care will continue to be a high priority for patients and payers alike. Early results with payment reform around value have been mixed, in large part because of challenges in health systems and practices developing the competencies required for such reform.12 These competencies include governance and culture, financial readiness, health information technology, patient risk assessment, care coordination, quality, and patient centeredness. I will use this conceptual framework of organizational competencies, and their application in gastroenterology and hepatology, to help curate the Road Ahead section (Table 1). Key themes will include the following:
- • Governance and culture: The structure of health delivery systems, as conceptualized by Donabedian,13 is a key determinant of quality. Structural attributes include regulatory requirements on gastrointestinal practices, such as the rules governing use of anesthesia providers in ambulatory surgical settings; role of allied health professionals in clinical settings; and the impact of financial incentives in driving provider behavior.
- • Financial readiness: Value-based reimbursement, accountable care, medical homes, reference pricing, and physician tiering are some of the new terms in this era of value-based medicine. It is important for practices to assess patient costs longitudinally and manage financial risks. The Road Ahead section will continue to include papers that describe the impact of these reforms on gastroenterology and hepatology practices while providing guidance on implementation of these new models of care. Some examples include papers on the effect of payment policy on specialty practices, the development of a medical home in inflammatory bowel disease, and the physician experience with episode-based payments for colonoscopy.
- • Health information technology: All of the organizational competencies required for reform rely on a robust information technology platform that collects meaningful data and harnesses that data for analytic purposes. These platforms can be enterprise systems deployed by large health delivery systems or smaller, more nimble platforms, created by innovative start-up companies. The Road Ahead will include papers that share best practices in the use of these platforms to provide high-quality and cost-efficient care. In addition, the Road Ahead will continue to explore the use of health information technology to expand the reach of clinicians beyond brick and mortar clinics.
- • Patient risk assessment: Tailoring interventions to high-risk patients is necessary to deploy limited resources in a cost-effective manner. Risk assessment is also needed to more accurately and effectively personalize care for patients with chronic conditions. The Road Ahead will include papers that evaluate risk assessment tools and/or describe real-life implementation of these tools in different contexts.
- • Care coordination: The ability to provide team-based longitudinal care across the continuum of care will be integral to providing high value health care. The Road Ahead will serve as a means to disseminate best practices and innovative methods to care for increasingly complex patients, especially those with chronic diseases, such as cirrhosis and inflammatory bowel disease. For example, papers will explore the implementation of specialty medical homes, patient navigators, community-based care services, and involvement of patients in their own care.
- • Quality improvement: Providing high-value care by definition will require clinicians to accurately measure the quality of care provided to patients and use data to guide process improvement. The Road Ahead will continue to serve as an educational resource for clinicians with papers that discuss challenges and opportunities in quality measurement and improvement. Similarly, this section will present data on novel or impactful quality-improvement initiatives.
- • Patient centeredness: Patient experience measures and patient-reported outcomes are becoming increasingly important as meaningful indicators of quality. These measures are designed to ensure that patient perspectives are incorporated into the governance, design, and delivery of health care. The Road Ahead will serve as a dissemination mechanism for sharing best practices in developing, validating, implementing, and tracking patient-reported outcomes.
I consider Dr. Brill and Dr. Allen as mentors who have taught me tremendously about the business of medicine and the importance of physician leadership. I had the opportunity to coauthor several papers and book chapters with them. More recently, I have had the privilege to work closely with them in my role as the Chair of the American Gastroenterological Association Quality Measures Committee. It is an honor to now join their league as the editor for the Road Ahead section of Clinical Gastroenterology and Hepatology. These are indeed big shoes to fill. The section will retain the “Road Ahead” title in an acknowledgement of the continued importance of the issues outlined by Dr Allen. We will build on this theme to focus on not just the destination, but also the bumps in the road, the unexpected curves, the rest areas, beautiful vistas, and the indulgent road food. Hopefully no accidents along the way!
References
1. Allen, J.I. The road ahead. Clin Gastroenterol Hepatol. 2012;10:692-6.
2. Dorn, S.D., Vesy, C.J. Medicare’s revaluation of gastrointestinal endoscopic procedures: implications for academic and community-based practices. Clin Gastroenterol Hepatol. 2017;14:924-8.
