STOP-Bang score and probability of OSA
In both sleep clinic patients (Fig 1; Panel A) and surgical patients (Fig 1; Panel B), the probability of moderate-to-severe OSA or severe OSA increased a s the STOP-Bang score increased from 3 to 7/8. With higher scores, there is a more profound increase in the probability of severe OSA, compared with moderate OSA (Chung et al. Br J Anaesth. 2012;108[5]:768).
Alternative models for scoring the STOP-Bang Questionnaire
The individual items on the Questionnaire do not share an equal predictive weight for OSA. In the “Bang” components, body mass index greater than 35 kg/m2, neck circumference greater than 40 cm, and male gender are more predictive than age greater than 50 years. The predictive performance of the specific combinations of items has been explored. Compared with the specificity of 31% for detecting moderate to severe OSA, specific combinations significantly improve the specificity to detect any OSA (AHI greater than 5), moderate to severe OSA (AHI greater than 15), and severe OSA (AHI greater than 30) at the expense of sensitivity. The specificity to detect moderate to severe OSA increases to 85% for a STOP score greater than or equal to 2 + BMI greater than 35 kg/m2; to 79% for a STOP score greater than or equal to 2 + neck circumference > greater than 40 cm (16 in); and to 77% for a STOP score greater than or equal to 2 + male, respectively. These combinations can assist in accurately identifying more patients with moderate to severe OSA (Chung et al. J Clin Sleep Med. 2014;10[9]:951).
The STOP-Bang Questionnaire and serum bicarbonate
Serum bicarbonate (HCO3–) is significantly correlated to AHI, and the addition of serum HCO3– greater than or equal to 28 mmol/L to a STOP-Bang score greater than or equal to 3 improves the specificity to predict moderate-severe OSA but decreases its sensitivity (Chung et al. Chest. 2013;143[5]:1284). For a STOP-Bang score of greater than or equal to 3 + HCO3– greater than or equal to 28 mmol/L), the specificity for detecting moderate to severe OSA increases from 30% to 82%, and from 28% to 80% for detecting severe OSA, respectively.
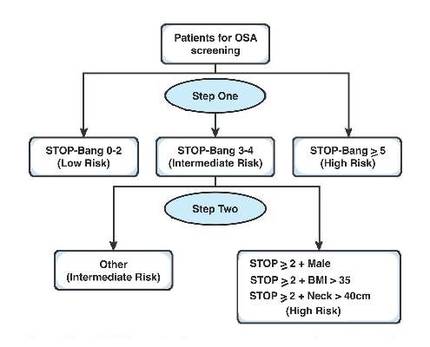
A two-step strategy for using STOP-Bang Questionnaire
A two-step algorithm using the STOP-Bang Questionnaire identifies patients effectively with a high probability of moderate to severe sleep apnea (Fig 2) (Chung et al. Chest. 2016;149[3]:631). The first step is to check the STOP-Bang score. If a patient scores 0-2 on the STOP-Bang Questionnaire, he or she is unlikely to have moderate to severe OSA. Conversely, a patient with a STOP-Bang score of 5-8 has a high probability of moderate to severe OSA.
The second step is for the patients with STOP-Bang scores of 3 or 4. These patients can be further classified as having a higher risk for moderate to severe OSA if one of the following conditions is met: (1) a STOP score greater than or equal to 2 + BMI greater than 35 kg/m2; (2) a STOP score greater than or equal to 2 + male gender; (3) a STOP score greater than or equal to 2 + neck circumference greater than 40 cm (16 in); or (4) a STOP-Bang score greater than or equal to 3 + serum HCO3– greater than or equal to 28 mmol/L.
The STOP-Bang Questionnaire and perioperative complications
The STOP-Bang Questionnaire not only identifies the high-risk patients with OSA but also may have a strong association toward predicting perioperative complications (Vasu et al. Arch Otolaryngol Head Neck Surg. 2010;136[10]:1020). The important step of screening patients with OSA using the STOP-Bang Questionnaire may create an awareness among the perioperative team resulting in decreased complications (Veenstra et al. Crit Care Nurs Clin N Am. 2014;26[4]:499).
The Joint Commission’s Division of Healthcare Improvement has raised strong concerns regarding the lack of training for health-care professionals to recognize OSA. A recent guideline published by the Society of Anesthesia and Sleep Medicine recommends using a screening tool to identify high-risk patients with OSA (Chung et al. Anesthesia Analgesia. 2016;June 1: Epub ahead of print).
There is preliminary evidence that patients with diagnosed OSA and a CPAP prescription had significantly reduced postoperative cardiovascular complications (cardiac arrest and shock) by more than 50% vs patients with undiagnosed OSA (Mutter et al. Anesthesiology. 2014;121[4]:707).
Conclusion
The STOP-Bang Questionnaire is a simple, practical, and flexible screening tool to identify the high-risk OSA patients. More information is available at www.stopbang.ca.
Dr. Chung is with the department of anesthesia, Toronto Western Hospital – University Health Network, University of Toronto, ON, Canada; Dr. Nagappa is with the department of anesthesia & perioperative medicine, London Health Sciences Centre and St. Joseph Health Care London, Western University, London, ON, Canada.