3. Dorn, S.D. The road ahead 3.0: changing payments, changing practice. Clin Gastroenterol Hepatol. 2016;14:785-9.
4. Meier, S.K., Shah, N.D., Talwalkar, J.A. Adapting the patient-centered specialty practice model for populations with cirrhosis. Clin Gastroenterol Hepatol. 2016;14:492-6.
5. Mehta, S.J. Bundled payment for gastrointestinal hemorrhage. Clin Gastroenterol Hepatol. 2016;14:1681-4.
6. Weizman, A.V., Mosko, J., Bollegala, N., et al. Quality improvement primer series: launching a quality improvement initiative. Clin Gastroenterol Hepatol. 2017;14:1067-71.
7. Bernstein, M., Hou, J.K., Weizman, A.V., et al. Quality improvement primer series: how to sustain a quality improvement effort. Clin Gastroenterol Hepatol. 2017;14:1371-5.
8. Bollegala, N., Patel, K., Mosko, J.D., et al. Quality improvement primer series: the plan-do-study-act cycle and data display. Clin Gastroenterol Hepatol. 2016;14:1230-3.
9. Adams, M.A. Covert recording by patients of encounters with gastroenterology providers: path to empowerment or breach of trust?. Clin Gastroenterol Hepatol. 2017;15:13-6.
10. Oza, V.M., El-Dika, S., and Adams, M.A. Reaching safe harbor: legal implications of clinical practice guidelines. Clin Gastroenterol Hepatol. 2016;14:172-4.
11. Lin, M., Pappas, S.C., Sellin, J., et al. Curbside consultations: the good, the bad, and the ugly. Clin Gastroenterol Hepatol. 2016;14:2-4.
12. McClellan, M.B., Leavitt, M.O. Competencies and tools to shift payments from volume to value. JAMA. 2016; 316: 1655–1656
13. Donabedian, A. Evaluating the quality of medical care. Milbank Q. 1966;44:166-203.
14. Rosenberg, F.B., Kim, L.S., Ketover, S.R. Challenges facing independent integrated gastroenterology. Clin Gastroenterol Hepatol. 2017;15:335-8.
15. Leiman, D.A., Metz, D.C., Ginsberg, G.G., et al. A novel electronic medical record-based workflow to measure and report colonoscopy quality measures. Clin Gastroenterol Hepatol. 2016;14:333-7.
16. Cross, R.K., Kane, S. Integration of telemedicine into clinical gastroenterology and hepatology Practice. Clin Gastroenterol Hepatol. 2017;15:175-81.
17. Llor, X. Building a cancer genetics and prevention program. Clin Gastroenterol Hepatol. 2016;14:1516-20.
18. Patel, K.K., Cummings, S., Sellin, J., et al. Applying Lean design principles to a gastrointestinal endoscopy program for uninsured patients improves health care utilization. Clin Gastroenterol Hepatol. 2015;13:1556-9.
19. Saini, S.D., Adams, M.A., Brill, J.V., et al. Colorectal cancer screening quality measures: beyond colonoscopy. Clin Gastroenterol Hepatol. 2016;14:644-7.
Dr. Gellad is an associate professor of medicine in the division of gastroenterology at Durham VA Medical Center, Durham, N.C.; and Duke Clinical Research Institute, Durham, N.C. He reports a consulting relationship with Merck & Co. and he is also a cofounder and equity holder in Higgs Boson, LLC. He is funded by Veterans Affairs Health Services Research and Development Career Development Award (CDA 14-158 ).
It is my privilege this month to assume responsibility for the “Practice Management: The Road Ahead” section of Clinical Gastroenterology and Hepatology. I am honored to join an impressive board of editors led by Dr Fasiha Kanwal, and anchored by global leaders in the field of gastroenterology and hepatology. This board of editors promises to continue the high level of excellence that has propelled the journal to its preeminent position among clinical journals. I am confident that the practice management section will uphold that tradition and continue to meet the expectation of our readers. I would like to mark this transition by acknowledging the history of the practice management section of Clinical Gastroenterology and Hepatology and outlining a vision for the future.
The section was introduced in 2010 under the leadership of Dr. Joel V. Brill. The section, titled “Practice Management: Opportunities and Challenges,” aimed to help practices navigate the disparate issues facing the field. Some of these issues included use of capnography in endoscopy, the importance of registries for quality reporting, and the burdens of meaningful use on physician practices. Dr Brill introduced this section in a video in May 2010 (https://www.youtube.com/watch?v=8FMsc2Wl5E8). Dr. Brill’s reference to these “interesting and challenging times” in gastroenterology resonates even more loudly today.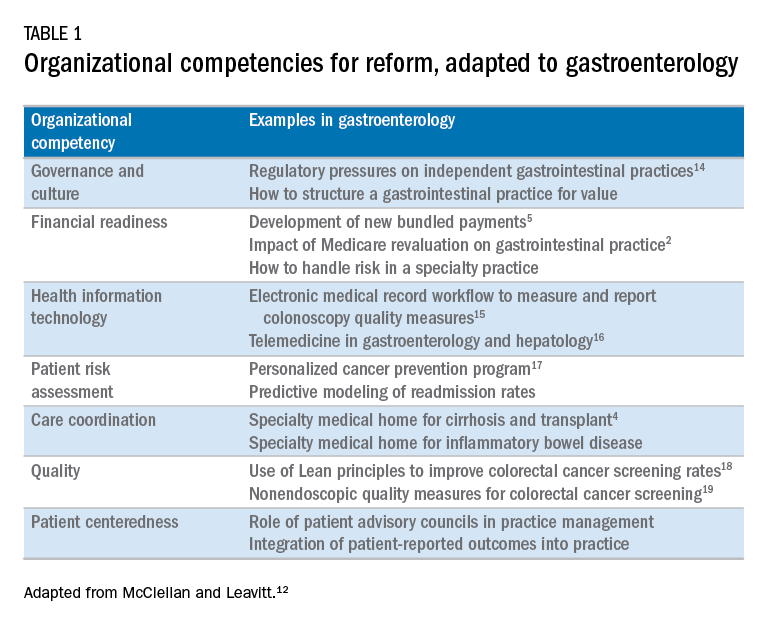
Over the next 5 years, the Road Ahead section will continue and strengthen its focus on the current and emerging issues facing gastroenterology and hepatology practices. I believe that high-value care will continue to be a high priority for patients and payers alike. Early results with payment reform around value have been mixed, in large part because of challenges in health systems and practices developing the competencies required for such reform.12 These competencies include governance and culture, financial readiness, health information technology, patient risk assessment, care coordination, quality, and patient centeredness. I will use this conceptual framework of organizational competencies, and their application in gastroenterology and hepatology, to help curate the Road Ahead section (Table 1). Key themes will include the following:
- • Governance and culture: The structure of health delivery systems, as conceptualized by Donabedian,13 is a key determinant of quality. Structural attributes include regulatory requirements on gastrointestinal practices, such as the rules governing use of anesthesia providers in ambulatory surgical settings; role of allied health professionals in clinical settings; and the impact of financial incentives in driving provider behavior.
- • Financial readiness: Value-based reimbursement, accountable care, medical homes, reference pricing, and physician tiering are some of the new terms in this era of value-based medicine. It is important for practices to assess patient costs longitudinally and manage financial risks. The Road Ahead section will continue to include papers that describe the impact of these reforms on gastroenterology and hepatology practices while providing guidance on implementation of these new models of care. Some examples include papers on the effect of payment policy on specialty practices, the development of a medical home in inflammatory bowel disease, and the physician experience with episode-based payments for colonoscopy.
- • Health information technology: All of the organizational competencies required for reform rely on a robust information technology platform that collects meaningful data and harnesses that data for analytic purposes. These platforms can be enterprise systems deployed by large health delivery systems or smaller, more nimble platforms, created by innovative start-up companies. The Road Ahead will include papers that share best practices in the use of these platforms to provide high-quality and cost-efficient care. In addition, the Road Ahead will continue to explore the use of health information technology to expand the reach of clinicians beyond brick and mortar clinics.
- • Patient risk assessment: Tailoring interventions to high-risk patients is necessary to deploy limited resources in a cost-effective manner. Risk assessment is also needed to more accurately and effectively personalize care for patients with chronic conditions. The Road Ahead will include papers that evaluate risk assessment tools and/or describe real-life implementation of these tools in different contexts.
- • Care coordination: The ability to provide team-based longitudinal care across the continuum of care will be integral to providing high value health care. The Road Ahead will serve as a means to disseminate best practices and innovative methods to care for increasingly complex patients, especially those with chronic diseases, such as cirrhosis and inflammatory bowel disease. For example, papers will explore the implementation of specialty medical homes, patient navigators, community-based care services, and involvement of patients in their own care.
- • Quality improvement: Providing high-value care by definition will require clinicians to accurately measure the quality of care provided to patients and use data to guide process improvement. The Road Ahead will continue to serve as an educational resource for clinicians with papers that discuss challenges and opportunities in quality measurement and improvement. Similarly, this section will present data on novel or impactful quality-improvement initiatives.
- • Patient centeredness: Patient experience measures and patient-reported outcomes are becoming increasingly important as meaningful indicators of quality. These measures are designed to ensure that patient perspectives are incorporated into the governance, design, and delivery of health care. The Road Ahead will serve as a dissemination mechanism for sharing best practices in developing, validating, implementing, and tracking patient-reported outcomes.
I consider Dr. Brill and Dr. Allen as mentors who have taught me tremendously about the business of medicine and the importance of physician leadership. I had the opportunity to coauthor several papers and book chapters with them. More recently, I have had the privilege to work closely with them in my role as the Chair of the American Gastroenterological Association Quality Measures Committee. It is an honor to now join their league as the editor for the Road Ahead section of Clinical Gastroenterology and Hepatology. These are indeed big shoes to fill. The section will retain the “Road Ahead” title in an acknowledgement of the continued importance of the issues outlined by Dr Allen. We will build on this theme to focus on not just the destination, but also the bumps in the road, the unexpected curves, the rest areas, beautiful vistas, and the indulgent road food. Hopefully no accidents along the way!
References
1. Allen, J.I. The road ahead. Clin Gastroenterol Hepatol. 2012;10:692-6.
2. Dorn, S.D., Vesy, C.J. Medicare’s revaluation of gastrointestinal endoscopic procedures: implications for academic and community-based practices. Clin Gastroenterol Hepatol. 2017;14:924-8.
3. Dorn, S.D. The road ahead 3.0: changing payments, changing practice. Clin Gastroenterol Hepatol. 2016;14:785-9.
4. Meier, S.K., Shah, N.D., Talwalkar, J.A. Adapting the patient-centered specialty practice model for populations with cirrhosis. Clin Gastroenterol Hepatol. 2016;14:492-6.
5. Mehta, S.J. Bundled payment for gastrointestinal hemorrhage. Clin Gastroenterol Hepatol. 2016;14:1681-4.
6. Weizman, A.V., Mosko, J., Bollegala, N., et al. Quality improvement primer series: launching a quality improvement initiative. Clin Gastroenterol Hepatol. 2017;14:1067-71.
7. Bernstein, M., Hou, J.K., Weizman, A.V., et al. Quality improvement primer series: how to sustain a quality improvement effort. Clin Gastroenterol Hepatol. 2017;14:1371-5.
8. Bollegala, N., Patel, K., Mosko, J.D., et al. Quality improvement primer series: the plan-do-study-act cycle and data display. Clin Gastroenterol Hepatol. 2016;14:1230-3.
9. Adams, M.A. Covert recording by patients of encounters with gastroenterology providers: path to empowerment or breach of trust?. Clin Gastroenterol Hepatol. 2017;15:13-6.
10. Oza, V.M., El-Dika, S., and Adams, M.A. Reaching safe harbor: legal implications of clinical practice guidelines. Clin Gastroenterol Hepatol. 2016;14:172-4.
11. Lin, M., Pappas, S.C., Sellin, J., et al. Curbside consultations: the good, the bad, and the ugly. Clin Gastroenterol Hepatol. 2016;14:2-4.
12. McClellan, M.B., Leavitt, M.O. Competencies and tools to shift payments from volume to value. JAMA. 2016; 316: 1655–1656
13. Donabedian, A. Evaluating the quality of medical care. Milbank Q. 1966;44:166-203.
14. Rosenberg, F.B., Kim, L.S., Ketover, S.R. Challenges facing independent integrated gastroenterology. Clin Gastroenterol Hepatol. 2017;15:335-8.
15. Leiman, D.A., Metz, D.C., Ginsberg, G.G., et al. A novel electronic medical record-based workflow to measure and report colonoscopy quality measures. Clin Gastroenterol Hepatol. 2016;14:333-7.
16. Cross, R.K., Kane, S. Integration of telemedicine into clinical gastroenterology and hepatology Practice. Clin Gastroenterol Hepatol. 2017;15:175-81.
17. Llor, X. Building a cancer genetics and prevention program. Clin Gastroenterol Hepatol. 2016;14:1516-20.
18. Patel, K.K., Cummings, S., Sellin, J., et al. Applying Lean design principles to a gastrointestinal endoscopy program for uninsured patients improves health care utilization. Clin Gastroenterol Hepatol. 2015;13:1556-9.
19. Saini, S.D., Adams, M.A., Brill, J.V., et al. Colorectal cancer screening quality measures: beyond colonoscopy. Clin Gastroenterol Hepatol. 2016;14:644-7.
Dr. Gellad is an associate professor of medicine in the division of gastroenterology at Durham VA Medical Center, Durham, N.C.; and Duke Clinical Research Institute, Durham, N.C. He reports a consulting relationship with Merck & Co. and he is also a cofounder and equity holder in Higgs Boson, LLC. He is funded by Veterans Affairs Health Services Research and Development Career Development Award (CDA 14-158 ).
It is my privilege this month to assume responsibility for the “Practice Management: The Road Ahead” section of Clinical Gastroenterology and Hepatology. I am honored to join an impressive board of editors led by Dr Fasiha Kanwal, and anchored by global leaders in the field of gastroenterology and hepatology. This board of editors promises to continue the high level of excellence that has propelled the journal to its preeminent position among clinical journals. I am confident that the practice management section will uphold that tradition and continue to meet the expectation of our readers. I would like to mark this transition by acknowledging the history of the practice management section of Clinical Gastroenterology and Hepatology and outlining a vision for the future.
The section was introduced in 2010 under the leadership of Dr. Joel V. Brill. The section, titled “Practice Management: Opportunities and Challenges,” aimed to help practices navigate the disparate issues facing the field. Some of these issues included use of capnography in endoscopy, the importance of registries for quality reporting, and the burdens of meaningful use on physician practices. Dr Brill introduced this section in a video in May 2010 (https://www.youtube.com/watch?v=8FMsc2Wl5E8). Dr. Brill’s reference to these “interesting and challenging times” in gastroenterology resonates even more loudly today.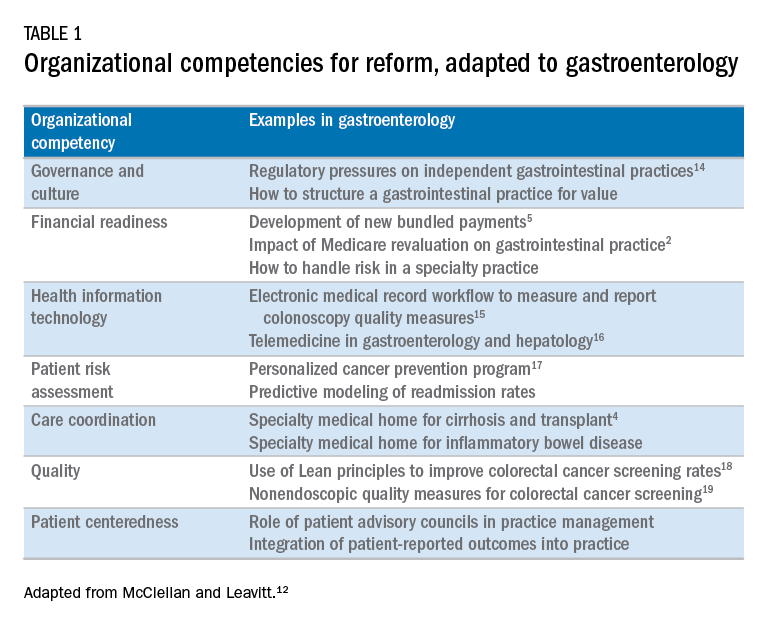
Over the next 5 years, the Road Ahead section will continue and strengthen its focus on the current and emerging issues facing gastroenterology and hepatology practices. I believe that high-value care will continue to be a high priority for patients and payers alike. Early results with payment reform around value have been mixed, in large part because of challenges in health systems and practices developing the competencies required for such reform.12 These competencies include governance and culture, financial readiness, health information technology, patient risk assessment, care coordination, quality, and patient centeredness. I will use this conceptual framework of organizational competencies, and their application in gastroenterology and hepatology, to help curate the Road Ahead section (Table 1). Key themes will include the following:
- • Governance and culture: The structure of health delivery systems, as conceptualized by Donabedian,13 is a key determinant of quality. Structural attributes include regulatory requirements on gastrointestinal practices, such as the rules governing use of anesthesia providers in ambulatory surgical settings; role of allied health professionals in clinical settings; and the impact of financial incentives in driving provider behavior.
- • Financial readiness: Value-based reimbursement, accountable care, medical homes, reference pricing, and physician tiering are some of the new terms in this era of value-based medicine. It is important for practices to assess patient costs longitudinally and manage financial risks. The Road Ahead section will continue to include papers that describe the impact of these reforms on gastroenterology and hepatology practices while providing guidance on implementation of these new models of care. Some examples include papers on the effect of payment policy on specialty practices, the development of a medical home in inflammatory bowel disease, and the physician experience with episode-based payments for colonoscopy.
- • Health information technology: All of the organizational competencies required for reform rely on a robust information technology platform that collects meaningful data and harnesses that data for analytic purposes. These platforms can be enterprise systems deployed by large health delivery systems or smaller, more nimble platforms, created by innovative start-up companies. The Road Ahead will include papers that share best practices in the use of these platforms to provide high-quality and cost-efficient care. In addition, the Road Ahead will continue to explore the use of health information technology to expand the reach of clinicians beyond brick and mortar clinics.
- • Patient risk assessment: Tailoring interventions to high-risk patients is necessary to deploy limited resources in a cost-effective manner. Risk assessment is also needed to more accurately and effectively personalize care for patients with chronic conditions. The Road Ahead will include papers that evaluate risk assessment tools and/or describe real-life implementation of these tools in different contexts.
- • Care coordination: The ability to provide team-based longitudinal care across the continuum of care will be integral to providing high value health care. The Road Ahead will serve as a means to disseminate best practices and innovative methods to care for increasingly complex patients, especially those with chronic diseases, such as cirrhosis and inflammatory bowel disease. For example, papers will explore the implementation of specialty medical homes, patient navigators, community-based care services, and involvement of patients in their own care.
- • Quality improvement: Providing high-value care by definition will require clinicians to accurately measure the quality of care provided to patients and use data to guide process improvement. The Road Ahead will continue to serve as an educational resource for clinicians with papers that discuss challenges and opportunities in quality measurement and improvement. Similarly, this section will present data on novel or impactful quality-improvement initiatives.
- • Patient centeredness: Patient experience measures and patient-reported outcomes are becoming increasingly important as meaningful indicators of quality. These measures are designed to ensure that patient perspectives are incorporated into the governance, design, and delivery of health care. The Road Ahead will serve as a dissemination mechanism for sharing best practices in developing, validating, implementing, and tracking patient-reported outcomes.
I consider Dr. Brill and Dr. Allen as mentors who have taught me tremendously about the business of medicine and the importance of physician leadership. I had the opportunity to coauthor several papers and book chapters with them. More recently, I have had the privilege to work closely with them in my role as the Chair of the American Gastroenterological Association Quality Measures Committee. It is an honor to now join their league as the editor for the Road Ahead section of Clinical Gastroenterology and Hepatology. These are indeed big shoes to fill. The section will retain the “Road Ahead” title in an acknowledgement of the continued importance of the issues outlined by Dr Allen. We will build on this theme to focus on not just the destination, but also the bumps in the road, the unexpected curves, the rest areas, beautiful vistas, and the indulgent road food. Hopefully no accidents along the way!
References
1. Allen, J.I. The road ahead. Clin Gastroenterol Hepatol. 2012;10:692-6.
2. Dorn, S.D., Vesy, C.J. Medicare’s revaluation of gastrointestinal endoscopic procedures: implications for academic and community-based practices. Clin Gastroenterol Hepatol. 2017;14:924-8.
3. Dorn, S.D. The road ahead 3.0: changing payments, changing practice. Clin Gastroenterol Hepatol. 2016;14:785-9.
4. Meier, S.K., Shah, N.D., Talwalkar, J.A. Adapting the patient-centered specialty practice model for populations with cirrhosis. Clin Gastroenterol Hepatol. 2016;14:492-6.
5. Mehta, S.J. Bundled payment for gastrointestinal hemorrhage. Clin Gastroenterol Hepatol. 2016;14:1681-4.
6. Weizman, A.V., Mosko, J., Bollegala, N., et al. Quality improvement primer series: launching a quality improvement initiative. Clin Gastroenterol Hepatol. 2017;14:1067-71.
7. Bernstein, M., Hou, J.K., Weizman, A.V., et al. Quality improvement primer series: how to sustain a quality improvement effort. Clin Gastroenterol Hepatol. 2017;14:1371-5.
8. Bollegala, N., Patel, K., Mosko, J.D., et al. Quality improvement primer series: the plan-do-study-act cycle and data display. Clin Gastroenterol Hepatol. 2016;14:1230-3.
9. Adams, M.A. Covert recording by patients of encounters with gastroenterology providers: path to empowerment or breach of trust?. Clin Gastroenterol Hepatol. 2017;15:13-6.
10. Oza, V.M., El-Dika, S., and Adams, M.A. Reaching safe harbor: legal implications of clinical practice guidelines. Clin Gastroenterol Hepatol. 2016;14:172-4.
11. Lin, M., Pappas, S.C., Sellin, J., et al. Curbside consultations: the good, the bad, and the ugly. Clin Gastroenterol Hepatol. 2016;14:2-4.
12. McClellan, M.B., Leavitt, M.O. Competencies and tools to shift payments from volume to value. JAMA. 2016; 316: 1655–1656
13. Donabedian, A. Evaluating the quality of medical care. Milbank Q. 1966;44:166-203.
14. Rosenberg, F.B., Kim, L.S., Ketover, S.R. Challenges facing independent integrated gastroenterology. Clin Gastroenterol Hepatol. 2017;15:335-8.
15. Leiman, D.A., Metz, D.C., Ginsberg, G.G., et al. A novel electronic medical record-based workflow to measure and report colonoscopy quality measures. Clin Gastroenterol Hepatol. 2016;14:333-7.
16. Cross, R.K., Kane, S. Integration of telemedicine into clinical gastroenterology and hepatology Practice. Clin Gastroenterol Hepatol. 2017;15:175-81.
17. Llor, X. Building a cancer genetics and prevention program. Clin Gastroenterol Hepatol. 2016;14:1516-20.
18. Patel, K.K., Cummings, S., Sellin, J., et al. Applying Lean design principles to a gastrointestinal endoscopy program for uninsured patients improves health care utilization. Clin Gastroenterol Hepatol. 2015;13:1556-9.
19. Saini, S.D., Adams, M.A., Brill, J.V., et al. Colorectal cancer screening quality measures: beyond colonoscopy. Clin Gastroenterol Hepatol. 2016;14:644-7.
Dr. Gellad is an associate professor of medicine in the division of gastroenterology at Durham VA Medical Center, Durham, N.C.; and Duke Clinical Research Institute, Durham, N.C. He reports a consulting relationship with Merck & Co. and he is also a cofounder and equity holder in Higgs Boson, LLC. He is funded by Veterans Affairs Health Services Research and Development Career Development Award (CDA 14-158 ).
